Abstract
Background
Falls occur frequently among older individuals, leading to high morbidity and mortality. This study was to assess the efficacy of vitamin D in preventing older individuals from falling.
Methods
We searched the PubMed, Cochrane Library, and EMBASE databases systematically using the keywords “vitamin D” and “fall” for randomized controlled trials (RCTs) comparing the effects of vitamin D with or without calcium supplements with those of a placebo or no treatment on fall incidence in adults older than 50 years. A meta-analysis was performed to calculate risk ratios (RRs), absolute risk differences (ARDs) and 95% CIs with random-effects models.
Results
A total of 38 RCTs involving 61 350 participants fulfilled the inclusion criteria. Compared with placebo, high-dose vitamin D (≥ 700 IU) can prevent falls [RR, 0.87 (95% CI 0.79 to 0.96); ARD, -0.06 (95% CI, -0.10 to -0.02)]. Low-dose vitamin D (<700 IU) was not significantly associated with falls. Subgroup analysis showed that supplemental calcium, 25(OH) D concentration and frequency influenced the effect of vitamin D in preventing falls. Sensitivity analysis showed that vitamin D prevented falls, which was consistent with the primary analysis. In addition, the active form of vitamin D also prevented falls.
Conclusion
In this meta-analysis of RCTs, doses of 700 IU to 2000 IU of supplemental vitamin D per day were associated with a lower risk of falling among ambulatory and institutionalized older adults. However, this conclusion should be cautiously interpreted, given the small differences in outcomes.
Systematic Review Registration
https://www.crd.york.ac.uk/prospero/, identifier CRD42020179390.
Keywords: vitamin D, fall, prevention, association, risk
Introduction
Falls are the leading cause of accidental injuries and fractures in the elderly (1). One out of every three people over 65 years of age has experienced at least one fall (2), and approximately 20% of the falls required medical attention (2). Globally, approximately 684,000 people die from falls each year, more than 80% of which occur in low- and middle-income countries (3). In 2019, the incidence rate of falls among people aged 60 years and older was 3799.4 new falls per 100 000 population in China (4). Therefore, prevention of falls is widely regarded as the most important element in injury and fracture prevention plans for older individuals.
Vitamin D has a direct influence on muscle strength and is regulated by specific vitamin D receptors in muscle tissue (5). Insufficient vitamin D is associated with lower physical performance and greater declines in physical functioning (6, 7). And vitamin D deficiency can lead to secondary hyperparathyroidism, increased bone resorption, decreased bone mineral density (BMD) and the consequent increase of fracture risk. In some studies of older people at risk of vitamin D deficiency, vitamin D supplements can improve strength, function, and balance., which resulted in a reduction in falls (6, 8). However, the meta-analyses of clinical trials have not found the role of vitamin D in reducing falls. The vitamin D supplement intervention has mixed results on all aspects of prevention (2, 9–11).
Older people living in nursing homes are more likely to fracture than people living in the community (12). However, it is not clear whether life dwelling affect the role of vitamin D in preventing falls. Previous studies have not distinguished the impact of vitamin D on different populations (2, 10, 13). Whether taking calcium affects falling is still uncertain. Therefore, we conducted this meta-analysis to evaluate the effectiveness of vitamin D in preventing falls.
Methods
This meta-analysis is based on the Cochrane Handbook for Systematic Reviews of Interventions (14) and the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines (15, 16). The protocol was published in PROSPERO (CRD42020179390).
Data Sources and Searches
A systematic online search was performed for eligible trials using the electronic databases PubMed, Embase and the Cochrane Library from their inception dates to February 15, 2020, to identify recently published randomized controlled studies (RCTs) assessing the relationship between vitamin D (with or without calcium) and the incidence of falls (search strategies are reported in eTable 1 ). The initial searches were updated on May 10, 2020. Two authors worked independently (F-L W, T L).
Study Selection
Each study’s abstract and full text was reviewed by two reviewers (F-L W, T L) independently to determine eligibility. Conflicts were resolved through discussion. RCTs were selected based on the following inclusion criteria (1): Studies comparing vitamin D or combination of vitamin D and calcium with no placebo or treatment (2); RCTs including adults aged 50 years old or older; and (3) trials providing fall data. The exclusion criteria were as follows (1): RCTs with no placebo or no treatment group (2); observational or animal studies (3); studies for stroke patients, organ transplant patients, or parkinson patients (4) RCTs that evaluated intramuscular injection of vitamin D. Only those trial designs that were double-blind and fully assigned an evaluation of falls were included in the primary analysis: (a) falling was the main outcome; (b) the study should clarify the definition of a fall and its assessment; and (c) falling must be evaluated throughout the study. Otherwise, trials were included in the sensitivity analysis.
Data Extraction and Quality Assessment
Our primary outcome was the relative risk of a person who had at least one fall and took vitamin D supplements compared with a person who took a placebo or calcium supplements alone. The effects of supplemental vitamin D and active forms of vitamin D were analyzed separately.
Data were independently extracted by two researchers (F-L W, T L). The informations obtained from each study were as follows: year of publication; first author; country of origin; characteristics of participant; calcium and vitamin D doses, alone or combination; serum 25-hydroxyvitamin D concentration; and duration. We only extracted the relevant data.
The methodological quality of the included RCTs was independently evaluated by two authors (F-L W, T L). Disagreements were resolved through consensus. According to Cochrane’s bias risk criteria, Each quality item was classified as low, high, or undefined risk (14, 17). Trials with dissimilar baseline characteristics between different intervention groups were considered to have other bias.
Data Synthesis and Analysis
The researchers evaluated the effects of vitamin D supplementation and the active form of vitamin D supplementation on falls. The effects of supplemental vitamin D and active forms of vitamin D were separately analyzed. A random effects model was used for the meta-analysis and risk ratios (RRs), absolute risk differences (ARDs) and 95% CI were calculated. When there was inconsistency between the RR and ARD, the results were interpreted based on the RR model, since the RR model is more consistent than the ARD model, especially for interventions designed to prevent adverse events (14, 18). We pooled the data with a random-effects model (19), and statistical heterogeneity was evaluated using the I 2 statistic. We identified additional trials that did not meet the primary analysis criteria to be included in the sensitivity analysis. STATA 16.0 (Stata Corp, College Station, TX, USA) was used to perform all meta-analyses (20). A 2-tailed P<0.05 was considered statistically significant.
To assess whether the relationship between vitamin D and falls was modified according to clinical features, we assessed the dose and frequency of vitamin D supplementation (≥700 IU/d; <700 IU/d); sex (only for female studies or including male and female studies); dwelling (community or institutionalized); dietary supplemental calcium; serum 25-hydroxyvitamin D concentration (≥60 or <60 nmol/L); form of vitamin D (D3 only or D2 only); the use of intermittent high doses given once a year, once every 3 or 4 months and other frequencies; and daily doses including twice a day and daily. Subgroup analysis was performed to assess whether the differences between subgroups were statistically significant.
Results
Studies Retrieved and Characteristics
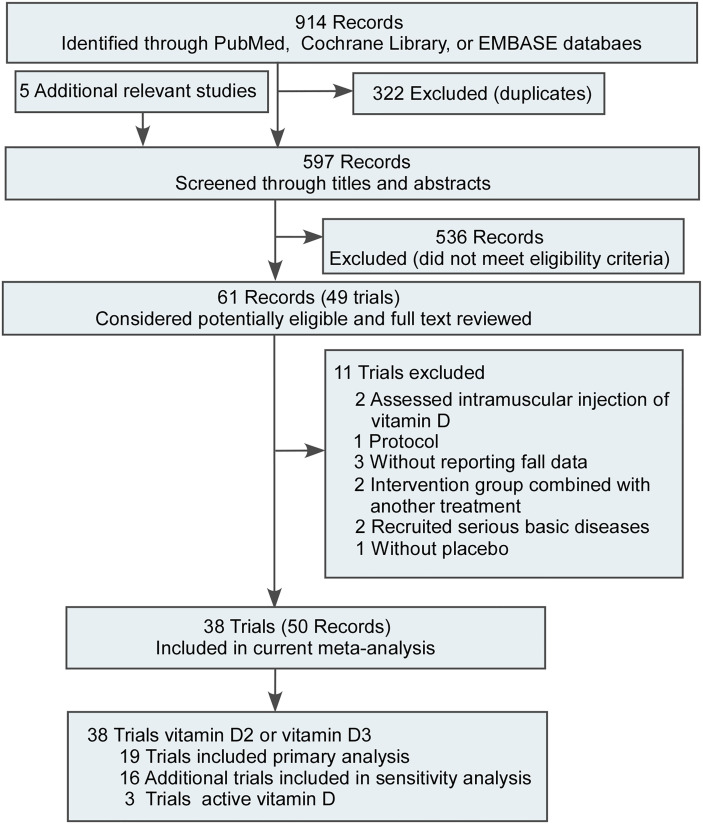
We excluded duplicate studies and 38 RCTs (8, 21–57) including 61 350 participants in this meta-analysis ( Figure 1 ). One study was shown a high risk for randomization sequence generation (46). Three studies showed a high risk in blinding of participants and personnel (44, 46, 49). One study showed a high risk in blinding of outcome assessment (44). Four studies showed a high risk in incomplete outcome data (35, 41, 44, 48). Two studies showed a high risk in selective reporting (27, 35). Most studies were of moderate or high quality (36/38). The assessment of the risk of bias were shown in eFigures 1 , 2 . The characteristics of the included RCTs were reported in Table 1 . Eighteen RCTs on supplemental vitamin D were identified that met our inclusion criteria for the main analysis. There were explicit fall ascertainments in trials. A previous study found that there was a difference in the rate of falling between the high-dose group and the low-dose group (2), so we divided trials into high-dose and low-dose groups based on a daily dose of 700 IU of vitamin D2 or D3.
Figure 1.
Literature Search and Screening Process.
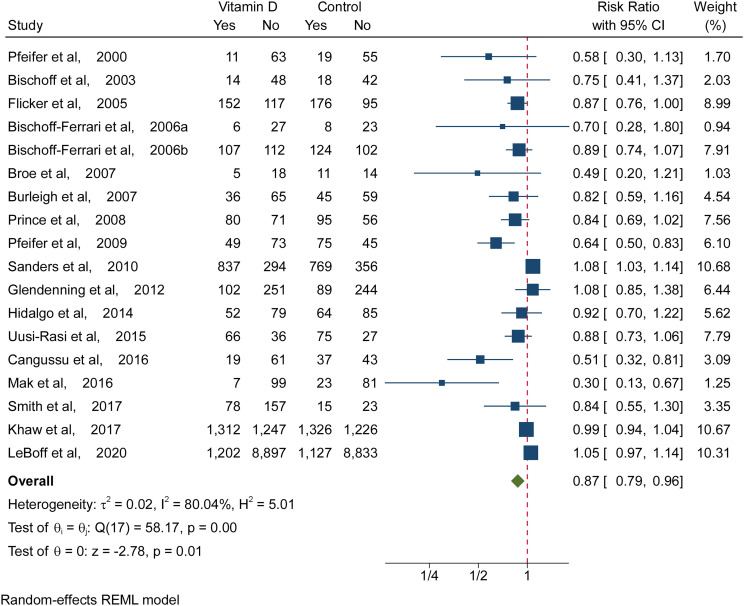
Figure 2.
Meta-analysis Results of Vitamin D Supplementation for the Incidence of Fall. Risk ratios and 95% CIs were calculated using a random-effects model to pool data. Boxes represent relative risks, and the size of the boxes is proportional to the size of the high dose supplemental vitamin D trials included in the primary analysis. Error bars represent 95% confidence intervals.
Table 1.
Characteristics of the included trials and participants.
| Source | Study Country | Treatment | Numbe of Participants | Age(Mean ± SD) | Gender (M/F) | Dwelling | StudyLength | Change in 25-Hydroxyvitamin D Level in Intervention Group, Mean (SD), nmol/L | Osteoporotic |
|---|---|---|---|---|---|---|---|---|---|
| Pfeifer, ( 8 ) | Germany | 800 IU Cholecalciferol + 1200 mg of calcium | 148 | 74.7 (0.5) | 0/74 | Ambulatory | 2 months + 1 year | 25.7 (20.9) to 40.5 (27.0) | NA |
| Placebo+1200 mg of calcium | 74.8 (0.5) | 0/74 | 24.6 (12.1) to 42.9 (33.1) | ||||||
| Graafmans, ( 21 ) | The Netherlands | 400 IU Cholecalciferol + estimated calcium intake from dairy products 800-1000 mg/d | 354 | >70 | 52/302 | Ambulatory in homes for older individuals | 7 months | Not stated | NA |
| Placebo | |||||||||
| Bischoff, ( 22 ) | Switzerland | 800 IU Cholecalciferol + 1200 mg calcium | 122 | 84.9 ± 7.7 | 0/62 | hospitalized | 12 weeks | 30.8 (23-55) to 65.5 (49.8-82.8) | NA |
| 1200 mg calcium | 85.4 ± 5.9 | 0/60 | 29 (23-55) to28.5 (24.5-41.5) | ||||||
| Flicker, ( 23 ) | Australia | 600 mg of elemental calcium daily + 10,000 IU ergocalciferol once per week/1,000 IU ergocalciferol once daily | 625 | 83.6 ± 7.8 | 16/297 | Nursing home + Hostel | 2 years | 25-60 at baseline | NA |
| Placebo | 83.3 ± 8.8 | 16/296 | 25-60 at baseline | ||||||
| Bischoff-Ferrari, ( 57 ) | USA | 600 mg of calcium carbonate + 400 IU of cholecalciferol twice a day | 89 | 85.6 ± 6.4 | 0/33 | hospitalized | 12 weeks | Not stated | NA |
| 600 mg of calcium carbonate twice a day | 85.7 ± 5.9 | 0/31 | |||||||
| Bischoff-Ferrari, ( 24 ) | USA | 700 IU of cholecalciferol + 500 mg of calcium citrate malate per day | 445 | 71 ± 5 | 98/121 | Ambulatory | 3 years | 76 (35) to 107 (38) | NA |
| Placebo | 101/125 | 73 (32) to 72 (30) | |||||||
| Broe, ( 25 ) | USA | 200 IU vitamin D daily | 124 | 92 ± 6 | 7/19 | Nursing home patients | 5 months | 45 (23) to 60 (20) | NA |
| 400 IU vitamin D daily | 88 ± 5 | 7/18 | 53 (28) to 55 (22) | ||||||
| 600 IU vitamin D daily | 89 ± 6 | 8/17 | 40 (19) to 60 (20) | ||||||
| 800 IU vitamin D daily | 89 ± 5 | 7/16 | 54 (23) to 75 (15) | ||||||
| Placebo | 86 ± 7 | 5/20 | 50 (23) to 61 (34) | ||||||
| Burleigh, ( 26 ) | UK | cholecalciferol 800 IU + calcium 1,200 mg daily | 205 | 82.3 ± 7.6 | 40/61 | Geriatric medical unit | 1 month | 25 to 27 | NA |
| Calcium 1,200 mg daily | 83.7 ± 7.6 | 44/60 | 22 to 22 | ||||||
| Pfeifer, ( 28 ) | Germany, Austria | 800 IU vitamin D3 + 1000 mg calcium/d | 242 | 77 ± 4 | 30/91 | Ambulatory individuals | 20 months | 55.4 (18.5) to 84.5 (18.0) | NA |
| Placebo + 1000 mg calcium | 76 ± 4 | 31/90 | 53.8 (18.4) to 56.6 (20) | ||||||
| Prince, ( 27 ) | Australia | Ergocalciferol, 1000 IU/d + calcium citrate, 1000 mg/d | 302 | 77.0 ± 4.2 | 0/151 | Community dwelling | 1 year | 45 to 60 | None |
| Placebo + calcium citrate, 1000 mg/d | 77.4 ± 5.0 | 0/151 | 44.3 to 49 | ||||||
| Sanders, ( 29 ) | Australia | A single oral dose of cholecalciferol 500 000 IU in autumn or winter | 2,256 | 76 | 0/1131 | Community dwelling | 3 to 5 years | Not stated | Osteoporosis diagnosis 1.0% (n = 23/2256) |
| Placebo | 76.1 | 0/1125 | |||||||
| Glendenning, ( 30 ) | Australia | Vitamin D3 150,000 IU every 3 months | 686 | 76.9 ± 4.0 | 0/353 | Community dwelling | 9 months | 65.0 (17.8) to 74.6 (25.8) | NA |
| Placebo | 76.5 ± 4.0 | 0/333 | 66.5 (27.1) to 60.2 (26.3) | ||||||
| Hidalgo, (31) | Spain | 800 IU of vitamin D3 + 1,000 mg of calcium daily | 508 | 72.6 ± 4.9 | 85/103 | Community dwelling | 2 years | 86.77 (41.0) at baseline | None |
| Placebo | 72.4 ± 5.2 | 105/105 | 79.3 (42.7) at baseline | ||||||
| Uusi-Rasi, ( 32 ) a | Finland | Vitamin D3 800 IU vitamin/d | 409 | 74.1 ± 2.9 | 0/204 | home-dwelling | 2 years | 63 to 93 | NA |
| Placebo | 74.3 ± 3.0 | 0/205 | 69 to 69 | ||||||
| Cangussu, ( 33 ) | Brazil | vitamin D3 1,000 IU/day/orally | 160 | 58.8 ± 6.6 | 0/80 | Ambulatory | 9 months | 37.29 to 68.37 | None |
| Placebo | 59.3 ± 6.7 | 0/80 | 42.0 to 34.3 | ||||||
| Mak, ( 34 ) | Australia | 250,000 IU vitamin D (loading dose)+800 IU vitamin D and 500 mg calcium daily | 218 | 83.7 ± 7.5 | 27/84 | Community dwelling | 4 weeks | 55.6 to 77 | NA |
| placebo+800 IU vitamin D and 500 mg calcium daily | 84.1 ± 7.0 | 23/84 | 49.6 to 74 | ||||||
| Smith, ( 35 ) | USA | 400 IU vitamin D3 daily | 273 | 66 | 0/67 | Community dwelling | 12 months | 36 at baseline | NA |
| 800-4800 IU vitamin D3 daily | 0/168 | ||||||||
| Placebo | 0/38 | ||||||||
| Khaw, ( 36 ) | New Zealand | 200 000 IU followed by 100 000 IU monthly | 5108 | 65.9 ± 8.3 | 1512/1046 | Ambulatory | 3.4 years | 63 (24) at baseline | Osteoporosis diagnosis |
| Placebo | 1457/1093 | 1.4%(N=71/5108) | |||||||
| LeBoff, ( 37 ) | USA | 2000 IU/day of vitamin D3 | 25,871 | 67.13 (7.05) | 6380/6547 | Ambulatory | 5.3 years | 76.8 (25) at baseline | NA |
| Placebo | 67.14 (7.08) | 6406/6538 | 76.6 (25) at baseline |
We extracted only the information and data in placebo without exercise and vitamin D (800 IU/d) without exercise groups. NA, not available.
Vitamin D and Fall Risk
Figure 2 shows the comparison of vitamin D with placebo or no treatment. Compared with a placebo or no treatment, vitamin D (≥700 IU/d) prevented falling (RR, 0.87 [95% CI 0.79 to 0.96]; ARD, -0.06 [95% CI, -0.10 to -0.02], Figure 2 and eFigure 3 ). The results suggested that daily intake of high doses of vitamin D reduced the risk of falls in older individuals by 13%, and the number needed to treat was 17 (95% CI, 10 to 50). However, there was no significant association of low-dose vitamin D with falling (RR, 1.09 [95% CI, 0.90 to 1.32]; ARD, 0.03 [95% CI, -0.05 to 0.12], eFigures 4, 5 ). eFigure 6 in the Supplement, a contour-enhanced funnel plot, did reveal significant publication bias.
Primary Subgroup Analyses
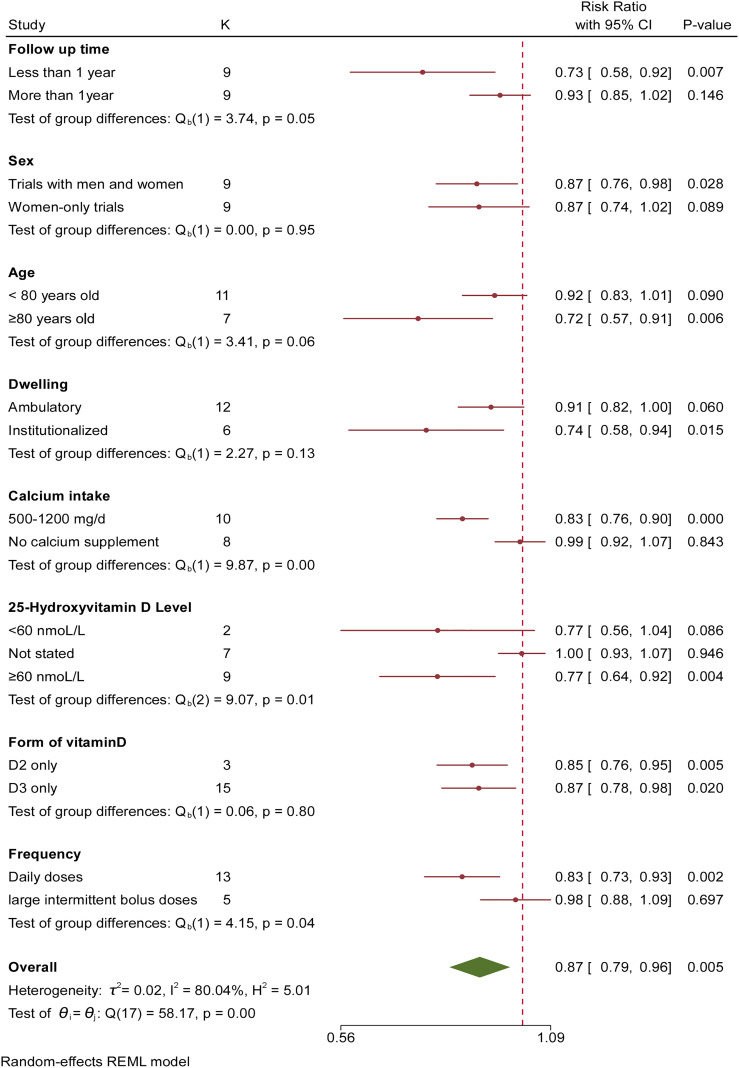
As a result of statistical heterogeneity, we performed a subgroup analysis for high doses of supplemental vitamin D (more than 700 IU). The role of vitamin D was highly regulated by treatment duration: fall reduction was 27% with less than 12 months of treatment (RR, 0.73 [95% CI, 0.58 to 0.92]) compared with 7% with 12 months or more of treatment (RR, 0.93 [95% CI, 0.85 to 1.02], Figure 3 ). There was no difference in the number of falls between women-only trials and trials with men and women (P=0.95). The pooled risk reduction for falling was 28% in trials in which participants were older than 80 years old (RR, 0.72 [95% CI, 0.57 to 0.91]) compared with 8% for trials in which participants were less than 80 years old (RR, 0.92 [95% CI, 0.83 to 1.01]). Therefore, participants older than 80 years old benefited more from supplemental vitamin D. Vitamin D was equally effective for elderly individuals in community (RR, 0.91 [95% CI, 0.82 to 1.00]) and institutionalized dwellings (RR, 0.74 [95% CI, 0.58 to 0.94]). Vitamin D2 and vitamin D3 achieved similar effects (P=0.80). The role of vitamin D was highly modulated by supplemental calcium: no calcium supplement did not reduce the risk of falls (RR, 0.99 [95% CI, 0.92 to 1.07]). However, the pooled risk reduction for falling was 17% (RR, 0.83 [95% CI, 0.76 to 0.90]) in trials with supplemental calcium of 500-1200 mg/d. The results implied that the efficacy of vitamin D depended on additional calcium supplementation. The pooled risk reduction for falling was 23% in trials with 25(OH)D concentrations ≥60 nmol/l (RR, 0.77 [95% CI, 0.64 to 0.92]) compared with trials with 25(OH)D concentrations <60 nmol/l (RR, 0.77 [95% CI, 0.56 to 1.04]). The results suggested that a 25(OH)D concentration of 60 nmol/l was important for preventing falls. In addition, the pooled risk reduction for falling was 17% in trials with high daily doses (RR, 0.83 [95% CI, 0.73 to 0.93]) compared with trials with large intermittent bolus doses (RR, 0.98 [95% CI, 0.88 to 1.09]). The results suggested that high-dose bolus vitamin D supplementation did not prevent falls.
Figure 3.
Subgroup Analysis of Association Between Vitamin D Supplementation and Fall Incidence for Each Variable. Risk ratios and 95% CIs were calculated using a random-effects model to pool data. Boxes represent relative risks, and the size of the boxes is proportional to the size of the high dose supplemental vitamin D trials included in the primary analysis. Error bars represent 95% confidence intervals.
Sensitivity Analysis of Supplemental Vitamin D
To understand the reliability and accuracy of the results, we performed sensitivity analysis. We included the studies eliminated in the primary analysis in sensitivity analysis. Twelve eliminated studies were excluded for unclear definitions of falling (38–41, 43, 45, 47, 49–51, 53). These trial designs were not double-blind, or they did not describe the generation of random sequences (41, 42, 44–46, 48–51). Sixteen additional RCTs were included to examine the effect, which expanded the participant population to 55 318. The characteristics of these studies are shown in Table 2 . The results showed that compared with a placebo or no treatment, vitamin D prevented falling (RR, 0.96 [95% CI, 0.92 to 1.00]; ARD, -0.03 [95% CI, -0.05 to -0.01], Table 3 and eFigures 7, 8 ), which was consistent with the primary analysis. The number of effects was reduced by these additional studies, but the benefits remained statistically significant.
Table 2.
Trials of supplemental vitamin D excluded from the primary analyses but included in sensitivity analyses.
| Source | Study Country | Treatment | Numbe of Participants | Age(Mean ± SD) | Gender (M/F) | Dwelling | StudyLength | Change in 25-Hydroxyvitamin D Level in Intervention Group, Mean (SD), nmol/L | Osteoporotic |
|---|---|---|---|---|---|---|---|---|---|
| Chapuy, ( 38 ) | France | 800 IU Cholecalciferol + 1200 mg/d of calcium | 583 | 85 (7) | 0/393 | Ambulatory in homes for the elderly | 2 years | 21.3 (13.3) to 77.5 | None |
| Placebo | 0/190 | 22.8 (17.3) to 15 | |||||||
| Trivedi, ( 39 ) | UK | 800 IU vitamin D3 (100 000 IU every 4 months) | 2386 | 74.8 (4.6) | 1019/326 | Community dwelling | 1 year | 74.3 (20.7) at 48 months | NA |
| Placebo | 74.7 (4.6) | 1018/323 | 53.4 (21.1) at 48 months | ||||||
| Latham, ( 40 ) | New Zealand, Australia | 300 000 IU Cholecalciferol once + no calcium | 243 | 79 (77–80) | 57/64 | Acute care recruitment of frail elderly | 6 months | 37.5 (35-45) to 60 | NA |
| Placebo | 80 (78–81) | 57/65 | 47.5 (40-52.5) to 47.5 | ||||||
| Harwood, ( 41 ) | UK | 800 IU vitamin D3 +1g calcium | 150 | 81 (67-92) | 0/113 | Patients in rehabilitationwards, previously community dwelling | 1 year | 30 (6-75) to 50 | None |
| Placebo | 0/37 | 30 (12-64) to 27 | |||||||
| Larsen, ( 42 ) | Denmark | 1000 mg Ca+400 IU vitamin D3/Day | 4256 | 74 (65–103) | 843/1273 | Community dwelling | 42 months | Not stated | NA |
| Control | 1974/2983 | ||||||||
| Grant, ( 43 ) | UK | 800 IU vitamin D3 with or without 1000 mg calcium per day | 5292 | 77 ± 6 | 409/2240 | Individuals who were mobile before developing a low trauma fracture | 2 years | 38 (16) to 62 (19.5) | NA |
| Placebo | 422/2241 | 38 (16) to 45.8 (18) | |||||||
| Porthouse, ( 44 ) | UK | Vitamin D3 800 IU + 1000 mg calcium | 2541 | 77.0 ± 5.10 | 0/914 | community-dwelling | 1 year | Not stated | NA |
| No supplementation | 76.7 ± 5.02 | 0/1627 | |||||||
| Law, ( 45 ) a | UK | 1100 IU vitamin D2 (100 000 IU ergocalciferol every 3 months) | 3137 | 85 | 929/2788 | Patients living in residential | 10 months | 47 (35-102) to 74 (52-110) | NA |
| No treatment (no placebo) | Not stated | ||||||||
| Kärkkäinen, ( 46 ) | Finland | 800 IU vitamin D3 + 1g calcium | 3432 | 67.4 ± 1.9 | 0/1718 | Community dwelling | 3 years | Not stated | NA |
| Control group (no placebo) | 67.3 ± 1.8 | 0/1714 | |||||||
| Wood, ( 47 ) | UK | 1100 IU vitamin D3 daily | 305 | 60–70 | 0/203 | Community | 12 months | 33 to 70 | NA |
| Placebo | 0/102 | 36 to 32 | |||||||
| Rizzoli, ( 48 ) | 13 countries | 1000 IU vitamin D3 + 1g calcium | 518 | 66.9 ± 8.3 | 41/372 | Ambulatory | 6 months | 44.0 (14.9) to 67 | Yes |
| Control | 66.6 ± 8.0 | 8/97 | 44.4 (13.3) to 45 | ||||||
| Houston, ( 49 ) a | USA RCT(Cluster) | Vitamin D3 two 50,000 IU capsules/month; | 68 | 77.6 ± 9.0 | 8/30 | Community dwelling | 5 months | 22.5 (12.2) at baseline | NA |
| Placebo (400 IU vitamin E/month) | 78.2 ± 8.4 | 11/19 | 18.9 (10.6) at baseline | ||||||
| Hansen, ( 50 ) | USA | 800 IU vitamin D3 daily or twice monthly 50,000 IU vitamin D3 | 230 | 61 | 0/154 | Community dwelling | 12 months | 53 to 86 | None |
| Placebo | 0/76 | 53 to 45 | |||||||
| Levis, ( 51 ) | USA | 4,000 IU cholecalciferol daily | 130 | 71.8 ± 6.3 | 66/0 | Ambulatory | 9 months | 58 to 115 | NA |
| Placebo | 73.0 ± 7.3 | 64/0 | 57 to 60 | ||||||
| Hin, ( 53 ) | UK | 2000 IU/day | 305 | 71 ± 6 | 52/50 | Community-dwelling | 1 year | Not stated | NA |
| 4000 IU/day | 72 ± 6 | 51/51 | |||||||
| Placebo | 72 ± 6 | 52/49 | |||||||
| Dhaliwal, ( 52 ) | USA | 2400, 3600 or 4800IU vitamin D3 +1200 mg calcium daily | 260 | 67.8 | 0/130 | Community-dwelling | 3 years | 94 achieved | None |
| Placebo +1200 mg calcium daily | 69.0 | 0/130 | 52 achieved |
They is a randomized controlled trial of cluster design. They was adjusted for the number of participants. NA, not available.
Table 3.
Sensitivity analysis of the eighteen trials from the primary analysis and the sixteen eligible trials that did not meet the criteria for the primary analysis.
| Study | Number of participants | Vitamin D | Placebo | Fall, RR (95% CI) | ||
|---|---|---|---|---|---|---|
| With Fall | Total | With Fall | Total | |||
| Pooled primary analysis of the eighteen trials | 31355 | 4135 | 15850 | 4096 | 15505 | 0.87 (0.79-0.96) |
| Heterogeneity: τ2 = 0.02; I2 = 80.04%; H2 = 5.01 Test of θ=0: z =-2.78 (P =0.01) | ||||||
| Sensitivity analysis including the sixteen trials that did not meet criteria for primary analysis | ||||||
| Trivedi, (39) | 2038 | 254 | 1027 | 261 | 1011 | 0.96 (0.83-1.11) |
| Latham, (40) | 222 | 64 | 108 | 60 | 114 | 1.13 (0.89-1.42) |
| Chapuy, (38) | 583 | 251 | 393 | 118 | 190 | 1.03 (0.90-1.18) |
| Harwood, (41) | 119 | 15 | 84 | 13 | 35 | 0.48 (0.26-0.90) |
| Larsen, (42) | 4607 | 466 | 2491 | 403 | 2116 | 0.98 (0.87-1.11) |
| Grant, (43) | 5292 | 380 | 2649 | 381 | 2643 | 1.00 (0.87-1.13) |
| Porthouse, (44) | 2541 | 289 | 914 | 498 | 1627 | 1.03 (0.92-1.16) |
| Law, (45) | 3137 | 770 | 1762 | 833 | 1955 | 1.03 (0.95-1.10) |
| Kärkkäinen, (46) | 3139 | 812 | 1566 | 833 | 1573 | 0.98 (0.92-1.05) |
| Wood, (47) | 196 | 27 | 96 | 31 | 100 | 0.91 (0.59-1.40) |
| Rizzoli, (48) | 518 | 65 | 413 | 21 | 105 | 0.79 (0.51-1.23) |
| Houston, (49) | 66 | 11 | 37 | 12 | 29 | 0.72 (0.37-1.39) |
| Hansen, (50) | 230 | 46 | 154 | 23 | 76 | 0.99 (0.65-1.50) |
| Hin, (53) | 305 | 34 | 204 | 14 | 101 | 1.20 (0.68-2.14) |
| Dhaliwal, (52) | 260 | 51 | 130 | 50 | 130 | 1.02 (0.75-1.38) |
| Levis, (51) | 130 | 8 | 66 | 11 | 64 | 0.71 (0.30-1.64) |
| Pooled sensitivity analysis | 55318 | 7678 | 27944 | 7658 | 27374 | 0.96 (0.92-1.00) |
| Heterogeneity: τ2 = 0.00; I2 = 47.98%; H2 = 1.92 Test of θ=0: z =-1.98 (P =0.05) | ||||||
I2 estimates above 25% are considered to represent modest heterogeneity, and values above 50% represent large heterogeneity beyond chance.
Active Vitamin D Supplementation and Fall Risk
Three RCTs (54–56) on the active forms of vitamin D met our inclusion criteria ( eTable 2 ). There were clear definitions of falling in these trials. However, the random sequence generation was not described in one trial (56), so we excluded it from the primary analysis. This study was included in the sensitivity analysis. Compared with a placebo or no treatment, active forms of vitamin D prevented falls (RR, 0.78 [95% CI, 0.64 to 0.95]; ARD, -0.09 [95% CI, -0.20 to 0.02], eFigures 9, 10 ). Active vitamin D intake can reduce the risk of falls by 22%, based on the RR. The sensitivity analysis was consistent with the primary analysis ( eFigure 11 ).
Discussion
This meta-analysis included thirty-eight double-blind RCTs with 61 350 elderly individuals treated with vitamin D for 2 to 63 months. Seventeen RCTs were excluded from all primary analyses because they did not meet the criteria. The pooled ARD in the primary analysis indicated that 17 people need vitamin D treatment to prevent one person from falling and daily intake of high doses of vitamin D reduced the risk of falls in elderly individuals by 13%. When 16 additional RCTs were included in the sensitivity analysis, these results were not modulated. However, the effectiveness of vitamin D for preventing falling depended on the dose, time, supplemental calcium, 25-hydroxyvitamin D level and frequency, according to the subgroup analysis.
Not only can a fall cause serious injury or death but elderly people who have experienced a fall also have increased anxiety and depression (58, 59), and their quality of life is reduced (60). However, there is still much controversy about the role of vitamin D in preventing falls. Therefore, we conducted this study to evaluate the effectiveness of vitamin D in preventing falls. A meta-analysis conducted by Bischoff-Ferrari et al. showed that vitamin D reduced the risk of falls among healthy ambulatory or institutionalized older individuals by 22% (13). However, they included a cluster experiment with a large sample (45) did not adjust for the number of participants. There was no distinction between the form and dose of vitamin D in their study. This meta-analysis did not find a significant association between low vitamin D intake and fall prevention. (RR, 1.09 [95% CI, 0.90 to 1.32]; ARD, 0.03 [95% CI, -0.05 to 0.12]). The results manifested that the efficacy has nothing to do with the form of vitamin D (vitamin D2, D3 and active forms of vitamin D) in preventing falls. In a meta-analysis from 2009 (2), it was reported that Vitamin D has nothing to do with calcium intake. However, they did not compare vitamin D combined with calcium supplementation with vitamin D alone. We found that supplemental calcium influenced the effect of vitamin D on the prevention of falls in the subgroup analysis. Therefore, we suggest that Vitamin D and calcium should be supplemented at the same time. In less than 1 year of treatment, the risk of taking high-dose vitamin D was reduced by 27% and a sustained 7% fall reduction for 1-5.3 years. These results were consistent with those of a previous study (2).
A Cochrane review suggested that vitamin D did not appear to reduce falls (61). This difference might be because they did not include some high-quality RCTs. It has been found that vitamin D supplementation did not prevent falls in a prior study, and there was no difference between high-dose and low-dose vitamin D. The possible reason for the differences was that Bolland et al. excluded a large amount of literature on vitamin D from their meta-analysis. Their reason was that calcium supplements have uncommon but clinically important side effects (62). However, a recent meta-analysis conducted by Chung reported that supplemental calcium within tolerable upper intake levels (2000 to 2500 mg/d), healthy adults were generally not associated with a risk of cardiovascular disease (63). We believe that when analyzing the role of vitamin D, some studies could not be excluded despite the side effects of calcium, which would lead to unreliable results. Current research showed that vitamin D and calcium can reduce the risk of falls by 18%. Guirguis-Blake performed random-effects meta-analyses and the conclusion was that vitamin D supplementation has mixed effects in preventing falls (10). However, they only included a small part of the research on vitamin D. Their review was focused on community-dwelling older adults. They reported that large intermittent bolus doses increased the rate of fall. A previous RCT reported that in this healthy and active adult group, high doses of vitamin D did not prevent falls or fractures (36). In this meta-analysis, it was shown that large intermittent bolus doses of vitamin D had no preventive effect on falls, which was consistent with a previous study (10, 36).
Davies reported that a 6% reduction in the risk of fall associated with vitamin D would be cost effective (64). The results reported here showed that daily intake of high doses of vitamin D could reduce the risk of falling in elderly individuals by 13%, which was higher than 6%. Therefore, vitamin D supplementation was cost effective.
Limitations
This study had several limitations. First, the results of some meta-analysis were moderately heterogeneous because several studies reported negative results regarding high-dose bolus vitamin D. High-dose bolus vitamin D was proven to be useless in fall prevention in some RCTs (29, 30, 34, 36). Second, some small sample studies might affect the results. Then, the results showed the relationship between 25(OH) D concentration and falls. However, there was no RCTs to confirm the relationship between 25(OH) D concentration and falls. In this regard, further research is needed to determine the relationship between 25(OH) D concentration and falls. In addition, a publication bias has likely affected the results presented in this review.
Conclusions
In this study, doses of 700 IU to 2000 IU of supplemental vitamin D per day were associated with a lower risk of falling among ambulatory and institutionalized older adults. This benefit might depend on additional calcium supplementation. However, this conclusion should be cautiously interpreted, given the small differences in outcomes.
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding authors.
Author Contributions
Conception and design, F-LW, C-PZ, WW, and J-XQ; Analysis and interpretation of the data, F-LW, TL, Q-YG, YH, C-PZ, WW, and J-XQ; Drafting of the article, F-LW; Critical revision of the article for important intellectual content, Q-YG, YH, C-PZ, WW, and J-XQ; Final approval of the article, F-LW, TL, Q-YG, YH, C-PZ, WW, and J-XQ; Statistical expertise, F-LW, TL, and YH; Obtaining of funding, J-XQ; Administrative, technical, or logistic support, YH, C-PZ, WW, and J-XQ; Collection and assembly of data, F-LW, TL, YH, C-PZ, WW, and J-XQ; All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81871818), Tangdu Hospital Seed Talent Program (F-LW) and Social Talent Fund of Tangdu Hospital (No.2021SHRC034). The funding body had no role in the design of the study, data collection, analysis, interpretation or in writing the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Tangdu Hospital, Fourth Military Medical University for supporting our work and Home for Researchers (www.home-for-researchers.com) for a language polishing service.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2022.919839/full#supplementary-material
References
- 1. Tinetti ME. Clinical Practice. Preventing Falls in Elderly Persons. N Engl J Med (2003) 348(1):42–9. [DOI] [PubMed] [Google Scholar]
- 2. Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, Orav JE, Stuck AE, Theiler R, et al. Fall Prevention With Supplemental and Active Forms of Vitamin D: A Meta-Analysis of Randomised Controlled Trials. BMJ (2009) 339:b3692. doi: 10.1136/bmj.b3692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WWHOG . Step Safely: Strategies for Preventing and Managing Falls Across the Life-Course. (2021). CDC of USA. [Google Scholar]
- 4. Ye P, Er Y, Wang H, Fang L, Li B, Ivers R, et al. Burden of Falls Among People Aged 60 Years and Older in Mainland China, 1990-2019: Findings From the Global Burden of Disease Study 2019. Lancet Public Health (2021) 6(12):e907–18. doi: 10.1016/s2468-2667(21)00231-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bischoff-Ferrari HA, Borchers M, Gudat F, Dürmüller U, Stähelin HB, Dick W. Vitamin D Receptor Expression in Human Muscle Tissue Decreases With Age. J Bone Miner Res (2004) 19(2):265–9. [DOI] [PubMed] [Google Scholar]
- 6. Bischoff-Ferrari HA, Dietrich T, Orav EJ, Hu FB, Zhang Y, Karlson EW, et al. Higher 25-Hydroxyvitamin D Concentrations are Associated With Better Lower-Extremity Function in Both Active and Inactive Persons Aged > or =60 Y. Am J Clin Nutr (2004) 80(3):752–8. [DOI] [PubMed] [Google Scholar]
- 7. Aibana O, Huang CC, Aboud S, Arnedo-Pena A, Becerra MC, Bellido-Blasco JB, et al. Vitamin D Status and Risk of Incident Tuberculosis Disease: A Nested Case-Control Study, Systematic Review, and Individual-Participant Data Meta-Analysis. PloS Med (2019) 16(9):e1002907. doi: 10.1371/journal.pmed.1002907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pfeifer M, Begerow B, Minne HW, Abrams C, Nachtigall D, Hansen C. Effects of a Short-Term Vitamin D and Calcium Supplementation on Body Sway and Secondary Hyperparathyroidism in Elderly Women. J Bone Miner Res (2000) 15(6):1113–8. [DOI] [PubMed] [Google Scholar]
- 9. Robertson MC, Gillespie LD. Fall Prevention in Community-Dwelling Older Adults. JAMA (2013) 309(13):1406–7. doi: 10.1001/jama.2013.3130 [DOI] [PubMed] [Google Scholar]
- 10. Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL. Interventions to Prevent Falls in Older Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA (2018) 319(16):1705–16. doi: 10.1001/jama.2017.21962 [DOI] [PubMed] [Google Scholar]
- 11. Grossman DC, Curry SJ, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Interventions to Prevent Falls in Community-Dwelling Older Adults: US Preventive Services Task Force Recommendation Statement. JAMA (2018) 319(16):1696–704. doi: 10.1001/jama.2018.3097 [DOI] [PubMed] [Google Scholar]
- 12. Duque G, Lord SR, Mak J, Ganda K, Close JJT, Ebeling P, et al. Treatment of Osteoporosis in Australian Residential Aged Care Facilities: Update on Consensus Recommendations for Fracture Prevention. J Am Med Dir Assoc (2016) 17(9):852–9. doi: 10.1016/j.jamda.2016.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, et al. Effect of Vitamin D on Falls: A Meta-Analysis. JAMA (2004) 291(16):1999–2006. [DOI] [PubMed] [Google Scholar]
- 14. Higgins JPT, Green SE. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 (Updated March 2011) (2011). Cochrane Collaboration website. Available at: http://trainingcochraneorg/handbook (Accessed November 22, 2017). [Google Scholar]
- 15. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ (2009) 339:b2700w. doi: 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wei FL, Zhou CP, Liu R, Zhu KL, Du MR, Gao HR, et al. Management for Lumbar Spinal Stenosis: A Network Meta-Analysis and Systematic Review. Int J Surg (London England) (2021) 85:19–28. doi: 10.1016/j.ijsu.2020.11.014 [DOI] [PubMed] [Google Scholar]
- 17. Wei F-L, Gao Q-Y, Heng W, Zhu K-L, Yang F, Du M-R, et al. Association of Robot-Assisted Techniques With the Accuracy Rates of Pedicle Screw Placement: A Network Pooling Analysis. eClinicalMedicine (2022) 48:101421. doi: 10.1016/j.eclinm.2022.101421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Deeks JJ. Issues in the Selection of a Summary Statistic for Meta-Analysis of Clinical Trials With Binary Outcomes. Stat Med (2002) 21(11):1575–600. [DOI] [PubMed] [Google Scholar]
- 19. Berkey CS, Hoaglin DC, Mosteller F, Colditz GA. A Random-Effects Regression Model for Meta-Analysis. Stat Med (1995) 14(4):395–411. [DOI] [PubMed] [Google Scholar]
- 20. Zhao J, Dong X, Zhang Z, Gao Q, Zhang Y, Song J, et al. Association of Use of Tourniquets During Total Knee Arthroplasty in the Elderly Patients With Post-Operative Pain and Return to Function. Front Public Health (2022) 10:825408. doi: 10.3389/fpubh.2022.825408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Graafmans WC, Ooms ME, Hofstee HM, Bezemer PD, Bouter LM, Lips P. Falls in the Elderly: A Prospective Study of Risk Factors and Risk Profiles. Am J Epidemiol (1996) 143(11):1129–36. [DOI] [PubMed] [Google Scholar]
- 22. Bischoff HA, Stähelin HB, Dick W, Akos R, Knecht M, Salis C, et al. Effects of Vitamin D and Calcium Supplementation on Falls: A Randomized Controlled Trial. J Bone Miner Res (2003) 18(2):343–51. [DOI] [PubMed] [Google Scholar]
- 23. Flicker L, MacInnis RJ, Stein MS, Scherer SC, Mead KE, Nowson CA, et al. Should Older People in Residential Care Receive Vitamin D to Prevent Falls? Results of a Randomized Trial. J Am Geriatr Soc (2005) 53(11):1881–8. [DOI] [PubMed] [Google Scholar]
- 24. Bischoff-Ferrari HA, Orav EJ, Dawson-Hughes B. Effect of Cholecalciferol Plus Calcium on Falling in Ambulatory Older Men and Women: A 3-Year Randomized Controlled Trial. Arch Intern Med (2006) 166(4):424–30. [DOI] [PubMed] [Google Scholar]
- 25. Broe KE, Chen TC, Weinberg J, Bischoff-Ferrari HA, Holick MF, Kiel DP. A Higher Dose of Vitamin D Reduces the Risk of Falls in Nursing Home Residents: A Randomized, Multiple-Dose Study. J Am Geriatr Soc (2007) 55(2):234–9. [DOI] [PubMed] [Google Scholar]
- 26. Burleigh E, McColl J, Potter J. Does Vitamin D Stop Inpatients Falling? A Randomised Controlled Trial. Age Ageing (2007) 36(5):507–13. [DOI] [PubMed] [Google Scholar]
- 27. Prince RL, Austin N, Devine A, Dick IM, Bruce D, Zhu K. Effects of Ergocalciferol Added to Calcium on the Risk of Falls in Elderly High-Risk Women. Arch Intern Med (2008) 168(1):103–8. doi: 10.1001/archinternmed.2007.31 [DOI] [PubMed] [Google Scholar]
- 28. Pfeifer M, Begerow B, Minne HW, Suppan K, Fahrleitner-Pammer A, Dobnig H. Effects of a Long-Term Vitamin D and Calcium Supplementation on Falls and Parameters of Muscle Function in Community-Dwelling Older Individuals. Osteoporos Int (2009) 20(2):315–22. doi: 10.1007/s00198-008-0662-7 [DOI] [PubMed] [Google Scholar]
- 29. Sanders KM, Stuart AL, Williamson EJ, Simpson JA, Kotowicz MA, Young D, et al. Annual High-Dose Oral Vitamin D and Falls and Fractures in Older Women: A Randomized Controlled Trial. JAMA (2010) 303(18):1815–22. doi: 10.1001/jama.2010.594 [DOI] [PubMed] [Google Scholar]
- 30. Glendenning P, Zhu K, Inderjeeth C, Howat P, Lewis JR, Prince RL. Effects of Three-Monthly Oral 150,000 IU Cholecalciferol Supplementation on Falls, Mobility, and Muscle Strength in Older Postmenopausal Women: A Randomized Controlled Trial. J Bone Miner Res (2012) 27(1):170–6. doi: 10.1002/jbmr.524 [DOI] [PubMed] [Google Scholar]
- 31. López-Torres Hidalgo J. [Effect of Calcium and Vitamin D in the Reduction of Falls in the Elderly: A Randomized Trial Versus Placebo]. Med Clin (Barc) (2014) 142(3):95–102. doi: 10.1016/j.medcli.2012.11.025 [DOI] [PubMed] [Google Scholar]
- 32. Uusi-Rasi K, Patil R, Karinkanta S, Kannus P, Tokola K, Lamberg-Allardt C, et al. Exercise and Vitamin D in Fall Prevention Among Older Women: A Randomized Clinical Trial. JAMA Intern Med (2015) 175(5):703–11. doi: 10.1001/jamainternmed.2015.0225 [DOI] [PubMed] [Google Scholar]
- 33. Cangussu LM, Nahas-Neto J, Orsatti CL, Poloni PF, Schmitt EB, Almeida-Filho B, et al. Effect of Isolated Vitamin D Supplementation on the Rate of Falls and Postural Balance in Postmenopausal Women Fallers: A Randomized, Double-Blind, Placebo-Controlled Trial. Menopause (2016) 23(3):267–74. doi: 10.1097/GME.0000000000000525 [DOI] [PubMed] [Google Scholar]
- 34. Mak JC, Mason RS, Klein L, Cameron ID. An Initial Loading-Dose Vitamin D Versus Placebo After Hip Fracture Surgery: Randomized Trial. BMC Musculoskelet Disord (2016) 17:336. doi: 10.1186/s12891-016-1174-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Smith LM, Gallagher JC, Suiter C. Medium Doses of Daily Vitamin D Decrease Falls and Higher Doses of Daily Vitamin D3 Increase Falls: A Randomized Clinical Trial. J Steroid Biochem Mol Biol (2017) 173:317–22. doi: 10.1016/j.jsbmb.2017.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Khaw K-T, Stewart AW, Waayer D, Lawes CMM, Toop L, Camargo CA, et al. Effect of Monthly High-Dose Vitamin D Supplementation on Falls and non-Vertebral Fractures: Secondary and Post-Hoc Outcomes From the Randomised, Double-Blind, Placebo-Controlled ViDA Trial. Lancet Diabetes Endocrinol (2017) 5(6):438–47. doi: 10.1016/S2213-8587(17)30103-1 [DOI] [PubMed] [Google Scholar]
- 37. LeBoff MS, Murata EM, Cook NR, Cawthon P, Chou SH, Kotler G, et al. VITamin D and OmegA-3 TriaL (VITAL): Effects of Vitamin D Supplements on Risk of Falls in the US Population. J Clin Endocrinol Metab (2020) 105(9):2929–38. doi: 10.1210/clinem/dgaa311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chapuy MC, Pamphile R, Paris E, Kempf C, Schlichting M, Arnaud S, et al. Combined Calcium and Vitamin D3 Supplementation in Elderly Women: Confirmation of Reversal of Secondary Hyperparathyroidism and Hip Fracture Risk: The Decalyos II Study. Osteoporos Int (2002) 13(3):257–64. [DOI] [PubMed] [Google Scholar]
- 39. Trivedi DP, Doll R, Khaw KT. Effect of Four Monthly Oral Vitamin D3 (Cholecalciferol) Supplementation on Fractures and Mortality in Men and Women Living in the Community: Randomised Double Blind Controlled Trial. BMJ (2003) 326(7387):469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Latham NK, Anderson CS, Lee A, Bennett DA, Moseley A, Cameron ID. A Randomized, Controlled Trial of Quadriceps Resistance Exercise and Vitamin D in Frail Older People: The Frailty Interventions Trial in Elderly Subjects (FITNESS). J Am Geriatr Soc (2003) 51(3):291–9. [DOI] [PubMed] [Google Scholar]
- 41. Harwood RH, Sahota O, Gaynor K, Masud T, Hosking DJ. A Randomised, Controlled Comparison of Different Calcium and Vitamin D Supplementation Regimens in Elderly Women After Hip Fracture: The Nottingham Neck of Femur (NONOF) Study. Age Ageing (2004) 33(1):45–51. [DOI] [PubMed] [Google Scholar]
- 42. Larsen ER, Mosekilde L, Foldspang A. Vitamin D and Calcium Supplementation Prevents Severe Falls in Elderly Community-Dwelling Women: A Pragmatic Population-Based 3-Year Intervention Study. Aging Clin Exp Res (2005) 17(2):125–32. [DOI] [PubMed] [Google Scholar]
- 43. Grant AM, Avenell A, Campbell MK, McDonald AM, MacLennan GS, McPherson GC, et al. Oral Vitamin D3 and Calcium for Secondary Prevention of Low-Trauma Fractures in Elderly People (Randomised Evaluation of Calcium Or Vitamin D, RECORD): A Randomised Placebo-Controlled Trial. Lancet (2005) 365(9471):1621–8. [DOI] [PubMed] [Google Scholar]
- 44. Porthouse J, Cockayne S, King C, Saxon L, Steele E, Aspray T, et al. Randomised Controlled Trial of Calcium and Supplementation With Cholecalciferol (Vitamin D3) for Prevention of Fractures in Primary Care. BMJ (2005) 330(7498):1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Law M, Withers H, Morris J, Anderson F. Vitamin D Supplementation and the Prevention of Fractures and Falls: Results of a Randomised Trial in Elderly People in Residential Accommodation. Age Ageing (2006) 35(5):482–6. [DOI] [PubMed] [Google Scholar]
- 46. Kärkkäinen MK, Tuppurainen M, Salovaara K, Sandini L, Rikkonen T, Sirola J, et al. Does Daily Vitamin D 800 IU and Calcium 1000 Mg Supplementation Decrease the Risk of Falling in Ambulatory Women Aged 65-71 Years? A 3-Year Randomized Population-Based Trial (OSTPRE-FPS). Maturitas (2009) 65(4):359–65. doi: 10.1016/j.maturitas.2009.12.018 [DOI] [PubMed] [Google Scholar]
- 47. Wood AD, Secombes KR, Thies F, Aucott LS, Black AJ, Reid DM, et al. A Parallel Group Double-Blind RCT of Vitamin D3 Assessing Physical Function: Is the Biochemical Response to Treatment Affected by Overweight and Obesity? Osteoporos Int (2013) 25(1):305–15. doi: 10.1007/s00198-013-2473-8 [DOI] [PubMed] [Google Scholar]
- 48. Rizzoli R, Dawson-Hughes B, Kaufman JM, Fardellone P, Brandi ML, Vellas B, et al. Correction of Vitamin D Insufficiency With Combined Strontium Ranelate and Vitamin D3 in Osteoporotic Patients. Eur J Endocrinol (2014) 170(3):441–50. doi: 10.1530/EJE-13-0775 [DOI] [PubMed] [Google Scholar]
- 49. Houston DK, Tooze JA, Demons JL, Davis BL, Shertzer-Skinner R, Kearsley LB, et al. Delivery of a Vitamin D Intervention in Homebound Older Adults Using a Meals-On-Wheels Program: A Pilot Study. J Am Geriatr Soc (2015) 63(9):1861–7. doi: 10.1111/jgs.13610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hansen KE, Johnson RE, Chambers KR, Johnson MG, Lemon CC, Vo TNT, et al. Treatment of Vitamin D Insufficiency in Postmenopausal Women: A Randomized Clinical Trial. JAMA Intern Med (2015) 175(10):1612–21. doi: 10.1001/jamainternmed.2015.3874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Levis S, Gómez-Marín O. Vitamin D and Physical Function in Sedentary Older Men. J Am Geriatr Soc (2017) 65(2):323–31. doi: 10.1111/jgs.14510 [DOI] [PubMed] [Google Scholar]
- 52. Dhaliwal R, Mikhail M, Usera G, Stolberg A, Islam S, Ragolia L, et al. The Relationship of Physical Performance and Osteoporosis Prevention With Vitamin D in Older African Americans (PODA). Contemp Clin Trials (2018) 65:39–45. doi: 10.1016/j.cct.2017.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hin H, Tomson J, Newman C, Kurien R, Lay M, Cox J, et al. Optimum Dose of Vitamin D for Disease Prevention in Older People: BEST-D Trial of Vitamin D in Primary Care. Osteoporos Int (2017) 28(3):841–51. doi: 10.1007/s00198-016-3833-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Gallagher JC, Fowler SE, Detter JR, Sherman SS. Combination Treatment With Estrogen and Calcitriol in the Prevention of Age-Related Bone Loss. J Clin Endocrinol Metab (2001) 86(8):3618–28. [DOI] [PubMed] [Google Scholar]
- 55. Dukas L, Bischoff HA, Lindpaintner LS, Schacht E, Birkner-Binder D, Damm TN, et al. Alfacalcidol Reduces the Number of Fallers in a Community-Dwelling Elderly Population With a Minimum Calcium Intake of More Than 500 Mg Daily. J Am Geriatr Soc (2004) 52(2):230–6. [DOI] [PubMed] [Google Scholar]
- 56. Gallagher JC, Rapuri PB, Smith LM. An Age-Related Decrease in Creatinine Clearance is Associated With an Increase in Number of Falls in Untreated Women But Not in Women Receiving Calcitriol Treatment. J Clin Endocrinol Metab (2007) 92(1):51–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bischoff-Ferrari HA, Conzelmann M, Stähelin HB, et al. Is Fall Prevention by Vitamin D Mediated by a Change in Postural or Dynamic Balance? Osteoporos Int. (2006) 17(5):656–63. doi: 10.1007/s00198-005-0030-9 [DOI] [PubMed] [Google Scholar]
- 58. Gill TM, Murphy TE, Gahbauer EA, Allore HG. Association of Injurious Falls With Disability Outcomes and Nursing Home Admissions in Community-Living Older Persons. Am J Epidemiol (2013) 178(3):418–25. doi: 10.1093/aje/kws554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Siracuse JJ, Odell DD, Gondek SP, Odom SR, Kasper EM, Hauser CJ, et al. Health Care and Socioeconomic Impact of Falls in the Elderly. Am J Surg (2012) 203(3):335–8. doi: 10.1016/j.amjsurg.2011.09.018 [DOI] [PubMed] [Google Scholar]
- 60. Kumar A, Carpenter H, Morris R, Iliffe S, Kendrick D. Which Factors are Associated With Fear of Falling in Community-Dwelling Older People? Age Ageing (2014) 43(1):76–84. doi: 10.1093/ageing/aft154 [DOI] [PubMed] [Google Scholar]
- 61. Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for Preventing Falls in Older People Living in the Community. Cochrane Database Syst Rev (2012) 9):CD007146. doi: 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium Supplements With or Without Vitamin D and Risk of Cardiovascular Events: Reanalysis of the Women's Health Initiative Limited Access Dataset and Meta-Analysis. BMJ (2011) 342:d2040. doi: 10.1136/bmj.d2040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Chung M, Tang AM, Fu Z, Wang DD, Newberry SJ. Calcium Intake and Cardiovascular Disease Risk: An Updated Systematic Review and Meta-Analysis. Ann Intern Med (2016) 165(12):856–66. doi: 10.7326/M16-1165 [DOI] [PubMed] [Google Scholar]
- 64. Davies JS, Poole CD. Vitamin D and Falls. Lancet Diabetes Endocrinol (2014) 2(7):540–1. doi: 10.1016/S2213-8587(14)70125-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/ Supplementary Material . Further inquiries can be directed to the corresponding authors.