Abstract
Objective
Our study aimed to investigate the level of depression, anxiety, and fatigue in patients with leukemias, and analyze the influence of sleep duration on the mental symptoms of patients with leukemias.
Methods
A total of 127 patients were enrolled in our study and completed the questionnaire survey. Self-Assessment Depression Scale (SDS), Self-Assessment Anxiety Scale (SAS), and the Fatigue Scale-14 (FS-14) were adopted. The patient’s lifestyle information, including exercise, alcohol abuse, and smoking, was obtained from the patient’s self-report.
Results
Depression score of patients with sleep duration >8 hours (long duration group) was 56.21±11.63, which was significantly lower than that of patients sleep duration between 6 and 8 hours (medium duration group) with 59.61±8.77 and patients sleep <6 hours (short duration group) with 64.82±6.42 (P = 0.007). Similarly, the anxiety score of long duration group, medium duration group and short duration group was 45.36±11.41, 48.26±6.96 and 53.53±5.87, respectively (P = 0.005). The fatigue score of short duration group is 8.47±2.45, which is higher than others (P = 0.046). To further identify the relationship, we evaluated physical fatigue and mental fatigue levels in patients with or without symptoms of depression. We found that patients with symptoms of depression have a higher score both in physical fatigue and mental fatigue (all p < 0.001). Similar trend was observed in patients with or without symptoms of anxiety (all p < 0.001). However, alzhough patients with leukemia in long duration group have the highest score of physical fatigue (p = 0.016), no significant difference in mental fatigue was found in different sleeping duration group (p = 0.587). Furthermore, multivariate analyses were conducted and revealed that sleep duration was the independent factor associated with depression (OR = 0.270, P = 0.003) and anxiety (OR = 0.473, P = 0.010).
Conclusion
For leukemia patients with short sleep duration, a prompt evaluation of their level of depression, anxiety, and fatigue and the initiation of timely interventions is essential.
Keywords: fatigue, depression, anxiety, sleep duration, leukemia
Introduction
Leukemias are a group of life-threatening malignant disorders that present with increased numbers of leucocytes in the blood and/or the bone marrow.1 Leukemias may present different forms with different age distributions. Acute lymphoblastic leukemia (ALL) is common in early childhood while acute myeloid leukemia (AML) is common in adults.2 In 2018, it is estimated there were a total of 437.0 thousand new cases of and 309.0 thousand cancer deaths from leukemia worldwide.3 For ALL, the reported incidence is 1.7 cases per 100,000 individuals per year within the USA.4 In the world, new cases had reached 64,200, with age-standardized morbidity reaching 0.85/100,000 by 2017.5,6 For AML, acute myeloid leukemia (AML) accounted for 18.0% of the total leukemia cases in 1990 and increased to 23.1% in 2017 worldwide, with age-standardized incidence rate increased from 1.35/100,000 to 1.54/100,000.5 Major advances in the diagnosis, classification, and treatment of leukemias have achieved, resulted in significant increases in the number of complete remissions and long-term disease-free survivors. However, there are still many problems that need to be solved urgently in patients with leukemia. Study has reported that people living with cancer have a substantial burden of mental health disorders.7 The odds of being depressed are more than 5 times greater for cancer patients than for the general population.8
How to improve the mental health of patients is a key issue. Symptoms of anxiety and depression are common in patients with various chronic diseases.9–12 Some studies have indicated that more than 50% of patients have anxiety and depression.13,14 Anxiety and depression have a significant correlation to leukemia.15–17 Patients with leukemias may have anxiety, depression, psychological, and emotional disorders. Depression and anxiety in patients may also result in adverse consequences of disease such as poor health-related quality of life, delays in treatment, non-adherence to care and worse survival.18–20 However, until now, the depression, anxiety, and fatigue of patients with leukemias has not been fully studied. Prior studies evaluating mental health in patients with leukemia suggest a concerning burden of depression and anxiety.21,22 Klepin et al conducted a prospective cohort study of 74 patients with AML showed that 39% had symptoms of depression.23 Although some studies provide vital information regarding mental health in patients with leukemia, many were included only one type of hematologic malignancy, thus limiting the generalizability of findings. Prevalence and how to relieve the mental health in patients with leukemia is still unknown.
It is well established that sleep quality is associated with mental disorder.24,25 Adequate sleep is a prerequisite for the body to receive sufficient rest. Inappropriate sleep duration is a common sleep complaint in the population and is increasingly recognized as deleterious to good health.26–28 Previous studies have shown that sleep duration is closely related to many diseases including depression and anxiety symptoms.29–31 However, additional research is required, especially in patients with leukemias. To further expand the understanding of sleep duration, depression and anxiety in patients with leukemia, a study with a broad range of hematologic diagnoses is needed. Moreover, identifying factors associated with mental health disorders would be critical in ensuring the psychosocial care needs of leukemia patients are addressed in a timely manner. Therefore, we conducted this study aimed to investigate the level of depression, anxiety, and fatigue in patients with leukemias, and analyze the influence of sleep duration on the mental symptoms of patients with leukemias. We have further assessed the risk factors associated with depression, anxiety among leukemia patients.
Subjects and Methods
Subjects
Patients were enrolled from March 2020 to March 2021 in Department of Hematology, The First People’s Hospital of Chenzhou. All enrolled patients have confirmed diagnosed with leukemia (22 were acute lymphocytic leukemia, 92 were acute myeloid leukemia with 7 of M3 subtype, 13 were chronic myeloid leukemia). The inclusion criteria were: 1). The patient was confirmed as a leukemia patient with pathologic evidences; and 2). The patient can fully understand the content of the questionnaire survey. If the patient was younger than 18 years of age, had central nervous system disease, or cognitive dysfunction they were excluded. The institutional review board of the The First People’s Hospital of Chenzhou approved this study. The informed consent of all patients was obtained. The sociodemographic data of all enrolled patients were also recorded. Sleep duration was self-reported by the patient and confirmed by wearable device. The patient’s lifestyle information, including exercise, alcohol abuse, and smoking, was obtained from the patient’s self-report. In our study, low weight was defined as a patient’s weight less than <57.9 kg based on the mean weight of all enrolled patients (57.9 kg).
Questionnaires
All the participants completed the following questionnaires: the Self-Assessment Depression Scale (SDS), the Self-Assessment Anxiety Scale (SAS), and the Fatigue Scale-14 (FS-14).
SDS: The SDS questionnaire contains 20 items. All items have four options including “a little of the time”, “some of the time”, “good part of the time” and “most of the time” The total score is calculated by adding these 20 scores. The depression score was x 1.25. Patients with a depression score of <50 were divided into the non-depression group, and those with a depression score of ≥50 were divided into the depression group.32
SAS: Anxiety scores assessed with SAS are the same as the depression scores. All items have four options including “a little of the time”, “some of the time”, “good part of the time” and “most of the time”. The anxiety score was x 1.25. Patients with an anxiety score of ≥50 were considered to have an anxiety disorder.33
FS-14: Fatigue level was evaluated by FS-14. FS-14 consists of 14 items, each of which has two options (yes or no). The 14 items reflect the severity of fatigue from different perspectives. FS-14 including physical fatigue (items from 1 to 8) and mental fatigue (items from 9 to 14).34,35
Statistical Analysis
Mean ± SD and categorical variables are used when appropriate. A chi square test and t-test were used to determine whether the results were significantly different. Univariate and multivariate analyses were performed to assess factors associated with depression, and anxiety. The significant level was set as P < 0.05 (two tails). SPSS 13.0 (Chicago, USA) was used for data analysis and quality control procedures.
Results
Demographic Data of Leukemia Patients According to Daytime Sleepiness
A total of 127 patients were enrolled in our study and completed the questionnaire survey. Among them, there are 22 cases of acute lymphocytic leukemia, 92 cases of acute myeloid leukemia (7 cases of M3 subtype), and 13 cases of chronic myeloid leukemia.
There were 71 people who slept 8 hours or less during the day, and 56 patients that slept more than 8 hours. Interestingly, we found that the age of patients (sleep duration >8 hours) was younger (P = 0.016), proportion of patients (sleep duration >8 hours) who regular exercise was lower (P = 0.027), as shown in Table 1.
Table 1.
Characteristics of Leukemia Patients Enrolled
| Variable | Leukemia Patients with Sleeping Duration | P | ||
|---|---|---|---|---|
| <6 Hours (n=17) | 6–8 Hours (n=54) | >8 Hours (n=56) | ||
| Age | 58.71 ± 15.86 | 51.00 ± 15.07 | 45.63 ± 17.78 | 0.014 |
| Sex | 0.183 | |||
| Male | 7 (41.2%) | 35 (64.8%) | 36 (64.3%) | |
| Female | 10 (58.8%) | 19 (35.2%) | 20 (35.7%) | |
| Height | 161.12 ± 6.87 | 163.54 ± 7.64 | 161.93 ± 10.54 | 0.510 |
| Weight | 56.91 ± 10.01 | 59.67 ± 10.93 | 56.61 ± 12.50 | 0.355 |
| Type of work | 0.248 | |||
| Manual | 16 (94.1%) | 41 (75.9%) | 43 (76.8%) | |
| Mental | 1 (5.9%) | 13 (24.1%) | 13 (23.2%) | |
| Marriage | 0.321 | |||
| Single | 1 (5.9%) | 2 (3.7%) | 9 (16.1%) | |
| Married | 15 (88.2%) | 49 (90.7%) | 45 (80.3%) | |
| Divorced | 0 (0.0%) | 2 (3.7%) | 1 (1.8%) | |
| Unknown | 1 (5.9%) | 1 (1.9%) | 1 (1.8%) | |
| Medical Insurance | 0.334 | |||
| Yes | 15 (88.2%) | 38 (70.4%) | 42 (75.0%) | |
| No | 2 (11.8%) | 16 (29.6%) | 14 (25.0%) | |
| Exercise | 0.005 | |||
| Yes | 4 (23.5%) | 30 (55.6%) | 16 (28.6%) | |
| No | 13 (76.5%) | 24 (44.4%) | 40 (71.4%) | |
| Alcohol abused | 0.230 | |||
| Yes | 3 (15.8%) | 11 (20.4%) | 5 (8.9%) | |
| No | 14 (82.4%) | 43 (79.6%) | 51 (91.1%) | |
| Smoking | 0.339 | |||
| Yes | 1 (5.9%) | 8 (14.8%) | 4 (7.1%) | |
| No | 16 (94.1%) | 46 (85.2%) | 52 (92.9%) | |
| Education | 0.441 | |||
| <6 years | 3 (17.6%) | 6 (11.1%) | 4 (7.1%) | |
| 6–9 years | 14 (82.4%) | 41 (75.9%) | 45 (80.4%) | |
| >9 years | 0 (0.0%) | 7 (13.0%) | 7 (12.5%) | |
Fatigue, Depression and Anxiety Levels Among Leukemia Patients
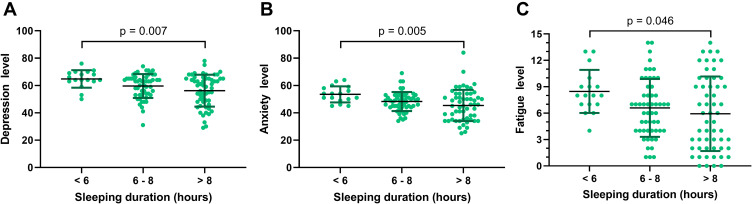
Among the included patients, the depression score of patients with sleep duration >8 hours (long duration group) was 56.21±11.63, which was significantly lower than that of patients sleep duration between 6 and 8 hours (medium duration group) with 59.61±8.77 and patients sleep <6 hours (short duration group) with 64.82±6.42 (P = 0.007), as shown in Figure 1A. Similarly, for the SAS score, the anxiety score of long duration group, medium duration group and short duration group was 45.36±11.41, 48.26±6.96 and 53.53±5.87, respectively (P = 0.005, Figure 1B). The results of the fatigue score suggest that the fatigue score of short duration group is 8.47±2.45, which is higher than others (P = 0.046), as shown in Figure 1C.
Figure 1.
Depression level, anxiety level and fatigue level in patients with different sleep duration. (A) The depression score of patients with long-, medium-, and short-sleep duration was 56.21±11.63, 59.61±8.77 and 64.82±6.42 (P = 0.007). (B) The anxiety score of long-, medium-, short- sleep duration patients was 45.36±11.41, 48.26±6.96 and 53.53±5.87, respectively (P = 0.005). (C) Fatigue score short duration group is 8.47±2.45, which is higher than others (P = 0.046).
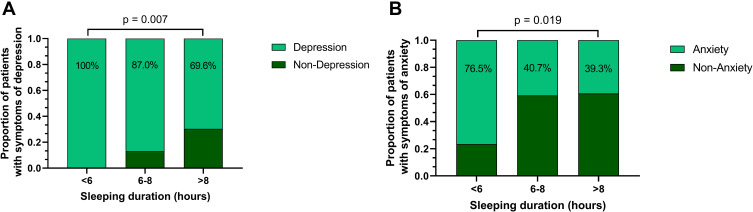
Proportion of Patients with Symptoms of Depression, Anxiety, and Fatigue
We further subdivided the proportion of depression, anxiety of patients with various sleep time. Among patients in the short duration group, medium duration group and long duration group, the proportion of patients with symptoms of depression was 100%, 87.0%, and 69.6%, respectively (P=0.007). Similarly, there was a significant difference in the proportion of patients with symptoms of anxiety (76.5%, 40.7%, and 39.3%, P=0.019), as shown in Figure 2.
Figure 2.
Proportion of depression and anxiety of patients with different sleep duration. (A) The proportion of patients with symptoms of depression was 100%, 87.0%, and 69.6%, respectively, in long-, medium-, and short-sleep duration (P = 0.007). (B) The proportion of patients with symptoms of anxiety was 76.5%, 40.7%, and 39.3% in long-, medium-, and short-sleep duration (P = 0.019).
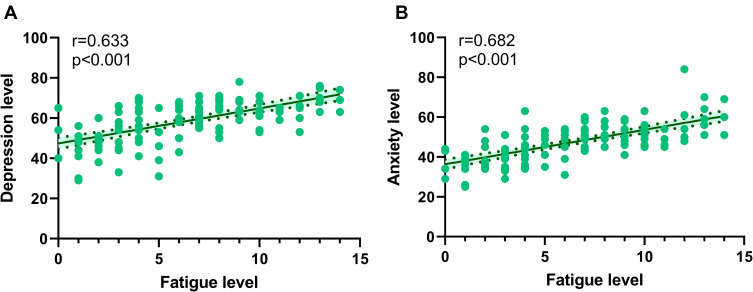
Relationship Between Depression, Anxiety and Fatigue in Leukemia Patients
To identify the relationship between depression, anxiety and fatigue in patients with leukemia, correlation analysis was conducted. Results shown that, in Figure 3, depression levels were positively correlated with fatigue level (r = 0.633, p < 0.001). Similar trend was observed in anxiety levels and fatigue (r = 0.628, p < 0.001).
Figure 3.
Relationship between depression, anxiety and fatigue in leukemia patients. (A) Depression levels were positively correlated with fatigue level (r = 0.633, p < 0.001). (B) Anxiety levels were positively correlated with fatigue (r = 0.628, p < 0.001).
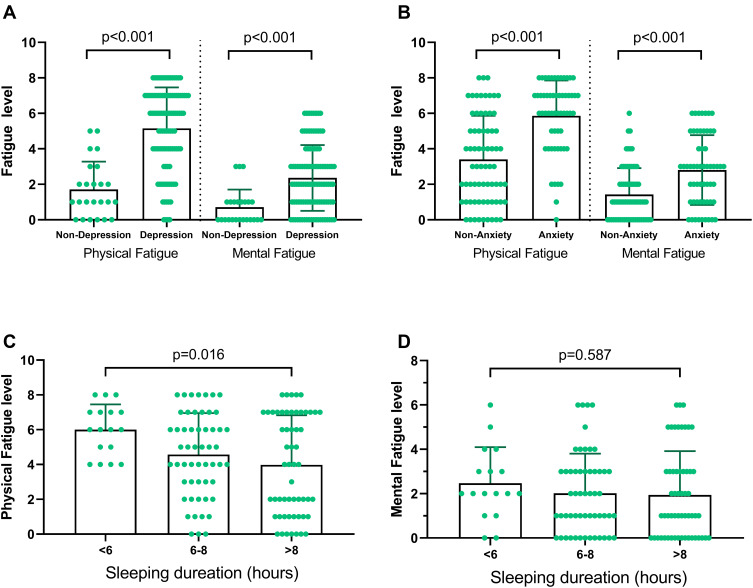
To further identify the relationship, we evaluated physical fatigue and mental fatigue levels in patients with or without depression. As shown in Figure 4, we found that patients with symptoms of depression have a higher score both in physical fatigue and mental fatigue (all p < 0.001, Figure 4A). Similar trend was observed in patients with or without anxiety (all p < 0.001, Figure 4B). However, we found that, although patients with leukemia in long duration group have highest score of physical fatigue (p = 0.016, Figure 4C), no significant difference in mental fatigue was found in different sleeping duration group (p = 0.587, Figure 4D).
Figure 4.
Relationship between depression, anxiety and fatigue in leukemia patients with different sleep duration. (A) Patients with symptoms of depression have higher score both in physical fatigue (1.71±1.57 vs 5.16±2.31, p < 0.001) and mental fatigue (0.71±0.99 vs 2.36±1.86, p < 0.001). (B) Patients with symptoms of anxiety have higher score both in physical fatigue (3.41±2.46 vs 5.86±1.99, p < 0.001) and mental fatigue (1.43±1.48 vs 2.81±1.96, p < 0.001). (C) Patients with leukemia in long duration group have highest score of physical fatigue (6.00±1.46 vs 4.57±2.38 vs 3.98±2.84, p = 0.016). (D) No significant difference in mental fatigue was found.
Risk Factors Associated with Depression, Anxiety, and Fatigue
To further evaluate the factors related to anxiety, depression in leukemia patients, univariate and multivariate analyses were conducted. The multivariate analysis revealed that sleep duration was the independent factor associated with depression (OR = 0.270, P=0.003, Table 2). For anxiety, low weight (OR = 0.473, P=0.010), and sleep duration (OR = 0.473, P=0.010) were the independent factors (Table 3).
Table 2.
Factors Associated Depression in Leukemia Patients
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Age | 1.030 | 1.003–1.058 | 0.029 | |||
| Sex | 2.150 | 0.788–5.865 | 0.135 | |||
| Height | 0.958 | 0.904–1.015 | 0.148 | |||
| Weight | 0.990 | 0.953–1.028 | 0.606 | |||
| Type of work | 0.768 | 0.271–2.176 | 0.620 | |||
| Marriage | 2.505 | 0.748–8.392 | 0.137 | |||
| Medical Insurance | 0.365 | 0.101–1.316 | 0.123 | |||
| Exercise | 1.740 | 0.664–4.561 | 0.260 | |||
| Alcohol abused | 0.852 | 0.255–2.844 | 0.795 | |||
| Smoking | 3.033 | 0.375–24.537 | 0.298 | |||
| Education | 0.391 | 0.145–1.056 | 0.064 | |||
| Sleeping duration | 0.269 | 0.113–0.640 | 0.003 | 0.270 | 0.113–0.644 | 0.003 |
Table 3.
Factors Associated Anxiety in Leukemia Patients
| Variables | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Age | 1.008 | 0.987–1.030 | 0.437 | |||
| Sex | 2.253 | 1.087–4.669 | 0.029 | |||
| Height | 0.948 | 0.907–0.991 | 0.018 | |||
| Weight | 0.953 | 0.920–0.986 | 0.006 | 0.473 | 0.264–0.837 | 0.010 |
| Type of work | 0.978 | 0.416–2.300 | 0.959 | |||
| Marriage | 1.354 | 0.471–3.897 | 0.574 | |||
| Medical Insurance | 0.898 | 0.402–2.006 | 0.793 | |||
| Exercise | 1.406 | 0.687–2.878 | 0.351 | |||
| Alcohol abused | 0.385 | 0.129–1.142 | 0.085 | |||
| Smoking | 0.512 | 0.149–1.757 | 0.287 | |||
| Education | 0.500 | 0.224–1.118 | 0.091 | |||
| Sleeping duration | 0.564 | 0.335–0.949 | 0.031 | 0.473 | 0.267–0.837 | 0.010 |
Discussion
In our study, we found that the characteristics of leukemia patients with different sleep duration are significantly different. Leukemia patients with long sleep duration are younger. In leukemia patients with short sleep duration, the level of depression, anxiety, and fatigue are significantly higher. Multivariable analysis suggested that sleep duration was the independent factor associated with depression and anxiety.
Previous study has found that women are under a higher incidence of anxiety and depression than men.36,37 However, in our research, there are no significant differences of depression and anxiety among male and female patients. Age has an effect on negative emotions. With the increase of age, the functions of various organs gradually decline, and the ability to withstand economic and social pressure gradually decreases.38–40 Especially, the susceptibility of the disease among the elderly is also a related factor. In our research, we found that older patients generally sleep less than younger patients, and those with short sleep duration have higher levels of depression, anxiety, and fatigue. Therefore, it may be more appropriate for elderly patients with leukemias to receive relevant psychological assessment.
Inappropriate sleep duration can seriously affect the patient’s daytime functioning, causing work, study, and life to be disrupted. It also has high potential risks, such as when driving. Fatigue is a common non-specific symptom. It is an abnormal state of the physiological change of patients. The definition of fatigue remains inconclusive. Some studies41 believe that fatigue is a feeling of lack of energy or exhaustion. The North American Nursing Diagnosis Association defines fatigue as a strong and long-lasting sense of feelings of weakness when engaged in mental and physical work.42 However, there is no research on the relationship between sleep duration and fatigue in patients with leukemias.
Studies have demonstrated that people with chronic fatigue generally have emotional problems such as depression, anxiety, obsession, and paranoia.43–45 Jenkins46 reported the relationship between adult sleep quality and fatigue, anxiety, depression and hostility. Sleep disorders were significantly positively correlated with anxiety, depression, hostility and fatigue. Morrison47 found that the incidence of anxiety, depression in people with sleep problems was significantly higher than that of those without sleep problems. Our research suggests that sleep duration is an important factor for depression, anxiety, and fatigue in patients with leukemias. For patients with leukemias with short sleep duration, a timely psychological evaluation should be carried out.
Previous study suggested that a blood cancer diagnosis itself may contribute to the development of underlying mental health disorders.48 In our study, we found a significant proportion of leukemia patients had symptoms of depression or anxiety. However, the proportion of leukemia patients with mental health problems may vary.15,17,49 In our study, we found the proportion of leukemia patients with symptoms of depression symptom was 81.1%, and the proportion of anxiety symptom was 44.9%. Our results confirmed the conclusions of a previous study that mental health screening and systematic implementation of psychosocial interventions for patients with blood cancers are essential to achieve high-quality cancer care.48 Interestingly, Castelli et al highlighted the sleep problems in hematological cancer patients.50 Our study confirmed this result. In addition, we further found that sleep duration was the independent factor associated with depression and anxiety in patients with leukemia.
Our study has a few limitations. First, we did not consider the severity of the leukemias. In our study, we did not further refine the type of leukemia enrolled. Second, the relatively small sample size of our study may induce bias. Third, all patients were enrolled in one center. How to screen mental health in patients with leukemia and target intervention requires a larger prospective multicenter study.
Conclusions
In our study, we found that, during the COVID-19 pandemic, the level of depression, anxiety, and fatigue are significantly higher in leukemia patients with short sleep duration. Sleep duration is an independent factor associated with depression and anxiety. For leukemia patients with short sleep duration, an evaluation of their level of depression, anxiety, and fatigue and the initiation of timely interventions is essential.
Acknowledgments
We want to thank nurses in our department for the helpful assistance.
Funding Statement
There is no funding to report.
Data Sharing Statement
Authors can confirm all relevant data are included in the article and materials.
Ethics Statement
The Institutional Review Board of The First People’s Hospital of Chenzhou had approved this study. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Informed consents were obtained from all patients enrolled.
Informed Consent
Informed consent was obtained from all patients.
Disclosure
All authors declare that they have no conflicts of interest.
References
- 1.Juliusson G, Hough R. Leukemia. Prog Tumor Res. 2016;43:87–100. doi: 10.1159/000447076 [DOI] [PubMed] [Google Scholar]
- 2.Inaba H, Mullighan CG. Depresión en escolares y adolescentes portadores de leucemia aguda en fase de tratamiento [Pediatric acute lymphoblastic leukemia]. Haematologica. 2020;105(11):2524–2539. doi: 10.3324/haematol.2020.247031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 4.Malard F, Mohty M. Acute lymphoblastic leukaemia. Lancet. 2020;395(10230):1146–1162. doi: 10.1016/S0140-6736(19)33018-1 [DOI] [PubMed] [Google Scholar]
- 5.Dong Y, Shi O, Zeng Q, et al. Leukemia incidence trends at the global, regional, and national level between 1990 and 2017. Exp Hematol Oncol. 2020;9(1):14. doi: 10.1186/s40164-020-00170-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu Y, Zhang X, Zhang A, et al. Global burden and attributable risk factors of acute lymphoblastic leukemia in 204 countries and territories in 1990–2019: estimation based on Global Burden of Disease Study 2019. Hematol Oncol. 2022;40(1):92–104. doi: 10.1002/hon.2936 [DOI] [PubMed] [Google Scholar]
- 7.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12(2):160–174. doi: 10.1016/S1470-2045(11)70002-X [DOI] [PubMed] [Google Scholar]
- 8.Hartung TJ, Brahler E, Faller H, et al. The risk of being depressed is significantly higher in cancer patients than in the general population: prevalence and severity of depressive symptoms across major cancer types. Eur J Cancer. 2017;72:46–53. doi: 10.1016/j.ejca.2016.11.017 [DOI] [PubMed] [Google Scholar]
- 9.Dunkel SC, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25(2):141–148. doi: 10.1097/YCO.0b013e3283503680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elbinoune I, Amine B, Shyen S, Gueddari S, Abouqal R, Hajjaj-Hassouni N. Chronic neck pain and anxiety-depression: prevalence and associated risk factors. Pan Afr Med J. 2016;24:89. doi: 10.11604/pamj.2016.24.89.8831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guvenc G, Yesilcinar I, Ozkececi F, et al. Anxiety, depression, and knowledge level in postpartum women during the COVID-19 pandemic. Perspect Psychiatr Care. 2021;57(3):1449–1458. doi: 10.1111/ppc.12711 [DOI] [PubMed] [Google Scholar]
- 12.Cai S, Liu L, Wu X, Pan Y, Yu T, Ou H. Depression, anxiety, psychological symptoms and health-related quality of life in people living with HIV. Patient Prefer Adherence. 2020;14:1533–1540. doi: 10.2147/PPA.S263007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lowe B, Spitzer RL, Williams JB, Mussell M, Schellberg D, Kroenke K. Depression, anxiety and somatization in primary care: syndrome overlap and functional impairment. Gen Hosp Psychiatry. 2008;30(3):191–199. doi: 10.1016/j.genhosppsych.2008.01.001 [DOI] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004 [DOI] [PubMed] [Google Scholar]
- 15.Ding T, Wang X, Fu A, Xu L, Lin J. Anxiety and depression predict unfavorable survival in acute myeloid leukemia patients. Medicine. 2019;98(43):e17314. doi: 10.1097/MD.0000000000017314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robbertz AS, Weiss DM, Awan FT, Byrd JC, Rogers KA, Woyach JA. Identifying risk factors for depression and anxiety symptoms in patients with chronic lymphocytic leukemia. Support Care Cancer. 2020;28(4):1799–1807. doi: 10.1007/s00520-019-04991-y [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Yan J, Chen J, et al. Comparison of the anxiety, depression and their relationship to quality of life among adult acute leukemia patients and their family caregivers: a cross-sectional study in China. Qual Life Res. 2021;30(7):1891–1901. doi: 10.1007/s11136-021-02785-6 [DOI] [PubMed] [Google Scholar]
- 18.Smith EM, Gomm SA, Dickens CM. Assessing the independent contribution to quality of life from anxiety and depression in patients with advanced cancer. Palliat Med. 2003;17(6):509–513. doi: 10.1191/0269216303pm781oa [DOI] [PubMed] [Google Scholar]
- 19.Iglay K, Santorelli ML, Hirshfield KM, et al. Impact of preexisting mental illness on all-cause and breast cancer-specific mortality in elderly patients with breast cancer. J Clin Oncol. 2017;35(36):4012–4018. doi: 10.1200/JCO.2017.73.4947 [DOI] [PubMed] [Google Scholar]
- 20.Iglay K, Santorelli ML, Hirshfield KM, et al. Diagnosis and treatment delays among elderly breast cancer patients with pre-existing mental illness. Breast Cancer Res Treat. 2017;166(1):267–275. doi: 10.1007/s10549-017-4399-x [DOI] [PubMed] [Google Scholar]
- 21.Shreders AJ, Niazi SK, Hodge DO, et al. Correlation of sociodemographic and clinical parameters with depression and distress in patients with hematologic malignancies. Ann Hematol. 2018;97(3):519–528. doi: 10.1007/s00277-017-3198-0 [DOI] [PubMed] [Google Scholar]
- 22.Clinton-McHarg T, Carey M, Sanson-Fisher R, Tzelepis F, Bryant J, Williamson A. Anxiety and depression among haematological cancer patients attending treatment centres: prevalence and predictors. J Affect Disord. 2014;165:176–181. doi: 10.1016/j.jad.2014.04.072 [DOI] [PubMed] [Google Scholar]
- 23.Klepin HD, Geiger AM, Tooze JA, et al. Geriatric assessment predicts survival for older adults receiving induction chemotherapy for acute myelogenous leukemia. Blood. 2013;121(21):4287–4294. doi: 10.1182/blood-2012-12-471680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Angehrn A, Teale SM, Ricciardelli R, MacPhee RS, Anderson GS, Carleton RN. Sleep quality and mental disorder symptoms among Canadian public safety personnel. Int J Environ Res Public Health. 2020;17(8):2708. doi: 10.3390/ijerph17082708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cavalheiri JC, Pascotto CR, Tonini NS, Vieira AP, Ferreto L, Follador F. Sleep quality and common mental disorder in the hospital nursing team. Rev Lat Am Enfermagem. 2021;29:e3444. doi: 10.1590/1518-8345.4280.3444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li J, Cao D, Huang Y, et al. Sleep duration and health outcomes: an umbrella review. Sleep Breath. 2021. doi: 10.1007/s11325-021-02458-1 [DOI] [PubMed] [Google Scholar]
- 27.Erren TC. Sleep duration and cancer risk: time to use a “sleep-years” index? Cancer Causes Control. 2012;23(9):1399–1403. doi: 10.1007/s10552-012-0027-6 [DOI] [PubMed] [Google Scholar]
- 28.Ordway MR, Wang G, Jeon S, Owens J. Role of sleep duration in the association between socioecological protective factors and health risk behaviors in adolescents. J Dev Behav Pediatr. 2020;41(2):117–127. doi: 10.1097/DBP.0000000000000721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williams JM, Kay DB, Rowe M, McCrae CS. Sleep discrepancy, sleep complaint, and poor sleep among older adults. J Gerontol B Psychol Sci Soc Sci. 2013;68(5):712–720. doi: 10.1093/geronb/gbt030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhai L, Zhang H, Zhang D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety. 2015;32(9):664–670. doi: 10.1002/da.22386 [DOI] [PubMed] [Google Scholar]
- 31.Liu F, Yang Y, Wang S, et al. Impact of sleep duration on depression and anxiety after acute ischemic stroke. Front Neurol. 2021;12:630638. doi: 10.3389/fneur.2021.630638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zung WW. A self-rating depression scale. Arch Gen Psychiatry. 1965;12(1):63–70. doi: 10.1001/archpsyc.1965.01720310065008 [DOI] [PubMed] [Google Scholar]
- 33.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0 [DOI] [PubMed] [Google Scholar]
- 34.Wong WS, Fielding R. Construct validity of the Chinese version of the Chalder Fatigue Scale in a Chinese community sample. J Psychosom Res. 2010;68(1):89–93. doi: 10.1016/j.jpsychores.2009.05.008 [DOI] [PubMed] [Google Scholar]
- 35.Chalder T, Berelowitz G, Pawlikowska T, et al. Development of a fatigue scale. J Psychosom Res. 1993;37(2):147–153. doi: 10.1016/0022-3999(93)90081-p [DOI] [PubMed] [Google Scholar]
- 36.Basudan S, Binanzan N, Alhassan A. Depression, anxiety and stress in dental students. Int J Med Educ. 2017;8:179–186. doi: 10.5116/ijme.5910.b961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gao W, Ping S, Liu X. Gender differences in depression, anxiety, and stress among college students: a longitudinal study from China. J Affect Disord. 2020;263:292–300. doi: 10.1016/j.jad.2019.11.121 [DOI] [PubMed] [Google Scholar]
- 38.Pantzar A, Atti AR, Fratiglioni L, Fastbom J, Backman L, Laukka EJ. Cognitive performance in unipolar old-age depression: a longitudinal study. Int J Geriatr Psychiatry. 2017;32(6):675–684. doi: 10.1002/gps.4510 [DOI] [PubMed] [Google Scholar]
- 39.Pantzar A, Laukka EJ, Atti AR, Fastbom J, Fratiglioni L, Backman L. Cognitive deficits in unipolar old-age depression: a population-based study. Psychol Med. 2014;44(5):937–947. doi: 10.1017/S0033291713001736 [DOI] [PubMed] [Google Scholar]
- 40.Maiera E. Old age depression and its treatment. Psychiatr Danub. 2010;22(Suppl 1):S124–S125. [PubMed] [Google Scholar]
- 41.Schwartz JE, Jandorf L, Krupp LB. The measurement of fatigue: a new instrument. J Psychosom Res. 1993;37(7):753–762. doi: 10.1016/0022-3999(93)90104-N [DOI] [PubMed] [Google Scholar]
- 42.Aaronson LS, Teel CS, Cassmeyer V, et al. Defining and measuring fatigue. Image J Nurs Sch. 1999;31(1):45–50. doi: 10.1111/j.1547-5069.1999.tb00420.x [DOI] [PubMed] [Google Scholar]
- 43.Engl T, Drescher D, Bickeboller R, Grabhorn R. Fatigue, depression, and quality of life in patients with prostatic diseases. Cent Eur J Urol. 2017;70(1):44–47. doi: 10.5173/ceju.2017.940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jain A, Sharma R, Choudhary PK, Yadav N, Jain G, Maanju M. Study of fatigue, depression, and associated factors in type 2 diabetes mellitus in industrial workers. Ind Psychiatry J. 2015;24(2):179–184. doi: 10.4103/0972-6748.181731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Azimian M, Shahvarughi-Farahani A, Rahgozar M, Etemadifar M, Nasr Z. Fatigue, depression, and physical impairment in multiple sclerosis. Iran J Neurol. 2014;13(2):105–107. [PMC free article] [PubMed] [Google Scholar]
- 46.Jenkins CD, Stanton BA, Niemcryk SJ, Rose RM. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41(4):313–321. doi: 10.1016/0895-4356(88)90138-2 [DOI] [PubMed] [Google Scholar]
- 47.Morrison DN, McGee R, Stanton WR. Sleep problems in adolescence. J Am Acad Child Adolesc Psychiatry. 1992;31(1):94–99. doi: 10.1097/00004583-199201000-00014 [DOI] [PubMed] [Google Scholar]
- 48.Kuczmarski TM, Jaung T, Mancuso CE, et al. Precancer and cancer-associated depression and anxiety among older adults with blood cancers in the United States. Blood Adv. 2022;6(4):1126–1136. doi: 10.1182/bloodadvances.2021005862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rivas-Molina NS, Mireles-Perez EO, Soto-Padilla JM, Gonzalez-Reyes NA, Barajas-Serrano TL, Barrera DLJ. [Depression in school children and adolescents carriers of acute leukemia during the treatment phase]. Gac Med Mex. 2015;151(2):186–191. Spanish. [PubMed] [Google Scholar]
- 50.Castelli L, Elter T, Wolf F, et al. Sleep problems and their interaction with physical activity and fatigue in hematological cancer patients during onset of high dose chemotherapy. Support Care Cancer. 2022;30(1):167–176. doi: 10.1007/s00520-021-06377-5 [DOI] [PMC free article] [PubMed] [Google Scholar]