Abstract
Introduction
Type 2 diabetes (T2D) is characterised by elevated plasma glucose, free fatty acid (FFA) and insulin concentrations, and this metabolic profile is linked to diabetic cardiomyopathy, a diastolic dysfunction at first and increased cardiovascular disease (CVD) risk. Shifting cardiac metabolism towards glucose utilisation has been suggested to improve cardiovascular function and CVD risk, but insulin treatment increases overall glucose oxidation and lowers lipid oxidation, without reducing CVD risk, whereas SGLT2 inhibitors (SGLT2i) increase FFA, ketone body concentrations and lipid oxidation, while decreasing insulin concentrations and CVD risk. The aim of the present study is to elucidate the importance of different metabolic profiles obtained during treatment with a SGLT2i versus insulin for myocardial function in patients with T2D.
Methods and analyses
Randomised, crossover study, where 20 patients with T2D and body mass index>28 kg/m2 receive 25 mg empagliflozin daily or NPH insulin two times per day first for 5 weeks followed by a 3-week washout before crossing over to the remaining treatment. Insulin treatment is titrated to achieve similar glycaemic control as with empagliflozin. In those randomised to insulin first, glycaemia during an initial empagliflozin run-in period prior to randomisation serves as target glucose. Metabolic and cardiac evaluation is performed before and at the end of each treatment period.
The primary endpoint is change (treatment—washout) in left ventricular peak filling rate, as assessed by cardiac MRI with and without acute lowering of plasma FFAs with acipimox. Secondary and explorative endpoints are changes in left atrial passive emptying fraction, left ventricular ejection fraction, central blood volume and metabolic parameters.
Ethics and dissemination
This study is approved by the Danish Medicines Agency (ref. nr.: 2017061587), the Danish Data Protection Agency (ref. nr.: AHH-2017-093) and the Capital Region Ethics Committee (ref. nr.: H-17018846). The trial will be conducted in accordance with ICH-GCP guidelines and the Declaration of Helsinki and all participants will provide oral and written informed consent. Our results, regardless of outcome, will be published in relevant scientific journals and we also will seek to disseminate results through presentations at scientific meetings.
Trial registration number
EudraCT: 2017-002101.
Keywords: coronary heart disease, ischaemic heart disease, myocardial infarction, diabetic nephropathy & vascular disease, diabetes & endocrinology
Strengths and limitations of this study.
Comparison with NPH insulin, which has opposite metabolic effects to empagliflozin, provides a strong basis for detecting metabolic effects on cardiac function.
Repeated cardiac MRI during depletion of plasma free fatty acids (FFAs) with acipimox during treatments and washouts allows for dissection of the individual roles of hyperglycaemia, hyperinsulinaemia and elevated FFAs on cardiac function in type 2 diabetes (T2D).
A crossover design is vulnerable to dropout, but provides greater statistical power.
Effects of metabolic changes on cardiac function are limited to the 5-week intervention period, which excludes effects arising from longer-term treatment.
Introduction
Type 2 diabetes (T2D) is characterised by hyperglycaemia, hyperinsulinaemia, increased free fatty acids (FFAs) and impaired tissue glucose uptake and oxidation.1 T2D is associated with an increased cardiovascular morbidity, and the more dysregulated the metabolic state, the greater the cardiovascular risk.2–5 T2D develops when insulin secretion can no longer compensate for the ambient insulin resistance, and therefore previous treatments has focused on increasing insulin signalling by either exogenous insulin administration, stimulation of endogenous insulin secretion or enhancing insulin sensitivity.1
Diabetic cardiomyopathy (DCM) is an early ‘silent’ complication to T2D, independent of hypertension and/or coronary heart disease. It is characterised by left ventricular (LV) hypertrophy and diastolic dysfunction6 7 and has been linked to the increased cardiovascular risk in T2D.8 DCM may be accurately described by measuring left ventricular peak filling rate (LVPFR) and left ventricular ejection fraction (LVEF) using cardiac MRI (CMR).9 10 Both diastole and systole are energy requiring processes and sensitive to changes in energy availability.11 12 Interestingly, cardiac metabolism in patients with T2D is altered and depends more on lipid oxidation and less on glucose oxidation compared with non-diabetic controls.13 14 It has been argued that glucose oxidation is a better source of energy for the heart than lipid oxidation, especially during stress, such as myocardial ischaemia, because this yields more adenosine triphosphate unit oxygen.15 However, manipulating cardiac metabolism towards glucose oxidation, by administering glucose–insulin (–potassium) infusions in patients with hyperglycaemia and myocardial infarction has been attempted, but did not improve survival in neither diabetic nor non-diabetic patients.16–18 In intensive care unit patients, strict glycaemic control using insulin has been associated with increased mortality,19 and in patients with T2D and increased cardiovascular disease (CVD) risk, intensive glycaemic control has not reduced CVD risk compared with conventional glycaemic control20–23 and in the ACCORD Study, which involved aggressive insulin treatment resulted in excess mortality.24 Thus, insulin treatment does not prevent cardiovascular events in patients with T2D nor improve prognosis when such occur.24
SGLT2 inhibition (SGLT2i), on the other hand, is a newer treatment principle in T2D, which has proven effective in attenuating the risk of myocardial infarctions, worsening of heart failure, cardiovascular mortality and all-cause mortality in patients with T2D.25–27
SGLT2i increases renal glucose excretion thereby lowering plasma glucose (PG) and insulin levels and increasing glucagon release, lipolysis and ketogenesis.28 29 Additionally, tissue glucose uptake and oxidation is reduced and hepatic glucose production increased.30 The exact cardioprotective mechanisms of SGLT2i are not yet understood, but has been proposed to be linked to improved haemodynamics,31 inhibition of myocardial Na+/H+ exchange32 33 or reductions in inflammatory activity.34 35
An early and interesting hypothesis proposed that changes in cardiac metabolism may be responsible for the cardioprotective effect of SGLT2i. The lowered glucose and insulin concentrations, persistent hyperketonaemia and elevated FFAs, caused by SGLT2i treatment, leads to reduced glucose uptake, increased ketone body uptake and oxidation and unchanged uptake of FFAs in the heart while overall lipid oxidation is increased.28 36 This altered energy metabolism may rapidly improve myocardial function, especially during myocardial stress.37–40 The SGLT2i-induced myocardial fuel switch from glucose to fatty acids and ketone bodies has been suggested to ameliorate adverse cardiac remodelling and heart failure in non-diabetic porcine models,41 and it is noteworthy that eliminating the availability of FFAs to insulin resistant hearts can lead to cardiac dysfunction in rodents and in humans, suggesting an important role for lipid metabolism in cardiac function.42–45 Cardiovascular endpoint trials with SGLT2 inhibitors have shown effects within weeks after initiation of treatment, coinciding with the metabolic effects of the treatment.25 28
Altogether, SGLT2 inhibitors ‘amplify’ some components of the dysmetabolic profile of T2D and works opposite the metabolic effects of insulin. This raises the question of how cardiac function in patients with T2D depends on lipid and glucose oxidation in the resting state and during stress, and how increasing or lowering blood glucose, FFAs, ketone bodies and insulin concentrations influence cardiac function.
Objective
The primary objective of the present study is to evaluate myocardial function in patients with T2D and high risk of CV events using advanced CMR scans during rest, chronotropic stress and under depletion of plasma FFAs before and after 5 weeks of empagliflozin treatment (high FFA and ketone body concentrations, high lipid oxidation and low insulin concentrations) and before and after 5 weeks of human insulin treatment titrated to yield glycaemic control similar to the empagliflozin treatment period (low FFA and ketone body concentrations, high insulin concentrations and glucose oxidation).
Hypothesis
We hypothesise that hyperinsulinaemia and hyperglycaemia are conditions that negatively affect cardiac function in T2D, while the availability of FFAs and ketone bodies and switching metabolism towards lipid oxidation improves cardiac diastolic and systolic function. Thus, we expect that lowering PG insulin independently, and increasing fatty acid concentrations, lipid oxidation and ketone body availability with empagliflozin treatment, improves myocardial function in patients with T2D, and that depleting plasma of FFAs during empagliflozin treatment will impair cardiac function.
Methods and analyses
Design
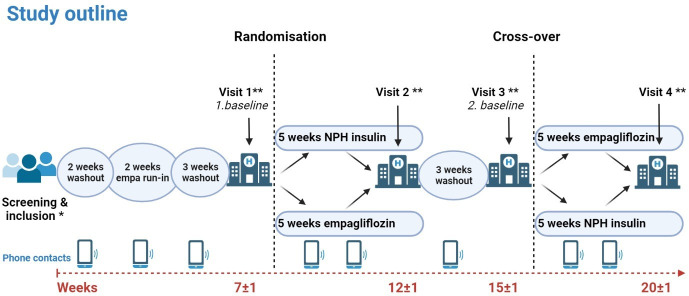
This is a 20-week prospective, investigator-initiated, comparator-controlled, open-label, two-arm crossover, human study where subjects are randomised in blocks of 3–5 to Neutral Protamine Hagedorn (NPH) insulin twice daily or empagliflozin treatment (25 mg once daily) for 5±1 weeks, followed by 3±1 weeks washout and crossover of treatment for 5±1 weeks (figure 1). For 7 weeks preceding randomisation, but after inclusion, patients undergo a programme of 2 weeks of washout of pre-existing antiglycaemic treatment (except metformin), 2 weeks of empagliflozin run-in (used for glycaemic target and titration of treatment in participants randomised to insulin first, see below) followed by 3 weeks of washout. During run-in and treatment periods, participants measure blood glucose two times per day (fasting and before evening meal) and during washouts patients measure fasting blood glucose.
Figure 1.
Study outline. included patients undergo a 7-week programme of washout of pre-existing antiglycemic treatment (except metformin) and run-in of empagliflozin. Hereafter, they are randomised to treatment for 5±1 weeks, followed by 3±1 weeks washout and crossover to 5±1 weeks treatment with the remaining study drug. Tests performed at each visit are summarised in tables 3 and 4. *See table 2 for screening procedure. **See tables 3 and 4 for visit overview. NPH, Neutral Protamine Hagedorn.
After the screening visit (V0) there are four study visits (V1–4)—before and at the end of each treatment period. Each visit consists of three study days—a metabolic study day (MET) and two CMR study days. Randomisation is performed at V1 after the metabolic study day.
Participants
Twenty subjects older than 18 years diagnosed with T2D, a body mass index≥28 kg/m2, glycated haemoglobin≤9%, fasting C-peptide>500 pmol/L and unchanged antiglycaemic treatment for 12 weeks prior to screening, and who are at a risk of CVD, are eligible for the study. High CVD risk is modified from the EMPA-REG protocol.46 Inclusion, exclusion and withdrawal criteria are listed in box 1.
Box 1. Eligibility criteria.
Inclusion criteria
Age≥18 years
Body mass index≥28 kg/m2
Glycated haemoglobin≤9% (≤10% in diet or metformin treated only)
Fasting C-peptide≥500 pmol/L
Unchanged glycaemic treatment for 3 months prior to inclusion
-
High cardiovascular risk as one of the following:
Previous myocardial infarction, stroke or peripheral arterial disease more than 2 months prior to informed consent
Evidence of multivessel coronary arterial disease (CAD) but without prior myocardial infarction, if more than 50% stenosis is present, if revascularised (Coronary Arterial Bypass Graft (CABG) or Percutaneous Coronary Intervention (PCI)) more than 2 months prior or if one vessel is vascularised and the other with 50% stenosis
Single vessel CAD without prior myocardial infarction if more than 50% stenosis is present, not revascularised and positive stress test for ischaemia
Exclusion criteria
Insulin treatment within 3 months from informed consent
Type 1 diabetes
Psychiatric disorder or mental retardation
Drug or alcohol abuse within 3 months from informed consent
Poor compliance
Anaemia (haemoglobin<103.1 g/L) or other blood dyscrasias causing haemolysis or unstable erythrocytes
Indication of liver disease (Alanine transferase or alkaline phosphatase elevation above three times the upper normal limit)
Impaired renal function (estimated glomerular filtration rate<45 mL/min/1.73 m2)
Antiobesity medication within 3 months from informed consent
Systemic steroid treatment within 6 weeks from informed consent
Any uncontrolled endocrine disorder except type 2 diabetes
Bariatric surgery or other gastrointestinal conditions that may compromise gastrointestinal absorption
Peptic ulcer—verified endoscopically
Any form of surgery within 3 months of informed consent
Acute myocardial infarction, stroke or peripheral arterial disease within 2 months of informed consent
Persistent or permanent atrial fibrillation
Inability to undergo experimental procedures including exclusion criteria for cardiac MRI scanning:
Implantable cardioverter defibrillator/pacemaker
Ferromagnetic clips
Claustrophobia
Contraindication to glycopyrrolate infusion:
Known closed-angle glaucoma known severe prostate hyperplasia
Tachycardia (HR>100 at rest)
Known bladder atony
Cardiac insufficiency or non-congenital pylorus stenosis—verified endoscopically
Known gastroparesis
Contraindications to adenosine:
Second or third degree atrioventricular block
Severe hypotension (blood pressure≤90/50 mm Hg)
Long QT syndrome
Unstable angina pectoris
Decompensated heart failure
Sinus node dysfunction
Chronic obstructive pulmonary disease or asthma bronchiale (forced expiratory volume in one second≤50% of expected)
Allergy towards any of the drugs or diagnostics used in the protocol (insulin, empagliflozin, acipimox, glycopyrrolate, adenosine, gadolinium contrast enhancer)
Any condition, which in the opinion of the investigator, may jeopardise subject safety or compliance with the protocol.
Withdrawal criteria
Subjects may withdraw from the study without any notice or reason
Pregnancy discovered during the experiment
Unacceptable adverse reactions or reactions associated with the planned experiments, including severe glycaemic dysregulation during washout periods
Recruitment
Participants are recruited from the Department of Endocrinology and Cardiology at Hvidovre Hospital and are identified by reviewing laboratory results and patient files. Potential participants will be contacted by means of a recruitment letter, in which they are informed of the opportunity to participate in a scientific research project. We also will advertise for participant in local newspapers and on the internet as well as social media (eg, www.forsøgsperson.dk; www.sundhed.dk and www.facebook.com).
Outcomes
The primary outcome is change in myocardial diastolic function. This was chosen because first, diastole is a highly energy requiring process,11 12 and second, because diastolic dysfunction (with or without LV hypertrophy) is the notable early manifestation of DCM.47 Thus, if changes in overall energy metabolism are to affect cardiac function in patients with T2D, it may well occur in diastole at the earliest. Diastolic cardiac function can be accurately assessed using CMR by measuring LVPFR and LAPEF.48 Our primary outcome measure is change (LVPFRtreatment–LVPFRwashout) in LVPFR (ΔLVPFR). All endpoints are listed in table 1.
Table 1.
Endpoints
| Primary end point | Change in left ventricular peak filling rate (ΔLVPFR) |
| Secondary endpoints | Change in left atrial passive emptying fraction (ΔLAPEF) Change in left ventricular ejection fraction (ΔLVEF) |
| Explorative endpoints include | Cardiovascular: Change in oxygen consumption max and exercise tolerance test variables Change in central blood volume and haematocrite Change in heart rate variability Change in left ventricular volume Metabolic: Basal and postprandial AUC free fatty acids and glycerol turnover Endogenous glucose production and tissue glucose disposal (metabolic clearance of glucose) Fasting and postprandial energy expenditure and respiratory quotient Glucagon–insulin ratio Insulin sensitivity (AUC glucose metabolic clearance/AUC insulin concentration) Beta-cell function (prehepatic insulin secretion rate, correlated to ambient glucose) |
AUC, area under the curve.
Randomisation and intervention
Participants are randomised consecutively by lottery in blocks of 3–5 to treatment with either subcutaneous NPH insulin (Insulatard) two times per day or oral empagliflozin (Jardiance) 25 mg once daily first. All patient will receive both treatments during the trial. Randomisation is performed at V1. NPH insulin is initiated at a dose of 0.2 IU/kg body weight/day and is titrated daily over phone (phone contacts, figure 1) by 0.05 IU/kg body weight/day until average blood glucose (BG) over three consecutive days is within ±1 mmol/L of the individual glycaemic target. In participants randomised to insulin first, the glycaemic target is average fasting and evening glucose concentrations during the second week of empagliflozin run-in. In patients randomised to insulin second, the glycaemic target is average fasting and preprandial evening BG values of week 3 and 4 during the first (empagliflozin) treatment period.
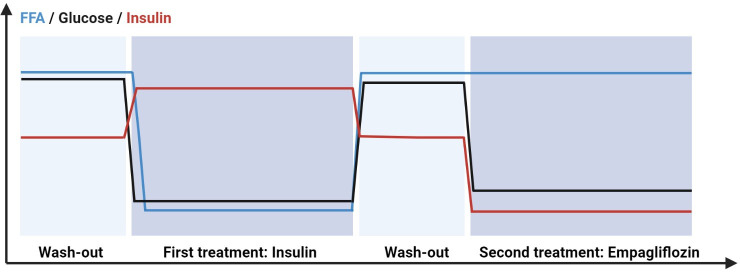
As previously discussed, insulin and empagliflozin represents two metabolically opposing methods for lowering PG concentrations. By titrating insulin treatment to match the glycaemic control found with empagliflozin in the same participants, the result is two distinct metabolic phenotypes: one with hyperinsulinaemia and suppressed levels of FFAs (NPH insulin treatment), and one with reduced insulin levels and increased levels of FFAs (empagliflozin treatment)—but both with the same levels of glycaemic control (figure 2). NPH insulin has been chosen over more modern human insulin analogues, as it is not albumin bound and can be measured in an ordinary insulin assay.
Figure 2.
Metabolic profile of the two study drugs. Schematic representation of the metabolic changes expected with the two study drug treatments in a patient randomised to insulin first. Insulin treatment is characterised by low glucose, low free fatty acids (FFAs) and high insulin concentrations; empagliflozin treatment by low glucose, high FFAs and low insulin.
Safety considerations
During washout periods, blood glucose concentrations will increase—that is a separate point of the study, but severely dysregulated diabetes is an exclusion criterium to ensure participant safety. The risk of severe hyperglycaemia is reduced in several ways in the study:
Existing metformin treatment is continued throughout the whole study as background antiglycaemic treatment.
In case of fasting BG concentrations of more than 13 mmol/L, patients are instructed to contact study personnel.
Phone contacts by study investigator are planned in the second week of washout periods to follow-up on the patient and enquire to hyperglycaemic events or other adverse events.
As soon as the final day (CMR with acipimox) of a washout visit (visit 1 or 3) is completed, antiglycaemic treatment according to study drug sequence is commenced to minimise time spent in hyperglycaemia.
In case of fasting BG>13 mmol/L, the patient will be contacted daily for two additional days. If average fasting BG over the 3 days>13 mmol/L that triggers an extra safety visit, where fasting PG is measured. If PG>13 mmol/L on the day of the extra visit, then the patient is withdrawn from the study and antihyperglycaemic treatment is initiated.
Screening visit (V0)
Once oral and written informed consent is obtained by the study investigator, the screening procedure follows. Medical history is recorded, screening blood samples drawn and an ECG, recording of blood pressure, pulse rate and registration of anthropometric data are performed, and patients are screened according to inclusion and exclusion criteria. A standard transthoracic echocardiography is performed, and oxygen consumption (VO2)max is estimated (table 2).
Table 2.
Screening procedures
| Blood samples | Haematology (haemoglobin, thrombocytes, haematocrit, leucocytes), liver and renal function tests (creatinine, eGFR (Cockroft-Gault formula), alkaline phosphatases, alanine aminotransferases, lactate dehydrogenase, bilirubin, amylase, sodium, potassium), fasting P-glucose, C-peptide, glycated haemoglobin, TSH, urinary albumin/creatinine mass ratio and in fertile women, U-hCG. |
| Echocardiography | Parasternal long axis view, parasternal short axis view at aortic, mitral and apex levels, apical four-chamber view, left ventricular ejection fraction (LVEF), E/E’, E’, LVEDV/BSA. |
| Estimation of oxygen consumption (VO2)max | Maximum oxygen uptake is estimated using Åstrøm’s two-point test performed on a cycle ergometer during indirect calorimetry. From measurements of VO2 at two submaximal pulse rates VO2max is estimated by linear extrapolation to the theoretical maximal pulse rate (220-age)67 |
Study visits
All study visits consist of three study days—a metabolic study day and two CMR study days (table 3).
Table 3.
Visit overview
| Metabolic study day | Cardiac MRI (CMR) | Cardiac MRI, acipimox |
|
|
|
The metabolic study day
The metabolic study is conducted at the Department of Endocrinology, Hvidovre Hospital, to document the metabolic effects of each study drug.
Participants meet in the morning after an overnight fast. Anthropometric data, blood pressure, pulse rate and an ECG are recorded, and two catheters, one in each arm are inserted for infusion of tracers and for repeated drawing of arterialised blood samples, respectively. Baseline and safety blood samples are taken (table 4), the participant empties bladder and the investigational drug (V2, V4) and the participants’ usual medications are administered at 08:00 hours. Body composition is determined by dual energy X-ray absorptiometry scan.
Table 4.
Blood samples on metabolic and cardiac MRI (CMR) study days include
| Metabolic study day | Blood samples: glucose, insulin, C-peptide, glucagon, free fatty acids (FFAs), triglycerides, total amino acids and ketone bodies (beta-hydroxybuturate), tracers/tracees, gut hormones Glycated haemoglobin, urate, blood urea nitrogen, cortisol are sampled at baseline |
| CMR | Markers of cardiac function, including pro-atrial natriuretic pepetide (pro-ANP) and pro-brain natriuretic peptide (pro-BNP), glucose, insulin, C-peptide, glucagon, FFAs, triglycerides, ketone bodies, haematocrit are drawn before and after CMR. |
Basal metabolism
Primed infusions of stable glucose ([6,6-D2]-glucose) and glycerol ([1,1,2,3,3-D5]-glycerol) tracers are initiated (T=−180 min). Blood is sampled at −30 to –15 and −2 min to characterise glucose, lipid and amino acid metabolism. The patient empties bladder, urine is weighed and samples are taken for determination of tracer concentrations and urinary nitrogen excretion, and the 5-hour oral glucose tolerance test (OGTT) is initiated.
Five-hour OGTT
The patient ingests anhydrous glucose (72 g) with added [U-13C6]-glucose tracer (3 g) dissolved in 250 mL of water over 5 min (T=0 min). Intravenous tracer infusions continue unchanged. Blood is sampled regularly for 5 hours for characterisation of postprandial glucose, lipid and amino acid metabolism (tables 3 and 4). The patient empties bladder regularly during and at the end of the OGTT. Urine is sampled for nitrogen excretion and tracers/tracees.
Fat and muscle biopsies: biopsies are obtained during the basal (T=−60 min) and the maximally insulin stimulated (T=60 min) state. Muscle biopsies are considered proxies for cardiomyocyte metabolic status. Overall, 30 min ventilated hood indirect calorimetry (Vyaire Vyntus CPX) is performed during the basal period (prior to biopsies) t= −90 min and postprandially at t=60 min for determination of fasting and postprandial energy expenditure and respiratory quotient.
Exercise test (50% VO2max)
At T=300 min, the participant is exercised at 60 W for 4 min after which work load is increased until oxygen consumption is 50% of estimated VO2max. Pulse rate is recorded with a chest mounted pulse rate monitor and oxygen consumption with a mask mounted indirect calorimeter. Blood is sampled to characterise glucose, lipid and amino acid metabolism (tables 3 and 4). After 30 min, VO2max is estimated by increasing workload by 50 W until a pulse rate increase of 30. When the pulse is steady for 2 min, oxygen consumption and pulse rate are recorded, and the test is stopped. VO2max is estimated by linear extrapolation to the theoretical maximum pulse rate (220-age).
Ad libitum meal test
SGLT2 inhibition is associated with a lower weight reduction than predicted from the urinary energy loss. SGLT2 inhibition does not change resting energy expenditure or blunt the thermogenic effect of feeding, suggesting that energy intake is increased.28 Therefore, the metabolic study day is ended with an ad libitum meal, consisting of thoroughly mixed pasta bolognese (fixed nutrient composition and energy content). Patients are placed in a quiet corner and instructed to eat until full. Two glasses of water (total 300 mL) are allowed with the meal. The meal is weighed before and after serving and ad libitum meal intake defined as the difference. Throughout the day, patients are asked to score their hunger, satiety and sensation of fullness on a visual analogue scale.49
Cardiac evaluation
Two CMR days are performed during each visit (V1–V4). In addition, diurnal blood pressure and Holter monitoring are performed. CMR is conducted at the Department of Cardiology, Rigshospitalet, Copenhagen, whereas Holter monitoring and diurnal blood pressure monitoring are performed at the Department of Cardiology, Hvidovre Hospital.
Participants meet fasting and morning medication, including investigational medicinal product (V2 and V4), is administered. Anthropometric data are recorded, and two intravenous catheters are inserted into an antecubital and the contralateral dorsal hand vein for infusion of adenosine, gadolinium contrast and glycopyrrolate and for blood sampling respectively (table 4). Prior to CMR, a transthoracic echocardiography is performed (table 2)
CMR is performed on a 1.5 Tesla scanner (Siemens Aera; Siemens; Erlangen; Germany) with the patient lying supine on the back, using an 18-channel cardiac coil with continuous ECG gating.
Cine 2-chamber, 3-chamber and 4-chamber images, complete transverse and short axis cine stacks covering the whole heart are acquired. All images are obtained during end expiratory breath holds.
Myocardial perfusion images during rest and stress are obtained at the basal, mid-ventricular and apical cardiac short-axis level. Rest perfusion images of the myocardium are acquired using an intravenous bolus of gadolinium contrast (Gadovist, Bayer AG, Germany) 0.075 mmol/kg bodyweight. The time of gadolinium contrast entry into the right and the left ventricle is accurately determined, and this transit time of gadovist multiplied by cardiac output is used to calculate the pulmonary and central (pulmonary+cardiac) blood volume.
Myocardial stress perfusion images are obtained with an intravenous dose of 0.075 mmol/kg of gadovist during and 10 min after an intravenous adenosine (140 µg/min) administrated for maximum 4 min). This is followed by evaluation of cardiac function during chronotropic stress, where short axis cine stack will be reacquired 10 min after the administration of intravenous glycopyrrolate (4 µg/kg, max. 400 µg, given as a bolus). This approach has been shown to unmasque subclinical diastolic dysfunction as has been demonstrated in normal healthy elderly.48
Cardiac MRI, acipimox
CMR scans will follow the same procedure as described above, but participants are instructed to ingest 250 mg acipimox two times per day, 4 hours before and right before the scan, to determine myocardial function. This repeated administration of acipimox is required for adequate suppression of hormone sensitive lipase activity and depletion of plasma FFAs.50 This has been shown to gradually impair cardiac function,42 and is done to disclose any coupling between FFA availability and cardiac function.
CMR image analysis
It is performed using Circle42 (Circle Cardiovascular Imaging, Calgary Canada, V.5.5.1). LV volumes, LV mass, LVEF and LVPFR are determined by tracing of the endocardial and epicardial contours in end-diastolic and end-systolic phases. The papillary muscles are excluded from the myocardium. On native and postcontrast T1-mappings, endocardial and epicardial borders are traced, and the mean extracellular volume (ECV) is calculated from areas outside late gadolinium enhancement (LGE) lesions. For determination of the ECV within an LGE lesion, myocardium without LGE in the segment is excluded. Myocardial perfusion scans are inspected for perfusion defects. Regions with infarctions, subendocardial perfusion defects or dark-rim artefacts will be excluded. Blinded to clinical data, the analyses will be reviewed and finalised by two CMR specialists.
Diurnal blood pressure and Holter monitoring
Between study days during each visit, diurnal blood pressure is recorded (ScottCare, ABP 320, Cleveland, Ohio, USA) for 24 hours with 15 min intervals between 6:00 and 22:00 and 60 min intervals during night-time. Cardiac rhythm is evaluated with Holter monitoring (SCOTTCARE, CHROMA, model RZ153C, Cleveland, Ohio, USA) for 48 hours.
Patient and public involvement
No patient involved.
Analyses
Blood and tissue samples
Subcutaneous fat and muscle biopsies: local analgesia is applied before sampling with a Bergströms cannula. Samples are immediately frozen in liquid nitrogen and stored at −80°C. Blood and urine samples: samples are spun, aliquoted and stored at –20°C (GLP-1, PYY, Glucagon) or –80°C for later analysis. Bedside PG measurements are performed using the glucose oxidase technique (YSI model 2300 STAT Plus; YSI, Yellow Springs, Ohio, USA). Home blood glucose measurements are carried out on Contour XT (Ascensia Diabetes Care Holdings AG, Basel, Switzerland). Safety blood and urine samples are analysed on the same day at the Department of Clinical Biochemistry, Hvidovre Hospital.
Statistical methods
Sample size calculation
Measures of myocardial function are highly reproducible when assessed using CMR, and interstudy and cohort coefficients of variation are in the range of 3%–5%51–53
Using the same CMR protocol as the present, Ahtarovski et al found a mean difference of 92 mL/s in LVPFR between healthy young (585±62 mL/s) and healthy elderly subjects (493±55 mL/s).53 We assume that patients with T2D have LVPFR corresponding to healthy elderly subjects, and we assume that empagliflozin treatment improves LVPFR by 30 mL/s (ΔLVPFR=30 mL/s) from baseline and that insulin treatment does not improve LVPFR (ΔLVPFR=0 mL/s).
Conservatively, setting the SD of between treatment differences of ΔLVPFR at 30 mL/s, a number of 20 patients would be adequate to determine a 30 mL/s difference between the two treatments with a power of 93% and a two-sided significance level of 0.01, when evaluating data with the paired student’s t-test. In case of a 20% dropout rate, power would still be acceptable (83%, p=0.01).
Statistical analysis plan
The primary and secondary endpoints are analysed assuming no period effect or treatment–period interaction. This assumption is reasonable, given results from similar studies, where no such interactions or effects have been reported.54 Normally distributed data are presented using standard descriptive statistics, and reported as mean (SD) for normally distributed and median (Q1;Q3) for non-normally distributed data. Likewise, comparisons of normally distributed data are done using the paired Student’s t-test for all completers, whereas Wilcoxon’s paired signed rank test will be used if data are non-normally distributed.
Timeframe
Screenings are performed from January 2018. Last patient, last visit is expected second half of 2021 after which the study will be unregistered with the Danish Medicines Agency and the Capital Region Municipal Ethical Committee within 90 days. Data analyses are expected to be completed by Winter 2022. No later than 12 months after unregistering of the study, will results be made publicly available (www.clinicalregister.eu). Trial registration number: EudraCT: 2017-002101.
Ethics and dissemination
The study is conducted according to ICH GCP guidelines E6 (R2) and the Declaration of Helsinki and all participants will provide oral and written informed consent. The study is approved by the Danish Medicines Agency (ref. id: 2017061587), The Capital Region Ethical Committee (H-17018846) and the Danish Data Protection Agency (AHH-2017-093). Our results, regardless of outcome, will be published in relevant scientific journals. In addition, we will seek to disseminate results through presentations at scientific meetings. Publication will take place as soon as scientifically feasible.
Discussion
The profound and swift benefits of SGLT2i on cardiovascular risk in T2D have inspired the discussion of metabolism and its importance for cardiac function in patients with T2D.37 39 55–57 Especially since, SGLT2 inhibitors have metabolic effects that by and large are opposite to those of insulin treatment. Thus, insulin treatment is associated with increased tissue glucose uptake and utilisation, but suppression of lipid mobilisation and oxidation as well as lowering of plasma concentrations of ketone bodies.58 SGLT2 inhibitors increase lipid mobilisation and oxidation, increase plasma ketone body concentrations and reduce tissue glucose uptake.28 29 Both treatments lower PG, but insulin treatment increases, whereas SGLT2i treatment decreases plasma insulin concentrations. Whether such changes in metabolism affect cardiac function, is still unsettled, but forcing cardiac glucose uptake and utilisation through insulin treatment has been suggested by some to benefit and by others to impair cardiac function,45 59–62 while yet others have suggested increased lipid and ketone body oxidation to be important for proper cardiac function in T2D.37 44 62 Studies on SGLT2i treatments and the effects on cardiac function are beginning to emerge. In a recent study, 42 patients with T2D were randomised to 12 weeks of empagliflozin 10 mg or placebo once daily. SGLT2 inhibition was shown to rapidly improve diastolic cardiac function as evaluated with echocardiography.63 In a placebo-controlled crossover design, after 4 weeks of empagliflozin treatment in patients with T2D, myocardial glucose uptake was reduced and fatty acid oxidation unaltered, but this did not significantly change myocardial oxygen consumption or cardiac efficiency, nor any measure of cardiac function.36 In a Swedish study, 6-week dapagliflozin treatment showed unchanged cardiac fatty acid uptake, a trend towards reduced left atrial maximal volume, and reduced LV oxygen consumption and external work compared with placebo,64 and in the only study found, where an active comparator was used, 10 mg empagliflozin once daily for 12 weeks did not change cardiac lipid accumulation (as measured by MRI spectrometry), cardiac function or cardiac metabolism compared with sitagliptin 50 mg daily.65
In conclusion, existing studies in humans have shown divergent results regarding changes in cardiac diastolic function with little changes in cardiac metabolism. However, most studies have compared cardiac effects of SGLT2i to placebo, thus not accounting for the circumstances that characterised the EMPA-REG trial, where antiglycaemic treatment was intensified in the placebo group concurrently.25 Thus, the CVD risk benefits of the study may have arisen from unfavourable metabolic consequences of the treatment in the placebo arm. In the one study with an active comparator empagliflozin was compared with sitagliptin, which not only affects the incretin system but also has less specific metabolic effect.66 Therefore, to date, our study is the one to most directly pursue the coupling between metabolism and cardiac function, by choosing insulin as the comparator, and by including the effects of acute lowering of FFA concentrations in plasma on cardiac function.
bmjopen-2021-054100supp001.pdf (38.4KB, pdf)
Supplementary Material
Footnotes
Contributors: RT conducted the study, collected all the data, performed data analyses and cosubmit the study. EAR contributed to the study design, designed the keton body and biopsy analysis scheme and performed these analyses. JPG designed the pro-ANP and pro-BNP analysis scheme and performed these analyses. MF designed multiple metabolic analysis schemes (triglycerides, insulin, free fatty acids, uric acid, urea and nitrogen) and performed these analyses. GVH designed the three-tracer measuring analysis schemes we are using in this study and performed these analyses. UD provided the study with analysis tools (Holter monitors and blood pressure monitors). He performed the analyses of these data. JJH participated in the protocol design, designed multiple metabolic analyses (GLP-1, glucagon and PYY) and performed the analyses of these data. SM is the principal investigator, coplanned the study and contributed with several analysing tools. NV codesigned the cardiac MRI guideline for the study and contributed with analysing tool (MRI scanner). PLM coplanned the study, codesigned the cardiac MRI guideline for the study and analysed the cardiac MRI data. NBJ coplanned the study, performd all data analyses with RT and cosubmit the study. All of the authors contributed with writing, revising and approving this manuscript.
Funding: The study is funded by an investigator-initiated study grant from Boehringer Ingelheim. Additional funding comes from Grosserer L. F. Foghts Fond, Charlottenlund, Denmark. Grant numbers not applicable.
Competing interests: SM and NBJ have received research grants from Boehringer Ingelheim and JJH serves on advisory boards for Novo Nordisk.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Defronzo RA. Banting lecture. from the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009;58:773–95. 10.2337/db09-9028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Vegt F, Dekker JM, Ruhé HG, et al. Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn study. Diabetologia 1999;42:926–31. 10.1007/s001250051249 [DOI] [PubMed] [Google Scholar]
- 3.Pyörälä M, Miettinen H, Laakso M, et al. Plasma insulin and all-cause, cardiovascular, and noncardiovascular mortality: the 22-year follow-up results of the Helsinki Policemen study. Diabetes Care 2000;23:1097–102. 10.2337/diacare.23.8.1097 [DOI] [PubMed] [Google Scholar]
- 4.Lakka HM, Lakka TA, Tuomilehto J, et al. Hyperinsulinemia and the risk of cardiovascular death and acute coronary and cerebrovascular events in men: the Kuopio ischaemic heart disease risk factor study. Arch Intern Med 2000;160:1160–8. 10.1001/archinte.160.8.1160 [DOI] [PubMed] [Google Scholar]
- 5.Selvin E, Marinopoulos S, Berkenblit G, et al. Meta-Analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med 2004;141:421–31. 10.7326/0003-4819-141-6-200409210-00007 [DOI] [PubMed] [Google Scholar]
- 6.Redfield MM, Jacobsen SJ, Burnett JC, et al. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 2003;289:194–202. 10.1001/jama.289.2.194 [DOI] [PubMed] [Google Scholar]
- 7.Boyer JK, Thanigaraj S, Schechtman KB, et al. Prevalence of ventricular diastolic dysfunction in asymptomatic, normotensive patients with diabetes mellitus. Am J Cardiol 2004;93:870–5. 10.1016/j.amjcard.2003.12.026 [DOI] [PubMed] [Google Scholar]
- 8.Jørgensen PG, Biering-Sørensen T, Mogelvang R, et al. Predictive value of echocardiography in type 2 diabetes. Eur Heart J Cardiovasc Imaging 2019;20:687–93. 10.1093/ehjci/jey164 [DOI] [PubMed] [Google Scholar]
- 9.Tarquini R, Lazzeri C, Pala L, et al. The diabetic cardiomyopathy. Acta Diabetol 2011;48:173–81. 10.1007/s00592-010-0180-x [DOI] [PubMed] [Google Scholar]
- 10.Komi S, Inoue Y, Hata H, et al. Cardiovascular magnetic resonance evaluation of left ventricular peak filling rate using steady-state free precession and phase contrast sequences. Springerplus 2016;5:1163. 10.1186/s40064-016-2878-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diamant M, Lamb HJ, Groeneveld Y, et al. Diastolic dysfunction is associated with altered myocardial metabolism in asymptomatic normotensive patients with well-controlled type 2 diabetes mellitus. J Am Coll Cardiol 2003;42:328–35. 10.1016/s0735-1097(03)00625-9 [DOI] [PubMed] [Google Scholar]
- 12.Rosano G, Coats A. Modulation of cardiac metabolism in heart failure. ICFJ 2019;17:99–103. 10.17987/icfj.v17i0.597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ungar I, Gilbert M, Siegel A, et al. Studies on myocardial metabolism. IV. myocardial metabolism in diabetes. Am J Med 1955;18:385–96. 10.1016/0002-9343(55)90218-7 [DOI] [PubMed] [Google Scholar]
- 14.Rijzewijk LJ, van der Meer RW, Lamb HJ, et al. Altered myocardial substrate metabolism and decreased diastolic function in nonischemic human diabetic cardiomyopathy: studies with cardiac positron emission tomography and magnetic resonance imaging. J Am Coll Cardiol 2009;54:1524–32. 10.1016/j.jacc.2009.04.074 [DOI] [PubMed] [Google Scholar]
- 15.Stanley WC, Lopaschuk GD, Hall JL, et al. Regulation of myocardial carbohydrate metabolism under normal and ischaemic conditions. potential for pharmacological interventions. Cardiovasc Res 1997;33:243–57. 10.1016/s0008-6363(96)00245-3 [DOI] [PubMed] [Google Scholar]
- 16.Mehta SR, Yusuf S, Díaz R, et al. Effect of glucose-insulin-potassium infusion on mortality in patients with acute ST-segment elevation myocardial infarction: the CREATE-ECLA randomized controlled trial. JAMA 2005;293:437–46. 10.1001/jama.293.4.437 [DOI] [PubMed] [Google Scholar]
- 17.Malmberg K, Rydén L, Wedel H, et al. Intense metabolic control by means of insulin in patients with diabetes mellitus and acute myocardial infarction (DIGAMI 2): effects on mortality and morbidity. Eur Heart J 2005;26:650–61. 10.1093/eurheartj/ehi199 [DOI] [PubMed] [Google Scholar]
- 18.Malmberg K, Rydén L, Efendic S, et al. Randomized trial of insulin-glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year. J Am Coll Cardiol 1995;26:57–65. 10.1016/0735-1097(95)00126-k [DOI] [PubMed] [Google Scholar]
- 19.NICE-SUGAR Study Investigators, Finfer S, Chittock DR, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med 2009;360:1283–97. 10.1056/NEJMoa0810625 [DOI] [PubMed] [Google Scholar]
- 20.Hemmingsen B, Lund SS, Gluud C, et al. Intensive glycaemic control for patients with type 2 diabetes: systematic review with meta-analysis and trial sequential analysis of randomised clinical trials. BMJ 2011;343:d6898. 10.1136/bmj.d6898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129–39. 10.1056/NEJMoa0808431 [DOI] [PubMed] [Google Scholar]
- 22.ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–72. 10.1056/NEJMoa0802987 [DOI] [PubMed] [Google Scholar]
- 23.ORIGIN Trial Investigators, Gerstein HC, Bosch J, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med 2012;367:319–28. 10.1056/NEJMoa1203858 [DOI] [PubMed] [Google Scholar]
- 24.Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–59. 10.1056/NEJMoa0802743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117–28. 10.1056/NEJMoa1504720 [DOI] [PubMed] [Google Scholar]
- 26.McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 2019;381:1995–2008. 10.1056/NEJMoa1911303 [DOI] [PubMed] [Google Scholar]
- 27.Zou C-Y, Liu X-K, Sang Y-Q, et al. Effects of SGLT2 inhibitors on cardiovascular outcomes and mortality in type 2 diabetes. Medicine 2019;98:e18245. 10.1097/MD.0000000000018245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ferrannini E, Muscelli E, Frascerra S, et al. Metabolic response to sodium-glucose cotransporter 2 inhibition in type 2 diabetic patients. J Clin Invest 2014;124:499–508. 10.1172/JCI72227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merovci A, Solis-Herrera C, Daniele G, et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest 2014;124:509–14. 10.1172/JCI70704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferrannini E, Baldi S, Frascerra S, et al. Renal handling of ketones in response to Sodium–Glucose cotransporter 2 inhibition in patients with type 2 diabetes. Diabetes Care 2017;40:771–6. 10.2337/dc16-2724 [DOI] [PubMed] [Google Scholar]
- 31.Chilton R, Tikkanen I, Cannon CP, et al. Effects of empagliflozin on blood pressure and markers of arterial stiffness and vascular resistance in patients with type 2 diabetes. Diabetes Obes Metab 2015;17:1180–93. 10.1111/dom.12572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Trum M, Riechel J, Lebek S, et al. Empagliflozin inhibits Na+ /H+ exchanger activity in human atrial cardiomyocytes. ESC Heart Fail 2020;7:4429–37. 10.1002/ehf2.13024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baartscheer A, Schumacher CA, Wüst RCI, et al. Empagliflozin decreases myocardial cytoplasmic Na+ through inhibition of the cardiac Na+/H+ exchanger in rats and rabbits. Diabetologia 2017;60:568–73. 10.1007/s00125-016-4134-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garvey WT, Van Gaal L, Leiter LA, et al. Effects of canagliflozin versus glimepiride on adipokines and inflammatory biomarkers in type 2 diabetes. Metabolism 2018;85:32–7. 10.1016/j.metabol.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 35.Heerspink HJL, Perco P, Mulder S, et al. Canagliflozin reduces inflammation and fibrosis biomarkers: a potential mechanism of action for beneficial effects of SGLT2 inhibitors in diabetic kidney disease. Diabetologia 2019;62:1154–66. 10.1007/s00125-019-4859-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lauritsen KM, Nielsen BRR, Tolbod LP, et al. Sglt2 inhibition does not affect myocardial fatty acid oxidation or uptake, but reduces myocardial glucose uptake and blood flow in individuals with type 2 diabetes: a randomized double-blind, placebo-controlled crossover trial. Diabetes 2021;70:800–8. 10.2337/db20-0921 [DOI] [PubMed] [Google Scholar]
- 37.Jørgensen NB, Pedersen J, Vaag AA. EMPA-REG: Glucose excretion and lipid mobilization - not storage - saves lives. J Diabetes Complications 2016;30:753. 10.1016/j.jdiacomp.2016.02.015 [DOI] [PubMed] [Google Scholar]
- 38.Ekanayake P, Hupfeld C, Mudaliar S. Sodium-Glucose cotransporter type 2 (SGLT-2) inhibitors and ketogenesis: the good and the bad. Curr Diab Rep 2020;20:74. 10.1007/s11892-020-01359-z [DOI] [PubMed] [Google Scholar]
- 39.Ferrannini E, Mark M, Mayoux E. CV Protection in the EMPA-REG OUTCOME Trial: A "Thrifty Substrate" Hypothesis. Diabetes Care 2016;39:1108–14. 10.2337/dc16-0330 [DOI] [PubMed] [Google Scholar]
- 40.Nielsen R, Møller N, Gormsen LC, et al. Cardiovascular effects of treatment with the ketone body 3-hydroxybutyrate in chronic heart failure patients. Circulation 2019;139:2129–41. 10.1161/CIRCULATIONAHA.118.036459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Santos-Gallego CG, Requena-Ibanez JA, San Antonio R, et al. Empagliflozin Ameliorates Adverse Left Ventricular Remodeling in Nondiabetic Heart Failure by Enhancing Myocardial Energetics. J Am Coll Cardiol 2019;73:1931–44. 10.1016/j.jacc.2019.01.056 [DOI] [PubMed] [Google Scholar]
- 42.Wolf P, Winhofer Y, Krssak M, et al. Suppression of plasma free fatty acids reduces myocardial lipid content and systolic function in type 2 diabetes. Nutr Metab Cardiovasc Dis 2016;26:387–92. 10.1016/j.numecd.2016.03.012 [DOI] [PubMed] [Google Scholar]
- 43.Tuunanen H, Engblom E, Naum A, et al. Free fatty acid depletion acutely decreases cardiac work and efficiency in cardiomyopathic heart failure. Circulation 2006;114:2130–7. 10.1161/CIRCULATIONAHA.106.645184 [DOI] [PubMed] [Google Scholar]
- 44.Harmancey R, Vasquez HG, Guthrie PH, et al. Decreased long-chain fatty acid oxidation impairs postischemic recovery of the insulin-resistant rat heart. Faseb J 2013;27:3966–78. 10.1096/fj.13-234914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harmancey R, Lam TN, Lubrano GM, et al. Insulin resistance improves metabolic and contractile efficiency in stressed rat heart. Faseb J 2012;26:3118–26. 10.1096/fj.12-208991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zinman B, Inzucchi SE, Lachin JM, et al. Rationale, design, and baseline characteristics of a randomized, placebo-controlled cardiovascular outcome trial of empagliflozin (EMPA-REG OUTCOME™). Cardiovasc Diabetol 2014;13:102. 10.1186/1475-2840-13-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li N, Zhou H. Sglt2 inhibitors: a novel player in the treatment and prevention of diabetic cardiomyopathy. Drug Des Devel Ther 2020;14:4775–88. 10.2147/DDDT.S269514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ahtarovski KA, Iversen KK, Lønborg JT, et al. Left atrial and ventricular function during dobutamine and glycopyrrolate stress in healthy young and elderly as evaluated by cardiac magnetic resonance. Am J Physiol Heart Circ Physiol 2012;303:H1469–73. 10.1152/ajpheart.00365.2012 [DOI] [PubMed] [Google Scholar]
- 49.Flint A, Raben A, Blundell JE, et al. Reproducibility, power and validity of visual analogue scales in assessment of appetite sensations in single test meal studies. Int J Obes Relat Metab Disord 2000;24:38–48. 10.1038/sj.ijo.0801083 [DOI] [PubMed] [Google Scholar]
- 50.Worm D, Henriksen JE, Vaag A, et al. Pronounced blood glucose-lowering effect of the antilipolytic drug acipimox in noninsulin-dependent diabetes mellitus patients during a 3-day intensified treatment period. J Clin Endocrinol Metab 1994;78:717–21. 10.1210/jcem.78.3.8126147 [DOI] [PubMed] [Google Scholar]
- 51.Grothues F, Smith GC, Moon JCC, et al. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol 2002;90:29–34. 10.1016/s0002-9149(02)02381-0 [DOI] [PubMed] [Google Scholar]
- 52.Morton G, Jogiya R, Plein S, et al. Quantitative cardiovascular magnetic resonance perfusion imaging: inter-study reproducibility. Eur Heart J Cardiovasc Imaging 2012;13:954–60. 10.1093/ehjci/jes103 [DOI] [PubMed] [Google Scholar]
- 53.Ahtarovski KA, Iversen KK, Lønborg JT, et al. Left atrial and ventricular function during dobutamine and glycopyrrolate stress in healthy young and elderly as evaluated by cardiac magnetic resonance. Am J Physiol Heart Circ Physiol 2012;303:H1469–73. 10.1152/ajpheart.00365.2012 [DOI] [PubMed] [Google Scholar]
- 54.Kumarathurai P, Anholm C, Larsen BS, et al. Effects of liraglutide on heart rate and heart rate variability: a randomized, double-blind, placebo-controlled crossover study. Diabetes Care 2017;40:117–24. 10.2337/dc16-1580 [DOI] [PubMed] [Google Scholar]
- 55.The Lancet Diabetes Endocrinology . Getting to the heart of the matter in type 2 diabetes. Lancet Diabetes Endocrinol 2015;3:827. 10.1016/S2213-8587(15)00384-8 [DOI] [PubMed] [Google Scholar]
- 56.DeFronzo RA. The EMPA-REG study: what has it told us? A diabetologist's perspective. J Diabetes Complications 2016;30:1–2. 10.1016/j.jdiacomp.2015.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nirengi S, Peres Valgas da Silva C, Stanford KI. Disruption of energy utilization in diabetic cardiomyopathy; a mini review. Curr Opin Pharmacol 2020;54:82–90. 10.1016/j.coph.2020.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Defronzo RA, Lecture B. Banting lecture. from the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009;58:773–95. 10.2337/db09-9028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stanley WC, Lopaschuk GD, McCormack JG. Regulation of energy substrate metabolism in the diabetic heart. Cardiovasc Res 1997;34:25–33. 10.1016/s0008-6363(97)00047-3 [DOI] [PubMed] [Google Scholar]
- 60.Taegtmeyer H, Beauloye C, Harmancey R, et al. Comment on Nolan et al. Insulin Resistance as a Physiological Defense Against Metabolic Stress: Implications for the Management of Subsets of Type 2 Diabetes. Diabetes 2015;64:673-686. Diabetes 2015;64:e37. 10.2337/db15-0655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nolan CJ, Ruderman NB, Kahn SE, et al. Insulin resistance as a physiological defense against metabolic stress: implications for the management of subsets of type 2 diabetes. Diabetes 2015;64:673–86. 10.2337/db14-0694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Taegtmeyer H, Beauloye C, Harmancey R, et al. Insulin resistance protects the heart from fuel overload in dysregulated metabolic states. Am J Physiol Heart Circ Physiol 2013;305:H1693–7. 10.1152/ajpheart.00854.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rau M, Thiele K, Hartmann N-UK, et al. Empagliflozin does not change cardiac index nor systemic vascular resistance but rapidly improves left ventricular filling pressure in patients with type 2 diabetes: a randomized controlled study. Cardiovasc Diabetol 2021;20:6. 10.1186/s12933-020-01175-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Oldgren J, Laurila S, Åkerblom A, et al. Effects of 6 weeks of treatment with dapagliflozin, a sodium-glucose co-transporter-2 inhibitor, on myocardial function and metabolism in patients with type 2 diabetes: A randomized, placebo-controlled, exploratory study. Diabetes Obes Metab 2021;23:1505–17. 10.1111/dom.14363 [DOI] [PubMed] [Google Scholar]
- 65.Hiruma S, Shigiyama F, Hisatake S, et al. A prospective randomized study comparing effects of empagliflozin to sitagliptin on cardiac fat accumulation, cardiac function, and cardiac metabolism in patients with early-stage type 2 diabetes: the asset study. Cardiovasc Diabetol 2021;20:32. 10.1186/s12933-021-01228-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Deacon CF. A review of dipeptidyl peptidase-4 inhibitors. hot topics from randomized controlled trials. Diabetes Obes Metab 2018;20 Suppl 1:34–46. 10.1111/dom.13135 [DOI] [PubMed] [Google Scholar]
- 67.Nordsborg N, Timmerman M. Testmanual - patientinterview og konditionstest. 2.0. København. Sundhedsstyrelsen, 2006. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-054100supp001.pdf (38.4KB, pdf)