Abstract
Background
Knowledge about the causes and outcomes of pediatric cardiac arrest in the emergency department is limited. The aim of our study was to evaluate the characteristics and outcomes of pediatric cardiac arrest in the emergency department (EDCA) and inpatient (IPCA) settings in the United States using a large database designed to provide nationwide estimates.
Methods
We performed a retrospective cohort study using the Nationwide Emergency Department Sample (NEDS), a database that includes both ED and inpatient encounters. The NEDS was analyzed for episodes of cardiac arrest between 2016-2018 in patients aged ≤18 years. Patients with cardiac arrest were identified using the International Classification of Diseases, 10th revision codes.
Results
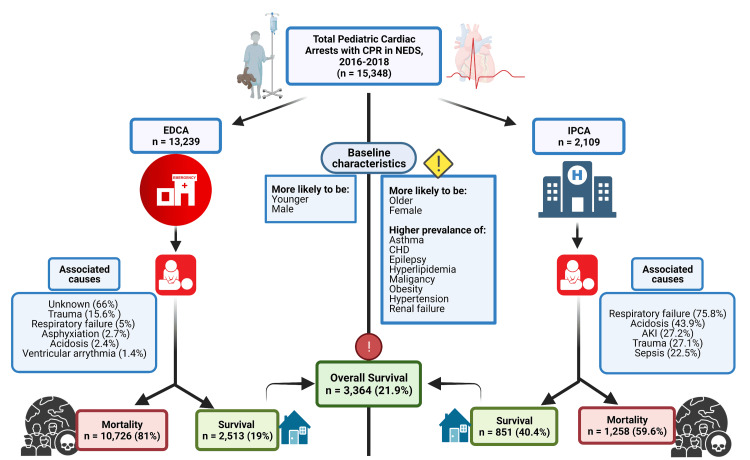
A total of 15,348 pediatric cardiac arrest events with cardiopulmonary resuscitation were recorded, of which 13,239 had EDCA and 2,109 had IPCA. A lower survival rate of 19% was observed for EDCA compared to 40.4% for IPCA. While more than half of the EDCA events had no associated diagnoses, trauma (15.6%), respiratory failure (5%), asphyxiation (2.7%), acidosis (2.4%), and ventricular arrhythmia (1.4%) were associated with the remaining events. In comparison, the most frequently associated diagnoses for IPCA were respiratory failure (75.8%), acidosis (43.9%), acute kidney injury (27.2%), trauma (27.1%), and sepsis (22.5%).
Conclusions
Survival rates for EDCA were less than half of that for IPCA. The low survival rates along with the distinctive characteristics of EDCA events suggest the need for further research in this area to identify remediable factors and improve survival.
Keywords: outcomes, inpatient, emergency department, survival rate, nationwide emergency database sample, cardiopulmonary resuscitation, pediatric cardiac arrest
Introduction
It is estimated that more than 20,000 children have a cardiac arrest (CA) annually in the United States (US) [1-4]. Pediatric CA requiring resuscitation with chest compression and/or defibrillation can be classified as a pulseless event or as a non-pulseless event such as bradycardia leading to poor perfusion [5]. Approximately 15,000 children receive cardiopulmonary resuscitation (CPR) for in-hospital cardiac arrest (IHCA) annually [1]. In 2015, the incidence of IHCA in children was approximately 1.89 events per 1000 inpatient days and 12.66 events per 1000 admissions [4]. The overall incidence rate for out-of-hospital cardiac arrest (OHCA) is 8.3 per 100,000 person-years [6]. In comparison to OHCA, pediatric IHCA has higher rates of survival [6-8].
There are limited national-level studies regarding the outcomes of emergency department cardiac arrest (EDCA) in comparison to IHCA for the pediatric population within the US. IHCA events in pediatric patients differ substantially from adults [7,9,10]. The majority of pediatric IHCA (85-90%) occur in monitored settings, often in the backdrop of progressive shock or respiratory failure [4,7,11-13]. While outcomes for pediatric IHCA improved during the first decade of the 21st century, the survival rates have plateaued since 2010 [4,5,14]. The overall survival rates for pediatric IHCA were 41.1% compared to 11.4% for OHCA [4,5,14]. Despite higher survival rates of IHCA, more national-level studies are needed to further assess the clinical characteristics and outcomes for CA at different locations within the hospital [14,15]. Worldwide, studies of pediatric CA in the emergency department (ED) have reported survival rates between 12.8 to 33.8% [16-19].
Previously, studies have evaluated the survival of pediatric patients as IHCA and OHCA; however, no studies have analogized the clinical outcomes of inpatient cardiac arrest (IPCA) and EDCA. Assessing the prevalence, predictors, and causes of pediatric CA based on location within a hospital would allow for a better understanding of this modifiable disease process to help improve outcomes and healthcare policy. Thus, we evaluated the characteristics and survival rates for pediatric cardiac arrest in the ED and inpatient settings from the Nationwide Emergency Department Sample (NEDS) database.
Materials and methods
Study population and inclusion criteria
This is an observational cohort study of patients with cardiac arrest in the Nationwide Emergency Department Sample (NEDS) database between 2016-2018. The NEDS is the largest all-payer ED database that is publicly available in the United States and has in-hospital encounters, which include ED encounters and inpatient encounters. Since the database constitutes approximately 20% of the population, a weighted analysis is recommended to generalize it for the entire population of the US, with unweighted estimates considered invalid [20]. Thus, all NEDS estimates were calculated using national weighted values and accounted for sample weighting. Using a stratified, random sampling design, a sample of hospital-owned emergency departments from the US participating in both the State Inpatient Databases (SID) and the State Emergency Department Databases (SEDD) was selected. One hundred percent of the emergency department visits and inpatient encounters from the selected emergency departments were retained for the study dataset. The SEDD captures information on ED visits that do not result in an admission, while the SID contains information on patients initially seen in the emergency and then admitted to the hospital [20].
Hospitals were included in the NEDS sample based on geographic region, teaching status (non-teaching or teaching), location (urban or rural), ownership (public, private for-profit, private not-for-profit), and trauma center designation. A total of 990 emergency departments were included in the NEDS database. From each selected emergency department, all visits were included, which amounted to more than 33 million unweighted visits each year. Weighted, the database estimates more than 140 million ED visits and more than 20 million inpatient admissions per year. The institutional review board declared this study exempt from review. However, it was performed according to the ethical criteria set up by Healthcare Cost and Utilization Project (HCUP) [20].
Study definitions
Cardiac arrest was defined by International Classification of Diseases-10 (ICD-10) codes of I46.2, I46.8, I46.9, I97.121, and I97.11. We excluded patients older than 18 years. We divided patients into EDCA and IPCA based on the site where CPR was performed. Patients who had a CA in the emergency department (EDCA) were identified with "current procedural terminology codes (CPT)" for cardiopulmonary resuscitation as ED procedures are added to the database as CPT codes. Patients who had a CA in the inpatient (IPCA) setting were identified using "procedure codes (PR)" for CPR as the inpatient sample does not have CPT codes (supplemental file, section II). This method has been previously validated and published in the literature [21]. Patient demographics, payer information, and comorbidities were obtained from the database. The information about diagnoses associated with CA was defined by the ICD-10 codes using the links provided in the appendix.
Patient and hospital characteristics
Baseline patient demographic characteristics (age, sex, insurance payer, hospital location) were extracted using database variables. Diagnostic codes were used to identify comorbidities of hypertension, congenital heart disease, malignancy, diabetes mellitus, hyperlipidemia, obesity, asthma, epilepsy, sickle cell disease, and renal failure. Since HCUP databases cannot evaluate causation and can only check for an association, we extracted data for variables that have been related as causes and contributing factors by previously published studies, which included asphyxiation and strangulation, cardiac surgery, ventricular tachycardia/fibrillation, shock, acidosis, sepsis, trauma, respiratory failure, hyperkalemia, cerebral edema, pneumonia, cardiomyopathy, hypothermia, bronchiolitis, pneumothorax, acute kidney injury, and pulmonary embolism [7,19,22,23].
Outcomes
The primary outcome of the study was survival to discharge. We also studied the characteristics associated with CA at different locations.
Statistical methods
Categorical variables were expressed as weighted values and percentages. Continuous variables were expressed as mean ± standard deviation if the variable was not skewed; otherwise, it was expressed as a median with 25th and 75th percentiles (interquartile range). Descriptive statistics were performed for demographics and comorbidities, which were stratified by the type of CA (IPCA and EDCA). We used survey statistics to calculate Pearson's chi-square test for categorical variables and the t-test for the continuous variables. We also evaluated the associated diagnoses and provided weighted values along with their percentages for the subgroups of patients that had CA in the emergency department and inpatient setting. The proportions were compared using Pearson's chi-square test. All analyses were weighted analyses. Statistical analysis was performed using STATA version 16.1 (College Station, USA). Using STATA 16.1, we confirmed that there was no overlap in our cohort of patient encounters for those who had a cardiac arrest in the emergency department and those with cardiac arrest in the inpatient setting. All p-values were two-sided, with a significance threshold of p<0.05.
Results
A total of 34,763 pediatric CAs were recorded in the NEDS database for the years 2016-2018. Of the 15,348 patients (mean age 4.8±6 years, 39.9% females) who had CPR, 13,239 had EDCA, and 2,109 had IPCA (Figure 1).
Figure 1. Graphical abstract of the analysis.
AKI - acute kidney injury; CHD - congenital heart disease; CPR - cardiopulmonary resuscitation; EDCA - emergency department cardiac arrest; IPCA - inpatient cardiac arrest; NEDS - Nationwide Emergency Department Sample
Image created with BioRender.com.
The mean age of patients with EDCA was 4.5±5.9 years, compared to 6.2±6.2 years for IPCA (p<0.001). The proportion of males was 60.8% and 56.6% in the ED and inpatient groups (p=0.044), respectively. The baseline characteristics for both groups are compared in Table 1. The proportion of patients with comorbidities of asthma, congenital heart disease, epilepsy, hyperlipidemia, obesity, hypertension, malignancy, and renal failure were all more common in the group with IPCA. Medicaid was the predominant payer among all CA patients.
Table 1. Baseline characteristics of patients with EDCA and IPCA.
EDCA - emergency department cardiac arrest; IPCA - inpatient cardiac arrest
| Variables, n (%) | EDCA (n=13,239) | IPCA (n=2,109) | p-value |
| Primary payer | |||
| Medicare | 392 (2.9%) | 79 (3.8%) | <0.001 |
| Medicaid | 7,608 (57.5%) | 1,253 (59.4%) | <0.001 |
| Private insurance | 3,270 (24.7%) | 699 (33.1%) | <0.001 |
| Self-pay | 1,969 (14.9%) | 78 (3.7%) | <0.001 |
| Hospital characteristics | |||
| Teaching hospital | 7,933 (59.9%) | 2,053 (97.4%) | <0.001 |
| Urban location | 11,969 (90.4%) | 1,907 (90.5%) | 0.986 |
| Pre-existing conditions | |||
| Asthma | 324 (2.5%) | 215 (10.2%) | <0.001 |
| Congenital heart disease | 289 (2.18%) | 293 (13.9%) | <0.001 |
| Diabetes mellitus | 57 (0.4%) | 30 (1.4%) | 0.077 |
| Epilepsy | 192 (1.5%) | 138 (6.5%) | <0.001 |
| Hyperlipidemia | 10 (0.06%) | 18 (0.8%) | 0.049 |
| Hypertension | 58 (0.4%) | 231 (11%) | <0.001 |
| Malignancy | 23 (0.17%) | 56 (2.7%) | 0.002 |
| Obesity | 11 (0.06%) | 19 (0.9%) | 0.043 |
| Renal failure | 32 (0.24%) | 34 (1.6%) | 0.032 |
| Sickle cell disease | 49 (0.37%) | 20 (0.9%) | 0.207 |
Survival
The overall survival to discharge rate for patients with CA undergoing CPR was 21.9% (n=3,364) during the study period. Of the patients who had EDCA, 2,513 (19%) survived post-CPR to discharge. Among IPCA patients, 851 (40.4%) survived post-CPR to discharge.
Characteristics associated with cardiac arrest
Eight thousand eight hundred and four patients with EDCA had no evidently associated diagnosis. Among those EDCA patients with an associated diagnosis, trauma was the predominant diagnosis, accounting for 15.6% of patients. Others were respiratory failure (5.01%), asphyxiation and strangulation (2.7%), acidosis (2.4%), ventricular arrhythmia (1.4%), hyperkalemia (1.4%), hypothermia (1.2%) and sepsis (1.1%). In contrast, the most frequently associated factors among IPCA were respiratory failure (75.8%), acidosis (43.9%), acute kidney injury (27.2%), trauma (27.1%), sepsis (22.5%), pneumonia (20.7%), shock (19%), cerebral edema (13.6%), ventricular tachycardia/fibrillation (12.9%), and hyperkalemia (11.1%). Conditions associated with EDCA and IPCA are presented in Table 2.
Table 2. Conditions associated with EDCA and IPCA.
Since cardiac arrest can be multifactorial, the percentages do not add up.
EDCA - emergency department cardiac arrest; IPCA - inpatient cardiac arrest
| Variables, n (%) | EDCA (n=13,239) | IPCA (n=2,109) | p-value |
| Acidosis | 320 (2.4%) | 926 (43.9%) | <0.001 |
| Acute kidney injury | 28 (0.21%) | 573 (27.2%) | <0.001 |
| Asphyxiation and strangulation | 357 (2.7%) | 49 (2.3%) | 0.606 |
| Bronchiolitis | 17 (0.13%) | 201 (9.5%) | <0.001 |
| Cardiac surgery | 11 (0.07%) | 52 (2.5%) | <0.001 |
| Cardiomyopathy | 22 (0.17%) | 64 (3%) | <0.001 |
| Cerebral edema | 31 (0.23%) | 287 (13.6%) | <0.001 |
| Hyperkalemia | 181 (1.4%) | 233 (11.1%) | <0.001 |
| Hypothermia | 157 (1.2%) | 43 (2%) | 0.129 |
| Pneumonia | 106 (0.8%) | 436 (20.7%) | <0.001 |
| Pneumothorax | 104 (0.8%) | 138 (6.5%) | <0.001 |
| Pulmonary embolism | 10 (0.06%) | 131 (6.2%) | <0.001 |
| Respiratory failure | 663 (5.01%) | 1,598 (75.8%) | <0.001 |
| Sepsis | 140 (1.1%) | 474 (22.5%) | <0.001 |
| Shock | 21 (0.2%) | 393 (19%) | <0.001 |
| Trauma | 2,059 (15.6%) | 571 (27.1%) | <0.001 |
| Ventricular tachycardia/fibrillation | 186 (1.4%) | 272 (12.9%) | <0.001 |
Discussion
This study, based on our literature review, is the first study to have evaluated the different characteristics and survival rates of pediatric patients who had cardiac arrest based on their location in the ED or inpatient setting. While previous studies have looked at attributes of OHCA and IHCA, our study explored attributes of pediatric EDCA and IPCA. The most salient features of our study were: (a) survival was lower for patients with EDCA, and (b) while more than half of the patients with EDCA did not have another primary diagnosis, trauma was the most frequently observed associated diagnosis in the remaining patients. In contrast, patients with IPCA were commonly observed to have disorders of respiratory failure, acidosis, acute kidney injury, sepsis, and shock, in addition to trauma.
Survival
We observed an overall survival to discharge rate of 21.9%. There was a significant difference in rates of survival based on location, with pediatric IPCA patients (40.4%) having more than twice the survival rates compared to those with EDCA (19%). Since no previous studies have looked at survival rates for pediatric CA based on their location like our study, it is difficult to make precise comparisons.
The rates of survival to discharge for pediatric patients with CA in the inpatient setting (40.4%) agree closely with findings reported in the 2020 update from the American Heart Association (AHA) for pediatric IHCA (41.1%) [4]. Other studies have also looked at the trends in the survival rates for pediatric CA. Girotra et al., in their 2013 study, using the Get With The Guidelines-Resuscitation (GWTG-R) registry, described survival rates of 14% and 39% for pediatric IHCA in 2000 and 2009, respectively [14]. A more recent study utilizing the same GWTG-R registry reported rates for survival to discharge of 38% and 66% in 2018 for pediatric IHCA patients with pulseless and non-pulseless CA, respectively [5]. Virani et al., in their 2020 report for the AHA, delineated 41.1 % survival rates for children with IHCA [4]. Although the survival rates have increased by 0.67% per year on average between 2000 to 2018, there has been a plateau in the increase of survival rates since 2010, hence the need for continued focus, research, and improvement in this area [5]. Skellett et al. reported an overall survival to discharge rate of 54.2% after pediatric in-hospital cardiac arrest in the United Kingdom from their seven-year review of the National Cardiac Arrest Audit (NCAA) database [24].
There is a paucity of literature on rates of survival for pediatric patients with EDCA. Michelson et al., in a retrospective study using the NEDS, established a survival rate of 21.7% for pediatric cardiac arrest in the ED for the years 2009-2014. For non-traumatic CAs, they reported survival rates of 33.8% in the pediatric ED versus 18.9% in the general ED. In their study, the survival rates for traumatic OHCA were 31.7% and 26.1% in pediatric and general EDs, respectively [19]. Our findings of a survival rate of 19% in patients with EDCA are like the overall rate in the study by Michelson et al. (21.7%), where notably, the same NEDS database was utilized [19]. Donoghue et al., utilizing the GWTG-R registry, reported a survival to discharge rate of 20% for pediatric patients with CPR initiated in the ED [17]. Another study reported survival rates of 12.8% in children with CA between 2008-2012 using the Korean ED-based clinical registry [16]. A single-center, retrospective study from Turkey observed a survival rate of 18% for cardiac arrest in a tertiary-center pediatric ED over a period of three years [18].
The higher survival rates for IPCA compared to EDCA could stem from a myriad of reasons, including early recognition in a monitored setting, greater availability of experienced staff, better preparedness, and known etiology of CA. The disparate nature of EDCA, where some OHCA events may have been included in the analysis, could also contribute to lower survival rates for this location in our study.
Characteristics associated with cardiac arrest
The causes for cardiac arrest in pediatrics are numerous and include respiratory, traumatic, infectious, and cardiac conditions. Pertinently, pediatric CA is less likely to be a primary cardiac event in comparison to adults [25]. In our study, trauma was recorded as the most associated factor for EDCA events, reported in 15.6% of patients. Michelson et al. reported trauma to be associated in around 25% (24.9% to 28.6%) of patients with EDCA [19]. Other characteristics associated with this group included respiratory failure, asphyxiation and strangulation, and acidosis. In contrast, pediatric IHCA is often caused by progressive respiratory insufficiency and/or shock [7,11,12]. The most frequently associated characteristics with IPCA in our study were also respiratory failure, acidosis, acute kidney injury, trauma, sepsis, and shock.
Acidosis has been frequently observed in patients with CA and is likely due to a combination of metabolic abnormalities, including increased lactate levels, unmeasured anions, and acute kidney injury, as well as respiratory insufficiency [26]. Acidosis is an important contributing factor and complication of CA, as acidemia impairs myocardial function and diminishes myocardial response to catecholamines [23,27]. In addition, acidosis and sepsis are directly related to each other and worsen the mortality outcomes [28]. The high rates of sepsis and acidosis observed in our study suggest that clinicians should remain vigilant for early identification and proper management of these likely reversible contributing factors of CA.
Interestingly, the EDCA patients had fewer comorbidities than IPCA but higher mortality rates. Since almost one-sixth of EDCA patients had trauma as the associated diagnosis, they could potentially have been previously healthy. This could also suggest that the patients with more comorbidities get triaged quicker to perform a lifesaving intervention, or it could reflect the under-evaluation of patients with EDCA. This emphasizes the need to further evaluate the other predictors of EDCA in pediatric patients.
Important strengths of this study are the large number of cases on which estimates are based and its national representativeness. However, the study also has certain limitations. Since the study is a retrospective, observational study, inference regarding causation should be made with caution. The NEDS database can show association but can not imply causation or provide temporal event data. Additionally, the NEDS registry is unable to definitively differentiate in-ED cardiac arrests from OHCA and only includes information for inpatients that are admitted through the ED. Also, we relied on reported ICD-10 codes to identify diagnoses to perform our analysis, which may not accurately reflect the true cause of cardiac arrest. The NEDS is an administrative database that could be subject to inaccurate coding and underreporting of comorbid diagnoses. There is an absence of valuable information related to patients' physical examination, electrocardiography, echocardiography, medications, laboratory results, radiologic findings, and long-term complications. Also, since the NEDS contains encounter-level records, a single patient may be represented multiple times in the database for different ED visits. However, the NEDS and the codes used in this study have been used in multiple clinical studies and can be considered a reliable database, given the large cohorts analyzed.
Conclusions
In a nationally representative cohort from the NEDS database, over one-fifth of pediatric cardiac arrest patients undergoing CPR survived to hospital discharge. The survival for EDCA events was less than half of the rates for IPCA events. While trauma was a notably associated diagnosis in both settings, respiratory failure, acidosis, acute kidney injury, and sepsis were also commonly associated factors for the inpatient location. The low survival rates for EDCA suggest the need for further research to identify remediable factors and potentially improve survival.
Acknowledgments
Drs. Mir and Shafi contributed equally to this work.
Appendices
Supplemental information for identification of ICD codes, and procedure codes
Section I
Codes used for generating cardiac arrest files. All codes were ICD-10 codes.
I46.2, I46.8, I46.9, I97.121, and I97.11.
Section II
1) CPT codes used for procedures in the emergency department.
Procedure codes for cardiopulmonary resuscitation in the emergency department. (cpt1-cpt15)
92950
2) PR codes used for procedures in the in-patient setting.
Procedure codes for cardiopulmonary resuscitation for in-hospital cardiac arrest. (i10_pr_ip1-i10_pr_ip15)
5A12012, 02QA0ZZ
Codes used for the comorbidities were obtained from the following websites:
2) https://www.icd10data.com/ICD10PCS/Codes
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Annual incidence of adult and pediatric in-hospital cardiac arrest in the United States. Holmberg MJ, Ross CE, Fitzmaurice G, et al. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6758564/ Circ Cardiovasc Qual Outcomes. 2019;12:0. [PMC free article] [PubMed] [Google Scholar]
- 2.Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, Berg RA. Circulation. 2009;119:1484–1491. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prevalence and outcomes of pediatric in-hospital cardiopulmonary resuscitation in the United States: an analysis of the Kids' Inpatient Database*. Knudson JD, Neish SR, Cabrera AG, et al. Crit Care Med. 2012;40:2940–2944. doi: 10.1097/CCM.0b013e31825feb3f. [DOI] [PubMed] [Google Scholar]
- 4.Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Virani SS, Alonso A, Benjamin EJ, et al. Circulation. 2020;141:139–596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 5.Trends in survival after pediatric in-hospital cardiac arrest in the United States. Holmberg MJ, Wiberg S, Ross CE, Kleinman M, Hoeyer-Nielsen AK, Donnino MW, Andersen LW. Circulation. 2019;140:1398–1408. doi: 10.1161/CIRCULATIONAHA.119.041667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Unchanged pediatric out-of-hospital cardiac arrest incidence and survival rates with regional variation in North America. Fink EL, Prince DK, Kaltman JR, et al. Resuscitation. 2016;107:121–128. doi: 10.1016/j.resuscitation.2016.07.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pediatric in-hospital cardiac arrest and cardiopulmonary resuscitation in the United States: a review. Morgan RW, Kirschen MP, Kilbaugh TJ, Sutton RM, Topjian AA. JAMA Pediatr. 2021;175:293–302. doi: 10.1001/jamapediatrics.2020.5039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pediatric out-of-hospital cardiac arrest characteristics and their association with survival and neurobehavioral outcome. Meert KL, Telford R, Holubkov R, Slomine BS, Christensen JR, Dean JM, Moler FW. Pediatr Crit Care Med. 2016;17:543–550. [Google Scholar]
- 9.Part 11: pediatric basic life support and cardiopulmonary resuscitation quality. 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Atkins DL, Berger S, Duff JP, et al. Circulation. 2015;132:519–525. doi: 10.1161/CIR.0000000000000265. [DOI] [PubMed] [Google Scholar]
- 10.Part 12: pediatric advanced life support. 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. de Caen AR, Berg MD, Chameides L, et al. Circulation. 2015;132:526–542. doi: 10.1161/CIR.0000000000000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. Nadkarni VM, Larkin GL, Peberdy MA, et al. JAMA. 2006;295:50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 12.Incidence and outcomes of cardiopulmonary resuscitation in PICUs. Berg RA, Nadkarni VM, Clark AE, et al. Crit Care Med. 2016;44:798–808. doi: 10.1097/CCM.0000000000001484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.In-hospital cardiac arrest: a review. Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. JAMA. 2019;321:1200–1210. doi: 10.1001/jama.2019.1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Survival trends in pediatric in-hospital cardiac arrests: an analysis from get with the guidelines-resuscitation. Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, Chan PS. Circ Cardiovasc Qual Outcomes. 2013;6:42–49. doi: 10.1161/CIRCOUTCOMES.112.967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Matos RI, Watson RS, Nadkarni VM, et al. Circulation. 2013;127:442–451. doi: 10.1161/CIRCULATIONAHA.112.125625. [DOI] [PubMed] [Google Scholar]
- 16.Epidemiological and survival trends of pediatric cardiac arrests in emergency departments in korea: a cross-sectional, nationwide report. Ahn JY, Lee MJ, Kim H, Yoon HD, Jang HY. J Korean Med Sci. 2015;30:1354–1360. doi: 10.3346/jkms.2015.30.9.1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cardiopulmonary resuscitation for in-hospital events in the emergency department: a comparison of adult and pediatric outcomes and care processes. Donoghue AJ, Abella BS, Merchant R, Praestgaard A, Topjian A, Berg R, Nadkarni V. Resuscitation. 2015;92:94–100. doi: 10.1016/j.resuscitation.2015.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pediatric cardiac arrest in the emergency department: outcome is related to the time of admission. Yurtseven A, Turan C, Akarca FK, Saz EU. Pak J Med Sci. 2019;35:1434–1440. doi: 10.12669/pjms.35.5.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cardiac arrest survival in pediatric and general emergency departments. Michelson KA, Hudgins JD, Monuteaux MC, Bachur RG, Finkelstein JA. Pediatrics. 2018;141:0. doi: 10.1542/peds.2017-2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.2018 introduction to the NEDS. Healthcare cost and utilization project (HCUP) [ Sep; 2021 ];http://www.hcup-us.ahrq.gov/db/nation/neds/NEDS_Introduction_2018.jsp April 2021 20:2021. [Google Scholar]
- 21.Predictors and outcomes of cardiac arrest in the emergency department and in-patient settings in the United States (2016-2018) Mir T, Qureshi WT, Uddin M, Soubani A, Saydain G, Rab T, Kakouros N. Resuscitation. 2022;170:100–106. doi: 10.1016/j.resuscitation.2021.11.009. [DOI] [PubMed] [Google Scholar]
- 22.Arrest etiology among patients resuscitated from cardiac arrest. Chen N, Callaway CW, Guyette FX, Rittenberger JC, Doshi AA, Dezfulian C, Elmer J. Resuscitation. 2018;130:33–40. doi: 10.1016/j.resuscitation.2018.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.European Resuscitation Council Guidelines for Resuscitation 2015. Section 6: paediatric life support. Maconochie IK, Bingham R, Eich C, et al. Resuscitation. 2015;95:223–248. doi: 10.1016/j.resuscitation.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 24.The landscape of paediatric in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Skellett S, Orzechowska I, Thomas K, Fortune PM. Resuscitation. 2020;155:165–171. doi: 10.1016/j.resuscitation.2020.07.026. [DOI] [PubMed] [Google Scholar]
- 25.Vega RM, Kaur H, Edemekong PF. Treasure Island: StatPearls Publishing; 2022. Cardiopulmonary arrest In children. [PubMed] [Google Scholar]
- 26.Severe metabolic acidosis after out-of-hospital cardiac arrest: risk factors and association with outcome. Jamme M, Ben Hadj Salem O, Guillemet L, et al. Ann Intensive Care. 2018;8:62. doi: 10.1186/s13613-018-0409-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sodium bicarbonate: basically useless therapy. Aschner JL, Poland RL. Pediatrics. 2008;122:831–835. doi: 10.1542/peds.2007-2400. [DOI] [PubMed] [Google Scholar]
- 28.Metabolic acidosis in patients with severe sepsis and septic shock: a longitudinal quantitative study. Noritomi DT, Soriano FG, Kellum JA, Cappi SB, Biselli PJ, Libório AB, Park M. Crit Care Med. 2009;37:2733–2739. doi: 10.1097/ccm.0b013e3181a59165. [DOI] [PubMed] [Google Scholar]