Abstract
Background:
There are limited data on the use of video laryngoscopy for pediatric patients outside of the operating room.
Aim:
Our primary aim is to evaluate whether implementation of video laryngoscopy guided coaching for tracheal intubation is feasible with a high level of compliance and associated with a reduction in adverse tracheal intubation-associated events.
Methods:
This is a pre-post observational study of video laryngoscopy implementation with standardized coaching language for tracheal intubation in a single-center, pediatric intensive care unit. The use of video laryngoscopy as a coaching device with standardized coaching language was implemented as a part of practice improvement. All patients in the pediatric intensive care unit were included between January 2016 and December 2017 who underwent primary tracheal intubation with either video laryngoscopy or direct laryngoscopy. The uptake of the implementation, sustained compliance, tracheal intubation outcomes including all adverse tracheal intubation-associated events, oxygen desaturations (<80% SpO2), and first attempt success were measured.
Results:
Among 580 tracheal intubations, 284 (49%) were performed during the pre-implementation phase, and 296 (51%) post-implementation. Compliance for the use of video laryngoscopy with standardized coaching language was high (74% post-implementation) and sustained. There were no statistically significant differences in adverse tracheal intubation-associated events between the two phases (pre- 9% vs. post- 5%, absolute difference −3%, CI95: −8% to 1%, p = 0.11), oxygen desaturations <80% (pre- 13% vs. post- 13%, absolute difference 1%, CI95 −6% to 5%, p = 0.75), or first attempt success (pre- 73% vs. post- 76%, absolute difference 4%, CI95 −3% to 11%, p = 0.29). Supervisors were more likely to use the standardized coaching language when video laryngoscopy was used for tracheal intubation than with standard direct laryngoscopy (80% vs. 43%, absolute difference 37%, CI95 23% to 51%, p < 0.001).
Conclusions:
Implementation of video laryngoscopy as a supervising device with standardized coaching language was feasible with high level of adherence, yet not associated with an increased occurrence of any adverse tracheal intubation-associated events and oxygen desaturation.
Keywords: Airway management, pediatrics, endotracheal intubation, video laryngoscopy, tracheal intubation, PICU
Introduction
Tracheal intubation (TI) can be a life-saving maneuver; however, adverse tracheal intubation-associated events (TIAEs) are common in pediatric care environments (15-22%).1–7 Oxygen desaturation and adverse TIAEs occur more frequently when resident trainees are the laryngoscopist.1,5 There is also significant variability in the achievement of competency in TI amongst pediatric critical care fellows, suggesting a need for standardization of TI training.8 Literature indicates that adverse TIAEs are associated with worse ICU outcomes, such as longer duration of mechanical ventilation and ICU stay4, highlighting the importance of proper TI training.
Video laryngoscopy (VL), compared to traditional direct laryngoscopy (DL), is associated with higher TI success rates in multiple clinical environments, including pediatric ICUs (PICUs), neonatal ICUs (NICUs), adult ICUs, and emergency departments.9–12 However, a meta-analysis of randomized controlled trials comparing VL versus DL in pediatric patients found an increased rate of failed TI with VL and a prolonged time to completion.13
Based on this knowledge, we carried out a practice improvement project which aimed to improve TI safety while still prioritizing TI educational opportunities for trainees in our PICU. Our primary aim was to describe the uptake of our VL guided coaching intervention and sustained compliance for one year post-implementation. Our secondary aim was to assess the association of VL guided coaching with any adverse TIAEs, first attempt success, and oxygen desaturation. We hypothesized that the implementation of VL with structured coaching and post-procedure debriefing would be feasible at a high level of adherence and associated with a reduction in overall adverse TIAEs and oxygen desaturations.
Methods
Setting
We conducted a pre-post observational study of consecutive patients who underwent TI in the PICU at the Children’s Hospital of Philadelphia from January 1, 2016 through November 30, 2017. This study was designed in preparation for a large multicenter VL implementation study. Tracheal intubations in December 2016 were excluded due to a transition period between pre- and post-implementation. All primary TIs in the PICU were included. VL with non-standard (hyper-angulated) VL blades such as Airtraq (Prodol Meditec, Bilbao, Spain) and Glidescope (Verathon Inc, Bothell, WA, USA) in the both the pre- and post-implementation phases were excluded from the analysis. Tracheal tube exchange, tracheostomy, laryngeal mask placement, or TIs facilitated by flexible or rigid fiberoptic laryngoscopy were also excluded. These TIs were excluded due to the inability of laryngoscopists to perform direct laryngoscopy with these modalities (as opposed to the CMAC) and because many of these TIs were performed by non-PICU providers (anesthesiology, otolaryngology). This observational study met the criteria for exemption from review by the Institutional Review Board.
Intervention
The intervention consisted of VL implementation along with simulation-based coaching training for faculty and a standardized coaching language. The utilization of VL as a device to augment supervision and coaching was intended to provide more visual information and opportunity for better technical oversight by the supervisor during trainees’ performance of laryngoscopy with a direct view (DL technique). To preemptively address the drawbacks of VL supervision, including longer laryngoscopy time and technical challenges that arise from the discrepancy between the VL (supervisor) and DL (laryngoscopist) view,14 we implemented coaching training for VL supervisors, including senior critical care fellows (2nd and 3rd year fellows), attending physicians, and senior nurse practitioners. The training included hands-on VL device training and simulation-based coaching training that emphasized use of a standardized coaching language (detailed description below), outlined the potential benefits and drawbacks of VL, described the differences between the VL (supervisor) and DL (laryngoscopist) view, and highlighted best coaching practices.
Tracheal intubation data collection
All TI data were prospectively collected using the National Emergency Airway Registry for Children (NEAR4KIDS), an international QI registry for pediatric TI through the Pediatric Acute Lung Injury and Sepsis Investigator network.2,3,5 The NEAR4KIDS registry database includes de-identified patient, provider, and practice characteristics involved in the TI encounter, outcomes (e.g., attempt success, occurrence of adverse TIAEs, severe TIAEs, oxygen saturation), and process variances.3 Data collection followed a prospectively defined site-specific data compliance plan to ensure >95% of TI data capture with accuracy: the data were initially collected by clinicians at the time of each TI then followed by a standardized data verification process before the data entry. Monthly, site leaders (NN, AN) reviewed the consistency and completeness of the processes and outcomes data and reported it at a local quality and safety committee meeting.
Outcome definitions
Our primary outcome was to assess the feasibility and uptake of our VL guided coaching intervention. Adverse events were defined as TIAEs which includes both severe TIAEs and non-severe TIAEs. Severe TIAEs include cardiac arrest, esophageal intubation with delayed recognition, emesis with witnessed aspiration, hypotension requiring intervention, laryngospasm, malignant hypothermia, pneumothorax/pneumomediastinum, or direct airway injury and non-severe TIAEs include mainstem bronchial intubation, esophageal intubation with immediate recognition, hypertension requiring therapy, epistaxis, emesis without aspiration, dental or lip trauma, medication error, arrhythmia, and pain and/or agitation requiring additional medication and causing delay in intubation.3,5 Our secondary outcomes were the occurrence of any TIAEs, severe TIAEs, technical TIAEs (e.g., mainstem intubation, esophageal intubation, airway trauma, dental or lip trauma, and laryngospasm), severe oxygen desaturation defined as oxygen saturation <80% for those TIs with initial oxygen saturation >90%,15 and first attempt success.4,16
Video laryngoscopy implementation as a coaching device
After in-person simulation-based training for all critical care trainees and supervisors, who perform TI in the PICU, the C-MAC video laryngoscope (Karl Storz Inc, Germany) was introduced as a device to facilitate coaching of trainee performing TI and post-procedural debriefing after the TI procedure. We recommended that trainees or less experienced laryngoscopists use the C-MAC VL as a direct laryngoscopy device to continue to practice DL skills, without access to the video screen. The decision to use VL, and the laryngoscopist’s access to the video view, was determined by the supervisor through discussion with the laryngoscopist. As a result, when clinically indicated, the laryngoscopists used the video (indirect) view of the C-MAC to intubate the trachea. In some situations, providers considered the C-MAC VL blade size not suitable for the patient size and chose a standard DL blade instead. At the time of the project standard VL blades (Miller 1, Macintosh 2, and Macintosh 3 blades) were available for the C-MAC, and Miller 1, 2, Wisconsin-Hipple 1.5 straight blades and Macintosh 2 and 3 curved blades were available for DL in the PICU both pre- and post-implementation. Enabling video recording during the TI was encouraged by the supervisor for TI post-procedure debriefing, however, data on video recording were not captured in this study. This debriefing was expected to address specific aspects of anatomy, technique, and performance to improve laryngoscopist skills and to identify challenges encountered during TI, also known as technical debriefing.
Coaching language development
The C-MAC video laryngoscope allows supervisors the opportunity to view laryngoscopy on the video screen while the laryngoscopist performs TI using a direct view technique. Supervisors were trained to use specific succinct, standardized coaching language to instruct laryngoscopists and guide or adjust technique while performing the procedure. The concise coaching language (supplemental Figure A) was developed and piloted by an expert group of pediatric clinicians, educators, implementation scientists, and research scientists from the International Network for Simulation-base Pediatric Innovation, Research, and Education (INSPIRE). Once one or two preferred coaching phrases were chosen for each step of laryngoscopy, two experts in coaching language [NY, CMW] and the primary investigator [AN] helped to further refine the language. All providers, both TI supervisors and TI laryngoscopists, received in-person simulation-based training on the use of standardized coaching language for VL prior to implementation of the intervention.
TI coaching and procedure-related feedback data collection
To evaluate adherence to the VL coaching practice, we implemented an anonymous Research Electronic Data Capture (REDCap) survey to identify the merits and challenges of VL as a device to augment supervision and coaching and to identify common technical challenges and discrepancies in perception between laryngoscopists and supervisors. The survey was sent to involved airway providers (both laryngoscopists and supervisors) after each TI within 72 hours. Data were collected regarding the use of coaching language, encountered technical challenges, use of post-procedure debriefing, and procedure-related feedback offered during the post-procedure debriefing. These data points were merged with the local NEAR4KIDS data for analyses.
A priori, we determined the study period as the 11 months before (pre-implementation phase) and 11 months after (post-implementation phase) VL implementation to match the included months and control for secular trend (i.e., seasonal variability of patient population and provider training cycle), after excluding one month as a transition period. For summary statistics, categorical variables were described as numbers and percentages, and non-normally distributed continuous variables were summarized with median and interquartile ranges (IQR). The differences in the secondary outcomes between pre- and post- implementation phases were evaluated by Chi-squared tests at a two-sided significance level of 0.05. Data were analyzed using STATA 15.0 (College Station, TX, USA).
Results
Six hundred and twenty-one primary TIs occurred during the study period, of which 580 were performed with standard blade laryngoscopy. Of these, 284 (49%) were performed during the pre-implementation phase, and 296 (51%) post-implementation. Twenty-nine (5%) primary TIs were excluded due to use of non-standard VL blades, and 12 (2%) were excluded due to use of flexible or rigid fiberoptic scope. Twenty-one TIs (3%) were excluded in the pre-implementation phase and 20 (3%) excluded post-implementation. Patient demographics, indications for intubation, difficult airway features, and first attempt provider characteristics were not different between two phases, Table 1. Standard DL was used for all cases during the pre-implementation phase, and post-implementation, 219 (74%) TIs used VL and 77 (26%) used standard DL. There was a sustained high uptake of VL use during the post-implementation phase, with a mean of 74% of TIs performed using VL, Figure 1. Laryngoscopists reported using a direct view only in 124 (70%) of the VL intubations for which they completed survey data.
Table 1.
Patient and provider characteristics (N=580)
| Pre-Implementation of VL (N=284) | Post-Implementation of VL (N=296) | |
|---|---|---|
| Patient demographics | ||
| Age category (N, %) | ||
| Infant | 60 (21%) | 66 (22%) |
| Young child (-7 yrs) | 133 (47%) | 111 (37%) |
| Older child (8-17 yrs) | 78 (27%) | 100 (34%) |
| Adult (≥18 yrs) | 12 (5%) | 20 (7%) |
| Weight in kg (median, IQR) | 16.4 (9.3, 32.8) | 17.8 (9.4, 39.5) |
| Sex (male, %) | 154 (54%) | 152 (51%) |
| Indication | ||
| Respiratory | 171 (60%) | 161 (54%) |
| Shock | 23 (8%) | 24 (8%) |
| Neurological | 33 (12%) | 46 (16%) |
| Procedural | 110 (39%) | 113 (38%) |
| History of difficult airway | 53 (19%) | 48 (16%) |
| Difficult airway feature(s) | 75 (26%) | 61 (21%) |
| First attempt provider | ||
| Resident | 11 (4%) | 13 (4.5%) |
| Fellow | 179 (63%) | 195 (66%) |
| Attending | 11 (4%) | 18 (6%) |
| Nurse practitioner/hospitalist | 55 (19%) | 57 (19%) |
| Subspecialist/other | 28 (10%) | 13 (4.5%) |
Figure 1:
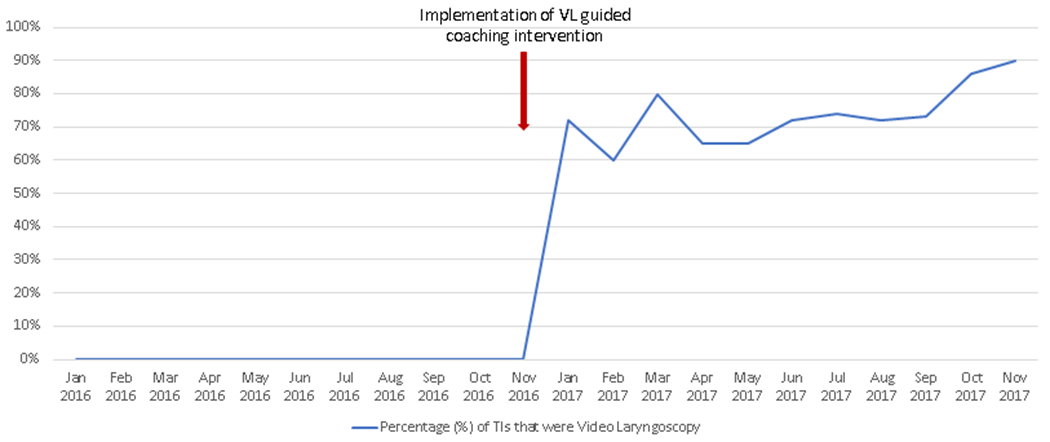
Video laryngoscopy (VL) usage by month
Comparisons of outcomes between pre- and post-implementation
There were no statistically significant differences for the secondary outcome of overall adverse TIAEs between the pre-implementation (25/284: 9%) and post-implementation phases (16/296: 5%), absolute difference −3%, CI95: −8% to 1%, p = 0.11, Table 2. There were no statistically significant differences in the number of technical TIAEs (pre- 6% vs. post- 3%, absolute difference −3%, CI95 −6% to 1%, p = 0.1), severe TIAEs (pre- 2% vs. post- 2%, absolute difference −1%, CI95 −3% to 2%, p = 0.51), desaturations (pre- 13% vs. post- 13%, absolute difference 1%, CI95 −6% to 5%, p = 0.75), or first attempt successes (pre- 73% vs. post- 76%, absolute difference 4%, CI95 −3% to 11%, p = 0.29).
Table 2.
Outcomes for Pre- versus Post- Implementation of Video Laryngoscopy with structured coaching and post-procedure debriefing
| Outcome | Pre-Implementation of VL (N=284) | Post-Implementation of VL (N=296) | P-value | Absolute Difference |
|---|---|---|---|---|
| Overall TIAEs | 25 (9%) | 16 (5%) | 0.11 | −3%, CI95: −8% to 1% |
| Technical TIAEs | 18 (6%) | 10 (3%) | 0.1 | −3%, CI95 −6% to 1% |
| Severe TIAEs | 7 (2%) | 5 (2%) | 0.51 | −1%, CI95 −3% to 2% |
| Oxygen Desaturations | 38 (13%) | 37 (13%) | 0.75 | 1%, CI95 −6% to 5% |
| First attempt successes | 206 (73%) | 226 (76%) | 0.29 | 4%, CI95 −3% to 11% |
VL denotes video laryngoscopy
TIAE denotes tracheal intubation associated events
Technical TIAE includes: mainstem intubation, esophageal intubation, airway trauma, dental or lip trauma, and laryngospasm
Severe TIAE includes: cardiac arrest, esophageal intubation with delayed recognition, emesis with witnessed aspiration, hypotension requiring intervention, laryngospasm, malignant hyperthermia, pneumothorax/pneumomediastinum, or direct airway injury
Oxygen desaturation is defined as <80% for those TIs with initial oxygen saturation >90%
The detailed definitions are described in the methods
Comparisons of outcomes with DL versus VL post-implementation
Among the 296 TIs completed during the post-implementation phase, there were no statistically significant differences between DL versus VL regarding overall adverse TIAEs (DL 9% vs. VL 4%, absolute difference −5%, CI95 −12% to 2%, p = 0.1), technical TIAEs (DL 4% vs. VL 3%, absolute difference −1%, CI95 −6% to 4%, p = 0.77), severe TIAEs (DL 4% vs. VL 1%, absolute difference −3%, CI95 −7% to 2%, p = 0.08), oxygen desaturations (DL 10% vs. VL 13%, absolute difference 3%, CI95 −5% to 11%, p = 0.52), or first attempt successes (DL 73% vs. VL 78%, absolute difference 5%, CI95 −6% to 16%, p = 0.38), Table 3.
Table 3.
Outcomes for Direct Laryngoscopy versus Video Laryngoscopy during the Post-implementation Phase (N=296)
| Outcome | DL (n=77) | VL (n=219) | P-value | Absolute Difference |
|---|---|---|---|---|
| Overall TIAEs | 7 (9%) | 9 (4%) | 0.1 | −5%, CI95 −12% to 2% |
| Technical TIAEs | 3 (4%) | 7 (3%) | 0.77 | −1%, CI95 −6% to 4% |
| Severe TIAEs | 3 (4%) | 2 (1%) | 0.08 | −3%, CI95 −7% to 2% |
| Oxygen Desaturations | 8 (10%) | 29 (13%) | 0.52 | 3%, CI95 −5% to 11% |
| First attempt successes | 56 (73%) | 170 (78%) | 0.38 | 5%, CI95 −6% to 16% |
DL denotes direct laryngoscopy
VL denotes video laryngoscopy
TIAE denotes tracheal intubation associated events
Technical TIAE includes: mainstem intubation, esophageal intubation, airway trauma, dental or lip trauma, and laryngospasm
Severe TIAE includes: cardiac arrest, esophageal intubation with delayed recognition, emesis with witnessed aspiration, hypotension requiring intervention, laryngospasm, malignant hyperthermia, pneumothorax/pneumomediastinum, or direct airway injury
Oxygen desaturation is defined as <80% for those TIs with initial oxygen saturation >90%
The detailed definitions are described in the methods
Coaching language use and post-procedure debriefing post-implementation
Both laryngoscopists and supervisors consistently reported more frequent use of standardized coaching language with VL (laryngoscopist: DL 45% vs. VL 73%, absolute difference 28%, CI95 14% to 42%, p < 0.001, supervisor: DL 43% vs. VL 80%, absolute difference 37%, CI95 23% to 51%, p < 0.001), Table 4. A post-procedure debriefing occurred after the majority of laryngoscopy cases (DL: 76%, VL 75%, supervisor report). Laryngoscopists reported the post-procedure debrief to be helpful in 213 (89%) of laryngoscopy cases with completed surveys.
Table 4.
Post-Implementation Survey Results: Coaching Language Use, Technical Challenges, Debriefing, and Post-Procedure Feedback for Tracheal Intubations
| Outcome | Laryngoscopist Report (N=239) | Supervisor Report (N=248) | ||||
|---|---|---|---|---|---|---|
| Direct laryngoscopy (N=62) | Video laryngoscopy (N=177) | P-value | Direct laryngoscopy (N=60) | Video laryngoscopy (N=188) | P-value | |
| Coaching Language Used | 28 (45%) | 129 (73%) | <0.001 | 26 (43%) | 151 (80%) | <0.001 |
| Technical Challenges | 10 (16%) | 46 (26%) | 0.12 | 10 (17%) | 45 (24%) | 0.29 |
| Post-procedure Debrief Performed | 40 (66%) | 128 (72%) | 0.33 | 45 (76%) | 141 (75%) | 1 |
| Procedure-Related Feedback | 17 (27%) | 57 (32%) | 0.53 | 18 (30%) | 60 (32%) | 0.87 |
Technical challenges encountered during laryngoscopy and procedure-related feedback by supervisors
Technical challenges were reported by supervisors for 17% of DLs and 24% of VLs . Procedure-related feedback was provided by supervisors for 30% of DLs and 32% of VLs. Laryngoscopists reported similar results, Table 4. Difficulty with neck flexion/extension was reported more often for DL (10%), while difficulty in handling the epiglottis was reported more commonly for VL (9%), Table 5. Common technical suggestions included optimizing patient positioning (DL: 7%, VL 10%) and different laryngoscopy handling (DL 10%, VL 13%) in both groups.
Table 5.
Technical Challenges Encountered and Procedure-related Feedback as Reported by Supervisors Post-Implementation
| Supervisor Reported Challenges | Tracheal Intubations (N=248) | ||
|---|---|---|---|
| Direct laryngoscopy (N=60) | Video laryngoscopy (N=188) | P-value | |
| Technical Challenges | |||
| Difficulty with neck flexion/extension | 6 (10%) | 14 (7%) | 0.59 |
| Difficulty with laryngoscope insertion | 2 (3%) | 10 (5%) | 0.74 |
| Difficulty lifting laryngoscope without rocking | 2 (3%) | 11 (6%) | 0.74 |
| Difficulty handling tongue | 3 (5%) | 10 (5%) | 1 |
| Difficulty handling epiglottis | 2 (3%) | 17 (9%) | 0.175 |
| Difficulty with communication | 0 (0%) | 2 (1%) | 1 |
| Other challengesa | 9 (15%) | 16 (9%) | 0.15 |
| Procedure-Related Feedback Provided | |||
| Optimize patient positioning | 4 (7%) | 20 (10%) | 0.46 |
| Optimize body mechanics | 2 (3%) | 4 (2%) | 0.63 |
| Optimize patient physiology | 2 (3%) | 2 (1%) | 0.25 |
| Different equipment choice | 1 (2%) | 7 (4%) | 0.68 |
| Different equipment preparation | 2 (3%) | 9 (5%) | 1 |
| Improved communication | 2 (3%) | 4 (2%) | 0.64 |
| Crowd control | 2 (3%) | 1 (1%) | 0.15 |
| Better role assignment | 0 (0%) | 1 (1%) | 1 |
| Better understanding of anatomy | 3 (5%) | 15 (8%) | 0.57 |
| Different laryngoscopy handling | 6 (10%) | 24 (13%) | 0.66 |
| Other suggestionsb | 4 (7%) | 11 (6%) | 0.76 |
Other challenges included: Tube styletting, CPR ongoing, pulmonary hemorrhage, C-spine precautions
Other suggestions included: Techniques for dealing with secretions, tube handling
Discussion
In this prospective observational study, we demonstrated that implementing VL with standardized coaching language and post-procedure debriefing is feasible with sustained high compliance for one year after implementation in a large academic PICU. Post-implementation, there were no significant changes in TI outcomes including any TIAEs, oxygen desaturations, or first attempt successes. Both laryngoscopists and supervisors reported a high frequency of standardized coaching language use during TI in the post-implementation phase.
There is limited data on the use of VL for pediatric patients outside of the operating room environment, especially for use in supervising and coaching trainees and relatively inexperienced laryngoscopists.12,17 A recent study demonstrated that VL was associated with a higher first-attempt success rate and fewer complications in young infants in the operating room.18 The use of video laryngoscopy in the PICU has been associated with a decreased rate of adverse TIAEs.12 Our study had a lower rate of adverse TIAEs than previously described in the PICU, and was not powered to detect a difference between the two groups. In adult practice, there remains considerable controversy surrounding the use of VL in the emergency and ICU settings. A recent meta-analysis of randomized, controlled trials comparing VL to DL did not demonstrate a difference in first-attempt success rate between the two methods.19
We implemented VL as a device to augment trainee supervision and coaching so that trainees could continue to practice direct laryngoscopy. This approach was taken as our local PICU leadership felt it was important for trainees and junior providers to continue to develop their DL skills after VL implementation because VL is not available in many clinical environments.
This use of VL as a coaching device has been examined in the NICU.20,21 O’Shea randomized neonates to undergo TI with or without the video screen available to supervisors and demonstrated a significant improvement in TI success when the video screen was available (66%) as compared to when it was covered (41%). Notably, standardized coaching language was not used in this study. The other study by Volz conducted a pilot randomized trial for neonatal intubation to compare VL combined with structured coaching versus DL, and demonstrated higher TI success with VL. Importantly, this study did not examine whether use of the coaching language differed between the two groups. Our study implemented VL with standardized coaching language and post-procedure debriefing and documented the high frequency of coaching language use for direction and redirection at critical points during laryngoscopy. Additionally, implementation of VL with standardized coaching language was not associated with an increase in patient-centered adverse outcomes, suggesting that this technique can be safely implemented as a practice improvement intervention in the PICU setting. This is especially pertinent, as some prior VL studies have demonstrated increased TI attempt failure rates, prolonged laryngoscopy time, and greater oxygen desaturations when compared to traditional DL for pediatric intubation.13
To date, there is little information regarding technical challenges encountered in performing TI in the PICU setting. Our study provided a detailed description of the technical challenges and suggested solutions. While not statistically different, more difficulties with neck positioning were reported with DL, as it may be more easily detected by supervisors when their eyes are not focused on the video screen. Alternatively, more difficulty with handling of the epiglottis was reported with VL, as it would not be easily known to supervisors without the video screen during regular DL unless expressly communicated by the laryngoscopist. Interestingly, the quantity of procedure-related feedback provided by supervisors was similar for VL and DL, with feedback related to laryngoscopy handling and patient positioning being most common. Understanding technical challenges commonly encountered during TI may provide the opportunity to improve both the safety of the procedure and the educational approach for pediatric trainees. A recent small neonatal study demonstrated a difference in laryngoscopists’ perceptions of intubation success (21% success reported) as compared to neonatologist confirmation (6% success reported) via video review in TIs performed for aspirating meconium from the trachea.22 Understanding differences in how laryngoscopists and supervisors perceive challenges encountered during TI provides a clue for further educational interventions. Although not explored in this study, the ability of the video screen to allow the supervisor to visualize and troubleshoot difficult airways may also potentially augment the trainee experience, providing information and reassurance to allow the laryngoscopist to take a second attempt at intubation rather than taking over.
Our study showed that the majority of laryngoscopists reported the post-procedure debriefing to be helpful despite no difference in patient outcomes. This is consistent with the existing literature in pediatric emergency care. Video recording review after laryngoscopy is perceived as a valuable educational opportunity for airway providers23 and can provide useful information about the procedural approach and associated adverse events.24
This study has several limitations. It was conducted at a single academic PICU as a feasibility study and may not be generalizable to other clinical settings. The study’s primary purpose was to assess the feasibility of and adherence to VL guided coaching and post-procedure debriefing. Therefore, the limited the sample size (type II error) is a possible explanation for the non-significant TI outcome results. Apneic oxygenation practice was implemented in August 2016 during our study period.25 This likely confounded our results, especially for the oxygen desaturation rate. There may have been more of a difference between oxygen desaturation rates between implementation periods without this practice and thus this may have biased this comparison towards the null. Additionally, by potentially allowing more time for intubation without oxygen desaturation, apneic oxygenation may have also impacted the first attempt success rate. There was an ongoing quality improvement effort to improve TI safety in the PICU throughout the study period. Therefore, we were not able to control for the secular trend and other unmeasured sources of biases due to the nature of a single center pre-post study design. The use of coaching language and post-procedure debriefing, and technical challenges encountered are based on the anonymous survey results from laryngoscopists and supervisors and are, therefore, subject to reporting and recall bias. The consistent response results from both laryngoscopists and supervisors, however, suggest the impact of this bias may be small. We did not objectively measure the quality or frequency of coaching language used, so any variability in the use of coaching language by supervisors is unknown; potential effects such as a dose response to coaching language were not assessed. There is also the possibility of under reporting of adverse events. Standard operating definitions were followed with rigorous compliance monitoring and validation procedures to minimize inaccuracy.
Conclusion
This single-center observational study demonstrated the feasibility of VL implementation with standardized coaching language and post-procedure debriefing in the PICU, with sustained compliance for one year post-implementation. There were no significant differences in TIAEs, oxygen desaturation, or first attempt success between the pre- and post-implementation phases. Post-procedure debriefing occurred often and reported as helpful by laryngoscopists.
Supplementary Material
Clinical Implications.
What is already known about the topic:
Adverse tracheal intubation-associated events are common in pediatric care environments and there is significant variability in the achievement of competency in tracheal intubation amongst pediatric care providers.
What new information this study adds:
It is feasible to implement video laryngoscopy supervision of tracheal intubation with standardized coaching language in a pediatric intensive care unit with a high level of adherence, and it is not associated with an increased occurrence of any adverse tracheal intubation-associated events.
Financial support/COI
This study was supported by Agency for Healthcare Research and Quality: AHRQ R03HS021583, AHRQ R18HS022464, R18HS024511 and Endowed Chair, Critical Care Medicine, The Children’s Hospital of Philadelphia.
Ms. Napolitano and Drs. Nadkarni and Nishisaki are supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development R21 HD089151.
Ms. Napolitano has received support from Draeger, Aerogen, Vero Biotech, Smiths Medical, Actuated Medical, and NHLBI 1UG3HL141736-01/1U24HL141723-01.
Data Availability Statement:
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Foglia EE, Ades A, Napolitano N, Leffelman J, Nadkarni V, Nishisaki A. Factors Associated with Adverse Events during Tracheal Intubation in the NICU. Neonatology. 2015;108(1):23–29. doi: 10.1159/000381252 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nett S, Emeriaud G, Jarvis JD, Montgomery V, Nadkarni VM, Nishisaki A. Site-level variance for adverse tracheal intubation-associated events across 15 North American PICUs: a report from the national emergency airway registry for children*. Philadelphia, PA: ] :: Lippincott Williams & Wilkins; 2014. p. 306–313. [DOI] [PubMed] [Google Scholar]
- 3.Nishisaki A, Turner DA, Brown CA, 3rd, et al. A National Emergency Airway Registry for children: landscape of tracheal intubation in 15 PICUs. Critical Care Medicine. 2013;41(3):874–885. doi: 10.1097/CCM.0b013e3182746736 [doi] [DOI] [PubMed] [Google Scholar]
- 4.Parker MM, Nuthall G, Brown C, 3rd, et al. Relationship Between Adverse Tracheal Intubation Associated Events and PICU Outcomes. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2017;doi: 10.1097/PCC.0000000000001074 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanders RC Jr., Giuliano JS Jr., Sullivan JE, et al. Level of trainee and tracheal intubation outcomes. Pediatrics. 2013;131(3):821. doi: 10.1542/peds.2012-2127 [doi] [DOI] [PubMed] [Google Scholar]
- 6.Branca A, Tellez D, Berkenbosch J, et al. The New Trainee Effect in Tracheal Intubation Procedural Safety Across PICUs in North America: A Report From National Emergency Airway Registry for Children*. Pediatric Critical Care Medicine. 2020;21(12) [DOI] [PubMed] [Google Scholar]
- 7.Nishisaki A, Lee A, Li S, et al. Sustained Improvement in Tracheal Intubation Safety Across a 15-Center Quality-Improvement Collaborative: An Interventional Study From the National Emergency Airway Registry for Children Investigators*. Critical Care Medicine. 2021;49(2) [DOI] [PubMed] [Google Scholar]
- 8.Ishizuka M, Rangarajan V, Sawyer TL, et al. The Development of Tracheal Intubation Proficiency Outside the Operating Suite During Pediatric Critical Care Medicine Fellowship Training: A Retrospective Cohort Study Using Cumulative Sum Analysis. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2016;17(7):309. doi: 10.1097/PCC.0000000000000774 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moussa A, Luangxay Y, Tremblay S, et al. Videolaryngoscope for Teaching Neonatal Endotracheal Intubation: A Randomized Controlled Trial. Pediatrics. 2016;137(3):e20152156–2156. Epub 2016 Feb 12. doi: 10.1542/peds.2015-2156 [doi] [DOI] [PubMed] [Google Scholar]
- 10.Hypes CD, Stolz U, Sakles JC, et al. Video Laryngoscopy Improves Odds of First-Attempt Success at Intubation in the Intensive Care Unit. A Propensity-matched Analysis. Annals of the American Thoracic Society. 2016;13(3):382–390. doi: 10.1513/AnnalsATS.201508-505OC [doi] [DOI] [PubMed] [Google Scholar]
- 11.Sakles JC, Mosier J, Chiu S, Cosentino M, Kalin L. A comparison of the C-MAC video laryngoscope to the Macintosh direct laryngoscope for intubation in the emergency department. Annals of Emergency Medicine. 2012;60(6):739–748. doi: 10.1016/j.annemergmed.2012.03.031 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grunwell JR, Kamat PP, Miksa M, et al. Trend and Outcomes of Video Laryngoscope Use Across PICUs. Philadelphia, PA: ] :: Lippincott Williams & Wilkins; 2017. p. 741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun Y, Lu Y, Huang Y, Jiang H. Pediatric video laryngoscope versus direct laryngoscope: a meta-analysis of randomized controlled trials. Paediatric anaesthesia. 2014;24(10):1056–1065. doi: 10.1111/pan.12458 [doi] [DOI] [PubMed] [Google Scholar]
- 14.Donoghue AJ, Ades AM, Nishisaki A, Deutsch ES. Videolaryngoscopy versus direct laryngoscopy in simulated pediatric intubation. Annals of Emergency Medicine. 2013;61(3):271–277. doi: 10.1016/j.annemergmed.2012.09.008 [doi] [DOI] [PubMed] [Google Scholar]
- 15.Nishisaki A, Ferry S, Colborn S, et al. Characterization of tracheal intubation process of care and safety outcomes in a tertiary pediatric intensive care unit. Philadelphia, PA: ] :: Lippincott Williams & Wilkins; 2012. p. 5. [DOI] [PubMed] [Google Scholar]
- 16.Li S, Hsieh T-C, Rehder KJ, et al. Frequency of Desaturation and Association With Hemodynamic Adverse Events During Tracheal Intubations in PICUs. Philadelphia, PA: ] :: Lippincott Williams & Wilkins; 2018. p. e41–e50. [DOI] [PubMed] [Google Scholar]
- 17.Pouppirt NR, Nassar R, Napolitano N, et al. Association Between Video Laryngoscopy and Adverse Tracheal Intubation-Associated Events in the Neonatal Intensive Care Unit. St. Louis, MO: :: Mosby Inc; 2018. p. 281–284.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garcia-Marcinkiewicz AG, Kovatsis PG, Hunyady AI, et al. First-attempt success rate of video laryngoscopy in small infants (VISI): a multicentre, randomised controlled trial. Lancet (London, England). 2020;396(10266):1905–1913. doi:S0140-6736(20)32532-0 [pii] [DOI] [PubMed] [Google Scholar]
- 19.Jiang J, Ma D, Li B, Yue Y, Xue F. Video laryngoscopy does not improve the intubation outcomes in emergency and critical patients - a systematic review and meta-analysis of randomized controlled trials. London: ] :: Current Science Ltd; 2017. p. 288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Volz S, Stevens TP, Dadiz R. A randomized controlled trial: does coaching using video during direct laryngoscopy improve residents’ success in neonatal intubations? Philadelphia, Pa.] :: WB Saunders; 2018. p. 1074–1080. [DOI] [PubMed] [Google Scholar]
- 21.O’Shea JE, Thio M, Kamlin CO, et al. Videolaryngoscopy to Teach Neonatal Intubation: A Randomized Trial. Pediatrics. 2015;136(5):912–919. doi: 10.1542/peds.2015-1028 [DOI] [PubMed] [Google Scholar]
- 22.Robinson M-È, Diaz I, Barrowman NJ, Huneault-Purney N, Lemyre B, Rouvinez-Bouali N. Trainees success rates with intubation to suction meconium at birth. London: ] :: BMJ Pub Group; 2018. p. F413–F416. [DOI] [PubMed] [Google Scholar]
- 23.Nagler J, Nagler A, Bachur RG. Development and Assessment of an Advanced Pediatric Airway Management Curriculum With Integrated Intubation Videos. Philadelphia, PA: :: Lippincott Williams & Wilkins; 2017. p. 239–244. [DOI] [PubMed] [Google Scholar]
- 24.Green-Hopkins I, Werner H, Monuteaux MC, Nagler J. Using Video-recorded Laryngoscopy to Evaluate Laryngoscopic Blade Approach and Adverse Events in Children. Philadelphia, PA: :: Hanley & Belfus; 2015. p. 1283–1289. [DOI] [PubMed] [Google Scholar]
- 25.Napolitano N, Laverriere EK, Craig N, et al. Apneic Oxygenation As a Quality Improvement Intervention in an Academic PICU. (1529–7535 (Print)) [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


