Abstract
Background:
Using alternating orthogonal suture throws with the looped whipstitch technique may allow enhanced suture fixation.
Hypothesis:
It was hypothesized that this novel multiplanar, perpendicular looped whipstitch (MP) technique would have improved biomechanical properties compared with the standard looped whipstitch (WS) and Krackow stitch (KS).
Study Design:
Controlled laboratory study.
Methods:
A total of 30 cadaveric tibialis anterior tendons were randomly assigned into 3 groups of 10. Tendons were secured to a custom clamp, and the other end was sutured using 1 of 3 techniques: the KS, WS, or novel MP. The MP was performed with alternating orthogonal throws starting right to left, then front to back, left to right, and back to front. Each technique used 4 passes of No. 2 FiberWire spaced 5 mm apart and ending 10 mm from the tendon end. Tendons were preloaded to 5 N, pretensioned to 50 N at 100 mm/min for 3 cycles, returned to 5 N for 1 minute, cycled from 5 to 100 N at 200 mm/min for 100 cycles, and then loaded to failure at 20 mm/min. Elongation was recorded after pretensioning and cycling and was measured both across the suture-tendon interface and from the base of the suture-tendon interface to markings on the suture limbs (construct elongation). One-way analyses of variance were performed, with Bonferroni post hoc analysis when appropriate.
Results:
There were no differences in cross-sectional area or stiffness among the 3 techniques. The ultimate load for WS (183.33 ± 57.44 N) was less compared with both MP (270.76 ± 39.36 N) and KS (298.90 ± 25.94 N) (P ≤ .001 for both). There was less construct elongation for KS compared with WS and MP for total displacement, measured from pretensioning to the end of cycling (P < .001). All 3 techniques saw a decrease in length (shortening) at the suture-tendon interface during testing. There was more shortening at the suture-tendon interface for WS compared with KS (P = .006).
Conclusion:
The KS appears superior, as it maximized strength while minimizing construct elongation or graft shortening. The ultimate load of the MP technique was greater than that of the standard technique but not significantly different from that of the KS technique.
Clinical Relevance:
The KS is preferred. If using a WS, multiplanar, perpendicular passes should be considered.
Keywords: whipstitch, Krackow, biomechanics, tendon, ultimate failure load, fatigue testing
Successful soft tissue suture repair and reconstruction relies on secure and stable fixation. This is necessary for early initiation of rehabilitation that may improve outcomes 12,15 and the stability of the construct during the healing phase. Although numerous soft tissue suture techniques have been described, 2 more commonly used techniques are the Krackow stitch (KS) and looped commercial whipstitch (WS). The KS is a locking stitch originally designed as an alternative to an in-bone staple fixation. 14 It has been shown to be widely successful in multiple soft tissue repair and reconstruction techniques, including the Achilles, ulnar collateral ligament, distal biceps, quadriceps, and patellar tendons. 2,6,13,24 More recently, predesigned looped sutures have been developed to assist in graft preparation and soft tissue repairs. The commercial whipstitch is a nonlocking looped suture developed to reduce graft preparation time, increase strength, and allow for ease of intraoperative adjustments. The WS may also benefit from an overall reduction in multiple needle passes, which may weaken the tendon strength. 19,23 There does appear to be an anecdotal gain in popularity in looped whipstitch use because of these proposed benefits and perceived improved efficiency.
The biomechanical properties of both the WS and KS have been extensively compared. Some investigators have found the 2 techniques to have a similar force to ultimate failure, 3,7,8 while others have reported that the KS is significantly stronger than the WS. 1,20 The KS has also been shown by some to reduce elongation compared with the looped whipstitch, 3,20 while others have reported that the KS reduced gap formation but increased elongation. 7
Using alternating orthogonal suture throws with the WS technique may allow enhanced fixation. McKeon et al 17 found a significant increase in load to failure by adding a second interlocking KS perpendicularly, and the secondary plane of fixation likely attributed to the increase in load to failure. Furthermore, a comparison of 3 different double KS techniques found that the technique with a second stitch passed orthogonally had significantly less elongation with cyclic loading, although there was no difference in load to failure. 9
Despite evidence of improved strength with perpendicular fixation, as well as extensive biomechanical analyses of different suture techniques, to our knowledge, no investigation has been performed directly comparing the traditional KS and standard WS suturing techniques with a multiplanar, perpendicular looped whipstitch (MP) technique. We hypothesized that a looped whipstitch suture passed with alternating orthogonal throws would result in less elongation, a higher ultimate load and yield load, greater stiffness, and a different mode of failure than either the WS or the KS.
The purpose of our study was to biomechanically evaluate a novel MP by comparing the elongation, ultimate load, yield load, stiffness, and method of failure with those of the WS and KS.
Methods
Three suture configurations were evaluated using cadaveric tibialis anterior tendons (RTI Surgical) that were frozen and stored at –20°C and thawed for 1 hour at room temperature before use. Visual inspection was performed to ensure that no tendon demonstrated signs of degenerative or pathologic changes. Thirty tendons were randomly assigned into 3 study groups to minimize any variability due to variation in tendon size. We performed a power analysis using load-to-failure data derived from Hong et al, 9 which revealed that 3 groups of 10, for a total of 30 specimens, with alpha = .05 and beta = 0.80, would result in an effect size of 0.60. Furthermore, similar studies found a sample size of 10 to be sufficient to detect differences. 9,10
Tendon Preparation, Suture Techniques, and Setup
Each tendon was cut to 16 cm, and a mark was made every 5 mm to indicate the location of suture passage beginning from the more circular end of the tendon and ending at 25 mm. All suturing was performed by the same sports medicine fellowship-trained orthopaedic surgeon (D.P.P.). Tendon circumference, width, and thickness were measured just proximal to the base of the tendon-suture interface after suturing. Width and thickness were orthogonal measurements used to estimate the cross-sectional area with the assumption that the tendon was elliptical. A 0.9% saline solution was sprayed on the tendons intermittently during setup and testing to keep the specimens moist.
Three suture techniques were performed using No. 2 FiberWire (Arthrex). These included the classic KS, performed as originally described 14 ; the SpeedWhip whipstitch with FiberLoop (WS) (Arthrex); and a novel multiplanar, perpendicular modification to the SpeedWhip whipstitch with FiberLoop (MP) (Figure 1). The SpeedWhip looped whipstitch was performed according to the manufacturer’s guidelines. The MP technique involved orthogonally alternating the direction of suture passage, starting right to left, then front to back, left to right, and finally back to front (Figure 2). All techniques used 4 stitches, as using 5 or fewer has been shown to be biomechanically optimal to more than 5. 7,8 The stitching ended 10 mm from the end of the tendon, as this is a common distance point, and a 10-mm bite size from the tendon edge has been shown to have greater load to failure than a 5-mm bite size. 7,19 The distance between each suture pass was 5 mm, as this has been shown to reduce elongation after cyclic loading compared with longer intervals. 10 Therefore, the whipstitch techniques started 25 mm from the tendon edge and ended 10 mm from the tendon edge. The KS started 10 mm from the tendon edge on one side, traveled to 25 mm from the tendon edge, and then transitioned to the contralateral side and traveled back down to 10 mm from the tendon edge.
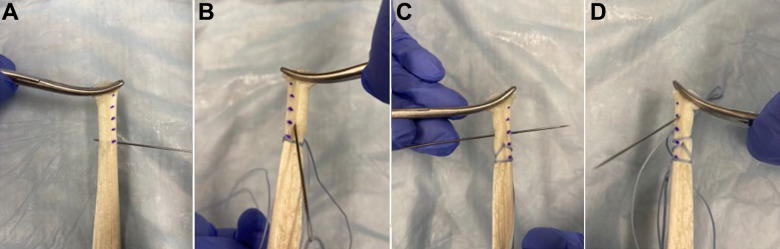
Figure 1.
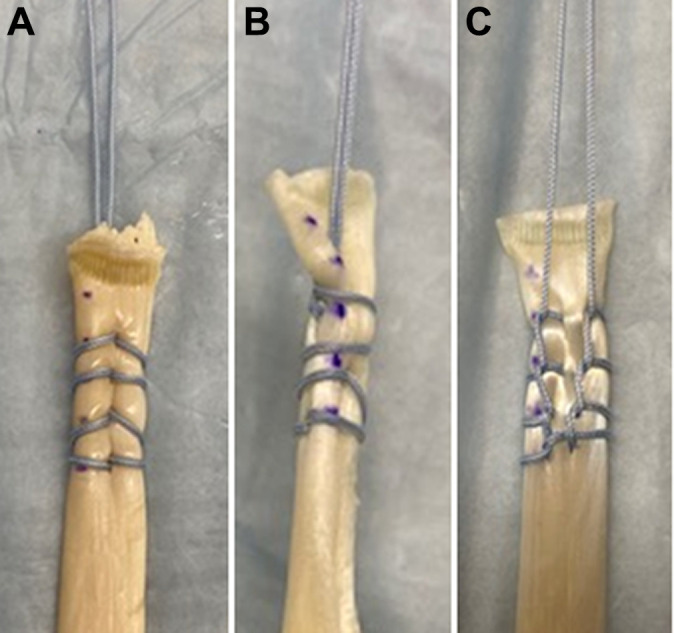
Three suturing techniques, including the (A) standard whipstitch; (B) multiplanar, perpendicular whipstitch; and (C) Krackow stitch.
Figure 2.
Technique for the multiplanar, perpendicular whipstitch: (A) right to left, (B) front to back, (C) left to right, and (D) back to front.
After suturing was complete, each sample was marked at the tendon-clamp interface to ensure that there was no slippage, at the base of the suture-tendon interface near the 25-mm mark, and at the end of the suture-tendon interface near the 10-mm mark. Each suture limb was also marked 1 mm distal to the level of the tendon to allow for calculation of construct elongation. The samples were secured in a custom 3-dimensionally printed clamp using the fixation seen in Figure 3. The clamp was designed with a straight central channel for the tendon that included hand-rendered texturing for grip of the tendon with a slight channel diameter decrease near the end for improved grip. The suture ends were tied at the same distance for each trial, with 6 square knots over a smooth half-inch ring to promote equal load distribution over the suture limbs. A Blackfly detector (FLIR Systems) and 25-mm lens were placed perpendicular to the test setup to collect digital images, and a ruler was placed in the imaging path in-plane with the tensile axis for visual displacement calibration.
Figure 3.
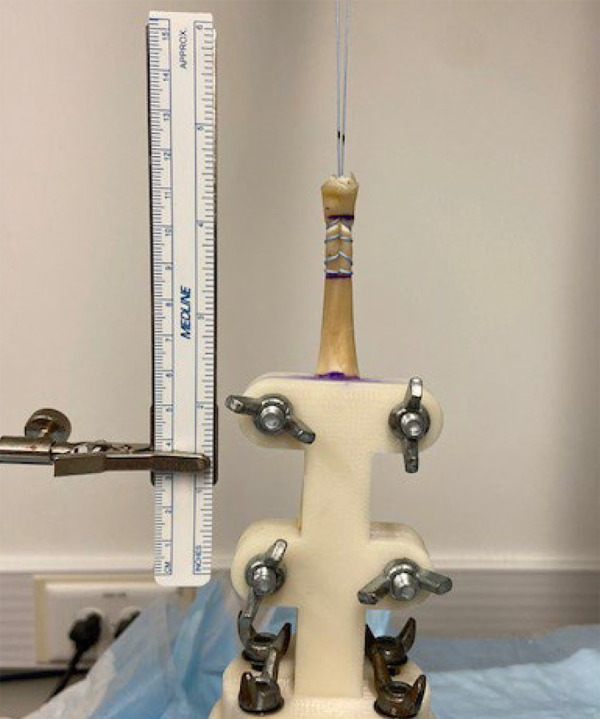
Tendon biomechanical testing setup.
Biomechanical Testing and Data Acquisition
Biomechanical testing was performed with an MTS 858 Mini-Bionix II system with a Sensotec 1000-pound load cell. Based on load cell and machine crosshead measurements, the samples were first preloaded to 5 N and then pretensioned to 50 N at a rate of 100 mm/min for 3 cycles to simulate operating room pretensioning. The samples were then returned to a load of 5 N for 1 minute, followed by cyclic loading from 5 N to 100 N at a rate of 200 mm/min for 100 cycles. We developed this loading protocol based on consensus from previous studies 5,8 –10,21,22 as well as our own preliminary testing, which revealed no further changes in elongation or architecture after initial settling. After cyclic testing, the specimens were loaded to failure at a rate of 20 mm/min. 8 –10,25 Static images were taken at 5 N after preloading, pretensioning, and cycling.
Tendon elongation was measured both for the total construct and at the suture-tendon interface, as shown in Figure 4. These measurements were performed using ImageJ software (National Institutes of Health) with a resolution of 9 pixels/mm, length calibrated to the in-plane ruler scale. Construct length and subsequent elongation were recorded from the mark at the base of the suture-tendon interface to the marks on each suture limb, and the average of the measurement for both limbs was calculated. Suture-tendon interface length and subsequent elongation were recorded from the mark at the base of the suture-tendon interface to the tip of the tendon. Because of tendon deformation during testing, we could not reliably measure only the portion of the tendon with the suture included and therefore chose to measure to the tip of the tendon for consistency.
Figure 4.
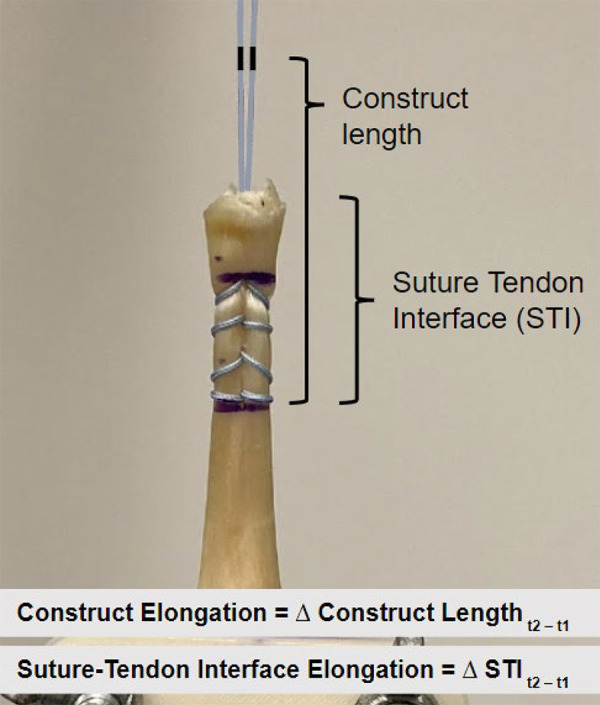
Description of the measurement and calculation of elongation variables.
Construct length and suture-tendon interface length measurements were taken at each imaging time point, and elongation was calculated as the displacement measured between time points. Negative displacement was referred to as shortening. Displacement due to pretensioning was calculated from preload to pretension (Tpre). Displacement due to cyclic loading was calculated from pretension to cyclic load (Tcyc). Total displacement before loading to failure was calculated from preload to cyclic load (Ttotal).
Yield load was calculated as the yield point where the force-displacement curve intersected with a 0.25% offset line from the linear region during the load-to-failure testing. Ultimate load was calculated as the maximum force reached during load-to-failure testing. Failure mode was reported as suture pullout through the tendon or suture breakage. Stiffness was calculated from the slope of the linear region of the force-displacement curve on load-to-failure testing.
Statistical Analysis
Sample and power calculations were completed using G*Power Version 3.1.9.2 (Heine University of Dusseldorf). Descriptive statistics for tendon circumference, width, and thickness were calculated and represented as means and standard deviations. The distribution of data for each variable was determined to be normal as assessed by the Shapiro-Wilk test. One-way analyses of variance were performed to compare each individual variable of cross-sectional area, yield load, ultimate load, failure load, and stiffness between the 3 groups. Repeated-measures analyses of variance were used to analyze measurement differences within and between suture technique groups across the 3 time points for suture-tendon interface and construct elongation. The Mauchly test was utilized to assess sphericity. In the event sphericity had been violated, a Greenhouse-Geisser correction was employed. The Bonferroni method was used for post hoc analysis as appropriate. Statistical significance was set at P ≤ .05. All analyses were performed with SPSS Version 26 (IBM).
Results
Descriptive statistics, including circumference, width, thickness, and cross-sectional area, of the tendons are presented in Table 1. No statistically significant differences existed between the groups for any characteristic.
Table 1.
Descriptive Statistics of the Cadaveric Tendons According to Suture Technique a
| WS, n = 10 | MP, n = 10 | KS, n = 10 | P | |
|---|---|---|---|---|
| Circumference, mm | 18.70 ± 2.00 | 18.80 ± 2.20 | 19.70 ± 3.50 | WS = MP (.80) WS = KS (.44) MP = KS (.35) |
| Width, mm | 5.35 ± 1.36 | 5.00 ± 1.15 | 6.65 ± 1.70 | |
| Thickness, mm | 2.65 ± 0.41 | 3.15 ± 0.47 | 2.70 ± 0.82 | |
| CSA, mm2 | 28.11 ± 6.21 | 28.47 ± 6.70 | 31.76 ± 11.72 | WS = MP (.70) WS = KS (.33) MP = KS (.49) |
a Data are reported as mean ± SD. CSA, cross-sectional area; KS, Krackow stitch; MP, multiplanar, perpendicular whipstitch; WS, standard whipstitch.
Tendon stiffness did not differ between the 3 groups (Table 2). The yield load was significantly greater for the KS compared with WS (186.32 ± 32.66 vs 147.60 ± 31.93 N; P = .019). The ultimate load for WS (183.33 ± 57.44 N) was significantly less compared with both MP (270.76 ± 39.36 N) and KS (298.90 ± 25.94 N) (P ≤ .001 for both) (Table 2). The method of failure for all 10 KSs was suture breakage. For MP, 6 of 10 failures were due to suture breakage, while the remaining 4 failed due to suture pullout through the tendon. For WS, all 10 failures were a result of suture pullout.
Table 2.
Yield Load, Ultimate Load, and Stiffness According to Suture Technique a
| WS, n = 10 | MP, n = 10 | KS, n = 10 | P | |
|---|---|---|---|---|
| Yield load, N | 147.60 ± 31.93 | 161.05 ± 21.72 | 186.32 ± 32.66 | WS = MP (.26) MP = KS (.18) KS > WS (.019) |
| Ultimate load, N | 183.33 ± 57.44 | 270.76 ± 39.36 | 298.90 ± 25.94 | MP = KS (.08) WS < MP (≤.001) WS < KS (≤.001) |
| Stiffness, N/mm | 30.16 ± 2.51 | 29.09 ± 1.52 | 29.66 ± 2.02 | WS = MP (.35) WS = KS (.72) MP = KS (.54) |
a Data are reported as mean ± SD. KS, Krackow stitch; MP, multiplanar, perpendicular whipstitch; WS, standard whipstitch.
During testing, there was noted to be a decrease in tendon length at the suture-tendon interface because of a purse-string effect; thus, we describe this negative elongation value as shortening (Figure 5). When examining the suture-tendon interface displacement within each group, all 3 suture techniques demonstrated significantly more shortening at the suture-tendon interface for Ttotal compared with Tpre (P ≤ .005). There was also significantly more shortening at the suture-tendon interface for Ttotal compared with Tcyc for both WS (P < .001) and MP (P = .031) (Table 3). For total construct elongation within each group, all 3 groups demonstrated significantly greater elongation for Ttotal compared with Tpre (P ≤ .005). Construct elongation was also significantly greater for Ttotal compared with Tcyc for WS and MP (P < .001), and for Tcyc compared with Tpre for WS (P = .009) and MP (P < .001) (Table 3).
Figure 5.

Decrease in tendon length at suture-tendon interface (shortening) because of the purse-string effect in a multiplanar, perpendicular looped whipstitch trial.
Table 3.
Elongation at Different Time Points for Suture-Tendon Interface and Overall Construct a
| Elongation, mm | ||||
|---|---|---|---|---|
| Tpre | Tcyc | Ttotal | P | |
| Suture-tendon interface | ||||
| WS, n = 10 | –2.11 ± 1.17 | –1.67 ± 1.16 | –3.78 ± 1.25 | Ttotal < Tpre and Tcyc (both <.001) |
| MP, n = 10 | –0.87 ± 1.18 | –1.85 ± 1.29 | –2.73 ± 1.21 | Ttotal < Tpre (<.001) and Tcyc (.031) |
| KS, n = 10 | –0.53 ± 0.47 | –1.34 ± 1.17 | –1.87 ± 1.27 | Ttotal < Tpre (.005) |
| P | WS < MP and KS (both ≤.03) |
WS < KS (.006) | ||
| Total construct | ||||
| WS, n = 10 | 7.57 ± 5.88 | 12.96 ± 5.11 | 20.54 ± 8.24 | Ttotal > Tpre and Tcyc (both
<.001) Tcyc > Tpre (.009) |
| MP, n = 10 | 5.14 ± 2.00 | 19.13 ± 5.37 | 24.27 ± 6.16 | Ttotal > Tpre and Tcyc (both
<.001) Tcyc > Tpre (<.001) |
| KS, n = 10 | 1.17 ± 0.42 | 4.79 ± 0.73 | 5.96 ± 0.86 | Ttotal > Tpre (.005) |
| P | WS > KS (.001) | MP > WS and KS (both ≤.01) KS < WS and MP (both ≤.001) |
KS < WS and MP (both <.001) |
|
a Data are reported as mean ± SD. Negative values in the suture-tendon interface represent shortening. KS, Krackow Stitch; MP, multiplanar, perpendicular whipstitch; Tcyc, displacement due to cycling; Tpre, displacement due to pretension; Ttotal, total displacement throughout the entire time period from preload to end of cycling; WS, standard whipstitch.
When examining between-group differences for elongation at each time point, WS demonstrated significantly more shortening at the suture-tendon interface compared with MP (P = .03) and KS (P = .004) for Tpre. WS also demonstrated significantly more shortening at the suture-tendon interface compared with KS (P = .006) for Ttotal (Table 3 and Figure 6). With regard to construct elongation, WS showed significantly greater elongation compared with KS at Tpre and Tcyc (P = .001). MP demonstrated significantly greater construct elongation compared with WS (P = .01) and KS (P < .001) at Tcyc. KS construct elongation was significantly smaller compared with WS and MP at Ttotal (P < .001) (Table 3 and Figure 7).
Figure 6.
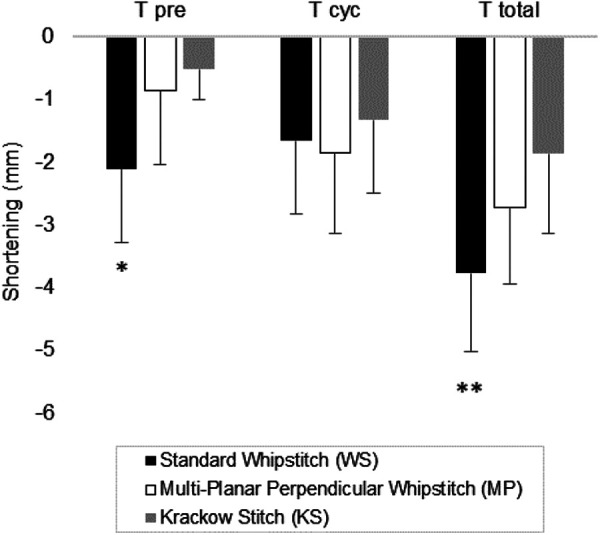
Suture-tendon interface elongation between each group at each time point. *WS has significantly more shortening compared with MP (P = .03) and KS (P = .004). **WS has significantly more shortening compared with KS (P = .006). Tcyc, displacement due to cycling; Tpre, displacement due to pretension; Ttotal, total displacement throughout the entire time period from preload to end of cycling.
Figure 7.
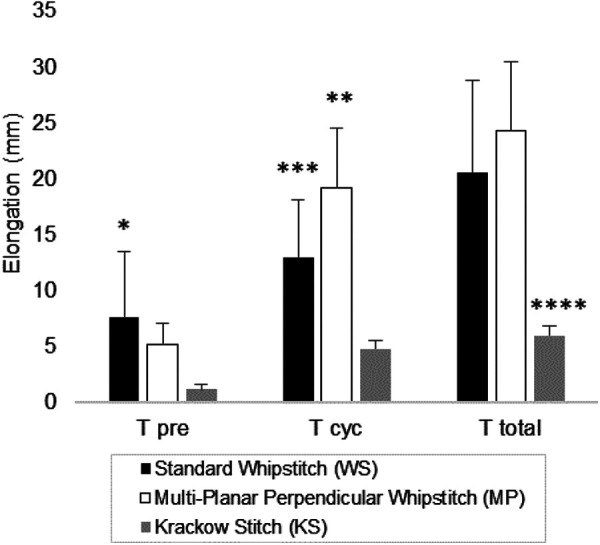
Construct elongation between each group at each time point. *WS has significantly more elongation compared with KS (P = .001). **MP has significantly more elongation compared with WS (P = .01) and KS (P < .001). ***WS has significantly more elongation compared with KS (P = .001). ****KS has significantly less elongation compared with WS and MP (P < .001). Tcyc, displacement due to cycling; Tpre, displacement due to pretension; Ttotal, total displacement throughout the entire time period from preload to end of cycling.
Discussion
The purpose of our study was to evaluate the biomechanical properties of 3 suturing techniques: the classic KS, standard WS, and a novel MP technique. To the best of our knowledge, this is the first study to measure and compare elongation, stiffness, yield load, ultimate load, and method of failure for these techniques using cadaveric tibialis anterior tendon. We did not prove our hypothesis of superiority of MP over the WS or KS. Although the MP group did outperform the WS group in ultimate load, the KS group outperformed the MP group in elongation and also outperformed the WS group in nearly all variables tested. Therefore, we have demonstrated that the KS should be considered the preferred technique. If a commercial looped whipstitch is chosen over the KS to reduce operating time and technical complexity, the authors would recommend the MP technique.
In our study, KS and MP demonstrated greater ultimate load than WS, and there was no difference in ultimate load between KS and MP. This finding is clinically important, as this suggests that the perpendicular passage of the looped whipstitch improves the strength of the construct over the standard technique and results in strength comparable with that of the KS. The KS is ubiquitously used and trusted and has been shown in some studies to have stronger biomechanical properties than the standard looped whipstitch, including less elongation, 1,3 fewer suture pullouts, 1,20 and higher ultimate load. 20 While others have reported no difference in load to failure between the standard WS and KS, 3,7 our study demonstrated that making orthogonal needle passes with a WS improves the ultimate load and is a practical modification. This increase in strength makes this an attractive technique, as it does not introduce some of the criticisms of the KS, which include increased operative time and more needle passages through the tendon. 1 Failure occurred from suture breakage in all 10 KSs and 6 out of 10 MPs. This would suggest that a clinical failure would be expected to occur from suture failure before construct failure, and therefore, detecting differences between the 2 techniques may not be clinically relevant.
The yield load of KS was greater than that of WS, but there were no differences between KS and MP or MP and WS. Additionally, it was observed during testing that both MP and WS would typically have a pullout of the suture loop closest to the tendon end during yield, whereas the KS would have a pullout of the sutures closest to the clamp. This form of suture pullout through the tendon with the looped whipstitch has been reported by previous authors. 3,20 This may be because of the difference in suture construct, as the KS is a locking stitch, whereas the whipstitch is nonlocking, and the locking may result in less suture slippage as force is applied. Additionally, it may take more force to disrupt the suture closest to the base compared with the suture closest to the tendon edge, which would explain the difference in yield load.
A noteworthy finding in all 3 techniques was the shortening at the suture-tendon interface, with the greatest shortening occurring in WS. We chose to describe this negative value for change in displacement as shortening because the length of the suture-tendon interface decreased and could be visualized as the tendon shortening in this area because of suture slippage as force was applied, similar to a purse-string effect (as seen in Figure 5), which has been previously described by Hahn and colleagues. 7 This decrease in tendon length may theoretically reduce the amount of tendon available for healing after repair or reconstruction. For all 3 techniques, shortening was greatest when measured as total displacement from preload to the end of cycling compared with displacement only due to pretensioning. This demonstrates that settling of the construct occurred during cycling, which is expected and the reason for intraoperative cycling. Furthermore, there was more shortening at the suture-tendon interface for WS compared with KS but no difference in shortening at the suture-tendon interface between MP and KS. This suggests more tendon deformation and less tendon available for healing with WS compared with KS.
When evaluating total construct elongation from the base of the suture-tendon interface to marks on the suture limbs for all 3 techniques, there was greater elongation when measured as total displacement from preload to the end of cycling compared with displacement only due to pretensioning. Again, this demonstrates the construct settling and the purpose of intraoperative cycling. In contrast to shortening at the suture-tendon interface, the reason for this finding’s being a positive number and being reported as elongation is that this value captures the suture slippage and pullout through the tendon that occurs as force is applied; it is an expected finding. Another notable finding was that there was significantly more construct elongation at multiple time points with WS and MP compared with KS, possibly because of more suture slippage. Both WS and MP are nonlocking techniques, while KS is a locking technique, and therefore we would expect less suture slippage with KS. When combining these construct elongation data together with the suture-tendon interface shortening findings, this suggests that the KS, because of overall less total elongation and less suture-tendon interface shortening, results in less suture pullout, less elongation, and less soft tissue deformity than the standard looped whipstitch. This finding of increased tendon shortening and increased construct elongation with the looped whipstitch compared with the KS may be most relevant in suspensory fixation.
We have highlighted elongation and ultimate load, as these appear to be the most clinically important variables. Elongation has been shown to be a determinant of outcome after Achilles tendon rupture. 11,16 Load to failure intuitively is important, as a higher load to failure means that the repair can withstand a greater force. The shortening of the graft could also be an important factor in selection of the best suture technique construct. Shortening of the graft could decrease the amount of tendon available for a repair, the amount docked in a tunnel, and ultimately the amount available for healing. While a paucity of literature exists regarding this factor, this could be a theoretical shortcoming.
Limitations
Our study has several limitations. First, we used cadaveric tibialis anterior tendons, which are different from the xenograft tissues commonly used in other biomechanical studies. 3,9,10,20,25 This may make direct comparisons of previous research with our study unreliable. However, we feel this is also a strength, as human cadaveric tissue is commonly used in soft tissue reconstruction procedures. However, these grafts were prepared by the distributor and underwent freezing and thawing, and therefore, this may have affected our findings and is not directly comparable with fresh tissue. Additionally, the age of the specimens was not available, and as such, comparison among groups was not able to be performed. Another limitation is that both KS and MP mainly failed because of suture breakage; therefore, we were unable to truly compare the failure loads of these 2 techniques, as the suture failed before the construct. Furthermore, our failure load was lower than in some studies 3,7,10,20,25 although these studies used xenograft tissue with reportedly larger cross-sectional areas. In contrast, the failure load in our study was greater than that in other studies that used cadaveric tibialis anterior tendon. 4,18 Last, as with all biomechanical studies, this does not represent any biologic response or healing that may occur before this loading. However, with 100 cycles and loads in the physiologic range, this testing regimen may not be far from an early rehabilitation experience for a patient.
Conclusion
When comparing the KS, the standard WS, and a novel MP, the KS is likely the best suture technique for maximizing strength and minimizing suture pullout, construct elongation, or graft shortening. This may be most relevant to suspensory fixation constructs in contrast to interference screw fixation, in which suture is mainly used to assist in graft passage. Because of the increased technical challenges and operative time incurred when using the KS, many surgeons choose to use a WS. For surgeons who elect to use this device, the findings of this study support the technique of the MP, as it offers improved ultimate load over the standard looped whipstitch technique, with similar efficiency.
Acknowledgment
The authors thank RTI Surgical for the donation of the cadaveric tendons and Arthrex for the donation of the suture material.
Footnotes
Final revision submitted March 18, 2022; accepted April 5, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: The cadaveric tendons used in this study were donated by RTI Surgical, and the suture material (FiberWire and FiberLoop) was donated by Arthrex. The University of Michigan Research Advisory Committee provided grant funding for supplies. dsdf S.M. has received education payments from Pinnacle. D.P.P. has received education payments from Arthrex. M.T.F. has received education payments from Evolution Surgical, consulting fees from Stryker, speaking fees from Smith & Nephew, and hospitality payments from Wright Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the University of Michigan (study No. HUM00168622).
References
- 1. Barber FA, Howard MS, Piccirillo J, Spenciner DB. A biomechanical comparison of six suture configurations for soft tissue-based graft traction and fixation. Arthroscopy. 2019;35(4):1163–1169. doi:10.1016/j.arthro.2018.10.140 [DOI] [PubMed] [Google Scholar]
- 2. Choi GW, Kim HJ, Lee TH, Park SH, Lee HS. Clinical comparison of the two-stranded single and four-stranded double Krackow techniques for acute Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1878–1883. doi:10.1007/s00167-016-4265-0 [DOI] [PubMed] [Google Scholar]
- 3. Deramo DM, White KL, Parks BG, Hinton RY. Krackow locking stitch versus nonlocking premanufactured loop stitch for soft-tissue fixation: a biomechanical study. Arthroscopy. 2008;24(5):599–603. doi:10.1016/j.arthro.2007.11.020 [DOI] [PubMed] [Google Scholar]
- 4. Fennell CW, Ballard JM, Pflaster DS, Adkins RH. Comparative evaluation of bone suture anchor to bone tunnel fixation of tibialis anterior tendon in cadaveric cuboid bone: a biomechanical investigation. Foot ankle Int. 1995;16(10):641–645. doi:10.1177/107110079501601011 [DOI] [PubMed] [Google Scholar]
- 5. Frank RM, Bernardoni ED, Veera SS, et al. Biomechanical analysis of all-suture suture anchor fixation compared with conventional suture anchors and interference screws for biceps tenodesis. Arthroscopy. 2019;35(6):1760–1768. doi:10.1016/j.arthro.2019.01.026 [DOI] [PubMed] [Google Scholar]
- 6. Grewal R, Athwal GS, MacDermid JC, et al. Single versus double-incision technique for the repair of acute distal biceps tendon ruptures: a randomized clinical trial. J Bone Joint Surg Am. 2012;94(13):1166–1174. doi:10.2106/JBJS.K.00436 [DOI] [PubMed] [Google Scholar]
- 7. Hahn JM, Inceoʇlu S, Wongworawat MD. Biomechanical comparison of Krackow locking stitch versus nonlocking loop stitch with varying number of throws. Am J Sports Med. 2014;42(12):3003–3008. doi:10.1177/0363546514550989 [DOI] [PubMed] [Google Scholar]
- 8. Hong CK, Lin CL, Chang CH, Jou IM, Su WR. Effect of the number of suture throws on the biomechanical characteristics of the suture-tendon construct. Arthroscopy. 2014;30(12):1609–1615. doi:10.1016/j.arthro.2014.06.029 [DOI] [PubMed] [Google Scholar]
- 9. Hong CK, Lin CL, Kuan FC, Wang PH, Yeh ML, Su WR. A biomechanical evaluation of various double Krackow suture techniques for soft-tissue graft fixation. Arthroscopy. 2018;34(3):663–668. doi:10.1016/j.arthro.2017.09.025 [DOI] [PubMed] [Google Scholar]
- 10. Hong CK, Lin CL, Kuan FC, Wang PH, Yeh ML, Su WR. Longer stitch interval in the Krackow stitch for tendon graft fixation leads to poorer biomechanical property. J Orthop Surg. 2018;26(3). doi:10.1177/2309499018799514 [DOI] [PubMed] [Google Scholar]
- 11. Kangas J, Pajala A, Ohtonen P, Leppilahti J. Achilles tendon elongation after rupture repair: a randomized comparison of 2 postoperative regimens. Am J Sports Med. 2007;35(1):59–64. doi:10.1177/0363546506293255 [DOI] [PubMed] [Google Scholar]
- 12. Kearney RS, Costa ML. Current concepts in the rehabilitation of an acute rupture of the tendo Achillis. J Bone Joint Surg Br. 2012;94(1):28–31. doi:10.1302/0301-620X.94B1.28008 [DOI] [PubMed] [Google Scholar]
- 13. Krackow KA. The Krackow suture: how, when, and why. Orthopedics. 2008;31(9):931–933. doi:10.3928/01477447-20080901-19 [DOI] [PubMed] [Google Scholar]
- 14. Krackow KA, Thomas SC, Jones LC. A. new stitch for ligament-tendon fixation. Brief note. J Bone Joint Surg Am. 1986;68(5):764–766. [PubMed] [Google Scholar]
- 15. Maffulli N, Tallon C, Wong J, Lim KP, Bleakney R. Early weightbearing and ankle mobilization after open repair of acute midsubstance tears of the Achilles tendon. Am J Sports Med. 2003;31(5):692–700. doi:10.1177/03635465030310051001 [DOI] [PubMed] [Google Scholar]
- 16. Maquirriain J. Achilles tendon rupture: avoiding tendon lengthening during surgical repair and rehabilitation. Yale J Biol Med. 2011;84(3):289–300. [PMC free article] [PubMed] [Google Scholar]
- 17. McKeon BP, Heming JF, Fulkerson J, Langeland R. The Krackow stitch: a biomechanical evaluation of changing the number of loops versus the number of sutures. Arthroscopy. 2006;22(1):33–37. doi:10.1016/j.arthro.2005.10.008 [DOI] [PubMed] [Google Scholar]
- 18. Núñez-Pereira S, Pacha-Vicente D, Llusá-Pérez M, Nardi-Vilardaga J. Tendon transfer fixation in the foot and ankle: a biomechanical study. Foot Ankle Int. 2009;30(12):1207–1211. doi:10.3113/FAI.2009.1207 [DOI] [PubMed] [Google Scholar]
- 19. Ponce BA, Hosemann CD, Raghava P, Tate JP, Sheppard ED, Eberhardt AW. A biomechanical analysis of controllable intraoperative variables affecting the strength of rotator cuff repairs at the suture-tendon interface. Am J Sports Med. 2013;41(10):2256–2261. doi:10.1177/0363546513499228 [DOI] [PubMed] [Google Scholar]
- 20. Sakaguchi K, Tachibana Y, Oda H. Biomechanical properties of porcine flexor tendon fixation with varying throws and stitch methods. Am J Sports Med. 2012;40(7):1641–1645. doi:10.1177/0363546512450406 [DOI] [PubMed] [Google Scholar]
- 21. Salata MJ, Bailey JR, Bell R, et al. Effect of interference screw depth on fixation strength in biceps tenodesis. Arthroscopy. 2014;30(1):11–15. doi:10.1016/j.arthro.2013.08.033 [DOI] [PubMed] [Google Scholar]
- 22. Slabaugh MMA, Frank RM, Van Thiel GS, et al. Biceps tenodesis with interference screw fixation: a biomechanical comparison of screw length and diameter. Arthroscopy. 2011;27(2):161–166. doi:10.1016/j.arthro.2010.07.004 [DOI] [PubMed] [Google Scholar]
- 23. Wang RY, Arciero RA, Obopilwe E, Mazzocca AD. A comparison of structural and mechanical properties of tubularized and native semitendinosus graft. Am J Sports Med. 2010;38(6):1246–1249. doi:10.1177/0363546509359061 [DOI] [PubMed] [Google Scholar]
- 24. West JL, Keene JS, Kaplan LD. Early motion after quadriceps and patellar tendon repairs: outcomes with single-suture augmentation. Am J Sports Med. 2008;36(2):316–323. doi:10.1177/0363546507308192 [DOI] [PubMed] [Google Scholar]
- 25. White KL, Camire LM, Parks BG, Corey WS, Hinton RY. Krackow locking stitch versus locking premanufactured loop stitch for soft-tissue fixation: a biomechanical study. Arthroscopy. 2010;26(12):1662–1666. doi:10.1016/j.arthro.2010.05.013 [DOI] [PubMed] [Google Scholar]