Abstract
Objectives
To examine how ecological inequalities in COVID-19 mortality rates evolved in England, and whether the first national lockdown impacted them. This analysis aimed to provide evidence for important lessons to inform public health planning to reduce inequalities in any future pandemics.
Design
Longitudinal ecological study.
Setting
307 lower-tier local authorities in England.
Primary outcome measure
Age-standardised COVID-19 mortality rates by local authority, regressed on Index of Multiple Deprivation (IMD) and relevant epidemic dynamics.
Results
Local authorities that started recording COVID-19 deaths earlier were more deprived, and more deprived authorities saw faster increases in their death rates. By 6 April 2020 (week 15, the earliest time that the 23 March lockdown could have begun affecting death rates) the cumulative death rate in local authorities in the two most deprived deciles of IMD was 54% higher than the rate in the two least deprived deciles. By 4 July 2020 (week 27), this gap had narrowed to 29%. Thus, inequalities in mortality rates by decile of deprivation persisted throughout the first wave, but reduced during the lockdown.
Conclusions
This study found significant differences in the dynamics of COVID-19 mortality at the local authority level, resulting in inequalities in cumulative mortality rates during the first wave of the pandemic. The first lockdown in England was fairly strict—and the study found that it particularly benefited those living in more deprived local authorities. Care should be taken to implement lockdowns early enough, in the right places—and at a sufficiently strict level—to maximally benefit all communities, and reduce inequalities.
Keywords: COVID-19, Epidemiology, Public health
Strengths and limitations of this study.
This study examines the evolution of inequalities in COVID-19 in the first wave of the pandemic in England and the impact of the national lock down.
National level official (Office for National Statistics) data used, covering nearly all local authorities in England and including all deaths that made any mention of COVID-19 on death certificates, requiring sensitive data acquisition.
Age-standardised deaths rates at lower geographies are not available at the time of writing but could lend extra nuance to these findings.
Ecological study not using individual-level data, so unable to examine the individual-level risks for COVID-19 mortality.
Introduction
Since the early days of the SARS-CoV-2 pandemic in 2020, inequalities in case, hospitalisation and death rates have been noted internationally.1–8 The most deprived populations and areas in the USA, Europe and other high-income countries (in terms of a range of deprivation measures) have suffered up to twice the mortality rates of the least deprived sections of society.2 7 9–12 In addition, inequalities in disease burden have been noted across levels of income, education, employment, sex, age and especially between different ethnic groups, where people of black and minority ethnic backgrounds have suffered many more cases (and deaths) than their white counterparts.13 However, the evolution of ecological inequalities in the pandemic over time in England—and the impact of national lock downs on them—has not previously been examined. This study addresses this evidence gap by providing the first analysis of inequalities in the evolution of the pandemic in different English local authorities and the impact of the first national lock down on them.
Most countries employed national lockdowns of varying duration and severity to mitigate disease spread, alongside social distancing and hygiene-related advice. The factors used to determine when a lockdown should begin or cease were rarely transparent, but most appeared to reduce infection rates to some degree after a lag phase, and saw a rebound of varying size following their release.14–16 The first confirmed cases of COVID-19 were recorded in England in York in January 2020 and the first death in England was on 5 March. From 23 April 2020 to 4 July 2020, a national lockdown was implemented across England. In keeping with many other European countries, this was characterised by a 12-week ‘stay at home’ order (SI 350)—whereby people could only go outside for certain ‘very limited purposes’—to buy food, to exercise once a day, for medical reasons or to care for a vulnerable person, or to go to work if they absolutely could not work from home.17 Face-to-face education was suspended and many workplaces closed down—and staff furloughed—particularly in the hospitality, travel and retail sectors. As nationally cases, hospitalisation and death rates started to fall the lockdown was gradually released over a period of several months—culminating in the so-called ‘Super Saturday’ on 4 July 2020 when pubs, restaurants, hairdressers, and cinemas reopened—although with strict social distancing rules.18
It has been noted that when national epidemic dynamics are used to examine population health, they can mask important subnational variation in disease spread, thus mitigation strategies that rely solely on the national data to inform implementation timings could inadvertently worsen health inequalities across geographical areas.14 16 Previous descriptive studies and reports of inequalities in COVID-19 mortality have only focused on cumulative measures over set timespans, without documenting the disparities in evolution of mortality rates,5 19 20 have been restricted to higher geographies21 or have not focused on the effects of lockdowns.7 22 An understanding of how the evolution of the pandemic differed by area and the impact of national mitigation strategies on ecological inequalities in COVID-19 mortality could help inform future policies targeted at minimising viral spread while preventing the widening (or even actively decreasing) health inequalities.
This paper uses COVID-19 mortality data from the first wave of the pandemic in England to provide the first examination of ecological inequalities in the evolution of the pandemic in this country. It sets out the first analysis of when death rates rose, peaked and fell in local authorities of differing levels of deprivation, and it describes the effects—and the timing of—the first national lockdown on these inequalities.
Methods
Weekly counts of COVID-19 deaths (based on any mention of Coronavirus on the death certificate) for 312 lower-tier local authorities (excluding county councils) in England were obtained from the Office for National Statistics (ONS) covering the period from 1 January 2020 to 4 July 2020, by date of registration (local authorities are local government organisations covering variable population sizes from just over 2000 to more than 1.5 million residents).23 Weekly COVID-19 death counts at the local authority level were not available per age group, thus age-standardised rates were calculated via monthly age-standardised rates. Monthly age-standardised COVID-19 mortality rates per local authority for the period March 2020 to July 2020 were similarly obtained from ONS.24 The monthly rate was divided between the constituent weeks based on the share of monthly deaths in each week. Where all age-standardised rates for a local authority were suppressed by ONS due to disclosure controls, the authority was excluded from analyses (n=4). The level of deprivation of each local authority was determined by the rank of average rank of the Index of Multiple Deprivation (IMD, a relative measure of deprivation across multiple dimensions at small local area level25), which was converted into deciles (decile 1 contained the most deprived 10% of local authorities) from downloaded data.26 In addition, data from the Isles of Scilly and the City of London were excluded due to well-known mortality data quality issues and low population counts.
A number of metrics were calculated for each local authority; the ‘starting week’ was the first week where one or more COVID-19 deaths were registered, the ‘peak’ was the highest weekly age-standardised mortality rate per area using a 3-week rolling mean of weekly death rates, and the ‘total mortality rate’ was the cumulative sum of age-standardised weekly mortality rates over the whole study period. The speed of increase was defined as the change in mortality rate between 25% of the peak death rate and the peak rate itself, divided by the number of weeks between them, and similarly the speed of descent was calculated using the peak death rate and subsequent reduction to 50% of this peak rate (25% and 50% selected to include time window when epidemic peaks were visibly most stable). An assumption was made that any change in population incidence of COVID-19 cases may begin to be seen 2 weeks later in mortality data, thus analyses of the effect of lockdown focused on the period before or after week 15 (lockdown was announced in week 13 (March 2020) and ended on ‘Super Saturday’ (4 July, week 27), which is shown in timeline plots). The ‘peak difference’ was the difference in weeks between the peak mortality rate and the week in which lockdown began to take effect (week 15).
Weekly age-standardised mortality rates per IMD decile (as opposed to per local authority) were not available at the time of writing, thus they were calculated from the age-standardised estimates from the local authority data (please see online supplemental file 1 for more details).
bmjopen-2021-058658supp001.pdf (93.4KB, pdf)
Simple linear models were employed to analyse the associations between visually normally distributed measures such as the total cumulative mortality rate with other metrics (eg, the speed of increase in death rate) and IMD decile. The purpose of these simple models was to understand the relative contribution of deprivation (measured by IMD) and relevant epidemic dynamics (eg, date of first recorded COVID-19 deaths) to the metric of interest, therefore no model selection was employed, and covariate inclusion was based on empirical knowledge. Any covariates found to fall above the threshold of statistical significance (Wald p>0.05 in multivariable models) would be removed from the model (however, no covariates needed to be removed in this way). Differences between mean speed of increase or decrease per IMD decile were assessed by non-overlap of 95% CIs.
Maps were drawn based on 2020 geographical boundaries from the ONS Open Geography Portal.27
All analyses were conducted in R statistical software V.3.6.2.
Patient and public involvement
Our public involvement panel inputted into project design and considered the research topic to be of contemporary importance and value. The data used do not require patient permissions for use and are publicly available.
Results
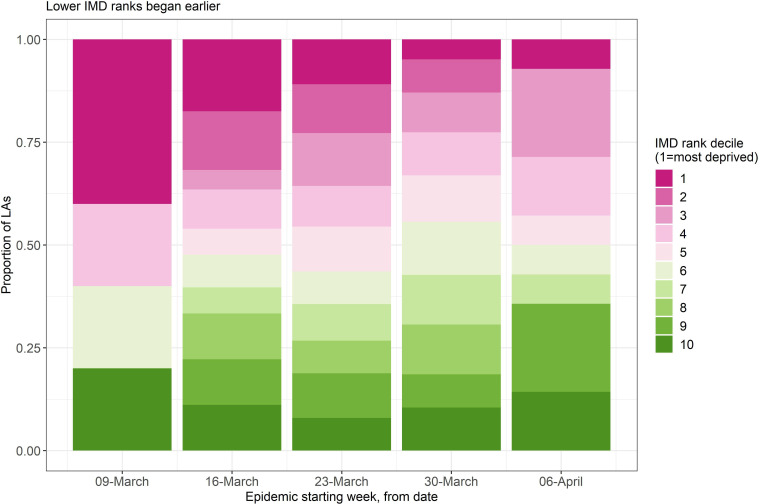
All 307 lower-tier local authorities in England began registering deaths involving COVID-19 between weeks 11 and 15. The proportion of areas of each IMD decile per ‘starting week’ is shown in figure 1. From this it can be seen that more deprived areas (most deprived decile=1) tended to begin recording COVID-19 deaths earlier than less deprived areas (least deprived decile=10).
Figure 1.
Proportion of 312 English local authorities within each IMD decile that began recording COVID-19 deaths between weeks 11 and 15 of 2020. IMD, Index of Multiple Deprivation; LA, Local Authorities.
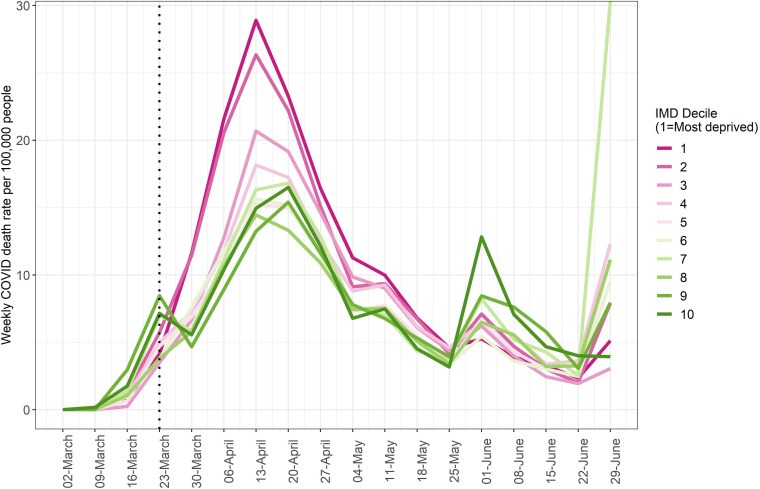
Figure 2 depicts the weekly mortality rates per 100 000 people for each IMD decile. After the first 2 weeks of the epidemic, the two most deprived deciles (20% of local authorities) had the highest speed of increase in age-standardised mortality rates and reached higher peak rates than less deprived areas.
Figure 2.
Weekly age-standardised COVID-19 mortality rates per 100 000 in areas of each IMD decile. Dotted line indicates the start of the first national lockdown (26 March). IMD, Index of Multiple Deprivation.
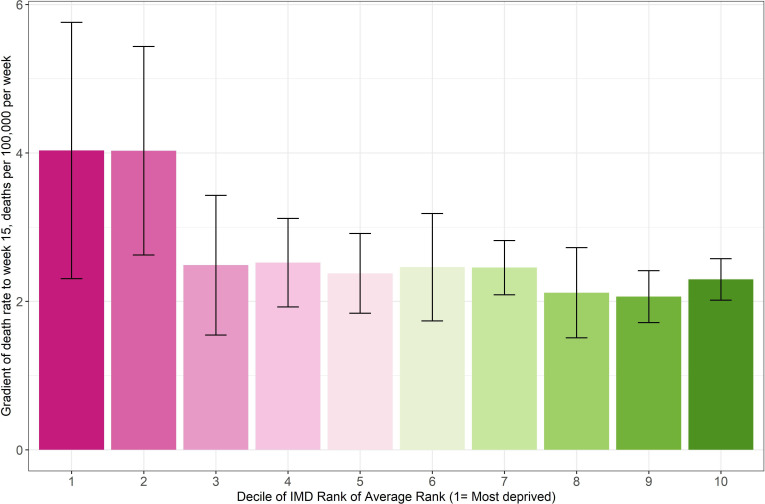
From the week of their first COVID-19 deaths to week 15 (when lockdown could plausibly have begun affecting death rates), local authorities in the two most deprived deciles had the highest speed of increase in death rate (although not statistically significantly different), and the less deprived deciles increased more slowly (figure 3). The mean speed of increase in the two most deprived IMD deciles was 4.03 deaths per 100 000 persons per week, and in the two least deprived deciles was 2.18 deaths per 100 000 persons per week (a difference of 46%).
Figure 3.
Simple linear gradient of age-standardised COVID-19 death rate per 100 000 people between the first week of recorded COVID-19 deaths and week 15, across rank of average rank of IMD deciles. IMD, Index of Multiple Deprivation.
All local authorities’ death rate curves peaked and began to decline between 3 and 10 weeks following the start of the first lockdown. Those local authorities whose death rates were increasing faster before lockdown peaked sooner after lockdown commenced compared with slower local authorities.
The total age-standardised cumulative mortality over the first wave (up to week 27, week commencing 28 June 2020) varied from 119 to 2349 deaths per 100 000 persons per local authority. Table 1 describes the multivariable linear model of total cumulative death rates per local authority. It shows that, compared with the most deprived 10% of local authorities, less deprived areas (deciles 3–10) recorded lower cumulative death rates, and that areas with higher speeds of increase—and more weeks of recorded COVID-19 deaths before lockdown (plus those that peaked later)—saw higher total death rates.
Table 1.
Linear multivariable model of the total cumulative age-standardised COVID-19 death rate per 100 000 persons between weeks 1 and 27 of 2020, among 307 local authorities in England
| Metric | Adjusted beta coefficient (SE) | P value |
| IMD decile | ||
| 1 (most deprived) | REF | |
| 2 | −41.16 (49.30) | 0.40 |
| 3 | −108.20 (50.46) | 0.03 |
| 4 | −132.11 (49.80) | 0.008 |
| 5 | −140.82 (50.83) | 0.006 |
| 6 | −183.66 (50.64) | <0.001 |
| 7 | −225.06 (50.81) | <0.001 |
| 8 | −170.43 (51.01) | <0.001 |
| 9 | −213.73 (50.82) | <0.001 |
| 10 | −262.16 (50.28) | <0.001 |
| Speed of increase (to week 15), deaths per 100 000 per week | 12.87 (0.47) | <0.001 |
| Weeks from week of first registered COVID-19 deaths to lockdown | 216.98 (13.04) | <0.001 |
| Weeks between peak and lockdown | 104.56 (17.38) | <0.001 |
IMD, Index of Multiple Deprivation.
As mentioned, all local authorities began recording COVID-19 deaths between weeks 11 and 15, that is, from 2 weeks before the announcement of the first lockdown, to 2 weeks after. The difference in total cumulative death rates for areas grouped by starting week are as seen in table 2.
Table 2.
Mean cumulative COVID-19 death rate per 100 000 persons over the first wave (weeks 1–27, 2020) of the pandemic among 307 local authorities in England
| Timing of start week relative to week 13 (when lockdown 1 was announced) | Total cumulative age-standardised COVID-19 death rate per 100 000 persons for whole of wave 1 (weeks 1–27, 2020), (SD) | No of local authorities |
| 2 weeks before | 465 (451) | 14 |
| 1 week before | 780 (324) | 124 |
| Same week | 984 (407) | 101 |
| 1 week after | 1188 (505) | 63 |
| 2 weeks after | 1147 (255) | 5 |
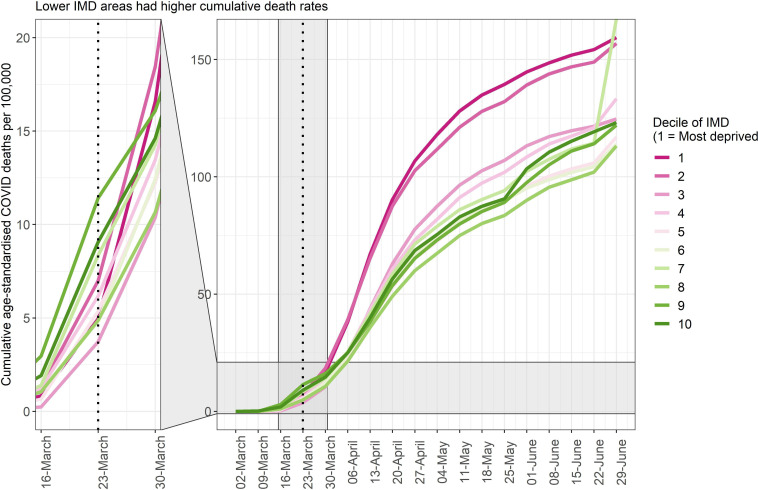
Figure 4 depicts the cumulative COVID-19 death rates of each IMD decile over the whole of the first wave. Mortality rates in more deprived areas (deciles 1 and 2) were rising faster than others at the start of lockdown (vertical dotted line), and the disparity in cumulative mortality grew as the pandemic progressed.
Figure 4.
Cumulative COVID-19 death rates per 100 000 for areas of each IMD decile over the first wave of the pandemic in 307 local authorities in England. Dotted line marks timing of the announcement of the first lockdown, zoomed in area between weeks 13 and 14. IMD, Index of Multiple Deprivation.
Up until week 15 when the effects of lockdown may have started to be seen in mortality data, the cumulative death rate per 100 000 persons already differed by IMD decile. The two most deprived deciles recorded 77.16 deaths per 100 000 persons by this time, whereas the two least deprived deciles recorded only 50.01 deaths per 100 000 persons. This inequality reduced by the time the first wave had passed (by week 27), but did not equalise, with the most deprived two deciles recording 316.14 total deaths per 100 000 persons, and the least deprived recording 245.10 deaths per 100,00 persons. These equate to an excess of 54% before lockdown vs 29% after lockdown.
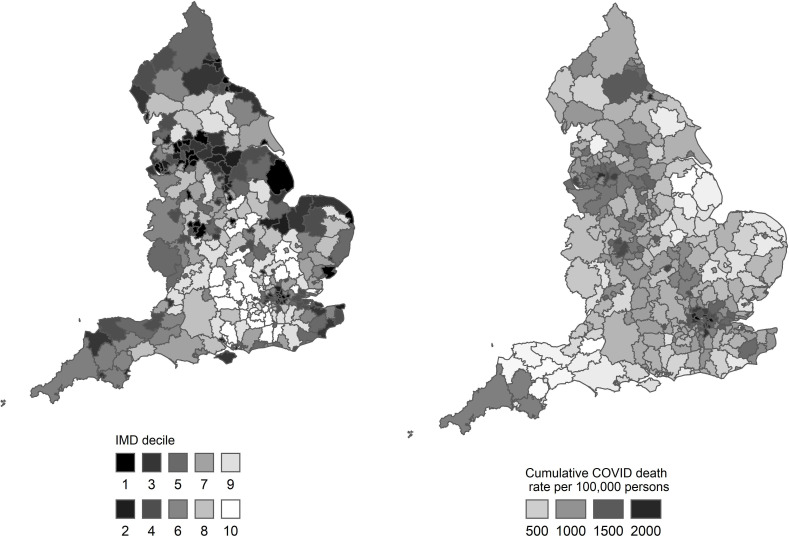
Figure 5 illustrates the geographical distribution of deprivation based on IMD and the total cumulative age-standardised COVID-19 death rate per 100 000 persons over the first wave of the pandemic. London and the North West featured many of the areas with the highest overall death rates. Although these areas featured many deprived local authorities, the distributions were not identical.
Figure 5.
Average rank of the Index of Multiple Deprivation (IMD) and total cumulative COVID-19 death rate per 100 000 persons over the first wave of the pandemic (weeks 1–27, 2020) per local authority in England.
Discussion
This study has provided the first examination of the evolution of inequalities in the COVID-19 pandemic. It has found that inequalities in COVID-19 mortality rates by deprivation in England began to appear early in the first wave. More deprived local authorities generally started recording COVID-19 deaths earlier than less deprived areas, and mortality rates also increased faster in more deprived areas, and rose to higher peak rates. All of the 307 lower-tier local authorities in England began recording COVID-19 deaths as early as 2 weeks before first national lockdown in England was announced, or up to 2 weeks afterwards, with the latter—less deprived—group of local authorities recording fewer cumulative deaths over the whole of the first wave, compared with the former—more deprived—group of local authorities.
The study has also provided the first assessment of the impacts of the first English national lock down on the evolution of the pandemic. It has found that following the implementation of the national lockdown, local authorities where death rates had been rising faster (ie, more deprived areas), peaked and began to descend earlier than the other—less deprived—local authorities. Cumulative death rates were higher in more deprived areas by the time lockdown began, but the difference narrowed moderately towards the end of the first wave.
England imposed a national lockdown during the first wave of the COVID-19 epidemic in March 2020.28 This measure aimed to drastically reduce instances of interpersonal contact between infected individuals (whether symptomatic or not) and the wider susceptible population. Confining the public to their homes, suspending face-to-face education and restricting travel placed great burdens on the health and welfare of many individuals and communities, through a number of pathways that are still being elucidated, and which will continue to emerge.29–31 There is no doubt that the economic implications of such lockdowns can be severe, and disruptions to usual healthcare provision have led to increased mortality from non-COVID-19 causes.32 However, the risks posed to society of not imposing such lockdowns are likely much greater.33 Unchecked viral spread would lead to mass fatalities, increased disability rates especially in the young from the effects of non-fatal infection (so-called ‘long COVID-19’34), and an increased risk of viral mutation into forms which may pose even greater threat.35 Importantly, the National Health Service (NHS) could potentially be filled beyond capacity with COVID-19 patients, leaving insufficient resources for non-COVID patients of all ages and diagnoses. Economic implications of unchecked viral spread are likely to be considerably worse than those caused by national lockdowns, and could continue for longer due to the likelihood of future outbreaks of mutated viral strains and multiple waves of infection.33 A well-timed national lockdown has the ability to reduce case incidence to low levels at which ‘test, trace and isolate' programmes can efficiently extinguish local outbreaks, and lends time for mass vaccination to offer protection, especially to the most vulnerable. However, a lockdown that is imposed too late, that is, when disease incidence is already high and rising, needs to be substantially more stringent and protracted to offer the same slowing effect on case numbers and, subsequently, deaths.33
Previous work has focused on comparing COVID-19 mortality rates between areas of England using set time periods without considering the evolution of the inequalities reported,36 or have identified inequalities in case rates and other metrics.16 Using mortality data removes some of the uncertainty surrounding early case ascertainment, since early in the English epidemic, testing was only being performed in hospitals on symptomatic individuals, and so many infections would not have been recorded.
It has been noted internationally that the seeding of SARS-CoV-2 into a country tends to be via travel by people at the upper end of the socioeconomic spectrum, taking international holidays or travelling for business.37 38 Cases then increase within these less deprived populations until social distancing and national lockdowns are advised or mandated. At this point, the disease burden shifts to the more deprived, who are less able to fully adhere to these guidelines due to less ability to work from home, fewer resources, precarious work, higher population densities and other pre-existing factors.37 These communities may also face barriers to health system access and differences in treatment or care. These two ‘phases’ of pandemic spread likely apply to COVID-19 cases in England, where the index cases were holidaymakers returning from skiing trips to Austria.39 40 Plümper and Neumayer37 reported that in Germany, despite a somewhat reduced likelihood of infection for those in more deprived areas in the first phase of the epidemic, these communities were nevertheless at similar risk of death. This relative risk of mortality increases for more deprived areas once transmission is established in ‘phase 2’ of the pandemic—due to population vulnerabilities including poverty, overcrowding and pre-existing chronic conditions (a so-called ‘syndemic’ pandemic).41 Our analysis of early-stage mortality in England confirmed this structure, in that mortality rates rose first to a small initial ‘peak’ in less deprived areas, before being dominated by more deprived local authorities. The earliest data available to the German study began more than 2 weeks following the implementation of government lockdowns, whereas the analysis we present here predate the UK lockdown by a number of months, and hence capture the very earliest data available on COVID-19 deaths.
We have shown that inequalities in cumulative death rates during the first wave of infection in England existed from the earliest stages of COVID-19 mortality reporting, and were entrenched by differences in the speed of increase, leading to unequal burdens of cumulative mortality at local authority level by the time the first national lockdown was called. These inequalities reduced marginally but were not abolished by the national control measures implemented in the lockdown. The first national lockdown in England was fairly strict (eg, a ‘stay at home order’) and it was a universal intervention, enforced and applied to the whole population and thereby requiring little by way of individual agency. Previous public health research has shown that such measures are more likely to reduce inequalities in health than those that require individual choice/compliance.42 That the lockdown did not completely eliminate ecological inequalities in COVID-19 mortality may well be as a result of inequalities in (1) vulnerability (whereby more deprived areas had a higher burden of clinical risk factors); (2) susceptibility (whereby immune response was lower in more deprived populations due to the adverse consequences of long term exposures to harmful living and environmental conditions); (3) exposure (inequalities in working conditions notably less ability to work at home in the low-income jobs predominating within more deprived local authorities) and (4) transmission (higher rates of overcrowding and population density in the community may have impacted on infection spread in more deprived areas41).
Conclusion
This study has found that inequalities in death rates during the first wave of infection in England existed from the earliest stages of the COVID-19 pandemic, and were entrenched by differences in the speed of increase. This led to a significant unequal burden in cumulative mortality between the most and least deprived local authorities by the time the first national lockdown was implemented. These inequalities reduced marginally—but were not abolished—during the national lockdown. It is difficult to say with certainty whether an earlier—or longer—national lockdown could have further reduced these inequalities, but it should be noted that, although the lockdown did reverse the trend in mortality rates across the country, it had to do so at more advanced stages of the epidemic in more deprived areas, compounding the unequal disease burden on these communities and local healthcare systems. Susceptibility to infection and fatality from COVID-19 is undoubtedly closely associated with deprivation, but other factors also play an important part, as well as the stochasticity implicit in viral spread. Nevertheless, our understanding of how deprivation associates with mortality from a novel infectious disease within a susceptible population it can help to focus future public health attention on those communities most in need and at risk.
Limitations
Weekly age-standardised mortality rates were not available at local authority level at the time of writing. However, we were able to pro rata monthly age-standardised rates to weekly ones using weekly death counts. Age-standardised weekly rates are unlikely to become available at lower geography levels due to disclosure risks. Death counts did not include deaths of non-residents of England, nor where place of residence was unknown, and was based on date of registration rather than date of death.
Deprivation is undoubtedly linked to COVID-19 mortality, it cannot explain all of the variation in area-level mortality rates, hence COVID-19 mortality and IMD are not perfectly correlated. Many other factors including comorbidity, healthcare provision, employment types and variation in transport links all likely play a part in the causal web linking lockdowns to mortality inequalities. A deeper analysis of these underlying associations was beyond the scope of the current paper, but warrants further scrutiny.
Testing was limited to hospitalised patients in the earliest months of the pandemic in England. This may have introduced bias to our initial analyses since deaths from COVID-19 may not have been correctly attributed, had the person not received a positive test prior to death. However, we were unable to retrospectively account for this, and it would have applied to a small number of deaths in the earliest time period. Given consistency of trends across areas that began recording deaths at different stages of the national pandemic, we do not believe that this would have introduced serious bias.
Supplementary Material
Footnotes
Twitter: @DrClaireEWelsh
Contributors: FM, CB and CW designed the study. CW completed all analyses with input from FM and CB. CW, VA, FM and CB contributed to drafting the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. CW is guarantor of the analysis.
Funding: This work was supported by a grant from The Health Foundation (Ref: 2211473), who took no part in the design, analysis or writing of this study.
Map disclaimer: The depiction of boundaries on the map(s) in this article does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Pillai J, Motloba P, Motaung KSC, et al. The effect of lockdown regulations on SARS-CoV-2 infectivity in Gauteng Province, South Africa. S Afr Med J 2020;110:1119–23. 10.7196/SAMJ.2020.v110i11.15222 [DOI] [PubMed] [Google Scholar]
- 2.Chen JT, Krieger N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US County versus ZIP code analyses. J Public Health Manag Pract 2021;27 Suppl 1, COVID-19 and Public Health: Looking Back, Moving Forward:S43–56. 10.1097/PHH.0000000000001263 [DOI] [PubMed] [Google Scholar]
- 3.Laster Pirtle WN. Racial capitalism: a fundamental cause of novel coronavirus (COVID-19) pandemic inequities in the United States. Health Educ Behav 2020;47:504–8. 10.1177/1090198120922942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Barneveld K, Quinlan M, Kriesler P, et al. The COVID-19 pandemic: lessons on building more equal and sustainable societies. Econ Labour Relat Rev 2020;31:133–57. 10.1177/1035304620927107 [DOI] [Google Scholar]
- 5.Nazroo J, Becares L. Evidence for ethnic inequalities in mortality related to COVID-19 infections: findings from an ecological analysis of England and Wales. medRxiv 2020. 10.1101/2020.06.08.20125153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roxo L, Bambra C, Perelman J. Gender equality and gender inequalities in self-reported health: a longitudinal study of 27 European countries 2004 to 2016. Int J Health Serv 2021;51:1–9. 10.1177/0020731420960344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.England PH. Disparities in the risk and outcomes of COVID-19, 2020: 89. https://www.gov.uk/government/publications/covid-19-review-of-disparities-in-risks-and-outcomes [Google Scholar]
- 8.Dahal S, Luo R, Swahn MH, et al. Geospatial variability in excess death rates during the COVID-19 pandemic in Mexico: examining Socio demographic, climate and population health characteristics. Int J Infect Dis 2021;113:347–54. 10.1016/j.ijid.2021.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baena-Díez JM, Barroso M, Cordeiro-Coelho SI, et al. Impact of COVID-19 outbreak by income: hitting hardest the most deprived. J Public Health 2020;42:698–703. 10.1093/pubmed/fdaa136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benita F, Gasca-Sanchez F. The main factors influencing COVID-19 spread and deaths in Mexico: a comparison between phases I and II. Appl Geogr 2021;134:102523. 10.1016/j.apgeog.2021.102523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martines MR, Ferreira RV, Toppa RH, et al. Detecting space–time clusters of COVID-19 in Brazil: mortality, inequality, socioeconomic vulnerability, and the relative risk of the disease in Brazilian municipalities. J Geogr Syst 2021;23:7–36. 10.1007/s10109-020-00344-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Franch‐Pardo I, Desjardins MR, Barea‐Navarro I, et al. A review of GIS methodologies to analyze the dynamics of COVID‐19 in the second half of 2020. Transactions in GIS 2021;25:2191–239. 10.1111/tgis.12792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katikireddi SV, Lal S, Carrol ED, et al. Unequal impact of the COVID-19 crisis on minority ethnic groups: a framework for understanding and addressing inequalities. J Epidemiol Community Health 2021;75:970–4. 10.1136/jech-2020-216061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salvatore M, Basu D, Ray D, et al. Comprehensive public health evaluation of lockdown as a non-pharmaceutical intervention on COVID-19 spread in India: national trends masking state-level variations. BMJ Open 2020;10:e041778. 10.1136/bmjopen-2020-041778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desvars-Larrive A, Dervic E, Haug N, et al. A structured open dataset of government interventions in response to COVID-19. Scientific Data 2020;7:1–9. 10.1038/s41597-020-00609-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morrissey K, Spooner F, Salter J, et al. Area level deprivation and monthly COVID-19 cases: the impact of government policy in England. Soc Sci Med 2021;289:114413. 10.1016/j.socscimed.2021.114413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.HM Government . The Health Protection (Coronavirus, Restrictions) (No. 2) (England) Regulations 2020 [Internet]. SI2020/684, 2020. Available: https://www.legislation.gov.uk/uksi/2020/684/contents/made [Accessed 23 Feb 2021].
- 18.HM Government . The Health Protection (Coronavirus, Restrictions) (England) Regulations 2020 [Internet]. SI 350, 2020. Available: https://www.legislation.gov.uk/uksi/2020/350/contents/made [Accessed 23 Feb 2021].
- 19.Sun Y, Hu X, Xie J. Spatial inequalities of COVID-19 mortality rate in relation to socioeconomic and environmental factors across England. Sci Total Environ 2021;758:143595. 10.1016/j.scitotenv.2020.143595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Platt L, Warwick R. COVID‐19 and Ethnic Inequalities in England and Wales *. Fisc Stud 2020;41:259–89. 10.1111/1475-5890.12228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Timson A. What geographic inequalities in COVID-19 mortality rates and health can tell us about levelling up | The Health Foundation. The Health Foundation [Internet], 2021. Available: https://www.health.org.uk/news-and-comment/charts-and-infographics/what-geographic-inequalities-in-covid-19-mortality-rates-can-tell-us-about-levelling-up
- 22.Griffith GJ, Davey Smith G, Manley D, et al. Interrogating structural inequalities in COVID-19 mortality in England and Wales. J Epidemiol Community Health 2021;75:1–7. 10.1136/jech-2021-216666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Office for National Statistics . Analysis of death registrations not involving coronavirus (COVID-19), England and Wales: 28 December 2019 to 1 may 2020; 2020.
- 24.ONS . Deaths due to COVID-19 by local area and deprivation [Internet], 2021. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/deathsduetocovid19bylocalareaanddeprivation
- 25.Ministry of Housing Communities & Local Government . English Indices of Deprivation 2019 - Summaries at Local Authority Level [Internet], 2019. Open data. Available: http://opendatacommunities.org/data/societal-wellbeing/imd2019/indicesbyla
- 26.Ministry of Housing C & LG . English indices of deprivation [Internet], 2020. Available: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019
- 27.Office for National Statistics . Local Authority Districts (December 2019) Boundaries UK BUC. Open Geography Portal [Internet]. Available: https://geoportal.statistics.gov.uk/datasets/local-authority-districts-december-2019-boundaries-uk-buc
- 28.News BBC. Coronavirus: Strict new curbs on life in UK announced by PM [Internet], 2020. Available: https://www.bbc.co.uk/news/uk-52012432
- 29.Richardson DL, Duncan MJ, Clarke ND, et al. The influence of COVID-19 measures in the United Kingdom on physical activity levels, perceived physical function and mood in older adults: a survey-based observational study. J Sports Sci 2021;39:1–13. 10.1080/02640414.2020.1850984 [DOI] [PubMed] [Google Scholar]
- 30.Ball S, Banerjee A, Berry C, et al. Monitoring indirect impact of COVID-19 pandemic on services for cardiovascular diseases in the UK. Heart 2020;106:1890–7. 10.1136/heartjnl-2020-317870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henry N, Parthiban S, Farroha A. The effect of COVID-19 lockdown on the incidence of deliberate self-harm injuries presenting to the emergency room. Int J Psychiatry Med 2021;56:1–12. 10.1177/0091217420982100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vandoros S. Excess mortality during the Covid-19 pandemic: early evidence from England and Wales. Soc Sci Med 2020;258:113101. 10.1016/j.socscimed.2020.113101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Balmford B, Annan JD, Hargreaves JC, et al. Cross-country comparisons of Covid-19: policy, politics and the price of life. Environ Resource Econ 2020;76:525–51. 10.1007/s10640-020-00466-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Iacobucci G. Long covid: damage to multiple organs presents in young, low risk patients. BMJ 2020:m4470. 10.1136/bmj.m4470 [DOI] [Google Scholar]
- 35.European Centre for Disease Prevention and Control . Risk related to the spread of new SARS-CoV-2 variants of concern in the EU/EEA-first update, 2021: 29. https://beta.microreact.org/project/r8vBmatkC9mcfrJJ6bUtNr-cog-uk-2021-01-09-sars-cov-2-in-the-uk/ [Google Scholar]
- 36.ONS . Coronavirus (COVID-19) Infection Survey, UK: 16 July 2021 [Internet], 2021. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveypilot/16july2021
- 37.Plümper T, Neumayer E. The pandemic predominantly hits poor neighbourhoods? SARS-CoV-2 infections and COVID-19 fatalities in German districts. Eur J Public Health 2020;30:1176–80. 10.1093/eurpub/ckaa168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clouston SAP, Natale G, Link BG. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: a examination of the emergence of social inequalities. Soc Sci Med 2021;268:113554. 10.1016/j.socscimed.2020.113554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wikipedia . COVID-19 pandemic in the United Kingdom [Internet]. Available: https://en.wikipedia.org/wiki/COVID-19_pandemic_in_the_United_Kingdom [Accessed 04 Feb 2021].
- 40.Correa-Martínez CL, Kampmeier S, Kümpers P, et al. A pandemic in times of global tourism: Superspreading and exportation of COVID-19 cases from a Ski area in Austria. J Clin Microbiol 2020;58:19–21. 10.1128/JCM.00588-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bambra C, Riordan R, Ford J, et al. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;121:jech-2020-214401–8. 10.1136/jech-2020-214401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adams J, Mytton O, White M. Why are some population interventions for diet and obesity more equitable and effective than others? The role of individual agency. PLoS Medicine 2016;13:1–7. 10.1371/journal.pmed.1001990 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-058658supp001.pdf (93.4KB, pdf)
Data Availability Statement
Data are available on reasonable request.