Abstract
Objective/Design
Sleep patterns change during college, and students may nap to compensate for lost sleep. Despite the increased prevalence of napping among students, few studies have investigated daily relations between napping and nocturnal sleep, as well as how timing of naps and nocturnal sleep might influence one another. The present study used daily dairies to capture the occurrence, timing, and duration of napping and relation to nocturnal sleep.
Setting/Participants
Daily diary data, collected for 4 to 7 days, from 654 college students from a mid-sized midwestern university (81.5% female).
Measurement
Participants reported nightly sleep durations, bedtimes, and wake times as well as nap durations and nap start times.
Results:
Multi-level modeling (MLM) and multi-level logistic regressions revealed bidirectional relations between nocturnal sleep and napping. Regarding nocturnal sleep and its relation to next day napping, nocturnal sleep (including shorter duration and later bedtime) was associated with increased odds of napping and longer napping the following day. Shorter sleep duration was also associated with taking an earlier nap, while later bedtime was associated with a later nap the following day. Regarding napping and its association with same-night nocturnal sleep, taking a nap was associated with longer sleep duration that night, however, later nap start times and longer nap durations were associated with later bedtimes that night.
Conclusions:
Findings provide evidence for bidirectional associations between napping and nocturnal sleep. Future studies are needed to explore how naps could be optimized to promote nocturnal sleep among college students, as well as for whom naps might be most beneficial.
Keywords: Sleep, nap, college, daily relations
Introduction
Napping is common among college students, with studies reporting between 43%-54% of college age samples napping at least once per week (1-3). Despite the prevalence of napping, there have been very few investigations of daily associations between napping and nighttime sleep, especially timing of napping and nighttime sleep, among college students, whose schedules may provide more opportunities for napping. Although napping may attenuate negative cognitive effects that result from short sleep (4), ill-timed naps could further delay bedtimes and shorten sleep duration (5). Using a daily diary methodology, the current study aims to characterize napping patterns and explore daily relations between napping (e.g., occurrence, duration, and timing) and nocturnal sleep patterns among a large sample of college students to better understand its potential benefits and consequences.
Prior reports suggest that sleep duration shortens, sleep timing becomes more irregular, and sleep is less efficient following the transition to college (6-9). Students are often required to adjust to new living arrangements (e.g., residential halls) or a new commute to campus. In addition, compared to high school, college is less structured and offers more flexible class schedules as well as increased academic, extracurricular and social commitments. All of these contextual factors may influence sleep. Specifically, to fulfill these obligations, students may need to alter their sleep patterns by staying up later and napping in between classes (1). However, it is important to consider napping within the larger context of circadian rhythms and sleep pressure (homeostatic sleep drive). The Two-Process Model proposes that two systems, the 24-hour circadian timing system (Process C) and the homeostatic system (Process S), interact together to control sleep duration and timing (10). Process C dictates the timing of sleep across a 24-hour period and is influenced by the dark and light cycles, while Process S is influenced by previous sleep and wake history. In Process S, as a period of wakefulness extends, sleep pressure increases, and as sleep occurs, sleep pressure dissipates. Staring in adolescence, circadian timing (Process C) is delayed and sleep pressure (Process S) takes longer to build, often contributing to later bedtimes (11, 12). Prior reports propose that sleep timing is most delayed among emerging adults (13). Napping may delay bedtimes even further, as napping may reduce sleep pressure typically built before bed, thereby contributing to circadian misalignment and disrupted sleep patterns (e.g., delayed bedtimes). Therefore, studying the impact of napping on these processes is especially important to investigate during this emerging adulthood developmental period.
Studies have identified associations between various aspects of napping (i.e., frequency, timing, and duration) and nightly sleep patterns using cross-sectional data. Among college students, nappers reported shorter sleep compared to non-nappers (14) and students napping more than 3 times per week reported poor nighttime sleep (1). Students also reported poor nighttime sleep when their naps were longer than 2 hours and when their naps occurred later in the day (between 6 and 9 pm) (1). Similar findings have been reported among adolescents, where later bedtimes were reported among more frequent nappers and those who reported later naps (after 3:00 PM) (5). Other studies reported no significant differences in nightly sleep patterns among napping and non-napping college students (3). The cross-sectional nature of these studies makes it is difficult to determine whether aspects of napping may worsen nocturnal sleep patterns, or if poor nocturnal sleep leads to more frequent, long, and/or ill-timed naps. Further, few studies have used longitudinal designs (e.g., daily diary) that allow for examination of day-to-day relations between aspects of napping and nighttime sleep patterns.
To date, studies that have examined napping in relation to nocturnal sleep using daily actigraphy or daily diary methods, have typically focused on adolescents, middle-aged adults, and elderly adults, and have not examined the relations between the timing of naps and nighttime sleep (15-17). A study following adolescent’s nightly and daytime sleep using both actigraphy and daily diary found that shorter sleep duration was associated with longer nap durations the following day and napping was associated with shorter sleep duration that night (15). Similar results were found among adults when assessed over a 10-day period where shorter sleep duration at night was associated with taking a nap the next day, and the occurrence of a nap was associated with decreased sleep efficiency that same night (17). Another study of older adults also found that taking a longer nap during the day was associated with shorter nighttime sleep duration, but nocturnal sleep duration was not associated with next day nap length (16). Among Taiwanese college students, one daily diary study observed weekly patterns in sleep and found that those who reported napping longer than one hour also reported poorer sleep quality and more nighttime awakenings on weekdays when compared to the rest of the sample (18). However, this did not focus on day-to-day associations between these variables. Although these studies demonstrate associations between daytime nap duration and nighttime sleep, none of these prior studies examine either college students or the timing of naps in relation to sleep timing such as wake time and bedtime.
As stated, college students continue to experience bioregulatory delays in sleep timing and have more flexibility in their schedules as compared to high school or working adults; therefore, there is a greater propensity to nap and more flexibility or opportunities for napping (e.g., in between classes). Further, the literature suggests that college students demonstrate poor and irregular sleep patterns which have detrimental impacts on various aspects of functioning (19-21). Research is needed to investigate factors (e.g., napping) that could impact nightly sleep patterns. Therefore, the current study aims to: (1) characterize napping in this college sample (2) examine daily relations between aspects of napping (i.e., occurrence, timing, and duration) and nighttime sleep duration and sleep timing (i.e., bedtime, wake time) in college students. First the present study hypothesized that the occurrence of a nap, increased nap duration, and later naps would be associated with shorter nocturnal sleep duration and later bedtimes and wake times. Second, it was hypothesized that shorter sleep duration, later bedtime, and earlier wake time would be associated with greater likelihood of taking a nap that is longer and later in the day. There were no specific hypotheses regarding the characterization of napping in college students as this aim was exploratory in nature.
Method
Participants
A large sample of undergraduate college students (N = 708) from a mid-sized urban university located in the Midwest were recruited for this study. Participants were excluded from analyses if they completed less than 50% of the study protocol, as has been done in prior daily diary research (22, 23). 92.4% of the overall sample completed at least 4 days of daily diary, resulting in a final analytic sample of 654 participants (54 participants excluded). The final sample was not significantly different in age, year in school, gender, race (dichotomized), ethnicity, or residential status, compared to the excluded participants. The excluded sample reported significantly shorter average sleep duration (357.52 compared to 420.95; F(1,699)=33.20, p<.001) and significantly lower average number of naps (0.43 compared to 1.33; F(1,727)=31.52, p<.001). However, no significant differences were reported in wake times, bedtimes, nap start times, or nap duration. In the final sample, 58.4% had 7 days of data, 21.3% had 6 days, 10.9% had 5 days, and 9.5% had 4 days. Demographic information is presented in Table 1.
Table 1.
Demographics
| n | % | |
|---|---|---|
| Year in school | ||
| Freshman | 392 | 60.4 |
| Sophomore | 188 | 29.0 |
| Junior | 47 | 7.2 |
| Senior | 22 | 3.4 |
| Gender | ||
| Female | 532 | 81.5 |
| Male | 119 | 18.2 |
| Other | 2 | 0.3 |
| Race | ||
| White/Caucasian | 378 | 60.5 |
| Asian | 108 | 17.3 |
| Other | 60 | 9.6 |
| Black or African American | 36 | 5.8 |
| Multiracial | 16 | 2.6 |
| Middle Eastern or North African | 20 | 3.2 |
| Native Hawaiian or Other Pacific Islander | 4 | 0.6 |
| American Indian or Alaska Native | 3 | 0.5 |
| Ethnicity | ||
| Hispanic | 106 | 16.8 |
| Non-Hispanic | 525 | 83.2 |
| Residential status | ||
| Residential hall on campus | 451 | 69.3 |
| With parents/legal guardian | 123 | 18.9 |
| Off campus apartment | 72 | 11.1 |
| Other | 5 | 0.8 |
| Annual household income | ||
| Above $100,000 | 225 | 34.7 |
| $75,000-$100,000 | 142 | 21.9 |
| $50,000-$75,000 | 108 | 16.7 |
| $25,000-$50,000 | 92 | 14.2 |
| Less than $25,000 | 81 | 12.5 |
Procedure
Participants enrolled in the current study through their introductory psychology course and signed up through an online portal to receive “credits” as part of their course grade. Recruitment occurred over two school years (Fall 2017 through Spring 2019). Participants were given prorated credits depending on study completion and entered into a $50 raffle if they completed all seven days of the daily dairy. Recruitment weeks were scheduled to capture “typical” weeks and the researchers avoided sampling during academic breaks (e.g., spring break, national holidays) or academically rigorous periods (i.e., scheduled finals week). Participants who signed up for the current study were provided a link to complete informed consent, followed by an initial, larger survey which also included daily diary questions. If participants completed this initial survey, they were automatically enrolled in the daily diary portion of the study. The initial survey included measures related to demographics and psychological functioning. The daily diary asked participants to provide information about various health behaviors, such as mood, sleeping, eating, and physical activity. The current study investigated sleep patterns, including the timing and duration of nighttime and daytime sleep. The daily diary survey was e-mailed to participants at 8 PM each evening and a reminder email was sent at 11 PM. The response window closed at 12 PM the following day. Daily dairy questions were sent for a total of seven days. Informed consent and all study procedures were approved the university’s Institutional Review Board.
Measures
Demographics.
Participants reported on their background characteristics, including birthday, year in school, gender (male, female, or other), race (white, Black or African American, American Indian or Alaska Native, Asian or Indian, Native Hawaiian or Other Pacific Islander, Other), ethnicity (“Are you of Hispanic, Latino, or Spanish origin?”), and residential status (Residential hall on campus, off campus apartment, with parent(s)/legal guardian in the Chicago area, Other).
Nighttime sleep.
Participants reported on sleep patterns each night they received the daily diary. First, participants were asked if they fell asleep the previous night (vs. pulling an “all nighter”). If they responded yes, they were asked additional questions on sleep for the previous night including bedtime, wake time, and sleep duration. Each day of daily diary provided a prompt for what day they should be reporting on. Bedtime was coded as the time participants reported that they attempted to fall asleep and wake time was the time they reported that they woke up that morning. To explore for accidental AM/PM reporting errors that might have occurred, the current study investigated bedtimes that fell before 8 PM and after 5 AM, wake times that fell before 5 AM and after 1 PM, and nap start times that fell before 9 AM or after 9 PM. Sleep times that fell outside of these periods were considered unexpected and cross-referenced and investigated within the context of the participant’s other sleep data. For example, if participants reported an unexpected nap start time of 2:00 AM, but then also reported a 9:00 AM wake time and 12:00 AM bedtime, then the 2:00 AM was changed to 2:00 PM. If the data were ambiguous and a nap could have theoretically occurred, AM/PM was not changed. Changes were reviewed by the authors for consensus (LN and ER).Sleep duration was participant’s self-reported sleep duration (24).
Napping.
Participants were also asked to report the presence of daytime sleep each day. Specifically, participants were asked to report if they napped that day, including time they started their nap and duration of that nap.
Statistical Analyses
SPSS version 26 was used to run all analyses. Correlations between key study variables were examined. One-way ANOVAS were conducted to examine group differences in key study variables. Intra-Class Correlations (ICC) were calculated to determine whether it was appropriate to use multi-level modeling. Due to the nested nature of the data (diary entries nested within people), multi-level modeling (mixed logistic models were used when nap occurrence was the dependent variable) was performed to test the daily influences of napping variables (occurrence, timing, and duration) on nocturnal sleep variables (bedtime, duration, and wake time). All napping variables were tested separately in relation to each nocturnal sleep variable, in both directions (i.e., previous night sleep in relation to next-day napping, and napping in relation to sleep that night) resulting in 18 main effect models. Within-person daily measures (e.g., nocturnal sleep and napping variables) were entered at level 1 of the models while between-person covariates (e.g., race, ethnicity, SES) were entered at level 2. For analyses examining nap duration, 0s were imputed for those who did not take a nap on that day. However, for nap timing variables, nap start time was left as missing for those individuals who did not take naps. Lagged sleep duration and bedtime variables were created to test how nap variables were associated with same night sleep. In addition, for models examining how nap variables were associated with following day wake time, a wake time was shifted forward one day for those analyses. Socioeconomic status, race (dichotomized to be white versus non-white students), ethnicity, and residential status were included as covariates in all of the models. Given that sleep may differ across weekdays and weekends, weekday versus weekend was also explored as a covariate, using a dummy code (0=weekday, 1=weekend day) in all models. For analyses where bedtime or sleep duration were the outcome variables, Friday and Saturday were counted as weekend days. For analyses where nap or wake variables were the outcome variables, Saturday and Sunday were counted as weekend days. All results remained the same when controlling for weekday versus weekend in the full sample. Results below are presented without weekday versus weekend covariate for parsimony. There were no significant differences in sleep variables based on gender or year in school therefore they were not included as covariates. Slopes remained fixed in all MLM models.
Results
Preliminary Analyses
Regarding nap frequency, a majority of the sample (64.2%) took at least one nap at some point across a four to seven day period, with 25.1% taking one nap, 21.1% taking two naps, and 18% taking 3 or more naps per week. The average number of naps across the week was 1.33 (SD=1.37). As depicted in Figure 1, college students took more naps in the late afternoons followed by the afternoon with the average nap time occurring at 2:47 PM (SD=144.00 minutes). Some students reported napping in the mornings and evenings with morning naps occurring more frequently at the beginning of the week (Monday through Thursday) and evening naps occurring more frequently at the end of the week (Friday and Saturday). Further, students napped an average of 81.6 minutes (SD=54.21 minutes), however there was large range in nap duration (5 minutes to 315 minutes) and longer naps tended to occur on the weekends (97.57 min) compared to weekdays (78.34 min). Regarding nocturnal sleep, the average sleep duration in the sample was 471.56 minutes (7 hours and 51.56 minutes; SD=96.45 minutes) and the average bedtime was 12:52AM (SD=65.00 minutes). Average wake time was 8:22AM (SD=65.00 minutes).
Figure 1. Timing of naps broken down by time of day.
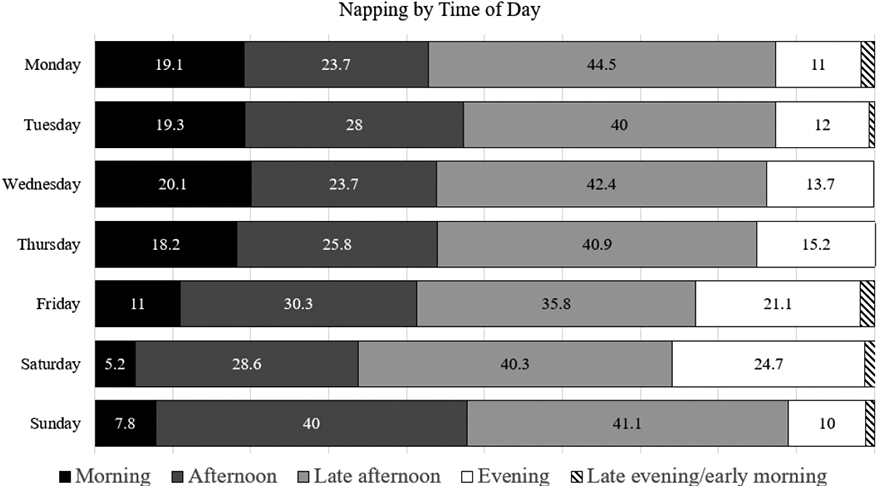
Note: The numbers presented within the bar graph represent percentages. Morning naps occurred between 5 AM – 11:59 AM, afternoon naps occurred between 12 PM – 2:59 PM, late afternoon naps occurred between 3 PM – 5:59 PM, evening naps occurred between 6 PM – 11:59 PM, and late evening/early morning naps occurred between 12:00 AM – 4:59 AM. These categories were based on Ye et al. (2015), however this study included a “late evening/early morning” category.
Correlations between key study variables are displayed in Table 2. Differences of key study variables by demographics were examined. One-way ANOVAs revealed that minority students (Black or African American, American Indian or Alaska Native, Asian or Indian, Native Hawaiian or Other Pacific Islander) reported significantly shorter sleep duration (F(1,623) =14.68, p<.001) and significantly later bedtimes (F(1,622)=6.36, p<.05) than White students. Independent samples T-tests demonstrated that Hispanic students reported significantly earlier bedtimes compared to non-Hispanic students (t(628)=−1.44, p<.05). Students who lived in a residential hall on campus reported significantly later wake-up times compared to those living in an off-campus apartment and those living with the parents/guardian (F(3,643)=19.53, p<.001). In addition, students living in a residential hall on campus reported significantly later bedtimes than those living with their parents (F(3,645)=6.94, p<.001). As previously indicated, there were no significant differences in sleep variables based on gender or year in school.
Table 2.
Correlations between key study variables and demographic variables
| Wa ke Time^ |
Bedtime^ | Sleep duration^ |
Nap frequencya |
Nap start time^ |
Nap length^ |
Genderb | Racec | Ethnicityd | Year in school |
Household incomee |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wake time | 1 | .59** | .20** | .01 | .05 | .04 | −.01 | .03 | .08* | −.08* | .15** |
| Bedtime | 1 | −.19** | .21** | .07 | .06 | .01 | −.10* | .06 | −.02 | .05 | |
| Sleep duration | 1 | −.24** | −.08 | −.06 | .06 | .10** | −.01 | −.03 | .12** | ||
| Nap frequency | 1 | .07 | .04 | −.03 | .01 | −.07 | −.08 | −.04 | |||
| Nap start time | 1 | −.12* | .02 | −.04 | .00 | .00 | .05 | ||||
| Nap length | 1 | .02 | −.07 | .05 | −.04 | −.02 | |||||
| Gender | 1 | −.03 | .01 | .12* * |
.06 | ||||||
| Race | 1 | .01 | −.03 | .11** | |||||||
| Ethnicity | 1 | .02 | .13** | ||||||||
| Year in school | 1 | −.03 | |||||||||
| Household income | 1 |
This variable includes the total number of naps taken across a week
Gender was dichotomized (0 =Female; 1=Male)
Race was dichotomized (0=Minority students ; 1=White)
Ethnicity (0=Non-Hispanic; 1=Hispanic)
Household income was assessed using five categories (1=Less than $25K; 5=Over $100K)
These variables are averaged across the entire week
Daily Relations Between Napping and Nocturnal Sleep
Intraclass correlation coefficients (ICCs) indicated the 79% of the variance in nocturnal sleep duration, 54% of the variance in nocturnal bedtime, and 66% of the variance in wake time existed within participants. In addition, 89% of the variance in nap occurrence, 89% of the variance in nap duration, and 84% of the variance in nap start time existed within participants.
Previous Night Sleep and Next-Day Napping
Associations between previous night sleep and next-day napping variables were tested (Table 3). Multilevel logistic regressions were run to examine how previous night sleep and same morning wake time were associated with the odds of a nap occurrence the following day. Analyses revealed that going to bed later significantly increased the odds of taking a nap the following day by 13% (B=0.13, p=<.001). Shorter sleep duration significantly increased the odds of taking a nap the following day by 0.3% (B=−0.00, p<.001). Earlier wake up time also significantly increased the odds of taking a nap that day by 18% (B=−0.20, p<.001).
Table 3.
HLM analyses demonstrating relations between previous night nocturnal sleep variables and next day nap variables
| Nap start time | Nap duration | Nap occurrence | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor | b | SEa | t | b | SEa | t | OR | 95% CI | B |
| Bedtime | 0.19 | 0.07 | 2.54* | 2.36 | 0.57 | 4.16*** | 1.13 | 1.07-1.20 | 0.13*** |
| “Other” living situationb | 0.46 | 1.09 | 0.42 | 6.57 | 11.09 | 0.59 | 1.69 | 0.61-4.69 | 0.53 |
| Living with parentsb | 0.81 | 0.35 | 2.30* | −0.59 | 2.73 | −0.22 | 0.88 | 0.64-1.20 | −0.13 |
| Living in off-campus apartmentb | 0.10 | 0.42 | 0.23 | −0.32 | 3.22 | −0.10 | 0.95 | 0.65-1.37 | −0.06 |
| Racec | −0.03 | 0.26 | −0.13 | 0.20 | 2.09 | 0.10 | 0.92 | 0.74-1.16 | −0.08 |
| Ethnicityd | 0.18 | 0.33 | 0.53 | 2.63 | 2.81 | 0.94 | 1.43 | 1.06-1.94 | 0.36* |
| Income | 0.02 | 0.09 | 0.20 | −1.36 | 0.74 | −1.83 | 0.95 | 0.88-1.03 | −0.05 |
| Wake time† | 0.42 | 0.07 | 5.62*** | −3.44 | 0.55 | −6.30*** | 0.82 | 0.77-0.88 | −0.20*** |
| “Other” living situationb | 0.56 | 1.08 | 0.52 | 6.74 | 11.52 | 0.59 | 1.64 | 0.49-5.44 | 0.49 |
| Living with parentsb | 1.05 | 0.35 | 2.97** | −4.60 | 2.85 | −1.61 | 0.69 | 0.49-0.97 | −0.37* |
| Living in off-campus apartmentb | 0.11 | 0.42 | 0.27 | −2.59 | 3.35 | −0.77 | 0.84 | 0.57-1.24 | −0.17 |
| Racec | 0.06 | 0.26 | 0.25 | 1.31 | 2.17 | 0.61 | 0.97 | 0.77-1.23 | −0.03 |
| Ethnicityd | 0.19 | 0.33 | 0.58 | 1.60 | 2.92 | 0.55 | 1.36 | 0.99-1.86 | 0.31 |
| Income | −0.01 | 0.09 | −0.11 | −1.10 | 0.77 | −1.41 | 0.97 | 0.89-1.05 | −0.03 |
| Sleep duration | 0.00 | 0.00 | 2.13* | −0.08 | 0.01 | −10.36*** | 0.99 | 0.99-0.99 | −0.00*** |
| “Other” living situationb | 0.51 | 1.10 | 0.46 | 5.67 | 11.59 | 0.49 | 1.69 | 0.58-4.87 | 0.52 |
| Living with parentsb | 0.74 | 0.35 | 2.12* | −2.22 | 2.83 | −0.79 | 0.80 | 0.58-1.11 | −0.22 |
| Living in off-campus apartmentb | 0.01 | 0.42 | 0.03 | −2.87 | 3.35 | −0.86 | 0.88 | 0.61-1.28 | −0.13 |
| Racec | 0.11 | 0.23 | 0.44 | 0.91 | 2.17 | 0.42 | 0.94 | 0.75-1.17 | −0.07 |
| Ethnicityd | 0.09 | 0.33 | 0.26 | 2.02 | 2.93 | 0.69 | 1.39 | 1.02-1.89 | 0.33* |
| Income | 0.05 | 0.09 | 0.58 | −0.75 | 0.77 | −0.97 | 0.97 | 0.90-1.05 | −0.03 |
p<.05
p<.01
p<.001
Standard error
Reference group=Living in a residential hall
Reference group=White students
Reference group=Non-Hispanic students
This reflects the wake time that occurred that morning prior to the nap occurring
Multi-level models revealed that later bedtime was associated with later nap start time (b=0.19, p<.05) and longer nap duration (b=2.36, p<.001) the next day. Specifically, a one-hour delay in bedtime was associated with an 11.1-minute delay in taking a nap, and a 2.4-minute increase in nap duration. In addition, shorter sleep duration the night before was significantly associated with an earlier nap start time (b=0.00, p<.05) and longer nap duration (b=−0.08, p<.001) the following day. Specifically, a one hour decrease in sleep duration was associated with a 7.1-minute earlier nap start time, and an increase in nap duration of 4.8 minutes.
Earlier morning wake time was associated with earlier nap start time that day (b=0.42, p<.001). Specifically, a one-hour earlier wake time was associated with a 25.1 minute earlier nap start time. Additionally, earlier wake time was significantly associated with longer nap duration (b=−3.44, p<.001). Specifically, a one-hour earlier wake time was associated with a 3.4 minute increase in nap duration.
Napping and Same-Night Sleep
Associations between napping and same-night nocturnal sleep variables and following day wake time were examined using multi-level modeling (Table 4). Multi-level models revealed that the occurrence of a nap was significantly associated with longer sleep duration that night (b=12.07, p<.05), earlier bedtime (b=−0.12, p<.05), and earlier next-day wake time (b=−.15, p<.05). Specifically, taking a nap was associated with a 12.1-minute increase in sleep duration and 7.3-minute earlier bedtime that night, and 8.81 minutes earlier wake time the next morning. Regarding timing of naps, later nap start time was significantly associated with shorter sleep duration (b=−4.47, p<.01) and later bedtime (b=0.06, p<.001) that night. Specifically taking a nap one hour later was associated with a 4.5-minute decrease in sleep duration, and a delay in bedtime by 3.5 minutes. Nap start time was not significantly associated with next-day wake time. Regarding nap duration, longer nap duration was significantly associated with a later bedtime (b=0.00, p<.01) and later next-day wake time (b=0.00, p<.01). Specifically, a one hour increase in nap duration delayed bedtime by 4.5 minutes and a 5.6-minute delay in wake time. Nap duration was not significantly associated with sleep duration.
Table 4.
HLM analyses demonstrating relations between aspects of napping and nocturnal sleep
| Bedtime | Wake time† | Sleep duration | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor | b | SEa | t | b | SEa | t | b | SEa | t |
| Nap occurrence | −0.12 | 0.06 | −2.02* | −0.15 | 0.06 | −2.31* | 12.07 | 4.93 | 2.45* |
| “Other” living situationb | −0.01 | 0.52 | −0.03 | −0.38 | 0.47 | −0.80 | 3.57 | 27.96 | 0.13 |
| Living with parentsb | −0.54 | 0.13 | −4.22*** | −0.73 | 0.12 | −6.27*** | −1.40 | 6.88 | −0.20 |
| Living in off-Campus apartmentb | −0.41 | 0.15 | −2.74** | −0.32 | 0.14 | −2.31* | 0.31 | 8.20 | 0.04 |
| Racec | 0.29 | 0.09 | 2.97** | 0.02 | 0.09 | 0.21 | −14.35 | 5.30 | −2.71** |
| Ethnicityd | −0.13 | 0.13 | −1.00 | −0.14 | 0.12 | −1.17 | −3.95 | 7.12 | −0.55 |
| Income | 0.01 | 0.04 | 0.45 | 0.06 | 0.03 | 1.74 | 1.93 | 1.89 | 1.02 |
| Nap start time | 0.06 | 0.02 | 3.29*** | 0.02 | 0.02 | 0.89 | −4.47 | 1.43 | −3.13** |
| “Other” living situationb | −1.00 | 0.63 | −1.58 | −0.59 | 0.65 | −0.90 | 3.34 | 42.03 | 0.08 |
| Living with parentsb | −0.31 | 0.21 | −1.50 | −0.79 | 0.21 | −3.71*** | −13.83 | 13.13 | −1.05 |
| Living in off-campus apartmentb | −0.41 | 0.26 | −1.60 | −0.39 | 0.26 | −1.45 | −1.21 | 16.16 | −0.08 |
| Racec | 0.29 | 0.15 | 1.86 | −0.19 | 0.16 | −1.23 | −22.19 | 9.80 | −2.27* |
| Ethnicityd | −0.08 | 0.20 | −0.41 | −0.30 | 0.21 | −1.46 | −8.90 | 12.61 | −0.71 |
| Income | −0.01 | 0.05 | −0.13 | 0.03 | 0.06 | 0.62 | 1.36 | 3.42 | 0.40 |
| Nap duration | 0.00 | 0.00 | 2.65** | 0.00 | 0.00 | 3.13** | −0.04 | 0.04 | −1.06 |
| “Other” living situationb | −0.01 | 0.53 | −0.19 | −.038 | 0.47 | −0.79 | 2.43 | 28.13 | 0.09 |
| Living with parentsb | −0.55 | 0.13 | −4.27*** | −0.74 | 0.12 | −6.38*** | −1.36 | 6.92 | −0.20 |
| Living in off-campus apartmentb | −0.42 | 0.15 | −2.77** | −0.32 | 0.14 | −2.30* | 0.46 | 8.24 | 0.06 |
| Racec | 0.29 | 0.10 | 2.96** | 0.01 | 0.90 | 0.12 | −14.52 | 5.33 | −2.72** |
| Ethnicityd | 0.12 | 0.13 | 0.92 | −0.14 | 0.12 | −1.14 | −4.73 | 7.16 | −0.67 |
| Income | 0.02 | 0.04 | 0.49 | 0.06 | 0.32 | 1.72 | 1.95 | 1.90 | 1.02 |
p<.05
p<.01
p<.001
Standard error
Reference group=Living in a residential hall
Reference group=White students
Reference group=Non-Hispanic students
Wake time reflects the following day participants woke up
Exploratory Analyses Excluding Non-Nappers
Exploratory analyses were conducted to determine if this pattern of findings would replicate with non-nappers (those individuals who never reported taking a nap over the course of the week; n =233) excluded from the analytic sample. Two differences were noted: first, the occurrence of a nap was significantly associated with longer sleep duration in the full sample, while there was no significant association between these two variables for the nappers only sample. Second, the occurrence of a nap was significantly associated with later bedtime in the full sample, while there was no significant association between these two variables for the nappers only sample. It should be noted that when weekday versus weekend was included as a covariate, the relationship between occurrence of a nap and later bedtime remained significant.
Discussion
The purpose of this study was to use daily diary data to characterize napping patterns in college students and examine the daily associations between daytime napping and nocturnal sleep. Little is known about the relations between napping patterns and nighttime sleep in college students, particularly how the timing of these behaviors might be related. The current study builds upon previous research by investigating the daily relations between nighttime sleep and napping among college students specifically, and exploring the importance of the timing of daytime and nighttime sleep.
A key takeaway from this study is that there are bidirectional associations between napping and nocturnal sleep. Analyses examining daily associations between napping and nocturnal sleep, overall, fit with previous findings demonstrating that shorter sleep durations are associated with longer nap durations the following day (15). However, the occurrence of a nap was associated with longer sleep durations that night diverging from prior research in adolescent and older adults (15, 17). Taking these two key findings into consideration together, it might be that college students nap after a poor night of sleep, and aim to achieve longer sleep duration that night. However, it is also important to keep in mind that longer sleep duration does not necessarily reflect restorative or high-quality sleep. Future studies should also examine associations between napping and sleep quality. In addition, it is important to note that when exploratory analyses excluding non-nappers from the sample were conducted, this finding between occurrence of a nap and longer sleep duration was not replicated. One explanation for this might be that there are inherent differences in sleep patterns between those students who nap compared to those who do not nap. Future research should focus on the best way to operationalize whether an individual is a “napper” and examining group differences in nocturnal sleep outcomes between nappers and non-nappers. One possibility for operationalization might be asking students specifically whether they consider themselves a “napper,” or defining a specific number of naps per week that a “napper” takes. Prior research has examined differences between “habitual” vs “non-habitual” nappers and found that in some cases, a nap improved cognitive performance for habitual nappers but not non-habitual nappers (25). However, more research is needed to understand how being a napper might influence nocturnal sleep in college.
Importantly, the present study adds to the literature by investigating sleep and nap timing. In fact, later nap start times were associated with later bedtimes and shorter sleep durations. In addition, the present study found that taking longer naps was associated with later wake times the following day and that earlier wake times were associated with earlier and longer naps. Therefore nap duration and nap timing both have important relations to nighttime sleep and wake timing. These findings also suggest that there may be a cyclical pattern, where poor sleep patterns (e.g., short and later nighttime sleep) may contribute to worsened napping behaviors (e.g., long and late naps) thereby contributing to poor nightly sleep (shorter duration, later bedtime). However, it is important to consider the clinical significance of these findings. For most variables, nap behaviors during the day contributed to no more than 10 minutes of difference in nocturnal sleep outcomes. Nocturnal sleep was associated with larger shifts in nap start time and occurrence, though still not necessarily clinically meaningful. It could be that college students in particular have poor nighttime sleep due to their academic and other commitments, and feel they need to take naps to decrease daytime sleepiness, not that naps themselves contribute to poor nightly sleep. Naps may in fact be a useful strategy to combat daytime sleepiness for some students. Future research should investigate levels of daytime sleepiness in relation to napping and nocturnal sleep, as well as college students’ motivation for napping to better understand this cycle. In addition, it might be that relations between napping and nocturnal sleep are different based on factors like differing motivations for napping or frequency of napping. For example, students with mood disorders may have different reasons for napping than those who did not have mood disorders. In fact, research has shown that emotional reasons for napping were associated with poor well-being, while other reasons for napping were not (2). This may also translate to differing relations between napping and nocturnal sleep. In addition, students who nap frequently (e.g., “habitual nappers”) may experience differential relations between these variables compared to students who do not regularly nap. Future research should examine these factors to determine if napping is more or less beneficial for particular groups.
Characterizing napping and nocturnal sleep in our sample revealed how contextual influences may contribute to adverse nightly sleep and napping patterns among college students. Preliminary analyses in the present study showed that students who lived in residential halls had significantly later wake up times than those living in an off-campus apartment or with caregivers, therefore this was used as a covariate. This could be due to the need to wake up to commute to campus (26). Other contextual factors that may influence sleep patterns including employment, participation in athletics, eating, physical activity, and mood (21) should also be explored. Future studies investigating sleep patterns should capture and investigate information related to employment status, involvement in athletics or extracurricular activities, other health behaviors and mental health to see if certain groups may be particularly vulnerable to compensatory or irregular sleep patterns.
Individual factors, such a racial minority status, are also important considerations for studies that investigate sleep patterns. In the current study, differences in sleep were reported across racial and ethnic backgrounds, such that minority students reported shorter sleep durations and later bedtimes when compared to White students, and students of Hispanic/Latinx origin reported earlier wake times as compared to non-Hispanic/Latinx individuals. In addition, minority status remained significant when included as a covariate in a majority of multi-level models, indicating it is an important factor when considering nighttime sleep duration and timing. Studies should continue to identify groups of students who may be at heightened risk of poor sleep to inform tailored health promotion efforts at universities, especially since poor sleep patterns have been associated with worsened mental health outcomes, weight gain, and lower academic performance (7, 24, 27).
Additionally, more work is needed to consider which aspects of napping (i.e., occurrence, timing, duration) may be adjusted in order to optimize naps to mitigate the effects of short or restricted sleep. For instance, experimental studies by a research group in Singapore found that cognition is benefited when adolescents are given an opportunity to nap in the context of restricted sleep (< 6.5 hours), whereas there were no cognitive benefits of napping among adolescents who were given ample time to sleep (>8 hours) over a 24-hour period (28, 29). Interestingly, the researchers highlight that these trends are not present among adults and speak to the need to investigate napping from a developmental perspective in adolescents. Further, future studies should capture longer assessments of sleep patterns to compare students who are “habitual” vs. “non-habitual” nappers. This distinction has been important in prior work among children, where toddlers who are habitual nappers experience better cognitive performance after a nap, but non-habitual nappers experienced worse performances and poorer nightly sleep (30-32). A study of adolescents suggested that napping benefited long-term memory in both non-habitual and habitual nappers, but performance declined among habitual nappers if they were not allowed to nap (25). Overall, future studies should focus on specific factors that might help to determine for whom napping is beneficial.
One major limitation of the study design is the use of self-report sleep data that was collected over a short time period of one week, and self-report and objective estimates of sleep are only moderately correlated (33). Future studies should explore these relations capitalizing on actigraphy methods (15). However, it can be challenging to interpret napping in actigraphy data (34). Studies using both actigraphy and sleep diary have found discrepancies in the identification of naps, with actigraphy identifying more naps that could be periods of inactivity or perhaps spontaneous unplanned naps (see discussion within (15)). Relatedly, participants who completed less than 4 days of survey data were excluded and there were significant differences between the excluded sample and current sample on average sleep duration and average number of naps (reported above), which may have contributed to a biased sample. For example, it is possible that students in the excluded group had higher levels of stress or responsibilities, which have been associated with shorter sleep duration (35), and may also coincide with challenges in consistently completing a daily diary. Another limitation of this study was the timing of the distribution of the survey. Participants were sent the survey link at 8:00PM and had until 12PM the following day to complete the survey for that day (e.g., had until 12PM on Tuesday to complete Monday’s survey). This may have introduced recall bias as participants may not have remembered exact sleep and napping times or duration. Another limitation of this study was the lack of data on other dimensions of sleep health (36), such as daytime sleepiness, sleep efficiency, sleep quality, or sleep latency. Napping may influence sleep quality which may contribute to daytime sleepiness and therefore increased desire to engage in a nap (18). Further, knowing why participants napped could differentiate those whom napping might be beneficial rather than detrimental. In addition, capturing daytime sleepiness prior to and following a nap would add to our understanding of the benefits of napping in this population. Finally, it is important to consider the possibility for Type I Error, given the total number of models run in the present study.
In conclusion, the results from this study demonstrate that there is a potential cyclical relation between daytime napping and nocturnal sleep, particularly in terms of the timing of naps, sleep, and wake in college students. Napping is common in college students, and it is associated with poor nocturnal sleep outcomes, especially longer and later naps taken later in the day. In addition, short and late nocturnal sleep may contribute to longer and later naps. Many college students veer from conventional sleep schedules in order to balance their many commitments, however, these sleep schedules may create a cycle in which students stay up later because they have napped earlier in the day, contributing to shorter sleep duration. These findings suggest that napping is an important area of future investigation as it may have far-reaching implications for college students’ well-being.
Supplementary Material
Acknowledgements:
This material is based upon work supported by the National Science Foundation Graduate Research Fellowship Program under Grant No. 1842190. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the National Science Foundation. Dr. Mead is supported by funding from the National Heart, Lung, and Blood Institute of the National Institutes of Health T32HL007909.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ye L, Hutton Johnson S, Keane K, Manasia M, Gregas M. Napping in college students and its relationship with nighttime sleep. Journal of American College Health. 2015;63(2):88–97. [DOI] [PubMed] [Google Scholar]
- 2.Duggan KA, McDevitt EA, Whitehurst LN, Mednick SC. To nap, perchance to DREAM: a factor analysis of college students’ self-reported reasons for napping. Behavioral sleep medicine. 2018;16(2):135–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lovato N, Lack L, Wright H. The napping behaviour of Australian university students. PloS one. 2014;9(11):e113666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lo JC, Lee SM, Teo LM, Lim J, Gooley JJ, Chee MW. Neurobehavioral impact of successive cycles of sleep restriction with and without naps in adolescents. Sleep. 2017;40(2):zsw042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fukuda K, Ishihara K. Routine evening naps and night-time sleep patterns in junior high and high school students. Psychiatry and Clinical Neurosciences. 2002;56(3):229–30. [DOI] [PubMed] [Google Scholar]
- 6.Park H, Chiang JJ, Irwin MR, Bower JE, McCreath H, Fuligni AJ. Developmental trends in sleep during adolescents' transition to young adulthood. Sleep medicine. 2019;60:202–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Becker SP, Jarrett MA, Luebbe AM, Garner AA, Burns GL, Kofler MJ. Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep health. 2018;4(2):174–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep health. 2015;1(1):40–3. [DOI] [PubMed] [Google Scholar]
- 9.Orzech KM, Salafsky DB, Hamilton LA. The state of sleep among college students at a large public university. Journal of American College Health. 2011;59(7):612–9. [DOI] [PubMed] [Google Scholar]
- 10.Borbély AA. A two process model of sleep regulation. Hum neurobiol. 1982;1(3):195–204. [PubMed] [Google Scholar]
- 11.Carskadon MA. Sleep in adolescents: the perfect storm. Pediatric Clinics. 2011;58(3):637–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crowley SJ, Wolfson AR, Tarokh L, Carskadon MA. An update on adolescent sleep: New evidence informing the perfect storm model. Journal of Adolescence. 2018;67:55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Randler C, Vollmer C, Kalb N, Itzek-Greulich H. Breakpoints of time in bed, midpoint of sleep, and social jetlag from infancy to early adulthood. Sleep Medicine. 2019;57:80–6. [DOI] [PubMed] [Google Scholar]
- 14.Vela-Bueno A, Fernandez-Mendoza J, Olavarrieta-Bernardino S. Sleep patterns in the transition from adolescence to young adulthood. Sleep Medicine Clinics. 2009;4(1):77–85. [Google Scholar]
- 15.Jakubowski KP, Hall MH, Lee L, Matthews KA. Temporal relationships between napping and nocturnal sleep in healthy adolescents. Behavioral sleep medicine. 2017;15(4):257–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldman SE, Hall M, Boudreau R, et al. Association between nighttime sleep and napping in older adults. Sleep. 2008;31(5):733–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Owens JF, Buysse DJ, Hall M, et al. Napping, nighttime sleep, and cardiovascular risk factors in mid-life adults. Journal of Clinical Sleep Medicine. 2010;6(4):330–5. [PMC free article] [PubMed] [Google Scholar]
- 18.Tsai L-L, Li S-P. Sleep patterns in college students: Gender and grade differences. Journal of psychosomatic research. 2004;56(2):231–7. [DOI] [PubMed] [Google Scholar]
- 19.Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. Journal of adolescent health. 2010;46(2):124–32. [DOI] [PubMed] [Google Scholar]
- 20.Becker SP, Dvorsky MR, Holdaway AS, Luebbe AM. Sleep problems and suicidal behaviors in college students. Journal of psychiatric research. 2018;99:122–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nicholson L, Bohnert AM, Crowley SJ. A developmental perspective on sleep consistency: Preschool age through emerging adulthood. Behavioral Sleep Medicine. 2022:1–20. [DOI] [PubMed] [Google Scholar]
- 22.Moore CC, Hubbard JA, Bookhout MK, Mlawer F. Relations between reactive and proactive aggression and daily emotions in adolescents. Journal of abnormal child psychology. 2019;47(9):1495–507. [DOI] [PubMed] [Google Scholar]
- 23.Dalton ED. Exercise-related coping beliefs predict physical activity levels in response to naturally occurring stress: A daily diary study of college students. Journal of American College Health. 2020:1–9. [DOI] [PubMed] [Google Scholar]
- 24.Roane BM, Seifer R, Sharkey KM, et al. What role does sleep play in weight gain in the first semester of university? Behavioral sleep medicine. 2015;13(6):491–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leong RL, Yu N, Ong JL, et al. Memory performance following napping in habitual and non-habitual nappers. sleep. 2021;44(6):zsaa277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.BAKOTICA M, RADOŠEVICA-VIDAČEK B, KOŠCAEC A. Residential status and sleep regularity of university students in Croatia: P169. Journal of Sleep Research. 2006;15. [Google Scholar]
- 27.Wald A, Muennig PA, O'Connell KA, Garber CE. Associations between healthy lifestyle behaviors and academic performance in US undergraduates: a secondary analysis of the American College Health Association's National College Health Assessment II. American Journal of Health Promotion. 2014;28(5):298–305. [DOI] [PubMed] [Google Scholar]
- 28.Lo JC, Twan DC, Karamchedu S, et al. Differential effects of split and continuous sleep on neurobehavioral function and glucose tolerance in sleep-restricted adolescents. Sleep. 2019;42(5):zsz037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lo JC, Leong RL, Ng AS, et al. Cognitive effects of split and continuous sleep schedules in adolescents differ according to total sleep opportunity. Sleep. 2020;43(12):zsaa129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lam JC, Mahone EM, Mason TB, Scharf SM. The effects of napping on cognitive function in preschoolers. Journal of developmental and behavioral pediatrics: JDBP. 2011;32(2):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kurdziel L, Duclos K, Spencer RM. Sleep spindles in midday naps enhance learning in preschool children. Proceedings of the National Academy of Sciences. 2013;110(43):17267–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Werchan DM, Gómez RL. Wakefulness (not sleep) promotes generalization of word learning in 2.5-year-old children. Child development. 2014;85(2):429–36. [DOI] [PubMed] [Google Scholar]
- 33.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008:838–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Galland B, Meredith-Jones K, Terrill P, Taylor R. Challenges and emerging technologies within the field of pediatric actigraphy. Frontiers in psychiatry. 2014;5:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yap Y, Slavish DC, Taylor DJ, Bei B, Wiley JF. Bi-directional relations between stress and self-reported and actigraphy-assessed sleep: a daily intensive longitudinal study. Sleep. 2020;43(3):zsz250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


