Abstract
This study aimed to explore the association between sleep and suicidality in the presence and absence of depressive symptoms in the rural Chinese population. The research involved a cross-sectional survey conducted in Liuyang, China, between November 2010 and August 2011. A total of 2052 participants were surveyed (987 males and 1065 females). To investigate the mediating effect of depressive symptoms in the correlation between sleep quality and suicidality. The association between sleep quality and suicidality in the absence of depressive symptoms was also explored. Suicide risk was measured using the Mini-International Neuropsychiatric Interview subscale. The visual analog scale was used to assess sleep quality. Patient Health Questionnaire-9 and Patient Health Questionnaire-2, avoiding the overlap in sleep and suicidality assessments, were used for detecting depressive symptoms in participants. Depressive symptoms partially mediated the association between sleep quality and suicidality among rural adults. Furthermore, some participants did not exhibit depressive symptoms in this study yet still exhibited a risk for suicidality, with poor sleep quality contributing significantly to their suicidality even after adjusting for cofounders. Poor sleep quality significantly increases the likelihood of suicidality in the presence and absence of depressive symptoms in the rural Chinese population. Poor sleep quality could correlate with increased suicide risk independently of depressive symptoms.
Keywords: depressive symptoms, Sleep quality, suicidality
1. Introduction
Suicide is the act of intentionally causing one’s death, which is an essential public health and mental health concern worldwide. The World Health Organization reported in 2021 that 703,000 people commit suicide internationally annually,[1] and it was estimated that 77% of global suicides occur in low-income and middle-income countries.[1] It was reported that the average suicide rate was 6.75 per 100,000 people annually in China during 2012–2015.[2] According to the World Health Organization report, the suicide rate in China was 8.2 per 100,000 in 2016 and was 8.1 per 100,000 from 2017 to 2019.[3] The identification of modifiable predictive factors for suicidality in the general population could result in the development of management and prevention strategies for suicide risk. The association between poor sleep and suicidality had been reported; however, whether depressive symptoms mediate the correlation between sleep and suicidality is controversial.
Since Fawcett et al[4] initially reported the link between sleep, depression, and suicide in 1990, the associations between sleep, depressive symptoms, and suicidality have been widely reported.[5–17] The mediating role of depression was proposed in this association, including 2 hypotheses of either total mediation or partial mediation. Some studies have proposed that the impact of sleep quality on suicidality appears to be entirely mediated by depressive symptoms.[13,14] and sleep could not directly impact suicidality. However, a second mediation perspective proposes that depressive symptoms play a partial mediation role in the correlation. In other words, the associations between poor sleep quality and suicidality are connected both directly and indirectly via depressive symptoms.[7,15] Notably, other studies assert that the link between sleep and suicidality exists in the absence of, or independently from, depressive symptoms.[16–18]
Most studies investigating the correlation between sleep, depression, and suicidality include participants from western countries or developed areas.[5,8,10,11,19] Seldom investigated are adults from low-income and resource-poor regions such as rural China. It has been estimated that 79% of all suicides in China occur in rural residents from low-income and resource-poor areas.[20] The current study data are from a cross-sectional survey conducted in rural areas of Liuyang, China. The study explored: the association between sleep quality and suicidality in the presence of depressive symptoms: the mediation effects of depressive symptoms were assessed; if there are participants who were suicidal in the absence of depressive symptoms, the correlation between sleep quality and suicidality was explored.
2. Methods
2.1. Design overview
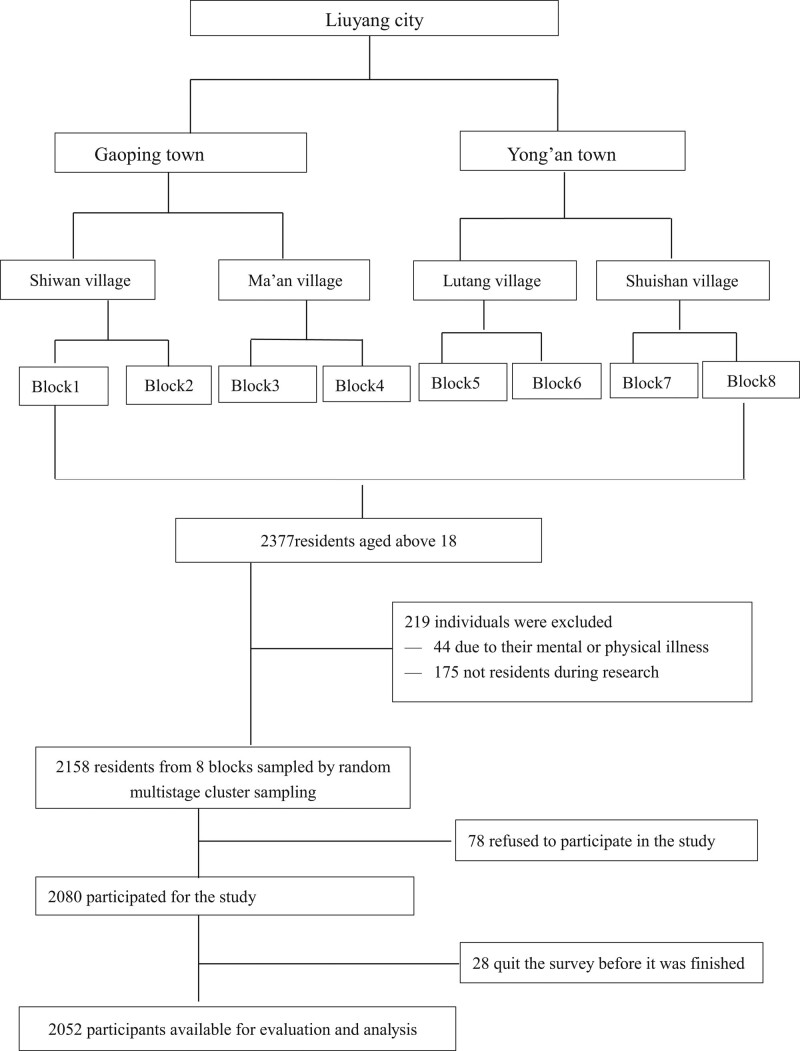
Before this study commenced, the bidding documents and oral informed consents were submitted to the ethics committee of the Institutional Review Board for review. All of these were approved by the School’s Institutional Review Board per the Declaration of Helsinki. Multistage sampling was employed, and a total of 8 sample sites (sample sites referred to a geographical neighborhood) were selected from rural areas of Liuyang by generating a list based on random numbers, from which participants were enrolled (Fig. 1). Interviewing teams were organized to conduct face-to-face surveys between November 2010 and August 2011.
Figure 1.
Flowchart of the participant’s enrollment.
2.2. Participants
Rural Chinese individuals source incomes from agricultural activities and related products. Participants in the study were selected from the rural Chinese population living in Liuyang, a representative rural city of the Hunan province,[21] southern China. Liuyang County, located in the center of Hunan province, has a population of 1.4235 million, including people of Han nationality and 34 ethnic minorities. Liuyang is the center of fireworks production in China, with a proud history spanning 1400 years. Other primary industries such as grain production, raising pigs, and black goats are also prominent in the region.
The eligibility criteria for this study included residents who were >18 years old and had lived in the rural areas of Liuyang for >6 months. The exclusion criteria included: participants who were physically injured or impaired cognitively, which could influence the experience of sleep quality or depressive symptoms; residents who could not be contacted after 3 attempts by the study team. A total of 2158 adults were invited to participate in the study. However, according to the exclusion criteria, 78 people (2.80%) were excluded, and 28 people (1.30%) discontinued their participation before study completion. The included responses from 2052 participants corresponded to a response rate of 95.09%.
2.3. Procedure
The survey team was composed of 1 principal investigator (a PhD student), post-graduate students, undergraduates and 3 local guides who were bilingual in Chinese Mandarin and the local dialect. All the team members were trained before data collection. The training included the interviews’ objectives and contents, vital communication skills, and dialect translation standards. The team was divided into 3 interviewing groups, and each interviewing team was composed of 5 investigators and 1 guide. The interviewing team visited each potential family at their house. The team introduced the project to the whole family in Mandarin, which was translated into the local dialect when necessary by the guide. Participants agreed that the results of this study would be published in the form of essays or articles, and no personal information would be disclosed in any reports. Interviews took place individually, and the interviewer recorded the verbal responses of each participant. The local guide would explain the interviewer’s statements in the native dialect when necessary. Each participant was reimbursed with a kitchen utensil. After completing the interview, the researchers collected the data and entered it into a centralized database.
2.4. Quality control
Centralized and standard training was given to the research team before the surveys were undertaken so that all investigators and guides understood the questionnaire contents. After respondents completed the survey, a quality-control person checked the questionnaire to ensure there were no missing items.
2.5. Dependent variables
2.5.1. Suicidality.
In this study, suicidality was measured using the subscale from the Mini-International Neuropsychiatric Interview: the Suicide Risk Screening Scale. The interview tool included 10 questions about suicidal ideation, suicidal planning, and suicide attempts during the past month. Suicidal ideation refers to an individual’s thoughts about ending their own life. Suicidal plans refer to an individual planning to die by suicide. Suicide attempts refer to attempting to end one’s life by any method that could result in death, such as drug overdose, hanging, or wrist cutting. Each question had 3 options “yes,” “no,” or “I do not know.” The answers to these questions were used to classify the participants into 4 subgroups: no risk, low risk (suicidal ideation), moderate risk (suicidal plans), and high risk (suicide attempts) of suicide. Having no suicide risk to the low, middle, and high risk was defined as y = 1–4.
2.6. Independent variables
2.6.1. Sleep quality.
The VAS could be interpreted into the local dialect quickly when necessary and easily understood by rural Chinese participants, who are less educated than urban residents, and so it was chosen to assess sleep quality. The VAS used in this study consisted of a 0 to 100 mm line calibrated with numbers from 0 to 10 to assist the rural participants in determining the distance between the worst sleep quality at one end and the best sleep quality at the other. The reliability and validity of VAS in measuring subjective experience have been reported in the literature.[22–24] VAS is often used in many research studies as a convenient and straightforward method to assess subjective sleep quality.[25–27]
2.7. Covariates
2.7.1. Sociodemographic variables.
Data about gender, age, education, marital status, and income were collected from participants. Education level was categorized into 3 groups: primary school or below, middle school, and high school or above. Marital status has 2 possible responses: stable or unstable relationship (the former included marriage or cohabitation). Incomes were expressed as annual figures.
2.7.2. Depressive symptoms.
The PHQ-9 is a 9-item scale, with each item based on the criteria for depressive disorders listed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Each item is rated using a scale from 0 (not at all) to 3 (nearly every day),[28] and the final score ranges from 0 to 27. The Chinese version of the PHQ-9 has a 2-week test–retest reliability of 0.86 as well as Cronbach alpha of 0.86.[29]
Additionally, PHQ-2 was used for assessing depressive symptoms in this study. PHQ-2 is composed of 2 primary items of PHQ-9 (first item: little interest or pleasure in doing things; second item: feeling down, depressed, or hopeless) and avoids the overlap in sleep quality and suicidality assessments. Its reliability and validity had previously been broadly demonstrated.[30,31] Many studies had demonstrated that a score of 3 (the total PHQ-2 score ranges from 0 to 6) was the cutoff point for screening for possible depression and is considered highly sensitive and valid.[30–32]
2.7.3. Physical health conditions.
Physical health correlates with an individual’s physical function and was measured using the self-reporting physical health subscale of the Self-Rated Health Measurement Scale, developed and revised by Xu et al,[33] with a Cronbach α coefficient of 0.93.[34] The highest possible scores for physical health are 170. The higher values indicated better physical health.
2.8. Statistical analysis
Sample characteristics were detailed using basic descriptive statistics, such as numbers and sample percentages. Sleep quality and related suicide risks were assessed. Structure equation models were conducted for the mediation tests. Sleep quality was recorded from 0.00 to 10.00 (from the worst to the best). Depressive symptoms were assessed using the PHQ-9 and PHQ-2 scoring systems. No, low, middle, or high suicidality was defined as y = 1–4.
Ordinal regression models explore the influence of sleep quality on suicidality. Suppose participants displayed no depressive symptoms but were still at risk of suicidality. First, an ordinal regression analysis investigated sleep quality as a single variable to predict suicide risk among the participants. Second, covariates that may be associated with suicide risk in real-life situations were adjusted for further ordinal regression analysis. The statistical significance was defined at a P value of <.05 (2-tailed). The SPSS 20.0 and Mplus 7.2 software packages were used for statistical analyses.
3. Results
3.1. Fundamental characteristics of the study population
The study had 2052 participants (Table 1), including 1065 females and 987 males. Most participants were in the middle-aged group (47.61%), while 38.79% and 13.60% were in the young and older groups. Only 15.3% of the participants had a high school education or above. In 2009, the national rural poverty line was defined as earning <1992 yuan/year. In the Hunan Province in 2010, the average income per farmer was 5523 yuan/ year. Participants’ income was divided into 3 groups in this study: low (≤1992 yuan/year), medium (1993–5523 yuan/year), and high (≥5524 yuan/year). Approximately one-tenth of the participants were below the poverty line, and almost two-thirds were above the average farmer income in the Hunan Province.
Table 1.
Sociodemographics characteristics of the sample (n = 2052).
| Characteristics | N | % |
|---|---|---|
| Gender | ||
| Male | 987 | 48.10 |
| Female | 1065 | 51.90 |
| Age (yr) | ||
| 18–44 | 796 | 38.79 |
| 45–59 | 977 | 47.61 |
| ≥60 | 279 | 13.60 |
| Education | ||
| Primary school or below | 814 | 39.70 |
| Middle school | 925 | 45.10 |
| High school or above | 313 | 15.30 |
| Marital status | ||
| Without partner | 195 | 9.02 |
| Married/cohabited | 1867 | 90.98 |
| Income (person/year) (RMB) | ||
| ≤1992 | 241 | 11.74 |
| 1993–5523 | 513 | 25.00 |
| ≥5524 | 1298 | 63.26 |
RMB = Ren Ming Bi.
3.2. The association between sleep quality and suicidality in the presence of depressive symptoms
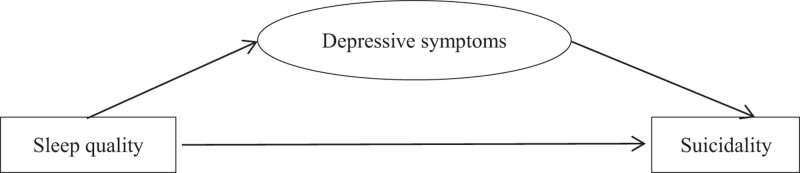
Structure equation models was conducted to test whether depressive symptoms could influence suicidality via sleep quality, as shown in Figure 2. The PHQ-9 and PHQ-2, respectively, assessed depression symptoms. The first mediation model used the data where depressive symptoms were assessed using the PHQ-9 system, as shown in Tables 2 to 4. The data did not fit well with the mediation model, for CFI = 0.837, TLI = 0.792, RMSEA = 0.102, and SRMR = 0.057. The partial mediation effect of depression symptoms in the association between sleep quality and suicidality was significant.
Figure 2.
Mediation diagram.
Table 2.
Model fit information of using PHQ-9.
| Model description | χ2 | df | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|---|
| 5699.319 | 55 | 0.837 | 0.792 | 0.102 | 0.057 |
PHQ-9 = Patient Health Questionnaire-9.
Table 4.
Effect of sleep on suicidality of using PHQ-9.
| Path way | B | Effect ratio |
|---|---|---|
| Sleep-suicidality | –0.011 | 5.7% |
| Sleep-(PHQ-9)-suicidality | –0.476 × (0.381) = –0.181 | 94.27% |
| Total effect of sleep on suicidality | –0.192 |
PHQ-9 = Patient Health Questionnaire-9.
Table 3.
Standardized model results of the mediation of using PHQ-9.
| Suicidality on | P value | 95% CI | |||
|---|---|---|---|---|---|
| b | SE | Lower 2.5% | Upper 2.5% | ||
| PHQ-9 | 0.381 | 0.017 | .000 | 0.301 | 0.459 |
| Sleep | –0.011 | 0.001 | .000 | –0.074 | 0.050 |
| PHQ-9 onsleep | –0.476 | 0.009 | .000 | –0.526 | –0.431 |
CI = confidence interval, PHQ-9 = Patient Health Questionnaire-9, SE = standard error.
The second mediation model used the depressive symptoms scoring by PHQ-2, which avoided the overlapping assessment of sleep and suicidality. As shown in Table 5, the data had a good fit with the mediation model, CFI = 0.999, TLI = 0.992, RMSEA = 0.025, and SRMR = 0.006. The Estimated standardized coefficient for the full path model is presented in Table 6. Depressive symptoms partially mediated the influence of sleep on suicidality. There was an independent effect of sleep quality on suicidality beyond depressive symptoms, as shown in Table 7.
Table 5.
Model fit information of using PHQ-2.
| Model description | χ2 | df | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|---|
| 2.309 | 1 | 0.999 | 0.992 | 0.025 | 0.006 |
PHQ-2 = Patient Health Questionnaire-2.
Table 6.
Standardized model results of the mediation of using PHQ-2.
| Suicide on | P value | 95% CI | |||
|---|---|---|---|---|---|
| b | SE | Lower 2.5% | Upper 2.5% | ||
| PHQ-2 | 0.345 | 0.044 | .000 | 0.227 | 0.398 |
| Sleep | –0.070 | 0.025 | .007 | –0.117 | –0.023 |
| PHQ-2 on sleep | –0.349 | 0.027 | .000 | –0.403 | –0.295 |
CI = confidence interval, PHQ-2 = Patient Health Questionnaire-2, SE = standard error.
Table 7.
Effect of sleep on suicidality of using PHQ-2.
| Path way | B | Effect ratio |
|---|---|---|
| Sleep-suicidality | –0.070 | 38.84% |
| Sleep-(PHQ-2)-suicidality | –0.349 × 0.345 = –0.120 | 63.16% |
| Total effect of sleep on suicidality | –0.190 |
PHQ-2 = Patient Health Questionnaire-2.
3.3. Association between sleep quality and suicidality in participants in the absence of depressive symptoms
Whether there were individuals without depressive symptoms yet still experiencing suicidality was explored. First, those participants with a total score of <5 for the PHQ-9 cohort of responses were categorized as not having any apparent symptoms of depression. The data in Table 8 shows that 1396 participants exhibited no depressive symptoms. However, the survey responses suggested that 112 of them were at either low risk (suicidal ideation), moderate risk (suicide plans), or high risk (suicide attempts) of suicidality. Second, a total score of <3 for the PHQ-2 was defined as not exhibiting any depressive symptoms. As shown in Table 8, 1845 participants showed no signs of depressive symptoms. However, the survey responses suggested that 206 of them were at either low risk (suicidal ideation), moderate risk (suicide plans), or high risk (suicide attempts) of suicidality.
Table 8.
Participants without depressive symptoms yet were at risk of suicidality.
| Distribution of suicidality | |||||
|---|---|---|---|---|---|
| N | No risk | Low risk | Middle risk | High risk | |
| PHQ-9 <5 | 1396 | 1284 | 110 | 1 | 1 |
| PHQ-2 <3 | 1845 | 1639 | 200 | 2 | 4 |
PHQ-2 = Patient Health Questionnaire-2, PHQ-9 = Patient Health Questionnaire-9.
The impact of sleep quality on suicidality among participants with no depressive symptoms was further investigated, as detailed in Table 9. First, a total score of <5 in the PHQ-9 and a total scoreof <3 in the PHQ-2 were defined as no apparent symptoms of depression, respectively, and converging results showed that poor sleep quality correlated significantly with suicidality. Second, gender, age, and physical health were included as covariates in the regression (Tables 10 and 11). Table 11 showed that the association between poor sleep quality and suicide risk persisted significant after adjusting related covariates.
Table 9.
Association between sleep quality and suicidality in participants absent of depressive symptoms.
| Variable | b | Se | Beta | t | P value | |
|---|---|---|---|---|---|---|
| PHQ-9 <5 | Sleep quality | –0.009 | 0.004 | –0.068 | –2.549 | .011 |
| PHQ-2 <3 | Sleep quality | –0.017 | 0.003 | –0.118 | –5.095 | .000 |
PHQ-2 = Patient Health Questionnaire-2, PHQ-9 = Patient Health Questionnaire-9.
Table 10.
Association between sleep quality, covariates and suicidality among participants absent of depressive symptoms (PHQ-9 <5).
| Variables | B | Se | Beta | t | P value |
|---|---|---|---|---|---|
| Gender | –0.041 | 0.015 | –0.072 | –2.701 | .007 |
| Age | 0.001 | 0.001 | 0.029 | 1.073 | .284 |
| Physical health | –0.002 | 0.001 | –0.098 | –3.316 | .001 |
| Sleep quality | –0.003 | 0.004 | –0.022 | –0.736 | .462 |
PHQ-9 = Patient Health Questionnaire-9.
Table 11.
Association between sleep quality, covariates, and suicidality among participants absent of depressive symptoms (PHQ-2 <3).
| Variables | B | Se | Beta | t | P value |
|---|---|---|---|---|---|
| Gender | –0.060 | 0.016 | –0.087 | –3.775 | .000 |
| Age | 0.001 | 0.001 | 0.036 | 1.541 | .124 |
| Physical health | –0.002 | 0.001 | –0.116 | –4.291 | .000 |
| Sleep quality | –0.008 | 0.004 | –0.053 | –1.995 | .046 |
PHQ-2 = Patient Health Questionnaire-2.
4. Discussion
In China, the limited mental health facilities and healthcare workforce are focused in large urban centers. Rural areas in China are less developed than urban areas, have worse medical conditions, and have minimal access to mental health information and services. The scarcity and inefficiency of mental health resources in rural areas present a challenge to managing and reducing suicidality in resource-poor communities. Factors that influence suicide risks, such as mental disorders,[35–38] substance abuse disorders,[39] socioeconomic status,[40,41] and marital status[42–45] were difficult and costly to mitigate in poorly resourced rural areas.
The results showed that depressive symptoms partially mediated the correlation between sleep quality and suicidality among rural adults. The current study used data derived from the PHQ-9 and PHQ-2 scoring systems, with the data modeling much better for the PHQ-2 dataset. Superior modeling may be because the PHQ-9 responses contain data overlap for sleep and suicidality. Results indicated that rural adults at risk of suicidality in combination with obvious depressive symptoms need to treat sleep quality and depressive symptoms to prevent suicidality. In addition, the results indicated that sleep quality could influence suicidality even in the absence of depressive symptoms in rural adults, which was convergent with the report of Geoffroy et al[46] that sleep complaints associated with increased suicide risk independently of psychiatric disorders in the US adult population. This finding led to the designation of poor sleep quality as an independent risk factor for suicidality. When considering previous reports,[12,47–49] improving sleep quality might be a preventative method for decreasing suicidality among people with and without depressive symptoms in rural China.
The treatment for sleep quality in poorly resourced rural communities for suicidality prevention has favorable advantages over other treatments deserving the attention of public policy makers, public health professionals, and clinicians. First, family members or neighbors could quickly undertake to screen and assess sleep quality in rural communities using a straightforward VAS scoring system, particularly since residents in rural China were less educated than urban residents. Even illiterate people could use VAS extended training simply because it is such a visual score that: consider sleep quality and ranks it from 0 to 100 mm. Second and controversially, using medications such as alprazolam to induce sleep is relatively inexpensive in rural China. Third, reducing suicide risk by seeking treatment for poor sleeping quality may be more acceptable to rural adults, who are reluctant to seek mental health assistance due to associated social stigmas in rural culture.[50]
The mechanism by which poor sleep quality influences suicidality remains unclear. Apart from common neurobiological factors for sleep quality and depressive symptoms, such as the 5-hydroxytryptamine neurotransmitter pathways, the influence of sleep quality on suicide risk probably involves a more complex neurobiological process and specific areas of the brain, such as hypothalamus–pituitary–adrenal dysfunction, cortisol release, and the circadian rhythm.[51] This could explain why some of the participants in this study showed no signs of depression in their survey responses yet revealed a suicide risk profile. Poor sleep quality may lead to cognitive decline,[52] worsening suicidal thoughts, and suicide attempts. The underlying physiological and psychological mechanism between sleep and suicidality needs further exploration.
4.1. Limitation
One apparent limitation of this study was that only a few participants reported high suicide risk in the survey (mainly suicide ideation). More in-depth investigations are required to replicate the associations between poor sleep quality and suicide behavior in the general population. The clinical significance of the association between poor sleep quality and suicidality needs to be further characterized with more detailed, longitudinal studies. A series of psychological and biological mechanisms warrant investigation to understand the association between sleep problems and suicidality more fully. Finally, sleep and clinical depression may mediate each other. Future research could include better strategies to account for an absence of depression by including clinical diagnoses.
5. Conclusion
Poor sleep quality would significantly increase the likelihood of suicidality in the presence and absence of depressive symptoms in the rural Chinese population. Poor sleep quality could correlate with increased suicide risk independently of depressive symptoms.
Acknowledgments
The authors would like to thank the village cadres for guiding us to visit each household in the rural areas of Liuyang City, Hunan province, China.
Abbreviations:
- PHQ-2 =
- Patient Health Questionnaire-2
- PHQ-9 =
- Patient Health Questionnaire-9
- VAS =
- visual analog scale
How to cite this article: Liu X-K, Li Q-F, Han D-C, Cheng W, Song N, Hu M, Xiao S-Y. The association between sleep and suicidality in the presence and absence of depressive symptoms: A cross-sectional study in rural China. Medicine 2022;101:33(e29725).
This writing process of the paper was supported by the Project from Education Department of Hainan Province (Number Hnjg2020-62) and Education Research Project of Hainan Medical University (Number HYZ201913).
The investigation in Liuyang was funded by the National Science and Technology Support Program, China (number: 2009BAI77B01; number: 2009BAI77B08).
The authors have no conflict of interest to disclose.
The ethics approval was obtained from the Institutional Review Boards of the School of Public Health (the previous name of the school, and it is now known as Xiangya School of Public Health) of Central South University. The study was externally peer reviewed.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Contributor Information
Xiao-Kun Liu, Email: lacyfairy@qq.com.
Qi-Fu Li, Email: lee-chief@163.com.
Na Song, Email: nanier1@163.com.
Mi Hu, Email: humi213@163.com.
References
- [1].WHO. Suicide. 2021. Available at: https://www.who.int/news-room/fact-sheets/detail/suicide.
- [2].Liu Z, et al. Suicide rate trends in China from 2002-2015. Chin Men Health J. 2017;31:756–67. [Google Scholar]
- [3].WHO. Suicide rate estimates, crude—estimates by country. 2019. Available at: https://apps.who.int/gho/data/view.main.MHSUICIDEv?lang=en.
- [4].Fawcett J, Scheftner WA, Fogg L, et al. Time-related predictors of suicide in major affective disorder. Am J Psychiatry. 1990;147:1189. [DOI] [PubMed] [Google Scholar]
- [5].Lee YJ, Cho SJ, Cho IH, et al. Insufficient sleep and suicidality in adolescents. Sleep. 2012;35:455–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76:84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Wong MM, Brower KJ. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J Psychiatr Res. 2012;46:953–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004;27:1351–8. [DOI] [PubMed] [Google Scholar]
- [9].Park T.-J, Kim J. Is insufficient sleep duration associated with suicidal behavior in Korean adolescents? Sleep Biol Rhythms. 2017;15:117–25. [Google Scholar]
- [10].Goodwin RD, Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. 2008;31:1097–101. [PMC free article] [PubMed] [Google Scholar]
- [11].Kim JH, Park EC, Cho WH, et al. Association between total sleep duration and suicidal ideation among the Korean general adult population. Sleep. 1572;36:1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ribeiro JD, Pease JL, Gutierrez PM, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord. 2012;136:743–50. [DOI] [PubMed] [Google Scholar]
- [13].Lettau LA. Sleep, depression and suicide. Sleep Med. 2011;12:198. [DOI] [PubMed] [Google Scholar]
- [14].Bryan CJ, Gonzales J, Rudd MD, et al. Depression mediates the relation of insomnia severity with suicide risk in three clinical samples of U.S. military personnel. Depress Anxiety. 2015;32:647–55. [DOI] [PubMed] [Google Scholar]
- [15].Becker SP, Dvorsky MR, Holdaway AS, et al. Sleep problems and suicidal behaviors in college students. J Psychiatr Res. 2018;99:122–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicide risk: duration of sleep disturbance matters. Suicide Life Threat Behav. 2013;43:139–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ribeiro JD, Pease JL, Gutierrez PM, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord. 2012;136:743–50. [DOI] [PubMed] [Google Scholar]
- [18].Jia C-X, Zhang W-C, Wei L, et al. Sleep disturbance and attempted suicide in rural China. J Nerv Ment Dis. 2015;203:463–8. [DOI] [PubMed] [Google Scholar]
- [19].Gunnell D, Chang SS, Tsai MK, et al. Sleep and suicide: an analysis of a cohort of 394,000 Taiwanese adults. Soc Psychiatry Psychiatr Epidemiol. 1465;48:1457. [DOI] [PubMed] [Google Scholar]
- [20].Wang CW, Chan CL, Yip PS. Suicide rates in China from 2002 to 2011: an update. Soc Psychiatry Psychiatr Epidemiol. 2014;49:929–41. [DOI] [PubMed] [Google Scholar]
- [21].Wikepedia. Liuyang. 2017. Available at: https://en.wikipedia.org/wiki/Liuyang.
- [22].Lara-Munoz C, De Leon SP, Feinstein AR, et al. Comparison of three rating scales for measuring subjective phenomena in clinical research. I. Use of experimentally controlled auditory stimuli. Arch Med Res. 2004;35:43–8. [DOI] [PubMed] [Google Scholar]
- [23].Dimitriadis Z, Strimpakos N, Kapreli E, et al. Validity of visual analog scales for assessing psychological states in patients with chronic neck pain. J Musculoskelet Pain. 2014;22:242–6. [Google Scholar]
- [24].Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–36. [DOI] [PubMed] [Google Scholar]
- [25].Sleep quality in heroin addicts under methadone maintenance treatment. Acta Neuropsychiatrica. 2012;24:356–60. [DOI] [PubMed] [Google Scholar]
- [26].Madsen MT, Hansen MV, Andersen LT, et al. Effect of melatonin on sleep in the perioperative period after breast cancer surgery: a randomized, double-blind, placebo-controlled trial. J Clin Sleep Med. 2016;12:225–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hamza W. Percutaneous electrical nerve stimulation: a novel analgesic therapy for diabetic neuropathic pain. Diabetes Care. 2000;23:365–70. [DOI] [PubMed] [Google Scholar]
- [28].Zimmerman M. Symptom severity and guideline-based treatment recommendations for depressed patients: implications of DSM-5’s potential recommendation of the PHQ-9 as the measure of choice for depression severity. Psychother Psychosom. 2012;81:329–32. [DOI] [PubMed] [Google Scholar]
- [29].Wang W, Bian Q, Zhao Y, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. 2014;36:539–44. [DOI] [PubMed] [Google Scholar]
- [30].Monahan PO, Shacham E, Reece M, et al. Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in western Kenya. J Gen Intern Med. 2009;24:189–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 1292;41:1284. [DOI] [PubMed] [Google Scholar]
- [32].Chen S, Conwell Y, Vanorden K, et al. Prevalence and natural course of late-life depression in China primary care: a population based study from an urban community. J Affect Disord. 2012;141:86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Xu J, Xie Y, Li B, et al. The study of validity on self-rated health measurement scale-the revised version 1.0. Chinese J Clin Rehabil. 2002;6:2082–5. [Google Scholar]
- [34].Xu J, Wang B-H, Xu H, et al. Research on self-rated health measurement scale. Chinese J Clin Rehabil. 2004;8:8382–6. [Google Scholar]
- [35].Rubin R. Recent suicides highlight need to address depression. JAMA. 2014;312:1725–7. [DOI] [PubMed] [Google Scholar]
- [36].Harrington R. Depression, suicide and deliberate self-harm in adolescence. Br Med Bull. 2001;57:47–60. [DOI] [PubMed] [Google Scholar]
- [37].Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–28. [DOI] [PubMed] [Google Scholar]
- [38].de la Vega Sánchez D, Guillén E, Gordillo MJ, et al. Prevalence of mental disorders in 1519 suicides: a meta-analysis. Eur Psychiatry. 2016;33:S272. [Google Scholar]
- [39].Zhang J, Wieczorek WF, Conwell Y, et al. Psychological strains and youth suicide in rural China. Soc Sci Med. 2010;72:2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Mäki NE, Martikainen PT. The effects of education, social class and income on non-alcohol- and alcohol-associated suicide mortality: a register-based study of Finnish men aged 25–64. Eur J Popul. 2008;24:385–404. [Google Scholar]
- [41].Myles N, Large M, Myles H, et al. Australia’s economic transition, unemployment, suicide and mental health needs. Aust N Z J Psychiatry. 2017;51:119–23. [DOI] [PubMed] [Google Scholar]
- [42].Stack S. Gender, marriage, and suicide acceptability: a comparative analysis. Sex Roles. 1998;38:501–20. [Google Scholar]
- [43].Stack S, Wasserman I. The effect of marriage, family, and religious ties on African American suicide ideology. J Marriage Fam. 1995;57:215. [Google Scholar]
- [44].Kposowa AJ. Marital status and suicide in the national longitudinal mortality study. J Epidemiol Community Health. 2000;54:254–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Smith JC, Mercy JA, Conn JM. Marital status and the risk of suicide. Am J Public Health. 1988;78:78–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Geoffroy PA, Oquendo MA, Courtet P, et al. Sleep complaints are associated with increased suicide risk independently of psychiatric disorders: results from a national 3-year prospective study. Mol Psychiatry. 2136;26:2126. [DOI] [PubMed] [Google Scholar]
- [47].Pigeon WR, Bishop TM, Titus CE. The relationship between sleep disturbance, suicidal ideation, suicide attempts, and suicide among adults: a systematic review. Psychiatr Ann. 2016;46:177–86. [Google Scholar]
- [48].Bernert RA, Kim JS, Iwata NG, et al. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. 2015;17:554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Blake MJ, Allen NB. Prevention of internalizing disorders and suicide via adolescent sleep interventions. Curr Opin Psychol. 2020;34:37–42. [DOI] [PubMed] [Google Scholar]
- [50].Bernert RA, Iwata N, Kim J, et al. Perceived stigma toward mental health in association with sleep disturbances and as an acute predictor of suicidal symptoms. Sleep. 2015;38:A340. [Google Scholar]
- [51].McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Curr Psychiatry Rep. 2013;15:389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Kim JH, Ahn JH, Min CY, et al. Association between sleep quality and subjective cognitive decline: evidence from a community health survey. Sleep Med. 2021;83:123–31. [DOI] [PubMed] [Google Scholar]