Abstract
In this report, we present a 38-year-old female with acute cholecystitis, in which an aberrant right hepatic duct draining directly into the cystic duct was revealed by intraoperative cholangiography during a laparoscopic cholecystectomy. This anomaly was classified as the class V variant using the Hisatsugu classification schema, which has an incidence of 1.02%. The use of Strasberg’s critical view of safety has become ubiquitous in laparoscopic cholecystectomy. Intraoperative cholangiography provides and additional layer of safety, and should be considered as a routine practice, particularly when imaging to delineate biliary anatomic aberrancies has not been performed prior to surgery.
Keywords: Aberrant right hepatic duct, Cholangiography, Critical field of view, Laparoscopic cholecystectomy
BACKGROUND
The first laparoscopic cholecystectomy was performed by Professor Dr. Med Erich Muhe of Boblingen, Germany in 1985.1 Laparoscopic cholecystectomy (LC) has been refined considerably since that time. However, one of the most feared complications continues to be injury to the biliary ducts.2,3 One of the risk factors for bile duct injuries include aberrant bile duct variations.2
The debate of routine versus selective intraoperative cholangiogram (IOC) has persisted due to its associated risks4 since the introduction of LC. Risks of IOC include iatrogenic bile duct injuries, unneeded common bile duct exploration, pancreatitis, or added time and increased costs.4 However, due to the variety in biliary anatomy, advocates of routine IOC point to its role in confirming certain ductal aberrancies and thus, decreasing the rate of injury.5
An aberrant right hepatic duct (ARHD) is a rare anatomic variant.6 Cases are documented on pre-operative and intraoperative findings using the Hisatsugu classification system (HCS), which has classified five variants with this schema, as shown below (Figure 1).6
Figure 1.
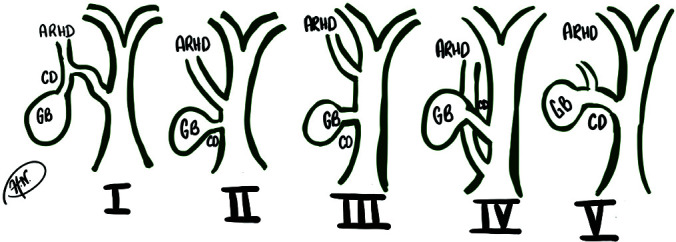
Hisatsugu classification system of aberrant right hepatic duct variants.
To recall the pertinent ductal anatomy: the right hepatic duct drains segments of the right liver lobe: V-VIII and further divides into two major branches: the right posterior branch, which drains posterior segments VI and VII and the right anterior duct that drains the anterior segments V and VIII. Ectopic drainage of the R hepatic duct into the cystic duct is typically limited to the R posterior branch draining segments V and VII. The rarest ectopic drainage type, according to HCS, is the fifth variant. According to Katoaka et al., this type V variant was reported with an incidence rate of 1.02%.7 Variants I and V have the greatest risk of injury during cholecystectomy because of their direct junction with the cystic duct.6
The case described below illustrates a successful laparoscopic cholecystectomy with the utility of intraoperative cholangiogram and critical view of safety method to reveal ARHD in a patient preoperatively diagnosed with acute cholecystitis. IOC imaging revealed the rare type V variant by HCS, in which the ARHD drained anomalously into the cystic duct (Figure 3).
Figure 3.
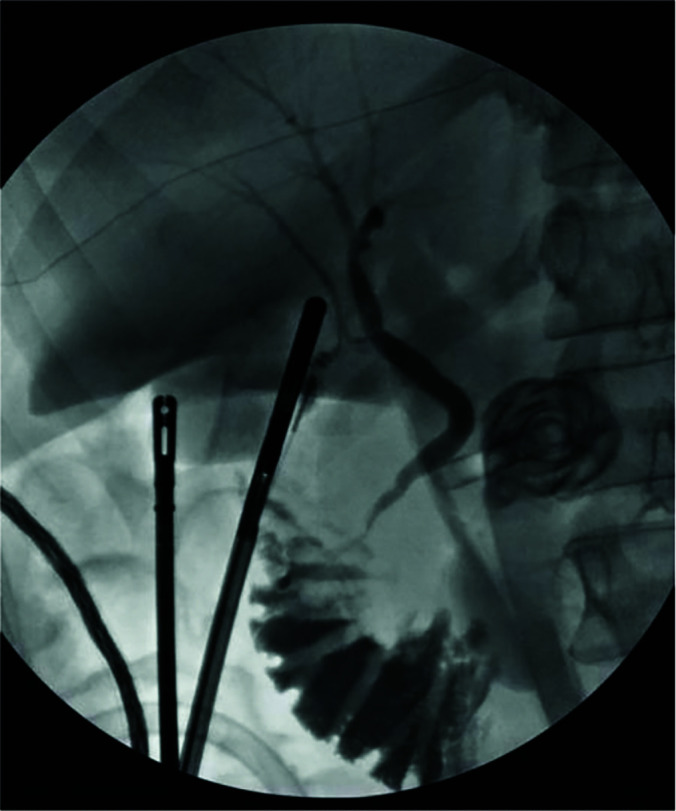
Intraoperative cholangiogram with contrast dye illustrating the type V aberrant posterior branch of Right Hepatic Duct Draining Into The Cystic Duct.
CASE PRESENTATION
A 38-year-old female who initially presented with progressive right upper quadrant abdominal pain with associated nausea and subjective fevers was referred to our department for surgical intervention.
Ultrasound revealed biliary sludge and small stones consistent with the diagnosis of cholelithiasis. The patient was then consented for laparoscopic cholecystectomy with an intraoperative cholangiogram. A standard 4 port technique was used for the procedure.
Intraoperative imaging revealed the cystic duct, the common bile duct without filling defects, and free flow of contrast into the duodenum and both the left and right hepatic ducts. The right hepatic duct was noted to drain directly into the cystic duct near its junction with the common bile duct. This is a type V ARHD variant using HCS. Seven mm clips were placed on the cystic duct distal to the aberrant anatomy near the infundibulum preserving the ARHD proximal cystic duct junction, and the cystic artery was then clipped and divided in the usual fashion. Electrocautery was used to dissect the gallbladder from the hepatic fossa. Pericholecystic edema was noted. The gallbladder was placed in an Endo Catch™ Retrieval pouch and removed through the periumbilical port.
The patient’s postoperative course was unremarkable.
DISCUSSION
The critical view of safety is a widely adopted algorithm for avoiding injury to major biliary ducts during laparoscopic cholecystectomy (Figure 2). This case emphasizes the utility of IOC in supplementing the critical view of safety in identifying aberrancies of the right hepatic duct, a common causes of bile duct injuries during laparoscopic cholecystectomy.3 Routine use of IOC during less challenging cases augments the surgeon’s skills so that the technique may be more easily applied in complex cases. Near infrared imaging with indocyanine green (ICG) is another option for intraoperative mapping of biliary anatomy. Multiple investigators have demonstrated equivalency of IOC and ICG for biliary tract visualization.8
Figure 2.
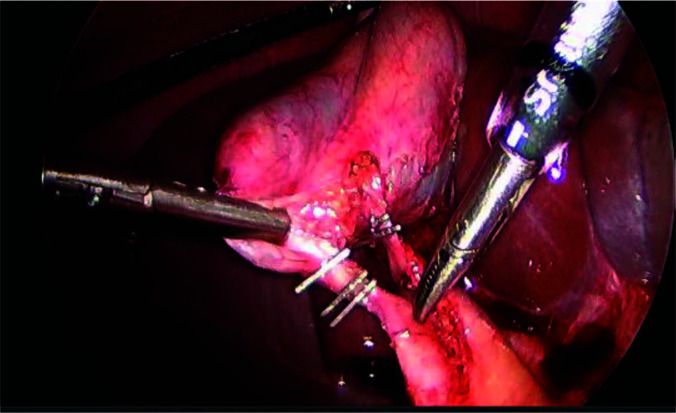
Critical view of safety technique in laparoscopic cholecystectomy, anterior view.
The critical According to Hisatsugu, et al. and Katoaka et al. the type V variant is the rarest of extrahepatic biliary anomalies and only one of two associated with high risk of intraoperative bile duct injury, with an incidence of 1.02%.7 Without proper anatomical awareness, clipping of the ARHD may result in recurrent obstructive cholangitis, as well as subsequent intrahepatic lithiasis, liver atrophy, and cholangiocarcinoma, as well as other iatrogenic complications.3 It is not uncommon to vary surgical technique in response to these anatomic variations.9 As well, accurate reporting of these rare anatomical anomalies is crucial to increase clinical awareness and prevent postoperative complications for future patients.
Further work-up in evaluating ARHD can include evaluating the extent of hepatic segment drainage into the anomalous right hepatic duct, as more segments involved may potentially correlate with the degree of postoperative complications.3,10 This may be of clinical value in select cases to further intraoperative technique in laparoscopic cholecystectomy, should the ARHD be in more challenging locations in relation to the cystic duct.5,11
CONCLUSION
This case summarizes a rare yet clinically crucial case of ARHD type V variant using the Hisatsugu classification framework during laparoscopic cholecystectomy for the treatment of cholelithiasis. The use of intraoperative cholangiography following the Critical View of Safety method to reveal this anomaly has shown to be an effective approach for successful management of an aberrant right hepatic duct during laparoscopic cholecystectomy.
Footnotes
Conflict of interests: none.
Disclosure: none.
Funding sources: none.
Disclaimer: The views expressed are those of the authors and do not reflect the official views of the Uniformed Services University of the Health Sciences, Womack Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of Defense, the Departments of the Army, Navy or Air Force, or the U.S. Government. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government.
Informed consent: Dr. Adam J. Kaplan declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Hema M. Narlapati, Edward Via College of Osteopathic Medicine, Spartanburg, SC, AL.
Simon H. Telian, Womack Army Medical Center, Ft Bragg, NC..
Gregory S. Peirce, Uniformed Services University of the Health Sciences, Bethesda, MD..
Adam J. Kaplan, Uniformed Services University of the Health Sciences, Bethesda, MD..
References:
- 1.Reynolds W., Jr. The first laparoscopic cholecystectomy. JSLS. 2001;5(1):89–94. [PMC free article] [PubMed] [Google Scholar]
- 2.Fletcher DR, Hobbs MS, Tan P, et al. Complications of cholecystectomy: risks of the laparoscopic approach and protective effects of operative cholangiography: a population-based study. Ann Surg. 1999;229(4):449–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strasberg SM. Avoidance of biliary injury during laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 2002;9(5):543–547. [DOI] [PubMed] [Google Scholar]
- 4.Callery MP. Cholecystitis and stones in the common bile duct. Blumgart's Surgery of the Liver, Biliary Tract and Pancreas. Vol 1: Elsevier. 2017:623–632. [Google Scholar]
- 5.Whitman NL, Longmire WP., Jr. A clinical and experimental evaluation of the primary treatment of injuries to the common bile duct. Am J Surg. 1958;96(2):287–295. [DOI] [PubMed] [Google Scholar]
- 6.Kurahashi S, Komatsu S, Matsumura T, et al. A novel classification of aberrant right hepatic ducts ensures a critical view of safety in laparoscopic cholecystectomy. Surg Endosc. 2020;34(7):2904–2910. [DOI] [PubMed] [Google Scholar]
- 7.Kataoka J, Nitta T, Inoue Y, et al. A case of an anomalous biliary tract diagnosed preoperatively. J Surg Case Rep. 2017;2017(6):rjx106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vlek SL, van Dam DA, Rubinstein SM, et al. Biliary tract visualization using near-infrared imaging with indocyanine green during laparoscopic cholecystectomy: results of a systematic review. Surg Endosc. 2017;31(7):2731–2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Talpur KA, Laghari AA, Yousfani SA, Malik AM, Memon AI, Khan SA. Anatomical variations and congenital anomalies of extra hepatic biliary system encountered during laparoscopic cholecystectomy. J Pak Med Assoc. 2010;60(2):89–93. [PubMed] [Google Scholar]
- 10.Longmire WP, Jr., Tompkins RK. Lesions of the segmental and lobar hepatic ducts. Ann Surg. 1975;182(4):478–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vasiliadis K, Moschou E, Papaioannou S, et al. Isolated aberrant right cysticohepatic duct injury during laparoscopic cholecystectomy: evaluation and treatment challenges of a severe postoperative complication associated with an extremely rare anatomical variant. Ann Hepatobiliary Pancreat Surg. 2020;24(2):221–227. [DOI] [PMC free article] [PubMed] [Google Scholar]