Abstract
Objective: The objectives were to assess early childhood caries (ECC) in rural areas of El Salvador and to investigate the changes in caries and mouth pain in the presence of community-based interventions. Methods: This study was a retrospective analysis of de-identified and anonymous data obtained from baseline and four annual follow-up visits that focused on the preventive oral health intervention and nutrition in a convenience sample of children 0–6 years of age. The decayed, missing and filled teeth (dmft) index for primary teeth was used as the survey tool. Caries was defined as a cavitated lesion. Descriptive statistics were used to describe the prevalence of ECC in the sample in relation to age and dmft score. Linear mixed model analysis of variance (ANOVA) and generalised linear mixed effects models were used to compare the pre-intervention and post-intervention outcomes. Results: The prevalence of caries was 58%. Incorporation of a community oral health education and fluoride supplementation programme contributed to significant reductions in caries experience (from 74% to 61%) and mouth pain (from 58% to 39%), in children 3–6 years of age. Conclusions: ECC is a common public health problem in rural El Salvador. In an established community-based maternal-child health programme in El Salvador, there appears to be an association between the incorporation of preventive oral health intervention and improvement in children’s oral health and quality of life over time.
Key words: Mouth pain, early childhood caries, community-based intervention
INTRODUCTION
The World Health Organization (WHO) identifies caries as one of the most prominent chronic diseases in the world, affecting 60–95% of children in developed and developing countries, with especially high rates in Latin America and Asia1. More than 80% of the world’s children live in developing countries where dental health-care resources are extremely limited2. From a public health perspective, the rate of early childhood caries (ECC) in developing countries is particularly alarming3., 4., 5..
Dental caries is a common chronic, bacterially mediated disease resulting from tooth-adherent bacteria, such as Streptococcus mutans, which cause disease when driven by ecological pressures. Thus, when oral bacteria are frequently exposed to fermentable carbohydrates, they metabolise sugars to produce acid, which, over time, demineralises tooth surfaces6., 7., 8..
The American Association of Pediatric Dentistry (AAPD) defines ECC as the presence of one or more decayed (noncavitated or cavitated lesions), missing (because of caries), or filled tooth surfaces in any primary tooth in a child under the age of 6. Severe ECC in children younger than 3 years of age is defined as any sign of smooth-surface caries. From ages 3–5, one or more cavitated, missing (because of caries), or filled smooth surfaces in primary maxillary anterior teeth or a decayed, missing, or filled score of ≥ 4 (at age 3), ≥ 5 (at age 4) or ≥ 6 (at age 5) surfaces also constitutes severe ECC. Caries-conducive dietary practices are established by 12 months of age and are maintained throughout early childhood9., 10.. Prolonged and frequent night-time bottle-feeding with cariogenic beverages increases the risk of caries11., 12., 13.. During night-time feeding, salivary flow is reduced and demineralisation occurs in the absence of salivary cleansing and buffering. Some evidence suggests that sugary liquids, as well as formula and breast milk, have cariogenic potential14.
To prevent ECC, the AAPD recommends minimising the frequency of sugar intake. Other important preventive factors include city water fluoridation, reducing baby bottle use and intake of dietary fermentable carbohydrates, and improved oral hygiene measures, including adequate plaque removal by daily tooth brushing, topical fluoride application (i.e. fluoride varnish) and regular dental office visits for screening and treatment15., 16., 17.. The optimal time to implement oral hygiene measures should be no later than the time of eruption of the first primary tooth (around 6 months of age)18., 19., 20.. In addition, toothbrushing with fluoridated toothpaste should be performed for young children by a parent twice daily3. A 2013 Cochrane systemic review showed that application of a fluoride varnish two to four times a year resulted in a reduction of caries by 64% and 44% in primary and permanent teeth, respectively21. Thus, most authorities have concluded that this is an extremely efficacious caries-preventive strategy to be used in public settings.
When these health maintenance practices are not adopted, and dental disease is allowed to develop and progress to cavities and abscesses, there are serious negative consequences on children’s oral health, and in turn, on their general health. Children’s quality of life can be significantly affected by dental pain. In a comparative study of two of the most common chronic paediatric diseases (asthma vs. dental caries), dental caries was shown to cause dental pain that can disturb children’s sleep, prevent them from playing and attending school and, most importantly, result in the inability to eat in the preceding week22.
Most global epidemiological studies on caries have been carried out in school-age children23., 24.. Few studies have looked at ECC and its risk factors in children from birth to 6 years of age11., 25., 26., 27.. However, as previous studies have shown18., 19., 20., prevention of dental caries is most effective in the preschool age group. Consequently, there is tremendous need to implement public-health interventions to prevent dental caries in preschool-age populations in developing countries. Such interventions must be accessible, affordable, culturally sensitive and effective. Unfortunately, there is a paucity of research on the feasibility and effectiveness of such interventions in developing countries2. Whilst we know that implementation of comprehensive dental-care programmes can substantially reduce morbidities associated with ECC, there is an urgent need to evaluate and adopt culturally and regionally appropriate intervention programs within the settings of developing countries28.
The aim of this study was to determine the prevalence and severity of ECC and oral pain in young children in rural El Salvador, and to evaluate the impact of oral health education and fluoride in reducing ECC and mouth pain in those communities.
METHODS
Research design
This study was a retrospective analysis of oral health and nutrition data derived from a community-based survey and intervention programme in rural El Salvador. De-identified and anonymous data were obtained from baseline and four annual follow-visits, which focused on oral health and nutrition in a convenience sample of children (0–6 years of age). The research was conducted in full accordance with the World Medical Association Declaration of Helsinki. The study was reviewed and approved by the Institutional Review Board at the University of California Office for the Protection of Human Subjects (2010-06-1655).
Intervention programme
ASAPROSAR (Asociación Salvadoreña Pro-Salud Rural – The Salvadoran Association for Rural Health) is a non-governmental, non-profit organisation that provides health, education, environmental and economic development programmes in El Salvador29. One of these programmes is designed to recruit and train rural community health workers, or health promoters, who are focused on maternal and children’s health and nutrition. The oral health programme was implemented as a partnership between the Salvadoran Ministry of Health and the University of California, Berkeley, School of Public Health in the 15 rural communities served by health promoters.
There were three main components to the preventive oral health intervention: (i) oral health education; (ii) distribution of oral care products (each child received a new toothbrush and toothpaste three times per year); and (iii) fluoride varnish application. The educational component included annual training of health promoters on topics regarding healthy and unhealthy foods, the importance of oral health and when to seek dental care. Health promoters then integrated the oral health education and practices into their work with parents through home visits and in preschools. Free toothbrushes and fluoride toothpaste were provided to all children and family members who were under the care of the health promoters. Lastly, fluoride varnish was applied to children’s teeth three times a year (except for a temporary suspension from July 2008 to July 2009).
Annual written reports and oral presentations identified areas of success and challenges (e.g. long duration of baby bottle use). Based on health promoters’ observations, the group developed a costumed character ‘The Bottle Fairy’ to take away babies’ bottles after their 1-year birthday. At the end of the 5-year pilot programme, ASAPROSAR continued the oral health programme with technical support from the Ministry of Health and supplies provided by Colgate Palmolive and private donors.
Data collection
Parents who participated in the dental intervention programme were required to give informed consent for their child’s and their own participation. The community health promoters explained the procedures, possible risks or discomforts and possible benefits. Written, informed consent was obtained from the parents before participating in the study.
Trained Spanish-speaking volunteers conducted interviews with the child’s primary caregiver (usually the mother), in as private a setting as possible. The interview questionnaire comprised 50 questions on household and mother and child characteristics: mother and child diet, oral hygiene and dental problems; medical and dental care utilisation; and the caregiver’s assessment of the child’s oral health and overall health. The interviewer read each question aloud and recorded the caregiver’s response on a data-collection form. Following the interviews, the UC Berkeley research team reviewed the forms for discrepancies, and conducted training updates for interviewers to address any problems. ASAPROSAR community health workers carried out the coordination, education on oral hygiene and fluoride varnish application three times a year in conjunction with dentists from the Ministry of Health.
Four licensed US dentists conducted children’s dental examinations. Caries was defined as a cavitated lesion. Caries were assessed by visual inspection using a headlamp under natural light and a dental mirror but without the use of a dental explorer. Children were examined in the position preferred for the examiner and for the child’s comfort – recumbent on a table, knee-to-knee with the mother or seated in a chair. During the dental examination, the status of each tooth was stated verbally for an assistant to record. The status categories included whether the tooth was deciduous, erupted, healthy, missing, decayed (only cavitated lesions were recorded) or filled. Thus, the decayed, missing or filled (dmft) index for primary teeth was used as the survey tool. At the initial health training session and annually, the dentists standardised their exam assessments by independently examining 3-5 children, and then comparing and reconciling their exam findings to ensure consistency between examiners. If any questionable judgments arose during the dental examinations, the examiners consulted with each other to agree upon the classification of a lesion. No official calibration tests were performed.
Statistical analyses
Study data were entered into Microsoft Excel (Microsoft, Redmond, WA) and verified by a second individual. Data were then translated into English. A trained study team member transferred de-identified coded data to spss 19.0 software (IBM, Armonk, NY, USA) for analysis. Descriptive statistics (counts and percentages) were used to describe the prevalence of ECC in the sample in relation to age and dmft score. Linear mixed model analysis of variance (ANOVA) was used to compare the pre-intervention and post-intervention caries counts and mouth pain frequency scores, and generalised linear mixed effects models were used to compare the pre-intervention and post-intervention binary caries variables. Age was included as a covariate. Random effects were included for village to account for clustering effects of the village, for family to account for correlations among siblings, and for subject to correlate multiple observations within a child over time.
RESULTS
Baseline results
Demographics
Table 1 illustrates the baseline (2006) demographic characteristics of the study population (children, mother and household), nutritional practices of children and oral health practices of both children and mothers. A total of 886 children were seen for 1,259 dental visits from 2006 to 2010. The children’s mean age was 3.9 years. The mothers had a mean age of 30.5 years and a mean level of education of 4.5 years. Of these households, 55% had potable water and 78% had electricity. Whilst nearly all (96%) children were breastfed, nearly half (45%) of the children were given a baby bottle, which often included sugary and acidic liquids such as coffee (7%), lemonade (14%) or juice, soda or sugary water (51%). Baseline survey data showed that 84% of children had a toothbrush, 74% had toothpaste and that only 30% had been to a dentist.
Table 1.
Demographic characteristics at baseline (2006)
| Characteristics | |
|---|---|
| Child (n = 204) | |
| Participating child mean age (years) | 3.9 (1.70) |
| Participating child gender (M/F) | 42/58 |
| Participating child immunisation up-to-date | 96 |
| Mother age (years) | 30.5 (9.57) |
| Mother’s level of education | 4.5 (3.4) |
| Mother’s prenatal care visits | 90 |
| Number of children in family | 3.0 (1.8) |
| Number living in the house | 5.1 (1.8) |
| Potable water | 55 |
| Electricity | 78 |
| Cooking materials | |
| Wood only | 41 |
| Wood and gas | 41 |
| Gas only | 18 |
| Nutrition practices | |
| Child ever breast fed | 96 |
| How long breast fed (months) | 17.8 (11.9) |
| Child ever bottle fed | 45 |
| How long bottle fed (months) | 25.4 (10.2) |
| Child drinks in the bottle | |
| Water | 13 |
| Milk | 38 |
| Formula | 4 |
| Coffee | 7 |
| Lemonade | 14 |
| Natural juice | 13 |
| Artificial juice | 19 |
| Soda | 8 |
| Sugar water | 11 |
| Oral health practices | |
| Participating child has a toothbrush | 84 |
| Participating child has toothpaste | 74 |
| Mother reports brushing child’s teeth | 65 |
| Participating child ever been to the dentist | 30 |
| Mother never been to the dentist | 54 |
| Mother last dental visit because of mouth pain | 60 |
Values are given as mean (standard deviation) or percentage. F, female; M, male.
Table 2 illustrates the percentage of children in each age group according to year. The results of this study show that the prevalence of caries, dmft (extent of caries experience) and mouth pain increased with age (Figure 1a–c). The prevalence of caries in the primary dentition increased from 10% at age 1 to 100% at age 6 (Figure 1a). The dmft score increased from <1 at age 1 to approximately 8 at age 6 (Figure 1b). The steepest slope for the increase in prevalence of caries and dmft was from birth to 3 years of age. The prevalence of mouth pain increased from approximately 25% of 3-year-old children to 50% of 6-year-old children.
Table 2.
Number of children in each age group according to year
| Age (years) | 2006 | 2007 | 2008 | 2009 | 2010 |
|---|---|---|---|---|---|
| 0 | 7 (15) | 25 (18) | 22 (20) | 19 (15) | 21 (14) |
| 1 | 19 (41) | 54 (39) | 49 (44) | 59 (45) | 52 (36) |
| 2 | 20 (43) | 59 (43) | 40 (36) | 52 (40) | 73 (50) |
| 3 | 27 (17) | 35 (23) | 42 (32) | 32 (29) | 43 (32) |
| 4 | 44 (28) | 41 (27) | 35 (27) | 26 (23) | 31 (23) |
| 5 | 50 (32) | 44 (29) | 33 (25) | 32 (29) | 37 (28) |
| 6 | 37 (23) | 34 (22) | 22 (17) | 21 (19) | 22 (17) |
| Total n | 204 | 292 | 243 | 241 | 279 |
Values are given as n (%) or n.
Figure 1.
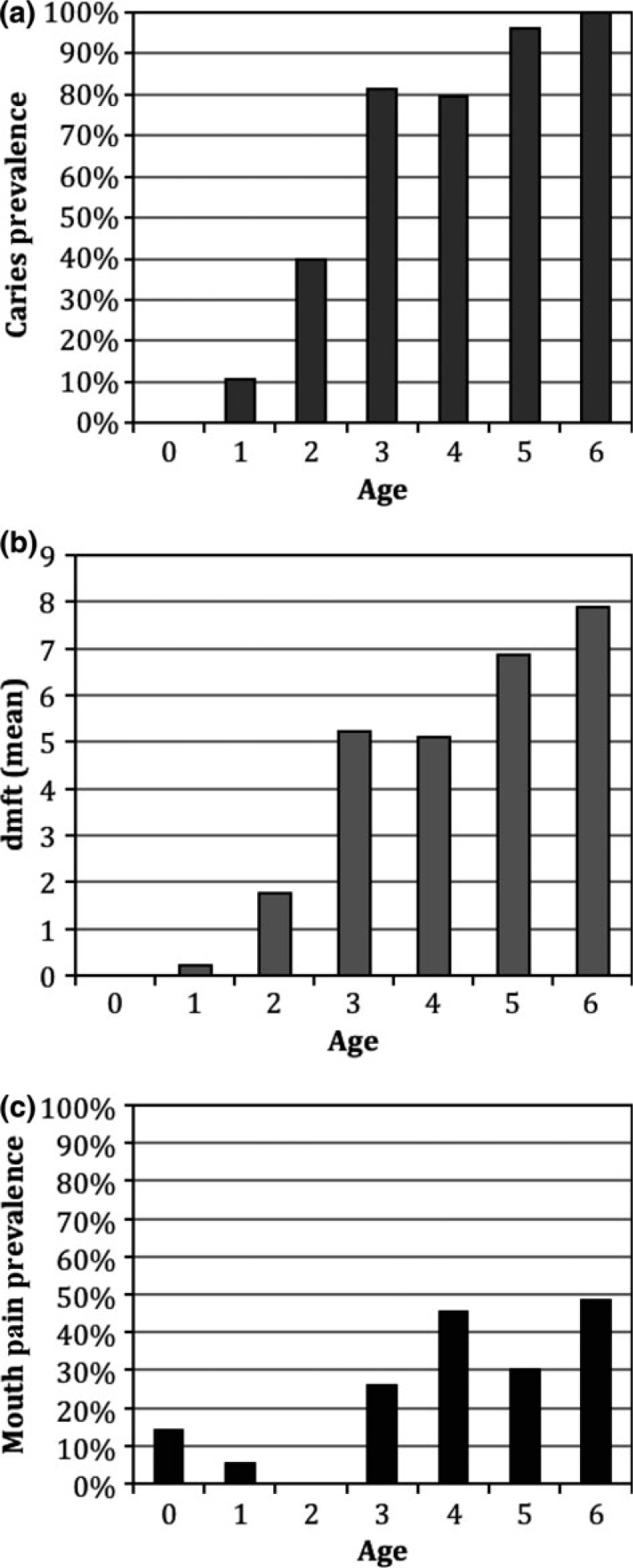
Mean decayed, missing and filled teeth (dmft) scores for primary teeth and the prevalence of caries and mouth pain increased with age in young El Salvadorean children from rural communities. The bar charts illustrate the prevalence of caries (a), dmft score (b) and mouth pain prevalence (c) across different age groups (n = 1,259 dental visits).
A cross-sectional evaluation of cavitated caries lesions in children from 2006 to 2010 is shown in Figure 2. Caries prevalence decreased from a high of 90% to a low of 70% from years 2006 to 2008, then when the intervention was interrupted, the numbers again increased to a high of 85% by year 2010. Similarly, mean dmft scores decreased from a high of 6.34 to a low of 4.27 from years 2006 to 2008, then when the intervention ceased/was interrupted the numbers again increased to a high of 4.92 by year 2010. For children 0–2 years of age, the prevalence of untreated dental caries, dmft and mouth pain did not significantly differ from 2006 to 2010.
Figure 2.
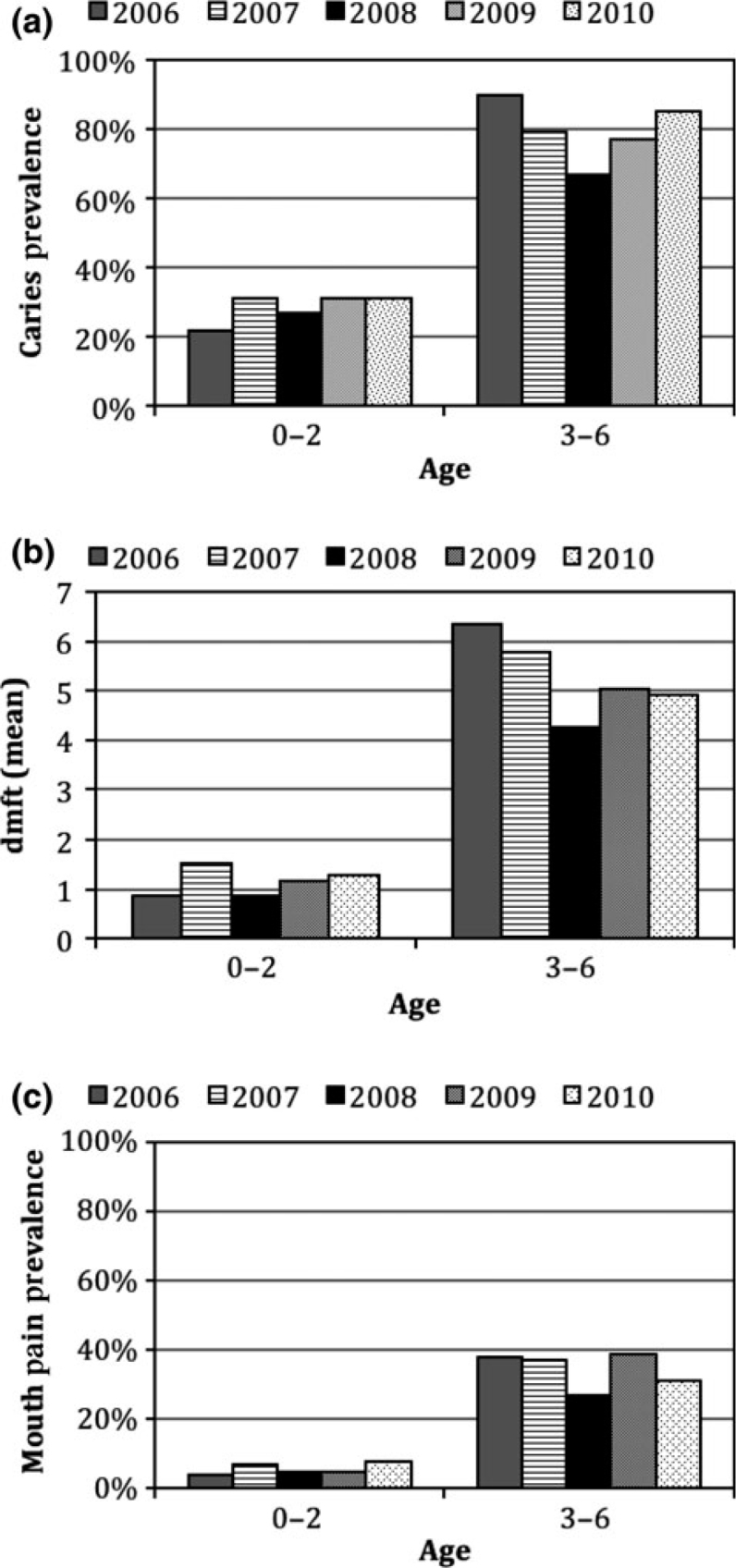
Mean decayed, missing and filled teeth (dmft) scores for primary teeth and the prevalence of caries and mouth pain in young El Salvadorean children from rural communities fluctuated in tandem with the presence of a community-based intervention programme. The bar charts illustrate the prevalence of caries (a), dmft score (b) and mouth pain prevalence (c) over time (2006–2010; n = 1,259 dental visits).
An assessment of the longitudinal data revealed that 273 children had at least one return dental visit with the UC Berkeley research team over the course of the study. For children who needed urgent dental treatment, referrals were made to the Ministry of Health dental clinics.
The pre-intervention and post-intervention changes in dmft and mouth pain for the children 3–6 years of age is illustrated in Figures 3 and 4. For older children (of 3–6 years of age), there was statistically significant reduction in the prevalence of severe ECC (dmft + DMFT) over time, from 74% to 61% (Figure 3); a non-significant reduction was also observed for dmft + DMFT counts (6.04 ± 0.44 to 5.45 ± 0.37, P = 0.15). Similarly, these children also revealed a significant reduction in the frequency of mouth pain, from 58% to 39% (Figure 4). The younger children, 0–2 years of age, did not experience a significant reduction in dmft or mouth pain (Figures 3 and 4, dmft + DMFT counts 1.45 ± 0.37 to 1.37 ± 0.14).
Figure 3.
Older El Salvadorean children experienced a significant reduction in the prevalence of severe early childhood caries (ECC) over time following the adoption of a community-based intervention programme. The bar chart illustrates the levels of severe ECC (S-ECC) in different age groups, pre- and post-intervention (n = 1,092 dental visits) (*P < 0.05).
Figure 4.
Older El Salvadorean children experienced a significant reduction in mouth pain over time following the adoption of a community-based intervention programme. The graph illustrates the changes in mouth-pain frequency of different age groups, pre- and post-intervention (n = 1,092 dental visits) (*P < 0.05).
DISCUSSION
Prevalence and severity
This study documents a widespread problem of ECC in a sample of children from rural El Salvador. ECC was present in the first 2 years of life and increased steadily in prevalence and severity with age, affecting virtually all children by 6 years of age. The extent of high caries experience, the prevalence of untreated decayed teeth and mouth pain, and limited access to dental care among the children in this study indicate a pressing need for both prevention and treatment of ECC in this population.
In this study of rural El Salvadorian children, the prevalence of ECC (58%) appears similar to that reported in previous studies. A 2003 WHO report stated that the prevalence of caries (treated and untreated) globally was 60–90%1., 30.. However, in our study population, most of the lesions were untreated. Thus, the prevalence of untreated caries in the El Salvadorian population is significant and high compared with other places in the world because it represents primarily untreated ECC.
A recent systematic review and metaregression analysis of the prevalence of the global burden of disease showed that in 2010, caries in deciduous teeth was the 10th most-prevalent condition, with the highest prevalence at age 6. In that review, countries in southern Latin America exhibited an 85% prevalence rate of caries of primary teeth. According to the United States, National Health and Nutrition Examination Survey (US-NHANES), the prevalence of caries in primary teeth in 1999–2004 was: total = 27.90% and untreated = 20.48% in children 2–5 years of age; and total = 51.17% and untreated = 24.49% in children 6–11 years of age. However, within the US American Indian/Alaska Native (AI/AN) population, 68% of AI/AN children had experienced caries. In these children, the prevalence of untreated dental decay was 43.6%, and the mean dmft score was three times higher than for non-Natives31. AI/AN children have similar social, economic and cultural issues to children of rural El Salvador. Therefore, it is important to survey unique populations that may exhibit significantly different characteristics from the overall group, such as very high prevalence rates of ECC. These subpopulations may need intensive oral health interventions. Thus, although global and national surveys highlight mean caries prevalence or dmft values for whole populations, it is critical to acknowledge the caries values for subpopulations that represent the most significant disease; these may go unnoticed within the larger context of reported mean values. This underscores the health disparities that exist in large populations.
Socio-economic status
Socio-economic status (SES) is consistently associated with caries levels in children. Indicators such as income, education and urbanisation are usually used to determine SES. AI/AN risk factors for ECC show close association with SES6., 32., 33., 34.. Low SES is associated with lack of formal education, lack of preventive health care (i.e. prenatal or dental) and limited nutritional access. In an attempt to dissect the relationship between SES and ECC, some researchers have focused their studies on specific immigrant groups within the US population. Latino immigrant children showed higher-than-average rates of ECC, second only to those of Native American children6., 24., 26.. These findings confirm that economic barriers and limited maternal oral health knowledge are potential contributors to children’s poor oral health35. Factors related to maternal oral health beliefs and behaviours may vary with different SES and education levels. Among the mothers in our study in rural El Salvador, the level of education was less than 5 years. Only 13% of mothers sought regular dental care for themselves, and 50% had never seen a dentist. These findings support the role of both economic barriers and limited maternal oral health knowledge as potential contributors to childrens’ oral health. Thus, limited overall literacy and health literacy may have played a role in the increased risk for ECC in these communities.
Parental practices and risk factors
Caries is the result of a complex interaction among sociodemographic, behavioural and microbiological factors. Prolonged or night-time bottle-feeding was correlated with ECC in studies from Saudi Arabia, the USA and Turkey12., 36., 37.. Guidelines prepared by the American Academy of Pediatrics (AAP) suggest that parents should begin bottle weaning when their child is approximately 9 months of age and accomplish weaning soon after the child’s first birthday38. Studies from Japan and the USA showed that later weaning is also correlated with increased risk for ECC26., 39.. Increased availability of fermentable carbohydrates in baby bottles has been reported in more than half of Saudi Arabian children with ECC11., 40.. In India, a high frequency of consumption of fermentable carbohydrates, which were given as part of a reward system, was correlated with ECC41. In this study, 45% of children were bottle fed, for a time period ranging from 15.4 to 35.6 months, which is longer than the recommended duration suggested by the AAP. In our study, both prolonged bottle-feeding and the increased availability of fermentable carbohydrates contents in baby bottles, such as milk, natural juice, artificial juice and lemonade, may contribute to the high prevalence of ECC observed in rural Salvadorian children.
Another contributing factor for ECC is a phenomenon often referred to as ‘breastfeeding at will’ or ‘breastfeeding on demand’19. Evidence that breastfeeding leads to ECC is controversial and confusing. In studies from Brazil and Turkey, there were no significant correlations between breastfeeding and ECC9. However, studies from Japan and Saudi Arabia support a correlation between breastfeeding on demand and ECC when continued for more than 18 months39., 40.. Similarly in our study, in rural El Salvador, 96% of children were breastfed for longer than 17 months. Therefore, it appears that feeding habits and the contents of baby bottles can have an impact on ECC28., 42., 43..
Mouth pain
In this study, 60% of older children (3–6 years of age) with ECC reported oral pain. Studies have shown that children’s oral health significantly impacts their physical, mental and social well-being, as assessed by their parents44. Painful caries can lead to difficulty eating and sleeping and in paying attention at school. Pain can also lead to challenges with daily activities that can disturb basic functioning and growth and development. In addition, research has shown that children with ECC were rated by their parents as having worse oral health-related quality of life than caries-free children, and experienced significant improvements in complaint of pain, eating preferences, quantity of food eaten and sleeping habits after treatment of dental caries45. Although formally assessing quality of life was beyond the scope of this study, our finding that more than half of the older children reported oral pain may indicate impairments in quality of life for this population.
Effectiveness of the community-based intervention
In 2002, the WHO and United Nations Children’s Fund (UNICEF) developed a Global Strategy on Infant and Young Child Feeding to focus world attention on the impact of community-based interventions to improve feeding in infants and young children and the identification of factors important to ensure that interventions are successful and sustainable. In this study, oral health awareness and fluoride application starting in infancy were incorporated into a rural community health programme in El Salvador. The results of the intervention show reductions in caries experience and mouth pain experience in children 3–6 years of age, which is consistent with the WHO and UNICEF recommendations on sustainable and successful community health intervention programmes.
This community-based programme has unique advantages and limitations. One important advantage is that families and communities were not just beneficiaries of the interventions but also became resources to shape the interventions. The use of trained health workers from the community allowed the implementation of health care close to where mothers, other caregivers and young children lived2. After the conclusion of the study, the local community took ownership of the programme and ensured its sustainability. The results of the study showed improvements in oral health and aspects relating to the quality of life of the children. A limitation of this study was the absence of standardised inter-examiner calibration, as the dental examiners were volunteer US dentists who visited El Salvador annually.
CONCLUSION
This study shows that ECC is a common public health problem in rural El Salvador. Incorporation of oral health education, oral hygiene supplies and fluoride supplementation in an established community-based maternal-child health programme beginning in infancy, appears to show improvements in children’s oral health and quality of life over time. ASAPROSAR community health workers continue to provide education on oral hygiene and fluoride varnish application in conjunction with Ministry of Health dentists in El Salvador.
Acknowledgement
We would like to thank ASAPROSAR’s directors, community health workers, and the Salvadoran Ministry of Health dentists and US-based health professional and student volunteers who enthusiastically implemented the intervention. We also thank the Salvadoran families who participated in this programme. This study was supported by MICHR-PORT Grant, 2UL1TR000433.
Competing interest
This study had no competing interest.
References
- 1.Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century–the approach of the WHO Global Oral Health Programme. Commun Dent Oral Epidemiol. 2003;31(Suppl 1):3–23. doi: 10.1046/j..2003.com122.x. [DOI] [PubMed] [Google Scholar]
- 2.Bhutta ZA, Darmstadt GL, Hasan BS, et al. Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: a review of the evidence. Pediatrics. 2005;115(2 Suppl):519–617. doi: 10.1542/peds.2004-1441. [DOI] [PubMed] [Google Scholar]
- 3.Harris R, Nicoll AD, Adair PM, et al. Risk factors for dental caries in young children: a systematic review of the literature. Community Dent Health. 2004;21(1 Suppl):71–85. [PubMed] [Google Scholar]
- 4.Horton S, Barker JC. Rural Latino immigrant caregivers’ conceptions of their children’s oral disease. J Public Health Dent. 2008;68:22–29. doi: 10.1111/j.1752-7325.2007.00078.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lawrence HP, Binguis D, Douglas J, et al. A 2-year community-randomized controlled trial of fluoride varnish to prevent early childhood caries in Aboriginal children. Community Dent Oral Epidemiol. 2008;36:503–516. doi: 10.1111/j.1600-0528.2008.00427.x. [DOI] [PubMed] [Google Scholar]
- 6.Ramos-Gomez FJ, Weintraub JA, Gansky SA, et al. Bacterial, behavioral and environmental factors associated with early childhood caries. J Clin Pediatr Dent. 2002;26:165–173. doi: 10.17796/jcpd.26.2.t6601j3618675326. [DOI] [PubMed] [Google Scholar]
- 7.Keyes PH. The infectious and transmissible nature of experimental dental caries. Findings and implications. Arch Oral Biol. 1960;1:304–320. doi: 10.1016/0003-9969(60)90091-1. [DOI] [PubMed] [Google Scholar]
- 8.Takahashi N, Nyvad B. The role of bacteria in the caries process: ecological perspectives. J Dent Res. 2011;90:294–303. doi: 10.1177/0022034510379602. [DOI] [PubMed] [Google Scholar]
- 9.Santos AP, Soviero VM. Caries prevalence and risk factors among children aged 0 to 36 months. Pesqui Odontol Bras. 2002;16:203–208. doi: 10.1590/s1517-74912002000300004. [DOI] [PubMed] [Google Scholar]
- 10.Ismail AI. The role of early dietary habits in dental caries development. Spec Care Dentist. 1998;18:40–45. doi: 10.1111/j.1754-4505.1998.tb01357.x. [DOI] [PubMed] [Google Scholar]
- 11.Wyne AH, Chohan AN, al-Begomi R. Feeding and dietary practices of nursing caries children in Riyadh, Saudi Arabia. Odontostomatol Trop. 2002;25:37–42. [PubMed] [Google Scholar]
- 12.Olmez S, Uzamris M. Risk factors of early childhood caries in Turkish children. Turk J Pediatr. 2002;44:230–236. [PubMed] [Google Scholar]
- 13.Adair PM, Pine CM, Burnside G, et al. Familial and cultural perceptions and beliefs of oral hygiene and dietary practices among ethnically and socio-economicall diverse groups. Community Dent Health. 2004;21(1 Suppl):102–111. [PubMed] [Google Scholar]
- 14.Erickson PR, Mazhari E. Investigation of the role of human breast milk in caries development. Pediatr Dent. 1999;21:86–90. [PubMed] [Google Scholar]
- 15.Marinho VC. Cochrane reviews of randomized trials of fluoride therapies for preventing dental caries. Eur Arch Paediatr Dent. 2009;10:183–191. doi: 10.1007/BF03262681. [DOI] [PubMed] [Google Scholar]
- 16.Wong MC, Clarkson J, Glenny AM, et al. Cochrane reviews on the benefits/risks of fluoride toothpastes. J Dent Res. 2011;90:573–579. doi: 10.1177/0022034510393346. [DOI] [PubMed] [Google Scholar]
- 17.Tubert-Jeannin S, Auclair C, Amsallem E, et al. Fluoride supplements (tablets, drops, lozenges or chewing gums) for preventing dental caries in children. Cochrane Database Syst Rev. 2011;12:Cd007592. doi: 10.1002/14651858.CD007592.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berkowitz RJ, Jordan HV, White G. The early establishment of Streptococcus mutans in the mouths of infants. Arch Oral Biol. 1975;20:171–174. doi: 10.1016/0003-9969(75)90005-9. [DOI] [PubMed] [Google Scholar]
- 19.Gardner DE, Norwood JR, Eisenson JE. At-will breast feeding and dental caries: four case reports. ASDC J Dent Child. 1977;44:186–191. [PubMed] [Google Scholar]
- 20.Weiss ME, Bibby BG. Effects of milk on enamel solubility. Arch Oral Biol. 1966;11:49–57. doi: 10.1016/0003-9969(66)90117-8. [DOI] [PubMed] [Google Scholar]
- 21.Marinho VC, Worthington HV, Walsh T, et al. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2013;7:Cd002279. doi: 10.1002/14651858.CD002279.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thikkurissy S, Glazer K, Amini H, et al. The comparative morbidities of acute dental pain and acute asthma on quality of life in children. Pediatr Dent. 2012;34:e77–e80. [PubMed] [Google Scholar]
- 23.Arruda AO, Senthamarai Kannan R, Inglehart MR, et al. Effect of 5% fluoride varnish application on caries among school children in rural Brazil: a randomized controlled trial. Community Dent Oral Epidemiol. 2012;40:267–276. doi: 10.1111/j.1600-0528.2011.00656.x. [DOI] [PubMed] [Google Scholar]
- 24.Kaste LM, Selwitz RH, Oldakowski RJ, et al. Coronal caries in the primary and permanent dentition of children and adolescents 1–17 years of age: United States, 1988–1991. J Dent Res. 1996;75:631–641. doi: 10.1177/002203459607502S03. [DOI] [PubMed] [Google Scholar]
- 25.Holm AK. Caries in the preschool child: international trends. J Dent. 1990;18:291–295. doi: 10.1016/0300-5712(90)90125-x. [DOI] [PubMed] [Google Scholar]
- 26.Huntington NL, Kim IJ, Hughes CV. Caries-risk factors for Hispanic children affected by early childhood caries. Pediatr Dent. 2002;24:536–542. [PubMed] [Google Scholar]
- 27.Tinanoff N, Kanellis MJ, Vargas CM. Current understanding of the epidemiology mechanisms, and prevention of dental caries in preschool children. Pediatr Dent. 2002;24:543–551. [PubMed] [Google Scholar]
- 28.Kassebaum NJ, Bernabe E, Dahiya M, et al. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 2015;94:650–658. doi: 10.1177/0022034515573272. [DOI] [PubMed] [Google Scholar]
- 29.Brentlinger PE, Hernan MA, Hernandez-Diaz S, et al. Childhood malnutrition and postwar reconstruction in rural El Salvador: a community-based survey. JAMA. 1999;281:184–190. doi: 10.1001/jama.281.2.184. [DOI] [PubMed] [Google Scholar]
- 30.Mandeep Singh Virdi RDSM. Intech; 2012. Oral Health Care – Pediatric, Research, Epidemiology and Clinical Practices; pp. 149–163. [Google Scholar]
- 31.Tiwari T, Quissell DO, Henderson WG, et al. Factors Associated with Oral Health Status in American Indian Children. J Racial Ethn Health Disparities. 2014;1:148–156. doi: 10.1007/s40615-014-0017-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rogers AH. The source of infection in the intrafamilial transfer of Streptococcus mutans. Caries Res. 1981;15:26–31. doi: 10.1159/000260496. [DOI] [PubMed] [Google Scholar]
- 33.DenBesten P, Berkowitz R. Early childhood caries: an overview with reference to our experience in California. J Calif Dent Assoc. 2003;31:139–143. [PubMed] [Google Scholar]
- 34.Reisine S, Douglass JM. Psychosocial and behavioral issues in early childhood caries. Commun Dent Oral Epidemiol. 1998;26(1 Suppl):32–44. doi: 10.1111/j.1600-0528.1998.tb02092.x. [DOI] [PubMed] [Google Scholar]
- 35.Quinonez RB, Keels MA, Vann WF, Jr, et al. Early childhood caries: analysis of psychosocial and biological factors in a high-risk population. Caries Res. 2001;35:376–383. doi: 10.1159/000047477. [DOI] [PubMed] [Google Scholar]
- 36.Olmez S, Uzamis M, Erdem G. Association between early childhood caries and clinical, microbiological, oral hygiene and dietary variables in rural Turkish children. Turk J Pediatr. 2003;45:231–236. [PubMed] [Google Scholar]
- 37.Al-Malik MI, Holt RD, Bedi R. The relationship between erosion, caries and rampant caries and dietary habits in preschool children in Saudi Arabia. Int J Paediatr Dent. 2001;11:430–439. [PubMed] [Google Scholar]
- 38.Koranyi K, Rasnake LK, Tarnowski KJ. Nursing bottle weaning and prevention of dental caries: a survey of pediatricians. Pediatr Dent. 1991;13:32–34. [PubMed] [Google Scholar]
- 39.Tsubouchi J, Higashi T, Shimono T, et al. A study of baby bottle tooth decay and risk factors for 18-month old infants in rural Japan. ASDC J Dent Child. 1994;61:293–298. [PubMed] [Google Scholar]
- 40.Wyne AH. Caries prevalence, severity, and pattern in preschool children. J Contemp Dent Pract. 2008;9:24–31. [PubMed] [Google Scholar]
- 41.Jose B, King NM. Early childhood caries lesions in preschool children in Kerala, India. Pediatr Dent. 2003;25:594–600. [PubMed] [Google Scholar]
- 42.Azevedo TD, Bezerra AC, de Toledo OA. Feeding habits and severe early childhood caries in Brazilian preschool children. Pediatr Dent. 2005;27:28–33. [PubMed] [Google Scholar]
- 43.Hallett KB, O’Rourke PK. Early childhood caries and infant feeding practice. Community Dent Health. 2002;19:237–242. [PubMed] [Google Scholar]
- 44.Colak H, Dulgergil CT, Dalli M, et al. Early childhood caries update: a review of causes, diagnoses, and treatments. J Nat Sci Biol Med. 2013;4:29–38. doi: 10.4103/0976-9668.107257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cunnion DT, Spiro A, 3rd, Jones JA, et al. Pediatric oral health-related quality of life improvement after treatment of early childhood caries: a prospective multisite study. J Dent Child. 2010;77:4–11. [PMC free article] [PubMed] [Google Scholar]




