Abstract
Arthroscopic Latarjet has evolved as a reproducible procedure to address significant anterior glenoid bone loss in recurrent anterior instability of the shoulder joint. While arthroscopic Bankart procedure for anterior shoulder instability has changed from metal anchors to absorbable or soft all-suture anchors to avoid metal-ware and subsequent abrasion in cases of osteolysis or backout, Latarjet procedure, until recently couple of titanium screws were used to fix the coracoid bone to the anterior glenoid. Arthroscopic techniques for Latarjet procedure of coracoid bone transfer have shown results similar to the open technique in many recent studies. We use an all-arthroscopic technique that is different and easier from the currently described technique using FiberTape cerclage loops, with 2 ultrabraid tapes fixing the coracoid bone to the prepared anteroinferior glenoid surface. The repair is completed using all-suture anchors to fix the anterior capsule over the attached coracoid, thus exteriorizing the transferred bone and preventing contact with the moving humeral head.
Technique Video
An arthroscopic Latarjet procedure is demonstrated using a simplified FiberTape cerclage passage technique. A beach-chair position is used for the procedure. Diagnostic arthroscopy is performed using the arthroscope from the posterior portal. Hill–Sachs lesion and engagement of this humeral bone defect on the anterior glenoid are demonstrated taking the arm through the abduction and external rotation movement. Viewing from the posterior portal using a 70° arthroscope, rotator interval clearance is done. The capsulolabral complex is elevated from the 3-o’clock to the 6-o’clock position on the glenoid using a radiofrequency probe. The capsule is elevated away from the glenoid using a tag suture. The breadth of the glenoid is measured using a measuring device introduced from the coracoid portal. Viewing from the posterior portal using the 70° arthroscope, the lateral side of the coracoid is cleared of the coracoacromial ligament. The pectoralis minor is released from the medial aspect of coracoid using the radiofrequency probe from the H portal, preserving the conjoint tendon attachment to the tip of the coracoid bone. The undersurface of coracoid is cleared of soft tissue and a rotary burr is used to decorticate the inferior surface of coracoid preparing it for the bone transfer. The length of the coracoid is measured and the base of the coracoid is decorticated in its inferior, superior, medial and lateral surfaces. The coracoid drill guide with 7 mm offset (Arthrex) is introduced from the H portal. Then, 1.2-mm guidewires are drilled into the coracoid and they are over drilled using a 2.4-mm cannulated drill bit. A curved osteotome is used to detach the coracoid at its base. Viewing from the anterosuperior portal, the radiofrequency probe is introduced from the I portal and, the subscapularis tendon and muscle are split horizontally at the junction of upper two-thirds and lower one-third to expose the anteroinferior glenoid. The hooked stylus of the glenoid jig is inserted from the posterior portal and guidewires are drilled from posterior to anterior using the glenoid jig, and over-drilled with a 2.4-mm cannulated drill bit. Differently colored sutures are used in the superior and inferior holes, Nylon and PDS, for easy identification and to prevent suture entanglement during passage. A crochet hook is passed through the respective holes in the coracoid and the two suture limbs are pulled out through the M portal. The FiberTape cerclage tip is shuttled across the glenoid and coracoid, posteroanteriorly in the superior holes and anteroposteriorly in the inferior holes. The cerclage tape is locked in the premade knot of the construct. You can see that the coracoid is pulled onto the prepared anteroinferior surface of glenoid as the cerclage construct is tightened. The FiberTape cerclage construct is tensioned using the tensioner to 80 N. Care is taken to visualize the coracoid movement from the anterosuperior portal while the tapes are tensioned. This method gives a robust fixation of the coracoid on the antero-inferior glenoid and the position of the coracoid with respect to the glenoid is always accurate as the drilling of the holes is done using the jigs. The previously elevated capsulolabral complex is repaired to the anterior glenoid using 1.6-mm Fiber-Tak all-suture anchors. This exteriorizes the transferred coracoid preventing any impingement of the humeral head on the bony coracoid. A computed tomography scan is taken at 3 months to confirm bony union before allowing full range of motion and sporting activities.
Addressing significant glenoid bone loss has evolved over the past few decades, and the arthroscopic Latarjet is presently an accepted reproducible procedure1,2 to reconstruct the lost bone from the anterior glenoid (Table 1). As the Bankart procedure of anterior capsulolabral reattachment has evolved from open techniques to arthroscopic techniques with good or better results in current literature,3,4 the arthroscopic treatment of glenoid bone loss with coracoid bone transfer (Latarjet procedure) also has shown similar results to open methods in terms of shoulder stability, with the added advantages of the ability to treat concomitant pathology like biceps anchor tears, Hill–Sachs lesions with remplissage, and simultaneous capsulolabral reattachment, thereby exteriorizing the transferred coracoid graft.5
Table 1.
Indications for Arthroscopic Latarjet Procedure
|
The Latarjet procedure evolved from the first description in 1954 by Michel Latarjet6 to initiation of arthroscopic method by Lafosse in 2007.1 Coracoid fixation was originally described in the Latarjet procedure using 3.5-mm metal screws that pass from the coracoid fixing it to the glenoid in an anteroposterior direction.7 The head of the metal screws used in open and arthroscopic Latarjet procedures, and the “top hat” of the arthroscopic Latarjet method using metal screws, can be associated with the complications of impingement on the humeral head.8 This impingement becomes more significant if osteolysis develops in the transferred coracoid, exposing the metal screw heads, especially the superior (alpha) screw.
Various methods are described for coracoid fixation involving metal screws, ENDOBUTTONS, FiberWires, and tapes with the coracoid drilling being done from anterior or posterior side using specially designed jigs. The metal-free cerclage tape method of arthroscopic Latarjet procedure reduces the change of metal prominence and impingement after anterior glenoid reconstruction with coracoid bone transfer. We propose a modification of the metal-free technique described earlier9 that aims to simplify the passage of the ultra-high strength fiber tapes through the glenoid and coracoid bones.
Surgical Technique (With Video illustration)
Video 1 demonstrates with surgical technique of Arthroscopic Latarjet procedure using FiberTape cerclage (Arthrex, Naples, FL) using as simplified suture shuttling technique through the osteotomized coracoid.
Preoperative Evaluation
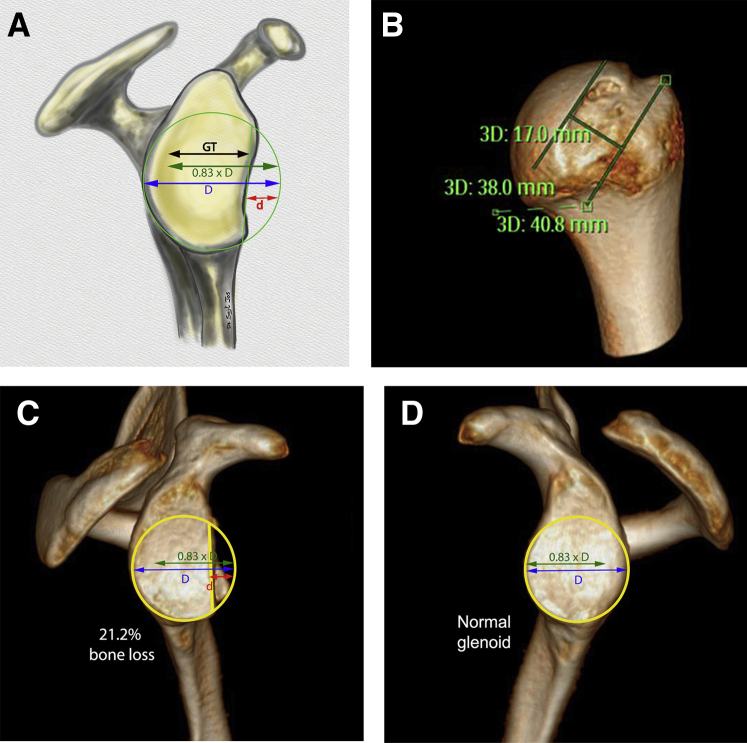
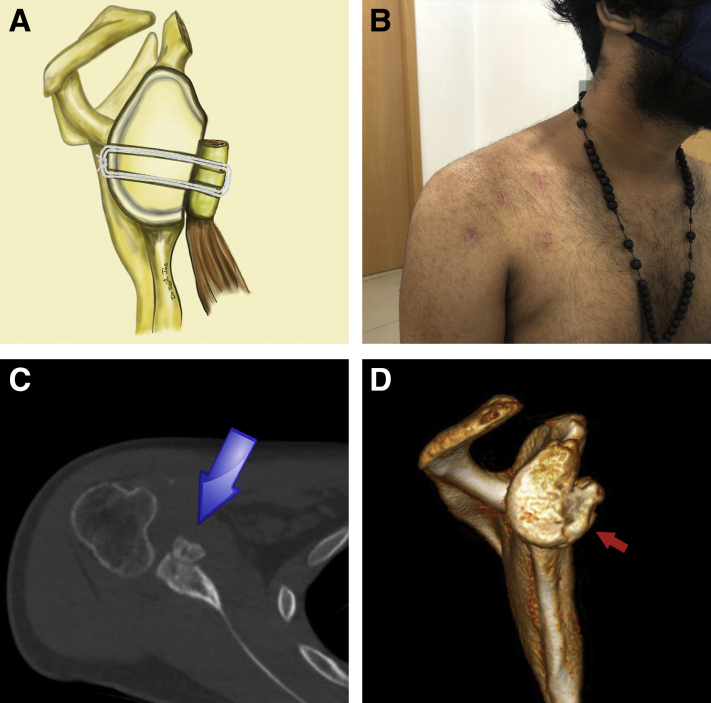
The patients are evaluated with radiographs and 3-dimensional (3D) computed tomography (CT) scans to assess the bone loss from the anterior glenoid (bony Bankart) and humeral head (Hill–Sachs lesion) (Fig 1). The best-fit circle method is used on the glenoid face 3D CT image to measure the glenoid bone loss in the anteroposterior dimension of the glenoid.10,11 The glenoid track is calculated and compared with Hill–Sachs interval. If the Hill–Sachs interval is found to be more than the glenoid track (off-track bipolar bone loss), the decision of adding a remplissage procedure is made depending on the age, sporting demands, and other significant parameters that may put the Latarjet procedure at a risk of inadequacy.12
Fig 1.
Preoperative computed tomography scan with 3-dimensional reconstruction. (A) Diagram showing the “best-fit circle method” to determine bone loss on the anterior glenoid of the right shoulder. (B) Affected glenoid (right side) with 21.2% anterior bone loss. (C) Glenoid on the normal side (left side).
Positioning and Portals
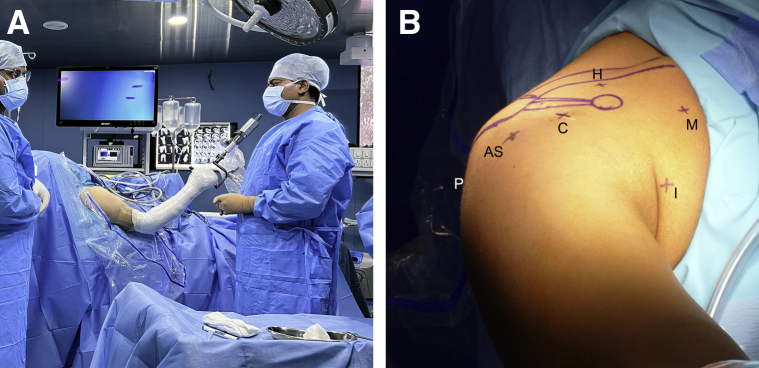
The patient is positioned in beach-chair position, under interscalene block anesthesia (Fig 2A). bony landmarks and portals are marked (Fig 2B). The portals used (Table 2) are standard posterior (P portal), anterosuperior portal (AS portal) 1 cm distal to anterolateral border of acromion, coracoid portal (C portal) in line with the tip of coracoid, high portal (H portal) for coracoid osteotomy and pectoralis minor detachment made superior to the coracoid and just anterior to the anterior border of the clavicle (final position decided during arthroscopy after visualizing trajectory with a needle), the inferior portal (I portal) in the anterior axillary fold, used for subscapularis splitting and part of coracoid preparation, and the medial portal (M portal) for shuttling the sutures and FiberTape cerclage through the osteotomized coracoid bone.
Fig 2.
(A) The patient is placed in the beach-chair position with a Spider II (Smith & Nephew, Watford, United Kingdom) arm positioner for the right shoulder. (B) Portals used for arthroscopic Latarjet procedure (details in Table 2).
Table 2.
Portals for All-Fiber Arthroscopic Latarjet Procedure
| P portal: standard posterior portal—for visualization during initial soft-tissue clearance and coracoid exposure |
| AS portal: Anterosuperior portal—1 cm distal to anterolateral border of acromion, |
| C portal: coracoid portal—in line with the tip of coracoid, |
| H portal: high portal—for coracoid osteotomy and pectoralis minor detachment made superior to the coracoid and just anterior to the anterior border of the clavicle (final position decided during arthroscopy after visualizing trajectory with a needle), |
| I portal: Inferior portal—in the anterior axillary fold used for subscapularis splitting and part of coracoid preparation |
| M portal: Medial portal—for shuttling the sutures in the glenoid drill holes and FiberTape cerclage through the coracoid bone. |
Anterior Glenoid Preparation
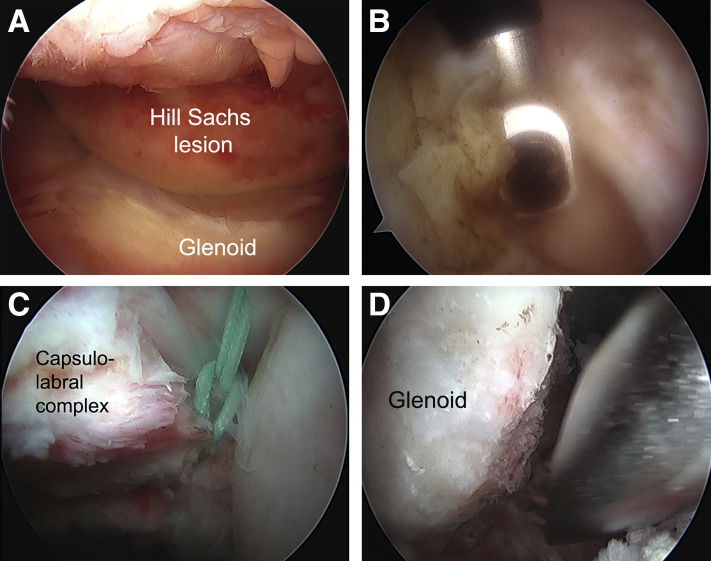
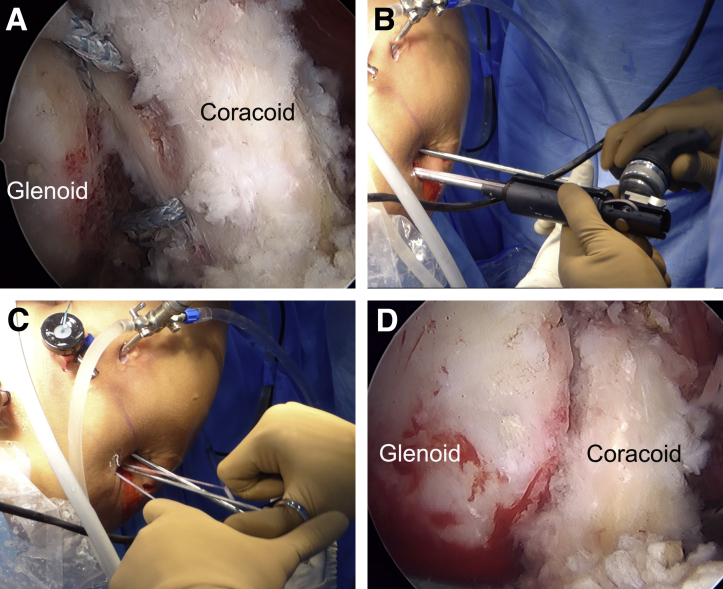
Diagnostic arthroscopy is performed through the P (Posterior) portal using a 70° arthroscope. The anterior glenoid, detached anterior labrum, superior labrum and biceps anchor, the Hill-sachs lesion on posterosuperior glenoid and other intra-articular areas are visualized. The glenoid dimensions and engagement of the Hill–Sachs lesion over the anterior glenoid are visualized and confirmed (Fig 3A). The anterior glenoid is prepared by introducing the radiofrequency probe through the AS (anterosuperior) portal. An L-shaped capsulotomy is made with the vertical limb near inferior most part of the glenoid (Fig 3B). A tug suture is placed on the apex of the capsular cut, and this is pulled superiorly away from the area of glenoid preparation and coracoid fixation in the anteroinferior glenoid (Fig 3C). The anteroinferior part of the glenoid is prepared using a radiofrequency probe and the superficial bone abraded with a rotary burr to create a bleeding surface to receive the coracoid bone graft (Fig 3D).
Fig 3.
(A) Engagement of the Hill–Sachs on the anterior glenoid of the right shoulder, viewed from the posterior (P) portal. (B) Capsulotomy using radiofrequency probe. (C) Elevation of capsulolabral complex. (D) Preparation of glenoid using rotary barrel burr 4 mm.
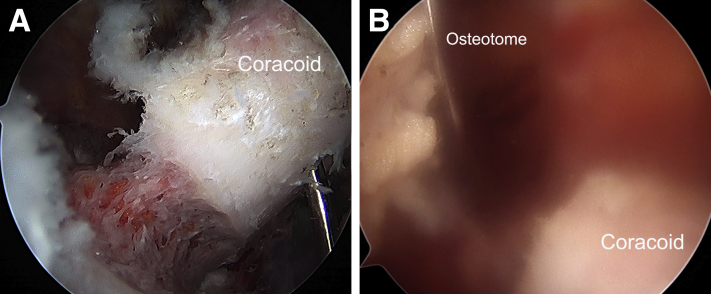
Coracoid Preparation
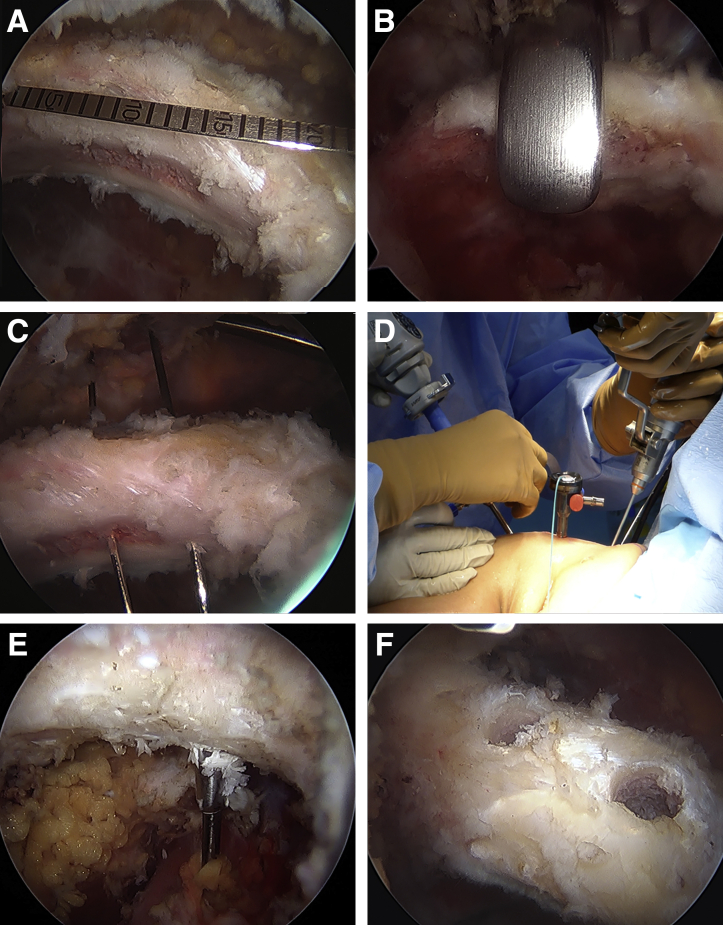
The soft-tissue attachments to coracoid are released, retaining the conjoint tendon attachment at the tip of the coracoid. The coracoacromial ligament is released form the lateral aspect. The undersurface is cleared and bone burred to decorticate using a rotary burr (4 mm) introduced through the AS portal. The C (central) portal is used to release the pectoralis minor from the medial aspect of coracoid. The superior surface of coracoid is cleared up till the attachment of the coracoclavicular ligaments (conoid and trapezoid). The length of the coracoid that can be used for the Latarjet procedure is measured using arthroscopic measuring device (usually about 20 mm) (Fig 4A). The H (high) portal is created, confirming the trajectory for coracoid drilling, using a needle. The coracoid drill guide is introduced from the superior aspect of the coracoid through the H portal (Fig 4B). Then, 1.2-mm guidewires are drilled into alpha and beta holes of the coracoid drill-guide (Fig 4C). These are further over drilled with 3.2-mm drill bit (Fig 4E).
Fig 4.
Coracoid preparation of the right shoulder. (A) Measurement of coracoid length using arthroscopic measurement probe (Arthrex, Naples, FL). (B) Coracoid drill-guide (Arthrex) placement for drilling the coracoid holes. (C) 1.2-mm guidewires drilled into the coracoid. (D) External picture of drilling over the guidewire. (E) Guidewires overdrilled with a 2.4-mm drill bit.
Coracoid Osteotomy
The base of the coracoid is demarcated for the osteotomy using the rotary burr, removing cortical bone in a circumferential area at its base (Fig 5A). A curved osteotome is introduced through the H portal and the osteotomy is completed using a gentle tap to detach the coracoid at the region where the base has been decorticated (Fig 5B). The coracoid base at the osteotomy site is cleared of any prominent bone spike using a rotary burr. The osteotomized coracoid rests in the region posterior to the pectoralis major.
Fig 5.
Coracoid osteotomy. (A) Cortical bone removed at base of coracoid circumferentially using rotary burr. (B) Curved osteotome used to detach the coracoid at its base.
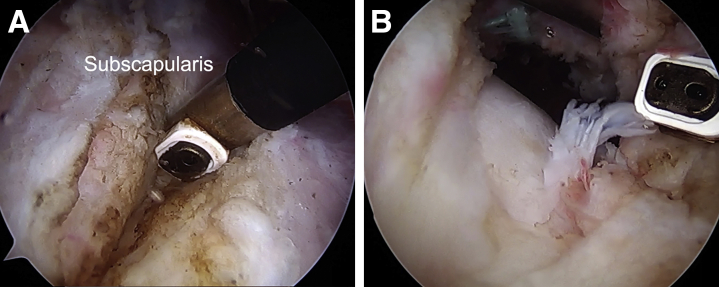
Subscapularis Muscle Split
A Wissinger rod introduced from the AS portal is used to push the pectoralis major, along with the osteotomized coracoid with conjoint tendon attached, away from the subscapularis muscle. Subscapularis muscle is split horizontally along at the junction of upper two-thirds (more tendinous) and lower one-third (more muscular) using a radiofrequency probe introduced through the I portal (Fig 6A). This can be safely done to the level of glenoid, medial to which lies the axillary nerve, where caution must be maintained. The anteroinferior aspect of the glenoid is exposed during this step, using a stitching stick in the I portal to push the inferior part of the subscapularis down and another one in the P portal to push the superior part of the subscapularis up (Fig 6B).
Fig 6.
Subscapularis split of right shoulder, viewed from the anterosuperior (AS) portal. (A) Radiofrequency probe used to split the subscapularis tendon at the junction of upper two-thirds and lower one-third. (B) Anteroinferior glenoid exposed through the split in the subscapularis tendon and muscle.
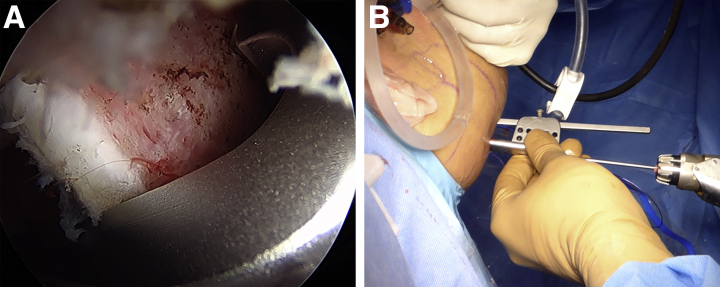
Glenoid Drilling and Suture Passage
The glenoid drill guide stylus is introduced from the P portal (Fig 7A). The drill guide body is introduced over the guide stylus and made to contact the glenoid bone through a longitudinal incision made medial to the P portal, about 1.5 cm long (Fig 7B). Then, 1.2-mm guidewires are drilled through the glenoid jig so that they exit about 8 mm medial to the glenoid edge in the anteroinferior area, parallel to each other. These are overdrilled with 3.2-mm drill bits. After the drill bit tips are seen exiting from the anterior surface of glenoid, shuttling sutures are passed through them, and these are pulled out through the M portal using a suture retriever (Fig 8A). (different-colored sutures are used in the inferior and superior holes in the glenoid so that entanglement and twisting can be prevented). A crochet hook is passed through the respective holes drilled in the coracoid to retrieve the different colored sutures through the M portal (Fig 8C).
Fig 7.
Glenoid jig positioning for right shoulder, viewed from the anterosuperior (AS) portal. (A) Arthroscopic picture of the hooked stylus of the glenoid jig introduced through the posterior portal. (B) Glenoid jig body positioned on the posterior glenoid through an incision medial to P portal.
Fig 8.
Suture shuttling (right shoulder). (A) Nylon No. 1 (black) and PDS No. 1 (violet) passed through the superior and inferior holes drilled in the glenoid. (B) Sutures passed out through the M portal avoiding entanglement. (C) Suture passage through the coracoid using crochet hook passed through the holes drilled in the coracoid bone. (D and E) FiberTape cerclage shuttled through the 2 drill holes in the coracoid and glenoid. (F) FiberTape cerclage limbs passing through the 2.4-mm drill hole in coracoid. (G) FiberTape loop in the M portal. (H) The tip of the FiberTape passed through the loop at the opposite end of the FiberTape construct to make the knot near the posterior portal.
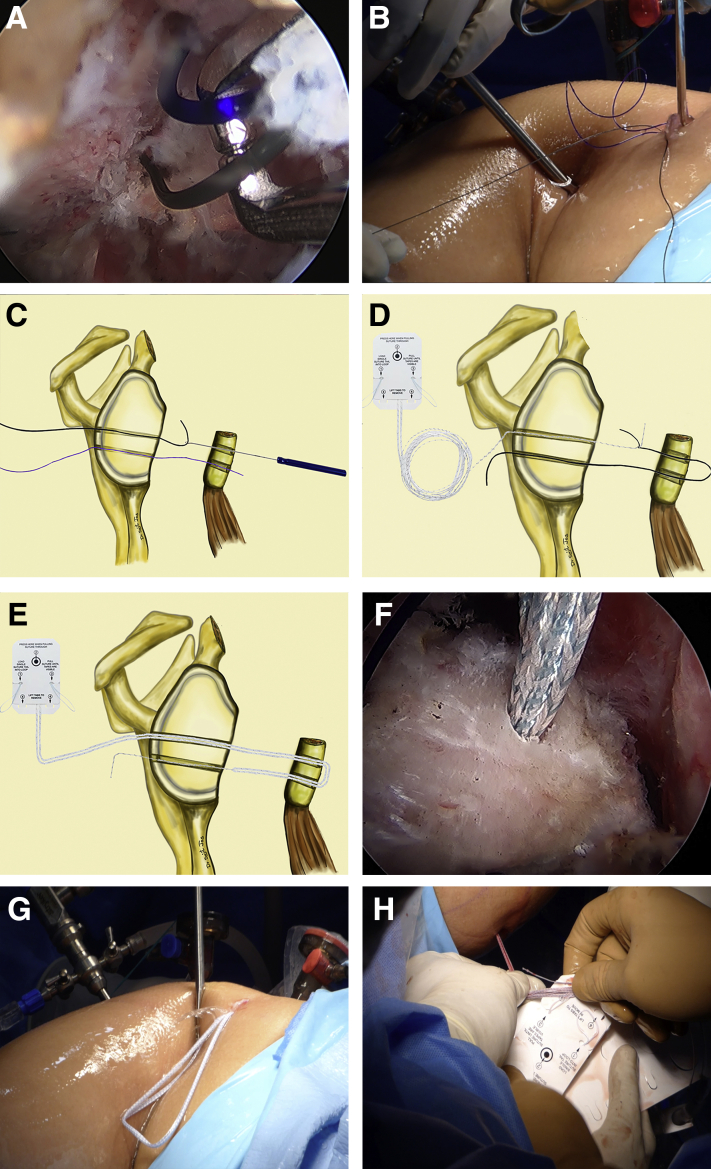
FiberTape Cerclage Passage
The FiberTape Cerclage (Arthrex) is shuttled from the posterior to anterior using the suture in the superior hole of glenoid and coracoid (Nylon No.1), to be passed outside anteriorly through the M portal, and passed back posteriorly using the second suture (PDS No.1) through the inferior hole in the coracoid and the glenoid (Fig 8, D and E).
Tensioning of the Cerclage Tape
The cerclage tape is tensioned using the tensioning device (Arthrex) on the posterior aspect of the glenoid (tension to 80 lbs) (Fig 9B). The coracoid bone can be seen to be compressed on the anteroinferior glenoid when tension is applied on the FiberTape cerclage loop. One major advantage of this technique is that there is no need to guide the coracoid on to its destination on the anteroinferior glenoid; it is automatically pulled to this location, through the split in the subscapularis muscle, when the FiberTape cerclage is tensioned (Fig 9D). The positioning of the glenoid with respect to the glenoid face is always accurate and easily reproducible as the drill holes are placed in the glenoid using a jig (ideally, 1 mm medial to the glenoid face is most desirable to prevent impingement on the humeral head during movement of the shoulder joint13).
Fig 9.
Cerclage tape tensioning. (A) Arthroscopic picture of FiberTape cerclage loop passed through the glenoid and coracoid; view from the anterosuperior (AS) portal. (B) External image of tensioning device (Arthrex, Naples, FL). (C) Knot being secured using 3half hitches over the FiberTape cerclage knot, using knot pusher. (D) The transferred coracoid compressed well over the prepared anteroinferior part of glenoid on tensioning the FiberTape construct.
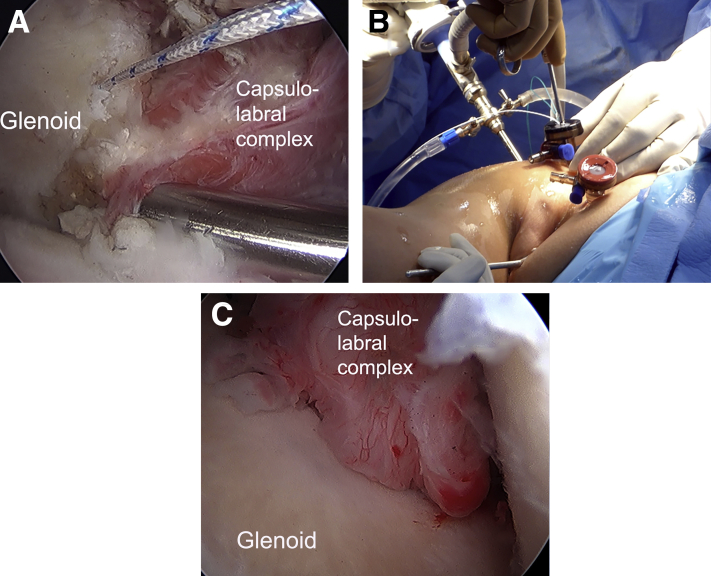
Capsulolabral Complex Repair With Suture Anchors
Two all-suture anchors (FiberTak 1.6 mm; Arthrex) are placed on the anterior glenoid rim to reattach the previously elevated anterior capsule. The drilling and insertion of the anchors are done through the C portal. The bites in the capsule are placed using an indirect suture passing device (SutureLasso; Arthrex). This capsular reattachment on to the glenoid rim [Fig: 10A] helps to exteriorize the coracoid bone (Fig 10C) and further aids in preventing inferior wear on humeral head reported in previous long-term studies of Latarjet procedure.14
Fig 10.
Capsulolabral complex repair. (A) Capsulolabral complex being reattached on the anterior glenoid using all-suture anchors (FiberTak 1.6, Arthrex, Naples, FL). View from the anterosuperior (AS) portal. (B) External picture of knot tying. (C) Capsulolabral complex repaired using suture anchor fixation to anteroinferior glenoid, thus exteriorizing the transferred coracoid bone.
Tips and tricks for this technique are given in Table 3, and pearls and pitfalls in Table 4.15 The limitations and risks of this procedure are described in Table 5.
Table 3.
Tips and Tricks for a Successful Procedure
|
|
|
|
|
Table 4.
Pearls and Pitfalls
| Pearls |
|
|
|
|
|
|
|
|
|
|
|
|
| Pitfalls |
|
|
|
Table 5.
Limitations and Risks
|
|
|
|
Postoperative Care
The shoulder is placed in a sling for 3 weeks after the procedure. During this period, pendulum exercises with isometric strengthening of the shoulder and scapular muscles are advised, along with elbow and hand mobilization. During this period, passive shoulder forward flexion and abduction up to 90° are allowed. External rotation in adduction is limited to 25°.
The arm sling is removed at 3 weeks active assisted mobilization is encouraged. Full range of movement is allowed, including external rotation, after 6 weeks. Muscle strengthening is increased progressively after 6 weeks. Return to sports is allowed at 4-6 months after evaluating bony union with a CT scan at 3 months (Fig 11B).
Fig 11.
(A) Diagrammatic representation of the final FiberTape cerclage fixation of the coracoid on to the glenoid (right shoulder). (B) Postoperative 3-dimensional reconstruction computed tomography scan showing accurate coracoid graft placement and bony healing on the anteroinferior glenoid recreating the circular inferior portion of the glenoid. (C) Postoperative clinical picture showing the healing arthroscopy portals during postoperative review.
Discussion
The Latarjet procedure6,7 has progressed over the last few decades from an open technique to a mini-open, and now an arthroscopic technique, encouraging more and more surgeons to switch over to the key-hole method. Osteoarthritis on long-term follow-up in the glenohumeral joint after traditional Latarjet procedure is a concern, and prominent bone block or metal-ware are the major attributed causes.14 Osteolysis of the superior aspect of the transferred coracoid bone after Latarjet is a common phenomenon,16,17 and this can make the screw heads used for Latarjet procedure more prominent. Cohen et al.16 report an incidence of osteolysis of up to 57.8%, although this did not affect the long-term outcome significantly. In the imaging and performance analysis by LeBus et al.8 in a National Football League group demonstrated metal-ware related complications in up to 46% of athletes among 2,617 players. This particular complication can be minimized in all-fiber Latarjet procedure as the soft FiberTapes used will not cause abrasive damage to the humeral head even in the presence of osteolysis.
Other screw-related complications are described in other studies are capsular or muscular impingement (subscapularis, infraspinatus) and nerve injury of suprascapular nerve due to the drill holes made from anterior to posterior, which can often be directed more medially.18,19
The glenoid tunnel drilling from posterior to anterior using the glenoid jig allows accurate placement of the coracoid graft with respect to the glenoid face, thus eliminating problems of coracoid graft impingement on the humeral head.14
The FiberTape passage is made simpler in our technique by shuttling them in a straight line through the glenoid drill holes and through the coracoid holes, using the M portal to shuttle the tapes to and fro. In the technique described earlier by Hachem et al.,9 the tape has to be passed as 90° to the glenoid drill holes and this often causes abrasion at the glenoid hole edges and difficulty in passage. Using a crochet hook to shuttle the passing sutures through the osteotomized coracoid simplifies the suture passage, which is usually a difficult step in the previously described all-fiber arthroscopic Latarjet technique.
The micromotion after the FiberTape fixation allows better bone healing than rigid fixation with metal screws.20 Latarjet fixation with FiberWire and cortical ENDOBUTTONS have been described by Boileau et al.2 and Valenti et al.21 However, a greater failure rate with cortical buttons has been described by in some studies.22 The technique described by Boileau et al.2 used only one ENDOBUTTON, which could allow the coracoid to rotate and thus compromising graft healing. The FiberTape method using 2 drill holes in glenoid and coracoid produces uniform compression of the coracoid graft while providing excellent strength neutralizing the pull of the conjoint tendon. The smaller drill tunnels of 2.4 mm reduce the risk of coracoid and glenoid fracture.
The capsular repair to the glenoid edge done after coracoid fixation allows exteriorization of the coracoid bone block thus further reducing abrasion of the humeral head with the raw surface of the transferred bone.5 Studies have shown that reattachment of the capsulolabral complex does not restrict glenohumeral external rotation range.23
The glenoid drill guide and coracoid drill guide, both supplied by Arthrex, are the only extra instruments required for this technique and these make the technique easily reproducible. We use the FiberTape cerclage of Arthrex for coracoid fixation and 2 all-suture single-loaded anchors for the capsular repair. These give a strong fixation of the coracoid by tensioning the continuous FiberTape using the tensioning device up to 80 N, while producing exteriorization of the coracoid by means of the capsular repair.
This all-fiber technique is described as an alternative to screw fixation in Latarjet procedure, eliminating the problems of screw impingement of soft-tissues and bones near the shoulder joint. Postoperative imaging for assessment of bony union is made more accurate as there will not be scatter from the metal screws. This technique has all the advantages of arthroscopic surgery including reduced bleeding, reduced risk of infection, faster rehabilitation, and smaller scar.19
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
An arthroscopic Latarjet procedure is demonstrated using a simplified FiberTape cerclage passage technique. A beach-chair position is used for the procedure. Diagnostic arthroscopy is performed using the arthroscope from the posterior portal. Hill–Sachs lesion and engagement of this humeral bone defect on the anterior glenoid are demonstrated taking the arm through the abduction and external rotation movement. Viewing from the posterior portal using a 70° arthroscope, rotator interval clearance is done. The capsulolabral complex is elevated from the 3-o’clock to the 6-o’clock position on the glenoid using a radiofrequency probe. The capsule is elevated away from the glenoid using a tag suture. The breadth of the glenoid is measured using a measuring device introduced from the coracoid portal. Viewing from the posterior portal using the 70° arthroscope, the lateral side of the coracoid is cleared of the coracoacromial ligament. The pectoralis minor is released from the medial aspect of coracoid using the radiofrequency probe from the H portal, preserving the conjoint tendon attachment to the tip of the coracoid bone. The undersurface of coracoid is cleared of soft tissue and a rotary burr is used to decorticate the inferior surface of coracoid preparing it for the bone transfer. The length of the coracoid is measured and the base of the coracoid is decorticated in its inferior, superior, medial and lateral surfaces. The coracoid drill guide with 7 mm offset (Arthrex) is introduced from the H portal. Then, 1.2-mm guidewires are drilled into the coracoid and they are over drilled using a 2.4-mm cannulated drill bit. A curved osteotome is used to detach the coracoid at its base. Viewing from the anterosuperior portal, the radiofrequency probe is introduced from the I portal and, the subscapularis tendon and muscle are split horizontally at the junction of upper two-thirds and lower one-third to expose the anteroinferior glenoid. The hooked stylus of the glenoid jig is inserted from the posterior portal and guidewires are drilled from posterior to anterior using the glenoid jig, and over-drilled with a 2.4-mm cannulated drill bit. Differently colored sutures are used in the superior and inferior holes, Nylon and PDS, for easy identification and to prevent suture entanglement during passage. A crochet hook is passed through the respective holes in the coracoid and the two suture limbs are pulled out through the M portal. The FiberTape cerclage tip is shuttled across the glenoid and coracoid, posteroanteriorly in the superior holes and anteroposteriorly in the inferior holes. The cerclage tape is locked in the premade knot of the construct. You can see that the coracoid is pulled onto the prepared anteroinferior surface of glenoid as the cerclage construct is tightened. The FiberTape cerclage construct is tensioned using the tensioner to 80 N. Care is taken to visualize the coracoid movement from the anterosuperior portal while the tapes are tensioned. This method gives a robust fixation of the coracoid on the antero-inferior glenoid and the position of the coracoid with respect to the glenoid is always accurate as the drilling of the holes is done using the jigs. The previously elevated capsulolabral complex is repaired to the anterior glenoid using 1.6-mm Fiber-Tak all-suture anchors. This exteriorizes the transferred coracoid preventing any impingement of the humeral head on the bony coracoid. A computed tomography scan is taken at 3 months to confirm bony union before allowing full range of motion and sporting activities.
References
- 1.Lafosse L., Lejeune E., Bouchard A., Kakuda C., Gobezie R., Kochhar T. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy. 2007;23:1242.e1–1242.e5. doi: 10.1016/j.arthro.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Boileau P., Gendre P., Baba M., Thélu C.É., Baring T., Gonzalez J.F., Trojani C. A guided surgical approach and novel fixation method for arthroscopic Latarjet. J Shoulder Elbow Surg. 2016;25:78–89. doi: 10.1016/j.jse.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Rashid M.S., Arner J.W., Millett P.J., Sugaya H., Emery R. The Bankart repair: Past, present, and future. J Shoulder Elbow Surg. 2020;29:e491–e498. doi: 10.1016/j.jse.2020.06.012. [DOI] [PubMed] [Google Scholar]
- 4.Petrera M., Patella V., Patella S., Theodoropoulos J. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surg Sports Traumatol Arthrosc. 2010;18:1742–1747. doi: 10.1007/s00167-010-1093-5. [DOI] [PubMed] [Google Scholar]
- 5.Zhu Y.M., Jiang C., Song G., Lu Y., Li F. Arthroscopic Latarjet procedure with anterior capsular reconstruction: Clinical outcome and radiologic evaluation with a minimum 2-year follow-up. Arthroscopy. 2017;33:2128–2135. doi: 10.1016/j.arthro.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 6.Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49:994–997. [PubMed] [Google Scholar]
- 7.Walch G., Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. Tech Shoulder Elbow Surg. 2000;1:256–261. [Google Scholar]
- 8.LeBus G.F., Chahla J., Sanchez G., et al. The Latarjet procedure at the National Football League scouting combine: An imaging and performance analysis. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117726045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hachem A.I., Rondanelli S.R., Rius X., Barco R. Latarjet cerclage: The all-arthroscopic metal-free fixation. Arthrosc Tech. 2021;10:e437–e450. doi: 10.1016/j.eats.2020.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vopat B.G., Cai W., Torriani M., et al. Measurement of Glenoid Bone Loss With 3-Dimensional magnetic resonance imaging: A matched computed tomography analysis. Arthroscopy. 2018;34:3141–3147. doi: 10.1016/j.arthro.2018.06.050. [DOI] [PubMed] [Google Scholar]
- 11.Skupiński J., Piechota M.Z., Wawrzynek W., Maczuch J., Babińska A. The bony Bankart lesion: How to measure the glenoid bone loss. Pol J Radiol. 2017;82:58–63. doi: 10.12659/PJR.898566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Di Giacomo G., Itoi E., Burkhart S.S. Evolving concept of bipolar bone loss and the Hill–Sachs lesion: From “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy. 2014;30:90–98. doi: 10.1016/j.arthro.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Woodmass J.M., Wagner E.R., Solberg M., Hunt T.J., Higgins L.D. Latarjet procedure for the treatment of anterior glenohumeral instability. JBJS Essent Surg Tech. 2019 25;9:e31. doi: 10.2106/JBJS.ST.18.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Menon A, Fossati C, Magnani M, Boveri S, Compagnoni R, Randelli PS. Low grade of osteoarthritis development after Latarjet procedure with a minimum 5 years of follow-up: A systematic review and pooled analysis [published online October 22, 2021]. Knee Surg Sports Traumatol Arthrosc.doi:10.1007/s00167-021-06771-w [DOI] [PMC free article] [PubMed]
- 15.Augat P., von Rüden C. Evolution of fracture treatment with bone plates. Injury. 2018;49(suppl 1):S2–S7. doi: 10.1016/S0020-1383(18)30294-8. [DOI] [PubMed] [Google Scholar]
- 16.Cohen M., Zaluski A.D., Siqueira G.S.L., Amaral M.V.G., Monteiro M.T., Filho G.R.M. Risk factors for coracoid graft osteolysis after the open Latarjet procedure. Rev Bras Ortop (Sao Paulo) 2020;55:585–590. doi: 10.1055/s-0039-1698799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Di Giacomo G., Costantini A., de Gasperis N., et al. Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: A computed tomography scan study of twenty-six patients. J Shoulder Elbow Surg. 2011;20:989–995. doi: 10.1016/j.jse.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 18.Lädermann A., Denard P.J., Burkhart S.S. Injury of the suprascapular nerve during Latarjet procedure: An anatomic study. Arthroscopy. 2012;28:316–321. doi: 10.1016/j.arthro.2011.08.307. [DOI] [PubMed] [Google Scholar]
- 19.Hurley E.T., Schwartz L.B., Mojica E.S., et al. Short-term complications of the Latarjet procedure: A systematic review. J Shoulder Elbow Surg. 2021;30:1693–1699. doi: 10.1016/j.jse.2021.01.024. [DOI] [PubMed] [Google Scholar]
- 20.Metais P., Clavert P., Barth J., et al. French Arthroscopic Society Preliminary clinical outcomes of Latarjet-Patte coracoid transfer by arthroscopy vs. open surgery: Prospective multicentre study of 390 cases [Erratum in: Orthop Traumatol Surg Res 2017;103:475.] Orthop Traumatol Surg Res. 2016;102:S271–S276. doi: 10.1016/j.otsr.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 21.Valenti P., Maroun C., Wagner E., Werthel J.D. Arthroscopic Latarjet procedure combined with bankart repair: A technique using 2 cortical buttons and specific glenoid and coracoid guides. Arthrosc Tech. 2018;7:e313–e320. doi: 10.1016/j.eats.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hardy A., Sabatier V., Schoch B., Vigan M., Werthel J.D., Study Investigators Latarjet with cortical button fixation is associated with an increase of the risk of recurrent dislocation compared to screw fixation. Knee Surg Sports Traumatol Arthrosc. 2020;28:2354–2360. doi: 10.1007/s00167-019-05815-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kleiner M.T., Payne W.B., McGarry M.H., Tibone J.E., Lee T.Q. Biomechanical Comparison of the Latarjet Procedure with and without capsular repair. Clin Orthop Surg. 2016;8:84–91. doi: 10.4055/cios.2016.8.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
An arthroscopic Latarjet procedure is demonstrated using a simplified FiberTape cerclage passage technique. A beach-chair position is used for the procedure. Diagnostic arthroscopy is performed using the arthroscope from the posterior portal. Hill–Sachs lesion and engagement of this humeral bone defect on the anterior glenoid are demonstrated taking the arm through the abduction and external rotation movement. Viewing from the posterior portal using a 70° arthroscope, rotator interval clearance is done. The capsulolabral complex is elevated from the 3-o’clock to the 6-o’clock position on the glenoid using a radiofrequency probe. The capsule is elevated away from the glenoid using a tag suture. The breadth of the glenoid is measured using a measuring device introduced from the coracoid portal. Viewing from the posterior portal using the 70° arthroscope, the lateral side of the coracoid is cleared of the coracoacromial ligament. The pectoralis minor is released from the medial aspect of coracoid using the radiofrequency probe from the H portal, preserving the conjoint tendon attachment to the tip of the coracoid bone. The undersurface of coracoid is cleared of soft tissue and a rotary burr is used to decorticate the inferior surface of coracoid preparing it for the bone transfer. The length of the coracoid is measured and the base of the coracoid is decorticated in its inferior, superior, medial and lateral surfaces. The coracoid drill guide with 7 mm offset (Arthrex) is introduced from the H portal. Then, 1.2-mm guidewires are drilled into the coracoid and they are over drilled using a 2.4-mm cannulated drill bit. A curved osteotome is used to detach the coracoid at its base. Viewing from the anterosuperior portal, the radiofrequency probe is introduced from the I portal and, the subscapularis tendon and muscle are split horizontally at the junction of upper two-thirds and lower one-third to expose the anteroinferior glenoid. The hooked stylus of the glenoid jig is inserted from the posterior portal and guidewires are drilled from posterior to anterior using the glenoid jig, and over-drilled with a 2.4-mm cannulated drill bit. Differently colored sutures are used in the superior and inferior holes, Nylon and PDS, for easy identification and to prevent suture entanglement during passage. A crochet hook is passed through the respective holes in the coracoid and the two suture limbs are pulled out through the M portal. The FiberTape cerclage tip is shuttled across the glenoid and coracoid, posteroanteriorly in the superior holes and anteroposteriorly in the inferior holes. The cerclage tape is locked in the premade knot of the construct. You can see that the coracoid is pulled onto the prepared anteroinferior surface of glenoid as the cerclage construct is tightened. The FiberTape cerclage construct is tensioned using the tensioner to 80 N. Care is taken to visualize the coracoid movement from the anterosuperior portal while the tapes are tensioned. This method gives a robust fixation of the coracoid on the antero-inferior glenoid and the position of the coracoid with respect to the glenoid is always accurate as the drilling of the holes is done using the jigs. The previously elevated capsulolabral complex is repaired to the anterior glenoid using 1.6-mm Fiber-Tak all-suture anchors. This exteriorizes the transferred coracoid preventing any impingement of the humeral head on the bony coracoid. A computed tomography scan is taken at 3 months to confirm bony union before allowing full range of motion and sporting activities.
An arthroscopic Latarjet procedure is demonstrated using a simplified FiberTape cerclage passage technique. A beach-chair position is used for the procedure. Diagnostic arthroscopy is performed using the arthroscope from the posterior portal. Hill–Sachs lesion and engagement of this humeral bone defect on the anterior glenoid are demonstrated taking the arm through the abduction and external rotation movement. Viewing from the posterior portal using a 70° arthroscope, rotator interval clearance is done. The capsulolabral complex is elevated from the 3-o’clock to the 6-o’clock position on the glenoid using a radiofrequency probe. The capsule is elevated away from the glenoid using a tag suture. The breadth of the glenoid is measured using a measuring device introduced from the coracoid portal. Viewing from the posterior portal using the 70° arthroscope, the lateral side of the coracoid is cleared of the coracoacromial ligament. The pectoralis minor is released from the medial aspect of coracoid using the radiofrequency probe from the H portal, preserving the conjoint tendon attachment to the tip of the coracoid bone. The undersurface of coracoid is cleared of soft tissue and a rotary burr is used to decorticate the inferior surface of coracoid preparing it for the bone transfer. The length of the coracoid is measured and the base of the coracoid is decorticated in its inferior, superior, medial and lateral surfaces. The coracoid drill guide with 7 mm offset (Arthrex) is introduced from the H portal. Then, 1.2-mm guidewires are drilled into the coracoid and they are over drilled using a 2.4-mm cannulated drill bit. A curved osteotome is used to detach the coracoid at its base. Viewing from the anterosuperior portal, the radiofrequency probe is introduced from the I portal and, the subscapularis tendon and muscle are split horizontally at the junction of upper two-thirds and lower one-third to expose the anteroinferior glenoid. The hooked stylus of the glenoid jig is inserted from the posterior portal and guidewires are drilled from posterior to anterior using the glenoid jig, and over-drilled with a 2.4-mm cannulated drill bit. Differently colored sutures are used in the superior and inferior holes, Nylon and PDS, for easy identification and to prevent suture entanglement during passage. A crochet hook is passed through the respective holes in the coracoid and the two suture limbs are pulled out through the M portal. The FiberTape cerclage tip is shuttled across the glenoid and coracoid, posteroanteriorly in the superior holes and anteroposteriorly in the inferior holes. The cerclage tape is locked in the premade knot of the construct. You can see that the coracoid is pulled onto the prepared anteroinferior surface of glenoid as the cerclage construct is tightened. The FiberTape cerclage construct is tensioned using the tensioner to 80 N. Care is taken to visualize the coracoid movement from the anterosuperior portal while the tapes are tensioned. This method gives a robust fixation of the coracoid on the antero-inferior glenoid and the position of the coracoid with respect to the glenoid is always accurate as the drilling of the holes is done using the jigs. The previously elevated capsulolabral complex is repaired to the anterior glenoid using 1.6-mm Fiber-Tak all-suture anchors. This exteriorizes the transferred coracoid preventing any impingement of the humeral head on the bony coracoid. A computed tomography scan is taken at 3 months to confirm bony union before allowing full range of motion and sporting activities.