Abstract
Annual influenza vaccination of health care students and workers helps protect themselves and patients from influenza, which has a high disease burden during seasonal peaks in Australia. Health care students are an important cohort whose early attitudes and habits towards influenza vaccination may influence future behaviours. We explored the knowledge, attitudes, and behaviours towards influenza vaccination of health care students in two universities from 2018 to 2020 using convergent mixed methodology. We also assessed the impact of two external events – the introduction of mandatory influenza vaccination for select students in 2019, and the COVID-19 pandemic in 2020. We found a significant increase in self-reported vaccination uptake between 2018 (73.5%) and 2020 (89.6%), with the mandate and COVID-19 pandemic being likely drivers of increased uptake. Vaccine mandates are effective but must be supported by easy accessibility, adequately addressing concerns around effectiveness and safety, and promotion of voluntary acceptance and trust.
Keywords: Vaccination, Mandates, Influenza, Respiratory virus, Health care workers, Students
1. Introduction
Influenza is an infectious seasonal viral respiratory illness that causes significant disease burden in Australia. [1], [2] Annual vaccination remains the mainstay of reducing infection[3] and well-matched vaccination in healthy adults and children can reduce infection risk by 50–60 %.[4].
Health care workers (HCW), including students, are recommended to receive annual influenza vaccination to protect both themselves and their patients, who may be at higher risk of severe disease. [5] Health care students’ attitudes and habits towards influenza vaccination may influence future behaviours and HCW influenza vaccination uptake.
Influenza vaccination uptake among health care students at the University of Notre Dame Australia, Fremantle Campus (UNDA) was suboptimal in 2014 at 55.9 % (95 % confidence interval [CI95] 52.2–59.6 %).[6] In 2020, independent of the COVID-19 pandemic, Western Australia (WA) strengthened its recommendation of influenza vaccines to HCW, requiring all staff to declare their influenza vaccination status via an annual electronic form. [7], [8] Although this policy includes health care students, implementation is the responsibility of their university and policies vary between and within institutions.
We explored the knowledge, attitudes, and behaviours towards influenza vaccination of health care students at UNDA and Murdoch University (MU) from 2018 to 2020, to inform interventions to increase influenza vaccination uptake. Influenza vaccination was recommended for health care students in both universities during the study period, with a notable addition of influenza vaccination being mandated for UNDA medical students from April 2019. [9] Promotional activities were developed and implemented in 2019 and 2020 by the study team, based on data collected in 2018 and 2019. In addition, the study provided a unique opportunity to assess the impact of significant external events; first, the introduction of mandatory influenza vaccination for UNDA medical students in 2019, and second, the COVID-19 pandemic in 2020.
2. Methods
We used a mixed methods convergent parallel design[10] to a) assess influenza vaccination uptake; and b) explore attitudes, barriers, and enablers to influenza vaccination; in health care students aged ≥ 18 years at UNDA and MU, from 2018 to 2020. Quantitative data collection comprised cross-sectional anonymous online surveys (2018, 2019, and 2020) (Supplementary material), while qualitative data collection comprised semi-structured telephone interviews (December 2019 and November 2020). Annual survey data were collected from late August to early September after WA’s May to July influenza vaccination season. Surveys were promoted via the student learning management system, while interview participants were self-selected via an invitation in the online survey.
We analysed quantitative data using R (Version 4.0.3, R Core Team, Austria). Proportions between subgroups were compared using Pearson chi-squared tests. We undertook a subgroup analysis of participants from UNDA School of Medicine and School of Nursing and Midwifery (hereafter referred to as Nursing) (≥40 responses in each year). We assessed univariate predictors of vaccination using chi-squared test (proportionally weighted by course), including variables with p < 0.25 in the weighted multivariable logistic regression model. Qualitative data from interview transcripts were analysed manually to identify emergent themes using the Braun & Clark six step process. [11].
Findings from 2018 and 2019 informed an influenza vaccine promotion strategy implemented in 2020 prior to the vaccination period. This comprised virtual promotional flyers and posters disseminated by students to their peers via social media.
We obtained ethical approval from the UNDA Human Research Ethics Committee (Reference 018061F) and reciprocal MU ethical approval.
3. Results
3.1. Study population
There were 949 health care student responses to the online surveys (Table 1 ). Response rates varied from 0 % to 20 % of students enrolled in each course/year. The subgroup analysis included survey data from 693 participants (73 % of total) enrolled in UNDA School of Medicine (n = 272) and Nursing (n = 421). Sixteen telephone interviews were conducted: ten in 2019 and six in 2020.
Table 1.
Demographic characteristics of health care student survey respondents.
| 2018 (N = 230) | 2019 (N = 344) | 2020 (N = 375) | TOTAL (N = 949) | ||
|---|---|---|---|---|---|
| Age | 18–24 years | 142 (62 %) | 217 (63 %) | 207 (55.2 %) | 566 (59.6 %) |
| 25–29 years | 55 (24 %) | 61 (18 %) | 60 (16.0 %) | 176 (18.5 %) | |
| 30–34 years | 17 (7 %) | 24 (7 %) | 47 (12.5 %) | 88 (9.3 %) | |
| 35 years and over | 16 (7 %) | 42 (12 %) | 61 (16.3 %) | 119 (12.5 %) | |
| Gender | Male | 44 (19 %) | 56 (16 %) | 60 (16.0 %) | 160 (16.9 %) |
| Female | 186 (81 %) | 288 (84 %) | 313 (83.5 %) | 787 (82.9 %) | |
| Unspecified | 0 (0 %) | 0 (0 %) | 2 (0.5 %) | 2 (0.2 %) | |
| Course | Medicine (UNDA)* | 107 (47 %) | 73 (21 %) | 92 (24.5 %) | 272 (28.7 %) |
| Nursing and Midwifery (UNDA)* | 91 (40 %) | 217 (63 %) | 113 (30.1 %) | 421 (44.4 %) | |
| Physiotherapy (UNDA)* | 0 (0 %) | 21 (6 %) | 18 (4.8 %) | 39 (4.1 %) | |
| Chiropractic (MU)† | 32 (14 %) | 19 (6 %) | 27 (7.2 %) | 78 (8.2 %) | |
| Counselling (MU)† | 0 (0 %) | 14 (4 %) | 19 (5.1 %) | 33 (3.5 %) | |
| Nursing (MU)† | 0 (0 %) | 0 (0 %) | 106 (28.3 %) | 106 (11.2 %) | |
| Course year | First | 79 (34 %) | 90 (26 %) | 147 (39.2 %) | 316 (33.3 %) |
| Second | 67 (29 %) | 114 (33 %) | 105 (28.0 %) | 286 (30.1 %) | |
| Third | 55 (24 %) | 107 (31 %) | 81 (21.6 %) | 243 (25.6 %) | |
| Fourth | 26 (11 %) | 28 (8 %) | 35 (9.3 %) | 89 (9.4 %) | |
| Other | 3 (1 %) | 5 (1 %) | 7 (1.9 %) | 15 (1.6 %) | |
| Eligible for NIP funded vaccine | No | 189 (82 %) | 268 (78 %) | 181 (48.3 %) | 638 (67.2 %) |
| Yes | 28 (12 %) | 52 (15 %) | 194 (51.7 %) | 274 (28.9 %) | |
| Unsure | 13 (6 %) | 19 (6 %) | 0 (0.0 %) | 32 (3.4 %) | |
| Current HCW | No | 118 (51 %) | 191 (56 %) | 250 (66.7 %) | 559 (58.9 %) |
| Yes | 44 (19 %) | 141 (41 %) | 125 (33.3 %) | 310 (32.7 %) | |
| No response | 68 (30 %) | 12 (3 %) | 0 (0.0 %) | 80 (8.4 %) | |
| Previous HCW | No | 50 (22 %) | 90 (26 %) | 164 (43.7 %) | 304 (32.0 %) |
| Yes | 112 (49 %) | 242 (70 %) | 211 (56.3 %) | 565 (59.5 %) | |
| No response | 68 (30 %) | 12 (3 %) | 0 (0.0 %) | 80 (8.4 %) |
University of Notre Dame Australia, Fremantle campus.
Murdoch University.
Almost three-quarters (73.1 %) of respondents were from UNDA Medicine and Nursing courses (28.7 % and 44.4 % respectively), in their first or second year of study (33.3 % and 30.1 % respectively), and 82.9 % were female (Table 1).
3.2. Self-reported influenza vaccination uptake
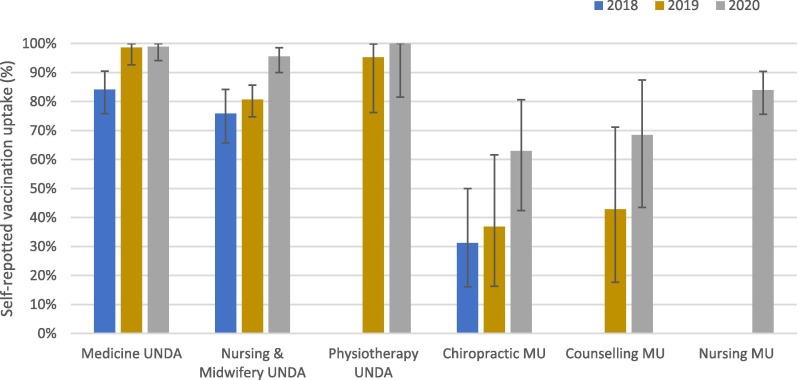
Overall, self-reported influenza vaccination uptake increased over the three years, from 73.5 % in 2018 (CI95 67.4–78.8 %), to 89.6 % in 2020 (CI95 86.1–92.2 %) (χ2 = 26.58, p < 0.001). However, there were significant differences between courses (χ2 = 124.57, p < 0.001), with UNDA Physiotherapy and Medicine reporting highest overall uptake at 97.4 % (CI95 86.8–99.5 %) and 93.0 % (CI95 89.3–95.5 %), respectively. MU Chiropractic (43.6 %, CI95 33.1–54.6 %) and Counselling (57.6 %, CI95 40.8–72.8 %), students reported the lowest uptake (Fig. 1 ). Due to the non-random sampling and low response rate for each course and year, differences between groups should be interpreted with caution.
Fig. 1.
Self-reported influenza vaccination uptake by course, 2018–2020. UNDA- University of Notre Dame Australia, Fremantle campus. MU- Murdoch University.
The subgroup analysis showed a significant and sustained increase in self-reported vaccination uptake among UNDA medical students after mandatory vaccination was introduced in April 2019 (84.1 % in 2018 [CI95 75.8–90.5 %]; 98.6 % in 2019 [CI95 92.6–100 %] and 98.9 % in 2020 [CI95 94.1–100 %]) (Fig. 1). Among UNDA nursing students, uptake was stable in 2018 and 2019 (75.8 % in 2018 [CI95 65.7–84.2 %] and 80.6 % in 2019 [CI95 74.8–85.7 %], p = 0.34), and increased significantly between 2019 and 2020 to 95.6 % (CI95 90.0–98.5 %, p < 0.001) (Fig. 1).
3.3. Enablers and barriers to influenza vaccination
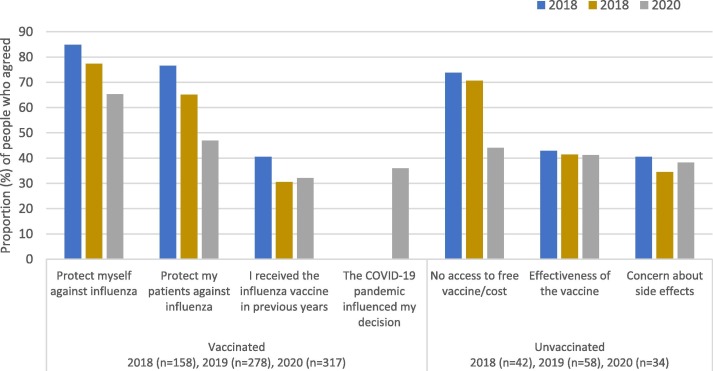
Across all three years, 753 vaccinated students provided at least one reason why they were vaccinated. Reasons included the desire to protect themselves (556/753; 73.8 %), the desire to protect their patients (451/753; 59.9 %), previous receipt of vaccine (251/753; 33.3 %) and access to free influenza vaccination (249/753; 33.0 %) (Fig. 2 ). In 2020, 114/317 (35.9 %) of vaccinated respondents indicated that the COVID-19 pandemic influenced their vaccination decision. Specific reasons included wanting to minimise additional pressure on the health-care system and concerns about co-infection of influenza with COVID-19.
Fig. 2.
Top three influential factors underlying the decision to be vaccinated or not vaccinated, all courses, 2018–2020 (additional question about COVID-19 included for vaccinated students in 2020).
Across all three years, 151 unvaccinated students gave at least one reason why they were not vaccinated. No access to free vaccines (n = 44) and cost (n = 43) were the most cited factors (combined total 87/151; 57.6 %). Additionally, concern about perceived poor effectiveness of the vaccine (55/151; 36.4 %), and side effects (50/151; 33.1 %) were commonly cited reasons for being unvaccinated (Fig. 2).
3.4. Predictors of vaccination status amongst UNDA medical and nursing students
Within the subgroup analysis, year of survey was the strongest independent predictor of vaccination status, with those surveyed in 2020 six times more likely to be vaccinated than those surveyed in 2018 (aOR = 6.35, CI95 2.78–16.32) (Table 2 ). Eligibility for National Immunisation Program (NIP)-funded (free) vaccine, being a medical student, and being a first-year student were also independent predictors of vaccination; all these factors remained independent predictors of vaccination in the multivariable analysis (Table 2).
Table 2.
Predictors of vaccination status, UNDA medical and nursing and midwifery students, 2018–2020.
| Total | Vaccinated Number (%) | Unvaccinated Number (%) | Weighted Univariable analysis†p-value | Weighted multivariable analysis‡aOR | ||
|---|---|---|---|---|---|---|
| Year | 2018 | 198 | 159 (80.3 %) | 39 (19.7 %) | <0.001 | ref |
| 2019 | 290 | 247 (85.2 %) | 43 (14.8 %) |
2.18 (1.30–3.68) |
||
| 2020 | 205 | 199 (97.1 %) | 6 (2.9 %) |
6.35 (2.78–16.32) |
||
| Gender | Male | 119 | 112 (94.1 %) | 7 (5.9 %) | 0.07 | – |
| Female | 573 | 492 (85.9 %) | 81 (14.1 %) | – | ||
| Unspecified | 1* | 1 (100 %) | 0 (0 %) | – | ||
| Course | Medicine (UNDA) | 272 | 253 (93.0 %) | 19 (7.0 %) | <0.01 | 3.48 (1.72–7.68) |
| Nursing and Midwifery (UNDA) | 421 | 352 (83.6 %) | 69 (16.4 %) | ref | ||
| Course year | First | 233 | 223 (95.7 %) | 10 (4.3 %) | <0.001 | ref |
| Second | 205 | 166 (81.0 %) | 39 (19.0 %) |
0.10 (0.04–0.22) |
||
| Third | 193 | 159 (82.4 %) | 34 (17.6 %) |
0.09 (0.03–0.20) |
||
| Fourth | 61 | 56 (91.8 %) | 5 (8.2 %) |
0.10 (0.02–0.45) |
||
| 4+ | 1* | 1 (100 %) | 0 (0 %) | – | ||
| Eligible for NIP funded vaccine | No | 498 | 426 (85.5 %) | 72 (14.5 %) | <0.01 | ref |
| Yes | 171 | 160 (93.6 %) | 11 (6.4 %) |
2.10 (1.09–4.38) |
||
| Unsure | 22* | 17 (77.3 %) | 5 (22.7 %) | – | ||
| Current HCW | No | 407 | 378 (92.9 %) | 29 (7.1 %) | 0.64 | – |
| Yes | 232 | 213 (91.8 %) | 19 (8.2 %) | – | ||
| No response | 54* | 40 (74.1 %) | 14 (25.9 %) | – | ||
| Previous HCW | No | 201 | 183 (91.0 %) | 18 (9.0 %) | 0.47 | – |
| Yes | 438 | 408 (93.2 %) | 30 (6.8 %) | – | ||
| No response | 54* | 40 (74.1 %) | 14 (25.9 %) | – |
excluded from Chi-squared test and multivariable analysis.
Weighted Pearson's Chi-squared test.
Year of survey (considered a proxy measure for policy change), gender, course, course year, and eligibility to receive a vaccine included in the final model.
3.5. Qualitative findings
All interview participants reported being vaccinated against influenza in the year they were interviewed. Similar themes were identified across both years, the exception being the influence of the COVID-19 pandemic in 2020. All participants demonstrated a sound understanding of the purpose of influenza vaccination with a consistent theme of protection from influenza infection and prevention of transmission to others being key drivers.
‘Also, it can help reduce transmission, I believe as well, because if you can’t contract that flu, you're less likely to pass it on’ (2020 P2)
‘It’s to protect the rest of the population and it's not only to protect yourself, it's to protect the herd. So you’re looking after every-one else that is vulnerable’ (2020 P6).
Students were aware of having seen promotional material. Most participants expressed a need to seek credible and trustworthy sources of information, including government websites, personal GPs, travel health clinics and the university. Trustworthy messaging was Identified as a potential enabler for vaccination, specifically focusing on benefits, risks, and the professional responsibility of getting vaccinated, and delivered via individual lecturers, peer to peer advocacy, and social media campaigns. Participants reported that free access to vaccine on-campus would also be effective in increasing uptake.
Perceived barriers to vaccination were cost, inconvenience of access, misinformation about the vaccine causing influenza, not considering themselves at risk, and concern about side effects. The majority of participants were aware of social peers being resistant to influenza vaccination and also being subject to misinformation about influenza and influenza vaccination.
‘I know that others are concerned about getting the flu from the vaccination…how vaccinations are actually created… people don’t understand… they are very scared about formaldehyde in vaccinations’ (2019 P7).
The COVID-19 pandemic was recognised as influential in 2020, with some participants reporting that they were more likely to get vaccinated. However, others expressed that they would have received the vaccination regardless of the pandemic.
Neither the survey nor interview respondents reported any negative attitudes about the mandatory policy for medical students.
4. Discussion
Influenza vaccination of health care students not only reduces the likelihood of illness in students and transmission of influenza to patients and other staff, [12] but is potentially an important factor in early establishment of professional expectations of vaccination against vaccine-preventable disease. Influenza vaccination uptake among health care students at UNDA was found to be suboptimal in 2014 (55.9 %). We found uptake had increased to 73.5 % in health care students across UNDA and MU in 2018, possibly due to increased promotion and the introduction of on-campus vaccination in 2018. Further significant improvements were seen across the three study years from 2018 to 2020, with 89.6 % of students self-reporting influenza vaccination in 2020. UNDA students overall reported higher rates of vaccination compared to MU students, however low sample size of MU students limits the generalisability of these results.
External events, including a severe 2019 influenza season and the COVID-19 pandemic in 2020 are likely to have contributed to the observed increase in uptake. This finding is consistent with an Australia-wide increase in influenza vaccination uptake in 2020. [13] However, the most notable increase in influenza vaccination (an increase in uptake from 78.8 % in 2018 to 98.6 % in 2019 in UNDA medical students) was observed after vaccination was mandated for these students in April 2019. The lack of a similar increase across UNDA nursing students over the same period suggests the mandate was the most important contributor to the observed increase. This is consistent with other studies that identify the positive influence of mandatory influenza vaccination policy on vaccination rates in healthcare workers. [14], [15], [16] Overall, attitudes towards influenza vaccination were positive, with key drivers for vaccination being a desire to protect themselves and others. Key barriers identified were concerns regarding poor effectiveness, potential side effects, and cost, which is consistent with barriers identified in other studies of health care students and workers. [17], [18], [19].
Access, availability and free vaccination were identified as enabling factors promoting vaccination in the qualitative interviews, while eligibility for a free vaccination was also found to be an independent predictor of vaccination. This is consistent with existing literature which highlights the importance of free vaccination across health care settings to support vaccination uptake. [15], [20] Our qualitative findings also highlight the importance of promotion through both commonly used social media and trusted sources such as lecturers and peers. This is consistent with previous studies that have identified the benefit of multiple strategies to promote vaccination uptake, although mandatory vaccination remains the most influential factor for sustained high vaccination rates. [14] These complementary activities are still important even in the context of mandates to prevent feelings of coercion and minimise negative impacts of mandates in communities. Recent studies regarding COVID-19 vaccine mandates also support this, suggesting that there should be a strong justification, accompanied by supportive measures facilitating ease of access and preceded by less restrictive measures, to build trust and promote voluntary acceptance of vaccination. [21].
Limitations of our study include potential sampling bias due to the voluntary nature of the online survey and qualitative interviews, highlighted by the fact that all interviewed participants were vaccinated. However, the convergent methodology strengthened findings by facilitating further qualitative exploration and validation of themes that arose in the quantitative surveys. Conducting the survey across several years also allowed identification of potential influencing factors on vaccine uptake external to the initial research design, such as the implementation of the mandatory vaccination policy for medical students at UNDA, and the COVID-19 pandemic.
5. Conclusion
We found a significant increase in self-reported uptake of influenza vaccination in health care students between 2018 and 2020, with introduction of a mandatory requirement for medical students, the COVID-19 pandemic, and a severe 2019 influenza season being likely drivers of the improvements. While vaccine mandates are an effective strategy, this study indicates mandates can be strengthened by being part of a multi-faceted approach which supports accessibility, adequately addresses concerns around effectiveness and safety, and promotes voluntary acceptance and trust.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Gervase Chaney was the Dean of the School of Medicine, University of Notre Dame Australia, Fremantle Campus, when the mandatory influenza vaccination requirement was introduced for medical students. He was not involved in the data analysis or primary interpretation of the results. With this exception, all authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was partly funded through The University of Notre Dame’s Research Grant Funding Scheme. The authors would like to thank Professor David Macey and Mr Paul Knight for their valuable contribution to the study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.08.040.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
Data availability
The authors do not have permission to share data.
References
- 1.Gavin K., Owen R., Barr I.G. Annual report of the National Influenza Surveillance Scheme, 2010. Communicable diseases intelligence quarterly report. 2017;41(4):E348–E368. [PubMed] [Google Scholar]
- 2.Australia Government Department of Health. 2017 Influenza Season in Australia: A summary from the National Influenza Surveillance Committee. https://www1.health.gov.au/internet/main/publishing.nsf/Content/ozflu-surveil-2017-final.htm#current. Published 2017. Accessed 9 Feb 2022.
- 3.World Health Organization. Vaccines against influenza: WHO position paper – May 2022. Weekly epidemiological record. 2022; 97: 185-208 https://apps.who.int/iris/bitstream/handle/10665/354. Accessed 21 Aug 2022.
- 4.Osterholm M.T., Kelley N.S., Sommer A., Belongia E.A. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(1):36–44. doi: 10.1016/S1473-3099(11)70295-X. [DOI] [PubMed] [Google Scholar]
- 5.The Australian Immunisation Handbook, 10th Edition. Canberra: National Health and Medical Research Council, Australian Government Department of Health and Ageing; 2013.
- 6.Nyandoro M.G., Kelly D.A., Macey D.J., Mak D.B. Student-centered interventions the key to student health care worker influenza vaccination. Infection, Disease, Health. 2016;21(3):108–115. [Google Scholar]
- 7.Government of Western Australia Department of Health. Health care worker immunisation policy. https://ww2.health.wa.gov.au/~/media/Files/Corporate/Policy-Frameworks/Public-Health/Policy/Health-Care-Worker-Immunisation-Policy/OD388-Health-Care-Worker-Immunisation-Policy.pdf. Published 2012. Accessed 9 February 2022.
- 8.Government of Western Australia Department of Health. Staff Member Influenza Vaccination Program Policy. https://ww2.health.wa.gov.au/~/media/Files/Corporate/Policy-Frameworks/Public-Health/Policy/Staff-Member-Influenza-Vaccination-Program-Policy/Staff-Member-Influenza-Vaccination-Program-Policy.pdf. Published 2020. Accessed 10 June 2022.
- 9.Yin J.K., Salkeld G., Lambert S.B., Dierig A., Heron L., Leask J., et al. Estimates and determinants of economic impacts from influenza-like illnesses caused by respiratory viruses in Australian children attending childcare: a cohort study. Influenza Other Respir Viruses. 2013;7(6):1103–1112. doi: 10.1111/irv.12138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Creswel JW. Research Design: Quantitative, Qualitative and mixed methods approaches. Lincoln, Nebraska, USA: Sage Publications; 2014.
- 11.Braun V., Clarke V. Can I use TA? Should I use TA? Should I not use TA? Comparing reflexive thematic analysis and other pattern-based qualitative analytic approaches. Counselling Psychotherapy Res. 2021;21(1):37–47. [Google Scholar]
- 12.Sydnor E., Perl T.M. Healthcare providers as sources of vaccine-preventable diseases. Vaccine. 2014;32(38):4814–4822. doi: 10.1016/j.vaccine.2014.03.097. [DOI] [PubMed] [Google Scholar]
- 13.Beard F., Hendry A., Macartney K. Influenza vaccination uptake in Australia in 2020: impact of the COVID-19 pandemic? Commun Dis Intell. 2018;2021:45. doi: 10.33321/cdi.2021.45.10. [DOI] [PubMed] [Google Scholar]
- 14.Schmid K., Merkl K., Hiddemann-Koca K., Drexler H. Obligatory occupational health check increases vaccination rates among medical students. J Hosp Infect. 2008;70(1):71–75. doi: 10.1016/j.jhin.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 15.Hollmeyer H., Hayden F., Mounts A., Buchholz U. Review: interventions to increase influenza vaccination among healthcare workers in hospitals. Influenza Other Respir Viruses. 2013;7(4):604–621. doi: 10.1111/irv.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kitt E., Burt S., Price S.M., et al. Implemtation of a mandatory influenza vaccination policy: A 10-year experience. Clin Infect Dis. 2021;73(2):290–296. doi: 10.1093/cid/ciaa782. [DOI] [PubMed] [Google Scholar]
- 17.Kunze U., Schweinzer H. Self-reported vaccination status and attitudes towards mandatory vaccinations for health care workers among medical students. Vaccine. 2020;38(35):5695–5699. doi: 10.1016/j.vaccine.2020.06.046. [DOI] [PubMed] [Google Scholar]
- 18.Corace K., Prematunge C., McCarthy A., Nair R.C., Roth V., Hayes T., et al. Predicting influenza vaccination uptake among health care workers: What are the key motivators? Am J Infect Control. 2013;41(8):679–684. doi: 10.1016/j.ajic.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 19.Walker L., Newall A., Heywood A.E. Knowledge, attitudes and practices of Australian medical students towards influenza vaccination. Vaccine. 2016;34(50):6193–6199. doi: 10.1016/j.vaccine.2016.10.074. [DOI] [PubMed] [Google Scholar]
- 20.Saro-Buendía M., Marrero-Sánchez Á., García-Ruiz de Morales D., Chiara-Graciani G., Coderch-Carretero J., Pérez-Jacoiste Asín M.A., et al. Implementation of a program to improve influenza vaccination rates among medical students: a comparative study involving two university affiliated hospitals. Human Vaccines Immunotherap. 2021;17(10):3662–3669. doi: 10.1080/21645515.2021.1920269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leask J., Seale H., Williams J.H., Kaufman J., Wiley K., Mahimbo A., et al. Policy considerations for mandatory COVID-19 vaccination from the Collaboration on Social Science and Immunisation. Med J Aust. 2021;215(11):499–503. doi: 10.5694/mja2.51269. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors do not have permission to share data.