Abstract
Background
Cardioprotective antihyperglycemic agents, SGLT2 inhibitors (SGLT2i) and GLP-1 receptor agonists (GLP1RA), improve outcomes of patients with type 2 diabetes, but adoption has been limited. Differences across individuals have been noted but area-level variation is unknown.
Objectives
Given healthcare access and sociodemographic differences, we evaluated whether SGLT2i and GLP-1RA utilization varies across US counties.
Methods
We linked 2019 Medicare Part D national prescription data with county-level demographic measures from the Agency for Health Quality and Research. We compared the number of beneficiaries receiving prescriptions for any cardioprotective antihyperglycemic to the number receiving metformin prescriptions across US counties. In multivariable linear regression with SGLT2i-to-metformin and GLP1RA-to-metformin prescriptions as outcomes, we evaluated county factors associated with use of cardioprotective agents while adjusting for sociodemographic measures, region, and cardiometabolic risk factor prevalence.
Results
In 3066 US counties, there were a median 2,416 (IQR, 1681–3190) metformin-receiving beneficiaries per 100,000 population. A median 6.2% of beneficiaries receiving metformin received SGLT2i therapy, varying across counties (IQR, 3.4%–9.2%). A median 9.4% (IQR, 5.0%–13.0%) of beneficiaries receiving metformin received GLP-1RA. In adjusted analyses, higher percentage of Black population was associated with lower use at the county level of people on SGLT2i or GLP-1RA relative to metformin (a SD higher proportion of Black individuals with 0.4% [95% CI, -0.6% to -0.1%] and 0.5% [-0.8% to -0.2%] lower SGLT2i and GLP-1RA prescribing relative to metformin, respectively; P < 0.01). A higher median age of county residents, rural location, and lower prevalence of diabetes were associated with lower SGLT2i prescribing. Similarly, more advanced age of county residents, rural location, proportion of Hispanic individuals, and household income and lower education levels were associated with lower GLP-1RA prescribing. Prescribing was higher in the Northeast and lower in the West as compared with the Midwest for both classes.
Conclusion
There was large variation by county in cardioprotective antihyperglycemic prescribing, with a pattern of lower use in Black-predominant and rural counties, highlighting the critical need to investigate equity in uptake of novel therapeutic agents.
Keywords: Glucagon like peptide-1 receptor agonists, Sodium glucose cotransporter-2 inhibitors, Medicare, Prescription fill
Abbreviations: SGLT2i, sodium-glucose cotransporter-2 inhibitors; GLP-1RA, glucagon-like peptide-1 receptor agonists; PCP, primary care physicians; IQR, interquartile range; CI, confidence interval
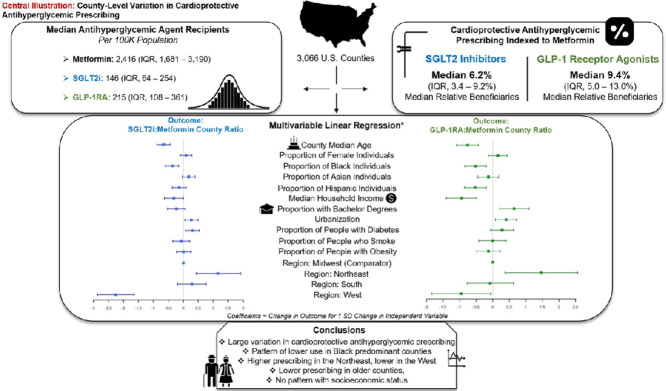
Graphical abstract
County-Level Variation in Cardioprotective Antihyperglycemic Prescribing. Figure demonstrating the distribution of antihyperglycemic prescribing across US counties, distribution of prescribing indexed to metformin, and county-level factors associated with indexed prescribing.
1. Background
Large randomized clinical trials have demonstrated the cardioprotective benefits of sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1RA) in patients with type 2 diabetes [1–4]. Society guidelines recommend initiation of these agents in patients with type 2 diabetes and heart failure, atherosclerotic cardiovascular disease, or diabetic kidney disease [5]. Patients with type 2 diabetes at high cardiovascular risk should also be considered for SGLT2i and GLP-1RA therapy. Clinical trials were performed on a background of metformin therapy and therefore, metformin remains the first-line anti-hyperglycemic agent; however, society guidelines recommend consideration of these agents independently of baseline hyperglycemia, target hyperglycemic levels, and metformin therapy [5,6].
In nationally representative data assessments, 65% and 40% of patients with type 2 diabetes age 65 years or older have indications for SGLT2i and GLP-1RA, respectively [7]. However, there has been limited adoption of these drugs in real-world practice, with less than 10% of eligible patients receiving these therapies [7–10]. It is unknown if geographic variation exists in the prescribing of cardioprotective antihyperglycemic drugs. Prior studies have reported regional and state-level variation in both cardiovascular outcomes and practice [11–14]. Geographic variation in cardiovascular pharmacotherapy, specifically, has been described [15–17]. We sought to identify if prescribing is universally low or whether geographic variation exists in the prescribing of cardioprotective antihyperglycemic agents. Such data may serve future policy interventions aimed at improving adoption of these important preventative therapies.
In this national study of Medicare prescription data of United States clinicians merged with county population characteristics, we compared county-level SGLT2i and GLP1-RA prescribing across United States counties. Comparing county-level drug prescribing for patients with diabetes requires indexing these prescription patterns to the county-level prevalence of diabetes requiring medical treatment in the same subpopulation. To this end, we elected to compare SGLT2i and GLP1-RA prescriptions as a proportion of the total prescriptions of first-line diabetes therapy, metformin. Indexing therefore allows comparison of the use of these novel agents in populations of patients actively managed for type 2 diabetes across counties. Prescribing indexed to metformin was compared with county racial and socioeconomic compositions while adjusting for available characteristics that may influence prescriptions, including cardiometabolic risk factor prevalence.
2. Methods
2.1. Data sources
In this cross-sectional study, we used 2019 Medicare Part D Prescriber data. The database includes all drugs prescribed for Medicare Part D enrollees, which comprise approximately 70% of all Medicare beneficiaries [18]. Data are organized by the prescriber's National Provider Identifier and include the number of prescriptions by each prescriber. The drug prescription counts represent the number of unique Medicare beneficiaries receiving at least one prescription from the provider for that drug at any time during 2019.
Two other databases were used. First, we obtained county demographic and socioeconomic data for year 2018 (most recent available data) from the Social Determinants of Health database created by the Agency for Healthcare Research and Quality. The database curates data from a variety of national sources including the United States Census Bureau and the Centers for Disease Control (CDC) [19]. The database includes a limited number of cardiometabolic risk factors from previous years, specifically the county prevalence of smoking (most recent data available from 2017) as well as diabetes and obesity (most recently available from 2016). County-level risk factor prevalence is based on the CDC's Behavioral Risk Factor Surveillance System [20].
Second, we acquired corresponding county codes for United States municipalities from the United States Cities database, a database of United States cities and towns, to link the municipal Medicare claims data with the Social Determinants of Health database county-level data [21]. Municipality is not a standardized entity and so 4% of Medicare Part D prescribers could not be linked to a county.
2.2. Study population
Counties within the 50 states and the District of Columbia were included. Counties in United States territories were excluded.
2.3. Study covariates
We identified the following county-level factors as possibly associated with prescribing patterns: (1) demographics (median county age, gender, race [proportion of individuals reporting White, Black, or Asian race], and ethnicity (proportion of individuals reporting Hispanic ethnicity] as reported by the United States Census Bureau), (2) education (proportion of population with a bachelor's degree), (3) measures of financial wellbeing (median household income), (4) measures of rural/urban status (nine categories based on population and degree of urbanization derived from the 2013 United States Department of Agriculture's Rural-Urban Continuum Codes), (5) cardiometabolic risk factors (county prevalence of adults age ≥20 of diabetes [proportion diagnosed with diabetes], smoking [proportion who are current smokers], and obesity [proportion with body mass index ≥30 kg/m2), (6) measures of healthcare access (number of primary care physicians [PCP] per 100,000 population as reported by the American Medical Association), (7) United States Census region (Midwest, Northeast, South, and West).
2.4. Study outcomes
We evaluated the number of Medicare beneficiaries in each county who received SGLT2i and GLP-1RA, relative to the number of beneficiaries receiving metformin, a surrogate for the number of patients being treated for type 2 diabetes in a community. The SGLT2i included canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin and GLP1-RA included albiglutide, dulaglutide, exenatide, liraglutide, lixisenatide, semaglutide, and teduglutide. Drug prescriptions represented both individual agents and fixed-dose drug combinations. Medicare data do not report beneficiary counts of less than 10 for individual drugs prescribed by a given prescriber. Beneficiary counts ranging from 1 to 9, which were recorded <10 in the data, were assigned a value of 5 for the count-based analyses.
2.5. Statistical analysis
We evaluated the univariate association between county-level SGLT2i prescribing relative to metformin and county characteristics including demographics, socioeconomic features, and the average cardiometabolic risk profile of county residents, using Spearman's correlation. We also evaluated differences in county characteristics across quartiles of SGLT2i prescribing using the Jonckheere-Terpstra test.
To assess independent association of county features with county SGLT2i prescriptions, we constructed a county-level multivariable linear regression model with the county SGLT2i-to-metformin prescription ratio as the dependent variable and county characteristics as independent variables. We used the model to calculate standardized regression coefficients, where each coefficient represented change in outcome for one standard deviation change in the independent variable. These procedures were repeated for indexed GLP-1RA prescribing. To explicitly evaluate the association of healthcare access to prescription counts, we constructed a second set of models that included county-level PCP counts per 100,000 population as additional covariates to the model.
Analyses were performed using R 4.0.3 (CRAN). The level of statistical significance was set at 0.05 and all analyses were 2-sided. The data are publicly available, deidentified data, and therefore this study was exempt from review by the Institutional Review Board.
3. Results
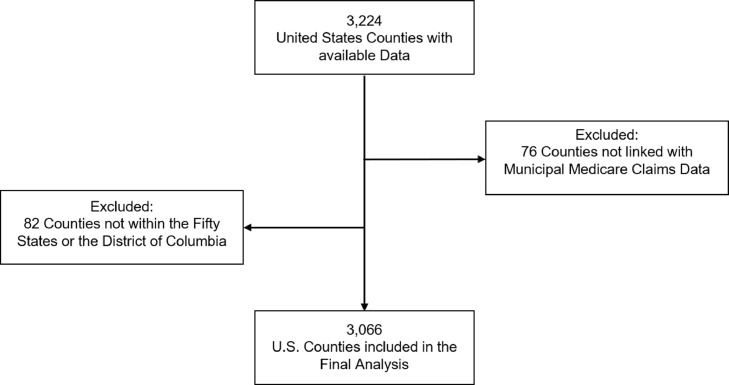
Data were available for 3,224 United States counties. Of the 3,143 within the 50 states or the District of Columbia, 77 (2.4%) could not be merged with prescription data based on county codes with 3,066 counties represented in the final analysis (Fig. 1). The total weighted population estimate for the included counties was 322,707,085 individuals (median proportion of women across counties, 50.4%; interquartile range [IQR], 49.4% - 51.1%; median proportion of Black individuals, 2.4%; IQR, 0.70% - 10.3%). The regional composition of the counites was: 1,019 (33%) Midwest, 217 (7%) Northeast, 1,398 (46%) South, and 432 (14%) West.
Fig. 1.
Inclusion and exclusion flow diagram.
3.1. Variation in cardioprotective antihyperglycemic therapy across United States counties
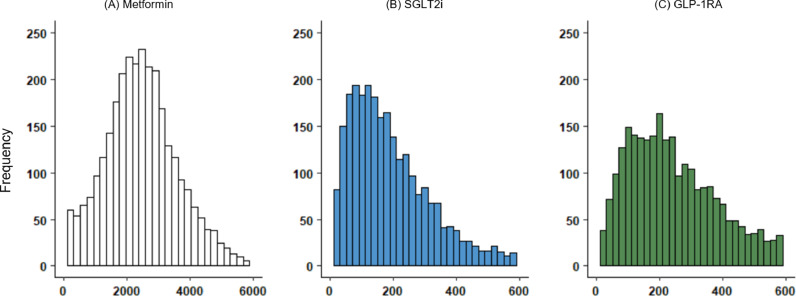
There were a median 2,416 metformin-receiving Medicare beneficiaries per 100,000 population in United States counties (IQR, 1681–3190). There were a median 146 (IQR, 64–254) SGLT2i-receiving beneficiaries and a median 215 (IQR, 108–361) GLP-1RA-receiving beneficiaries in the included counties (Fig. 2).
Fig. 2.
Variation of Antihyperglycemic Therapy Across United States Counties.
Histograms of the number of Medicare beneficiaries per 100,000 population in U.S. counties receiving (A) metformin, (B) sodium glucose cotransporter 2 inhibitors (SGLT2i), (C) glucagon-like peptide-1 receptor agonists (GLP-1RA).
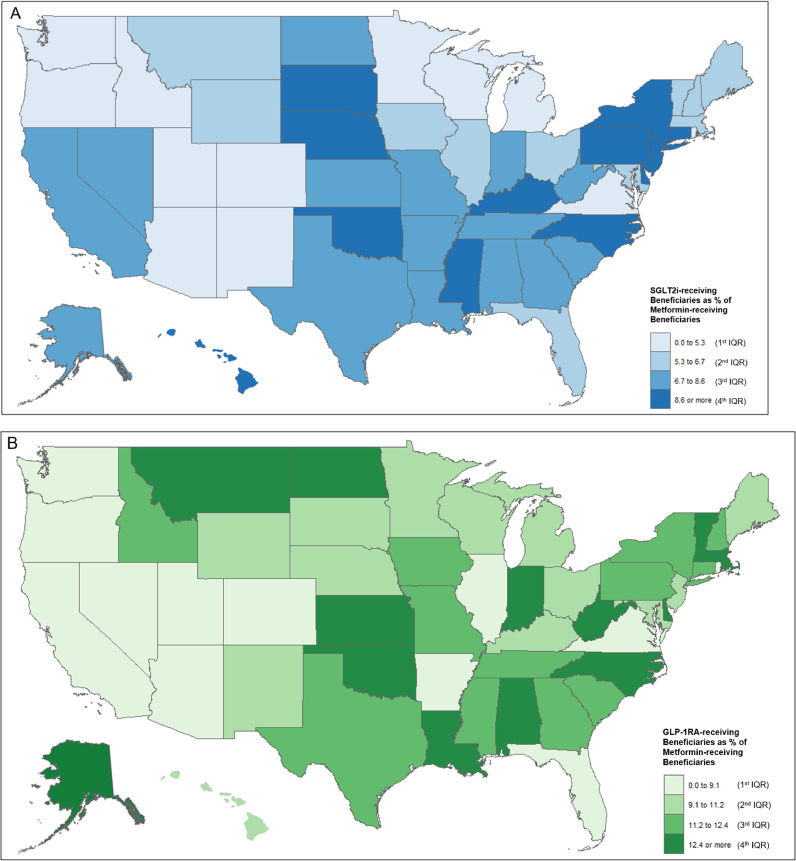
The use of SGLT2i and GLP-1RA agents relative to metformin was low across counties and varied nationally: beneficiaries receiving SGLT2i represented a median 6.2% (IQR, 3.4–9.2%) of beneficiaries receiving metformin, and a median 9.4% (IQR, 5.0–13.0%) beneficiaries received GLP-1RA indexed to metformin (Fig. 3).
Fig. 3.
Geospatial Representation of Cardioprotective Antihyperglycemic Prescribing across States.
(A) represents state SGLT2i-receiving beneficiaries as a percent of metformin-receiving beneficiaries, (B) represents the same for GLP-1RA. SGLT2i = sodium glucose cotransporter 2 inhibitors, GLP-1RA = glucagon-like peptide-1 receptor agonists.
3.2. County characteristics and SGLT2i prescribing
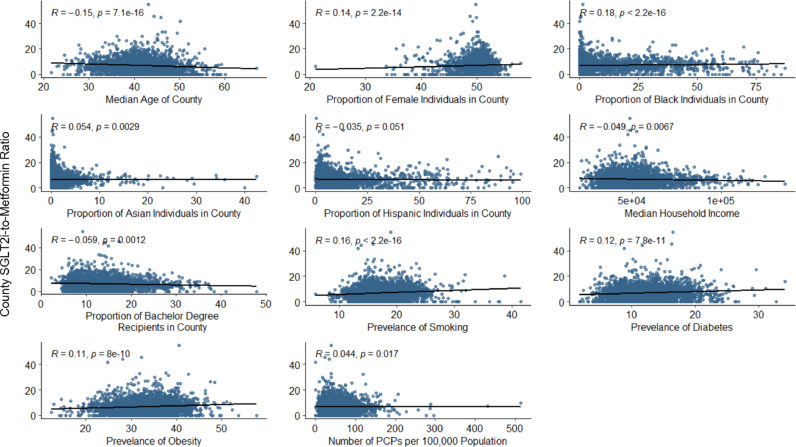
Across counties, higher median county age was associated with lower SGLT2i prescribing indexed to metformin (rho = -0.15, P < 0.001). The proportion of Black individuals in the population positively correlated with relative SGLT2i prescribing (rho = 0.18, P < 0.001). There was modest positive correlation between drug prescribing and the proportion of Asian individuals in the county (rho = 0.05; P < 0.01), without any correlation with the county's Hispanic population and the use of SGLT2i. There were weak negative correlations between socioeconomic measures (specifically measures of income and education) and the indexed number of SGLT2i-recieving beneficiaries (P < 0.01), while higher county prevalence of cardiometabolic risk factors were positively correlated with prescribing (P < 0.001) (Fig. 4).
Fig. 4.
County Characteristics and SGLT2i Prescribing.
Association of county characteristics with county-level prescribing of SGLT2i relative to metformin. Spearman's Rank test is given for each association. SGLT2i = sodium glucose cotransporter 2 inhibitors (SGLT2i), PCPs = primary care physicians.
When divided into quartiles of higher SGLT2i prescribing indexed to metformin, counties in higher quartiles had higher proportions of Black individuals and Asian individuals in the population and higher prevalence of cardiometabolic risk factors (P < 0.01). Table 1 lists county characteristics by quartile of higher indexed SGLT2i prescribing.
Table 1.
County Characteristics by Quartile of Higher Indexed SGLT2i Prescribing. P-values from Jonckheere-Terpstra testing of variance (or Chi-squared for categorical variables) are listed.
| Q1 | Q2 | Q3 | Q4 | P-value | |
|---|---|---|---|---|---|
| County Characteristic | |||||
| Median Age | 42.6 | 40.8 | 40.6 | 40.8 | 1 |
| Proportion of Female Individuals | 49.9 | 50.5 | 50.6 | 50.5 | 0.001 |
| Proportion of Black Individuals | 1.0 | 2.7 | 3.9 | 3.2 | 0.001 |
| Proportion of Asian Individuals | 0.5 | 0.7 | 0.7 | 0.6 | <0.01 |
| Proportion of Hispanic Individuals | 4.2 | 4.4 | 4.1 | 3.8 | 1 |
| Median Household Income | 49,752 | 51,186 | 50,473 | 48,222 | 1 |
| Proportion of Bachelor Degree Recipients | 13.3 | 13.4 | 13.3 | 12.0 | 1 |
| Prevalence of Diabetes | 11.1 | 11.4 | 11.9 | 12.2 | 0.001 |
| Prevalence of Smoking | 16.0 | 17.1 | 17.5 | 17.8 | 0.001 |
| Prevalence of Obesity | 32.6 | 32.7 | 33.5 | 34.0 | 0.001 |
| Number of PCPs per 100,000 Population | 43.6 | 51.8 | 52.0 | 47.1 | <0.01 |
| Census Region | <0.001 | ||||
| Midwest | 26.7 | 26.7 | 21.3 | 23.9 | |
| Northeast | 10.6 | 18.0 | 41.5 | 29.5 | |
| South | 18.2 | 24.6 | 27.3 | 28.6 | |
| West | 47.9 | 23.4 | 15.5 | 10.9 |
3.3. County characteristics and GLP-1RA prescribing
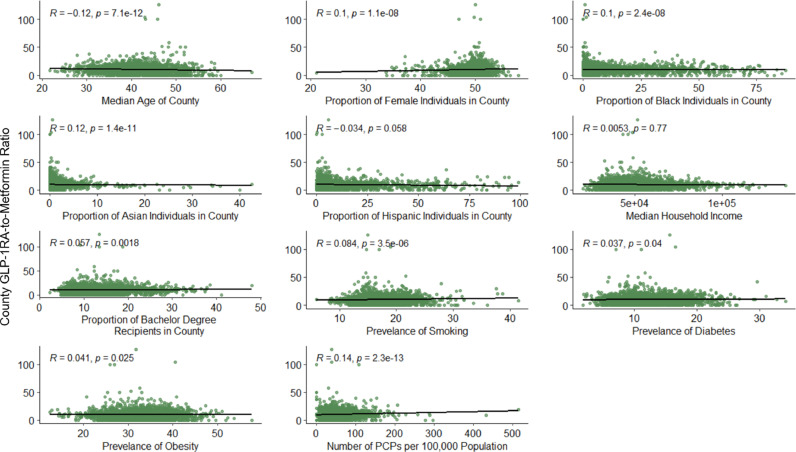
As was observed for SGLT2i prescribing, the indexed number of GLP-1RA-receiving beneficiaries correlated negatively with county median age (rho = -0.12, P < 0.001) and positively with the proportion of Black (rho = 0.10, P < 0.001) and Asian (rho = 0.12; P < 0.001) individuals in the county but there was no statistically significant correlation with the proportion of Hispanic individuals. For socioeconomic measures, median household income was not significantly correlated with GLP-1RA prescribing (P = 0.77), but there was a weak positive correlation with higher education attainment and GLP1-RA use (rho = 0.06, P = <0.01). Cardiometabolic risk factor prevalence was again positively associated with indexed prescribing (Fig. 5).
Fig. 5.
County Characteristics and GLP-1RA Prescribing.
Association of county characteristics with county-level prescribing of GLP-1RA relative to metformin. Spearman's Rank test for each association is given. GLP-1RA = glucagon-like peptide-1 receptor agonists, PCPs = primary care physicians.
Across quartiles of indexed GLP-1RA prescribing, as was seen for SGLT2i, counties in higher quartiles had higher proportions of Black and Asian individuals in the population (P = 0.001) and higher prevalence of cardiometabolic risk factors (P < 0.05) (Table 2).
Table 2.
County characteristics by quartile of higher indexed GLP-1RA prescribing. P-values from Jonckheere-Terpstra testing of variance (or Chi-squared for categorical variables) are listed.
| Q1 | Q2 | Q3 | Q4 | P-Value | |
|---|---|---|---|---|---|
| County Characteristic | |||||
| Median Age | 42.2 | 41.2 | 40.4 | 40.8 | 1 |
| Proportion of Female Individuals | 50.1 | 50.5 | 50.5 | 50.5 | 0.001 |
| Proportion of Black Individuals | 1.2 | 2.7 | 3.4 | 2.4 | 0.001 |
| Proportion of Asian Individuals | 0.5 | 0.6 | 0.7 | 0.6 | 0.001 |
| Proportion of Hispanic Individuals | 4.0 | 4.2 | 4.4 | 3.8 | 1 |
| Median Household Income | 49,234 | 51,393 | 50,543 | 49,144 | 0.45 |
| Proportion of Bachelor Degree Recipients | 12.4 | 12.9 | 13.5 | 13.1 | 0.001 |
| Prevalence of Diabetes | 11.5 | 11.7 | 11.5 | 12.0 | <0.05 |
| Prevalence of Smoking | 16.3 | 17.1 | 17.3 | 17.3 | 0.001 |
| Prevalence of Obesity | 32.9 | 33.2 | 32.9 | 33.6 | <0.05 |
| Number of PCPs per 100,000 Population | 40.0 | 50.6 | 52.7 | 51.4 | 0.001 |
| Census Region | <0.001 | ||||
| Midwest | 24.3 | 25.6 | 22.4 | 26.3 | |
| Northeast | 7.8 | 24.4 | 36.4 | 30.9 | |
| South | 23.4 | 24.0 | 26.4 | 24.8 | |
| West | 38.0 | 24.5 | 18.3 | 16.9 |
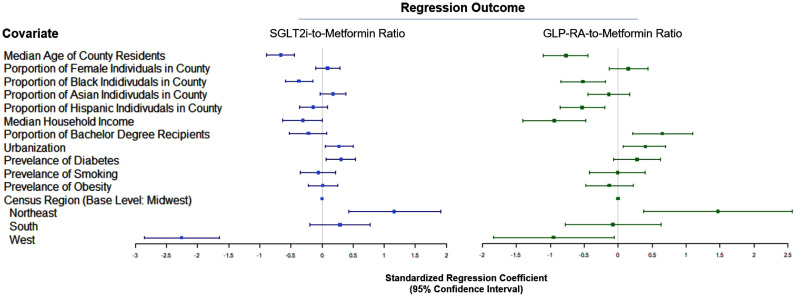
3.4. Independent association of cardioprotective antihyperglycemic prescribing
In multivariable linear regression models that included county demographics and county prevalence of cardiometabolic risk factors as dependent variables and indexed SGLT2i prescriptions as the outcome, a higher proportion of Black individuals in the county was associated with lower SGLT2i prescribing (Fig. 6). In multivariable analyses, one standard deviation increase in the proportion of black individuals was associated with a decrease of 0.4% in relative SGLT2i prescribing (95% confidence interval [CI], -0.6% to -0.1%; P < 0.01). The direction of the association was, therefore, opposite the direction observed in univariable testing. Neither the proportion of Hispanic individuals nor the proportion of Asian individuals in the county were associated with SGLT2i prescribing. Older county median age was also associated with lower prescribing indexed to metformin (standardized coefficient, -0.7%; 95% CI, -0.9% to -0.4%; P < 0.001). The prevalence of diabetes was positively associated with prescribing (P < 0.05), while lower urbanization was negatively associated (P < 0.05). Compared with the Midwest, the Northeast was associated with more prescribing (P < 0.01) while the West had lower SGLT2i prescribing (P < 0.001). The number of PCPs per 100,000 population was significantly associated with the county-level use of SGLT2i in models that included PCP counts as an additional covariate in the model (standardized coefficient, 0.3%, 95% CI, 0.1% to 0.5%; P < 0.05), but did not attenuate the association between Black population in the county and indexed SGLT2i prescriptions.
Fig. 6.
Independent Association of Cardioprotective Antihyperglycemic Prescribing.
Results from multivariable regression models. The plot displays regression coefficients and 95% confidence intervals, standardized to one standard deviation change in the independent variable, for each county characteristic. SGLT2i = sodium glucose cotransporter 2 inhibitors, GLP-1RA = glucagon-like peptide-1 receptor agonists.
Similar to SGLT2i prescribing, in multivariable regression models with GLP-1RA-to-metformin ratio as the outcome, higher proportion of Black individuals in the population was associated with lower relative GLP1-RA prescribing (standardized coefficient, -0.5%; 95% CI, -0.8% to -0.2%; P < 0.01) (Fig. 6). Higher proportion of Hispanic individuals was associated with lower relative GLP-1RA prescribing (standardized coefficient, -0.5%; 95% CI, -0.9% to -0.2%; P < 0.01) although the proportion of Asian individuals was not associated with GLP-1RA prescribing. Higher county median age (P < 0.001), median household income (P < 0.001), and lower urbanization (P < 0.05) were associated with lower prescribing. Higher average educational attainment was positively associated with number of prescriptions relative to metformin (P < 0.01). Associations with census regions were similar to associations with SGLT2i prescribing. There was a significant association between county-level marker of PCP access and GLP1-RA prescribing (standardized coefficient, 0.5%; 95% CI, 0.2% to 0.8%; P < 0.01). The county proportion of Black individuals remained significantly associated with SGLT2i and GLP-1RA prescribing in all secondary models.
4. Discussion
In this county-level, national study of US Medicare beneficiaries, there was low utilization of SGLT2i and GLP-1RA agents relative to Medicare beneficiaries being treated for type 2 diabetes, defined by number of beneficiaries in each county receiving metformin. Prescribing of cardioprotective antihyperglycemic agents varied across United States counties with an interquartile range across counties of 6 and 8% of SGLT2i and GLP-1RA as a proportion of metformin prescriptions. Moreover, across both drug classes, counties with larger proportions of Black individuals had lower relative use of cardioprotective antihyperglycemics after adjusting for county characteristics and average cardiometabolic risk profiles of county residents. There was an inconsistent prescribing pattern across the county's other racial and ethnic populations. There was no association between population of Asian individuals and prescription of cardioprotective therapy, while a higher proportion of Hispanic individuals was associated with lower GLP-1RA but not SGLT2i use. Higher median age and rural location were associated with lower prescribing of both drug classes. There was no clear association with socioeconomic status as lower educational attainment but higher median income was associated with lower GLP-1RA prescribing without an association with SGLT2i prescribing. These results in an insured population highlight a need for further investigation of equitable adoption of these novel agents in racial minority communities [22].
Previous studies have demonstrated disparities in SGLT2i and GLP-1RA utilization at the individual level. Data from national surveys as well as those from large private insurers and the Veterans Affairs healthcare system found patterns suggestive of lower SGLT2i and GLP1-RA prescribing for individual Black patients [23–26]. This was observed in a national British report as well [27]. Our study expands the existing evidence by finding such an association in a large publicly insured population across the US, a vast majority of whom are at an increased risk of cardiovascular morbidity and mortality due to a higher prevalence of cardiovascular conditions. Specifically, up to 44% of patients with diabetes in the Medicare age group have concomitant atherosclerotic cardiovascular disease and an estimated >20% have heart failure [28–32]. Recent clinical trial evidence suggests that these individuals would derive substantial benefit from cardioprotective anti-hyperglycemic therapy.
There was no consistent association between county-level socioeconomic markers and the use of novel antihyperglycemic agents. Neither measures of wealth nor measures of education were associated with SGLT2i prescribing. Higher median household income was associated with paradoxically lower indexed prescriptions of GLP-1RA in adjusted models. This may be a marker of lower levels of cardiovascular disease in more affluent counties as has been demonstrated in previous studies that found county measures of wealth have strong, negative correlations with cardiovascular mortality, which would support our assertion [33–36].
There was regional variation in the prescribing of cardioprotective antihyperglycemic agents indexed to metformin. In adjusted models, indexed prescriptions in the Northeast outnumbered those in the Midwest, while counties in the West had fewer indexed prescriptions. Such findings may aid policy interventions targeted at improving adoption of these drugs.
Counties with higher median age were associated with lower prescribing. This finding is paradoxical given the higher prevalence of cardiac disease with age and may represent avoidance of newer therapies in older adults. We emphasize that these findings are at the geographic and not individual level, though the association warrants further investigation.
The findings of the study should be interpreted in light of the following limitations. Our study focuses on patterns across US counties and cannot address the clinical and social risk profile of individual patients. Additionally, decisions that led to lack of prescribing of these drugs to individual patients was not available for analysis, but would represent an important avenue for future investigation. Second, we evaluated for the average cardiovascular risk profile of the county based on the prevalence of diabetes, smoking, and obesity, along with sociodemographic features, but patterns of certain risk factors such as established coronary artery disease, hypertension, and hyperlipidemia were not available. However, we presume that given the strong correlation between individual cardiovascular risk factors, we would identify counties with worse cardiovascular risk profiles based on the included measures. Third, if individuals received scripts for the same medications from multiple prescribers in the same year, they would be overcounted in the analysis. Additionally, not all Medicare Part D patients are covered for these drugs, or covered all the time. However, we do not expect such effects to be over-represented in counties with higher SGLT2i or GLP1-RA prescribing. Additionally, while we used metformin prescriptions as a surrogate for patients being actively managed for type 2 diabetes, the use of metformin for other indications, including prediabetes and polycystic ovarian syndrome, may be reflected in modest reductions in the observed use of SGLT2i and GLP1-RA as compared to metformin. However, the vast majority of metformin use is for patients with established type 2 diabetes as less than 1% of those with prediabetes are prescribed metformin and it is no longer strongly recommended for polycystic ovarian syndrome, and is therefore, unlikely to substantially affect our observations [37,[1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38]]. Finally, identifying counties based on city and state is slightly imprecise given variations in how administrative divisions are defined (e.g. census designated areas and townships) and because some cities span multiple counties, which may affect the results. However, these jurisdictions likely represent a small percentage of the data.
5. Conclusions
There was substantial variation in the use of cardioprotective anti-hyperglycemic agents across US counties; counties in the West, rural counties, and those with a larger proportion of Black individuals had a lower proportionate use of these agents relative to the number of Medicare beneficiaries being treated for type 2 diabetes. A higher county median age and rural location were associated with lower SGLT2i and GLP-1RA prescribing. These observations highlight a need for further investigation of potential disparities in the prescribing of cardioprotective antihyperglycemic drugs and the consequences.
Disclosures
Dr Krumholz reports receiving personal fees from UnitedHealth, IBM Watson Health, Element Science, Aetna, Facebook, F‐Prime, Siegfried & Jensen Law Firm, Arnold & Porter Law Firm, Martin/Baughman Law Firm, and the National Center for Cardiovascular Diseases, Beijing; serving as cofounder of HugoHealth and Refactor Health, and works under contract with Centers for Medicare and Medicaid Services; and grants from Medtronic and the Food and Drug Administration, Medtronic, Johnson & Johnson, and Shenzhen Center for Health Information outside the submitted work. Dr. Khera receives research support, through Yale, from Bristol-Myers Squibb. He is the coinventor of U.S. Provisional Patent Application No. 63/177,117, “Methods for neighborhood phenomapping for clinical trials” and a founder of Evidence2Health, a precision health platform to improve evidence-based cardiovascular care. The remaining authors have no disclosures to report.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Rohan Khera reports a relationship with Bristol-Myers Squibb that includes: funding grants. Rohan Khera reports a relationship with National Heart Lung and Blood Institute that includes: funding grants. Rohan Khera reports a relationship with Doris Duke Charitable Foundation that includes: funding grants. Harlan Krumholz reports a relationship with UnitedHealth Group that includes: consulting or advisory. Harlan Krumholz reports a relationship with IBM Watson Health that includes: board membership. Harlan Krumholz reports a relationship with Element Science that includes: consulting or advisory. Harlan Krumholz reports a relationship with Aetna Inc that includes: consulting or advisory. Harlan Krumholz reports a relationship with Facebook that includes: consulting or advisory. Harlan Krumholz reports a relationship with F-Prime that includes: consulting or advisory. Harlan Krumholz reports a relationship with Siegfried & Jensen Law Firm that includes: consulting or advisory. Harlan Krumholz reports a relationship with Arnold & Porter Law Firm that includes: consulting or advisory. Harlan Krumholz reports a relationship with Martin Baughman Law Firm that includes: consulting or advisory. Harlan Krumholz reports a relationship with National Center for Cardiovascular Diseases, Beijing that includes: consulting or advisory. Harlan Krumholz reports a relationship with Centers for Medicare and Medicaid Services that includes: employment. Harlan Krumholz reports a relationship with Medtronic Inc that includes: funding grants. Harlan Krumholz reports a relationship with US Food and Drug Administration that includes: funding grants. Harlan Krumholz reports a relationship with Johnson & Johnson that includes: funding grants. Harlan Krumholz reports a relationship with Shenzhen Center for Health Information that includes: funding grants. Rohan Khera has patent #63/177,117 pending to Rohan Khera. Cofounder of HugoHealth and Refactor Health - HK; Founder of Evidence2Health - RK
Funding
Dr Khera received support from the National Heart, Lung, and Blood Institute of the National Institutes of Health (Bethesda, Maryland) under the award K23HL153775 and the Doris Duke Charitable Foundation. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the article; and decision to submit the article for publication.
References
- 1.Zelniker T.A., Wiviott S.D., Raz I., et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393:31–39. doi: 10.1016/S0140-6736(18)32590-X. [DOI] [PubMed] [Google Scholar]
- 2.Zelniker T.A., Wiviott S.D., Raz I., et al. Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus. Circulation. 2019;139:2022–2031. doi: 10.1161/CIRCULATIONAHA.118.038868. [DOI] [PubMed] [Google Scholar]
- 3.Marso S.P., Bain S.C., Consoli A., et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:1834–1844. doi: 10.1056/NEJMoa1607141. [DOI] [PubMed] [Google Scholar]
- 4.Zinman B., Wanner C., Lachin J.M., et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association Professional Practice C. 9 Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2022. Diabetes Care. 2021;45:S125. doi: 10.2337/dc21-S009. -S43. [DOI] [PubMed] [Google Scholar]
- 6.Das S.R., Everett B.M., Birtcher K.K., et al. 2018 ACC expert consensus decision pathway on novel therapies for cardiovascular risk reduction in patients with type 2 diabetes and atherosclerotic cardiovascular disease: a report of the American college of cardiology task force on expert consensus decision pathways. J Am Coll Cardiol. 2018;72:3200–3223. doi: 10.1016/j.jacc.2018.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nargesi A.A., Jeyashanmugaraja G.P., Desai N., Lipska K., Krumholz H., Khera R. Contemporary national patterns of eligibility and use of novel cardioprotective antihyperglycemic agents in type 2 diabetes mellitus. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.121.021084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schernthaner G., Shehadeh N., Ametov A.S., et al. Worldwide inertia to the use of cardiorenal protective glucose-lowering drugs (SGLT2i and GLP-1 RA) in high-risk patients with type 2 diabetes. Cardiovasc Diabetol. 2020;19:185. doi: 10.1186/s12933-020-01154-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma A., Aziz H., Verma S., et al. Permission to prescribe: do cardiologists need permission to prescribe diabetes medications that afford cardiovascular benefit? Curr Opin Cardiol. 2021 doi: 10.1097/HCO.0000000000000892. [DOI] [PubMed] [Google Scholar]
- 10.Sangha V., Lipska K., Lin Z., et al. Patterns of prescribing sodium-glucose cotransporter-2 inhibitors for Medicare beneficiaries in the United States. Circ Cardiovasc Qual Outcomes. 2021 doi: 10.1161/CIRCOUTCOMES.121.008381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cunningham L.C., Fonarow G.C., Yancy C.W., et al. Regional variations in heart failure quality and outcomes: get with the guidelines-heart failure registry. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.120.018696. -e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kolte D., Khera S., Aronow W.S., et al. Regional variation in the incidence and outcomes of in-hospital cardiac arrest in the United States. Circulation. 2015;131:1415–1425. doi: 10.1161/CIRCULATIONAHA.114.014542. [DOI] [PubMed] [Google Scholar]
- 13.Vallabhajosyula S., Patlolla S.H., Dunlay S.M., et al. Regional variation in the management and outcomes of acute myocardial infarction with cardiogenic shock in the United States. Circ Heart Fail. 2020;13 doi: 10.1161/CIRCHEARTFAILURE.119.006661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pilote L., Califf R.M., Sapp S., et al. Regional variation across the United States in the management of acute myocardial infarction. N Engl J Med. 1995;333:565–572. doi: 10.1056/NEJM199508313330907. [DOI] [PubMed] [Google Scholar]
- 15.Kumar A., Fonarow G.C., Eagle K.A., et al. Regional and practice variation in adherence to guideline recommendations for secondary and primary prevention among outpatients with atherothrombosis or risk factors in the United States: a report from the REACH Registry. Crit Pathw Cardiol. 2009;8:104–111. doi: 10.1097/HPC.0b013e3181b8395d. [DOI] [PubMed] [Google Scholar]
- 16.Donohue J.M., Morden N.E., Gellad W.F., et al. Sources of regional variation in Medicare part D drug spending. N Engl J Med. 2012;366:530–538. doi: 10.1056/NEJMsa1104816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bittner V., Colantonio L.D., Dai Y., et al. Association of region and hospital and patient characteristics with use of high-intensity statins after myocardial infarction among medicare beneficiaries. JAMA Cardiol. 2019;4:865–872. doi: 10.1001/jamacardio.2019.2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medicare Part D Prescribers Methodology. CMS. (Accessed May 5, 2021, at https://data.cms.gov/resources/medicare-part-d-prescribers-methodology).
- 19.Social Determinants of Health Database. Agency for healthcare quality and research. (Accessed May 5, 2021, at https://www.ahrq.gov/sdoh/data-analytics/sdoh-data.html).
- 20.Pickens C.M., Pierannunzi C., Garvin W., Town M. Surveillance for certain health behaviors and conditions among states and selected local areas - behavioral risk factor surveillance system, United States. MMWR Surveill Summ. 2015;67:1–90. doi: 10.15585/mmwr.ss6709a1. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.United States Cities Database. SimpleMaps. (Accessed May 5, 2021, at https://simplemaps.com/data/us-cities).
- 22.Essien U.R., Dusetzina S.B., Gellad W.F. A policy prescription for reducing health disparities—achieving pharmacoequity. JAMA. 2021;326:1793–1794. doi: 10.1001/jama.2021.17764. [DOI] [PubMed] [Google Scholar]
- 23.Nargesi A.A., Jeyashanmugaraja G.P., Desai N., Lipska K., Krumholz H., Khera R. Contemporary national patterns of eligibility and use of novel cardioprotective antihyperglycemic agents in type 2 diabetes mellitus. J Am Heart Assoc. 2021 doi: 10.1161/JAHA.121.021084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eberly L.A., Yang L., Eneanya N.D., et al. Association of race/ethnicity, gender, and socioeconomic status with sodium-glucose cotransporter 2 inhibitor use among patients with diabetes in the US. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.6139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahtta D., Ramsey D.J., Lee M.T., et al. Utilization rates of SGLT2 inhibitors and GLP-1 receptor agonists and their facility-level variation among patients with atherosclerotic cardiovascular disease and type 2 diabetes: insights from the department of veterans affairs. Diabetes Care. 2022;45:372–380. doi: 10.2337/dc21-1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eberly L.A., Yang L., Essien U.R., et al. Racial, ethnic, and socioeconomic inequities in glucagon-like peptide-1 receptor agonist use among patients with diabetes in the US. JAMA Health Forum. 2021;2 doi: 10.1001/jamahealthforum.2021.4182. -e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whyte M.B., Hinton W., McGovern A., et al. Disparities in glycaemic control, monitoring, and treatment of type 2 diabetes in England: a retrospective cohort analysis. PLoS Med. 2019;16 doi: 10.1371/journal.pmed.1002942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bertoni A.G., Hundley W.G., Massing M.W., Bonds D.E., Burke G.L., Goff D.C. Heart failure prevalence, incidence, and mortality in the elderly with diabetes. Diabetes Care. 2004;27:699–703. doi: 10.2337/diacare.27.3.699. [DOI] [PubMed] [Google Scholar]
- 29.Dunlay S.M., Givertz M.M., Aguilar D., et al. Type 2 diabetes mellitus and heart failure: a scientific statement from the American heart association and the heart failure society of America: this statement does not represent an update of the 2017 ACC/AHA/HFSA heart failure guideline update. Circulation. 2019;140:e294–e324. doi: 10.1161/CIR.0000000000000691. [DOI] [PubMed] [Google Scholar]
- 30.Ness J., Nassimiha D., Feria M.I., Aronow W.S. Diabetes mellitus in older African-Americans, hispanics, and whites in an academic hospital-based geriatrics practice. Coron Artery Dis. 1999;10:343–346. doi: 10.1097/00019501-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Boonman-de Winter L.J., Rutten F.H., Cramer M.J., et al. High prevalence of previously unknown heart failure and left ventricular dysfunction in patients with type 2 diabetes. Diabetologia. 2012;55:2154–2162. doi: 10.1007/s00125-012-2579-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Corriere M., Rooparinesingh N., Kalyani R.R. Epidemiology of diabetes and diabetes complications in the elderly: an emerging public health burden. Curr Diab Rep. 2013;13:805–813. doi: 10.1007/s11892-013-0425-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khatana S.A.M., Venkataramani A.S., Nathan A.S., et al. Association between county-level change in economic prosperity and change in cardiovascular mortality among middle-aged US adults. JAMA. 2021;325:445–453. doi: 10.1001/jama.2020.26141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adepu S., Berman A.E., Thompson M.A. Socioeconomic determinants of health and county-level variation in cardiovascular disease mortality: an exploratory analysis of Georgia during 2014–2016. Prev Med Rep. 2020;19 doi: 10.1016/j.pmedr.2020.101160. (no pagination) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patel S.A., Ali M.K., Narayan K.M.V., Mehta N.K. County-level variation in cardiovascular disease mortality in the United States in 2009-2013: comparative assessment of contributing factors. Am J Epidemiol. 2016;184:933–942. doi: 10.1093/aje/kww081. [DOI] [PubMed] [Google Scholar]
- 36.Havranek E.P., Mujahid M.S., Barr D.A., et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American heart association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 37.Teede H.J., Misso M.L., Costello M.F., et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril. 2018;110:364–379. doi: 10.1016/j.fertnstert.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tseng E., Yeh H.C., Maruthur N.M. Metformin use in prediabetes among U.S. adults, 2005–2012. Diabetes Care. 2017;40:887–893. doi: 10.2337/dc16-1509. [DOI] [PMC free article] [PubMed] [Google Scholar]