Abstract
Background:
Although minimization of cervical spine motion by using a neck collar or manual in-line stabilization is recommended for urgent tracheal intubation (TI) in patients with known or suspected cervical spine injury (CSI), it may worsen glottic visualization. The overall performance of video-stylets during TI in patients with neck immobilization remains unclear. The current meta-analysis aimed at comparing the intubation outcomes of different video-stylets with those of conventional laryngoscopes in patients with cervical immobilization.
Method:
The databases of Embase, Medline, and the Cochrane Central Register of Controlled Trials were searched from inception to June 2021 to identify trials comparing intubation outcomes between video-stylets and conventional laryngoscopes. The primary outcome was first-pass success rate, while secondary outcomes included overall success rate, time to intubation, the risk of intubation-associated sore throat, or tissue damage.
Results:
Five randomized controlled trials published between 2007 and 2013 involving 487 participants, all in an operating room setting, were analyzed. The video-stylets investigated included Bonfils intubation fiberscope, Levitan FPS Scope, and Shikani optical stylet. There was no difference in first-pass success rate (risk ratio [RR] =1.08, 95% confidence interval [CI]: 0.89–1.31, P = .46], overall success rate (RR = 1.06, 95% CI: 0.93–1.22, P = .4), intubation time [mean difference = 4.53 seconds, 95% CI: –8.45 to 17.51, P = .49), and risk of tissue damage (RR = 0.46, 95% CI: 0.16–1.3, P = .14) between the 2 groups. The risk of sore throat was lower with video-stylets compared to that with laryngoscopes (RR = 0.45, 95% CI: 0.23–0.9, P = .02).
Conclusion:
Our results did not support the use of video-stylets as the first choice for patients with neck immobilization. Further studies are required to verify the efficacy of video-stylets in the nonoperating room setting.
Keywords: cervical spine injury, neck immobilization, trauma, video-stylets
1. Introduction
Despite the absence of apparent spinal deformity or evidence of acute spinal cord injury on imaging study, comatose patients with blunt trauma have been reported to have a 2.5% probability of cervical spine injury (CSI).[1] In clinical practice, minimization of cervical spine motion by the application of a neck collar or manual in-line stabilization (MILS) is recommended when tracheal intubation (TI) is urgently required in patients with known or suspected CSI.[2,3] However, 1 major concern during TI is the impairment of glottic visualization after cervical immobilization,[4,5]which may significantly prolong intubation time and increase the likelihood of failed intubation.[4] Such an impairment of laryngeal view, which occurs in 45% of patients after cervical immobilization,[4] may impede urgent airway establishment and lead to prolonged hypoxemia[6] as well as secondary neurologic injury in this patient population.[7] In addition, multiple TIs may increase the risk of cardiac arrest.[8] Another concern is that that physical trauma in adults may be complicated by other life-threatening conditions such as hemorrhagic shock and pulmonary aspiration.[9] These critical concerns highlighted the importance of implementing effective airway management strategies that allow rapid and successful TI.
Conventional direct laryngoscopy (DL) has been accepted as the standard for TI with a success rate being equal to or exceeding 99% in an elective or emergency setting.[10,11] With this technique, the laryngoscope is used to expose the laryngeal inlet under direct vision to facilitate insertion of a tracheal tube through the vocal cords. Despite the advantage of DL as a familiar technique for anesthesiologists and clinicians, a previous study demonstrated a doubling of applied pressure on the laryngoscope blade during TI because of suboptimal glottic visualization.[12] Such an elevation in pressure from the laryngoscope would potentially increase craniocervical motion and the risk of CSI.[12] Alternatively, other airway devices installed with video camera systems that allow indirect vocal cord visualization such as video-stylets[13,14] and video-laryngoscopes[15,16] have been developed for difficult airway management. Although there are several meta-analyses that reported a superior efficacy of video-laryngoscopy[17–19] in comparison to that of conventional DL for TI in patients with a difficult airway, the overall performance of rigid optical stylets for TI in patients with cervical immobilization remains unclear. Clarification of this issue may enable clinicians to develop effective airway rescue strategies to optimize critical care quality for this subgroup of patients.
The current meta-analysis aimed at comparing the intubation outcomes of different video-stylets with those of DL in patients with cervical immobilization. We hypothesize that TI with video-stylets may be associated with more favorable outcomes in patients with MILS compared to those undergoing DL. The primary outcome was the first-pass success rate, while the secondary outcomes included the overall success rate, the time to intubation, the risk of intubation-associated sore throat, and tissue damage.
2. Materials and Methods
2.1. Protocol and registration
The current study was reported following the recommendation of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and was registered with PROSPERO (CRD42021252611). The manuscript is a systematic review and meta-analysis of data based on published literature. Therefore, no ethical approval is required.
2.2. Search strategy
The databases of Embase, Medline, and the Cochrane Central Register of Controlled Trials (CENTRAL) were searched to identify randomized controlled trials (RCTs) comparing the intubation outcomes of video-stylets with those of DL using the keywords: (“cervical spine” adj4 [instability or stabilization or injury or immobilization or trauma] or “neck collar” or “collar” or “cervical spine stabilization maneuvers” or “manual inline stabilization” or “cervical adj4 spine”) AND (“Trachway” OR “video stylet” OR “Clarus Video System” OR “optiscope” OR “optical stylet” OR “Shikani Optical Stylet” OR “shikani” OR “bonfils” OR “Bonfils fiberscope” OR “StyletScope” OR “Levitan FPS” OR “InnoScope”) AND [“Macintosh laryngoscop*” or “Laryngoscop*” or “Miller” or “McCoy” or “conventional laryngoscopy” or “Direct Laryngoscopy”] AND “RCT” from inception to June 6, 2021. We also used subject headings (MeSH terms in Cochrane Library and PubMed as well as Emtree terms in Embase) to assist in searching. The Google scholar and reference lists of all the retrieved articles were manually searched to identify other studies not found during our electronic screening. No restriction on publication date was applied, but only trials published in English were included. The full search strategy for 1 of the databases (i.e., Medline) is provided in (Table 1, Supplemental Digital Content, http://links.lww.com/MD/H30).
2.3. Inclusion and exclusion criteria
Two investigators (I.W.C. and K.C.H.) independently performed title and abstract screening which was facilitated by using a web-based tool (https://rayyan.ai/). The full text of all trials was read if they fulfilled the eligibility criteria and provided data of at least 1 outcome of interest. A third investigator (C.K.S.) was consulted for conflicting judgments. The criteria for eligibility of studies included: (1) RCTs in which video-stylets or conventional laryngoscopes were used for TI, and (2) adult patients (age ≥18 years) subjected to cervical spine immobilization by using a neck collar or other techniques (e.g., MILS). The exclusion criteria were (1) Non-RCTs, (2) RCTs that focused on the pediatric population, (3) those in which information regarding intubation outcomes was unavailable, (4) manikin studies or studies involving TI during cardiopulmonary resuscitation, and (5) trials involving the use of conventional laryngoscopes as an adjunct for the video-stylet for TI. Reviews or case reports and trials featuring awake TI or cadaveric models were also excluded.
The same 2 reviewers independently extracted data that included: year of publication, first author, sample size, study setting, immobilization technique, patient characteristics, devices investigated, country, and intubation outcomes. In the situation of disagreements, a third author (C.K.S.) was consulted till a consensus was reached. If the included studies did not report data on outcomes of interest, the authors of individual trials were contacted for the missing information.
2.4. Risk of bias assessment
We used the Cochrane Risk of Bias Tool[20] to assess the methodological quality of the retrieved RCTs. Disagreements were settled through discussion. The risk of bias was categorized as “low,” “unclear,” or “high” in the following 7 domains: “random sequence generation,” “allocation concealment,” “blinding of participants and personnel,” “blinding of outcome assessment,” “incomplete data,” “selective reporting of outcomes,” and “other bias.” The risk of bias of individual studies and the overall risk of bias of all included studies were evaluated.
2.5. Primary and secondary outcomes
The primary outcome was the first-pass success rate (i.e., first-attempt intubation success rate). Secondary outcomes included the overall success rate, the time to intubation, the risk of intubation-associated sore throat, and tissue damage. Subgroup analysis was performed to compare the outcomes associated with the most frequently used video-stylet with those pertinent to the devices less commonly used.
2.6. Statistical analysis
For dichotomous outcomes in the current meta-analysis, the risk ratios (RRs) with 95% confidence intervals (CIs) were calculated with the Mantel-Haenszel (M-H) method. As different video-stylets and variations in the techniques for neck immobilization may be potential sources of heterogeneity, random-effects models were used. For continuous outcomes, the selected effect size was the mean difference (MD). The I2 statistic, which evaluates the percentage of variability in effect estimates due to heterogeneity rather than sampling error, was used to evaluate the impact of heterogeneity on study outcomes.
We conducted sensitivity analyses to examine the robustness of our results through omitting 1 trial from the meta-analysis at a time to assess the potential impact of a single study on the overall results. When 10 or more trials reported on an outcome of interest, we inspected the funnel plots to evaluate the probability of publication bias. The significance level was set at 0.05 for all analyses. Cochrane Review Manager (RevMan 5.4; Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was used for data synthesis.
3. Results
3.1. Study selection
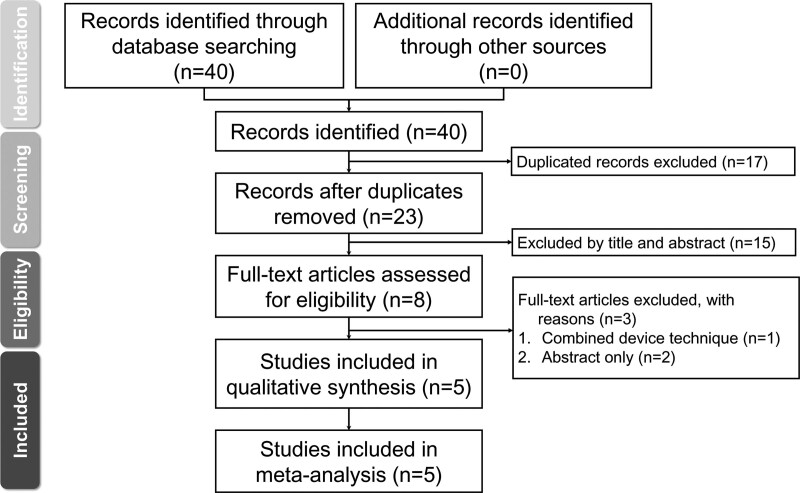
The process of study exclusion and selection in the current meta-analysis is demonstrated in Figure 1. Of the 40 records initially retrieved from the electronic databases for review, 32 were excluded because of data duplication (n = 17) or irrelevance (n = 15). As a result, 8 articles with full text were read independently by 2 investigators. After exclusion of 3 studies due to the availability of only abstracts (n = 2) and the combined use of conventional laryngoscopes and video-stylet for TI (n = 1), a total of 5 studies were included in the present meta-analysis.[21–25]
Figure 1.
Meta-analysis flowchart for selecting eligible studies.
3.2. Characteristics of included studies
Five RCTs involving 487 participants published between 2007 and 2013 were analyzed.[21–25] Study characteristics including patient populations and types of intubation devices are described in Table 1. The number of participants in the included RCTs ranged from 46 to 185. Four studies included patients with a mean body mass index (BMI) being <30 kg/m2,[21,22,24,25] while 1 study did not specify this information.[23] All studies excluded patients with anticipated difficult airways. The models of video-stylets investigated included Bonfils intubation fiberscope,[21–23] Levitan FPS Scope,[24] and Shikani optical stylet.[25] The types of DL examined included McCoy laryngoscope[21] and Macintosh laryngoscope.[22–25] Hard cervical collar was applied for neck stabilization in 3 RCTs,[21–23] while MILS was used in 2 studies.[24,25]
Table 1.
Characteristics of included studies (n = 5).
| Study | Age (yr) | BMI (kg/m2) | Intervention vs control | Technique for neck immobilization | Sample size | Country | Exclude difficult airway |
|---|---|---|---|---|---|---|---|
| Abdullah et al[21] | 49.9 ± 13.0 | 25.7 ± 4.8 23.4 | Bonfils intubation fiberscope | Hard cervical collar | 60 | Singapore | Yes |
| 43.8 ± 13.4 | ± 3.4 | McCoy laryngoscope | |||||
| Byhahn et al[22] | 46.4 ± 20.3 | 24.7 ± 2.7 | Bonfils intubation fiberscope | Hard cervical collar | 76 | Germany | Yes |
| 44.2 ± 19.3 | 25.2 ± 3.4 | Macintosh laryngoscope | |||||
| Gupta et al[23] | 34.3 ± 11.5 | NA | Bonfils intubation fiberscope | Hard cervical collar | 120 | India | Yes |
| 32.0 ± 10.3 | Macintosh laryngoscope | ||||||
| Kok et al[24] | 45 ± 13 | 27.0 ± 5.2 | Levitan FPS Scope | Manual in-line stabilization | 185 | Canada | Yes |
| Macintosh laryngoscope | |||||||
| Turkstra et al[25] | 52 ± 16 | 29 ± 5 | Shikani Optical Stylet | Manual in-line stabilization | 46 | Canada | Yes |
| 50 ± 18 | 29 ± 4 | Macintosh laryngoscope |
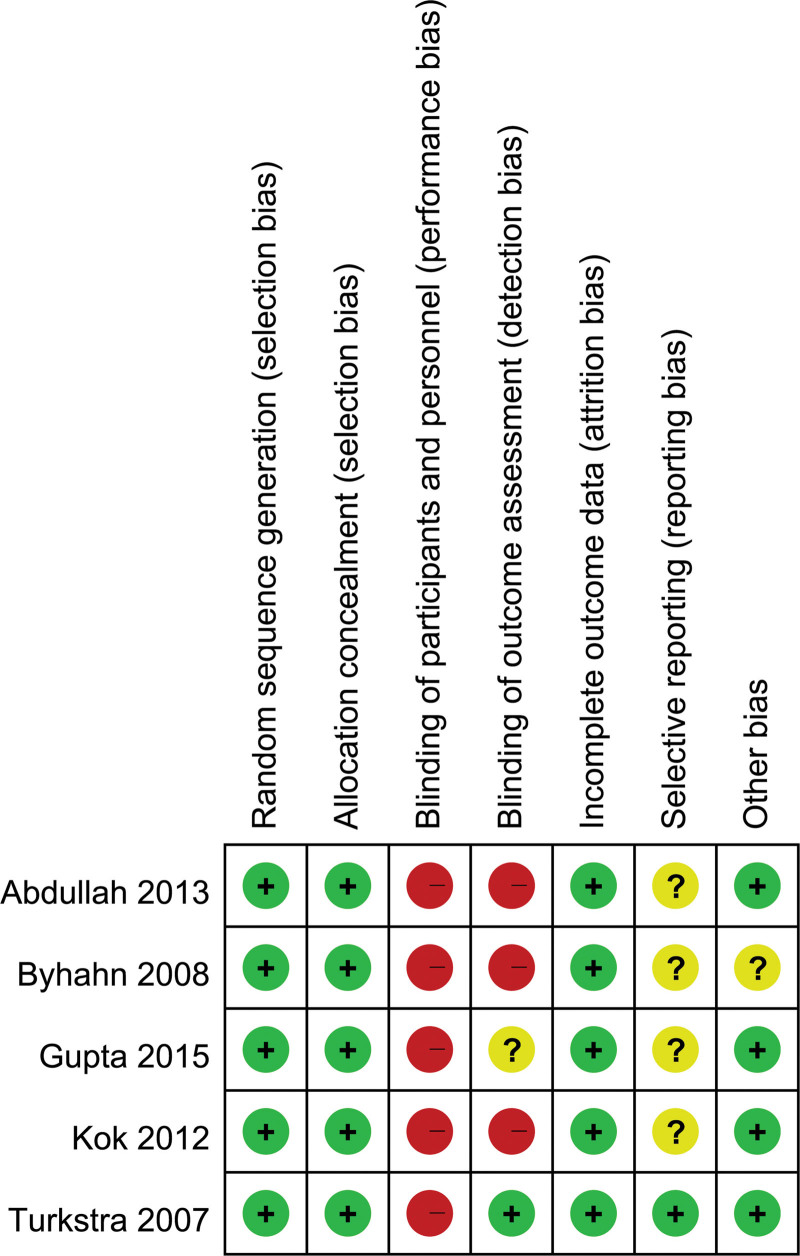
3.3. Risk of bias assessment
The risks of bias of RCTs are shown in Figure 2 and (Figure 1, Supplemental Digital Content, http://links.lww.com/MD/H31). The risks of selection bias and attrition bias were low in all studies due to their provision of sufficient information on randomization with relatively small proportions of patient exclusion.[21–25] However, the risk of blinding of participants was found to be high because it was difficult to blind the operators during TI.[21–25] The risk of detection bias was low in 1 trial,[25] uncertain in another,[23] and high in the other 3 trials.[21,22,24] The risk of reporting bias was uncertain in 4 trials[21–24] because registration information was not available. The risk of other bias was detected in 1 RCT[22] as information regarding conflict of interest was unavailable. Detailed information about bias assessment of the included trials is provided in (Table 2, Supplemental Digital Content, http://links.lww.com/MD/H32).
Figure 2.
Risks of bias of individual studies.
3.4. Intubation outcomes
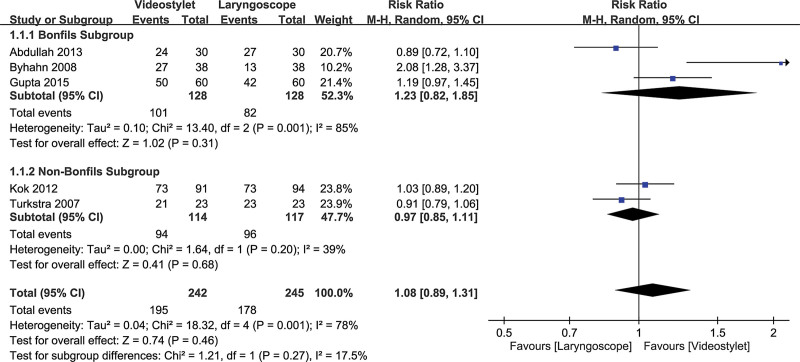
3.4.1. First-pass success rate.
Five studies with a total of 487 patients (video-stylet group, n = 242 vs laryngoscope group, n = 245) were eligible for the analysis.[21–25] The first-pass success rates were 80.6% and 72.7% in the video-stylet group and laryngoscope group, respectively. A forest plot showed no difference between the 2 groups (RR = 1.08, 95% CI: 0.89–1.31, P = .46; I2 = 78%) (Fig. 3). There was also no subgroup difference (P = .27) between the Bonfils intubation fiberscope and other video-stylets. Sensitivity analysis demonstrated no significant impact on outcome by omitting certain trials.
Figure 3.
Forest plot comparing first-pass success rate between video-stylet and laryngoscope groups. CI = confidence interval, M-H = Mantel-Haenszel, RR = risk ratio.
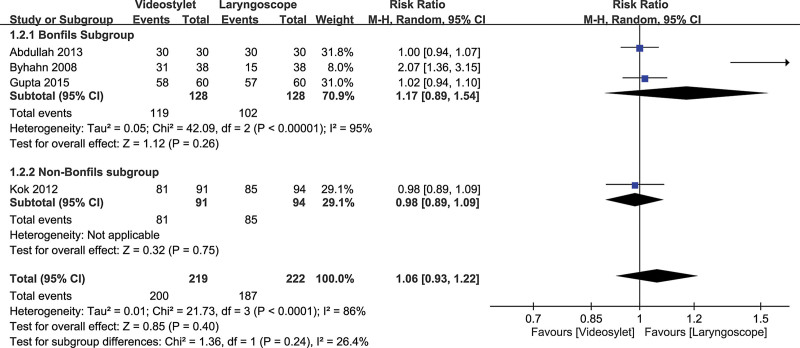
3.4.2. Overall intubation success rate.
The overall intubation success rates were 91.3% and 84.2% in the video-stylet group and the laryngoscope group, respectively. The forest plot on the 4 available studies[21–24] involving a total of 441 patients (video-stylet group, n = 219 vs laryngoscope group, n = 222) showed comparable overall intubation success rates between the video-stylet and the laryngoscope groups (RR = 1.06, 95% CI: 0.93–1.22, P = .4; I2 = 86%) (Fig. 4). Besides, there was no subgroup difference (P = .24) between the Bonfils intubation fiberscope and other video-stylets. No significant impact on outcome was noted by omitting certain trials on sensitivity analysis.
Figure 4.
Forest plot comparing overall intubation success rate between video-stylet and laryngoscope groups. CI = confidence interval, M-H = Mantel-Haenszel, RR = risk ratio.
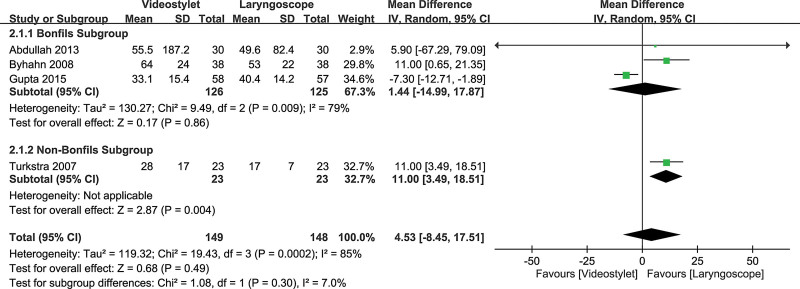
3.4.3. Intubation time.
Inspection of the forest plot of 4 available studies[21–23,25] that recruited a total of 297 patients (video-stylet group, n = 149 vs laryngoscope group, n = 148) revealed a comparable intubation time between the video-stylet and the laryngoscope groups (MD = 4.53, 95% CI: –8.45 to 17.51, P = .49; I2 = 85%) (Fig. 5). However, sensitivity analysis showed that the time to intubation was shorter with DL than that with video-stylets when 1 trial[23] was removed. No subgroup difference (P = .3) was found between the Bonfils intubation fiberscope and the other 2 video-stylets.
Figure 5.
Forest plot comparing time to successful intubation between video-stylet and laryngoscope groups. CI = confidence interval, IV = inverse variance, MD = mean difference.
3.4.4. Risk of tissue damage.
The incidences of tissue damage were 2.7% and 6.8% in the video-stylet group and the laryngoscope group, respectively. The forest plot on 4 available studies[21–24] with a total of 441 patients (video-stylet group, n = 219 vs laryngoscope group, n = 222) demonstrated a similar risk of tissue damage between the video-stylet and laryngoscope groups (RR = 0.46, 95% CI: 0.16–1.3, P = .14; I2 = 12%) (Figure 2, Supplemental Digital Content, http://links.lww.com/MD/H33). There was no subgroup difference (P = .3) between the Bonfils intubation fiberscope and other video-stylets. Sensitivity analysis showed no significant impact on outcome by omitting certain trials.
3.4.5. Risk of sore throat.
The incidence of tissue damage in the video-stylet group and the laryngoscope group was 5% and 11.3%, respectively. The forest plot on 4 available studies[21–24] enrolling a total of 441 patients (video-stylet group, n = 219 vs laryngoscope group, n = 222) revealed a lower risk of sore throat in the video-stylet group compared with that in the laryngoscope group (RR = 0.45, 95% CI: 0.23–0.9, P = .02; I2 = 0%) (Figure 3, Supplemental Digital Content, http://links.lww.com/MD/H34)]. Sensitivity analysis showed that their risks of sore throat were comparable after omitting certain trials.[23,24] No subgroup difference (P = .53) was noted between the Bonfils intubation fiberscope and the other 2 video-stylets.
4. Discussion
Video-stylets allow visualization of the vocal cords and related airway structures without a direct line of sight. Several studies have reported that the video-stylets may offer faster TI and a higher first-pass success rate than those associated with the use of Macintosh laryngoscope.[22,26] The results of our meta-analysis demonstrated that the use of video-stylets was unable to improve the first-pass success rate, overall success intubation rate, and shortening of the intubation time in patients with cervical immobilization compared with conventional DL. Besides, there was no significant difference in the risk of tissue damage between the 2 groups. On the other hand, the use of video-stylets significantly decreased the risk of sore throat compared with that associated with laryngoscopes.
For patients with blunt trauma, cervical in-line stabilization is recommended to reduce the risk of potential secondary injury to the cervical cord.[3] In addition to MILS-associated difficulty in visualization of the glottis, the presence of critical scenarios such as hypoventilation, persistent hypoxemia, airway obstruction, hemorrhagic shock, and cardiac arrest in trauma patients also present physiologic challenges to clinicians responsible for airway management. In general, rapid sequence induction/intubation (RSI) is the preferred method for securing the airway in most trauma patients.[27] Despite the continuous improvement in the design of intubation devices, airway management in the emergency setting still increases the risk of complications, especially in patients undergoing multiple attempts of TI.[27,28] Indeed, a previous study reported that at least one-fourth of all major airway events in a hospital setting occur in the intensive care unit (ICU) or the emergency department,[28] in which failure to secure the airway in a timely manner is likely to result in serious complications or death.[28,29] Since one of the possible reasons for an increased incidence of adverse events is the limited availability of skilled staff and equipment,[28] the availability of appropriate airway devices for TI may optimize the outcomes of trauma patients.
Our meta-analysis found that the first-pass success rate and overall success rate were comparable between patients receiving TI with video-stylets and those being intubated with DL. There were several possible explanations for the finding. First, because most TIs were electively performed by experienced anesthesiologists using DL in the operating room setting, the lack of significant difference in intubation outcomes between normal and difficult airways may mask the theoretical benefits of video-stylets (i.e., difficult airway management).[30] This was supported by the result of a previous study comparing the intubation outcomes between video-laryngoscopes and DL that demonstrated a higher first-pass success rate when TI was performed with the former than that with the latter among novice/trainee clinicians, while there was no significant difference among experienced clinicians.[30] The authors also reported an impact of intubation setting on outcomes; while the use of video-laryngoscopes was associated with a significantly higher first-pass success rate than that with DL in the ICU, the success rates were similar between the 2 devices in the emergency or prehospital setting.[30] Second, compared with DL, the absence of a blade in video-stylets may facilitate TI in patients with limited oral opening.[31] The authors of a previous study that demonstrated a reduction of inter-incisor distance from 4.3 to 2.6 cm after neck collar application suggested that approximately half of participants with a cervical collar were expected to fail TI with DL.[32] Therefore, the benefits of video-stylets may not predominate in our meta-analysis, in which neck collars were applied in only 3 studies[21–23] with the MILS technique being adopted in the other 2.[24,25] Furthermore, the lack of difference in the risk of tissue damage between the 2 approaches may explain their comparable first-pass and overall success rates.
Compared with the operating room setting, a rapid successful TI is especially important among critically ill patients in the emergency setting who may carry the risk of aspiration pneumonia and be unable to tolerate prolonged oxygen desaturation. Overall, we found no significant difference in intubation time between video-stylets and DL. Difficulty in identifying the laryngeal inlet due to an obscured vision of the camera by oral secretion or lens fogging on using video-stylets[33,34] may have masked their potential benefits in patients with cervical immobilization. It was noteworthy that intubation time was shorter with DL than that with video-stylets when 1 trial[23] was removed on sensitivity analysis. Despite reporting of a shorter mean time to visualize the laryngeal inlet with DL (i.e., 15.4 s) compared to that with video-stylets (i.e., 23.8 s) in that study,[23] the total intubation time was still longer with the former probably because of the use of a tube introducer with DL to facilitate TI. Therefore, based on limited evidence, our meta-analysis suggested that the intubation time could be shorter when TI was performed with DL than that with video-stylets. Further large-scale studies are required to validate our findings.
Overall, our meta-analysis did not support the use of video-stylets as the first-line device for TI in patients with neck immobilization except for reducing the risk of sore throat. Nevertheless, they may be used for airway rescue after failure of TI with DL.[35] Besides, there are specific situations where intubation with video-stylets may be advantageous over the conventional laryngoscopic approach such as difficulty in blade insertion in patients with limited oral opening[32] or the need for creating an unobstructed passageway through visualization of the vocal cords with video-stylets.[36] However, the latter does not guarantee an unobstructed path for tracheal tube insertion.[37] Although the operating principle of video-stylets is different from that of laryngoscopes, some authors reported that a steep learning curve can be achieved with video-stylets.[36,38] Taking into account the increasing availability of video-stylets,[36] they may be incorporated into the difficult airway management algorithm to optimize patient care.
There are several limitations in the current report. First, although there are new video-stylets available in the market,[36,39,40] only 3 models of video-stylets were available for analysis in the present meta-analysis. As the design and operating principle among various video-stylets may differ, our results may not be extrapolated to other video-stylets. Second, the high heterogeneity of results across the included trials may be attributed to the choice of different models of video-stylets and the variation in clinician familiarity with their uses. For instance, different curvatures of the distal tip of the video-stylets could contribute to bias and heterogeneity. Third, because the included studies recruited patients with cervical immobilization but excluded those with anticipated difficult airways, our results may not be applied to patients with difficult airways in clinical practice. Fourth, since the laryngoscopic view (i.e., Cormack-Lehane grade) has been reported to be significantly better with MILS than that with cervical collar immobilization,[41] the inclusion of both techniques in the included studies may bias our results. Finally, significant bias may arise from the fact that all anesthesiologists involved in the trials were not blinded to the airway devices that they chose.
5. Conclusion
Our meta-analysis demonstrated that video-stylets and conventional laryngoscopes had comparable first-pass intubation success rate, total successful intubation rate, intubation time, and risk of tissue damage in patients with cervical immobilization, although the risk of sore throat appeared to be lower with video-stylets compared to that with laryngoscopes. Taking into account that only 3 models of video-stylets were available for analysis in the current study, further clinical trials are warranted to elucidate the benefits of video-stylets in the nonoperating room setting.
Author contributions
I.-W.C. and Y.-Y.L. contributed equally as first authors to this work; P.-W.H. and C.-K.S. contributed equally as corresponding authors to this work. I.W.C., K.C.H. and Y.-Y.L. contributed in the design of this study. J.Y.C., M.C.L., K.F.W., and C.M.L. contributed in the data collection. K.C.H., P.-W.H., and C.K.S. contributed in the writing and critical edits of the article.
Supplementary Material
Abbreviations:
- BMI =
- body mass index
- CENTRAL =
- Cochrane Central Register of Controlled Trials
- CI =
- confidence interval
- CSI =
- cervical spine injury
- DL =
- direct laryngoscopy
- ICU =
- intensive care unit
- IV =
- inverse variance
- MD =
- mean difference
- M-H =
- Mantel-Haenszel
- MILS =
- manual in-line stabilization
- RCTs =
- randomized controlled trials
- RR =
- risk ratio
- RSI =
- sequence induction/intubation
- TI =
- tracheal intubation
How to cite this article: Chen I-W, Li Y-Y, Hung K-C, Chang Y-J, Chen J-Y, Lin M-C, Wang K-F, Lin C-M, Huang P-W, Sun C-K. Comparison of video-stylet and conventional laryngoscope for endotracheal intubation in adults with cervical neck immobilization: A PRISMA-compliant meta-analysis. Medicine 2022;101:33(e30032).
The manuscript is a systematic review and meta-analysis and as such data study reporting on published material. Therefore, no Ethics approval is required. The project was registered at PROSPERO, registration number CRD42021252611.
As this is no clinical study but a report on data analysis on published material, consent to publish consent does not apply.
Supplemental Digital Content is available for this article.
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. The full technical report of this meta-analysis and systematic review can be obtained from the authors on request.
Contributor Information
I-Wen Chen, Email: chenjenyin@gmail.com.
Yu-Yu Li, Email: Yuyuli33@hotmail.com.
Kuo-Chuan Hung, Email: ed102605@gmail.com.
Ying-Jen Chang, Email: 0201day@yahoo.com.tw.
Jen-Yin Chen, Email: chenjenyin@gmail.com.
Ming-Chung Lin, Email: chienming95@gmail.com.
Kuei-Fen Wang, Email: kikyw@hotmail.com.
Chien-Ming Lin, Email: chienming95@gmail.com.
Ping-Wen Huang, Email: benwenxx@gmail.com.
References
- [1].Dunham CM, Brocker BP, Collier BD, et al. Risks associated with magnetic resonance imaging and cervical collar in comatose, blunt trauma patients with negative comprehensive cervical spine computed tomography and no apparent spinal deficit. Crit Care. 2008;12:R89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Galvagno SM, Nahmias JT, Young DA. Advanced trauma life support® Update 2019: management and applications for adults and special populations. Anesthesiol Clin. 2019;37:13–32. [DOI] [PubMed] [Google Scholar]
- [3].Stein DM, Pineda JA, Roddy V, et al. Emergency neurological life support: traumatic spine injury. Neurocrit Care. 2015;23:155–64. [DOI] [PubMed] [Google Scholar]
- [4].Nolan JP, Wilson ME. Orotracheal intubation in patients with potential cervical spine injuries. An indication for the gum elastic bougie. Anaesthesia. 1993;48:630–3. [DOI] [PubMed] [Google Scholar]
- [5].Weiss M, Hartmann K, Fischer JE, et al. Use of angulated video-intubation laryngoscope in children undergoing manual in-line neck stabilization. Br J Anaesth. 2001;87:453–8. [DOI] [PubMed] [Google Scholar]
- [6].De Jong A, Rolle A, Pensier J, et al. First-attempt success is associated with fewer complications related to intubation in the intensive care unit. Intensive Care Med. 2020;46:1278–80. [DOI] [PubMed] [Google Scholar]
- [7].Crosby ET. Airway management in adults after cervical spine trauma. Anesthesiology. 2006;104:1293–318. [DOI] [PubMed] [Google Scholar]
- [8].Park C. Risk factors associated with inpatient cardiac arrest during emergency endotracheal intubation at general wards. Acute Crit Care. 2019;34:212–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Crosby ET, Lui A. The adult cervical spine: implications for airway management. Can J Anaesth. 1990;37:77–93. [DOI] [PubMed] [Google Scholar]
- [10].Heidegger T, Gerig HJ, Ulrich B, et al. Validation of a simple algorithm for tracheal intubation: daily practice is the key to success in emergencies—an analysis of 13,248 intubations. Anesth Analg. 2001;92:517–22. [DOI] [PubMed] [Google Scholar]
- [11].Levitan RM, Rosenblatt B, Meiner EM, et al. Alternating day emergency medicine and anesthesia resident responsibility for management of the trauma airway: a study of laryngoscopy performance and intubation success. Ann Emerg Med. 2004;43:48–53. [DOI] [PubMed] [Google Scholar]
- [12].Santoni BG, Hindman BJ, Puttlitz CM, et al. Manual in-line stabilization increases pressures applied by the laryngoscope blade during direct laryngoscopy and orotracheal intubation. Anesthesiology. 2009;110:24–31. [DOI] [PubMed] [Google Scholar]
- [13].Hung KC. A novel modified method of using trachway intubating stylet for awake tracheal intubation in patients with anticipated difficult airway. Acta Anaesthesiol Taiwan. 2013;51:90–3. [DOI] [PubMed] [Google Scholar]
- [14].Mahrous RSS, Ahmed AMM. The shikani optical stylet as an alternative to awake fiberoptic intubation in patients at risk of secondary cervical spine injury: a randomized controlled trial. J Neurosurg Anesthesiol. 2018;30:354–8. [DOI] [PubMed] [Google Scholar]
- [15].Nam K, Lee Y, Park H-P, et al. Cervical spine motion during tracheal intubation using an Optiscope versus the Mcgrath videolaryngoscope in patients with simulated cervical immobilization: a prospective randomized crossover study. Anesth Analg. 2019;129:1666–72. [DOI] [PubMed] [Google Scholar]
- [16].Yoon H-K, Lee H-C, Park J-B, et al. McGrath MAC Videolaryngoscope versus optiscope video Stylet for tracheal intubation in patients with manual inline cervical stabilization: a randomized trial. Anesth Analg. 2020;130:870–8. [DOI] [PubMed] [Google Scholar]
- [17].Hoshijima H, Kuratani N, Hirabayashi Y, et al. Pentax airway scope® vs Macintosh laryngoscope for tracheal intubation in adult patients: a systematic review and meta-analysis. Anaesthesia. 2014;69:911–8. [DOI] [PubMed] [Google Scholar]
- [18].Hoshijima H, Mihara T, Maruyama K, et al. C-MAC videolaryngoscope versus Macintosh laryngoscope for tracheal intubation: a systematic review and meta-analysis with trial sequential analysis. J Clin Anesth. 2018;49:53–62. [DOI] [PubMed] [Google Scholar]
- [19].Hoshijima H, Mihara T, Maruyama K, et al. McGrath videolaryngoscope versus Macintosh laryngoscope for tracheal intubation: a systematic review and meta-analysis with trial sequential analysis. J Clin Anesth. 2018;46:25–32. [DOI] [PubMed] [Google Scholar]
- [20].Higgins JP, Altman DG, Gøtzsche PC, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Abdullah HR, Li-Ming T, Marriott A, et al. A comparison between the Bonfils intubation fiberscope and Mccoy laryngoscope for tracheal intubation in patients with a simulated difficult airway. Anesth Analg. 2013;117:1217–20. [DOI] [PubMed] [Google Scholar]
- [22].Byhahn C, Nemetz S, Breitkreutz R, et al. Brief report: tracheal intubation using the Bonfils intubation fibrescope or direct laryngoscopy for patients with a simulated difficult airway. Can J Anaesth. 2008;55:232–7. [DOI] [PubMed] [Google Scholar]
- [23].Gupta A, Thukral S, Lakra A, et al. A comparison between left molar direct laryngoscopy and the use of a Bonfils intubation fibrescope for tracheal intubation in a simulated difficult airway. Can J Anaesth. 2015;62:609–17. [DOI] [PubMed] [Google Scholar]
- [24].Kok T, George RB, McKeen D, et al. Effectiveness and safety of the Levitan FPS scope™ for tracheal intubation under general anesthesia with a simulated difficult airway. Can J Anaesth. 2012;59:743–50. [DOI] [PubMed] [Google Scholar]
- [25].Turkstra TP, Pelz DM, Shaikh AA, et al. Cervical spine motion: a fluoroscopic comparison of Shikani optical stylet vs Macintosh laryngoscope. Can J Anaesth. 2007;54:441–7. [DOI] [PubMed] [Google Scholar]
- [26].Yang M, Kim JA, Ahn HJ, et al. Double-lumen tube tracheal intubation using a rigid video-stylet: a randomized controlled comparison with the Macintosh laryngoscope. Br J Anaesth. 2013;111:990–5. [DOI] [PubMed] [Google Scholar]
- [27].Kerslake D, Oglesby AJ, Di Rollo N, et al. Tracheal intubation in an urban emergency department in Scotland: a prospective, observational study of 3738 intubations. Resuscitation. 2015;89:20–4. [DOI] [PubMed] [Google Scholar]
- [28].Cook TM, Woodall N, Harper J, et al. Major complications of airway management in the UK: results of the fourth national audit project of the royal college of anaesthetists and the difficult airway society. Part 2: intensive care and emergency departments†. Br J Anaesth. 2011;106:632–42. [DOI] [PubMed] [Google Scholar]
- [29].Miraflor E, Chuang K, Miranda MA, et al. Timing is everything: delayed intubation is associated with increased mortality in initially stable trauma patients. J Surg Res. 2011;170:286–90. [DOI] [PubMed] [Google Scholar]
- [30].Arulkumaran N, Lowe J, Ions R, et al. Videolaryngoscopy versus direct laryngoscopy for emergency orotracheal intubation outside the operating room: a systematic review and meta-analysis. Br J Anaesth. 2018;120:712–24. [DOI] [PubMed] [Google Scholar]
- [31].Hung KC, Tan PH, Lin VC, et al. A comparison of the Trachway intubating stylet and the Macintosh laryngoscope in tracheal intubation: a manikin study. J Anesth. 2013;27:205–10. [DOI] [PubMed] [Google Scholar]
- [32].Yuk M, Yeo W, Lee K, et al. Cervical collar makes difficult airway: a simulation study using the LEMON criteria. Clin Exp Emerg Med. 2018;5:22–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Cho EA, Hwang SH, Lee SH, et al. Does glycopyrrolate premedication facilitate tracheal intubation with a rigid video-stylet? A randomized controlled trial. Medicine (Baltim). 2018;97:e11834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Halligan M, Charters P. A clinical evaluation of the Bonfils Intubation Fibrescope. Anaesthesia. 2003;58:1087–91. [DOI] [PubMed] [Google Scholar]
- [35].Frerk C, Mitchell VS, McNarry AF, et al. Difficult airway society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115:827–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Pius J, Noppens RR. Learning curve and performance in simulated difficult airway for the novel C-MAC® video-stylet and C-MAC® Macintosh video laryngoscope: a prospective randomized manikin trial. PLoS One. 2020;15:e0242154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Lascarrou JB, Boisrame-Helms J, Bailly A, et al. Video laryngoscopy vs direct laryngoscopy on successful first-pass orotracheal intubation among ICU patients: a randomized clinical trial. JAMA. 2017;317:483–93. [DOI] [PubMed] [Google Scholar]
- [38].Biro P, Bättig U, Henderson J, et al. First clinical experience of tracheal intubation with the sensascope®, a novel steerable semirigid video stylet. Br J Anaesth. 2006;97:255–61. [DOI] [PubMed] [Google Scholar]
- [39].Pius J, Ioanidis K, Noppens RR. Use of the novel C-MAC video stylet in a case of predicted difficult intubation: a case report. A A Pract. 2019;13:88–90. [DOI] [PubMed] [Google Scholar]
- [40].Tsay PJ, Hsu SW, Peng HC, et al. Trachway intubating stylet for tracheal intubation in an ankylosing spondylitis patient undergoing total hip replacement under general anesthesia. Acta Anaesthesiol Taiwan. 2011;49:159–61. [DOI] [PubMed] [Google Scholar]
- [41].Gerling MC, Davis DP, Hamilton RS, et al. Effects of cervical spine immobilization technique and laryngoscope blade selection on an unstable cervical spine in a cadaver model of intubation. Ann Emerg Med. 2000;36:293–300. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.