Abstract
In the twenty-first century, exposure to air pollution has become a threat to human health worldwide due to industrial development. Timely, comprehensive, and reliable assessment and prediction of disease burden can help mitigate the health hazards of air pollution. This study conducted a two-stage analysis. First, we reported the air pollution–related disease burden globally and for different subgroups like socio-demographic index (SDI), sex, and age. We analyzed the trend of the disease burden from 1990 to 2019. In addition, we explored whether and how some national indicators modified the disease burden. Second, we predicted the number and the age-standardized rates of death and disability-adjusted life years (DALYs) attributable to air pollution from 2020 to 2044 by the autoregressive integrated moving average (ARIMA) model and exponential smoothing model. The age-period-cohort (APC) model in the maximum likelihood framework and the Bayesian APC model integrated nested Laplace approximations (INLAs) were further applied to perform sensitivity analysis. In 2019, air pollution accounted for 11.62% of death and 0.84% of DALY worldwide. The corresponding age-standardized rate was 85.62 (95% uncertainty interval (UI): 75.71, 96.07) and 2791.08 (95% UI: 2468.81, 3141.39) per 100,000 population. From 1990 to 2019, the number of death attributable to air pollution remained stable, and the number of DALY exhibited a downward trend. The corresponding age-standardized rates both declined. In some countries with larger population densities, higher proportions of elders, and lower proportions of females, the disease burden attributable to air pollution was lower. The predicted results showed that the number of air pollution-related death and DALY would increase. This study comprehensively assessed and predicted the air pollution–related disease burden worldwide. The results indicated that the disease burden would remain very serious in the future. Hence, some relevant policies should be developed to prevent and manage air pollution.
Supplementary information
The online version contains supplementary material available at 10.1007/s11356-022-22318-z.
Keywords: Air pollution, Disease burden, Trend, Assessment, Prediction, Global
Introduction
Ambient air pollution was considered a risk factor for premature death with a high direct and indirect impact on the social burden (Cohen et al. 2017). Recently, it has attracted the attention of quite a few researchers (Shahrbaf et al. 2021; Noorimotlagh et al. 2021; Schraufnagel et al. 2019). Studies showed that exposure to air pollution increased the risk of respiratory disease, cardiovascular disease, type 2 diabetes, and cancers in the long term (Beelen et al. 2014; Hoek et al. 2013; Newby et al. 2015; Brook et al. 2017). Air pollution caused nearly nine million preventable premature deaths worldwide each year and shortened life expectancy worldwide by almost 3 years (Münzel et al. 2021). Air pollution had gotten worse over the past 3 years. Research showed that if we did not take any proactive interventions, air pollution–related deaths would double by 2050. In addition to the impact on human health, air pollution could also cause huge economic losses, with an estimated annual loss of 3.8 trillion US dollars (McNutt and Dzau 2019). Therefore, a timely, comprehensive, and reliable assessment and prediction of the global air pollution-related disease burden was required.
Among all air pollutants, ozone and particulate matter were of concern due to their negative effects on terrestrial ecosystems. Research by Guarin et al. showed that about 90% of the European urban population was currently exposed to high levels of ozone pollution (Guarin et al. 2019). In 2018, ozone concentrations in 14 of 36 European countries exceeded the WHO threshold more than 25 times per year, with 87% of monitoring stations monitoring ozone values that exceeded long-term target thresholds set by European authorities. Ozone pollution increased people’s risk of chronic respiratory and cardiovascular disease (McDonnell et al. 2010; Europe 2013; Chen et al. 2018; Rohr 2018). Short-term exposure to ozone might also lead to decreased lung mucociliary function, thereby weakening the body’s resistance (Balajee et al. 2017). About 16,400 people died prematurely in the EU each year due to ozone pollution. The particulate matter was a major risk factor affecting human health. And the particulate matter was closely associated with cardiovascular, respiratory, and neurovascular disease (Shah et al. 2015; Gowers et al. 2012; Bloemsma et al. 2016). Due to their small size, the particulate matter could enter the body and cause some diseases, including respiratory diseases (Tian et al. 2020). Studies showed that PM2.5 might induce airway inflammation and exacerbate wheezing symptoms in COPD patients (Chi et al. 2016). For every 10 μg/m3 increase in PM2.5 concentration, the risk of death from lung cancer increased by 9% (Krewski et al. 2009). In addition, PM2.5 also had short-term and long-term effects on pneumonia (Tian et al. 2019; Zhang et al. 2017). There was also an association with COVID-19 (Yao et al. 2020).
However, there were no studies that systematically assessed the global burden of air pollution–related disease in recent years. Most studies exploring the air pollution-related disease burden were conducted in one or several countries (Nunes et al. 2021; Khomenko et al. 2021; India State-Level Disease Burden Initiative Air Pollution Collaborators 2021b). Due to the different timing of the studies and the inconsistent methods of data collection and processing, it was difficult to compare and synthesize the results of these studies. Therefore, to prevent and control air pollution, it was urgent to assess the global air pollution–related disease burden, predict its development trend, and provide a basis for the formulation of relevant health policies. The Global Burden of Disease (GBD) Study 2019 listed air pollution as a risk factor (GBD 2019 Risk Factors Collaborators, 2020). The database contained air pollution–related data on the death and disability-adjusted life years (DALY) from 1990 to 2019. It used standardized methods for data collection and processing to systematically assess the air pollution–related disease burden worldwide from 1990 to 2019, providing globally representative and comparable results.
In recent years, research on disease burden has become more and more popular. Regrettably, most studies only estimated the disease burden (Jin et al. 2016; Muthiah and Sanyal 2020). To analyze the air pollution–related disease burden more comprehensively, we combined disease burden prediction and disease burden assessment. The model used for disease burden assessment was mainly a linear regression model (Li et al. 2021; Lin et al. 2021). Numerous models were used to predict the disease burden such as the autoregressive integrated moving average (ARIMA) model (Ceylan 2020; Zheng et al. 2020) and the exponential smoothing model (Fu et al. 2021; Liu et al. 2020) in the time series model, and the age-period-cohort (APC) model (Akita et al. 2014; Ji et al. 2019). Some studies compared the two models in the time series model (Adeyinka and Muhajarine 2020; Lin et al. 2021; Gecili et al. 2021), but the results were not consistent. This research innovatively combined the three models, compared the ARIMA model and the exponential smoothing model to determine the optimal model, and used the APC model for sensitivity analysis.
The purpose of this study was as follows. First, we aimed to report the air pollution–related disease burden globally and in different subgroups such as region, sociodemographic index (SDI), sex, and age in 2019. Second, we aimed to explore the trend of changes in the air pollution–related disease burden from 1990 to 2019. Third, we explored how and if the air pollution-related disease burden was modified by some national indicators. Finally, we aimed to use the ARIMA model and exponential smoothing model in the time series analysis to predict the air pollution–related disease burden from 2020 to 2044 and determine the optimal model. Furthermore, we applied the APC model in the maximum likelihood framework and the Bayesian APC model integrated nested Laplace approximations (INLAs) for sensitivity analysis. The findings of this study provided an evidence-based assessment of the effectiveness of current control and preventive measures, helped researchers fully understand the impact of global air pollution on human health, and provided a basis for policy-makers.
Methods
Data collection
The data on air pollution–related death and DALY from 1990 to 2019 were extracted from the GBD Study 2019 website (http://www.globalburden.org/). This was free of charge provided by the Institute for Health Metrics and Evaluation (IHME). The data for air pollution in the GBD database included two pollutants, ambient ozone pollution, and particulate matter pollution. The GBD study 2019 was a systematic survey that assesses the health effects of diseases, injuries, and risk factors based on age, sex, and region. The details of the methodology had been described in previous publications (GBD 2019 Blindness and Vision Impairment Collaborators 2021a; Roth et al. 2020; GBD 2017 Causes of Death Collaborators 2018). The following was a brief introduction to the GBD study 2019. First, the period of this study was from 1990 to 2019. Second, the scope of the study was global. All countries and territories were divided into 7 super-regions and 21 regions based on geographic contiguity and epidemiological homogeneity. At the same time, all countries and territories were divided into five areas according to the socio-demographic index (SDI) indicator. They were high SDI, high-middle SDI, middle SDI, low-middle SDI, and low SDI. The SDI indicator was a comprehensive measure of developmental level based on average education level, total fertility, and per capita income, ranging from worst zero to best one hundred. We chose air pollution from the database as the risk, death, and DALY for measures.
We collected the following national indicators from the World Bank databases to explore some potential factors affecting the disease burden attributable to air pollution (https://databank.worldbank.org/home.aspx#): (1) greening indicator: forest area; (2) demographic indicators: including the proportion of the population ages 65 years and above in the total population, population density, population growth, and female of the total population; (3) socioeconomic indicators: including adjusted national income, adjusted national income per capita, annual GDP growth, and annual GDP per capita growth; (4) urban characteristic: urban population of the total population. Since partial data were missed, we selected the above data from 121 countries and territories from 1990 to 2019 in the end.
The data of the APC model were as follows. The population forecast data came from the 2019 revised edition of the population of the world outlook (https://population.un.org/wpp/Download/Standard/CSV/). The standardization of the World Health Organization (WHO) in 2000–2025 demographic data came from a public website (https://seer.cancer.gov/stdpopulations/world.who.html/).
Statistical analysis
This study conducted a two-stage analysis: disease burden assessment and disease burden prediction. In the section on disease burden assessment, first, we assessed the air pollution–related disease burden in 2019 and analyzed it by subgroups such as age and sex. In addition, we analyzed whether the disease burden attributable to different types of air pollution varied by country and territory according to the dominant pollutant. We described the air pollution–related disease burden by using the number and the age-standardized rates of death and DALY. Second, the estimated annual percentage change (EAPC) from 1990 to 2019 was calculated by a linear regression model to reflect the trends in the air pollution–related disease burden. The t-test and the Kruskal–Wallis test were used to compare the differences in disease burden among different subgroups. Cluster analysis was used to compare the air pollution–related, the particulate matter pollution–related, and the ambient ozone pollution–related disease burden across countries and territories. Finally, the relationship between some national indicators and the air pollution–related disease burden was analyzed using a panel data model. The panel data model consisted of three models. They were the fixed-effects model, the mixed-effects model, and the random-effects model (Horio et al. 2013). The likelihood ratio test was first performed. When the data did not differ significantly in units and time, the mixed-effects model was used to blend the data and estimate the parameters using ordinary least squares. Otherwise, the Hausman test was used to choose between the other two models. If the null hypothesis of Hausman’s test was accepted, the random-effects model should be adopted (Song et al. 2021).
In the section on disease burden prediction, we predicted the number and the age-standardized rates of air pollution-related deaths and DALY from 2020 to 2044 by using the ARIMA model and the exponential smoothing model in time series analysis. To verify the stability of the prediction results, sensitivity analysis was further performed using the APC model under the maximum likelihood framework and the Bayesian APC model integrated nested Laplace approximations (INLAs). Mean absolute percentage error (MAPE) was used as a model evaluation indicator to determine the best model for predicting the trend of the air pollution–related disease burden. For a more precise forecast, we calculated the number of changes in three cases based on the rate observed in 2019, including the rate remaining stable, decreasing by 1% per year, and increasing by 1% per year. In addition, we considered air quality improvements from vehicle electrification and other technologies in the ARIMA model used to predict future disease burden to see if future disease burden trends remain consistent.
All data collation and analysis were performed by R (version 4.0.2) software. And the world map was drawn using ArcGIS software.
Results
The air pollution-related disease burden in 2019
In 2019, the number of air pollution-related death was 6.67 million (95% uncertainty intervals (UI): 7.49 million, 5.90 million), which accounted for 11.62% of global death. The corresponding age-standardized death rate was 85.62 (95% UI: 75.71, 96.07) per 100,000 population. The number of air pollution–related DALY was 21.33 million (95% UI: 18.89 million, 23.95 million) accounting for 0.84% of global DALY in 2019. However, the corresponding age-standardized rate of DALY related to air pollution was 2791.08 (95% UI: 2468.81, 3141.39) per 100,000 population.
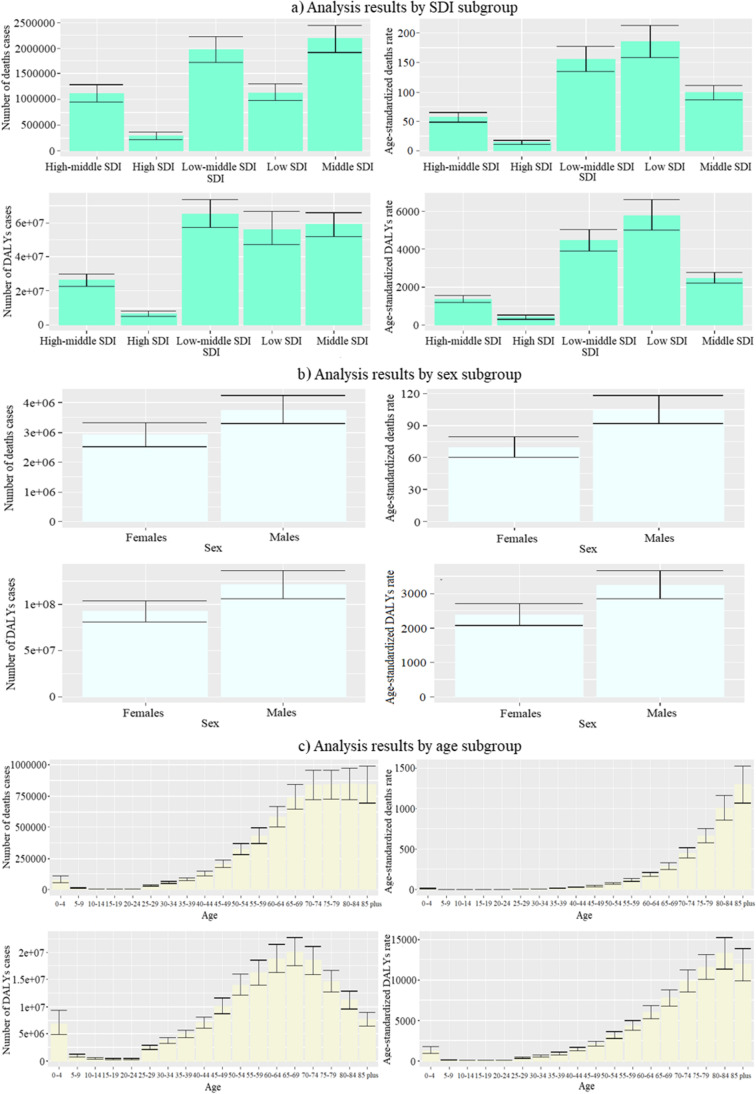
As shown in Fig. 1, the different indicators’ regularity of the regions grouped according to SDI was different. The number and corresponding age-standardized rates of air pollution–related death and DALY in high SDI locations were lower than in others. The age-standardized rates of death and DALY in low SDI locations were the highest. The number of death in middle SDI locations and the number of DALY in low-middle SDI locations were the highest. Regarding gender, the number and age-standardized rates of death and DALY attributable to air pollution were different between males and females. In 2019, the age-standardized rate of DALY and the age-standardized rate of death related to air pollution for males were 1.37 times higher and 1.50 times higher than that of females, respectively. We further explored whether the differences between males and females were present across all age groups. The results are shown in Supplementary Fig. S14 , Fig. S15, Fig. S16, Supplementary Fig. S17. In the indicators of the deaths number and DALY number, the numbers were slightly higher in females than in males in the age group of 0–9. Furthermore, more women were affected by air pollution than men at the age of 80 and above. However, the number of deaths and DALY was higher in males than in females in all other age groups. The death rate and DALY rate of women were slightly higher than men at ages 0–9. Also, men and women were roughly the same at the age of 10–14. In addition, the death rate and DALY rate of males were higher than females in all other age groups. Therefore, we could conclude that the differences between males and females nearly persisted across all age groups except for younger and older segments of the population. Figure 1 shows the age-standardized rates of death and DALY for different age groups.
Fig. 1.
Numbers and age-standardized rates of death and DALY attributable to air pollution in different subgroups in 2019. DALY, disability-adjusted life year
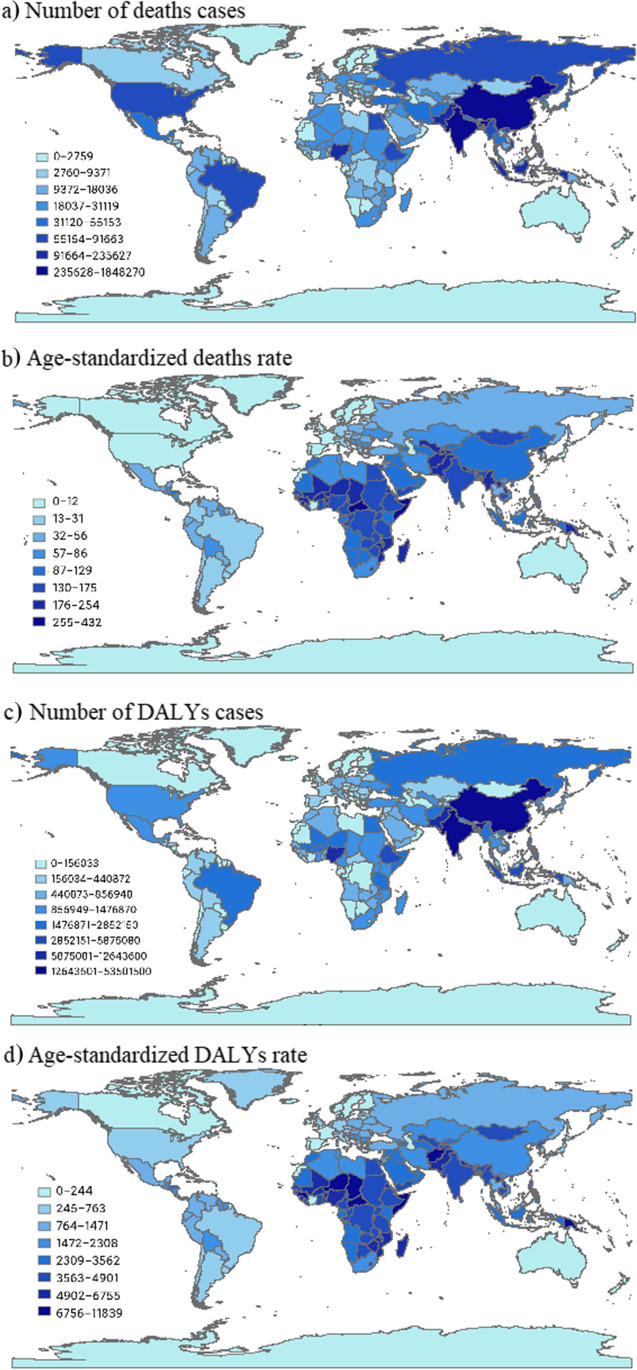
The air pollution–related disease burden varied widely around the world. In 2019, the largest air pollution–related number of death (1.85 million, 95% UI: 1.57 million, 2.17 million) was observed in China, followed by India, Pakistan, and Nigeria across the 204 countries and territories (Supplementary Table S3). The age-standardized death rate ranged from 3.14 (95% UI: 0.90, 6.05) in Iceland to 432.93 (95% UI: 348.13, 524.38) per 100,000 population in Solomon Islands. Meanwhile, the largest number of DALY (53.50 million, 95%UI: 46.59 million, 60.92 million) attributable to air pollution was observed in India, followed by China, Nigeria, and Pakistan. The age-standardized DALY rate ranged from 79.09 (95% UI: 22.40, 148.54) in Iceland to 11,839.88 (95% UI: 9443.57, 14,457.57) in Solomon Islands (Fig. 2).
Fig. 2.
Numbers and age-standardized rates of air pollution–related death and DALY across countries in 2019. DALY, disability-adjusted life year
According to Supplementary Fig. S5 , Fig. S6, Fig. S7, Supplementary Fig. S8, the countries with the largest number of DALY cases caused by particulate matter in 2019 were India and China, followed by Nigeria and Pakistan. The number of deaths cases was highest in China and India, followed by Pakistan, Nigeria, Indonesia, and Bangladesh. There are no countries whose age-standardized DALY rate and age-standardized death rate appear to be particularly high. As for air pollution caused by ozone, the countries with the largest number of DALY cases and deaths cases were India, followed by China, then Pakistan, the USA, and Bangladesh. The age-standardized DALY rate was highest in Nepal, the Democratic People’s Republic of Korea, and India, followed by Bhutan, Bangladesh, China, and Pakistan. The countries with the highest age-standardized death rate were the same as the age-standardized DALYs rate but followed by Bhutan, China, Spain, Bangladesh, and Italy.
The trend of the air pollution-related disease burden from 1990 to 2019
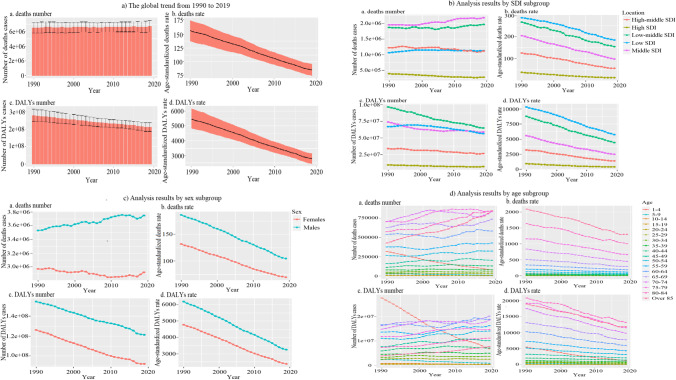
From 1990 to 2019, the number of air pollution-related death remained stable, and the number of DALY exhibited a downward trend. The corresponding age-standardized rates were both fallen. The air pollution–related disease burden varied substantially among different subgroups. For instance, the number of air pollution–related death showed a downward trend in some regions with higher SDI. However, in some areas with lower SDI, there were upward trends. However, the corresponding age-standardized rates showed downward trends in all SDI regions. The number of air pollution–related DALY and the corresponding age-standardized rate declined in all SDI regions from 1990 to 2019. In addition, the trends’ differences in the disease burden between males and females from 1990 to 2019 were observed. Except for the number of air pollution–related death for males increased, the other indicators for both sexes showed a downward trend. Different air pollution–related disease burdens for different age groups showed an inconsistent trend (Fig. 3).
Fig. 3.
The global trend and subgroup analysis of disease burden attributable to air pollution from 1990 to 2019
We used the t-test and the Kruskal–Wallis test to compare the differences in disease burden among different subgroups. The results showed that the differences between different subgroups were all statistically significant (Supplementary Table S1). In addition, 204 countries and territories were divided into four categories (a: significant growth; b: a slight increase; c: remain stable or decrease slightly; d: significantly decreased) through cluster analysis to compare the disease burden. The results are presented in Supplementary Fig. S1-Supplementary Fig. S2.
The 204 countries and territories were divided into four categories according to the two pollutants of particulate matter and ozone respectively (a: significant growth; b: a slight increase; c: remain stable or decrease slightly; d: significantly decreased) through cluster analysis to compare the disease burden. The results are presented in Supplementary Fig. S9, Fig. S10, Fig. S11, Supplementary Fig. S12.
Modified effect of national indicators on the air pollution–related disease burden
The greening indicator forest area was significantly associated with the number of air pollution–related DALY and was not significantly associated with the number of air pollution–related death, the age-standardized death rate, and the age-standardized DALY rate. Each increase of one unit of forest area would increase the number of 0.0000070288 for DALY. In terms of demographic indicators, the air pollution–related disease burden was lower in countries with larger population densities, higher proportions of elders, and lower proportions of females. However, the results of various indicators were different, as shown in Supplementary Table S1. Regarding socioeconomic indicators, countries with a higher economic level appeared to have a lower air pollution–related disease burden. Among the urbanization indicators, we found that the proportion of the urban population was directly proportional to the number of air pollution–related deaths. But other indicators seem to be the opposite (Supplementary Table S2).
Predictions of the air pollution–related disease burden
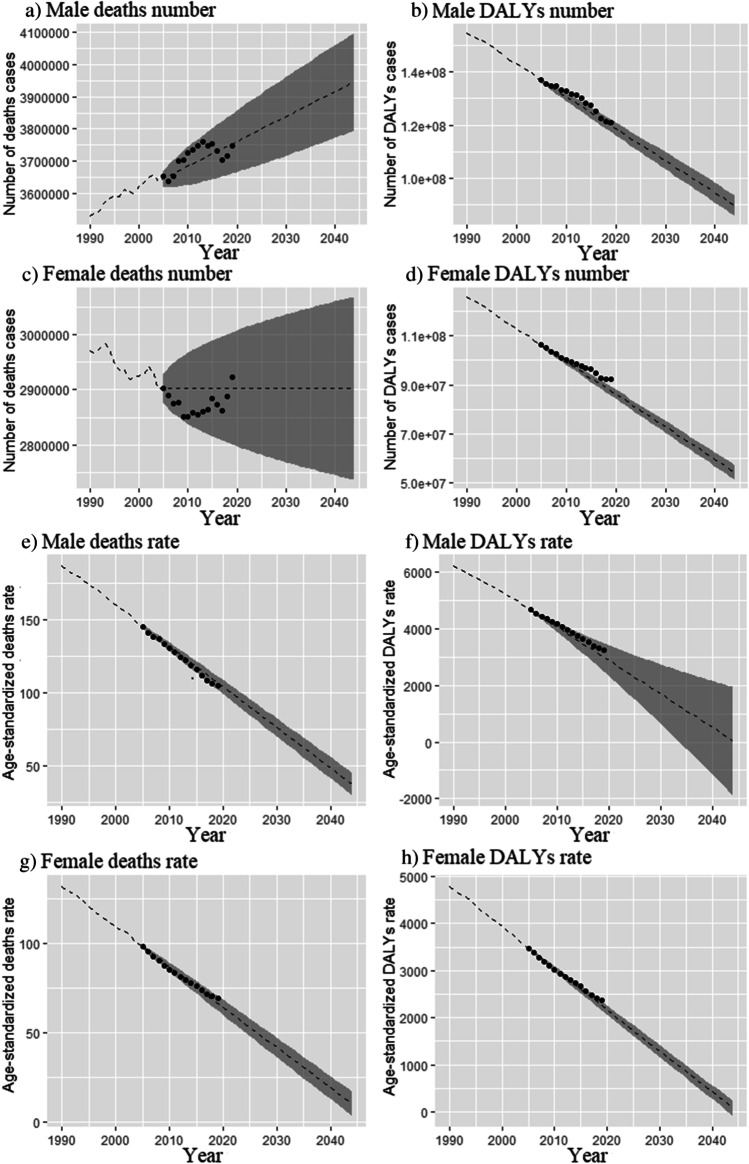
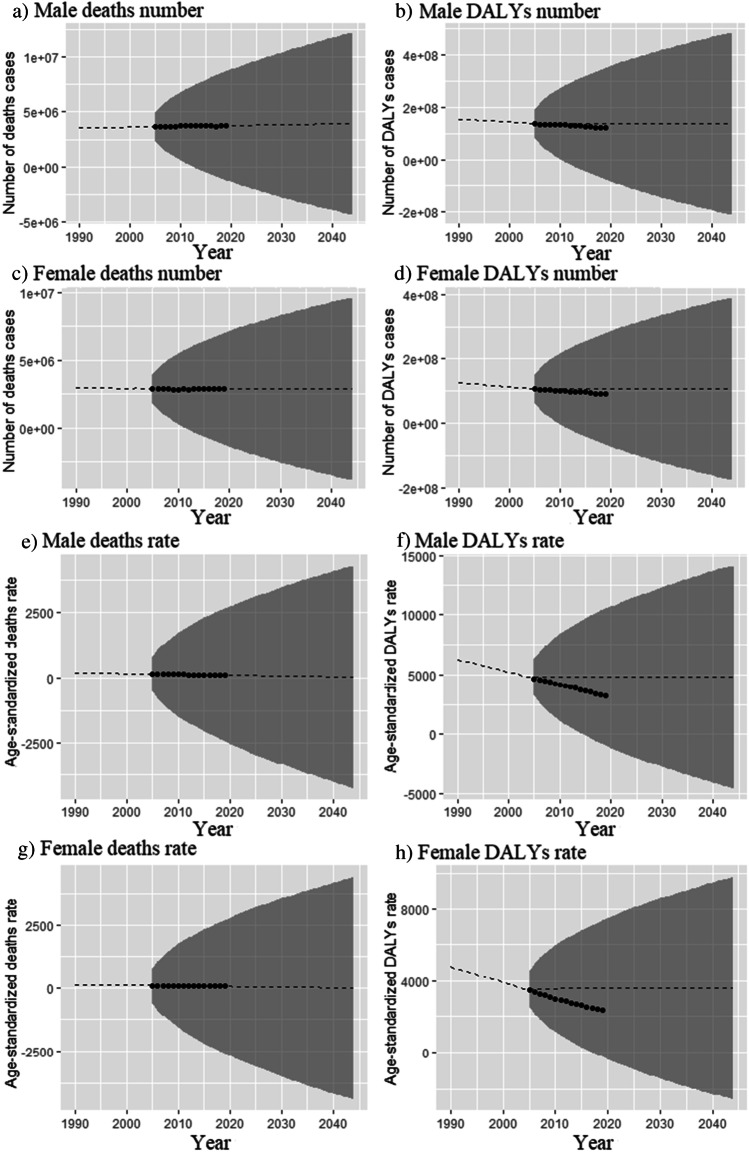
We used the ARIMA model and exponential smoothing model in time series analysis to predict the air pollution–related disease burden from 2020 to 2044. The results of the ARIMA model showed that the number of death for males would increase and would remain stable for females in the future 25 years. Other indicators for both sexes would continue to decrease (Fig. 4). The results of the exponential smoothing model showed that the number of air pollution–related death and the age-standardized death rate would remain stable. Furthermore, the number of air pollution–related DALY and the age-standardized DALY rate would decline (Fig. 5). The model evaluation indicator of MAPE showed that the exponential smoothing model was worse than the ARIMA model for predicting the trend of air pollution–related disease burden.
Fig. 4.
Predicted trends in the numbers and the age-standardized rates of death and DALY attributable to air pollution by sex by using the ARIMA model. The shaded part is a 95% confidence interval
Fig. 5.
Predicted trends in the numbers and the age-standardized rates of death and DALY attributable to air pollution by sex by using the exponential smoothing model. The shaded part is a 95% confidence interval
To assess the stability of the predictions, we further used the APC model in the maximum likelihood framework and the Bayesian APC model integrated nested Laplace approximations to predict the future air pollution–related disease burden for sensitivity analysis. The Bayesian APC model could not predict the age-standardized DALY rates due to problems with the data. The results showed that the future age-standardized rates of air pollution–related death and DALY would remain stable or continue to decrease. Although the trends of death and DALY rates were similar for males and females, the indicators for females were significantly lower than for males. Despite the estimated decreases in the rates of death and DALY attributable to air pollution, the number of death and DALY would continue to increase over the next 25 years. These might be due to global population growth. The shaded part of Supplementary Fig. S3 and Supplementary Fig. S4 showed that the number of death and DALY changed dramatically if the corresponding rates increased or decreased by 1% per year, further highlighting the importance of preventive measures and policies.
Discussion
This study comprehensively assessed and predicted the global air pollution–related disease burden and made notable discoveries. Globally, air pollution was responsible for 11.62% of death and 0.84% of DALY in 2019, underscoring that air pollution was a severe threat to global human health. The study also presented significant differences in the air pollution–related disease burden in terms of subgroups such as region, sex, and age and identified subgroups that deserved attention. We identified several national indicators related to air pollution, too. Moreover, we used multiple models to predict the air pollution–related disease burden, which provided a basis for future policy and measures. These findings could help us fully understand the health impacts of air pollution and contribute to the development of public policies.
This study presented a comprehensive assessment of the global status and trends in the air pollution–related disease burden. Cohen and his colleagues (Cohen et al. 2017) studied the air pollution–related disease burden in 2015. The results showed that PM2.5 pollution was the fifth most prominent risk factor for death in 2015. In that year, exposure to PM2.5 caused 4.2 million deaths and 103.1 million DALY, representing 7.6% of global deaths and 4.2% of global DALY. In addition, Yin’s research showed that 1.24 million people died from air pollution in China in 2017 (Yin et al. 2020). A study in India reported that air pollution caused 1.67 million deaths in 2019, accounting for 17.8% of the total death nationwide (India State-Level Disease Burden Initiative Air Pollution Collaborators, 2021b). The conclusion indicated that the air pollution–related disease burden was high and had a significant negative economic impact. The results of these studies were consistent with our research, although these estimates used older data. And these fully indicated that air pollution posed an enormous disease burden globally. Meanwhile, this study indicated that the age-standardized rate and the number of death, as well as DALY, were higher in males than in females. The possible reasons were as follows. First, this might be because of the differences in airway anatomy between males and females. Females had smaller lumen and disproportionately thicker bronchial walls than males (Manisalidis et al. 2020). Second, differences in hormones, organ size, and body size between males and females might affect the transport and tissue deposition of pollutants, resulting in gender differences in air pollution–related disease burden (Clougherty 2010). Finally, differences between men and women in social roles, personal activity preferences, and active treatment seeking might also explain the gender differences observed in this study.
Meanwhile, the differences between ages might be related to lung aging (Brandsma et al. 2017). In addition, this study indicated that lower SDI regions appeared to have a higher air pollution–related disease burden. According to WHO data, approximately 91% of premature deaths caused by air pollution occur in low- and middle-income countries (McNutt and Dzau 2019). Some other studies also showed that people living in developing countries bear a higher air pollution–related disease burden, such as 91% of the 4.2 million premature deaths in 2016 occurred in low-income and middle-income countries where exposure was higher, which was consistent with our study (Turner et al. 2020; Tiotiu et al. 2020). These results might be because higher SDI countries had relatively strict control over air pollution, and they had more medical resources compared to lower SDI regions (Watts et al. 2021). In addition, residents of areas with lower SDI worked in environments where air pollution could hardly be controlled.
By using panel models to analyze the relationship between specific national indicators and the air pollution–related disease burden, we further learned about the factors that influence air pollution. Our study indicated that the degree of urbanization was directly proportional to the number of death attributable to air pollution, which could be explained by that the traffic emissions were more severe in urban (Hankey and Marshall 2017; Brugha and Grigg 2014). With the progress of industrialization and urbanization worldwide, energy consumption, especially fossil energy, increased dramatically, which has led to growing global air pollution (Bereitschaft and Debbage 2013; Betha et al. 2014; Wang et al. 2014). The global urbanization rate reached 55% in 2018. In the future, urbanization would be more rapid, and the urban population would continue to increase. This would make the air pollution–related disease burden much more severe than expected globally. In this regard, there were some effective measures we could take, such as urban re-planning and design, to address the impact of urbanization on air pollution. This study showed that a higher proportion of forest area would reduce the number of air pollution–related DALY, which accorded with many previous studies (Aerts et al. 2020; Diener and Mudu 2021; Sun et al. 2020). Therefore, governments, institutions, and organizations needed to take several actions to increase and protect the green area and maximize the benefits of green space to deal with air pollution.
Our study presented evidence for reductions in the age-standardized rates over the past 30 years. This was consistent with many other studies (Amann et al. 2020; Gou et al. 2020; Yue et al. 2020). The number of air pollution–related death fluctuated, and the number of DALY decreased from 1990 to 2019 as the combined result of a series of environmental protection measures and people’s attention to environmental pollution over the past decades. Our predictions showed that the age-standardized rates would remain stable or decline in the next 25 years. However, the number of death and DALY attributable to air pollution would increase. This might be because of the population growth and aging trends (Han et al. 2018; Zhao et al. 2021). Therefore, practical strategies and measures should be proposed to strengthen the management and prevention of risk factors such as smoking. At the same time, some options to improve clinical diagnosis and treatment should be proposed to curb the increasing trend of the air pollution–related disease burden and reduce the disease burden.
However, this study had some limitations. First, the assessment of the disease burden was carried out at the country and region levels. However, some countries were vast, and the burden of disease could vary significantly between different provinces in a country. This was the issue that we could consider investigating further in the future. Second, the GBD database had defects such as data quality assurance. Finally, many other national indicators might be associated with the air pollution–related disease burden. However, since partial data were missed, analysis was not possible. Therefore, we will further assess the trend of the disease burden in different regions of countries. Beyond that, we need to better translate our research into action and develop public policies.
Conclusions
In conclusion, our findings showed that air pollution posed a substantial global disease burden and called for action and interventions by health policymakers. This study also revealed subgroups more severely affected by air pollution. In addition, we predicted the disease burden over the next 25 years, and the results showed that the situation remained grim. Based on these findings, more targeted and effective policies and measures should be developed to reduce the adverse air pollution–related health effects.
Supplementary information
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank the GBD 2019 collaborators.
Author contribution
Wan Hu: conceptualization, methodology, data curation, formal analysis, writing—original draft, supervision. Lanlan Fang: methodology, formal analysis. Hengchuan Zhang: software, validation. Ruyu Ni: visualization, writing—review and editing. Guixia Pan: methodology, writing—review & editing.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable (this study does not contain any individual person’s data in any form).
Consent to publication
The authors declare that they agree with the publication of this paper in this journal.
Conflict of interests
The authors declare no competing interests.
Footnotes
Highlights
• In the twenty-first century, exposure to air pollution has become a threat to human health worldwide due to economic development.
• The trend in the air pollution-related disease burden from 1990 to 2019 is assessed by the linear regression model. And the panel data model is used to explore potential factors that modify the air pollution–related disease burden.
• The autoregressive integrated moving average model and the exponential smoothing model are compared to determine the optimal model. The age-period-cohort model under the maximum likelihood framework and the Bayesian age-period-cohort model integrated nested Laplace approximations are used for sensitivity analysis.
• The air pollution–related disease burden of males is higher than that of females. The age is directly proportional to the disease burden. And regions with lower SDI seem to have a higher disease burden.
• This study comprehensively assesses and predicts the air pollution–related disease burden worldwide. The results indicate that the air pollution-related disease burden will remain very serious in the next 25 years.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Adeyinka DA, Muhajarine N. Time series prediction of under-five mortality rates for Nigeria: comparative analysis of artificial neural networks, Holt-Winters exponential smoothing and autoregressive integrated moving average models. BMC Med Res Methodol. 2020;20:292. doi: 10.1186/s12874-020-01159-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aerts R, Nemery B, Bauwelinck M, Trabelsi S, Deboosere P, Van Nieuwenhuyse A, Nawrot TS, Casas L. Residential green space, air pollution, socioeconomic deprivation and cardiovascular medication sales in Belgium: a nationwide ecological study. Sci Total Environ. 2020;712:136426. doi: 10.1016/j.scitotenv.2019.136426. [DOI] [PubMed] [Google Scholar]
- Akita T, Ohisa M, Kimura Y, Fujimoto M, Miyakawa Y, Tanaka J. Validation and limitation of age-period-cohort model in simulating mortality due to hepatocellular carcinoma from 1940 to 2010 in Japan. Hepatol Res. 2014;44:713–719. doi: 10.1111/hepr.12177. [DOI] [PubMed] [Google Scholar]
- Amann M, Kiesewetter G, Schöpp W, Klimont Z, Winiwarter W, Cofala J, Rafaj P, Höglund-Isaksson L, Gomez-Sabriana A, Heyes C, Purohit P, Borken-Kleefeld J, Wagner F, Sander R, Fagerli H, Nyiri A, Cozzi L, Pavarini C. Reducing global air pollution: the scope for further policy interventions. Philos Trans A Math Phys Eng Sci. 2020;378:20190331. doi: 10.1098/rsta.2019.0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anonymous Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anonymous Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anonymous Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–e160. doi: 10.1016/S2214-109X(20)30489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anonymous Health and economic impact of air pollution in the states of India: the Global Burden of Disease Study 2019. Lancet Planet Health. 2021;5:e25–e38. doi: 10.1016/S2542-5196(20)30298-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balajee K, Sujith B, Suliankatchi R, Sehgal M. Characteristics of the ozone pollution and its health effects in India. Int J Med Public Heal. 2017;7:56–60. [Google Scholar]
- Beelen R, et al. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet. 2014;383:785–795. doi: 10.1016/S0140-6736(13)62158-3. [DOI] [PubMed] [Google Scholar]
- Bereitschaft B, Debbage K. Urban form, air pollution, and CO2 emissions in large U.S. metropolitan areas. Prof Geogr. 2013;65:612–635. [Google Scholar]
- Betha R, Behera SN, Balasubramanian R. 2013 Southeast Asian smoke haze: fractionation of particulate-bound elements and associated health risk. Environ Sci Technol. 2014;48:4327–4335. doi: 10.1021/es405533d. [DOI] [PubMed] [Google Scholar]
- Bloemsma LD, Hoek G, Smit LAM. Panel studies of air pollution in patients with COPD: Systematic review and meta-analysis. Environ Res. 2016;151:458–468. doi: 10.1016/j.envres.2016.08.018. [DOI] [PubMed] [Google Scholar]
- Brandsma CA, de Vries M, Costa R, Woldhuis RR, Königshoff M, Timens W (2017) Lung ageing and COPD: is there a role for ageing in abnormal tissue repair? Eur Respir Rev 26:170073. 10.1183/16000617.0073-2017 [DOI] [PMC free article] [PubMed]
- Brook RD, Newby DE, Rajagopalan S. Air pollution and cardiometabolic disease: an update and call for clinical trials. Am J Hypertens. 2017;31:1–10. doi: 10.1093/ajh/hpx109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugha R, Grigg J. Urban air pollution and respiratory infections. Paediatr Respir Rev. 2014;15:194–199. doi: 10.1016/j.prrv.2014.03.001. [DOI] [PubMed] [Google Scholar]
- Ceylan Z. Estimation of COVID-19 prevalence in Italy, Spain, and France. Sci Total Environ. 2020;729:138817. doi: 10.1016/j.scitotenv.2020.138817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K, Fiore AM, Chen R, Jiang L, Jones B, Schneider A, Peters A, Bi J, Kan H, Kinney PL. Future ozone-related acute excess mortality under climate and population change scenarios in China: a modeling study. PLoS Med. 2018;15:e1002598. doi: 10.1371/journal.pmed.1002598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi MC, Guo SE, Hwang SL, Chou CT, Lin CM, Lin YC. Exposure to indoor particulate matter worsens the symptoms and acute exacerbations in chronic obstructive pulmonary disease patients of Southwestern Taiwan: a pilot study. Int J Environ Res Public Health. 2016;14:4. doi: 10.3390/ijerph14010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clougherty JE. A growing role for gender analysis in air pollution epidemiology. Environ Health Perspect. 2010;118:167–176. doi: 10.1289/ehp.0900994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AJ, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389:1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener A, Mudu P. How can vegetation protect us from air pollution? A critical review on green spaces’ mitigation abilities for air-borne particles from a public health perspective - with implications for urban planning. Sci Total Environ. 2021;796:148605. doi: 10.1016/j.scitotenv.2021.148605. [DOI] [PubMed] [Google Scholar]
- Europe WHOROf (2013) Review of evidence on health aspects of air pollution – REVIHAAP Project: Technical Report [Internet]. Copenhagen: WHO Regional Office for Europe; 2013. Available from: https://www.ncbi.nlm.nih.gov/books/NBK361805/ [PubMed]
- Fu Z, Xi X, Zhang B, Lin Y, Wang A, Li J, Luo M, Liu T. Establishment and evaluation of a time series model for predicting the seasonality of acute upper gastrointestinal bleeding. Int J Gen Med. 2021;14:2079–2086. doi: 10.2147/IJGM.S299208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gecili E, Ziady A, Szczesniak RD. Forecasting COVID-19 confirmed cases, deaths and recoveries: revisiting established time series modeling through novel applications for the USA and Italy. PLoS ONE. 2021;16:e0244173. doi: 10.1371/journal.pone.0244173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gou YY, Zhang K, Li JJ, LÜ WL, Zhu S, Li J, He SS, Zheng Y, Zhi MK. Variational trend and characteristics of air pollution in Baoding City. Huan Jing Ke Xue. 2020;41:4413–4425. doi: 10.13227/j.hjkx.201912193. [DOI] [PubMed] [Google Scholar]
- Gowers AM, Cullinan P, Ayres JG, Anderson HR, Strachan DP, Holgate ST, Mills IC, Maynard RL. Does outdoor air pollution induce new cases of asthma? Biological plausibility and evidence; a review. Respirology. 2012;17:887–898. doi: 10.1111/j.1440-1843.2012.02195.x. [DOI] [PubMed] [Google Scholar]
- Guarin JR, Emberson L, Simpson D, Hernandez-Ochoa IM, Rowland D, Asseng S. Impacts of tropospheric ozone and climate change on Mexico wheat production. Clim Change. 2019;155:157–174. [Google Scholar]
- Han L, Zhou W, Pickett ST, Li W, Qian Y. Multicontaminant air pollution in Chinese cities. Bull World Health Organ. 2018;96:233–242e. doi: 10.2471/BLT.17.195560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankey S, Marshall JD. Urban form, air pollution, and health. Curr Environ Health Rep. 2017;4:491–503. doi: 10.1007/s40572-017-0167-7. [DOI] [PubMed] [Google Scholar]
- Hoek G, Krishnan RM, Beelen R, Peters A, Ostro B, Brunekreef B, Kaufman JD. Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ Health. 2013;12:43. doi: 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horio H, Kikuchi H, Ikeda T. Panel data analysis of cardiotocograph (CTG) data. Stud Health Technol Inform. 2013;192:1041. [PubMed] [Google Scholar]
- Ji W, Xie N, He D, Wang W, Li H, Wang K (2019) Age-period-cohort analysis on the time trend of hepatitis B incidence in four prefectures of Southern Xinjiang, China from 2005 to 2017. Int J Environ Res Public Health 16:3886. 10.3390/ijerph16203886 [DOI] [PMC free article] [PubMed]
- Jin LJ, Lamster IB, Greenspan JS, Pitts NB, Scully C, Warnakulasuriya S. Global burden of oral diseases: emerging concepts, management and interplay with systemic health. Oral Dis. 2016;22:609–619. doi: 10.1111/odi.12428. [DOI] [PubMed] [Google Scholar]
- Khomenko S, Cirach M, Pereira-Barboza E, Mueller N, Barrera-Gómez J, Rojas-Rueda D, de Hoogh K, Hoek G, Nieuwenhuijsen M. Premature mortality due to air pollution in European cities: a health impact assessment. Lancet Planet Health. 2021;5:e121–e134. doi: 10.1016/S2542-5196(20)30272-2. [DOI] [PubMed] [Google Scholar]
- Krewski D et al. (2009) Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Res Rep Health Eff Inst 140:5–114; discussion 115 [PubMed]
- Li S, Chen H, Man J, Zhang T, Yin X, He Q, Yang X, Lu M. Changing trends in the disease burden of esophageal cancer in China from 1990 to 2017 and its predicted level in 25 years. Cancer Med. 2021;10:1889–1899. doi: 10.1002/cam4.3775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H, Shi L, Zhang J, Zhang J, Zhang C. Epidemiological characteristics and forecasting incidence for patients with breast cancer in Shantou, Southern China: 2006–2017. Cancer Med. 2021;10:2904–2913. doi: 10.1002/cam4.3843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Li C, Shao Y, Zhang X, Zhai Z, Wang X, Qi X, Wang J, Hao Y, Wu Q, Jiao M. Forecast of the trend in incidence of acute hemorrhagic conjunctivitis in China from 2011–2019 using the seasonal autoregressive integrated moving average (SARIMA) and exponential smoothing (ETS) models. J Infect Public Health. 2020;13:287–294. doi: 10.1016/j.jiph.2019.12.008. [DOI] [PubMed] [Google Scholar]
- Manisalidis I, Stavropoulou E, Stavropoulos A, Bezirtzoglou E. Environmental and health impacts of air pollution: a review. Front Public Health. 2020;8:14. doi: 10.3389/fpubh.2020.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonnell WF, Stewart PW, Smith MV. Prediction of ozone-induced lung function responses in humans. Inhal Toxicol. 2010;22:160–168. doi: 10.3109/08958370903089557. [DOI] [PubMed] [Google Scholar]
- McNutt M, Dzau V. Academies’ call to action: air pollution threatens global health. Ann Glob Health. 2019;85:145. doi: 10.5334/aogh.2660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Münzel T, Hahad O, Daiber A, Lelieveld J. Air pollution and cardiovascular diseases. Herz. 2021;46:120–128. doi: 10.1007/s00059-020-05016-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthiah MD, Sanyal AJ. Burden of disease due to nonalcoholic fatty liver disease. Gastroenterol Clin North Am. 2020;49:1–23. doi: 10.1016/j.gtc.2019.09.007. [DOI] [PubMed] [Google Scholar]
- Newby DE, et al. Expert position paper on air pollution and cardiovascular disease. Eur Heart J. 2015;36:83–93b. doi: 10.1093/eurheartj/ehu458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noorimotlagh Z, Azizi M, Pan HF, Mami S, Mirzaee SA. Association between air pollution and multiple sclerosis: a systematic review. Environ Res. 2021;196:110386. doi: 10.1016/j.envres.2020.110386. [DOI] [PubMed] [Google Scholar]
- Nunes RAO, Alvim-Ferraz MCM, Martins FG, Peñuelas AL, Durán-Grados V, Moreno-Gutiérrez J, Jalkanen JP, Hannuniemi H, Sousa SIV. Estimating the health and economic burden of shipping related air pollution in the Iberian Peninsula. Environ Int. 2021;156:106763. doi: 10.1016/j.envint.2021.106763. [DOI] [PubMed] [Google Scholar]
- Rohr AC. Ozone exposure and pulmonary effects in panel and human clinical studies: considerations for design and interpretation. J Air Waste Manag Assoc. 2018;68:288–307. doi: 10.1080/10962247.2018.1424056. [DOI] [PubMed] [Google Scholar]
- Roth GA, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schraufnagel DE, Balmes JR, De Matteis S, Hoffman B, Kim WJ, Perez-Padilla R, Rice M, Sood A, Vanker A, Wuebbles DJ. Health benefits of air pollution reduction. Ann Am Thorac Soc. 2019;16:1478–1487. doi: 10.1513/AnnalsATS.201907-538CME. [DOI] [PubMed] [Google Scholar]
- Shah AS, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W, Langrish JP, Newby DE, Mills NL. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ. 2015;350:h1295. doi: 10.1136/bmj.h1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahrbaf MA, Akbarzadeh MA, Tabary M, Khaheshi I. Air pollution and cardiac arrhythmias: a comprehensive review. Curr Probl Cardiol. 2021;46:100649. doi: 10.1016/j.cpcardiol.2020.100649. [DOI] [PubMed] [Google Scholar]
- Song J, Pan R, Yi W, Wei Q, Qin W, Song S, Tang C, He Y, Liu X, Cheng J, Su H. Ambient high temperature exposure and global disease burden during 1990–2019: an analysis of the Global Burden of Disease Study 2019. Sci Total Environ. 2021;787:147540. doi: 10.1016/j.scitotenv.2021.147540. [DOI] [PubMed] [Google Scholar]
- Sun Y, Sheridan P, Laurent O, Li J, Sacks DA, Fischer H, Qiu Y, Jiang Y, Yim IS, Jiang LH, Molitor J, Chen JC, Benmarhnia T, Lawrence JM, Wu J. Associations between green space and preterm birth: windows of susceptibility and interaction with air pollution. Environ Int. 2020;142:105804. doi: 10.1016/j.envint.2020.105804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian F, Qi J, Wang L, Yin P, Qian ZM, Ruan Z, Liu J, Liu Y, McMillin SE, Wang C, Lin H, Zhou M. Differentiating the effects of ambient fine and coarse particles on mortality from cardiopulmonary diseases: a nationwide multicity study. Environ Int. 2020;145:106096. doi: 10.1016/j.envint.2020.106096. [DOI] [PubMed] [Google Scholar]
- Tian Y, Liu H, Wu Y, Si Y, Li M, Wu Y, Wang X, Wang M, Chen L, Wei C, Wu T, Gao P, Hu Y. Ambient particulate matter pollution and adult hospital admissions for pneumonia in urban China: a national time series analysis for 2014 through 2017. PLoS Med. 2019;16:e1003010. doi: 10.1371/journal.pmed.1003010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiotiu AI, Novakova P, Nedeva D, Chong-Neto HJ, Novakova S, Steiropoulos P, Kowal K (2020) Impact of air pollution on asthma outcomes. Int J Environ Res Public Health 17:6212. 10.3390/ijerph17176212 [DOI] [PMC free article] [PubMed]
- Turner MC, Andersen ZJ, Baccarelli A, Diver WR, Gapstur SM, Pope CA, 3rd, Prada D, Samet J, Thurston G, Cohen A. Outdoor air pollution and cancer: an overview of the current evidence and public health recommendations. CA Cancer J Clin. 2020;70:460–479. doi: 10.3322/caac.21632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Tan S-C, Wang Y, Jiang C, Shi G-y, Zhang M-X, Che H. A multisource observation study of the severe prolonged regional haze episode over Eastern China in January 2013. Atmos Environ. 2014;89:807–815. doi: 10.1016/j.atmosenv.2014.03.004. [DOI] [Google Scholar]
- Watts N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397:129–170. doi: 10.1016/S0140-6736(20)32290-X. [DOI] [PubMed] [Google Scholar]
- Yao Y, Pan J, Liu Z, Meng X, Wang W, Kan H, Wang W. Temporal association between particulate matter pollution and case fatality rate of COVID-19 in Wuhan. Environ Res. 2020;189:109941. doi: 10.1016/j.envres.2020.109941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin P, Brauer M, Cohen AJ, Wang H, Li J, Burnett RT, Stanaway JD, Causey K, Larson S, Godwin W, Frostad J, Marks A, Wang L, Zhou M, Murray CJL. The effect of air pollution on deaths, disease burden, and life expectancy across China and its provinces, 1990–2017: an analysis for the Global Burden of Disease Study 2017. Lancet Planet Health. 2020;4:e386–e398. doi: 10.1016/S2542-5196(20)30161-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue H, He C, Huang Q, Yin D, Bryan BA (2020) Stronger policy required to substantially reduce deaths from PM(2.5) pollution in China. Nat Commun 11:1462. 10.1038/s41467-020-15319-4 [DOI] [PMC free article] [PubMed]
- Zhang Z, Hong Y, Liu N (2017) Association of ambient Particulate matter 2.5 with intensive care unit admission due to pneumonia: a distributed lag non-linear model. Sci Rep 7:8679. 10.1038/s41598-017-08984-x [DOI] [PMC free article] [PubMed]
- Zhao Z, Lao X, Gu H, Yu H, Lei P. How does air pollution affect urban settlement of the floating population in China? New evidence from a push-pull migration analysis. BMC Public Health. 2021;21:1696. doi: 10.1186/s12889-021-11711-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y, Zhang L, Zhu X, Guo G. A comparative study of two methods to predict the incidence of hepatitis B in Guangxi. China Plos One. 2020;15:e0234660. doi: 10.1371/journal.pone.0234660. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.