Abstract
Objective
Based on the increasing incidence of smell and taste dysfunction among coronavirus disease 2019 (COVID-19) patients, such issues have been considered an early symptom of infection. However, few studies have investigated the type of taste components that are most frequently affected in COVID-19 patients. This study investigated the difference in frequencies of the types of taste component disorders among hospitalized COVID-19 patients.
Methods
In this retrospective, single-center, observational study, patients' background characteristics, clinical course, laboratory and radiological findings, and details on taste and/or smell disorders were collected and analyzed from medical records.
Patients
A total of 227 COVID-19 patients were enrolled, among whom 92 (40.5%) complained of taste disorders.
Results
Multiple types of taste disorders (hypogeusia/ageusia and hypersensitivity, or hypersensitivity and changing tastes) were reported in 10 patients. In particular, 23 patients reported hypersensitivity to at least 1 type of taste, and 2 patients complained of a bitter taste on consuming sweet foods. Impairment of all taste components was found in 48 patients (52.2%). The most frequent taste disorder was salty taste disorder (81 patients, 89.0%). Hypersensitivity to salty taste was most frequently observed (19 patients, 20.9%).
Conclusion
Patients with COVID-19 develop multiple types of taste disorders, among which salty taste disorder was the most frequent, with many patients developing hypersensitivity to salty taste. As smell and taste are subjective senses, further studies with the combined use of objective examinations will be required to confirm the findings.
Keywords: SARS-CoV-2, taste-impaired, salty, hypersensitivity
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for coronavirus disease 2019 (COVID-19), emerged at the end of 2019. SARS-CoV-2 has rapidly spread worldwide, and many clinical studies have demonstrated that this virus can be transmitted from person to person via droplet inhalation. When preparing this manuscript on November 19, 2021, the World Health Organization confirmed 254,847,065 COVID-19 cases worldwide, and 1,726,063 cases were confirmed by the Ministry of Health, Labor, and Welfare in Japan.
Symptoms of COVID-19 include a fever, fatigue, sore throat, cough, and dyspnea. Recently, the loss or sensory disorder of taste and/or smell has been considered a key symptom of SARS-CoV-2 infection (1). Smell or taste dysfunction is common in upper respiratory tract infections (2-4), and there have been several studies on smell or taste dysfunction in COVID-19 patients. Lechien et al. showed that olfactory and gustatory dysfunctions were observed in 85.6% and 88.0% of COVID-19 patients, respectively (5). Based on the increasing awareness of these symptoms as potential early symptoms of COVID-19, “new loss of smell or taste” was recently added to the list of COVID-19 symptoms by the Centers for Disease Control and Prevention.
The basic tastes for humans include salty, sour, sweet, bitter, and umami (6). We detect taste using taste receptor cells present in the taste buds on the tongue and palate (7). Taste is mainly controlled by four nerves: the chorda tympani and greater petrosal nerves, which are branches of the facial nerve (VII), the glossopharyngeal nerve (IX), and the vagus nerve (X), which transmits signals to the nucleus of the solitary tract in the brain stem (6). Furthermore, there are different taste perception receptors: sweet, bitter, and umami are facilitated by G protein-coupled taste receptors, while salty and sour are facilitated by ion channels (8).
Many COVID-19 patients complain of taste disorders. However, to our knowledge, no studies have described the types of taste components most frequently affected. This study retrospectively investigated the difference in the frequencies of the types of taste component disorders in hospitalized patients with polymerase chain reaction (PCR)-confirmed COVID-19 in Japan.
Materials and Methods
This retrospective study was conducted at a single center, Juntendo University Urayasu Hospital, and was approved by the local ethics committee of the Juntendo University Urayasu Hospital (Institutional Review Board No. 20-04-310). The requirement for informed consent was waived due to the retrospective nature of the study.
A consecutive series of hospitalized patients were evaluated between March 26, 2020, the day the first patient was admitted, and March 26, 2021. All cases were confirmed using CoV-2 PCR. The study excluded patients with the following characteristics: age <14 years old, severe or critical status, and current comorbidities that made communication difficult during the interview. In brief, we included patients with mild-to-moderate COVID-19 as we focused on the prevalence of olfactory and gustatory disorders. Data were collected and analyzed by four authors (Y.N., T.O., K.S., and Y.S.), and the accuracy and completeness of the data were verified.
Administrative data were extracted from the hospital database. We classified the patients' disease severity based on the Guidelines on the Diagnosis and Treatment of the Novel Coronavirus issued by the Ministry of Health, Labour, and Welfare in Japan at the time of admission or diagnosis in the case of hospital-onset. In brief, mild cases were defined as those with no clinical or radiological signs of pneumonia. Patients with moderate disease I had any clinical or radiological sign of pneumonia without de-saturation (defined as percutaneous oxygen saturation >93%), and those with moderate disease II had de-saturation with pneumonia. Severe cases were defined as patients who required mechanical ventilation support or admittance to the intensive-care unit. Patients were asked about their symptoms, including fever, cough, dyspnea, sore throat, smell status, and taste status. In addition, we enquired about the taste status in further detail: What type of taste is affected? How is the sense of taste (weakened, lost, enhanced)? How long has it been affected?
Patients underwent blood tests [white blood cell count, lymphocyte count, lactate dehydrogenase (LDH), C-reactive protein (CRP), ferritin, D-dimer, and fibrin degradation product levels] and chest computed tomography (CT). Their histories of allergies, smoking, and comorbidities (hypertension, diabetes mellitus, bronchial asthma, cardiovascular diseases, autoimmune diseases, etc.) were also recorded.
Fisher's exact test was used to compare categorical variables between COVID-19 patients with and without smell or taste disorders. The t-test was used to compare the continuous quantitative variables. Statistical significance in this study was defined as p value <0.05. Data were analyzed using the Prism 8 software program (GraphPad Software, La Jolla, USA).
Results
Patients' characteristics, disease severity, and outcomes
The flow diagram of the study is presented in Figure. Of the 273 patients with COVID-19, 227 were ultimately enrolled. Forty-six patients were excluded: 14 patients were <14 years old, 12 had critical health conditions and could not communicate while in the hospital, and 20 were unable to accurately communicate because of prevalent comorbidities (i.e. cerebral infarction and dementia).
Figure.
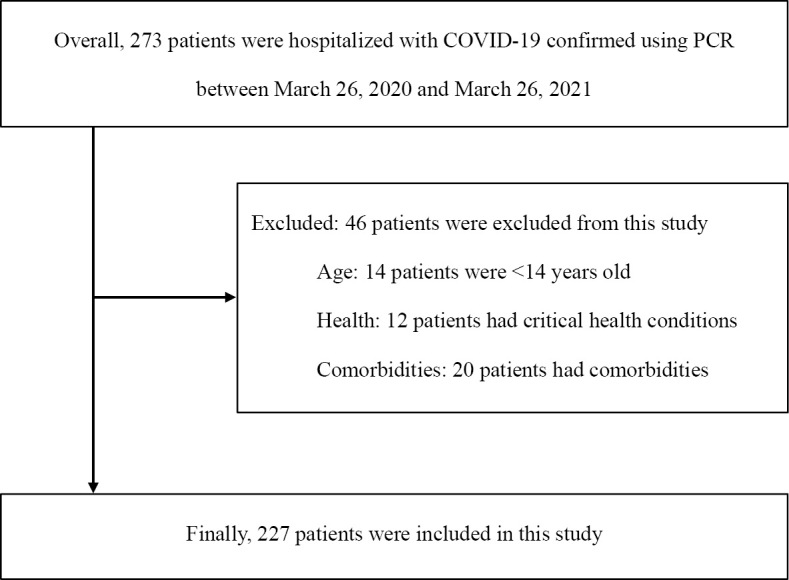
Flow chart of patient selection. COVID-19: coronavirus disease 2019, PCR: polymerase chain reaction
Table 1 shows the patients' characteristics, disease severity, and outcomes. The study included 136 men and 91 women with a mean age of 50.8±18.7 (range: 15-91) years old and a median age of 52 (interquartile range: 34-66) years old. A total of 218 patients (96.0%) were Japanese. Forty-nine patients were current smokers, and 55 were former smokers. The most prevalent comorbidities were hypertension (n=57, 25.1%), diabetes mellitus (n=43, 18.9%), hyperlipidemia (n=29, 12.8%), bronchial asthma (n=29, 12.8%), cardiovascular diseases (n=33, 14.5%), and autoimmune diseases (n=15, 6.6%). Furthermore, 29 patients had malignancies (12.8%), including lung cancer, malignant lymphoma, and colon cancer. Among the 227 patients enrolled, 7 had no symptoms or signs of COVID-19. In addition, the number of mild, moderate I, moderate II, and severe cases was 56 (24.7%), 102 (44.9%), 43 (18.9%), and 19 (8.4%), respectively. Nine patients died of COVID-19.
Table 1.
Clinical Characteristics of Patients with COVID-19.
| Characteristics | Total (n=227) |
|---|---|
| Age, years | 52 (34-66) |
| Sex | |
| Male | 136 (59.9) |
| Female | 91 (40.1) |
| Race | |
| Japanese | 218 (96.0) |
| Asian (other than Japanese) | 6 (2.6) |
| Others | 3 (1.3) |
| Smoking history | |
| Never | 123 (54.2) |
| Current | 49 (21.6) |
| Past | 55 (24.2) |
| Comorbidities | |
| Any | 149 (65.6) |
| Hypertension | 57 (25.1) |
| Diabetes mellitus | 43 (18.9) |
| Hyperlipidemia | 29 (12.8) |
| Bronchial asthma | 29 (12.8) |
| Chronic obstructive pulmonary disease | 3 (1.3) |
| Malignancy | 29 (12.8) |
| Cardiovascular diseases | 33 (14.5) |
| Autoimmune diseases | 15 (6.6) |
| Disease severity | |
| Asymptomatic | 6 (2.6) |
| Mild | 57 (25.1) |
| Moderate I | 102 (44.9) |
| Moderate II | 43 (18.9) |
| Severe | 19 (8.4) |
| Outcomes | |
| Ongoing hospitalization | 2 (0.9) |
| Discharge to home | 213 (93.8) |
| Transfer to other hospitals | 3 (1.3) |
| Died | 9 (4.0) |
Data are shown as median (interquartile range) or number (%)
Symptoms, radiological findings, and laboratory findings
The general symptoms experienced by the patients are presented in Table 2. Overall, 222 patients (97.8%) had ≥1 symptom. A fever (n=204, 89.8%) was the most prevalent symptom, followed by fatigue (n=146, 64.3%) and cough (n=139, 61.2%). A diagnosis of pneumonia was confirmed using chest CT or radiography; in total, 160 patients (70.5%) with COVID-19 were identified as having pneumonia at admission or on the day of confirmation of COVID-19 with reverse transcription PCR. Ten patients did not undergo chest CT or radiography because of pregnancy, doctors' judgments, or personal unwillingness.
Table 2.
Clinical Signs and Symptoms of Patients with COVID-19.
| Signs and symptoms | Total (n=227) |
|---|---|
| Any | 222 (97.8) |
| Fevera | 204 (89.8) |
| Fatigue | 146 (64.3) |
| Cough | 139 (61.2) |
| Disorder of smellb | 88 (38.9) |
| Disorder of taste | 92 (40.5) |
| Blocked nosec | 39 (17.6) |
| Running nosed | 39 (17.5) |
Data are shown as number (%).
aFever was defined as body temperature >37.5°C.
bThere was no record of smell disorder for one patient.
cThere was no record of blocked nose for six patients.
dThere was no record of running nose for four patients.
The laboratory findings on admission are presented in Table 3. A total of 112 patients (49.6%, one patient was not tested) were found to have lymphopenia (the lymphocyte count was <1,000/μL) on admission, and 117 (52.9%, six patients were not tested) had elevated ferritin levels (>300 ng/mL) on admission. CRP levels were increased in 133 patients (58.6%), while LDH levels were increased in 89 patients (39.2%).
Table 3.
Laboratory Findings of Patients with COVID-19.
| Laboratory values | Total (n=227) |
|---|---|
| White blood cell count, cells/μL | 5,000 (3,800-6,700) |
| Neutrophil counta, cells/μL | 3,305 (2,255-4,673) |
| Lymphocyte counta, cells/μL | 1,010 (680-1,333) |
| Neutrophil-to-lymphocyte ratioa | 3.35 (1.92-5.86) |
| Lactate dehydrogenase, IU/L | 221 (170-295) |
| C-reactive protein, mg/dL | 1.60 (0.30-5.40) |
| Ferritin, ng/mLb | 329 (149-699) |
| Procalcitonin, ng/mLc | 0.07 (0.05-0.11) |
Data are shown as median (interquartile range).
aNot measured in one patient.
bNot measured in six patients.
cNot measured in 27 patients.
Treatments for patients with COVID-19
As presented in Table 4, 93 (43.2%) patients with COVID-19 received treatment, of whom 71 (72.5%) were treated with corticosteroids, including dexamethasone, followed by remdesivir (n=33, 33.7%), heparin (n=29, 29.6%), nafamostat (n=25, 25.5%), favipiravir (n=12, 12.2%), and tocilizumab (n=6, 6.1%). Medications for the treatment of olfactory or gustatory dysfunction were not used because of the lack of useful evidence. Five patients required intubation and mechanical ventilation, and two were treated with extracorporeal membrane oxygenation.
Table 4.
Treatment of Patients with COVID-19.
| Treatment | Total (n=227) |
|---|---|
| Any | 93 (43.2) |
| Remdesivir (Veklury®) | 33 (33.7) |
| Favipiravir (Abigan®) | 12 (12.2) |
| Corticosteroids | 71 (72.5) |
| Tocilizumab (Actemra®) | 6 (6.1) |
| Heparin | 29 (29.6) |
| Nafamostat (Futhan®) | 25 (25.5) |
| Intubation | 5 (5.2) |
| ECMO | 2 (2.1) |
Data are presented as numbers (%). Percentages were based on data of 93 patients (100%).
ECMO: extracorporeal membrane oxygenation
Smell disorder in patients with COVID-19
Smell disorder was reported in 88 patients (38.8%) (Table 2). COVID-19 patients with smell disorders were significantly younger, more likely to be women, and had fewer comorbidities than those without smell disorders. Laboratory data showed that COVID-19 patients with smell disorder had significantly lower white blood cell counts, neutrophil counts, ferritin levels, CRP levels, and LDH levels and higher lymphocyte counts than those without smell disorder (Table 5). The time from the disease onset to the onset of smell disorder ranged from 0-12 days, and the mean was 3.2 days. The recovery time for smell disorder was 10 days, with none of the patients receiving any therapy.
Table 5.
Clinical Characteristics of COVID-19 Patients with/without Smell Disorder.
| Characteristics | Presence of smell disorder group (n=88) c |
Absence of smell disorder group (n=138)d |
p value | ||
|---|---|---|---|---|---|
| Number | % | Number | % | ||
| Age, years | 43.59±16.32 | 55.41±18.70 | <0.0001c | ||
| Sex | |||||
| Male | 39 | 44.3 | 97 | 70.3 | 0.0002a |
| Female | 49 | 55.7 | 41 | 29.7 | |
| History | |||||
| Non-smoker | 54 | 61.4 | 69 | 50.0 | 0.10a |
| Comorbidities (any) | 46 | 52.3 | 102 | 73.9 | 0.001a |
| Symptoms | |||||
| Feverd | 80 | 90.9 | 123 | 89.1 | 0.8223a |
| Taste disorder | 69 | 78.4 | 22 | 15.9 | <0.0001a |
| Findings | |||||
| Pneumoniae | 57 | 70.4 | 103 | 76.9 | 0.334a |
| Outcomes | |||||
| Death | 0 | 0 | 9 | 6.52 | 0.01a |
| Disease severity | |||||
| Mild | 29 | 33.0 | 27 | 19.6 | <0.0001b |
| Moderate I | 50 | 56.8 | 52 | 37.7 | |
| Moderate II | 7 | 8.0 | 36 | 26.1 | |
| Severe | 2 | 2.3 | 17 | 12.3 | |
| Laboratory values | |||||
| White blood cell count, cells/μL | 5,017±1,696 | 5,872±3,144 | 0.02c | ||
| Neutrophil count, cells/μL | 3,319±1,681 | 4,261±2,962 | 0.007c | ||
| Lymphocyte count, cells/μL | 1,164±512.3 | 1,016±530.8 | 0.04c | ||
| NLR | 3.744±3.367 | 6.204±9.241 | 0.02c | ||
| Ferritin, ng/mL | 363.4±388.1 | 657.8±756.3 | 0.0009c | ||
| C-reactive protein, mg/dL | 2.438±4.002 | 4.466±5.109 | 0.002c | ||
| Lactate dehydrogenase, IU/L | 222.0±89.47 | 298.2±209.7 | 0.001c | ||
Data are shown as mean±standard deviation or number (%). N/A: no analysis. NLR: neutrophil-to-lymphocyte ratio.
aFisher's exact test.
bChi-square test.
cUnpaired t-test.
dFever was defined as body temperature >37.5˚C.
ePneumonia was confirmed using chest computed tomography or radiography.
Taste disorder in patients with COVID-19
Ninety-two patients (40.5%) complained of taste disorders (Table 2). COVID-19 patients with taste disorders had a significantly higher rate of a fever than those without taste disorders. However, there were no marked differences in the sex, age, or presence of medical conditions between the two groups (Table 6). There were also no significant differences in laboratory data between COVID-19 patients with and without taste disorder. The time from the disease onset to the onset of taste disorder ranged from 0-14 days, and the mean was 3.3 days. The median recovery time for taste disorder was 9 days, with none of the patients receiving any specific therapy.
Table 6.
Clinical Characteristics of COVID-19 Patients with/without Taste Disorder.
| Characteristics | Presence of taste disorder group (n=92)c |
Absence of taste disorder group (n=135) |
p value | ||
|---|---|---|---|---|---|
| Number | % | Number | % | ||
| Age, years | 47.78±17.35 | 52.85±19.34 | 0.04c | ||
| Sex | |||||
| Male | 46 | 50.0 | 90 | 66.7 | 0.01a |
| Female | 46 | 50.0 | 45 | 33.3 | |
| History | |||||
| Non-smoker | 48 | 52.8 | 74 | 54.8 | 0.79a |
| Comorbidities (any) | 55 | 59.8 | 94 | 69.6 | 0.15a |
| Symptoms | |||||
| Feverd | 88 | 95.7 | 116 | 87.2 | 0.04a |
| Smell disorder | 69 | 75.0 | 19 | 14.0 | <0.0001a |
| Findings | |||||
| Pneumoniae | 63 | 73.26 | 97 | 75.19 | 0.75a |
| Outcomes | |||||
| Death | 1 | 1.1 | 8 | 5.93 | 0.09a |
| Disease severity | |||||
| Mild | 28 | 30.4 | 29 | 21.5 | 0.015b |
| Moderate I | 51 | 55.4 | 51 | 37.8 | |
| Moderate II | 10 | 10.9 | 33 | 24.4 | |
| Severe | 3 | 3.3 | 16 | 11.9 | |
| Laboratory values | |||||
| White blood cell count, cells/μL | 5,173±2,073 | 5,766±3,045 | 0.10c | ||
| Neutrophil count, cells/μL | 3,501±2,064 | 4,140±2,861 | 0.07c | ||
| Lymphocyte count, cells/μL | 1,141±514.8 | 1031±533.3 | 0.13c | ||
| NLR | 4.151±4.283 | 5.960±9.139 | 0.08c | ||
| Ferritin, ng/mL | 459.7±555.1 | 595.7±705.3 | 0.13c | ||
| C-reactive protein, mg/dL | 2.962±4.414 | 4.136±5.004 | 0.07c | ||
| Lactate dehydrogenase, IU/L | 240.9±117.9 | 286.7±205.5 | 0.055c | ||
| Type of taste disorder | |||||
| Hypogeusia/ageusia | 76 (82.6)f | ||||
| Hypersensitivity | 23 (25.0)f | ||||
| Changing | 2 (2.2)f | ||||
Data are shown as mean±standard deviation or number (%). N/A: no analysis. NLR: neutrophil-to-lymphocyte ratio.
aFisher's exact test.
bChi-square test.
cUnpaired t-test.
dFever was defined as body temperature >37.5˚C.
ePneumonia was confirmed using chest computed tomography or radiography.
fTen patients complained about hypogeusia/ageusia and hypersensitivity of taste disorder, or hypersensitivity of taste disorder and changing taste.
Among those with taste disorders, 76 patients (82.6%) complained of hypogeusia/ageusia. Interestingly, 23 patients (25.0%) reported hypersensitivity to taste, and 2 complained of bitter taste on consuming sweet foods. Furthermore, nine patients complained of hypogeusia/ageusia and hypersensitivity to taste, and one complained of hypersensitivity to taste and changing tastes (Table 6).
We interviewed patients with taste disorders to understand the type of taste affected (i.e. salty, sour, sweet, bitter, and umami) (Table 7). For one patient, there were no records regarding the taste disorder. All taste component disorders were observed in 48 (52.2%) patients (data not shown). The most frequently affected taste was salty (n=81, 89.0%), followed by sweet (n=63, 69.2%) and umami (62 patients, 68.1%). Surprisingly, as far as hypersensitivity to taste was concerned, it was most frequently observed for salty taste (n=19 patients, 20.9%); in contrast, no patients complained of hypersensitivity to umami taste.
Table 7.
Characteristics of Taste Disorder.
| Types | Type of taste disorder (n=91a) | |||
|---|---|---|---|---|
| Hypogeusia/ageusia | No change | Hypersensitivity | Changing to other taste | |
| Salty | 62 (68.1) | 10 (11.0) | 19 (20.9) | 0 (0.0) |
| Sweet | 59 (64.8) | 28 (30.8) | 2 (2.2) | 2 (2.2)b |
| Bitter | 57 (62.6) | 30 (33.0) | 4 (4.4) | 0 (0.0) |
| Sour | 58 (63.7) | 31 (34.1) | 2 (2.2) | 0 (0.0) |
| Umami | 62 (68.1) | 29 (31.9) | 0 (0.0) | 0 (0.0) |
Data are shown as number (%).
aFor one patient, there was no record of taste disorder.
bBoth patients complained of bitter taste when they ate sweet foods.
Discussion
There were several taste disorder types associated with COVID-19; disorders of the salty taste were the most frequent, and some patients with COVID-19 complained of a lost or weakened sense of taste and also of an enhanced sense or taste. Recent studies have shown that olfactory and gustatory disorders are prevalent and important diagnostic symptoms of COVID-19 (5-9). Furthermore, our study indicated that clinicians should not only ask patients whether or not they could taste food items but also ask whether or not they have experienced any change in their sense of taste, including loss or enhancement of the five taste components (salty, sweet, bitter, sour, and umami).
In our study, 88 patients (38.8%) complained of smell disorders (Table 2). The prevalence of smell disorder has varied among different studies (10-14). Moein et al. reported that the rate of smell disorder was 59/60 (98.3%) among patients with COVID-19 (12). In contrast, Lee et al. demonstrated that the rate of smell disorder was only 4.23% (13). Our findings lie within the range of data reported by Meng et al., where the prevalence of smell disorders ranged from 34-68% (15).
Furthermore, our study demonstrates that olfactory and gustatory disorders are more prevalent in women than in men, which is consistent with previous findings (5,11). Thus, our patient population was not likely to be highly biased compared with previous studies. Similarly, 40.5% of the patients in our study had taste disorders, which was more frequent than smell disorders (38.8%) (Table 2). The taste disorder rates have varied among studies (16,17); Song et al. showed that taste disorders were more frequent than smell disorders (21% vs. 11%) (16). These are very important findings, since they suggest that olfactory and gustatory disturbances are caused by different pathways.
In our study, the median recovery time for taste disorder was nine days, which is consistent with previous findings (18-20). The lifespan of taste bud cells is approximately 250±50 hours (21), which suggests that taste bud cells may be irreversibly damaged by SARS-CoV-2 itself, inflammatory cytokines, or other entities. In addition, our data showed that patients with mild disease were more likely to complain of taste or smell disorders than those with severe disease. This finding was consistent with a previous study (22), although another study showed that there was no correlation with disease severity (16). This difference may be due to differences in enrolled patients and analysis methods. Taste and smell disorders are largely subjective, and it may be that patients with mild disease are likely to be more aware of taste and smell disorders than those with severe disease because their other symptoms, such as fatigue and dyspnea, are less severe than in patients with more severe disease. More objective examinations are thus required for subsequent evaluations.
In addition, salty taste was the most impaired among the five taste types (Table 7), which was consistent with previous findings (23,24). Furthermore, 52% of COVID-19 patients experienced taste disorder in all taste components. However, this is an important finding for elucidating how taste is disrupted after SARS-CoV-2 infection, and there may be certain pathways associated with taste disorders. There are many hypotheses concerning the causes of taste and smell disorders (1,10,25-35). Several studies have reported a mixed pathogenesis of taste and smell disorders, as these senses are very closely associated with each other and influence each other. Mahmoud et al. summarized nine major pathogeneses of taste disorders: neurotropism, cytotoxicity and direct damage, renin-angiotensin-system and angiotensin II imbalances, augmented cytokine production, disturbances in salivary glands and sialic acid production, systemic diseases, zinc metabolism, and exposure to drugs (36). This study was unable to strongly suggest neurotropism because olfactory and gustatory disturbances are generally caused by central nervous system (CNS) involvement, and why patients had partial taste component disorders was unclear. The same reasons apply to cytokines, systemic diseases, and drugs. In contrast, this study supported routes of cytotoxicity, direct injury, and imbalances in the renin-angiotensin system and angiotensin II.
Generally, taste is recognized by the taste buds. Taste buds contain cells classified as types I, II, III, and basal cells, sometimes termed type IV cells (37). We believe that type I cells have a supportive role, similar to the glial cells in the nervous system; type II cells are responsible for recognizing sweet, bitter, and umami tastes, and type III cells are responsible for sour taste. Recently, type I cells have been shown to recognize salty taste (38). Therefore, only certain taste abnormalities can occur because of direct damage to these cells. In addition, types II and III cells express angiotensin-converting enzyme 2 (ACE2) (39), which is associated with COVID-19-induced dysgeusia (27-40), suggesting imbalances in the renin-angiotensin system and angiotensin II. Interestingly, in type I cells, which recognize the salty taste, ACE2 expression has not been measured (39). Therefore, this measurement may be an important clue to elucidate the mechanism of taste impairment due to SARS-CoV-2 infection.
It is also interesting to note that while most patients in our study lost their sense of taste, some developed hypersensitivity to taste. To our knowledge, there are no studies on this subject. The reason for this might be that the patients perceive only one taste as being stronger than the others because the other tastes have been impaired. Another possible reason is that type I cells, which recognize salty taste, overreact and cause a strong sensation. In any case, the cause of this phenomenon should be verified in future studies, possibly providing a clue to the cause of taste disorders in COVID-19 patients. Interestingly, two patients misidentified sweet taste as bitter. Sweetness and bitterness are taste sensations that are recognized by the same type 2 cells. In other words, an abnormality in type 2 cells may have led to this misidentification. The cause of these events remains unknown, and further verification is required.
Several limitations associated with the present study warrant mention. First, this was a single-center, retrospective study with small sample size. We must also consider the bias related to information, local factors, etc. Therefore, we cannot strongly suggest that the salty taste is most sensitive to taste disorders in COVID-19 patients. However, to our knowledge, the present study is the first detailed study on taste disorders. The number of COVID-19 patients is increasing worldwide; thus, further studies are required to confirm our findings. Second, since our study only focused on hospitalized patients with set exclusion criteria, there is a possibility of patient selection bias. A previous report on COVID-19 showed that the mortality rate was 1.4% (41); in contrast, 9 patients (4.0%) with COVID-19 died in our study. However, while our study has some biases, including selection bias, we were able to ask patients hospitalized with mild-to-moderate COVID-19 symptoms about their smell and taste disorders in detail. Third, we used a self-reported evaluation tool for smell and taste disorders, and all symptoms and medical histories were self-reported; this was a subjective evaluation and not an objective one, as our patients did not undergo nasal endoscopy, specific imaging, or an objective smell assessment, all of which yield objective results. Furthermore, nasal endoscopy is associated with a high risk of COVID-19 transmission; therefore, we were unable to perform it in the early term. As smell and taste are considered subjective senses, there may be cases in which patients experience smell and/or taste disorders without any abnormal findings. Furthermore, we did not perform objective examinations because we believed that questionnaires would be a quicker, easier, and safer method of collecting data than objective examinations. Fourth, we were unable to observe the duration of symptoms in the taste components. If there are differences in the recovery period of each taste component, it would help to elucidate the pathogenesis of this coronavirus. Fifth, zinc metabolism has been suggested to cause taste disorders (36). Therefore, the blood zinc level should be measured; however, we did not measure the zinc level in this study and thus were unable to conduct such evaluations. Finally, certain drugs can also cause taste disorders (36). Thus, we considered the influence of drugs but could not evaluate it in detail because of the small number of cases. These limitations should be addressed in future studies investigating and characterizing smell and taste dysfunction in COVID-19 patients.
In conclusion, our study demonstrated that there are several types of taste disorders associated with COVID-19. Salty taste disorder was most frequently observed in COVID-19 patients. These findings will help clinicians make accurate and early diagnoses of COVID-19.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Xydakis MS, Dehgani-Mobaraki P, Holbrook EH, et al. Smell and taste dysfunction in patients with COVID-19. Lancet Infect Dis 20: 1015-1016, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mullol J, Del Cuvillo A, Lockey RF. Rhinitis phenotypes. J Allergy Clin Immunol Pract 8: 1492-1503, 2020. [DOI] [PubMed] [Google Scholar]
- 3.Jaume F, Quintó L, Alobid I, Mullol J. Overuse of diagnostic tools and medications in acute rhinosinusitis in Spain: a population-based study (the PROSINUS study). BMJ Open 8: e018788, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cavazzana A, Larsson M, Münch M, Hähner A, Hummel T. Postinfectious olfactory loss: a retrospective study on 791 patients. Laryngoscope 128: 10-15, 2018. [DOI] [PubMed] [Google Scholar]
- 5.Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol 277: 2251-2261, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braud A, Boucher Y. Taste disorder's management: a systematic review. Clin Oral Investig 24: 1889-1908, 2020. [DOI] [PubMed] [Google Scholar]
- 7.Li F. Taste perception: from the tongue to the testis. Mol Hum Reprod 19: 349-360, 2013. [DOI] [PubMed] [Google Scholar]
- 8.Behrens M, Meyerhof W. A role for taste receptors in (neuro)endocrinology? J Neuroendocrinol 31: e12691, 2019. [DOI] [PubMed] [Google Scholar]
- 9.Yan CH, Faraji F, Prajapati DP, Boone CE, DeConde AS. Association of chemosensory dysfunction and COVID-19 in patients presenting with influenza-like symptoms. Int Forum Allergy Rhinol 10: 806-813, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 77: 683-690, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giacomelli A, Pezzati L, Conti F, et al. Self-reported olfactory and taste disorders in patients with severe acute respiratory coronavirus 2 infection: a cross-sectional study. Clin Infect Dis 71: 889-890, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moein ST, Hashemian SM, Mansourafshar B, Khorram-Tousi A, Tabarsi P, Doty RL. Smell dysfunction: a biomarker for COVID-19. Int Forum Allergy Rhinol 10: 944-950, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee Y, Min P, Lee S, Kim SW. Prevalence and duration of acute loss of smell or taste in COVID-19 patients. J Korean Med Sci 35: e174, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klopfenstein T, Kadiane-Oussou NJ, Toko L, et al. Features of anosmia in COVID-19. Med Mal Infect 50: 436-439, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meng X, Deng Y, Dai Z, Meng Z. COVID-19 and anosmia: a review based on up-to-date knowledge. Am J Otolaryngol 41: 102581, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Song J, Deng YK, Wang H, et al. Self-reported taste and smell disorders in patients with COVID-19: distinct features in China. Curr Med Sci 41: 14-23, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Izquierdo-Domínguez A, Rojas-Lechuga MJ, Chiesa-Estomba C, et al. Smell and taste dysfunction in COVID-19 is associated with younger age in ambulatory settings: a multicenter cross-sectional study. J Investig Allergol Clin Immunol 30: 346-357, 2020. [DOI] [PubMed] [Google Scholar]
- 18.Levinson R, Elbaz M, Ben-Ami R, et al. Time course of anosmia and dysgeusia in patients with mild SARS-CoV-2 infection. Infect Dis (Lond) 52: 600-602, 2020. [DOI] [PubMed] [Google Scholar]
- 19.Villarreal IM, Morato M, Martínez-RuizCoello M, et al. Olfactory and taste disorders in healthcare workers with COVID-19 infection. Eur Arch Otorhinolaryngol 278: 2123-2127, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Çalıca Utku A, Budak G, Karabay O, Güçlü E, Okan HD, Vatan A. Main symptoms in patients presenting in the COVID-19 period. Scott Med J 65: 127-132, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beidler LM, Smallman RL. Renewal of cells within taste buds. J Cell Biol 27: 263-272, 1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA 323: 2089-2090, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salmon Ceron D, Bartier S, Hautefort C, et al. Self-reported loss of smell without nasal obstruction to identify COVID-19. The multicenter Coranosmia cohort study. J Infect 81: 614-620, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parma V, Ohla K, Veldhuizen MG, et al. More than smell-COVID-19 is associated with severe impairment of smell, taste, and chemesthesis. Chem Senses 45: 609-622, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Almeria M, Cejudo JC, Sotoca J, Deus J, Krupinski J. Cognitive profile following COVID-19 infection: clinical predictors leading to neuropsychological impairment. Brain Behav Immun Health 9: 100163, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freni F, Meduri A, Gazia F, et al. Symptomatology in head and neck district in coronavirus disease (COVID-19): a possible neuroinvasive action of SARS-CoV-2. Am J Otolaryngol 41: 102612, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eshraghi AA, Mirsaeidi M, Davies C, Telischi FF, Chaudhari N, Mittal R. Potential mechanisms for COVID-19 induced anosmia and dysgeusia. Front Physiol 11: 1039, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ho BE, Ho AP, Ho MA, Ho EC. Case report of familial COVID-19 cluster associated with high prevalence of anosmia, ageusia, and gastrointestinal symptoms. IDCases 22: e00975, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fantozzi PJ, Pampena E, Di Vanna D, et al. Xerostomia, gustatory and olfactory dysfunctions in patients with COVID-19. Am J Otolaryngol 41: 102721, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sato T, Ueha R, Goto T, Yamauchi A, Kondo K, Yamasoba T. Expression of ACE2 and TMPRSS2 proteins in the upper and lower aerodigestive tracts of rats: implications on COVID 19 infections. Laryngoscope 131: E932-E939, 2021. [DOI] [PubMed] [Google Scholar]
- 31.Cazzolla AP, Lovero R, Lo Muzio L, et al. Taste and smell disorders in COVID-19 patients: role of interleukin-6. ACS Chem Neurosci 11: 2774-2781, 2020. [DOI] [PubMed] [Google Scholar]
- 32.Agyeman AA, Chin KL, Landersdorfer CB, Liew D, Ofori-Asenso R. Smell and taste dysfunction in patients with COVID-19: a systematic review and meta-analysis. Mayo Clin Proc 95: 1621-1631, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lozada-Nur F, Chainani-Wu N, Fortuna G, Sroussi H. Dysgeusia in COVID-19: possible mechanisms and implications. Oral Surg Oral Med Oral Pathol Oral Radiol 130: 344-346, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pellegrino R, Cooper KW, Di Pizio A, Joseph PV, Bhutani S, Parma V. Corona viruses and the chemical senses: past, present, and future. Chem Senses 45: 415-422, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aziz M, Perisetti A, Lee-Smith WM, Gajendran M, Bansal P, Goyal H. Taste changes (dysgeusia) in COVID-19: a systematic review and meta-analysis. Gastroenterology 159: 1132-1133, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mahmoud MM, Abuohashish HM, Khairy DA, Bugshan AS, Khan AM, Moothedath MM. Pathogenesis of dysgeusia in COVID-19 patients: a scoping review. Eur Rev Med Pharmacol Sci 25: 1114-1134, 2021. [DOI] [PubMed] [Google Scholar]
- 37.Chaudhari N, Roper SD. The cell biology of taste. J Cell Biol 190: 285-296, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vandenbeuch A, Clapp TR, Kinnamon SC. Amiloride-sensitive channels in type I fungiform taste cells in mouse. BMC Neurosci 9: 1, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cooper KW, Brann DH, Farruggia MC, et al. COVID-19 and the chemical senses: supporting players take center stage. Neuron 107: 219-233, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alexandre J, Cracowski JL, Richard V, Bouhanick B. Renin-angiotensin-aldosterone system and COVID-19 infection. Ann Endocrinol (Paris) 81: 63-67, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382: 1708-1720, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]


