Abstract
Objective
To count and describe the elements that overlap (ie, present in two or more) and diverge between models and frameworks of patient engagement in health services research. Our specific research question was ‘what are the elements that underlie models and frameworks of patient engagement in health services research?’
Design
Scoping review.
Data sources
On 6–7 July 2021, we searched six electronic databases (ie, CINAHL, Cochrane Database of Systematic Reviews, Joanna Briggs Institute Evidence Based Practice Database, MEDLINE, PsycINFO and Scopus) and Google Scholar for published literature, and ProQuest Dissertations & Theses, Conference Proceedings Citation Index, Google, and key agencies’ websites for unpublished (ie, grey) literature, with no date restrictions. These searches were supplemented by snowball sampling.
Eligibility criteria
We included published and unpublished literature that presented (a) models or frameworks (b) of patient engagement (c) in health services research. We excluded articles unavailable as full text or not written in English.
Data extraction and synthesis
Two independent reviewers extracted data from included articles using an a priori developed standardised form. Data were synthesised using both quantitative (ie, counts) and qualitative (ie, mapping) analyses.
Results
We identified a total of 8069 articles and ultimately included 14 models and frameworks in the review. These models and frameworks were comprised of 18 overlapping and 57 diverging elements, that were organised into six conceptual categories (ie, principles, foundational components, contexts, actions, levels and outcomes) and spanned intrapersonal, interpersonal, process, environmental, and health systems and outcomes domains.
Conclusions
There is little overlap between the elements that comprise existing models and frameworks of patient engagement in health services research. Those seeking to apply these models and frameworks should consider the ‘fit’ of each element, by conceptual category and domain, within the context of their study.
Keywords: statistics & research methods, health services administration & management, medical education & training
Strengths and limitations of this study.
The study’s methodological strengths include use of a published protocol and the analysis approach, which supported mapping model and framework elements to generate a toolbox of options for researchers to use in their own patient-engaged research.
Another strength is the involvement of an interdisciplinary research team comprised of content experts, including patient coresearchers.
A weakness of this study concerns the grey boundaries between health services research and other forms of health research.
Greater engagement of patient coresearchers would have likely resulted in other study insights through more direct contact with the study.
Introduction
Patient engagement in research involves the formation of meaningful and active collaborations between academic researchers and patients (ie, an overarching term that refers to individuals with personal experience of a health issue and informal caregivers) in research governance, priority setting, conduct and knowledge translation.1 Globally, it is also commonly referred to as patient and public involvement, patient involvement, consumer and community involvement, and stakeholder engagement in research. This research approach necessitates a shift from the patient’s traditional role as a study participant to that of a research collaborator or partner (ie, patient coresearcher). This shift in roles and power dynamics reflects the approach’s roots in participatory research2 and is founded on the premises that those affected by a problem should be actively involved in the generation of solutions to it3 and individuals’ critical reflections on first-hand experiences are essential to effecting individual and social change.4 A growing body of evidence supports the benefits of patient engagement in research, including improved enrolment and decreased attrition rates,5 increased relevance of research and accessibility of study materials to study participants,6 improved trial design7 and increased meaningfulness and understandability of disseminated findings.5 6 However, despite its underlying rationale and documented benefits, academic researchers report hesitance in adopting this research approach.8 9
Some of the reported challenges of patient engagement in research include uncertainty about the process (ie, ‘how to’ engage patients in research) and the need for a culture shift that supports these collaborations.8 9 As there is no standard process for engaging patients in research, this first challenge is not surprising.5 6 10 That is, how patient engagement is operationalised may vary according to the characteristics of a given project (eg, design, scope, time and financial resources) and patient and academic coresearchers (eg, personal and professional backgrounds, interests, skills). Further, the underlying cultural shift needed to support patient engagement in research necessitates the redistribution of power and restructuring of traditional research paradigms to support shared planning and decision-making throughout a study.10 This requires a mutual understanding and vision for what these research collaborations entail. An exploration of the models and frameworks that underlie patient engagement in research may help clarify the processes and support the culture shift necessary for this approach by shedding light on the universal elements that underlie it.
Three previous reviews have broadly synthesised the literature on models, frameworks and/or other systematic approaches to the engagement of patients (and in the case of Jull et al—other knowledge users) in research.11–13 Of these, only one described the elements that comprised identified frameworks and guidelines describing best practices for engaging patients in research.12 Perhaps more importantly, none of these reviews focused on health services research, which entails considerations unique to health research. Specifically, health services research focuses on the impact of social factors, financing systems, organisational structures and processes, health technologies, and personal behaviours on healthcare access, quality and cost, and population health and well-being.14 This differs substantially from general health research, whose goal is often to improve clinical outcomes, the effectiveness of a particular intervention, or uptake of research among patients with a specific condition. Engaging patients in health services research may require added considerations related to partnering with a more diverse group of patients with lived experience of different conditions, groups, interventions and/or interactions with the healthcare system. Therefore, we set out to contribute to the existing literature on patient engagement in research by conducting a knowledge synthesis of models and frameworks of patient engagement in health services research. Specifically, we undertook a scoping review, which is ‘a type of knowledge synthesis that addresses an exploratory research question aimed at mapping key concepts, types of evidence and gaps in research related to a defined area or field by systematically searching, selecting and synthesising existing knowledge’.15
Objectives
The research question driving our review was ‘what are the elements that underlie models and frameworks of patient engagement in health services research?’ Our primary objective was to count and describe the elements that overlap (ie, present in two or more models or frameworks) and diverge between identified models and frameworks. This objective intended to support a clearer understanding of similarities in thinking about patient engagement rather than to judge the relevance of elements or prescribe a ‘one-size-fits-all’ approach. Thus, rather than synthesising the identified elements, we chose to map them according to the categories developed by the original authors and the themes that arose among them, with the vision of presenting a ‘toolbox’ of potential approaches that researchers may choose from for their given research endeavour. Finally, the exploratory nature of our research question and our desire to identify and map key concepts that underlie patient engagement in research led us to adopt a scoping review methodology.16
Methods
Our scoping review’s design and conduct followed the methodological framework proposed by Arksey and O’Malley17 and enhanced by Levac et al.18 The protocol for this scoping review, including definitions of underlying key concepts, is published elsewhere.19 Reporting was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) extension for Scoping Review20 and the revised Guidance for Reporting Involvement of Patients and the Public short-form21 checklists.
Eligibility criteria
We included published and unpublished (ie, grey) literature that presented (1) models or frameworks (2) of patient engagement (3) in health services research. Both original and adapted models and frameworks were eligible as long as they were developed in or for health services research. Since patient engagement also encompasses participation in research governance,1 we included models and frameworks that conceptualised how patient engagement in research was embedded across the different levels of health services research centres. We excluded articles unavailable as full text due to the limited descriptive information they provide (eg, context, description of development, underlying elements) and not written in English due to feasibility-related considerations.
Information sources
The lead author (AMC) searched six electronic databases (ie, CINAHL, Cochrane Database of Systematic Reviews, Joanna Briggs Institute Evidence Based Practice Database, MEDLINE, PsycINFO and Scopus) and Google Scholar for published literature. Electronic databases (ie, ProQuest Dissertations & Theses and Conference Proceedings Citation Index), Google and the websites of key agencies (ie, Canadian Institutes of Health Research, INVOLVE, Patient-Centered Outcomes Research Institute) were searched for unpublished literature. These searches were supplemented by snowball sampling, which entailed backwards and forwards reference searches of included articles and contacting experts in patient engagement in research for recommendations about any potentially relevant models or frameworks.
Searches
The search strategy was codeveloped by an academic librarian (LD) and the lead author (AMC) and finalised through discussion with the rest of the research team. The search strategy used a combination of search terms related to our underlying concepts (ie, ‘models,’ ‘frameworks,’ ‘patient engagement’ and ‘health services research’) was adapted to the syntax used by each database, register and website, and used Boolean terms. The search strategies for all databases, registers and websites are found in online supplemental appendix 1. There were no restrictions on publication dates. Searches of the published and unpublished literature were conducted on 6 July 2021 and 7 July 2021, respectively, while backward and forward searches ended on 13 January 2022.
bmjopen-2022-063507supp001.pdf (54.8KB, pdf)
Selection
Search results for the six electronic databases and Google Scholar were imported into a reference management software (Endnote), and duplicate references were removed. Only the first 10 pages of Google Scholar results (n=100 citations) were imported as advised by an academic librarian (LD). One reviewer (AMC) conducted the level 1 (title) screening. The remaining relevant references were then imported into an online systematic review production and management software (Covidence; Veritas Health Innovation, Melbourne, Australia), where two reviewers (AMC and TH) independently conducted the level 2 (abstract) and level 3 (full text) screening. Potentially relevant literature identified through websites and snowball sampling was screened for inclusion by both reviewers (AMC and TH). A third reviewer (ASHS) helped resolve discrepancies at the close of level 2 and 3 screening, which predominantly dealt with whether identified literature focused on health services research.
Data charting process
A standardised data charting (ie, extraction) form was developed a priori in Microsoft Word by the study team (online supplemental appendix 2). Items were chosen that described the eligible models and frameworks, as well as provided context, including how and by whom the models/frameworks were developed. Two reviewers (AMC and TH) independently extracted information from the final set of included articles using the form. They met with the senior author (ASHS) to compare their data after extracting from an initial set of five and ten articles and on completion of data extraction. Any inconsistencies were resolved through discussion and ultimately referring back to the original article. Further, in two instances,22 23 the lead author (AMC) contacted the corresponding authors of included frameworks to obtain clarifying information. Consistent with methodological guidelines for scoping reviews, we did not appraise the methodological quality of included articles.15 16
bmjopen-2022-063507supp002.pdf (107.6KB, pdf)
Synthesis of results
Data were compiled into a single Microsoft Excel (2019) spreadsheet for synthesis, which included both quantitative (ie, counts) and qualitative (ie, mapping) analyses. In conducting the analyses, the lead author (AMC) first immersed herself in the included models and frameworks by thoroughly (and repeatedly) reading the associated literature and reviewing graphical representations (when available) along with element definitions. With increased familiarity, the lead author was able to combine and reframe (where appropriate) similar elements found in the original publications. For example, ‘improved quality health decisions’ and ‘improved patient decision-making’ were combined into the element ‘health decision-making’ based on similarities in the element names and descriptions provided by the original study authors. The revised elements were used to obtain counts of overlapping and diverging elements. During this process, it became evident that the elements were organised into similar over-arching conceptual categories by the original authors, and that they could also be located within multiple domains (table 1). These categories and domains were identified inductively during the synthesis exercise. As such, in our analysis, we mapped each element according to conceptual category and domain. The validity (ie, content and face) of the final set of elements was established through discussion with this study’s authors. Visual representations of the data (ie, concept maps) were created using Mind Manager 2020 software, V.20.1 (Corel Corp., Austin, Texas, USA). To support applicability, some elements within the concept maps contain clarifying examples in brackets.
Table 1.
Explanation of over-arching conceptual categories and domains
| Over-arching conceptual category | Explanation |
| Principles | Values that orient and rule the conduct of a group. |
| Foundational components | Core elements that comprise patient engagement. |
| Contexts | Resources or decisions that are external to but inform the engagement process. |
| Actions | Activities (eg, behaviours, phases, advisory bodies) involved in the actual conduct of engagement and associated research. |
| Outcomes | Results of engagement and its associated research. |
| Organisational levels | Different organisational levels at which engagement may occur in a research organisation. |
| Domain | Elements pertain to… |
| Intrapersonal | Individual-level knowledge, perceptions, attitudes and beliefs. |
| Interpersonal | Relationships with other people. |
| Process | Carrying out the engagement or broader research. |
| Environmental | Research or organisational policies, cultures, perceptions. |
| Health systems and outcomes |
Health systems and health outcomes. |
Patient and public involvement
We engaged two patient coresearchers (RS and SH), at the level of ‘involve’,24 in the design and conduct of this study. The patient coresearchers and lead author (AMC) arrived at this mutual decision at the study’s outset, during the development of a term of reference that guided the study’s engagement process. By ‘involve’ we mean that the lead author worked consistently with patient coresearchers to ensure that their ideas and perspectives were understood and considered at study milestones. Specifically, patient coresearchers contributed to developing and publishing the scoping review protocol,19 provided feedback on the analyses (including element groupings), provided their perspectives on the interpretation of the study findings and co-authored this manuscript. In helping shape these stages of the research cycle and related outputs, a notable impact of engagement also included identifying gaps in the current literature relevant to patient partners. The primary methods of engagement were one-on-one and small group meetings, as guided by a terms of reference codeveloped at the outset of the research partnership. The patient coresearchers will continue to be involved in further knowledge translation activities, such as synthesising the findings for our research group’s website (www.patientengagementinresearch.ca), copresenting about the engagement process and study findings, and identifying other appropriate methods of dissemination.
Results
Flow of models and frameworks into the study
Online supplemental appendix 3 displays the flow of eligible articles into the review (PRISMA flow chart). Of the 10 840 initially identified citations, 2771 duplicates were excluded. After applying inclusion criteria, 7150 articles were excluded at the title screen, 712 at the abstract screen and 194 at the full-text screen, leaving 13 models and frameworks. One unpublished framework was then identified through snowball sampling, resulting in a total of 14 models and frameworks included in the review.
bmjopen-2022-063507supp003.pdf (60.3KB, pdf)
Characteristics of included articles and models/frameworks
Select descriptive characteristics of the included models and frameworks and the articles they were published in (where applicable) are presented in online supplemental appendix 4. Included articles were published between 2012 and 2020 (n=10 were published in or after 2015) and based in the USA (n=5), the UK (n=5), Canada (n=2), and Australia (n=1). The included unpublished framework was developed in Canada as part of the The CONtiNuity of carE and serviCes for autistiC adulTs (CONNECT) project (Caroline Jose, Patricia George-Zwicker, Louise Tardif, Aaron Bouma, Darlene Pugsley, Luke Pugsley, Mathieu Bélanger, Jeffrey Gaudet, Marc Robichaud, CONNECT framework). Models and frameworks were developed in a variety of contexts including organisations (ie, Patient-Centered Outcomes Research Institute, British Columbia Support Unit, Sunnybrook Hospital, PRIME Centre Wales), medical specialties (ie, paediatric subspecialty care, palliative care), research disciplines (ie, healthcare operations research), diseases (ie, chronic or long-term conditions; cancer; dementia; stroke) and other health conditions (eg, autistic adults, persons with lived experience of long-term physical and/or mental health illness, parents of children with disabilities). They were developed for general use as well as in specific health services research contexts such as healthcare operational research, practice-based research and innovation, pragmatic trials, patient-centred outcomes research and comparative effectiveness research. None targeted a specific component of the research process, and patients were involved in the development of slightly over half (n=8) of the included models/frameworks. Eight of the models/frameworks took into account the public participation spectrum24 either explicitly or by including considerations related to control of decision-making and/or directionality of information exchange.
bmjopen-2022-063507supp004.pdf (73.6KB, pdf)
Overview of the elements of included models and frameworks
A total of 112 elements of patient engagement were identified across the 14 included models and frameworks. Combining and reframing similar elements reduced the total number to 75. Among these, 18 elements overlapped across the included models and frameworks and 57 diverged (ie, were unique to individual models and frameworks). We present the elements by conceptual category and identify the domains they are situated in below. In considering these results, it should be noted that we placed select elements from the models by Deverka et al25 (ie, inputs, methods, outputs) and Evans et al26 (ie, opportunities for engagement, research environment that actively supports engagement and its underlying principles, resources to support engagement, and system to enhance the breadth of patient and carer experience brought to research activities) in the ‘actions’ conceptual category despite that not being what the original authors labelled them. This is due to the fact that although these elements were uncategorized by Deverka et al25 they closely aligned with the actions category, and Evans et al’s definition of the conceptual category that encompassed these elements closely aligned with other authors’ conceptualization of ‘actions’.
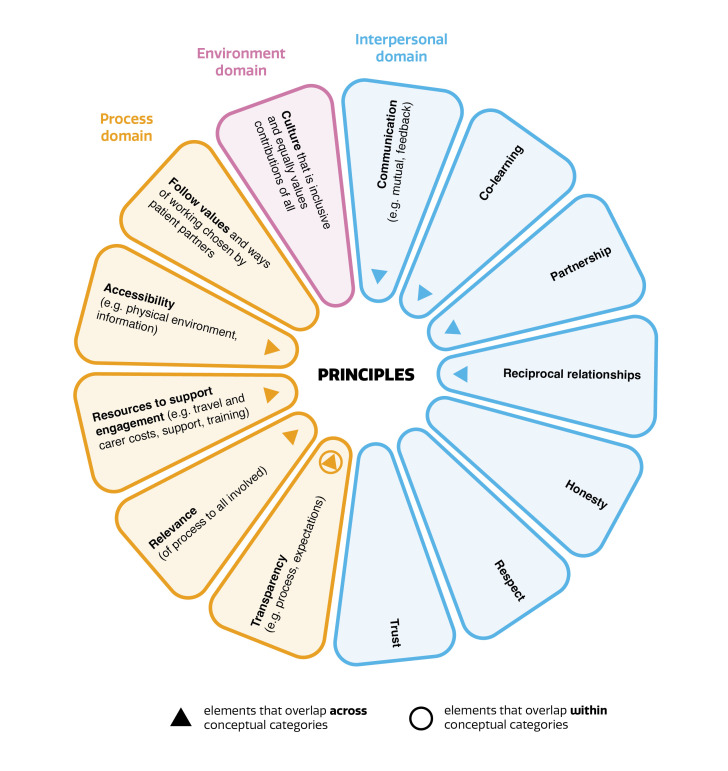
Principles
Principles represent the values that orient and rule the conduct of a group. They form the ethical backdrop of engagement27 and underpin effective collaborative involvement in research.26 For example, communication, which included mutual communication and feedback, was identified as a core principle of patient engagement by Evans et al.26 Figure 1 displays the 13 elements in this conceptual category, as reported by two articles.26 27 These elements were situated in interpersonal (n=7), process (n=5) and environmental (n=1) domains.
Figure 1.
Concept map—principles of patient engagement in health services research.
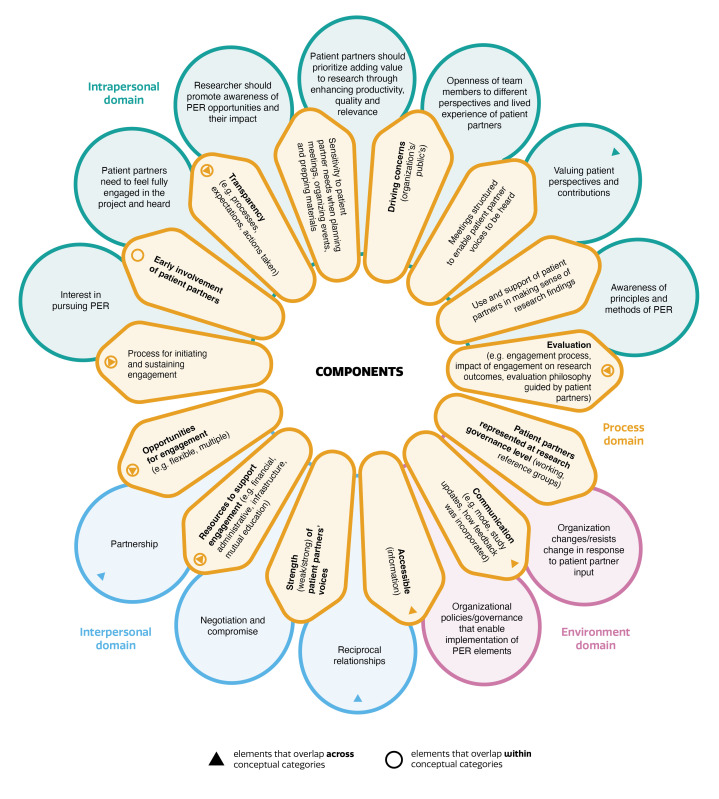
Foundational components
Foundational components represent the core elements that comprise patient engagement in health services research (figure 2). According to the eight models and frameworks27–33 represented here, the 26 underlying elements were primarily situated in the process domain (n=14 elements), with the remainder situated in intrapersonal (n=7), interpersonal (n=3) and environmental (n=2) domains.
Figure 2.
Concept map—foundational components of patient engagement in health services research. PER, patient engagement in research.
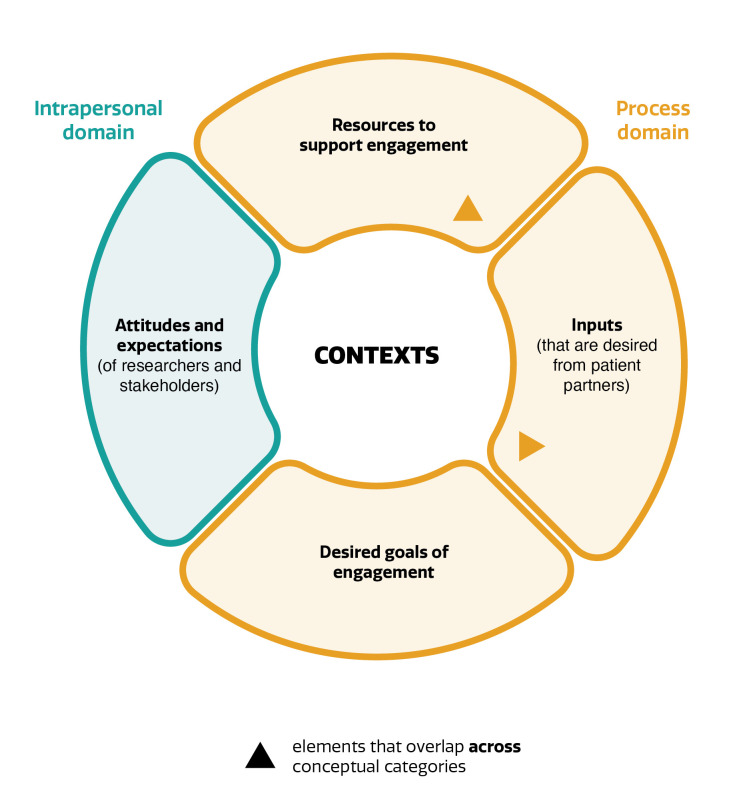
Contexts
This conceptual category identifies elements that relate to resources or decisions that are external to but inform the engagement process.34 Figure 3 presents the four elements in this category, as contributed by one article.34 Three of the underlying elements resided in the process, and one in the intrapersonal domains.
Figure 3.
Concept map—contexts of patient engagement in health services research.
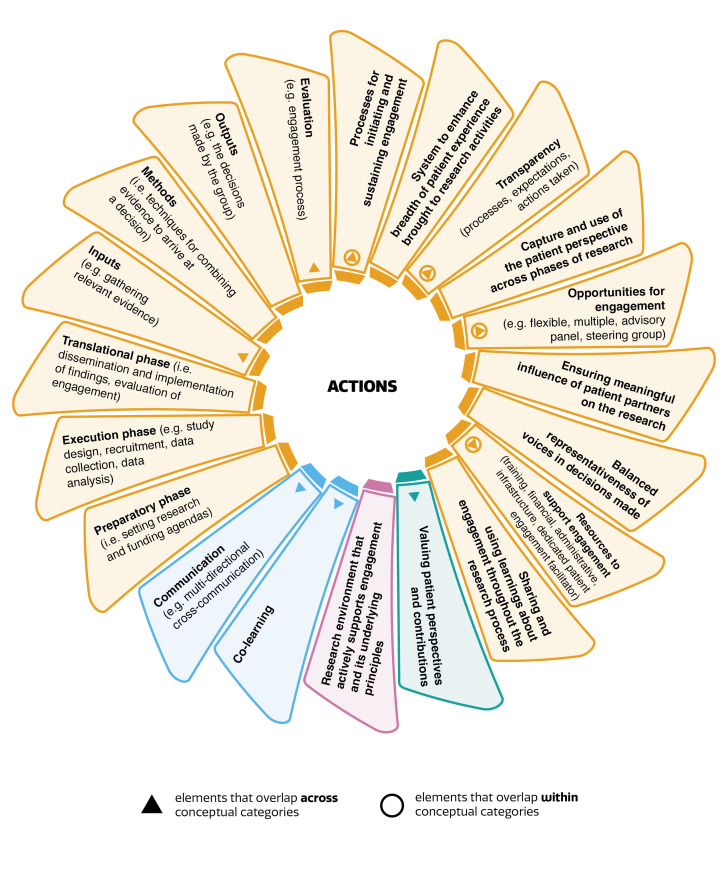
Actions
The elements within this category pertain to the activities (eg, behaviours, phases, advisory bodies) involved in the actual engagement of patients in health services research. Figure 4 presents the elements that comprised this category, as reported by six articles.22 25–27 32 34 These elements were primarily (n=18) situated in the process domain, with one element in each of intrapersonal and environmental domains, and two elements in the interpersonal domain. As displayed in the top half of elements in the process domain (figure 4), some of the elements located here were conceptualised in terms of phases of research (ie, preparatory, execution, translational phases and inputs, methods, outputs).
Figure 4.
Concept map—actions of patient engagement in health services research.
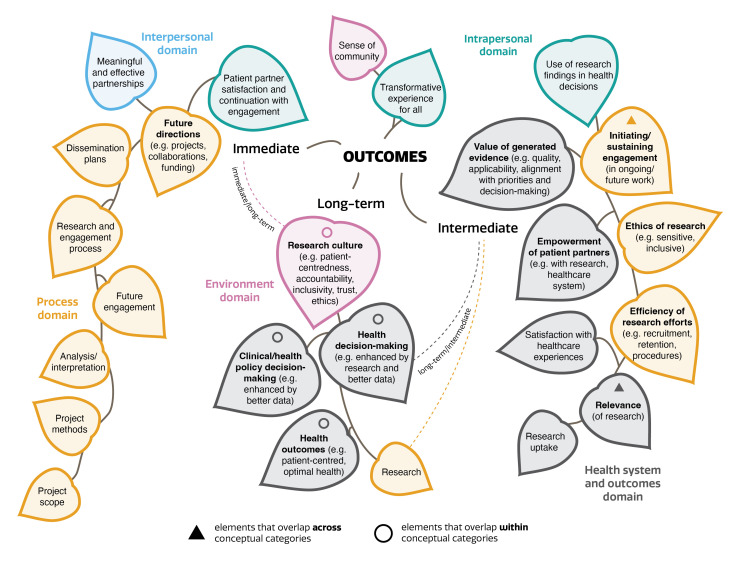
Outcomes
Figure 5 presents the elements that comprise the outcomes of patient engagement in health services research, based on three articles25 27 34 and the unpublished CONNECT framework. As reflected in the figure, all but the CONNECT framework further organised the elements by time frame (ie, immediate/near term, intermediate and long term), with three elements (ie, health decision-making, research culture and research outcomes) belonging to two time frames. Overall, this category’s elements were primarily situated in the process (n=11) and health systems and outcomes (n=8) domains. A further three elements were situated in the intrapersonal, one in the interpersonal and two in the environmental domains.
Figure 5.
Concept map—outcomes of patient engagement in health services research.
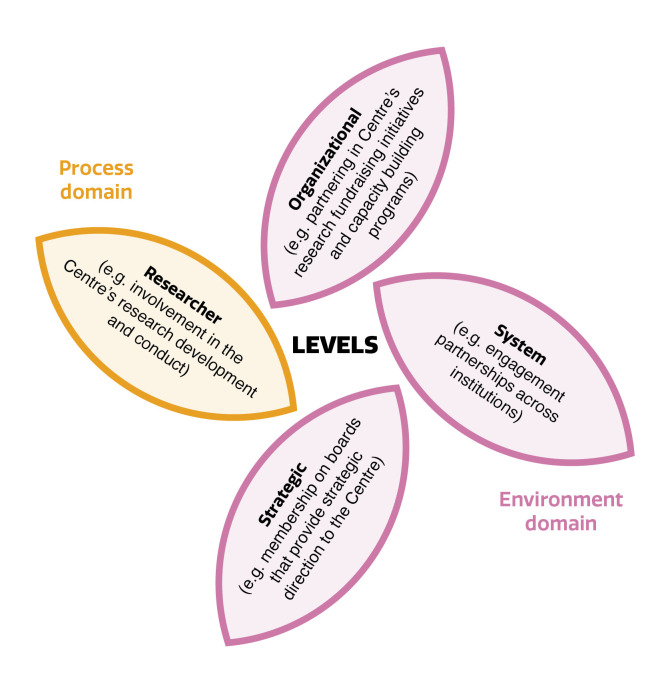
Organisational levels
Two articles presented frameworks whose elements captured the organisational levels at which patient engagement in health services research occurred within research centres.23 35 As displayed in figure 6, these elements were located in environmental (n=3) and process (n=1) domains.
Figure 6.
Concept map—organisational levels of patient engagement in health services research.
Discussion
Principal findings
Our scoping review identified 14 models and frameworks of patient engagement in health services research, which were comprised of 18 overlapping and 57 diverging elements (ntotal elements=75). This work represents a novel contribution as, to our knowledge, it is the first to synthesise the literature on models and frameworks of patient engagement in health services research. Our approach to data synthesis is also unique in that we attempt to maximise the intuitiveness and applicability of our findings by presenting elements by overarching conceptual categories (ie, principles, foundational components, contexts, actions, levels and outcomes) and corresponding domains (ie, intrapersonal, interpersonal, process, environmental, and health systems and outcomes). We anticipate this approach will facilitate the ready application of our findings to readers’ own research programmes by serving as a ‘toolbox’ of elements to consider according to the multilevel facets of a research team and study. To illustrate, research partners could begin to meet at a study’s outset to codevelop terms of reference that guide the relational and activity related aspects of the study’s engagement process. In doing so, they could reflect on whether/how elements within the domains of each conceptual category resonate with their study’s engagement process (as influenced by factors such as the study design, available resources, research partner strengths and interests, etc). These conversations could be guided by prompts such as ‘do we want to embody or incorporate this element within our study (why/why not)?’, ‘what does the embodiment or incorporation of this element look and feel like to us?’ and ‘how will we know when we have or have not embodied or incorporated this element within our study?’ In doing so, the ‘toolbox’ of elements found within our review is transformed into a codeveloped ‘roadmap’ to help guide a study’s engagement process.
Strengths and weaknesses of the study
Strengths of this study include its scoping review design, which enabled us to gain a broad perspective of the literature on models and frameworks of patient engagement in health services research. Other strengths include (1) a published protocol, (2) the use of an established methodological framework to guide its design and conduct, (3) the involvement of an interdisciplinary research team that included patient coresearchers with lived experience of engaging in health services research and other researchers with content expertise in health services research and participatory approaches (including patient engagement in research) and (4) and the codesign of the search strategy with an academic librarian (LD) and the rest of the research team. A weakness of this study concerns the grey boundaries between health services research and other forms of health research, which may have resulted in the inclusion or exclusion of models or frameworks that others could argue do/do not belong in this review. We attempted to minimise this possibility through a screening process that used two reviewers (with a third to resolve discrepancies), an a priori agreed on definition of health services research and reaching out to study authors for clarification when necessary. Further, the engagement of patient coresearchers in our scoping review at the level of involve limited their opportunities to formally provide insights and expertise to predetermined study milestones. Engagement at the level of collaborate or empower may have resulted in other insights through more direct contact with the study.
Comparison with other studies
Previous reviews of models, frameworks and/or other systematic approaches to the engagement of patients and other knowledge users in research had a broader scope11–13 (although only one involved a comprehensive search of multiple databases11) and different levels of analyses. Specifically, rather than report underlying elements, Greenhalgh et al developed a taxonomy for the classification of identified systematic approaches (ie, tools, frameworks, benchmarks, guidelines and critical appraisal checklists) based on their primary focus and intended purpose (ie, power focused, priority setting, study focused, report focused, partnership focused).11 Innovatively, they piloted codesign workshops that aimed to improve the aesthetic appeal and usability of ‘best in-class’ resources identified through the review. Similar to our questioning of the appropriateness of a ‘one-size-fits-all’ framework, preliminary findings from their codesign workshops indicated that although stakeholders were presented with a common set of resources, they generated widely differing frameworks suited to meet their different needs and purposes. The review by Jull et al reported 15 high-level concepts for knowledge user engagement in research that they identified through a directed content analysis of underlying elements.13 Although they organised these concepts across four general research phases (ie, prepare, plan, conduct, apply), they concluded that variation in the reported concepts between frameworks indicated that research teams should consider the concepts as fluid rather than strictly required. Lastly, the findings of Harrison et al’s narrative review of frameworks and guidelines culminated in the proposal of an overarching framework that (similar in principle to our scoping review) conceptualised three distinct but inter-related elements of the patient engagement in research process—engagement foundational principles (ie, domains that original study authors ‘… considered foundational to patient engagement in research’; n=15 elements), engagement best practices (ie, best practice activities to support engagement; n=25 elements) and research phases where engagement should occur (n=3 elements).12 Taken together, existing reviews demonstrate diversity in how patient engagement in research has been conceptualised through models, frameworks and other systematic approaches and the approaches used to synthesise their findings.
The meaning of the study
Our findings indicate that the conceptualisation of patient engagement in health services research varies between existing models and frameworks. Although models and frameworks posit to break down a concept into its base components (which implies the existence of convergence among underlying elements), this finding is not surprising as patient engagement is an approach to research rather than a method. Contributing to the heterogeneity among identified elements is the diversity in the populations, contexts and approaches used to develop the models and frameworks, which also emphasises the importance of avoiding a ‘one-size-fits-all’ approach to engagement. Perhaps congruence between models and frameworks actually exists at the level of conceptual categories. These could be taken to represent the essential components of patient engagement in health services research. The elements that underlie them, as identified across the various models and frameworks, would then serve as considerations for researchers and patient coresearchers when planning and operationalising patient engagement in health services research. For this to be better developed from the current literature, consensus is needed on the definitions of the underlying categories, followed by some reshuffling of the elements across the conceptual categories in order to align with the agreed on definitions.
Unanswered questions and future research
In sum, our study found that there is little overlap between the elements that comprise existing models and frameworks of patient engagement in health services research. Readers seeking to apply our findings to their own engaged work should consider the ‘fit’ of each element, by conceptual category and domain, within the context of their study. Future research that builds on our work should consider addressing three major gaps. First, most existing models and frameworks identified factors that needed improvement for patient coresearchers to be better research partners, with a lot less consideration paid to factors that needed improvement for academic coresearchers to be better research partners. This may be in large part due to the fact the majority of the models and frameworks were written from an academic researcher lens (as evidenced, eg, by the fact that only a third of the included models and frameworks stated that they involved patients in their development). Second, there is a lack of focus on the intrapersonal domain of engagement, including the ‘soft skills’ that underlie interpersonal interactions and relationships (eg, body language, wording, tone) and the environmental domain of engagement, which shapes the context in which engagement is set. Third, patient coresearchers are not just ‘patients’ that can be lumped into a single homogenous category. They are people with different backgrounds, skills and interests extending beyond their health conditions or needs. Thus, it is important to incorporate a trauma-informed and intersectional approach that acknowledges and promotes an understanding of human beings as shaped by the interactions of different social locations and experiences.36 Relatedly, it is important for patient coresearchers and academic researchers to get to know each other as people, instead of making assumptions (including about a patient coresearcher’s experience with healthcare services). Engagement is as much about relational interactions as it is research processes. Careful attention needs to be paid to both for academic–patient coresearcher relationships to thrive.
Supplementary Material
Acknowledgments
We offer our sincerest thanks to Mr. Patrick Faucher for designing our figures, and to the Manitoba SPOR Support Unit (George & Fay Yee Centre for Healthcare Innovation) for Mr. Faucher’s services.
Footnotes
Twitter: @AMChudyk, @tarahorrill, @CarolynShimmin, @inuk37
Deceased: CW deceased.
Contributors: AMC and ASHS were responsible for all major areas of concept development, study planning and manuscript writing. In addition, AMC was also responsible for data collection and analysis and is the guarantor of this work. TH, LD, CS, RS and SH were responsible for all major areas of concept development and study planning, were consulted on the data analysis and its interpretation and provided manuscript edits. In addition, TH was responsible for data collection. CW led concept development but passed away prior to the completion of the manuscript.
Funding: This work was supported by a grant from the University Collaborative Research Program (University of Manitoba), grant number 50664. The patient engagement activities were supported by the George and Fay Yee Centre for Health Innovation (CHI) Patient and Public Engagement Award (CHI), grant number 49876. AMC’s postdoctoral fellowship is supported by the Canadian Institute of Health Research’s Patient-Oriented Research Awards—Transition to Leadership Stream award, grant number 170670. The research team had full autonomy in all aspects of the study.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data are available upon reasonable request to the corresponding author (https://orcid.org/0000-0001-8476-2093).
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Research ethics approval was not required as this study did not involve participants.
References
- 1.Strategy for patient-oriented research - patient engagement framework 2014.
- 2.Allen ML, Salsberg J, Knot M, et al. Engaging with communities, engaging with patients: amendment to the NAPCRG 1998 policy statement on responsible research with communities. Fam Pract 2017;34:313–21. 10.1093/fampra/cmw074 [DOI] [PubMed] [Google Scholar]
- 3.Lewin K. Frontiers in group dynamics: II. channels of group life; social planning and action research. Human relations 1947;1:143–53. [Google Scholar]
- 4.Freire P. Pedagogy of the oppressed. New York: Herder & Herder, 1970. [Google Scholar]
- 5.Domecq JP, Prutsky G, Elraiyah T, et al. Patient engagement in research: a systematic review. BMC Health Serv Res 2014;14:89. 10.1186/1472-6963-14-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manafo E, Petermann L, Mason-Lai P, et al. Patient engagement in Canada: a scoping review of the 'how' and 'what' of patient engagement in health research. Health Res Policy Syst 2018;16:5. 10.1186/s12961-018-0282-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boote J, Baird W, Beecroft C. Public involvement at the design stage of primary health research: a narrative review of case examples. Health Policy 2010;95:10–23. 10.1016/j.healthpol.2009.11.007 [DOI] [PubMed] [Google Scholar]
- 8.Carroll SL, Embuldeniya G, Abelson J, et al. Questioning patient engagement: research scientists' perceptions of the challenges of patient engagement in a cardiovascular research network. Patient Prefer Adherence 2017;11:1573–83. 10.2147/PPA.S135457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crockett LK, Shimmin C, Wittmeier KDM, et al. Engaging patients and the public in health research: experiences, perceptions and training needs among Manitoba health researchers. Res Involv Engagem 2019;5:28. 10.1186/s40900-019-0162-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Riet M, Boettiger M. Shifting research dynamics: addressing power and maximising participation through participatory research techniques in participatory research. S Afr J Psychol 2009;39:1–18. 10.1177/008124630903900101 [DOI] [Google Scholar]
- 11.Greenhalgh T, Hinton L, Finlay T, et al. Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot. Health Expect 2019;22:785–801. 10.1111/hex.12888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harrison JD, Auerbach AD, Anderson W, et al. Patient stakeholder engagement in research: a narrative review to describe foundational principles and best practice activities. Health Expect 2019;22:307–16. 10.1111/hex.12873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jull JE, Davidson L, Dungan R, et al. A review and synthesis of frameworks for engagement in health research to identify concepts of knowledge user engagement. BMC Med Res Methodol 2019;19:211. 10.1186/s12874-019-0838-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Canadian Institutes of Health Services Research . Ethical considerations about health research. Available: http://www.cihr-irsc.gc.ca/e/48801.html [Accessed 5 Aug 2021].
- 15.Colquhoun HL, Levac D, O'Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014;67:1291–4. 10.1016/j.jclinepi.2014.03.013 [DOI] [PubMed] [Google Scholar]
- 16.Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018;18:143. 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 18.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chudyk AM, Waldman C, Horrill T, et al. Models and frameworks of patient engagement in health services research: a scoping review protocol. Res Involv Engagem 2018;4:28. 10.1186/s40900-018-0111-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 21.Staniszewska S, Brett J, Simera I, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017;358:j3453. 10.1136/bmj.j3453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holmes BJ, Bryan S, Ho K, et al. Engaging patients as partners in health research: lessons from BC, Canada. Healthc Manage Forum 2018;31:41–4. 10.1177/0840470417741712 [DOI] [PubMed] [Google Scholar]
- 23.Evans BA, Gallanders J, Griffiths L, et al. Public involvement and engagement in primary and emergency care research: the story from prime centre Wales. Int J Popul Data Sci 2020;5:1363. 10.23889/ijpds.v5i3.1363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.IAP2 International Federation for Public Participation, Public Participation Spectrum . IAP2 public participation spectrum 2014;1. [Google Scholar]
- 25.Deverka PA, Lavallee DC, Desai PJ, et al. Stakeholder participation in comparative effectiveness research: defining a framework for effective engagement. J Comp Eff Res 2012;1:181–94. 10.2217/cer.12.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evans BA, Porter A, Snooks H, et al. A co-produced method to involve service users in research: the SUCCESS model. BMC Med Res Methodol 2019;19:34. 10.1186/s12874-019-0671-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frank L, Forsythe L, Ellis L, et al. Conceptual and practical foundations of patient engagement in research at the patient-centered outcomes research Institute. Qual Life Res 2015;24:1033–41. 10.1007/s11136-014-0893-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daveson BA, de Wolf-Linder S, Witt J, et al. Results of a transparent expert consultation on patient and public involvement in palliative care research. Palliat Med 2015;29:939–49. 10.1177/0269216315584875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gesell SB, Klein KP, Halladay J, et al. Methods guiding stakeholder engagement in planning a pragmatic study on changing stroke systems of care. J Clin Transl Sci 2017;1:121–8. 10.1017/cts.2016.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gibson A, Welsman J, Britten N. Evaluating patient and public involvement in health research: from theoretical model to practical workshop. Health Expect 2017;20:826–35. 10.1111/hex.12486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pearson M, Monks T, Gibson A, et al. Involving patients and the public in healthcare operational research—The challenges and opportunities. Oper Res Health Care 2013;2:86–9. 10.1016/j.orhc.2013.09.001 [DOI] [Google Scholar]
- 32.Shippee ND, Domecq Garces JP, Prutsky Lopez GJ, et al. Patient and service user engagement in research: a systematic review and synthesized framework. Health Expect 2015;18:1151–66. 10.1111/hex.12090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goeman DP, Corlis M, Swaffer K, et al. Partnering with people with dementia and their care partners, aged care service experts, policymakers and academics: a co-design process. Australas J Ageing 2019;38:53–8. 10.1111/ajag.12635 [DOI] [PubMed] [Google Scholar]
- 34.Ray KN, Miller E. Strengthening stakeholder-engaged research and research on stakeholder engagement. J Comp Eff Res 2017;6:375–89. 10.2217/cer-2016-0096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ruco A, Nichol K. Patient engagement in research and innovation: a new framework. J Med Imaging Radiat Sci 2016;47:290–3. 10.1016/j.jmir.2016.10.008 [DOI] [PubMed] [Google Scholar]
- 36.Shimmin C, Wittmeier KDM, Lavoie JG, et al. Moving towards a more inclusive patient and public involvement in health research paradigm: the incorporation of a trauma-informed intersectional analysis. BMC Health Serv Res 2017;17:539. 10.1186/s12913-017-2463-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-063507supp001.pdf (54.8KB, pdf)
bmjopen-2022-063507supp002.pdf (107.6KB, pdf)
bmjopen-2022-063507supp003.pdf (60.3KB, pdf)
bmjopen-2022-063507supp004.pdf (73.6KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data are available upon reasonable request to the corresponding author (https://orcid.org/0000-0001-8476-2093).