Abstract
Objective
The objective of this study was to evaluate the utilization of telehealth for headache services within the Veterans Health Administration’s facilities housing a Headache Centers of Excellence and multiple stakeholder’s perspectives to inform future telehealth delivery.
Background
Telehealth delivery of headache treatment may enhance patient access to headache care, yet little is known about the utilization or patient and provider perceptions of telehealth for veterans with headache.
Methods
This mixed‐methods study analyzed multiple data sources: (1) administrative data, which included 58,798 patients with medically diagnosed headache disorders, documented in at least one outpatient visit, from August 2019 through September 2020 from the 12 Veterans Health Administration’s facilities with a Headache Center of Excellence and (2) qualitative semistructured interviews with 20 patients and 43 providers 6 months before the coronavirus disease 2019 (COVID‐19) pandemic, and 10 patients and 20 providers 6 months during the beginning of the pandemic.
Results
During the pandemic, in‐person visits declined from 12,794 to 6099 (52.0%), whereas video (incidence rate ratio [IRR] = 2.05, 95% confidence interval [CI] = 1.66, 2.52), and telephone visits (IRR = 15.2, 95% CI = 10.7, 21.6) significantly increased. Utilization differed based on patient age, race/ethnicity, and rurality. Patients and providers perceived value in using telehealth, yet had limited experience with this modality pre‐pandemic. Providers preferred in‐person appointments for initial encounters and telehealth for follow‐up visits. Providers and patients identified benefits and challenges of telehealth delivery, often relying on multiple delivery methods for telehealth to enhance patient engagement.
Conclusions
The uptake of telehealth delivery of headache‐related care rapidly expanded in response to the pandemic. Patients and providers were amenable to utilizing telehealth, yet also experienced technological barriers. To encourage equitable access to telehealth and direct resources to those in need, it is crucial to understand patient preferences regarding in‐person versus telehealth visits and identify patient groups who face barriers to access.
Keywords: access to care, headache, mixed methods, telehealth
Abbreviations
- CVT
Clinical Video Telehealth
- HCoE
Headache Center of Excellence
- VHA
Veterans Health Administration
- VVC
VA Video Connect
INTRODUCTION
Remote, real‐time delivery of healthcare services (telehealth) had been gaining popularity even before the coronavirus disease 2019 (COVID‐19) pandemic. Although telehealth has generally been associated with higher patient satisfaction, 1 increased access to specialty care 2 , 3 , 4 , 5 , 6 , 7 , 8 and decreased geographic barriers, 9 the rapid expansion of telehealth during the pandemic 10 has been accompanied by technological challenges. 3 , 5 , 11 Headache disorders are among the most prevalent and disabling diseases in the world. Preliminary evidence suggests that neurology services can be successfully delivered via telehealth, 4 , 5 with more recent studies reporting on the benefits of telehealth for headache. 12 , 13 Between March 2020 and September 2020, the American Migraine Foundation conducted an online survey study with 1172 patients with headache, and found that patients valued telehealth which increased access to headache‐specific care. 12 Minen and colleagues’ recent online survey study with 225 American Headache Society clinicians who provide headache treatment reported that providers found telehealth an acceptable method of delivery of headache care. 13 The literature examining perceptions of telehealth for headache is still limited and little is known about the perceptions and utilization of telehealth for headache‐specific care within a veteran population in the pre‐pandemic and pandemic periods.
Headache can serve as an exemplar disorder to understand telehealth utilization and identify best practices for implementation of telehealth specialty care. Headache disorders are common, 14 and disabling, 15 migraine alone is the second leading cause of years lived in disability worldwide. 16 However, there are insufficient numbers of trained headache specialists in the United States, and more are congregated around urban areas, leaving vast swaths of the country with few specialists. 17 Headache disorders are chronic, requiring both acute (attack‐based) and preventive treatment. This complex management results in frequent appointments, 18 which are burdensome for a patient group for whom distribution of their routine and stress can exacerbate the disorder. 19 , 20
The COVID‐19 pandemic has been a catalyst for change in the provision of telehealth. Understanding the utilization and perceptions of telehealth for headache management will inform policies and help guide training, payors, and best practices for telehealth headache services. This study aimed to (1) examine telehealth utilization for headache care across the Veterans Health Administration (VHA) facilities with a Headache Center of Excellence (HCoE), and (2) elucidate patient and provider perceptions of telehealth for headache care, both before and during the COVID‐19 pandemic to inform best practices and understand telehealth implementation. We hypothesized that (1) telehealth utilization would increase and in‐person visits would decrease from the pre‐pandemic to pandemic period, (2) there would be differences in telehealth utilization based on patient demographic characteristics, and (3) patient and provider perceptions of telehealth may differ from the pre‐pandemic to the pandemic period.
METHODS
Administrative data
We performed a primary analysis using data for 58,798 patients receiving care within one of 12 VHA facilities which contain an HCoE, who had at least one outpatient visit, with an encounter code for any International Classification of Diseases (ICD)‐10 headache diagnosis including R51, G43, G44, S13.4, S13.8, and S13.9, drawn from the VHA Corporate Data Warehouse from August 2019 through September 2020. We did not include any patients who had an inpatient ICD‐10 code of headache, as they were more likely to have headache secondary to stroke or subarachnoid hemorrhage. The sample size was based on available data. Outpatient visit types were classified as in‐person, VA Video Connect (VVC), Clinical Video Telehealth (CVT), and telephone. Both VVC and CVT utilize real‐time videoconferencing to provide care remotely. VVC is not limited to location and patients can receive headache care on any computer, tablet, or mobile device. CVT utilizes VHA facility‐based videoconferencing technology and requires patients to attend a medical facility. 21 Telephone visits were defined using Common Procedural Terminology (CPT) codes for telephone calls by physicians or other qualified healthcare professionals for evaluation, consultation, or medical management. Patient‐level characteristics include age (18–44, 45–64, and ≥65 years), gender (men vs. women), race/ethnicity (White, Hispanic, black, or other), and rurality (urban, rural, or missing; Table 1).
TABLE 1.
Demographics of patients with headache encounter(s) served in the pre‐pandemic (August 2019–February 2020) and pandemic (March 2020–September 2020) across the 12 Veteran Health Administration’s Headache Centers of Excellence a
| Unique patients per period | Total unique in 14‐month period (N = 58,798) | p value | ||
|---|---|---|---|---|
| Pre‐pandemic (August 2019–February 2020) (N = 44,669) | Pandemic (March 2020–September 2020) (N = 28,621) | |||
| Type of visit (yes vs. no) not mutually exclusive | ||||
| In‐person | 44,037 (98.6%) | 21,188 (74.0%) | 54,239 (81.0%) | <0.001 |
| VVC | 405 (0.9%) | 9563 (33.4%) | 9829 (16.7%) | <0.001 |
| CVT | 723 (1.6%) | 200 (0.7%) | 882 (1.5%) | <0.001 |
| Telephone | 174 (0.4%) | 2756 (9.6%) | 2884 (4.9%) | <0.001 |
| Age (by FY19) | ||||
| Mean (SD) | 49.8 (14.9) | 49.0 (14.4) | 49.6 (15.0) | <0.001 |
| <45 | 18,218 (40.8%) | 12,246 (42.8%) | 24,439 (41.6%) | <0.001 |
| 45–64 | 17,995 (40.3%) | 11,700 (40.9%) | 23,346 (39.7%) | |
| ≥65 | 8456 (18.9%) | 4675 (16.3%) | 11,013 (18.7%) | |
| Gender | ||||
| Women | 11,672 (26.1%) | 8256 (28.8%) | 15,334 (26.1%) | <0.001 |
| Race/ethnicity | ||||
| White | 24,690 (55.3%) | 15,149 (52.9%) | 32,237 (54.8%) | <0.001 |
| Black | 10,106 (22.6%) | 6522 (22.8%) | 13,152 (22.4%) | |
| Hispanic | 5894 (13.2%) | 4241 (14.8%) | 7986 (13.6%) | |
| Other | 3979 (8.9%) | 2709 (9.5%) | 5423 (9.2%) | |
| Rurality | ||||
| Rural | 8830 (19.8%) | 5071 (17.7%) | 11,347 (19.3%) | <0.001 |
| Urban | 35,820 (80.2%) | 23,542 (82.3%) | 47,428 (80.7%) | |
| Unknown | 19 (0.0%) | 8 (0.0%) | 23 (0.0%) | |
| Headache center | ||||
| Birmingham, AL | 3104 (6.9%) | 1640 (5.7%) | 3749 (6.4%) | <0.001 |
| Cleveland, OH | 4350 (9.7%) | 2414 (8.4%) | 5525 (9.4%) | |
| Minneapolis, MN | 3050 (6.8%) | 1603 (5.6%) | 3905 (6.6%) | |
| Palo Alto, CA | 1935 (4.3%) | 1004 (3.5%) | 2547 (4.3%) | |
| Pittsburgh, PA | 2123 (4.8%) | 1412 (4.9%) | 2860 (4.9%) | |
| Richmond, VA | 4119 (9.2%) | 2417 (8.4%) | 5188 (8.8%) | |
| Salt Lake City, UT | 2729 (6.1%) | 1522 (5.3%) | 3483 (5.9%) | |
| San Antonio, TX | 6580 (14.7%) | 4565 (15.9%) | 8817 (15.0%) | |
| Tampa, FL | 5360 (12.0%) | 4138 (14.5%) | 7455 (12.7%) | |
| Orlando, FL | 5756 (12.9%) | 4145 (14.5%) | 7829 (13.3%) | |
| West Haven, CT | 1914 (4.3%) | 1073 (3.7%) | 2409 (4.1%) | |
| Los Angeles, CA | 3649 (8.2%) | 2688 (9.4%) | 5031 (8.6%) | |
Abbreviations: CVT, Clinical Video Telehealth; VVC, VA Video Connect.
Not mutually exclusive categories.
Statistical analyses
Categorical variables are displayed using frequency and percentages. Continuous variables are displayed using means and SDs. All statistical analyses were conducted with SAS 9.4 (Cary, NC). Chi‐square (χ 2) test evaluated differences between pre‐pandemic (August 2019 through February 2020) and pandemic periods (March 2020 through September 2020) for categorical variables and independent samples t‐test for continuous variables with normal distribution. We evaluated assumptions of parametric tests via inspection of histograms. A p value of less than 0.05 (2‐tailed) was used to indicate statistical significance. For the purposes of analysis, the total frequency counts were aggregated at a monthly level. We used univariate Poisson regression models with the pre‐pandemic period as the reference category to compare differences in visit counts for in‐person and telehealth appointments. We reported incident rate ratios (IRRs), the ratio of monthly incidence rates for in‐person or telehealth visits comparing the pandemic to pre‐pandemic period. To determine the effect of particular patient characteristics on the magnitude change of telehealth utilization during the pandemic period, Poisson regression models with a log link function were built using the monthly number of patients who scheduled in‐person, VVC, CVT, or telephone appointments. Relative risks (RRs) and 95% confidence intervals (CIs) are reported. Differences in age, gender, race/ethnicity, or rurality status were compared to the reference level, and tested by using interaction tests between each of the patient characteristics and time, respectively.
Qualitative interviews sample and recruitment
This is the primary analysis of these data. Between June 2019 and March 2020, we conducted semistructured interviews with 20 patients and 43 clinical providers across HCoEs. We invited a purposive sample of headache providers and patients with chronic headache who have received headache care. After the onset of the pandemic, we again interviewed these providers and additional patients to understand the impact of the pandemic on headache care. Between July 2020 and November 2020, we conducted semistructured in‐person/phone interviews with 10 patients and 20 clinical providers across HCoEs. No further inclusion/exclusion criteria were specified. The evaluation team discontinued interviewing patients and providers when they agreed that they had reached data saturation as no new themes emerged.
The VA Connecticut Healthcare System Institutional Review Board approved the entirety of the study and granted a waiver of written informed consent for the entirety of this study.
Interview guide development
We developed an open‐ended interview guide to address topics relevant to the establishment, and implementation of HCoE headache services, including telehealth, and the impact of the pandemic.
Qualitative data analysis
Pre‐pandemic interviews were professionally transcribed, de‐identified, and imported into NVivo12 software. 22 We reviewed the interview guide and a selection of transcripts to create and iteratively revise the codebook. Each transcript was independently coded by two members and reconciled for discrepancies. A case comparison content analysis identified themes for perceptions of telehealth based on patient age, gender, race/ethnicity, and rurality. Pandemic interviews were analyzed using a rapid qualitative analysis approach. 23 We completed a topical matrix to compare data across interviews and identify themes, and reviewed transcripts to identify supportive quotes.
RESULTS
Administrative data
Table 1 presents demographics during the pre‐pandemic and pandemic periods. Patients were approximately three‐quarters men with a mean age of 49.6 years ± 15.0. Over half (54.8%) of the patients were White, and almost a quarter (22.4%) were Black. The majority (80.7%) lived in urban areas. All demographics changed slightly from the pre‐pandemic to pandemic periods, with no clinically meaningful differences observed. There were 23 patients who did not report their rurality status and were therefore excluded in the subgroup analysis examining differences in rurality, but they were retained for all additional analyses.
Patterns of clinical care and telehealth utilization
Before the pandemic, almost all care occurred in‐person, with 98.6% of patients utilizing at least one in‐person visit. The number of patients using CVT were fairly low (1.6%), and further declined during the pandemic (0.7%). When comparing the number of visits during the pandemic period to pre‐pandemic (Table 2), the monthly in‐person appointments declined significantly (IRR = 0.48, 95% CI = 0.45, 0.51). As expected, telehealth utilization expanded dramatically. The number of VVC appointments increased 105% during the pandemic (IRR = 2.05, 95% CI = 1.66, 2.52), and telephone visits were 15 times compared to the pre‐pandemic usage (IRR = 15.2, 95% CI = 10.7, 21.6). However, in‐person visits were still the most common way patients accessed their headache care during the pandemic, with a steady recovering since May 2020 (Figure 1).
TABLE 2.
Estimated monthly patient visits and IRRs for pre‐pandemic and pandemic periods
| Type of visit | Pre‐pandemic (August 2019–February 2020) | Pandemic (March 2020–September 2020) | IRRs | p value |
|---|---|---|---|---|
| In‐person | 12,794 (95.6) | 6099.2 (175.7) | 0.48 (0.45, 0.51) | <0.0001 |
| VVC | 73.9 (6.8) | 151.2 (8.0) | 2.05 (1.66, 2.52) | <0.0001 |
| CVT | 100.3 (7.9) | 130.5 (47.9) | 1.30 (0.62, 2.72) | 0.484 |
| Telephone | 23.9 (3.7) | 362.9 (34.6) | 15.2 (10.7, 21.6) | <0.0001 |
Abbreviations: CVT, Clinical Video Telehealth; IRRs, incidence rate ratios; VVC, VA Video Connect.
FIGURE 1.
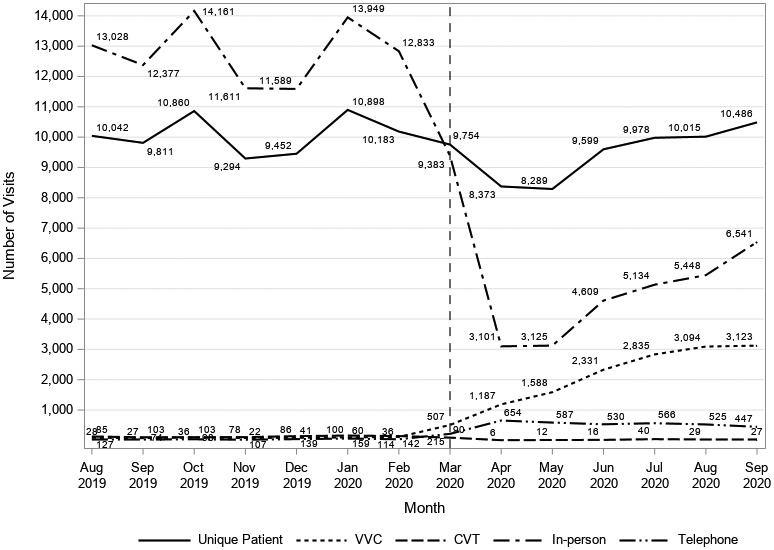
Monthly counts of in‐person visits, telehealth, and unique patients
Disparities in telehealth utilization during the pandemic period
Table 3 presents the effects of patient demographic and geographic factors on telehealth utilizations. Men had significantly decreased monthly in‐person (−1.4%) and CVT (−13.0%) utilization, and significantly increased telephone appointments (4.5%). Men and women had significantly increased monthly usage of VVC (24.7% and 24.9%) during the pandemic. There were no significant differences between men and women for in‐person and telehealth visits.
TABLE 3.
Relative risk of visit type by demographic and geographic factors during the pandemic period
| In‐person | VVC | CVT | Telephone | |||||
|---|---|---|---|---|---|---|---|---|
| RR (95% CI) | p value | RR (95% CI) | p value | RR (95% CI) | p value | RR (95% CI) | p value | |
| Gender | ||||||||
| Men | 0.90 (0.98–0.99) | Ref. | 1.25 (1.23–1.26) | Ref. | 0.87 (0.81–0.94) | Ref. | 1.05 (1.02–1.07) | Ref. |
| Women | 1.00 (0.99–1.01) | 0.070 | 1.25 (1.23–1.27) | 0.865 | 0.89 (0.76–1.04) | 0.834 | 1.04 (1.01–1.07) | 0.788 |
| Age, years | ||||||||
| <45 | 0.97 (0.96–0.98) | Ref. | 1.25 (1.23–1.26) | Ref. | 0.86 (0.77–0.95) | Ref. | 1.02 (1.00–1.05) | Ref. |
| 45–64 | 0.99 (0.98–1.00) | 0.003 | 1.25 (1.23–1.27) | 0.835 | 0.87 (0.78–0.98) | 0.769 | 1.05 (1.02–1.08) | 0.218 |
| ≥65 | 1.03 (1.02–1.05) | <0.0001 | 1.26 (1.22–1.30) | 0.598 | 0.93 (0.78–1.12) | 0.414 | 1.08 (1.04–1.13) | 0.037 |
| Race/ethnicity | ||||||||
| White | 1.00 (0.99–1.01) | Ref. | 1.25 (1.23–1.27) | Ref. | 0.95 (0.88–1.03) | Ref. | 1.03 (1.00–1.05) | Ref. |
| Black | 0.97 (0.96–0.98) | <0.0001 | 1.23 (1.20–1.25) | 0.201 | 0.48 (0.37–0.63) | <0.0001 | 1.09 (1.05–1.12) | 0.009 |
| Hispanic | 0.97 (0.96–0.99) | 0.0005 | 1.28 (1.25–1.31) | 0.039 | 0.98 (0.76–1.28) | 0.814 | 1.03 (0.98–1.08) | 0.975 |
| Other | 1.00 (0.98–1.02) | 0.926 | 1.23 (1.20–1.27) | 0.414 | 0.88 (0.70–1.10) | 0.507 | 1.04 (0.98–1.10) | 0.690 |
| Rurality | ||||||||
| Urban | 0.99 (0.98–0.99) | Ref. | 1.25 (1.24–1.26) | Ref. | 0.76 (0.69–0.84) | Ref. | 1.04 (1.02–1.06) | Ref. |
| Rural | 1.00 (0.99–1.01) | 0.169 | 1.23 (1.20–1.27) | 0.343 | 1.02 (0.92–1.13) | <0.0001 | 1.08 (1.03–1.12) | 0.096 |
Abbreviations: CI, confidence interval; CVT, Clinical Video Telehealth; RR, relative risk; IRRs, VVC, VA Video Connect.
There was a significant main effect of age, with all three age groups displaying significant changes across monthly visit modality. People under 64 years of age had significant decreases of in‐person appointments (−2.9%). However, people 65 years and older displayed an average increased trend of in‐person appointments (3.2%), which was significantly different when compared with younger people (p < 0.0001). Older patients were also more likely to have telephone appointments (8.3%) during the pandemic, which is significantly different when compared with patients under 45 years old (p = 0.037).
When stratified by race/ethnicity, all groups displayed significant increases of more than 20 percent in monthly VVC utilization during the pandemic. Black patients had significant changes in in‐person (−3.1%) and telephone (8.5%) utilization, and a dramatic 52.0% reduction in monthly CVT visits during the pandemic period. Black patients were less likely to utilize in‐person (p < 0.0001) and CVT (p < 0.0001) appointments and more likely to utilize telephone appointments (p = 0.009) during the pandemic compared with White patients. Hispanic patients were more likely to have VVC appointments (28.4% vs. 24.8%, p = 0.039) and less likely to have in‐person appointments (−2.9% vs. 0.2%, p < 0.0001) compared with White patients during the pandemic.
When compared with geographics, both urban and rural patients displayed significant increases in VVC and telephone usage during the pandemic. Urban patients had significant decreases in in‐person appointments (−1.2%). Moreover, rural‐dwelling patients were more likely to utilize CVT (−24.0% vs. 2.1%, p < 0.0001) compared with urban‐dwelling patients during the pandemic.
Qualitative data
Patients interviewed pre‐pandemic (n = 20) had a mean age of 54.8 years ± 13.77. The majority were White and male patients and had a migraine diagnosis (78.0%). Nine participated in a second interview during the pandemic with one additional patient interviewed. Patients interviewed during the pandemic (n = 10) had a mean age of 59.0 years ± 12.56. The majority were White and male patients and had a migraine diagnosis (80.0%).
Forty‐three providers interviewed pre‐pandemic work mostly as neurologists (30.2%), physiatrists (18.6%), and nurse practitioners (11.6%). Ten participated in a second interview during the pandemic, with an additional 10 new providers interviewed (n = 20). The majority were neurologists, (30.0%) physiatrists, (20.0%), nurse practitioners (20.0%), and clinical pharmacists (20.0%).
Perceptions of telehealth pre‐pandemic
Patient perceptions
Three key themes emerged: (1) telehealth decreases the impact of medical appointments on daily responsibilities; (2) telehealth improves access to headache specialists; and (3) traditional in‐person visits have disadvantages (Table 4). Many patients found telehealth appealing because they could attend headache appointments without disruption to daily responsibilities. Many drove long distances to their nearest VHA medical facility and found that telehealth would allow them to receive headache care without the long drive. Telehealth was attractive for brief follow‐up visits and for those who struggle to navigate medical facilities or have physical limitations. Several patients shared that attending in‐person appointments often contributes to their headache attacks. Whereas all patients felt that telehealth improves access to specialty headache care, many expressed concerns regarding the need for additional technology.
TABLE 4.
Key qualitative themes for patients and clinical provider perceptions of telehealth headache services
| Pre COVID‐19 pandemic themes | Illustrative interview quotes | During COVID‐19 pandemic themes | Illustrative interview quotes | |
|---|---|---|---|---|
| Patient perspectives | Telehealth decreases the impact of medical appointments on daily responsibilities | “I would love to do if I could do visits from home, that would be super simple for me in my workday. If that’s something I could do then that would be fantastic” | Traditional in‐person visits are still desirable for some, but attendance impact ability to engage in daily responsibilities | “I have to drive 45 minutes, and then by the time I’m done sitting in the bright lights and, you know, all these things kinds of stress and everything adds up so that I realize my headache’s getting worse” |
| Telehealth improves access to headache specialists | “It would be [helpful]. We have some guys that drive over 100 miles” | |||
| Telehealth is comparable to in‐person care and even enhances patient experience | “I like that I get to sit in a comfortable environment and I’m not having to drive in. I get more out of it than going to the appointment. With me the providers even seem calmer. I don’t feel like they’re rushing from one patient to next. Telehealth has been great for me” | |||
| Traditional in‐person visits have disadvantages | “By the time I get here, I sit and I wait, and then I’m in the room with the bright lights, and then I have to drive 45 minutes home, the whole process ends up being a headache‐inducing day” | Telehealth improves access but requires availability of technology and connectivity | “I don’t have a cell phone. I don’t have a home computer. I’ve got a tablet, but you know, I’m not a tech guru. I just would probably have to be walked through it I’m sure” | |
| Provider perspectives | Use of telehealth differs for initial encounters vs. follow‐up visits | “Telehealth is awesome for headaches, especially follow‐ups. Initial evals with the complicated headache patients, probably not the best. But a follow‐up just to see how things are going or just to check in and make sure that you don’t need to make any medication adjustments, that’s perfect” | Improvements in access have occurred due to telehealth | “Headache is probably the easiest one to do virtually. I think we’ve been more agile than we probably would’ve been previously because we’re able to see more people from a distance to have to come all the way for an hour to get a headache eval that we could do via video connect or phone” |
| Telehealth improves access to headache specialists | “We have a lot of Vets that come from a distance as a barrier” | Use of multiple delivery methods/tools for telehealth is essential to enhance patient engagement | “I’ll try to do an exam over the VVC even with its delays, and then we’ll just switch to a telephone call. Some people can’t connect that all, and that has to do with ‐ mostly I think it’s their WiFi connection, or their technological ability” | |
| Appropriate infrastructure is essential for telehealth headache care | “I’m not trained, and I want to do it, and I know I need to do it. It’s just it’s very difficult” | Openness to utilize telehealth differs for initial encounters vs. follow‐up visits | I think [telehealth] is a very good alternative to face‐to‐face visits, especially for follow‐up visits, it’s absolutely non‐inferior to face‐to‐face visits” | |
| There is a range of telehealth adopters from early to late (COVID forced) with varying recognition of the benefits and drawbacks | “Well, you get everything. Some people love it, some people hate it, some people just don’t like the technology or they had a difficulty with it, but even people who don’t ‐ you know, eventually when they do get it, I think they like it. There’s people that travel so they don’t want to come in” |
Abbreviations: COVID‐19, coronavirus disease 2019; VVC, VA Video Connect.
Provider perceptions
Three key themes emerged: (1) use of telehealth differs for initial encounters versus follow‐up visits; (2) telehealth improves access to headache specialists; and (3) appropriate infrastructure is essential for telehealth headache care (Table 4). Providers discussed how telehealth could be used at different stages of care, ranging from initial encounters to follow‐up visits, with many preferring an initial in‐person appointment for physical examinations. Telehealth was deemed appropriate for monitoring and adjusting pharmacotherapy and reviewing side‐effects of migraine‐specific medications. Providers expressed support for use of telehealth for behavioral headache treatments. Providers believed that telehealth is beneficial for patients who have limited access to headache specialists, especially those living in rural areas or with rare headache disorders. Providers had divided opinions on infrastructure barriers to delivering telehealth. Some found equipment setup straightforward, whereas others asserted that acquiring and utilizing equipment and logistics were burdensome. Providers lacked staff dedicated to scheduling, which frequently resulted in empty clinic slots and inefficient use of time. There were no differences in provider perceptions based on discipline.
Perceptions of telehealth during the pandemic period
Patient perceptions
Three key themes emerged; (1) traditional in‐person visits are still desirable for some, but attendance impacted the ability to engage in daily responsibilities; (2) telehealth is comparable to in‐person care and even enhances patient experience; and (3) telehealth improves access but requires availability of technology and connectivity (Table 4). Some patients preferred in‐person appointments as this mode of care was more familiar, whereas others found telehealth was comparable or more efficient than in‐person care. Those preferring telehealth cited the benefits of the reduced need to travel for a medical appointment, diminished travel stress, less disruption to their daily schedule, and not experiencing headache symptom exacerbation from in‐person appointments. Despite the strong patient interest in telehealth, patients often reported experiencing some technological barriers.
Most patients younger than age 65 years reported positive experiences with telehealth and preferred it to in‐person care. They cited an improved quality of care because providers seemed less rushed and were on time for telehealth appointments. However, some said they would need additional equipment and technological assistance for video visits. Conversely, most patients over age 65 years reported negative perceptions of telehealth citing missed interpersonal connections typical of in‐person appointments. Additionally, many continued receiving in‐person care during the pandemic.
Most women viewed telehealth favorably. They preferred not having to drive to a medical facility, which typically adds to their headache symptomatology. They viewed the pandemic as a catalyst for making telehealth more accessible and in a more comfortable location. Men had mixed opinions of telehealth; some were glad to avoid the long drive for in‐person care, however, others were concerned about technological challenges and preferred in‐person care.
Some White patients preferred telehealth, whereas others preferred in‐person care. Many Black patients found that telehealth helped them with attending medical appointments and noted they did not cancel their appointments as frequently as when they scheduled in‐person visits. Overall, there were no differences in the perceptions of telehealth based on rurality, however, people living in rural areas expressed that telehealth would minimize their need to travel for care. They also more frequently reported experiencing multiple challenges with technology and connectivity compared with patients in urban settings.
Provider perceptions
Four key themes emerged: (1) improvements in access have occurred due to telehealth; (2) use of multiple delivery methods/tools for telehealth is essential to enhance patient engagement; (3) openness to utilize telehealth differs for initial encounters versus follow‐up visits; and (4) there is a range of telehealth adopters from early to late (COVID forced) with varying recognition of the benefits and drawbacks (Table 4). Providers recognized their increased ability to expand access to care with the growth of telehealth during the pandemic. Many providers preferred in‐person appointments for initial evaluations and favored telehealth for follow‐up care. Providers who were willing to adopt telehealth reported ease of access or worked in facilities with pre‐pandemic commitments to telehealth. They used multiple telehealth or remote care tools. There were no differences in provider perceptions based on discipline.
DISCUSSION
This mixed‐methods study presents snapshots over time of a national (VHA) healthcare system’s rapid uptake of telehealth headache care from the 6 months before to the first 6 months of the COVID‐19 pandemic, along with stakeholders’ perceptions of telehealth utilization.
The dramatic shift we report of in‐person to virtual care due to the COVID‐19 pandemic is comparable to studies within 24 and outside of the VHA. 25 In‐person visits decreased from the pre‐pandemic to pandemic period, whereas telehealth utilization increased. Patients and providers considered telehealth a viable solution to increase access to headache care, a trend seen for headache 12 , 13 and other neurological conditions. 7 , 26 , 27 Patients reported receiving high‐quality care via telehealth and remaining engaged in their headache‐related care without experiencing the stress and disruption of their routines that paradoxically may exacerbate the headache disorder for which they are seeking care. 15 , 19 , 20 , 28 Minimizing disruptions to the routine of patients with headache while maintaining high‐quality headache care is invaluable.
During the pandemic, the increase in the use of telephone visits was larger than video visits. This may be because, during the very early stages of the pandemic, facilities were encouraged to convert in‐person appointments to telehealth. Many patients and providers appeared to have experienced fewer technological barriers with telephone‐only appointments or were simply more comfortable with telephone appointments. The reduction in the number of patients with headache served during the pandemic was impacted only in April and May 2020, suggesting that this was a transition period where patients and providers were becoming acclimated to telehealth while medical facilities were expanding their video telehealth infrastructure.
During the pandemic, most older patients appeared to prefer receiving in‐person care and displayed a faster update of telephone appointments when not seeing a provider in‐person, and reported difficulties with utilizing telehealth technology. Many of these patients reported missing interpersonal connection experiences during in‐person visits to their VHA medical facility. Many of the younger patients preferred receiving their headache care via video telehealth rather than conducted in‐person or by telephone. These differences in preference for headache care delivery likely reflect the combination of relative comfort levels with traditional care delivery, technology, and the means by which these patient populations form personal connections with their providers. Future efforts should be mindful of these preferences when implementing and cultivating interpersonal patient and provider connections when delivering headache care.
Uptake of telehealth during the pandemic also varied based on patient characteristics and was similar to other studies reporting on VHA telehealth utilization. 24 We found no significant differences in the actual uptake of telehealth based on patient gender. Before the pandemic, while the majority of patients had little to no experience with telehealth, many women viewed telehealth as an attractive alternative to in‐person care. During the pandemic, most women preferred telehealth and viewed the pandemic as a catalyst for change in making telehealth more accessible.
When compared with non‐Hispanic White patients, Hispanic patients had faster uptake of video visits, whereas Black patients were less likely to utilize CVT and have in‐person visits and more likely to use telephone‐only appointments. It is possible that these differences reflect patient preference, differences in access to technology or other unknown variables, or may simply be a result of difficulties with race/ethnicity categorization within VHA. 24 Future research examining the differences in uptake across different racial groups would be beneficial. Continued efforts focusing on addressing these disparities remain critical.
We expected that the increase in telehealth utilization would be higher for those living in rural regions, given that patients and providers found telehealth was desirable for those who live far from a medical facility. However, we found no differences in VVC, telephone, or in‐person visits based on rurality, and faster uptake of CVT for those living in rural areas, which still requires attending a medical facility. Our qualitative data suggest that while people living in rural and urban areas did not differ in their perceptions of telehealth, rural patients experienced more difficulties with technology access. Prior research conducted within VHA also found that utilization of VVC was more challenging for facilities that were not as experienced in providing telehealth services and/or had difficulties with broadband connection. 29 Differences in access to internet and technology may explain the observed differences in our study, or it may be a result of the pandemic impacting rural and urban areas at different times and intensities as the pandemic evolved. Continued efforts to address the digital divide in technology and connectivity for rural patients with headache are warranted, 30 in addition to examination of differences in utilization based on geographic region across the entire VHA may provide further insights into where to best direct efforts to address disparities.
Providers largely reported telehealth would improve access to headache care and would be ideal for follow‐up visits, as flexibility with care delivery methods enhances patient engagement. Before the pandemic, providers voiced concerns that their medical facilities did not have the requisite infrastructure to provide optimal care, yet during the pandemic, this became less problematic as facilities prioritized rapidly expanding telehealth capacity. This highlights that despite a rapid shift to telehealth delivery, the VHA was prepared to take on the increasing demand, and may guide future efforts for the sustainability of telehealth for headache and other healthcare.
There are limitations to this study. We examined patients receiving care within the VHA, which may differ from other healthcare systems where lack of or variability with telehealth reimbursement has historically been a barrier to telehealth adoption. Additionally, VHA‐based providers are not required to have separate medical licenses for each state in which they deliver healthcare. Noting these differences compared to the private section, studying telehealth delivery in the largest integrated healthcare system in the United States, provides a unique setting to evaluate the utilization of and preferences regarding telehealth for headache and provide insights on best practices for telehealth implementation. 31 We report data from VHA facilities that house an HCoE. Given the prevalence of headache managed exclusively by primary care providers, 32 future work is needed to understand if similar perceptions of telehealth exist solely in primary care compared with facilities where specialty care may be more easily accessible. Additionally, during the early stages of the pandemic the VHA recommended that in‐person appointments were to be cancelled and/or changed in order to minimize the need for patients to come into the hospital. However, the exact timing of when this occurred differed based on each sites ability to handle switching over to telehealth, in addition to a lack of clear cutoffs or policy changes at the facility level. Moreover, each facility was impacted by the pandemic at different time periods and policy changes may have varied across sites. This study did not have access to the specific changes implemented across sites, which may have impacted differences in utilization of the different types of telehealth modality.
CONCLUSIONS
The uptake of telehealth for headache care has increased dramatically since the start of the COVID‐19 pandemic. The use of telehealth for managing headache disorders appears to be highly acceptable to both patients and providers. Differences exist in telehealth utilization based on patient age, race/ethnicity, and rurality. Our findings support a hybrid approach to headache care delivery utilizing combinations of in‐person, telephone, and video telehealth visits. In‐person visits may be more appropriate for initial appointments and when directly administering treatments, whereas telehealth may be more conducive for follow‐up visits that involve monitoring and adjusting treatment for headache. To facilitate more equitable access to telehealth, it is crucial to identify patient groups who face barriers, and consider whether the requisite infrastructure is in place to foster the optimal implementation of telehealth for headache. Understanding patients’ values and preferences regarding visit type is critical for directing educational efforts and resources to those most in need. Future research examining ways to increase and improve access to telehealth for headache care, both within VHA and the private sector, is essential.
CONFLICT OF INTEREST
A.S.G., B.T.F., K.W., H.L., R.G., S.B., S.R., L.B., and T.M.D. report no conflicts of interest. E.K.S. has consulted for GlaxoSmithKline, Eli Lilly, and Click Therapeutics. J.J.S. has received grant support from the Department of Veterans Affairs, the American Academy of Neurology, and the American Heart Association/American Stroke Association.
AUTHOR CONTRIBUTIONS
Study concept and design: Amy S. Grinberg, Brenda T. Fenton, Elizabeth K. Seng, Teresa M. Damush. Acquisition of data: Amy S. Grinberg, Brenda T. Fenton, Kaicheng Wang, Hayley Lindsey, Roberta E. Goldman, Sean Baird, Samantha Riley, Laura Burrone, Elizabeth K. Seng, Teresa M. Damush, Jason J. Sico. Analysis and interpretation of data: Amy S. Grinberg, Brenda T. Fenton, Kaicheng Wang, Hayley Lindsey, Roberta E. Goldman, Sean Baird, Samantha Riley, Laura Burrone, Elizabeth K. Seng, Teresa M. Damush, Jason J. Sico. Drafting of the manuscript: Amy S. Grinberg. Revising it for intellectual content: Amy S. Grinberg, Brenda T. Fenton, Kaicheng Wang, Roberta E. Goldman, Elizabeth K. Seng, Teresa M. Damush, Jason J. Sico. Final approval of the completed manuscript: Amy S. Grinberg, Brenda T. Fenton, Kaicheng Wang, Hayley Lindsey, Roberta E. Goldman, Sean Baird, Samantha Riley, Laura Burrone, Elizabeth K. Seng, Teresa M. Damush, Jason J. Sico.
Supporting information
Fig S1‐S4
Table S1
ACKNOWLEDGEMENTS
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Grinberg AS, Fenton BT, Wang K, et al. Telehealth perceptions and utilization for the delivery of headache care before and during the COVID‐19 pandemic: A mixed‐methods study. Headache. 2022;62:613–623. doi: 10.1111/head.14310
Funding information
This study was supported by the Veterans Health Administration Headache Centers of Excellence (Sico)’ VA HSRD 51K6HX002715‐02 (Damush)
REFERENCES
- 1. Schreiber SS. Teleneurology for veterans in a major metropolitan area. Telemed J E Health. 2018;24(9):698‐701. [DOI] [PubMed] [Google Scholar]
- 2. Wechsler LR. Advantages and limitations of teleneurology. JAMA Neurol. 2015;72(3):349‐354. [DOI] [PubMed] [Google Scholar]
- 3. Roy B, Nowak RJ, Roda R, et al. Teleneurology during the COVID‐19 pandemic: a step forward in modernizing medical care. J Neurol Sci. 2020;414:116930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McGinley MP, Ontaneda D, Wang Z, et al. Teleneurology as a solution for outpatient care during the COVID‐19 pandemic. Telemed J E Health. 2020;26(12):1537‐1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Grossman SN, Han SC, Balcer LJ, et al. Rapid implementation of virtual neurology in response to the COVID‐19 pandemic. Neurology. 2020;94(24):1077‐1087. [DOI] [PubMed] [Google Scholar]
- 6. Friedman DI, Rajan B, Seidmann A. A randomized trial of telemedicine for migraine management. Cephalalgia. 2019;39(12):1577‐1585. [DOI] [PubMed] [Google Scholar]
- 7. Hatcher‐Martin JM, Adams JL, Anderson ER, et al. Telemedicine in neurology: telemedicine work group of the American Academy of Neurology update. Neurology. 2020;94(1):30‐38. [DOI] [PubMed] [Google Scholar]
- 8. Demaerschalk BM, Raman R, Ernstrom K, Meyer BC. Efficacy of telemedicine for stroke: pooled analysis of the Stroke Team Remote Evaluation using a Digital Observation Camera (STRokE DOC) and STRokE DOC Arizona telestroke trials. Telemed J E Health. 2012;18(3):230‐237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zulman DM, Wong EP, Slightam C, et al. Making connections: nationwide implementation of video telehealth tablets to address access barriers in veterans. JAMIA Open. 2019;2(3):323‐329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID‐19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020;27(7):1132‐1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Weigel G, Ramaswamy A, Sobel L, Salganicoff A, Cubanski J, Freed M. Opportunities and Barriers for Telemedicine in the U.S. During the COVID‐19 Emergency and Beyond; 2020. Accessed July 7, 2020. https://www.kff.org/womens‐health‐policy/issue‐brief/opportunities‐and‐barriers‐for‐telemedicine‐in‐the‐u‐s‐during‐the‐covid‐19‐emergency‐and‐beyond/ [Google Scholar]
- 12. Chiang C‐C, Halker Singh R, Lalvani N, et al. Patient experience of telemedicine for headache care during the COVID‐19 pandemic: an American Migraine Foundation survey study. Headache. 2021;61(5):734‐739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Minen MT, Szperka CL, Kaplan K, et al. Telehealth as a new care delivery model: the headache provider experience. Headache. 2021;61(7):1123‐1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Burch RC, Loder S, Loder E, Smitherman TA. The prevalence and burden of migraine and severe headache in the United States: updated statistics from government health surveillance studies. Headache. 2015;55(1):21‐34. [DOI] [PubMed] [Google Scholar]
- 15. Leonardi M, Raggi A. A narrative review on the burden of migraine: when the burden is the impact on people’s life. J Headache Pain. 2019;20(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stovner LJ, Nichols E, Steiner TJ, et al. Global, regional, and national burden of migraine and tension‐type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):954‐976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mauser ED, Rosen NL. So many migraines, so few subspecialists: analysis of the geographic location of United Council for Neurologic Subspecialties (UCNS) certified headache subspecialists compared to United States headache demographics. Headache. 2014;54(8):1347‐1357. [DOI] [PubMed] [Google Scholar]
- 18. Bonafede M, Sapra S, Shah N, Tepper S, Cappell K, Desai P. Direct and indirect healthcare resource utilization and costs among migraine patients in the United States. Headache. 2018;58(5):700‐714. [DOI] [PubMed] [Google Scholar]
- 19. Burstein R, Noseda R, Borsook D. Migraine: multiple processes, complex pathophysiology. J Neurosci. 2015;35(17):6619‐6629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Borkum JM. The migraine attack as a homeostatic, neuroprotective response to brain oxidative stress: preliminary evidence for a theory. Headache. 2018;58(1):118‐135. [DOI] [PubMed] [Google Scholar]
- 21. US Department of Veteran Affairs . What is Telehealth?; 2020. Accessed April 20, 2020. https://www.telehealth.va.gov/what‐telehealth [Google Scholar]
- 22. Nvivo . NVivo Qualitative Data Analysis Software; 2020. Accessed June 29, 2020. https://www.qsrinternational.com/nvivo‐qualitative‐data‐analysis‐software/home [Google Scholar]
- 23. Hamilton AB, Finley EP. Qualitative methods in implementation research: an introduction. Psychiatry Res. 2019;280:112516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ferguson JM, Jacobs J, Yefimova M, Greene L, Heyworth L, Zulman DM. Virtual care expansion in the Veterans Health Administration during the COVID‐19 pandemic: clinical services and patient characteristics associated with utilization. J Am Med Inform Assoc. 2021;28(3):453‐462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Verma S. Early Impact Of CMS Expansion Of Medicare Telehealth During COVID‐19, Health Affairs Blog, July 15, 2020. doi: 10.1377/hblog20200715.454789 [DOI]
- 26. Bramanti A, Calabrò RS. Telemedicine in neurology: where are we going? Eur J Neurol. 2018;25(1):e6. [DOI] [PubMed] [Google Scholar]
- 27. Cardinale AM. The opportunity for telehealth to support neurological healthcare. Telemed J E Health. 2018;24(12):969‐978. [DOI] [PubMed] [Google Scholar]
- 28. Leonardi M, Steiner TJ, Scher AT, Lipton RB. The global burden of migraine: measuring disability in headache disorders with WHO’s classification of functioning, disability and health (ICF). J Headache Pain. 2005;6(6):429‐440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jacobs J, Ferguson JM, Van Campen J, et al. Organizational and external factors associated with video telehealth use in the Veterans Health Administration before and during the COVID‐19 pandemic. Telemed J E Health. 2022;28(2):199‐211. [DOI] [PubMed] [Google Scholar]
- 30. Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: How COVID‐19’s telemedicine expansion could exacerbate disparities. J Am Acad Dermatol. 2020;83(5):e345‐e346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kichloo A, Albosta M, Dettloff K, et al. Telemedicine, the current COVID‐19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Fam Med Community Health. 2020;8:e000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Steiner TJ, Jensen R, Katsarava Z, et al. Aids to management of headache disorders in primary care (2nd edition). J Headache Pain. 2019;20(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1‐S4
Table S1


