Abstract
Objectives
Increased exposure to digital devices as part of online classes increases susceptibility to visual impairments, particularly among school students taught using e-learning strategies. This study aimed to identify the impact of remote learning during the COVID-19 lockdown on children’s visual health.
Design
Systematic review using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Data sources
Scopus, PubMed and ScienceDirect databases from the year 2020 onwards.
Eligibility criteria
We included cross-sectional, case–control, cohort studies, case series and case reports, published in English, Spanish or French, that approached the effects of remote learning during the COVID-19 lockdown on visual health in neurotypical children.
Data extraction and synthesis
We included a total of 21 articles with previous quality assessments using the Joanna Briggs checklist. Risk of bias assessment was applied using the National Institutes of Health quality assessment tool for before-and-after studies with no control group; the tool developed by Hoy et al to assess cross-sectional studies; the Murad et al tool to evaluate the methodological quality of case reports and case series; and the Newcastle-Ottawa Scale for cohort studies.
Results
All but one study reported a deleterious impact of the COVID-19 lockdown on visual health in children. Overall, the most frequently identified ocular effects were refractive errors, accommodation disturbances and visual symptoms such as dry eye and asthenopia.
Conclusions
Increased dependence on digital devices for online classes has either induced or exacerbated visual disturbances, such as rapid progression of myopia, dry eye and visual fatigue symptoms, and vergence and accommodation disturbances, in children who engaged in remote learning during the COVID-19 lockdown.
PROSPERO registration number
CRD42022307107.
Keywords: COVID-19, paediatrics, paediatric ophthalmology
Strengths and limitations of this study.
A systematic review was conducted in three different databases, studies were filtered following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Analysed studies approached the effects of remote learning during the COVID-19 lockdown on visual health in children.
To facilitate comparison, eligible studies were clustered according to the main ocular effects evaluated, including refractive errors (myopia), accommodation disturbances (esotropia) and visual symptoms (dry eye and fatigue).
We used quality assessment guidelines and specific risk of bias assessment tools for each study design included.
Heterogeneous methods used in each study, including both subjective and objective measures, limit precise comparisons between them.
Introduction
Since the WHO declared a global pandemic in March 2020, COVID-19 has become the focus of governmental decisions aimed at protecting the public and limiting the death toll. Schools, universities and businesses have been forced to close to prevent the spread of the virus, limiting in-person relationships and substantially enhancing our digital dependence. The lifestyle and behavioural modifications that have emerged in response to the lockdowns have affected approximately 80% of the world’s student population.1 2
The establishment of in-house quarantine led to a significant decrease in the amount of time spent engaged in outdoor activities, reduction in exposure to sunlight and increase in time spent doing near work. These factors can enhance the risk of visual impairments, especially among school and university students encouraged to adopt a digital learning approach.3 A growing dependence on e-learning and electronic devices has increased the incidence of visual fatigue, the onset and progression of myopia, dry eye, irregular astigmatism and acute concomitant esotropia among other ocular pathologies.4
Even before the COVID-19 pandemic, an estimated 22.9% of the global population had myopia.5 During the COVID-19 lockdown, the increased need for electronic devices, digital screens and virtual classrooms might have caused previously healthy students to develop myopia, and faster progression in those who already had impaired vision. Obligatory confinement, intensive near work activities and decreased exposure to sunlight can lead to visual fatigue, and may also enhance the risk of myopia, the most prevalent ocular condition.4
Digital screen use is considered a common risk factor for dry eye, characterised by the deterioration of tear film quality. The risk of dry eye and symptom severity can be exacerbated by increased digital screen time.6–8 Myopia and dry eye are potential visual health consequences associated with the increasing demand for children to engage in e-learning, which often starts at a very young age. To address this in the present systematic review, we sought to identify the impact of remote learning during the COVID-19 pandemic on visual health in school-age children.
Methods
Search strategy and selection criteria
In January 2022, we conducted a systematic review using three online databases. We used the following terms in PubMed: (https://pubmed.ncbi.nlm.nih.gov/advanced/) (((((vision) OR (visual impairment)) OR (myopia [MeSH Terms])) AND (COVID-19)) AND (lockdown)) AND (screen time); ScienceDirect: (https://www.sciencedirect.com/search) ((vision) OR (visual impairment) OR (myopia)) AND ((COVID-19 lockdown)) AND (screen time)); and Scopus: (https://www.scopus.com) ALL (vision OR (‘visual’ AND ‘impairment’) OR myopia AND (‘COVID-19’ AND ‘lockdown’) AND (‘screen’ AND ‘time’)) AND (LIMIT-TO (SUBJAREA, ‘MEDI’) OR LIMIT-TO (SUBJAREA, ‘COMP’) OR LIMIT-TO (SUBJAREA, ‘NEUR’) OR LIMIT-TO (SUBJAREA, ‘NURS’) OR LIMIT-TO (SUBJAREA, ‘HEAL’)). The ID CRD42022307107 was generated in the International Prospective Register of Systematic Reviews (PROSPERO).
Data collection
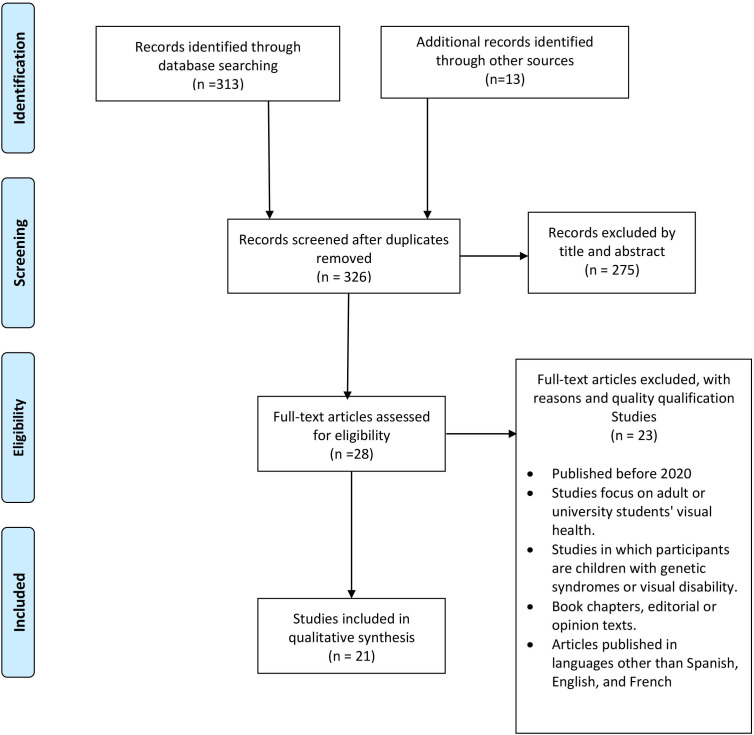
A total of 326 articles were initially retrieved. Duplicates were removed, and the remaining articles were filtered by title and abstract following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (figure 1 and online supplemental table 1). Five researchers divided into two groups screened all of the articles, and 28 were selected for study inclusion. At weekly meetings, the authors analysed the studies, debated disagreements and double-checked all of the articles according to the inclusion and exclusion criteria. Articles were included if they described studies on the effects of remote learning during the COVID-19 lockdown on visual health in neurotypical children. They were excluded if they (1) were published before 2020; (2) studied the effects of remote learning during the COVID-19 lockdown on visual health in adults or university students; (3) assessed children with genetic syndromes or visual disabilities; (4) were book chapters, editorials or opinion pieces; and (5) were published in languages other than Spanish, English and French. Following this procedure, a total of 21 articles were included. These were evaluated using Joanna Briggs checklist to guarantee study quality. Additionally, we conducted a risk of bias assessment using several tools. First, we used the National Institutes of Health quality assessment tool for before-and-after (pre-post) studies with no control group.9 This instrument evaluates 12 major components with response options of yes/no/not applicable/cannot determine/not reported and gives a final quality rating of good, poor or fair depending on the overall item response.9 Second, we used the tool developed by Hoy et al to assess cross-sectional studies by categorising the article bias as low, moderate or high risk according to responses to 10 questions.10 11 Third, we used the tool proposed by Murad et al to evaluate the methodological quality of case reports and case series. This tool appraises the selection, ascertainment, causality and reporting bias of each article and makes an overall judgement about the methodology based on the responses to eight questions.12 Finally, we used the Newcastle-Ottawa Scale for cohort studies to assess the selection, comparability and outcome bias of the article by applying a qualitative star scale.9 All domains evaluated using these tools can be found in online supplemental table 2.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (adapted from Moher et al.52
bmjopen-2022-062388supp001.pdf (39.8KB, pdf)
bmjopen-2022-062388supp002.pdf (74.6KB, pdf)
Finally, we extracted data to obtain the following information: title, authors, digital object identifier number, objective, type of study, country in which the study was conducted, population (age and sample), presence of control group (age and sample), implemented test or evaluation methodology, main visual outcome, results, conclusion and answers to the question ‘Did the COVID-19 lockdown impact visual health (improvement, deterioration, no change)?’ All information was synthesised using qualitative and quantitative synthesis (see the Results section). Considering the heterogeneity among studies, we created subgroups for analysis, for example, studies regarding dry eye, refractive errors, clinical symptoms and other clusters. All investigators participated in the data collection and synthesis.
Patient and public involvement
This research was done without patient or public involvement. However, the findings will be shared at conferences attended by paediatric ophthalmologists and patients with myopia who access ophthalmological services.
Results
We grouped the articles included in the review based on the main visual outcome associated with vision status and changes in vision in children during the COVID-19 lockdown. Overall, the main ocular effects observed were refractive errors (myopia), accommodation disturbances (esotropia) and visual symptoms (dry eye and fatigue) (table 1). Among the studies, 16 were conducted in Asia,13–28 2 in Europe29 30 and 3 in America.31 32 The risk of bias assessment revealed that all of the cross-sectional studies and case series had a low risk of bias. Three of the before-and-after studies had fair quality, and one had good quality.
Table 1.
Articles related to visual outcomes and the impact of remote learning during the COVID-19 pandemic
| Title | Authors | Year | Type of study | Country of the study | Results | Is there an effect of COVID-19 lockdown on visual health? |
| Comparison of myopic progression before, during, and after COVID-19 lockdown | Chang et al15 | 2021 | Before-and-after study | China | Proportions of myopia and high myopia: Round 1: 48.0% and 1.3% Round 2 : 53.2% and 1.9% Round 3: 73.7% and 2.8% Round 4: 67.9% and 2.7% Mean rDSER: Period 1: −0.030 D/month (95% CI e0.031 to e0.029) Period 2 (lockdown): −0.074 D/month (95% CI e0.075 to e0.074) Period 3: 0.016 D/month (95% CI 0.015 to e0.018) |
Worsen |
| Impact of COVID-19 home confinement in children’s refractive errors | Alvarez-Peregrina et al30 | 2021 | Cross-sectional | Spain | Spherical equivalent: Average value in 2019: +0.66±2.03 D Average value in 2020: +0.48±1.81 D Children’s lifestyle during confinement: 56% changed the amount of time spent outdoors (95% CI 53% to 58%). 47% (95% CI 45% to 50%; p<0.001) of the cases decreased this time. Children’s near vision during confinement: 49% changed the amount of time they spent doing near distance activities (95% CI 47% to 52%). 44% (95% CI 41% to 46%; p<0.001) of the children increased near distance activities. 42% of the children changed the amount of time they spent with electronic devices (95% CI 40% to 45%). 39% (95% CI 37% to 42%; p<0.001) of cases increase electronic use. Children who spent more time outdoors had higher SE in preconfinement and postconfinement (p<0.001 and p=0.049). |
Worsen |
| Objective and subjective behavioral measures in myopic and non-myopic children during the COVID-19 pandemic | Mirhajianmoghadam et al32 | 2021 | Cross-sectional | USA |
|
Unclear |
| Progression of myopia in school-aged children after COVID-19 home confinement | Wang et al17 | 2021 | Prospective cross-sectional | China | Mean SER:
Prevalence of myopia:
|
Worsen |
| Survey on the progression of myopia in children and adolescents in Chongqing during COVID-19 pandemic | Wang et al19 | 2021 | Before-and-after study | China | Myopia prevalence among teenagers:
Average progression rate: 10.49% Spherical equivalent:
Myopia percentage was 84.89% in high school, 73.39% in junior school and 39.27% in primary school. |
Worsen |
| The effect of home education on myopia progression in children during the COVID-19 pandemic | Aslan and Sahinoglu-Keskek20 | 2022 | Before-and-after study | Turkey | Mean duration spent in front of the screen was 5.77±1.34 hours/day. The mean SER were:
The mean myopic progression in 2020:
The myopia progression in 2020 was slow (0.31±0.2 D) in 42.6% of the subjects, moderate (0.82±0.14 D) in 39.1% and rapid (1.42±0.29 D) in 18.3%. No correlation was found between the 2020 progression and the daily digital device use. |
Worsen |
| The impact of COVID-19 home confinement on axial length in myopic children undergoing orthokeratology | Lv et al21 | 2022 | Before-and-after study | China | Monthly axial length growth:
The monthly axial length growth after and before confinement was not significantly different (p=0.333). |
Remains the same |
| The impact of study-at-home during the COVID-19 pandemic on myopia progression in Chinese children | Ma et al22 | 2021 | Cohort | China | Myopia progression: p<0.001
In the exposed group, children had a larger change in myopia progression in the follow-up period (−0.83±0.56 D) compared with the baseline period (−0.33±0.46 D; p<0.001). Increment on near work time from 2.96±1.05 to 4.33±1.04 hours/day (p<0.001) during COVID-19. Decrease on outdoor activities from 1.84±1.43 to 0.98±1.01 hours/day (p<0.001) during COVID-19. |
Worsen |
| COVID-19 quarantine reveals that behavioral changes have an effect on myopia progression | Xu et al23 | 2021 | Before-and-after study | China | Myopia prevalence:
Increase in myopia prevalence:
Half-year incidence rate of myopia:
|
Worsen |
| Rates of myopia development in young Chinese schoolchildren during the outbreak of COVID-19 | Hu et al24 | 2021 | Cohort | China | The mean AL was 0.11 mm (95% CI 0.05 to 0.16). Exposed group:
|
Worsen |
| Impact of online classes and home confinement on myopia progression in children during COVID-19 pandemic: Digital Eye Strain among Kids (DESK study 4) | Mohan et al28 | 2022 | Cross-sectional | India | Myopia progression report:
|
Worsen |
| Acute acquired concomitant esotropia from excessive application of near vision during the COVID-19 lockdown | Vagge et al29 | 2020 | Case series | Italy |
|
Worsen |
| Binocular accommodation and vergence dysfunction in children attending online classes during the COVID-19 pandemic: Digital Eye Strain in Kids (DESK study-2) | Mohan et al13 | 2021 | Cross-sectional | India | Mean CISS scores:
Mean values of near exophoria (p=0.03), NFV (p=0.02), NRA (p=0.057) and AA (p=0.002). Spearman correlation between CISS score and the duration of online classes: weak linear association (coefficient rs=0.39, p=0.007). |
Worsen |
| The visual consequences of virtual school: acute eye symptoms in healthy children | Hamburger et al33 | 2022 | Cross-sectional | USA | CISS score:
The asthenopia score:
|
Worsen |
| Series of cases of acute acquired comitant esotropia in children associated with excessive online classes on smartphone during COVID-19 pandemic; Digital Eye Strain among Kids (DESK study-3) | Mohan et al27 | 2021 | Case series | India |
|
Worsen |
| Relationship between screen time and dry eye symptoms in pediatric population during the COVID-19 pandemic | Elhusseiny et al18 | 2021 | Cross-sectional | Egypt | m-SPEED questionnaire score:
Screen time:
|
Worsen |
| New indicator of children’s excessive electronic screen use and factors in meibomian gland atrophy | Cremers et al31 | 2021 | Cross-sectional | USA | CHESUD:
Severe MGA related to:
CHESUD’s positive association with the increase in combined meibography scores (OR=2.81; 95% CI 1.66 to 4.77). |
Worsen |
| Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: Digital Eye Strain among Kids (DESK study-1) | Mohan et al14 | 2021 | Cross-sectional | India | During the COVID-19:
Before COVID-19:
Survey report:
|
Worsen |
| Impact of e-schooling on digital eye strain in coronavirus disease era: a survey of 654 students | Gupta et al16 | 2021 | Cross-sectional | India | Asthenopia and dry eye symptoms:
Digital device use: <4 hours: 30 (12.5%) children, 5–6 hours: 13 (6.6%) children, >6 hours: 4 (2.3%) children, had not reported any AS (p=0.001). Computer vision syndrome score: CVS score was statistically significantly lower in the group aged 5–7 years versus the group aged 11–16 years (p=0.004). |
Worsen |
| Prevalence of self-reported symptoms of computer vision syndrome and associated risk factors among school students in China during the COVID-19 pandemic | Li et al26 | 2021 | Cross-sectional | China | 53% used glasses, 47% myopia, 2.9% myopia, 2.1% hyperopia, 13% astigmatism, 0.8% amblyopia, 0.7% anisometropia, 1.5% strabismus, 2.5% conjunctivitis, 1.7% previous eye surgery. Mean screen time 4.6 hours/day, 1.2 hours/day on outdoor activities, 9.9 hours/day on sleep. Self-reported symptoms: 13% double vision, 48% itching, eye dryness.
|
Worsen |
| Contribution of total screen/online-course time to asthenopia in children during COVID-19 pandemic via influencing psychological stress | Li et al25 | 2021 | Cross-sectional | China | 63.1% had myopia, 36% had astigmatism and 12.1% reported asthenopia. Students with asthenopia had longer screen/online-course time and less daily rest time. A 100-hour increment was associated with an increased risk of asthenopia at 9% (OR=1.09) and 11% (OR=1.11). |
Worsen |
AA, accommodative amplitude; AL, axial length; AS, asthenopic symptoms; CHESUD, cumulative hours of electronic screen use per day; CISS, Convergence Insufficiency Symptom Survey; CVS, computer vision syndrome; DED, Dry eye disease; DES, Digital eye strain; MGA, Meibomian gland atrophy; m-SPEED, modified Standardized Patient Evaluation of Eye Dryness questionnaire; NFV, negative fusional weakness; NRA, negative relative accommodation; PD, prism dioptre; rDSER, rate of SER change; SER, spherical equivalent refraction.
We identified 11 articles that examined refractive errors related to virtual learning during the COVID-19 lockdown. Most of these examined myopia progression as the main visual outcome. Eight studies reported that myopia worsened throughout the COVID-19 lockdown in children and teenagers between 5 and 18 years old.15 17 19 21–24 27 One study reported a significant decrease in spherical equivalent refraction (SER) in children with hyperopia and emmetropia (see table 2, Glossary).30 Interestingly, a study evaluating axial length in myopic children undergoing orthokeratology (see table 2, Glossary) did not find any change in myopia progression after lockdown.21 Furthermore, one study focused on risk factors and behavioural changes during the COVID-19 lockdown in terms of myopia found that all children had changes in near work time, electronic device use and outdoor time. However, myopic children had a significantly lower level of daily light exposure compared with non-myopic children.32 The monthly extent of myopia progression during the COVID-19 lockdown was reported to be –0.074 D/month, which corresponds to an annual progression in 2020 of –0.71±0.46 D.15 20 Furthermore, rapid myopia progression was reported in a sample of 133 school students. Specifically, the percentage of children with reported annual progression for whom progression was rapid increased from 10.5% before to 45.9% during the pandemic.27 SER was estimated in several studies. In 2020, the mean SER in myopic children and teenagers was between −1.94±2.13 D and −2.7±1.21 D, and this was significantly lower than in 2019 (−1.64±5.49 D and −1.99±1.04 D, p<0.001).19 20 Similarly, there was a significant decrease in the mean SER of hyperopic and emmetropic children from 2019 to 2020, that is, 0.66±2.03 D (2019) and 0.48±1.81 D (2020), respectively, p≤0.001.30 Finally, studies examining virtual learning during the COVID-19 lockdown as an exposure risk factor found a higher incidence of myopia in children who engaged in virtual learning (p<0.01).22–24
Table 2.
Glossary
| Term | Definition |
| Accommodation | Contraction of the ciliary muscle resulting in a change of lens shape.53 |
| Asthenopia | Subjective symptoms of ocular fatigue or eye strain.53 |
| Astigmatism | Type of refractive error due to imperfection in the curvature of the eye that causes blurred distance and near vision.54 |
| Cycloplegic refraction | A technique used to calculate the complete refractive error by temporarily paralysing the ciliary muscle of the eye that aids in focusing.53 |
| Diplopia | Disorder of vision in which two images of a single object are seen.53 |
| Dry eye | Alteration of ocular surface homeostasis characterised by an alteration of the tear film. |
| Emmetropia | Refractive state of an eye in which parallel rays of light entering the eye are focused on the retina, creating an image that is perceived as crisp and in focus.55 |
| Esotropia | Eye misalignment in which one eye is deviated inward, or nasally.54 |
| Hyperopia | Ocular condition in which the refracting power of the eye causes light rays entering the eye to have a focal point that is posterior to the retina while accommodation is maintained in a state of relaxation.54 |
| Myopia | Ocular condition in which the refracting power of the eye causes light rays entering the eye to have a focal point that is anterior to the retina while accommodation is maintained in a state of relaxation.54 |
| Orthokeratology | Use of specially designed and fitted contact lenses to temporarily reshape the cornea to improve vision.56 |
| Refractive errors | Type of vision problem that makes it hard to see clearly and happens when the shape of your eye keeps light from focusing correctly on your retina.55 |
| Spherical equivalent refraction | Estimate of the eyes’ refractive error, calculated independently for each eye. It is calculated by merging the spherical (near-sightedness or far-sightedness) and cylindrical (astigmatism) refractive error components.54 |
| Vergence | The turning motion of the eyeballs towards (convergence) or away (divergence) from each other.53 |
Four studies reported accommodation and vergence dysfunction (see table 2, Glossary) secondary to near work and increased screen use time.13 26 29 33 Two studies focused on binocular accommodation in a sample of 156 children aged 10–17 years and reported a significant increase in Convergence Insufficiency Symptom Survey (CISS) scores after exposure to longer screen time during online classes.11 29 The other two were case series of children who developed acquired concomitant esotropia and vergence abnormalities secondary to the excessive use of digital devices.27 29
Emerging visual symptoms were identified in six studies with populations ranging from 8 to 20 years old. The studies reported worsening of visual symptoms such as vision impairment, asthenopia, dryness, scratchiness, headache, eye redness, eye strain and light sensitivity, among others.14 16 18 25 26 33
Overall, the results of qualitative data syntheses showed a negative effect of the COVID-19 lockdown on visual health in children. Only one of the articles included did not report a deleterious impact of the lockdown on vision.21
Discussion
Most of the studies included in this systematic review showed some degree of worsening in visual health in children exposed to virtual learning strategies during the COVID-19 lockdown. The majority of the articles focused on myopia development and progression, and reported a faster onset and progression following the beginning of the lockdown. Also, prolonged exposure to screens was associated with worsened ocular symptoms such as eye strain, blurred vision and redness, as well as an increase in the rate of dry eye, which is traditionally considered to be uncommon in the paediatric population.
Refractive errors
The COVID-19 lockdown impacted the behaviour and daily life of children and teenagers, resulting in increased digital time, near work and decreased outdoor time.34 It is estimated that close to 1.37 billion students worldwide switched to a digital or e-learning school modality during the lockdown.34 These changes have been related to an increase in myopia incidence and progression.34 First, the relationship between near work, especially near reading, and myopia was well established before the COVID-19 pandemic, as stated in the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error Study.34 35 Second, several studies have focused on screen time and its association with myopia development.34 36 37 Third, outdoor time has been considered a protective factor against myopia onset. He et al showed a 23% reduction in myopia incidence after 40 min of outdoor time daily.34 38
During the COVID-19 pandemic in 2020, Mirhajianmoghadam et al assessed subjective and objective measures in 14 myopic and 39 non-myopic children in the USA.32 Initially, parents completed the University of Houston Near Work, Environment, Activity, and Refraction survey in three sessions. The first session included questions related to summer 2020, which was during the COVID-19 pandemic. The second session served to collect data about a typical school period before the COVID-19 pandemic, and the goal of the third session was to collect data about a typical summer period before the pandemic. Later, the investigators used an actigraph device to measure physical activity, sleep and ambient illumination exposure (time spent outdoors) in children for 10 days. The results indicated that all of the children spent less time outdoors during the summer of the pandemic (2020) compared with before the lockdown and showed an increase in daily electronic device use. Furthermore, myopic children had less daily light exposure (183.6±39.3 lux) and spent less time outdoors (0.2 hours/day) during COVID-19 compared with non-myopic children (279.5±23.5 lux, p=0.04).32
The authors of several previous studies have proposed that increased time spent using digital devices is associated with decreased time spent outdoors and impaired retinal dopamine release, which is normally stimulated by daylight exposure. This suppresses axial expansion of the eye, preventing myopia progression.39 40 For instance, Wu et al reported that children who spent more than 11 hours/week outdoors had a 53% decrease in myopia progression,41 and Ip et al reported an increased incidence of progression in children living in apartment buildings compared with those living in detached houses.42 Additionally, Xu et al found that the amount of time spent online was significantly positively associated with an increased incidence of myopia and progression in students.23 However, not all studies have shown this correlation.20 Aslan and Sahinoglu-Keskek reported that myopia advancement in 2020 was mainly slow (0.31±0.2 D) in most of the children evaluated (49 subjects), followed by moderate progression in 45 children (0.82±0.14 D). The authors found no correlation between myopia progression and digital device time or glasses use.20 Thus, the relationship between myopia progression and digital device use requires further investigation.
The studies by Mirhajianmoghadam et al and Aslan and Sahinoglu-Keskek support the findings of myopia progression during the COVID-19 lockdown. For example, Chang et al compared myopic progression before, during and after the COVID-19 lockdown in 44 187 students in China by assessing non-cycloplegic autorefraction and the SER.15 Four evaluation rounds separated by 6 months during 2019 and 2020 indicated a transitory period of accelerated myopic progression in children that reversed after the lockdown. The mean SER during the prepandemic assessment was –0.030 D/month, shortly after the lockdown was –0.074 D/month and later during the lockdown was 0.016 D/month. The proportion of myopic participants was 48% before the lockdown, 45.2% at a second assessment before the lockdown, 73.7% shortly after the lockdown and 67.9% later after the lockdown during rounds 1, 2, 3 and 4, respectively. The authors considered the influence of accommodative spasms and structural changes related to restricted outdoor time, increased screen time and limited indoor space to be the leading cause of the progression. Moreover, they found that younger children were at a higher risk of myopic progression during the lockdown because their lifestyle changes were strongly associated with reduced light exposure, and accordingly, reduced retinal dopamine levels.15
This is concordant with the findings of Wang et al, who reported a substantial decrease in the SER after COVID-19 home confinement, especially for children aged 6 (−0.32 D), 7 (–0.28 D) and 8 (−0.29 D) years, p<0.05.17 Furthermore, they found myopia development to occur earlier in girls than boys. The prevalence of myopia appeared to be approximately 3 times higher in 2020 than in other years for children aged 6 years, 2 times higher for children aged 7 years and 1.4 times higher for those aged 8 years. This led the authors to hypothesise that younger children are more sensitive to environmental changes than older children.17 Furthermore, Wang et al reported a prevalence of myopia of 39.27% in primary school students, 73.39% in junior school students and 84.89% in high school students, identifying an increase in the rate of myopia among teenagers in 2020 (55.02%) compared with that in 2019 (44.64%).19
Lv et al investigated the potential impacts of home confinement on myopia progression from the perspective of axial growth length in children undergoing orthokeratology treatment.21 They found a monthly axial growth length of 0.023±0.019 mm/month, 0.018±0.021 mm/month and 0.014±0.016 mm/month before, during and after home confinement, respectively. However, the monthly axial growth length before confinement was not significantly different from that after confinement (p=0.333), although age was negatively associated with the axial length growth rate during confinement in myopic children.21 This coincides with the findings of a previous meta-analysis that suggested that orthokeratology decreases the rate of myopia progression in children.43
In contrast, Alvarez-Peregrina et al did not find an increase in the prevalence of myopia among children between 2019 and 2020.30 However, they observed that the percentage of hyperopes decreased, and the percentage of emmetropes increased (p<0.001). The average SE value in 2019 was +0.66±2.03 D, compared with +0.48±1.81 D in 2020 (p≤0.001). This decrease was significant in children aged 5 years. Additionally, 47% (95% CI 45% to 50%) of children spent less time outdoors in 2020 vs 2019 (p<0.001). Children who spent more time outdoors had higher SE values both preconfinement and postconfinement (p<0.001 and p=0.049).26 Even though Alvarez-Peregrina et al did not demonstrate myopia progression, a reduction in SER is a strong predictive factor for myopia in emmetropic and hyperopic children, as indicated by the Wenzhou Medical University Essilor Progression and Onset of Myopia study.44
Accommodation and vergence disturbances
A longer duration of digital device use requires more accommodative effort, and consequently increases the chance of asthenopia symptoms and dysfunctional accommodation and vergence (see table 2, Glossary). Mohan et al studied the effects of online classes during the COVID-19 pandemic, and considered the time spent in online classes and using digital devices such as television, video game systems and smartphones. According to the CISS survey, followed by evaluations by an optometrist and paediatric ophthalmologist, 36 out of 46 examined children had symptoms of convergence insufficiency. However, children who attended online classes for less than 4 hours/day exhibited fewer symptoms than those who attended online classes for more than 4 hours/day. Furthermore, near exophoria, near point convergence, positive fusional weakness and accommodation excess were more frequent in children exposed to longer online classes.13
Similarly, Hamburger et al evaluated ocular symptoms in 110 children who attended virtual school during the COVID-19 pandemic. They found that 61% of the children reported a significant increase in convergence insufficiency, as evidenced by a higher CISS score after attending online classes.33
Vagge et al reported four cases of children between 4 and 16 years old who developed acute acquired concomitant esotropia after intense digital device use during the COVID-19 lockdown.29 All of the children experienced acute-onset diplopia (see table 2, Glossary) after more than 8 hours/day spent looking at digital screens. Ophthalmological examination reported manifest esotropia from 20 to 35 prism dioptres at far and near distances in all four patients. Two out of the four children presented bilaterally cycloplegic refraction of +1.00 to +2.00 dioptre sphere. One of them presented cycloplegic refraction of –2.50 in the right eye and –2.25 in the left eye, and another presented –0.5 bilaterally.29 Some studies have suggested that digital device-induced esotropia is associated with excessive application of near vision, as well as dynamic activation of the medial rectus muscles when exposed to longer periods of digital screen time. This may affect the near vision triad, that is, the accommodation-convergence reflex: convergence of both eyes, contraction of the ciliary muscle resulting in a change of lens shape (accommodation) and pupillary constriction.29 45 46
Visual symptoms
The increase in digital device use associated with the COVID-19 lockdown and remote learning has precipitated a rise in dry eye symptoms and asthenopia. Hamburger et al reported a significant increase in asthenopia symptoms after online classes with discomfort, fatigue and impaired vision as dominant symptoms. Moreover, an increased asthenopia score was identified after online classes in more than half of the children evaluated.33 Likewise, Li et al identified a positive association between screen time and the risk of asthenopia in approximately 25 000 students aged 8–20 years, and attributed a higher risk of asthenopia to conditions such as myopia, astigmatism and mechanical factors like distance from the screen.25
Elhusseiny et al reported a significant increase in symptoms such as eye dryness, grittiness and scratchiness associated with prolonged exposure to digital screens for education and leisure purposes in 403 children aged 10–18 years.18 Similarly, Mohan et al identified longer screen time during the COVID-19 lockdown compared with the pre-COVID era in 217 children, of which almost half attended online classes.14 More than a third of the evaluated children used digital devices for over 5 hours/day, and 50.23% manifested dry eye with itching and headache as predominant symptoms.
Gupta et al evaluated 654 students between 5 and 18 years old using the Rasch-based Computer Vision Symptom Scale.16 The authors reported a significant increase in average digital device exposure during confinement, particularly smartphone, which was greater than 5 hours/day. Visual symptoms in the children were eye redness, eye strain, blurred vision, light sensitivity and heaviness of eyelids.16 Furthermore, Li et al identified a higher risk of computer vision syndrome in children with myopia with and without correction, astigmatism, fewer outdoor activities and prolonged screen time.26
The relationship between digital screen time and dry eye has already been described in both adults and children, as well as before the global COVID-19 pandemic.47–50 Changes in blinking dynamics and ocular surface abnormalities are some of the consequences that arise from intense screen exposure. Regarding ocular surface measures, longer screen time can decrease blinking frequency and completeness, resulting in reduced tear break-up time and tear volume, as well as changes in tear lipid composition.6 51 This means that a longer exposure to digital devices can enhance the deterioration of tear film quality, and thus increase the risk of developing dry eye symptoms.6
A main limitation of this study is the inclusion of articles with different study designs, as it is difficult to compare them quantitatively and qualitatively. Moreover, the evidence reported in the selected studies was obtained using distinct evaluation methods, from symptom surveys to detailed ophthalmological examinations, influencing the objectiveness of the conclusions obtained. Given that most of the studies were developed specifically in Asian countries, extrapolations to other parts of the world should be made with caution.
Conclusions
The changes in habits and lifestyles as a result of the COVID-19 pandemic have severely impacted eye health in children. Children attending classes as part of a remote learning strategy had more rapid myopia progression, increased frequency of dry eye and visual fatigue symptoms, and exhibited signs of vergence and accommodation disturbances such as acute acquired concomitant esotropia and convergence insufficiency. Ophthalmologists, paediatricians and general physicians should make themselves aware of the effect of virtual learning on the paediatric population to enable early identification and management of these conditions. In addition, countries around the world must implement public health strategies to mitigate the impacts of a more screen-focused life, especially with respect to conditions as common and costly as myopia. Further studies are required to evaluate the long-term impacts of such changes associated with the COVID-19 pandemic.
Supplementary Material
Footnotes
Twitter: @warc97
Contributors: Conceptualisation: MCC-A, SR-G, WR-C, Ad-l-T, CT-G. Methodology: MCC-A, SR-G, WR-C, CT-G. Investigation: MCC-A, SR-G, WR-C, Ad-l-T, CT-G. Resources: MCC-A, SR-G, WR-C, Ad-l-T, CT-G. Data curation: MCC-A, SR-G, CT-G. Writing—original draft preparation: MCC-A, SR-G, WR-C, Ad-l-T, CT-G. Writing—review and editing: MCC-A, SR-G, WR-C, Ad-l-T, CT-G. Supervision: Ad-l-T, CT-G. Guarantor: CT-G. All authors have read and agreed to the published version of the manuscript.
Funding: The review was supported by the Universidad del Rosario. We thank Sydney Koke, MFA, from Edanz (https://www.edanz.com/ac) for editing a draft of this manuscript.
Disclaimer: The sponsors had no role in the design, data collection or analysis of the study.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Arora T, Grey I. Health behaviour changes during COVID-19 and the potential consequences: a mini-review. J Health Psychol 2020;25:1155–63. 10.1177/1359105320937053 [DOI] [PubMed] [Google Scholar]
- 2.Almarzooq ZI, Lopes M, Kochar A. Virtual learning during the COVID-19 pandemic. J Am Coll Cardiol 2020;75:2635–8. 10.1016/j.jacc.2020.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Enthoven CA, Tideman JWL, Polling JR, et al. The impact of computer use on myopia development in childhood: the generation R study. Prev Med 2020;132:105988. 10.1016/j.ypmed.2020.105988 [DOI] [PubMed] [Google Scholar]
- 4.Fan Q, Wang H, Kong W, et al. Online learning-related visual function impairment during and after the COVID-19 pandemic. Front Public Health 2021;9:645971. 10.3389/fpubh.2021.645971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016;123:1036–42. 10.1016/j.ophtha.2016.01.006 [DOI] [PubMed] [Google Scholar]
- 6.Al-Mohtaseb Z, Schachter S, Shen Lee B, et al. The relationship between dry eye disease and digital screen use. Clin Ophthalmol 2021;15:3811–20. 10.2147/OPTH.S321591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Napoli PE, Nioi M, Fossarello M. The ‘quarantine dry eye’: the lockdown for coronavirus disease 2019 and its implications for ocular surface health. Risk Manag Healthc Policy 2021;14:1629–36. 10.2147/RMHP.S277067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Inomata T, Iwagami M, Nakamura M, et al. Characteristics and risk factors associated with diagnosed and undiagnosed symptomatic dry eye using a smartphone application. JAMA Ophthalmol 2020;138:58–68. 10.1001/jamaophthalmol.2019.4815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma L-L, Wang Y-Y, Yang Z-H. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med Res 2020;7. 10.1186/s40779-020-00238-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoy D, Brooks P, Woolf A, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 2012;65:934–9. 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 11.Simo LP, Agbor VN, AgborNdip E, et al. Prevalence and determinants of anaemia in children aged 6-59 months in Africa: a protocol for systematic review and meta-analysis. BMJ Open 2020;10:e032042. 10.1136/bmjopen-2019-032042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murad MH, Sultan S, Haffar S, et al. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med 2018;23:60–3. 10.1136/bmjebm-2017-110853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohan A, Sen P, Shah C, et al. Binocular accommodation and vergence dysfunction in children attending online classes during the COVID-19 pandemic: digital eye strain in kids (DESK study-2). J Pediatr Ophthalmol Strabismus 2021;58:224–31. 10.3928/01913913-20210217-02 [DOI] [PubMed] [Google Scholar]
- 14.Mohan A, Sen P, Shah C, et al. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: digital eye strain among kids (DESK study-1). Indian J Ophthalmol 2021;69:140–4. 10.4103/ijo.IJO_2535_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang P, Zhang B, Lin L, et al. Comparison of myopic progression before, during, and after COVID-19 lockdown. Ophthalmology 2021;128:1655–7. 10.1016/j.ophtha.2021.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gupta R, Chauhan L, Varshney A. Impact of e-schooling on digital eye strain in coronavirus disease era: a survey of 654 students. J Curr Ophthalmol 2021;33:158–64. 10.4103/joco.joco_89_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang J, Li Y, Musch DC, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol 2021;139:293–300. 10.1001/jamaophthalmol.2020.6239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elhusseiny AM, Eleiwa TK, Yacoub MS, et al. Relationship between screen time and dry eye symptoms in pediatric population during the COVID-19 pandemic. Ocul Surf 2021;22:117–9. 10.1016/j.jtos.2021.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang W, Zhu L, Zheng S, et al. Survey on the progression of myopia in children and adolescents in Chongqing during COVID-19 pandemic. Front Public Health 2021;9:646770. 10.3389/fpubh.2021.646770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aslan F, Sahinoglu-Keskek N. The effect of home education on myopia progression in children during the COVID-19 pandemic. Eye 2022;36:1427–32. 10.1038/s41433-021-01655-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lv H, Wang Y, Sun S, et al. The impact of COVID-19 home confinement on axial length in myopic children undergoing orthokeratology. Clin Exp Optom 2022:1–5. 10.1080/08164622.2021.2016352 [DOI] [PubMed] [Google Scholar]
- 22.Ma D, Wei S, Li S-M, et al. The impact of study-at-home during the COVID-19 pandemic on myopia progression in Chinese children. Front Public Health 2021;9:720514. 10.3389/fpubh.2021.720514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu L, Ma Y, Yuan J, et al. COVID-19 quarantine reveals that behavioral changes have an effect on myopia progression. Ophthalmology 2021;128:1652–4. 10.1016/j.ophtha.2021.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hu Y, Zhao F, Ding X, et al. Rates of myopia development in young Chinese schoolchildren during the outbreak of COVID-19. JAMA Ophthalmol 2021;139:1115–21. 10.1001/jamaophthalmol.2021.3563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li L, Zhang J, Chen M, et al. Contribution of total screen/online-course time to asthenopia in children during COVID-19 pandemic via influencing psychological stress. Front Public Health 2021;9:736617. 10.3389/fpubh.2021.736617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li R, Ying B, Qian Y, et al. Prevalence of self-reported symptoms of computer vision syndrome and associated risk factors among school students in China during the COVID-19 pandemic. Ophthalmic Epidemiol 2021:1–11. 10.1080/09286586.2021.1963786 [DOI] [PubMed] [Google Scholar]
- 27.Mohan A, Sen P, Mujumdar D, et al. Series of cases of acute acquired comitant esotropia in children associated with excessive online classes on smartphone during COVID-19 pandemic; digital eye strain among kids (DESK study-3). Strabismus 2021;29:163–7. 10.1080/09273972.2021.1948072 [DOI] [PubMed] [Google Scholar]
- 28.Mohan A, Sen P, Peeush P, et al. Impact of online classes and home confinement on myopia progression in children during COVID-19 pandemic: digital eye strain among kids (DESK study 4). Indian J Ophthalmol 2022;70:241. 10.4103/ijo.IJO_1721_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vagge A, Giannaccare G, Scarinci F, et al. Acute acquired concomitant esotropia from excessive application of near vision during the COVID-19 lockdown. J Pediatr Ophthalmol Strabismus 2020;57:e88–91. 10.3928/01913913-20200828-01 [DOI] [PubMed] [Google Scholar]
- 30.Alvarez-Peregrina C, Martinez-Perez C, Villa-Collar C. Impact of COVID-19 home confinement in children’s refractive errors. Int J Environ Res Public Health 2021;18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cremers SL, Khan ARG, Ahn J, et al. New indicator of children’s excessive electronic screen use and factors in meibomian gland atrophy. Am J Ophthalmol 2021;229:63–70. 10.1016/j.ajo.2021.03.035 [DOI] [PubMed] [Google Scholar]
- 32.Mirhajianmoghadam H, Piña A, Ostrin LA. Objective and subjective behavioral measures in myopic and non-myopic children during the COVID-19 pandemic. Transl Vis Sci Technol 2021;10:4. 10.1167/tvst.10.11.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamburger JL, Lavrich JB, Rusakevich AM, et al. The visual consequences of virtual school: acute eye symptoms in healthy children. J AAPOS 2022;26:2.e1–2.e5. 10.1016/j.jaapos.2021.10.003 [DOI] [PubMed] [Google Scholar]
- 34.Wong CW, Tsai A, Jonas JB, et al. Digital screen time during the COVID-19 pandemic: risk for a further myopia boom? Am J Ophthalmol 2021;223:333–7. 10.1016/j.ajo.2020.07.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones-Jordan LA, Mitchell GL, Cotter SA, et al. Visual activity before and after the onset of juvenile myopia. Invest Ophthalmol Vis Sci 2011;52:1841–50. 10.1167/iovs.09-4997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mccrann S, Loughman J, Butler JS, et al. Smartphone use as a possible risk factor for myopia. Clin Exp Optom 2021;104:35–41. 10.1111/cxo.13092 [DOI] [PubMed] [Google Scholar]
- 37.Lanca C, Saw S-M. The association between digital screen time and myopia: a systematic review. Ophthalmic Physiol Opt 2020;40:216–29. 10.1111/opo.12657 [DOI] [PubMed] [Google Scholar]
- 38.He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA 2015;314:1142–8. 10.1001/jama.2015.10803 [DOI] [PubMed] [Google Scholar]
- 39.McCarthy CS, Megaw P, Devadas M, et al. Dopaminergic agents affect the ability of brief periods of normal vision to prevent form-deprivation myopia. Exp Eye Res 2007;84:100–7. 10.1016/j.exer.2006.09.018 [DOI] [PubMed] [Google Scholar]
- 40.Feldkaemper M, Schaeffel F. An updated view on the role of dopamine in myopia. Exp Eye Res 2013;114:106–19. 10.1016/j.exer.2013.02.007 [DOI] [PubMed] [Google Scholar]
- 41.Wu P-C, Chen C-T, Lin K-K, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology 2018;125:1239–50. 10.1016/j.ophtha.2017.12.011 [DOI] [PubMed] [Google Scholar]
- 42.Ip JM, Saw S-M, Rose KA, et al. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci 2008;49:2903–10. 10.1167/iovs.07-0804 [DOI] [PubMed] [Google Scholar]
- 43.Si J-K, Tang K, Bi H-S, et al. Orthokeratology for myopia control: a meta-analysis. Optom Vis Sci 2015;92:252–7. 10.1097/OPX.0000000000000505 [DOI] [PubMed] [Google Scholar]
- 44.Wong YL, Yuan Y, Su B, et al. Prediction of myopia onset with refractive error measured using non-cycloplegic subjective refraction: the WEPrOM study. BMJ Open Ophthalmol 2021;6:e000628. 10.1136/bmjophth-2020-000628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee HS, Park SW, Heo H. Acute acquired comitant esotropia related to excessive smartphone use. BMC Ophthalmol 2016;16:37. 10.1186/s12886-016-0213-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Motlagh M, Geetha R. Physiology, accommodation. Treasure Island, FL: StatPearls Publishing, 2022. [PubMed] [Google Scholar]
- 47.Uchino M, Yokoi N, Uchino Y, et al. Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol 2013;156:759–66. 10.1016/j.ajo.2013.05.040 [DOI] [PubMed] [Google Scholar]
- 48.Hanyuda A, Sawada N, Uchino M, et al. Physical inactivity, prolonged sedentary behaviors, and use of visual display terminals as potential risk factors for dry eye disease: JPHC-NEXT study. Ocul Surf 2020;18:56–63. 10.1016/j.jtos.2019.09.007 [DOI] [PubMed] [Google Scholar]
- 49.Bhattacharya S, Saleem SM, Singh A. Digital eye strain in the era of COVID-19 pandemic: an emerging public health threat. Indian J Ophthalmol 2020;68:1709–10. 10.4103/ijo.IJO_1782_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rojas-Carabali W, Uribe-Reina P, Muñoz-Ortiz J, et al. High prevalence of abnormal ocular surface tests in a healthy pediatric population. Clin Ophthalmol 2020;14:3427–38. 10.2147/OPTH.S266261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rossi GCM, Scudeller L, Bettio F, et al. Prevalence of dry eye in video display terminal users: a cross-sectional Caucasian study in Italy. Int Ophthalmol 2019;39:1315–22. 10.1007/s10792-018-0947-6 [DOI] [PubMed] [Google Scholar]
- 52.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Merriam-Webster . Medical dictionary, 2022. Available: https://www.merriam-webster.com/
- 54.EyeWiki . American Academy of ophthalmology (online). Available: https://eyewiki.aao.org/Main_Page
- 55.Palay D, Krachmer J. Primary care ophthalmology. Mosboy, 2005: 1–23. 10.1016/B978-0-323-03316-9.X5001-3 [DOI] [Google Scholar]
- 56.Mukamal R. What is orthokeratology (online), 2018. Available: https://www.aao.org/eye-health/glasses-contacts/what-is-orthokeratology
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-062388supp001.pdf (39.8KB, pdf)
bmjopen-2022-062388supp002.pdf (74.6KB, pdf)
Data Availability Statement
Data are available in a public, open access repository.