Abstract
Surface disinfection is part of school protocols designed to decrease the risk of students and staff contracting COVID-19. However, exposure to disinfectants can have short- and long-term health consequences. Given that the risks are well-described and safer products are readily available, it is critical that schools consciously employ safer disinfection strategies.
Keywords: Asthma, Child, Disinfectants
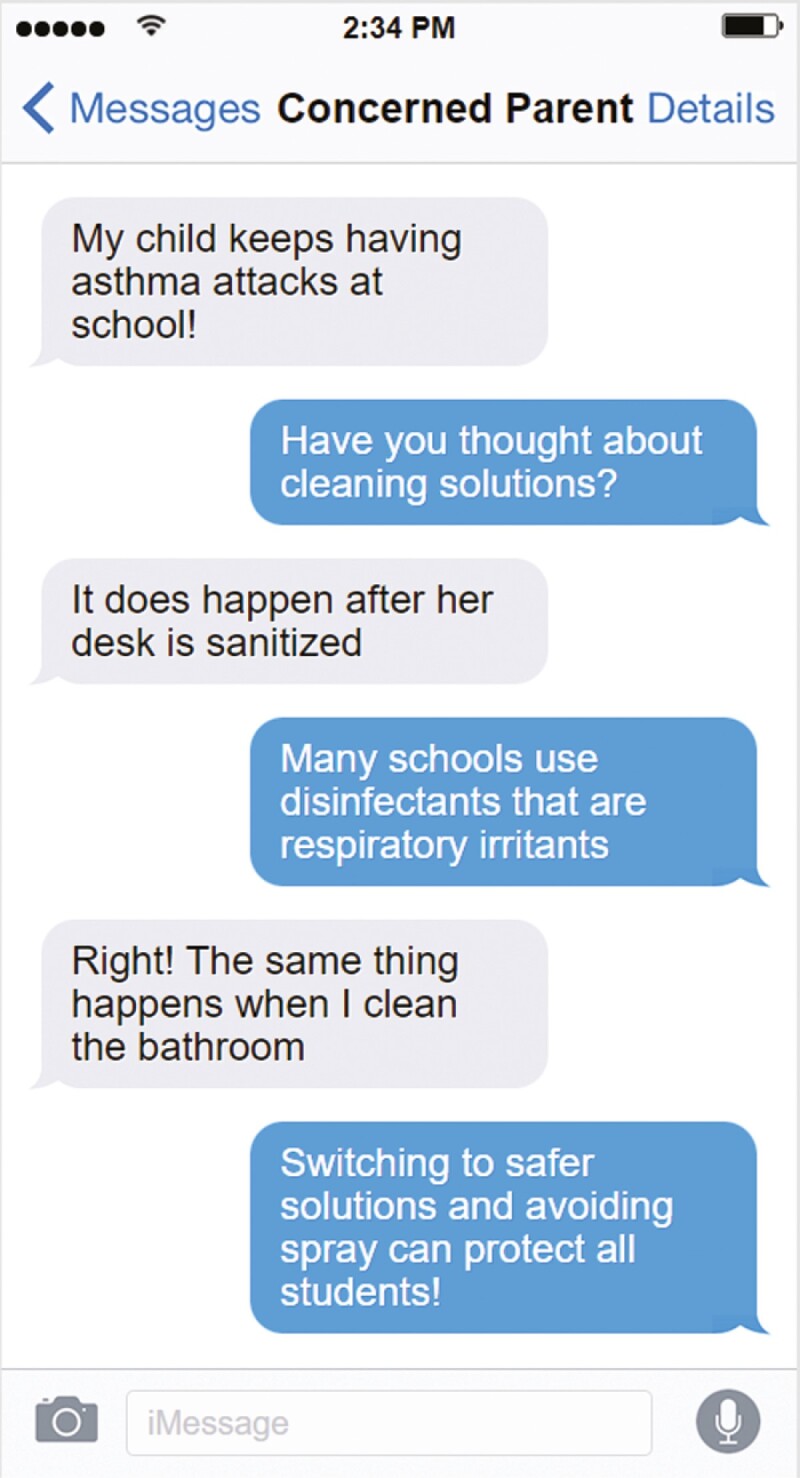
Graphical Abstract
Graphical Abstract.
INTRODUCTION
After lockdowns in the early part of the COVID-19 pandemic and multiple school outbreaks, particularly since the emergence of the Delta and Omicron variants, it is apparent that children need to be able to attend school safely (1). As well as clean air, mask use and immunization, in spite of evidence that COVID-19 transmission is predominantly airborne, surface cleaning, disinfection and hand hygiene are strategies that are widely employed to decrease school-based spread of COVID-19 (2). Unfortunately, many commonly used disinfectants are respiratory irritants implicated in the incidence and prevalence of asthma (3–7), posing a potential risk to all children in school with disproportionate impacts on children with respiratory diseases such as asthma.
DISCUSSION
Chronic exposure to some commonly used disinfectants increases the incidence of asthma and, with acute exposure, its prevalence (3–5,8–10). While most reports focus on adults involved in cleaning as a profession (4,8–10) or who use disinfectants frequently at home (5), similar observations have been made for children exposed at home (3,7). Pandemic-level school disinfection routines have increased children’s exposure to these chemicals at school. While reports of exposure to Poison Control in the United States rose in the under-5 group from home settings (11), studies examining school-based exposures are lacking in the literature.
School administrators face multiple and constantly evolving challenges to provide a safe in-person learning environment for teachers and children (1). A widely adopted strategy is frequent disinfection of high-use surfaces, including desks (12). Multiple classes of disinfectant are available for individual and institutional use (4,5,9,13,14). They can be grouped by chemical type. Some common agents are linked to respiratory irritation, inflammation, and asthma exacerbation (5,6,9). Quaternary ammonium compounds (e.g., benzalkonium chloride) and aldehydes are strongly linked with asthma (5,6,9,13); chlorine-releasing compounds such as hypochlorite (bleach) also increase respiratory problems including asthma (4,6,8). The mode of use is also important, with spray application increasing respiratory problems compared to other forms of administration (5).
Safer and effective solutions, including those that employ hydrogen peroxide, citric acid, or ethanol as active disinfection agents and safer application formats that avoid spraying, are already commercially available and well described in the literature (5,6,13). Information designed for clinicians, school and other administrators, and the general public is available (11,14).
Asthma is the most common chronic disease in Canadian children. Typical factors associated with asthma triggers at school include poor ventilation, dust, pets, and exposure to viral infections. Exacerbations in children lead to child and parental anxiety, unanticipated physician visits, and school and work absences (15). Exacerbations triggered by school factors risk creating negative associations for children who may already be marginalized by their chronic disease. By increasing the use of common and well-known asthma triggers in schools while they are in session, we are not only failing a large and vulnerable population of children, we also may be promoting unnecessary risk for the entire school cohort. Children with respiratory disease may act as the proverbial “canary in the coal mine” with respect to potentially harmful respiratory exposures.
CONCLUSION
Disinfectants are an important part of public health strategies to control the spread of viral infections, including COVID-19. While some disinfectants can present health hazards, particularly to children with asthma and other respiratory conditions, safer alternatives, and safe practices, are broadly available and well-described. For children experiencing respiratory issues such as asthma exacerbations in school, disinfectants should be considered as a potential cause. Physicians, schools, and parents will benefit from working together to address this preventable issue.
ACKNOWLEDGEMENT
There were no sources of funding for this work. The authors have no direct links to industry. The authors would like to sincerely thank Dr. Connie Yang, a pediatric respirologist at the University of British Columbia, for bringing forward concerns about increased asthma exacerbations in schools potentially attributable to increased disinfectant use. The authors would also like to acknowledge Caroline Di Rui Xu for her help with the graphical abstract.
Contributor Information
Anne Hicks, Department of Pediatrics, University of Alberta, Edmonton, Canada.
Patrick Hicks, Department of Kinesiology, University of Alberta, Edmonton, Canada.
FUNDING
There are no funders to report.
POTENTIAL CONFLICTS OF INTEREST
AH is a member of the editorial board. Another editor was assigned to handle the peer review of this manuscript. Outside the context of this manuscript, she also reports a CIHR Team Grant and a grant from the Lung Association of Alberta, as well as support from the American Thoracic Society and the Canadian Paediatric Society for travel costs. AH is also President of the Canadian Paediatric Society Section of Environmental Health and a Member of the American Thoracic Society Environmental Health Policy Committee. There are no other disclosures. Both authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
REFERENCES
- 1. Viner RM, Bonell C, Drake L, et al. . Reopening schools during the COVID-19 pandemic: Governments must balance the uncertainty and risks of reopening schools against the clear harms associated with prolonged closure. Arch Dis Child 2021;106:111–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Reducing COVID-19 risk in community settings: A tool for operators [Internet]. Government of Canada. [cited 2022 Mar 22]. Available from: https://health.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/reducing-covid-19-risk-community-settings-tool-operators.html [Google Scholar]
- 3. Abrams EM. Cleaning products and asthma risk: A potentially important public health concern. CMAJ 2020;192:E164–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Carder M, Seed MJ, Money A, Agius RM, Van Tongeren M.. Occupational and work-related respiratory disease attributed to cleaning products. Occup Environ Med 2019;76:530–6. [DOI] [PubMed] [Google Scholar]
- 5. Zock JP, Plana E, Jarvis D, et al. . The use of household cleaning sprays and adult asthma: An international longitudinal study. Am J Respir Crit Care Med 2007;176:735–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Siracusa A, De Blay F, Folletti I, et al. . Asthma and exposure to cleaning products—A European Academy of Allergy and Clinical Immunology task force consensus statement. Allergy Eur J Allergy Clin Immunol 2013;68:1532–45. [DOI] [PubMed] [Google Scholar]
- 7. Parks J, McCandless L, Dharma C, et al. . Association of use of cleaning products with respiratory health in a Canadian birth cohort. CMAJ 2020;192:E154–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hadrup N, Frederiksen M, Wedebye EB, et al. . Asthma-inducing potential of 28 substances in spray cleaning products—Assessed by quantitative structure activity relationship (QSAR) testing and literature review. J Appl Toxicol 2022;42:130–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Migueres N, Debaille C, Walusiak-Skorupa J, et al. . Occupational asthma caused by quaternary ammonium compounds: A multicenter cohort study. J Allergy Clin Immunol Pract 2021;9:3387–95. [DOI] [PubMed] [Google Scholar]
- 10. Weinmann T, Forster F, Von Mutius E, et al. . Association between occupational exposure to disinfectants and asthma in young adults working in cleaning or health services: Results from a cross-sectional analysis in Germany. J Occup Environ Med 2019;61:754–9. [DOI] [PubMed] [Google Scholar]
- 11. Babajanian, M, Marden M.. Safer cleaning products and asthma: Tips and resources for health professionals. AAP in Action [Internet]. 2021;6–10. https://nyscheck.org/wp-content/uploads/2021/11/AAP_-in_Action_November_2021_Newsletter_6-10.pdf [Google Scholar]
- 12. CDC. Coronavirus disease 2019 (COVID-19): Guidance for cleaning and disinfecting public spaces [Internet]. p. 1–9. [cited 2022 Feb 10]. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/cleaning-disinfecting-public-spaces.html [Google Scholar]
- 13. Vandenplas O, D’Alpaos V, Evrard G, et al. . Asthma related to cleaning agents: A clinical insight. BMJ Open 2013;3:e0035681–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hicks P, Zhang C, Lam K, Osornio A, Hicks A.. Cleaning agents, COVID and child health [Internet]. 2021. [cited 2021 Feb 10]. https://cps.ca/blog-blogue/cleaning-agents-covid-and-child-health
- 15. Hughes D. Childhood asthma and school. Paediatr Child Heal 2021;26:E4–5. [DOI] [PMC free article] [PubMed] [Google Scholar]


