Abstract
The COVID-19 pandemic led to a worldwide implementation of measures to contain the virus from spreading, and social isolation was one of those measures. Social isolation is associated with increased susceptibility to various neuropsychiatric disorders, including depression. Because this risk varies between populations and their respective habits, understanding which behaviors play a positive or harmful role is fundamental for people with depression under these conditions. This study aims to 1) compare health-related behaviors (HRBs) and perceived addictions between healthy individuals and individuals who reported having a depressive disorder at the time of the first outbreak of the COVID-19 pandemic in Portugal, and 2) test which HRB and perceived addictions are associated with depression. Participants were a matched for age and sex and comprised 968 adults divided into two groups: healthy (484, 50%) and depressed (484, 50%). They completed online self-report questionnaires, and the data were analyzed in SPSS. Logistic regressions showed that being a health professional, getting up in a later time during weekends, and a higher consumption of soft drinks increased the risk for depression. In contrast, higher education and higher intensity of physical activity decreased this risk. Perceived addictions to TV, social networking, and gaming increased the risk for depression. HRBs and the identified addictions associated with depression during the confinement should be targeted in clinical and community interventions.
Key Words: Depression, COVID-19 pandemic, addictions, diet, physical activity
In Psychiatry of Pandemics (2019), Damir Huremović and colleagues conceptualized parallel processes in the mirror that seem to apply to both infectious and mental illness in the context of a pandemic. Just as pathogens are identified and transmitted by vectors, from a psychological perspective, (dis)information sources (e.g., false, contradictory, alarming news) are disseminated through the various media: the measures taken to contain the spread of the infectious agent and the incubation period parallel the growing psychological effects of isolation and uncertainty (e.g., fear of infection, the health of loved ones, and the future; Huremović, 2019).
Several studies have examined the effects of isolation and quarantine on mental health, and most have shown increased susceptibility to various neuropsychiatric disorders, including feelings of hopelessness, anxiety, depression, cognitive dysfunction, and suicidal ideation (Brooks et al., 2020; Hawryluck et al., 2004; Marjanovic et al., 2007; Reynolds et al., 2008). It is very important to understand the behavior of depressed people under these conditions.
Since the first outbreak of the disease caused by the new coronavirus SARS-Cov-2, identified in December 2019 and declared a pandemic by the World Health Organization in March 2020, various measures such as social isolation and quarantine (sometimes 14–21 days) have been widely used to contain the virus spread.
Nervousness and anxiety are issues that greatly affect our society (World Health Organization, 2017). The advent of COVID-19, with the rapid spread of news, rumors, misinformation, and fabricated reports, has exacerbated anxiety in populations worldwide (Moghanibashi-Mansourieh, 2020; Salari et al., 2020), as well as depression, with a 3-fold higher prevalence of depressive symptoms in general (Ettman et al., 2020). According to a systematic review and meta-analysis, the prevalence values of stress, anxiety, and depression, as a result of the COVID-19 pandemic in the general population, were 29.6%, 31.9%, and 33.7%, respectively (Salari et al., 2020). A review described a substantial risk of increasing substance use disorders during lockdown (Mallet et al., 2021). However, the mental health consequences of mass traumatic events are not evenly distributed across populations. The risk seems to be higher in developing and underdeveloped countries and for people aged 21 to 40 years; moreover, people with higher education might exhibit increased anxiety and stress for having more insight and awareness of their health-state than those with lower education (Moghanibashi-Mansourieh, 2020; Salari et al., 2020; Wang et al., 2019). Other studies identified other populations at higher risk for negative mental health outcomes, including homeless, migrants, pregnant women, health care workers, and individuals with preexisting physical or psychiatric morbidity (Rajkumar, 2020; Solomou and Constantinidou, 2020). Among the latter, depressive disorder highlights a common problem worldwide, affecting more than 264 million people (James et al., 2018). Despite the evidence of these risk factors, it is sometimes difficult to change them in the short to medium term.
Therefore, it seems fundamental to think about behaviors that depend partly on one's will, namely, behaviors that are related to health (e.g., screen exposure, physical activity [PA], sedentarism, sleep patterns, eating habits). For example, some dietary patterns seem to be associated with depression, whereas others seem to have a protective role on mood (Li et al., 2017). Sleep and PA have a bidirectional relationship with mood (Pascoe and Parker, 2019; Watling et al., 2017), and several studies report a high rate of mood disorders in patients with addictions (Lai et al., 2015). Although previous studies have identified everyday behaviors associated with mental health, existing data applied to the context of the COVID-19 pandemic are scarce. Identifying everyday behaviors associated with mental health could help in developing appropriate psychological strategies and interventions to mitigate the mental health impact of public health measures used to prevent infectious disease outbreaks. This information could also complement other studies regarding the impact of COVID-19 on mental health and an overall need for services and policies reorganization to prevent a possible future epidemic of psychiatric disorders (Chevance et al., 2020). Therefore, the aim of our study was to identify and compare health-related behaviors (HRBs) and perceived addictions between healthy individuals and individuals who reported having a depressive disorder at the time of the first outbreak of the COVID-19 pandemic in Portugal. Furthermore, our intention was to test which HRB and perceived addictions increased the risk of depression during this period.
METHODS
Procedures
Data were collected online during the first COVID-19 outbreak, from April to August 2020 (during lockdown), using the Survey Legend platform. This platform is used for scientific purposes, assuring security by data encryption (Gaur et al., 2020). Only adults (>18 years) completed a self-report questionnaire. The sample was obtained by a nonprobabilistic snowball method, as part of a larger project. The total sample was composed of 5459 individuals, and all participants gave informed consent after being assured of confidentiality and voluntariness of participation. For this study, participants who reported experiencing depression were selected for the depressed group. Then, a propensity score matching for age and sex was performed to find matched healthy participants (who did not report experiencing any health condition) for the control group. This procedure was an attempt to reduce bias due to confounding variables (age and sex). This study took into account the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Measures
The following sociodemographic variables were questioned: age, sex, marital status, education, and field of work. HRB included PA, sleep, diet, toxic habits (tobacco, alcohol, and other drugs), and electronics use.
One of the questions included in the questionnaire was if people had a current diagnosis of a specific health condition (e.g., depression, hypertension, diabetes, obstructive sleep apnea). From these, we selected the depressed group based on people who reported a diagnosis of depression; for all the ones that did not report any condition, we considered as healthy (control group).
PA included two items: hours per week and intensity that ranged from 1 = “none” to 4 = “intense.” Sleep was assessed with 10 items: bedtime, get up time, total sleep time, total time in bed, and time in bed awake (calculated from total time in bed − total sleep time), all values were reported for weekdays and weekends. Diet was composed of 18 items: number of meals per day and frequency of consumption of certain foods (e.g., fruits/vegetables, milk and derivatives, chocolate, meat and fish, tea/coffee; the scale ranged from 1 = “never” to 6 = “more than 3 times a day”). Toxic habits were assessed by asking frequency of use during the confinement (number of glasses of beer and/or wine and number of cigarettes per day; from 1 = “never” to 3 = “regularly” for drugs). Electronic use included four items: hours per day of TV, social networking, mobile phone, and gaming.
Perceived addiction was assessed with four items rated on a 10-point Likert scale (ranging from 1 = “not addicted” to 10 = “very addicted”) across TV, social networking, gaming, and alcohol.
Data Analyses
The present study followed a cross-sectional design. Descriptive statistics and frequencies were conducted to characterize the present sample. Normality of the data was tested using the Kolmogorov-Smirnov test and skewness (sk) and kurtosis (ku) values (normality assumed for sk < 3 and ku < 8; Kline, 2011). Differences between groups were examined using the Student's t-test for independent samples. In the current study, the dependent variable was being healthy (0) or with depression (1). The independence of the errors was tested by the Durbin-Watson value (independence assumed at D-W < 2.5). Multicollinearity or singularity among variables was tested considering variance inflation factors (VIFs); this assumption being assured when VIF < 5 (Kline, 2011). Variables for input to the model were selected for a p-value < 0.01 in the bivariate analysis (Pearson t test or χ2 test).
We created two models: 1) for HRB, with the covariates educational status, being a health professional “yes versus no,” PA intensity, sleep duration on weekdays and weekends, get up time for weekdays and weekends, frequency of biscuits and cakes, processed foods, candies, soft drinks, wine, desserts, watching TV, and social networks; 2) for perceived addictions, with the covariate's educational status, being a health professional “yes versus no.” A receiver operator characteristic (ROC) analysis was computed for the two models to calculate the model's overall measure of discrimination for experiencing depression.
The G*Power software determined a power of 0.90 (alpha = 0.05) for logistic regressions and independent group differences considering our sample size (N = 968). Statistical significance was established at p-value < 0.05. Statistical analyses were performed in IBM SPSS Statistics, version 27 (IBM Corp, Armonk, NY).
RESULTS
Participants
The characteristics of the sample are described in Table 1. Participants were 968 adults divided into two groups: healthy (50%) and depressed (50%). Healthy participants were 484 with a mean age of 50.75 (SD = 12.75) years, of whom 104 were male (21.5%) and 380 were female (78.5%). Three hundred were graduates (62%) and 122 masters (25.2%). Depressed participants were 484 with a mean age of 50.88 (SD = 13.08), of which 104 were males (21.5%) and 380 were females (78.5%). Two hundred two were graduates (41.7%) and 123 were masters (25.6%). Nonsignificant differences between groups were found for age, t(966) = 0.15, p = 0.88.
TABLE 1.
Sample Characteristics by Group (Healthy and Depressed) and Differences on Sociodemographic Variables (N = 968)
| Healthy | Depressed | p | |
|---|---|---|---|
| n (%) | 484 (50) | 484 (50) | NA |
| Sex, n (%) | |||
| Male | 104 (21.5) | 104 (21.5) | NA |
| Female | 380 (78.5) | 380 (78.5) | |
| Age, mean ± (SD) | 50.8 (12.8) | 50.2 (13.1) | 0.877 |
| Education level, n (%) | |||
| Primary | 1 (0.2) | 12 (2.5) | <0.001 |
| Secondary | 22 (4.5) | 89 (18.4) | |
| Professional | 4 (0.8) | 26 (5.4) | |
| Bachelor | 7 (1.4) | 15 (3.1) | |
| Graduate | 300 (62) | 202 (41.7) | |
| Master | 122 (25.2) | 124 (25.6) | |
| PhD | 26 (5.4) | 7 (1.4) | |
| Marital status, n (%) | |||
| Single | 82 (16.9) | 116 (24) | 0.002 |
| Married | 274 (56.6) | 223 (46.1) | |
| Divorced | 69 (14.3) | 76 (15.7) | |
| Widowed | 11 (2.3) | 25 (5.2) | |
| Consensual union | 48 (9.9) | 43 (8.9) | |
| Health professional, n (%) | |||
| Yes | 374 (77.3) | 200 (41.3) | <0.001 |
| No | 104 (21.5) | 266 (55.0) | |
Values in boldface indicate statistical significance.
HRB of Healthy and Depressed People During the Confinement
The differences in HRB between healthy and depressed individuals during the confinement are shown in Table 2. The results showed that healthy individuals reported higher PA, both in frequency and intensity. Depressed individuals had higher sleep duration on both weekdays and weekends and reported getting up later on weekdays and weekends as well. Time in bed was also higher for the depressed group, both on weekdays and weekends. Time awake in bed was also higher for the depressed group, although only with statistical significance for weekends. They reported eating more biscuits and cakes, precooked and processed foods, charcuterie, candies, soft drinks, and sweet desserts, and fewer eggs during the confinement compared with healthy subjects. In addition, the depressed group reported higher wine consumption and drug use, as well as more hours watching TV and using social networks and mobile phones.
TABLE 2.
Means (M) and Standard Deviations (SD) of HRB Indicators by Group (Healthy and Depressed)
| Healthy | Depressed | p | |
|---|---|---|---|
| n (%) | 484 (50) | 484 (50) | — |
| PA | |||
| Hours per week, mean ± (SD) | 2.97 (3.13) | 2.24 (4.08) | 0.020 |
| Intensity, mean ± (SD) | 2.35 (0.89) | 1.97 (0.87) | <0.001 |
| Sleep (weekdays), mean ± (SD) | |||
| Bedtime, h | 0.09 (1.60) | 0.06 (1.70) | 0.808 |
| Get up time, h | 7.54 (1.28) | 8.22 (1.76) | <0.001 |
| Sleep duration, h | 6.23 (1.32) | 6.82 (1.87) | <0.001 |
| Time in bed, h | 7.50 (1.53) | 8.25 (1.91) | <0.001 |
| Time in bed awake, h | 1.28 (1.45) | 1.43 (2.38) | 0.348 |
| Sleep (weekends), mean ± (SD) | |||
| Bedtime, h | 0.46 (1.65) | 0.33 (1.77) | 0.314 |
| Get up time, h | 8.43 (1.55) | 9.19 (1.67) | <0.001 |
| Sleep duration, h | 7.11 (1.92) | 7.53 (1.97) | 0.005 |
| Time in bed, h | 7.97 (1.86) | 8.89 (1.83) | <0.001 |
| Time in bed awake, h | 0.86 (2.24) | 1.35 (2.47) | 0.009 |
| Nutrition (frequency of consumption), mean ± (SD) | |||
| Meals per day | 3.82 (0.90) | 3.83 (0.96) | 0.852 |
| Fruits/vegetables | 4.98 (0.97) | 4.90 (1.12) | 0.281 |
| Dairy products | 4.34 (1.30) | 4.36 (1.36) | 0.832 |
| Chocolates | 2.74 (1.31) | 2.86 (1.46) | 0.255 |
| Biscuits and cakes | 2.78 (1.23) | 3.34 (1.49) | <0.001 |
| Carbs | 4.37 (1.16) | 4.52 (1.19) | 0.095 |
| Precooked food | 1.72 (0.97) | 1.88 (1.13) | 0.045 |
| Processed food | 2.02 (1.03) | 2.28 (1.25) | 0.003 |
| Charcuterie | 2.35 (1.08) | 2.54 (1.28) | 0.029 |
| Eggs | 2.74 (0.80) | 2.89 (1.04) | 0.041 |
| Honey and jams | 2.07 (1.21) | 2.08 (1.22) | 0.889 |
| Dry fruits | 2.78 (1.33) | 2.71 (1.40) | 0.473 |
| Candies | 1.50 (0.93) | 1.74 (1.27) | 0.004 |
| Legumes | 3.19 (1.19) | 3.06 (1.20) | 0.139 |
| Meat and fish | 4.43 (0.96) | 4.29 (1.03) | 0.061 |
| Tea and coffee | 4.89 (1.22) | 4.72 (1.35) | 0.073 |
| Soft drinks | 1.57 (0.87) | 1.92 (1.33) | <0.001 |
| Sweet desserts | 2.22 (0.85) | 2.48 (1.10) | 0.001 |
| Alcohol and substances, mean ± (SD) | |||
| Cigarettes | 12.78 (7.74) | 14.19 (9.56) | 0.380 |
| Beer | 0.72 (1.84) | 0.48 (1.12) | 0.102 |
| Wine | 0.05 (0.31) | 0.27 (0.76) | <0.001 |
| Drugs | 1 (0.05) | 1.04 (0.24) | 0.010 |
| Electronics use (hours per day) | |||
| TV | 2.49 (1.65) | 3.64 (3.04) | <0.001 |
| Social networks | 2.22 (2.44) | 2.94 (2.96) | 0.002 |
| Mobile phone | 2.26 (1.93) | 2.67 (2.71) | 0.033 |
| Games | 1.64 (1.85) | 2.03 (1.34) | 0.137 |
Student’s t-tests performed for differences between groups (N = 968). Values in boldface indicate statistical significance.
A logistic regression model for HRB associated with depression was performed, with the following covariates: educational status, being a health professional, PA intensity, sleep duration on weekdays and weekends, get up time for weekdays and weekends, frequency of biscuit and cakes, processed foods, candies, soft drinks, wine, desserts, watching television, and social networks. Variables with predictive value for increased risk of being depressed were being a health professional (odds ratio [OR], 2.45 [1.10–5.45]), later get up time for weekends (OR, 1.498 [1.09–2.06]), and a higher consumption of soft drinks (OR, 1.51 [1.07–2.13]); variables associated with a protective value for depression were a higher level of educational (OR, 0.73 [0.54–0.99]) and a higher intensity of PA (OR, 0.65 [0.44–0.97]) (Table 3).
TABLE 3.
Logistic Regression Analysis for HRB Indicators for Being Depressed
| Odds Ratio | 95% CI | ||
|---|---|---|---|
| Lower | Upper | ||
| Educational level | 0.734 | 0.544 | 0.989 |
| Being a health professional | 2.451 | 1.102 | 5.452 |
| PA intensity | 0.654 | 0.443 | 0.966 |
| Sleep duration weekdays | 1.177 | 0.883 | 1.569 |
| Sleep duration weekends | 0.910 | 0.693 | 1.195 |
| Get up time weekdays | 0.946 | 0.675 | 1.325 |
| Get up time weekends | 1.498 | 1.091 | 2.057 |
| Frequency of biscuits and cakes | 1.302 | 0.983 | 1.725 |
| Frequency of processed food | 1.221 | 0.869 | 1.716 |
| Frequency of candies | 0.756 | 0.523 | 1.094 |
| Frequency of soft drinks (glasses/day) | 1.508 | 1.068 | 2.131 |
| Frequency of wine (glasses/day) | 1.388 | 0.744 | 2.590 |
| Frequency of sweet desserts | 0.929 | 0.630 | 1.370 |
An ROC curve (Fig. 1) was plotted to calculate the overall measure of discrimination (area under the curve). This model showed a good discriminatory power for depression with an area under the curve of 0.82 (95% CI, 0.77–0.88).
FIGURE 1.
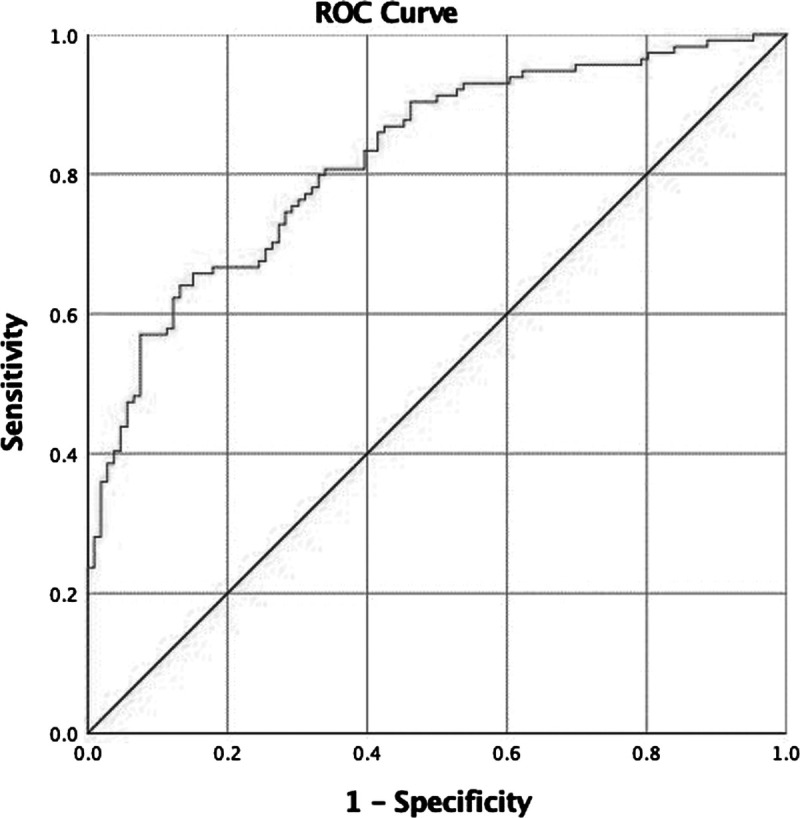
ROC curve for the HRBs model.
Perceived Addictions of Healthy and Depressed People During the Confinement
The perceived addition of TV, social networking, and gaming during the confinement is shown in Table 4. Depressed individuals reported higher levels of perceived addiction to TV, social networking, gaming, and alcohol compared with healthy individuals.
TABLE 4.
Means (M) and Standard Deviations (SD) of Perceived Addictions by Group (Healthy and Depressed)
| Healthy | Depressed | p | |
|---|---|---|---|
| Perceived addition, M (SD) | |||
| TV | 2.73 (1.74) | 3.64 (2.17) | <0.001 |
| Social networks | 3.20 (2.17) | 4.31 (2.56) | <0.001 |
| Games | 1.49 (1.35) | 1.95 (1.88) | <0.001 |
| Alcohol | 1.32 (0.89) | 1.52 (1.36) | 0.028 |
Student's t-tests performed for differences between groups (N = 968). Values in boldface indicate statistical significance.
A logistic regression model for perceived addictions, which is associated with depression, was conducted using the covariates: educational status, being a health professional, TV, social networks, and gaming. In this model, all variables have predictive value. There was an increased risk of being depressed for the following variables: being a health professional (OR, 3.17 [2.17–4.64]), watching television (OR, 1.19 [1.08–1.30]), social networking (OR, 1.14 [1.05–1.22]), gaming (OR, 1.13 [1.01–1.26]), and having a higher level of education had a protective value for depression (OR, 0.76 [0.65–0.90]) (Table 5). This model showed an acceptable discriminatory power for depression with an area under the curve of 0.75 (95% CI, 0.71–0.79) (Fig. 2).
TABLE 5.
Logistic Regression Analysis for Perceived Addictions Indicators for Being Depressed
| Odds Ratio | 95% CI | ||
|---|---|---|---|
| Lower | Upper | ||
| Educational level | 0.764 | 0.649 | 0.899 |
| Being a health professional | 3.172 | 2.169 | 4.638 |
| Television | 1.188 | 1.084 | 1.301 |
| Social networks | 1.135 | 1.053 | 1.223 |
| Games | 1.129 | 1.013 | 1.259 |
FIGURE 2.
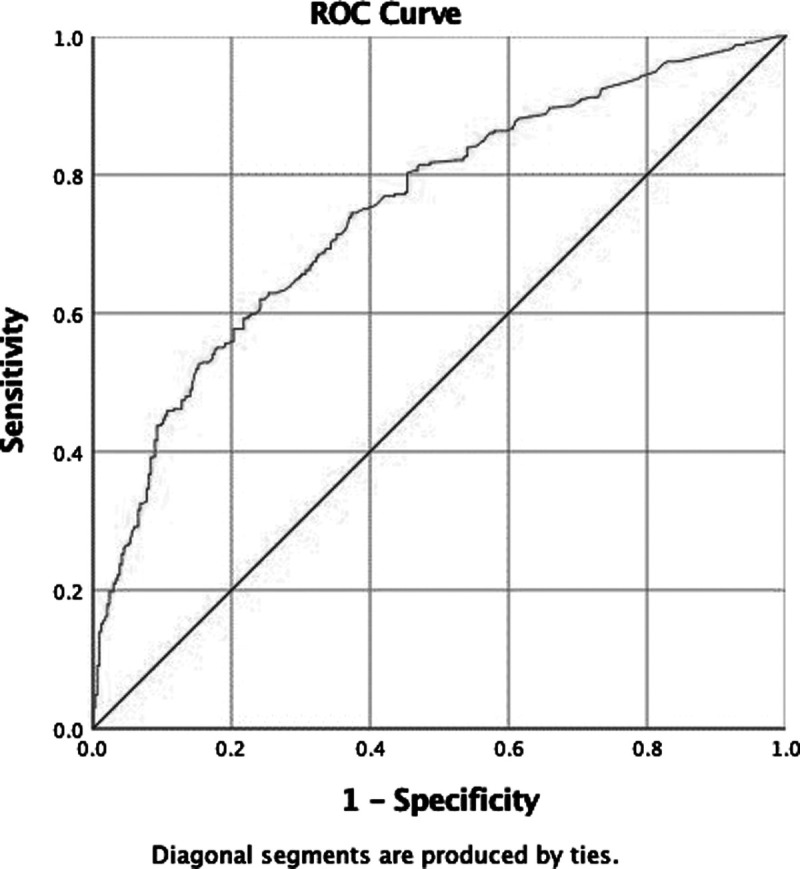
ROC curve for the perceived addictions model.
The summary of our results is described on Figure 3.
FIGURE 3.
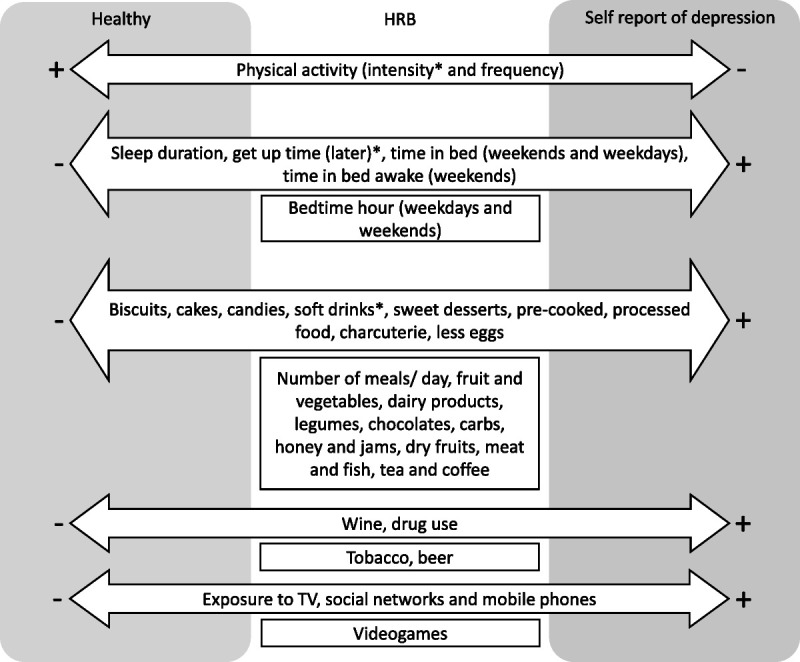
Evaluated HRB during the first outbreak of the COVID-19 pandemic in Portugal and their association to healthy people and people with a self-perception of being depressed. Note. The variables with a predictive risk are marked with an asterisk.
DISCUSSION
With regard to the aim of our study to identify HRB in individuals who reported experiencing depression compared with healthy individuals at the time of the first outbreak of the COVID-19 pandemic in Portugal, we found several differences.
Physical Activity
PA is recommended for prevention and treatment of depressive episodes (Sutherland, 2019), regardless of age or geographic region (de Oliveira et al., 2019; Schuch et al., 2018). However, depression is not associated with a lower opportunity to be physically active (Sutherland, 2019), despite a described bidirectional relationship between exercise and mood (Pascoe and Parker, 2019). Our findings are consistent with current evidence on the benefits of PA against depressive symptoms. Notwithstanding, studies about physical intensity, frequency, and mood during the COVID-19 pandemic are scarce. Caputo and Reichert (2020) reported decreasing levels of PA after social distancing measures were applied and suggested that being physically active may attenuate the mental health burden after the outbreak. Hu et al. (2020) also supported that regular PA during the pandemic could buffer its effects on depression and anxiety after COVID-19. Moreover, in a study of depression in middle-aged and elderly Chinese community samples, moderate PA and lower frequency were associated with lower depression risk in women, whereas a higher risk was observed in men who spent higher frequency and more time in intense PA (Wang et al., 2019). In our sample, intensity of PA (but not frequency) had a significant effect on being healthy. Many of the benefits of PA are thought to stem from optimization of brain-derived neurotrophic factor, particularly in the hippocampus (Phillips et al., 2014), and its antidepressant effects by altering cortisol reactivity and the hypothalamic-pituitary-adrenal axis response (Kandola et al., 2019). It is unclear whether the intensity of PA is related to these pathways. Therefore, future studies should focus on the physiological differences between intensity and frequency of PA and their respective roles on mood.
Sleep
More than a bidirectional relationship between depressed mood and disturbed sleep, recent studies suggest that emotion regulation acts as a moderator of the relationship between sleep and mood (Watling et al., 2017). On the other hand, clinophilia, anhedonia, a tendency to isolation, and insomnia are symptoms of depression that are not infrequently associated with poor sleep habits, namely, spending more time in bed (Reynold et al., 2014). In our study, depressed individuals reported higher sleep duration on both weekdays and weekends, spent more time in bed, and got up later—the latter having a significant association with the depressed group. Time awake in bed was also higher for the depressed group although only with statistical significance for weekends. However, depression is associated with both shortening and lengthening of sleep duration (Reis et al., 2018; Zhai et al., 2015). We hypothesize that experiencing the COVID-19 constriction measures in effect at the time of the questionnaire appliance may have conditioned this aspect: fewer hours or sleep in more active individuals, more hours of sleep-in confined individuals. A recent study about sleep and wake quality for a Portuguese sample during confinement suggested that, to sleep well, each individual should practice positive behaviors and dismiss negative behaviors and attitudes (Paiva et al., 2021).
Diet
Existing evidence suggests that a healthy diet, particularly a Mediterranean diet or with a lower dietary inflammatory index, reduces the risk of depression (Lassale et al., 2019; Molendijk et al., 2018), is linked with better sleep quality, and is a better coping mechanism with the pandemic (Paiva et al., 2021).
To prevent depression, some authors suggest increased consumption of fish, vegetables and fruits (Molendijk et al., 2018), legumes, and whole grains, and limit intake of processed foods and sweets (Opie et al., 2017), processed meat (Gómez-Donoso et al., 2020), butter, and high-fat sauces (Li et al., 2017). A meta-analysis suggests that sugar-sweetened beverages may be associated with a higher risk of depression (Hu et al., 2019). Consistent with this evidence, in our study, depressed individuals reported eating more biscuits and cakes, precooked and processed foods, charcuterie, candies, sweet desserts, and drinking more soft drinks during confinement compared with healthy individuals. The latter was associated with a predictive value (OR, 1.51 [1.07–2.13]; p = 0.020) for increased risk of being depressed. However, another meta-analysis published in the same year concluded that carbohydrates in general had no effect on mood after consumption, despite higher fatigue and reduced alertness in the first hour after ingestion (Mantantzis et al., 2019), which is consistent with our results. Among sweets, chocolate was not associated with depression, as previously reported in the literature (Grases et al., 2019). On the other hand, the association between a low dietary inflammatory index and a lower incidence of depressive symptom does not seem to happen in a dose-response manner, despite differences among healthy food groups, including fruits (Molendijk et al., 2018). We also found that eating fewer eggs was related to being depressed; one of the reasons behind this association might be the protective role of docosahexaenoic acid, a fatty acid present on eggs, despite its low concentration (Horrocks and Yeo, 1999).
Regarding directionality, although depression does not necessarily predict a change in sweets/sugar intake, the opposite is true: sweet foods/drinks seem to have a negative effect on long-term mental health (Knüppel et al., 2017). On the other hand, because inflammation plays a role in depression (Dowlati et al., 2010), dietary fiber from fruits and vegetables may be fermented to short-chain fatty acids, which could regulate the integrity of the intestinal epithelial barrier and thus reduce permeability for proinflammatory factors into the systemic circulation (Taylor and Holscher, 2020). Preclinical studies also show that other pathways besides inflammation, such as oxidative stress, mitochondrial dysfunction, and changes in the gut microbiota, may affect mental health (Marx et al., 2021). However, the evidence for recommending a high fiber diet for the treatment of depressive disorders is still weak. In fact, in our study, the association between fruit, vegetable, and legume consumption and being healthy was not statistically significant.
Overall, we might consider that healthy people report a more healthy and balanced diet in comparison to depressed people. This diet includes less sugar, sweets, and charcuterie, and more eggs. Evidence has supported that poor nutrition may be related to low mood (Cook et al., 2020).
Addictions: Electronics, Cigarettes, Alcoholic Beverages, and Other Drugs
Electronics
Although baseline depression was not associated with higher social media use, baseline social media use is independently associated with later development of depressive symptoms (Lin et al., 2016; Shensa et al., 2018). Frequent social media exposure was also associated with higher risk of depression and anxiety during the COVID-19 pandemic onset (Gao et al., 2020). Low-quality social relationships were associated with depression in university students (Wathelet et al., 2020). Our study is consistent with the findings: the depressed group reported watching more hours of TV, using more social networks and mobile phones, with higher perceived dependence on TV and social networks compared with healthy individuals. It would have been useful to determine the pattern of social media use, as not all patterns are associated with depression or anxiety (Shensa et al., 2018). Despite these conclusions, we must highlight the implications of the internationally cited study by Brooks et al. (2020) (and one of the first studies on COVID-19 pandemic and mental health), which discussed the benefits of social media and mobile phones on isolation and quarantine.
Tobacco
Studies conducted during the pandemic COVID-19 report an association between tobacco and alcohol use and depression (Stanton et al., 2020; Ustun, 2021).
Despite several studies reporting a clear association between tobacco use and mental illness, the literature remains inconsistent regarding the prospective directionality of this association (Fluharty et al., 2017). However, in our study, cigarette use was not associated with either group (healthy or depressed). We believe this conclusion may be based on differences for internalizing (depression, anxiety) and externalizing (conduct, attention and hyperactivity) problems across tobacco products, including initiation of use, and by age, sex, and ethnicity (Green et al., 2018).
Alcoholic Beverages and Other Substances
Regarding alcohol use and general drug use, several epidemiological studies report comorbidities between substance use disorders and other mental problems, including a high proportion of mood disorders (Lai et al., 2015). In our study, despite a higher perceived dependence on alcohol and higher drug use reported by the depressed group, we observed a difference in the type of alcoholic beverage: wine was associated with the depressed group, whereas beer was not.
The study of emotions in relation to wine and beer consumption is poorly described. One possible reason could be the difference in alcohol volume, as alcohol promotes the depressive effects of the neurotransmitter gamma-aminobutyric acid: beer may contain from 0% (nonalcoholic beer) to 6% alcohol by volume (Bamforth, 2002), whereas wine may contain from 8% to 15% alcohol by volume (German and Walzem, 2000; Silva et al., 2017). Wine consumers perceive a dominance of emotional benefits over functional outcomes (Barrena and Sanchez, 2009; Charters and Pettigrew, 2008). Sweetness could be another possible bridge between alcohol and depression (as discussed previously). In addition, wine (either white or red) is perceived as healthier than beer (Wright et al., 2008), partly because of its strong association with meals and therefore health (Silva et al., 2017). However, as far as we know, studies linking mental health and beer are scarce. Beer is mainly perceived for relaxation-oriented and solitary occasions (Charters and Pettigrew, 2006; Silva et al., 2017). Moderate beer consumption may also be beneficial for the endothelial functioning (Spaggiari et al., 2020). Therefore, we believe that the type of alcoholic beverage could be a promising area for research.
In an Australian study on a survey distributed in April 2020, negative change in PA, alcohol, smoking, and sleep was associated with higher risk of depression, stress, and anxiety symptoms since the onset of the COVID-19 pandemic (Stanton et al., 2020). However, in our study, the association between smoking and depression was not statistically significant. Other studies evaluated a change in behaviors in the general population, before and after the onset of the COVID-19 pandemic (Weaver et al., 2021).
General Considerations and Limitations
Limitations of the current study are important to acknowledge. Our study was part of a larger research addressing several questions. As so, we opted to use visual analog scales to provide a broad and multithemed questionnaire with as few questions as possible, not allowing the use of extensive and validated questionnaires. Visual analog scales have a high response rate, have a high completion rate, and are reliable in terms of test-retest and interrater reliability (Brazier and Ratcliffe, 2016). Moreover, one study showed that the simple question “Are you depressed?” had a sensitivity and specificity of 100% in diagnosing major depression in terminally ill patients (Chochinov et al., 1997). Another limitation is that self-reported dietary records may not accurately reflect the amount of food consumed by a participant resulting in underestimated or overestimated scores.
We also found an association between lower educational level and working in health care with depression, which is consistent with current evidence (Wathelet et al., 2020). According to other studies, health care workers have an increased risk of negative mental health outcomes during COVID-19 (Rajkumar, 2020; Solomou and Constantinidou, 2020). Our study also suggested that being a health professional increases the risk of being depressed in both models, being this risk higher when considering perceived additions. Moreover, our results add that HRB might decrease the risk of depression in health professionals, more than perceived addictions.
Most of the patients from our sample have a high education level (62% college graduates and 25% masters in the healthy group; 41.7% college graduates and 25.6% masters in the depressed group) and are female (78.5% in the healthy group; 78.5% in the depressed group), despite nonsignificant differences between groups for age (t[966] = 0.15, p = 0.88). Similar to other studies conducted during the same period, the majority of participants were female (Wathelet et al., 2020). Although with a large size, this nonrepresentative sample stresses the need to be cautious in our conclusions. Some longitudinal studies are already bringing some light about the impact of the COVID-19 on mental health; older adults, for instance, seem to have more adaptive resources (López et al., 2022).
The cross-sectional design of the current study does not allow drawing conclusions about causal relationships between variables or analyze a behavior or condition over time namely the effect of seasons. The nature of our study did not allow us to attribute any of the findings specifically to the pandemic because we are not reporting prepandemic information in this report. Because adding the prepandemic values would have some reporting bias associated (representing more than 1 month before), the authors prefer to perform a group comparison study reporting during lockdown behaviors. Therefore, futures studies are encouraged to conduct longitudinal designs about the consequences of the COVID-19 HRBs on mental health outcomes.
Nonetheless, this study has some strengths. This is the first study to compare HRB, which includes sleep, PA, eating behaviors, addictions, and their respective perceptions, between groups of depressed and healthy individuals. We used a large sample and a propensity score matching for age and sex to control confounding effects. Moreover, our results have important implications for research and clinical practice.
CONCLUSIONS
There are important differences regarding HRB and their relation to a self-perception of depression, regarding PA (less intensity and frequency), sleep (higher sleep duration, more time in bed, getting up later on both weekdays and weekends, time awake in bed during weekends), diet (eating more candies, sweet desserts, biscuits and cakes, precooked and processed foods, charcuterie, soft drinks, and fewer eggs), electronics use (more hours of exposure to TV, social networks, and mobile phones), and substance use (higher wine consumption and drug use). As behavioral activation is an effective strategy against depression (Ekers et al., 2014), knowledge of which HRBs are associated with depression could be an effective intervention target in treating such patients during the pandemic. Considering that addictions were also predictors of depression, interventions could address this issue through motivational interviewing and reinforcement of functional alternative strategies for emotional regulation.
DISCLOSURE
The current study is part of a larger research project approved by CENC’s Ethical Committee 1/2020, taking into account the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
There were no sources of funding, public or private, and no conflict of interest. All participants gave informed consent after being assured of confidentiality and voluntariness of participation. Data availability is controlled by Professor Teresa Paiva, the team leader of the “COVID, Health, Sleep, Habits” group.
The authors declare no conflict of interest.
H.C.S. and C.R. contributed to the data collection, data analysis, manuscript writing, and final review. D.C. contributed to the data analysis, manuscript writing, and final review. P.E.S. contributed to the manuscript writing and final review. T.P. contributed to the study design, final review, and study coordination.
Contributor Information
Cátia Reis, Email: ccreis@ucp.pt.
Diogo Carreiras, Email: diogocarreiras1@gmail.com.
Pedro Espada-Santos, Email: pdsantos@campus.ul.pt.
Teresa Paiva, Email: teresapaiva0@gmail.com.
REFERENCES
- Bamforth CW. (2002) Nutritional aspects of beer—a review. Nutr Res. 22:227–237. [Google Scholar]
- Barrena R, Sanchez M. (2009) Connecting product attributes with emotional benefits: Analysis of a Mediterranean product across consumer age segments. Br Food J. 111:120–137. [Google Scholar]
- Brazier J, Ratcliffe J. (2016) Measurement and Valuation of Health for Economic Evaluation. In International Encyclopedia of Public Health (pp 586–593). Amsterdam, Netherlands: Elsevier. [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. (2020) The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 395:912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caputo EL, Reichert FF. (2020) Studies of physical activity and COVID-19 during the pandemic: A scoping review. J Phys Act Health. 17:1275–1284. [DOI] [PubMed] [Google Scholar]
- Charters S, Pettigrew S. (2006) Conceptualizing product quality: The case of wine. Mark Theory. 6:467–483. [Google Scholar]
- Charters S, Pettigrew S. (2008) Why do people drink wine? A consumer-focused exploration. J Food Prod Mark. 14:13–32. [Google Scholar]
- Chevance A, Gourion D, Hoertel N, Llorca PM, Thomas P, Bocher R, Moro MR, Laprévote V, Benyamina A, Fossati P, Masson M, Leaune E, Leboyer M, Gaillard R. (2020) Ensuring mental health care during the SARS-CoV-2 epidemic in France: A narrative review. Encephale. 46:193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chochinov HM, Wilson KG, Enns M, Lander S. (1997) “Are you depressed?” screening for depression in the terminally ill. Am J Psychiatry. 154:674–676. [DOI] [PubMed] [Google Scholar]
- Cook NR, He FJ, MacGregor GA, Graudal N. (2020) Sodium and health-concordance and controversy. BMJ. 369:m2440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Oliveira LDSSCB, Souza EC, Rodrigues RAS, Fett CA, Piva AB. (2019) The effects of physical activity on anxiety, depression, and quality of life in elderly people living in the community. Trends Psychiatry Psychother. 41:36–42. [DOI] [PubMed] [Google Scholar]
- Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, Lanctôt KL. (2010) A meta-analysis of cytokines in major depression. Biol Psychiatry. 67:446–457. [DOI] [PubMed] [Google Scholar]
- Ekers D, Webster L, Van Straten A, Cuijpers P, Richards D, Gilbody S. (2014) Behavioural activation for depression; An update of meta-analysis of effectiveness and sub group analysis. PLoS One. 9:e100100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. (2020) Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 3:e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fluharty M, Taylor AE, Grabski M, Munafò MR. (2017) The Association of Cigarette Smoking with Depression and Anxiety: A systematic review. Nicotine Tob Res. 19:3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, Wang Y, Fu H, Dai J. (2020) Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 15:e0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaur PS, Zimba O, Agarwal V, Gupta L. (2020) Reporting survey based studies—A primer for authors. J Korean Med Sci. 35:e398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- German JB, Walzem RL. (2000) The health benefits of wine. Annu Rev Nutr. 20:561–593. [DOI] [PubMed] [Google Scholar]
- Gómez-Donoso C, Sánchez-Villegas A, Martínez-González MA, Gea A, Mendonça RD, Lahortiga-Ramos F, Bes-Rastrollo M. (2020) Ultra-processed food consumption and the incidence of depression in a Mediterranean cohort: The SUN project. Eur J Nutr. 59:1093–1103. [DOI] [PubMed] [Google Scholar]
- Grases G, Colom MA, Sanchis P, Grases F. (2019) Possible relation between consumption of different food groups and depression. BMC Psychol. 7:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green VR, Conway KP, Silveira ML, Kasza KA, Cohn A, Cummings KM, Stanton CA, Callahan-Lyon P, Slavit W, Sargent JD, Hilmi N, Niaura RS, Reissig CJ, Lambert E, Zandberg I, Brunette MF, Tanski SE, Borek N, Hyland AJ, Compton WM. (2018) Mental health problems and onset of tobacco use among 12- to 24-year-olds in the PATH study. J Am Acad Child Adolesc Psychiatry. 57:944–954.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. (2004) SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 10:1206–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horrocks LA, Yeo YK. (1999) Health benefits of docosahexaenoic acid (DHA). Pharmacol Res. 40:211–225. [DOI] [PubMed] [Google Scholar]
- Hu D, Cheng L, Jiang W. (2019) Sugar-sweetened beverages consumption and the risk of depression: A meta-analysis of observational studies. J Affect Disord. 245:348–355. [DOI] [PubMed] [Google Scholar]
- Hu S, Tucker L, Wu C, Yang L. (2020) Beneficial effects of exercise on depression and anxiety during the COVID-19 pandemic: A narrative review. Front Psychiatry. 11:587557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huremović D. (2019) Psychiatry of pandemics: A mental health response to infection Outbreak. Gewerbestrasse, Switzerland: Springer Nature. [Google Scholar]
- James SL Abate D Abate KH Abay SM Abbafati C Abbasi N Abbastabar H Abd-Allah F Abdela J Abdelalim A Abdollahpour I Abdulkader RS Abebe Z Abera SF Abil OZ Abraha HN Abu-Raddad LJ Abu-Rmeileh NME Accrombessi MMK Murray CJL, GBD 2017 Disease and Injury Incidence and Prevalence Collaborators (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the global burden of disease study 2017. Lancet. 392:1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B. (2019) Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity. Neurosci Biobehav Rev. 107:525–539. [DOI] [PubMed] [Google Scholar]
- Kline RB. (2011) Principles and Practice of Structural Equation Modeling. New York, NY: Guilford Press. [Google Scholar]
- Knüppel A, Shipley MJ, Llewellyn CH, Brunner EJ. (2017) Sugar intake from sweet food and beverages, common mental disorder and depression: Prospective findings from the Whitehall II study. Sci Rep. 7:6287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai HMX, Cleary M, Sitharthan T, Hunt GE. (2015) Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug Alcohol Depend. 154:1–13. [DOI] [PubMed] [Google Scholar]
- Lassale C, Batty GD, Baghdadli A, Jacka F, Sánchez-Villegas A, Kivimäki M, Akbaraly T. (2019) Healthy dietary indices and risk of depressive outcomes: A systematic review and meta-analysis of observational studies. Mol Psychiatry. 24:965–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Lv MR, Wei YJ, Sun L, Zhang JX, Zhang HG, Li B. (2017) Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 253:373–382. [DOI] [PubMed] [Google Scholar]
- Lin LY, Sidani JE, Shensa A, Radovic A, Miller E, Colditz JB, Hoffman BL, Giles LM, Primack BA. (2016) Association between social media use and depression among U.S. Young adults. Depress Anxiety. 33:323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López J, Perez-Rojo G, Noriega C, Martinez-Huertas JA, Velasco C. (2022) Emotional distress among older adults during the COVID-19 outbreak: Understanding the longitudinal psychological impact of the COVID-19 pandemic. Psychogeriatrics. 22:77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallet J, Dubertret C, Le Strat Y. (2021) Addictions in the COVID-19 era: Current evidence, future perspectives a comprehensive review. Prog Neuropsychopharmacol Biol Psychiatry. 106:110070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantantzis K, Schlaghecken F, Sünram-Lea SI, Maylor EA. (2019) Sugar rush or sugar crash? A meta-analysis of carbohydrate effects on mood. Neurosci Biobehav Rev. 101:45–67. [DOI] [PubMed] [Google Scholar]
- Marjanovic Z, Greenglass ER, Coffey S. (2007) The relevance of psychosocial variables and working conditions in predicting nurses’ coping strategies during the SARS crisis: An online questionnaire survey. Int J Nurs Stud. 44:991–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx W, Lane M, Hockey M, Aslam H, Berk M, Walder K, Borsini A, Firth J, Pariante CM, Berding K, Cryan JF, Clarke G, Craig JM, Su KP, Mischoulon D, Gomez-Pinilla F, Foster JA, Cani PD, Thuret S, Staudacher HM, Jacka FN. (2021) Diet and depression: Exploring the biological mechanisms of action. Mol Psychiatry. 26:134–150. [DOI] [PubMed] [Google Scholar]
- Moghanibashi-Mansourieh A. (2020) Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr. 51:102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molendijk M, Molero P, Ortuño Sánchez-Pedreño F, Van der Does W, Angel Martínez-González M. (2018) Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. J Affect Disord. 226:346–354. [DOI] [PubMed] [Google Scholar]
- Opie RS, Itsiopoulos C, Parletta N, Sanchez-Villegas A, Akbaraly TN, Ruusunen A, Jacka FN. (2017) Dietary recommendations for the prevention of depression. Nutr Neurosci. 20:161–171. [DOI] [PubMed] [Google Scholar]
- Paiva T, Reis C, Feliciano A, Canas-Simião H, Machado MA, Gaspar T, Tomé G, Branquinho C, Silva MS, Ramiro L. (2021) Sleep and awakening quality during COVID-19 confinement: Complexity and relevance for health and behavior. Int J Environ Res Public Health. 18:3506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe MC, Parker AG. (2019) Physical activity and exercise as a universal depression prevention in young people: A narrative review. Early Interv Psychiatry. 13:733–739. [DOI] [PubMed] [Google Scholar]
- Phillips C, Baktir MA, Srivatsan M, Salehi A. (2014) Neuroprotective effects of physical activity on the brain: A closer look at trophic factor signaling. Front Cell Neurosci. 8:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar RP. (2020) COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr. 52:102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis C, Dias S, Rodrigues AM, Sousa RD, Gregório MJ, Branco J, Canhão H, Paiva T. (2018) Sleep duration, lifestyles and chronic diseases: A cross-sectional population-based study. Sleep Science. 11:217–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynold AM, Bowles ER, Saxena A, Fayad R, Youngstedt SD. (2014) Negative effects of time in bed extension: A pilot study. J Sleep Med Disord. 1:1002. [PMC free article] [PubMed] [Google Scholar]
- Reynolds DL, Garay JR, Deamond SL, Moran MK, Gold W, Styra R. (2008) Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. 136:997–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, Rasoulpoor S, Khaledi-Paveh B. (2020) Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Global Health. 16:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, Hallgren M, Ponce De Leon A, Dunn AL, Deslandes AC, Fleck MP, Carvalho AF, Stubbs B. (2018) Physical activity and incident depression: A meta-analysis of prospective cohort studies. Am J Psychiatry. 175:631–648. [DOI] [PubMed] [Google Scholar]
- Shensa A, Sidani JE, Dew MA, Escobar-Viera CG, Primack BA. (2018) Social media use and depression and anxiety symptoms: A cluster analysis. Am J Health Behav. 42:116–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva AP, Jager G, Van Zyl H, Voss HP, Pintado M, Hogg T, De Graaf C. (2017) Cheers, proost, saúde: Cultural, contextual and psychological factors of wine and beer consumption in Portugal and in the Netherlands. Crit Rev Food Sci Nutr. 57:1340–1349. [DOI] [PubMed] [Google Scholar]
- Solomou I, Constantinidou F. (2020) Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: Age and sex matter. Int J Environ Res Public Health. 17:4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaggiari G, Cignarelli A, Sansone A, Baldi M, Santi D. (2020) To beer or not to beer: A meta-analysis of the effects of beer consumption on cardiovascular health. PloS One. 15:e0233619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, Fenning AS, Vandelanotte C. (2020) Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 17:4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland ME. (2019) Physical activity and depression. Nat Hum Behav. 3:320. [DOI] [PubMed] [Google Scholar]
- Taylor AM, Holscher HD. (2020) A review of dietary and microbial connections to depression, anxiety, and stress. Nutr Neurosci. 23:237–250. [DOI] [PubMed] [Google Scholar]
- Ustun G. (2021) Determining depression and related factors in a society affected by COVID-19 pandemic. Int J Soc Psychiatry. 67:54–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang R, Bishwajit G, Zhou Y, Wu X, Feng D, Tang S, Chen Z, Shaw I, Wu T, Song H, Fu Q, Feng Z. (2019) Intensity, frequency, duration, and volume of physical activity and its association with risk of depression in middle- and older-aged Chinese: Evidence from the China health and retirement longitudinal study, 2015. PLoS One. 14:e0221430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, Debien C, Molenda S, Horn M, Grandgenèvre P, Notredame CE, D'Hondt F. (2020) Factors associated with mental health disorders Among University students in France confined during the COVID-19 pandemic. JAMA Netw Open. 3:e2025591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watling J, Pawlik B, Scott K, Booth S, Short MA. (2017) Sleep loss and affective functioning: More than just mood. Behav Sleep Med. 15:394–409. [DOI] [PubMed] [Google Scholar]
- Weaver RH, Jackson A, Lanigan A, Power TG, Anderson A, Cox AE, Eddy L, Parker L, Sano Y, Weybright E. (2021) Health behaviors at the onset of the covid-19 pandemic. Am J Health Behav. 45:44–61. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2017) Depression and Other Common Mental Disorders: Global Health Estimates. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Wright CA, Bruhn CM, Heymann H, Bamforth CW. (2008) Beer consumers’ perceptions of the health aspects of alcoholic beverages. J Food Sci. 73:12–17. [DOI] [PubMed] [Google Scholar]
- Zhai L, Zhang H, Zhang D. (2015) Sleep duration and depression among adults: A meta-analysis of prospective studies. Depress Anxiety. 32:664–670. [DOI] [PubMed] [Google Scholar]


