Abstract
The aim of this review is to explore how metabolic changes induced by diets high in saturated fat (HFD) affect nucleus accumbens (NAc) dopamine neurotransmission and food intake, and to explore how stress and inflammation influence this process. Recent evidence linked diet-induced obesity and HFD with reduced dopamine release and reuptake. Altered dopamine neurotransmission could disrupt satiety circuits between NAc dopamine terminals and projections to the hypothalamus. The NAc directs learning and motivated behaviours based on homeostatic needs and psychological states. Therefore, impaired dopaminergic responses to palatable food could contribute to weight gain by disrupting responses to food cues or stress, which impacts type and quantity of food consumed. Specifically, saturated fat promotes neuronal resistance to anorectic hormones and activation of immune cells that release proinflammatory cytokines. Insulin has been shown to regulate dopamine neurotransmission by enhancing satiety, but less is known about effects of diet-induced stress. Therefore, changes to dopamine signalling due to HFD warrant further examination to characterise crosstalk of cytokines with endocrine and neurotransmitter signals. A HFD promotes a proinflammatory environment that may disrupt neuronal endocrine function and dopamine signalling that could be exacerbated by the hypothalamic–pituitary–adrenal and κ-opioid receptor stress systems. Together, these adaptive changes may dysregulate eating by changing NAc dopamine during hedonic versus homeostatic food intake. This could drive palatable food cravings during energy restriction and hinder weight loss. Understanding links between HFD and dopamine neurotransmission will inform treatment strategies for diet-induced obesity and identify molecular candidates for targeted therapeutics.
Keywords: High-fat diet, Dopamine neurotransmission, Nucleus accumbens, Homeostatic feeding, Hedonic feeding, Inflammation, Insulin resistance, Diet-induced obesity, Hypothalamic–pituitary–adrenal stress axis, Kappa-opioid receptors
Introduction
Overweight and obesity prevalence has steadily increased with 42·4 % of US adults currently classified as obese1. Food intake is controlled by many factors, including an obesogenic food environment with ubiquitous access to cheap, calorie-rich, palatable foods. Herein, ‘palatable foods’ are defined as those with high energy density primarily from fat or sugar. Over-consumption of palatable food is proposed to shift brain dopamine signalling within the nucleus accumbens (NAc)2,3. The NAc is a limbic–motor interface which integrates salient stimuli with memory and context, reward availability and value, sensory information, physiological state and homeostatic needs4. It sends efferent projections to cortical and motor regions, processing environmental and biological stimuli to drive motivated behaviour. Disrupting homeostasis in the NAc by stimulating excessive dopamine release may contribute to obesity with extended access to highly palatable foods that acutely cause phasic dopamine release in the NAc5,6. Perturbations to NAc dopamine by consuming a diet high in saturated fat (HFD) may disrupt natural NAc food reward learning and reduce NAc dopamine tone over time7–11. Changes in dopamine tone or phasic dopamine release in the NAc may significantly impact food seeking8,11–13, reward8,9,11,12 and satiety11,13,14. However, the mechanisms by which diet and obesity alter dopamine neurotransmission and behaviour are not fully characterised. Therefore, the purpose of this review is to highlight the literature and identify research gaps related to mechanisms by which diet-induced obesity interfere with NAc dopamine, including interactions between inflammation, physiological stress and κ-opioid receptor function which together with endocrine hormones modulate NAc dopamine to influence food intake behaviours.
Dopamine circuitry and motivated behaviour
Food intake is controlled by energy status and neural circuits regulating homeostasis and reward. Two primary dopamine circuits include the nigrostriatal tract from substantia nigra to dorsal striatum/caudate putamen controlling motivation and habitual behaviour, and the mesocorticolimbic tract from ventral tegmental area (VTA) to NAc controlling Pavlovian reward learning15. These dopamine neurons form synaptic terminals with γ-aminobutyric (GABA)-releasing medium spiny neurons (MSNs), comprising ~90–95 % of neurons within the NAc16, which express dopamine D1 receptor (D1R) and dopamine D2 receptor (D2R) subtypes that propagate dopamine signalling to control cortical and motor processing17. An excellent review of homeostatic crosstalk with the dopamine reward system by Ferrario and colleagues highlighted how glucose and endocrine indicators of energy status (insulin, leptin) inhibit or excite dopaminergic reward activity directly in the VTA, NAc and striatum2. Hormones also indirectly modulate dopaminergic activity by targeting key homeostatic regions in the hypothalamus that initiate food seeking behaviours via GABAergic and glutamatergic inputs to VTA and NAc2,18. There are multiple subtypes of these neurons within the lateral hypothalamus (LH) and arcuate nucleus (ARC) that respond to energy status by releasing appetitive neuropeptides. These include orexin/hypocretin (orexigenic, LH to VTA/NAc), melanin-concentrating hormone (orexigenic, LH to NAc), neurotensin (anorectic, LH to VTA/LH orexin neurons), neuropeptide Y (NPY)/agouti-related peptide (AGRP) (orexigenic, ARC to LH) and pro-opiomelanocortin (POMC)/cocaine- and amphetamine-regulated transcript (CART) (anorectic, ARC to VTA/NAc)2. These appetitive systems underly many mechanisms by which HFD and stress perturb dopamine control of food intake and will be discussed in detail throughout this review. In addition to homeostatic engagement of hypothalamus afferents to the VTA and NAc, feeding is also controlled by a NAc to hypothalamus satiety circuit. This was demonstrated by direct inhibition or stimulation of D1R-expressing MSNs that project from the NAc shell to the LH, where D1R inhibition increased licking for fat and sugar but stimulation decreased ingestive responses19. Overall, NAc dopamine neurotransmission and subsequent GABA output controls motivated behaviour, and homeostatic signals from the hypothalamus comprise important inputs that regulate feeding. Therefore, diet-induced disruption to these circuits may be particularly consequential for individuals restricting food intake (Fig. 1).
Fig. 1.
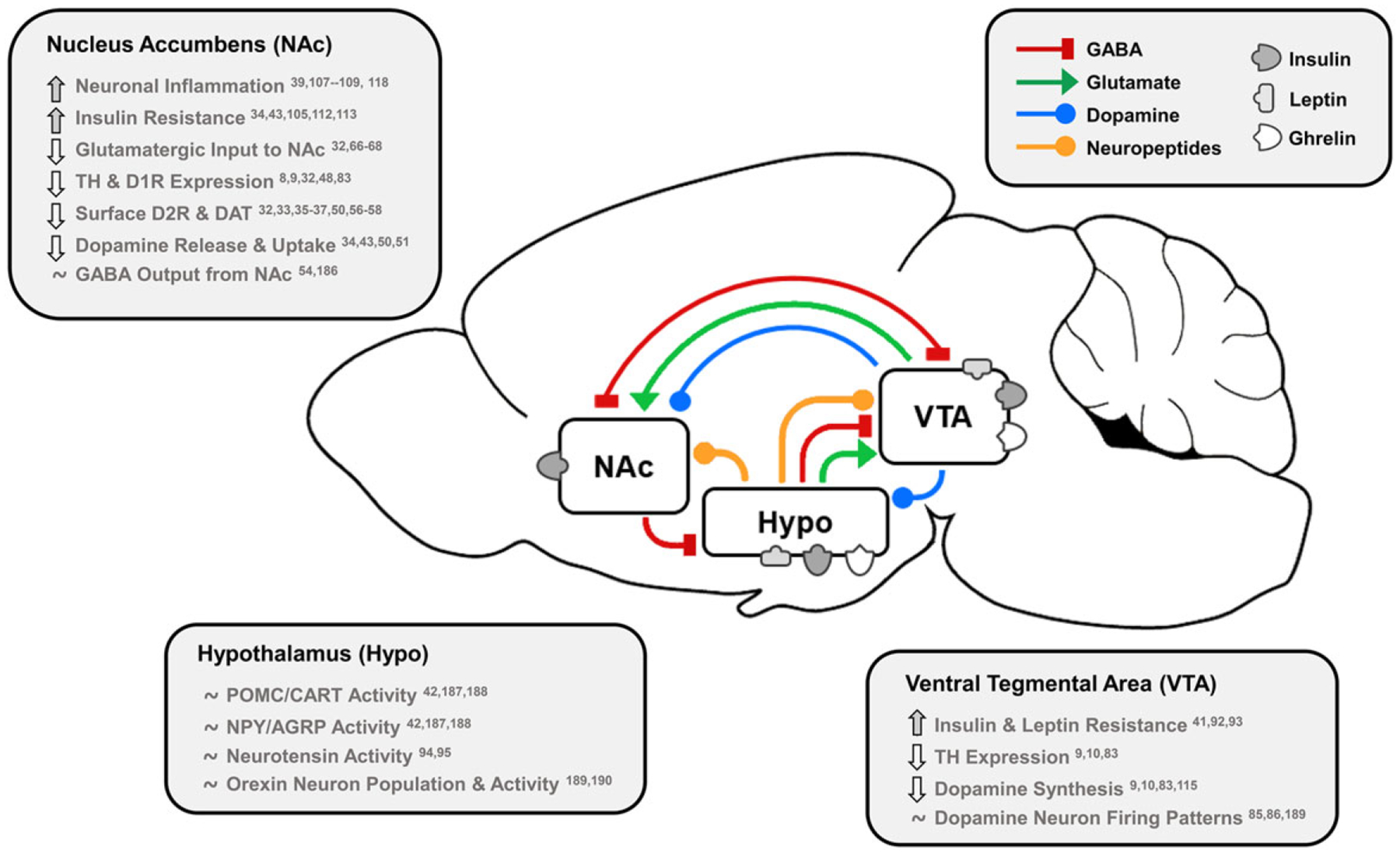
Effects of dietary fat and obesity on hedonic and homeostatic dopamine circuits: homeostatic, dopamine-motivated feeding and reward learning circuits overlap as insulin and leptin convey body energy status to the hypothalamus (Hypo) and VTA. In response, hypothalamic nuclei send appetitive neuropeptides to the VTA and NAc to influence food intake, and NAc dopamine neurotransmission is directly stimulated by hormonal action in the NAc and VTA. This information is also conveyed via dopamine, GABA and glutamate from the VTA to NAc, and the NAc responds by sending GABA to hypothalamic feeding regions, the VTA as a regulatory feedback circuit, and thalamic, motor and cognitive cortical regions. Effects of long-term HFD or palatable food consumption are highlighted by region. This characterises how diet-induced obesity dysregulates key neurotransmitters, neuropeptides and hormones that regulate food intake to reduce dopamine neurotransmission leading to overeating and further weight gain.
TH, tyrosine hydroxylase; D1R/D2R, dopamine type 1/2 receptors; DAT, dopamine transporter; POMC/CART, pro-opiomelanocortin/cocaine- and amphetamine-regulated transcript; NPY/AGRP, neuropeptide Y/agouti-related peptide.
The ventral striatum is central to reward processing, integrating glutamatergic and GABAergic inputs from the hypothalamus, cortex, amygdala and hippocampus with dopaminergic projections from the VTA or substantia nigra20. The NAc assimilates these signals to determine hedonic value and sends GABA via the ‘direct’ route with direct control of dopamine release with afferents to VTA, internal globus pallidus or substantia nigra (MSNs with D1Rs), or the ‘indirect’ route via globus pallidus externa and ventral pallidum (MSNs with D2Rs). GABA afferents to the thalamus then modulate excitatory output to the cortex that controls behavioural selection and motor activity17. D1Rs have lower affinity for dopamine than do D2Rs21,22 and respond to phasic dopamine release due to unexpected rewards and cue learning that promotes cyclic adenosine monophosphate (cAMP) signalling with downstream phosphorylation of dopamine-regulating proteins15 and increased MSN firing probability23. Conversely, D2Rs are activated at lower dopamine concentrations by spontaneous pacemaking activity of dopamine neurons24 than D1Rs, and activate opposing intracellular signalling, to decrease MSN firing probability23. Consequently, D2Rs communicate dopamine tone so that phasic release events (unexpected rewards) or lack thereof (absence of expected reward) alter concentration that is detected by D1Rs to promote response. This dopamine signalling pattern is important for NAc learning that relies on phasic dopamine release initiated by a rewarding, unconditioned stimulus that becomes tied to a conditioned cue over repeated exposures. In the theory of reward prediction error25, hedonic value is determined based on magnitude of dopamine release, which is up- or down-regulated upon further cue exposures. This reward-learning model is central to motivation and survival and may become ‘hijacked’ by palatable foods.
Dopamine in the NAc responds to food intake and may promote obesity
Dopamine pathways control motivated and habitual behaviour, including that related to food. The VTA–NAc mesolimbic dopaminergic pathway influences motivated behaviour by enhancing willingness to work for rewards26. Mesolimbic dopamine increased during lever pressing to obtain food27, and NAc core dopamine depletion reduced response in fixed ratio tasks with more pronounced decreases in higher ratio schedules28. Moreover, food deprivation augments dopaminergic responses to food, demonstrated by increased NAc dopamine in response to maize oil feeding after food restriction6. Interestingly, phasic dopamine release was enhanced in food-restricted rats following cues that predict sucrose versus cues for saccharin5. This suggested energy-providing foods have greater salience than energy-null foods when homeostatic energy needs influence physiological state, but dopamine release induced by food cues that initiate food intake could be enhanced in individuals with obesity. Indeed, those who were obese showed enhanced striatal and NAc dopamine release in response to palatable food images after consumption of an energy-dense meal29. This was in contrast to healthy, lean individuals whose meal pleasantness ratings correlated with striatal dopamine release30 and who experienced striatal dopaminergic activation immediately during milkshake consumption and 20 min post-ingestion when gut signals reached the brain31. Additionally, when food access is not interrupted but availability of palatable foods is limited, dopamine release is increased during access to the preferred food under limited compared with ad libitum access in rodents. For instance, constant access to sucrose for 21 d failed to evoke the same magnitude of dopamine release in the NAc shell as daily intermittent access to sucrose14. Therefore, dopamine release in response to food can be influenced by physiological state and food availability, and the NAc controls initial hedonic responses to palatable food intake and promotes cue-associated learning and motivation to obtain food that is interfaced with homeostatic need.
Effects of HFD on dopamine
Prolonged consumption of highly palatable diets may disrupt dopamine reward signalling. Chronic HFD intake and diet-induced obesity impact VTA dopamine neuron activity and interfere with mechanisms regulating dopamine at synaptic terminals within the NAc. Changes include lowered D2R binding potential as well as reduced dopamine transporter (DAT) function and membrane localisation32–37. Furthermore, HFD intake activates inflammatory processes that may contribute to neuronal insulin resistance34,38–40. Central insulin and leptin resistance attenuate satiation and reward valuation of palatable foods by altering NAc synaptic dopamine and disrupt orexigenic and anorectic communication between the LH, ARC and VTA34,40–43. Finally, chronic HFD intake shifts opioid control of NAc dopamine neurotransmission44, which could amplify stress-induced feeding8,45 and have consequences for obese individuals on energy restricted diets. Overall, studies presented below demonstrate HFD consumption acutely increases NAc dopamine6,46,47, but prolonged intake reduces capacity for dopamine neurotransmission through repeated stimulation of dopamine receptors9,48, resistance to hormonal and homeostatic signals34,40–43, and up-regulated inflammatory signalling38,39.
Effects on synaptic control of dopamine within the NAc
Dopamine transporter, D1 receptors and D2 receptor availability.
Chronic HFD intake alters dopamine neurotransmission to promote food seeking with obesity susceptibility dependent on the activation of NAc dopamine and alteration to dopamine receptors and the DAT. For example, genetic differences in the DAT gene significantly increased likelihood of obesity49. Further, intake of a HFD or intraperitoneal injection of lipid solution acutely increased NAc dopamine46, and sucrose intake dose-dependently increased NAc dopamine47. Conversely, chronic HFD feeding reduced maximal dopamine reuptake rate (Vmax)34, while extended access to a Western diet (WD), a HFD with added sugar, decreased striatal and NAc core dopamine release and reuptake43. Further, while obesogenic diet and food restriction both reduced striatal DAT surface expression and reuptake50, obesogenic diet decreased but food restriction increased D2R protein expression. These findings suggest food restriction primes the dopamine system to respond to food exposure. HFD-induced changes develop over time, as 6-week but not 2-week exposure to HFD decreased NAc dopamine Vmax and membrane-associated DAT expression33. Effects of HFD also depend on fat type, as rats chronically fed 50 % saturated HFD experienced reduced DAT and increased D1R protein expression versus 50 % monounsaturated olive oil or control diet32. Similarly, consumption of a HFD versus control diet reduced dopamine reuptake Vmax and attenuated phasic dopamine release, which did not occur in mice fed a diet high in polyunsaturated flax-seed oil51. Further, consumption of a WD versus low-fat control diet for 12 weeks reduced NAc D1R protein expression but increased total D2R and p-dopamine- and cAMP-regulated phosphoprotein-32 (DARPP-32) protein expression9, the latter which activates D1R-mediated signalling downstream52. HFD feeding from lactation through adulthood similarly increased NAc DARPP-32 but decreased D1R and D2R gene expression that was exacerbated after HFD was removed for 4 weeks48. Conversely, HFD-induced reduction in D1Rs and D2Rs was restored by HFD removal. These results suggest adaptive changes in DAT, D1R and D2R expression due to repeated HFD-mediated activation of D1R signal transduction leading to down-regulated D1R and D2R availability. Interestingly, D1R-expressing MSNs were activated in proportion to palatable food consumption while intra-uterine protein-restriction-induced reduction of NAc shell D1Rs increased palatable milk consumption53, leading Durst et al. (2019) to suggest D1R stimulation during consumption builds to a ‘satiety threshold’ sent to LH GABA neurons. Endocannabinoid-mediated synaptic plasticity of this circuit was later demonstrated to promote overeating after food restriction or exposure to HFD54. Therefore, the NAc–LH satiety circuit may be inhibited due to HFD-induced disruption of D1R signalling.
Much attention has also been paid by neuroimaging studies to striatal D2R availability. Decreased NAc core but increased NAc shell D2R binding potential were linked to impulsive behaviour55. Furthermore, calorie restriction was used to maintain similar intake between groups, and chronic HFD in absence of obesity decreased NAc D2R protein expression and increased impulsivity in a task to obtain food56. Conversely, obesity in absence of diet manipulations also affects D2Rs, as chow-fed, obese mice with genetic leptin receptor inactivation increased NAc and striatal D2R availability in vivo using [11C]raclopride but decreased D2R availability ex vivo using [3H]spiperone57. Interestingly, these differences were eliminated between calorie-restricted lean and obese mice57. Based on the radio-ligands used, results suggested obesity reduced striatal dopamine concentration and postsynaptic D2R availability. Conversely, 3–4 weeks of limited daily access to a cafeteria diet reduced ethanol intake but increased D2R autoreceptor function58. One group used [3H]raclopride35–37 to assess diet-induced alterations to D2Rs over time and found that 20 d on a 40 % HFD versus chow increased D2R binding density in the NAc and striatum that was maintained after HFD removal35. Conversely, diet-induced obesity that developed over 20 weeks of HFD feeding decreased striatal D2R binding36 but increased NAc core and striatal D2R mRNA expression37. Further, obesity-resistant mice had increased NAc DAT binding36, which may promote dopamine clearance and protect against obesity. These studies suggest palatable foods up-regulate dopamine neurotransmission which is shifted by chronic HFD intake to decreased D2R binding and capacity for dopamine release. However, clinical research showed negative correlation between age and D2R binding throughout midbrain regions with body mass index (BMI) correlating positively with D2R availability only for those over 30 years old59. This suggests that adolescent striatal development and decline of D2R expression patterns with age could partially explain associations between D2R availability and BMI. Overall, HFD-induced obesity alters function and expression of NAc proteins regulating dopamine to reduce capacity for NAc dopaminergic reward that promotes overeating and weight gain.
Acetylcholine, GABA and glutamate in the NAc.
Control of VTA–NAc dopamine signals that initiate motivated actions relies on a complex network of acetylcholine, glutamate and GABA, which are all affected by HFD intake. About 5 % of NAc neurons are GABAergic or cholinergic interneurons (CIN)17. The latter stimulate dopamine release via acetylcholine that activates acetylcholine receptors on dopamine axon terminals60. Activation of MSNs relies on glutamate targeting ionotropic N-methyl-d-aspartate (NMDA) and α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptors (AMPAR) on CINs to release acetylcholine60,61. Glutamate also negatively regulates dopamine directly by metabotropic glutamate receptors62 and indirectly via MSN retrograde H2O2 release63. Glutamatergic inputs to NAc communicate physical and nutritive qualities of food, memory, physiological need and environmental cues20, which prompts initiation or cessation of feeding. Indeed, either AMPA and NMDA receptor agonism64 or antagonism65 in the NAc shell can induce voracious feeding. However, consumption of a WD66 or a HFD32,67,68 increased AMPA/NMDA receptor ratio66,67, prolonged excitatory postsynaptic currents onto MSNs66, and increased NAc phosphorylated GluR1 AMPA subunit32 and NAc shell NMDAR and metabotropic glutamate receptor68 expression, but inhibited ability to induce long-term depression onto MSNs67, effects which together increased motivation to obtain palatable food67,68. Further, the NAc receives GABA from VTA69, globus pallidus externa70, cortex71, bed nucleus of the stria terminalis72, and local MSNs and interneurons24. GABA signals reduce dopamine concentration73 to stop cue-associated reward behaviour70 or food intake and induce avoidance behaviour69,71. These effects occur directly via dopamine axon terminal74 GABAB-receptor-mediated reduction of dopamine73 and indirectly via GABAA-receptor-mediated reduction of acetylcholine69,73. Conversely, NAc shell GABAA and GABAB antagonism decreased food intake while fasted75, but agonism increased fat and sucrose76 as well as regular food intake while sated77, suggesting GABA inhibits NAc-LH MSNs to disinhibit feeding. However, GABAB agonism also inhibited bingeing on HFD during an intermittent access paradigm78. Overall, glutamatergic and cholinergic signalling within NAc promotes food intake, while the system of GABAergic disinhibition throughout the NAc, VTA and hypothalamus may decrease dopamine release and stop intake or disinhibit feeding via NAc shell MSNs, but prolonged HFD intake reduces sensitivity of these systems to promote overeating and highlights the complexity of dopaminergic regulation of ingestive behaviours.
Effects on the VTA
VTA dopaminergic output underlies motivated behaviours and is affected by consumption of a HFD24,79,80. The VTA receives glutamatergic and GABAergic signals from local interneurons and limbic and cortical regions80 as well as local somatodendritic dopamine release that negatively regulates dopamine neuron excitability24. Glutamatergic and cholinergic inputs activate receptors on VTA dopamine neurons to promote NAc dopamine release81. The VTA receives orexin from LH, NPY from orexigenic glucose-sensing ARC neurons2,82, and anorectic POMC/CART signals from ARC2. The VTA integrates this information related to homeostasis and environmental cues with dopamine neurons projecting to the NAc. However, HFD intake reduced VTA tyrosine hydroxylase (TH) mRNA10 and protein9,83 expression, which occurred regardless of obesity and was restored after switching to low-fat diet10. This showed HFD intake reduced capacity for dopamine synthesis, because TH is the rate-limiting enzyme in synthesising dopamine84. Further, 6-week ad libitum HFD feeding attenuated D2R agonist quinpirole-induced inhibition of VTA dopamine neuron firing, suggesting D2R desensitisation85, whereas intermittent access to cafeteria diet for 3 weeks increased inhibitory effects of quinpirole and reduced ethanol and sucrose intake58, showing sensitivity of VTA autoreceptor function to type and length of diet. HFD intake similarly reduced excitability of mouse VTA GABA neurons86 that reduce NAc dopamine concentration69,73 and stop behaviour (e.g. food intake)69–71. Overall, HFD and obesity affect VTA dopamine and GABA neuron protein expression and function, and a further diet-induced effect includes altered sensitivity to direct responses of VTA neurons to hormonal indicators of energy status.
VTA neurons express receptors for insulin and leptin87 with leptin-receptor-expressing dopamine and GABA neurons projecting to the NAc88, and activation of these receptors decreases food intake. Insulin in the VTA is important in reducing dopamine neuron activity to control behaviour, demonstrated by reduced locomotion and NAc dopamine after VTA application of insulin89. In the VTA, insulin reduced somatodendritic dopamine release and hedonic feeding, which was abolished by blocking the DAT90. Furthermore, insulin induced AMPAR- and endocannabinoid-mediated long-term depression in VTA dopamine neurons which was attenuated by genetic or diet-induced elevation of insulin91,92, showing a role of insulin in the VTA to signal satiety that is inhibited by HFD. VTA signalling is also affected by leptin resistance, as HFD consumption reduced ability of VTA leptin administration to limit food intake and weight gain in obesity-prone rats93 and induced leptin resistance specifically in the VTA and ARC41. Diet-induced obesity also spurred leptin resistance in ARC NPY/AGRP and POMC/CART neurons42 and LH neurotensin–galanin–GABA neurons94,95 necessary for reducing food intake by inhibiting orexin and activating VTA neurons2,94,95. Therefore, lack of hypothalamic and VTA insulin and leptin signalling may reduce capacity for NAc dopamine release to promote compensatory over-seeking of palatable food.
Effects on anorectic hormones in the NAc
Insulin gains access to the brain via transport across the blood–brain barrier96 and local production in the brain97, and activation of tyrosine kinase receptors by insulin promotes phosphatidylinositol-3 kinase (PI3K) and protein kinase B (Akt) or the mitogen-activated protein kinase (MAPK)/extracellular-signal-regulated kinase (ERK) pathways, the latter which is also known as the Ras-Raf-MAPK/ERK kinase (MEK)-ERK cascade96. Insulin valuates food reward by fine-tuning dopamine neurotransmission at NAc dopamine terminals. For example, NAc core and shell insulin administration increased dopamine release and reuptake in control animals but not in animals consuming HFD34,40. Furthermore, HFD-induced impairments were reversed by promoting insulin receptor substrates, while effects of insulin were abolished by inhibiting insulin receptor or PI3K34, implicating HFD-induced insulin resistance in impaired dopamine control. Insulin receptors expressed on NAc dopamine neuron terminals40 activate Akt and ERK to shuttle DAT to the plasma membrane to promote dopamine reuptake98. Dopamine release is also promoted by insulin as NAc CINs expressed insulin receptors at high density40 and released acetylcholine in response to insulin40,43, supporting necessity of insulin in encoding sucrose preference40. While an obesogenic diet blunted insulin-induced NAc dopamine release and reuptake43, food restriction alternately enhanced insulin receptor expression and stimulated dopamine reuptake50. Similar effects have been shown with impaired leptin signalling, as leptin-deficient mice had reduced electrically evoked NAc shell dopamine release and reduced TH and DAT expression88, whereas leptin increased activity of NAc DAT and TH and increased amphetamine-evoked dopamine release99. Leptin activates intracellular signalling cascades similarly to insulin in addition to the Janus-activated kinases (JAK)–signal transducers and activators of transcription (STAT)–suppressors of cytokine signalling (SOCS) pathway that reduce NPY/AGRP but increase POMC/CART and LH neurotensin neuronal activity2,100. Further, leptin is also transported into the brain101 and is expressed in plasma and cerebrospinal fluid in proportion to adipocyte size102 and adiposity103, suggesting that leptin conveys energy sufficiency. However, individuals with obesity have elevated plasma leptin100, supporting leptin resistance as a comorbidity of obesity. Collectively, these studies showed NAc insulin promotes reward seeking by encoding reward salience via increased dopamine release and maintenance of dopamine reuptake, and, whereas food restriction may prime dopamine responses through insulin, HFD-induced insulin and leptin resistance may reduce NAc dopamine neurotransmission to alternately promote food seeking. A putative contributor to leptin and insulin resistance associated with diet-induced obesity is chronic inflammation triggered by saturated fats and rapid adipose tissue expansion38,104,105.
HFD and obesity drive inflammatory processes that modulate dopamine control of food intake
Adipose tissue expansion in obesity reduces blood flow to adipocytes to induce hypoxia and release of cytokines causing local and systemic inflammation104. Indeed, increased expression of inflammatory genes triggered by hypoxia-inducible factor 1α were found in the adipose tissue of insulin-resistant individuals with obesity106. Further, obesity and HFD intake both stimulated cytokine release from peripheral and central immune cells106–108. Saturated fatty acids promote inflammation directly by promoting lipopolysaccharide (LPS) absorption109 and activating macrophages, microglia and astrocytes similarly to LPS by binding to toll-like receptor-4 (TLR4) and binding partners cluster of differentiation 14 and myeloid differentiation factor-2 (MD-2) to prompt receptor internalisation38,39,108,110. Toll-like immune receptors recognise pathogens, trigger nuclear factor-kappa B (NF-κB) signalling, and promote cytokine release38,111. Macrophages exposed to saturated fatty acids showed direct binding to MD-2 and TLR4, increased NF-κB and MAPK signalling, and interleukin-6 (IL-6) and tumour necrosis factor-α (TNFα) release39. Additionally, TNFα dampened the insulin signal via serine phosphorylation of insulin receptor substrate 1 in adipocytes112 whereas loss-of-function mutations in TNFα and TNFα receptors prevented HFD-induced insulin resistance113. Similarly, TLR4 gene mutation protected against HFD-induced obesity and promoted insulin signalling105. Insulin resistance due to inflammation is one key mediator of HFD-induced alterations to dopamine.
Inflammatory cytokines decrease dopamine packaging and signal transduction via reduced function and expression of vesicular monoamine transporter 2 and D2R but increase function or expression of DAT, which alters dopamine reuptake114. Additionally, inflammatory cytokines and reactive oxygen species reduced availability of the cofactor tetrahydrobiopterin required by TH for dopamine synthesis115. Further, systemic administration of proinflammatory cytokines IL-6 and IL-2 decreased NAc extracellular dopamine, though IL-1β had no effects116. Inflammatory processes may lower synaptic dopamine and alter feeding behaviours. Indeed, TLR4 knockout (KO) mice exhibited reduced preference for fat and sugar and attenuated WD-induced food intake, weight gain and palatable food preference117. Additionally, saturated HFD but not monounsaturated fat increased anxiety and depressive behaviour in conjunction with increased plasma cytokines and NAc cytokine and NF-κB transcriptional activity associated with heightened expression of microglial and astrocytic markers118. Further, intake of a free-choice cafeteria diet altered morphology of NAc MSNs and increased proinflammatory cytokine expression related to microglial activation, whereas microglial inhibition restored these effects and prevented diet-induced intake and weight gain119. Together, saturated fat and obesity may promote inflammation and insulin resistance that decrease dopamine synthesis, vesicular packaging, and capacity for dopamine release and reuptake. However, we posit that HFD-induced neuroinflammation uniquely promotes insulin resistance within the NAc as a primary driver of reduced reward value that promotes overconsumption of palatable foods, but a major gap involves lack of pharmacological investigation assessing interactions between insulin, LPS, inflammatory cytokines and microglial activation on behaviour and presynaptic dopamine neurotransmission in the NAc after chronic HFD intake during obesity.
Neuroinflammation interacts with stress to modulate dopamine and food intake
Stress encompasses a variety of homeostatic disruptions which may be acute or chronic and physiological or psychological in nature. Food intake and body weight can change in response to stress depending on the type, intensity and duration of the stressor and activation of specific stress circuits. As discussed above, the physiological stress of diet-induced inflammation alters dopamine signalling in the NAc. Likewise, psychological stress related to substance use disorders120 and diet-induced118,121 anxiety have been linked to disruptions in dopamine homeostasis. This next section highlights how acute or chronic stress responses alter food intake, discussing the impacts of dietary fat and induction of inflammation on these processes.
Acute stress: role of HPA, CRF and inflammation on food intake
Acute stress encompasses a huge variety of physiological and psychological triggers that activate the hypothalamic–pituitary–adrenal (HPA) stress axis in a coordinated effort with metabolic, immune, autonomic nervous, and digestive systems to increase breathing and heart rate but slow digestion in preparation for ‘fight or flight’ response122,123. Various stressors induce the hypothalamic paraventricular nucleus (PVN) to release corticotrophin-releasing factor (CRF), stimulating the pituitary gland to release adrenocorticotropin (ACTH) that targets adrenal glands to release glucocorticoids (corticosterone in rodents) and promote stress responses124. The hypothalamus also activates sympathetic neurons in response to stress that induce adrenal release of epinephrine and NPY to mobilise nutrients via glycogenolysis and gluconeogenesis124. In this context, CRF acutely produces anorexia and weight loss that may last several days124. Indeed, either a single exposure to LPS or acute immobilisation stress reduced food intake and body weight that persisted for over a week125. Human studies support this construct, as the most stressful event of each day increased the likelihood of eating less126, which was mediated by delayed digestive processes induced by acute stress127. Acute stress in healthy adults lacking comorbidities and stressors related to obesity appear to slow digestion and reduce food intake. However, induction of inflammation during saturated HFD consumption could interact with classical stress systems to promote effects of stress on reward pathways. For example, intraperitoneal LPS injection increased plasma ACTH and corticosterone and hypothalamic/pituitary proinflammatory cytokines in CRF KO and wild type mice128. Reciprocally, CRF promoted cortical microglial proliferation and dose-dependently increased TNFα release mediated by phosphorylation of MAPK intracellular signalling proteins shared by TLR4 activation129. Therefore, HPA axis and proinflammatory molecules engage in intracellular crosstalk and can independently promote stress. Acutely, stress mobilises nutrients and dampens food intake, but these behavioural effects might be altered during up-regulated inflammatory signalling. Overall, effects of HFD intake on the interactions between inflammatory and stress systems in the NAc have not been tested to determine effects on dopamine or behaviour during obesity or diet-related stressors (Fig. 2).
Fig. 2.
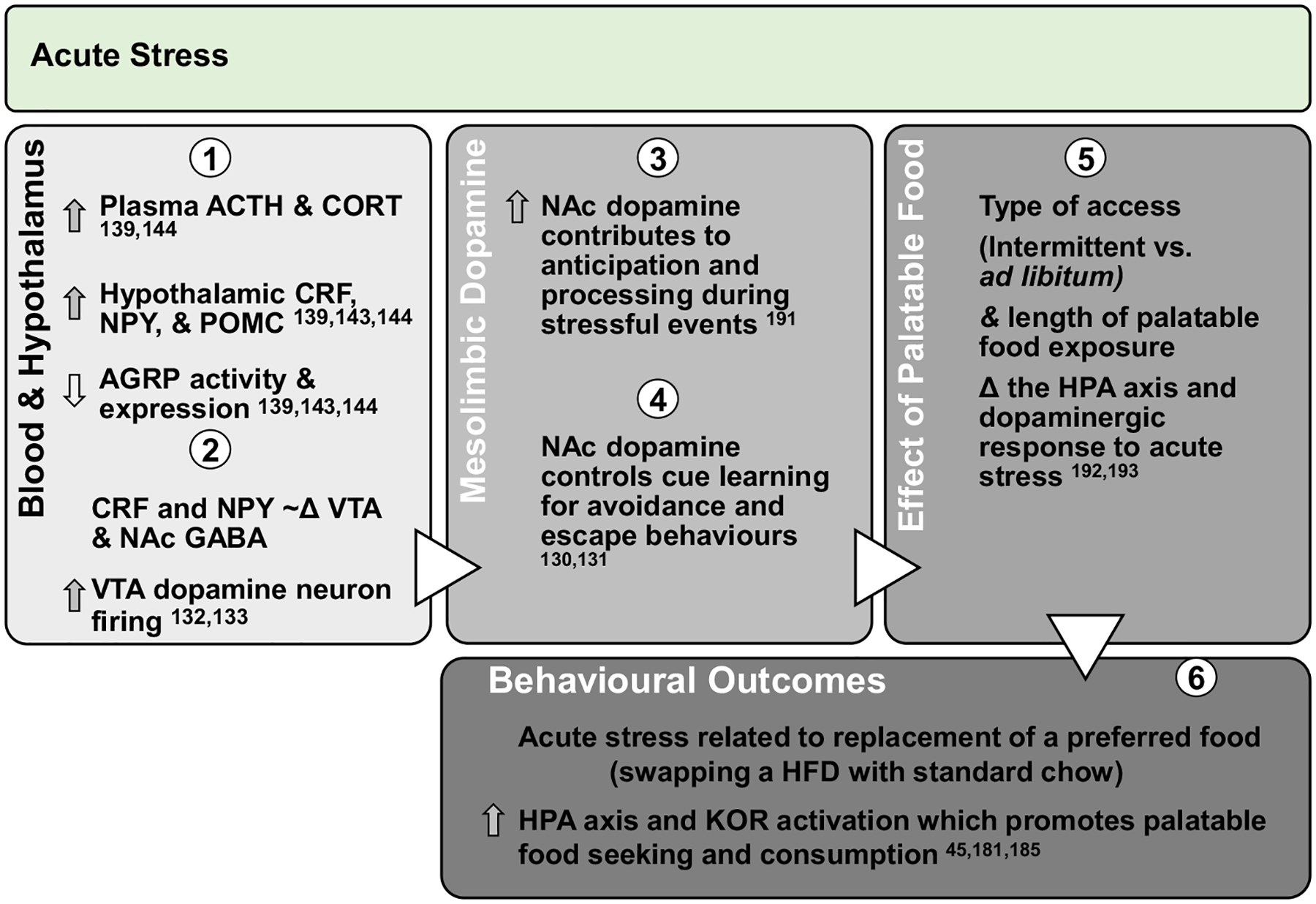
Effect of acute stress on dopamine neurotransmission and palatable food intake: acute exposures to stress engage the PVN and promote sympathetic and HPA axis activation leading to direct engagement of dopamine pathways. Downstream, glucocorticoid response and promotion of anorectic versus orexigenic neuropeptides inhibit food intake. However, acute stress associated with short-term removal of HFD activates stress systems that may persist for extended periods to promote seeking and intake of palatable foods. Further, activation of stress systems may reduce chow intake but promote consumption of palatable foods that acutely activate NAc dopamine neurotransmission and provide an alternate ‘avoidance or escape’ behaviour.
ACTH, adrenocorticotropin; CORT, corticosterone/cortisol; CRF, corticotrophin-releasing factor; NPY, neuropeptide Y; POMC, pro-opiomelanocortin; AGRP, agouti-related peptide; HPA, hypothalamic–pituitary–adrenal; KOR, κ-opioid receptor; Δ, change.
The immediate effects of acute stress are contextual and influenced by environmental factors. Interestingly, NAc dopamine release was increased during cues predicting foot shock, decreased during foot shock, then stimulated after lever pressing to stop the shock130,131. This shows NAc dopamine neurotransmission is involved in learning behaviours to avoid negative stimuli. Stress may directly induce dopamine activity, as CRF dose-dependently increased VTA dopamine neuron firing which was abolished by antagonising CRF receptor 1132, and CRF may activate both VTA GABA and dopamine neurons133. However, pharmacological activation of the HPA axis increased progressive ratio response in HFD but not chow-fed groups, which was reversed by antagonising CRF receptor 1134. Importantly, acute stress does not occur in isolation, and up-regulation of inflammatory signalling by HFD consumption could alter effects of acute stress. For example, LPS application 24 h after acute, inescapable tail shock promoted hippocampal NF-κB, TNFα, IL-6 and IL-1β gene expression, corticosterone, and microglial NF-κB and IL-1β responsiveness that was fully attenuated when TLR2, TLR4135 and glucocorticoid receptors136 were blocked during stress, and this stress-induced priming of neuroinflammation was mediated by transition of microglia, but not astrocytes, from a quiescent to an active state137. There are also sex effects within stress-induced priming of inflammatory microglial activation. The same stress paradigm similarly primed central proinflammatory cytokines, reduced anti-inflammatory pathways, and acutely reduced sucrose intake in males and females138. However, LPS 24 h after tail shock or glucocorticoid injection induced peripheral proinflammatory cytokines and reduced central glucocorticoid receptors in females but induced microglial IL-6 and IL-1β mRNA expression specifically in males138. Overall, specific effects of acute stress on food intake depend on prior exposure to a stressor and complex peripheral and central inflammatory signalling, suggesting those with chronic, diet-induced elevated proinflammatory states might be primed to be more reactive and have alternate behavioural responses to chronic stress, though further study is required explore this interaction in dopaminergic centres that influence food intake, like the NAc.
Chronic stress and food intake
Chronic, repeated stressors may affect food intake and body weight differently than acute stress, particularly in an obesogenic state which may promote socio-behavioural and physiological stressors. Effects of stress on hypothalamic nuclei may override homeostatic feeding. For example, inescapable foot shock engaged the HPA axis in addition to increased NPY but decreased AGRP expression, and α-melanocyte stimulating hormone released by ARC POMC/CART neurons increased stress-induced HPA activation139. Furthermore, associating a place or flavour with NPY/AGRP neuron activation reduced preference for that place or food140, and AGRP neuron activity was reduced due to food cues140 and initiation of feeding141. Therefore, negative valence associated with firing of AGRP neurons may provide motivation to perform behaviours that induce positive valence like eating2 which could provide a stress alleviating effect. This is important given obesity-prone rats fed HFD for 6 weeks had greater HPA axis activity with greater central CRF concentrations and plasma corticosterone than chow counterparts142. Therefore, the transition in stress response that occurs over repeated stress exposures could be exacerbated by diet-induced obesity and greater stress reactivity. Acute restraint decreased ARC AGRP expression143 but increased hypothalamic POMC expression in conjunction with reduced food intake144. Conversely, chronic restraint increased LH AGRP and decreased ARC melanocortin 4 receptor143 that responds to POMC. This showed unique activation of hypothalamic anorectic versus orexigenic signalling, respectively, in response to acute versus chronic stress. Diet-induced inflammation may mediate these effects, as acute lipid infusion or palmitate exposure in AGRP/NPY neurons increased TNFα, proinflammatory cytokines and NPY expression145. Conversely, 8-week HFD consumption reduced TNFα and AGRP expression while 20-week consumption promoted TNFα in NPY and AGRP neurons145. This suggests palatable foods acutely induce hypothalamic inflammation in regions that innervate the NAc followed by up-regulation of protective mechanisms which are eventually overcome with extended HFD intake, and dietary responses to chronic stress likely depend on inflammatory status related to food composition and availability associated with responsivity of NPY/AGRP and POMC/CART neurons and NAc dopamine cue learning.
Extended glucocorticoid responses may shift stress reactivity and impact hormonal regulation of energy stores. Glucocorticoids act to mobilise nutrients via gluconeogenesis146 and adipose tissue lipolysis147 during stress. However, these effects over an extended period could lead to hyperinsulinemia147,148, hyperleptinemia149, and insulin148,150 and leptin resistance. Indeed, 7 d of artificial glucocorticoid administration in healthy women increased food intake, plasma insulin and plasma leptin151, while exercise decreased cortisol response to stress (i.e. cortisol reactivity) accompanied by reduced disordered eating152. Maniam and Morris153 proposed glucocorticoid-induced stimulation of the dopamine system provides motivation to resolve stressful situations which may be ‘hijacked’ into motivation to obtain palatable foods. For example, in samples of women, presence of obesity increased cortisol reactivity154 which was associated with increased calorie consumption155. Downstream, glucocorticoids promote feeding by negatively regulating CRF and activating orexigenic NPY neurons149,153 that are inhibited by insulin and leptin and interconnected with the LH, NAc and VTA2. Therefore, during diet-induced obesity, chronic stress promotes glucocorticoid-induced activation of feeding centres and removes the stop signal from hypothalamus to VTA to promote dopamine-motivated feeding. It is important to note that glucocorticoids are involved in normal feeding responses, as restoring corticosterone to adrenalectomised rats increased saccharin156 and sucrose157 intake to control levels. On the other hand, access to lard blunted corticosterone response during restraint stress158. Therefore, diet interacts with glucocorticoids to modulate stress-induced feeding. Indeed, mice exposed to chronic social stress after 12 weeks on a HFD showed improved weight loss, reduced plasma insulin and leptin, and dampened anxio-depressive behaviours versus stressed controls or non-stressed HFD groups159, suggesting a potentially stress-alleviating effect of palatable food intake. Overall, diet-induced obesity produces neurochemical shifts and maladaptive stress responses, but an opportunity for future investigation lies in whether HPA axis and κ-opioid receptor stress responses drive food intake for obese individuals during the chronic diet-related stress of restricting calories for weight loss (Fig. 3).
Fig. 3.
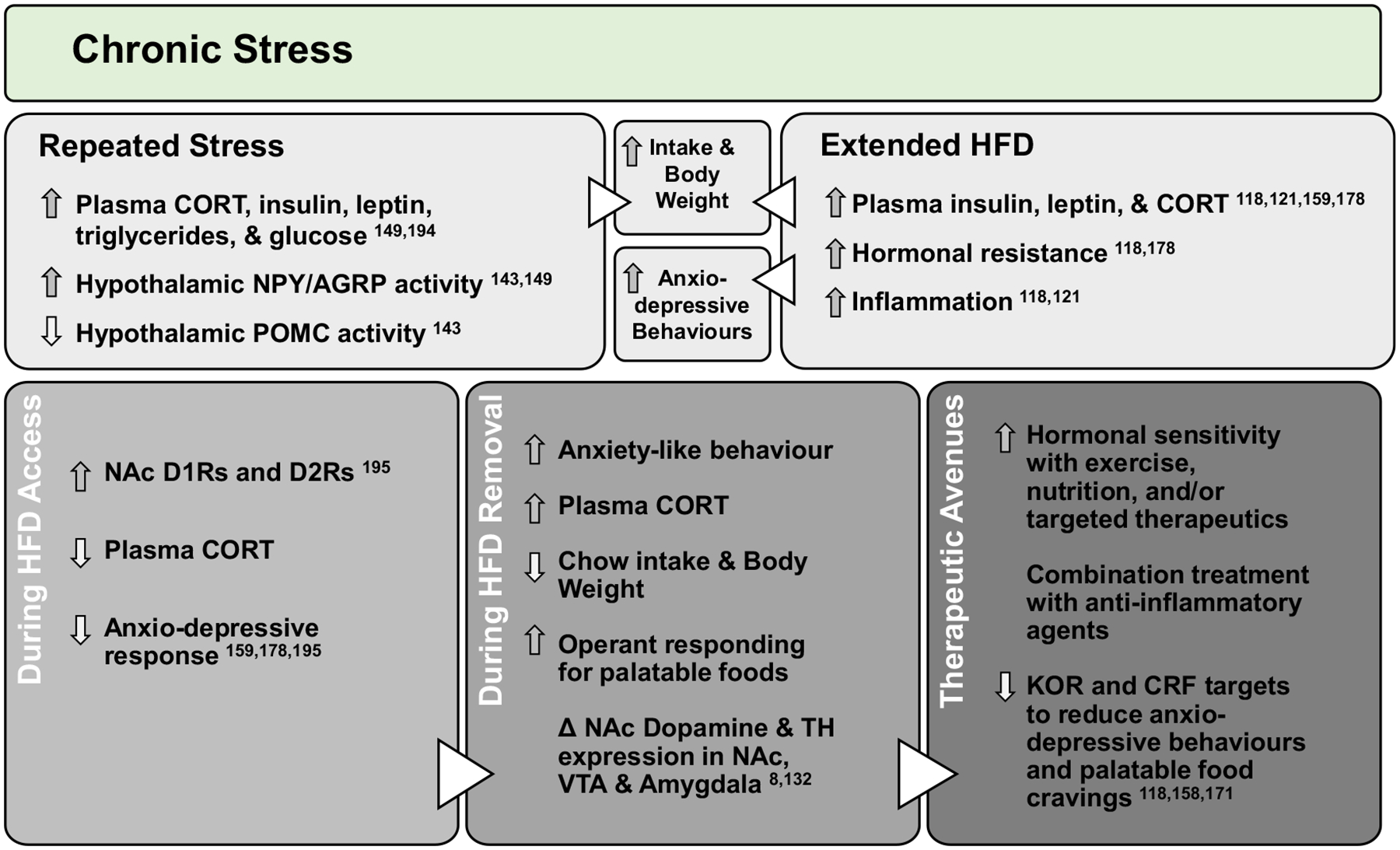
Chronic stress alters dopamine and promotes consumption of palatable food: repeated stress exposures, including long-term physiological stresses related to diet-induced obesity, chronically up-regulate stress pathways to promote orexigenic neuropeptides, inflammation and hormonal resistance. This leads to dysregulation of dopamine and increased food intake, weight gain and anxio-depressive behaviours. However, consumption of palatable foods during stress activates the dopamine system and reduces metabolic and behavioural responsivity to stress, highlighting stress alleviative properties of palatable foods. Behavioural and pharmacological interventions which improve diet-induced alterations to inflammatory, hormonal, stress and dopamine systems may reduce craving, seeking and consumption of highly palatable foods for obese individuals attempting to lose weight.
CORT, corticosterone/cortisol; NPY, neuropeptide Y; AGRP, agouti-related peptide; POMC, pro-opiomelanocortin; D1R/D2R, dopamine type 1 or type 2 receptor; TH, tyrosine hydroxylase; KOR, κ-opioid receptor; CRF, corticotrophin-releasing factor; Δ, change.
Effects of a HFD on κ-opioid-receptor-mediated stress, dopamine, and food intake
The HPA axis interacts with κ-opioid receptors (KORs) to gate NAc dopamine signalling. Indeed, expression of CRF, ACTH and glucocorticoids systemically and centrally are co-regulated with dynorphin, a ligand for KORs, and its precursor prodynorphin with ligands in either system inducing expression and release reciprocally to promote stress responses160–163. KORs are G-protein-coupled receptors that inhibit adenylyl cyclase and cAMP activity164,165 and are co-expressed within NAc DAT-expressing neurons166. Blocking NAc KORs inhibited dopamine reuptake and increased extracellular dopamine167, while KOR activation increased reuptake to limit extracellular dopamine168,169. KORs are present within NAc presynaptic dopamine terminals, MSNs, and GABAergic and cholinergic interneurons and reduce extracellular dopamine to promote feeding cessation170. However, ventricular KOR agonism promoted HFD intake during satiation, whereas KOR antagonism in a fasted state reduced HFD intake171, and systemic KOR agonism reduced NAc core phasic dopamine release parallel to reduced motivation to obtain sucrose172. This suggests KORs control extracellular dopamine to alter rewarding effects of food. In the NAc, KOR activation during nicotine exposure173 and amphetamine withdrawal174 decreased basal and evoked dopamine, while KOR antagonism attenuated alcohol self-administration during withdrawal175. Furthermore, acute stress promoted TNFα in the amygdala, and amygdalar TNFα potentiated anxiety during withdrawal that was blocked by CRF antagonism176. Therefore, HPA axis, KOR and inflammatory systems interact to induce dysphoria and relapse during withdrawal, and up-regulation of these symptoms during diet-induced obesity could promote food cravings when energy is restricted for weight loss.
Neuroinflammation interacts with stress and reward systems. Indeed, exposing women to stress induced plasma IL-6 concentrations that correlated with reduced NAc activation during an fMRI reward learning task177. Further, chronic intake of saturated HFD versus low fat118,121,178 or monounsaturated fat118 increased anxio-depressive behaviours, plasma corticosterone, and hypothalamic and NAc inflammatory cytokine and TLR4 expression. Conversely, prodynorphin overexpression promoted anti-inflammatory M2 versus M1 phenotype of hippocampal microglia and inhibited LPS-induced TLR4 activation of NF-κB to promote IL-4 and IL-10 but inhibit IL-1β and IL-6 release179. Reciprocally, intraplantar injection of IL-1β increased KOR mRNA expression in basal root ganglia neurons180. However, dynorphin, enkephalin and KOR expression in the NAc were not affected by WD intake or 18-d replacement with chow181 or 18 d of ad libitum or intermittent access to a HFD182. Therefore, while HFD intake itself does not appear to alter dynorphin/KOR expression, it appears that KORs dampen proinflammatory responses induced by saturated fat and could engage in intracellular crosstalk with inflammatory molecules similarly to the HPA axis. Human neuroimaging studies linked a dopaminergic response to the consumption of palatable food183, palatable food cues29 or smelling food odours184 with increased reports of pleasure183,184 and wanting29 of food. Therefore, changing a lifetime of food preferences by restricting energy intake to lose weight may be particularly stressful and activate stress pathways that dampen dopamine signalling.
In support of KOR system involvement during palatable food restriction, pair feeding of WD to chow intake levels in controls reduced NAc KOR expression in absence of obesity, but 18 d of WD replacement with chow did not alter KOR expression181. Therefore, it is possible that differences in KOR expression become neutralised over 18 d of diet replacement or by diet-induced weight gain, or that specifically KOR function could be up-regulated. HFD intake alters food preferences, as replacement of a WD45 or HFD8 with chow persistently reduced food intake and acutely increased plasma corticosterone and anxiety-like behaviour8. Further, whereas HFD intake promoted sucrose anhedonia8,48,185, palatable food removal increased preference for sucrose48,185 and motivation to obtain sucrose8,45 and fat8 that occurred as soon 3 d8 after diet removal but persisted for several weeks45,48,185. This indicates prolonged enhancement of salience for palatable food when a preferred diet is not available, and it is possible that KORs, which contribute to the rewarding properties of food, promote this effect. Further, HFD intake started at parturition reduced VTA TH and NAc D1R and D2R expression in male and female mice, but 4 weeks of HFD replacement exacerbated this reduction in the VTA of females and NAc of males but oppositely restored these effects in the VTA of males and NAc of females48. However, when HFD is introduced in adolescence, HFD replacement does not recover D2R expression in females with strong promotion of palatable food intake, though effects were attenuated during adult-onset HFD185. This suggests prolonged effects of a HFD on dopamine synthesis and signalling in the VTA alter the capacity for neurotransmission in the NAc. Changes in NAc neurotransmission occur via alterations to D1Rs and D2Rs resulting in increased salience of palatable foods when they are no longer available. These effects were significantly mediated by sex and age of palatable food introduction with high vulnerability during adolescence. Overall, individuals with clinical obesity or that persistently consume a HFD may be poorly adapted to control palatable food cravings during energy restriction owing to diet-induced or psychological stress that engages the HPA or KOR systems.
Conclusions
NAc dopamine neurotransmission is affected by physiological state and access to highly palatable foods that promote obesity, inflammation and hormonal resistance. Chronic engagement of the HPA axis and KOR stress systems by repeated exposures to daily life stressors interact with the inflammatory and hormonal systems disrupted during obesity. Ultimately, palatable food intake acutely increases dopamine release and reuptake, but extended HFD intake reduces the capacity for dopamine neurotransmission. These trends are related to the physiological consequences of obesity that together promote the vulnerability to overeat in order to promote synaptic dopamine to combat obesity-related dysphoria and reduction of dopamine tone. The effect of dietary fat on dopamine’s influence overfeeding could be exacerbated by stress due to dietary restriction or removal of preferred foods. However, pharmacologically targeting receptors that mediate stress in the brain, like KORs, or controlling diet-induced inflammation that engages in crosstalk with KOR system-mediated stress may improve the success of weight loss interventions by attenuating the impact of stress on the dopamine system. Moreover, the dampening of dopamine neurotransmission by long-term consumption of a HFD, specifically high in saturated fat, could be potentiated by inflammation acting on dopamine neurons, which could heighten stress responses that further attenuate dopamine signalling. The result could be an increase in palatable food seeking and consumption to curb potential negative affect with an acute but transient increase in dopaminergic signalling.
Acknowledgements
This publication was supported by the National Institute of Diabetes and Digestive.
Financial Support
Kidney Diseases of the National Institutes of Health under Award Number R15DK119897. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Hales CM, Carroll MD, Fryar CD & Ogden CL (2020) Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief 360. https://www.cdc.gov/nchs/products/databriefs/db360.htm [PubMed] [Google Scholar]
- 2.Ferrario CR, Labouèbe G, Liu S, et al. (2016) Homeostasis meets motivation in the battle to control food intake. J Neurosci 36, 11469–11481. doi: 10.1523/JNEUROSCI.2338-16.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matikainen-Ankney BA & Kravitz AV (2018) Persistent effects of obesity: a neuroplasticity hypothesis. Ann N Y Acad Sci 1428, 1–19. doi: 10.1111/nyas.13665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Day JJ & Carelli RM (2007) The nucleus accumbens and Pavlovian reward learning. Neuroscientist 13, 148–159. doi: 10.1177/1073858406295854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mccutcheon JE, Beeler JA & Roitman MF (2012) Sucrose-predictive cues evoke greater phasic dopamine release than saccharin-predictive cues. Synapse 66, 346–351. doi: 10.1002/syn.21519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liang N-C, Hajnal A & Norgren R (2006) Sham feeding corn oil increases accumbens dopamine in the rat. Am J Physiol Integr Comp Physiol 291, R1236–R1239. doi: 10.1152/ajpregu.00226.2006 [DOI] [PubMed] [Google Scholar]
- 7.Lee Y, Kroemer NB, Oehme L, Beuthien-Baumann B, Goschke T & Smolka MN (2018) Lower dopamine tone in the striatum is associated with higher body mass index. Eur Neuropsychopharmacol 28, 719–731. doi: 10.1016/j.euroneuro.2018.03.009 [DOI] [PubMed] [Google Scholar]
- 8.Sharma S, Fernandes MF & Fulton S (2013) Adaptations in brain reward circuitry underlie palatable food cravings and anxiety induced by high-fat diet withdrawal. Int J Obes 37, 1183–1191. doi: 10.1038/ijo.2012.197 [DOI] [PubMed] [Google Scholar]
- 9.Sharma S & Fulton S (2013) Diet-induced obesity promotes depressive-like behaviour that is associated with neural adaptations in brain reward circuitry. Int J Obes 37, 382–389. doi: 10.1038/ijo.2012.48 [DOI] [PubMed] [Google Scholar]
- 10.Li Y, South T, Han M, Chen J, Wang R & Huang XF (2009) High-fat diet decreases tyrosine hydroxylase mRNA expression irrespective of obesity susceptibility in mice. Brain Res 1268, 181–189. doi: 10.1016/j.brainres.2009.02.075 [DOI] [PubMed] [Google Scholar]
- 11.Geiger BM, Haburcak M, Avena NM, Moyer MC, Hoebel BG & Pothos EN (2009) Deficits of mesolimbic dopamine neurotransmission in rat dietary obesity. Neuroscience 159, 1193–1199. doi: 10.1016/j.neuroscience.2009.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mikhailova MA, Bass CE, Grinevich VP, et al. (2016) Optogenetically-induced tonic dopamine release from VTA-nucleus accumbens projections inhibits reward consummatory behaviors. Neuroscience 333, 54–64. doi: 10.1016/j.neuroscience.2016.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avena NM, Rada P, Moise N & Hoebel BG (2006) Sucrose sham feeding on a binge schedule releases accumbens dopamine repeatedly and eliminates the acetylcholine satiety response. Neuroscience 139, 813–820. doi: 10.1016/j.neuroscience.2005.12.037 [DOI] [PubMed] [Google Scholar]
- 14.Rada P, Avena NM & Hoebel BG (2005) Daily bingeing on sugar repeatedly releases dopamine in the accumbens shell. Neuroscience 134, 737–744. doi: 10.1016/j.neuroscience.2005.04.043 [DOI] [PubMed] [Google Scholar]
- 15.Baik J-H (2013) Dopamine signaling in food addiction: role of dopamine D2 receptors. BMB Rep 46, 519–526. doi: 10.5483/BMBRep.2013.46.11.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kemp JM & Powell T (1971) The structure of the caudate nucleus of the cat: light and electron microscopy. Philos Trans R Soc Lond B Biol Sci 262, 383–401. [DOI] [PubMed] [Google Scholar]
- 17.Burke DA, Rotstein HG & Alvarez VA (2017) Striatal local circuitry: a new framework for lateral inhibition. Neuron 96, 267–284. doi: 10.1016/j.neuron.2017.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jais A & Bruning JC (2017) Hypothalamic inflammation in obesity and metabolic disease. J Clin Invest 127, 24–32. doi: 10.1172/JCI88878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Connor EC, Kremer Y, Lefort S, et al. (2015) Accumbal D1R neurons projecting to lateral hypothalamus authorize feeding. Neuron 88, 553–564. doi: 10.1016/j.neuron.2015.09.038 [DOI] [PubMed] [Google Scholar]
- 20.Steiner H & Tseng KY, eds (2016) Handbook of Basal Ganglia Structure and Function. Second. Cambridge, MA: Academic Press, 2016. [Google Scholar]
- 21.Beaulieu J-M & Gainetdinov RR (2011) The physiology, signaling, and pharmacology of dopamine receptors. Pharmacol Rev 63, 182–217. doi: 10.1124/pr.110.002642 [DOI] [PubMed] [Google Scholar]
- 22.Richfield EK, Penney JB & Young AB (1989) Anatomical and affinity state comparisons between dopamine D1 and D2 receptors in the rat central nervous system. Neuroscience 30, 767–777. doi: 10.1016/0306-4522(89)90168-1 [DOI] [PubMed] [Google Scholar]
- 23.Surmeier DJ, Ding J, Day M, Wang Z & Shen W (2007) D1 and D2 dopamine-receptor modulation of striatal glutamatergic signaling in striatal medium spiny neurons. Trends Neurosci 30, 228–235. doi: 10.1016/j.tins.2007.03.008 [DOI] [PubMed] [Google Scholar]
- 24.Gantz SC, Ford CP, Morikawa H & Williams JT (2018) The evolving understanding of dopamine neurons in the substantia nigra and ventral tegmental area. Annu Rev Physiol 80, 219–241. doi: 10.1146/annurev-physiol-021317-121615 [DOI] [PubMed] [Google Scholar]
- 25.Volkow ND & Morales M (2015) The brain on drugs: from reward to addiction. Cell 162, 712–725. doi: 10.1016/j.cell.2015.07.046 [DOI] [PubMed] [Google Scholar]
- 26.Bailey MR, Simpson EH & Balsam PD (2016) Neural substrates underlying effort, time, and risk-based decision making in motivated behavior. Neurobiol Learn Mem 133, 233–256. doi: 10.1016/j.nlm.2016.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCullough LD & Salamone JD (1992) Involvement of nucleus accumbens dopamine in the motor activity induced by periodic food presentation: a microdialysis and behavioral study. Brain Res 592, 29–36. doi: 10.1016/0006-8993(92)91654-W [DOI] [PubMed] [Google Scholar]
- 28.Aberman J & Salamone J (1999) Nucleus accumbens dopamine depletions make rats more sensitive to high ratio requirements but do not impair primary food reinforcement. Neuroscience 92, 545–552. doi: 10.1016/S0306-4522(99)00004-4 [DOI] [PubMed] [Google Scholar]
- 29.Eisenstein SA, Black KJ, Samara A, et al. (2020) Striatal dopamine responses to feeding are altered in people with obesity. Obesity 28, 765–771. doi: 10.1002/oby.22753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Small DM, Jones-Gotman M & Dagher A (2003) Feeding-induced dopamine release in dorsal striatum correlates with meal pleasantness ratings in healthy human volunteers. Neuroimage 19, 1709–1715. doi: 10.1016/S1053-8119(03)00253-2 [DOI] [PubMed] [Google Scholar]
- 31.Thanarajah SE, Backes H, DiFeliceantonio AG, et al. (2019) Food intake recruits orosensory and post-ingestive dopaminergic circuits to affect eating desire in humans. Cell Metab 29, 695–706.e4. doi: 10.1016/j.cmet.2018.12.006 [DOI] [PubMed] [Google Scholar]
- 32.Hryhorczuk C, Florea M, Rodaros D, et al. (2016) Dampened mesolimbic dopamine function and signaling by saturated but not monounsaturated dietary lipids. Neuropsychopharmacology 41, 811–821. doi: 10.1038/npp.2015.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cone JJ, Chartoff EH, Potter DN, Ebner SR & Roitman MF (2013) Prolonged high fat diet reduces dopamine reuptake without altering DAT gene expression. PLoS One 8, e58251. doi: 10.1371/journal.pone.0058251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fordahl SC & Jones SR (2017) High-fat-diet-induced deficits in dopamine terminal function are reversed by restoring insulin signaling. ACS Chem Neurosci 8, 290–299. doi: 10.1021/acschemneuro.6b00308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.South T & Huang XF (2008) High-fat diet exposure increases dopamine D2 receptor and decreases dopamine transporter receptor binding density in the nucleus accumbens and caudate putamen of mice. Neurochem Res 33, 598–605. doi: 10.1007/s11064-007-9483-x [DOI] [PubMed] [Google Scholar]
- 36.Huang XF, Zavitsanou K, Huang X, et al. (2006) Dopamine transporter and D2 receptor binding densities in mice prone or resistant to chronic high fat diet-induced obesity. Behav Brain Res 175, 415–419. doi: 10.1016/j.bbr.2006.08.034 [DOI] [PubMed] [Google Scholar]
- 37.Huang XF, Yu Y, Zavitsanou K, Han M & Storlien L (2005) Differential expression of dopamine D2 and D4 receptor and tyrosine hydroxylase mRNA in mice prone, or resistant, to chronic high-fat diet-induced obesity. Mol Brain Res 135, 150–161. doi: 10.1016/j.molbrainres.2004.12.013 [DOI] [PubMed] [Google Scholar]
- 38.Wang Z, Liu D, Wang F, et al. (2012) Saturated fatty acids activate microglia via Toll-like receptor 4/NF-κB signalling. Br J Nutr 107, 229–241. doi: 10.1017/S0007114511002868 [DOI] [PubMed] [Google Scholar]
- 39.Wang Y, Qian Y, Fang Q, et al. (2017) Saturated palmitic acid induces myocardial inflammatory injuries through direct binding to TLR4 accessory protein MD2. Nat Commun 8, 1–14. doi: 10.1038/ncomms13997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stouffer MA, Woods CA, Patel JC, et al. (2015) Insulin enhances striatal dopamine release by activating cholinergic interneurons and thereby signals reward. Nat Commun, 6, 1–12. doi: 10.1038/ncomms9543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matheny M, Shapiro A, Tümer N & Scarpace PJ (2011) Region-specific diet-induced and leptin-induced cellular leptin resistance includes the ventral tegmental area in rats. Neuropharmacology 60, 480–487. doi: 10.1016/j.neuropharm.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Enriori PJ, Evans AE, Sinnayah P, et al. (2007) Diet-induced obesity causes severe but reversible leptin resistance in arcuate melanocortin neurons. Cell Metab 5, 181–194. doi: 10.1016/j.cmet.2007.02.004 [DOI] [PubMed] [Google Scholar]
- 43.Patel JC, Stouffer MA, Mancini M, Nicholson C, Carr KD & Rice ME (2019) Interactions between insulin and diet on striatal dopamine uptake kinetics in rodent brain slices. Eur J Neurosci 49, 794–804. doi: 10.1111/ejn.13958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bruijnzeel AW (2009) kappa-Opioid receptor signaling and brain reward function. Brain Res Rev 62, 127–146. doi: 10.1016/j.brainresrev.2009.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pickering C, Alsiö J, Hulting AL & Schiöth HB (2009) Withdrawal from free-choice high-fat high-sugar diet induces craving only in obesity-prone animals. Psychopharmacol (Berl) 204, 431–443. doi: 10.1007/s00213-009-1474-y [DOI] [PubMed] [Google Scholar]
- 46.Rada P, Avena NM, Barson JR, Hoebel BG & Leibowitz SF (2012) A high-fat meal, or intraperitoneal administration of a fat emulsion, increases extracellular dopamine in the nucleus accumbens. Brain Sci 2, 242–253. doi: 10.3390/brainsci2020242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hajnal A, Smith GP & Norgren R (2004) Oral sucrose stimulation increases accumbens dopamine in the rat. Am J Physiol Integr Comp Physiol 286, R31–R37. doi: 10.1152/ajpregu.00282.2003 [DOI] [PubMed] [Google Scholar]
- 48.Carlin J, Hill-Smith TE, Lucki I & Reyes TM (2013) Reversal of dopamine system dysfunction in response to high-fat diet. Obesity 21, 2513–2521. doi: 10.1002/oby.20374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Epstein LH, Jaroni JL, Paluch RA, et al. (2002) Dopamine transporter genotype as a risk factor for obesity in African-American smokers. Obes Res 10, 1232–1240. doi: 10.1038/oby.2002.168 [DOI] [PubMed] [Google Scholar]
- 50.Jones KT, Woods C, Zhen J, Antonio T, Carr KD & Reith MEA (2017) Effects of diet and insulin on dopamine transporter activity and expression in rat caudate-putamen, nucleus accumbens, and midbrain. J Neurochem 140, 728–740. doi: 10.1111/jnc.13930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barnes CN, Wallace CW, Jacobowitz BS & Fordahl SC (2020) Reduced phasic dopamine release and slowed dopamine uptake occur in the nucleus accumbens after a diet high in saturated but not unsaturated fat. Nutr Neurosci 1–13. doi: 10.1080/1028415X.2019.1707421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Baik J-H (2013) Dopamine Signaling in reward-related behaviors. Front Neural Circuits 7, 1–16. doi: 10.3389/fncir.2013.00152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Durst M, Könczöl K, Balázsa T, Eyre MD & Tóth ZE (2019) Reward-representing D1-type neurons in the medial shell of the accumbens nucleus regulate palatable food intake. Int J Obes 43, 917–927. doi: 10.1038/s41366-018-0133-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thoeni S, Loureiro M, O’Connor E & Luscher C (2020) Depression of accumbal to lateral hypothalamic synapses gates overeating. Neuron 107, 1–15. doi: 10.1016/j.neuron.2020.03.029 [DOI] [PubMed] [Google Scholar]
- 55.Barlow RL, Gorges M, Wearn A, et al. (2018) Ventral striatal D 2/3 receptor availability is associated with impulsive choice behavior as well as limbic corticostriatal connectivity. Int J Neuropsychopharmacol 21, 705–715. doi: 10.1093/ijnp/pyy030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Adams WK, Sussman JL, Kaur S, D’souza AM, Kieffer TJ & Winstanley CA. Long-term, calorie-restricted intake of a high-fat diet in rats reduces impulse control and ventral striatal D2 receptor signalling – two markers of addiction vulnerability. Eur J Neurosci 42, 3095–3104. doi: 10.1111/ejn.13117 [DOI] [PubMed] [Google Scholar]
- 57.Thanos P, Michaelides M, Piyis Y, Wang G & Volkow N. Food restriction markedly increases dopamine D2 receptor (D2R) in a rat model of obesity as assessed with in-vivo muPET imaging ([11C] raclopride) and in-vitro ([3H] spiperone) autoradiography. Synapse 62, 50–61. doi: 10.1002/syn.20468 [DOI] [PubMed] [Google Scholar]
- 58.Cook JB, Hendrickson LM, Garwood GM, Toungate KM, Nania CV. & Morikawa H. Junk food diet-induced obesity increases D2 receptor autoinhibition in the ventral tegmental area and reduces ethanol drinking. PLoS One 12, 1–17. doi: 10.1371/journal.pone.0183685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dang LC, Samanez-Larkin GR, Castrellon JJ, Perkins SF, Cowan RL & Zald DH. Associations between dopamine D2 receptor availability and BMI depend on age. Neuroimage 138, 176–183. doi: 10.1016/j.neuroimage.2016.05.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sulzer D, Cragg SJ & Rice ME. Striatal dopamine neurotransmission: regulation of release and uptake. Basal Ganglia 6, 123–148. doi: 10.1016/j.baga.2016.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kosillo P, Zhang Y-F, Threlfell S & Cragg SJ. Cortical control of striatal dopamine transmission via striatal cholinergic interneurons. Cereb Cortex 26, 4160–4169. doi: 10.1093/cercor/bhw252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang H & Sulzer D. Glutamate spillover in the striatum depresses dopaminergic transmission by activating Group I metabotropic glutamate receptors. J Neurosci 23, 10585–10592. doi: 10.1523/jneurosci.23-33-10585.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Avshalumov MV, Patel JC & Rice ME (2008) AMPA receptor-dependent H2O2 generation in striatal medium spiny neurons but not dopamine axons: one source of a retrograde signal that can inhibit dopamine release. J Neurophysiol 100, 1590–1601. doi: 10.1152/jn.90548.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Echo JA, Lamonte N, Christian G, Znamensky V, Ackerman TF & Bodnar RJ (2001) Excitatory amino acid receptor subtype agonists induce feeding in the nucleus accumbens shell in rats: opioid antagonist actions and interactions with μ-opioid agonists. Brain Res 921, 86–97. doi: 10.1016/S0006-8993(01)03094-3 [DOI] [PubMed] [Google Scholar]
- 65.Maldonado-Irizarry CS, Swanson CJ & Kelley AE (1995) Glutamate receptors in the nucleus accumbens shell control feeding behavior via the lateral hypothalamus. J Neurosci 15, 6779–6788. doi: 10.1523/jneurosci.15-10-06779.1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fritz BM, Muñoz B, Yin F, Bauchle C & Atwood BK (2008) A high-fat, high-sugar ‘Western’ diet alters dorsal striatal glutamate, opioid, and dopamine transmission in mice. Neuroscience 372, 1–15. doi: 10.1016/j.neuroscience.2017.12.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brown RM, Kupchik YM, Spencer S, et al. (2017) Addiction-like synaptic impairments in diet-induced obesity. Biol Psychiatry 81, 797–806. doi: 10.1016/j.biopsych.2015.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Camacho A, Montalvo-Martinez L, Cardenas-Perez RE, Fuentes-Mera L & Garza-Ocañas L (2017) Obesogenic diet intake during pregnancy programs aberrant synaptic plasticity and addiction-like behavior to a palatable food in offspring. Behav Brain Res 330, 46–55. doi: 10.1016/j.bbr.2017.05.014 [DOI] [PubMed] [Google Scholar]
- 69.Brown MTC, Tan KR, O’Connor EC, Nikonenko I, Muller D & Lüscher C (2012) Ventral tegmental area GABA projections pause accumbal cholinergic interneurons to enhance associative learning. Nature 492, 452–456. doi: 10.1038/nature11657 [DOI] [PubMed] [Google Scholar]
- 70.Mallet N, Schmidt R, Leventhal D, et al. (2016) Arkypallidal cells send a stop signal to striatum. Neuron 89, 308–316. doi: 10.1016/j.neuron.2015.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee AT, Vogt D, Rubenstein JL & Sohal VS (2014) A class of GABA-ergic neurons in the prefrontal cortex sends long-range projections to the nucleus accumbens and elicits acute avoidance behavior. J Neurosci 34, 11519–11525. doi: 10.1523/JNEUROSCI.1157-14.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Smith JB, Klug JR, Ross DL, et al. (2016) Genetic-based dissection unveils the inputs and outputs of striatal patch and matrix compartments. Neuron 91, 1069–1084. doi: 10.1016/j.neuron.2016.07.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Smolders I, De Klippel N, Sarre S, Ebinger G & Michotte Y (1995) Tonic GABA-ergic modulation of striatal dopamine release studied by in vivo microdialysis in the freely moving rat. Eur J Pharmacol 284, 83–91. doi: 10.1016/0014-2999(95)00369-V [DOI] [PubMed] [Google Scholar]
- 74.Charara A, Heilman C, Levey AI & Smith Y (2000) Pre- and postsynaptic localization of GABA(B) receptors in the basal ganglia in monkeys. Neuroscience 95, 127–140. doi: 10.1016/S0306-4522(99)00409-1 [DOI] [PubMed] [Google Scholar]
- 75.Kandov Y, Israel Y, Kest A, et al. (2006) GABA receptor subtype antagonists in the nucleus accumbens shell and ventral tegmental area differentially alter feeding responses induced by deprivation, glucoprivation and lipoprivation in rats. Brain Res 1082, 86–97. doi: 10.1016/j.brainres.2006.01.112 [DOI] [PubMed] [Google Scholar]
- 76.Basso AM & Kelley AE (1999) Feeding induced by GABA(A) receptor stimulation within the nucleus accumbens shell: regional mapping and characterization of macronutrient and taste preference. Behav Neurosci 113, 324–336. doi: 10.1037/0735-7044.113.2.324 [DOI] [PubMed] [Google Scholar]
- 77.Stratford TR & Kelley AE (1997) GABA in the nucleus accumbens shell participates in the central regulation of feeding behavior. J Neurosci 17, 4434–4440. doi: 10.1523/jneurosci.17-11-04434.1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tsunekawa T, Banno R, Yaginuma H, et al. (2019) GABA(B) receptor signaling in the mesolimbic system suppresses binge-like consumption of a high-fat diet. iScience 20, 337–347. doi: 10.1016/j.isci.2019.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Butler MJ & Eckel LA (2018) Eating as a motivated behavior: modulatory effect of high fat diets on energy homeostasis, reward processing and neuroinflammation. Integr Zool 13, 673–686. doi: 10.1111/1749-4877.12340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Morales M & Margolis EB (2017) Ventral tegmental area: cellular heterogeneity, connectivity and behaviour. Nat Rev Neurosci 18, 73–85. doi: 10.1038/nrn.2016.165 [DOI] [PubMed] [Google Scholar]
- 81.Wickham R, Solecki W, Rathbun L, McIntosh JM & Addy NA (2013) Ventral tegmental area α6β2 nicotinic acetylcholine receptors modulate phasic dopamine release in the nucleus accumbens core. Psychopharmacology (Berl) 229, 73–82. doi: 10.1007/s00213-013-3082-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gumbs MCR, Vuuregge AH, Eggels L, et al. (2019) Afferent neuropeptide Y projections to the ventral tegmental area in normal-weight male Wistar rats. J Comp Neurol 527, 2659–2674. doi: 10.1002/cne.24698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Naneix F, Tantot F, Glangetas C, et al. (2017) Impact of early consumption of high-fat diet on the mesolimbic dopaminergic system. eNeuro 4, 1–12. doi: 10.1523/ENEURO.0120-17.2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Levitt M, Spector S, Sjoerdsma A & Udenfriend S (1964) Elucidation of the rate-limiting step in norepinephrine biosynthesis in the perfused guinea-pig heart. J Pharmacol Exp Ther 148, 1–8. [PubMed] [Google Scholar]
- 85.Koyama S, Mori M, Kanamaru S, et al. (2014) Obesity attenuates D2 autoreceptor-mediated inhibition of putative ventral tegmental area dopaminergic neurons. Physiol Rep 2, 1–11. doi: 10.14814/phy2.12004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Koyama S, Kawaharada M, Terai H, et al. (2013) Obesity decreases excitability of putative ventral tegmental area GABAergic neurons. Physiol Rep 1, 1–12. doi: 10.1002/phy2.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Figlewicz DP, Evans SB, Murphy J, Hoen M & Baskin DG (2003) Expression of receptors for insulin and leptin in the ventral tegmental area/substantia nigra (VTA/SN) of the rat. Brain Res 964, 107–115. doi: 10.1016/S0006-8993(02)04087-8 [DOI] [PubMed] [Google Scholar]
- 88.Fulton S, Pissios P, Manchon RP, et al. (2006) Leptin regulation of the mesoaccumbens dopamine pathway. Neuron 51, 811–822. doi: 10.1016/j.neuron.2006.09.006 [DOI] [PubMed] [Google Scholar]
- 89.Naef L, Seabrook L, Hsiao J, Li C & Borgland SL (2019) Insulin in the ventral tegmental area reduces cocaine-evoked dopamine in the nucleus accumbens in vivo. Eur J Neurosci 50, 2146–2155. doi: 10.1111/ejn.14291 [DOI] [PubMed] [Google Scholar]
- 90.Mebel DM, Wong JCY, Dong YJ & Borgland SL (2012) Insulin in the ventral tegmental area reduces hedonic feeding and suppresses dopamine concentration via increased reuptake. Eur J Neurosci 36, 2336–2346. doi: 10.1111/j.1460-9568.2012.08168.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Labouèbe G, Liu S, Dias C, et al. (2013) Insulin induces long-term depression of ventral tegmental area dopamine neurons via endocannabinoids. Nat Neurosci 16, 300–308. doi: 10.1038/nn.3321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Liu S, Labouèbe G, Karunakaran S, Clee SM & Borgland SL (2013) Effect of insulin on excitatory synaptic transmission onto dopamine neurons of the ventral tegmental area in a mouse model of hyperinsulinemia. Nutr Diabetes 3, e97. doi: 10.1038/nutd.2013.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bruijnzeel AW, Qi X & Corrie LW (2013) Anorexic effects of intra-VTA leptin are similar in low-fat and high-fat-fed rats but attenuated in a subgroup of high-fat-fed obese rats. Pharmacol Biochem Behav 103, 573–581. doi: 10.1016/j.pbb.2012.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Opland D, Sutton A, Woodworth H, et al. (2013) Loss of neurotensin receptor-1 disrupts the control of the mesolimbic dopamine system by leptin and promotes hedonic feeding and obesity. Mol Metab 2, 423–434. doi: 10.1016/j.molmet.2013.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Leidmaa E, Gazea M, Patchev AV., et al. (2020) Blunted leptin sensitivity during hedonic overeating can be reinstated by activating galanin 2 receptors (Gal2R) in the lateral hypothalamus. Acta Physiol 228, 1–16. doi: 10.1111/apha.13345 [DOI] [PubMed] [Google Scholar]
- 96.Zeng Y, Zhang L & Hu Z (2016) Cerebral insulin, insulin signaling pathway, and brain angiogenesis. Neurol Sci 37, 9–16. doi: 10.1007/s10072-015-2386-8 [DOI] [PubMed] [Google Scholar]
- 97.Mehran AE, Templeman NM, Brigidi GS, et al. (2012) Hyperinsulinemia drives diet-induced obesity independently of brain insulin production. Cell Metab 16, 723–737. doi: 10.1016/j.cmet.2012.10.019 [DOI] [PubMed] [Google Scholar]
- 98.Nash AI (2017) Crosstalk between insulin and dopamine signaling: a basis for the metabolic effects of antipsychotic drugs. J Chem Neuroanatx 83–84, 59–68. doi: 10.1016/j.jchemneu.2016.07.010 [DOI] [PubMed] [Google Scholar]
- 99.Perry ML, Leinninger GM, Chen R, et al. (2010) Leptin promotes dopamine transporter and tyrosine hydroxylase activity in the nucleus accumbens of Sprague-Dawley rats. J Neurochem 114, 666–674. doi: 10.1111/j.1471-4159.2010.06757.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Houseknecht KL & Spurlock ME (2003) Leptin regulation of lipid homeostasis: dietary and metabolic implications. Nutr Res Rev 16, 83. doi: 10.1079/nrr200256 [DOI] [PubMed] [Google Scholar]
- 101.Banks WA, Kastin AJ, Huang W, Jaspan JB & Maness LM (1996) Leptin enters the brain by a saturable system independent of insulin. Peptides 17, 305–311. doi: 10.1016/0196-9781(96)00025-3 [DOI] [PubMed] [Google Scholar]
- 102.Hamilton B, Paglia D, Kwan A & Deitel M (1995) Increased obese mRNA expression in omental fat cells from massively obese humans. Nat Med 1, 953–956. doi: 10.1038/nm0995-953 [DOI] [PubMed] [Google Scholar]
- 103.Schwartz M, Peskind E, Raskind M, Boyko E & Porte D Jr (1996) Cerebrospinal fluid leptin levels: relationship to plasma levels and to adiposity in humans. Nat Med 2, 589–593. doi: 10.1038/nm0596-589 [DOI] [PubMed] [Google Scholar]
- 104.Lee MJ, Wu Y & Fried SK (2010) Adipose tissue remodeling in pathophysiology of obesity. Curr Opin Clin Nutr Metab Care 13, 371–376. doi: 10.1097/MCO.0b013e32833aabef [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tsukumo D, Carvalho-Filho M, Carvalheira J, et al. (2007) Loss-of-function mutation in toll-like receptor 4 prevents diet-induced obesity and insulin resistance. Diabetes 56, 1986–1998. doi: 10.2337/db06-1595 [DOI] [PubMed] [Google Scholar]
- 106.Lawler HM, Underkofler CM, Kern PA, Erickson C, Bredbeck B & Rasouli N (2016) Adipose tissue hypoxia, inflammation, and fibrosis in obese insulin-sensitive and obese insulin-resistant subjects. J Clin Endocrinol Metab 101, 1422–1428. doi: 10.1210/jc.2015-4125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wu H, Liu Q, Kalavagunta PK, et al. (2017) Normal diet vs high fat diet – a comparative study: behavioral and neuroimmuno-logical changes in adolescent male mice. Metab Brain Dis 1–14. doi: 10.1007/s11011-017-0140-z [DOI] [PubMed] [Google Scholar]
- 108.Boura-Halfon S, Pecht T, Jung S & Rudich A (2019) Obesity and dysregulated central and peripheral macrophage–neuron cross-talk. Eur J Immunol 49, 19–29. doi: 10.1002/eji.201747389 [DOI] [PubMed] [Google Scholar]
- 109.Fritsche K (2015) The science of fatty acids and inflammation. Adv Nutr 6, 293S–301S. doi: 10.3945/an.114.006940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ciesielska A & Kwiatkowska K (2015) Modification of pro-inflammatory signaling by dietary components: the plasma membrane as a target. BioEssays 37, 789–801. doi: 10.1002/bies.201500017 [DOI] [PubMed] [Google Scholar]
- 111.Kennedy A, Martinez K, Chuang C-C, LaPoint K & McIntosh M (2008) Saturated fatty acid-mediated inflammation and insulin resistance in adipose tissue: mechanisms of action and implications. J Nutr 139, 1–4. doi: 10.3945/jn.108.098269 [DOI] [PubMed] [Google Scholar]
- 112.Hotamisligil G, Peraldi P, Budavari A, Ellis R, White M & Spiegelman B (1996) IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNF-alpha- and obesity-induced insulin resistance. Science (80-) 271, 665–668. doi: 10.1126/science.271.5249.665 [DOI] [PubMed] [Google Scholar]
- 113.Uysal K, Wiesbrock S, Marino M & Hotamisligil G (1997) Protection from obesity-induced insulin resistance in mice lacking TNF-alpha function. Nature 389, 610–614. doi: 10.1038/39335 [DOI] [PubMed] [Google Scholar]
- 114.Felger JC & Treadway MT (2017) Inflammation effects on motivation and motor activity: role of dopamine. Neuropsychopharmacology 42, 216–241. doi: 10.1038/npp.2016.143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Neurauter G, Schrocksnadel K, Scholl-Burgi S, et al. (2008) Chronic immune stimulation correlates with reduced phenylalanine turnover. Curr Drug Metab 9, 622–627. doi: 10.2174/138920008785821738 [DOI] [PubMed] [Google Scholar]
- 116.Song C, Merali Z & Anisman H (1999) Variations of nucleus accumbens dopamine and serotonin following systemic interleukin-1, interleukin-2 or interleukin-6 treatment. Neuroscience 88, 823–836. doi: 10.1016/S0306-4522(98)00271-1 [DOI] [PubMed] [Google Scholar]
- 117.Camandola S & Mattson MP (2017) Toll-like receptor 4 mediates fat, sugar, and umami taste preference and food intake and body weight regulation. Obesity 25, 1237–1245. doi: 10.1002/oby.21871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Décarie-Spain L, Sharma S, Hryhorczuk C, et al. (2018) Nucleus accumbens inflammation mediates anxiodepressive behavior and compulsive sucrose seeking elicited by saturated dietary fat. Mol Metab 10, 1–13. doi: 10.1016/j.molmet.2018.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gutiérrez-Martos M, Girard B, Mendonça-Netto S, et al. (2017) Cafeteria diet induces neuroplastic modifications in the nucleus accumbens mediated by microglia activation. Addict Biol 23, 735–749. doi: 10.1111/adb.12541 [DOI] [PubMed] [Google Scholar]
- 120.Radke AK & Gewirtz JC (2012) Increased dopamine receptor activity in the nucleus accumbens shell ameliorates anxiety during drug withdrawal. Neuropsychopharmacology 37, 2405–2415. doi: 10.1038/npp.2012.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Dutheil S, Ota KT, Wohleb ES, Rasmussen K & Duman RS (2016) High-fat diet induced anxiety and anhedonia: impact on brain homeostasis and inflammation. Neuropsychopharmacology 41, 1874–1887. doi: 10.1038/npp.2015.357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.McEwen BS (2007) Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev 87, 873–904. doi: 10.1152/physrev.00041.2006 [DOI] [PubMed] [Google Scholar]
- 123.Mcewen BS & Gianaros PJ (2010) Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann N Y Acad Sci 1186, 190–222. doi: 10.1111/j.1749-6632.2009.05331.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Rabasa C & Dickson SL (2016) Impact of stress on metabolism and energy balance. Curr Opin Behav Sci 9, 71–77. doi: 10.1016/j.cobeha.2016.01.011 [DOI] [Google Scholar]
- 125.Vallès A, Martí O, García A & Armario A (2000) Single exposure to stressors causes long-lasting, stress-dependent reduction of food intake in rats. Am J Physiol Regul Integr Comp Physiol 279, 1138–1144. doi: 10.1152/ajpregu.2000.279.3.r1138 [DOI] [PubMed] [Google Scholar]
- 126.Stone A & Brownell K (1994) The stress-eating paradox: multiple daily measurements in adult males and females. Psychol Heal 9, 425–436. doi: 10.1080/08870449408407469 [DOI] [Google Scholar]
- 127.Wing RR, Blair EH, Epstein LH & McDermott MD (1990) Psychological stress and glucose metabolism in obese and normal-weight subjects: a possible mechanism for differences in stress-induced eating. Heal Psychol 9, 693–700. doi: 10.1037/0278-6133.9.6.693 [DOI] [PubMed] [Google Scholar]
- 128.Kariagina A, Romanenko D, Ren SG & Chesnokova V (2004) Hypothalamic-pituitary cytokine network. Endocrinology 145, 104–112. doi: 10.1210/en.2003-0669 [DOI] [PubMed] [Google Scholar]
- 129.Wang W, Ji P & Dow KE (2003) Corticotropin-releasing hormone induces proliferation and TNF-α release in cultured rat microglia via MAP kinase signalling pathways. J Neurochem 84, 189–195. doi: 10.1046/j.1471-4159.2003.01544.x [DOI] [PubMed] [Google Scholar]
- 130.Oleson EB, Gentry RN, Chioma VC & Cheer JF (2012) Subsecond dopamine release in the nucleus accumbens predicts conditioned punishment and its successful avoidance. J Neurosci 32, 14804–14808. doi: 10.1523/JNEUROSCI.3087-12.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wenzel JM, Rauscher NA, Cheer JF & Oleson EB (2015) A role for phasic dopamine release within the nucleus accumbens in encoding aversion: a review of the neurochemical literature. ACS Chem Neurosci 6, 16–26. doi: 10.1021/cn500255p [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wanat MJ, Hopf FW, Stuber GD, Phillips PEM & Bonci A (2008) Corticotropin-releasing factor increases mouse ventral tegmental area dopamine neuron firing through a protein kinase C-dependent enhancement of Ih. J Physiol 586, 2157–2170. doi: 10.1113/jphysiol.2007.150078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Korotkova TM, Brown RE, Sergeeva OA, Ponomarenko AA & Haas HL (2006) Effects of arousal- and feeding-related neuropeptides on dopaminergic and GABAergic neurons in the ventral tegmental area of the rat. Eur J Neurosci 23, 2677–2685. doi: 10.1111/j.1460-9568.2006.04792.x [DOI] [PubMed] [Google Scholar]
- 134.Liu X (2015) Enhanced motivation for food reward induced by stress and attenuation by corticotrophin-releasing factor receptor antagonism in rats: implications for overeating and obesity. Psychopharmacology (Berl) 232, 2049–2060. doi: 10.1007/s00213-014-3838-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Weber MD, Frank MG, Sobesky JL, Watkins LR & Maier SF (2013) Blocking toll-like receptor 2 and 4 signaling during a stressor prevents stress-induced priming of neuroinflammatory responses to a subsequent immune challenge. Brain Behav Immun 32, 112–121. doi: 10.1016/j.bbi.2013.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Frank MG, Thompson BM, Watkins LR & Maier SF (2012) Glucocorticoids mediate stress-induced priming of microglial pro-inflammatory responses. Brain Behav Immun 26, 337–345. doi: 10.1016/j.bbi.2011.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Frank MG, Baratta MV, Sprunger DB, Watkins LR & Maier SF (2007) Microglia serve as a neuroimmune substrate for stress-induced potentiation of CNS pro-inflammatory cytokine responses. Brain Behav Immun 21, 47–59. doi: 10.1016/j.bbi.2006.03.005 [DOI] [PubMed] [Google Scholar]
- 138.Fonken LK, Frank MG, Gaudet AD, et al. (2018) Neuroinflammatory priming to stress is differentially regulated in male and female rats. Brain Behav Immun 70, 257–267. doi: 10.1016/j.bbi.2018.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Kas MJH, Bruijnzeel AW, Haanstra JR, Wiegant VM & Adan RAH (2005) Differential regulation of agouti-related protein and neuropeptide Y in hypothalamic neurons following a stressful event. J Mol Endocrinol 35, 159–164. doi: 10.1677/jme.1.01819 [DOI] [PubMed] [Google Scholar]
- 140.Betley JN, Xu S, Cao ZFH, et al. (2015) Neurons for hunger and thirst transmit a negative-valence teaching signal. Nature 521, 180–185. doi: 10.1038/nature14416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mandelblat-Cerf Y, Ramesh RN, Burgess CR, et al. (2015) Arcuate hypothalamic AgRP and putative POMC neurons show opposite changes in spiking across multiple timescales. eLife 4, 1–25. doi: 10.7554/eLife.07122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Shin AC, Mohankumar SMJ, Sirivelu MP, et al. (2010) Chronic exposure to a high-fat diet affects stress axis function differentially in diet-induced obese and diet-resistant rats. Int J Obes 34, 1218–1226. doi: 10.1038/ijo.2010.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Chagra SL, Zavala JK, Hall MV. & Gosselink KL (2011) Acute and repeated restraint differentially activate orexigenic pathways in the rat hypothalamus. Regul Pept 167, 70–78. doi: 10.1016/j.regpep.2010.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Calvez J, Fromentin G, Nadkarni N, et al. (2011) Inhibition of food intake induced by acute stress in rats is due to satiation effects. Physiol Behav 104, 675–683. doi: 10.1016/j.physbeh.2011.07.012 [DOI] [PubMed] [Google Scholar]
- 145.Dalvi PS, Chalmers JA, Luo V, et al. (2017) High fat induces acute and chronic inflammation in the hypothalamus: effect of high-fat diet, palmitate and TNF-α on appetite-regulating NPY neurons. Int J Obes 41, 149–158. doi: 10.1038/ijo.2016.183 [DOI] [PubMed] [Google Scholar]
- 146.Stumpo DJ & Kletzien RF (1981) Gluconeogenesis in rat liver parenchymal cells in primary culture: permissive effect of the glucocorticoids on glucagon stimulation of gluconeogenesis. J Cell Physiol 107, 11–19. doi: 10.1002/jcp.1041070103 [DOI] [PubMed] [Google Scholar]
- 147.Gravholt CH, Dall R, Christiansen JS, Møller N & Schmitz O (2002) Preferential stimulation of abdominal subcutaneous lipolysis after prednisolone exposure in humans. Obes Res 10, 774–781. doi: 10.1038/oby.2002.105 [DOI] [PubMed] [Google Scholar]
- 148.Nicod N, Giusti V, Besse C & Tappy L (2003) Metabolic adaptations to dexamethasone-induced insulin resistance in healthy volunteers. Obes Res 11, 625–631. doi: 10.1038/oby.2003.90 [DOI] [PubMed] [Google Scholar]
- 149.Zakrzewska KE, Cusin I, Stricker-Krongrad A, et al. (1999) Induction of obesity and hyperleptinemia by central glucocorticoid infusion in the rat. Diabetes 48, 365–370. doi: 10.2337/diabetes.48.2.365 [DOI] [PubMed] [Google Scholar]
- 150.Giordano R, Marzotti S, Berardelli R, et al. (2012) BClI polymorphism of the glucocorticoid receptor gene is associated with increased obesity, impaired glucose metabolism and dyslipidaemia in patients with Addison’s disease. Clin Endocrinol (Oxf) 77, 863–870. doi: 10.1111/j.1365-2265.2012.04439.x [DOI] [PubMed] [Google Scholar]
- 151.Uddén J, Björntorp P, Arner P, Barkeling B, Meurling L & Rössner S (2003) Effects of glucocorticoids on leptin levels and eating behaviour in women. J Intern Med 253, 225–231. doi: 10.1046/j.1365-2796.2003.01099.x [DOI] [PubMed] [Google Scholar]
- 152.Hopkins LB, Medina JL, Baird SO, Rosenfield D, Powers MB & Smits JAJ (2016) Heated hatha yoga to target cortisol reactivity to stress and affective eating in women at risk for obesity-related illnesses: a randomized controlled trial. J Consult Clin Psychol 84, 558–564. doi: 10.1037/ccp0000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Maniam J & Morris MJ (2012) The link between stress and feeding behaviour. Neuropharmacology 63, 97–110. doi: 10.1016/j.neuropharm.2012.04.017 [DOI] [PubMed] [Google Scholar]
- 154.Lorig F, KieBl G & Laessle R (2016) Stress-related cortisol response and laboratory eating behavior in obese women. Eat Weight Disord Stud Anorexia, Bulemia Obes 21, 237–243. doi: 10.1007/s40519-015-0190-3 [DOI] [PubMed] [Google Scholar]
- 155.Epel E, Lapidus R, McEwen B & Brownell K (2001) Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology 26, 37–49. doi: 10.1016/s0306-4530(00)00035-4 [DOI] [PubMed] [Google Scholar]
- 156.Bhatnagar S, Bell ME, Liang J, Soriano L, Nagy TR & Dallman MF (2000) Corticosterone facilitates saccharin intake in adrenalectomized rats: does corticosterone increase stimulus salience? J Neuroendocrinol 12, 453–460. doi: 10.1046/j.1365-2826.2000.00487.x [DOI] [PubMed] [Google Scholar]
- 157.Bell ME, Bhatnagar S, Liang J, Soriano L, Nagy TR & Dallman MF (2000) Voluntary sucrose ingestion, like corticosterone replacement, prevents the metabolic deficits of adrenalectomy. J Neuroendocrinol 12, 461–470. doi: 10.1046/j.1365-2826.2000.00488.x [DOI] [PubMed] [Google Scholar]
- 158.La Fleur SE, Houshyar H, Roy M & Dallman MF (2005) Choice of lard, but not total lard calories, damps adrenocorticotropin responses to restraint. Endocrinology 146, 2193–2199. doi: 10.1210/en.2004-1603 [DOI] [PubMed] [Google Scholar]
- 159.Finger BC, Dinan TG & Cryan JF (2011) High-fat diet selectively protects against the effects of chronic social stress in the mouse. Neuroscience 192, 351–360. doi: 10.1016/j.neuroscience.2011.06.072 [DOI] [PubMed] [Google Scholar]
- 160.Volkow ND, Wang GJ & Baler RD (2011) Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci 15, 37–46. doi: 10.1016/j.tics.2010.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Iyengar S, Kim HS & Wood PL (1987) μ-, δ-, κ- and ϵ-Opioid receptor modulation of the hypothalamic-pituitary-adrenocortical (HPA) axis: subchronic tolerance studies of endogenous opioid peptides. Brain Res 435, 220–226. doi: 10.1016/0006-8993(87)91604-0 [DOI] [PubMed] [Google Scholar]
- 162.Thai L, Lee PHK, Ho J, Suh H & Hong JS (1992) Regulation of prodynorphin gene expression in the hippocampus by glucocorticoids. Mol Brain Res 16, 150–157. doi: 10.1016/0169-328X(92)90205-P [DOI] [PubMed] [Google Scholar]
- 163.Wittmann W, Schunk E, Rosskothen I, et al. (2009) Prodynorphin-derived peptides are critical modulators of anxiety and regulate neurochemistry and corticosterone. Neuropsychopharmacology 34, 775–785. doi: 10.1038/npp.2008.142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Konkoy CS & Childers SR (1989) Dynorphin-selective inhibition of adenylyl cyclase in guinea pig cerebellum membranes. Mol Pharmacol 36, 627–633. [PubMed] [Google Scholar]
- 165.Prather PL, McGinn TM, Claude PA, Liu-Chen LY, Loh HH & Law PY (1995) Properties of a κ-opioid receptor expressed in CHO cells: interaction with multiple G-proteins is not specific for any individual Gα subunit and is similar to that of other opioid receptors. Mol Brain Res 29, 336–346. doi: 10.1016/0169-328X(94)00264-F [DOI] [PubMed] [Google Scholar]
- 166.Svingos AL, Chavkin C, Colago EEO & Pickel VM (2001) Major coexpression of κ-opioid receptors and the dopamine transporter in nucleus accumbens axonal profiles. Synapse 42, 185–192. doi: 10.1002/syn.10005 [DOI] [PubMed] [Google Scholar]
- 167.Zhu J & Reith MEA (2008) Role of dopamine transporter in the action of psychostimulants, nicotine, and other drugs of abuse. CNS Neurol Disord Drug Targets 7, 393–409. doi: 10.2174/187152708786927877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Spanagel R, Herz A & Shippenberg TS (1990) The effects of opioid peptides on dopamine release in the nucleus accumbens: an in vivo microdialysis study. J Neurochem 55, 1734–1740. doi: 10.1111/j.1471-4159.1990.tb04963.x [DOI] [PubMed] [Google Scholar]
- 169.Thompson AC, Zapata A, Justice JB, Vaughan RA, Sharpe LG & Shippenberg TS (2000) k-Opioid receptor activation modifies dopamine uptake in the nucleus accumbens and opposes the effects of cocaine. J Neurosci 20, 9333–9340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Karkhanis A, Holleran KM & Jones SR (2017) Dynorphin/Kappa Opioid Receptor Signaling in Preclinical Models of Alcohol, Drug, and Food Addiction. Vol 136. 1st ed. Elsevier Inc. doi: 10.1016/bs.irn.2017.08.001 [DOI] [PubMed] [Google Scholar]
- 171.Ookuma K, Barton C, York DA & Bray GA (1997) Effect of enterostatin and kappa-opioids on macronutrient selection and consumption. Peptides 18, 785–791. doi: 10.1016/S0196-9781(97)00029-6 [DOI] [PubMed] [Google Scholar]
- 172.Ebner SR, Roitman MF, Potter DN, Rachlin AB & Chartoff EH (2010) Depressive-like effects of the kappa opioid receptor agonist salvinorin A are associated with decreased phasic dopamine release in the nucleus accumbens. Psychopharmacology (Berl) 210, 241–252. doi: 10.1007/s00213-010-1836-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Tejeda HA, Natividad LA, Orfila JE, Torres OV & O’Dell LE (2012) Dysregulation of kappa-opioid receptor systems by chronic nicotine modulate the nicotine withdrawal syndrome in an age-dependent manner. Psychopharmacology (Berl) 224, 289–301. doi: 10.1007/s00213-012-2752-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Del Pilar Escobar A, Cornejo FA, Andrés ME & Fuentealba JA (2012) Repeated treatment with the kappa opioid receptor agonist U69593 reverses enhanced K+ induced dopamine release in the nucleus accumbens, butþnot the expression of locomotor sensitization in amphetamine-sensitized rats. Neurochem Int 60, 344–349. doi: 10.1016/j.neuint.2012.01.014 [DOI] [PubMed] [Google Scholar]
- 175.Nealey KA, Smith AW, Davis SM, Smith DG & Walker BM (2011) κ-opioid receptors are implicated in the increased potency of intra-accumbens nalmefene in ethanol-dependent rats. Neuropharmacology 61, 35–42. doi: 10.1016/j.neuropharm.2011.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Knapp DJ, Whitman BA, Wills TA, et al. (2011) Cytokine involvement in stress may depend on corticotrophin releasing factor to sensitize ethanol withdrawal anxiety. Brain Behav Immun 25(Suppl. 1), S146–S154. doi: 10.1016/j.bbi.2011.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Treadway MT, Admon R, Arulpragasam AR, et al. (2017) Association between interleukin-6 and striatal prediction-error signals following acute stress in healthy female participants. Biol Psychiatry 82, 570–577. doi: 10.1016/j.biopsych.2017.02.1183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Aslani S, Vieira N, Marques F, Costa PS, Sousa N & Palha JA (2015) The effect of high-fat diet on rat’s mood, feeding behavior and response to stress. Transl Psychiatry 5, e684–688. doi: 10.1038/tp.2015.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Liu L, Xu Y, Dai H, Tan S, Mao X & Chen Z (2020) Dynorphin activation of kappa opioid receptor promotes microglial polarization toward M2 phenotype via TLR4/NF-κB pathway. Cell Biosci 10, 1–12. doi: 10.1186/s13578-020-00387-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Puehler W, Rittner HL, Mousa SA, et al. (2006) Interleukin-1 beta contributes to the upregulation of kappa opioid receptor mRNA in dorsal root ganglia in response to peripheral inflammation. Neuroscience 141, 989–998. doi: 10.1016/j.neuroscience.2006.03.078 [DOI] [PubMed] [Google Scholar]
- 181.Alsiö J, Olszewski PK, Norbäck AH, et al. (2010) Dopamine D1 receptor gene expression decreases in the nucleus accumbens upon long-term exposure to palatable food and differs depending on diet-induced obesity phenotype in rats. Neuroscience 171, 779–787. doi: 10.1016/j.neuroscience.2010.09.046 [DOI] [PubMed] [Google Scholar]
- 182.Bake T, Baron J, Duncan JS, Morgan DGA & Mercer JG (2017) Arcuate nucleus homeostatic systems reflect blood leptin concentration but not feeding behaviour during scheduled feeding on a high-fat diet in mice. J Neuroendocrinol 29, 1–10. doi: 10.1111/jne.12498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Small DM, Zatorre R, Dagher A, Evans A & Jones-Gotman M (2001) Changes in brain activity related to eating chocolate: from pleasure to aversion. Brain 124, 1720–1733. doi: 10.1093/brain/124.9.1720 [DOI] [PubMed] [Google Scholar]
- 184.Frasnelli J, Hummel C, Bojanowski V, Warr J, Gerber J & Hummel T (2015) Food-related odors and the reward circuit: functional MRI. Chemosens Percept 8, 192–200. doi: 10.1007/s12078-015-9193-8 [DOI] [Google Scholar]
- 185.Carlin JL, McKee SE, Hill-Smith T, et al. (2016) Removal of high-fat diet after chronic exposure drives binge behavior and dopaminergic dysregulation in female mice. Neuroscience 326, 170–179. doi: 10.1016/j.neuroscience.2016.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Sandoval-Salazar C, Ramírez-Emiliano J, Trejo-Bahena A, Oviedo-Solís CI & Solís-Ortiz MS (2016) A high-fat diet decreases GABA concentration in the frontal cortex and hippocampus of rats. Biol Res 49, 1–6. doi: 10.1186/s40659-016-0075-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.van den Top M, Zhao FY, Viriyapong R, et al. (2017) The impact of ageing, fasting and high-fat diet on central and peripheral glucose tolerance and glucose-sensing neural networks in the arcuate nucleus. J Neuroendocrinol 29, 1–23. doi: 10.1111/jne.12528 [DOI] [PubMed] [Google Scholar]
- 188.Lee AK, Mojtahed-Jaberi M, Kyriakou T, et al. (2010) Effect of high-fat feeding on expression of genes controlling availability of dopamine in mouse hypothalamus. Nutrition 26, 411–422. doi: 10.1016/j.nut.2009.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Linehan V, Fang LZ & Hirasawa M (2018) Short-term high-fat diet primes excitatory synapses for long-term depression in orexin neurons. J Physiol 596, 305–316. doi: 10.1113/JP275177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Nobunaga M, Obukuro K, Kurauchi Y, et al. (2014) High fat diet induces specific pathological changes in hypothalamic orexin neurons in mice. Neurochem Int 78, 61–66. doi: 10.1016/j.neuint.2014.09.002 [DOI] [PubMed] [Google Scholar]
- 191.Vaessen T, Hernaus D, Myin-Germeys I & van Amelsvoort T (2015) The dopaminergic response to acute stress in health and psychopathology: a systematic review. Neurosci Biobehav Rev 56, 241–251. doi: 10.1016/j.neubiorev.2015.07.008 [DOI] [PubMed] [Google Scholar]
- 192.Tannenbaum BM, Brindley DN, Tannenbaum GS, Dallman MF, McArthur MD & Meaney MJ (1997) High-fat feeding alters both basal and stress-induced hypothalamic-pituitary-adrenal activity in the rat. Am J Physiol Endocrinol Metab 273, 1168–1177. doi: 10.1152/ajpendo.1997.273.6.e1168 [DOI] [PubMed] [Google Scholar]
- 193.Foster MT, Warne JP, Ginsberg AB, et al. (2009) Palatable foods, stress, and energy stores sculpt corticotropin-releasing factor, adrenocorticotropic and corticosterone concentrations after restraint. Endocrinology 150, 2325–2333. doi: 10.1210/en.2008-1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Foster MT, Solomon MB, Huhman KL & Bartness TJ (2006) Social defeat increases food intake, body mass, and adiposity in Syrian hamsters. Am J Physiol Regul Integr Comp Physiol 290, 1284–1293. doi: 10.1152/ajpregu.00437.2005 [DOI] [PubMed] [Google Scholar]
- 195.Ali EF, MacKay JC, Graitson S, et al. (2018) Palatable food dampens the long-term behavioral and endocrine effects of juvenile stressor exposure but may also provoke metabolic syndrome in rats. Front Behav Neurosci 12, 1–15. doi: 10.3389/fnbeh.2018.00216 [DOI] [PMC free article] [PubMed] [Google Scholar]


