Abstract
Background and Objectives:
Falls are the leading cause of fatal and nonfatal injuries among older adults. Decreasing falls is highly dependent on engagement in fall prevention activities. The Health Belief Model (HBM) theoretical framework was used to explore older adults’ perceptions about falls prevention.
Research Design and Methods:
An informed grounded theory approach was applied. Four focus groups were conducted using semi-structured interview guides based on the HBM with 27 community-dwelling older adults (average age = 78 years). Deductive content analysis was used to apply constructs of the HBM to the data and explain the findings.
Results:
Potential reasons for not engaging in falls prevention included lack of self-perceived severity, susceptibility, and self-efficacy with a subtheme of lack of information about falls prevention from medical providers. Potential facilitators included older adults’ knowledge and current engagement in falls prevention and socializing while engaging in falls prevention. Participants recommended cues to action to improve engagement in falls prevention from family, friends, physicians, pharmacists, and insurance companies; and using various modes to deliver cues to action, including print, audiovisual, online, and reminders.
Discussion and Implications:
In this study, the HBM was used to understand older adults’ potential barriers, facilitators, and cues to action to support engagement in falls prevention. Engagement in fall prevention behaviors could be improved by addressing barriers such as lack of knowledge, and lack of self-perceived severity and susceptibility to falls. Reinforcing the benefits of fall prevention, and promoting cues to action to engage in falls prevention may also support engagement.
Keywords: Accidental injury, implementation science
Background and Objectives
Falls are the leading cause of fatal and nonfatal injuries among adults 65 years and older (Centers for Disease Control and Prevention, 2020). Twenty-eight percent of older adults fall annually, resulting in $50 billion in medical costs (Florence et al., 2018). Direct costs do not account for long term effects of falls such as disability, loss of independence, and decreased quality of life.
Modifiable factors increase an older adults’ risk of falling, such as fear of falling, decreased strength or balance, unsteady gait, visual and foot impairments, environment, and some medications (Ganz & Latham, 2020; Gillespie et al., 2012). Systematic reviews demonstrate that several interventions addressing modifiable factors can reduce falls (Gillespie et al., 2012; Hopewell et al., 2018), yet mortality rates continue to rise (Hartholt, Lee, Burns, & Van Beeck, 2019). Evidence-based interventions include, but are not limited to, exercise, management of visual and foot issues, medication management, physical therapy, and home modifications (Grossman et al., 2018). At least 22 interventions, investigated in randomized control trials, demonstrated that implementing even a single intervention could decrease falls and save $94-$442 million in medical costs (Stevens & Lee, 2018). Although interventions are efficacious, barriers to older adults’ engagement in falls prevention still exists (Farrance, Tsofliou, & Clark, 2016; Stevens, Sleet, & Rubenstein, 2018). Strategies for increasing older adults’ engagement in falls prevention are imperative to address these public health issues. Employing constructs from a behavioral change model, such as the health belief model (HBM), to identify older adults’ barriers, facilitators, and recommended cues to action for engagement in falls prevention may be helpful to target behavior change.
Health Belief Model
The HBM is a theoretical framework developed to explain individuals’ engagement in preventive health behavior based on the following constructs; (1) perceived susceptibility of the health condition, (2) perceived severity of the health condition, (3) perceived benefits to taking the recommended action, (4) perceived barriers to taking the recommended action, (5) cues to action to engage in the preventive-health behavior, and (6) self-efficacy to engage in the prevention-health behavior (Janz & Becker, 1984). There are several modifying factors in the HBM as well; such as knowledge about the health condition (Davidhizar, 1983). The HBM is one of the most widely used theoretical frameworks used to explain the health intervention uptake and behavior and has been useful in planning and designing fall prevention strategies. For example, an expanded HBM, adding habits and intention as constructs, was used to identify determinants of physical activity among older adults who have and have not experienced a fall. The authors found that perceived barriers to physical activity significantly predicted intention to participate among people with a history of falls (Kaushal, Preissner, Charles, & Knäuper, 2021). Another study found that older females participating in an osteoporosis and falls prevention program, which included 4 sessions of education and counseling based on the HBM constructs, demonstrated greater knowledge and adoption of preventive behaviors compared to a group education only program that was not based on the HBM (Ahn & Oh, 2021). Huang, Tzeng, and Chen (2021) used the HBM to develop a prediction model for the likelihood of community dwelling older adults to engage in fall prevention activities. Results showed that self-efficacy had the largest influence on engagement followed by cues to action. Perceived barriers did not directly affect the likelihood of taking fall prevention action.
Barriers and Facilitators to Engaging in Falls Prevention
Addressing the public health issue of falls in older adults is highly dependent on sustained adherence to fall prevention strategies (Sjosten et al., 2007). A meta-analysis of older adults’ adherence to home exercise programs to prevent falls found only 21% of older adults were adherent (Simek, McPhate, & Haines, 2012), while a systematic review found that ~50% adhered to falls prevention interventions at 12 months (Nyman & Victor, 2011). Barriers to engagement and adherence identified in the literature include lack of knowledge, low self-efficacy, perceptions that falls are not preventable, being unaware of the risk for falling, feeling limited by health, not feeling supported by medical providers and family, and lack of access to programs (Bunn, Dickinson, Barnett-Page, Mcinnes, & Horton, 2008; McMahon, Talley, & Wyman, 2011; Pin, Spini, Bodard, & Arwidson, 2015; Stevens et al., 2018). Facilitators, which affect perceived benefits and barriers, to adopting falls prevention recommendations include personal relevance and appropriateness of programs, self-efficacy, participation in decision making, convenience, and encouragement by medical providers or social supports (Bunn et al., 2008; Pin et al., 2015; Stevens et al., 2018). Strategies to address barriers are sparse and are recommended as a priority by the Centers for Disease Control (CDC) and imperative to effective falls prevention (Bergen & Eckstrom, 2018). Literature identified strategies to improve engagement in falls prevention programs, including convenience, proximity, socializing, and group exercise (Howard et al., 2018; Kiami, Sky, & Goodgold, 2019), but not in the context of engagement in falls prevention not included in a formal program nor the context of a behavior change model. Although the HBM has been used to develop and implement falls prevention programs, it has not been used to identify themes and index meaning units from primary qualitative data in an effort to understand older adults’ attitudes and beliefs on engaging in falls prevention. Given that the aim of preventing falls is highly dependent on adherence to fall prevention behaviors, it is important to understand older adults’ perceptions of their susceptibility to falling, perceived severity of falling as having serious medical and social consequences, perceived benefits of taking action to reduce the risk of falling, perceived barriers in taking the action, and recommended cues to action to engage in falls prevention. Therefore, the purpose of this study was to explore older adults’ perceptions about engagement in falls prevention behaviors using constructs from the HBM.
Research Design and Methods
Ethical Considerations
The institutional review board approved the study.
Design
An informed grounded theory approach was used to explore older adults’ perceptions of falls, falls prevention, and strategies to improve engagement in falls prevention using constructs from the HBM (Thornberg, 2012). Informed grounded theory supports using existing literature and theories to inform the approach to qualitative research. The HBM and additional modifying factors related to fall prevention engagement (Figure 1) informed the approach to the semi-structured interview guide (Table 1; (Janz & Becker, 1984; Vincenzo & Patton, 2021). Three one-on-one interviews were conducted to assess and modify the interview guides, which are not included in this study. Participants completed a questionnaire on demographics and medical history before participation in a focus group.
Figure 1.
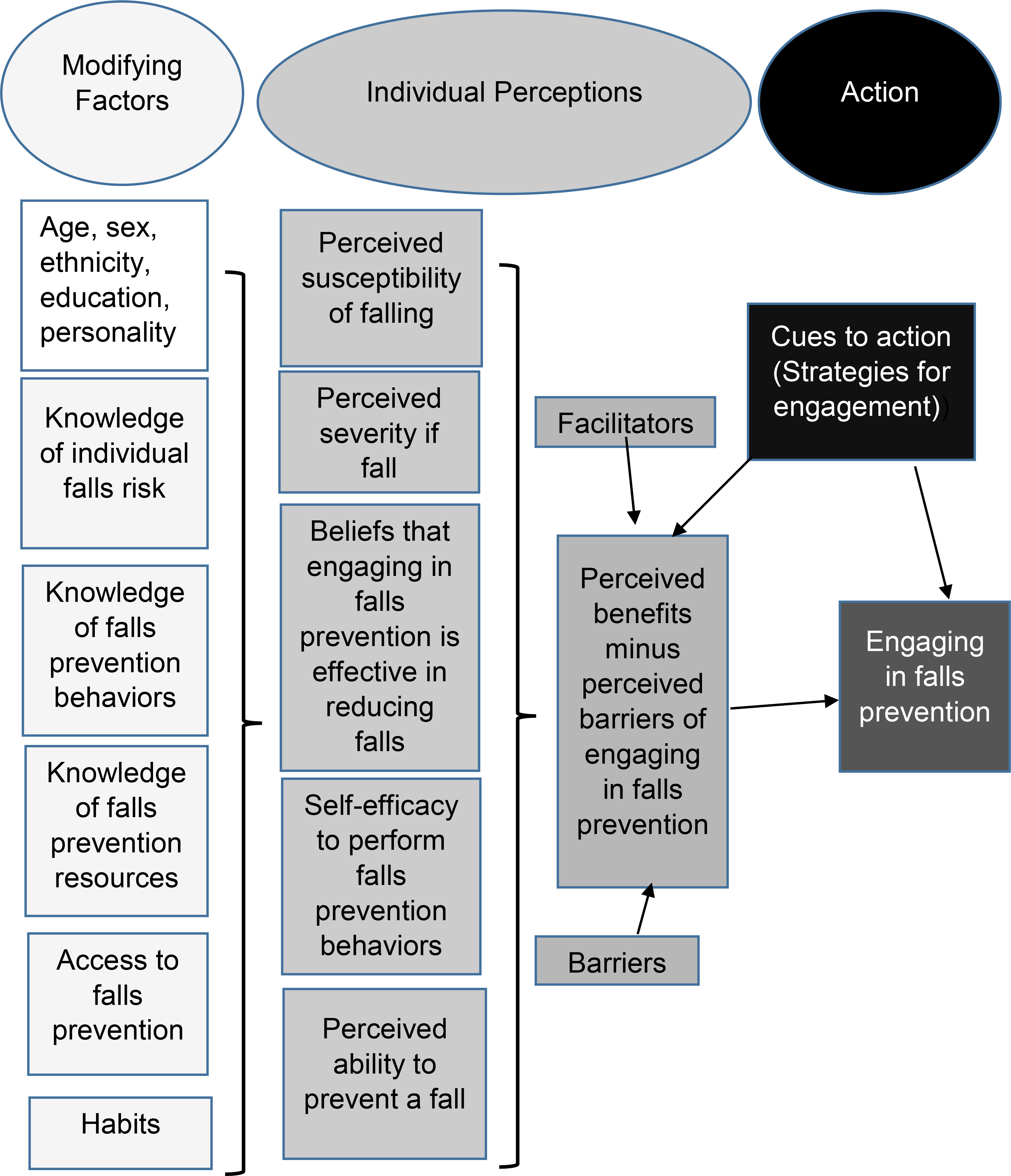
Health Belief Model Adapted to Falls Prevention
Table 1.
Semi-Structured Interview Guide about Perceptions and Strategies for Falls Prevention
| 1. Tell me what you know about older people having a fall or multiple falls. |
| • Prompt: What do you think most older adults know about their risk of falling? |
| 2. Tell me about how falls have or have not personally affected you? |
| • Prompts: Have you fallen? If yes, were you injured? Describe how the fall affected you. Do you know someone who has suffered a fall? How did it affect them? Tell me your understanding of the consequences of falling. |
| 3. Tell me about information, if any, you have gotten about falls and preventing them? |
| • Prompts: Where did you get this information and/or who gave you the information? How was it provided to you? How was it helpful? What were the difficulties with using the information? Did you do or change anything due to the information; why or why not? |
| 4. Tell me about how habits may help or hurt you or others to prevent falls. |
| 5. Tell me about how you feel about your control or lack of control over preventing a fall? |
| 6. What would help an older adult to engage in falls prevention behaviors? |
Participant Sampling
Individuals who participated in a prior, unrelated study at the University and were interested in participating in future studies were recruited. The inclusion criteria were adults >65 years of age, community-dwelling, and able to understand and answer the study questions. Guided by evidence that gender differences in attitudes and beliefs regarding falls prevention exists (Sandlund et al., 2017), two focus groups consisted solely of women, and two focus groups consisted solely of men.
Data Collection
Before conducting the focus groups, informed consent, demographics, and health history were collected. Krueger and Casey’s (2014) guide to designing and conducting focus group interviews was followed. Four focus groups of six to eight participants were conducted between December, 2019 and February, 2020. The primary researcher, a physical therapist with 20 years of experience and a trained qualitative researcher, served as the moderator for three focus groups, and a research assistant trained by the primary investigator who took field notes in the first three focus groups, moderated the fourth focus group. Ground rules were established at the start of each session (speak one at a time, be respectful, engage and share opinions and experiences). Two focus groups were conducted in a conference room at a university, one was in a conference room at a senior center, and one was hosted at the house of a participant per their request. Focus groups were recorded on a digital voice recorder (Olympus WS-853, Pennsylvania). Before concluding the focus groups, the interviewer summarized themes regarding group and participants’ perspectives for confirmability. Focus groups lasted between 1.25 – 1.5 hours. Participants received a $30 gift card.
Data Analysis
Data from the demographic questionnaires were entered into excel. Descriptive statistics were calculated. Interviews were uploaded to computerized software (Descript, San Francisco, CA) for initial transcription and edited for accuracy. Data from focus groups were analyzed using deductive content analysis to identify, analyze, and interpret meaning and themes in the data. In the deductive (directed) approach, analysis starts with a theory as guidance for initial codes (Hsieh & Shannon, 2005). The HBM served as the framework for the analysis. A deductive approach was applied whereby key categories were pre-determined according to the HBM (perceived susceptibility, perceived severity, perceived barriers, cues to action, and self-efficacy). Meaning units were extracted from the focus groups and assigned a code which was placed under a pre-determined HBM category. The steps involved in the data analysis process are listed below:
Step 1: Identification of relevant behavior change theory and a priori themes: core constructs of the HBM were listed and used as codes.
Step 2: Deductive analysis: data was analyzed to identify and sort meaning units. The a priori themes were applied and used to index the meaning units from the data.
Step 3: During the final step, researchers reached a consensus on interrelationships between the research questions, codes, and core themes (Bingham & Witkowsky, 2021). Researchers agreed that data saturation, when no new information or themes emerge, was obtained with the four focus groups (Bailey & Bailey, 2017).
Trustworthiness in our study was ensured by engaging in member checking and investigator triangulation (Wilson, 2014). The two researchers held regular meetings throughout the process of analysis. Investigator triangulation was applied by having two researchers with expertise in fall prevention and qualitative research (Removed for blinded review) read and code the data separately, followed by discussion and agreement on codes, themes, and exemplary quotes. Investigator triangulation also lessoned potential bias when applying data to the HBM codes.
Results
Sample Description
Participants (n=27) averaged 78 years old with an approximately even distribution of males and females (Table 2). Ten participants (37%) experienced at least one fall in the last year and 26% suffered an injury. Participants in the focus groups were engaged and collectively accepting of others’ experiences and ideas.
Table 2.
Participant Demographics
| Characteristic | N (27) |
|---|---|
| Sex | |
| Male | 13 |
| Female | 14 |
| Age | |
| Male | 79.4 |
| Female | 76.1 |
| Race/Ethnicity | |
| Non-Hispanic - white | 21 |
| No response | 6 |
| Educational level | |
| Less than a high school diploma | 2 |
| High school degree or equivalent (GED) | 0 |
| Some college, no degree | 11 |
| Associate degree | 2 |
| Bachelor’s degree | 5 |
| Master’s degree | 3 |
| Professional degree (MD, DDS, DVM) | 0 |
| Doctorate (PhD, EdD) | 2 |
| No response | 2 |
| Yearly income | |
| Less than $20,000 | 3 |
| $20,000 to $34,999 | 6 |
| $35,000 to $49,999 | 2 |
| $50,000 to $74,999 | 5 |
| $75,000 to $99,999 | 7 |
| Over $100,000 | 3 |
| No answer | 1 |
| Marital Status | |
| Married, or in a domestic partnership | 19 |
| Widowed | 8 |
| Comorbid conditions | |
| Cardiovascular disease | 5 |
| Cancer | 1 |
| Chronic obstructive pulmonary disease | 1 |
| Hyperlipidemia | 4 |
| Hypertension | 7 |
| Thyroid impairment (hyper/hypothyroidism) | 2 |
| Enlarged prostate | 2 |
| Osteoporosis | 1 |
| Arthritis | 5 |
| Vestibular impairment | 3 |
| Vision impairment (glaucoma, cataracts) | 2 |
| Musculoskeletal impairments (low back pain, knee pain) | 6 |
| Neuromuscular impairments (sciatica, fibromyalgia) | 2 |
| Depression | 2 |
| Number of Medications | |
| 1–2 | 15 |
| 3–4 | 6 |
| ≥5 | 3 |
| No answer | 3 |
| Experienced a fall in the last year | |
| Yes | 10 |
| No | 17 |
| Number of falls in the last year | |
| 1 | 2 |
| 2 | 2 |
| ≥3 | 3 |
| No answer | 3 |
| Falls resulting in injury | |
| Yes | 7 |
| No | 6 |
| No answer | 14 |
| Injury type from falls | |
| Fracture | 2 |
| Musculoskeletal pain or soreness | 3 |
| Bruising or scrapes | 3 |
Potential Barriers to Engaging in Falls Prevention
Participants identified barriers to engaging in falls prevention which fit within the pre-determined HBM constructs and included lack of self-perceived severity, susceptibility, and self-efficacy and lack of information from medical providers regarding how to prevent falls.
Lack of Self-Perceived Severity of Falls
Although most participants felt that falls resulted in severe consequences, they related the severity and consequences of falls to anecdotal experiences of friends and family rather than how a fall would affect themselves, “you’ve seen the consequences of what can happen with other people.” Participants shared examples, “My dad broke a hip and that was the beginning of the end,” and “I had a great aunt who fell… she spiral fractured both her arms,” and “I have a neighbor who recently slipped off a stool and her hip broke and she fell.” Some participants who experienced a fall minimized the health consequence; stating for example, “I don’t fall that much,” and, “I haven’t gotten hurt. I usually have some bruises.” Only one participant addressed the severe consequences of falls; however, from their friend’s perspective, “My friend said…you realize we’re just one fall away from the nursing home.”
Lack of Self-Perceived Susceptibility of Experiencing a Fall
Older adults’ perceived susceptibility of experiencing a fall did not reflect their expressed general knowledge about falls and prevention described in the facilitators theme below. Some who had not experienced a fall did not believe that they were at risk for falling. “The threat is not there individually,” and, “I think I’m just fine, I don’t have any problems,” and, “I hadn’t worried about falling … I don’t have a balance problem.” Other participants suggested that older adults do not feel susceptible until they experience a fall, “You don’t think about it until you have a problem,” and “Until you go down, it just doesn’t click,” and “when I tripped, I wasn’t aware… I didn’t even imagine falling.” Only one participant seemed to accept and recognize their susceptibility of experiencing a fall, “part of it is, we have to come to grips at some point. We have to accept the reality condition. We have to accept the fact that I am who I am and where I’m at and make adjustments.”
Lack of Self-efficacy to Prevent a Fall
Some participants recognized their susceptibility to falling and described falls as “inevitable”, indicating a lack of self-efficacy to prevent a fall. “You’re going to fall probably,” and “You’re waiting; something is going to happen.” Another participant shared, “The times that I fell; I tried really hard to just fall. There’s no stopping the fall.” Other participants talked about preparing themselves for a fall, “practice getting up” from the floor in case they fall. One participant shared, “I get down on the floor because … my mom used to fall, and my husband used to fall.”
Subtheme - Lack of Falls Prevention Information from a Healthcare Provider
Although many older adults in the focus groups were aware of and engaged in some falls prevention behaviors described in the facilitators’ theme below, the majority of participants shared that they had not received information about falls prevention from their doctor. One participant stated, “My doctor always asks… have you had any falls in the last six months or a year or so? That kind of makes me more aware of it, but it’s not really information.” Another participant had a similar experience, “It’s always their first question when you have an appointment, have you fallen? But then there’s no follow-ups.” One participant asked another participant in the group, “You said you’ve had a fall. Have you had a doctor asked you, and you said yes? What happens then?” The other participant answered, “Nothing, well they always say, did you hurt yourself? No.” Some participants were specific regarding the information they felt they lacked from their doctor.
When I talked to the doctor after I fell, he did not ask me if I had any throw rugs or anything like that,” and “When we go in for a wellness visit annually, or just go to see the doc, I never hear a word from them or even the nurses… how to prevent falls.
Potential Facilitators to Engaging in Falls Prevention
We found that participants’ general knowledge and engagement in falls prevention is a modifying factor from the HBM that serves as a facilitator. Other facilitators included perceived benefits of socializing with group activities and cues to action. Participants suggested strategies to increase awareness of falls prevention, including advice from family and friends, doctors, and pharmacists; and cues to action via print, audiovisual, online modes, and reminders.
Modifying factor - General Knowledge about Falls and Current Engagement in Falls Prevention
Focus group participants were generally aware of falls, consequences, and various interventions for falls prevention,. One participant stated, “There’s a lot of awareness that old people are falling.” Another participant suggested, “It’s common … I would think it’s pretty high for folks over the age of 65 at least or 70 to have fallen at least one time in the last 10 years.” When asked about how they could prevent falls, participants most frequently related prevention to being more “careful.” The terms careful or cautious were used 39 times across all focus groups. Participants described, “As you get older you’re more careful,” and “I am very careful … I never thought about falling before.” Some older adults described actions they employed to be careful to prevent falls. For example, “I take blood pressure medicine, so I have to be real careful standing up. I have to wait until the dizziness passes so I won’t fall,” and, “I have been unbalanced occasionally, and I notice it sometimes in the shower when I close my eyes I get unbalanced, and I have several hand grips in the shower.” Participants also mentioned the ways that they restricted their activities to be more “careful.” For example, “I don’t walk out here in the garden … that is really dangerous to me,” and “I always opt-out of the stairs.” Participants also mentioned they either are aware of or engage in various forms of exercise that may help prevent a fall (21 quotes), that they wear proper footwear (mentioned 9 times), and use rails on the stairs (mentioned 10 times).
Perceived Benefit-Socializing with Group Activities
Socializing with group activities was the only theme that emerged as a perceived benefit to falls prevention. Participants made several statements that exemplified this theme. For example, “getting out and about is a big thing…encouraging involvement,” “doing things with people makes a big difference,” and that with “classes and things…socialization can improve.” One participant felt that group support and socializing helps with accountability,
“Well, if you go and you can talk about, I had trouble with this, or I did this four times this week, and I feel so much better. Especially too of being older, I mean, the socialization for some people … maybe some people are like “I don’t want to do it,” but I think it’s important and it reinforces, you doing it. And plus, there’s some accountability if you do it in a group.”
Cues to Action from Family and Friends
Participants shared how cues to action arose from social influences such as their family or friend’s involvement in falls prevention. One participant stated, “I have a close cousin that fell several times. Her family went in and removed all of her little throw rugs and everything.” Others talked about adult children that check on them regularly, “My daughter checks on me every day,” and “my son fixed the house and I have a lifeline,” and “We’ve got a daughter, and she is always questioning both of us about how are you? What are you doing? What have you been doing? Be careful.” One participant noticed their balance impairment when playing with their grandkids on a gaming system,
I came to be aware that my balance was not what it used to be. My grandkids got a Wii … and it had a deal where you balance on it … it said I was 72 years old according to my balance.
Two participants noted that friends and loved ones can provide valuable action to facilitate engagement in falls prevention. For example, “A loved one telling you or reminding you that something’s wrong and you don’t realize it,” and “Friends, those really affect me when someone I know has something that they feel like they need to bring to me or make me aware.” Finally, one participant indicated that going to the wellness center with her spouse helps her with adherence, “My husband and I come every day, and if he didn’t go, then I don’t know if I would come every day.”
Cues to Action from a Doctor or Pharmacist
The majority of participants voiced how doctors could provide older adults with information to prevent falls and preferred their doctor to discuss falls prevention with them. One participant stated, “The doctor would say, this is what you need to do.” Another explicitly preferred,
If somebody’s on a visit, the doctor says, after age … the statistics show that you are more apt to have a fall and here are some of the things that can happen at that age or as you get older.
Some preferred receiving falls prevention information from a brochure provided by their doctor. One participant stated, “If he (your doctor) could discuss some of it with you, just a verbal discussion would be more lasting than handing you a brochure, but then we would look at the brochure.” Another stated, “If the doctor doesn’t have time to talk about it … a brochure or something, at least that’s a start.” Finally, one participant suggested there should be a policy for doctors to include falls prevention education as part of the Medicare well examination:
We’re probably all seeing doctors on some regular basis, and I think those practitioners or those physicians need to have some policy. Maybe at some point, when a person reaches a certain age, the risk becomes greater. That it needs to be a part of their well examination to educate us in those areas rather than waiting until we fall and break a hip and then say, Hey, you know, you shouldn’t be doing that.
A few participants suggested that pharmacists could provide cues to action. One participant would like to receive “handouts with prescriptions because your visits with the doctor are less frequent, but your prescription filling is pretty much ongoing.” Another participant suggested the information be provided via “a flyer or something that a pharmacist would make available.”
Cues to Action or Financial Incentives from Insurance Companies
Across all focus groups, insurance companies’ role in supporting falls prevention was a suggested strategy to improve engagement. One participant reported that a nurse practitioner from her insurance company comes for a yearly home safety visit. This information resulted in discussion and interest from others in the same focus group. For example, “If it was provided to me through the insurance company or through Medicare… we want to communicate these principles to you. I would pay attention, but it’s not something I would go out and seek on my own.” Another participant suggested that home evaluations should be provided by insurance, “Even with each client [insurance]… somebody goes into someone’s home and makes the evaluation.” Other participants suggested insurance companies should provide financial incentives for older adults to participate in falls prevention. For example, “Money… if Medicare or somebody like that decided… prevention of falls,” and “I wonder if insurance companies could be involved … [you would get] lower rates if you get a home evaluation.”
Print Cues to Action
Along with suggestions of print materials that doctors or pharmacists could provide, participants mentioned other print/print materials that would increase older adults’ engagement in falls prevention. For example, “A newspaper, a visible ad.,” and “A magazine or a medical magazine.” More specifically, two people mentioned the American Association of Retired Persons (AARP) magazine, “AARP magazine, but I haven’t seen anything like that in there,” and “I have noted articles in the AARP magazine. They’re pretty good.” One man suggested, “From time to time, you read about someone that’s fallen out of the tree stand. The sports shooting magazines would have articles.” Finally, one participant suggested that a poster or something would be helpful at “Doctor’s appointments…in a waiting room… a poster or something”.
Audiovisual Cues to Action
Participants suggested different audiovisual modes to increase older adults’ engagement in falls prevention. One participant suggested, “The doctor’s office…a little screen in the waiting room… 30-second segments on falls and being careful.” Another participant suggested that a visual machine like the blood pressure screening near the pharmacy would be helpful,
In a pharmacy where you’re having to stand and wait for your prescription. If there was a line on the floor, walk this line, how difficult or easy is it? Or some visual things like the little machine where you can take your blood pressure.
Some participants suggested audiovisual options for broader dissemination. For example, a “Public service announcement… if you’re a senior citizen, listen to this about falls and give tips periodically,” and “State public television… half-hour snippets,” and “CNN and fox news... stations that a lot of seniors listen to.”
Online Cues to Action
Participants mentioned using the internet to look up or provide information on falls prevention. Statements exemplified this, “My wife would go on the internet and learn all about it,” and that to find out about falls prevention, another participant would “look at some information on the internet.” Another participant suggested that there should be a falls prevention knowledge test on the internet because, “Popular things on the internet or quizzes…people like to answer questions about things, particularly if it has to do with their intelligence.” Finally, another participant indicated they would like to receive falls prevention information from their health system or insurance, “an email that you knew was coming from a place you recognize.”
Reminders Cue to Action
Numerous participants felt that they needed reminders to engage in falls prevention, “Because we forget things, we need to be reminded.” They suggested forms of reminders such as, “A ring, like a bell,” or “A ding on your phone every day.” However, only one participant suggested using a virtual assistant, for example, Amazon’s Alexa, asking, “Have you walked today?”
Discussion and Implications
This study is the first, to our knowledge, to use qualitative methods to apply constructs from the HBM to identify older adults’ barriers, facilitators, and recommended cues to action to increase awareness and engagement in falls prevention. The older adults in our focus groups were generally knowledgeable about falls, the consequences of falling, and falls prevention, but had barriers to engaging in falls prevention, including lack of perceived self-susceptibility, severity, and self-efficacy and felt they did not receive falls prevention information from healthcare providers. The participants mentioned multiple facilitators that would increase their engagement in falls prevention, including socializing with group activities for falls prevention and cues to action. Ours is the first study to identify older adults’ recommended cues to action to increase engagement in falls prevention; receiving personalized information from their doctor or pharmacist, cues from family and friends, cues or financial incentives from insurance companies, and modes of cues including print, audiovisual, online, and reminder.
Barriers to engagement in falls prevention that emerged align with barriers previously identified in the research, including lack of knowledge, perceptions that falls are not preventable, being unaware of the risk for falling, and not feeling supported by health care providers (Bunn et al., 2008; McMahon et al., 2011; Pin et al., 2015; Stevens et al., 2018). In an observational study of older adults with a history of falls, Jansen and colleagues found that only 16% who experienced a fall recognized their risk, and only 10% prioritized fall prevention. Older adults who prioritized falls prevention were more likely to have recurrent falls, severe fear of falling, and use an assistive device for walking (Jansen et al., 2015). It is not surprising that our study sample did not prioritize falls prevention considering only three focus group participants in our study had recurrent falls, and none came to the interview with an assistive device. Our data supports the existing literature that many older adults do not receive fall prevention information from their healthcare providers (Shubert, Smith, Prizer, & Ory, 2013). Although a cross-sectional survey found that physician advice did not facilitate older adults to enroll in a fall prevention program (Kiami et al., 2019), participants in our study felt that if they received individualized recommendations from their physician, they would engage in falls prevention. Differences in the results of our study may be due to the survey included two multiple answer questions regarding what would make older adults more likely and less likely to participate in a falls prevention program, including an option of ‘doctor’s advice to attend’. In contrast, our qualitative study had open-ended questions to identify barriers and facilitators to engagement in falls prevention, not a program.
Our research aligns with the literature regarding facilitators to engagement in falls prevention, including increased knowledge and awareness, personal relevance, socializing, and encouragement by medical providers or other social supports (Bunn et al., 2008; Pin et al., 2015; Stevens et al., 2018). To our knowledge, ours is the first study to identify older adults’ recommended cues to action to support engagement in falls prevention. We found that cues to action from family and friends served as facilitators to engage in falls prevention behaviors. Participants mentioned that family members performed home modifications to prevent falls, and participants value friends or family member’s concerns. These findings suggest that family and friends of older adults should be provided information about falls prevention to facilitate older adults’ engagement. Engaging both older adults and their families improves falls prevention behaviors among hospitalized older adults (Opsahl et al., 2017), and community-dwelling adults with cancer (Potter, Pion, Klinkenberg, Kuhrik, & Kuhrik, 2014).
An unexpected finding in our study was that some older adults shared that pharmacies or pharmacists could improve engagement in falls prevention by providing information, scripts, or having information readily available. Pharmacists’s roles in falls prevention are primarily focused on medication management (Blalock et al., 2020; Robinson et al., 2019). Future research would be beneficial to explore expanding the pharmacist’s role beyond medication management for falls prevention.
Another novel finding in each of our focus groups included that insurance companies and financial incentives could facilitate older adults to engage in falls prevention. Participants suggested insurances provide information, support, annual home safety evaluations, or lower rates for people that engaged in falls prevention. Indeed, falls are costly to health insurance, with the most recent data indicating falls result in over $50 billion in direct medical costs annually (Florence et al., 2018). Numerous studies indicate that investing in falls prevention saves money. For example, a study analyzing three different evidence-based falls prevention programs (Otago Exercise Program, Tai Chi: Moving for Better Balance, and Stepping On) found that the return on investment for averting direct medical costs from falls ranged from 36% to 491% (Carande-Kulis, Stevens, Florence, Beattie, & Arias, 2015). Individual interventions such as home safety modifications (Pega, Kvizhinadze, Blakely, Atkinson, & Wilson, 2016) and cataract surgery are also cost-effective (Boyd, Kvizhinadze, Kho, Wilson, & Wilson, 2020).
To our knowledge, ours is the first study to identify older adults’ recommended modes for cues to action to support engagement in falls prevention. Participants recommended print, audiovisual, online, and reminder cues to action. Falls prevention articles were recommended in a newspaper or a magazine that an older adult would be likely to read, for example, AARP magazine or a sports magazine for older men. Participants recommended brochures, flyers, or prescriptions as an adjunct to education provided by a physician or pharmacist. Non-tailored falls prevention advice appears to affect older adults’ rate of falls. Hopewell and colleagues (2018) found that the rate of falls for multifactorial interventions compared to usual care favored multifactorial interventions; however, when usual care included non-tailored advice like a brochure or handout, there were no group differences. Another study compared the effects of a 1-hour fall prevention class with a pamphlet to a pamphlet only on immediate fall prevention knowledge and 2-week uptake of fall prevention among community-dwelling older adults and found no differences between groups (Hakim, Roginski, & Walker, 2007). Although some research indicates that adults infrequently read handouts (Shaw, Ibrahim, Reid, Ussher, & Rowlands, 2009), print materials can supplement healthcare providers’ education, resulting in increased knowledge and uptake of preventive health behaviors (Coulter & Ellins, 2007).
Audiovisual cues to action were recommend, including information on a screen in the doctor’s office or pharmacy, a public service announcement, or the news. Khong and colleagues (2017) found that older adults preferred falls prevention information be disseminated by a health professional and provided to the broader community. A fall prevention campaign in Australia increased older adults’ attitudes that falls are preventable and high priority; however, did not change self-perceived risk (Hughes et al., 2008). De Jong and colleagues (2019) conducted a study that included older adults collaboratively designing audiovisual fall prevention messages. They found that some older adults’ awareness and knowledge increased; however, perceptions about the messaging’s negative or positive perspectives was interpreted by each individual differently.
Participants recommended online sources to find information regarding falls prevention or receive an email from a reputable and familiar source. One suggestion was to provide a quiz about falls as a cue to action. Only one person mentioned the use of a smartphone/application as a cue to action. Surprisingly, these suggestions did not lead to group discussion, possibly because older adults over 75 years of age are less likely to own digital devices and use the internet to obtain health information (Gordon & Hornbrook, 2016) and the average age of our sample was 78 years. Future studies should investigate older adults’ health literacy and digital technology use for falls prevention, especially considering that several internet and smartphone applications target older adults for falls prevention.
There are other contextual cultural, societal, and healthcare factors that may affect older adults’ engagement in falls prevention behaviors. A systematic review of cultural influences on participation in exercise and fall prevention programs conducted in numerous countries and cultures revealed that societal and cultural norms greatly impacted older adults’ perceptions and engagement in falls prevention (Jang et al., 2016). Cultural and family perceptions of aging, family roles, and the inevitability of frailty with aging negatively impacted engagement in falls prevention. Language barriers compounded lack of engagement among migrants. Conversely, positive reinforcement from family and healthcare providers positively influenced engagement in falls prevention, similar to our study. A qualitative study was conducted with 30 Chinese older adults living in England. In contrast to our study, the authors found that Chinese older adults were reluctant to talk about falls, had fatalistic views about falls, and lacked knowledge regarding falls prevention interventions and availability (Horton & Dickinson, 2011). In addition, fall prevention programs in Asian countries have not shown the same level of effectiveness as fall prevention programs in Western countries. A recent systematic review and meta-analysis, although limited in the number of studies, found that only exercise was consistently preventive of falls and that other interventions such as footwear modifications and home modifications did not prevent future falls among older Asian adults (Hill et al., 2018). The authors postulate that the differences in fall prevention intervention effectiveness between Western and Asian countries are due to different cultures and other factors such as different indoor and outdoor environments, footwear, lifestyles, and health services. Because our study did not address culture, healthcare systems factors, and/or social context, the ability to generalize findings to different countries and cultures is a limitation.
Our study has strengths. Using constructs from a theory-based health behavior change model to identify older adults’ barriers, facilitators, and cues to action to engage in falls prevention can assist future efforts towards targeted behavior change. Identified cues to action provide various modes to deliver falls prevention messages. Although our study offers insight, it has limitations that warrant consideration. First, cues to action were not specific to different falls prevention interventions. Future research should identify which cues to action work for different interventions, such as exercise or home modifications. Second, the sample was not representative of all community-dwelling older adults. Our sample was independent without any assistive devices and lacked diversity. In addition, most of our sample had at least some college experience, which may affect their perceptions, preferences, and health literacy. Therefore, it would be beneficial to conduct this study with older adults from diverse backgrounds and education to determine if they have different barriers, facilitators, and cues to action to engage in falls prevention.
Our study provides insights into older adults’ potential barriers, facilitators, and cues to action to engage in falls prevention using the HBM. Healthcare providers, public health practitioners, and researchers can apply these findings to improve older adults’ engagement in falls prevention. Future studies would be beneficial to investigate the impact of family engagement, insurance or financial incentives, and cues to action for specific falls prevention interventions in order to improve older adults’ engagement in falls prevention.
Highlights.
Older adults do not perceive they are personally at risk of falls or injury.
Older adults want more information about falls from healthcare providers.
Older adults are interested in fall prevention support from friends and family.
Older adults are interested in fall prevention support from insurance companies.
Older adults suggest various cues to action for fall prevention engagement.
Acknowledgements
The authors would like to thank the participants for their valuable input in this study. We would also like to thank Holly Bennett, PT, DPT for assisting with data collection and formatting the manuscript.
Funding
This work and Dr. Vincenzo were supported by the Translational Research Institute (TRI), grant [KL2 TR003108] and [UL1 TR003107] through the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). Dr. Curran is supported by TRI [UL1 TR003107], through NCATS of the NIH. Dr. McElfish is supported by TRI [UL1TR000039] through NCATS of the NIH. The funders played no role in the design, conduct, or reporting of this study. The content is solely the authors’ responsibility and does not necessarily represent the official views of the NIH.
Footnotes
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jennifer L. Vincenzo, University of Arkansas for Medical Sciences, Department of Physical Therapy, College of Health Professions.
Susan Kane Patton, University of Arkansas, Department of Nursing, College of Education and Health Professions.
Leanne L. Lefler, University of Arkansas for Medical Sciences, College of Nursing.
Pearl A. McElfish, University of Arkansas for Medical Sciences, Office of Community Health and Research.
Jeanne Wei, University of Arkansas for Medical Sciences, Department of Geriatrics, College of Medicine, Reynolds Institute on Aging.
Geoffrey Curran, University of Arkansas for Medical Sciences, Departments of Pharmacy Practice and Psychiatry, Central Arkansas Veterans Healthcare System.
References
- Ahn S, & Oh J (2021). Effects of a health-belief-model-based osteoporosis-and fall-prevention program on women at early old age. Applied Nursing Research, 59, 151430. [DOI] [PubMed] [Google Scholar]
- Bailey CR, & Bailey CA (2017). A guide to qualitative field research Sage Publications. [Google Scholar]
- Bergen G, & Eckstrom E (2018). Building the evidence base for falls prevention: The cdc’s steadi initiative. Innovation in Aging, 2(suppl_1), 237. [Google Scholar]
- Blalock SJ, Ferreri SP, Renfro CP, Robinson JM, Farley JF, Ray N, & Busby-Whitehead J (2020). Impact of STEADI-rx: A community pharmacy-based fall prevention intervention. Journal of the American Geriatrics Society, 68(8), 1778–1786. doi: 10.1111/jgs.16459 [DOI] [PubMed] [Google Scholar]
- Boyd M, Kvizhinadze G, Kho A, Wilson G, & Wilson N (2020). Cataract surgery for falls prevention and improving vision: Modelling the health gain, health system costs and cost-effectiveness in a high-income country. Injury Prevention, 26(4), 302–309. [DOI] [PubMed] [Google Scholar]
- Bunn F, Dickinson A, Barnett-Page E, Mcinnes E, & Horton K (2008). A systematic review of older people’s perceptions of facilitators and barriers to participation in falls-prevention interventions. Ageing & Society, 28(4), 449–472. [Google Scholar]
- Carande-Kulis V, Stevens JA, Florence CS, Beattie BL, & Arias I (2015). A cost–benefit analysis of three older adult fall prevention interventions. Journal of Safety Research, 52, 65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). WISQARS (web-based injury statistics query and reporting system)|Injury Center|CDC. Retrieved from https://www.cdc.gov/injury/wisqars/index.html [Google Scholar]
- Coulter A, & Ellins J (2007). Effectiveness of strategies for informing, educating, and involving patients. Bmj, 335(7609), 24–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidhizar R (1983). Critique of the health-belief model. Journal of Advanced Nursing, 8(6), 467–472. [DOI] [PubMed] [Google Scholar]
- Farrance C, Tsofliou F, & Clark C (2016). Adherence to community based group exercise interventions for older people: A mixed-methods systematic review. Preventive Medicine, 87, 155–166. [DOI] [PubMed] [Google Scholar]
- Florence CS, Bergen G, Atherly A, Burns E, Stevens J, & Drake C (2018). Medical costs of fatal and nonfatal falls in older adults. Journal of the American Geriatrics Society, 66(4), 693–698. doi: 10.1111/jgs.15304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganz DA, & Latham NK (2020). Prevention of falls in community-dwelling older adults. New England Journal of Medicine, 382(8), 734–743. doi: 10.1056/NEJMcp1903252 [DOI] [PubMed] [Google Scholar]
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, & Lamb SE (2012). Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev, 9(11) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon NP, & Hornbrook MC (2016). Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: A database and survey study of seniors in a large health plan. Journal of Medical Internet Research, 18(3), e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman DC, Curry SJ, Owens DK, Barry MJ, Caughey AB, Davidson KW, … Krist AH (2018). Interventions to prevent falls in community-dwelling older adults: US preventive services task force recommendation statement. Jama, 319(16), 1696–1704. doi: 10.1001/jama.2018.3097 [DOI] [PubMed] [Google Scholar]
- Hakim RM, Roginski A, & Walker J (2007). Comparison of fall risk education methods for primary prevention with community-dwelling older adults in a senior center setting. Journal of Geriatric Physical Therapy, 30(2), 60–68. [DOI] [PubMed] [Google Scholar]
- Hartholt KA, Lee R, Burns ER, & Van Beeck EF (2019). Mortality from falls among US adults aged 75 years or older, 2000–2016. Jama, 321(21), 2131–2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill KD, Suttanon P, Lin S, Tsang WW, Ashari A, Abd Hamid TA, … Burton E (2018). What works in falls prevention in Asia: A systematic review and meta-analysis of randomized controlled trials. BMC Geriatrics, 18(1), 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopewell S, Adedire O, Copsey BJ, Boniface GJ, Sherrington C, Clemson L, … Lamb SE (2018). Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews, 7(7), CD012221. doi: 10.1002/14651858.CD012221.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton K, & Dickinson A (2011). The role of culture and diversity in the prevention of falls among older chinese people. Canadian Journal on Aging/La Revue Canadienne Du Vieillissement, 30(1), 57–66. [DOI] [PubMed] [Google Scholar]
- Howard B, Baca R, Bilger M, Cali S, Kotarski A, Parrett K, & Skibinski K (2018). Investigating older adults’ expressed needs regarding falls prevention. Physical & Occupational Therapy in Geriatrics, 36(2–3), 201–220. [Google Scholar]
- Hsieh H, & Shannon SE (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. [DOI] [PubMed] [Google Scholar]
- Hughes K, van Beurden E, Eakin EG, Barnett LM, Patterson E, Backhouse J, … Newman B (2008). Older persons’ perception of risk of falling: Implications for fall-prevention campaigns. American Journal of Public Health, 98(2), 351–357. doi: 10.2105/AJPH.2007.115055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang H, Clemson L, Lovarini M, Willis K, Lord SR, & Sherrington C (2016). Cultural influences on exercise participation and fall prevention: A systematic review and narrative synthesis. Disability and Rehabilitation, 38(8), 724–732. [DOI] [PubMed] [Google Scholar]
- Jansen S, Schoe J, van Rijn M, Abu-Hanna A, van Charante Eric P Moll, van der Velde N, & de Rooij SE (2015). Factors associated with recognition and prioritization for falling, and the effect on fall incidence in community dwelling older adults. BMC Geriatrics, 15(1), 169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janz NK, & Becker MH (1984). The health belief model: A decade later. Health Education Quarterly, 11(1), 1–47. [DOI] [PubMed] [Google Scholar]
- Kaushal N, Preissner C, Charles K, & Knäuper B (2021). Differences and similarities of physical activity determinants between older adults who have and have not experienced a fall: Testing an extended health belief model. Archives of Gerontology and Geriatrics, 92, 104247. [DOI] [PubMed] [Google Scholar]
- Kiami SR, Sky R, & Goodgold S (2019). Facilitators and barriers to enrolling in falls prevention programming among community dwelling older adults. Archives of Gerontology and Geriatrics, 82, 106–113. [DOI] [PubMed] [Google Scholar]
- Krueger RA & Casey MA (2014). Focus groups: A practical guide for applied research (5th ed.). Thousand Oaks, CA: Sage publications. [Google Scholar]
- McMahon S, Talley KM, & Wyman JF (2011). Older people’s perspectives on fall risk and fall prevention programs: A literature review. International Journal of Older People Nursing, 6(4), 289–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyman SR, & Victor CR (2011). Older people’s participation in and engagement with falls prevention interventions in community settings: An augment to the cochrane systematic review. Age and Ageing, 41(1), 16–23. [DOI] [PubMed] [Google Scholar]
- Opsahl AG, Ebright P, Cangany M, Lowder M, Scott D, & Shaner T (2017). Outcomes of adding patient and family engagement education to fall prevention bundled interventions. Journal of Nursing Care Quality, 32(3), 252–258. doi: 10.1097/NCQ.0000000000000232 [DOI] [PubMed] [Google Scholar]
- Pega F, Kvizhinadze G, Blakely T, Atkinson J, & Wilson N (2016). Home safety assessment and modification to reduce injurious falls in community-dwelling older adults: Cost-utility and equity analysis. Injury Prevention, 22(6), 420–426. [DOI] [PubMed] [Google Scholar]
- Pin S, Spini D, Bodard J, & Arwidson P (2015). Facilitators and barriers for older people to take part in fall prevention programs: A review of literature. [Facteurs facilitant et entravant la participation des personnes agees a des programmes de prevention des chutes : une revue de la litterature] Revue D’Epidemiologie Et De Sante Publique, 63(2), 105–118. doi: 10.1016/j.respe.2014.10.008 [doi] [DOI] [PubMed] [Google Scholar]
- Potter P, Pion S, Klinkenberg D, Kuhrik M, & Kuhrik N (2014). An instructional DVD fall-prevention program for patients with cancer and family caregivers. Oncology Nursing Forum, 41(5), 486–494. doi: 10.1188/14.ONF.486-494 [DOI] [PubMed] [Google Scholar]
- Robinson JM, Renfro CP, Shockley SJ, Blalock SJ, Watkins AK, & Ferreri SP (2019). Training and toolkit resources to support implementation of a community pharmacy fall prevention service. Pharmacy, 7(3), 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandlund M, Skelton DA, Pohl P, Ahlgren C, Melander-Wikman A, & Lundin-Olsson L (2017). Gender perspectives on views and preferences of older people on exercise to prevent falls: A systematic mixed studies review. BMC Geriatrics, 17(1), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw A, Ibrahim S, Reid F, Ussher M, & Rowlands G (2009). Patients’ perspectives of the doctor–patient relationship and information giving across a range of literacy levels. Patient Education and Counseling, 75(1), 114–120. doi: 10.1016/j.pec.2008.09.026 [DOI] [PubMed] [Google Scholar]
- Shubert TE, Smith ML, Prizer LP, & Ory MG (2013). Complexities of fall prevention in clinical settings: A commentary. The Gerontologist, 54(4), 550–558. doi: 10.1093/geront/gnt079 [DOI] [PubMed] [Google Scholar]
- Simek EM, McPhate L, & Haines TP (2012). Adherence to and efficacy of home exercise programs to prevent falls: A systematic review and meta-analysis of the impact of exercise program characteristics. Preventive Medicine, 55(4), 262–275. [DOI] [PubMed] [Google Scholar]
- Sjosten NM, Salonoja M, Piirtola M, Vahlberg TJ, Isoaho R, Hyttinen HK, … Kivela SL (2007). A multifactorial fall prevention programme in the community-dwelling aged: Predictors of adherence. European Journal of Public Health, 17(5), 464–470. doi:ckl272 [pii] [DOI] [PubMed] [Google Scholar]
- Stevens JA, & Lee R (2018). The potential to reduce falls and avert costs by clinically managing fall risk. American Journal of Preventive Medicine, 55(3), 290–297. doi: 10.1016/j.amepre.2018.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, Sleet DA, & Rubenstein LZ (2018). The influence of older adults’ beliefs and attitudes on adopting fall prevention behaviors. American Journal of Lifestyle Medicine, 12(4), 324–330. doi: 10.1177/1559827616687263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberg R (2012). Informed grounded theory. Scandinavian Journal of Educational Research, 5v6(3), 243–259. [Google Scholar]
- Vincenzo JL, & Patton SK (2021). Older adults’ experience with fall prevention recommendations derived from the STEADI. Health Promotion Practice, 22(2) doi: 10.1177/1524839919861967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson V (2014). Research methods: Triangulation. Evidence Based Library and Information Practice, 9(1), 74–75. [Google Scholar]


