Abstract
Reagents to monitor T cell responses to the entire HIV genome, based on well characterized epitopes, are missing. Evaluation of HIV-specific T cell responses is of importance to study natural infection, and therapeutic and vaccine interventions. Experimentally derived CD4+ and CD8+ HIV epitopes from the HIV molecular immunology database were developed into Class I and Class II HIV megapools (MPs). We assessed HIV responses in persons with HIV pre antiretroviral therapy (ART) (n = 17) and post-ART (n = 18) and compared these responses to 15 controls without HIV (matched by sex at birth, age, and ethnicity). Using the Activation Induced Marker (AIM) assay, we quantified HIV-specific total CD4+, memory CD4+, circulating T follicular helper, total CD8+ and memory CD8+ T cells. We also compared the Class I and Class II HIV MPs to commercially available HIV gag peptide pools. Overall, HIV Class II MP detected HIV-specific CD4+ T cells in 21/35 (60%) HIV positive samples and 0/15 HIV negative samples. HIV Class I MP detected an HIV-specific CD8+ T cells in 17/35 (48.6%) HIV positive samples and 0/15 HIV negative samples. Our innovative HIV MPs are reflective of the entire HIV genome, and its performance is comparable to other commercially available peptide pools. Here, we detected HIV-specific CD4+ and CD8+ T cell responses in people on and off ART, but not in people without HIV.
Introduction
The Human Immunodeficiency Virus (HIV) infects CD4+ T cells and, if unchecked, slowly obliterates the host immune response over time [1]. During initial infection, the host mounts an HIV-specific immune response with the development of HIV-specific CD4+ and CD8+ T cells [2–4]. With antiretroviral treatment (ART), HIV RNA levels in blood fall below the limit of detection, and the host immune system is “restored” with a rebound in CD4+ T cell count [5, 6]. The quality of HIV-specific CD4+ and CD8+ T cells depends on if these individuals are elite controllers or chronic progressors.
To understand the HIV host immune response, it is necessary to precisely identify and quantify HIV-specific T cells. Classic methodologies to detect HIV-specific CD4+ and CD8+ T cell responses have relied on intracellular cytokine staining, Major Histocompatibility Complex (MHC) tetramer binding assays, lymphoproliferative assays, and ELISpots [7]. Intracellular cytokine staining requires fixation of cells which cannot be used in subsequent functional assays or most gene expression analyses. MHC tetramer binding assays require foreknowledge of an individual’s Human Leukocyte Antigen (HLA). Both lymphoproliferative assays and ELISpots require long term cultures during which cell phenotypes might change [8]. We therefore developed the Activation Induced Marker (AIM) assay to directly detect antigen-specific CD4+ T cells after a 24 hour cell culture [8–11]. The AIM assay is cytokine-independent and detects antigen-specific cells utilizing surface co-expression of specific activation markers, e.g. OX40, PD-L1, CD25, CD69, CD40L, and 41BB (CD137). Advantages of the AIM assay include (1) the ability to sort live cells by flow cytometry for subsequent assays or sequencing, (2) a short assay duration which limits detection of bystander activated cells, and (3) the ability to further classify antigen-specific T cells into different T cell memory subsets and T helper cell functions. For human lymphocytes, marker combinations of CD25/OX40, OX40/PD-L1, OX40/41BB, OX40/CD40L, CD69/CD40L, and CD69/41BB have been used to detect antigen-specific CD4+ and CD8+ T cells [8, 10, 12–14].
The HIV proteins gag and env are major targets of HIV-specific CD4+ and CD8+ T cell responses [2, 15–17]. Prior studies have demonstrated a correlation of gag-specific CD4+ T cells and viremic control, whereas the reverse has been observed with env-specific CD4+ T cells [15]. However, gag and env do not reflect the entirety of the host immune response to HIV viral proteins. Herein, we generated a Class I HIV-specific megapool (MP) and Class II HIV MP, reflective of the entire HIV proteome from clades A, B, and C. Using the HIV molecular immunology database to extract experimentally derived HIV epitopes and Immune Epitope Database (IEDB) cluster tool [18], we designed a Class I HIV MP and Class II HIV MP consisting of immunodominant peptides from env (envelope), gag, gp160 (polyprotein of env), nef, pol, rev, tat, vif, vpr, and vpu. We show that the Class I and Class II HIV MP are able to detect HIV-specific CD8+ and CD4+ T cells, respectively.
Materials and methods
Study subjects
Peripheral blood mononuclear cells (PBMCs) were collected from people living with HIV (PWH) pre-ART and post-ART (Table 1) between 2001 and 2018. These 21 study participants were enrolled under the San Diego Primary Infection Research Consortium (PIRC) (https://www.pirc.ucsd.edu) [19]. These individuals were diagnosed early in their HIV infection and were followed longitudinally before and after ART initiation. PWH were recruited under a protocol approved by the Institutional Review Board (IRB) at the University of California, San Diego (UCSD).
Table 1. Clinical Characteristics of HIV positive patients.
| Pre-ART (n = 17) | [Median, IQR] |
|---|---|
| Age (Years) | 39 [29 – 43] |
| Time from aEDI (days) | 98 [74–2004] |
| CD4 (cells/mm 3 ) | 606 [415–718] |
| HIV viral load (copies/mL) | 120,000 [55,087–244,480] |
| Sex at Birth | |
| Male (%) | 100% |
| Ethnicity | |
| Hispanic (%) | 11.8% |
| Non-Hispanic (%) | 88.2% |
| Race | |
| White (%) | 82.3% |
| Black (%) | 5.9% |
| Other (%) | 11.8% |
| Sexual Orientation | |
| Men who have sex with men (%) | 100% |
| Post-ART (n = 18) | [Median, IQR] |
| Age (Years) | 40 [33 – 46] |
| Time from EDI (days) | 983 [672–2838] |
| Time from ART (days) | 667 [495–1388] |
| Time from ART to undetectable HIV viral load (days) | 236 [162–644] |
| CD4 (cells/mm 3 ) | 825 [563–1025] |
| HIV viral load (copies/mL) | 50 [45–50] |
| Sex at birth | |
| Male (%) | 100% |
| Ethnicity | |
| Hispanic (%) | 22.2% |
| Non-Hispanic (%) | 77.8% |
| Race | |
| White (%) | 77.7% |
| Black (%) | 5.6% |
| Other (%) | 16.7% |
| Sexual Orientation | |
| Men who have sex with men | 100% |
aEDI: estimated date of infection
Blood specimens were taken from 11 individuals at an early time point post infection (21–138 days post the estimated date of infection). Nine of the 11 individuals had paired pre- and post-ART specimens. One individual had only a pre-ART specimen and one individual had only a post-ART specimen. Blood specimens were taken from 10 individuals who were chronically infected (441–3598 days post the estimated date of infection). Five of the 10 individuals had paired pre- and post-ART specimens. Two individuals had only a pre-ART specimen and three individuals had only a post-ART specimen.
As a control group, we used PBMCs from 15 HIV seronegative donors matched by sex at birth, age, and ethnicity. Participants for the control group were recruited under a protocol approved by IRB at La Jolla Institute for Immunology (LJI).
HIV megapools (MP)
HLA Class I and II restricted epitopes have been extracted from HIV molecular immunology database (https://www.hiv.lanl.gov/content/immunology/) using the T Helper/CD4+ Search and the CTL/CD8+ search [20]. The list of epitopes spanning all the HIV proteins (env, gag, gp160, nef, pol, rev, tat, vif, vpr, vpu) have been then clustered using the Epitope Cluster Analysis Tool 2.0 (http://tools.iedb.org/main/analysis-tools/) via the cluster-break method with a 70% homology cutoff, as previously described for other megapool generation [18, 21]. The corresponding list of HIV peptides were synthesized by TC Peptide Lab (San Diego) as crude material on 1–2 mg scale. Individual peptides were resuspended in dimethyl sulfoxide (DMSO), pooled, and sequentially lyophilized, as previously reported. The resulting lyocake was resuspended in DMSO at a stock concentration of 1mg/mL. The Class I MP consists of 187 peptides (46 gag peptides, 34 gp160 peptides, 25 nef peptides, 59 pol peptides, 4 rev peptides, 2 tat peptides, 9 vif peptides, 6 vpr peptides, and 2 vpu peptides) (S1 Table). The Class II MP consists of 164 peptides (7 env peptides, 5 gag peptides, 61 gp160 peptides, 15 nef peptides, 61 pol peptides, 2 rev peptides, 4 tat peptides, 1 vif peptides, 7 vpr peptides, and 1 vpu peptide) (S2 Table). The HIV MPs consist of A, B, and C subtypes.
Other antigens
CMV Class I and II peptide MPs were synthesized by TC Peptide Lab (San Diego) as crude material on 1–2 mg scale. Individual peptides were resuspended in DMSO and pooled into two different MPs for this study. The peptide pools were sequentially lyophilized and each pool resuspended at a stock concentration of 1mg/mL [8, 22]. JPT HIV-1 gag peptide pool (JPT PepMix HIV (GAG) Ultra), consisting of 150 overlapping peptides of 15-mers with 11 amino acid overlap, was purchased from JPT Peptide Technologies. National Institutes of Health (NIH) HIV-1 Clade B gag peptide pool (NIH AIDS Reagent Program #12425), consisting of 123 overlapping peptides of 15-mers with 11 amino acid overlap, was provided by the AIDS Reagent Program. Each peptide pool (JPT and NIH) was suspended in DMSO at a final concentration of 1mg/mL.
PBMC isolation
PBMCs were isolated from whole blood by density gradient centrifugation using Histopaque 1077 (Sigma) and cryopreserved in liquid nitrogen in fetal bovine serum containing 10% DMSO.
AIM assays
Cells were cultured in RPMI supplemented with 5% human AB serum (Gemini Bioscience), Glutamax (Gibco), and Penicillin/Streptomycin (Gibco). Cryopreserved PBMCs were thawed and cultured at ~ 1x106 cells per well in a 96 well round bottom plate. Cells were stimulated with peptides: HIV Class 1 MP (1μg/mL), HIV Class II MP (2μg/mL), HIV JPT gag peptide pool (2μg/mL), HIV NIH gag peptide pool (2μg/mL), CMV Class 1 MP (1μg/mL), and CMV Class II MP (2μg/mL). As a positive control, cells were stimulated with SEB (100ng/mL, Toxin Technology). As a negative control, cells were stimulated with media containing an equivalent volume of DMSO to the one used for the peptide stimulation. When cells were limiting, priority stimulations were HIV Class II MP > HIV Class I MP and CMV Class II MP > CMV Class I MP. Cells were cultured for 24 hours and stained by flow cytometry (FACS). FACS staining buffer consisted of 0.5% Bovine serum albumin (BSA) in phosphate buffered saline (PBS).
Cells were labeled with fixable viability dye eFluor 780 (Thermo Fisher Scientific). Antibodies from Thermo Fisher Scientific included CD19 e780 (clone HIB19), CD14 e780 (clone 61D3), CD16 e780 (clone eBioCB16), OX40 FITC (clone Ber-ACT35), CD69 PeCy7 (clone FN50). Antibodies from Biolegend included: CD45RA BV570 (clone HI100), CXCR5 BV421 (clone J252D4), PD-L1 PE (clone 29E.2A3), CCR7 APC (clone G043H7), CD8a BV650 (clone RPA-T8), CD4 PerCpCy5.5 (clone OKT4). Cells were acquired on a BD Celesta and analyzed using FlowJo Software, version 9.9.6. Antigen-specific CD4+ and CD8+ T cells were measured as background (DMSO) subtracted data, with a minimal DMSO level set to 0.005% (limit of detection, LOD). The threshold for positivity (limit of sensitivity, LOS) was calculated using 2x SD of all HIV negative controls measured (n = 15).
Statistical analyses
Statistical analyses were performed using GraphPad Prism 9. Non-parametric tests were used in all cases. Wilcoxon matched-pairs signed rank test and Mann-Whitney U tests were used to compare the magnitude of responses in paired and independent two-sample comparisons, respectively. McNemar’s test and Fisher’s exact test were used to compare the proportion of responders. Friedman’s test was used to compare repeated measures across three groups.
Results
Study population
Men who have sex with men with HIV were enrolled, from whom blood was taken pre-ART (n = 17) and post-ART (n = 18) (Table 1). The pre-ART median CD4+ T cell count was 606 cells/ul [interquartile range (IQR), 415–718]. The HIV RNA load was 120,000 copies/ml [IQR, 55,087–244,480] with a median estimated date of infection of 98 days [IQR, 74–2004] at the time of sample collection. The post-ART median CD4+ T cell count was 825 cells/mm3 [IQR, 563–1025]. The HIV RNA load was below the limit of detection with a median of 667 days [IQR, 495–1388] from beginning ART and a median of 236 days [162–644] from starting ART till an undetectable HIV viral load (VL).
The duration of ART for 8 chronically infected persons was 1567 days (range of 407 to 2751 days from time of ART start date to date of blood draw). One chronically infected person had a detectable VL of 9,695 copies/mL at time of blood draw. The duration of ART for the 10 early infected patients was 551 days (range of 368 to 762 days from time of ART start date to date of blood draw). None of the early infected persons had detectable VL.
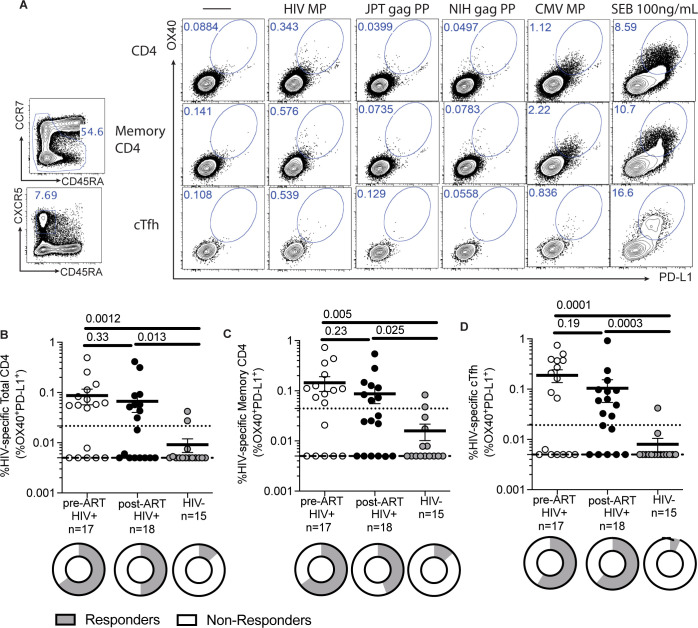
Detection of HIV-specific CD4+ T cells
Using a Class II HIV MP consisting of immunodominant epitopes from the entire HIV proteome, we first tested its ability to detect HIV-specific CD4+ T cells in HIV positive and HIV negative samples. In HIV-specific CD4+ T cells, there is lower 41BB expression, attributed to T-cell exhaustion from chronic infection which precludes use of 41BB by AIM assay [23]. Additionally, a combination of CD25/OX40 on PBMCs captures more T regulatory cells which may be elevated in chronic infections [10]. We thus identified HIV-specific CD4+ T cells by a combination of OX40 and PD-L1 by AIM assay (Fig 1A) [10]. Higher magnitudes of HIV-specific CD4+ T cells responses were detected for pre-ART (p = 0.0012) and post-ART samples (p = 0.013) compared to HIV negative samples (Fig 1B). There was no difference in magnitude of responses between paired pre- and post-ART samples (p = 0.24). With a limit of sensitivity of 0.022%, higher proportions of responders were detected for pre-ART (11/17, p = 0.0046) and post-ART (9/18, p = 0.034) samples compared to HIV negative samples (2/15); there was no difference in the proportion of responders detected between paired pre- and post-ART samples (p = 0.51). Compared to HIV negative samples, this limit yielded a sensitivity of 57.14% and a specificity of 86.67%.
Fig 1. Detection of HIV-specific CD4+ T cells.
(A) Sample flow cytometry plot showing gating strategy for HIV-specific CD4+ T cells based on co-expression of OX40 and PD-L1 on total CD4, memory CD4, and cTfh cells. Specimens from HIV infected donors have a higher frequency of (B) HIV-specific total CD4+ T cells (C) HIV-specific memory CD4+ T cells, and (D) HIV-specific cTfh cells compared to HIV uninfected specimens. There was no statistical difference between the mean frequencies pre-ART and post-ART specimens. Data was background subtracted. P-values by Mann-U Whitney test. Limit of detection (dashed line) was set at 0.005%. Limit of sensitivity (dotted line) was 0.022% for HIV-specific total CD4+ T cells, 0.044% for HIV-specific memory CD4+ T cells, and 0.019% for HIV-specific cTfh cells. Data presented represents mean ± standard error of the mean. Pie charts depict proportion of responders.
As the memory T cell compartment is important in chronic infection, we quantified memory CD4+ T cells. We identified HIV-specific total memory CD4+ T cells and circulating T follicular helper (Tfh) cells. We defined total memory CD4+ T cells as a combination of central memory + effector memory + TEMRA (Fig 1A). Higher magnitudes of HIV-specific memory CD4+ T cell responses were detected in both pre-ART (p = 0.005) and post-ART HIV-infected individuals (p = 0.025) compared to HIV negative individuals (Fig 1C). There was no difference in the magnitudes of responses between paired pre and post-ART samples (p = 0.23). There was a higher proportion of responders pre-ART (11/17, p = 0.0046) and post-ART (8/18, p = 0.070) samples compared to HIV negative samples (2/15). There was no difference in the proportion of responders detected between paired pre- and post-ART samples (p = 0.51).
Circulating Tfh (cTfh) cells are CD4+ T cells which provide help to B cells to promote the development high affinity antibodies [24]. We defined cTfh cells by CCR5+CD45RA- CD4+ T cells (Fig 1A). Similarly, higher magnitudes of HIV-specific cTfh tells were detected in pre-ART (p = 0.0001) and post-ART HIV-infected individuals (p = 0.0003) compared to HIV negative individuals (Fig 1D). There was no difference in the magnitudes of responses between paired pre and post-ART samples (p = 0.19). There was no difference in the proportion of responders pre-ART (10/17, p = 0.0028) and post-ART (11/18, p = 0.0028) samples compared to HIV negative samples (1/15). There was no difference in the proportion of responders detected between paired pre- and post-ART samples (p = 1.00).
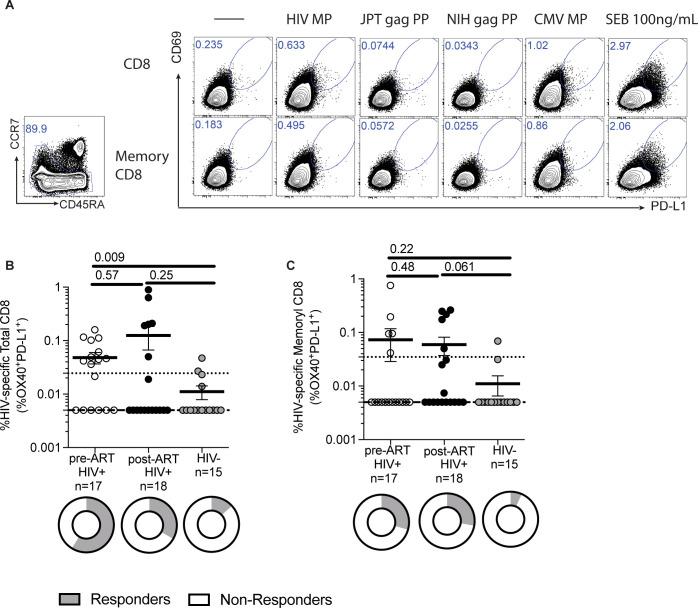
Detection of HIV-specific CD8+ T cells
Using a Class I HIV MP consisting of immunodominant epitopes from the entire HIV proteome, we tested its ability to detect HIV-specific CD8+ T cells in HIV positive and HIV negative samples. By co-expression of CD69 and PD-L1 by AIM assay (Fig 2A), we detected HIV-specific CD8+ T cells. The Class I HIV MP detected higher magnitudes of HIV-specific CD8+ T cell responses were detected in pre-ART (p = 0.009) samples but comparable post-ART HIV-infected individuals (p = 0.25) compared to HIV negative individuals (Fig 2B). With a limit of sensitivity of 0.025%, there was no difference in the magnitudes of responses between paired pre and post-ART samples (p = 0.73). There was a higher proportion of responders pre-ART (10/17, p = 0.012) but comparable proportion of responders post-ART (6/18, p = 0.24) samples compared to HIV negative samples (2/15). There was no difference in the proportion of responders detected between paired pre- and post-ART samples (p = 0.22).
Fig 2. Detection of HIV-specific CD8+ T cells.
(A) Sample flow cytometry plot showing gating strategy for HIV-specific CD8+ T cells based on co-expression of CD69 and PD-L1 on total CD8 and memory CD8 T cells. Specimens from HIV infected donors have a higher frequency of (B) HIV-specific total CD8+ T cells and (C) HIV-specific memory CD8+ T cells compared to HIV negative specimens. There was no statistical difference between pre-ART and post-ART specimens. Data was background subtracted. P-values by Mann-U Whitney test. Limit of detection (dashed line) was set at 0.005%. Limit of sensitivity (dotted line) was 0.025% for HIV-specific total CD8+ T cells and 0.035% for HIV-specific memory CD8+ T cells. Data presented represents mean ± standard error of the mean.
For memory CD8+ T cells, HIV Class I MP detected comparable magnitudes of HIV-specific memory CD8+ T cell responses in pre-ART (p = 0.22) and post-ART HIV samples (p = 0.061) compared to HIV negative individuals (Fig 2C). There was no difference in the magnitudes of responses between paired pre and post-ART samples (p = 0.84). There was a comparable proportion of responders pre-ART (5/17, p = 0.18) and post-ART (5/18, p = 0.19) samples compared to HIV negative samples (1/14). There was no difference in the proportion of responders detected between paired pre- and post-ART samples (p = 1.00). The Class I HIV MP had a 47.1% sensitivity and 86.7% specificity.
Comparison of HIV MP to commercially available gag peptide pools
The detection of gag-specific T cells is the most common way to quantify HIV-specific T cells. We therefore compared the Class I and II HIV MP to 2 commercially available clade B gag peptide pools from JPT and NIH. The frequencies of HIV-specific CD4+ T cells, memory CD4+ T cells, and cTfh were comparable when using the Class II MP, JPT gag, or NIH gag peptide pools (S1 Fig), as clade B is predominantly found in North America and Europe. The frequencies of HIV-specific total CD8+ T cells and memory CD8+ T cells were also comparable (S2 Fig).
Detection of CMV-specific CD4+ and CD8+ T cells
To demonstrate our ability to detect antigen-specific T cells, as a control, we tested for CMV-specific T cells in these same specimens [25, 26]. Using our Class II MP, we were able to detect CMV-specific CD4+ T-cells. The magnitudes of CMV-specific CD4+ T cells were comparable pre- and post-ART for total CD4+ T cells, memory CD4+ T cells, and cTfh (S3 Fig). Using the Class I CMV MP, we additionally tested the magnitudes of CMV-specific CD8+ T cells pre- and post-ART. There was no difference between the magnitudes of total and memory CMV-specific CD8+ T cell among pre-ART and post-ART specimens and HIV negative individuals (S3 Fig).
Discussion
The HIV MP was designed to encompass all HIV proteins instead of only gag, as other HIV proteins such as nef [16, 27, 28], pol [29], and tat [30] can elicit HIV-specific T cell responses. Using the Class I and Class II MP reflective of the immunodominant epitopes from the entire HIV proteome, we were able to detect either HIV-specific CD4+, memory CD4+ T, cTfh, CD8+ T, or memory CD8+ cells in 20/21 (95%) of PWH. Prior studies have demonstrated that 81% of individuals with acute HIV infection had detectable gag-specific CD4+ T cells [16] whereas up to 83% had detectable gag-specific CD8+ T cells [28]. The one participant in whom we could not detect HIV-specific T-cells had detectable CMV-specific CD8+ T cells. Using the HIV MPs, we were unable to detect HIV-specific T cells or their subsets in 1 pre-ART specimen and 3 post-ART specimens. This is consistent with prior studies, in which ART treated individuals have lower frequencies of HIV-specific CD4+ and CD8+ T cells [4, 15, 31]. For the JPT and NIH gag peptide pools, 19/21 (90%) PWH had either a detectable HIV-specific CD4+, memory CD4+ T, cTfh, CD8+ T, or memory CD8+ cells. Overall, our HIV Class I and Class II MP were comparable in their ability to detect HIV-specific responses to the gag peptide pools alone, regardless of acute or chronic infection.
PWH are almost universally co-infected with CMV [32]. Our HIV cohort were all CMV IgG seropositive. We were able to detect CMV-specific CD4+, memory CD4+ T, cTfh, CD8+ T, or memory CD8+ cells in 21/21 (100%) of PWH.
Limitations of this study include a small sample size comprising entirely of men who have sex with men. These individuals comprised both acute infections which were treated early and chronic infections. The frequency of HIV-specific CD4+ T cells vary with duration of viremia and therefore antigen exposure, particularly if the patient is suppressed on ART which removes detectable antigen from the bloodstream versus an elite controller [15]. Our cohort consisted of patients with an estimated date of infection ranging from 21 to 3598 days in our pre-ART specimens and time to undetectable viral load ranging from 81 to 1620 days in our post-ART specimens. Moreover, as these participants were enrolled over 2 decades, there were varying ART regimens which differ from today’s first line treatment options. However, we did not observe a clear correlation with T cell responses and ART used.
In summary, we describe an innovative Class I and Class II HIV MP, reflective of the entire HIV proteome, which can be used in future studies to better understand the full repertoire of HIV-specific CD4+ and CD8+ T cell dynamics. The AIM assay allows for easy quantification of antigen-specific T cells. This methodology permits sorting of live antigen-specific T cells for further functional analyses, allowing for sequencing of CD4+ and CD8+ subsets, including Tfh cells [8]. These HIV-specific CD4+ and CD8+ T cells could be sorted and sequenced in hyperacute infections [3] and/or HIV exposed but seronegative individuals [33] and compared to ART treated individuals or elite controllers to assess transcriptomic differences [2].
Supporting information
(PDF)
(PDF)
Comparison of responses between HIV Class II MP, JPT gag, and NIH gag for HIV-specific total CD4+ T cells in pre-ART (A, p = 0.88 by Friedman test) and post-ART (B, p = 0.22 by Friedman test) specimens, HIV-specific memory CD4+ T cells in pre-ART (C, p = 0.46 by Friedman test) and post-ART (D, p = 0.26 by Friedman test) specimens, and HIV-specific cTfh cells in pre-ART (E, p = 0.70 by Friedman test) and post-ART (F, p = 0.93 by Friedman test) specimens. Data was background subtracted. Data presented represents mean ± standard error of the mean. P-values by Wilcoxon matched-pairs signed rank test.
(EPS)
Comparison of responses between HIV Class I MP, JPT gag, and NIH gag for HIV-specific total CD8+ T cells in pre-ART (A, p = 0.22 by Friedman test) and post-ART (B, p = 0.60 by Friedman test) specimens and HIV-specific memory CD8+ T cells in pre-ART (C, p = 0.41 by Friedman test) and post-ART (D, p = 0.33 by Friedman test) specimens. Data was background subtracted. Data presented represents mean ± standard error of the mean. P-values by Wilcoxon matched-pairs signed rank test.
(EPS)
Class II MP detects CMV-specific (A) total CD4+ T cells, (B) memory CD4+ T cells, and (C) cTfh cells. CMV Class I MP detects CMV-specific (D) total CD8+ T cells and (E) memory CD8+ T cells. Data was background subtracted. Data presented represents mean ± standard error of the mean. P-values by Mann-U Whitney test.
(EPS)
LOD = 0.005.
(XLSX)
Acknowledgments
We want to thank the statistics group at the Antiviral Research Center at UCSD–Gordon Honerkamp-Smith, Christy Anderson, and Allan Wells.
Data Availability
Data is included as S1 Dataset.
Funding Statement
This study has been funded by the NIH NIAID contract Nr. 75N93019C00065 to A.S., R24 AI106039 (Primary Infection Resource Consortium) to Susan Little, R01 AI47821 to S.G., P30 AI036214 (San Diego Center for AIDS Research), and K08 AI135078 to J.D. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Okoye AA, Picker LJ. CD4+ T‐cell depletion in HIV infection: mechanisms of immunological failure. Immunol Rev. 2013;254: 54–64. doi: 10.1111/imr.12066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morou A, Brunet-Ratnasingham E, Dubé M, Charlebois R, Mercier E, Darko S, et al. Altered differentiation is central to HIV-specific CD4+ T cell dysfunction in progressive disease. Nat Immunol. 2019;20: 1059–1070. doi: 10.1038/s41590-019-0418-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ndhlovu ZM, Kazer SW, Nkosi T, Ogunshola F, Muema DM, Anmole G, et al. Augmentation of HIV-specific T cell function by immediate treatment of hyperacute HIV-1 infection. Sci Transl Med. 2019;11: eaau0528. doi: 10.1126/scitranslmed.aau0528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Behrens NE, Wertheimer A, Love MB, Klotz SA, Ahmad N. Evaluation of HIV-specific T-cell responses in HIV-infected older patients with controlled viremia on long-term antiretroviral therapy. Plos One. 2020;15: e0236320. doi: 10.1371/journal.pone.0236320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ford N, Meintjes G, Vitoria M, Greene G, Chiller T. The evolving role of CD4 cell counts in HIV care. Curr Opin Hiv Aids. 2017;12: 123–128. doi: 10.1097/COH.0000000000000348 [DOI] [PubMed] [Google Scholar]
- 6.Le T, Wright EJ, Smith DM, He W, Catano G, Okulicz JF, et al. Enhanced CD4+ T-Cell Recovery with Earlier HIV-1 Antiretroviral Therapy. New Engl J Medicine. 2013;368: 218–230. doi: 10.1056/NEJMoa1110187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maecker H, Maino V. T Cell Immunity to HIV: Defining Parameters of Protection. Curr Hiv Res. 2003;1: 249–259. doi: 10.2174/1570162033485294 [DOI] [PubMed] [Google Scholar]
- 8.Dan JM, Arlehamn CSL, Weiskopf D, Antunes R da S, Havenar-Daughton C, Reiss SM, et al. A Cytokine-Independent Approach To Identify Antigen-Specific Human Germinal Center T Follicular Helper Cells and Rare Antigen-Specific CD4+ T Cells in Blood. J Immunol Baltim Md 1950. 2016;197: 983–93. doi: 10.4049/jimmunol.1600318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Havenar-Daughton C, Reiss SM, Carnathan DG, Wu JE, Kendric K, Peña AT de la, et al. Cytokine-Independent Detection of Antigen-Specific Germinal Center T Follicular Helper Cells in Immunized Nonhuman Primates Using a Live Cell Activation-Induced Marker Technique. J Immunol Baltim Md 1950. 2016;197: 994–1002. doi: 10.4049/jimmunol.1600320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reiss S, Baxter AE, Cirelli KM, Dan JM, Morou A, Daigneault A, et al. Comparative analysis of activation induced marker (AIM) assays for sensitive identification of antigen-specific CD4 T cells. Plos One. 2017;12: e0186998. doi: 10.1371/journal.pone.0186998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Antunes R da S, Paul S, Sidney J, Weiskopf D, Dan JM, Phillips E, et al. Definition of Human Epitopes Recognized in Tetanus Toxoid and Development of an Assay Strategy to Detect Ex Vivo Tetanus CD4+ T Cell Responses. Plos One. 2017;12: e0169086. doi: 10.1371/journal.pone.0169086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grifoni A, Weiskopf D, Ramirez SI, Mateus J, Dan JM, Moderbacher CR, et al. Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell. 2020;181: 1489–1501.e15. doi: 10.1016/j.cell.2020.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moderbacher CR, Ramirez SI, Dan JM, Grifoni A, Hastie KM, Weiskopf D, et al. Antigen-Specific Adaptive Immunity to SARS-CoV-2 in Acute COVID-19 and Associations with Age and Disease Severity. Cell. 2020;183: 996–1012.e19. doi: 10.1016/j.cell.2020.09.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dan JM, Mateus J, Kato Y, Hastie KM, Yu ED, Faliti CE, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021; eabf4063. doi: 10.1126/science.abf4063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ranasinghe S, Flanders M, Cutler S, Soghoian DZ, Ghebremichael M, Davis I, et al. HIV-specific CD4 T cell responses to different viral proteins have discordant associations with viral load and clinical outcome. J Virol. 2011;86: 277–83. doi: 10.1128/JVI.05577-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schieffer M, Jessen HK, Oster AF, Pissani F, Soghoian DZ, Lu R, et al. Induction of Gag-specific CD4 T cell responses during acute HIV infection is associated with improved viral control. J Virol. 2014;88: 7357–66. doi: 10.1128/JVI.00728-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wendel BS, Alcazar DD, He C, Río-Estrada PMD, Aiamkitsumrit B, Ablanedo-Terrazas Y, et al. The receptor repertoire and functional profile of follicular T cells in HIV-infected lymph nodes. Sci Immunol. 2018;3: eaan8884. doi: 10.1126/sciimmunol.aan8884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dhanda SK, Vaughan K, Schulten V, Grifoni A, Weiskopf D, Sidney J, et al. Development of a novel clustering tool for linear peptide sequences. Immunology. 2018;155: 331–345. doi: 10.1111/imm.12984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morris SR, Zhao M, Smith DR, Vargas MV, Little SJ, Gianella S. Longitudinal Viral Dynamics in Semen During Early HIV Infection. Clin Infect Dis. 2016;64: ciw784. doi: 10.1093/cid/ciw784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yusim K, Korber BTM, Barouch D, Koup R, Boer R de, Moore JP, et al. HIV Molecular Immunology 2014. doi: 10.2172/1169681 [DOI] [Google Scholar]
- 21.Grifoni A, Angelo MA, Lopez B, O’Rourke PH, Sidney J, Cerpas C, et al. Global Assessment of Dengue Virus-Specific CD4+ T Cell Responses in Dengue-Endemic Areas. Front Immunol. 2017;8: 1309. doi: 10.3389/fimmu.2017.01309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pro SC, Sidney J, Paul S, Arlehamn CL, Weiskopf D, Peters B, et al. Automatic Generation of Validated Specific Epitope Sets. J Immunol Res. 2015;2015: 763461. doi: 10.1155/2015/763461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kassu A, D’Souza M, O’Connor BP, Kelly-McKnight E, Akkina R, Fontenot AP, et al. Decreased 4-1BB expression on HIV-specific CD4+ T cells is associated with sustained viral replication and reduced IL-2 production. Clin Immunol. 2009;132: 234–245. doi: 10.1016/j.clim.2009.03.531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crotty S. T Follicular Helper Cell Biology: A Decade of Discovery and Diseases. Immunity. 2019;50: 1132–1148. doi: 10.1016/j.immuni.2019.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gianella S, Massanella M, Richman DD, Little SJ, Spina CA, Vargas MV, et al. Cytomegalovirus replication in semen is associated with higher levels of proviral HIV DNA and CD4+ T cell activation during antiretroviral treatment. J Virol. 2014;88: 7818–27. doi: 10.1128/JVI.00831-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dan JM, Massanella M, Smith DM, Spina CA, Schrier R, Daar ES, et al. Brief Report: Effect of CMV and HIV Transcription on CD57 and PD-1 T-Cell Expression During Suppressive ART. J Acquir Immune Defic Syndromes 1999. 2016;72: 133–7. doi: 10.1097/QAI.0000000000000936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pancré V, Delhem N, Yazdanpanah Y, Delanoye A, Delacre M, Depil S, et al. Presence of HIV-1 Nef specific CD4 T cell response is associated with non-progression in HIV-1 infection. Vaccine. 2007;25: 5927–5937. doi: 10.1016/j.vaccine.2007.05.038 [DOI] [PubMed] [Google Scholar]
- 28.Radebe M, Gounder K, Mokgoro M, Ndhlovu ZM, Mncube Z, Mkhize L, et al. Broad and persistent Gag-specific CD8+ T-cell responses are associated with viral control but rarely drive viral escape during primary HIV-1 infection. Aids. 2015;29: 23–33. doi: 10.1097/QAD.0000000000000508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kallas EG, Grunenberg NA, Yu C, Manso B, Pantaleo G, Casapia M, et al. Antigenic competition in CD4 + T cell responses in a randomized, multicenter, double-blind clinical HIV vaccine trial. Sci Transl Med. 2019;11: eaaw1673. doi: 10.1126/scitranslmed.aaw1673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meddows-Taylor S, Shalekoff S, Kuhn L, Gray GE, Tiemessen CT. Development of a whole blood intracellular cytokine staining assay for mapping CD4+ and CD8+ T-cell responses across the HIV-1 genome. J Virol Methods. 2007;144: 115–121. doi: 10.1016/j.jviromet.2007.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chevalier MF, Didier C, Girard P-M, Manea ME, Campa P, Barré-Sinoussi F, et al. CD4 T-Cell Responses in Primary HIV Infection: Interrelationship with Immune Activation and Virus Burden. Front Immunol. 2016;7: 395. doi: 10.3389/fimmu.2016.00395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Christensen-Quick A, Massanella M, Frick A, Rawlings SA, Spina C, Vargas-Meneses M, et al. Subclinical Cytomegalovirus DNA Is Associated with CD4 T Cell Activation and Impaired CD8 T Cell CD107a Expression in People Living with HIV despite Early Antiretroviral Therapy. J Virol. 2019;93. doi: 10.1128/JVI.00179-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ritchie AJ, Campion SL, Kopycinski J, Moodie Z, Wang ZM, Pandya K, et al. Differences in HIV-Specific T Cell Responses between HIV-Exposed and -Unexposed HIV-Seronegative Individuals †. J Virol. 2011;85: 3507–3516. doi: 10.1128/JVI.02444-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
Comparison of responses between HIV Class II MP, JPT gag, and NIH gag for HIV-specific total CD4+ T cells in pre-ART (A, p = 0.88 by Friedman test) and post-ART (B, p = 0.22 by Friedman test) specimens, HIV-specific memory CD4+ T cells in pre-ART (C, p = 0.46 by Friedman test) and post-ART (D, p = 0.26 by Friedman test) specimens, and HIV-specific cTfh cells in pre-ART (E, p = 0.70 by Friedman test) and post-ART (F, p = 0.93 by Friedman test) specimens. Data was background subtracted. Data presented represents mean ± standard error of the mean. P-values by Wilcoxon matched-pairs signed rank test.
(EPS)
Comparison of responses between HIV Class I MP, JPT gag, and NIH gag for HIV-specific total CD8+ T cells in pre-ART (A, p = 0.22 by Friedman test) and post-ART (B, p = 0.60 by Friedman test) specimens and HIV-specific memory CD8+ T cells in pre-ART (C, p = 0.41 by Friedman test) and post-ART (D, p = 0.33 by Friedman test) specimens. Data was background subtracted. Data presented represents mean ± standard error of the mean. P-values by Wilcoxon matched-pairs signed rank test.
(EPS)
Class II MP detects CMV-specific (A) total CD4+ T cells, (B) memory CD4+ T cells, and (C) cTfh cells. CMV Class I MP detects CMV-specific (D) total CD8+ T cells and (E) memory CD8+ T cells. Data was background subtracted. Data presented represents mean ± standard error of the mean. P-values by Mann-U Whitney test.
(EPS)
LOD = 0.005.
(XLSX)
Data Availability Statement
Data is included as S1 Dataset.