Abstract
Objective:
The proportion of fatal nontraffic injuries that involve high levels of alcohol use or alcohol intoxication was assessed by cause of injury to generate alcohol-attributable fractions (AAFs). Updated AAFs can contribute to improved estimates of the public health impact of excessive alcohol use.
Methods:
Peer-reviewed and “gray” literature for 1995–2019 on 15 causes of fatal nontraffic injuries in the United States, Canada, or Mexico were systematically reviewed, and state data systems were queried, for available estimates of fatalities with recorded blood alcohol content (BAC) levels and proportions of decedents with BACs ≥ 0.10g/dL by cause of injury. For each injury cause, AAFs across studies were synthesized by meta-analysis of single proportions using generalized linear mixed models.
Results:
In total, 60 published studies and 40 additional population-level data points from six state data systems were included. The meta-analyzed AAFs by cause of injury follow: air-space transport (0.03), aspiration (0.24), child maltreatment (0.09), drowning (0.31), fall injuries (0.37), fire injuries (0.34), firearm injuries (0.24), homicide (0.29), hypothermia (0.29), motor vehicle nontraffic crashes (0.42), occupational and machine injuries (0.08), other road vehicle crashes (railroad trespasser injuries) (0.63), poisoning (not alcohol) (0.20), suicide (0.21), and water transport (0.27), yielding an overall median AAF of 0.27.
Conclusions:
Excessive alcohol use is associated with substantial proportions of violent and non-violent injury deaths. These findings can improve the data used for estimating alcohol-attributable injury deaths and inform the planning and implementation of evidence-based strategies (e.g., increasing alcohol taxes, regulating alcohol outlet density) to prevent them.
INTRODUCTION
Excessive alcohol use is a leading cause of preventable death in the United States,1 and it was responsible for more than 95,000 deaths each year during 2011–2015.2 It is a risk factor for unintentional and intentional injuries.3 Binge drinking (i.e., the consumption of four or more drinks for women, or five or more drinks for men, on an occasion or in about a 2-hour period, which generally raises one’s blood alcohol concentration [BAC] level to 0.08 g/dL or higher) is associated with an increase in the likelihood of fatal injuries.2,4 Nearly one-seventh of U.S. high school students reported binge drinking in 2019,5 as did one-sixth of adults in 2018; and 25% of adults did so at least weekly.6
Alcohol-attributable fractions (AAFs) measure the contribution of alcohol use to a given health outcome or cause of death and are important for estimating alcohol-related morbidity and mortality. Direct estimates of AAFs (i.e., the proportion of persons dying from a particular alcohol attributable condition that had a BAC above a specified level) are often used to measure the contribution of alcohol to acute causes of death, such as injuries. With approximately 10,000 deaths from alcohol-impaired driving recorded each year, AAFs for fatal motor vehicle crashes are well-monitored in the U.S. relative to other causes of alcohol-related injuries, and such data are accessible from the Fatality Analysis Reporting System.7
Earlier reviews have examined the role of alcohol use in fatal injuries.8–10 However, limited current data are available on alcohol involvement in fatal nontraffic injuries, and more are needed to improve estimates of the public health burden of excessive alcohol use. The most recent meta-analysis on alcohol involvement in fatal nontraffic injuries in the U.S. was published more than 20 years ago using data from medical examiner reports from 1975 to 1995.9 Given the increases in binge drinking and alcohol-related emergency department visits since then,11–13 findings from earlier studies may no longer reflect the current situation. For example, binge drinking is a risk factor for other substance use,14 and high levels of alcohol are commonly involved in drug overdoses.15 Use of alcohol at the same time as benzodiazepines or opioids can increase the risk of a fatal overdose.16 With the rise in drug overdose deaths,17 the extent to which high levels of alcohol are involved in fatal drug overdoses and other poisonings may have changed since earlier reviews.
The purpose of this systematic review and meta-analysis is to assess the proportion of fatal nontraffic injuries that involve high levels of alcohol (BAC ≥ 0.10 g/dL or indications of alcohol intoxication) by cause of injury. The results from this meta-analysis can improve the data used for estimating alcohol-attributable deaths from nontraffic injuries, such as in data systems that rely on AAFs (e.g., the Centers for Disease Control and Prevention’s [CDC] Alcohol-Related Disease Impact [ARDI] application). The findings from this study could also inform the planning and implementation of evidence-based population-level strategies18 to reduce binge drinking and associated injuries and deaths.
METHODS
Fifteen mutually exclusive acute causes of death from alcohol-attributable nontraffic-related injuries were included in this systematic review and meta-analysis: air-space transport, aspiration, child maltreatment, drowning, poisoning (not alcohol), fall injuries, fire injuries, firearm injuries, homicide, hypothermia, motor vehicle nontraffic crashes, other road vehicle crashes, occupational and machine injuries, suicide, and water transport. These categories align with the acute causes of death from partially alcohol-attributable nontraffic-related injuries that are used in the CDC’s ARDI application19 and are identified primarily by International Classification of Diseases (ICD)-9 and ICD-10 codes (Appendix 1). Deaths from homicide or suicide are characterized as being intentional injuries. Deaths from child maltreatment included unintentional and intentional injuries. All other causes of death included only unintentional injuries.
The CDC’s ARDI application is a comprehensive tool for estimating state and national alcohol-attributable deaths and years of potential life lost from nearly 60 causes of alcohol-related death. Data on alcohol-related deaths from chronic conditions were not included in this study, nor were injuries that are fully alcohol-attributable (e.g., alcohol poisoning). Fully alcohol-attributable deaths (AAF = 1.0) are those that would not occur in the absence of alcohol; therefore, no estimation is required. Since annual AAFs for fatal motor vehicle traffic crashes are available from the Fatality Analysis Reporting System,20 they are not estimated in this meta-analysis, though they are included in ARDI. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines were followed.21 This study involved secondary analyses of deidentified data; therefore, Institutional Review Board oversight was not required.
Search Strategy
For each of the 15 causes of fatal nontraffic injuries, published studies in peer-reviewed journals, government reports (e.g., medical examiners’ reports), and other “gray” literature were systematically reviewed to identify studies, reports, and data systems that independently assessed alcohol involvement. Boolean algorithms were submitted to literature search engines that index relevant published studies, including PubMed, Science Direct, Web of Science, Cochrane Central, EMBASE, SCOPUS, CINAHL, Google Scholar, and Epistomonikos. Gray literature was also searched to capture data from sources that might not otherwise be available in the peer-reviewed literature (Appendix 2),22 including proceedings of professional association meetings, coroners’ and medical examiners’ reports, and U.S. federal and state government and Canadian reports.
State health surveillance systems, vital death records, and medical examiner/coroner offices have traditionally been the primary sources of data underlying fatal injury AAFs. Therefore, between January 2020 and August 2020, emails were sent to health departments or medical examiner government offices in 20 states that have centralized medical examiner systems or an epidemiologist working on alcohol. Each was provided with a table specifying the 15 causes of fatal injuries and the cause-specific ICD-10 codes. Recent five years of data were requested to calculate the number of fatalities with a valid BAC test result and the number of decedents with BAC ≥ 0.10 g/dL, by cause of injury.
An iterative, snowball search strategy was employed,23 scanning reference lists and authors’ names of primary sources identified as well as citations to studies ascertained through Web of Science to ensure literature saturation. This approach can be particularly effective in systematic reviews of multidisciplinary areas such as alcohol involvement in fatal injuries since primary sources may reference other reports with relevant data or additional literature from other fields. The ICD-9 and ICD-10 codes from the CDC’s ARDI application were used to identify literature on the 15 types of injuries.24 Systematic reviews were conducted from October 2019 through October 2020. Appendix 2 contains details of the search strategy.
Inclusion criteria
Inclusion criteria consisted of studies and reports on any of the 15 causes of fatal nontraffic injuries published from 1995 through 2019, or data from state systems during this period; involving human subjects; based in the United States, Canada, or Mexico; and written in English. The search started with 1995, being the final year of reports included in the prior comprehensive meta-analysis on alcohol-related nontraffic injuries.9
Studies were primarily sought that reported direct AAF estimates or included data to directly assess AAFs (i.e., the proportion of persons that died of a particular injury with BAC ≥ 0.10 g/dL at the time of injury among those who had a valid BAC test). In other words, AAF is an estimate of the percentage of deaths that are attributed to alcohol. Consistent with the CDC’s ARDI application, 0.10 g/dL was used as the threshold for determining alcohol involvement instead of 0.08 g/dL (a common threshold level for acute intoxication). Injury fatalities can be due to many non-alcohol-related factors, and the higher BAC threshold provides a greater level of assurance for a death being attributable to alcohol.9,25 Alcohol measurements from tissues other than blood were not included because of limited comparability with more common BAC measures.9 BAC measurements are typically, although not always, obtained during injury death investigations conducted by medical examiners, coroners, or other government officials (e.g., forensic toxicology laboratories). These measurements are often included in state and local health surveillance and vital death records systems. Studies in which the AAF was equal to zero were included if selection bias was not suspected. A minimum sample size of at least five decedents with BAC test results per cause of death was required for inclusion.
Upon completion of comprehensive full-text reviews, minimal studies with suitable BAC data were identified for seven fatal injury causes (aspiration, child maltreatment, fall injuries, homicide, hypothermia, occupational and machine injuries, and other road vehicle crashes). Therefore, the inclusion criteria were broadened for these to include descriptions of alcohol intoxication that would approximate BAC ≥ 0.10 g/dL (i.e., alcohol intoxication, alcohol impaired, inebriated, under the influence, drunk, or alcohol was a factor). This broader approach aligns with the seminal English and Holman meta-analysis on alcohol and numerous related outcomes.10 Since our study reports AAFs by cause of injury, AAFs for the aforementioned seven causes can be viewed separately from AAFs for the other causes. Appendix 1 provides further details on study inclusion by cause of death.
All citations identified in the systematic literature reviews were compiled and managed in an EndNote reference management database after initial screening for eligibility by a bibliographic research librarian (N.W.) based on cause of injury, location, and presence of BAC information. Prior to data abstraction, two investigators closely examined the full-text reports for specificity and linkage of BAC information with fatal injuries, minimum sample size requirements, remaining eligibility criteria, and any redundancies among reports. Each eligible source was compared with the remaining reports with respect to dates, places of data collection, and populations sampled to exclude duplicates. When the same underlying data were reported by more than one source, the source with the largest number of decedents was included.
Data abstraction and quality assessments
Data abstraction forms were developed to collect the following information from each published report: report information (e.g., data source type, funding source); study eligibility (e.g., causes of death, BAC or alcohol intoxication data); study setting; population characteristics; methodology, including study design, sampling frame, selection criteria, fatal injury data sources, and BAC sources and timing; effect size, including the numbers of decedents, BAC tests, BAC test results ≥ 0.10 g/dL, and missing or unreported BAC tests; and risk of bias assessment.
The risk of bias assessment for individual studies was adapted from the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach.26 The GRADE approach uses specific evaluation criteria to identify the subset of studies likely to yield the most accurate approximation of the effect size of alcohol on each cause of death. It allows for optimal objectivity and clear communication of any subjective judgements. Consistent with this approach, two primary investigators with formal epidemiologic training and experience evaluating quality and risk of bias in research (H.R.A., C.M.C.) independently performed data abstraction and evaluation. Discrepancies were adjudicated by a third epidemiologist-investigator (M.E.S.), and any remaining issues were discussed and resolved among all investigators prior to analysis. Calibration exercises were held using clear instructions with explicit evaluation criteria, and a structured approach was employed to ensure transparency.
The potential study-level biases (selection bias, imprecision, missing data, external validity, and reporting bias) relevant to measures of direct AAF estimates (i.e., incidence and proportions) for fatal nontraffic injuries were evaluated following the PRISMA statement and GRADE recommendations.21,27 Evaluation of non-peer-reviewed data considered internal consistency, reliability, and face validity of the sources. The risk of bias score was increased by one point for each type of bias judged to potentially influence the accuracy or precision of the AAF significantly. Points were summed for an overall rating of each study. Published studies that met inclusion criteria were selected for analysis if they had risk of bias scores no greater than three. In the absence of suitably defined data, emails were sent to authors of eight potentially eligible studies requesting clarification of reported BAC data or other important missing information, or to resolve observed inconsistencies.
Statistical analysis
Data abstracted included the numerator and denominator of the study-level AAF for each cause of death. The numerator was defined as the number of deaths where the decedent (or offender in homicide and child maltreatment cases) either had BAC ≥ 0.10 g/dL or was reported to be alcohol intoxicated. The denominator was defined as the number of deaths where the decedent (or offender) had either a valid BAC test result or descriptive indication of alcohol involvement. For each cause of death, AAFs across studies were synthesized by meta-analysis of single proportions using generalized linear mixed models (GLMMs). GLMM was used rather than alternative methods (e.g., standard inverse variance methods such as Freeman-Tukey double arcsine transformation) because it avoids potential problems with back-transformations by considering the binomial structure of AAF data.28 The results were summarized in forest plots, which included point estimates and 95% confidence intervals (CI), to facilitate visual inspection of study heterogeneity. In addition, the I2 statistic29 was calculated to quantify the percentage of total variance contributed by between-study variance. The meta-analyzed AAFs were derived from the random-effects model, regardless of study heterogeneity. The analysis was conducted using the meta and metafor packages30, 31 implemented in R 4.0.5.32 A sensitivity analysis was conducted by analyzing US-only data to assess whether results were biased by the inclusion of data from Canadian studies for six causes of death (aspiration, drowning, hypothermia, occupational and machine injuries, suicide, and water transport).
RESULTS
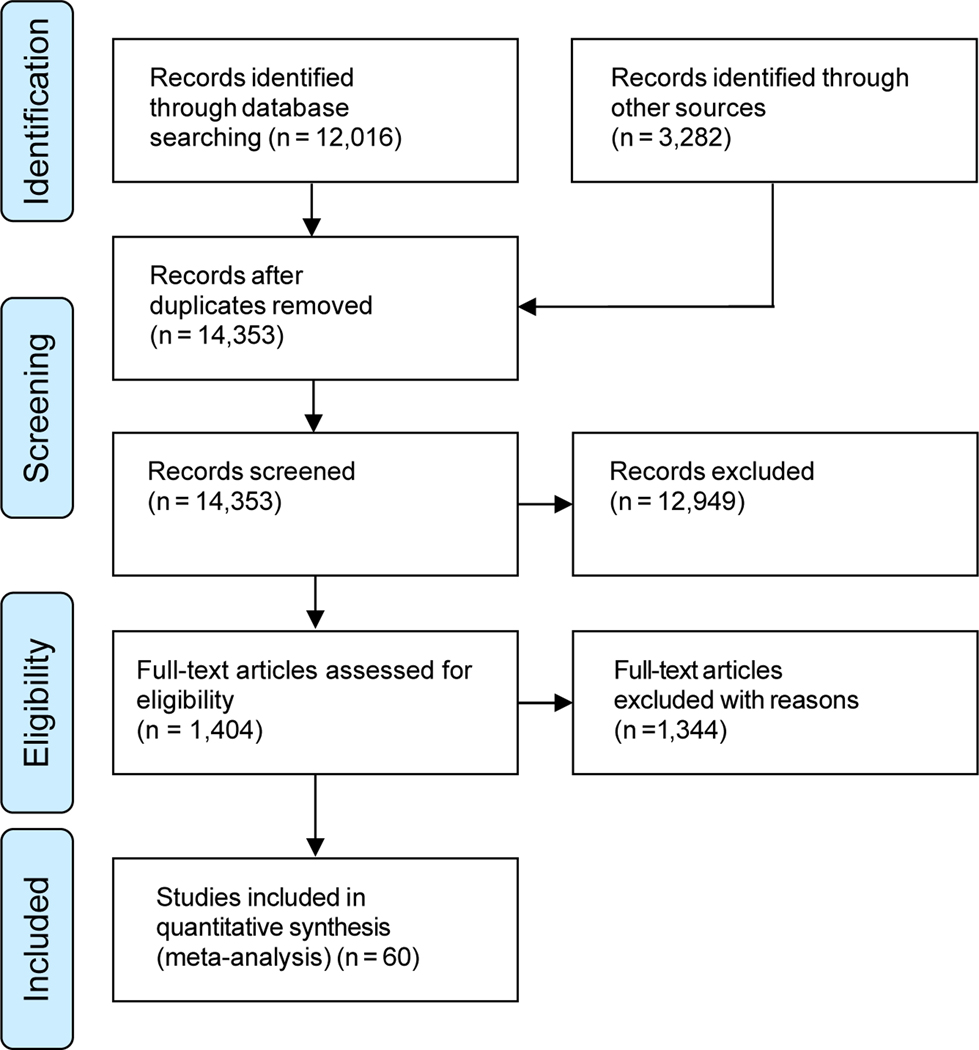
The data in this meta-analysis were sourced from a total of 60 published studies (Figure 1) and six state data and surveillance systems (Colorado, Michigan, Minnesota, North Carolina, Utah, and Virginia) that provided data for 40 AAF estimates. Overall, data were included from 28 U.S. states, five national-level U.S. studies, and six Canadian studies. Characteristics of individual data sources, including study-level AAFs used for calculating the meta-analyzed AAFs, are presented in Table 1. The number of original data sources included in the meta-analyses varied by cause of death, ranging from two for fall injuries to 19 for suicide (Figure 2). Risk of bias score totals were similar between investigators and reflected low risk of bias within and across included studies (Table 1).
Figure 1:
Flowchart of selection of studies for inclusion in meta-analysis
Table 1.
Study characteristics and risk of bias scores for 15 causes of fatal nontraffic injuries.
| Studies by Cause of Death | Dates of Injuries | Geographical Location | BAC ≥ 0.10g/dL | BAC Tests (N) | Alcohol-Attributable Fraction | Risk of Bias Scorea |
|---|---|---|---|---|---|---|
| Air-space transport | ||||||
| Botch et al. (2009)64b | 1997–2007 | United States | 1 | 139 | 0.01 | 2 |
| Botch et al. (2008)65b | 2000–2007 | United States | 8 | 215 | 0.04 | 2 |
| Li et al. (1998)66 | 1985–1994 | North Carolina | 4 | 101 | 0.04 | 2 |
| Virginia data system | 2014–2018 | Virginia | 0 | 17 | 0.00 | NA |
| Utah data system | 2014–2018 | Utah | 0 | 13 | 0.00 | NA |
| Aspiration | ||||||
| Boghossian et al. (2010)67c | 2000–2005 | Quebec, Canada | 2 | 11 | 0.18 | 1 |
| Virginia data system | 2014–2018 | Virginia | 4 | 50 | 0.08 | NA |
| Utah data system | 2014–2018 | Utah | 5 | 26 | 0.19 | NA |
| North Carolina data system | 2014–2019 | North Carolina | 15 | 21 | 0.71 | NA |
| Child maltreatment | ||||||
| Colorado CFPS (2021)68c | 2009–2018 | Colorado | 41 | 452 | 0.09 | 2 |
| Parks et al. (2011)69c | 2005–2007 | Texas | 25 | 260 | 0.10 | 1 |
| South Carolina SCFAC (2019)70c | 7/1/2018–6/30/2019 | South Carolina | 15 | 145 | 0.10 | 2 |
| Drowning | ||||||
| Okuda et al. (2015)71 | 2003–2013 | Maryland | 8 | 57 | 0.14 | 2 |
| Cummings & Quan (1999)72 | 1975–1995 | King County, Washington | 91 | 304 | 0.30 | 2 |
| Browne et al. (2003)73 | 1988–1994 | New York | 58 | 178 | 0.33 | 2 |
| Canadian Red Cross Society (2006)74 | 1991–2000 | Canada | 583 | 1,500 | 0.39 | 0 |
| Lincoln et al. (1996)75 | 1988–1992 | Alaska | 94 | 186 | 0.51 | 3 |
| Utah data system | 2014–2018 | Utah | 11 | 130 | 0.08 | NA |
| Virginia data system | 2014–2018 | Virginia | 83 | 346 | 0.24 | NA |
| Minnesota data system | 2014–2018 | Minnesota | 49 | 136 | 0.36 | NA |
| North Carolina data system | 2014–2019 | North Carolina | 131 | 230 | 0.57 | NA |
| Fall injuries | ||||||
| Virginia data system | 2014–2018 | Virginia | 89 | 760 | 0.12 | NA |
| North Carolina data system | 2014–2019 | North Carolina | 116 | 159 | 0.73 | NA |
| Fire injuries | ||||||
| Levine et al. (2001)76 | 3-year period prior to 2001 | Maryland | 45 | 196 | 0.23 | 1 |
| Tridata Corporation (1999)77 | 1993–1996 | Minnesota | 67 | 255 | 0.26 | 2 |
| US Fire Administration (2003)78 | 1996–2002 | Minnesota | 113 | 374 | 0.30 | 0 |
| McGwin et al. (2000)79 | 1992–1997 | Alabama | 114 | 247 | 0.46 | 2 |
| Marshall et al. (1998)80 | 2/1/1988–1/31/1989 | North Carolina | 69 | 130 | 0.53 | 0 |
| Utah data system | 2014–2018 | Utah | 5 | 40 | 0.12 | NA |
| Virginia data system | 2014–2018 | Virginia | 51 | 338 | 0.15 | NA |
| North Carolina data system | 2014–2019 | North Carolina | 80 | 100 | 0.80 | NA |
| Firearm injuries | ||||||
| Cherry et al. (2001)81 | 1985–1994 | North Carolina | 55 | 351 | 0.16 | 0 |
| Collins (2010)82 | 1987–2006 | South Carolina | 2 | 7 | 0.29 | 2 |
| Shields et al. (2008)83 | 1993–2002 | Kentucky | 10 | 20 | 0.50 | 3 |
| Minnesota data system | 2015–2018 | Minnesota | 1 | 17 | 0.06 | NA |
| Virginia data system | 2014–2018 | Virginia | 7 | 67 | 0.10 | NA |
| Colorado data system | 2014–2018 | Colorado | 10 | 42 | 0.24 | NA |
| Utah data system | 2014–2018 | Utah | 9 | 30 | 0.30 | NA |
| North Carolina data system | 2014–2019 | North Carolina | 11 | 19 | 0.58 | NA |
| Homicide | ||||||
| Spunt et al. (1998)84c | 1992–1993 | New York | 41 | 181 | 0.23 | 2 |
| Spunt et al. (1995)85c | 1984 | New York | 86 | 269 | 0.32 | 2 |
| Banks et al. (2008)86 | 1993–2002 | New Mexico | 12 | 37 | 0.32 | 2 |
| Greenfeld (1998)87 | 1996 | United States | 65 | 173 | 0.38 | 2 |
| Utah data system | 2014–2018 | Utah | 6 | 39 | 0.15 | NA |
| Hypothermia | ||||||
| Koutsavlis et al. (2003)88c | 1994–1998 | Montreal Island & Ile-Bizard, Quebec, Canada |
3 | 12 | 0.25 | 2 |
| Utah data system | 2014–2018 | Utah | 13 | 55 | 0.24 | NA |
| Virginia data system | 2014–2018 | Virginia | 26 | 101 | 0.26 | NA |
| North Carolina data system | 2014–2019 | North Carolina | 11 | 21 | 0.52 | NA |
| Motor vehicle nontraffic crashes | ||||||
| Minnesota DNR (2002–2010)89 | 2002–2010 | Minnesota | 44 | 166 | 0.27 | 1 |
| Hall et al. (2009)90 | 2004–2006 | West Virginia | 23 | 52 | 0.44 | 1 |
| Wisconsin DNR (2002–2020)91d | 2002–2020 | Wisconsin | 118 | 245 | 0.48 | 1 |
| Minnesota DNR (2001–2015)89 | 2001–2015 | Minnesota | 81 | 165 | 0.49 | 1 |
| Wisconsin DNR (2001–2020)92d | 2001–2020 | Wisconsin | 206 | 343 | 0.60 | 1 |
| Landen et al. (1999)93 | 1990–1994 | Alaska | 11 | 17 | 0.65 | 2 |
| Utah data system | 2014–2018 | Utah | 5 | 48 | 0.10 | NA |
| Occupational and machine injuries | ||||||
| West et al. (1996)94 | 1986–1991 | Ontario, Canada | 0 | 24 | 0.00 | 3 |
| Foster & Dissanaike (2014)95 | 2007–2011 | Texas | 0 | 11 | 0.00 | 3 |
| Davis & Brissie (2000)96 | 1981–1996 | Jefferson County, Alabama | 0 | 10 | 0.00 | 2 |
| Fullerton et al. (1995)97 | 1980–1991 | New Mexico | 29 | 449 | 0.06 | 1 |
| Lucas & Lincoln (2007)98c | 1990–2005 | Alaska | 14 | 71 | 0.20 | 2 |
| Utah data system | 2014–2018 | Utah | 1 | 5 | 0.20 | NA |
| North Carolina data system | 2014–2019 | North Carolina | 3 | 7 | 0.43 | NA |
| Other road vehicle crashes (railroad trespasser injuries) | ||||||
| North American Management (2013)52c | 2005–2010 | United States | 470 | 940 | 0.50 | 1 |
| CDC (1999)53 | 1990–1996 | Georgia | 40 | 78 | 0.51 | 2 |
| Pelletier et al. (1997)51 | 1990–1994 | North Carolina | 100 | 125 | 0.80 | 1 |
| North Carolina data system | 2014–2019 | North Carolina | 33 | 48 | 0.69 | NA |
| Poisoning (not alcohol) | ||||||
| Przepyszny & Jenkins (2007)99 | 2000–2003 | Cuyahoga County, Ohio | 19 | 84 | 0.23 | 1 |
| Moolenaar et al. (1995)100 | 1980–1988 | New Mexico | 17 | 74 | 0.23 | 2 |
| Levine et al. (1995)101 | A 12-month period prior to 1995 | Maryland | 48 | 119 | 0.40 | 2 |
| Utah data system | 2014–2018 | Utah | 170 | 1,719 | 0.10 | NA |
| Michigan data system | 2017–2018 | Michigan | 475 | 4,081 | 0.12 | NA |
| Virginia data system | 2014–2018 | Virginia | 668 | 5,576 | 0.12 | NA |
| Minnesota data system | 2019 | Minnesota | 60 | 500 | 0.12 | NA |
| North Carolina data system | 2014–2019 | North Carolina | 1,126 | 2,388 | 0.47 | NA |
| Suicide | ||||||
| Weinberger et al. (2001)102 | 1996–1997 | Los Angeles County, California | 1 | 46 | 0.02 | 3 |
| Lewis et al. (2007)103 | 1993–2002 | United States | 0 | 14 | 0.00 | 2 |
| San Nicolas & Lemos (2015)104 | 2011–2013 | San Francisco County, California | 14 | 102 | 0.14 | 1 |
| Bullock & Diniz (2000)105 | 1993–1997 | Ontario, Canada | 11 | 77 | 0.14 | 2 |
| Davis (1999)106 | 1994–1998 | Broward County, Florida | 4 | 24 | 0.17 | 2 |
| Wolford-Clevenger et al. (2020)107 | 2013–2019 | Jefferson County, Alabama | 75 | 447 | 0.17 | 1 |
| Cherpitel et al. (1996)108 | 12/1987–11/1988 and 02/1992–01/1993 |
Contra Costa County, California & Hinds County, Mississippi | 17 | 101 | 0.17 | 1 |
| Fisher et al. (2015)109 | 1994–2008 | Cuyohoga County, Ohio | 380 | 2,178 | 0.17 | 1 |
| Branas et al. (2011)110 | 2003–2006 | Philadelphia, Pennsylvania | 24 | 123 | 0.20 | 2 |
| Kaplan et al. (2012)111 | 2003–2009 | 16 statese | 7,777 | 39,579 | 0.20 | 0 |
| Shields et al. (2006, 2008)83, 112 | 1993–2002 | Kentucky | 656 | 2,702 | 0.24 | 0 |
| Przepyszny & Jenkins (2007)99 | 2000–2003 | Cuyohoga County, Ohio | 8 | 31 | 0.26 | 1 |
| Conner et al. (2016)113 | 2012 | New Mexico | 88 | 224 | 0.39 | 3 |
| Utah data system | 2014–2017 | Utah | 485 | 2,416 | 0.20 | NA |
| Virginia data system | 2014–2018 | Virginia | 493 | 2,417 | 0.20 | NA |
| Minnesota data system | 2015–2018 | Minnesota | 588 | 2,490 | 0.24 | NA |
| Colorado data system | 2014–2018 | Colorado | 1,038 | 4,221 | 0.25 | NA |
| Michigan data system | 2014–2018 | Michigan | 962 | 3,645 | 0.26 | NA |
| North Carolina data system | 2014–2019 | North Carolina | 1,249 | 1,886 | 0.66 | NA |
| Water transport | ||||||
| New York State OPRHP (2013–2019)114 | 2013–2019 | New York | 14 | 83 | 0.17 | 2 |
| Wisconsin DNR (2004–2018)115 | 2004–2018 | Wisconsin | 37 | 170 | 0.22 | 1 |
| Browne et al. (2003)116 | 1988–1994 | New York | 18 | 73 | 0.25 | 2 |
| Smith et al. (2001)117 | 1990–1998 | Maryland & North Carolina | 60 | 221 | 0.27 | 1 |
| Barss (2011)118 | 1991–2008 | Canada | 565 | 1,923 | 0.29 | 1 |
| Virginia data system | 2014–2018 | Virginia | 3 | 7 | 0.43 | NA |
| Minnesota data system | 2014–2018 | Minnesota | 20 | 45 | 0.44 | NA |
BAC, Blood Alcohol Concentration; NA, Not applicable; CFPS, Child Fatality Prevention System; DNR, Department of Natural Resources; OPRHP, Office of Parks, Recreation & Historic Preservation; SCFAC, State Child Fatality Advisory Committee.
State data systems were not assigned a risk of bias score.
Cases are from separate, nonoverlapping samples in Botch et al. reports.
Data were based on descriptive reports of alcohol intoxication, drunkenness, or alcohol being a factor involved in the fatalities.
Cases are from separate, nonoverlapping samples (including snowmobiles and all-terrain vehicles) in the Wisconsin Department of Natural Resources motor vehicle nontraffic crash reports.
States included were Alaska, Colorado, Georgia, Kentucky, Maryland, Massachusetts, New Jersey, New Mexico, North Carolina, Oklahoma, Oregon, Rhode Island, South Carolina, Utah, Virginia, Wisconsin.
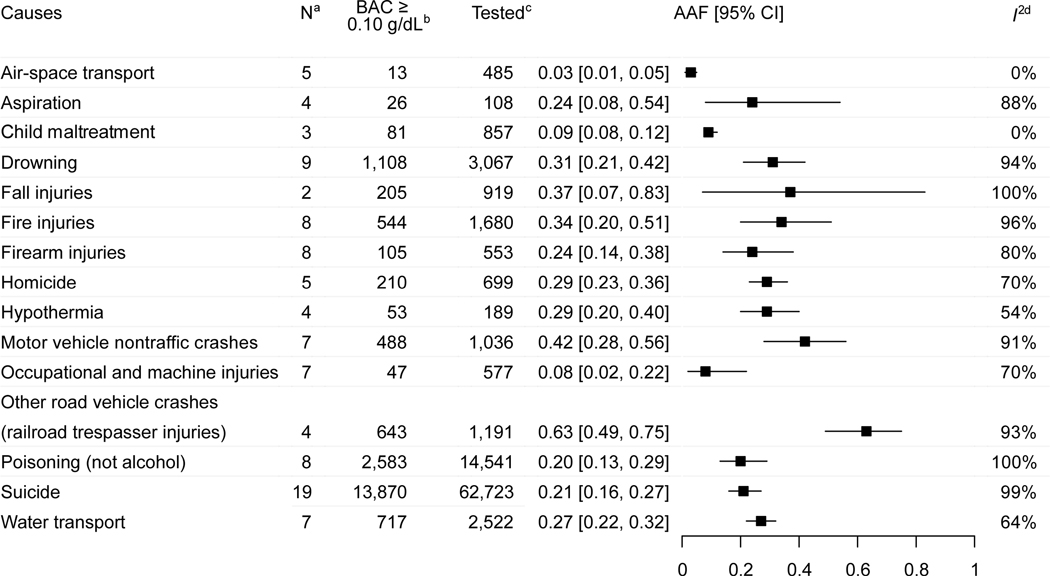
Figure 2:
Meta-analysis of alcohol-attributable fractions for 15 causes of fatal nontraffic injuries
a N: Total number of studies and data from states included for a given cause of fatal injury.
b BAC ≥ 0.10 g/dL: Number of deaths where the involved decedent (or offender in homicide and child maltreatment cases) had Blood Alcohol Concentration (BAC) ≥ 0.10 g/dL or were reported to be alcohol intoxicated.
c Tested: Number of deaths where the involved decedent (or offender in homicide and child maltreatment cases) had either valid BAC test results or valid measures of alcohol involvement.
d I²: a statistic that describes the percentage of variation across studies that is due to heterogeneity rather than chance.
AAF: Alcohol-Attributable Fraction; CI: Confidence Interval.
The meta-analysis results for the 15 causes of fatal nontraffic injuries are summarized in Figure 2, including AAFs and associated 95% CIs. In alphabetical order, the AAFs were: air-space transport (0.03), aspiration (0.24), child maltreatment (0.09), drowning (0.31), fall injuries (0.37), fire injuries (0.34), firearm injuries (0.24), homicide (0.29), hypothermia (0.29), motor vehicle nontraffic crashes (0.42), occupational and machine injuries (0.08), other road vehicle crashes (railroad trespasser injuries) (0.63), poisoning (not alcohol) (0.20), suicide (0.21), and water transport (0.27). The AAF for each cause of death can be interpreted as the percent of deaths attributable to alcohol among those with known BAC levels or intoxication status. For example, 24% of 553 firearm injury deaths with known BAC levels were attributable to alcohol. In sensitivity analyses, no statistically significant differences (based on overlapping 95% CIs) were observed between AAFs derived with and without inclusion of Canadian data (Appendix 4). Overall, cause-specific analyses yielded a median AAF of 0.27. Study heterogeneity, based on I2, varied by cause of death, ranging from 0% for air-space transport and child maltreatment to 100% for fall injuries and poisoning (not alcohol) (Appendix 3).
DISCUSSION
This study is the most current and comprehensive systematic review and meta-analysis assessing involvement of excessive alcohol use in deaths from 15 causes of fatal nontraffic injuries. The study shows that excessive drinking was associated with more than one-quarter of violent and non-violent injury deaths. For example, the findings show that almost one in four unintentional firearm injury deaths, one in three homicides, one in five poisonings (not alcohol), and one in five suicides involved alcohol, with a BAC ≥ 0.10 g/dL or a descriptive indication of alcohol intoxication. The mechanisms by which excessive drinking might lead to these deaths could include the effects of alcohol and impaired brain function resulting in poor judgment; slow decision-making and reaction time; reduced perception and response to hazards; loss of balance and motor skills; and through behavioral effects, such as increased risk-taking, reduced inhibitions, reduced processing of communications, and increased aggression.8,33,34 Some effects of alcohol, including impairment in judgment and motor dysfunction, are apparent at BAC levels less than 0.10 g/dL.35
AAF estimates were determined in this study using the direct method, which is based on the proportion of deaths from a given cause of injury due to alcohol. This method has advantages compared with approaches for estimating alcohol-related injury fatalities that are not based on individual causes of death. For example, applying continuous distributions that consider the prevalence of alcohol use and the relative risk of dying from a given injury to the estimated number of deaths from that injury generally involves aggregating alcohol-attributable injuries into broad categories (e.g., road injuries, other unintentional injuries, intentional injuries).36 This is because limited cause-specific data are available to inform risk functions. Others have indicated that a systematic review of data from medical examiners and coroners’ reports on the contribution of alcohol to injury deaths, such as those used in the present study, might be more accurate than estimates generated from continuous risk functions.37
Unlike other studies on alcohol-related homicides that rely on BAC among victims, a strength of this study is that it uniquely considered alcohol intoxication among homicide offenders.38 Offender BACs for homicides and child maltreatment are typically not collected by state data and surveillance systems. Sources of homicide and maltreatment data in this study used either offender BAC, or alternatively, observer or self-reports of alcohol intoxication among offenders.
Most of the poisoning (not alcohol) deaths in this study were from drug overdose fatalities that involved a BAC ≥ 0.10 g/dL. However, the AAF of 0.20 may underestimate the role of alcohol in drug overdose deaths because alcohol can contribute to overdoses at low levels, particularly when combined with substances such as opioids or benzodiazepines.39,40 Nevertheless, binge drinking is associated with use of other substances and increases the risk of concurrently misusing prescription drugs, which increases the chance of overdose.14
Limitations
This meta-analysis also has limitations. The contribution of alcohol to mortality is generally underestimated in studies, in part due to incomplete alcohol use documentation in death certificates.41,42 Alcohol testing rates among decedents vary by decedents’ characteristics (e.g., race/ethnicity), cause of death, and state of residence.42,43 State-level data in this study were from 28 states, including six state surveillance systems. Additional states did not provide data from their surveillance systems for reasons provided such as labor intensiveness and insufficient resources during the SARS-Cov-2 (COVID-19) pandemic. The inclusion of data from only some state data systems potentially introduces biases in the AAFs due to socioeconomic, demographic, policy environment, or social norm differences between states regarding drinking.
Because AAFs in this meta-analysis were calculated as a percentage among decedents tested for alcohol, the estimates might be high if decedents who were not tested for alcohol had consistently lower BAC levels. Testing rates, procedures for conducting postmortem BAC tests, and timing of alcohol testing (relative to both the time since alcohol was consumed and time after death) likely varied across states,43 although most potential systematic biases in BAC testing (e.g., lag between death and BAC test) likely led to conservative AAF estimates.37,44,45 Postmortem BACs used to estimate antemortem drinking can vary in either direction relative to antemortem BACs.43,44,46 Variability exists in AAFs from individual sources within causes of death. Some relatively extreme values might have contributed to non-statistically significant differences observed between random-effects and fixed-effect estimates for certain causes. These could also be partially explained by factors such as differences in alcohol use by sex, age, race/ethnicity, or location. However, sufficient data were not available to estimate AAFs by decedents’ characteristics; and observed variation in AAFs by location across individual sources improves generalizability.
The sensitivity analyses suggest that biases did not result from inclusion of Canadian data, although the AAFs in this meta-analysis might not reflect those that would be obtained from meta-analyses of exclusively Canadian data. The U.S. and Canada are comparable on several indicators of population-level alcohol consumption (e.g., per capita alcohol consumption, prevalence of heavy episodic drinking),47 though they may differ in other relevant aspects (e.g., implementation and enforcement of alcohol control policies). These AAFs also might not be generalizable to Mexico because only studies in English were searched.
There were some limitations because of the data available for certain causes of death. Deaths from poisonings have the potential for misclassification of intent (suicide versus unintentional) and for unobserved heterogeneity.48 For deaths from homicide and child maltreatment, BAC data among offenders are potentially limited because the offenders are often not apprehended immediately at the time of injury. Given the sensitive nature of child maltreatment deaths, further data on alcohol involvement in these deaths may be discovered from restricted sources, such as the National Child Death Review Case Reporting System.
For fall injuries, the AAF estimate was based on the data of more than 900 decedents, although high study heterogeneity between the two data sources and the wide 95% CIs suggest some uncertainty around the estimate. The extent to which excessive alcohol use contributes to deaths from falls might vary by age group. More data pertaining to the age distribution of decedents would be needed to differentially estimate alcohol-related falls among younger and older people. Nevertheless, falls contribute to a substantial number of deaths each year, especially among older adults;49 and a linear association has been documented between the amount of alcohol consumed and risk of fall injuries.50
Fatal injuries from other road vehicle crashes involve pedestrians or occupants who collide with or fall from pedal cycles, other nonmotor vehicles, or railway trains; however, the available studies of alcohol involvement in these deaths pertained solely to scenarios involving railroad trespassers (i.e., persons on railroad property whose presence was prohibited or unlawful). One of these studies documented that alcohol intoxication was the most frequently reported factor associated with these deaths,51 as when people walk across railroad tracks while intoxicated.52,53 The AAF for these circumstances might not be applicable to different situations of other road vehicle crash deaths.
Available data regarding air-space transport were limited to pilot fatalities. Data reported in one of the studies on aviation-related crashes suggests that the number of aviation passenger deaths per crash did not differ between crashes involving and not involving alcohol.54 The AAF for this cause of death may therefore be appropriate for estimating the total number of alcohol-attributable deaths among persons who die from air-space transport injuries.
Despite these limitations, the findings in this meta-analysis have public health implications. Effective population-level approaches for preventing excessive drinking include those recommended by the Community Preventive Services Task Force, such as strategies to decrease the availability of and access to alcohol or to increase alcohol prices.55–57 In addition to reducing the number and concentration of alcohol outlets, having dram shop liability laws to hold retailers accountable for harms incurred by service to intoxicated or underage patrons could also reduce alcohol-attributable injury deaths.56, 58 These population-level alcohol policies have been found to be associated with reductions in several causes of death, including homicides,59 suicides,60 and pedestrian injuries.61 Screening and brief interventions to reduce excessive alcohol use might also reduce alcohol-related injuries if delivered face-to-face in clinical settings or using electronic devices in a variety of settings (e.g., healthcare facilities, universities, workplaces).62, 63
CONCLUSIONS
The results of this meta-analysis show that a median of 27% of fatalities from nontraffic injuries are attributable to excessive alcohol use, which is a preventable risk behavior. The updated AAFs in this meta-analysis are fundamental for improving estimates of alcohol-attributable deaths (as in the CDC’s ARDI application) and for calculating the economic burden of excessive drinking. Such data are essential for establishing public health priorities. Future research would benefit from more routine and widespread data collection on alcohol involvement in nontraffic fatal injuries, particularly those where previous investigation has been lacking. Our findings underscore the importance of implementing and enforcing evidence-based strategies for preventing excessive drinking and designing and encouraging safer community environments.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the Colorado Department of Public Health and Environment, Michigan Department of Health and Human Services, Minnesota Department of Health, North Carolina Office of the Chief Medical Examiner, Utah Department of Health, and Virginia Office of the Chief Medical Examiner for state level fatality and blood alcohol concentration data.
This study was supported by the Centers for Disease Control and Prevention (CDC) of the U.S. Department of Health and Human Services (HHS), as part of a financial assistance award totaling $219,325.27 with 100% funded by CDC/HHS. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC.
Footnotes
None of the authors have any conflicts of interest or financial disclosures.
REFERENCES
- 1.Murray CJL, Mokdad AH, Ballestros K, et al. The state of US health, 1990–2016: Burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444–1472. doi: 10.1001/jama.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Esser MB, Sherk A, Liu Y, et al. Deaths and years of potential life lost from excessive alcohol use — United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2020; 69(39):1428–1433. doi: 10.15585/mmwr.mm6939a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cherpitel CJ, Borges G, Giesbrecht N, Monteiro M, Stockwell T. Prevention of Alcohol-Related Injuries in the Americas: From Evidence to Policy Action. Pan American Health Organization and World Health Organization; 2013. [Google Scholar]
- 4.Li G, Smith GS, Baker SP. Drinking behavior in relation to cause of death among US adults. Am J Public Health. 1994;84(9):1402–1406. doi: 10.2105/AJPH.84.9.1402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones CM, Clayton HB, Deputy NP, et al. Prescription opioid misuse and use of alcohol and other substances among high school students - Youth Risk Behavior Survey, United States, 2019. MMWR Suppl. 2020;69(1):38–46. doi: 10.15585/mmwr.su6901a55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bohm MK, Liu Y, Esser MB, et al. Binge drinking among adults, by select characteristics and state — United States, 2018. MMWR Morb Mortal Wkly Rep 2021;70:1441–1446. doi: 10.15585/mmwr.mm7041a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Department of Transportation, National Highway Transportation Safety Administration. Fatal Analysis Reporting System. Accessed April 11, 2021. https://www.nhtsa.gov/research-data/fatality-analysis-reporting-system-fars.
- 8.Hingson R, Howland J. Alcohol and non‐traffic unintended injuries. Addiction. 1993;88(7):877–883. doi: 10.1111/j.1360-0443.1993.tb02105.x [DOI] [PubMed] [Google Scholar]
- 9.Smith GS, Branas CC, Miller TR. Fatal nontraffic injuries involving alcohol: A metaanalysis. Ann Emerg Med. 1999;33(6):659–668. 10.1016/S0196-0644(99)80004-3 [DOI] [PubMed] [Google Scholar]
- 10.English DR, Holman CDJ, Milne E, et al. The Quantification of Drug-Caused Mortality and Morbidity in Australia.; Canberra, Australia: Commonwealth Department of Human Services and Health;1995. [Google Scholar]
- 11.White AM, Slater ME, Ng G, Hingson R, Breslow R. Trends in alcohol-related emergency department visits in the United States: Results from the Nationwide Emergency Department Sample, 2006 to 2014. Alcohol Clin Exp Res. 2018;42(2):352–359. doi: 10.1111/acer.13559 [DOI] [PubMed] [Google Scholar]
- 12.Mullins PM, Mazer-Amirshahi M, Pines JM. Alcohol-related visits to US emergency departments, 2001–2011. Alcohol. 2016;52(1):119–125. doi: 10.1093/alcalc/agw074 [DOI] [PubMed] [Google Scholar]
- 13.Grucza RA, Sher KJ, Kerr WC, et al. Trends in adult alcohol use and binge drinking in the early 21st-century United States: A meta-analysis of 6 national survey series. Alcohol Clin Exp Res. 2018;42(10):1939–1950. doi: 10.1111/acer.13859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Esser MB, Pickens CM, Guy GP, Evans ME. Binge drinking, other substance use, and concurrent use in the U.S., 2016–2018. Am J Prev Med. 2021;60(2):169–178. doi: 10.1016/j.amepre.2020.08.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahdi I, Tomedi LE, Gerrard CY, Lathrop S, Landen M. Excessive alcohol use and drug overdose deaths, New Mexico, 2015–2016. Drug Alcohol Depend. 2020;215. doi: 10.1016/j.drugalcdep.2020.108175 [DOI] [PubMed] [Google Scholar]
- 16.Tori ME, Larochelle MR, Naimi TS. Alcohol or benzodiazepine co-involvement with opioid overdose deaths in the United States, 1999–2017. JAMA Netw Open. 2020;3(4):e202361. doi: 10.1001/jamanetworkopen.2020.2361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Understanding the Epidemic. https://www.cdc.gov/drugoverdose/epidemic/index.html. Updated March 17, 2021. Accessed April 9, 2021.
- 18.Community Preventive Services Task Force. The Guide to Community Preventive Services (The Community Guide): Excessive Alcohol Consumption. https://www.thecommunityguide.org/topic/excessive-alcohol-consumption. Accessed April 9, 2021.
- 19.Centers for Disease Control and Prevention. Alcohol Related Disease Impact (ARDI) application. 2020. www.cdc.gov/ARDI. Accessed April 9, 2021.
- 20.National Highway Traffic Safety Administration. Traffic Safety Facts 2018 Annual Report: A Compilation of Motor Vehicle Crash Data. Washington, DC. U.S. Department of Transportation, National Center for Statistics and Analysis; November, 2020. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/812981. Accessed June 3, 2021. [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paez A. Grey literature: An important resource in systematic reviews. J Evid Based Med. 2017. doi: 10.1111/jebm.12266 [DOI] [PubMed] [Google Scholar]
- 23.Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ. 2005. 331(7524):1064–5. doi: 10.1136/bmj.38636.593461.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Alcohol-related ICD Codes. https://www.cdc.gov/alcohol/ardi/alcohol-related-icd-codes.html. Updated September 10, 2020. Accessed April 28, 2021.
- 25.Centers for Disease Control and Prevention. ARDI Methods. https://www.cdc.gov/alcohol/ardi/methods.html. Updated July 27, 2020. Accessed April 28, 2021.
- 26.Schünemann H BJ, Guyatt G, Oxman AE. GRADE Handbook. https://gdt.gradepro.org/app/handbook/handbook.html. Updated October, 2013. Accessed April 9, 2021. [Google Scholar]
- 27.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008; 336:924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schwarzer G, Chemaitelly H, Abu-Raddad LJ, Rücker G. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res Synth Methods. 2019;10(3):476–483. doi: 10.1002/jrsm.1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: A practical tutorial. Evid Based Ment Health. 2019;22(4):153–160. doi: 10.1136/ebmental-2019-300117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3). doi: 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 32.R Core Team. R: A language and environment for statistical computing. Published 2021. https://www.r-project.org. Accessed April 12, 2021
- 33.Lunetta P, Smith GS. The role of alcohol in injury deaths. In: Preedy VR, Watson RR, ed. Comprehensive Handbook of Alcohol Related Pathology. Vol 1–3. San Diego: Elsevier Science & Technology; 2005:147–164. doi: 10.1016/B978-012564370-2/50015-5 [DOI] [Google Scholar]
- 34.Collins JJ, Messerschmidt PM. Epidemiology of alcohol-related violence. Alcohol Health Res World. 1993;17(2):93–100. [Google Scholar]
- 35.Koob GF, Arends MA, Le Moal M. Alcohol. In: Koob GF, Arends MA, Le Moal M, eds. Drugs, Addiction, and the Brain. New York: Academic Press; 2014:173–219. doi. 10.1016/B978-0-12-386937-1.00006-4 [DOI] [Google Scholar]
- 36.Shield K, Manthey J, Rylett M, et al. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: a comparative risk assessment study. Lancet Public Health. 2020;5(1):e51–e61. doi: 10.1016/S2468-2667(19)30231-2 [DOI] [PubMed] [Google Scholar]
- 37.Chrystoja BR, Rehm J, Manthey J, et al. A systematic comparison of the global comparative risk assessments for alcohol. Addiction. Published online 2021. doi: 10.1111/add.15413. [DOI] [PubMed] [Google Scholar]
- 38.Naimi TS, Xuan Z, Cooper SE, et al. Alcohol involvement in homicide victimization in the United States. Alcohol Clin Exp Res. 2016;40(12):2614–2621. doi: 10.1111/acer.13230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Singh AK. Alcohol interaction with cocaine, methamphetamine, opioids, nicotine, cannabis, and γ-hydroxybutyric acid. Biomedicines. 2019;7(1):16. doi: 10.3390/biomedicines7010016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dasgupta A. Combined alcohol and drug abuse: A potentially deadly mix. In: Dasgupta A, ed. Alcohol, Drugs, Genes and the Clinical Laboratory. New York: Academic Press; 2017:75–88. doi. 10.1016/B978-0-12-805455-0.00004-X [DOI] [Google Scholar]
- 41.White AM, Castle IJP, Hingson RW, Powell PA. Using death certificates to explore changes in alcohol-related mortality in the United States, 1999 to 2017. Alcohol Clin Exp Res. 2020;44(1):178–187. doi: 10.1111/acer.14239 [DOI] [PubMed] [Google Scholar]
- 42.Castle IJP, Yi HY, Hingson RW, White AM. State variation in underreporting of alcohol involvement on death certificates: Motor vehicle traffic crash fatalities as an example. J Stud Alcohol Drugs. 2014;75(2):299–312. doi: 10.15288/jsad.2014.75.299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greene N, Tomedi LE, Cox ME, Mello E, Esser MB. Alcohol testing and alcohol involvement among violent deaths by state, 2014–2016. Prev Med. 2021;148. doi: 10.1016/j.ypmed.2021.106527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Greene N, Esser MB, Vesselinov R, et al. Variability in antemortem and postmortem blood alcohol concentration levels among fatally injured adults. Am J Drug Alcohol Abuse. 2021. 2;47(1):84–91. doi: 10.1080/00952990.2020.1822856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thomas M, Riemann, Jones J. Epidemiology of alcohol and drug screening among pedestrian fatalities in the United States , 2014 – 2016. Traffic Injury Prevention. 2019. 20(6): 557–562. 10.1080/15389588.2019.16220064646. [DOI] [PubMed] [Google Scholar]
- 46.Quintas MJ, Costa P, Melo P, et al. Postmortem in vitro ethanol production-It could be more common than we think! Forensic Sci Int. 2017. May;274:113–116. doi: 10.1016/j.forsciint.2016.12.040. Epub 2017 Jan 5. PMID: 28108144. [DOI] [PubMed] [Google Scholar]
- 47.World Health Organization. Global status report on alcohol and health 2018. Geneva. World Health Organization: 2018. https://www.who.int/publications/i/item/9789241565639 [Google Scholar]
- 48.Rockett IRH, Caine ED, Connery HS, et al. Unrecognised self-injury mortality (SIM) trends among racial/ethnic minorities and women in the USA. Inj Prev. 2020;26(5):439–447. doi. 10.1136/injuryprev-2019-043371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Centers for Disease Control and Prevention. CDC Wonder. https://wonder.cdc.gov. Updated December, 22, 2020. Accessed April 28, 2021. [Google Scholar]
- 50.Taylor B, Irving HM, Kanteres F, et al. The more you drink, the harder you fall: A systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend. 2010;110(1–2):108–116. doi: 10.1016/j.drugalcdep.2010.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pelletier A. Deaths among railroad trespassers: The role of alcohol in fatal injuries. JAMA. 1997;277(13):1064–1066. doi: 10.1001/jama.277.13.1064 [DOI] [PubMed] [Google Scholar]
- 52.North American Management. Rail Trespasser Fatalities: Demographic and Behavioral Profiles. Washington, DC. U.S. Department of Transportation, Federal Railroad Administration: June, 2013. https://railroads.dot.gov/sites/fra.dot.gov/files/fra_net/3315/RailTrespasserFatalitiesDemograph62013.pdf. Accessed June 3, 2021. [Google Scholar]
- 53.Centers for Disease Control and Prevention. Injuries among railroad trespassers--Georgia, 1990–1996. MMWR Morb Mortal Wkly Rep. 1999;48(25):537–541. [PubMed] [Google Scholar]
- 54.Li G, Baker SP, Lamb MW, et al. Characteristics of alcohol-related fatal general aviation crashes. Accid Anal Prev. 2005;37(1):143–148. doi: 10.1016/j.aap.2004.03.005 [DOI] [PubMed] [Google Scholar]
- 55.Middleton JC, Hahn RA, Kuzara JL, et al. Effectiveness of policies maintaining or restricting days of alcohol sales on excessive alcohol consumption and related harms. Am J Prev Med. 2010;39(6):575–589. doi: 10.1016/j.amepre.2010.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Campbell CA, Hahn RA, Elder R, et al. The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. Am J Prev Med. 2009;37(6):556–569. doi: 10.1016/j.amepre.2009.09.028 [DOI] [PubMed] [Google Scholar]
- 57.Elder RW, Lawrence B, Ferguson A, et al. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. Am J Prev Med. 2010;38(2):217–229. doi: 10.1016/j.amepre.2009.11.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rammohan V, Hahn RA, Elder R, et al. Effects of dram shop liability and enhanced overservice law enforcement initiatives on excessive alcohol consumption and related harms: Two community guide systematic reviews. Am J Prev Med. 2011;41(3):334–343. doi: 10.1016/j.amepre.2011.06.027 [DOI] [PubMed] [Google Scholar]
- 59.Naimi TS, Xuan Z, Coleman SM, et al. Alcohol policies and alcohol-involved homicide victimization in the United States. J Stud Alcohol Drugs. 2017;78(5):781–788. doi: 10.15288/jsad.2017.78.781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Coleman SM, Lira MC, Blanchette J, Heeren TC, Naimi TS. Alcohol policies, firearm policies, and suicide in the United States: a lagged cross-sectional study. BMC Public Health. 2021;21(1). doi: 10.1186/s12889-021-10216-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nesoff ED, Milam AJ, Branas CC, Martins SS, Knowlton AR, Furr-Holden DM. Alcohol outlets, neighborhood retail environments, and pedestrian injury risk. Alcohol Clin Exp Res. 2018;42(10):1979–1987. doi: 10.1111/acer.13844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.O’Connor EA, Perdue LA, Senger CA, et al. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: Updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2018;320(18):1910–1928. doi: 10.1001/jama.2018.12086 [DOI] [PubMed] [Google Scholar]
- 63.Tansil KA, Esser MB, Sandhu P, et al. Alcohol electronic screening and brief intervention: a Community Guide systematic review. Am J Prev Med. 2016;51(5):801–811. doi: 10.1016/j.amepre.2016.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Botch SR, Johnson RD. Toxicological Findings of Pilots Involved in Aviation Accidents Operated under Title 14 CFR Part 135. Washington, DC: Office of Aerospace Medicine, Federal Aviation Administration. August, 2009. [Google Scholar]
- 65.Botch SR, Johnson RD. Alcohol-Related Aviation Accidents Involving Pilots with Previous Alcohol Offenses. Washington, DC: Office of Aerospace Medicine, Federal Aviation Administration. October, 2008. [Google Scholar]
- 66.Li G, Hooten EG, Baker SP, Butts JD. Alcohol in aviation-related fatalities: North Carolina, 1985–1994. Aviat Space Environ Med. 1998;69(8):755–760. [PubMed] [Google Scholar]
- 67.Boghossian E, Tambuscio S, Sauvageau A. Nonchemical suffocation deaths in forensic setting: A 6-year retrospective study of environmental suffocation, smothering, choking, and traumatic/positional asphyxia. J Forensic Sci. 2010;55(3):646–651. doi: 10.1111/j.1556-4029.2010.01351.x [DOI] [PubMed] [Google Scholar]
- 68.Colorado Department of Public Health and Environment. Colorado Child Fatality Prevention System Data Dashboard. https://cohealthviz.dphe.state.co.us/t/PSDVIP-MHPPUBLIC/views/CFPSDashboardFinalLocal/Story1?iframeSizedToWindow=true&:embed=y&:showAppBanner=false&:display_count=no&:showVizHome=no. Accessed April 9, 2021.
- 69.Parks SE, Mirchandani G, Rodriguez S, Hellsten J. History of maltreatment among unintentional injury deaths: Analyses of Texas child fatality review data, 2005–2007. Inj Prev. 2011;17(SUPPL. 1). doi: 10.1136/ip.2010.026336 [DOI] [PubMed] [Google Scholar]
- 70.South Carolina State Child Fatality Advisory Committee. State Fiscal Year 2019. Report. https://scfacsc.files.wordpress.com/2020/02/2019-scfac-annual-report-final.pdf. Accessed April 12, 2021.
- 71.Okuda T, Wang Z, Lapan S, Fowler DR. Bathtub drowning: An 11-year retrospective study in the state of Maryland. Forensic Sci Int. 2015;253:64–70. doi: 10.1016/j.forsciint.2015.05.013 [DOI] [PubMed] [Google Scholar]
- 72.Cummings P, Quan L. Trends in unintentional drowning the role of alcohol and medical care. JAMA. 1999;281(23):2198–2202. doi: 10.1001/jama.281.23.2198 [DOI] [PubMed] [Google Scholar]
- 73.Browne ML, Lewis-Michl EL, Stark AD. Unintentional drownings among New York State residents, 1988–1994. Public Health Rep. 2003;118(5):448–458. doi: 10.1016/S0033-3549(04)50276-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Canadian Red Cross Society. Drownings and Other Water-Related Injuries in Canada: 10 Years of Research, Module 1 Overview. https://www.redcross.ca/training-and-certification/swimming-and-water-safety-tips-and-resources/drowning-research. Published 2006. Accessed April 9, 2021.
- 75.Lincoln JM, Perkins R, Melton F, Conway GA. Drowning in Alaskan waters. Public Health Rep. 1996;111(6):531–535. [PMC free article] [PubMed] [Google Scholar]
- 76.Levine B, Moore KA, Fowler D. Interaction between carbon monoxide and ethanol in fire fatalities. Forensic Sci Int. 2001;124(2–3):115–116. [DOI] [PubMed] [Google Scholar]
- 77.Tridata Corporation. Establishing a Relationship Between Alcohol and Casualties of Fire. Arlington, VA: Federal Emergency Management Agency, United States Fire Administration National Fire Data Center. October, 1999. [Google Scholar]
- 78.U.S. Fire Administration, National Fire Data Center. Case Study: Contribution of Alcohol to Fire Fatalities in Minnesota. Topical Fire Research Series, Vol. 3-Issue 4. Washington, DC: U.S. Department of Homeland Security/Federal Emergency Management Agency; July 2003. [Google Scholar]
- 79.McGwin G, Chapman V, Rousculp M, Robison J, Fine P. The epidemiology of fire-related deaths in Alabama, 1992–1997. J Burn Care Rehabil. 2000;21(1):75–83. doi: 10.1097/00004630-200021010-00016 [DOI] [PubMed] [Google Scholar]
- 80.Marshall SW, Runyan CW, Bangdiwala SI, Linzer MA, Sacks JJ, Butts JD. Fatal residential fires: Who dies and who survives? JAMA. 1998;279(20):1633–1637. doi: 10.1001/jama.279.20.1633 [DOI] [PubMed] [Google Scholar]
- 81.Cherry D, Runyan C, Butts J. A population based study of unintentional firearm fatalities. Inj Prev. 2001;7(1):62–65. doi: 10.1136/ip.7.1.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Collins KA. Adolescent Russian roulette deaths. Am J Forensic Med Pathol. 2010;31(1):4–6. doi: 10.1097/PAF.0b013e3181c6849f [DOI] [PubMed] [Google Scholar]
- 83.Shields LBE, Hunsaker JC, Stewart DM. Russian roulette and risk-taking behavior: A medical examiner study. Am J Forensic Med Pathol. 2008;29(1):32–39. doi: 10.1097/PAF.0b013e318160675e [DOI] [PubMed] [Google Scholar]
- 84.Spunt B, Brownstein HH, Crimmins SM, Langley S, Spanjol K. Alcohol-related homicides committed by women. J Psychoactive Drugs. 1998;30(1):33–43. doi: 10.1080/02791072.1998.10399669 [DOI] [PubMed] [Google Scholar]
- 85.Spunt B, Brownstein H, Goldstein P, Fendrich M, Liberty HJ. Drug use by homicide offenders. J Psychoactive Drugs. 1995;27(2):125–134. doi: 10.1080/02791072.1995.10471681 [DOI] [PubMed] [Google Scholar]
- 86.Banks L, Crandall C, Sklar D, Bauer M. A comparison of intimate partner homicide to intimate partner homicide-suicide: One hundred and twenty-four New Mexico cases. Violence Against Women. 2008;14(9):1065–1078. doi: 10.1177/1077801208321983 [DOI] [PubMed] [Google Scholar]
- 87.Greenfeld LA. Alcohol and Crime: An Analysis of National Data on the Prevalence of Alcohol Involvement in Crime. Washington, DC. US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; April 5–7, 1998. [Google Scholar]
- 88.Koutsavlis AT, Kosatsky T. Environmental-temperature injury in a Canadian metropolis. J Environ Health. 2003;66(5):40–45. [PubMed] [Google Scholar]
- 89.Minnesota Department of Natural Resources. Incident (Accident) Reports. https://www.dnr.state.mn.us/enforcement/incidentreports/index.html?__cf_chl_captcha_tk__=d75424ba4d2e1c70b375583390bef6fccc0f677d-1618131130-0-AeZxhJIZ3GwnN8Li8Fzo0OnztKNCpkvJp5hwVJcvj6u5a1BhhNUO-BWaZWJMovu2ICPEqUIk_pPUXEAcuUK9ABFhkY7f3CsoOJyVmfKTQNH5iQX-. Accessed April 9, 2021.
- 90.Hall AJ, Bixler D, Helmkamp JC, Kraner JC, Kaplan JA. Fatal all-terrain vehicle crashes: injury types and alcohol use. Am J Prev Med. 2009;36(4):311–316. doi: 10.1016/j.amepre.2008.11.019 [DOI] [PubMed] [Google Scholar]
- 91.Wisconsin Department of Natural Resources. Fatality Summary, Annual Reports and Crash Reporting, All-Terrain Vehicle Crash Incident Reports. https://dnr.wisconsin.gov/topic/ATV/CrashInfo. Accessed April 9, 2021.
- 92.Wisconsin Department of Natural Resources. Fatality Summary, Annual Reports and Crash Reporting, Recreational Vehicle Incident Reports. https://dnr.wisconsin.gov/topic/snowmobile/CrashInfo. Accessed April 9, 2021.
- 93.Landen MG, Middaugh J, Dannenberg AL. Injuries associated with snowmobiles, Alaska, 1993–1994. Public Health Rep. 1999;114(1):48–52. doi: 10.1093/phr/114.1.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.West R, Shkrum MJ, Young JG. Commercial logging fatalities in Ontario, 1986–1991. Am J Forensic Med Pathol. 1996;17(4):299–304. doi: 10.1097/00000433-199612000-00004 [DOI] [PubMed] [Google Scholar]
- 95.Foster CA, Dissanaike SD. Prevalence and consequences of positive blood alcohol levels among patients injured at work. J Emerg Trauma Shock. 2014;7(4):268–273. doi: 10.4103/0974-2700.142748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Davis GG, Brissie RM. A review of crane deaths in Jefferson County, Alabama. J Forensic Sci. 2000;45(2):392–396. doi: 10.1520/jfs14692j [DOI] [PubMed] [Google Scholar]
- 97.Fullerton L, Olson L, Crandall C, Sklar D, Zumwalt R. Occupational injury mortality in New Mexico. Ann Emerg Med. 1995;26(4):447–454. doi: 10.1016/S0196-0644(95)70113-3 [DOI] [PubMed] [Google Scholar]
- 98.Lucas DL, Lincoln JM. Fatal falls overboard on commercial fishing vessels in Alaska. Am J Ind Med. 2007;50(12):962–968. doi: 10.1002/ajim.20509 [DOI] [PubMed] [Google Scholar]
- 99.Przepyszny LM, Jenkins AJ. The prevalence of drugs in carbon monoxide-related deaths: A retrospective study, 2000–2003. Am J Forensic Med Pathol. 2007;28(3):242–248. doi: 10.1097/01.paf.0000257417.26383.e4 [DOI] [PubMed] [Google Scholar]
- 100.Moolenaar RL, Etzel RA, Gibson Parrish R. Unintentional deaths from carbon monoxide poisoning in New Mexico, 1980 to 1988. A comparison of medical examiner and national mortality data. West J Med. 1995;163(5):431–434. [PMC free article] [PubMed] [Google Scholar]
- 101.Levine B, Green D, Smialek JE. The role of ethanol in heroin deaths. J Forensic Sci. 1995;40(5):808–810. doi: 10.1520/jfs15389j [DOI] [PubMed] [Google Scholar]
- 102.Weinberger LE, Sreenivasan S, Sathyavagiswaran L, Markowitz E. Child and adolescent suicide in a large, urban area: Psychological, demographic, and situational factors. J Forensic Sci. 2001;46(4):902–907. doi: 10.1520/jfs15066j [DOI] [PubMed] [Google Scholar]
- 103.Lewis RJ, Johnson RD, Whinnery JE, Forster EM. Aircraft-assisted pilot suicides in the United States, 1993–2002. Arch Suicide Res. 2007;11(2):149–161. doi: 10.1080/13811110701247636 [DOI] [PubMed] [Google Scholar]
- 104.San Nicolas AC, Lemos NP. Toxicology findings in cases of hanging in the City and County of San Francisco over the 3-year period from 2011 to 2013. Forensic Sci Int. 2015;255:146–155. doi: 10.1016/j.forsciint.2015.07.006 [DOI] [PubMed] [Google Scholar]
- 105.Bullock MJ, Diniz D. Suffocation using plastic bags: A retrospective study of suicides in Ontario, Canada. J Forensic Sci. 2000;45(3):14736J. doi: 10.1520/jfs14736j [DOI] [PubMed] [Google Scholar]
- 106.Davis LG. Suicidal drowning in South Florida. J Forensic Sci. 1999;44(5):902–905. doi: 10.1520/jfs12013j [DOI] [PubMed] [Google Scholar]
- 107.Wolford-Clevenger C, McCleskey B, Cropsey KC. An assessment of blood alcohol concentration and potential for reversal of method used in suicides. Alcohol Clin Exp Res. 2020;44(S1):171A. doi: 10.1111/acer.14358 [DOI] [Google Scholar]
- 108.Cherpitel CJ. Regional differences in alcohol and fatal injury: A comparison of data from two county coroners. J Stud Alcohol. 1996;57(3):244–248. doi: 10.15288/jsa.1996.57.244 [DOI] [PubMed] [Google Scholar]
- 109.Fisher LB, Overholser JC, Dieter L. Methods of committing suicide among 2,347 people in Ohio. Death Stud. 2015;39(1):39–43. doi: 10.1080/07481187.2013.851130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Branas CC, Richmond TS, Ten Have TR, Wiebe DJ. Acute alcohol consumption, alcohol outlets, and gun suicide. Subst Use Misuse. 2011;46(13):1592–1603. doi: 10.3109/10826084.2011.604371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kaplan MS, McFarland BH, Huguet N, et al. Acute alcohol intoxication and suicide: A gender-stratified analysis of the National Violent Death Reporting System. Inj Prev. 2013;19(1):38–43. doi: 10.1136/injuryprev-2012-040317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Shields LBE, Hunsaker DM, Hunsaker JC, Ward MK. Toxicologic findings in suicide: A 10-year retrospective review of Kentucky medical examiner cases. Am J Forensic Med Pathol. 2006;27(2):106–112. doi: 10.1097/01.paf.0000220913.19508.99 [DOI] [PubMed] [Google Scholar]
- 113.Conner KR, Lathrop S, Caetano R, Silenzio V, Nolte KB. Blood alcohol concentrations in suicide and motor vehicle crash decedents ages 18 to 54. Alcohol Clin Exp Res. 2016;40(4):772–775. doi: 10.1111/acer.13002 [DOI] [PubMed] [Google Scholar]
- 114.New York State Office of Parks, Recreation & Historic Preservation, Boating Resources. Recreational Boating Reports. https://parks.ny.gov/recreation/boating/resources.aspx. Accessed April 9, 2021.
- 115.Wisconsin Department of Natural Resources. Fatality Summary, Annual Reports and Crash Reporting, Boat Crash Incident Reports. https://dnr.wisconsin.gov/Topic/Boat/CrashInfo. Accessed April 9, 2019
- 116.Browne ML, Lewis-Michl EL, Stark AD. Watercraft-related drownings among New York State residents, 1988–1994. Public Health Rep. 2003;118(5):459–463. doi: 10.1016/S0033-3549(04)50277-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Smith GS, Keyl PM, Hadley JA, et al. Drinking and recreational boating fatalities: A population-based case-control study. JAMA. 2001;286(23):2974–2980. doi: 10.1001/jama.286.23.2974 [DOI] [PubMed] [Google Scholar]
- 118.Barss P. Boating Immersion and Trauma Deaths in Canada: 18 Years of Research. Transport Canada and The Canadian Red Cross Society. 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.