Abstract
Objectives:
This study examined the association between parenting adult children with serious conditions and mothers’ midlife health in the United States.
Background:
The literature about the link between the parenting status of having an adult child with a serious condition and maternal wellbeing can be advanced by systematic analysis of the cumulative role that this parenting status can play in maternal health over the life course as opposed to at any one point.
Method:
Propensity score reweighting models of data from the National Longitudinal Study of Youth 1979 and its linked child and young adult data estimated disparities in midlife health among mothers of adult children with serious conditions (disabilities, developmental disorders, chronic diseases) and mothers of typically developing children, including examining variation by how long mothers had been in this parenting role and moderation by maternal education and marital status.
Results:
Mothers of young adult children with serious conditions had poorer physical (but not mental) health at midlife than other mothers, especially when more years had elapsed since the child was diagnosed with or developed the condition. These patterns did not differ by maternal education and marital status.
Conclusion:
The dynamics of epidemiological risk and protection among parents of children with serious conditions were temporally situated in the maternal life course but were consistent across different segments of the maternal population.
Keywords: Child with disabilities, Families in middle and later life, Health, Life course
INTRODUCTION
Parents of children with serious conditions—such as disabilities, developmental disorders, and chronic diseases—face challenges that take a toll on the body and mind, including daily stresses, financial strains, disrupted social relationships, and long-term anxieties (Umberson et al., 2010). Although countered by the rewards of this parenting experience (e.g., personal fulfillment, sense of purpose), they tend to have poorer physical and mental health than other parents (Ha et al., 2008; Pinquart, 2017; Reichman et al., 2004). As medical advances extend the life expectancy of such children, the duration of their parents’ active parenting careers is increasing. Consequently, at a time when many parents receive care and support from their adult children, others experience the challenges of caring for adult children with serious conditions while also dealing with the challenges of aging (Janus, 2009; Osgood et al., 2010; Umberson et al., 2010). Although research on this growing population suggests that parenting adult children with serious conditions can accelerate physical, emotional, and cognitive aging (Barker et al., 2012; Seltzer et al., 2011; Song et al., 2016), critical questions about the role of parenting children with serious conditions in health disparities remain unanswered. Does the link between this parenting experience and parental health reflect the accumulation of experiences across many years? What are the social and economic resources that might affect the vulnerability or resilience of those engaging in this parenting experience over time?
This study attempted to answer such questions. Integrating life course theory with the epidemiological model of risk and protection (e.g., Ferraro & Shippee, 2009; Masten & Garmezy, 1985), it posits that parenting adult children with serious conditions is a risk factor for poorer physical and mental health among parents at midlife, that this risk increases with “dosage” across life, and that two socially patterned dimensions of life course attainment (educational, partnership) protect against this risk over time. Tests of hypotheses derived from this conceptual model drew on propensity score reweighting, internal moderation, and post-hoc tests of endogeneity with data from the National Longitudinal Survey of Youth:79 (NLSY79) and its linked Child and Young Adult surveys (NLSY79-CYA). The reality that women carry the primary responsibility for parenting and tend to be most affected by raising children in stressful circumstances (Ha et al., 2008; Pinquart, 2017; Reichman et al., 2004; Ruppanner et al., 2019), coupled with the linkage of the NLSY datasets through the original female respondents, focused these analyses on women. Mothers, therefore, were tracked into midlife (operationalized here as age 50) as the children of the former were born, were diagnosed with serious conditions at varying ages or developed more typically, and reached their 20s and 30s.
Conceptually, this research can expand knowledge of how vulnerable children may influence family ecologies over time and their parents’ abilities to serve them. Methodologically, the triangulation of statistical techniques recognizes the value of longitudinal approaches for revealing key insights about timing and cumulative stress and addressing the threats of observable and unobservable confounds for drawing strong conclusions about life course dynamics. Practically, this research clarifies which parents of children with serious conditions are most in need—in terms of the length of their experience, family situation, and socioeconomic background—to help identify potentially critical points or groups of intervention.
Background
The Health Implications of Parenting Children with Serious Conditions
Parents of children with serious conditions—typically defined as disabilities, developmental disorders, and chronic diseases but also occasionally mental conditions—face many strains that can undermine their health, such as financial hardship, time demands, anxieties about the future, empathic distress, disrupted social participation, and emotional stress (Hastings, 2002; Pinquart, 2017; Reichman et al., 2004). They also derive rewards from this parenting experience (e.g. sense of purpose, self-learning, new skills), but its average negative associations with indicators of wellbeing suggest that strains outweigh rewards for many (Horton & Wallander, 2001; Lin et al., 2013; Schwartz, 2003).
Improvements in health and human services have helped many children with serious conditions live longer, so their aging parents maintain an intensive parenting role long after their same-age peers are “done” with that portion of their parenting careers (Janus, 2009; Umberson et al., 2010). This extension of the parenting career also raises the likelihood that parents will face the health-undermining challenges of membership in the sandwich generation, which refers to parents’ simultaneous provision of care to their children and their own parents (Chassin et al., 2010). Those challenges can co-occur with normative age-related changes in parents’ personal capacities and social circumstances, the anxieties of children aging out of services, and the tensions of social comparisons with same-age parents who have more independent grown children (Birditt, Fingerman, & Zarit, 2010; Umberson et al., 2010). Thus, older parents of older children could face an even more serious imbalance of strains and rewards than the younger parents of younger children who are more often studied. Indeed, caring for adult children with serious conditions predicts an array of deleterious outcomes for parents at midlife and beyond, including poorer psychological wellbeing, more somatic symptoms, lower cognitive functioning, and higher allostatic load (Ha et al., 2008; Song et al., 2016).
Following the epidemiological risk and protection framework (Masten & Garmezy, 1985), parenting an adult child with a serious condition is a risk factor for the health of parents at midlife (i.e., health outcomes are probabilistically poorer in the face of this parenting status than they otherwise would be). As more people move into midlife parenting adult children with serious conditions, understanding this risk factor becomes more important to efforts to support the health of the population. Life course theory can advance this understanding by widening the lens of inquiry (Ferraro & Shippee, 2009; Umberson et al., 2010). Reflecting the theory’s emphasis on personal and interpersonal dimensions of family life (e.g., health of parents and children, parent-child relations) as unfolding trajectories, the lens can be widened temporally to consider the potentially cumulative effects of this dynamic parenting status. Reflecting the theory’s emphasis on the ways that family trajectories are embedded within the broader constraints and opportunities organized by social structure, the lens can be widened contextually by situating the longitudinal health risks of this parenting status within systems of social and economic stratification that exacerbate these risks for some and buffers against them for others.
Temporally Studying the Health of Parents of Adult Children with Serious Conditions
One life course approach to epidemiological risk and protection is to explore dosage effects, in which the impact of a risk factor depends on its magnitude or duration (Burchinal et al., 2016; Ferraro & Shippee, 2009). Again, past research has documented that parents of adult children with serious conditions have poorer health at midlife than parents of typically developing adult children, but that research has paid less attention to the potential differences among parents of adult children with serious conditions. Do parents whose adult children have had such conditions for many years (higher dosage) have poorer health than parents whose adult children have had such conditions for fewer years (lower dosage)?
In this dosage effect, the risks for midlife health faced by parents of adult children with serious conditions are conceptualized to increase as the length of time that parents have inhabited this status across the life course increases. In statistical terms, the degree to which a binary variable for midlife parenting status significantly predicts midlife health outcomes is conditional on a continuous variable gauging duration in this status up to midlife. Such a dosage effect would indicate that vulnerability builds over time, so that parents with the same parenting status at midlife have different health outcomes depending on their journey to that point. Mechanisms for this dosage effect could encompass the buildup of social, psychological, and physical strains over long periods of prolonged exposure to this potentially challenging experience of parenting, including the residue of past history (Ha et al., 2008; Thoits, 2010; Willson et al., 2007).
Contextually Studying the Health of Parents of Children with Serious Conditions
According to the epidemiological framework (Masten & Garmezy, 1985; Sameroff, 2006), the link between a risk factor and poor health can be attenuated by a protective factor, which brings heightened benefits to groups of people with the risk factor. Life course theory guides the search for such protection to the unequal social and economic resources that shape adjustment to roles and influence life trajectories (Elder et al., 2003; Ferraro & Shippee, 2009). The integration of these perspectives suggests that systems of social and economic stratification leave broad groups more at risk for poor outcomes over time but also more responsive to protective factors that buffer this dynamic risk (Mirowsky & Ross, 2003; Umberson et al., 2010). This interplay of risk and protection is under-examined in the literature on health disparities related to parenting adult children with serious conditions. Yet, as argued below, the inequalities of the modern economy and neoliberal welfare regime mean that parents who are more educated and stably married likely have more resources to cope with the challenges of raising children with serious conditions into adulthood. Those resources may protect parents from some of the impact of this risk factor even if they do not reduce actual exposure to this risk factor.
First, educational attainment is a powerful component of socioeconomic status that influences individual health and mitigates the health impact of many personal and social disadvantages (Hayward et al., 2015; Mirowsky & Ross, 2003). It facilitates the accumulation of financial and social capital that increases access to valuable services for families, including high-quality health care, childcare, therapy, and enrichment activities as well as systems of instrumental and socioemotional support. It also represents the development of human capital—through formal learning and informal socialization processes—that enhances self-efficacy, health literacy, time/resource management, and harm reduction and that brings prestige and status to increase the likelihood and effectiveness of enacting power (Mirowsky & Ross, 2003). These varied resources are common foci of explanations for why more educated mothers tend to maintain more sensitive and stimulating parenting in the face of economic, personal, and other challenges than less educated mothers (Augustine, 2014; Prickett & Augustine, 2016).
Second, ample research has documented that long-term partnerships predict better health across life, although more for marriage than other partnerships (Kiecolt-Glaser & Newton, 2001). Common explanations involve the financial and human capital that partners—same- or different-sex—pool and the health maintenance and emotional support they provide (Tumin & Zheng, 2018; Williams & Umberson, 2004). This health advantage is often more pronounced in the face of risks to wellbeing, such as the case of parents of young children with serious conditions maintaining better health when they have a partner to meet challenges and share strains compared to when they are unpartnered or in lower-quality partnerships (Pinquart, 2017).
Study Aims, Hypotheses, and Contributions
Following the integration of life course theory with the epidemiological model of risk and protection, this study attempts to “complicate” the documented association between parenting an adult child with a serious condition and poorer physical and mental health among parents at midlife across two aims. The first aim is to test the dosage hypothesis—whether this association strengthens as the length of time since the diagnosis or development of the condition increases. The second aim is to test the socioeconomic variability hypothesis—whether evidence of dosage weakens in the context of greater educational attainment and stable marital histories. For both aims, hypothesis-testing draws on methodologies that help to address the confounding role of factors that can be straightforwardly measured (propensity score reweighting) and factors that are more difficult to observe (post-hoc robustness indices) and that account for the difficulties of measuring the interplay between risk factor and dosage (internal moderation).
Such research can advance the scientific literature on parents of adult children with serious conditions and provide general guidance to any interventions aiming to serve such parents. It introduces the possibility of temporal variability in this risk status in the form of dosage effects, which can help interventions target when in the risk process to focus attention. It expands the possibility of contextual variability in this risk status in the form of social and economic moderation, which can help interventions target who in the at-risk group requires more attention. Without establishing causality, it takes more innovative steps than past studies to improve causal inference, which can help interventions assess the feasibility of action.
Methods
Data Source
Designed to study the school-to-work paths of young people growing up in the late 1970s, NLSY79 is a nationally representative study of 12,686 men and women aged 14 to 22 in 1979 who were followed annually until 1994 and then biennially. We used data spanning 1979 to 2016. This endpoint was chosen (rather than 2018) because all participants had completed the focal age 50 health module by this wave but too few had completed the age 60 module by 2018. NLSY79-CYA is a biennial survey of the children of the female NLSY79 respondents, beginning with just over 5,200 children in 1986 (born as early as 1970), adding any new children born afterwards, and transitioning to a young adult module when the children reached age 15. NLSY79-CYA data can be linked to data on the children and young adults’ families of origin using the original NLSY79 mothers’ identifiers. This intergenerational linkage narrowed the possible sample to mothers, which alters the generalizability of the findings from parents in that specific birth cohort to mothers in that specific cohort.
Based on this intergenerational linkage, this study’s analytical sample included 3,072 mothers who participated at age 50 and had a child who was at least 18 by that point (mean child age of 27.84, with a range of 18–38), which excluded 298 mothers of children with serious conditions who were still minors. We used multiple imputation with chained equations (five imputations following Rubin’s (2004) rules; Stata 16 mi impute) to impute missing values on the covariates, which are described below along with their proportion of missing cases. Results estimated using listwise deletion were substantively similar and are not shown here.
The long time span of data collection with this analytical sample is important to consider. During data collection in 1979, federal employment and training programs for youth were expanding while global economic restructuring was gaining momentum. The original NLSY79 respondents then navigated adulthood, completed education, entered the labor force, and started families amidst economic fluctuations, the expansion of higher education, growing population diversity, and policy change over many decades (Fischer & Hout, 2006; Hoffman et al., 2008; Mann et al., 2003). Given that rapid societal change, macro-level forces could have differentially affected the experiences of children with serious conditions and their mothers depending on when, historically, children were born and their serious conditions developed or were diagnosed. We return to this issue in the discussion section.
Measures
To give a sense of the complicated timeline for measurement, the dependent variables were measured at whatever wave the NLSY79 mothers reached age 50, the focal independent variables (parenting adult child with serious condition, duration in this status) were measured from 1994 until the wave in which mothers turned 50, and the control variables were either measured at the wave in which mothers turned 50 or at the first wave of NLSY79. Because most mothers in the NLSY79 cohort did not have adult children with serious conditions at age 40 and because only a portion of them were old enough by the most recent wave to complete the age 60 health module, age 50 offered the best available measurement point of “midlife”.
Health in the mother generation.
Women responded to a series of questions on the Short-Form 12, a widely used and clinically validated self-report instrument (Brazier et al., 1992), assessing physical and mental health at ages 40 (1998–2006 depending on their years of birth) and 50 (2008–2016). We derived continuous composite scores from the sum of physical health items (e.g., reports of pain, mobility, self-rated health) and mental health items (e.g., emotional distress, feelings of calm, emotional problems), respectively. NLSY’s proprietary scoring standardized these variables to a mean of 50 and standard deviation of 10 (range = 0–100). Thus, a score of 50 corresponded with the U.S. adult average, and a 1-point difference represented one-tenth of a standard deviation. Higher scores indicated better physical and mental health. Supplemental models used the frequency of depressive symptoms (CES-D score) and self-rated global physical health as outcomes, and these sensitivity tests yielded similar results.
Serious conditions in the child generation.
At each wave since 1994, parents reported their children’s health conditions and/or their children, if older and capable, reported their own. Following work with the Midlife in the United States (MIDUS) study (Seltzer et al., 2011; Song et al., 2016) and NLSY79 (Van Cleave et al., 2010), we identified three categories: disabilities (physical/orthopedic impairments, blindness, learning disability, speech impairments), developmental disorders (autism, intellectual disabilities, epilepsy), and chronic conditions (asthma, anemia, immune deficiency, cancer/tumor, diabetes, heart trouble, nervous and respiratory disorder). As in prior research (Gilligan et al., 2017; Van Cleave et al., 2010), we collapsed these conditions into a single binary variable in order to be more parsimonious and preserve power, capture commonalities among serious conditions, and consider conditions with waxing and waning symptoms that may lead to other condition. Still, recognizing that these conditions vary in emergence, severity, and stress, we also examined how the constituent categories might have driven the results for the total score. A single binary indicator of ever having the condition was created for each of the three categories. Bivariate analyses showed that, for each category, ever experiencing that category was significantly associated with physical (not mental) composite score, consistent with the main results presented below.
The time-varying variable for ever experiencing any category of conditions was measured at each wave from 1994 to 2016, with children transitioning from 0 to 1 at the age/year when the condition developed or was diagnosed and from 1 to 0 if the condition resolved (5.86% missing). At age 50, mothers in the analytical sample had 411 adult children who had at least one serious condition at that point (chronic diseases being the most common), with development and diagnosis varying across many years of children’s lives since birth. Based on these time-varying values, a categorical variable measured different temporal patterns: 1) Mothers whose adult children never had any serious condition (never), 2) mothers whose adult children did not have a serious condition at the final wave (when mothers were age 50) but did have serious conditions at one or more previous waves (previously), 3) mothers whose adult children had serious conditions at the final wave (currently).
Duration of parenting experience.
Consistent with previous research (Ha et al., 2008), we measured duration of parenting children with serious conditions for the “currently” category between maternal age at onset of the child’s condition and age 50. For the “previously” category, we calculated the duration between maternal age at onset and when the condition resolved.
Mothers’ educational attainment and marital history by age 50.
A binary indicator differentiated women who had graduated from college by age 50 from all others, which yielded comparable results to more detailed measures, including a categorical measure designating specific diploma/degree benchmarks (Hayward et al., 2015), a pair of categorical/binary measures of mother’s educational attainment at the target child’s birth and whether she completed additional education following this birth (Augustine, 2021), and a continuous measure of years of education (Mirowsky & Ross, 2003). The life course measure of marital status up to age 50 had three categories: never married, experienced marital disruptions, and continuously married (missing for 6.05% of cases). Consistent with prior research (Tumin & Zheng, 2018), alternating a binary variable of marital status at age 50 did not reveal different results.
Covariates measured at maternal age 50.
Measures for potential confounds in the focal associations included maternal statuses at age 50: unemployment (6.77% missing), logged family income (13.61% missing), and parity. The corresponding child-level covariates included educational attainment (5.47% missing), age, gender, current co-residence with mother (6.84% missing), and experience of more than one condition. A final set of covariates, also measured at maternal age 50, accounted for the cross-influence in maternal health—mental health scores at age 50 when predicting physical health and physical health scores at age 50 when estimating mental health (Frech & Damaske, 2012).
Covariates measured at/prior to mothers’ first birth.
As described below, propensity scores indexed variables for a host of factors potentially selecting women into the status of parenting adult children with serious conditions. They were created by estimating multinomial logistic regressions predicting the “treatment” (i.e., mother ever had a child with a serious condition at age 50) by the selection factors and then outputting the predicted odds. The selection factors measured whether the mother grew up with two married parents, completed college by her first birth (1.14% missing), was single at the target child’s birth (19.4% missing), had a teen birth, was born in the U.S., had health problems limiting work (3.13% missing), and was raised by a mother who did complete high school (1.14% missing) as well as the mother’s race/ethnicity (Non-Hispanic White, Black, Hispanic), age at first birth, and cognitive ability (using the Armed Forces Qualification Test-revised, which all respondents took in 1980; 4.07% missing). A final factor measured the number of active nonfederal physicians in the county per 100,000 residents to account for medical availability for mothers at birth (4.13% missing).
Analytical Strategy
To test the dosage hypothesis, Model 1 regressed the age 50 health variables on the categorical variables measuring the parenting status of having children with serious conditions, Model 2 added the sociodemographic controls, and Model 3 added the conditionally relevant variables (see internal moderator approach below) for maternal duration of the parenting status and the parenting status variables. To test the socioeconomic variability hypothesis, Models 1–3 were estimated within subsamples defined first by mothers’ educational attainment and second by mothers’ marital histories. For both sets of analyses, Chow tests indicated whether any observed differences in focal coefficients across subsamples were statistically significant.
Internal moderator approach.
Any non-zero value of maternal duration in the parenting status required that mothers had children with a serious condition in the first place; as such, they were conditionally relevant variables (i.e., a valid value on this variable depended on having a specific value on another variable). We estimated the “effects” of these conditionally relevant variables with an internal moderator approach (Mirowsky, 1999).
| (1) |
Equation 1 shows a simplified form of the internal moderator model where C = the set of covariates, T = duration of having a child with a serious condition up to age 50, and P = parenting an adult child with a serious condition at age 50. The first set of brackets shows an overall intercept and the set of controls that is equivalent to the age 50 health of mothers who did not have adult children with a serious condition. The second set represents the age 50 health of mothers who had adult children with serious conditions as a function of the duration since this parenting status began. It is multiplicative between P and T (i.e., effectively an interaction).
In the internal moderator approach, however, the main effect of duration was not in the model (here, the main effect of P is represented as β2). When mothers did not have any experience parenting adult children with serious conditions, they were assigned a placeholder value for T to include them in the overall model estimation. That value dropped out when multiplied by P = 0. The model distinguished between states by P and T. Substituting values of P and T based on the mother’s parenting experience, the equations below represent age 50 health when mothers had no experience parenting an adult child with serious conditions (Equation 2) and when they had 8 years of this experience (Equation 3). In short, the focal variables were actually a set of dummy variables interacted with a continuous variable of duration.
| (2) |
| (3) |
Efforts to improve causal inference.
Two strategies assessed confounds that could simultaneously influence the likelihood that a mother had a young adult child diagnosed with serious conditions and her health in ways that created the false impression of links between the two. As already described, we created propensity scores to index the likelihood that mothers had a young adult child with a serious condition (the “treatment”) by estimating multinomial models that predicted the categorical outcome (never, previously, or currently experienced parenting a child with serious condition) by a large set of covariates. The predicted probabilities from these models then served as the propensity scores by which the focal regressions described above were reweighted according to how much any one case resembled the profile of a case in the treatment group regardless of actual treatment status. We used the inverse propensity score weights as model weights in all analyses, calculated as:
where ω= weight, t= treatment (parenting adult child with serious conditions), and e(x) = the propensity of receiving the treatment. Using propensity scores as model weights (vs. matching) facilitated the estimation of covariates and interactions and efficiently gauged biases associated with a large number of observable selection processes at once (Heckman & Robb, 1985; Rosenbaum & Rubin, 1983). We did not combine the inverse propensity score weights with normal poststratification sample weights because the models included covariates related to sample selection, but using inverse propensity score weights without sampling weights produces unbiased estimates (Winship & Radbill, 1994).
To gauge biases related to unobservable selection processes, we calculated the Impact Threshold for Confounding Variables (ITCV; Frank, 2000). The equation is: rx,y – r#x,y/1-r#x,y, where r#x,y = t / SQRT[(n-q-1) + t2], t is the critical t-value, n is the sample size, and q is the number of parameters. It quantified how much an unobserved confound would have to be correlated with both predictor and outcome to reduce the focal regression coefficient for their association to non-significance; in other words, how likely the inclusion of some unobserved confound would nullify the focal results if such a confound could be measured and modeled. We calculated the ITCV for any significant parenting status coefficient in the final models.
Results
Table 1 describes the analytical sample. The mean physical health score was slightly lower than the U.S. average (represented by the standardized score of 50). Mental health, on the other hand, was moderately higher than the U.S. average. At age 50, 14% of mothers had an adult child with serious conditions, and 18% had some experience parenting a child with a serious condition prior to age 50. The average mother of an adult child with a serious condition had experienced this parenting status for 8 years and was 38 years old when their young adult child’s condition was initially developed or was first diagnosed.
Table 1:
Descriptive Statistics for Analytical Sample (n = 3,072)
| Mean | SD | |
|---|---|---|
| Mother’s Health at Age 50 | ||
| Physical composite score | 47.99 | 11.09 |
| Mental composite score | 51.81 | 9.51 |
| Parenting Status | ||
| Never had adult children with serious conditions (never) | .68 | |
| Once had child with serious condition but not at age 50 (previously) | .18 | |
| Had adult child with serious condition at age 50 (currently) | .14 | |
| Duration (mother’s age when child diagnosed with/developed condition) a | 38.05 | 5.81 |
| Mother’s Circumstances at Age 50 | ||
| Attained college degree by age 50 | .47 | |
| Marital history up to age 50 | ||
| Continuously married | .33 | |
| Experienced marital disruptions | .58 | |
| Never married | .09 | |
| Not in the paid labor force | .26 | |
| Logged family income | 10.05 | 2.12 |
| Parity | 2.51 | 1.21 |
| Mother’s Circumstances at/prior to First Birth | ||
| Did not live with married parents | .23 | |
| Mother had less than high school education | .48 | |
| Educational attainment in years | 12.40 | 2.32 |
| Non-Hispanic White (reference) | .47 | |
| Black | .32 | |
| Hispanic | .20 | |
| Unmarried at birth | .34 | |
| Teenage birth (under age 18) | .12 | |
| Nativity (1 = U.S. born) | .93 | |
| Age at first birth | 22.87 | 4.75 |
| Health problems limiting work | .10 | |
| AFQT-80 percentile | 37.39 | 27.60 |
| Rate of active nonfederal physicians at county (per 100,000) | 16.72 | 11.62 |
| Characteristics of Target Child at Mother’s Age 50 | ||
| Graduated from high school | .92 | |
| Age | 27.84 | 4.88 |
| Gender (female) | .47 | |
| Currently lived with mother | .27 | |
| Had more than one with serious conditions | .08 |
Note: Statistics calculated for the nonimputed analytical sample from the National Longitudinal Study of Youth: 1979 (1994–2016).
Estimates among mothers who have had children with serious conditions.
In analyses not shown (see online appendix), mothers who currently had a young adult child with serious conditions averaged significantly lower physical health composite scores than mothers who never had experience raising a child with serious conditions (by 5.12 points) or who had some prior experience (2.94 points), with slightly smaller but still significant differences for mental health (2.5 and 1.44 points, respectively). These differences were also seen in educational attainment (e.g., 42% of mothers in the “currently” category had graduated from college compared to 47% and 52% in the “never” and “previously” categories), marital history (e.g., they were 5 percentage points more likely than women in the other two categories to experience marital disruptions across the life course), and several other sociodemographic factors (e.g., significantly more likely to have had a teen birth, have health limitations, and be employed and scoring significantly lower on the cognitive test). In sum, mothers of adult children with serious conditions appeared to be in poorer health than other mothers, but that disparity could reflect systematic disparities in other circumstances of their lives.
Parenting Adult Children with Serious Conditions as a Risk Factor for Women’s Health
The first aim was to test the hypothesis that associations between parenting an adult child with a serious condition and midlife health would be sensitive to dosage. To this end, Table 2 presents the focal results from regression models predicting the age 50 health outcomes, weighted by the propensity scores. According to Model 1, mothers whose adult children never had a serious condition (never) scored 3.28 points higher on the physical health composite than mothers who at age 50 had an adult child with a serious condition (currently) and 1.75 points higher than mothers who once but no longer had a child with a serious condition (previously). Accounting for the full set of control variables in Model 2 reduced the first health disparity by slightly less than one point but actually increased the second by slightly less than one point. In this fully controlled model, the small health disadvantage of the currently category relative the previously category was not significant. For mental health, there were no significant differences among the three categories of mothers once the full set of control variables were included.
Table 2.
Results for Physical and Mental Health Composite Scores Predicted by Parenting Status (n =3,072)
| Coefficients (SE) |
||||||
|---|---|---|---|---|---|---|
| Physical health | Mental health | |||||
|
|
||||||
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| Parenting Child with Serious Conditions (Ref. Never) | ||||||
| Once had child with serious condition but not at 50 (previously) | −1.75** | −2.34*** | −2.68* | −0.83 | 0.05 | −0.27 |
| (0.57) | (0.56) | (1.05) | (0.50) | (0.52) | (1.12) | |
| Had child with serious condition at age 50 (currently) | −3.28*** | −2.39*** | −2.08 | −2.10*** | −0.73 | −0.92 |
| (0.67) | (0.69) | (1.15) | (0.58) | (0.59) | (1.08) | |
| Parental Status x Duration | ||||||
| Previously x duration | −0.09 | −0.01 | ||||
| (0.12) | (0.13) | |||||
| Currently x duration | −0.30*** | −0.07 | ||||
| (0.09) | (0.09) | |||||
Note: Robust standard errors in parentheses.
p < 0.001
p < 0.01
p < 0.05.
All models controlled for maternal characteristics prior to first birth (as listed in Table 1). Models 2–3 controlled for maternal and child circumstances at maternal age 50 (as listed in Table 1). Reflecting the internal moderator approach, there is no row for the main effect of the duration variable because the coefficient of duration was conditional on there being adult children with serious conditions present.
Thus, having adult children with serious conditions—either currently when mothers were 50 or previously—was a significant risk factor for poorer physical but not mental health. Did these physical health risks reflect dosage effects? Following the internal moderator approach, the one significant interactive pattern in Model 3 in Table 2—between the currently category and duration in this category—was negative and significant. In line with a dosage effect, the physical health risks of having an adult child with a serious condition strengthened with more years in this parenting status (see Figure 1). The absence of other significant interactive patterns suggested that this dosage effect only applied to the physical health of mothers whose children currently had serious conditions, not to their mental health or to the physical or mental health of mothers whose adult children once but no longer had serious conditions.
Figure 1. Predicted Physical Health Composite Score among Mothers who Had a Young Adult Child with a Serious Condition at Age 50, by the Duration of the Serious Condition.
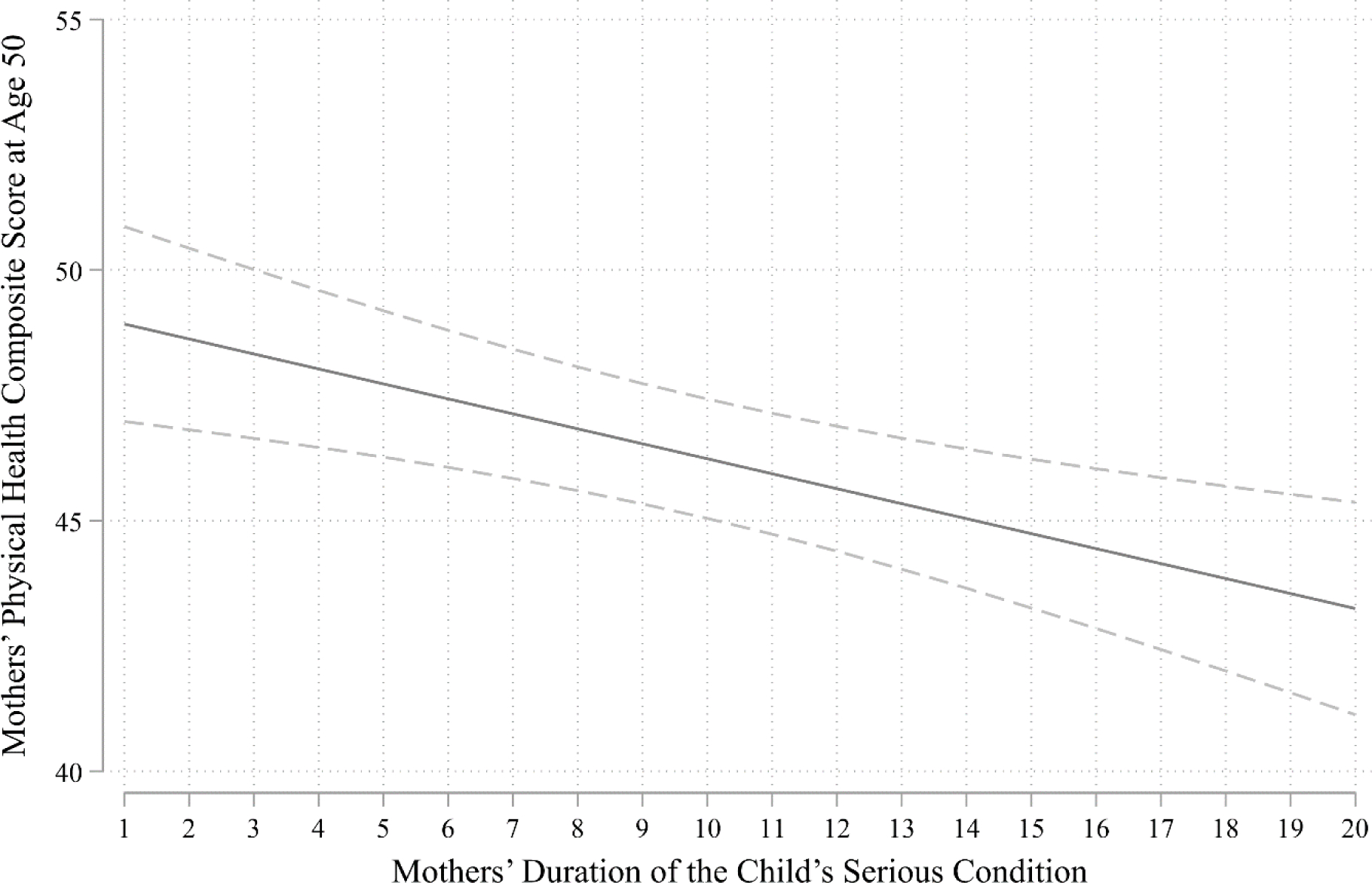
Note: The predicted value was estimated from Model 3 in Table 2.
Education and Partnership as Potential Protective Factors for Maternal Health
The second aim of this study was to test the hypothesis that associations between having an adult child and maternal health would vary (i.e., be moderated) by mothers’ social and economic resources. First, we re-estimated Models 1–2 in Table 2 separately for mothers who had not graduated from college and mothers who had. The results for physical health are presented in Table 3. The coefficients for both the “currently” and “previously” categories were stronger in the college-educated group, and the interaction between the currently category and the duration variable also was stronger (and significant at a more conservative p value) for such mothers. Chow tests, however, revealed no significant differences in any of these coefficients between the two groups of mothers. Similarly, there were no significant differences in focal coefficients between the two groups for mental health (see online appendix), and there were no significant differences in focal coefficients across categories of marital history (never married, history of marital disruption, continuously married) for either physical or mental health.
Table 3.
Results for Physical Health Composite Score Predicted by Parenting Status for Two Educational Groups (n =3,072)
| Coefficients (SE) |
||||
|---|---|---|---|---|
| Mother Not College-Educated by Age 50 | Mother College-Educated by Age 50 | |||
|
|
||||
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Parenting Child with Serious Conditions (Ref. Never) | ||||
| Once had child with serious condition but not at age 50 (previously) | −2.14* | −3.01 | −2.39** | −1.89 |
| (0.86) | (1.76) | (0.80) | (1.89) | |
| Had child with serious condition at age 50 (currently) | −2.20* | −2.39 | −2.57* | −1.43 |
| (0.94) | (2.02) | (1.06) | (2.13) | |
| Parental Status x Duration | ||||
| Previously x duration | −0.16 | −0.01 | ||
| (0.18) | (0.18) | |||
| Currently x duration | −0.20+ | −0.41** | ||
| (0.11) | (0.14) | |||
| Observations | 1,647 | 1,425 | ||
Note: Robust standard errors in parentheses.
p < 0.001
p < 0.01
p < 0.05
p < 0.1.
All models controlled for maternal characteristics prior to first birth (as listed in Table 1). Models 2–3 controlled for maternal and child circumstances at maternal age 50 (as listed in Table 1). Reflecting the internal moderator approach, there is no row for the main effect of the duration variable because the coefficient of duration was conditional on there being adult children with serious conditions present.
Thus, the patterns from Table 2—indicating the health risks of currently or previously parenting a young adult child with a serious condition, the former increasing the earlier in the mother’s life that the condition emerged—did not appreciably differ by mothers’ educational attainment or marital histories by age 50. Overall, then, the results revealed a risk factor for mothers’ physical health but did not identify protective factors buffering against this risk.
Sensitivity Analyses
Assessing the sensitivity of the results to several different specifications of the sample, the variables, and the models revealed few differences. The basic pattern of results reported above, therefore, was fairly robust.
First, the ITCV for the significant “currently” coefficient in Model 2 of Table 2 was 0.035. That value indicated that an unobserved confound (e.g., genetic characteristics) would have to be simultaneously correlated with this parenting status and physical health at .17 if its measurement and inclusion in Model 2 were to reduce the parenting experience coefficient in that model to non-significance. This ITCV value supported a moderate degree of confidence in causal inference, although there was a small number of NLSY variables that met this threshold.
Second, we tested the sensitivity of the results to alternative definitions of health: self-rated health at age 50 and CES-D scale at age 50. The only difference from the original models was that the coefficient for the “currently” status in the fully controlled CES-D model was statistically significant, when it was attenuated to non-significance by the inclusion of the control variables in the model with the mental health composite as the outcome.
Third, rather than stratifying the sample by educational attainment and marital history, we estimated models for the full sample that included interactions between the parenting status variables and both categorical and continuous measures of educational attainment. We also tested interactions in the full sample between the parenting status variables and the binary measure of marital status at age 50. None of these models yielded differences in the focal results.
Fourth, an alternate test dosage effects counted the years that children were categorized as having serious conditions across their lives. Testing this categorical variable (0 = no children with conditions, 1= 1–5 years, 2 = 5–10 years, 3 = 10+ years) did not change the focal results.
Fifth, to further explore socioeconomic moderation, we re-estimated the models stratified by educational attainment using two income-based measures, annual income and poverty status, neither of which yielded new evidence for the socioeconomic variability hypothesis.
Discussion
Prior research with MIDUS and other data sets has documented that raising children with serious conditions can pose risks to their parents’ health, despite the psychological and emotional rewards that such parents often enjoy, and that these risks are increasingly evident in the lives of older parents whose children have transitioned into adulthood (Barker et al., 2012; Ha et al., 2008; Pinquart, 2017; Seltzer et al., 2011). This potentially risky imbalance between the strains and rewards of this parenting experience is a window into family life and its role in individual development across generations. Answering questions about the variability in these patterns across the life course and across the population, therefore, is important to understanding families, health, and the interplay of the two. This study attempted to do so with a life course approach (e.g., Ferraro & Shippee, 2009; Elder et al., 2003) that temporally and contextually situated epidemiological risk and protection among parents of children with serious conditions.
In sum, the results revealed that, at midlife, mothers of young adult children with serious conditions had poorer physical (but not mental) health than otherwise similar mothers, as did mothers of young adult children who once but no longer had serious conditions. This status of parenting a child with serious conditions as a risk factor suggested a dosage effect, but only when those conditions persisted as the child transitioned into adulthood. The younger that mothers were when their children were diagnosed with serious conditions (i.e., the longer the duration of this parenting experience prior to age 50), the poorer their physical health at age 50. Notably, the models revealed no evidence that two key dimensions of life course attainment (educational attainment and marital history) operated as protective factors that buffered against this risk factor. Thus, this dimension of parenting was experienced in similar ways by mothers in diverse circumstances and social positions. This general pattern of results suggests four important questions for discussion with the goal of guiding future research that takes this topic in new directions and also addresses the limitations of what we have done here.
First, what does the evidence of a dosage effect suggest about the experience of raising a child with a serious condition across the full parenting career? Conceptually, there is a possibility that the more time a mother has experience with a source of stress, the more she will adapt to this challenge, and some cross-sectional or short-term evidence confirms this possibility among caregivers (Ha et al., 2008; Lazarus & Folkman, 1984). The longitudinal design employed here revealed instead that mothers may be worn down the longer they experience this parenting role, perhaps because the imbalance between strains and rewards grew over many years as children grew up and mothers aged. Such a process would be in line with the notion of cumulative stress, in which biological and psychological systems gradually weaken under repetitive stressors (Ferraro & Shippee, 2009). The interesting wrinkle is that, although mothers whose adult children once but no longer had serious conditions also reported poorer health at age 50 than the other mothers whose children did not have serious conditions at this point, this health disparity did not represent a dosage effect. This pattern suggests a legacy of earlier challenges that fades with some recovery time without disappearing. More detailed information about biological and psychological systems could support mediational analyses that elucidate the cumulative role of parenting strains, parenting rewards, and their dynamic interplay over the life course of parents.
Second, why were the health risks of parenting children with serious conditions into adulthood primarily physical? Whether looking at parents of adult children who once or still had serious conditions, they seemed to maintain comparable mental health as other parents while their physical health appeared to erode. This finding was unexpected considering the emotional and social toll of parenting under difficult circumstances. It reinforces the theme of interdisciplinary research that psychosocial stress and related strains (e.g., constrained time, exertion) are written on the body, taxing physiological functioning regardless of emotional and psychological adjustment (Jackson et al., 2010; Mezuk et al., 2010). It could also suggest that parents of children with serious conditions are able to draw on the emotional rewards and personal fulfillment of parenting such children in ways that protect their mental health even as the associated strains wear them down physically (Thoits, 2011). This interplay of strains and rewards is ripe for a more qualitative investigation, especially comparing mothers who are juggling these strains and rewards with the experiences of sandwich generation caregiving.
Third, how does the moderating role of duration shed light on the experience of the “longer” parenting career? Parents of children with serious conditions often maintain an active parenting role even when their children have reached adulthood, but this extended parenting is certainly not confined to this particular subset of parents (Birditt et al., 2010). This study’s operationalization of dosage, which reflected maternal age at the onset of a child’s condition, likely tapped into potential age-related changes in mothers’ responsiveness to and efficacy in this particular parenting role. Perhaps the dosage effect is not simply about the cumulative toll of parenting a child in these circumstances over the long term but also about the enhanced ability of mothers who transitioned into this role at older ages to cope, adapt, and recognize rewards amidst strains. For many mothers, age brings the accumulation of material resources (e.g., money, status) and psychosocial resources (e.g., maturity, social networks) that could help to make this parenting experience easier and more fulfilling. Future research needs to tease apart these different dimensions of dosage to ascertain which parents need the most attention.
Fourth, why did two well-documented life course correlates of better health not protect against the health risks of parenting young adult children with serious conditions? A fundamental cause approach suggests that greater social and economic status (e.g., higher levels of educational attainment and more stable marital histories) promotes health in general and particularly amidst trying circumstances (Link & Phelan, 1995). This pattern did not emerge in this study, perhaps because our focus on women highlighted the intersection of gender with social and economic statuses that might complicate the degree to which mothers (vs. fathers) can draw on resources to protect their health when their parenting poses risks (Ha et al., 2008; Song et al., 2016). Future research with fathers will be able to test this possibility, which gets at the ways that motherhood weighs more heavily on women than fatherhood weighs on men in a society that equates parenting with gender and imposes particularly high standards on more advantaged women (i.e., the intensive mothering phenomenon; Hays, 1998).
In posing and addressing these four questions, we recognize that the future research they are intended to inform needs to address some of the limitations of this study’s approach. For example, NLSY79 followed mothers over a long period of the parenting career but did not consistently measure health across that same period. Ideally, a life course examination of the associations between parenting and health would include variables over the long term. This longitudinal framework also raises the challenges of macro-level changes that might trickle down to the individual level. Such factors as the beginning and end of health and human service policies over time need to be taken into account in the search for protective factors and to improve causal inference. As another example, the conceptualization underlying the study of parenting and health involves physiological, biological, and psychological mechanisms that are not often studied in long-term longitudinal studies at the population level. Additionally, this line of research needs to do more to assess the severity of children’s serious conditions and to tease out different categories of serious conditions rather than relying on a single category.
Despite these limitations, we argue that documenting, unpacking, and understanding the connection between parenting adult children with serious conditions and the health of aging parents based on a life course framework that emphasizes human development and societal inequality (e.g., Ferraro & Shippee, 2009) is a valuable enterprise. Not only does this research touch on some of the core tenets of social and behavioral theory theories (e.g., social stress and health, family systems), it also adds a layer of nuance to concerns that more parents are facing this parental role’s challenges for longer periods of their lives (Osgood et al., 2010; Umberson et al., 2010). Although it does not offer specific guidance for particular efforts aiming to support parents and adult children, it can more generally inform the development of new interventions and the targeting of extant interventions by revealing which families are more or less at risk and when and how they are at risk. In these ways, rigorous interdisciplinary attention to this timely topic can offer insight into the evolving nature of family contexts of health disparities and strategy-building around these disparities.
Supplementary Material
Acknowledgments
The authors acknowledge the support of a grants from the National Science Foundation (#1519686; Co-PIs: Elizabeth Gershoff and Robert Crosnoe), the National Institute of Child Health and Human Development (P2CHD042849, PI: Debra Umberson; T32HD007081, PI: Mark Hayward), and the National Institute on Aging (P2CHD042849, PI: Debra Umberson) to the University of Texas at Austin.
Contributor Information
Hyungmin Cha, Department of Sociology and Population Research Center, The University of Texas at Austin
Robert Crosnoe, Department of Sociology and Population Research Center, The University of Texas at Austin.
References
- Augustine JM (2014). Maternal education and the unequal significance of family structure for children’s early achievement. Social Forces, 93(2), 687–718. 10.1093/sf/sou072 [DOI] [Google Scholar]
- Augustine JM (2021). Mothers’ out-of-sequence postsecondary education and their health and health behaviors. Journal of Health and Social Behavior, 0022146520979664. 10.1177/0022146520979664 [DOI] [PubMed] [Google Scholar]
- Barker ET, Greenberg JS, Seltzer MM, & Almeida DM (2012). Daily stress and cortisol patterns in parents of adult children with a serious mental illness. Health Psychology, 31(1), 130–134. 10.1037/a0025325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt KS, Fingerman KL, & Zarit SH (2010). Adult children’s problems and successes: Implications for intergenerational ambivalence. Journals of Gerontology: Series B, 65B(2), 145–153. 10.1093/geronb/gbp125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, & Westlake L (1992). Validating the SF-36 health survey questionnaire. BMJ, 305(6846), 160–164. 10.1136/bmj.305.6846.160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burchinal M, Xue Y, Auger A, Tien H-C, Mashburn A, Cavadel EW, & Peisner-Feinberg E (2016). Quality thresholds, features, and dosage in early care and education: Methods. Monographs of the Society for Research in Child Development, 81(2), 27–45. 10.1111/mono.12237 [DOI] [PubMed] [Google Scholar]
- Chassin L, Macy JT, Seo DC, Presson CC, & Sherman SJ (2010). The association between membership in the sandwich generation and health behaviors: A longitudinal study. Journal of Applied Developmental Psychology, 31, 38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder GH, Johnson MK, & Crosnoe R (2003). The emergence and development of life course theory. In Mortimer JT & Shanahan MJ (Eds.), Handbook of the Life Course (pp. 3–19). New York: Springer US. [Google Scholar]
- Ferraro KF, & Shippee TP (2009). Aging and cumulative inequality: How does inequality get under the skin? Gerontologist, 49(3), 333–343. 10.1093/geront/gnp034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer CS, & Hout M (2006). Century of difference: How America changed in the last one hundred years. New York: Russell Sage Foundation. [Google Scholar]
- Frank KA (2000). Impact of a confounding variable on a regression coefficient. Sociological Methods & Research, 29(2), 147–194. 10.1177/0049124100029002001 [DOI] [Google Scholar]
- Frech A, & Damaske S (2012). The relationships between mothers’ work pathways and physical and mental Health. Journal of Health and Social Behavior, 53(4), 396–412. 10.1177/0022146512453929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha J-H, Hong J, Seltzer MM, & Greenberg JS (2008). Age and gender differences in the well-being of midlife and aging parents with children with mental health or developmental problems: Report of a national study. Journal of Health and Social Behavior, 49(3), 301–316. 10.1177/002214650804900305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hastings RP (2002). Parental stress and behaviour problems of children with developmental disability. Journal of Intellectual & Developmental Disability, 27(3), 149–160. 10.1080/1366825021000008657 [DOI] [Google Scholar]
- Hays S (1998). The cultural contradictions of motherhood. Yale University Press. [Google Scholar]
- Hayward MD, Hummer RA, & Sasson I (2015). Trends and group differences in the association between educational attainment and U.S. adult mortality: Implications for understanding education’s causal influence. Social Science & Medicine, 127, 8–18. 10.1016/j.socscimed.2014.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman JJ, & Robb R (1985). Alternative methods for evaluating the impact of interventions: An overview. Journal of Econometrics, 30(1), 239–267. 10.1016/0304-4076(85)90139-3 [DOI] [Google Scholar]
- Hoffman B (2008). Health care reform and social movements in the U.S. American Journal of Public Health, 98, S69–S79. 10.2105/AJPH.98.Supplement_1.S69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton TV, & Wallander JL (2001). Hope and social support as resilience factors against psychological distress of mothers who care for children with chronic physical conditions. Rehabilitation Psychology, 46(4), 382–399. 10.1037/0090-5550.46.4.382 [DOI] [Google Scholar]
- Jackson JS, Knight KM, & Rafferty JA (2010). Race and unhealthy behaviors: Chronic stress, the hpa axis, and physical and mental health disparities over the life course. American Journal of Public Health, 100(5), 933–939. 10.2105/AJPH.2008.143446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janus AL (2009). Disability and the transition to adulthood. Social Forces, 88(1), 99–120. 10.1353/sof.0.0248 [DOI] [Google Scholar]
- Kiecolt-Glaser JK, & Newton TL (2001). Marriage and health: His and hers. Psychological Bulletin, 127(4), 472–503. 10.1037/0033-2909.127.4.472 [DOI] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, appraisal, and coping. New York: Free Press. [Google Scholar]
- Lin F-Y, Rong J-R, & Lee T-Y (2013). Resilience among caregivers of children with chronic conditions: A concept analysis. Journal of Multidisciplinary Healthcare, 6, 323–333. 10.2147/JMDH.S46830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, & Phelan J (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, 35, 80. 10.2307/2626958 [DOI] [PubMed] [Google Scholar]
- Mann C, Rowland D, & Garfield R (2003). Historical overview of children’s health care coverage. Future of Children, 13, 31–53. 10.2307/1602638 [DOI] [PubMed] [Google Scholar]
- Masten AS, & Garmezy N (1985). Risk, vulnerability, and protective factors in developmental psychopathology. In Lahey BB & Kazdin AE (Eds.), Advances in Clinical Child Psychology (pp. 1–52). Springer US. [Google Scholar]
- Mezuk B, Rafferty JA, Kershaw KN, Hudson D, Abdou CM, Lee H, Eaton WW, & Jackson JS (2010). Reconsidering the role of social disadvantage in physical and mental health: Stressful life events, health behaviors, race, and depression. American Journal of Epidemiology, 172(11), 1238–1249. 10.1093/aje/kwq283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirowsky J (1999). Analyzing associations between mental health and social circumstances. In Handbook of the Sociology of Mental Health (pp. 105–123). Springer Nature. [Google Scholar]
- Mirowsky J, & Ross CE (2003). Education, social status, and health (1 edition). Routledge. [Google Scholar]
- Osgood DW, Foster EM, & Courtney ME (2010). Vulnerable populations and the transition to adulthood. Future of Children, 21, 209–229. 10.1353/foc.0.0047 [DOI] [PubMed] [Google Scholar]
- Pinquart M (2017). Associations of parenting dimensions and styles with externalizing problems of children and adolescents: An updated meta-analysis. Developmental Psychology, 53(5), 873–932. 10.1037/dev0000295 [DOI] [PubMed] [Google Scholar]
- Prickett KC, & Augustine JM (2016). Maternal education and investments in children’s health. Journal of Marriage and Family, 78(1), 7–25. 10.1111/jomf.12253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichman NE, Corman H, & Noonan K (2004). Effects of child health on parents’ relationship status. Demography, 41(3), 569–584. 10.1353/dem.2004.0026 [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR, & Rubin DB (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70(1), 41–55. 10.1093/biomet/70.1.41 [DOI] [Google Scholar]
- Rubin DB (2004). Multiple imputation for nonresponse in surveys. John Wiley & Sons. [Google Scholar]
- Ruppanner L, Perales F, & Baxter J (2019). Harried and unhealthy? Parenthood, time pressure, and mental health. Journal of Marriage and Family, 81(2), 308–326. 10.1111/jomf.12531 [DOI] [Google Scholar]
- Sameroff A (2006). Identifying risk and protective factors for healthy child development. In Families count: Effects on child and adolescent development (pp. 53–76). Cambridge University Press. [Google Scholar]
- Schwartz C (2003). Parents of children with chronic disabilities: The gratification of caregiving. Families in Society, 84(4), 576–584. 10.1606/1044-3894.143 [DOI] [Google Scholar]
- Seltzer MM, Floyd F, Song J, Greenberg J, & Hong J (2011). Midlife and aging parents of adults with intellectual and developmental disabilities: Impacts of lifelong parenting. American Journal on Intellectual and Developmental Disabilities, 116(6), 479–499. 10.1352/1944-7558-116.6.479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song J, Mailick MR, Greenberg JS, Ryff CD, & Lachman ME (2016). Cognitive aging in parents of children with disabilities. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71(5), 821–830. 10.1093/geronb/gbv015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoits PA (2010). Stress and health: Major findings and policy implications. Journal of Health and Social Behavior, 51, S41–S53. 10.1177/0022146510383499 [DOI] [PubMed] [Google Scholar]
- Thoits PA (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52(2), 145–161. 10.1177/0022146510395592 [DOI] [PubMed] [Google Scholar]
- Tumin D, & Zheng H (2018). Do the health benefits of marriage depend on the likelihood of marriage? Journal of Marriage and Family, 80(3), 622–636. 10.1111/jomf.12471 [DOI] [Google Scholar]
- Umberson D, Pudrovska T, & Reczek C (2010). Parenthood, childlessness, and well-being: A life course perspective. Journal of Marriage and Family, 72(3), 612–629. 10.1111/j.1741-3737.2010.00721.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Cleave J, Gortmaker SL, & Perrin JM (2010). Dynamics of obesity and chronic health conditions among children and youth. JAMA, 303(7), 623–630. 10.1001/jama.2010.104 [DOI] [PubMed] [Google Scholar]
- Williams K, & Umberson D (2004). Marital status, marital transitions, and health: A gendered life course perspective. Journal of Health and Social Behavior, 45(1), 81–98. 10.1177/002214650404500106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willson AE, Shuey KM, & Elder GH (2007). Cumulative advantage processes as mechanisms of inequality in life course health. American Journal of Sociology, 112(6), 1886–1924. [Google Scholar]
- Winship C, & Radbill L (1994). Sampling weights and regression analysis. Sociological Methods & Research, 23(2), 230–257. 10.1177/0049124194023002004 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


