Abstract
Background:
The frequency and severity of extreme weather events such as wildfires are expected to increase due to climate change. Childbearing women, that is, women who are pregnant, soon to be pregnant, or have recently given birth, may be particularly vulnerable to the effect of wildfire exposure.
Objectives:
This review sought to systematically assess what is known about birth outcomes, health, and health care needs of childbearing women during and after exposure to wildfires.
Methods:
An integrative review methodology was utilized to enable article selection, data extraction, and synthesis across qualitative and quantitative studies. Comprehensive searches of SCOPUS (including MEDLINE and Embase), CINAHL, PubMed, and Google Scholar identified studies for inclusion with no date restriction. Included studies were independently appraised by two reviewers using the Crowe Critical Appraisal Tool. The findings are summarized and illustrated in tables.
Results:
Database searches identified 480 records. Following title, abstract, and full text screening, sixteen studies published between 2012 and 2022 were identified for this review. Eleven studies considered an association between in utero exposure to wildfire and impacts on birth weight and length of gestation. One study reported increased rates of maternal gestational diabetes mellitus and gestational hypertension following exposure; whereas one study reported differences in the secondary sex ratio. Two studies reported higher incidence of birth defects following in utero exposure to wildfire smoke. Three studies reported increased mental health morbidity, and one study associated a reduction in breastfeeding among women who evacuated from a wildfire disaster.
Discussion:
Evidence indicates that wildfire exposure may be associated with changes to birth outcomes and increased morbidity for childbearing women and their babies. These effects may be profound and have long-term and wide-ranging public health implications. This research can inform the development of effective clinical and public health strategies to address the needs of childbearing women exposed to wildfire disaster. https://doi.org/10.1289/EHP10544
Introduction
Although fire, both naturally occurring and anthropogenic in nature, has shaped the landscape and influenced the natural biome for millions of years, wildland fires that are catastrophic to the ecosystem or human society have been rare throughout history.1 Climate change and an increase in populations living close to the wildland–urban interface have contributed to increased frequency and intensity of wildfires.2
The United Nations identifies climate change as “the defining issue of our time… global in scope and unprecedented in scale.”3 The World Health Organization (WHO) cites climate change and related natural disasters as having a major negative effect on the social and environmental determinants of health and estimates more than 250,000 climate-related deaths per year by 2030.4
The impetus for this work arose in response to the extreme Australian 2019–2020 bushfire season (the Black Summer). Throughout the spring and summer of 2019–2020, the changing global climate contributed to an extreme bushfire season across the Australian continent, resulting in devastating loss of life, property, wildlife, and environmental destruction.5
Numerous studies and reviews are available on natural disasters and the effects of exposure to disaster events on the health and well-being of childbearing women and their babies, with outcomes related to decreased fetal growth, increased maternal mental health morbidity, adverse outcomes relating to the sexual and reproductive health of women, and their increased economic vulnerability both during and after disaster.6 Exposure to disaster has also been reported to influence the secondary sex ratio.7–9
The smoke from wildfires is a source of fine particulate matter (, particulate matter with aerodynamic diameter ) and presents a risk to human health.10,11 Maternal exposure to is well studied, and exposure is associated with a reduction in birth weight,12,13 increased incidence of preterm birth,14 increased incidence of cleft palate,15 as well as development of gestational diabetes mellitus (GDM).16–18
The effect of wildfire exposure on birth, health outcomes, and health care needs of childbearing women—i.e., women who are pregnant, soon to be pregnant, or have recently given birth—and their babies is the focus of this review. In this context, wildfire is defined as an unplanned, uncontrolled fire in areas of vegetation and includes fires that would be described using the Australian English term “bushfire.” Given that climate change will continue and natural disasters including wildfires are anticipated to increase in frequency and severity, understanding how wildfires impact on birth outcomes and gathering evidence to support the health and health care needs of childbearing women during and after wildfire events is important. To our knowledge, this is the first integrative review to consolidate the evidence on the impact of this exposure on birth outcomes and childbearing women’s health and health care needs.
Methodology
An integrative review methodology based on the framework proposed by Whittemore and Knafl,19 was chosen to enable article selection, data extraction, and synthesis across qualitative and quantitative studies to gain a holistic understanding of the topic and to present comprehensive perspectives to answer the research question, “What do we know about birth outcomes and health and health care needs of childbearing women during and after exposure to wildfire smoke or a wildfire disaster?”
A protocol for this review was registered in the International Prospective Register of Systematic Reviews database (PROSPERO # 42020214499) on 15 November 2020.
Search Strategy
A comprehensive, reproducible search strategy was developed to identify relevant qualitative and quantitative studies. Thematic searches were performed by J.E. and replicated by D.D., using the search string described in Table 1. Final searches were performed on 19 May 2022. SCOPUS (including MEDLINE and Embase), PubMed, and CINAHL searches used identical terms; the Google Scholar search used a simpler syntax in an effort to conveniently return relevant gray literature. To maintain manageable scope, only the first 50 Google Scholar matches were considered. To further scope, reference lists of studies for full text review were manually searched to identify additional studies (J.E.).
Table 1.
Formal search strategy.
| Search engine | Search terms |
|---|---|
| SCOPUS (including MEDLINE and Embase), CINAHL, PubMed | bushfire or wildfire or “bush fire” or “wild fire” or “wildland fire” AND pregnan* or prenatal or antenatal or postnatal or labor or birth or lactat* or breastfe* or matern* or baby or newborn or infant or mother or “domestic violence” or “family violence” or “mental health” |
| Google Scholar |
(bushfire OR wildfire) AND (pregnant OR pregnancy OR prenatal OR labor OR birth OR lactation OR lactating OR maternal OR maternity OR baby OR newborn OR infant OR birth outcome) |
Inclusion and Exclusion Criteria
Titles and abstracts were double screened independently (J.E., D.D.) to assess eligibility by applying inclusion and exclusion criteria. They were first screened by title and abstract and further after full text review. To be included in the review, studies had to be original, wildfire-specific research with outcomes relevant to the research question. Case studies and reviews were excluded. Any pregnancy or birth outcome was considered, and health care and social needs of childbearing women were included. No date limitation was applied to the search. Nonwildfire studies were excluded [for example, studies involving fires associated with other disasters, fires associated with specific industries, and prescribed burns or fires that were agricultural in nature (such as fires to clear land for farming or to prepare a crop for harvest)]. Non-English language articles were excluded, as were nonhuman studies.
Quality Assessment
Critical appraisal of the sixteen full text articles was undertaken by two reviewers independently (J.E. and D.D.) and scored using the Crowe Critical Appraisal Tool (CCAT; version 1.4).20 The CCAT is particularly suited to assess quality of evidence in this review because it is a tool that can be used to compare and appraise evidence quality in a standardized way across a range of research designs, including quantitative and qualitative studies.21
Following the CCAT framework, appraisal of each study focused on items across eight domains: preliminaries, introduction, design, sampling, data collection, ethical matters, results, and discussion. A detailed, descriptive list of items to be assessed is provided for each domain to guide appraisal, and details of the criteria can be found in the CCAT User Guide.22
The CCAT User Guide encourages appraisers to take a holistic view of studies to make a judgment in relation to scoring rather than relying solely on the checklist. For this review, the reviewers met prior to scoring to formalize a strategy and discuss how CCAT scores would be attributed for each domain. Central to the appraisal was the notion that not every item on the checklist would be applicable to every study design, and absence of an item did not mean the domain for that study would be marked with a lower score, but rather overall quality of the domain would be considered when assigning a score.
Each domain was scored (from 0 to 5), with 0 being the lowest possible score and 5 the highest. To obtain a high score in a domain, the study being assessed needed to demonstrate characteristics of that domain appropriate to the research design, how well aspects of the domain suited the research question, and how well aspects of the domain were expressed throughout the text. A lower score was given where characteristics of a domain applicable to a research design were omitted, problematic, or poorly conveyed.
The following domains and items were assessed using the CCAT framework:
“Preliminaries” included an assessment of the quality of the title, abstract, study aims, design and clarity of the overall study text.
“Introduction” included an assessment of the background section of each study, the summary of current knowledge, study context, objective, hypothesis and/or aim, and secondary questions.
“Design” included an assessment of the justification for design, the suitability of the design to support the research question, definitions, and validity of exposures and outcomes (including methods of measurement, potential sources of bias including confounding, effect modification, procedures for randomization (where appropriate), group balance, and equivalence).
“Sampling” included an assessment of suitability and justification of sampling methods to both the study question and study design, description of sample sizes and protocols, suitability for purpose, sample size calculations (where applicable), inclusion and exclusion criteria, and recruitment strategy.
“Data collection” included an assessment of data collection protocols and suitability of methods for individual study designs; use of tools to enhance data quality, validity, and reliability; efforts to eliminate bias; control for confounding and effect modifiers; and assessment of how nonparticipation and incomplete or missing data were treated.
“Ethical matters” included an assessment of participant ethics, including equity and informed consent (where applicable), privacy and anonymity consideration, and an assessment of researcher ethics comprising ethical approval (where appropriate), identification of conflicts of interest, and sources of funding.
“Results” included an assessment of the suitability and robustness of analysis; integration and interpretation methods, including statistical and nonstatistical methods; demographic data and subgroup analyses (where relevant); and whether analysis and interpretation methods were suited to research design and objectives.
“Discussion” included an assessment of how study results could be interpreted and could build on current evidence and considered limitations and the role of bias as well as the generalizability of findings and recommendations for further research.
Although the CCAT allows the appraisal framework to be used across study designs, it also introduces a level of subjectivity to the process. Appraisers are encouraged to publish scores for each domain rather than only totals so that a more granular understanding of the appraisal is presented. The strength of this framework lies in the comprehensive, consistent, and standardized framework provided for the appraisal across a variety of research designs.
Overall, all 16 studies were deemed of sufficient quality to be included in this review, with CCAT scores ranging between 66.5 and 96.365. Each reviewer’s score across each of the domains as well as the average of reviewers’ total scores are included in Table 2.
Table 2.
Crowe Critical Appraisal Tool (CCAT) scores for the 16 studies included in this review.
| Heft-Neal et al.27 | Requia, Amini et al.35 | Requia, Paptheodorou et al.36 | Costello28 | Jones and McDermott29 | Park et al.30 | Requia et al.31 | McCoy and Zhao32 | Abdo et al.33 | O’Donnell and Behie25 | O’Donnell and Behie24 | Holstius et al.34 | O’Donnell23 | Brémault-Phillips et al.39 | Verstraeten et al.37 | DeYoung et al.38 | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CCAT domains | R1a | R2b | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 | R1 | R2 |
| Preliminaries | 5 | 5 | 4 | 3 | 4 | 4 | 3 | 4 | 4 | 2 | 4 | 5 | 3 | 3 | 3 | 2 | 5 | 5 | 4 | 4 | 5 | 4 | 4 | 4.5 | 5 | 5 | 5 | 4 | 5 | 4 | 3 | 2 |
| Introduction | 4 | 5 | 4 | 3.5 | 4 | 4 | 3 | 3 | 4 | 3 | 5 | 5 | 4 | 3 | 3 | 4 | 5 | 5 | 4 | 4 | 4 | 5 | 4 | 5 | 5 | 4.5 | 4 | 2 | 4 | 4.5 | 3 | 3.5 |
| Design | 5 | 5 | 5 | 5 | 4 | 4 | 4 | 4 | 3 | 3 | 4 | 4 | 4 | 4 | 4 | 3 | 5 | 5 | 3 | 4 | 3 | 3 | 4 | 4.5 | 4 | 5 | 4 | 4.5 | 5 | 4 | 4 | 3.5 |
| Sampling | 5 | 5 | 4 | 5 | 4 | 4 | 4 | 4 | 4 | 3 | 4 | 4 | 4 | 4 | 3 | 2 | 4 | 4 | 4 | 4.5 | 4 | 3 | 4 | 5 | 4 | 4.5 | 3 | 3 | 5 | 3.5 | 4 | 3 |
| Data collection | 5 | 4 | 4 | 4 | 4 | 4 | 4 | 5 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 5 | 4 | 5 | 3 | 3 | 4 | 5 | 5 | 4.5 | 4 | 4 | 4 | 4 | 4 | 2.5 |
| Ethical matters | 4 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 4 | 4 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 5 | 4 | 5 | 5 | 5 | 5 | 5 | 4 | 3.5 | 4 | 4 |
| Results | 5 | 5 | 4 | 4 | 4 | 4 | 3 | 4 | 4 | 4 | 5 | 5 | 3 | 4 | 3 | 3.5 | 5 | 5 | 4 | 4 | 4 | 4 | 4 | 4.5 | 4 | 5 | 5 | 4.5 | 4 | 4 | 4 | 2 |
| Discussion | 5 | 5 | 4 | 5 | 4 | 5 | 3 | 4 | 4 | 4 | 5 | 5 | 4 | 4 | 2 | 2.5 | 5 | 5 | 4 | 4.5 | 5 | 5 | 4 | 4 | 5 | 5 | 5 | 4.5 | 5 | 4 | 4 | 3 |
| Average CCAT score/100 | 96.25 | 85.62 | 83.75 | 77.5 | 72.5 | 91.25 | 77.5 | 66.5 | 96.365 | 83.75 | 81.5 | 88.125 | 94.375 | 83.175 | 85.625 | 66.875 | ||||||||||||||||
Note: CCAT domains and items assessed within the domain [Refer to: Crowe Critical Appraisal Tool (CCAT) User Guide Version 1.422 for further detail]. Preliminaries refer to title, abstract, and text. Introduction refers to background and objectives. Design refers to research design, intervention, treatment, exposure; outcome, output, predictor, measure; bias. sampling refers to sampling method, sample size, sampling protocol. Data collection refers to collection method and collection protocol. Ethical matters includes participant ethics and researcher ethics. Results refers to analysis, integration, interpretation method, essential analysis, outcome, output, and predictor analysis. Discussion includes interpretation, generalization and concluding remarks.
Reviewer 1.
Reviewer 2.
Data Extraction and Synthesis
Features of included studies were extracted in tabular format to facilitate analysis and comparison across studies by one researcher and audited by a second. This table comprised data on individual studies including year of publication, study duration, study design, study objective, and data sources; characteristics of the wildfire event of interest, including fire duration and fire size; exposure measurement, including exposure period; outcomes assessed; findings, including outcomes assessed, statistics, and qualitative themes. Pooling of data for meta-analysis was not deemed reasonable, given heterogeneity in study designs, methods, exposures, and outcomes. Rather, a synthesis was undertaken whereby findings related to specific outcomes from a range of studies are presented within descriptive themes.
Results
Search Results
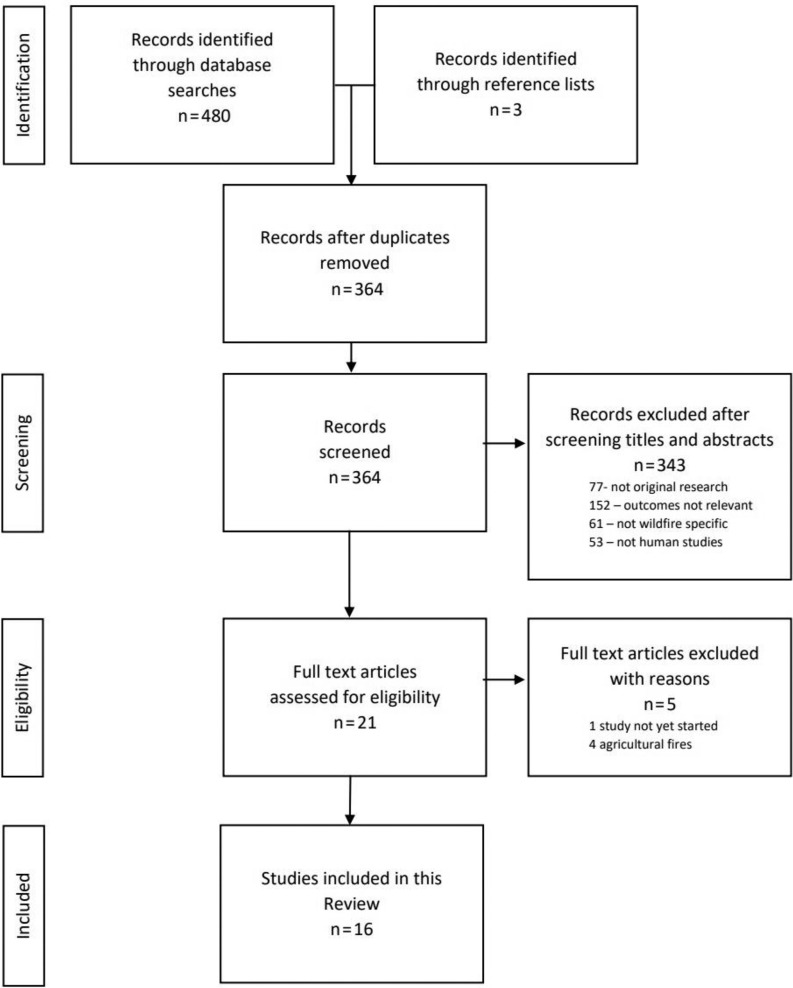
Database searches identified 480 records. Three records were identified through reference list searches. After duplicates were removed, 364 records were screened by title and abstract. Title and abstract screening resulted in the removal of 343 records for the following reasons: A total of 77 were not original research, 152 had outcomes that were not relevant to the objectives of this study, 61 were not wildfire-specific studies, and 53 were not human studies. Twenty-one full-text articles were assessed for eligibility, with four excluded because they were deemed “agricultural” fires, and one was excluded because it outlined a protocol for a study that had not yet started.
Sixteen studies published between 2012 and 2022 met criteria and were included in this review.
One study23 rereported some outcomes from previously published studies24,25; however because this study also included reanalysis of some data and a qualitative component, it was deemed worthwhile to be included as a separate body of work.
The search results are summarized in Figure 1 using the Preferred Reporting Items for Systemic Reviews and Meta-Analysis (PRISMA)26 flowchart to depict the process.
Figure 1.
Preferred reporting items for Systematic Reviews and Meta-Analyses (PRISMA) Flow Diagram.
Study Designs
Of the included studies in this review, 13 were quantitative (10 retrospective cohort studies,24,25,27–34 one case–control study,35 one time-stratified case–crossover study,36 and one longitudinal study37), 2 used mixed methods,23,38 and one was a qualitative study39 (Table 3).
Table 3.
Characteristics of the 16 studies included in this review.
| Author/Year/Title | Location/event of interest | Study design | Data sources | Exposure measurement | Outcomes assessed/findings |
|---|---|---|---|---|---|
|
Heft-Neal, S., Driscoll, A., Yang, W., Shaw, G., & Burke, M 2022 Associations between wildfire smoke exposure during pregnancy and risk of preterm birth in California. |
California, USA Wildfire smoke exposure 2006–2012 |
Retrospective cohort study of 3,002,014 births between 2006 and 2012 |
Administrative data: birth certificate data from Vital Records, Department of Health, California Satellite imagery: National Oceanic and Atmospheric Administration (NOAA) satellite-based Hazard Mapping System and Geostationary Operational Environmental Satellite system (GOES) Daily levels: Daily and annual concentrations for the contiguous United States, grids data set |
Exposure window: in utero at time of wildfire smoke exposure Temporal-spatial Wildfire smoke plumes were assembled using satellite imaging and combined with gridded estimates of surface . Smoke exposure was assigned to individual pregnancies at the maternal ZIP-code level. Comparison: dose–response measured as median wildfire smoke exposure and each additional day of wildfire smoke exposure |
Risk of preterm birth at median smoke exposure (7 d)
Each additional day of exposure increased relative risk of preterm birth
|
|
Requia, W.J., Amini, H., Adams, M.D., & Schwartz, J.D. 2022 Birth weight following pregnancy wildfire smoke exposure in more than newborns in Brazil: A nationwide case control study. |
Brazil Wildfire smoke exposure 2001–2018 |
Case–control study of 1,602,471 observations between 2001 and 2018 |
Administrative data: birth certificate data from Ministry of Health–Brazil Satellite imagery: National Institute of Spatial Research–Brazil/Instituto Nacional de Pesquisas Espaciais (INPE) in a grid Ambient air pollution including daily levels and weather data: Environmental Information System for Health/Instituto Nacional de Pesquisas Espaciais (INPE) Precipitation data derived from the Climate Prediction Center and National Oceanic and Atmospheric Administration (NOAA) |
Exposure window: in utero at time of wildfire smoke exposure Temporal-spatial Spatial resolution of birth data was based on the mother’s home municipality. A total of 5,572 municipalities were grouped into 5 regions. Average and meteorological covariates were calculated for each trimester within the boundaries of the mother’s home municipality Comparison: dose–response measured as an increase of 100 wildfire records |
Risk of LBW increased following wildfire smoke exposure by
|
|
Requia, W.J., Papatheodorou, S., Koutrakis, P., Mukherjee, R., & Roig, H.L. 2022 Increased preterm birth following maternal wildfire smoke exposure in Brazil. |
Brazil Wildfire smoke exposure 2001–2018 |
Time-stratified case-crossover study of 190,911 preterm births 2001–2018 |
Administrative data: birth certificate data from Ministry of Health–Brazil Satellite imagery: National Institute of Spatial Research–Brazil/Instituto Nacional de Pesquisas Espaciais (INPE) at an image resolution from to Ambient air pollution and weather data: Environmental Information System for Health/Instituto Nacional de Pesquisas Espaciais (INPE) : ground observations of the Aerosol Robotic Network (AERONET) Precipitation data derived from the Climate Prediction center and National Oceanic and Atmospheric Administration (NOAA) |
Exposure window: in utero at time of wildfire smoke exposure Each trimester exposure was based on the average of daily estimated wildfire exposure, pollutant concentrations (, CO, , and ) and meteorological variables. Spatial resolution of birth data was based on the mother’s home municipality. 5,572 municipalities were grouped into 5 regions Comparison: exposure to a “wildfire wave” vs. nonexposure. The “wildfire wave” concept was adopted to capture periods with high wildfire occurrences: A “wildfire wave” was any average value of wildfire records and concentration that exceeded the 90th percentile of the time series. |
Risk of preterm birth increased following exposure to during a “wildfire wave”
|
|
Costello, J. 2021 Air quality and preterm birth: distance to highways, exposure to wildfires, and effect modification by COVID-19 |
San Francisco Bay Area, USA “Camp Fire” November 2018 (12-day event) |
Retrospective cohort study of 68,006 births of women who were pregnant during the fire dates in 2017 or 2018 |
Administrative data: Vital Records, Department of Health, California, and hospital records from California Office of Statewide Planning and Development Daily average levels: data from Purple Air personal pollution sensors data within specific coordinates Wildfire smoke mapping: Geostationary Operational Environmental Satellite (GOES) |
Exposure window: pregnancies which overlapped the full fire period (12 d) and lived within the study extent. Comparison: exposed vs. unexposed. An unexposed status was assigned to pregnancies that occurred during the same time period and study area, but 1 y earlier, in November 2017. |
Risk of preterm birth following exposure to the Camp Fire was associated with:
The level of exposure was associated with preterm birth
|
|
Jones, B.A., & McDermott, S. 2021 Infant health outcomes in mega-fire affected communities |
USA Any mega-fire acres in size 2010–2017 |
Retrospective cohort study of 689,762 births between 2010 and 2017 |
Administrative data: neonatal collection: Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS) Sources of mega-fires: Geospatial Multi-Agency Coordination Group (GeoMAC) Weather data: National Oceanic and Atmospheric Administration (NOAA) National Centers for Environmental Information (NCEI) |
Exposure window: in utero at time of mega-fire (wildfire acres) flame zone exposure Temporal-spatial Wildfire perimeter shapefiles and acres burned data were obtained from the GeoMAC system. These data were matched to maternal county of residence geodata to ascertain exposure. Comparison: exposed vs. nonexposed |
Risk of LBW following mega-fire exposure compared to nonexposed
Risk of preterm birth following mega-fire exposure compared to nonexposed
|
|
Park, B.Y., Boles, I., Monavvari, S., Patel, S., Alvarez, A., Phan, M., Perez., & Yao, R. 2021 The association between wildfire exposure in pregnancy and fetal gastroschisis: A population-based cohort study. |
California, USA Wildfire exposure 2007–2010 |
Retrospective cohort study of 2,093,185 births 2007–2010 |
Administrative data: The Office of Statewide Health Planning Birth File (OSHPD), California Geospatial fire imaging from The California Department of Forestry and Fire Protection (CAL FIRE) |
Exposure window: preconception (30 d prior to pregnancy) or in utero at time of wildfire exposure Geospatial Wildfire exposure was defined as the mother’s primary residence zip code within 15 miles of the edge of a wildfire Comparison: exposed vs non-exposed |
Risk of gastroschisis increased following the following exposure to wildfire compared to no exposure:
|
|
Requia, W.J., Kill. E., Papatheodorou, S., Koutrakis, P., & Schwartz, J.D. 2021 Prenatal exposure to wildfire-related air pollution and birth defects in Brazil. |
Brazil Wildfire smoke exposure 2001–2018 |
Retrospective cohort study of 16,825,497 births between 2001 and 2018 |
Administrative data: birth certificate data from Ministry of Health–Brazil Satellite imagery: National Institute of Spatial Research–Brazil/Instituto Nacional de Pesquisas Espaciais (INPE) Ambient air pollution including daily levels and weather data: Environmental Information System for Health/Instituto Nacional de Pesquisas Espaciais (INPE) Precipitation data derived from the Climate Prediction Center and National Oceanic and Atmospheric Administration (NOAA) |
Exposure window: in utero at time of wildfire smoke exposure Temporal-spatial Spatial resolution of birth data was based on the mother’s home municipality. 5,572 municipalities were grouped into five regions Birth defects were categorized using International Statistical Classification of Diseases and Related Health Problems (ICD) codes Comparison: dose–response—sum of wildfire records |
Cleft lip/palate: increased incidence following exposure
Congenital anomalies of the respiratory system increased following exposure
Congenital anomalies of the nervous system increased following exposure
|
|
McCoy, S.J., & Zhao, X. 2020 Wildfire and infant health: a geospatial approach to estimating the health impacts of wildfire smoke exposure |
Colorado, USA Wildfire smoke exposure 2007–2013 |
Retrospective cohort study of 90,779 births between 2007 and 2013 |
Administrative data: neonatal collection, Colorado Vital Records Registry, Colorado Department of Public Health and Environment (CDPHE) Dates of smoke exposure: Geospatial Multi-Agency Coordination Group (GeoMAC) and Monitoring Trends in Burn Severity (MTBS) Satellite imagery: University of Wisconsin-Madison Space Science and Engineering Center |
Exposure window: in utero at time of wildfire smoke exposure Temporal-spatial Reconstruction of wildfire smoke plumes using daily satellite images over the first 4 d following fire ignition within Colorado State were linked to the latitude and longitude of maternal residential address to determine exposure. Comparison: exposed vs. non-exposed |
Birth weight following exposure
LBW following exposure
|
|
Abdo, M., Ward, I., O’Dell, K., Ford, B., Pierce, J.R., Fischer, E.V., & Crooks, J.L. 2019 Impact of Wildfire Smoke on Adverse Pregnancy Outcomes in Colorado, 2007–2015 |
Colorado, USA Wildfire smoke exposure 2007–2015 |
Retrospective cohort study of 535,895 births between 2007–2015 |
Administrative data: neonatal collection, Colorado Vital Records Registry, Colorado Department of Public Health and Environment (CDPHE) Satellite imagery: National Oceanic and Atmospheric Administration (NOAA) satellite-based Hazard Mapping System Air quality monitoring: U.S. EPA Air Quality System (AQS) |
Exposure window: in utero at time of wildfire smoke exposure Temporal-spatial Wildfire smoke and non-smoke characterized by combining both satellite imagery and ground-based monitors. Daily concentrations were matched to maternal ZIP code using the mean of the concentrations in a grid to estimate exposure Comparison: concentration of by ZIP code |
Birth weight: reduction following exposure
Preterm birth: increased incidence following exposure
Gestational Diabetes Melitis: increased incidence following exposure
Gestational Hypertension: increased incidence following exposure
NICU admission: reduced incidence following exposure
Assisted ventilation: reduced incidence following exposure
|
|
O’Donnell, M.H., & Behie, A.M. 2015 Effects of wildfire disaster exposure on male birth weight in an Australian population |
Canberra, ACT, Australia “Canberra bushfire” 18 January 2003 (10-day event) |
Retrospective cohort study of 48,408 births between 2000 and 2010 |
Administrative data: neonatal collection, ACT Government Health Directorate Epidemiology Section (Population Health Informatics) Fire-affected Statistical Local Area geodata |
Exposure window: in utero at time of Canberra Bushfire (births occurred between February and October 2009) in fire-affected statistical local government areas) Geospatial Comparison: Fire exposure was divided into Statistical Local Areas (SLA) described as “severely affected,” areas where deaths and property damage occurred; “moderately affected,” where property damage occurred; and “least affected,” where no damage occurred and linked to maternal residential address at the time of the fires. |
Male birth weight
|
|
O’Donnell, M.H., & Behie, A.M. 2013 Effects of bushfire stress on birth outcomes: A cohort study of the 2009 Victorian Black Saturday bushfires |
Victoria, Australia “Black Saturday bushfire” 7 February 2009 (31-day event) |
Retrospective cohort study of 73,831 births between 2006 and 2009 Births over 20 wk gestation in Victoria |
Administrative neonatal collection: Victorian Consultative Council on Obstetric and Paediatric Mortality and Morbidity–Victorian State Department of Health Fire-affected Local Government Area geodata |
Exposure window: in utero at time of Black Saturday fires (births occurred between February and October 2009 in fire-affected local government areas). Geospatial Comparison: Fire exposure was divided into “fire-affected” and “not affected” local government areas (LGA) and linked to maternal residential address at the time of the fires. |
When compared to births in nonexposed areas: LBW in the 2 months following exposure
Gestational Age: thirsd trimester exposure
Gestational Age: second trimester exposure
Gestational Age: first trimester exposure
|
|
Holstius, D.M., Reid, C.E., Jesdale, B.M., & Morello-Frosch, R. 2012 Birth weight following pregnancy during the 2003 Southern California wildfires |
South Coast Air Basin, California, USA Southern California wildfire October 2003 (20-day event) |
Retrospective cohort study of 886,034 births between 1 January 2001 and 31 December 2005 |
Administrative neonatal collection: Birth Statistical Master File (Center for Health Statistics, Department of Health Services, California) Satellite imagery: Moderate Resolution Imaging Spectroradiometer (NASA) Dates of smoke exposure: Department of Forestry and Fire Protection, California |
Exposure window: in utero at time of fires: 21 October 2003–10 November 2003 Temporal-spatial The window of potential exposure was identified using government reporting and satellite imagery. Primary analysis used temporal contrast as the basis for exposure assessment, however sensitivity analysis included spatial contrast based on the proximity of maternal residence to monitors. This exposure was further classified as low exposure (average measures of during fires) and high exposure Comparison: exposed pregnancies compared to nonexposed pregnancies in years before/after the fires |
Mean birth weight at term: reduction following exposure compared to nonexposed pregnancies from earlier/later years
|
|
O’Donnell, M.H. 2017 Effects of bushfire exposure on prenatal and early life development in humans: A life history perspective |
Canberra, ACT “Canberra bushfire” 18 January 2003 (10-day event) Victoria, Australia “Black Saturday bushfires” 7 February 2009 (31-day event) |
Mixed methods Retrospective cohort study of 122,239 births between 2000 and 2012 Survey Semistructured interviews |
Administrative neonatal collection:
Fire-affected Statistical and Local Government Area geodata Self-selected survey and interview participants recruited via social media and internet forums, government websites and health care providers Survey (30 questions), respondents Semi-structured interview, 7 participants |
Exposure window: in utero at time of fires Geospatial For the Canberra bushfires: Fire exposure was divided into Statistical Local Areas (SLA) described as “severely affected,” areas where deaths and property damage occurred; “moderately affected,” where property damage occurred, and; “least affected,” where no damage occurred and linked to maternal residential address at the time of the fires For the Black Saturday bushfires: Fire exposure was divided into “fire-affected” and “not affected” local government areas (LGA) and linked to maternal residential address at the time of the fires. |
Secondary sex ratio: decrease in male births
Qualitative themes explored:
|
|
Brémault-Phillips, S., Pike, A., Olson, J., Severson, E., & Olson D. 2020 Expressive writing for wildfire-affected pregnant women: Themes of challenge and resilience |
Fort McMurray, Alberta, Canada Fort McMurray Wood Buffalo wildfire May 2016 (32-day event) |
Qualitative analysis of expressing writing journals |
54 self-selected participants recruited via social and mainstream media completed:
|
Resident of Fort McMurray Wood Buffalo in May 2016, evacuated from Fort McMurray because of the wildfire, and pregnant at the time of the wildfire or became pregnant within 6 months of the wildfire |
Qualitative themes explored following exposure and evacuation:
|
|
Verstraeten, B.S., Elgbeili, G., Hyle, A., King, S., & Olson, D.M. 2020 Maternal Mental Health after a Wildfire: Effects of Social Support in the Fort McMurray Wood Buffalo Study |
Fort McMurray, Alberta, Canada Fort McMurray Wood Buffalo wildfire May 2016 (32-day event) |
Longitudinal study |
200 self-selected participants recruited via social media, online forums, the study website, and flyers distributed in community centers completed:
|
Resident of Fort McMurray Wood Buffalo in May 2016, evacuated from Fort McMurray because of the wildfire, and pregnant at the time of the wildfire or became pregnant within 6 months of the wildfire |
Severe PTSD-like symptoms correlated with:
Greater social support satisfaction associated with less severe PTSD-like symptoms when peritraumatic distress is below average (social support satisfaction is not protective where peritraumatic distress is high) |
|
DeYoung, S.E., Chase, J., Branco, M.P., & Park, B. 2018 The Effect of Mass Evacuation on Infant Feeding: The Case of the 2016 Fort McMurray Wildfire |
Fort McMurray, Alberta, Canada Fort McMurray Wood Buffalo wildfire May 2016 (32-day event) |
Mixed Methods Survey Qualitative analysis of free text |
164 participants recruited through purposive sampling recruited via social media and local mainstream newspapers completed a 30-question survey which consisted of both open-ended items and items with categorical responses. | Resident of Fort McMurray Wood Buffalo in May 2016, evacuated from Fort McMurray because of the wildfire and also feeding infants (birth–36 months) during the evacuation and aftermath of fire |
Infant feeding:
Qualitative themes:
|
Note: aRR, adjusted relative risk; CI, confidence interval; df, degrees of freedom; LBW, low birth weight; OR, odds ratio; PTSD, posttraumatic stress disorder; RR, relative risk.
Study Population, Exposure Measurement, and Data Sources
Fifteen studies included women who were pregnant or soon to become pregnant at the time of wildfire disaster or wildfire smoke hazard; the exception to this is the De Young et al. study,38 which used feeding an infant 0–36 months of age at the time of exposure to wildfire as inclusion criteria. Eight studies focused on local populations exposed to a single, specific wildfire event,23–25,28,34,37–39 whereas seven focused on longer term exposure to wildfire smoke across fire seasons over a span of years,27,30–32,35,36 and one focused on exposure to mega-fire flame zones (that is, fires over 100,000 acres in size).29
All quantitative studies, as well as the quantitative component of the O’Donnell23 mixed-methods study, used local administrative neonatal collections for birth statistics. Maternal residential address,23,24,32,34 ZIP code,27,30,33 county,28,29 or maternal municipality31,35,36 at time of birth were used as a proxy for nearness to fires or smoke. Each study used a different method to determine exposure to the wildfire disaster or wildfire smoke hazard, including a mix of land-based geographical borders,23–25,29,30 satellite-based imagery or models,27,28,31–36 land-based air quality monitors,27,31,33–36 and personal air quality monitors within specific coordinates.28 Detailed information is included in Table 3.
The two mixed methods, one qualitative, and one longitudinal study used purposive sampling,23,37–39 and women were recruited into studies using social media,23,37–39 mainstream media,38,39 online forums,23,37 websites,23,37 and local medical services or community centres23,37 to assist with recruitment. All qualitative studies collected maternal demographic data, and all measured exposure as direct exposure to and/or evacuation from a wildfire event. These studies included a demographic survey component, two included a thematic analysis of open-ended responses,37,38 whereas one included thematic analysis of women’s expressive writing journal entries,39 and one included semistructured interviews.23 Two studies incorporated standardized questionnaires.23,37
Study findings by theme.
Birth weight and gestational age at birth, including incidence of preterm birth, were the most studied outcomes of the quantitative studies, whereas mental health impacts and protective factors were the most studied outcomes in the mixed methods/qualitative studies (Table 4).
Table 4.
Summary of findings by theme.
| Study | Birth weight | Gestational age | Birth defect | Gestational diabetes mellitus | Secondary sex ratio | Gestational hypertension | NICU admission/assisted ventilation | Mental health impacts and protective factors | Social outcomes and domestic violence | Breastfeeding/infant feeding | Access to health care |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Heft-Neal et al.27 | — | D | — | — | — | — | — | — | — | — | — |
| Requia et al.35 | D | — | — | — | — | — | — | — | — | — | — |
| Requia et al.36 | — | D | — | — | — | — | — | — | — | — | — |
| Costello28 | — | D | — | — | — | — | — | — | — | — | — |
| Jones and McDermott29 | D | D | — | — | — | — | — | — | — | — | — |
| Park et al.30 | — | — | I | — | — | — | — | — | — | — | — |
| Requia et al.31 | — | — | I | — | — | — | — | — | — | — | — |
| McCoy and Zhao32 | D | — | — | — | — | — | — | — | — | — | — |
| Abdo et al.33 | D | D | — | I | — | I | D | — | — | — | — |
| O’Donnell and Behie25 | I | NE | — | NE | — | — | — | — | — | — | — |
| O’Donnell and Behie24 | D | D/I | — | — | NE | — | — | — | — | — | — |
| Holstius et al.34 | D | — | — | — | — | — | — | — | — | — | — |
| O’Donnell23 | I | NE | — | — | D | — | — | a | a | — | a |
| Brémault-Phillips et al.39 | — | — | — | — | — | — | — | a | a | — | a |
| Verstraeten et al.37 | — | — | — | — | — | — | — | a | — | — | a |
| DeYoung et al.38 | — | — | — | — | — | — | — | — | — | a | a |
Note: —, no data; D, decrease; I, increase; NE, no effect; NICU, neonatal intensive care unit.
Thematic qualitative finding.
Birth Outcomes Findings
Twelve quantitative studies and the quantitative component of the O’Donnell study23 reported on birth outcomes during and after exposure to wildfire smoke or a wildfire disaster.
Birth weight and gestational age at birth.
Eight studies sought to test various hypotheses that exposure to a wildfire disaster would affect birth weight.23–25,29,32–35 All studies considered the relationship between birth weight and gestational age and used various methods to control for this relationship within the analysis. Six studies reported lower birth weights following exposure to a wildfire disaster or wildfire smoke. Findings included higher rates of incidence of low birth weight (LBW) (), (an increase of 0.8% from a base of 7%), and lower birth weight (from a base of ) following exposure to mega-fires in comparison with nonexposure in the United States 2010–201729; 3.8% lower birth weight, and 0.034 increase in the probability of LBW () in comparison with an unexposed group following wildfire smoke exposure in Colorado, USA, between 2007–201332; an increase of 18.55% in risk associated with LBW () following an increase of 100 wildfire records in the south region in Brazil 2001–201835; a reduction in birth weight for each microgram per cubic meter increase in trimester average wildfire exposure in the first trimester of pregnancy in Colorado 2007–201533; 150% higher incidence of very LBW babies () in affected areas in the 2 months following exposure to the 2009 Black Saturday bushfires in Victoria, Australia, in comparison with those of not affected areas24; and, lower birth weight at term (, 37–41 wk gestation) for any trimester exposure to the 2003 California wildfires, with a difference at term for third trimester exposure and a difference at term for second trimester exposure when compared to unexposed pregnancies in years before and after the fires.34
Two studies reported higher birth weights following maternal exposure to the 2003 Canberra bushfire.23,25 After controlling for differences in birth weight by sex, male babies born in the severely affected area were on average heavier in comparison with male babies born in the moderately affected area following in utero exposure to the 2003 Canberra bushfire.23,25 These studies also reported an increased incidence of macrosomia, which birth weight greater than the 90th centile for gestational age, for male babies following in utero exposure to this bushfire, with the largest increase occurring for males born between .23,25
Where timing of exposure to wildfire and association with birth weight were considered, results varied. Both first trimester exposure33,35 and all trimester exposure32,34 were associated with lower birth weight. Proximity of exposure and severity of exposure to wildfire disaster was also associated with lower birth weight,24,25,29 whereas elevated exposure to wildfire-related was associated with lower birth weight, with a dose–response relationship observed.33
Eight studies reported on wildfire exposure and gestational age at birth.23–25,27–29,33,36 Findings varied between studies and fire events. Findings included increased odds of preterm birth after exposure to “wildfire-wave” related with differences between Brazil’s geographic regions and trimester of exposure [; 95% confidence interval (CI): 1.31, 1.51] following first trimester exposure in southeast region, (; 95% CI: 1.01, 1.07) following first trimester exposure in Midwest region (; 95% CI: 1.01, 1.09) following second trimester exposure in north region, and (; 95% CI: 1.04, 1.0) following second trimester exposure in south region36; increased risk of preterm birth following exposure to the 2018 Camp Fire, California (; 95% CI: 1.03, 1.17) when compared to births that occurred a year earlier, with a dose–response effect evident when comparing exposure between the highest and lowest tertiles.28
The incidence of preterm birth in areas affected by fire was higher by 50% for babies born at 20–27 wk gestation in the 3 months following the 2009 Black Saturday bushfires in Victoria, Australia, and both preterm and postterm birth rates were higher for second and third trimester exposure to the fires in comparison with births in areas that were not affected by fire.24 There was little or no difference in gestational age at birth for babies born to women who resided in severely affected areas in comparison with least-affected areas following the 2003 Canberra Bushfires,23,25 although each increase in concentration of wildfire-generated was associated with increased incidence of preterm birth for babies born to women exposed to wildfire smoke in Colorado during the period 2007–2015 at any time during pregnancy (; 95% CI: 1.016, 1.139; ), with increased effect for second trimester exposure (; 95% CI: 1.088, 1.178; ).33 Incidence of preterm birth was higher by 1.2%, from a base of 10% for women exposed to mega-fires in comparison with nonexposure in the United States during the period 2010–2017,29 and a higher risk of preterm birth with each additional day of wildfire smoke exposure in California during the period 2006–2012 at any time during pregnancy [; 95% CI: 0.41%, 0.59%], with a larger effect for second trimester (; 95% CI: 0.71%, 0.96%) and third trimester (; 95% CI: 0.49%, 0.87%) exposure.27
Birth defects.
Two studies examined the association between exposure to wildfire and birth defects.30,31 One study of wildfire exposure in California between 2007 and 2010 reported that first trimester exposure, in comparison with no exposure, was associated with higher rates of gastroschisis: 7.8 vs. 5.7 per 10,000 births (; 95% CI: 1.07, 1.54).30 This study also found that prepregnancy wildfire exposure (up to 30 d before pregnancy) compared to no prepregnancy exposure resulted in higher rates of gastroschisis: 12.5 vs. 5.7 per 10.000 births (; 95% CI: 1.42, 3.52).30
A study of wildfire-related air pollution exposure in Brazil 2001–2018 reported that an increase in exposure to wildfire (measured as an increase in number of wildfire records) increased odds of cleft lip/cleft palate and second trimester exposure (; 95% CI: 1.001, 1.013), congenital anomalies of the respiratory system following second trimester exposure (; 95% CI: 1.002, 1.023), and congenital anomalies of the nervous system following first trimester exposure (; 95% CI: 1.001, 1.003) in the South, North and Midwest regions in Brazil.31
Secondary sex ratio.
Changes to secondary sex ratio (proportion of male to female babies at birth) following wildfire exposure was considered in two studies.23,24 One study of the 2009 Black Saturday bushfires found no difference in the secondary sex ratio for babies in utero at the time of the fire in comparison with nonexposed births.24 However, a later analysis that included births that were conceived after the fires showed a statistically significant decrease in the secondary sex ratio, with a male birth rate of 46.6% in the severely affected regions in comparison with a male birth rate of 51.1% in the remainder of Victoria.23
Other findings: Neonatal intensive care unit (NICU) admission and assisted ventilation following birth.
One study reported each increase in concentration of wildfire-generated was associated with a negative association between NICU admission and wildfire smoke exposure (; 95% CI: 0.926, 0.989, ), and a negative association between assisted ventilation following birth following in utero wildfire smoke exposure (; 95% CI: 0.837, 0.915, ).33
Childbearing Women’s Health Care Needs Findings
Five studies reported on childbearing women’s health care needs during and after exposure to wildfire smoke or a wildfire disaster.23,33,37–39 The outcomes reported were gestational diabetes mellitus; gestational hypertension; mental health impacts, including fear, stress, trauma, posttraumatic stress disorder (PTSD), and protective effects of social support and resilience; social outcomes, including use of alcohol and smoking; violence against women; breastfeeding and infant feeding; and access to health care.
Health of childbearing women: gestational diabetes mellitus (GDM) and gestational hypertension.
One study of the Canberra bushfires found no difference in the incidence of GDM for women who resided in severely affected or least affected areas during the fires.25 In contrast, a study of wildfire smoke exposure in pregnancy in Colorado between 2007 and 2015 reported a significant positive association with each increase in concentration of wildfire-generated and GDM for women exposed in the first trimester (; 95% CI: 1.064, 1.230, ) and also across the entire pregnancy (; 95% CI: 1.034, 1.281, ).33
One study reported a dose–response association, with each increase in concentration of wildfire-generated increasing the odds of gestational hypertension across whole pregnancy (; 95% CI: , 1.339, ), as well as for first trimester (; 95% CI: 1.071, 1.231, ) and second trimester (; 95% CI , 1.211, ) exposure.33
Childbearing women’s experience of wildfires.
Three studies considered mental health impacts of exposure to wildfires on childbearing women.23,37,39 The women in each of these studies were pregnant or breastfeeding infants at the time of exposure to wildfire. These qualitative and longitudinal studies explored outcomes in thematic analysis, used formal screening tools, and looked at the possible protective effects of strong social support and personal resilience.
One study hypothesized that peritraumatic stress would predict PTSD-like symptoms in childbearing women exposed to the Fort McMurray wildfire and that social support and resilience would be protective factors. Peritraumatic distress and dissociative experiences were positively correlated with PTSD symptoms and with each other. Resilience had a protective effect on PTSD symptoms. Social support and satisfaction with social support were protective for women with less severe PTSD symptoms; however, for women who reported very high PTSD symptoms, social support satisfaction no longer provided a protective effect.37
The themes of trauma and fear were identified in two studies. Women identified exposure to wildfire as the most traumatic event in their lives, expressing trauma due to the fear of dying, or fear of their family dying or being injured in the fires, or fear of becoming trapped or separated from their family as they evacuated from the fires.23,39 Some women expressed despair due to loss of livestock and pets as well as damage to property and returning to damaged environments, and others reported that they often relived wildfire-associated trauma when others in their community retold their experiences of the fires.23
Some women expressed being particularly fearful of both the immediate and long-term effects of wildfire-related stress on their unborn babies, themselves, and other family members.39 Concerns about air quality and pre- and postnatal smoke exposure effects on themselves and their babies were conveyed by women.23
Women reported that being displaced or evacuated from the family home, leaving partners to defend against fires, or being separated from family members during evacuation was stressful.23,39 In Australia, mandatory bushfire evacuation is not enforced; instead, a policy of “stay and defend or leave early” exists, although around half of the women in the O’Donnell23 study chose to evacuate as the fires approached. In comparison, the whole population of Fort McMurray was under a mandatory evacuation order and left the city as the wildfire approached. Psychological stressors, including pressure to complete paperwork when dealing with government and insurance agencies following the fires and lack of support around alternate housing after the fires, persisted long after the fires were out.23,39
Practices and strategies that foster resilience were identified as major themes in two studies. Women reported that expressive writing was therapeutic because it offered an opportunity for self-reflection, revaluation, and clarity.39 Journal writing, sharing stories of the evacuation, connecting with faith, meditation, yoga, breathing, and physical exercise were identified as useful while coping with the evacuation and the aftermath of the fires.23,39 Formal counseling was identified by some women as effective to achieve positive recovery from trauma.23,39 Many women found that the fire experience resulted in personal, interpersonal, and community posttraumatic growth, with adaptability and acceptance of change accelerating the healing process.23,39
The theme of relationships and changes to relationships was a focus of the experiences of women who participated in three studies.23,38,39 Some women reported positive relationship changes following the evacuation from the fire; the reported changes included becoming more appreciative of relationships with family, friends, and new connections that were made with others in the community who had also experienced the fire.39
Conversely, for others, the fire and its aftermath had a negative effect on relationships, which in some cases lasted for years. Some respondents reported that the evacuation and financial, emotional, and mental stressors following the fires caused relationship strain on intimate partnerships23,38 and problems with extended family, particularly if they evacuated to households with family members who were unused to having small children around or who did not have an understanding of what the fire-affected community had gone through.38
Social outcomes and violence against women.
An examination of women’s tobacco use and alcohol consumption following wildfire exposure found that although several women started smoking following the fires, overall maternal cigarette smoking declined following the fires, and only a small number of women reported that they consumed more alcohol following the fires.23 Women reported increased stress if their partners exhibited alcohol-related problems following evacuation from wildfires.39
Although included studies did not report on specific incidences of violence against women following wildfire exposure, some women identified past domestic violence as being a source of historical trauma when recounting trauma incurred during exposure to wildfire.39 Some women recounted tension in intimate relationships and intimate relationship breakdown in the aftermath of fires.23,39
Breastfeeding/infant feeding.
One study reported that infant feeding was adversely affected during and after evacuation from the Fort McMurray wildfire.38 Breastfeeding women reported that there was no access to lactation support and a lack of safe and private places in which to feed their baby or use a breast pump, and some reported pressure from family members to wean their baby or introduce solids. Many reported that breastfeeding was a source of comfort and support and assisted to soothe their infants during the evacuation. However, during and after the evacuation breastfeeding rates declined, and substitute feeding increased; many women perceived their breastmilk supply was adversely affected by exposure to the wildfires and the uncertainty of evacuation. Some breastfeeding women reported being provided with artificial formula even though they did not need it.38
Access to health care.
Women’s access to health care during evacuation and exposure to wildfire events was examined in four studies.23,37–39 Participants in these studies lived in well-resourced settings, and there were no reports of women being unable to access health care services, although some women reported that they were unable to access their usual health care providers following evacuation from the fire.38
Women were satisfied with health care support they received after the fire, especially support from doctors, midwives, and maternal and child health nurses and were able to access medications and prenatal vitamins.23 Some women reported an increase in antenatal care appointments following the fire—mostly attributable to managing stress from the fires.23 Some women reported that although counseling was available after the fires, it was generally not considered adequate and was provided in a community setting that was not private.23
Limitations of Included Studies
Assessment of the quality of the primary studies included in this review was undertaken using the CCAT, and scores are included in Table 2. This assessment included an evaluation of identification of bias, judgment of methodological quality, and consideration of the value and suitability of the information presented in each study to answer the research question. A degree of subjectivity was introduced to the process, limiting the replicability of appraisal and scoring. Further, critical appraisal tools have been criticized for lacking a strong evidence base.40 Scoring systems can imply that each domain is of equal weight, and total scores for two different studies can suggest that they are of equal quality, where this may not be the case.
A lack of precision for maternal exposure to wildfire smoke was identified within each of the quantitative studies. Generally, limitations were two-fold: Maternal exposure was estimated based on maternal residential address, ZIP code, county, or municipality at time of birth; and PM exposure levels were estimated from satellite data rather than assessment at an individual level. Exposure measurement was not uniform, and none of the studies relied on personal air quality monitoring, although Costello28 incorporated data from personal pollution sensors data within specific coordinates. Using address to define exposure did not account for actual time spent in the exposure location or actual levels of smoke exposure, particularly for women who relocated or evacuated during fires or smoky periods. A lack of precision for spatial data may result in exposure misclassification bias in studies that rely on satellite imaging of smoke plumes because smoke on satellites may not necessarily correlate with smoke exposure at ground level, and satellite imaging may not be reliable on cloudy days.
Most quantitative studies in this review relied on forms of categorical data to describe birth outcomes, and that may have impacted the accuracy of analyses, which may make it more difficult to compare results across studies. Two studies relied on birth weight analysis based on categorical increments24,25 rather than considering birth weight as a continuous variable. Four studies only included month and year of birth, which may have affected the accuracy of attributing gestation and trimester of exposure to conclusions around timing of exposure.,23–25,33
Variance in study results may be attributed to methodological heterogeneity. There were challenges in comparing results across studies due to differences in inclusion and exclusion criteria. For example, four studies included births between 37 and 42 wk gestation,31,34–36 one study included births between 30 and 42 wk gestation,33 one study included births up to 42 wk gestation,32 one study included births between 23 and 41 wk gestation,27 whereas the other studies included registered births over 20 wk gestation.23–25,28,30
Similarly, there were differences in the way included studies attributed gestational age at the limits of study periods. It is therefore possible that fixed cohort bias exists in some studies. Other biases may be present in included studies, for example due to conditioning on intermediates around gestational age, or an underestimation of adverse outcomes as a result of wildfire exposure because included studies do not consider the extent to which wildfire exposure may have led to spontaneous abortion or stillbirth.
Limitations for qualitative studies included the passage of time and recall bias with study surveys and interviews occurring between 6 and 23 months after fire exposure. Small sample sizes in the qualitative studies may limit the generalizability of findings; however, in this review synthesis of findings was possible across all four studies. Similar themes emerged across studies indicating that content saturation occurred and identified themes that are universal to childbearing women’s experience of wildfire exposure across well-resourced settings.
Discussion
Deviations from expected birth weight for gestational age, including both lighter and heavier babies as well as increases in preterm and postterm birth, are associated with increased infant mortality and morbidity.41 Shifts in population-based distribution of birth weight or increased incidence of preterm birth can have broader public health implications, including child development challenges and health issues in adolescence and beyond.42
This review found that exposure to wildfire disaster may result in differences in birth weight and length of gestation, with the weight of evidence toward lower birth weight (controlled for gestational age) and birth at earlier gestational age associated with exposure. Causal factors are complex but are likely to include an intersection of maternal exposure to with a dose–response effect present in several studies and prenatal maternal stress responses to disaster at both a personal and population level.
Maternal exposure to is associated with lower birth weight12,13 and an increase in incidence of cleft palate.15 Wildfire smoke is a major contributor to air particulate pollution, a complex source of , and it is a risk to human health.10 The contribution of wildfire-generated to atmospheric concentrations has risen since 2000 in North America, and concentrations are expected to continue to increase in fire-prone areas.43 Concentrations of exceed ambient concentrations during active wildfire events.11,43 Wildfire-generated is made up of a heterogeneous mix of chemicals, depending on the type of biomass burned and burning conditions, and this can remain in the atmosphere for long periods during fire seasons and can be transported over long distances.10 One recent study reported that wildfire-generated may be more toxic and cause more harm than equal doses of ambient .11
A life history theory hypothesis suggests exposure to wildfire disasters is associated with increased prenatal maternal stress, which in turn may trigger reproductive trade-offs such as reduced maternal investment in a current pregnancy leading to lower birth weight and/or reduced gestation.23 Prenatal maternal stress may also lead to poor fetal health outcomes, including abnormal fetal neurodevelopment44 and offspring behavior45; impaired physiology46,47; childhood sleep disorder48; and immune dysfunction.49 These can be mediated via multiple mechanisms, including epigenetic modifications (for example, DNA methylation changes),50,51 and altered maternal52 and atypical offspring microbiome.53,54
Exposure to wildfires may have an effect on the prevalence of postdate pregnancies, with fewer inductions of labor occurring, potentially due to fire acuity disrupting obstetric care or women making different decisions about timing of birth due to wildfire exposure.24 However, prolonged gestation following extreme maternal stress may be an adaptive strategy, whereby birth is delayed until women perceive conditions have improved, with the risk of postterm birth outweighing the risk of birth in a stochastic environment.55
Exposure to wildfires may be associated with an increased prevalence of GDM among exposed women, with maternal stress, maternal diet and exercise, and exposure to fine PM contributors to increased risk. Women who report high stress levels in the first and second trimesters of pregnancy are more than twice as likely to develop GDM than women who do not perceive themselves stressed.56 Stress may have a negative effect on food choice,57 so it is feasible that maternal dietary choices during and after exposure to wildfires may have an impact on the fetus and/or maternal glucose levels.
Women exposed to wildfires reported that although there was not widespread interruption to food supply during the fires, they were concerned about their own nutrition and dietary choices while evacuated.23,38,39 Furthermore, hot, smoky weather and public health advice to remain indoors may have reduced women’s usual exercise regimes.23,25 Exposure to elevated levels of ambient during preconception and first and second trimesters of pregnancy has been associated with increased rates of GDM among exposed women in the United States.16–18 Exposure to other fire and smoke disasters in Australia has also demonstrated an association between smoke exposure and GDM.58
The effect of wildfire exposure may extend beyond women directly affected by fire events. Although the numbers of women directly exposed to acute wildfire disaster may be small, many more women can be exposed at a distance, whether via emergency sirens, via evacuation from wildfire-prone areas as a precautionary measure, through exposure to wildfire smoke, and through social media and media broadcasts.
This secondary exposure to wildfire disaster may have longer term consequences for some less exposed women. Population-wide impacts on birth outcomes, including a reduction in infants’ birth weights and gestational ages at birth among women who were not directly affected by the disaster, were reported following the 11 September 2001 terrorist attacks,59,60 and it is possible that such indirect impact may also be present for childbearing women who are exposed to wildfires in a nonacute setting.
Similarly, birth weight and gestational age at birth are negatively affected following maternal exposure to terrorist attacks61–64 and natural disasters, for example following Cyclone Yasi in 2011,65 Hurricane Katrina in 2005,66 and the Quebec Ice Storm in 1998.67,68 Natural disasters such as earthquakes have also affected birth weight and length of gestation, with some studies reporting sex-specific differences in results.7,9,69
Timing of exposure to acute wildfire events may influence the secondary sex ratio. Sex-specific response to in utero stressors is well studied, albeit an area of debate. The female fetus may have a greater capacity to respond to prenatal maternal stress, possibly due to double X genome adaptability.9 Similarly, male genetic frailty may mean that male fetuses are less resilient, or conception of male fetuses is reduced during periods of maternal or population-based stress.70 Changes to the secondary sex ratio have previously been demonstrated following population-wide stress events including earthquakes7,8,71–73 and terrorist attacks.70
Women who are exposed to a traumatic event like a wildfire disaster are at risk of mental health morbidity and may develop PTSD-like symptoms and insomnia immediately after the event, with some developing major depression and/or PTSD.74,75 The stress response following exposure to disaster is highly individualized; past traumatic experience as well as degree of traumatic exposure (for example, fearing for one’s life, witnessing death, losing a family member, being evacuated, or losing property) is a key factor in predicting development of posttraumatic morbidity, including development of PTSD or PTSD-like symptoms.76
Exposure to wildfire smoke has a negative effect on psychological well-being.77 Exposure to multiple disasters over time has a cumulative effect on mental health morbidity, with increased depression and anxiety symptoms reported in Australian adults exposed to COVID-19 restrictions who had previously been exposed to smoke from the Black Summer bushfires in comparison with those exposed only to COVID-19 restrictions.78 Following Hurricane Katrina, severity of exposure, proximity to disaster, and repeated exposure to disasters impacted childbearing women’s mental health experience.66,79
Across the broader population, exposure to the Australian Black Saturday and Ash Wednesday bushfire disasters had medium-term to lifelong impacts for affected populations. Although mental health morbidity decreased over time, rates of PTSD, depression, severe distress, and heavy alcohol use remained higher in exposed populations and persisted for many years after exposure.80,81
This review identified social connectedness, satisfaction with social support, resilience, and being able to frame disaster exposure in a way that promotes posttraumatic growth as protective for childbearing women’s mental health and well-being. Demonstrating resilience and seeking out social support as an active coping strategy was associated with less mental health morbidity following trauma than social withdrawal or avoidant coping strategies.82 Higher self-reported peritraumatic distress following disaster exposure was correlated to higher levels of anxiety and depression over time, whereas a neutral or positive cognitive appraisal of disaster was protective for anxiety and depression.83
This review found that women sought out and had access to health care support following wildfire disasters. Collaborative health care support in partnership with a known midwife had a protective effect for women’s mental health and a positive effect on perception of subjective stress and depression.84 Having access to a known midwife through midwifery-led continuity of care may be protective for childbearing women exposed to wildfire disaster and among other profound benefits for childbearing women and their babies was protective for preterm birth.85
Strengths and Limitations
Strengths of this review include: a comprehensive search strategy, screening, and independent quality assessment of included studies by two researchers. New searches were undertaken regularly to identify contemporary studies. Although the search strategy was intentionally broad—and included search terms to identify wildfire-related studies concerned with pregnancy, birth, and maternal outcomes during the antenatal, intrapartum, and postnatal periods—it is possible that this strategy did not identify all studies within the intended scope of this review.
Findings were informed by a small number of studies with diverse methodologies, differences in exposure definitions, and varying inclusion and exclusion criteria. Thus, review results should be interpreted with some caution. This review was limited to studies published in English, so it is possible this study does not capture research from all regions afflicted by wildfires. Most studies in this review were set in well-resourced, high-income countries where women did not experience disruption to health care services. Consequently, the experience of women included in this review may not reflect the experience of women exposed to wildfire disasters in other settings.
Conclusion
The effect of wildfire disaster on women and their babies can be profound, with changes to expected birth weight and length of gestation, and it includes findings suggestive of increased rates of gestational hypertension, GDM, fetal macrosomia and increased incidence of some birth defects. Timing of exposure, severity, and proximity to the wildfires can influence morbidity. Following wildfire exposure, women’s health may be affected by higher rates of mental health acuity, including development of PTSD-like symptoms in the short term.
To better support childbearing women exposed to wildfire disasters, public health interventions that promote social connectedness, foster personal resilience, and include prompt referral to supportive health care, including midwifery-led continuity of care and mental health programs, should be developed in areas prone to wildfire disasters and implemented following wildfire disaster exposure.
This study highlighted several gaps in existing literature. There is a need for more systematic and detailed identification of the impacts of wildfires on a greater range of birth and maternal outcomes over the short- and long-term impact because this evidence base is needed to improve outcomes for childbearing women and their babies. There is also a need for longitudinal studies to define windows of susceptibility to wildfire smoke and wildfire-generated concentrations on birth outcomes, health, and the health care needs of childbearing women with more precision.
Additionally, it is important that access to maternity and child health services, reproductive and family planning services, and mental health support following wildfire disaster be evaluated. This evidence will inform the development of effective clinical and public health strategies to further support the needs of childbearing women following exposure to a wildfire disaster.
Acknowledgments
The authors acknowledge the Mother and Child 2020 collaborative research project under whose auspices this research was conducted (https://medicalschool.anu.edu.au/research/projects/mother-child-2020-mc2020).
J.E.: conceptualization, methodology, formal analysis, writing (original draft). A.B.: conceptualization; draft review and editing. D.A.J.M.S.: conceptualization; draft review and editing. N.C.: conceptualization; draft review and editing. M.J.P.: conceptualization; draft review and editing. D.L.D.: conceptualization, supervision, and validation; draft review and editing. All authors approved the final version for submission.
References
- 1.Pausas JG, Keeley JE. 2019. Wildfires as an ecosystem service. Front Ecol Environ 17(5):289–295, 10.1002/fee.2044. [DOI] [Google Scholar]
- 2.Williams AP, Abatzoglou JT, Gershunov A, Guzman‐Morales J, Bishop DA, Balch JK, et al. 2019. Observed impacts of anthropogenic climate change on wildfire in California. Earth’s Future 7(8):892–910, 10.1029/2019EF001210. [DOI] [Google Scholar]
- 3.United Nations. Climate Change. https://www.un.org/en/global-issues/climate-change [accessed 17 June 2022].
- 4.World Health Organization. Climate Change and Health. https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health [accessed 17 June 2022].
- 5.Commonwealth of Australia. 2020. The Royal Commission into National Natural Disaster Arrangements Report. Barton, ACT: Commonwealth of Australia. [Google Scholar]
- 6.Harville E, Xiong X, Buekens P. 2010. Disasters and perinatal health: a systematic review. Obstet Gynecol Surv 65(11):713–728, PMID: , 10.1097/OGX.0b013e31820eddbe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suzuki K, Yamagata Z, Kawado M, Hashimoto S. 2016. Effects of the Great East Japan Earthquake on secondary sex ratio and perinatal outcomes. J Epidemiol 26(2):76–83, PMID: , 10.2188/jea.JE20150055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Catalano R, Yorifuji T, Kawachi I. 2013. Natural selection in utero: evidence from the Great East Japan Earthquake. Am J Hum Biol 25(4):555–559, PMID: , 10.1002/ajhb.22414. [DOI] [PubMed] [Google Scholar]
- 9.Torche F, Kleinhaus K. 2012. Prenatal stress, gestational age and secondary sex ratio: the sex-specific effects of exposure to a natural disaster in early pregnancy. Hum Reprod 27(2):558–567, PMID: , 10.1093/humrep/der390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Black C, Tesfaigzi Y, Bassein JA, Miller LA. 2017. Wildfire smoke exposure and human health: significant gaps in research for a growing public health issue. Environ Toxicol Pharmacol 55:186–195, PMID: , 10.1016/j.etap.2017.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aguilera R, Corringham T, Gershunov A, Benmarhnia T. 2021. Wildfire smoke impacts respiratory health more than fine particles from other sources: observational evidence from Southern California. Nat Commun 12(1):1493, PMID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun X, Luo X, Zhao C, Zhang B, Tao J, Yang Z, et al. 2016. The associations between birth weight and exposure to fine particulate matter (PM2.5) and its chemical constituents during pregnancy: a meta-analysis. Environ Pollut 211:38–47, PMID: , 10.1016/j.envpol.2015.12.022. [DOI] [PubMed] [Google Scholar]
- 13.Lamichhane DK, Leem JH, Lee JY, Kim HC. 2015. A meta-analysis of exposure to particulate matter and adverse birth outcomes. Environ Health Toxicol 30:e2015011, PMID: , 10.5620/eht.e2015011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu C, Sun J, Liu Y, Liang H, Wang M, Wang C, et al. 2017. Different exposure levels of fine particulate matter and preterm birth: a meta-analysis based on cohort studies. Environ Sci Pollut Res Int 24(22):17976–17984, PMID: , 10.1007/s11356-017-9363-0. [DOI] [PubMed] [Google Scholar]
- 15.Zhou Y, Gilboa SM, Herdt ML, Lupo PJ, Flanders WD, Liu Y, et al. 2017. Maternal exposure to ozone and PM2.5 and the prevalence of orofacial clefts in four U.S. states. Environ Res 153:35–40, PMID: , 10.1016/j.envres.2016.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zheng Y, Wen X, Bian J, Lipkind H, Hu H. 2021. Associations between the chemical composition of PM2.5 and gestational diabetes mellitus. Environ Res 198:110470, PMID: , 10.1016/j.envres.2020.110470. [DOI] [PubMed] [Google Scholar]
- 17.Rammah A, Whitworth KW, Symanski E. 2020. Particle air pollution and gestational diabetes mellitus in Houston, Texas. Environ Res 190:109988, PMID: , 10.1016/j.envres.2020.109988. [DOI] [PubMed] [Google Scholar]
- 18.Choe S-A, Eliot MN, Savitz DA, Wellenius GA. 2019. Ambient air pollution during pregnancy and risk of gestational diabetes in New York City. Environ Res 175:414–420, PMID: , 10.1016/j.envres.2019.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whittemore R, Knafl K. 2005. The integrative review: updated methodology. J Adv Nurs 52(5):546–553, PMID: , 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- 20.Crowe M. 2022. Crowe Critical Appraisal Tool (CCAT) Version 1.4. https://conchra.com.au/2015/12/08/crowe-critical-appraisal-tool-v1-4/ [accessed 16 June 2022].
- 21.Crowe M, Sheppard L, Campbell A. 2012. Reliability analysis for a proposed critical appraisal tool demonstrated value for diverse research designs. J Clin Epidemiol 65(4):375–383, PMID: , 10.1016/j.jclinepi.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 22.Crowe M. 2022. Crowe Critical Appraisal Tool (CCAT) User Guide. https://conchra.com.au/wp-content/uploads/2015/12/CCAT-user-guide-v1.4.pdf [accessed 13 June 2022].
- 23.O’Donnell MH. 2017. Effects of Bushfire Exposure on Prenatal and Early Life Development in Humans: A Life History Perspective. Canberra, Australia: Australian National University. [Google Scholar]
- 24.O’Donnell MH, Behie AM. 2013. Effects of bushfire stress on birth outcomes: a cohort study of the 2009 Victorian Black Saturday bushfires. Int J Disaster Risk Reduct 5:98–106, 10.1016/j.ijdrr.2013.08.002. [DOI] [Google Scholar]
- 25.O’Donnell MH, Behie AM. 2015. Effects of wildfire disaster exposure on male birth weight in an Australian population. Evol Med Public Health 2015(1):344–354, PMID: , 10.1093/emph/eov027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097, PMID: , 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heft-Neal S, Driscoll A, Yang W, Shaw G, Burke M. 2022. Associations between wildfire smoke exposure during pregnancy and risk of preterm birth in California. Environ Res 203:111872, PMID: , 10.1016/j.envres.2021.111872. [DOI] [PubMed] [Google Scholar]
- 28.Costello J. 2022. Air Quality and Preterm Birth: Distance to Highways, Exposure to Wildfires, and Effect Modification by COVID-19. San Francisco, CA: University of California, San Francisco. [Google Scholar]
- 29.Jones BA, McDermott S. 2022. Infant health outcomes in mega-fire affected communities. Appl Econ Lett 29(14):1325–1335, 10.1080/13504851.2021.1927959. [DOI] [Google Scholar]
- 30.Park BY, Boles I, Monavvari S, Patel S, Alvarez A, Phan M, et al. 2022. The association between wildfire exposure in pregnancy and foetal gastroschisis: a population-based cohort study. Paediatr Perinat Epidemiol 36(1):45–53, PMID: , 10.1111/ppe.12823. [DOI] [PubMed] [Google Scholar]
- 31.Requia WJ, Kill E, Papatheodorou S, Koutrakis P, Schwartz JD. 2021. Prenatal exposure to wildfire-related air pollution and birth defects in Brazil. J Expo Sci Environ Epidemiol, PMID: , 10.1038/s41370-021-00380-y. [DOI] [PubMed] [Google Scholar]
- 32.McCoy SJ, Zhao X. 2021. Wildfire and infant health: a geospatial approach to estimating the health impacts of wildfire smoke exposure. Appl Econ Lett 28(1):32–37, 10.1080/13504851.2020.1730747. [DOI] [Google Scholar]
- 33.Abdo M, Ward I, O’Dell K, et al. 2019. Impact of wildfire smoke on adverse pregnancy outcomes in Colorado, 2007–2015. Int J Environ Res Public Health 16(19), PMID: , 10.3390/ijerph16193720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holstius DM, Reid CE, Jesdale BM, Morello-Frosch R. 2012. Birth weight following pregnancy during the 2003 Southern California wildfires. Environ Health Perspect 120(9):1340–1345, PMID: , 10.1289/ehp.1104515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Requia WJ, Amini H, Adams MD, Schwartz JD. 2022. Birth weight following pregnancy wildfire smoke exposure in more than 1.5 million newborns in Brazil: a nationwide case-control study. Lancet Reg Health Am 11:100229, 10.1016/j.lana.2022.100229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Requia WJ, Papatheodorou S, Koutrakis P, Mukherjee R, Roig HL. 2022. Increased preterm birth following maternal wildfire smoke exposure in Brazil. Int J Hyg Environ Health 240:113901, PMID: , 10.1016/j.ijheh.2021.113901. [DOI] [PubMed] [Google Scholar]
- 37.Verstraeten BSE, Elgbeili G, Hyde A, King S, Olson DM. 2020. Maternal mental health after a wildfire: effects of social support in the Fort McMurray Wood Buffalo study. Can J Psychiatry, PMID: , 10.1177/0706743720970859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.DeYoung SE, Chase J, Branco MP, Park B. 2018. The effect of mass evacuation on infant feeding: the case of the 2016 Fort McMurray wildfire. Matern Child Health J 22(12):1826–1833, PMID: , 10.1007/s10995-018-2585-z. [DOI] [PubMed] [Google Scholar]
- 39.Brémault-Phillips S, Pike A, Olson J, Severson E, Olson D. 2020. Expressive writing for wildfire-affected pregnant women: themes of challenge and resilience. Int J Disaster Risk Reduct 50:101730, 10.1016/j.ijdrr.2020.101730. [DOI] [Google Scholar]
- 40.Tod D, Booth A, Smith B. 2022. Critical appraisal. Int Rev Sport Exerc Psychol 15(1):52–72, 10.1080/1750984X.2021.1952471. [DOI] [Google Scholar]
- 41.Goldenberg RL, Culhane JF, Iams JD, Romero R. 2008. Epidemiology and causes of preterm birth. Lancet 371(9606):75–84, PMID: , 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Newnham JP, Kemp MW, White SW, Arrese CA, Hart RJ, Keelan JA. 2017. Applying precision public health to prevent preterm birth. Front Public Health 5:66, PMID: , 10.3389/fpubh.2017.00066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burke M, Driscoll A, Heft-Neal S, Xue J, Burney J, Wara M. 2021. The changing risk and burden of wildfire in the United States. Proc Natl Acad Sci USA 118(2):e2011048118, PMID: , 10.1073/pnas.2011048118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walsh K, McCormack CA, Webster R. 2019. Maternal prenatal stress phenotypes associate with fetal neurodevelopment and birth outcomes. Proc Natl Acad Sci USA 116(48):23996–24005, PMID: , 10.1073/pnas.1905890116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tuovinen S, Lahti-Pulkkinen M, Girchenko P, Heinonen K, Lahti J, Reynolds RM, et al. 2021. Maternal antenatal stress and mental and behavioral disorders in their children. J Affect Disord 278:57–65, PMID: , 10.1016/j.jad.2020.09.063. [DOI] [PubMed] [Google Scholar]
- 46.Eberle C, Fasig T, Brüseke F, Stichling S. 2021. Impact of maternal prenatal stress by glucocorticoids on metabolic and cardiovascular outcomes in their offspring: a systematic scoping review. PLoS One 16(1):e0245386, PMID: , 10.1371/journal.pone.0245386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schulz KM, Pearson JN, Neeley EW, Berger R, Leonard S, Adams CE, et al. 2011. Maternal stress during pregnancy causes sex-specific alterations in offspring memory performance, social interactions, indices of anxiety, and body mass. Physiol Behav 104(2):340–347, PMID: , 10.1016/j.physbeh.2011.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van den Heuvel MI, Hect JL, Smarr BL, Qawasmeh T, Kriegsfeld LJ, Barcelona J, et al. 2021. Maternal stress during pregnancy alters fetal cortico-cerebellar connectivity in utero and increases child sleep problems after birth. Sci Rep 11(1):2228, PMID: , 10.1038/s41598-021-81681-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Veru F, Laplante DP, Luheshi G, King S. 2014. Prenatal maternal stress exposure and immune function in the offspring. Stress 17(2):133–148, PMID: , 10.3109/10253890.2013.876404. [DOI] [PubMed] [Google Scholar]
- 50.Cao-Lei L, Laplante DP, King S. 2016. Prenatal maternal stress and epigenetics: review of the human research. Curr Mol Bio Rep 2(1):16–25, 10.1007/s40610-016-0030-x. [DOI] [Google Scholar]
- 51.Meaney MJ, Szyf M, Seckl JR. 2007. Epigenetic mechanisms of perinatal programming of hypothalamic-pituitary-adrenal function and health. Trends Mol Med 13(7):269–277, PMID: , 10.1016/j.molmed.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 52.Hechler C, Borewicz K, Beijers R, Saccenti E, Riksen-Walraven M, Smidt H, et al. 2019. Association between psychosocial stress and fecal microbiota in pregnant women. Sci Rep 9(1):4463, PMID: , 10.1038/s41598-019-40434-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jašarević E, Howard CD, Misic AM, Beiting DP, Bale TL. 2017. Stress during pregnancy alters temporal and spatial dynamics of the maternal and offspring microbiome in a sex-specific manner. Sci Rep 7(1):44182, PMID: , 10.1038/srep44182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zijlmans MAC, Korpela K, Riksen-Walraven JM, de Vos WM, de Weerth C. 2015. Maternal prenatal stress is associated with the infant intestinal microbiota. Psychoneuroendocrinology 53:233–245, PMID: , 10.1016/j.psyneuen.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 55.Margerison-Zilko CE, Goodman JM, Anderson E, Gemmill A, Catalano RA. 2015. Post-term birth as a response to environmental stress: the case of September 11, 2001. Evol Med Public Health 2015(1):13–20, PMID: , 10.1093/emph/eov001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Silveira ML, Whitcomb BW, Pekow P, Braun B, Markenson G, Dole N, et al. 2014. Perceived psychosocial stress and glucose intolerance among pregnant Hispanic women. Diabetes Metab 40(6):466–475, PMID: , 10.1016/j.diabet.2014.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lobel M, Cannella DL, Graham JE, DeVincent C, Schneider J, Meyer BA. 2008. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychol 27(5):604–615, PMID: , 10.1037/a0013242. [DOI] [PubMed] [Google Scholar]
- 58.Melody SM, Ford J, Wills K, Venn A, Johnston FH. 2019. Maternal exposure to fine particulate matter from a coal mine fire and birth outcomes in Victoria, Australia. Environ Int 127:233–242. PMC], PMID: , 10.1016/j.envint.2019.03.028. [DOI] [PubMed] [Google Scholar]
- 59.Smits L, Krabbendam L, de Bie R, Essed G, van Os J. 2006. Lower birth weight of Dutch neonates who were in utero at the time of the 9/11 attacks. J Psychosom Res 61(5):715–717, PMID: , 10.1016/j.jpsychores.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 60.Brown R. 2020. The intergenerational impact of terror: did the 9/11 tragedy impact the initial human capital of the next generation? Demography 57(4):1459–1481, PMID: , 10.1007/s13524-020-00876-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Eskenazi B, Marks AR, Catalano R, Bruckner T, Toniolo PG. 2007. Low birthweight in New York City and upstate New York following the events of September 11th. Hum Reprod 22(11):3013–3020, PMID: , 10.1093/humrep/dem301. [DOI] [PubMed] [Google Scholar]
- 62.Lederman SA, Rauh V, Weiss L, Stein JL, Hoepner LA, Becker M, et al. 2004. The effects of the World Trade Center event on birth outcomes among term deliveries at three lower Manhattan hospitals. Environ Health Perspect 112(17):1772–1778, PMID: , 10.1289/ehp.7348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Quintana-Domeque C, Ródenas-Serrano P. 2017. The hidden costs of terrorism: the effects on health at birth. J Health Econ 56:47–60, PMID: , 10.1016/j.jhealeco.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 64.Maric NP, Dunjic B, Stojiljkovic DJ, Britvic D, Jasovic-Gasic M. 2010. Prenatal stress during the 1999 bombing associated with lower birth weight—a study of 3,815 births from Belgrade. Arch Womens Ment Health 13(1):83–89, PMID: , 10.1007/s00737-009-0099-9. [DOI] [PubMed] [Google Scholar]
- 65.Parayiwa C, Behie AM. 2018. Effects of prenatal maternal stress on birth outcomes following tropical cyclone Yasi in Queensland, Australia (2011). Int J Disaster Risk Reduct 28:768–775, 10.1016/j.ijdrr.2018.02.005. [DOI] [Google Scholar]
- 66.Xiong X, Harville EW, Mattison DR, Elkind-Hirsch K, Pridjian G, Buekens P. 2010. Hurricane Katrina experience and the risk of post-traumatic stress disorder and depression among pregnant women. Am J Disaster Med 5(3):181–187, PMID: , 10.5055/ajdm.2010.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dancause KN, Laplante DP, Oremus C, Fraser S, Brunet A, King S. 2011. Disaster-related prenatal maternal stress influences birth outcomes: project ice storm. Early Hum Dev 87(12):813–820, PMID: , 10.1016/j.earlhumdev.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 68.Auger N, Kuehne E, Goneau M, Daniel M. 2011. Preterm birth during an extreme weather event in Québec, Canada: a “natural experiment”. Matern Child Health J 15(7):1088–1096, PMID: , 10.1007/s10995-010-0645-0. [DOI] [PubMed] [Google Scholar]
- 69.Lian Q, Ni J, Zhang J, Little J, Luo S, Zhang L. 2020. Maternal exposure to Wenchuan earthquake and prolonged risk of offspring birth outcomes: a natural experiment study. BMC Pregnancy Childbirth 20(1):552, PMID: , 10.1186/s12884-020-03206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bruckner TA, Catalano R, Ahern J. 2010. Male fetal loss in the U.S. following the terrorist attacks of September 11, 2001. BMC Public Health 10(1):273, PMID: , 10.1186/1471-2458-10-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fukuda M, Fukuda K, Shimizu T, Møller H. 1998. Decline in sex ratio at birth after Kobe earthquake. Hum Reprod 13(8):2321–2322, PMID: , 10.1093/humrep/13.8.2321. [DOI] [PubMed] [Google Scholar]
- 72.Saadat M. 2008. Decline in sex ratio at birth after bam (Kerman province, Southern Iran) earthquake. J Biosoc Sci 40(6):935–937, PMID: , 10.1017/S0021932008002745. [DOI] [PubMed] [Google Scholar]
- 73.Doğer E, Cakıroğlu Y, Köpük SY, Ceylan Y, Simşek HU, Calışkan E. 2013. Impact of earthquakes on sex ratio at birth: eastern Marmara earthquakes. J Turk Ger Gynecol Assoc 14(2):92–97, PMID: , 10.5152/jtgga.2013.69320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Belleville G, Ouellet M-C, Morin CM. 2019. Post-traumatic stress among evacuees from the 2016 Fort McMurray wildfires: exploration of psychological and sleep symptoms three months after the evacuation. Int J Environ Res Public Health 16(9):1604, PMID: , 10.3390/ijerph16091604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Grant N, Marshall PD, Terry L, Schell PD, Marc N, Elliott PD, et al. 2007. Psychiatric disorders among adults seeking emergency disaster assistance after a wildland-urban interface fire. Psychiatr Serv 58(4):509–514, PMID: , 10.1176/ps.2007.58.4.509. [DOI] [PubMed] [Google Scholar]
- 76.Youngner CG, Burton MS, Price M, Zimmerman L, Kearns MC, Houry D, et al. 2012. The contributions of prior trauma and peritraumatic dissociation to predicting post-traumatic stress disorder outcome in individuals assessed in the immediate aftermath of a trauma. West J Emerg Med 13(3):220–224, PMID: , 10.5811/westjem.2012.3.11777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dawel AS, Smithson M, Cherbuin N, Banfield M, Calear AL, Farrer LM, et al. 2020. The effect of COVID-19 on mental health and wellbeing in a representative sample of Australian adults. Front Psychiatry 11(579985), PMID: , 10.3389/fpsyt.2020.579985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Batterham PJ, Calear AL, McCallum SM, Morse AR, Banfield M, Farrer LM, et al. 2021. Trajectories of depression and anxiety symptoms during the COVID-19 pandemic in a representative Australian adult cohort. Med J Aust 214(10):462–468, PMID: , 10.5694/mja2.51043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Harville EW, Xiong X, Pridjian G, Elkind-Hirsch K, Buekens P. 2009. Postpartum mental health after Hurricane Katrina: a cohort study. BMC Pregnancy Childbirth 9(1):21, PMID: , 10.1186/1471-2393-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bryant RA, Gibbs L, Gallagher HC, Pattison P, Lusher D, MacDougall C, et al. 2018. Longitudinal study of changing psychological outcomes following the Victorian Black Saturday bushfires. Aust N Z J Psychiatry 52(6):542–551, PMID: , 10.1177/0004867417714337. [DOI] [PubMed] [Google Scholar]
- 81.Bryant RA, Waters E, Gibbs L, Gallagher HC, Pattison P, Lusher D, et al. 2014. Psychological outcomes following the Victorian Black Saturday bushfires. Aust N Z J Psychiatry 48(7):634–643, PMID: , 10.1177/0004867414534476. [DOI] [PubMed] [Google Scholar]
- 82.Thompson NJ, Fiorillo D, Rothbaum BO, Ressler KJ, Michopoulos V. 2018. Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. J Affect Disord 225:153–159, PMID: , 10.1016/j.jad.2017.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Paquin V, Elgbeili G, Laplante DP, Kildea S, King S. 2021. Positive cognitive appraisal “buffers” the long-term effect of peritraumatic distress on maternal anxiety: The Queensland Flood Study. J Affect Disord 278:5–12, PMID: , 10.1016/j.jad.2020.09.041. [DOI] [PubMed] [Google Scholar]
- 84.Kildea S, Simcock G, Liu A, Elgbeili G, Laplante DP, Kahler A, et al. 2018. Continuity of midwifery carer moderates the effects of prenatal maternal stress on postnatal maternal wellbeing: the Queensland flood study. Arch Womens Ment Health 21(2):203–214, PMID: , 10.1007/s00737-017-0781-2. [DOI] [PubMed] [Google Scholar]
- 85.Sandall J, Soltani H, Gates S, Shennan A, Devane D, Cochrane Pregnancy and Childbirth Group. 2016. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2016(4), 10.1002/14651858.CD004667.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]