Abstract
Background and Purpose—
Continuous positive airway pressure (CPAP) for the treatment of obstructive sleep apnea may improve stroke recovery, but adherence is poor. We assessed the effectiveness of an intensive CPAP adherence program during and after inpatient stroke rehabilitation on 3-month adherence and stroke recovery.
Methods—
In a single-arm study, 90 stroke rehabilitation patients were enrolled into an intensive CPAP adherence program. CPAP was continued after a run-in among qualifying patients with evidence of obstructive sleep apnea. The primary outcome was CPAP adherence, defined as ≥4 hours of use on ≥70% of days, over 3 months.
Results—
A total of 62 patients qualified for continued CPAP and 52 of these were willing to continue CPAP after discharge from rehabilitation. At 3 months, the average daily CPAP use was 4.7 hours (SD 2.6), and 32/52 (62%) patients were adherent. Factors significantly associated with adherence included more severe stroke, aphasia, and white race. Compared with nonadherent patients, adherent patients experienced greater improvements in the cognitive component of the Functional Independence Measure (P=0.02) and in the National Institutes of Health Stroke Scale (P=0.03).
Conclusions—
This intensive CPAP adherence program initiated during stroke rehabilitation can lead to CPAP adherence in the majority of patients with evidence of obstructive sleep apnea, including those with more severe stroke and aphasia, and may promote recovery.
Keywords: aphasia, apnea, continuous positive airway pressure, rehabilitation, sleep
Therapies to improve recovery after stroke are limited, especially in the subacute setting. Obstructive sleep apnea (OSA), a common yet under-recognized risk factor for stroke, is associated with worse functional outcome, longer hospitalization, and increased dependency following stroke.1 Continuous positive airway pressure (CPAP) may improve recovery after stroke, though poor adherence limits efficacy and could explain the inconsistent results seen in preliminary randomized trials of CPAP after stroke.2–4 Effective interventions are lacking that improve CPAP adherence after stroke. We, therefore, conducted a study in stroke patients undergoing inpatient rehabilitation (IPR) to assess the effectiveness of a multifaceted and intensive adherence program on 3-month CPAP adherence and measures of stroke outcome.
Methods
The data that support the findings of this study are available from the corresponding author on request. The SCOUTS (Stroke and CPAP Outcome Study) was a single-arm, open-label study performed at 2 IPR units of the University of Washington. For a summary of inclusion and exclusion criteria, see Supplemental Table I in the online-only Data Supplement. SCOUTS was approved by the University of Washington Human Subjects Review Committee. Participants provided written informed consent.
Enrolled stroke patients trialed auto-adjusting CPAP (4–20 cm H2O; Dream Station, Philips Respironics) over a 3-night run-in period during IPR. Devices were interrogated for nightly usage, average pressure, and a residual apnea-hypopnea index (the respiratory events per hour of sleep). At the end of the run-in period, evidence of OSA was determined based on airflow resistance detected by the machine (Methods in the online-only Data Supplement). Patients with evidence of OSA were eligible for CPAP treatment during IPR and after discharge from IPR.
Nurses, respiratory therapists, sleep technologists, and clinical psychologists initiated the SCOUTS intensive CPAP adherence protocol during IPR emphasizing early CPAP tolerance, individual motivation (Table II in the online-only Data Supplement) and support throughout the treatment period. The primary end point was CPAP adherence over 90 days from CPAP initiation, defined as ≥4 hours of use on ≥70% of days. Secondary efficacy end points were changes in the motor and cognitive components of the Functional Independence Measure (FIM) between admission and 3 to 4 months after discharge from IPR and in the National Institutes of Health Stroke Scale (NIHSS) between enrollment and 90 days. For details of the adherence program, efficacy end points, and statistical analyses, see Methods in the online-only Data Supplement.
Results
Between June 2016 and March 2018, 90 patients with stroke were enrolled. Over the 3-night run-in period with auto-adjusting CPAP, 28 patients (31%) were excluded: 14 with CPAP use <3 hours, 5 with no evidence of OSA, and 9 with evidence of central or complex sleep apnea. Among the 62 patients (69%) with evidence of OSA, 52 (84%) chose to continue CPAP on IPR discharge. At the end of the 90-day treatment period, average daily CPAP use among these 52 patients was 4.7 hours (SD 2.6) with average use on 5.4 d/wk and an average residual apnea-hypopnea index of 6.1 events/h. Over the 90 days, 32 patients (62%) were adherent (Table 1). After controlling for baseline factors and IPR length of stay, significant and independent predictors of 3-month adherence included NIHSS ≥5, aphasia, and white race (Table III in the online-only Data Supplement). Among those with 3-month outcome measures, adherent patients had significantly greater improvements in the cognitive FIM and NIHSS compared with nonadherent (Table 2; Figure). Descriptive results based on dichotomizing these measures are provided in Table IV in the online-only Data Supplement. In the adjusted analyses (Table 2), those who were adherent with CPAP had an estimated 7.0-point (95% CI, 2.2–11.8) greater improvement over 3 months in the cognitive component of the FIM and 1.6-point NIHSS score (95% CI, 0.2–3.1) improvement compared with those who were not adherent. With the adjustment, the cognitive FIM differences were more significant, but the NIHSS differences were less significant (Table 2). These changes in P values were driven mostly by imbalances in race and baseline stroke severity. The change in motor FIM was not significant in either unadjusted or adjusted analyses.
Table 1.
Main Characteristics of CPAP Adherent and Nonadherent Patients
| Patient Characteristics | Adherent (n=32) | Nonadherent (n=20) | P Value |
|---|---|---|---|
| Age, mean (SD), y | 58.6 (10.4) | 59.6 (11.5) | 0.89 |
| Women, n (%) | 10 (31) | 10 (50) | 0.18 |
| White non-Hispanic, n (%) | 24 (75) | 7 (35) | <0.01 |
| Body mass index, mean (SD), kg/m2 | 30.4 (5.9) | 30.4 (8.3) | 0.99 |
| Hypertension, n (%) | 19 (59) | 12 (60) | 0.96 |
| Diabetes mellitus, n (%) | 9 (28) | 5 (25) | 0.81 |
| Hyperlipidemia, n (%) | 10 (31) | 9 (45) | 0.32 |
| Total ischemic stroke, n (%) | 22 (69) | 13 (65) | 0.78 |
| Total hemorrhagic stroke, n (%) | 10 (31) | 7 (35) | 0.78 |
| Aphasia, n (%) | 14 (44) | 1 (5) | <0.01 |
| Neglect, n (%) | 2 (6) | 3 (15) | 0.30 |
| NIHSS on CPAP initiation, mean (SD) | 6.5 (4.3) | 4.1 (2.2) | 0.02 |
| Epworth Sleepiness Scale, mean (SD) | 9.6 (5.0) | 9.5 (4.6) | 0.95 |
| Days from stroke to CPAP initiation, mean (SD) | 16.8 (21) | 14.1 (7.4) | 0.50 |
| Days on rehabilitation unit, mean (SD) | 16.4 (7.4) | 15.4 (10.7) | 0.72 |
| Average h/day CPAP used, mean (SD) | 6.5 (1.1) | 1.8 (1.3) | <0.01 |
| Average d/wk CPAP used, mean (SD) | 6.6 (0.4) | 3.4 (1.9) | <0.01 |
CPAP indicates continuous positive airway pressure; and NIHSS, National Institutes of Health Stroke Scale.
Table 2.
Neurological and Functional Outcomes Among Adherent and Nonadherent Patients
| Adherent, Mean (SD) | Nonadherent, Mean (SD) | P Value* | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3 Months | Change | Baseline | 3 Months | Change | Unadjusted | Adjusted | |
| Motor FIM† | 48.5 (11.2) | 79.7 (12.1) | 31.2 (15.7) | 47.3 (17.6) | 77.5 (10.8) | 30.2 (13.2) | 0.83 | 0.65 |
| Cognitive FIM† | 24.1 (6.9) | 32.4 (3.7) | 8.2 (6.5) | 28.5 (3.9) | 33.1 (2.4) | 4.6 (3.0) | 0.03 | 0.02 |
| NIHSS‡ | 6.5 (4.3) | 2.7 (3.1) | −3.8 (2.6) | 4.1 (2.2) | 2.6 (2.6) | −1.6 (2.2) | 0.003 | 0.03 |
FIM indicates Functional Independence Measure; and NIHSS, National Institutes of Health Stroke Scale.
Difference between mean changes in outcome between adherent and nonadherent patients: unadjusted using t test with unequal variances and adjusted for age, sex, body mass index, race, and baseline NIHSS using linear regression.
n=22 adherent group and n=12 nonadherent.
n=30 adherent group and n=19 nonadherent.
Figure.
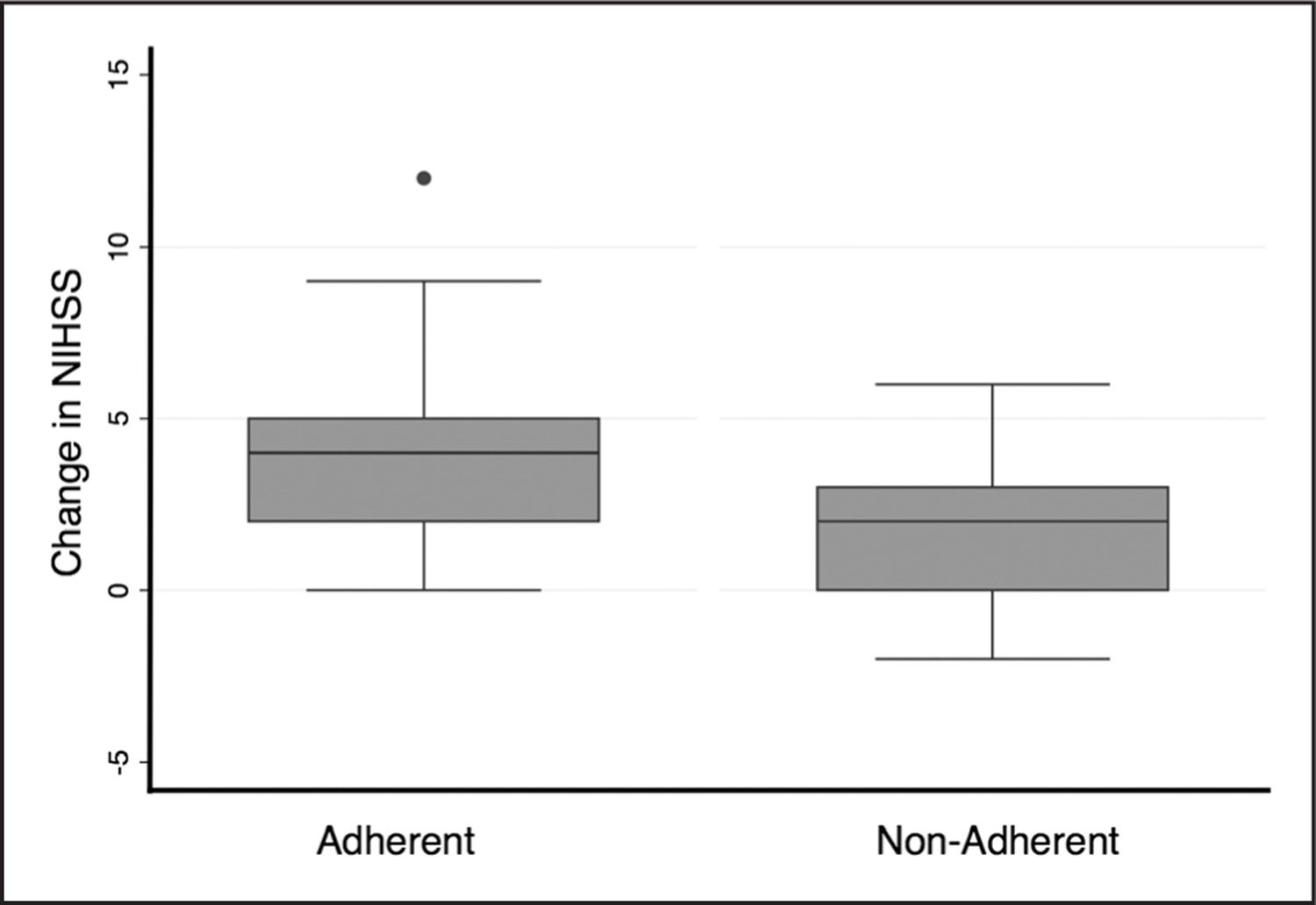
Changes over 3 mo in stroke severity by adherence status. Participants adherent to continuous positive airway pressure (CPAP) had significantly greater improvements in the National Institutes of Health Stroke Scale (NIHSS; 4 [interquartile range (IQR), 2, 5] versus 2 [IQR, 0, 3], P=0.005) compared with nonadherent participants.
Discussion
This single-arm study of patients with stroke demonstrates that this intensive CPAP adherence program initiated during IPR can facilitate CPAP adherence in the majority of patients with evidence of OSA, including those with more severe stroke and aphasia. Participants adherent to CPAP compared with those who were not improved more in measures of cognitive recovery and stroke severity. Many prior randomized trials of CPAP after stroke have investigated adherence only within the supportive IPR environment and for a shorter treatment period.2,4 In one trial, CPAP during IPR improved aspects of cognition after 4 weeks but not mobility, self-care skills, or NIHSS scores.2 The poor average CPAP adherence of only 2.5 h/night in that study may have been insufficient to yield benefit. Assuming a dose-response relationship, the number of hours of CPAP use to achieve stroke recovery may need to be higher, especially given that CPAP may be more beneficial later in the night during rapid eye movement sleep when apneic events and hypoxemia are often most severe. In another IPR trial with average daily adherence of nearly 5 hours, CPAP use over 4 weeks improved both neurological and functional recovery, though more in motor than cognitive function.4 However, patients with more severe aphasia were excluded from this study. CPAP use of >6 hours nightly in the adherent group of our study is comparable to a study of patients with ischemic stroke enrolled within the hospital and treated with CPAP over 24 months, where average daily adherence was 5.3 hours.3 In this trial, stroke severity and functional recovery improved at 1 month in patients treated with CPAP compared with controls but not at 3, 12, or 24 months, suggesting that early benefits of CPAP were lost over time. However, this trial focused on motor rather than cognitive recovery and did not account for potential late cross-overs whereby control subjects initiated CPAP. Also, this study enrolled patients with stroke not participating in IPR, potentially suggesting the need for both IPR and adequate CPAP use for a sustained benefit in stroke recovery.
The limitations of our study include the small sample size, short follow-up period, and missing outcome measures. How patient factors associated with adherence in general, not CPAP in particular, may affect outcomes will need to be addressed in future studies that include control subjects. Finally, in this study, the diagnosis of OSA was based on airflow resistance rather than a diagnostic sleep study.
Conclusions
Our findings suggest that CPAP adherence can be achieved and sustained over the 3-month period of maximal stroke recovery with this intensive CPAP adherence program initiated during IPR. Early CPAP tolerance and long-term adherence have been major limitations of prior studies in patients with stroke. Improved CPAP adherence in our study may be the result of the individually tailored and multifaceted SCOUTS intensive CPAP adherence program. Although our findings suggest that CPAP adherence improves stroke outcome, larger randomized trials are needed to assess this potential benefit.
Supplementary Material
Sources of Funding
This work was supported by grants from the American Sleep Medicine Foundation and the University of Washington (UW) Institute of Translational Health Sciences. Philips Respironics (Murrysville, PA) and ResMed (San Diego, CA) provided continuous positive airway pressure (CPAP) devices and masks for the study.
Footnotes
The online-only Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/STROKEAHA.119.024795.
Clinical Trial Registration—URL: https://www.clinicaltrials.gov. Unique identifier: NCT02809430.
Disclosures
None.
Contributor Information
Sandeep Khot, Department of Neurology, University of Washington School of Medicine, Seattle..
Heather Barnett, Department of Physical Medicine and Rehabilitation, University of Washington School of Medicine, Seattle..
Arielle Davis, Department of Neurology, University of Washington School of Medicine, Seattle..
Jenny Siv, Department of Neurology, University of Washington School of Medicine, Seattle..
Deborah Crane, Department of Physical Medicine and Rehabilitation, University of Washington School of Medicine, Seattle..
Allison Kunze, Department of Neurology, University of Washington School of Medicine, Seattle..
Denise Li Lue, Department of Physical Medicine and Rehabilitation, University of Washington School of Medicine, Seattle..
Aaron Bunnell, Department of Physical Medicine and Rehabilitation, University of Washington School of Medicine, Seattle..
Barbara McCann, Department of Psychiatry and Behavioral Sciences, University of Washington School of Medicine, Seattle..
Charles Bombardier, Department of Physical Medicine and Rehabilitation, University of Washington School of Medicine, Seattle..
W.T. Longstreth, Jr, Department of Neurology, University of Washington School of Medicine, Seattle..
Nathaniel Watson, Department of Neurology, University of Washington School of Medicine, Seattle..
Martha Billings, Division of Pulmonary, Critical Care and Sleep Medicine, Department of Medicine, University of Washington School of Medicine, Seattle..
References
- 1.Kaneko Y, Hajek VE, Zivanovic V, Raboud J, Bradley TD. Relationship of sleep apnea to functional capacity and length of hospitalization following stroke. Sleep 2003;26:293–297. [DOI] [PubMed] [Google Scholar]
- 2.Aaronson JA, Hofman WF, van Bennekom CA, van Bezeij T, van den Aardweg JG, Groet E, et al. Effects of continuous positive airway pressure on cognitive and functional outcome of stroke patients with obstructive sleep apnea: a randomized controlled trial. J Clin Sleep Med 2016;12:533–541. doi: 10.5664/jcsm.5684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parra O, Sánchez-Armengol A, Bonnin M, Arboix A, Campos-Rodríguez F, Pérez-Ronchel J, et al. Early treatment of obstructive apnoea and stroke outcome: a randomised controlled trial. Eur Respir J 2011;37:1128–1136. doi: 10.1183/09031936.00034410 [DOI] [PubMed] [Google Scholar]
- 4.Ryan CM, Bayley M, Green R, Murray BJ, Bradley TD. Influence of continuous positive airway pressure on outcomes of rehabilitation in stroke patients with obstructive sleep apnea. Stroke 2011;42:1062–1067. doi: 10.1161/STROKEAHA.110.597468 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


