Abstract
Mitochondria are not only the main energy supplier but are also the cell metabolic center regulating multiple key metaborates that play pivotal roles in epigenetics regulation. These metabolites include acetyl-CoA, α-ketoglutarate (α-KG), S-adenosyl methionine (SAM), NAD+, and O-linked beta-N-acetylglucosamine (O-GlcNAc), which are the main substrates for DNA methylation and histone post-translation modifications, essential for gene transcriptional regulation and cell fate determination. Tumorigenesis is attributed to many factors, including gene mutations and tumor microenvironment. Mitochondria and epigenetics play essential roles in tumor initiation, evolution, metastasis, and recurrence. Targeting mitochondrial metabolism and epigenetics are promising therapeutic strategies for tumor treatment. In this review, we summarize the roles of mitochondria in key metabolites required for epigenetics modification and in cell fate regulation and discuss the current strategy in cancer therapies via targeting epigenetic modifiers and related enzymes in metabolic regulation. This review is an important contribution to the understanding of the current metabolic-epigenetic-tumorigenesis concept.
Keywords: mitochondria, epigenetics, cancer, metabolism
1. Introduction
Mitochondria in eukaryotic cells likely evolved from bacteria by endosymbiosis [1,2], and they are composed of two separate and functionally distinct membranes (the outer membrane and the inner membrane), the intermembrane space, and matrix compartments. Mitochondria also have a circular genome called mitochondrial DNA (mtDNA) [3]. The mitochondrial genome encompasses thousands of copies of the mtDNA and more than one thousand nuclear DNA (nDNA)-encoded genes [4]. Mitochondria form a dynamic and interconnected network that is intimately integrated with other cellular compartments such as nuclear, endoplasmic reticulum (ER), and plasma [5,6,7]. Mitochondria are not only the center for energy metabolism, but also the headquarters for different catabolic and anabolic processes, calcium fluxes, and various signaling pathways [8,9,10,11]. During these processes, many intermediates are generated, which are critical for cell anabolic metabolism and cellular signaling, as well as for providing substrates required for epigenetic modification [12]. Metabolites that are essential for epigenetic modification include acetyl coenzyme A (Acetyl-CoA), oxidized nicotinamide adenine dinucleotide (NAD+), α-ketoglutarate (α-KG), succinate, etc., and they perform diverse functions, including contributing to gene transcription modulation and cell fate determination.
The concept of epigenetics can be traced back to 1942. Waddington described the divergence between genotype and phenotype during development [13]. Now, epigenetics commonly refers to heritable alterations in gene expression without DNA sequence changing [14,15]. Epigenetic modification mainly includes DNA and histone modifications, which lead to nucleosome remodeling and gene transcription alternations. There are many types of epigenetic modifications, but all are tightly regulated by the specific enzymes and the corresponding substrates required [16]. The expression of enzymes is determined by the cell linage and state, while the substrates are highly dependent on the cell metabolism, which is tightly regulated by extracellular signaling and available nutrition [17,18,19]. These epigenetic modifications are also strictly dependent on the cellular energy status [20]. Metabolites generated in the tricarboxylic acid cycle (TCA) in mitochondria or related metabolism are crucial for epigenetics, which links the relation among mitochondria, gene expression, and cell fate dictation. We briefly explored the function of several important metabolites in basic epigenetics such as DNA methylation and histone modification. The aberration of epigenetics exerts a significant impact on cellular function, thus leading to the dysregulation of gene expression and finally resulting in various diseases, such as cancers [21].
Oncogene overactivation and tumor suppressor inactivation transform somatic cells into cancer cells [22,23,24]. This transformation can take place during tissue regeneration and can be accelerated under infections, toxins, or other metabolic influences that cause mutations [25,26]. After transformation, additional gene mutation, gene expression alteration, and change in tumor microenvironment drive tumor evolution [27].
Historically, the notion of cancer stem cells (CSCs) is adopted from somatic stem cells, and it refers to a subpopulation of cancer cells with relatively slow cycling but that can regenerate the entire tumor after treatment. CSCs originate from either differentiated cells or tissue-resident stem cells [28]. CSC was first discovered as the leukemia-initiating cell in human acute myeloid leukemia in 1994 [29]. After that, CSCs were also found in tumors in the brain, breast, colon, liver, etc. [30,31,32,33,34]. These CSCs drive tumor initiation and tumor malignant growth and are often responsible for drug resistance and relapses. Unlike normal somatic stem cells, CSCs evolve with tumor evolution, which results from additional gene expression alternations and tumor microenvironment changes. CSCs can propagate tumors and promote tumor progression compared with the non-tumorigenic cells within the bulk tumor [35].
Metabolic and epigenetic reprogramming is essential for tumor initiation, evolution, and metastasis [36,37]. Epigenetics dictates the cell fate of both embryonic cells and somatic cells in differentiation and development [38], and different epigenetic regulations on gene expression also affect tumorigenesis [39,40]. A multitude of epigenetic mechanisms, including DNA methylation and post-translational modification of histones, contribute to diversity within tumors [41,42]. Epigenetic deregulation participates in the earliest stages of tumor initiation and has been increasingly recognized as a hallmark of cancer [43,44]. The deregulation of various epigenetic pathways contributes to tumorigenesis, especially concerning the maintenance and survival of CSCs [35]. For example, DNA hypermethylation has been associated with the silencing of tumor suppressor genes as well as differentiation genes in various cancers [45].
Considering the critical role of mitochondria in cellular metabolism and the essential role of epigenetics in tumorigenesis, it is recognized that the interplay between mitochondria metabolism and epigenetic enzymes plays a critical role in tumor initiation and evolution [46,47,48,49]. The metabolites such as acetyl-CoA, α-KG, S-adenosyl methionine (SAM), NAD+, and O-linked beta-N-acetylglucosamine (O-GlcNAc) play crucial roles in cell fate determination by regulating epigenetic modifications and gene expression.
Tumorigenesis affected by both genetic and non-genetic determinants constitutes a major source of therapeutic resistance. Targeting epigenetics as well as mitochondrial metabolism has been demonstrated as a promising therapeutic strategy to inhibit tumor growth. Mitochondrial and epigenetic targeting cancer therapy reduces tumor malignancy and often exhibits synergistic effects when combined with classical cytotoxic cancer therapy.
2. Mitochondria Function in Epigenetic Regulation
Mitochondria are the energy and metabolic center in the cell, which are essential for catabolic and anabolic metabolism. Mitochondrial function is tightly regulated by the expression of the mitochondrial genome as well as the surrounding microenvironment, both of which determine the cellular level of acetyl-CoA, α-KG, SAM, NAD+, and O-GlcNAc required for epigenetic modification [50,51]. Epigenetic modification is a genetic regulation model that is independent of DNA sequence and plays an important role in establishing and maintaining specific gene expression. DNA methylation, histone post-translational modification, and chromatin remodeling are the major forms of epigenetic modifications [52,53]. Epigenetic alterations are the main mechanisms in development and tumorigenesis. Mitochondria, as the main energy supplier, play a pivotal role in the regulation of epigenetics [54].
2.1. Mitochondria and DNA Methylation
Methylation is the only known modification that occurs on DNA, RNA, and proteins [55].
DNA methylation is a major form of DNA modification in the mammalian genome, which mainly occurs at cytosine in a dinucleotide CpG [56,57,58]. DNA methyltransferases (DNMTs) are responsible for the establishment and maintenance of methylation patterns [59]. They transfer the methyl group donated from SAM to cytosine and generate 5-methylcytosine (5mC) [60] (Figure 1). DNMT1 is responsible for maintaining the existing DNA methylation during DNA replication, and DNMT3A and DNMT3B are responsible for establishing de novo DNA methylation patterns [61]. The pattern of DNA methylation in the genome changes is a dynamic process regulated by both de novo DNA methylation and demethylation [62].
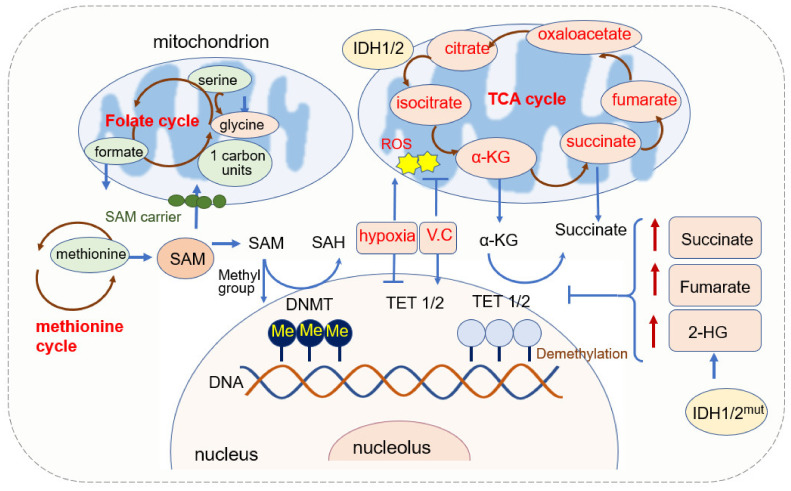
Figure 1.
Mitochondrial function in DNA methylation.
The demethylation of DNA requires the function of the ten-eleven translocation (TET) enzyme. TETs belong to the 2-oxoglutarate-dependent dioxygenases (2-OGDO) family and their activity requires coenzyme factors such as Fe2+ and α-KG [63,64]. They catalyze the oxidation of 5-methylcytosine (5mC) to 5-hydroxymethylcytosine (5hmC), 5-formylcytosine (5fC), and 5-carboxylcytosine (5caC) [65,66]. 5hmc resulted from the hydroxylation of methylcytosine and hydroxylation is involved in more than 90% reduction in cytosine methylation. 5hmC is not only an intermediate in the DNA demethylation process but also an independent epigenetic marker [67,68,69,70].
2.1.1. SAM Source and Mitochondrial Regulation of SAM
SAM is a significant biological sulfonium compound that participates in a variety of biochemical processes. SAM is synthesized through the reaction of methionine with ATP catalyzed by methionine adenosyltransferase (MAT). This reaction mainly occurs in the cytosol through the one-carbon (1C) metabolism pathway that encompasses both the folate and methionine cycles [71]. Since SAM is synthesized in the cytosol [72], it has to be transported into mitochondria by the mitochondrial SAM carrier, and it is converted into S-adenosylhomocysteine (SAH) in the methylation reaction of DNA, RNA, and proteins [73]. SAH is further hydrolyzed in a reversible reaction by SAH hydrolase (SAHH) to give rise to adenosine and homocysteine. SAH is a competitive inhibitor of the methylation process, therefore both the increase of SAH and the decrease of SAM or SAM/SAH ratio inhibit the transmethylation reactions [74,75].
SAM is utilized in the cell by three metabolic pathways: transmethylation, transsulfuration, and polyamine synthesis [72]. It is the universal and sole methyl donor to DNMTs. The methyl group from SAM can be transferred to a variety of substrates, including nucleic acids, proteins, phospholipids, biologic amines, and other small molecules [74].
SAM levels are regulated by the level of methionine that is an essential amino acid in one-carbon metabolism, and methionine deficiency reduces liver SAM levels and H3K4 trimethylation drastically [76]. 1C units can be generated from serine by cytosolic or mitochondrial folate metabolism, and the loss of mitochondrial pathway renders cells dependent on extracellular serine to make 1C units [77].
2.1.2. α-KG Source and Its Function in DNA Methylation
α-KG is generated in cell cytoplasm via glycolysis and in mitochondria from isocitrate catalyzed by isocitrate dehydrogenase (IDH) [78]. It is a membrane-impermeable crucial metabolite in the TCA cycle, contributing to the oxidation of nutrients such as amino acids, glucose, and fatty acids and it then provides energy for cell processes [79]. The level of α-KG changes upon fasting, exercise, and aging [80,81].
α-KG possesses a variety of physiological functions, besides its function in the TCA cycle in ATP production, and it reacts with ammonia and is converted into glutamate and glutamine. It can be metabolized into succinate, carbon dioxide (CO2), and water, and it also eliminates H2O2 by this process, acting as an antioxidant [79,82].
α-KG is an important metabolic intermediate and cofactor for several chromatin-modifying enzymes [83]. The family of α-KG-dependent dioxygenases includes Jumonji C-domain (JmjC) lysine demethylases, TET DNA cytosine-oxidizing enzymes, and prolyl hydroxylases (PHDs) [84]. In terms of DNA methylation, α-KG is an essential cofactor for αKG-dependent dioxygenases and the TET family of DNA demethylases [65,66,85]. α-KG is dramatically required and is increased for the activation of DNA methylation of the PRDM16 promoter during the early stage of adipogenesis [86]. In AML, decreased intracellular α-KG levels cause DNA hypermethylation through altering TET activity [87].
The level of α-KG is regulated by other metabolites. Fumarate and succinate, the intermediates of the TCA cycle and substrates of fumarate hydratase (FH) and succinate dehydrogenase (SDH), are competitive inhibitors of α-KG-dependent dioxygenases [88,89,90] (Figure 1). The accumulation of fumarate and succinate caused by mutation of enzymes inhibits α-KG-dependent enzymes, including TETs [91], thus leading to the global decreases in 5hmC and inactivation of FH and SDH and causing the loss of 5hmC [90,92,93]. Both fumarate and succinate accumulation are involved in glycolytic pathways by the inhibition of TET1 and TET3 [90]. FH-mediated TET inhibition promotes epithelial-mesenchymal transitions (EMT)-related transcription factors and enhances cell migration [88]. Mutations in isocitrate dehydrogenase 1 (IDH1), another TCA enzyme, lead to the accumulation of 2-hydroxyglutarate (2-HG), and 2-HG acts as a competitive inhibitor of α-KG-dependent enzymes, including TETs [66,93]. IDH mutations not only generate 2-HG but also result in hypermethylation of tumor suppressor genes [94]. Non-specific α-KG analogue dimethyloxallyl glycine (DMOG) has been used as a TET inhibitor, which blocks multiple α-KG-dependent dioxygenases [64].
2.1.3. Mitochondrial ROS and DNA Methylation
Reactive oxygen species (ROS) is regarded as the byproduct of oxygen consumption and cellular metabolism [95]. Mitochondria and NADPH oxidases (NOX) are two major contributors to endogenous ROS in tumor cells [96]. ROS plays an important role in physiology and the pathophysiology of aerobic life [97]. Excessive or inappropriately localized ROS damages cell growth. Higher levels of ROS contribute to tumor development through both genetic and epigenetic mechanisms [98,99,100]. ROS also acts as signaling molecules in DNA damage, thus promoting genetic instability and tumorigenesis. ROS-induced oxidative stress is closely related to both hypermethylation of tumor suppressor gene promoter regions and global hypomethylation.
ROS can function as the catalyst of DNA methylation by facilitating the transfer of methyl group to cytosine such as the formation of large complexes containing DNMT1/DNMT3B or increasing the expression of DNMTs, thus leading to hypermethylation of genes [101,102,103]. DNMT expression can be upregulated by superoxide anion, which is a form of ROS. The elevation of superoxide anion upregulates DNMT1 and DNMT3B and inhibits superoxide anion, thus leading to a decrease in DNMT upregulation and DNA methylation. In colon cancer, H2O2 reduces the expression of RUNX1 by elevating methylation at its promoter [104]. H2O2 also induces the upregulation of DNMT1 and HDAC1, thus leading to gene silence via histone deacetylation and promoter methylation [105,106]. In a brain function study, it was found that 5mC levels seemed to be increased and the 5hmC levels decreased coupled with increased ROS in the adult cerebellum, which suggested the promotion role of ROS in DNA methylation [107].
Epigenetic modifications within the mammalian nuclear genome include DNA methylation (5mC) and hydroxymethylation (5hmC) or DNA demethylation [65,108]. DNA hydroxymethylation can occur as a result of oxidative stress or the action of TET1 [65,108]. Oxidative stress has been suggested to activate TET via the increased production of α-KG and leads to an increase in 5hmC levels [109]. As the TET enzymes that convert 5mC to 5hmC may respond to oxidative stress, oxidative stress leads to the demethylation of genes. The redox-linked alterations to TET function can be reflected by the addition of ascorbate (vitamin C) to cellular 5hmC levels. Vitamin C is an antioxidant that can scavenge the primary ROS, and vitamin C treatment leads to an increase in 5hmC levels; thus, demethylation was promoted [110,111,112].
Besides ROS, oxygen availability modulates both DNMT’s and TETs’ enzymatic activity, and hypoxia induces hypermethylation by reducing TET activity [104,113,114]. DNA hypermethylation and hypoxia are well-recognized cancer hallmarks. TET belongs to the subfamily of 2OG oxygenases, which also act as an oxygen sensor [115]. Tumor hypoxia directly reduces TET activity, thus causing a 5hmC decrease predominantly at gene promoters and enhancers. Reduced TET activity leads to an accumulation of 5mC, thus decreasing the expression of associated genes. 5hmC is reduced under hypoxia in a dose-dependent manner, with decreasing concentrations of purified TET1 and TET2 [113].
2.1.4. Mitochondria Dysfunction and DNA Methylation
Mitochondrial dysfunction invokes mitochondria to nucleus responses [116]. It reduces oxygen and SAM-CH3 production in the cell, and the unbalanced redox homeostasis leads to perturbed methylation of nuclear DNA [117]. The mtDNA copy number is one of the signals by which mitochondria affect nDNA methylation patterns; changes in mtDNA copy number, often observed in cancer, induce changes in nDNA methylation [118]. Cells with depleted mitochondria (rho0 cell) result in the aberrant methylation of promoter CpG islands which were previously unmethylated in the parental cells, and the repletion of mitochondria back into rho0 cells reestablishes methylation partially to their original parental state, indicating the crucial role of mitochondria for DNA methylation [118,119].
The presence of mtDNA methylation is controversial [120,121,122]. In 2011, Shock et al. reported that mammalian mitochondria have mtDNA cytosine methylation; mitochondrial DNA methyltransferase (mtDNMT1) binds to mtDNA in the mitochondrial matrix; mtDNMT1 is upregulated by nuclear respiratory factor 1 (NRF1), PGC1-α, and the loss of p53. The expression of mtDNMT1 asymmetrically affects the expression of transcripts of mtDNA, and thus affects the function of mitochondria [123,124]. However, this discovery was overturned in 2021 by Lacopo Bicci et al. [125], and they found that there is no CpG methylation in human mtDNA via whole genome bisulfite sequencing (WGBS) for studying the methylation of mtDNA.
The demethylase TETs’ activity requires coenzyme factors such as Fe2+ and α-KG. IDH mutation leads to the increase of succinate, fumarate, and 2-HG, and they inhibit TET activity. DNMTs transfer the methyl group from SAM to substrates. SAM is regulated by 1C unit metabolism. ROS can function as the catalysts of DNA methylation by facilitating the transfer of methyl group to cytosine and by adding vitamin C; an antioxidant can scavenge the ROS and leads to the increase in 5hmC. The oxidative stress also activates TET via increasing α-KG and finally leads to an increase in 5hmC.
2.2. Mitochondria and RNA Methylation
Over 100 different types of RNA modification have been identified. RNA methylation, especially the N6-methyladenine (m6A) modification, is the most abundant RNA modification confirmed in viruses, yeast, and mammals [126,127]. m6A modification was established by pioneering studies in 1974 [128,129]. Around 15,000 human genes have m6A modification, which is a widespread regulatory mechanism that controls gene expression by affecting the splicing, stability, and translation efficiency of the modified mRNA molecules in diverse physiological processes [127,130,131,132]. m6A RNA modification affects cell division, immune homeostasis, and biological rhythm. The dysregulation of m6A modification has been suggested to drive human cancers [133].
2.2.1. The Effect of Mitochondria-Associated Metabolites on RNA Methylation
RNA methyltransferases, also named RNA methylation writers such as METTL3-METTL14, move the methyl group from SAM to mRNA, and the demethylases FTO and ALKBH5 remove the RNA methylation [134]. RNA methylation is decoded by proteins such as YTHDF1 and YTHDF2 [130]. FTO and ALKBH5 belong to the α-KG-dependent dioxygenase family [135]. The α-ketoglutarate dehydrogenase (OGDH) is the first rate-limiting enzyme in the TCA cycle, and ALKBH5 promotes viral replication metabolically by upregulating OGDH [136]. Furthermore, the enzymatic activity of FTO is inhibited in IDH mutation AML cells, thus leading to an increase in m6A levels [137,138].
In addition, several mitochondrial proteins also regulate RNA methylation. For example, mitochondrial RNA methyltransferase METTL8 facilitates 3-methyl-cytidine (m3C) methylation of the mt-tRNA and thus promotes mitochondrial ETC activity [139].
2.2.2. The Roles of RNA Methylation in Mitochondria
Mitochondrial function is closely associated with RNA methylation, including both mRNA and tRNA methylation. Mitochondria possess specific translation machinery for the synthesis of proteins in ETC, and tRNA modification is indispensable during mitochondrial translation and the OXPHOS process, which require folate-dependent tRNA methylation [140]. A recent study indicates that mitochondrial tRNA methylation is necessary for tumor metastasis due to its critical role in mitochondria gene translation [141]. Moreover, tRNA methyltransferase 10C (TRMT10C), catalyzing the mitochondrial ND5 mRNA at N1-methyladenosine (m1A) site, promotes cancer cell metabolism by reducing the mitochondrial ribonuclease P protein 1 (MRPP1) in mitochondria and inducing protein instability and mt-tRNA processing [142]. In short, RNA methylation plays pivotal roles in mitochondrial synthesis and function.
2.3. Mitochondria and Histone Modifications
Besides DNA methylation, mitochondrial metabolism also plays a pivotal role in the modifications of histone tails [143]. Chromatin structure and function are regulated by post-translational modifications (PTMs) of histones, such as histone methylation, acetylation, succinylation, ubiquitylation, and SUMOylation [144]. By altering interactions between nucleosome components, including histones and DNA, histone PTMs affect chromatin structures. Histone modifications are both highly dynamic and tightly regulated by the histone modification enzymes as well as their substrates, which are tightly regulated by mitochondria [145] (Figure 2).
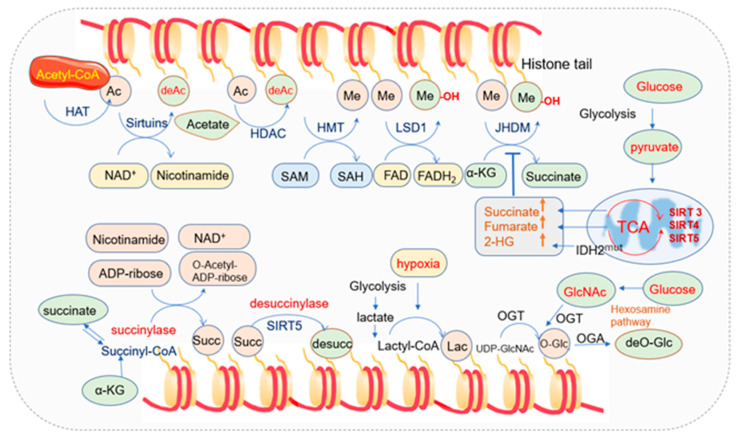
Figure 2.
Mitochondria metabolites and histone post-translation modification.
2.3.1. Mitochondria and Histone Acetylation
-
a.
Concept and enzymes of histone acetylation
Histone acetylation usually occurs on the lysine residues of histone tails. Acetyl groups are transferred from acetyl-CoA by histone acetyltransferases to the ε-amino group of lysine residues. Acetylation in histone tails generally reduces interaction between histones and DNA and increases accessibility to transcription factors [146,147]. Three major types of acetylation have been described based on the acetylation site in the protein, including: (a) N-terminal acetylation that is commonly named N-ter acetylation or Nα-acetylation; (b) lysine acetylation that is commonly named K-acetylation (KAc) or Nε-acetylation; (c) O-acetylation [148]. Histone acetylation is one of the key epigenetic modifications regulated by histone acetyltransferases (HATs) and histone deacetylases (HDACs) [149,150,151,152]. HATs catalyze the transfer of an acetyl group from acetyl-CoA to the ε-NH2 group of lysine residues in proteins while HDACs remove it [153]. HDACs are organized in four classes depending on sequence identity and domain organization. Class I (HDAC1, 2, 3, and 8), class II (HDAC4, 5, 6, 7, 9, and 10), and class IV (HDAC11) are zinc-dependent HDACs, while class III (SIRT1–7) deacetylases are NAD+-dependent [154]. The NAD+-dependent deacetylases sirtuins consist of seven members (SIRT1 to SIRT7) with different subcellular locations: SIRT1 and SIRT2 are in the nucleus, and cytosol SIRT3, SIRT4, and SRIT5 are in mitochondria, while SIRT6 and SIRT7 are in the nuclear location. Sirtuins play important roles in inflammation, cell growth, circadian rhythm, energy metabolism, neuronal function, and stress resistance [155,156,157].
-
b.
Function of histone acetylation
Histone acetylation loosens contacts between histones and DNA, and it masks the positive charges present on the lysine residues, reducing the affinity between histones and negatively charged DNA, facilitating the recruitment of transcriptional co-activators, and making transcription factor binding sites more accessible, thereby enhancing gene transcription [149]. HDACs remove the acetyl groups, tightening the interaction between DNA and histones, thus repressing transcription. Therefore, HATs play the transcription-promoting role via histone acetylation while HDACs conduct the transcription-delimiting function through deacetylation [158]. HATs function as both oncogenes and tumor suppressors in cancer. The deregulation of these enzymes by genetic or epigenetic alterations accompanied by defects in gene transcription has been implicated in oncogenesis [159]. Aberrations in histone modifications occur frequently in cancer, including changes in their levels and distribution at gene promoters, gene coding regions, repetitive DNA sequences, and other genomic elements [160]. Low histone acetylation levels are associated with a poorer prognosis of cancer patients due to increased risk of tumor recurrence and/or decreased survival probability [161].
-
c.
Mitochondria regulate histone acetylation
The TCA intermediate metabolites in mitochondria such as acetyl-CoA and NAD+ regulate the nuclear epigenome as the substrate of acetylation and a cofactor of deacetylation, respectively [54,162]. Other co-factors, including flavin adenine dinucleotide (FAD) and α-KG are closely associated with the above process, and the biosynthesis of the metabolic coenzymes depends on intracellular ATP levels and mitochondrial function [20,163,164].
Histone acetylation levels are strictly dependent on energy status. Reduced energy supplies not only reduce acetyl-CoA levels but also lead to the oxidation of NADH to NAD+. Since NAD+ but not NADH is a substrate for histone deacetylases—the sirtuins, energy deficiency activates the sirtuins to deacetylate the histones, thus increasing the positive charge of the chromatin proteins, causing chromatin condensation, and finally suppressing transcription, replication, growth, and proliferation [20]. When the energy supply is sufficient, acetyl-CoA is upregulated, and ATP and acetyl-CoA phosphorylate and acetylate chromatin, thus opening the nDNA for transcription and replication, and histone acetylation will be increased. When cells are in starvation or calories are limited, acetyl-CoA is required to be oxidized in the mitochondria for ATP synthesis. Chromatin phosphorylation and acetylation are lost, gene expression is suppressed, and the nucleo-cytosolic acetyl-CoA will be reduced [20].
Mitochondria are required to maintain histone acetylation (H3K27ac) in human colon cancer cells after inhibiting the electron transport chain (ETC) in mitochondria or depleting mitochondrial DNA, and histone acetylation is reduced accordingly. Pan-histone acetylation and H3K27ac marked acetylation are reduced in ρ0 DLD-1 cells compared with their complete parental cells [165]. In human glioblastoma tumors, histone acetylation is generally upregulated, and ROS pathways have negative correlations with H2B acetylation [166]. In addition, the increased level of lactic acid generated from glycolysis contributes to the higher local acidic pH to promote histone deacetylation and favors an aggressive and pro-metastatic phenotype of cancer cells [167,168].
Genes in mitochondria also affect histone acetylation. For example, C1qbp, which is primarily located in the mitochondrial matrix but can also be found at the cell surface, cytosol, and nucleus, is required for mitochondria oxidative phosphorylation (OXPHOS) as an RNA-binding protein to facilitate mitochondrial translation [169,170,171]. There is a reduction of acetyl-CoA in C1qbp-deficient CD8+ T cells and a significant decrease of H3K27ac in effector genes [172,173].
-
d.
NAD+ function in histone acetylation
Nicotinamide adenine dinucleotide exists in two forms inside the cell (in the cytoplasm, nucleus, Golgi, mitochondria, and other peroxisomes), oxidized form NAD+ and reduced form NADH. NAD+ can be synthesized de novo from tryptophan or through the recycling of its precursors. In de novo pathway, it is synthesized through the Preiss–Handler pathway from nicotinic acid (NA) or via salvage of the NAD+ precursors such as nicotinamide mononucleotide (NMN), nicotinamide riboside (NR), reduced nicotinamide mononucleotide (NMNH), or reduced nicotinamide riboside (NRH). Besides the Preiss–Handler pathway, NAD+ salvage also occurs through the recycling of other precursors such as nicotinamide (NAM) [174]. It plays an important role in intermediary metabolism, especially in numerous oxidation/reduction reactions [174].
NAD+ is required for over 500 enzymatic reactions and plays key roles in the regulation of almost all major biological processes [175]. It is used as a substrate by several families of enzymes (the so-called NAD+ consumers): sirtuins (SIRTs), poly (ADP-ribose) polymerases (PARPs) and cyclic ADP-ribose (cADPr) synthases [176,177,178,179], and all of them generate NAM as a result of NAD+ utilization.
The proper acetylation level within cells is modulated by the balanced activities of HAT and HDAC, and HDACs are regulated by fluctuations in NAD+ concentrations [180,181]. NAD+ served as a catalytic cofactor for HDAC III (sirtuins)-mediated histone deacetylation reactions [181,182]. Sirtuin family is NAD+-dependent protein lysine deacetylases, playing important roles in various physiological functions, from energy metabolism to stress response [183]. The elevated level of NAD+ has been demonstrated to activate Sirt1 and reduce acetylation [184].
-
e.
Acetyl-CoA function in histone acetylation
Acetyl-CoA is a metabolite derived from several pathways such as glycolysis, fatty acid oxidation, and amino acid catabolism [185,186,187]. The generation of acetyl-CoA via glycolysis is achieved by pyruvates. Pyruvates are synthesized from glycolysis. When oxygen is sufficient in normal cells, they traverse the mitochondria via the voltage-dependent anion channel (VDAC) or porin and the impermeable inner mitochondrial membrane with the aid of two mitochondrial pyruvate carriers (i.e., MPC1 and MPC2). Then, they are converted to acetyl-CoA to fuel the TCA cycle for efficient energy supply. In the mitochondria, acetyl-CoA is catalyzed by citrate synthase with oxaloacetate to yield citrate, and citrate can be transported to the cytosol and cleaved by ATP-citrate lyase (ACL) to regenerate acetyl-CoA and oxaloacetate [188]. Mammalian cells generate acetyl-CoA in mitochondria with a complex of nucleus-encoded proteins known as pyruvate dehydrogenase complex (PDC) [189]. PDC can be translocated to the nucleus generating acetyl-CoA in the nucleus independent of mitochondria. The knockdown of nuclear PDC in isolated functional nuclei decreased the de novo synthesis of acetyl-CoA and acetylation of core histones [190]. The dynamic translocation of mitochondrial PDC provides a pathway for nuclear acetyl-CoA synthesis required for histone acetylation and epigenetic regulation [190].
Acetyl-CoA controls key cellular processes, including energy metabolism, mitosis, and autophagy [186]. Mitochondrial acetyl-CoA is used to synthesize ketone bodies as an alternative fuel. Besides roles in ATP production, acetyl-CoA also represents a key node in metabolism due to its intersection with many metabolic pathways and transformations [187]. Glycolytic pyruvate enters the TCA cycle through acetyl-CoA, and acetyl-CoA is a key precursor of lipid synthesis and the sole donor of the acetyl groups for acetylation [186,191].
Acetyl-CoA, acting as a substrate for HATs, is crucial for histone acetylation. Alteration of pools of intracellular acetyl-CoA manipulates histone acetylation [164,192], and lower nucleo-cytosolic acetyl-CoA limits histone acetylation and cell proliferation. Many protein acetylation modifications are indeed regulated by acetyl-CoA availability [193,194].
Histone acetylation is also affected by modulating enzymes that regulate acetyl-CoA syntheses such as acetate-dependent acetyl-CoA synthetase 2 (ACSS2) and citrate-dependent ACL [164,195]. ACSS2 and ACL are two principal enzymes that generate Acetyl-CoA for histone acetylation [186]. ACSS2 directly regulates histone acetylation in neurons and spatial memory in mammals [196].
2.3.2. Mitochondria and Histone Methylation
-
a.
Histone methylation
The addition of methyl group from SAM on lysine or arginine amino acid residue in histone, usually on H3 or H4, is marked as histone methylation [197]. Lysine residues undergo single, double, or trimethylation modification, while arginine residues only undergo single and double methylation modification (symmetrically or asymmetrically), acting as active or repressive marks of gene expression. Common lysine methylations on H3, including H3K4, H3K79, and H3K36, are markers of active transcription, whereas H3K20, H3K9, and K3K27 are associated with suppressive transcription [198]. Histone methylation, as one of the most important histone marks, plays a critical role in gene expression, cell cycle, genome stability, and chromosome maintenance [199].
-
b.
Enzymes of histone methylation
Histone methylations are catalyzed by histone methyltransferase (HMTs) enzymes [199]. HMTs include lysine methyltransferases (KMTs) such as SET-domain-containing enzymes and Dot1-like proteins and arginine methyltransferases such as protein arginine methyltransferase (PRMTs) [200,201,202]. Histone lysine and arginine methylation can be removed by histone demethylases (HDMs) [203,204]. Lysine demethyltransferases (KDMs) have been clustered into two families: the Jumonji domain depending on iron and oxoglutarate as cofactors and amine oxidases relying on FAD as a cofactor [163,205,206,207]. The two families are also named Jumonji-domain histone demethylase (JHDM, Jumonji domain containing family) and LSD (lysine-specific demethylase). LSD1 can specifically remove the single and double methylation modification of histones H3K4 and H3K9, while Jumonji family can remove the modification of lysine trimethylation. Sites on H3K 4, 9, 27, 36, 79, and H4K20 can be methylated, among which histones H3K4 and H3K9 are two common modification sites.
-
c.
Mitochondrial metabolites and histone methylation
Metabolites in mitochondria regulate histone methylation. Besides serving as a cofactor for TET-mediated DNA demethylation, α-KG also serves as a cofactor for JHDM family and HDM activity to modify epigenetic marks [208,209]. IDH1-mediated α-KG modulates trimethylation of H3K4 in the promoters of genes associated with brown adipogenesis [210]. Ectopic expression of SDH inhibits histone demethylation and hydroxylation of 5mC, suggesting that defective SDH contributes to tumor growth positively [93]. Nicotinamide N-methyltransferase (NNMT) is a metabolic enzyme that increases mitochondrial function and reduces oxidative stress [211], meanwhile catalyzing the transfer of methyl moiety from SAM to nicotinamide. Cancer cells with the overexpression of NNMT exhibit alterations in SAM level and histone methylation, and with the procurement of a more aggressive phenotype [212].
The histone methylation and acetylation are not separated modification processes, and they are dynamically interactive. For instance, histone H3K27ac distinguishes active enhancers from inactive/poised enhancer elements containing H3K4me1 alone [213].
2.3.3. Mitochondria and Histone Succinylation
-
a.
Concept of histone succinylation
Lysine succinylation (Ksucc) is a newly discovered histone post-translational modification that changes the chemical environment of histones similar to other acylation modifications [214,215,216]. Histone lysine succinylation has been considered as an intermediate reaction of succinyl group (-CO-CH2-CH2-COOH) transfer from succinyl-CoA to homoserine [217]. It refers to the process of covalently binding a succinyl group to the ε-amine of lysine with the enzymatic or non-enzymatic mechanisms [218,219]. It brings more significant structural changes in space than other modifications like methylation and acetylation since succinylation changes the charge state of lysine residues to a high degree [214,219]. Most lysine succinylation is located in mitochondria, followed by the cytoplasm and the nucleus.
Lysine succinylation was identified in E coli proteins first and later in mammalian proteins, which indicates that lysine succinylation is a highly evolved conserved marker in eukaryotes. [214,216]. Lysine succinylation generally accumulates at transcriptional start sites to modulate gene expression. Histone succinylation at H3K79 contributes to transcription and tumor development [220].
-
b.
Enzymes of histone succinylation
The writers and erasers that are responsible for catalyzing the succinylation and desuccinylation are still under investigation, but accumulated evidence has indicated that succinylation is modulated by acetyltransferase and deacetylases [221]. Lysine acetyltransferase 2A (KAT2A, also named GCN5) has been identified as a histone succinyltransferase that catalyzes the succinylation of histone H3K79 [220]. Histone acetyltransferase 1 (HAT1) succinylated histone H3 at K122, which could provide epigenetic and gene expression regulation in cancer cells [222]. The NAD+-dependent deacetylase SIRT5 located in mitochondria has been recognized as desuccinylase, and succinylation is sensitive to both the increase and decrease of SIRT5 [216,223,224,225]. Another deacetylase SIRT7 is an eraser of succinylation of histone H3K122 for modulating DNA damage response and genome stability [226].
-
c.
Mitochondrial metabolites and histone succinylation
Succinyl-CoA is the succinyl donor produced in the cytoplasm, nucleus, or in the mitochondrial tricarboxylic acid (TCA) [215]. The concentration of succinyl-CoA produced in TCA regulates the level of histone succinylation [215].
Intracellular succinyl-CoA is mainly synthesized in mitochondria and is produced from α-KG, succinyl-carnitine, and succinate [227]. Succinyl group output from mitochondria to histone lysine can be achieved through permeable nuclear pores [228]. The oxoglutarate carrier SLC25A11 transports α-KG from mitochondria [229,230], and α-KG is converted to succinyl coenzyme A in the nucleus under the catalyzation of α-KG dehydrogenase (α-KGDH). Succinyl-CoA provides materials for GCN5, and then GCN5 activates succinyl-transferase to succinylate a histone lysine [220].
The dysfunction of mitochondria affects histone succinylation, and defective TCA cycle metabolism results in histone hypersuccinylation and non-histone hypersuccinylation associated with transcriptional responses [231].
2.3.4. Mitochondria and Histone O-GlcNAcylation
-
a.
Concept of O-GlcNAcylation
O-linked-N-acetylglucosaminylation (O-GlcNAcylation) is a post-translational modification by glycosylation that links a single GlcNAc molecule to the serine/threonine site on proteins by an O-linked β-glycosidic bond [232]. O-GlcNAcylation is a key integrator of cellular nutritional status and occurs in the nucleus, cytoplasm, and mitochondrion. It participates in the process of nutrient sensing and metabolism and plays crucial roles in physiology and physiopathology [233,234].
-
b.
Enzymes of O-GlcNAcylation
The addition and removal of monosaccharides are regulated by O-GlcNAc transferase (OGT) and O-GlcNAcase (OGA), respectively. O-GlcNAcylation is highly enriched on histone and other proteins in nuclear pore complexes [235,236,237,238]. OGT has three isoforms: nucleocytoplasmic OGT, mitochondrial OGT (mOGT), and the shortest form of OGT. The mOGT isoform is targeted to the mitochondrial matrix and is pro-apoptotic [239,240], and it tends to accumulate in the mitochondrial inner membrane. OGT utilizes UDP-GlcNAc to catalyze the addition of O-GlcNAc to target proteins.
Histone O-GlcNAcylation that occurs on H2A and H2B may be linked to histone exchange, and core histones H3 and H4 can also be modified with O-GlcNAc [241,242,243,244]. Three sites of O-GlcNAcylation were mapped by tandem mass spectrometry on histone H2A Thr101, histone H2B Ser36, and histone H4 Ser47, respectively [245]. The modification sites of O-GlcNAcylation on histone are distinct from H3 and H4 tail modification, which is linked to the regulation of gene expression more directly. O-GlcNAcylation on H3 Ser10 site is mitosis-specific and the O-GlcNAc is conditionally phosphorylated as well, which points out the crucial role of OGT in modifying histone H3 during mitosis [246,247,248]. The role of OGT in gene transcription regulation is probably associated with polycomb repression, which is linked with the trimethylation of histone H3 at Lys-27 [249,250,251].
-
c.
Mitochondria and O-GlcNAcylation
The synthesis of UDP-GlcNAc is from the hexosamine biosynthetic pathway (HBP), which is a series of enzymatic reactions requiring key metabolites, including glucose, glutamine, ATP, and acetyl-CoA [252,253]. The pool of UDP-GlcNAc available for O-GlcNAcylation is influenced by many factors, including metabolic flux. Glutamine is one of these key metabolites, and the regulated entry of glutamine may be influenced by the synthesis of UDP-GlcNAc [254]. Acetyl-CoA, generated from the conversion of pyruvate via the mitochondrial pyruvate dehydrogenase complex during the oxidation of glucose and the β-oxidation of fatty acids, is one of the precursors of UDP-GlcNAc [255].
Mitochondria are considered the primary source of ATP production in the cell. Adenosine-monophosphate-activated protein kinase (AMPK) is a sensor of energy status whose activity is controlled by ATP/AMP ratio, and it serves as a guardian of metabolism and mitochondrial homeostasis. AMPK has been identified as a regulator of H2B Ser112 O-GlcNAcylation, and the activation of AMPK decreases H2B Ser112 O-GlcNAcylation and H2B K120 ubiquitination [244].
-
d.
O-GlcNAcylation and other modifications
Besides the functions in O-GlcNAcylation, OGT also binds to the TET class of DNA cytosine demethylases that may serve as 5-methylcytosine erasers [256,257,258]. O-GlcNAcylation may promote DNA demethylation by interacting with members of the TET family proteins, thus favoring gene transcription. O-GlcNAcylation influences other PTMs of histones indirectly and treating cells with glucosamine to increase O-GlcNAcylation is associated with decreased phosphorylation of histone H3 Ser10 [248]. O-GlcNAcylation at Ser642 of histone deacetylase 4 (HDAC4) is cardioprotective in diabetes mellitus [259]. In addition, the O-GlcNAcylation of HDAC1 overexpressed in hepatocellular carcinoma (HCC) promotes cancer progression, thus inhibiting O-GlcNAcylation of HDAC1, repressing the progression of HCC [260].
2.3.5. Mitochondria and Histone Lactylation
-
a.
Concept and function of histone lactylation
Lactylation is a novel histone acylation code proposed in 2019 [261]. Twenty-eight lactylation sites on core histones in human and mouse cells have been identified [261]. Lactylation of histone lysine residues derived from lactate directly modulates gene transcription from chromatin in a p53-dependent and p300-mediated manner [262]. Lactate is a critical energy source for mitochondrial respiration and a primary circulating TCA substrate [263].
Lactylation plays important roles in inflammation and cancer. In BMDMs, the treatment with lactate derived from tumor cells drives tumor-associated macrophages to an M2-like phenotype, and this polarization increases depending on the treating time [261,264]. Furthermore, histone lactylation regulates gene expression during M1 macrophage polarization. It also promotes oncogenesis by facilitating m6A reader protein YEHDF2 expression in ocular melanoma [265]. In addition, the elevation of exogenous lactate rescued the defect of B cell adapter for PI3K (BCAP)-deficient BMDMs to enhance histone lactylation [266]. In lung fibrosis, histone lactylation at the promoter regions of representative genes was increased in lactate-treated macrophages.
Histone lactylation has been demonstrated as an epigenetic mark of the glycolytic switch. Lactate and acetyl-CoA are the key metabolites to bridge the glycolytic switch with two distinct epigenetic coding programs: lactylation and acetylation. Both can be generated from glycolysis. In malignant tumor cells, pyruvates are converted to lactate, and the glycolytic switch is adapted to meet the higher demands of fast cell growth and proliferation [267]. Lactate accumulation in tumor microenvironment leads to reprogrammed cell metabolism and induces a glycolytic switch or the Warburg effect [24].
-
b.
Regulation of histone lactylation
Histone lysine lactylation is specially modulated by lactate level. Lactate is a major energy source for mitochondrial respiration and the major gluconeogenic precursor [268], and it has major influences on energy substrate partitioning. Lactate secreted by fermenting cells can be oxidized or used as a gluconeogenic substrate by other cells and tissues, and the relation between lactate and mitochondria has been extensively reviewed elsewhere [269,270]. The accumulation of lactate by exercise affects the expression of regulatory enzymes of glycolysis and mitochondrial biogenesis [271]. Lactate is the fulcrum of metabolic regulation in vivo [268].
Lactate metabolism influences epigenetics under diverse cellular conditions. Hypoxia induces the production of lactate by glycolysis and stimulates histone lactylation [261]. Mitochondrial inhibitors or hypoxia with increased lactate production amplify lysine lactylation [272]. Histone lactylation and acetylation compete for epigenetic modification of lysine and mark the levels of lactates and acetyl-CoA. Histone lactylation is regulated by the level of both lactate and acetyl-CoA, which functions as the donor of the acetyl group and affects the level of acetylation.
2.4. Epigenetic Modification Regulates Mitochondrial Function
Metabolites related to mitochondria play important roles in epigenetic regulation as mentioned above, and in turn, epigenetic modification also influences the function of mitochondria.
DNA and histone methylation affect mitochondrial function via the regulation of SAM levels. SAM-regulated histone methylation has a positive effect on energy metabolism. The knockdown of NNMT, which catalyzes the methylation of nicotinamide with methyl from SAM, elevates SAM levels and increases H3K4 methylation in adipose tissue, and this enhances the key enzymes in the polyamine flux to increase systemic energy metabolism [273]. Maternal one-carbon metabolism related to SAM also affects the offspring’s energy metabolism [274]. Moreover, elevated lysine-specific demethylase LSD1 stimulates OXPHOS gene expression in NRF1 [275]. In addition, the differential DNA methylation patterns in skeletal muscle in obese and high-fat diet individuals alter the mitochondrial β-oxidation and mitochondrial number, while exercise training altering epigenetic modifications can improve mitochondrial function [276,277].
Histone acetylation has close relations with mitochondrial functions. HDAC inhibitors suppress oxidative stress and tissue damage caused by mitochondria dysfunction in mouse models [278]. HDA-1, the C. elegans ortholog of mammalian histone deacetylase (HDAC), is required for mitochondrial-stress-mediated activation of mitochondrial unfolded protein response, and it modulates mitochondrial stress response and longevity [279]. HDAC3 is essential for shaping mitochondrial adaptations for IL-1β production in macrophages through non-histone deacetylation. Furthermore, the loss of histone deacetylase SIRT3 or SIRT6 can activate the key glycolytic enzymes and lead to an increase in aerobic glycolysis or Warburg effect [280]. ATP-citrate lyase (ACL) is the enzyme that converts glucose-derived citrate into acetyl-CoA, and histone acetylation level depends on ACL [164]. However, conversely, histone acetylation also stabilizes ACL to promote tumor growth. When the acetylation is restrained, the ACL is inhibited at both the transcriptional and post-translational levels [281,282].
Different from methylation and acetylation, succinylation causes larger mass change and alters a positively charged side chain into a negatively charged one, thus causing a two-unit charge shift in the modified residues. Succinylation alters the rates of enzymes and pathways, especially mitochondrial metabolic pathways. For example, several SIRT5-targeted lysine residues related to the SDH subunit and succinylation at these sites may disrupt Complex II subunit–subunit interactions and electron transfer [283]. Succinylation also suppresses SDH activity. SIRT5-KO liver exhibits a compromised Complex II and ATP synthesis function in vivo [284], and SIRT5 KO reduces fatty acid oxidation and accumulation of long-chain fatty acyl-CoAs, as 60% of all proteins in fatty acid metabolism are succinylated [224]. This demonstrates that SIRT5 is a promoter of mitochondrial energy metabolism.
Other modifications of histones such as phosphorylation, sumolyation, and ubiquitination also have an extensive and dynamic interplay with mitochondria. The dysregulation of the balance between them and mitochondria leads to the disorder of metabolism and finally cellular homeostasis.
Mitochondrial regulation on epigenetics not only can occur via mitochondria-regulated metabolites, but also might occur via aerobic glycolysis (Warburg effect), which is tightly associated with mitochondrial OXPHOS activity. Inhibition of OXPHOS or mitochondrial synthesis may lead to the Warburg effect, and tumor cells switch their energy production from OXPHOS to glycolysis when mitochondrial energy is insufficient [285]. The Warburg effect leads to the increased production of lactate in cancer, and the lactate converted from pyruvate in tumor cells is the precursor for histone lactylation [261], and thus the Warburg effect regulates histone lactylation. Whether mitochondria have an effect on other epigenetics through the Warburg effect deserves further investigation. In turn, epigenetics also regulates the Warburg effect. For example, DNA methylation regulates the enzymes of glycolysis and the mitochondria dysfunction caused by aberrant DNA methylation triggers aerobic glycolysis [286,287]. M2 isoform of pyruvate kinase (PKM2), a key rate-limiting enzyme, contributes to the metabolism shift from OXPHOS to aerobic glycolysis, and the acetylation of PKM2 is stimulated by high glucose and thus promotes the Warburg effect.
HAT transfers acetyl group from acetyl-CoA to histone, leading to histone acetylation. HDACs, including the NAD+-dependent deacetylases sirtuins, remove the acetyl group from histones, and thus histone deacetylation occurs. The TCA intermediate metabolites in mitochondria such as acetyl-CoA and NAD+ regulate the acetylation. HMT transfers the methyl group from SAM to the histone, leading to histone methylation. Demethyltransferases such as LSD1 and JHDM remove the methyl group from histone, and thus histone demethylation occurs. JHDM requires FAD as a cofactor. Histone succinylation refers to the addition of succinyl group transferred from succinyl-CoA to histone. Histone succinyltransferase such as KAT catalyzes the succinylation of histone. Sirt5 located in mitochondria is a desuccinylase. O-GlcNAcylation is regulated by OGT and OAT. OGT utilizes UDP-GlcNAc to catalyze the addition of O-GlcNAc onto target proteins. Acetyl-CoA is one of the precursors of UDP-GlcNAc. Histone lactylation depends on intracellular lactate levels, and lactate and acetyl-CoA are the key metabolites to bridge the glycolytic switch. The IDH mutation also leads to an increase of succinate, fumarate, and 2-HG, and inhibits JHDM activity.
3. Epigenetics in Normal Development and Tumorigenesis
Cell fate is determined by the genes expressed, which are mainly regulated by epigenetic modifications of the genome. Epigenetic regulatory mechanisms are heritable changes in a sequence of stable but reversible gene function modifications yet do not affect the DNA primary sequence [288]. Epigenetics is one of the primary mechanisms causing early programming of cell proliferation, differentiation, death, and disease [289]. Epigenetics plays a key role in normal development such as embryonic development and stem cell differentiation. Its dysregulation often leads to diseases, including cancer.
Two models have been proposed to account for tumorigenesis: the clonal evolution model and cancer stem cell (CSC) model [290,291,292,293,294,295,296]. CSCs generate cellular heterogeneity, harboring stem-cell-like properties such as self-renewal and aberrant differentiation potential, and the differential hierarchy can be reversible under certain conditions [297,298,299]. Both genetic and epigenetic alterations are attributed to the stemness features installed in cancer cells. Cancer initiation and progression induced by oncogenic mutations are accompanied by significant epigenetic alterations. Epigenetic dynamics such as DNA methylation and histone modification patterns and nucleosome remodeling regulate cancer cell state [300,301]. Epigenetic modifications are associated with the silencing of tumor suppressor and differentiation genes in various cancers, and they can also deregulate fundamental signaling pathways controlling self-renewal and differentiation, including Wnt, Notch, Myc, and Hedgehog pathways [302]. Besides stem cells, epigenetics also regulates other cells: epigenetic pathways functioning in T cell fate stability and plasticity have been reviewed [303]. In addition, epigenetic regulation on gene expression controls innate immune cell differentiation, activation, and function [304,305].
Cell fate determination requires faithful execution of gene expression programs affected by alteration in genome and epigenome, which are increasingly recognized to respond to metabolic inputs. Metabolites such as acetyl-CoA, α-KG, SAM, NAD+, and O-GlcNAc play crucial roles in cell fate determination by the regulation of epigenetic modifications and gene expression.
3.1. DNA Methylation in Cell Development and Tumorigenesis
Most cell types display relatively stable DNA methylation patterns with up to 80% of CpG islands being methylated [306]. DNA methylation is essential for tissue development and aberrant DNA methylation contributes to tumorigenesis. DNA methylation controls chromatin conformation together with other histone modifications [307].
3.1.1. DNA Methylation in Normal Development
DNA methylation plays important roles in physiology, including stabilizing cell-fate decisions, cell development, cell differentiation, and cell signaling [308,309,310,311]. It functions as a defense mechanism in preventing genomic instability due to transposon movements or the insertion of endoparasitic sequences in the genome. In females, DNA methylation is involved in the regulation of housekeeping genes and tissue-specific genes, and it can silence one allele of imprinted genes and compensate for the extra copy of the X chromosome [307,312]. The methylation level of the genome of oocytes is less than that of spermatozoa [313]. DNA methylation on CpG island in lineage-specific genes is essential for cell stemness and differentiation in human female hematopoietic stem/progenitor cells (HSPCs) [307,314].
In undifferentiated human embryonic stem cells (ETS), the promoter of key transcription factors OCT4 and NANOG genes are unmethylated or in a hypomethylation state [315], but they are undergoing rapid DNA methylation on differentiation in vitro and after implantation in vivo [315,316,317]. The expression of stem cell transcription factors such as OCT4, NANOG, and SOX2 is closely associated with the self-renewal of stem cells [318,319], and their expression is controlled by their promoter methylation level. The partial or full methylation of these pluripotency-associated genes leads to the downregulation of their expression and differentiation of ES cells [317,320,321]. Human ETS has unique CpG methylation characteristics, and it works together with histone modifications to drive stem cell differentiation [322,323]. The lack of DNA methylation in stem cells is associated with the differentiation ability, especially in the activation of cell-specific genes [38]. Similar to ES cells, DNA methylation is also crucial for the differentiation and maturation of the mammalian central nervous system (CNS) [324]. In fibroblasts, hundreds of DMGs involved in pluripotency and differentiation have been identified as being associated with lower transcriptional activity [325].
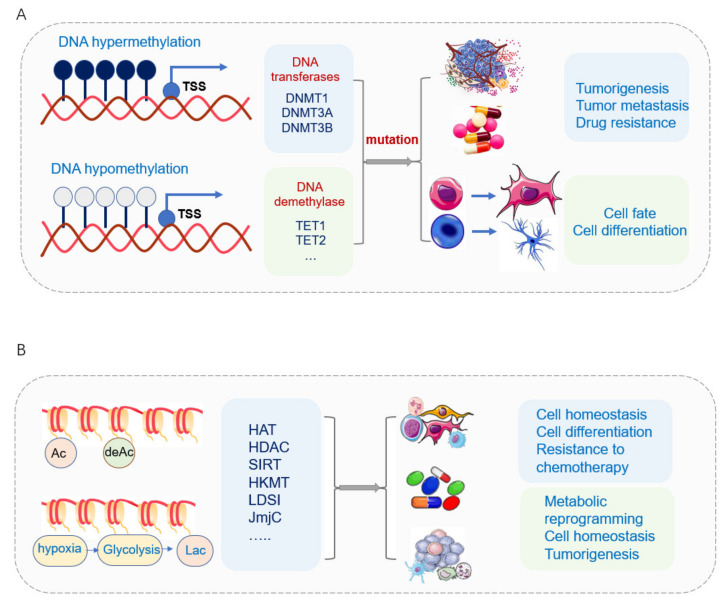
3.1.2. DNA Methylation in Tumorigenesis
DNA methylation is the most extensively studied epigenetic mark for human diseases [326]. Aberrant DNA methylation has been associated with pathological gene expressions in a variety of human cancers [327]. Hypermethylation leads to the inactivation of certain tumor-suppressor genes in its promotor regions, thus resulting in gene silence in different cancer types [59] (Figure 3A). The changes in DNA methylation and differentially methylated regions (DMRs) have occurred in normal development and diseases [328,329]. Different DMR classes display tissue-specific DMRs [330,331], cell-type-specific DMRs, and DMRs arising in tumor heterogeneity [332,333,334,335,336]. Different classes of CpG islands are subject to different modes of regulation [337]. The alternative promoters have been frequently used by tumors to increase the isoform diversity and to activate the oncogenes that are repressed normally, thus changing the tumor status and evading host immune attacks by immunoediting [338,339,340,341]. Pediatric tumors are more prone to mutations and using epigenetic deregulation to promote tumorigenesis and progression compared with cancers in adults [342,343,344]. A high methylation level with decreased TET1 activity has been found to increase glioblastoma tumorigenesis and malignancy [345,346].
Figure 3.
DNA methylation and histone modification affect normal development and tumorigenesis. (A) DNA hypermethylation of tumor suppressor genes and hypomethylation of oncogenes involved with tumorigenesis, tumor metastasis, and tumor drug resistance. DNA demethylation enzymes TET1 and TET2 play important roles in cancer stem cells. The loss of TET1/2 leads to hypermethylation and enhancement of cancer cell stemness. The status of DNA demethylases regulates CSC maintenance and differentiation. (B) The malfunction of HATs often perturbs the appropriate gene-expression program, leading to the development of disease. The key enzymes of histone acetylation KATs directly acetylate several important transcription factors to modulate the transcription activity and affect cell differentiation and cell homeostasis. The deacetylase sirtuin family affects cell fate via deacetylation, demalonylation, and desuccinylation. Histone acetylation is involved in CSC activity and drug resistance.
DNA methylation also regulates the neurodegenerative process. The dysregulation of 5hmC during brain development, including different 5hmC concentrations, affects gene regulation in neurodegenerative processes, and the reduction in TET activity in parallel with the reduction of 5hmC concentrations promotes neurodegeneration in the mouse model of Alzheimer’s disease [347,348,349,350].
3.1.3. DNA Methylation in Cancer Stem Cell
DNA methylation includes hypermethylation and hypomethylation. Generally, hypermethylation of promoter DNA indicates that the gene is silenced, whereas hypomethylation indicates that the gene is activated [351,352,353]. DNA hypermethylation of tumor suppressor genes and global hypomethylation of oncogenes contribute to the formation of cancer stem cells and cancer cells’ drug resistance [354]. Hypermethylation of the LDHA gene promoter silences its expression in IDH-mutant-derived brain tumor stem cells (BTSCs) [355]. DNA methylation can be reduced by mutant KRAS-mediated glutaminolysis to increase Wnt signaling pathway, thus increasing cancer cell stemness and drug resistance in colorectal cancer [356]. In addition, breast CSCs have specific DNA methylation signatures that distinguish them from their non-BCSC counterparts [357].
The expression of DNMTs plays an important role in cancer stem cell development. Genetic mutations of DNMTs lead to epigenetic alterations that control cellular fate. For example, mutation of DNMT3A accompanied by mutation of KRAS supports self-renewal and induces malignancy in AML, which shows the synergistic effect between genetic and epigenetic alteration in initiating self-renewal proliferation of CSC population and malignancy [358,359]. DNMT1 promotes EMT to CSC in triple-negative breast CSCs. The inhibition of DNMT1 suppresses triple-negative breast CSCs populations [360]. In liver cancer, DNMT1-mediated methylation of BEX1 promoter leads to different stemness of cells in hepatoblastoma (HB) and hepatocellular carcinoma (HCC) and a subtype of HCC with high CSC features (CSC-HCC) [361]. The ubiquitin-like PHD and RING finger domains 1 (UHRF1) factor recruits DNMT1 to preserve the status of DNA methylation during DNA replication, and the UHRF1-DNMT1 complex is crucial for preserving genomic imprinting and overall epigenetic memory during cell divisions. Their activity is impaired upon cellular transformations into malignant states [362,363,364], and UHRF1 suppression promotes cancer stem cell differentiation to reduce metastasis [365].
DNA demethylation enzymes TET1 and TET2 not only promote somatic cells reprogramming into iPSCs but also play important roles in cancer stem cells. TET2 is essential for hematopoietic stem cell (HSC) differentiation and lineage commitment and is frequently mutated in myeloid malignancies, and its inhibition contributes to HSC expansion in aplastic anemia. The level of 5hmC has been demonstrated as an independent prognostic marker for renal cancer and is intimately associated with its overall survival [366]. The low expression of TET1 and 5hmC inhibited by Fisetin decreased proliferation and invasion of renal cancer stem cells [353]. Inhibition of TET2 and the corresponding hypermethylation enhanced the stem cell signature of AML stem cells. In glioblastoma, the CSCs possess increased levels of 5fC and 5caC [300,367].
TET-mediated DNA oxidation is highly dependent on metabolic states that reprogram the epigenome to maintain the stemness and promote tumor growth and metastasis [300] (Figure 3A). Various metabolites affect TET activity. Succinate and α-KG serve as key regulators of self-renewal and differentiation through the modulation of TET enzymes. Succinate, an important metabolite in the TCA cycle, serves as a mitochondrial retrograde signal that exerts effects on the epigenome by inhibiting histone demethylases and TET family activity [90,93]. Succinate accumulation links to mitochondrial MnSOD depletion via SDH/succinate/TET axis, thus leading to aberrant nuclear DNA methylation and altered cell fate [368]. α-KG is also important for the facilitation of epigenetic remodeling during premalignant cells, in which p53 has been activated [369]. Inhibition or mutation of SDH results in the accumulation of succinate and inhibition of α-KG-dependent enzymes, as mentioned above [92,93,370,371].
3.2. Histone Acetylation and Methylation in Normal Development and Tumorigenesis
3.2.1. Histone Acetylation and Methylation in Normal Development
Histone acetylation plays important roles in biological processes that are involved in cell proliferation and differentiation [289]. Histone acetylation at transcriptional enhancers reflects global cell-type-specific expression [372]. Pluripotent embryonic stem cells (ES) exhibit chromatin domains with both transcriptionally active and silent histone modifications [373]. In the early differentiation period, gene transcription is regulated by histone modifications during their temporal transcription [374]. Pluripotent embryonic stem cells (PSCs) require acetyl-CoA and histone acetylation for the maintenance of pluripotency [375]. The differentiation of PSCs leads to a metabolic switch from glycolysis to OXPHOS, which in turn promotes their differentiation since inhibition of glycolysis leads to loss of histone acetylation and the pluripotent state [375,376,377].
HATs stimulate transcription through the acetylation of histones, thus leading to the relaxation of nucleosomes [378]. HATs and HDACs transmit differentiation signals to initiate appropriate epigenetic modifications, including the establishment of new histone modification or erasure of existing chromatin structure in in vitro differentiation of ES cells [379]. H3K9ac and H3K9me3 are almost undetectable in pluripotent ES cells and dramatically increase when cells leave the undifferentiated state in a short time [380]. H3K9me3 level increased within 2 days, corresponding to the deacetylation of this residue [381]. Maternal H3K27me3 controls DNA methylation-independent imprinting, and it is a hallmark of facultative heterochromatin that maintains transcriptional repression established during early development in many eukaryotes, allowing genes to encode specific transcription factors or early differentiation factors [373,382,383]. When the expression of pluripotent genes such as Oct4, Nanog, and Foxd3 is elevated, the genes’ chromatins are opened in stem cells and condensed after differentiation. The key enzymes of histone acetylation, KATs, directly acetylate several key transcription factors such as p53, FOXO1, and C/EBPα to modulate the transcription activity and affect cell homeostasis [300,384,385,386]. Besides ES, epigenetics also plays important roles in somatic stem cells, and HDACs, especially HDAC1 and HDAC2 expression levels, decrease significantly upon tissue differentiation, while HDAC3 and DNMT1 keep the same expression [387,388,389].
Histone acetylation and methylation affect each other; H3K4me1 and H3K27ac affect each other in different ways and play direct roles in nucleosome eviction and mRNA transcription at enhancers, respectively [390]. ES cell chromatin is in a highly dynamic state, with global DNA hypomethylation and a general abundance of transcriptionally active chromatin marks such as H3K4me3 and acetylation of histone H4, which leads to relatively relaxed chromatin of ES cells [38,391].
3.2.2. Histone Acetylation and Methylation in Tumorigenesis
Histone lysine acetylation positively regulates gene transcription by promoting DNA accessibility via creating relaxation of chromatin structure and a more conducive environment for transcription, and the malfunction of HATs often perturbs appropriate gene-expression programs, thus leading to the development of disease [392] (Figure 3B).
Histone methylation and acetylation levels are closely associated with tumor initiation and growth. H3K27me3 induces gene silencing and regulates cell differentiation, and its dysregulation frequently happens in tumorigenesis [393,394]. Histone methylation reader protein ZMYND11 interacts with histone H3.3K36me3, thus leading to the suppression of tumor growth [395]. The epigenetic mark H4K16ac of H4 is prone to higher acetylation with age in healthy cells, while it tends to disappear in regions of the genome near age- and AD-dependent genes [396].
Histone deacetylase plays an important role in tumorigenesis (Figure 3B). The increased activity of HDAC2 and the decrease of H3K18/K23 acetylation have been found in AD [397,398]. KDACs, the erasers of acetylation, play a critical role in oncogenesis, and the inactivation of HDAC1 enhanced DOT1 activity and lymphomagenesis in mice [399]. Another typical example of epigenetics in modulating CSC properties is the epithelial-mesenchymal transition (EMT) process. ZEB1 is the key transcription factor of EMT, and it drives non-CSC to CSCs. Histone acetylation of the ZEB1 poises its chromatin and promotes EMT’s acquisition of CSC features in breast cancer [400,401,402,403]. Hypoxia inhibits the oxygen-dependent H3K27me3 demethylases and increases ZEB1 expression and prompts EMT’s acquisition of a CSCs phenotype [403].
The deacetylase sirtuin family plays an important role in cancer stem cells (Figure 3B). The NAD+-dependent deacetylase sirtuin family members, especially SIRT3, SIRT4, and SIRT5 located in mitochondria, play important roles in epigenetics such as deacetylation, demalonylation, and desuccinylation, thus affecting various aspects of cell fate [404].
Sirt3, the mitochondrial antioxidant, deacetylates FOXO3 and upregulates antioxidant enzymes such as manganese superoxide dismutase (MnSOD) to protect mitochondria against oxidative damage and maintain hematopoietic stem cells (HSCs) homeostasis [405,406,407]. The upregulation of Sirt3 expression improves their regenerative capacity in aged HSCs [408]. SIRT3 is highly upregulated in colon cancer and correlates with metastasis and tumor stages [409]. The knockdown of SIRT3 in ovarian cancer enhances the migration and invasion towards liver metastasis, while the overexpression of SIRT3 suppresses metastasis dramatically [410].
SIRT4 regulates the catabolism of multiple nutrients [411], and the loss of SIRT4 promotes the self-renewal of breast cancer stem cells [412]. High expression of SIRT5 increased migration and proliferation in prostate cancer cells and renal cell carcinoma [413,414]. SIRT5 deacetylates lactate dehydrogenase B (LDHB) and promotes its enzymatic activity, thus generating additional protons and increasing autophagy and tumorigenesis in colorectal cancer, and the knockdown of SIRT5 reduces cancer cell proliferation [415]. A high level of SIRT5 desuccinylates SDH and reduces its activity promoting cancer cell proliferation, while SIRT5 silencing results in hyper-succinylation of SDHA and reactivates it, thus preventing the growth of cancer cells [414]. SIRT5 also desuccinylates serine hydroxymethyl transferase (SHMT2), and the inactivation of SIRT5 downregulates SHM2 succinylation and decreases its activity in serine catabolism and inhibits cancer cell growth [416]. Chemoresistant prostate cancer cells shift the metabolism from glycolysis to OXPHOS, and this chemoresistance is modified by all three mitochondria sirtuins [417,418,419,420]. SIRT6 plays important roles in the regulation of cancer cell metabolism and the promotion of cancer cell apoptosis [421,422,423,424]. SIRT6 directly binds to the CDC25A promoter and decreases the acetylation level of histone H3 lysine 9 to inhibit colorectal cancer stem cell proliferation [425].
3.2.3. Mitochondrial Metabolites Contribute to Normal Development and Tumorigenesis via Regulation of Epigenetics
The cofactors participating in histone acetylation affect cell fate. For example, α-KG generated from glutaminolysis is important for the M2 activation of macrophages, and it orchestrates macrophage activation through metabolic and epigenetic reprogramming. Glutamine metabolism supports M2 activation by facilitating the demethylation of H3K27, which is a repressive epigenetic mark that prevents the expression of M2 marker genes [426,427]. Acetyl-CoA, serving as acetyl donors for acetylation and co-factors for deacetylase enzymes, is critical in determining both macrophage and dendritic cell differentiation and function [428,429]. The treatment with acetate (a precursor of acetyl-CoA) increases H3K9ac and H3K27ac and delays early differentiation in human PSCs and mESCs, suggesting that a decline in acetyl-CoA drives the early differentiation in PSCs by reducing histone acetylation [375,430]. Therefore, acetyl-CoA is necessary for differentiation via histone-mediated regulation of gene expression in adult stem cells [431].
The intracellular metabolite levels are subject to both cell-intrinsic metabolic pathway activity and factors in the extrinsic environment such as nutrient availability. For example, tissue-specific and systemic nutrient availability modulates stem cell fate via α-KG-dependent dioxygenases, and this links the extracellular cues and cell fate decisions [84].
4. Reagents and Drugs Targeting Mitochondria and Epigenetics for Cancer Treatment
4.1. Targeting Mitochondrial Metabolites and Enzymes in TCA in Cancer
Targeting mitochondria in cancer has been reviewed often [9,432,433,434,435,436,437], and multiple mitochondria-targeted drugs have been developed [438,439,440,441]. Metabolites and enzymes in TCA cycles have been demonstrated to be therapeutic targets in cancers.
The level of acetyl-CoA is treated as a key indicator of a cell’s metabolic state and a second messenger in cells [186], and its fluctuation is associated with gene expression via the global changes in histone acetylation, and it promotes the upregulation of cell-migration-and-adhesion-related genes in glioblastoma [442,443]. Furthermore, acetyl-CoA production by specific metabolites promotes cardiac repair after myocardial infarction by histone acetylation [444]. In addition, acetyl-CoA metabolism supports pancreatic tumorigenesis, and it is used in histone acetylation and in the mevalonate pathway facilitating cell plasticity and proliferation, which suggests potential to target these pathways [445]. Acetyl-CoA carboxylase (ACC) is an ATP-dependent carboxylation of acetyl-CoA, and this rate-limiting enzyme in de novo fatty acid synthesis has also been demonstrated as a cancer therapy target [446].
Citrate is a key metabolite that bridges many important metabolic pathways. Abnormalities of citrate-metabolizing enzymes such as citrate synthase enzyme and ACL happen in various cancers [447,448,449,450]. Targeting citrate and citrate enzymes is a novel therapeutic strategy in cancer treatment [451]. Isocitrate dehydrogenase (IDH) enzymes catalyze the oxidative decarboxylation of isocitrate and therefore play key roles in the Krebs cycle and cellular homeostasis. IDH1 and IDH2 catalyze the conversion of isocitrate to αKG in the cell cytoplasm and mitochondria, respectively. They have been shown to induce cancer stem cell differentiation successfully in AML patients, and the IDH mutants produce oncometabolite d-2-hydroxyglutarate that inhibits downstream 2-oxoglutarate-dependent epigenetic modifiers, thus resulting in differentiation arrest of blast cells [452]. IDH-mutated human malignancies include glioblastoma [211,453], AML [454,455], intrahepatic cholangiocarcinoma, chondrosarcoma, and thyroid carcinomas [456,457]. Enasidenib and ivosidenib are potent and selective inhibitors of mutant IDH2 and IDH1, respectively, and both drugs have been approved by the Food and Drug Administration (FDA) for the treatment of AML [78].
The metabolite α-KG is membrane-impermeable, and intracellular α-KG inhibits starvation-induced autophagy and it has no direct respiration-inhibitory effect [80]. α-KG is an effector of p53-mediated tumor suppression, and the elevated intracellular levels of succinate (a competitive inhibitor of αKG-dependent dioxygenases) can blunt p53-driven tumor suppression [369].
Succinate plays an important role in inflammatory, hypoxic, and metabolic signaling [458], and targeting succinate and succinate metabolism can be a potential therapeutic method in aortic aneurysm and dissection, and in ischemia/reperfusion injury [459,460]. Dimethyl fumarate (DMF), a derivative of the Krebs cycle intermediate fumarate, is an immunomodulatory drug used in patients with multiple sclerosis and psoriasis [461,462].
Malate is a standard component in fluid therapy within a wide range of medical applications [463], and sunitinib malate has been used in the treatment of urothelial cancer [464].
Malate dehydrogenase (MDH) catalyzes the reversible interconversion of malate and oxaloacetate and their transport [465], and it has unique pharmacological selective and specificity properties and can be used as the potential antiparasitic target for drug development [466]. For example, urine malate dehydrogenase 2 can be used as a biomarker for the early detection of non-small-cell lung cancer [467]. Oxaloacetate (OAA) is a competitive inhibitor of human lactate dehydrogenase A (LDHA) in cancer cells, and there is an inverse correlation between lactate and OAA concentration in cells from patients with myeloma and normal healthy individuals, which indicates the relevance of OAA as a regulator of the Warburg effect in rapidly proliferating cells in humans [468]. Oxaloacetate treatment has a neuroprotective effect in rodent models of seizure and neurodegeneration. In amyotrophic lateral sclerosis (ALS) mice model, oxaloacetate treatment evaluates the neuromuscular function and lifespan [469]. Oxaloacetic acid (OA) is an intermediate of citric acid and a potential natural anti-pigmentation agent, and it can inhibit tyrosinase [470].
4.2. Targeting Epigenetics in Cancer
4.2.1. Targeting DNA Methylation
Targeting epigenetics in cancer has emerged as a promising anticancer strategy. The analysis of epigenetic changes in DNA may help to identify new druggable targets for the treatment of cancer [471,472]. DNA methylation profile alteration leads to DNA instability and triggers tumorigeneses. Hypermethylation of tumor suppressors or hypomethylation of oncogenes may arise in diseases such as cancers [473,474,475]. DNA-methylation-targeted drugs have been developed widely. Nucleoside-derived inhibitors 5′-AZA, decitabine, and zebularine were approved by the FDA for the treatment of various types of cancer [476,477,478].
-
a.
Targeting DNMTs
Since 5′-AZA is unstable and highly toxic to cells, far less toxic DNMT inhibitors were developed, including RG108, which is a non-cytidine analog successfully tested in human prostate cancer cells, breast cancer cells, and colon cancer cells [479,480,481,482]. Hydralazine and procainamide act as competitive inhibitors by preferentially binding to DNMT1 [483,484]. SGI-1027 and its regioisomer MC3343 cause the degradation of DNMT1 [485], suppression of growth of leukemia cell line, and, in osteosarcoma, patient-derived xenograft [486,487]. The combination uses of AH507 (JAK 1/2 inhibitor) and SGI-1027 have a synergistic effect on the suppression of survival and proliferation of cervical cancer cells [488]. GSK3685032, a potent first-in-class DNMT1-selective inhibitor with improved in vivo tolerability, yields superior tumor regression and survival mouse models of AML [489]. CM272, a G9a/DNMT1 inhibitor, inhibits cholangiocarcinoma tumoroids and xenograft growth significantly [490]. UHRF1-DNMT1 is responsible for DNA methylation in DNA replication, and UHRF1 links DNA methylation and histone modifications. The downregulation of UHRF1/DNMT1 is upstream of many cellular events, including G1 cell arrest, demethylation of p16, and apoptosis [491]. UHRF1-DNA binding domain has been proposed as a drug target for cancer therapy [492,493,494]. UHRF1/DNMT1 axis is also a regulator of senescence [495].
Besides small molecular inhibition of DNMTs, other strategies to inhibit DNMT1 include the use of antisense oligonucleotides and miRNAs such as MG98 to suppress renal cell carcinoma [496]. Epigallocatechin-3-gallate, a polyphenol flavonoid, is involved in both DNA demethylation and modifications of histone acetylation and methylation [497]. Procaine (a local anesthetic) is capable of reducing the methylation level of CpG island in some cancers such as hepatoma, breast cancer, and gastric cancer [498] by inhibiting the binding of DNMT1 to the target genes [485,499].
Besides inhibiting DNMTs to suppress DNA methylation, the activation of DNA methylation can also be a therapeutic strategy. The DNMT activator budesonide supplementation increases DNA methylation and decreases tumor size [500,501].
-
b.
Targeting demethylases
DNA demethylation, as a potential target for cancer epigenetic therapy, has been reviewed before [502].
The demethylase TET 2 is an α-KG- and Fe2+-dependent dioxygenase catalyzing the iterative oxidation of 5mC, and the mutation and dysregulation of TET2 contribute to the development of multiple hematological malignancies [503]. Hydroxymethylation of DNA leads to hypomethylation of DNA in lupus [504]. Increased expression of TET enzymes in monocytes and T cells leads to abnormal global DNA hydroxymethylation in early RA patients, and methotrexate treatment partly reduces the level of DNA hydroxymethylation in rheumatoid arthritis [505]. TET inhibition by AGI-5198 and HMS-101 compound leads to tumor growth suppression in glioblastoma and AML cells [506,507]. In all, modification of DNA methylation either by hypo- or hypermethylation is effective in different types of tumors.
4.2.2. Targeting Histone Methylation
Targeting histone methylation has been reviewed [508]. Both histone methyltransferases and demethylases can be targets in cancer.
The disruptor of telomeric silencing 1-like (DOT1L), a histone H3K79 methyltransferase, is a target for many diseases [509]. It sensitizes RB cells to chemotherapeutic drugs by impairing the DNA damage response, thereby potentiating apoptosis [510]. Many inhibitors were developed to target DOT1L, and among them, EPZ-5676 has been in clinical trials, but the clinical result is modest, and long-time treatment leads to drug resistance in AML [511,512,513].
Histone demethylase LSDl, the first identified demethylase of histone methylation, belongs to the FAD-dependent family of monoamine oxidases [163]. The dysregulation and overexpression of LSD1 are hallmarks of a number of human diseases [514]. LSDl inhibitor CC-90011 induces the cancer stem cell to differentiation in AML and small-cell-lung cancer (SCLC) cell lines, with antitumor efficacy, and CC-90011 is currently in phase 2 trials in patients with first-line, extensive-stage SCLC [514].
4.2.3. Targeting Histone Acetylation
Histone acetylation renders a more relaxed DNA structure to facilitate the binding of transcription factors and other proteins for gene expression. Histone acetylation enzymes, including HATs and HDACs, are potential drug targets in many diseases [515,516].
CBP/p300, functioning as histone acetyltransferases and transcriptional co-factors, represents an attractive target for various diseases, including malignant tumor cancers such as leukemia and prostate [517,518,519]. CBP/p300 inhibitors have been widely developed, including pyrazolone derivatives, oxazolidinedione, barbituric derivatives, etc. [518]. The treatment with p300/CBP inhibitor B029-2 specifically decreases H3K18Ac and H3K27Ac and displays significant antitumor effects on hepatocellular carcinoma (HCC) cells in vitro and in vivo [520]. Its bromodomain inhibitor CCS1477, identified by CellCentric, is the only CBP/p300 inhibitor currently in clinical trials for the treatment of hematological malignancies and prostate cancer [518,521,522].
Bromodomain and extra-terminal domain (BET) proteins, including BRD1, BRD2, BRD3, BRD4, and BRDt, act as “readers” of acetylated histones, and they can recognize H3K27ac through their bromodomains [523,524]. BET inhibition has been applied in both solid tumors and hematological malignancies [525]. Blocking the binding between BRD4 and chromatin by BET inhibitor JQ1 inhibits the proliferation and differentiation in BRD4-dependent tumors [526].
Many HDAC inhibitors have been developed and characterized in tumors, thus causing tumor cell differentiation and apoptosis and resulting in the inhibition of tumor growth in animals [527,528]. HDAC inhibitors have been applied in many clinical trials for hematologic and solid cancers [529]. Some of the inhibitors have been approved by FDA and targeting lactylation suggests novel onco-therapeutic opportunities [267]. Histone deacetylation (HDAC) inhibitor mocetinostat synergizes with gemcitabine to inhibit in vivo pancreatic xenograft growth by disrupting EMT and the CSC phenotype [530]. Inhibition of HDACs with trichostatin A and vorinostat promotes epithelial differentiation, thus disrupting tumor sphere formation and subcutaneous tumor xenograft growth [531]. Abexinostat is a potent and pan-HDAC inhibitor with a favorable pharmacokinetic profile and no expected drug-drug interactions with pazopanib [532].
4.2.4. Targeting Histone Lactylation
Lactate-derived lysine lactylation in histones serves as a new type of histone mark [265]. Lactylation and lactate have been proposed for cancer treatment. Histone lactylation could drive oncogene expression and accelerate tumorigenesis by activating the m6A reader protein, YTHDF2, which is a novel potential histone lactylation target for treating ocular melanoma [265]. The function of lactylation and targeting lactylation in tumorigenesis and development deserve further investigation.
5. Conclusions and Perspectives
In this review, we have presented an extensive discussion on mitochondria function in tumorigenesis from an epigenetic perspective. Even the primary function of mitochondria in cellular metabolism is energy production, and the metabolites generated in this process contribute to tumorigenesis by influencing gene expression and cell signaling via epigenetic regulations [85]. The interconnected metabolites generated in the TCA cycle communicate to the epigenetic machinery by providing precursors for epigenetic modifications, including DNA methylation and post-translation modification of histones. Post-translation modification of histones regulates the interaction of histones with DNA and the ability to recruit chromatin remodeling complexes necessary for transcription, replication, recombination, repair, and mitosis. Epigenetic regulation is a dynamic process that allows a high degree of plasticity of cell fate in response to tumor microenvironment.
The key metabolic enzymes in the TCA cycle such as IDH, SDH, and FH are mutated in various cancers, and these enzymes and other metabolites or intermediates in mitochondria have been proven to be tumor targets. Inhibition of the key enzymes in epigenetics such as methyltransferases or histone acetylases/deacetylases can reactivate epigenetically silenced tumor suppressor genes and thus decrease tumor cell growth. Some of the inhibitors targeting cancer stemness lead to cancer stem cell differentiation and suppress its growth by changing cell fate. Much more research can be observed in studies on epigenetics, which plays important roles in human diseases and is demonstrated as therapeutic targets in the treatment and diagnosis of cancer and proliferative diseases. Our current understanding and summary are not comprehensive enough to include all kinds of epigenetics regulation, but we believe that the recognition of the importance of understanding tumorigenesis, combined with mitochondrial metabolites and epigenetics, would be helpful for the design of therapeutic interventions.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Funding for this project includes the National Natural Science Foundation of China (81872072, J.C.), (82073274, Y.S.), and the Science Technology Commission of Shanghai Municipality (20S11900700, Y.S.).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lane N., Martin W. The energetics of genome complexity. Nature. 2010;467:929–934. doi: 10.1038/nature09486. [DOI] [PubMed] [Google Scholar]
- 2.Archibald J.M. Endosymbiosis and Eukaryotic Cell Evolution. Curr. Biol. 2015;25:R911–R921. doi: 10.1016/j.cub.2015.07.055. [DOI] [PubMed] [Google Scholar]
- 3.Nunnari J., Suomalainen A. Mitochondria: In sickness and in health. Cell. 2012;148:1145–1159. doi: 10.1016/j.cell.2012.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wallace D.C. Mitochondria and cancer. Nat. Rev. Cancer. 2012;12:685–698. doi: 10.1038/nrc3365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gomes A.P., Price N.L., Ling A.J., Moslehi J.J., Montgomery M.K., Rajman L., White J.P., Teodoro J.S., Wrann C.D., Hubbard B.P., et al. Declining NAD(+) induces a pseudohypoxic state disrupting nuclear-mitochondrial communication during aging. Cell. 2013;155:1624–1638. doi: 10.1016/j.cell.2013.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janssen J.J.E., Grefte S., Keijer J., de Boer V.C.J. Mito-Nuclear Communication by Mitochondrial Metabolites and Its Regulation by B-Vitamins. Front. Physiol. 2019;10:78. doi: 10.3389/fphys.2019.00078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rigon M., Townley A.R., Campanella M. Mitochondria ensure immune surveillance by retro-communication with the nucleus. Cell Metab. 2021;33:853–855. doi: 10.1016/j.cmet.2021.04.013. [DOI] [PubMed] [Google Scholar]
- 8.Scatena R. Mitochondria and drugs. Adv. Exp. Med. Biol. 2012;942:329–346. doi: 10.1007/978-94-007-2869-1_15. [DOI] [PubMed] [Google Scholar]
- 9.Liu Y.E., Shi Y.F. Mitochondria as a target in cancer treatment. Medcomm. 2020;1:129–139. doi: 10.1002/mco2.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen K., Zhang J., Beeraka N.M., Tang C., Babayeva Y.V., Sinelnikov M.Y., Zhang X., Zhang J., Liu J., Reshetov I.V., et al. Advances in the Prevention and Treatment of Obesity-Driven Effects in Breast Cancers. Front. Oncol. 2022;12:820968. doi: 10.3389/fonc.2022.820968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen K., Lu P., Beeraka N.M., Sukocheva O.A., Madhunapantula S.V., Liu J., Sinelnikov M.Y., Nikolenko V.N., Bulygin K.V., Mikhaleva L.M., et al. Mitochondrial mutations and mitoepigenetics: Focus on regulation of oxidative stress-induced responses in breast cancers. Semin. Cancer Biol. 2022;83:556–569. doi: 10.1016/j.semcancer.2020.09.012. [DOI] [PubMed] [Google Scholar]
- 12.Matilainen O., Quiros P.M., Auwerx J. Mitochondria and Epigenetics—Crosstalk in Homeostasis and Stress. Trends Cell Biol. 2017;27:453–463. doi: 10.1016/j.tcb.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Waddington C.H. The Epigenotype. Int. J. Epidemiol. 2011;41:10–13. doi: 10.1093/ije/dyr184. [DOI] [PubMed] [Google Scholar]
- 14.Holliday R., Pugh J.E. DNA modification mechanisms and gene activity during development. Science. 1975;187:226–232. doi: 10.1126/science.187.4173.226. [DOI] [PubMed] [Google Scholar]
- 15.Riggs A.D. X-Inactivation, Differentiation, and DNA Methylation. Cytogenet. Genome Res. 1975;14:9–25. doi: 10.1159/000130315. [DOI] [PubMed] [Google Scholar]
- 16.Sun L., Zhang H., Gao P. Metabolic reprogramming and epigenetic modifications on the path to cancer. Protein Cell. 2021;13:877–919. doi: 10.1007/s13238-021-00846-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daniel M., Tollefsbol T.O. Epigenetic linkage of aging, cancer and nutrition. J. Exp. Biol. 2015;218:59–70. doi: 10.1242/jeb.107110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martin S.L., Hardy T.M., Tollefsbol T.O. Medicinal chemistry of the epigenetic diet and caloric restriction. Curr. Med. Chem. 2013;20:4050–4059. doi: 10.2174/09298673113209990189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ross S.A., Dwyer J., Umar A., Kagan J., Verma M., Van Bemmel D.M., Dunn B.K. Introduction: Diet, epigenetic events and cancer prevention. Nutr. Rev. 2008;66((Suppl. S1)):S1–S6. doi: 10.1111/j.1753-4887.2008.00055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wallace D.C., Fan W. Energetics, epigenetics, mitochondrial genetics. Mitochondrion. 2010;10:12–31. doi: 10.1016/j.mito.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang L., Lu Q., Chang C. Epigenetics in Health and Disease. Adv. Exp. Med. Biol. 2020;1253:3–55. doi: 10.1007/978-981-15-3449-2_1. [DOI] [PubMed] [Google Scholar]
- 22.Bowden G.T., Schneider B., Domann R., Kulesz-Martin M. Oncogene activation and tumor suppressor gene inactivation during multistage mouse skin carcinogenesis. Cancer Res. 1994;54:1882s–1885s. [PubMed] [Google Scholar]
- 23.Solomon H., Brosh R., Buganim Y., Rotter V. Inactivation of the p53 tumor suppressor gene and activation of the Ras oncogene: Cooperative events in tumorigenesis. Discov. Med. 2010;9:448–454. [PubMed] [Google Scholar]
- 24.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 25.Basu A.K. DNA Damage, Mutagenesis and Cancer. Int. J. Mol. Sci. 2018;19:970. doi: 10.3390/ijms19040970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blackadar C.B. Historical review of the causes of cancer. World J. Clin. Oncol. 2016;7:54–86. doi: 10.5306/wjco.v7.i1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu F., Fan J., He Y., Xiong A., Yu J., Li Y., Zhang Y., Zhao W., Zhou F., Li W., et al. Single-cell profiling of tumor heterogeneity and the microenvironment in advanced non-small cell lung cancer. Nat. Commun. 2021;12:2540. doi: 10.1038/s41467-021-22801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walcher L., Kistenmacher A.K., Suo H., Kitte R., Dluczek S., Strauss A., Blaudszun A.R., Yevsa T., Fricke S., Kossatz-Boehlert U. Cancer Stem Cells-Origins and Biomarkers: Perspectives for Targeted Personalized Therapies. Front. Immunol. 2020;11:1280. doi: 10.3389/fimmu.2020.01280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lapidot T., Sirard C., Vormoor J., Murdoch B., Hoang T., Caceres-Cortes J., Minden M., Paterson B., Caligiuri M.A., Dick J.E. A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature. 1994;367:645–648. doi: 10.1038/367645a0. [DOI] [PubMed] [Google Scholar]
- 30.Batlle E., Clevers H. Cancer stem cells revisited. Nat. Med. 2017;23:1124–1134. doi: 10.1038/nm.4409. [DOI] [PubMed] [Google Scholar]
- 31.Patel A.P., Tirosh I., Trombetta J.J., Shalek A.K., Gillespie S.M., Wakimoto H., Cahill D.P., Nahed B.V., Curry W.T., Martuza R.L., et al. Single-cell RNA-seq highlights intratumoral heterogeneity in primary glioblastoma. Science. 2014;344:1396–1401. doi: 10.1126/science.1254257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barker N., Ridgway R.A., van Es J.H., van de Wetering M., Begthel H., van den Born M., Danenberg E., Clarke A.R., Sansom O.J., Clevers H. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature. 2009;457:608–611. doi: 10.1038/nature07602. [DOI] [PubMed] [Google Scholar]
- 33.Zhu L.Q., Gibson P., Currle D.S., Tong Y., Richardson R.J., Bayazitov I.T., Poppleton H., Zakharenko S., Ellison D.W., Gilbertson R.J. Prominin 1 marks intestinal stem cells that are susceptible to neoplastic transformation. Nature. 2009;457:603–607. doi: 10.1038/nature07589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roskams T. Liver stem cells and their implication in hepatocellular and cholangiocarcinoma. Oncogene. 2006;25:3818–3822. doi: 10.1038/sj.onc.1209558. [DOI] [PubMed] [Google Scholar]
- 35.Toh T.B., Lim J.J., Chow E.K. Epigenetics in cancer stem cells. Mol. Cancer. 2017;16:29. doi: 10.1186/s12943-017-0596-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kroemer G., Pouyssegur J. Tumor cell metabolism: Cancer’s Achilles’ heel. Cancer Cell. 2008;13:472–482. doi: 10.1016/j.ccr.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 37.Miranda Furtado C.L., Dos Santos Luciano M.C., Silva Santos R.D., Furtado G.P., Moraes M.O., Pessoa C. Epidrugs: Targeting epigenetic marks in cancer treatment. Epigenetics. 2019;14:1164–1176. doi: 10.1080/15592294.2019.1640546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reik W. Stability and flexibility of epigenetic gene regulation in mammalian development. Nature. 2007;447:425–432. doi: 10.1038/nature05918. [DOI] [PubMed] [Google Scholar]
- 39.Cai S.F., Levine R.L. Genetic and epigenetic determinants of AML pathogenesis. Semin. Hematol. 2019;56:84–89. doi: 10.1053/j.seminhematol.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ilango S., Paital B., Jayachandran P., Padma P.R., Nirmaladevi R. Epigenetic alterations in cancer. Front. Biosci. 2020;25:1058–1109. doi: 10.2741/4847. [DOI] [PubMed] [Google Scholar]
- 41.Mazor T., Pankov A., Song J.S., Costello J.F. Intratumoral Heterogeneity of the Epigenome. Cancer Cell. 2016;29:440–451. doi: 10.1016/j.ccell.2016.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wainwright E.N., Scaffidi P. Epigenetics and Cancer Stem Cells: Unleashing, Hijacking, and Restricting Cellular Plasticity. Trends Cancer. 2017;3:372–386. doi: 10.1016/j.trecan.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Murphy S.K., Jirtle R.L. Imprinting evolution and the price of silence. Bioessays. 2003;25:577–588. doi: 10.1002/bies.10277. [DOI] [PubMed] [Google Scholar]
- 44.Das R., Hampton D.D., Jirtle R.L. Imprinting evolution and human health. Mamm. Genome. 2009;20:563–572. doi: 10.1007/s00335-009-9229-y. [DOI] [PubMed] [Google Scholar]
- 45.Esteller M. Epigenetic gene silencing in cancer: The DNA hypermethylome. Hum. Mol. Genet. 2007;16:R50–R59. doi: 10.1093/hmg/ddm018. [DOI] [PubMed] [Google Scholar]
- 46.Marusyk A., Almendro V., Polyak K. Intra-tumour heterogeneity: A looking glass for cancer? Nat. Rev. Cancer. 2012;12:323–334. doi: 10.1038/nrc3261. [DOI] [PubMed] [Google Scholar]
- 47.Gerlinger M., Rowan A.J., Horswell S., Math M., Larkin J., Endesfelder D., Gronroos E., Martinez P., Matthews N., Stewart A., et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N. Engl. J. Med. 2012;366:883–892. doi: 10.1056/NEJMoa1113205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shackleton M., Quintana E., Fearon E.R., Morrison S.J. Heterogeneity in cancer: Cancer stem cells versus clonal evolution. Cell. 2009;138:822–829. doi: 10.1016/j.cell.2009.08.017. [DOI] [PubMed] [Google Scholar]
- 49.Peng Y., Liu H., Liu J., Long J. Post-translational modifications on mitochondrial metabolic enzymes in cancer. Free Radic. Biol. Med. 2022;179:11–23. doi: 10.1016/j.freeradbiomed.2021.12.264. [DOI] [PubMed] [Google Scholar]
- 50.Dai Z., Ramesh V., Locasale J.W. The evolving metabolic landscape of chromatin biology and epigenetics. Nat. Rev. Genet. 2020;21:737–753. doi: 10.1038/s41576-020-0270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhu J., Thompson C.B. Metabolic regulation of cell growth and proliferation. Nat. Rev. Mol. Cell Biol. 2019;20:436–450. doi: 10.1038/s41580-019-0123-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou V.W., Goren A., Bernstein B.E. Charting histone modifications and the functional organization of mammalian genomes. Nat. Rev. Genet. 2011;12:7–18. doi: 10.1038/nrg2905. [DOI] [PubMed] [Google Scholar]
- 53.Margueron R., Reinberg D. Chromatin structure and the inheritance of epigenetic information. Nat. Rev. Genet. 2010;11:285–296. doi: 10.1038/nrg2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu S., Zhang X., Liu C., Liu Q., Chai H., Luo Y., Li S. Role of Mitochondria in Neurodegenerative Diseases: From an Epigenetic Perspective. Front. Cell Dev. Biol. 2021;9:688789. doi: 10.3389/fcell.2021.688789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Paik W.K., Paik D.C., Kim S. Historical review: The field of protein methylation. Trends Biochem. Sci. 2007;32:146–152. doi: 10.1016/j.tibs.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 56.Bird A.P. DNA methylation and the frequency of CpG in animal DNA. Nucleic Acids Res. 1980;8:1499–1504. doi: 10.1093/nar/8.7.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zeng Y., Chen T. DNA Methylation Reprogramming during Mammalian Development. Genes. 2019;10:257. doi: 10.3390/genes10040257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Li C., Fan Y., Li G., Xu X., Duan J., Li R., Kang X., Ma X., Chen X., Ke Y., et al. DNA methylation reprogramming of functional elements during mammalian embryonic development. Cell Discov. 2018;4:41. doi: 10.1038/s41421-018-0039-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kulis M., Esteller M. DNA methylation and cancer. Adv. Genet. 2010;70:27–56. doi: 10.1016/B978-0-12-380866-0.60002-2. [DOI] [PubMed] [Google Scholar]
- 60.Bestor T.H. The DNA methyltransferases of mammals. Hum. Mol. Genet. 2000;9:2395–2402. doi: 10.1093/hmg/9.16.2395. [DOI] [PubMed] [Google Scholar]
- 61.Lyko F. The DNA methyltransferase family: A versatile toolkit for epigenetic regulation. Nat. Rev. Genet. 2018;19:81–92. doi: 10.1038/nrg.2017.80. [DOI] [PubMed] [Google Scholar]
- 62.Moore L.D., Le T., Fan G. DNA methylation and its basic function. Neuropsychopharmacology. 2013;38:23–38. doi: 10.1038/npp.2012.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang J., Zhang K.X., Lu G.Z., Zhao X.H. Research progress on 5hmC and TET dioxygenases in neurodevelopment and neurological diseases. Yi Chuan. 2017;39:1138–1149. doi: 10.16288/j.yczz.17-086. [DOI] [PubMed] [Google Scholar]
- 64.Matuleviciute R., Cunha P.P., Johnson R.S., Foskolou I.P. Oxygen regulation of TET enzymes. FEBS J. 2021;288:7143–7161. doi: 10.1111/febs.15695. [DOI] [PubMed] [Google Scholar]
- 65.Tahiliani M., Koh K.P., Shen Y., Pastor W.A., Bandukwala H., Brudno Y., Agarwal S., Iyer L.M., Liu D.R., Aravind L., et al. Conversion of 5-methylcytosine to 5-hydroxymethylcytosine in mammalian DNA by MLL partner TET1. Science. 2009;324:930–935. doi: 10.1126/science.1170116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xu W., Yang H., Liu Y., Yang Y., Wang P., Kim S.H., Ito S., Yang C., Wang P., Xiao M.T., et al. Oncometabolite 2-Hydroxyglutarate Is a Competitive Inhibitor of alpha-Ketoglutarate-Dependent Dioxygenases. Cancer Cell. 2011;19:17–30. doi: 10.1016/j.ccr.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang J., Tang J., Lai M., Zhang H. 5-Hydroxymethylcytosine and disease. Mutat. Res. Rev. Mutat. Res. 2014;762:167–175. doi: 10.1016/j.mrrev.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 68.Valinluck V., Sowers L.C. Endogenous cytosine damage products alter the site selectivity of human DNA maintenance methyltransferase DNMT1. Cancer Res. 2007;67:946–950. doi: 10.1158/0008-5472.CAN-06-3123. [DOI] [PubMed] [Google Scholar]
- 69.Bhutani N., Burns D.M., Blau H.M. DNA demethylation dynamics. Cell. 2011;146:866–872. doi: 10.1016/j.cell.2011.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jin S.G., Kadam S., Pfeifer G.P. Examination of the specificity of DNA methylation profiling techniques towards 5-methylcytosine and 5-hydroxymethylcytosine. Nucleic Acids Res. 2010;38:e125. doi: 10.1093/nar/gkq223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ouyang Y., Wu Q., Li J., Sun S., Sun S. S-adenosylmethionine: A metabolite critical to the regulation of autophagy. Cell Prolif. 2020;53:e12891. doi: 10.1111/cpr.12891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lu S.C. S-Adenosylmethionine. Int. J. Biochem. Cell Biol. 2000;32:391–395. doi: 10.1016/S1357-2725(99)00139-9. [DOI] [PubMed] [Google Scholar]
- 73.Agrimi G., Di Noia M.A., Marobbio C.M., Fiermonte G., Lasorsa F.M., Palmieri F. Identification of the human mitochondrial S-adenosylmethionine transporter: Bacterial expression, reconstitution, functional characterization and tissue distribution. Biochem. J. 2004;379:183–190. doi: 10.1042/bj20031664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mato J.M., Alvarez L., Ortiz P., Pajares M.A. S-adenosylmethionine synthesis: Molecular mechanisms and clinical implications. Pharmacol. Ther. 1997;73:265–280. doi: 10.1016/S0163-7258(96)00197-0. [DOI] [PubMed] [Google Scholar]
- 75.Finkelstein J.D. Methionine metabolism in mammals. J. Nutr. Biochem. 1990;1:228–237. doi: 10.1016/0955-2863(90)90070-2. [DOI] [PubMed] [Google Scholar]
- 76.Mentch S.J., Mehrmohamadi M., Huang L., Liu X.J., Gupta D., Mattocks D., Padilla P.G., Ables G., Bamman M.M., Thalacker-Mercer A.E., et al. Histone Methylation Dynamics and Gene Regulation Occur through the Sensing of One-Carbon Metabolism. Cell Metab. 2015;22:861–873. doi: 10.1016/j.cmet.2015.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ducker G.S., Chen L., Morscher R.J., Ghergurovich J.M., Esposito M., Teng X., Kang Y., Rabinowitz J.D. Reversal of Cytosolic One-Carbon Flux Compensates for Loss of the Mitochondrial Folate Pathway. Cell Metab. 2016;24:640–641. doi: 10.1016/j.cmet.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 78.Martelli M.P., Martino G., Cardinali V., Falini B., Martinelli G., Cerchione C. Enasidenib and ivosidenib in AML. Minerva Med. 2020;111:411–426. doi: 10.23736/S0026-4806.20.07024-X. [DOI] [PubMed] [Google Scholar]
- 79.Liu S., He L., Yao K. The Antioxidative Function of Alpha-Ketoglutarate and Its Applications. Biomed. Res. Int. 2018;2018:3408467. doi: 10.1155/2018/3408467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Baracco E.E., Castoldi F., Durand S., Enot D.P., Tadic J., Kainz K., Madeo F., Chery A., Izzo V., Maiuri M.C., et al. alpha-Ketoglutarate inhibits autophagy. Aging. 2019;11:3418–3431. doi: 10.18632/aging.102001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Asadi Shahmirzadi A., Edgar D., Liao C.Y., Hsu Y.M., Lucanic M., Asadi Shahmirzadi A., Wiley C.D., Gan G., Kim D.E., Kasler H.G., et al. Alpha-Ketoglutarate, an Endogenous Metabolite, Extends Lifespan and Compresses Morbidity in Aging Mice. Cell Metab. 2020;32:447–456.e6. doi: 10.1016/j.cmet.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Long L.H., Halliwell B. Artefacts in cell culture: Alpha-Ketoglutarate can scavenge hydrogen peroxide generated by ascorbate and epigallocatechin gallate in cell culture media. Biochem. Biophys. Res. Commun. 2011;406:20–24. doi: 10.1016/j.bbrc.2011.01.091. [DOI] [PubMed] [Google Scholar]
- 83.Tran K.A., Dillingham C.M., Sridharan R. The role of alpha-ketoglutarate-dependent proteins in pluripotency acquisition and maintenance. J. Biol. Chem. 2019;294:5408–5419. doi: 10.1074/jbc.TM118.000831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Baksh S.C., Finley L.W.S. Metabolic Coordination of Cell Fate by alpha-Ketoglutarate-Dependent Dioxygenases. Trends Cell Biol. 2021;31:24–36. doi: 10.1016/j.tcb.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kaelin W.G., Jr., McKnight S.L. Influence of metabolism on epigenetics and disease. Cell. 2013;153:56–69. doi: 10.1016/j.cell.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yang Q., Liang X., Sun X., Zhang L., Fu X., Rogers C.J., Berim A., Zhang S., Wang S., Wang B., et al. AMPK/alpha-Ketoglutarate Axis Dynamically Mediates DNA Demethylation in the Prdm16 Promoter and Brown Adipogenesis. Cell Metab. 2016;24:542–554. doi: 10.1016/j.cmet.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Raffel S., Falcone M., Kneisel N., Hansson J., Wang W., Lutz C., Bullinger L., Poschet G., Nonnenmacher Y., Barnert A., et al. BCAT1 restricts alphaKG levels in AML stem cells leading to IDHmut-like DNA hypermethylation. Nature. 2017;551:384–388. doi: 10.1038/nature24294. [DOI] [PubMed] [Google Scholar]
- 88.Sciacovelli M., Goncalves E., Johnson T.I., Zecchini V.R., da Costa A.S.H., Gaude E., Drubbel A.V., Theobald S.J., Abbo S.R., Tran M.G.B., et al. Fumarate is an epigenetic modifier that elicits epithelial-to-mesenchymal transition. Nature. 2016;537:544–547. doi: 10.1038/nature19353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Xiao M.T., Yang H., Xu W., Ma S.H., Lin H.P., Zhu H.G., Liu L.X., Liu Y., Yang C., Xu Y.H., et al. Inhibition of alpha-KG-dependent histone and DNA demethylases by fumarate and succinate that are accumulated in mutations of FH and SDH tumor suppressors. Gene Dev. 2012;26:1326–1338. doi: 10.1101/gad.191056.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Laukka T., Mariani C.J., Ihantola T., Cao J.Z., Hokkanen J., Kaelin W.G., Jr., Godley L.A., Koivunen P. Fumarate and Succinate Regulate Expression of Hypoxia-inducible Genes via TET Enzymes. J. Biol. Chem. 2016;291:4256–4265. doi: 10.1074/jbc.M115.688762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Pollard P.J., Briere J.J., Alam N.A., Barwell J., Barclay E., Wortham N.C., Hunt T., Mitchell M., Olpin S., Moat S.J., et al. Accumulation of Krebs cycle intermediates and over-expression of HIF1alpha in tumours which result from germline FH and SDH mutations. Hum. Mol. Genet. 2005;14:2231–2239. doi: 10.1093/hmg/ddi227. [DOI] [PubMed] [Google Scholar]
- 92.Hoekstra A.S., de Graaff M.A., Briaire-de Bruijn I.H., Ras C., Seifar R.M., van Minderhout I., Cornelisse C.J., Hogendoorn P.C., Breuning M.H., Suijker J., et al. Inactivation of SDH and FH cause loss of 5hmC and increased H3K9me3 in paraganglioma/pheochromocytoma and smooth muscle tumors. Oncotarget. 2015;6:38777–38788. doi: 10.18632/oncotarget.6091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dang L., White D.W., Gross S., Bennett B.D., Bittinger M.A., Driggers E.M., Fantin V.R., Jang H.G., Jin S., Keenan M.C., et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009;462:739–744. doi: 10.1038/nature08617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Thienpont B., Galle E., Lambrechts D. TET enzymes as oxygen-dependent tumor suppressors: Exciting new avenues for cancer management. Epigenomics. 2016;8:1445–1448. doi: 10.2217/epi-2016-0126. [DOI] [PubMed] [Google Scholar]
- 95.Giorgio M., Trinei M., Migliaccio E., Pelicci P.G. Hydrogen peroxide: A metabolic by-product or a common mediator of ageing signals? Nat. Rev. Mol. Cell Biol. 2007;8:722–728. doi: 10.1038/nrm2240. [DOI] [PubMed] [Google Scholar]
- 96.Dan Dunn J., Alvarez L.A., Zhang X., Soldati T. Reactive oxygen species and mitochondria: A nexus of cellular homeostasis. Redox Biol. 2015;6:472–485. doi: 10.1016/j.redox.2015.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Li R., Jia Z., Trush M.A. Defining ROS in Biology and Medicine. React. Oxyg. Species. 2016;1:9–21. doi: 10.20455/ros.2016.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ziech D., Franco R., Pappa A., Panayiotidis M.I. Reactive oxygen species (ROS)—Induced genetic and epigenetic alterations in human carcinogenesis. Mutat. Res. 2011;711:167–173. doi: 10.1016/j.mrfmmm.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 99.Quan X., Lim S.O., Jung G. Reactive oxygen species downregulate catalase expression via methylation of a CpG island in the Oct-1 promoter. FEBS Lett. 2011;585:3436–3441. doi: 10.1016/j.febslet.2011.09.035. [DOI] [PubMed] [Google Scholar]
- 100.Lim S.O., Gu J.M., Kim M.S., Kim H.S., Park Y.N., Park C.K., Cho J.W., Park Y.M., Jung G. Epigenetic changes induced by reactive oxygen species in hepatocellular carcinoma: Methylation of the E-cadherin promoter. Gastroenterology. 2008;135:2128–2140.e8. doi: 10.1053/j.gastro.2008.07.027. [DOI] [PubMed] [Google Scholar]
- 101.Wu Q., Ni X. ROS-mediated DNA methylation pattern alterations in carcinogenesis. Curr. Drug Targets. 2015;16:13–19. doi: 10.2174/1389450116666150113121054. [DOI] [PubMed] [Google Scholar]
- 102.Afanas’ev I. New nucleophilic mechanisms of ros-dependent epigenetic modifications: Comparison of aging and cancer. Aging Dis. 2014;5:52–62. doi: 10.14336/ad.2014.050052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Fan W., Luo J.Y. SIRT1 Regulates UV-Induced DNA Repair through Deacetylating XPA. Mol. Cell. 2010;39:247–258. doi: 10.1016/j.molcel.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 104.Kang K.A., Zhang R., Kim G.Y., Bae S.C., Hyun J.W. Epigenetic changes induced by oxidative stress in colorectal cancer cells: Methylation of tumor suppressor RUNX3. Tumour Biol. 2012;33:403–412. doi: 10.1007/s13277-012-0322-6. [DOI] [PubMed] [Google Scholar]
- 105.Fuks F., Burgers W.A., Brehm A., Hughes-Davies L., Kouzarides T. DNA methyltransferase Dnmt1 associates with histone deacetylase activity. Nat. Genet. 2000;24:88–91. doi: 10.1038/71750. [DOI] [PubMed] [Google Scholar]
- 106.Fuks F. DNA methylation and histone modifications: Teaming up to silence genes. Curr. Opin. Genet. Dev. 2005;15:490–495. doi: 10.1016/j.gde.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 107.Delatte B., Jeschke J., Defrance M., Bachman M., Creppe C., Calonne E., Bizet M., Deplus R., Marroqui L., Libin M., et al. Genome-wide hydroxymethylcytosine pattern changes in response to oxidative stress. Sci. Rep. 2015;5:12714. doi: 10.1038/srep12714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kriaucionis S., Heintz N. The Nuclear DNA Base 5-Hydroxymethylcytosine Is Present in Purkinje Neurons and the Brain. Science. 2009;324:929–930. doi: 10.1126/science.1169786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chia N., Wang L., Lu X., Senut M.C., Brenner C., Ruden D.M. Hypothesis: Environmental regulation of 5-hydroxymethylcytosine by oxidative stress. Epigenetics. 2011;6:853–856. doi: 10.4161/epi.6.7.16461. [DOI] [PubMed] [Google Scholar]
- 110.Cimmino L., Dolgalev I., Wang Y., Yoshimi A., Martin G.H., Wang J., Ng V., Xia B., Witkowski M.T., Mitchell-Flack M., et al. Restoration of TET2 Function Blocks Aberrant Self-Renewal and Leukemia Progression. Cell. 2017;170:1079–1095.e20. doi: 10.1016/j.cell.2017.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Minor E.A., Court B.L., Young J.I., Wang G. Ascorbate induces ten-eleven translocation (Tet) methylcytosine dioxygenase-mediated generation of 5-hydroxymethylcytosine. J. Biol. Chem. 2013;288:13669–13674. doi: 10.1074/jbc.C113.464800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Yin R., Mao S.Q., Zhao B., Chong Z., Yang Y., Zhao C., Zhang D., Huang H., Gao J., Li Z., et al. Ascorbic acid enhances Tet-mediated 5-methylcytosine oxidation and promotes DNA demethylation in mammals. J. Am. Chem. Soc. 2013;135:10396–10403. doi: 10.1021/ja4028346. [DOI] [PubMed] [Google Scholar]
- 113.Thienpont B., Steinbacher J., Zhao H., D’Anna F., Kuchnio A., Ploumakis A., Ghesquiere B., Van Dyck L., Boeckx B., Schoonjans L., et al. Tumour hypoxia causes DNA hypermethylation by reducing TET activity. Nature. 2016;537:63–68. doi: 10.1038/nature19081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.MacLeod A.R., Rouleau J., Szyf M. Regulation of DNA methylation by the Ras signaling pathway. J. Biol. Chem. 1995;270:11327–11337. doi: 10.1074/jbc.270.19.11327. [DOI] [PubMed] [Google Scholar]
- 115.Ploumakis A., Coleman M.L. OH, the Places You’ll Go! Hydroxylation, Gene Expression, and Cancer. Mol. Cell. 2015;58:729–741. doi: 10.1016/j.molcel.2015.05.026. [DOI] [PubMed] [Google Scholar]
- 116.Singh K.K. Mitochondria damage checkpoint in apoptosis and genome stability. FEMS Yeast Res. 2004;5:127–132. doi: 10.1016/j.femsyr.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 117.Minocherhomji S., Tollefsbol T.O., Singh K.K. Mitochondrial regulation of epigenetics and its role in human diseases. Epigenetics. 2012;7:326–334. doi: 10.4161/epi.19547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Smiraglia D.J., Kulawiec M., Bistulfi G.L., Gupta S.G., Singh K.K. A novel role for mitochondria in regulating epigenetic modification in the nucleus. Cancer Biol. Ther. 2008;7:1182–1190. doi: 10.4161/cbt.7.8.6215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gardiner-Garden M., Frommer M. CpG islands in vertebrate genomes. J. Mol. Biol. 1987;196:261–282. doi: 10.1016/0022-2836(87)90689-9. [DOI] [PubMed] [Google Scholar]
- 120.Matsuda S., Yasukawa T., Sakaguchi Y., Ichiyanagi K., Unoki M., Gotoh K., Fukuda K., Sasaki H., Suzuki T., Kang D. Accurate estimation of 5-methylcytosine in mammalian mitochondrial DNA. Sci. Rep. 2018;8:5801. doi: 10.1038/s41598-018-24251-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Mechta M., Ingerslev L.R., Fabre O., Picard M., Barres R. Evidence Suggesting Absence of Mitochondrial DNA Methylation. Front. Genet. 2017;8:166. doi: 10.3389/fgene.2017.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hong E.E., Okitsu C.Y., Smith A.D., Hsieh C.L. Regionally specific and genome-wide analyses conclusively demonstrate the absence of CpG methylation in human mitochondrial DNA. Mol. Cell Biol. 2013;33:2683–2690. doi: 10.1128/MCB.00220-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Shock L.S., Thakkar P.V., Peterson E.J., Moran R.G., Taylor S.M. DNA methyltransferase 1, cytosine methylation, and cytosine hydroxymethylation in mammalian mitochondria. Proc. Natl. Acad. Sci. USA. 2011;108:3630–3635. doi: 10.1073/pnas.1012311108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sharma J., Kumari R., Bhargava A., Tiwari R., Mishra P.K. Mitochondrial-induced Epigenetic Modifications: From Biology to Clinical Translation. Curr. Pharm. Des. 2021;27:159–176. doi: 10.2174/1381612826666200826165735. [DOI] [PubMed] [Google Scholar]
- 125.Bicci I., Calabrese C., Golder Z.J., Gomez-Duran A., Chinnery P.F. Single-molecule mitochondrial DNA sequencing shows no evidence of CpG methylation in human cells and tissues. Nucleic Acids Res. 2021;49:12757–12768. doi: 10.1093/nar/gkab1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Yang B., Wang J.Q., Tan Y., Yuan R., Chen Z.S., Zou C. RNA methylation and cancer treatment. Pharm. Res. 2021;174:105937. doi: 10.1016/j.phrs.2021.105937. [DOI] [PubMed] [Google Scholar]
- 127.Jonkhout N., Tran J., Smith M.A., Schonrock N., Mattick J.S., Novoa E.M. The RNA modification landscape in human disease. RNA. 2017;23:1754–1769. doi: 10.1261/rna.063503.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Desrosiers R., Friderici K., Rottman F. Identification of methylated nucleosides in messenger RNA from Novikoff hepatoma cells. Proc. Natl. Acad. Sci. USA. 1974;71:3971–3975. doi: 10.1073/pnas.71.10.3971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Perry R.P., Kelley D.E. Existence of methylated messenger RNA in mouse L cells. Cell. 1974;1:37–42. doi: 10.1016/0092-8674(74)90153-6. [DOI] [Google Scholar]
- 130.Zaccara S., Ries R.J., Jaffrey S.R. Reading, writing and erasing mRNA methylation. Nat. Rev. Mol. Cell Biol. 2019;20:608–624. doi: 10.1038/s41580-019-0168-5. [DOI] [PubMed] [Google Scholar]
- 131.Dominissini D., Moshitch-Moshkovitz S., Schwartz S., Salmon-Divon M., Ungar L., Osenberg S., Cesarkas K., Jacob-Hirsch J., Amariglio N., Kupiec M., et al. Topology of the human and mouse m6A RNA methylomes revealed by m6A-seq. Nature. 2012;485:201–206. doi: 10.1038/nature11112. [DOI] [PubMed] [Google Scholar]
- 132.Meyer K.D., Saletore Y., Zumbo P., Elemento O., Mason C.E., Jaffrey S.R. Comprehensive analysis of mRNA methylation reveals enrichment in 3’ UTRs and near stop codons. Cell. 2012;149:1635–1646. doi: 10.1016/j.cell.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Deng X., Su R., Weng H., Huang H., Li Z., Chen J. RNA N6-methyladenosine modification in cancers: Current status and perspectives. Cell Res. 2018;28:507–517. doi: 10.1038/s41422-018-0034-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Huo F.C., Zhu Z.M., Pei D.S. N6-methyladenosine (m6 A) RNA modification in human cancer. Cell Prolif. 2020;53:e12921. doi: 10.1111/cpr.12921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zhang X., Wei L.H., Wang Y.X., Xiao Y., Liu J., Zhang W., Yan N., Amu G., Tang X.J., Zhang L., et al. Structural insights into FTO’s catalytic mechanism for the demethylation of multiple RNA substrates. Proc. Natl. Acad. Sci. USA. 2019;116:2919–2924. doi: 10.1073/pnas.1820574116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Liu Y., You Y., Lu Z., Yang J., Li P., Liu L., Xu H., Niu Y., Cao X. N6-methyladenosine RNA modification-mediated cellular metabolism rewiring inhibits viral replication. Science. 2019;365:1171–1176. doi: 10.1126/science.aax4468. [DOI] [PubMed] [Google Scholar]
- 137.Li Z.J., Weng H.Y., Su R., Weng X.C., Zuo Z.X., Li C.Y., Huang H.L., Nachtergaele S., Dong L., Hu C., et al. FTO Plays an Oncogenic Role in Acute Myeloid Leukemia as a N-6-Methyladenosine RNA Demethylase. Cancer Cell. 2017;31:127–141. doi: 10.1016/j.ccell.2016.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Su R., Li Z.J., Weng H.Y., Weng X.C., Zuo Z.X., Li C.Y., Huang H.L., Hu C., Qin X., Tang L.C., et al. Fto Plays an Oncogenic Role in Acute Myeloid Leukemia As a N-6-Methyladenosine RNA Demethylase. Blood. 2016;128:2706. doi: 10.1182/blood.V128.22.2706.2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Scholler E., Marks J., Marchand V., Bruckmann A., Powell C.A., Reichold M., Mutti C.D., Dettmer K., Feederle R., Huttelmaier S., et al. Balancing of mitochondrial translation through METTL8-mediated m3C modification of mitochondrial tRNAs. Mol. Cell. 2021;81:4810–4825. doi: 10.1016/j.molcel.2021.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Morscher R.J., Ducker G.S., Li S.H., Mayer J.A., Gitai Z., Sperl W., Rabinowitz J.D. Mitochondrial translation requires folate-dependent tRNA methylation. Nature. 2018;554:128–132. doi: 10.1038/nature25460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Delaunay S., Pascual G., Feng B., Klann K., Behm M., Hotz-Wagenblatt A., Richter K., Zaoui K., Herpel E., Munch C., et al. Mitochondrial RNA modifications shape metabolic plasticity in metastasis. Nature. 2022;607:593–603. doi: 10.1038/s41586-022-04898-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Vilardo E., Amman F., Toth U., Kotter A., Helm M., Rossmanith W. Functional characterization of the human tRNA methyltransferases TRMT10A and TRMT10B. Nucleic Acids Res. 2020;48:6157–6169. doi: 10.1093/nar/gkaa353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Fraga M.F., Ballestar E., Villar-Garea A., Boix-Chornet M., Espada J., Schotta G., Bonaldi T., Haydon C., Ropero S., Petrie K., et al. Loss of acetylation at Lys16 and trimethylation at Lys20 of histone H4 is a common hallmark of human cancer. Nat. Genet. 2005;37:391–400. doi: 10.1038/ng1531. [DOI] [PubMed] [Google Scholar]
- 144.Gong F., Miller K.M. Histone methylation and the DNA damage response. Mutat. Res. Rev. Mutat. Res. 2019;780:37–47. doi: 10.1016/j.mrrev.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Mazzio E.A., Soliman K.F. Basic concepts of epigenetics: Impact of environmental signals on gene expression. Epigenetics. 2012;7:119–130. doi: 10.4161/epi.7.2.18764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Brownell J.E., Allis C.D. Special HATs for special occasions: Linking histone acetylation to chromatin assembly and gene activation. Curr. Opin. Genet. Dev. 1996;6:176–184. doi: 10.1016/S0959-437X(96)80048-7. [DOI] [PubMed] [Google Scholar]
- 147.Tessarz P., Kouzarides T. Histone core modifications regulating nucleosome structure and dynamics. Nat. Rev. Mol. Cell Biol. 2014;15:703–708. doi: 10.1038/nrm3890. [DOI] [PubMed] [Google Scholar]
- 148.Diallo I., Seve M., Cunin V., Minassian F., Poisson J.F., Michelland S., Bourgoin-Voillard S. Current trends in protein acetylation analysis. Expert Rev. Proteom. 2019;16:139–159. doi: 10.1080/14789450.2019.1559061. [DOI] [PubMed] [Google Scholar]
- 149.Shahbazian M.D., Grunstein M. Functions of site-specific histone acetylation and deacetylation. Annu. Rev. Biochem. 2007;76:75–100. doi: 10.1146/annurev.biochem.76.052705.162114. [DOI] [PubMed] [Google Scholar]
- 150.Roth S.Y., Denu J.M., Allis C.D. Histone acetyltransferases. Annu. Rev. Biochem. 2001;70:81–120. doi: 10.1146/annurev.biochem.70.1.81. [DOI] [PubMed] [Google Scholar]
- 151.Swigut T., Wysocka J. H3K27 demethylases, at long last. Cell. 2007;131:29–32. doi: 10.1016/j.cell.2007.09.026. [DOI] [PubMed] [Google Scholar]
- 152.Bolden J.E., Peart M.J., Johnstone R.W. Anticancer activities of histone deacetylase inhibitors. Nat. Rev. Drug Discov. 2006;5:769–784. doi: 10.1038/nrd2133. [DOI] [PubMed] [Google Scholar]
- 153.Akimova T., Beier U.H., Liu Y., Wang L., Hancock W.W. Histone/protein deacetylases and T-cell immune responses. Blood. 2012;119:2443–2451. doi: 10.1182/blood-2011-10-292003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kida Y., Goligorsky M.S. Sirtuins, Cell Senescence, and Vascular Aging. Can. J. Cardiol. 2016;32:634–641. doi: 10.1016/j.cjca.2015.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Gertler A.A., Cohen H.Y. SIRT6, a protein with many faces. Biogerontology. 2013;14:629–639. doi: 10.1007/s10522-013-9478-8. [DOI] [PubMed] [Google Scholar]
- 156.Imai S., Yoshino J. The importance of NAMPT/NAD/SIRT1 in the systemic regulation of metabolism and ageing. Diabetes Obes. Metab. 2013;15((Suppl. S3)):26–33. doi: 10.1111/dom.12171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Berger S.L. The complex language of chromatin regulation during transcription. Nature. 2007;447:407–412. doi: 10.1038/nature05915. [DOI] [PubMed] [Google Scholar]
- 158.Demetriadou C., Kirmizis A. Histone Acetyltransferases in Cancer: Guardians or Hazards? Crit. Rev. Oncog. 2017;22:195–218. doi: 10.1615/CritRevOncog.2017024506. [DOI] [PubMed] [Google Scholar]
- 159.Eberharter A., Becker P.B. Histone acetylation: A switch between repressive and permissive chromatin—Second in review series on chromatin dynamics. EMBO Rep. 2002;3:224–229. doi: 10.1093/embo-reports/kvf053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kurdistani S.K. Histone modifications in cancer biology and prognosis. Prog. Drug Res. 2011;67:91–106. doi: 10.1007/978-3-7643-8989-5_5. [DOI] [PubMed] [Google Scholar]
- 161.Shen Y., Wei W., Zhou D.X. Histone Acetylation Enzymes Coordinate Metabolism and Gene Expression. Trends Plant Sci. 2015;20:614–621. doi: 10.1016/j.tplants.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 162.Shi Y., Lan F., Matson C., Mulligan P., Whetstine J.R., Cole P.A., Casero R.A., Shi Y. Histone demethylation mediated by the nuclear amine oxidase homolog LSD1. Cell. 2004;119:941–953. doi: 10.1016/j.cell.2004.12.012. [DOI] [PubMed] [Google Scholar]
- 163.Wellen K.E., Hatzivassiliou G., Sachdeva U.M., Bui T.V., Cross J.R., Thompson C.B. ATP-citrate lyase links cellular metabolism to histone acetylation. Science. 2009;324:1076–1080. doi: 10.1126/science.1164097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ohshima K., Oi R., Nojima S., Morii E. Mitochondria govern histone acetylation in colorectal cancer. J. Pathol. 2022;256:164–173. doi: 10.1002/path.5818. [DOI] [PubMed] [Google Scholar]
- 165.Wang L.B., Karpova A., Gritsenko M.A., Kyle J.E., Cao S., Li Y., Rykunov D., Colaprico A., Rothstein J.H., Hong R., et al. Proteogenomic and metabolomic characterization of human glioblastoma. Cancer Cell. 2021;39:509–528.e20. doi: 10.1016/j.ccell.2021.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.McBrian M.A., Behbahan I.S., Ferrari R., Su T., Huang T.W., Li K., Hong C.S., Christofk H.R., Vogelauer M., Seligson D.B., et al. Histone acetylation regulates intracellular pH. Mol. Cell. 2013;49:310–321. doi: 10.1016/j.molcel.2012.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Joyce J.A., Pollard J.W. Microenvironmental regulation of metastasis. Nat. Rev. Cancer. 2009;9:239–252. doi: 10.1038/nrc2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Krainer A.R., Mayeda A., Kozak D., Binns G. Functional expression of cloned human splicing factor SF2: Homology to RNA-binding proteins, U1 70K, and Drosophila splicing regulators. Cell. 1991;66:383–394. doi: 10.1016/0092-8674(91)90627-B. [DOI] [PubMed] [Google Scholar]
- 169.Jiang J., Zhang Y., Krainer A.R., Xu R.M. Crystal structure of human p32, a doughnut-shaped acidic mitochondrial matrix protein. Proc. Natl. Acad. Sci. USA. 1999;96:3572–3577. doi: 10.1073/pnas.96.7.3572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Ghebrehiwet B., Geisbrecht B.V., Xu X., Savitt A.G., Peerschke E.I.B. The C1q Receptors: Focus on gC1qR/p33 (C1qBP, p32, HABP-1)(1) Semin. Immunol. 2019;45:101338. doi: 10.1016/j.smim.2019.101338. [DOI] [PubMed] [Google Scholar]
- 171.Fogal V., Richardson A.D., Karmali P.P., Scheffler I.E., Smith J.W., Ruoslahti E. Mitochondrial p32 Protein Is a Critical Regulator of Tumor Metabolism via Maintenance of Oxidative Phosphorylation. Mol. Cell. Biol. 2010;30:1303–1318. doi: 10.1128/MCB.01101-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Yagi M., Uchiumi T., Takazaki S., Okuno B., Nomura M., Yoshida S., Kanki T., Kang D. p32/gC1qR is indispensable for fetal development and mitochondrial translation: Importance of its RNA-binding ability. Nucleic Acids Res. 2012;40:9717–9737. doi: 10.1093/nar/gks774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Zapata-Perez R., Wanders R.J.A., van Karnebeek C.D.M., Houtkooper R.H. NAD(+) homeostasis in human health and disease. Embo Mol. Med. 2021;13:e13943. doi: 10.15252/emmm.202113943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ansari H.R., Raghava G.P. Identification of NAD interacting residues in proteins. BMC Bioinform. 2010;11:160. doi: 10.1186/1471-2105-11-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Chambon P., Weill J.D., Mandel P. Nicotinamide mononucleotide activation of new DNA-dependent polyadenylic acid synthesizing nuclear enzyme. Biochem. Biophys. Res. Commun. 1963;11:39–43. doi: 10.1016/0006-291X(63)90024-X. [DOI] [PubMed] [Google Scholar]
- 176.Bai P. Biology of Poly(ADP-Ribose) Polymerases: The Factotums of Cell Maintenance. Mol. Cell. 2015;58:947–958. doi: 10.1016/j.molcel.2015.01.034. [DOI] [PubMed] [Google Scholar]
- 177.Gupte R., Liu Z., Kraus W.L. PARPs and ADP-ribosylation: Recent advances linking molecular functions to biological outcomes. Genes Dev. 2017;31:101–126. doi: 10.1101/gad.291518.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Imai S., Armstrong C.M., Kaeberlein M., Guarente L. Transcriptional silencing and longevity protein Sir2 is an NAD-dependent histone deacetylase. Nature. 2000;403:795–800. doi: 10.1038/35001622. [DOI] [PubMed] [Google Scholar]
- 179.Imai S., Guarente L. NAD+ and sirtuins in aging and disease. Trends Cell Biol. 2014;24:464–471. doi: 10.1016/j.tcb.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Houtkooper R.H., Pirinen E., Auwerx J. Sirtuins as regulators of metabolism and healthspan. Nat. Rev. Mol. Cell Biol. 2012;13:225–238. doi: 10.1038/nrm3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Thakur C., Chen F. Connections between metabolism and epigenetics in cancers. Semin. Cancer Biol. 2019;57:52–58. doi: 10.1016/j.semcancer.2019.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Dai H., Sinclair D.A., Ellis J.L., Steegborn C. Sirtuin activators and inhibitors: Promises, achievements, and challenges. Pharm. Ther. 2018;188:140–154. doi: 10.1016/j.pharmthera.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Murayama A., Ohmori K., Fujimura A., Minami H., Yasuzawa-Tanaka K., Kuroda T., Oie S., Daitoku H., Okuwaki M., Nagata K., et al. Epigenetic control of rDNA loci in response to intracellular energy status. Cell. 2008;133:627–639. doi: 10.1016/j.cell.2008.03.030. [DOI] [PubMed] [Google Scholar]
- 184.Menzies K.J., Zhang H., Katsyuba E., Auwerx J. Protein acetylation in metabolism—Metabolites and cofactors. Nat. Rev. Endocrinol. 2016;12:43–60. doi: 10.1038/nrendo.2015.181. [DOI] [PubMed] [Google Scholar]
- 185.Pietrocola F., Galluzzi L., Bravo-San Pedro J.M., Madeo F., Kroemer G. Acetyl coenzyme A: A central metabolite and second messenger. Cell Metab. 2015;21:805–821. doi: 10.1016/j.cmet.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 186.Shi L., Tu B.P. Acetyl-CoA and the regulation of metabolism: Mechanisms and consequences. Curr. Opin. Cell Biol. 2015;33:125–131. doi: 10.1016/j.ceb.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Srere P.A. The citrate cleavage enzyme. I. Distribution and purification. J. Biol. Chem. 1959;234:2544–2547. doi: 10.1016/S0021-9258(18)69735-2. [DOI] [PubMed] [Google Scholar]
- 188.Horner D.S., Hirt R.P., Embley T.M. A single eubacterial origin of eukaryotic pyruvate: Ferredoxin oxidoreductase genes: Implications for the evolution of anaerobic eukaryotes. Mol. Biol. Evol. 1999;16:1280–1291. doi: 10.1093/oxfordjournals.molbev.a026218. [DOI] [PubMed] [Google Scholar]
- 189.Sutendra G., Kinnaird A., Dromparis P., Paulin R., Stenson T.H., Haromy A., Hashimoto K., Zhang N., Flaim E., Michelakis E.D. A Nuclear Pyruvate Dehydrogenase Complex Is Important for the Generation of Acetyl-CoA and Histone Acetylation. Cell. 2014;158:84–97. doi: 10.1016/j.cell.2014.04.046. [DOI] [PubMed] [Google Scholar]
- 190.Choudhary C., Weinert B.T., Nishida Y., Verdin E., Mann M. The growing landscape of lysine acetylation links metabolism and cell signalling. Nat. Rev. Mol. Cell Biol. 2014;15:536–550. doi: 10.1038/nrm3841. [DOI] [PubMed] [Google Scholar]
- 191.Cai L., Sutter B.M., Li B., Tu B.P. Acetyl-CoA Induces Cell Growth and Proliferation by Promoting the Acetylation of Histones at Growth Genes. Mol. Cell. 2011;42:426–437. doi: 10.1016/j.molcel.2011.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Shi L., Tu B.P. Protein acetylation as a means to regulate protein function in tune with metabolic state. Biochem. Soc. T. 2014;42:1037–1042. doi: 10.1042/BST20140135. [DOI] [PubMed] [Google Scholar]
- 193.Cai L., Tu B.P. Cold Spring Harbor Symposia on Quantitative Biology. Volume 76. Cold Spring Harbor Laboratory Press; Cold Spring Harbor, NY, USA: 2011. On Acetyl-CoA as a Gauge of Cellular Metabolic State; pp. 195–202. [DOI] [PubMed] [Google Scholar]
- 194.Mews P., Egervari G., Nativio R., Sidoli S., Donahue G., Lombroso S.I., Alexander D.C., Riesche S.L., Heller E.A., Nestler E.J., et al. Alcohol metabolism contributes to brain histone acetylation. Nature. 2019;574:717–721. doi: 10.1038/s41586-019-1700-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Mews P., Donahue G., Drake A.M., Luczak V., Abel T., Berger S.L. Acetyl-CoA synthetase regulates histone acetylation and hippocampal memory. Nature. 2017;546:381–386. doi: 10.1038/nature22405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Greer E.L., Shi Y. Histone methylation: A dynamic mark in health, disease and inheritance. Nat. Rev. Genet. 2012;13:343–357. doi: 10.1038/nrg3173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Zhang Y., Sun Z., Jia J., Du T., Zhang N., Tang Y., Fang Y., Fang D. Overview of Histone Modification. Adv. Exp. Med. Biol. 2021;1283:1–16. doi: 10.1007/978-981-15-8104-5_1. [DOI] [PubMed] [Google Scholar]
- 198.Black J.C., Van Rechem C., Whetstine J.R. Histone lysine methylation dynamics: Establishment, regulation, and biological impact. Mol. Cell. 2012;48:491–507. doi: 10.1016/j.molcel.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Yang Y., Bedford M.T. Protein arginine methyltransferases and cancer. Nat. Rev. Cancer. 2013;13:37–50. doi: 10.1038/nrc3409. [DOI] [PubMed] [Google Scholar]
- 200.Bedford M.T., Clarke S.G. Protein Arginine Methylation in Mammals: Who, What, and Why. Mol. Cell. 2009;33:1–13. doi: 10.1016/j.molcel.2008.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Blanc R.S., Richard S. Arginine Methylation: The Coming of Age. Mol. Cell. 2017;65:8–24. doi: 10.1016/j.molcel.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 202.Dimitrova E., Turberfield A.H., Klose R.J. Histone demethylases in chromatin biology and beyond. EMBO Rep. 2015;16:1620–1639. doi: 10.15252/embr.201541113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Kooistra S.M., Helin K. Molecular mechanisms and potential functions of histone demethylases. Nat. Rev. Mol. Cell Biol. 2012;13:297–311. doi: 10.1038/nrm3327. [DOI] [PubMed] [Google Scholar]
- 204.Hou H.F., Yu H.T. Structural insights into histone lysine demethylation. Curr. Opin. Struc. Biol. 2010;20:739–748. doi: 10.1016/j.sbi.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Tsukada Y., Fang J., Erdjument-Bromage H., Warren M.E., Borchers C.H., Tempst P., Zhang Y. Histone demethylation by a family of JmjC domain-containing proteins. Nature. 2006;439:811–816. doi: 10.1038/nature04433. [DOI] [PubMed] [Google Scholar]
- 206.Whetstine J.R., Nottke A., Lan F., Huarte M., Smolikov S., Chen Z., Spooner E., Li E., Zhang G., Colaiacovo M., et al. Reversal of histone lysine trimethylation by the JMJD2 family of histone demethylases. Cell. 2006;125:467–481. doi: 10.1016/j.cell.2006.03.028. [DOI] [PubMed] [Google Scholar]
- 207.Teperino R., Schoonjans K., Auwerx J. Histone Methyl Transferases and Demethylases; Can They Link Metabolism and Transcription? Cell Metab. 2010;12:321–327. doi: 10.1016/j.cmet.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Yun J., Song S.H., Park J., Kim H.P., Yoon Y.K., Lee K.H., Han S.W., Oh D.Y., Im S.A., Bang Y.J., et al. Gene silencing of EREG mediated by DNA methylation and histone modification in human gastric cancers. Lab. Investig. 2012;92:1033–1044. doi: 10.1038/labinvest.2012.61. [DOI] [PubMed] [Google Scholar]
- 209.Kang H.S., Lee J.H., Oh K.J., Lee E.W., Han B.S., Park K.Y., Suh J.M., Min J.K., Chi S.W., Lee S.C., et al. IDH1-dependent alpha-KG regulates brown fat differentiation and function by modulating histone methylation. Metabolism. 2020;105:154173. doi: 10.1016/j.metabol.2020.154173. [DOI] [PubMed] [Google Scholar]
- 210.Parsons D.W., Jones S., Zhang X., Lin J.C., Leary R.J., Angenendt P., Mankoo P., Carter H., Siu I.M., Gallia G.L., et al. An integrated genomic analysis of human glioblastoma multiforme. Science. 2008;321:1807–1812. doi: 10.1126/science.1164382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Ulanovskaya O.A., Zuhl A.M., Cravatt B.F. NNMT promotes epigenetic remodeling in cancer by creating a metabolic methylation sink. Nat. Chem. Biol. 2013;9:300–306. doi: 10.1038/nchembio.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Creyghton M.P., Cheng A.W., Welstead G.G., Kooistra T., Carey B.W., Steine E.J., Hanna J., Lodato M.A., Frampton G.M., Sharp P.A., et al. Histone H3K27ac separates active from poised enhancers and predicts developmental state. Proc. Natl. Acad. Sci. USA. 2010;107:21931–21936. doi: 10.1073/pnas.1016071107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Xie Z., Dai J., Dai L., Tan M., Cheng Z., Wu Y., Boeke J.D., Zhao Y. Lysine succinylation and lysine malonylation in histones. Mol. Cell Proteom. 2012;11:100–107. doi: 10.1074/mcp.M111.015875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Weinert B.T., Scholz C., Wagner S.A., Iesmantavicius V., Su D., Daniel J.A., Choudhary C. Lysine succinylation is a frequently occurring modification in prokaryotes and eukaryotes and extensively overlaps with acetylation. Cell Rep. 2013;4:842–851. doi: 10.1016/j.celrep.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 215.Du J., Zhou Y., Su X., Yu J.J., Khan S., Jiang H., Kim J., Woo J., Kim J.H., Choi B.H., et al. Sirt5 is a NAD-dependent protein lysine demalonylase and desuccinylase. Science. 2011;334:806–809. doi: 10.1126/science.1207861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Rosen R., Becher D., Buttner K., Biran D., Hecker M., Ron E.Z. Probing the active site of homoserine trans-succinylase. FEBS Lett. 2004;577:386–392. doi: 10.1016/j.febslet.2004.10.037. [DOI] [PubMed] [Google Scholar]
- 217.Zhang Z.H., Tan M.J., Xie Z.Y., Dai L.Z., Chen Y., Zhao Y.M. Identification of lysine succinylation as a new post-translational modification. Nat. Chem. Biol. 2011;7:58–63. doi: 10.1038/nchembio.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Sabari B.R., Zhang D., Allis C.D., Zhao Y.M. Metabolic regulation of gene expression through histone acylations. Nat.Rev. Mol. Cell Biol. 2017;18:90–101. doi: 10.1038/nrm.2016.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Wang Y.G., Guo Y.R., Liu K., Yin Z., Liu R., Xia Y., Tan L., Yang P.Y., Lee J.H., Li X.J., et al. KAT2A coupled with the alpha-KGDH complex acts as a histone H3 succinyltransferase. Nature. 2017;552:273–277. doi: 10.1038/nature25003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Zhao S., Zhang X., Li H. Beyond histone acetylation-writing and erasing histone acylations. Curr. Opin. Struct. Biol. 2018;53:169–177. doi: 10.1016/j.sbi.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 221.Yang G., Yuan Y., Yuan H., Wang J., Yun H., Geng Y., Zhao M., Li L., Weng Y., Liu Z., et al. Histone acetyltransferase 1 is a succinyltransferase for histones and non-histones and promotes tumorigenesis. EMBO Rep. 2021;22:e50967. doi: 10.15252/embr.202050967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Peng C., Lu Z., Xie Z., Cheng Z., Chen Y., Tan M., Luo H., Zhang Y., He W., Yang K., et al. The first identification of lysine malonylation substrates and its regulatory enzyme. Mol. Cell Proteom. 2011;10:M111012658. doi: 10.1074/mcp.M111.012658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Park J., Chen Y., Tishkoff D.X., Peng C., Tan M., Dai L., Xie Z., Zhang Y., Zwaans B.M., Skinner M.E., et al. SIRT5-mediated lysine desuccinylation impacts diverse metabolic pathways. Mol. Cell. 2013;50:919–930. doi: 10.1016/j.molcel.2013.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Rardin M.J., He W., Nishida Y., Newman J.C., Carrico C., Danielson S.R., Guo A., Gut P., Sahu A.K., Li B., et al. SIRT5 regulates the mitochondrial lysine succinylome and metabolic networks. Cell Metab. 2013;18:920–933. doi: 10.1016/j.cmet.2013.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Li L., Shi L., Yang S.D., Yan R.R., Zhang D., Yang J.G., He L., Li W.J., Yi X., Sun L.Y., et al. SIRT7 is a histone desuccinylase that functionally links to chromatin compaction and genome stability. Nat. Commun. 2016;7:12235. doi: 10.1038/ncomms12235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Trefely S., Lovell C.D., Snyder N.W., Wellen K.E. Compartmentalised acyl-CoA metabolism and roles in chromatin regulation. Mol. Metab. 2020;38:100941. doi: 10.1016/j.molmet.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Paine P.L., Moore L.C., Horowitz S.B. Nuclear envelope permeability. Nature. 1975;254:109–114. doi: 10.1038/254109a0. [DOI] [PubMed] [Google Scholar]
- 228.Palmieri F. The mitochondrial transporter family (SLC25): Physiological and pathological implications. Pflug. Arch. 2004;447:689–709. doi: 10.1007/s00424-003-1099-7. [DOI] [PubMed] [Google Scholar]
- 229.Monne M., Miniero D.V., Iacobazzi V., Bisaccia F., Fiermonte G. The mitochondrial oxoglutarate carrier: From identification to mechanism. J. Bioenerg. Biomembr. 2013;45:1–13. doi: 10.1007/s10863-012-9475-7. [DOI] [PubMed] [Google Scholar]
- 230.Smestad J., Erber L., Chen Y., Maher L.J. Chromatin Succinylation Correlates with Active Gene Expression and Is Perturbed by Defective TCA Cycle Metabolism. Iscience. 2018;2:63–75. doi: 10.1016/j.isci.2018.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Holt G.D., Snow C.M., Senior A., Haltiwanger R.S., Gerace L., Hart G.W. Nuclear pore complex glycoproteins contain cytoplasmically disposed O-linked N-acetylglucosamine. J. Cell Biol. 1987;104:1157–1164. doi: 10.1083/jcb.104.5.1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Zhu Y., Hart G.W. Targeting O-GlcNAcylation to develop novel therapeutics. Mol. Asp. Med. 2021;79:100885. doi: 10.1016/j.mam.2020.100885. [DOI] [PubMed] [Google Scholar]
- 233.Lee J.B., Pyo K.H., Kim H.R. Role and Function of O-GlcNAcylation in Cancer. Cancers. 2021;13:5365. doi: 10.3390/cancers13215365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Finlay D.R., Newmeyer D.D., Price T.M., Forbes D.J. Inhibition of in vitro nuclear transport by a lectin that binds to nuclear pores. J. Cell Biol. 1987;104:189–200. doi: 10.1083/jcb.104.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Hanover J.A., Cohen C.K., Willingham M.C., Park M.K. O-Linked N-Acetylglucosamine Is Attached to Proteins of the Nuclear-Pore—Evidence for Cytoplasmic and Nucleoplasmic Glycoproteins. J. Biol. Chem. 1987;262:9887–9894. doi: 10.1016/S0021-9258(18)48017-9. [DOI] [PubMed] [Google Scholar]
- 236.Park M.K., D’Onofrio M., Willingham M.C., Hanover J.A. A monoclonal antibody against a family of nuclear pore proteins (nucleoporins): O-linked N-acetylglucosamine is part of the immunodeterminant. Proc. Natl. Acad. Sci. USA. 1987;84:6462–6466. doi: 10.1073/pnas.84.18.6462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Kelly W.G., Hart G.W. Glycosylation of chromosomal proteins: Localization of O-linked N-acetylglucosamine in Drosophila chromatin. Cell. 1989;57:243–251. doi: 10.1016/0092-8674(89)90962-8. [DOI] [PubMed] [Google Scholar]
- 238.Love D.C., Kochan J., Cathey R.L., Shin S.H., Hanover J.A. Mitochondrial and nucleocytoplasmic targeting of O-linked GlcNAc transferase. J. Cell Sci. 2003;116:647–654. doi: 10.1242/jcs.00246. [DOI] [PubMed] [Google Scholar]
- 239.Shin S.H., Love D.C., Hanover J.A. Elevated O-GlcNAc-dependent signaling through inducible mOGT expression selectively triggers apoptosis. Amino Acids. 2011;40:885–893. doi: 10.1007/s00726-010-0719-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Hanover J.A. Epigenetics Gets Sweeter: O-GlcNAc Joins the “Histone Code”. Chem. Biol. 2010;17:1272–1274. doi: 10.1016/j.chembiol.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Sakabe K., Wang Z.H., Hart G.W. beta-N-acetylglucosamine (O-GlcNAc) is part of the histone code. Proc. Natl. Acad. Sci. USA. 2010;107:19915–19920. doi: 10.1073/pnas.1009023107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Fujiki R., Hashiba W., Sekine H., Yokoyama A., Chikanishi T., Ito S., Imai Y., Kim J., He H.H., Igarashi K., et al. GlcNAcylation of histone H2B facilitates its monoubiquitination. Nature. 2011;480:557–560. doi: 10.1038/nature10656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Xu Q., Yang C., Du Y., Chen Y., Liu H., Deng M., Zhang H., Zhang L., Liu T., Liu Q., et al. AMPK regulates histone H2B O-GlcNAcylation. Nucleic Acids Res. 2014;42:5594–5604. doi: 10.1093/nar/gku236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Dehennaut V., Leprince D., Lefebvre T. O-GlcNAcylation, an epigenetic mark. Focus on the histone code, TET family proteins, and polycomb group proteins. Front. Endocrinol. 2014;5:155. doi: 10.3389/fendo.2014.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Hanover J.A., Krause M.W., Love D.C. The hexosamine signaling pathway: O-GlcNAc cycling in feast or famine. Biochim. Biophys. Acta. 2010;1800:80–95. doi: 10.1016/j.bbagen.2009.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Fong J.J., Nguyen B.L., Bridger R., Medrano E.E., Wells L., Pan S.J., Sifers R.N. beta-N-Acetylglucosamine (O-GlcNAc) Is a Novel Regulator of Mitosis-specific Phosphorylations on Histone H3. J. Biol. Chem. 2012;287:12195–12203. doi: 10.1074/jbc.M111.315804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Zhang S., Roche K., Nasheuer H.P., Lowndes N.F. Modification of histones by sugar beta-N-acetylglucosamine (GlcNAc) occurs on multiple residues, including histone H3 serine 10, and is cell cycle-regulated. J. Biol. Chem. 2011;286:37483–37495. doi: 10.1074/jbc.M111.284885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Sekine O., Love D.C., Rubenstein D.S., Hanover J.A. Blocking O-linked GlcNAc cycling in Drosophila insulin-producing cells perturbs glucose-insulin homeostasis. J. Biol. Chem. 2010;285:38684–38691. doi: 10.1074/jbc.M110.155192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Sinclair D.A.R., Syrzycka M., Macauley M.S., Rastgardani T., Komljenovic I., Vocadlo D.J., Brock H.W., Honda B.M. Drosophila O-GlcNAc transferase (OGT) is encoded by the Polycomb group (PcG) gene, super sex combs (sxc) Proc. Natl. Acad. Sci. USA. 2009;106:13427–13432. doi: 10.1073/pnas.0904638106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Kassis J.A., Kennison J.A. Recruitment of polycomb complexes: A role for SCM. Mol. Cell Biol. 2010;30:2581–2583. doi: 10.1128/MCB.00231-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Haltiwanger R.S., Holt G.D., Hart G.W. Enzymatic Addition of O-Glcnac to Nuclear and Cytoplasmic Proteins—Identification of a Uridine Diphospho-N-Acetylglucosamine-Peptide Beta-N-Acetylglucosaminyltransferase. J. Biol. Chem. 1990;265:2563–2568. doi: 10.1016/S0021-9258(19)39838-2. [DOI] [PubMed] [Google Scholar]
- 252.Kornfeld S., Kornfeld R., Neufeld E.F., O’Brien P.J. The Feedback Control of Sugar Nucleotide Biosynthesis in Liver. Proc. Natl. Acad. Sci. USA. 1964;52:371–379. doi: 10.1073/pnas.52.2.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Wellen K.E., Thompson C.B. A two-way street: Reciprocal regulation of metabolism and signalling. Nat. Rev. Mol. Cell Biol. 2012;13:270–276. doi: 10.1038/nrm3305. [DOI] [PubMed] [Google Scholar]
- 254.Gut P., Verdin E. The nexus of chromatin regulation and intermediary metabolism. Nature. 2013;502:489–498. doi: 10.1038/nature12752. [DOI] [PubMed] [Google Scholar]
- 255.Chen Q., Chen Y., Bian C., Fujiki R., Yu X. TET2 promotes histone O-GlcNAcylation during gene transcription. Nature. 2013;493:561–564. doi: 10.1038/nature11742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Deplus R., Delatte B., Schwinn M.K., Defrance M., Mendez J., Murphy N., Dawson M.A., Volkmar M., Putmans P., Calonne E., et al. TET2 and TET3 regulate GlcNAcylation and H3K4 methylation through OGT and SET1/COMPASS. EMBO J. 2013;32:645–655. doi: 10.1038/emboj.2012.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Ito R., Katsura S., Shimada H., Tsuchiya H., Hada M., Okumura T., Sugawara A., Yokoyama A. TET3-OGT interaction increases the stability and the presence of OGT in chromatin. Genes Cells. 2014;19:52–65. doi: 10.1111/gtc.12107. [DOI] [PubMed] [Google Scholar]
- 258.Kronlage M., Dewenter M., Grosso J., Fleming T., Oehl U., Lehmann L.H., Falcao-Pires I., Leite-Moreira A.F., Volk N., Grone H.J., et al. O-GlcNAcylation of Histone Deacetylase 4 Protects the Diabetic Heart From Failure. Circulation. 2019;140:580–594. doi: 10.1161/CIRCULATIONAHA.117.031942. [DOI] [PubMed] [Google Scholar]
- 259.Zhu G., Tao T., Zhang D., Liu X., Qiu H., Han L., Xu Z., Xiao Y., Cheng C., Shen A. O-GlcNAcylation of histone deacetylases 1 in hepatocellular carcinoma promotes cancer progression. Glycobiology. 2016;26:820–833. doi: 10.1093/glycob/cww025. [DOI] [PubMed] [Google Scholar]
- 260.Zhang D., Tang Z., Huang H., Zhou G., Cui C., Weng Y., Liu W., Kim S., Lee S., Perez-Neut M., et al. Metabolic regulation of gene expression by histone lactylation. Nature. 2019;574:575–580. doi: 10.1038/s41586-019-1678-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Liberti M.V., Locasale J.W. Histone Lactylation: A New Role for Glucose Metabolism. Trends Biochem. Sci. 2020;45:179–182. doi: 10.1016/j.tibs.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 262.Hui S., Ghergurovich J.M., Morscher R.J., Jang C., Teng X., Lu W., Esparza L.A., Reya T., Le Z., Yanxiang Guo J., et al. Glucose feeds the TCA cycle via circulating lactate. Nature. 2017;551:115–118. doi: 10.1038/nature24057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Colegio O.R., Chu N.Q., Szabo A.L., Chu T., Rhebergen A.M., Jairam V., Cyrus N., Brokowski C.E., Eisenbarth S.C., Phillips G.M., et al. Functional polarization of tumour-associated macrophages by tumour-derived lactic acid. Nature. 2014;513:559–563. doi: 10.1038/nature13490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Yu J., Chai P., Xie M., Ge S., Ruan J., Fan X., Jia R. Histone lactylation drives oncogenesis by facilitating m6A reader protein YTHDF2 expression in ocular melanoma. Genome Biol. 2021;22:85. doi: 10.1186/s13059-021-02308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Irizarry-Caro R.A., McDaniel M.M., Overcast G.R., Jain V.G., Troutman T.D., Pasare C. TLR signaling adapter BCAP regulates inflammatory to reparatory macrophage transition by promoting histone lactylation. Proc. Natl. Acad. Sci. USA. 2020;117:30628–30638. doi: 10.1073/pnas.2009778117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Dai X., Lv X., Thompson E.W., Ostrikov K.K. Histone lactylation: Epigenetic mark of glycolytic switch. Trends Genet. 2022;38:124–127. doi: 10.1016/j.tig.2021.09.009. [DOI] [PubMed] [Google Scholar]
- 267.Brooks G.A. Lactate as a fulcrum of metabolism. Redox Biol. 2020;35:101454. doi: 10.1016/j.redox.2020.101454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Passarella S., de Bari L., Valenti D., Pizzuto R., Paventi G., Atlante A. Mitochondria and L-lactate metabolism. FEBS Lett. 2008;582:3569–3576. doi: 10.1016/j.febslet.2008.09.042. [DOI] [PubMed] [Google Scholar]
- 269.Glancy B., Kane D.A., Kavazis A.N., Goodwin M.L., Willis W.T., Gladden L.B. Mitochondrial lactate metabolism: History and implications for exercise and disease. J. Physiol. 2021;599:863–888. doi: 10.1113/JP278930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Chen Y.J., Mahieu N.G., Huang X.J., Singh M., Crawford P.A., Johnson S.L., Gross R.W., Schaefer J., Patti G.J. Lactate metabolism is associated with mammalian mitochondria. Nat. Chem. Biol. 2016;12:937–943. doi: 10.1038/nchembio.2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Chen A.N., Luo Y., Yang Y.H., Fu J.T., Geng X.M., Shi J.P., Yang J. Lactylation, a Novel Metabolic Reprogramming Code: Current Status and Prospects. Front. Immunol. 2021;12:688910. doi: 10.3389/fimmu.2021.688910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Kraus D., Yang Q., Kong D., Banks A.S., Zhang L., Rodgers J.T., Pirinen E., Pulinilkunnil T.C., Gong F., Wang Y.C., et al. Nicotinamide N-methyltransferase knockdown protects against diet-induced obesity. Nature. 2014;508:258–262. doi: 10.1038/nature13198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Gao W., Liu J.L., Lu X., Yang Q. Epigenetic regulation of energy metabolism in obesity. J. Mol. Cell Biol. 2021;13:480–499. doi: 10.1093/jmcb/mjab043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Duteil D., Metzger E., Willmann D., Karagianni P., Friedrichs N., Greschik H., Gunther T., Buettner R., Talianidis I., Metzger D., et al. LSD1 promotes oxidative metabolism of white adipose tissue. Nat. Commun. 2014;5:4093. doi: 10.1038/ncomms5093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Barres R., Osler M.E., Yan J., Rune A., Fritz T., Caidahl K., Krook A., Zierath J.R. Non-CpG Methylation of the PGC-1 alpha Promoter through DNMT3B Controls Mitochondrial Density. Cell Metab. 2009;10:189–198. doi: 10.1016/j.cmet.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 276.Barres R., Yan J., Egan B., Treebak J.T., Rasmussen M., Fritz T., Caidahl K., Krook A., O’Gorman D.J., Zierath J.R. Acute exercise remodels promoter methylation in human skeletal muscle. Cell Metab. 2012;15:405–411. doi: 10.1016/j.cmet.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 277.Vizioli M.G., Liu T., Miller K.N., Robertson N.A., Gilroy K., Lagnado A.B., Perez-Garcia A., Kiourtis C., Dasgupta N., Lei X., et al. Mitochondria-to-nucleus retrograde signaling drives formation of cytoplasmic chromatin and inflammation in senescence. Genes Dev. 2020;34:428–445. doi: 10.1101/gad.331272.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Shao L.W., Peng Q., Dong M., Gao K., Li Y., Li Y., Li C.Y., Liu Y. Histone deacetylase HDA-1 modulates mitochondrial stress response and longevity. Nat. Commun. 2020;11:4639. doi: 10.1038/s41467-020-18501-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Vaupel P., Multhoff G. Revisiting the Warburg effect: Historical dogma versus current understanding. J. Physiol. 2021;599:1745–1757. doi: 10.1113/JP278810. [DOI] [PubMed] [Google Scholar]
- 280.Lin R., Tao R., Gao X., Li T., Zhou X., Guan K.L., Xiong Y., Lei Q.Y. Acetylation stabilizes ATP-citrate lyase to promote lipid biosynthesis and tumor growth. Mol. Cell. 2013;51:506–518. doi: 10.1016/j.molcel.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Uyeda K., Repa J.J. Carbohydrate response element binding protein, ChREBP, a transcription factor coupling hepatic glucose utilization and lipid synthesis. Cell Metab. 2006;4:107–110. doi: 10.1016/j.cmet.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 282.Yang Y., Gibson G.E. Succinylation Links Metabolism to Protein Functions. Neurochem. Res. 2019;44:2346–2359. doi: 10.1007/s11064-019-02780-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Zhang Y., Bharathi S.S., Rardin M.J., Lu J., Maringer K.V., Sims-Lucas S., Prochownik E.V., Gibson B.W., Goetzman E.S. Lysine desuccinylase SIRT5 binds to cardiolipin and regulates the electron transport chain. J. Biol. Chem. 2017;292:10239–10249. doi: 10.1074/jbc.M117.785022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Lu J., Tan M., Cai Q. The Warburg effect in tumor progression: Mitochondrial oxidative metabolism as an anti-metastasis mechanism. Cancer Lett. 2015;356:156–164. doi: 10.1016/j.canlet.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Zhu X.X., Xuan Z.F., Chen J., Li Z.Q., Zheng S.S., Song P.H. How DNA methylation affects the Warburg effect. Int. J. Biol. Sci. 2020;16:2029–2041. doi: 10.7150/ijbs.45420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Singh S., Narayanan S.P., Biswas K., Gupta A., Ahuja N., Yadav S., Panday R.K., Samaiya A., Sharan S.K., Shukla S. Intragenic DNA methylation and BORIS-mediated cancer-specific splicing contribute to the Warburg effect. Proc. Natl. Acad. Sci. USA. 2017;114:11440–11445. doi: 10.1073/pnas.1708447114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Subramaniam A.V., Yehya A.H.S., Cheng W.K., Wang X., Oon C.E. Epigenetics: The master control of endothelial cell fate in cancer. Life Sci. 2019;232:116652. doi: 10.1016/j.lfs.2019.116652. [DOI] [PubMed] [Google Scholar]
- 288.Jang S., Hwang J., Jeong H.S. The Role of Histone Acetylation in Mesenchymal Stem Cell Differentiation. Chonnam. Med. J. 2022;58:6–12. doi: 10.4068/cmj.2022.58.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Prasetyanti P.R., Medema J.P. Intra-tumor heterogeneity from a cancer stem cell perspective. Mol. Cancer. 2017;16:41. doi: 10.1186/s12943-017-0600-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Anderson A.R., Weaver A.M., Cummings P.T., Quaranta V. Tumor morphology and phenotypic evolution driven by selective pressure from the microenvironment. Cell. 2006;127:905–915. doi: 10.1016/j.cell.2006.09.042. [DOI] [PubMed] [Google Scholar]
- 291.Sottoriva A., Verhoeff J.J., Borovski T., McWeeney S.K., Naumov L., Medema J.P., Sloot P.M., Vermeulen L. Cancer stem cell tumor model reveals invasive morphology and increased phenotypical heterogeneity. Cancer Res. 2010;70:46–56. doi: 10.1158/0008-5472.CAN-09-3663. [DOI] [PubMed] [Google Scholar]
- 292.Waclaw B., Bozic I., Pittman M.E., Hruban R.H., Vogelstein B., Nowak M.A. A spatial model predicts that dispersal and cell turnover limit intratumour heterogeneity. Nature. 2015;525:261–264. doi: 10.1038/nature14971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Clevers H. The cancer stem cell: Premises, promises and challenges. Nat. Med. 2011;17:313–319. doi: 10.1038/nm.2304. [DOI] [PubMed] [Google Scholar]
- 294.Nowell P.C. The clonal evolution of tumor cell populations. Science. 1976;194:23–28. doi: 10.1126/science.959840. [DOI] [PubMed] [Google Scholar]
- 295.Bonnet D., Dick J.E. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat. Med. 1997;3:730–737. doi: 10.1038/nm0797-730. [DOI] [PubMed] [Google Scholar]
- 296.Eun K., Ham S.W., Kim H. Cancer stem cell heterogeneity: Origin and new perspectives on CSC targeting. BMB Rep. 2017;50:117–125. doi: 10.5483/BMBRep.2017.50.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Medema J.P. Cancer stem cells: The challenges ahead. Nat. Cell Biol. 2013;15:338–344. doi: 10.1038/ncb2717. [DOI] [PubMed] [Google Scholar]
- 298.Meacham C.E., Morrison S.J. Tumour heterogeneity and cancer cell plasticity. Nature. 2013;501:328–337. doi: 10.1038/nature12624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Ferrer A.I., Trinidad J.R., Sandiford O., Etchegaray J.P., Rameshwar P. Epigenetic dynamics in cancer stem cell dormancy. Cancer Metastasis Rev. 2020;39:721–738. doi: 10.1007/s10555-020-09882-x. [DOI] [PubMed] [Google Scholar]
- 300.Dawson M.A., Kouzarides T. Cancer epigenetics: From mechanism to therapy. Cell. 2012;150:12–27. doi: 10.1016/j.cell.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 301.Munoz P., Iliou M.S., Esteller M. Epigenetic alterations involved in cancer stem Cell Rep.rogramming. Mol. Oncol. 2012;6:620–636. doi: 10.1016/j.molonc.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Pace L., Amigorena S. Epigenetics of T cell fate decision. Curr. Opin. Immunol. 2020;63:43–50. doi: 10.1016/j.coi.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 303.Saeed S., Quintin J., Kerstens H.H., Rao N.A., Aghajanirefah A., Matarese F., Cheng S.C., Ratter J., Berentsen K., van der Ent M.A., et al. Epigenetic programming of monocyte-to-macrophage differentiation and trained innate immunity. Science. 2014;345:1251086. doi: 10.1126/science.1251086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Alvarez-Errico D., Vento-Tormo R., Sieweke M., Ballestar E. Epigenetic control of myeloid cell differentiation, identity and function. Nat. Rev. Immunol. 2015;15:7–17. doi: 10.1038/nri3777. [DOI] [PubMed] [Google Scholar]
- 305.Ziller M.J., Gu H., Muller F., Donaghey J., Tsai L.T., Kohlbacher O., De Jager P.L., Rosen E.D., Bennett D.A., Bernstein B.E., et al. Charting a dynamic DNA methylation landscape of the human genome. Nature. 2013;500:477–481. doi: 10.1038/nature12433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Berdasco M., Esteller M. DNA methylation in stem cell renewal and multipotency. Stem Cell Res. Ther. 2011;2:42. doi: 10.1186/scrt83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Neri F., Rapelli S., Krepelova A., Incarnato D., Parlato C., Basile G., Maldotti M., Anselmi F., Oliviero S. Intragenic DNA methylation prevents spurious transcription initiation. Nature. 2017;543:72–77. doi: 10.1038/nature21373. [DOI] [PubMed] [Google Scholar]
- 308.Skvortsova K., Stirzaker C., Taberlay P. The DNA methylation landscape in cancer. Essays Biochem. 2019;63:797–811. doi: 10.1042/EBC20190037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Vincent A., Van Seuningen I. Epigenetics, stem cells and epithelial cell fate. Differentiation. 2009;78:99–107. doi: 10.1016/j.diff.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 310.Berdasco M., Esteller M. Aberrant Epigenetic Landscape in Cancer: How Cellular Identity Goes Awry. Dev. Cell. 2010;19:698–711. doi: 10.1016/j.devcel.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 311.Esteller M. Epigenetics in cancer. N. Engl. J. Med. 2008;358:1148–1159. doi: 10.1056/NEJMra072067. [DOI] [PubMed] [Google Scholar]
- 312.Monk M., Boubelik M., Lehnert S. Temporal and regional changes in DNA methylation in the embryonic, extraembryonic and germ cell lineages during mouse embryo development. Development. 1987;99:371–382. doi: 10.1242/dev.99.3.371. [DOI] [PubMed] [Google Scholar]
- 313.Hodges E., Molaro A., Dos Santos C.O., Thekkat P., Song Q., Uren P.J., Park J., Butler J., Rafii S., McCombie W.R., et al. Directional DNA methylation changes and complex intermediate states accompany lineage specificity in the adult hematopoietic compartment. Mol. Cell. 2011;44:17–28. doi: 10.1016/j.molcel.2011.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Lagarkova M.A., Volchkov P.Y., Lyakisheva A.V., Philonenko E.S., Kiselev S.L. Diverse epigenetic profile of novel human embryonic stem cell lines. Cell Cycle. 2006;5:416–420. doi: 10.4161/cc.5.4.2440. [DOI] [PubMed] [Google Scholar]
- 315.Yeo S., Jeong S., Kim J., Han J.S., Han Y.M., Kang Y.K. Characterization of DNA methylation change in stem cell marker genes during differentiation of human embryonic stem cells. Biochem. Biophys. Res. Commun. 2007;359:536–542. doi: 10.1016/j.bbrc.2007.05.120. [DOI] [PubMed] [Google Scholar]
- 316.Fouse S.D., Shen Y., Pellegrini M., Cole S., Meissner A., Van Neste L., Jaenisch R., Fan G. Promoter CpG methylation contributes to ES cell gene regulation in parallel with Oct4/Nanog, PcG complex, and histone H3 K4/K27 trimethylation. Cell Stem Cell. 2008;2:160–169. doi: 10.1016/j.stem.2007.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Loh Y.H., Wu Q., Chew J.L., Vega V.B., Zhang W., Chen X., Bourque G., George J., Leong B., Liu J., et al. The Oct4 and Nanog transcription network regulates pluripotency in mouse embryonic stem cells. Nat. Genet. 2006;38:431–440. doi: 10.1038/ng1760. [DOI] [PubMed] [Google Scholar]
- 318.Boyer L.A., Lee T.I., Cole M.F., Johnstone S.E., Levine S.S., Zucker J.P., Guenther M.G., Kumar R.M., Murray H.L., Jenner R.G., et al. Core transcriptional regulatory circuitry in human embryonic stem cells. Cell. 2005;122:947–956. doi: 10.1016/j.cell.2005.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Hattori N., Imao Y., Nishino K., Hattori N., Ohgane J., Yagi S., Tanaka S., Shiota K. Epigenetic regulation of Nanog gene in embryonic stem and trophoblast stem cells. Genes Cells. 2007;12:387–396. doi: 10.1111/j.1365-2443.2007.01058.x. [DOI] [PubMed] [Google Scholar]
- 320.Hawkins R.D., Hon G.C., Lee L.K., Ngo Q., Lister R., Pelizzola M., Edsall L.E., Kuan S., Luu Y., Klugman S., et al. Distinct epigenomic landscapes of pluripotent and lineage-committed human cells. Cell Stem Cell. 2010;6:479–491. doi: 10.1016/j.stem.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Bibikova M., Chudin E., Wu B., Zhou L.X., Garcia E.W., Liu Y., Shin S., Plaia T.W., Auerbach J.M., Arking D.E., et al. Human embryonic stem cells have a unique epigenetic signature. Genome Res. 2006;16:1075–1083. doi: 10.1101/gr.5319906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Mohn F., Weber M., Rebhan M., Roloff T.C., Richter J., Stadler M.B., Bibel M., Schubeler D. Lineage-specific polycomb targets and de novo DNA methylation define restriction and potential of neuronal progenitors. Mol. Cell. 2008;30:755–766. doi: 10.1016/j.molcel.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 323.Qian X., Shen Q., Goderie S.K., He W., Capela A., Davis A.A., Temple S. Timing of CNS cell generation: A programmed sequence of neuron and glial cell production from isolated murine cortical stem cells. Neuron. 2000;28:69–80. doi: 10.1016/S0896-6273(00)00086-6. [DOI] [PubMed] [Google Scholar]
- 324.Lister R., Pelizzola M., Dowen R.H., Hawkins R.D., Hon G., Tonti-Filippini J., Nery J.R., Lee L., Ye Z., Ngo Q.M., et al. Human DNA methylomes at base resolution show widespread epigenomic differences. Nature. 2009;462:315–322. doi: 10.1038/nature08514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Tzika E., Dreker T., Imhof A. Epigenetics and Metabolism in Health and Disease. Front. Genet. 2018;9:361. doi: 10.3389/fgene.2018.00361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Easwaran H., Tsai H.C., Baylin S.B. Cancer epigenetics: Tumor heterogeneity, plasticity of stem-like states, and drug resistance. Mol. Cell. 2014;54:716–727. doi: 10.1016/j.molcel.2014.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Smith Z.D., Meissner A. DNA methylation: Roles in mammalian development. Nat. Rev. Genet. 2013;14:204–220. doi: 10.1038/nrg3354. [DOI] [PubMed] [Google Scholar]
- 328.Bergman Y., Cedar H. DNA methylation dynamics in health and disease. Nat. Struct. Mol. Biol. 2013;20:274–281. doi: 10.1038/nsmb.2518. [DOI] [PubMed] [Google Scholar]
- 329.Varley K.E., Gertz J., Bowling K.M., Parker S.L., Reddy T.E., Pauli-Behn F., Cross M.K., Williams B.A., Stamatoyannopoulos J.A., Crawford G.E., et al. Dynamic DNA methylation across diverse human cell lines and tissues. Genome Res. 2013;23:555–567. doi: 10.1101/gr.147942.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Irizarry R.A., Ladd-Acosta C., Wen B., Wu Z.J., Montano C., Onyango P., Cui H.M., Gabo K., Rongione M., Webster M., et al. The human colon cancer methylome shows similar hypo- and hypermethylation at conserved tissue-specific CpG island shores. Nat. Genet. 2009;41:178–186. doi: 10.1038/ng.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Nazor K.L., Altun G., Lynch C., Tran H., Harness J.V., Slavin I., Garitaonandia I., Muller F.J., Wang Y.C., Boscolo F.S., et al. Recurrent Variations in DNA Methylation in Human Pluripotent Stem Cells and Their Differentiated Derivatives. Cell Stem Cell. 2012;10:620–634. doi: 10.1016/j.stem.2012.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Weber M., Davies J.J., Wittig D., Oakeley E.J., Haase M., Lam W.L., Schubeler D. Chromosome-wide and promoter-specific analyses identify sites of differential DNA methylation in normal and transformed human cells. Nat. Genet. 2005;37:853–862. doi: 10.1038/ng1598. [DOI] [PubMed] [Google Scholar]
- 333.Meissner A., Mikkelsen T.S., Gu H., Wernig M., Hanna J., Sivachenko A., Zhang X., Bernstein B.E., Nusbaum C., Jaffe D.B., et al. Genome-scale DNA methylation maps of pluripotent and differentiated cells. Nature. 2008;454:766–770. doi: 10.1038/nature07107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Laurent L., Wong E., Li G., Huynh T., Tsirigos A., Ong C.T., Low H.M., Kin Sung K.W., Rigoutsos I., Loring J., et al. Dynamic changes in the human methylome during differentiation. Genome Res. 2010;20:320–331. doi: 10.1101/gr.101907.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Berman B.P., Weisenberger D.J., Aman J.F., Hinoue T., Ramjan Z., Liu Y., Noushmehr H., Lange C.P., van Dijk C.M., Tollenaar R.A., et al. Regions of focal DNA hypermethylation and long-range hypomethylation in colorectal cancer coincide with nuclear lamina-associated domains. Nat. Genet. 2011;44:40–46. doi: 10.1038/ng.969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Cohen N.M., Kenigsberg E., Tanay A. Primate CpG islands are maintained by heterogeneous evolutionary regimes involving minimal selection. Cell. 2011;145:773–786. doi: 10.1016/j.cell.2011.04.024. [DOI] [PubMed] [Google Scholar]
- 337.Davuluri R.V., Suzuki Y., Sugano S., Plass C., Huang T.H.M. The functional consequences of alternative promoter use in mammalian genomes. Trends Genet. 2008;24:167–177. doi: 10.1016/j.tig.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 338.Demircioglu D., Cukuroglu E., Kindermans M., Nandi T., Calabrese C., Fonseca N.A., Kahles A., Lehmann K.V., Stegle O., Brazma A., et al. A Pan-cancer Transcriptome Analysis Reveals Pervasive Regulation through Alternative Promoters. Cell. 2019;178:1465–1477.e17. doi: 10.1016/j.cell.2019.08.018. [DOI] [PubMed] [Google Scholar]
- 339.Qamra A., Xing M., Padmanabhan N., Kwok J.J.T., Zhang S., Xu C., Leong Y.S., Lee Lim A.P., Tang Q., Ooi W.F., et al. Epigenomic Promoter Alterations Amplify Gene Isoform and Immunogenic Diversity in Gastric Adenocarcinoma. Cancer Discov. 2017;7:630–651. doi: 10.1158/2159-8290.CD-16-1022. [DOI] [PubMed] [Google Scholar]
- 340.Sotillo E., Barrett D.M., Black K.L., Bagashev A., Oldridge D., Wu G., Sussman R., Lanauze C., Ruella M., Gazzara M.R., et al. Convergence of Acquired Mutations and Alternative Splicing of CD19 Enables Resistance to CART-19 Immunotherapy. Cancer Discov. 2015;5:1282–1295. doi: 10.1158/2159-8290.CD-15-1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Ma X., Liu Y., Liu Y., Alexandrov L.B., Edmonson M.N., Gawad C., Zhou X., Li Y., Rusch M.C., Easton J., et al. Pan-cancer genome and transcriptome analyses of 1699 paediatric leukaemias and solid tumours. Nature. 2018;555:371–376. doi: 10.1038/nature25795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Grobner S.N., Worst B.C., Weischenfeldt J., Buchhalter I., Kleinheinz K., Rudneva V.A., Johann P.D., Balasubramanian G.P., Segura-Wang M., Brabetz S., et al. The landscape of genomic alterations across childhood cancers. Nature. 2018;555:321–327. doi: 10.1038/nature25480. [DOI] [PubMed] [Google Scholar]
- 343.Huether R., Dong L., Chen X., Wu G., Parker M., Wei L., Ma J., Edmonson M.N., Hedlund E.K., Rusch M.C., et al. The landscape of somatic mutations in epigenetic regulators across 1000 paediatric cancer genomes. Nat. Commun. 2014;5:3630. doi: 10.1038/ncomms4630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Yan H., Parsons D.W., Jin G., McLendon R., Rasheed B.A., Yuan W., Kos I., Batinic-Haberle I., Jones S., Riggins G.J., et al. IDH1 and IDH2 mutations in gliomas. N. Engl. J. Med. 2009;360:765–773. doi: 10.1056/NEJMoa0808710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Muller T., Gessi M., Waha A., Isselstein L.J., Luxen D., Freihoff D., Freihoff J., Becker A., Simon M., Hammes J., et al. Nuclear Exclusion of TET1 Is Associated with Loss of 5-Hydroxymethylcytosine in IDH1 Wild-Type Gliomas. Am. J. Pathol. 2012;181:675–683. doi: 10.1016/j.ajpath.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 346.Williams K., Christensen J., Pedersen M.T., Johansen J.V., Cloos P.A.C., Rappsilber J., Helin K. TET1 and hydroxymethylcytosine in transcription and DNA methylation fidelity. Nature. 2011;473:343–348. doi: 10.1038/nature10066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Ficz G., Branco M.R., Seisenberger S., Santos F., Krueger F., Hore T.A., Marques C.J., Andrews S., Reik W. Dynamic regulation of 5-hydroxymethylcytosine in mouse ES cells and during differentiation. Nature. 2011;473:398–402. doi: 10.1038/nature10008. [DOI] [PubMed] [Google Scholar]
- 348.Kuehner J.N., Chen J., Bruggeman E.C., Wang F., Li Y., Xu C., McEachin Z.T., Li Z., Chen L., Hales C.M., et al. 5-hydroxymethylcytosine is dynamically regulated during forebrain organoid development and aberrantly altered in Alzheimer’s disease. Cell Rep. 2021;35:109042. doi: 10.1016/j.celrep.2021.109042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Zhang Y., Zhang Z., Li L., Xu K., Ma Z., Chow H.M., Herrup K., Li J. Selective loss of 5hmC promotes neurodegeneration in the mouse model of Alzheimer’s disease. FASEB J. 2020;34:16364–16382. doi: 10.1096/fj.202001271R. [DOI] [PubMed] [Google Scholar]
- 350.Hu L.L., Lu J.Y., Cheng J.D., Rao Q.H., Li Z., Hou H.F., Lou Z.Y., Zhang L., Li W., Gong W., et al. Structural insight into substrate preference for TET- mediated oxidation. Nature. 2015;527:118–122. doi: 10.1038/nature15713. [DOI] [PubMed] [Google Scholar]
- 351.Hu L.L., Li Z., Cheng J.D., Rao Q.H., Gong W., Liu M.J., Shi Y.J.G., Zhu J.Y., Wang P., Xu Y.H. Crystal Structure of TET2-DNA Complex: Insight into TET-Mediated 5mC Oxidation. Cell. 2013;155:1545–1555. doi: 10.1016/j.cell.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 352.Si Y., Liu J., Shen H., Zhang C., Wu Y., Huang Y., Gong Z., Xue J., Liu T. Fisetin decreases TET1 activity and CCNY/CDK16 promoter 5hmC levels to inhibit the proliferation and invasion of renal cancer stem cell. J. Cell. Mol. Med. 2019;23:1095–1105. doi: 10.1111/jcmm.14010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Choi S.J., Jung S.W., Huh S., Chung Y.S., Cho H., Kang H. Alteration of DNA Methylation in Gastric Cancer with Chemotherapy. J. Microbiol. Biotechnol. 2017;27:1367–1378. doi: 10.4014/jmb.1704.04035. [DOI] [PubMed] [Google Scholar]
- 354.Chesnelong C., Chaumeil M.M., Blough M.D., Al-Najjar M., Stechishin O.D., Chan J.A., Pieper R.O., Ronen S.M., Weiss S., Luchman H.A., et al. Lactate dehydrogenase A silencing in IDH mutant gliomas. Neuro-Oncol. 2014;16:686–695. doi: 10.1093/neuonc/not243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Wong C.C., Xu J., Bian X., Wu J.L., Kang W., Qian Y., Li W., Chen H., Gou H., Liu D., et al. In Colorectal Cancer Cells with Mutant KRAS, SLC25A22-Mediated Glutaminolysis Reduces DNA Demethylation to Increase WNT Signaling, Stemness, and Drug Resistance. Gastroenterology. 2020;159:2163–2180.e6. doi: 10.1053/j.gastro.2020.08.016. [DOI] [PubMed] [Google Scholar]
- 356.El Helou R., Wicinski J., Guille A., Adelaide J., Finetti P., Bertucci F., Chaffanet M., Birnbaum D., Charafe-Jauffret E., Ginestier C. Brief reports: A distinct DNA methylation signature defines breast cancer stem cells and predicts cancer outcome. Stem Cells. 2014;32:3031–3036. doi: 10.1002/stem.1792. [DOI] [PubMed] [Google Scholar]
- 357.Lu R., Wang P., Parton T., Zhou Y., Chrysovergis K., Rockowitz S., Chen W.Y., Abdel-Wahab O., Wade P.A., Zheng D., et al. Epigenetic Perturbations by Arg882-Mutated DNMT3A Potentiate Aberrant Stem Cell Gene-Expression Program and Acute Leukemia Development. Cancer Cell. 2016;30:92–107. doi: 10.1016/j.ccell.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Zhang J., Wang J., Liu Y.G., Sidik H., Young K.H., Lodish H.F., Fleming M.D. Oncogenic Kras-induced leukemogeneis: Hematopoietic stem cells as the initial target and lineage-specific progenitors as the potential targets for final leukemic transformation. Blood. 2009;113:1304–1314. doi: 10.1182/blood-2008-01-134262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Pathania R., Ramachandran S., Elangovan S., Padia R., Yang P.Y., Cinghu S., Veeranan-Karmegam R., Arjunan P., Gnana-Prakasam J.P., Sadanand F., et al. DNMT1 is essential for mammary and cancer stem cell maintenance and tumorigenesis. Nat. Commun. 2015;6:6910. doi: 10.1038/ncomms7910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Wang Q., Liang N., Yang T., Li Y., Li J., Huang Q., Wu C., Sun L., Zhou X., Cheng X., et al. DNMT1-mediated methylation of BEX1 regulates stemness and tumorigenicity in liver cancer. J. Hepatol. 2021;75:1142–1153. doi: 10.1016/j.jhep.2021.06.025. [DOI] [PubMed] [Google Scholar]
- 361.Bostick M., Kim J.K., Esteve P.O., Clark A., Pradhan S., Jacobsen S.E. UHRF1 plays a role in maintaining DNA methylation in mammalian cells. Science. 2007;317:1760–1764. doi: 10.1126/science.1147939. [DOI] [PubMed] [Google Scholar]
- 362.Stathopoulou A., Chhetri J.B., Ambrose J.C., Esteve P.O., Ji L., Erdjument-Bromage H., Zhang G., Neubert T.A., Pradhan S., Herrero J., et al. A novel requirement for DROSHA in maintenance of mammalian CG methylation. Nucleic Acids Res. 2017;45:9398–9412. doi: 10.1093/nar/gkx695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Liu L., Mao S.Q., Ray C., Zhang Y., Bell F.T., Ng S.F., Xu G.L., Li X. Differential regulation of genomic imprinting by TET proteins in embryonic stem cells. Stem Cell Res. 2015;15:435–443. doi: 10.1016/j.scr.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Wang B.C., Lin G.H., Wang B., Yan M., He B., Zhang W., Yang A.K., Long Z.J., Liu Q. UHRF1 suppression promotes cell differentiation and reduces inflammatory reaction in anaplastic thyroid cancer. Oncotarget. 2018;9:31945–31957. doi: 10.18632/oncotarget.10674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Chen K., Zhang J., Guo Z.Q., Ma Q., Xu Z.Z., Zhou Y.Y., Xu Z.Y., Li Z.W., Liu Y.Q., Ye X.J., et al. Loss of 5-hydroxymethylcytosine is linked to gene body hypermethylation in kidney cancer. Cell Res. 2016;26:103–118. doi: 10.1038/cr.2015.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Zhou Z.H., Li H.Q., Liu F. DNA Methyltransferase Inhibitors and their Therapeutic Potential. Curr. Top. Med. Chem. 2018;18:2448–2457. doi: 10.2174/1568026619666181120150122. [DOI] [PubMed] [Google Scholar]
- 367.Cramer-Morales K.L., Heer C.D., Mapuskar K.A., Domann F.E. Succinate Accumulation Links Mitochondrial MnSOD Depletion to Aberrant Nuclear DNA Methylation and Altered Cell Fate. J. Exp. Pathol. 2020;1:60–70. [PMC free article] [PubMed] [Google Scholar]
- 368.Morris J.P.t., Yashinskie J.J., Koche R., Chandwani R., Tian S., Chen C.C., Baslan T., Marinkovic Z.S., Sanchez-Rivera F.J., Leach S.D., et al. alpha-Ketoglutarate links p53 to cell fate during tumour suppression. Nature. 2019;573:595–599. doi: 10.1038/s41586-019-1577-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Letouze E., Martinelli C., Loriot C., Burnichon N., Abermil N., Ottolenghi C., Janin M., Menara M., Nguyen A.T., Benit P., et al. SDH mutations establish a hypermethylator phenotype in paraganglioma. Cancer Cell. 2013;23:739–752. doi: 10.1016/j.ccr.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 370.Cordes T., Wallace M., Michelucci A., Divakaruni A.S., Sapcariu S.C., Sousa C., Koseki H., Cabrales P., Murphy A.N., Hiller K., et al. Immunoresponsive Gene 1 and Itaconate Inhibit Succinate Dehydrogenase to Modulate Intracellular Succinate Levels. J. Biol. Chem. 2016;291:14274–14284. doi: 10.1074/jbc.M115.685792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Heintzman N.D., Hon G.C., Hawkins R.D., Kheradpour P., Stark A., Harp L.F., Ye Z., Lee L.K., Stuart R.K., Ching C.W., et al. Histone modifications at human enhancers reflect global cell-type-specific gene expression. Nature. 2009;459:108–112. doi: 10.1038/nature07829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Bernstein B.E., Mikkelsen T.S., Xie X., Kamal M., Huebert D.J., Cuff J., Fry B., Meissner A., Wernig M., Plath K., et al. A bivalent chromatin structure marks key developmental genes in embryonic stem cells. Cell. 2006;125:315–326. doi: 10.1016/j.cell.2006.02.041. [DOI] [PubMed] [Google Scholar]
- 373.Huebert D.J., Bernstein B.E. Genomic views of chromatin. Curr. Opin. Genet. Dev. 2005;15:476–481. doi: 10.1016/j.gde.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 374.Moussaieff A., Rouleau M., Kitsberg D., Cohen M., Levy G., Barasch D., Nemirovski A., Shen-Orr S., Laevsky I., Amit M., et al. Glycolysis-mediated changes in acetyl-CoA and histone acetylation control the early differentiation of embryonic stem cells. Cell Metab. 2015;21:392–402. doi: 10.1016/j.cmet.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 375.Cliff T.S., Wu T., Boward B.R., Yin A., Yin H., Glushka J.N., Prestegaard J.H., Dalton S. MYC Controls Human Pluripotent Stem Cell Fate Decisions through Regulation of Metabolic Flux. Cell Stem Cell. 2017;21:502–516. doi: 10.1016/j.stem.2017.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.Gu W., Gaeta X., Sahakyan A., Chan A.B., Hong C.S., Kim R., Braas D., Plath K., Lowry W.E., Christofk H.R. Glycolytic Metabolism Plays a Functional Role in Regulating Human Pluripotent Stem Cell State. Cell Stem Cell. 2016;19:476–490. doi: 10.1016/j.stem.2016.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Lee J.H., Hart S.R.L., Skalnik D.G. Histone deacetylase activity is required for embryonic stem cell differentiation. Genesis. 2004;38:32–38. doi: 10.1002/gene.10250. [DOI] [PubMed] [Google Scholar]
- 378.Keller G. Embryonic stem cell differentiation: Emergence of a new era in biology and medicine. Genes Dev. 2005;19:1129–1155. doi: 10.1101/gad.1303605. [DOI] [PubMed] [Google Scholar]
- 379.Meshorer E., Misteli T. Chromatin in pluripotent embryonic stem cells and differentiation. Nat. Rev. Mol. Cell Biol. 2006;7:540–546. doi: 10.1038/nrm1938. [DOI] [PubMed] [Google Scholar]
- 380.Golob J.L., Paige S.L., Muskheli V., Pabon L., Murry C.E. Chromatin remodeling during mouse and human embryonic stem cell differentiation. Dev. Dyn. 2008;237:1389–1398. doi: 10.1002/dvdy.21545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Inoue A., Jiang L., Lu F., Suzuki T., Zhang Y. Maternal H3K27me3 controls DNA methylation-independent imprinting. Nature. 2017;547:419–424. doi: 10.1038/nature23262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Meng T.G., Zhou Q., Ma X.S., Liu X.Y., Meng Q.R., Huang X.J., Liu H.L., Lei W.L., Zhao Z.H., Ouyang Y.C., et al. PRC2 and EHMT1 regulate H3K27me2 and H3K27me3 establishment across the zygote genome. Nat. Commun. 2020;11:6354. doi: 10.1038/s41467-020-20242-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Daitoku H., Hatta M., Matsuzaki H., Aratani S., Ohshima T., Miyagishi M., Nakajima T., Fukamizu A. Silent information regulator 2 potentiates Foxo1-mediated transcription through its deacetylase activity. Proc. Natl. Acad. Sci. USA. 2004;101:10042–10047. doi: 10.1073/pnas.0400593101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Rokudai S., Laptenko O., Arnal S.M., Taya Y., Kitabayashi I., Prives C. MOZ increases p53 acetylation and premature senescence through its complex formation with PML. Proc. Natl. Acad. Sci. USA. 2013;110:3895–3900. doi: 10.1073/pnas.1300490110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Sykes S.M., Mellert H.S., Holbert M.A., Li K., Marmorstein R., Lane W.S., McMahon S.B. Acetylation of the p53 DNA-binding domain regulates apoptosis induction. Mol. Cell. 2006;24:841–851. doi: 10.1016/j.molcel.2006.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Tou L., Liu Q., Shivdasani R.A. Regulation of mammalian epithelial differentiation and intestine development by class I histone deacetylases. Mol. Cell Biol. 2004;24:3132–3139. doi: 10.1128/MCB.24.8.3132-3139.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Wilson A.J., Byun D.S., Popova N., Murray L.B., L’Italien K., Sowa Y., Arango D., Velcich A., Augenlicht L.H., Mariadason J.M. Histone deacetylase 3 (HDAC3) and other class I HDACs regulate colon cell maturation and p21 expression and are deregulated in human colon cancer. J. Biol. Chem. 2006;281:13548–13558. doi: 10.1074/jbc.M510023200. [DOI] [PubMed] [Google Scholar]
- 388.De Marzo A.M., Marchi V.L., Yang E.S., Veeraswamy R., Lin X., Nelson W.G. Abnormal regulation of DNA methyltransferase expression during colorectal carcinogenesis. Cancer Res. 1999;59:3855–3860. [PubMed] [Google Scholar]
- 389.Kang Y., Kim Y.W., Kang J., Kim A. Histone H3K4me1 and H3K27ac play roles in nucleosome eviction and eRNA transcription, respectively, at enhancers. FASEB J. 2021;35:e21781. doi: 10.1096/fj.202100488R. [DOI] [PubMed] [Google Scholar]
- 390.Azuara V., Perry P., Sauer S., Spivakov M., Jorgensen H.F., John R.M., Gouti M., Casanova M., Warnes G., Merkenschlager M., et al. Chromatin signatures of pluripotent cell lines. Nat. Cell Biol. 2006;8:532–538. doi: 10.1038/ncb1403. [DOI] [PubMed] [Google Scholar]
- 391.Sheikh B.N., Akhtar A. The many lives of KATs—Detectors, integrators and modulators of the cellular environment. Nat. Rev. Genet. 2019;20:7–23. doi: 10.1038/s41576-018-0072-4. [DOI] [PubMed] [Google Scholar]
- 392.Margueron R., Reinberg D. The Polycomb complex PRC2 and its mark in life. Nature. 2011;469:343–349. doi: 10.1038/nature09784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Fan H., Lu J., Guo Y., Li D., Zhang Z.M., Tsai Y.H., Pi W.C., Ahn J.H., Gong W., Xiang Y., et al. BAHCC1 binds H3K27me3 via a conserved BAH module to mediate gene silencing and oncogenesis. Nat. Genet. 2020;52:1384–1396. doi: 10.1038/s41588-020-00729-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Wen H., Li Y., Xi Y., Jiang S., Stratton S., Peng D., Tanaka K., Ren Y., Xia Z., Wu J., et al. ZMYND11 links histone H3.3K36me3 to transcription elongation and tumour suppression. Nature. 2014;508:263–268. doi: 10.1038/nature13045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Rabaneda-Bueno R., Mena-Montes B., Torres-Castro S., Torres-Carrillo N., Torres-Carrillo N.M. Advances in Genetics and Epigenetic Alterations in Alzheimer’s Disease: A Notion for Therapeutic Treatment. Genes. 2021;12:1959. doi: 10.3390/genes12121959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Graff J., Rei D., Guan J.S., Wang W.Y., Seo J., Hennig K.M., Nieland T.J., Fass D.M., Kao P.F., Kahn M., et al. An epigenetic blockade of cognitive functions in the neurodegenerating brain. Nature. 2012;483:222–226. doi: 10.1038/nature10849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Zhang K., Schrag M., Crofton A., Trivedi R., Vinters H., Kirsch W. Targeted proteomics for quantification of histone acetylation in Alzheimer’s disease. Proteomics. 2012;12:1261–1268. doi: 10.1002/pmic.201200010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Vlaming H., McLean C.M., Korthout T., Alemdehy M.F., Hendriks S., Lancini C., Palit S., Klarenbeek S., Kwesi-Maliepaard E.M., Molenaar T.M., et al. Conserved crosstalk between histone deacetylation and H3K79 methylation generates DOT1L-dose dependency in HDAC1-deficient thymic lymphoma. EMBO J. 2019;38:e101564. doi: 10.15252/embj.2019101564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Mani S.A., Guo W., Liao M.J., Eaton E.N., Ayyanan A., Zhou A.Y., Brooks M., Reinhard F., Zhang C.C., Shipitsin M., et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133:704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Ye X., Tam W.L., Shibue T., Kaygusuz Y., Reinhardt F., Ng Eaton E., Weinberg R.A. Distinct EMT programs control normal mammary stem cells and tumour-initiating cells. Nature. 2015;525:256–260. doi: 10.1038/nature14897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Chaffer C.L., Marjanovic N.D., Lee T., Bell G., Kleer C.G., Reinhardt F., D’Alessio A.C., Young R.A., Weinberg R.A. Poised Chromatin at the ZEB1 Promoter Enables Breast Cancer Cell Plasticity and Enhances Tumorigenicity. Cell. 2013;154:61–74. doi: 10.1016/j.cell.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Van den Beucken T., Koch E., Chu K., Rupaimoole R., Prickaerts P., Adriaens M., Voncken J.W., Harris A.L., Buffa F.M., Haider S., et al. Hypoxia promotes stem cell phenotypes and poor prognosis through epigenetic regulation of DICER. Nat. Commun. 2014;5:5203. doi: 10.1038/ncomms6203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Jaiswal A., Xudong Z., Zhenyu J., Saretzki G. Mitochondrial sirtuins in stem cells and cancer. FEBS J. 2022;289:3393–3415. doi: 10.1111/febs.15879. [DOI] [PubMed] [Google Scholar]
- 404.Szade K., Gulati G.S., Chan C.K.F., Kao K.S., Miyanishi M., Marjon K.D., Sinha R., George B.M., Chen J.Y., Weissman I.L. Where Hematopoietic Stem Cells Live: The Bone Marrow Niche. Antioxid. Redox Signal. 2018;29:191–204. doi: 10.1089/ars.2017.7419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Qiu X., Brown K., Hirschey M.D., Verdin E., Chen D. Calorie restriction reduces oxidative stress by SIRT3-mediated SOD2 activation. Cell Metab. 2010;12:662–667. doi: 10.1016/j.cmet.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 406.Tseng A.H., Shieh S.S., Wang D.L. SIRT3 deacetylates FOXO3 to protect mitochondria against oxidative damage. Free Radic. Biol. Med. 2013;63:222–234. doi: 10.1016/j.freeradbiomed.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 407.Brown K., Xie S., Qiu X., Mohrin M., Shin J., Liu Y., Zhang D., Scadden D.T., Chen D. SIRT3 reverses aging-associated degeneration. Cell Rep. 2013;3:319–327. doi: 10.1016/j.celrep.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Liu C.Y., Huang Z.H., Jiang H., Shi F.J. The Sirtuin 3 Expression Profile Is Associated with Pathological and Clinical Outcomes in Colon Cancer Patients. Biomed Res. Int. 2014;2014:871263. doi: 10.1155/2014/871263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Dong X.C., Jing L.M., Wang W.X., Gao Y.X. Down-regulation of SIRT3 promotes ovarian carcinoma metastasis. Biochem. Biophys. Res. Commun. 2016;475:245–250. doi: 10.1016/j.bbrc.2016.05.098. [DOI] [PubMed] [Google Scholar]
- 410.Min Z.Y., Gao J.M., Yu Y. The Roles of Mitochondrial SIRT4 in Cellular Metabolism. Front. Endocrinol. 2019;9:783. doi: 10.3389/fendo.2018.00783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Du L., Liu X., Ren Y., Li J., Li P., Jiao Q., Meng P., Wang F., Wang Y., Wang Y.S., et al. Loss of SIRT4 promotes the self-renewal of Breast Cancer Stem Cells. Theranostics. 2020;10:9458–9476. doi: 10.7150/thno.44688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Guan J., Jiang X., Gai J., Sun X., Zhao J., Li J., Li Y., Cheng M., Du T., Fu L., et al. Sirtuin 5 regulates the proliferation, invasion and migration of prostate cancer cells through acetyl-CoA acetyltransferase 1. J. Cell. Mol. Med. 2020;24:14039–14049. doi: 10.1111/jcmm.16016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.Ma Y.Z., Qi Y.J., Wang L., Zheng Z.X., Zhang Y., Zheng J.F. SIRT5-mediated SDHA desuccinylation promotes clear cell renal cell carcinoma tumorigenesis. Free Radic. Biol. Med. 2019;134:468–477. doi: 10.1016/j.freeradbiomed.2019.01.030. [DOI] [PubMed] [Google Scholar]
- 414.Shi L., Yan H., An S., Shen M., Jia W., Zhang R., Zhao L., Huang G., Liu J. SIRT5-mediated deacetylation of LDHB promotes autophagy and tumorigenesis in colorectal cancer. Mol. Oncol. 2019;13:358–375. doi: 10.1002/1878-0261.12408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415.Yang X., Wang Z., Li X., Liu B., Liu M., Liu L., Chen S., Ren M., Wang Y., Yu M., et al. SHMT2 Desuccinylation by SIRT5 Drives Cancer Cell Proliferation. Cancer Res. 2018;78:372–386. doi: 10.1158/0008-5472.CAN-17-1912. [DOI] [PubMed] [Google Scholar]
- 416.Ippolito L., Marini A., Cavallini L., Morandi A., Pietrovito L., Pintus G., Giannoni E., Schrader T., Puhr M., Chiarugi P., et al. Metabolic shift toward oxidative phosphorylation in docetaxel resistant prostate cancer cells. Oncotarget. 2016;7:61890–61904. doi: 10.18632/oncotarget.11301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417.Schopf B., Weissensteiner H., Schafer G., Fazzini F., Charoentong P., Naschberger A., Rupp B., Fendt L., Bukur V., Giese I., et al. OXPHOS remodeling in high-grade prostate cancer involves mtDNA mutations and increased succinate oxidation. Nat. Commun. 2020;11:1487. doi: 10.1038/s41467-020-15237-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418.Ahn B.H., Kim H.S., Song S., Lee I.H., Liu J., Vassilopoulos A., Deng C.X., Finkel T. A role for the mitochondrial deacetylase Sirt3 in regulating energy homeostasis. Proc. Natl. Acad. Sci. USA. 2008;105:14447–14452. doi: 10.1073/pnas.0803790105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419.Zhang M., Wu J., Sun R., Tao X., Wang X., Kang Q., Wang H., Zhang L., Liu P., Zhang J., et al. SIRT5 deficiency suppresses mitochondrial ATP production and promotes AMPK activation in response to energy stress. PLoS ONE. 2019;14:e0211796. doi: 10.1371/journal.pone.0211796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Min L.H., Ji Y., Bakiri L., Qiu Z.X., Cen J., Chen X.T., Chen L.L., Scheuch H., Zheng H., Qin L.X., et al. Liver cancer initiation is controlled by AP-1 through SIRT6-dependent inhibition of survivin. Nat. Cell Biol. 2012;14:1203–1211. doi: 10.1038/ncb2590. [DOI] [PubMed] [Google Scholar]
- 421.Sebastian C., Zwaans B.M.M., Silberman D.M., Gymrek M., Goren A., Zhong L., Ram O., Truelove J., Guimaraes A.R., Toiber D., et al. The Histone Deacetylase SIRT6 Is a Tumor Suppressor that Controls Cancer Metabolism. Cell. 2012;151:1185–1199. doi: 10.1016/j.cell.2012.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Kugel S., Sebastian C., Fitamant J., Ross K.N., Saha S.K., Jain E., Gladden A., Arora K.S., Kato Y., Rivera M.N., et al. SIRT6 Suppresses Pancreatic Cancer through Control of Lin28b. Cell. 2016;165:1401–1415. doi: 10.1016/j.cell.2016.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Van Meter M., Mao Z., Gorbunova V., Seluanov A. SIRT6 overexpression induces massive apoptosis in cancer cells but not in normal cells. Cell Cycle. 2011;10:3153–3158. doi: 10.4161/cc.10.18.17435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Liu W., Wu M., Du H., Shi X., Zhang T., Li J. SIRT6 inhibits colorectal cancer stem cell proliferation by targeting CDC25A. Oncol. Lett. 2018;15:5368–5374. doi: 10.3892/ol.2018.7989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425.Liu P.S., Wang H.P., Li X.Y., Chao T., Christen T.T.S., Christen S., Di Conza G., Cheng W.C., Chou C.H., Vavakova M., et al. alpha-ketoglutarate orchestrates macrophage activation through metabolic and epigenetic reprogramming. Nat. Immunol. 2017;18:985–994. doi: 10.1038/ni.3796. [DOI] [PubMed] [Google Scholar]
- 426.Ishii M., Wen H., Corsa C.A., Liu T., Coelho A.L., Allen R.M., Carson W.F.t., Cavassani K.A., Li X., Lukacs N.W., et al. Epigenetic regulation of the alternatively activated macrophage phenotype. Blood. 2009;114:3244–3254. doi: 10.1182/blood-2009-04-217620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427.Wierda R.J., Goedhart M., van Eggermond M.C., Muggen A.F., Miggelbrink X.M., Geutskens S.B., van Zwet E., Haasnoot G.W., van den Elsen P.J. A role for KMT1c in monocyte to dendritic cell differentiation: Epigenetic regulation of monocyte differentiation. Hum. Immunol. 2015;76:431–437. doi: 10.1016/j.humimm.2015.03.017. [DOI] [PubMed] [Google Scholar]
- 428.Kurotaki D., Tamura T. Transcriptional and Epigenetic Regulation of Innate Immune Cell Development by the Transcription Factor, Interferon Regulatory Factor-8. J. Interferon Cytokine Res. 2016;36:433–441. doi: 10.1089/jir.2015.0138. [DOI] [PubMed] [Google Scholar]
- 429.Chakrabarty R.P., Chandel N.S. Mitochondria as Signaling Organelles Control Mammalian Stem Cell Fate. Cell Stem Cell. 2021;28:394–408. doi: 10.1016/j.stem.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Das S., Morvan F., Morozzi G., Jourde B., Minetti G.C., Kahle P., Rivet H., Brebbia P., Toussaint G., Glass D.J., et al. ATP Citrate Lyase Regulates Myofiber Differentiation and Increases Regeneration by Altering Histone Acetylation. Cell Rep. 2017;21:3003–3011. doi: 10.1016/j.celrep.2017.11.038. [DOI] [PubMed] [Google Scholar]
- 431.Mani S., Swargiary G., Tyagi S., Singh M., Jha N.K., Singh K.K. Nanotherapeutic approaches to target mitochondria in cancer. Life Sci. 2021;281:119773. doi: 10.1016/j.lfs.2021.119773. [DOI] [PubMed] [Google Scholar]
- 432.Yang L.D., Youngblood H., Wu C.Y., Zhang Q.G. Mitochondria as a target for neuroprotection: Role of methylene blue and photobiomodulation. Transl. Neurodegener. 2020;9:19. doi: 10.1186/s40035-020-00197-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Huang M.F., Myers C.R., Wang Y.A., You M. Mitochondria as a Novel Target for Cancer Chemoprevention: Emergence of Mitochondrial-targeting Agents. Cancer Prev. Res. 2021;14:285–306. doi: 10.1158/1940-6207.CAPR-20-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Ashton T.M., McKenna W.G., Kunz-Schughart L.A., Higgins G.S. Oxidative Phosphorylation as an Emerging Target in Cancer Therapy. Clin. Cancer Res. 2018;24:2482–2490. doi: 10.1158/1078-0432.CCR-17-3070. [DOI] [PubMed] [Google Scholar]
- 435.Willmes C. Mitochondria—A Powerful Therapeutic Target. Trends Mol. Med. 2020;26:1–2. doi: 10.1016/j.molmed.2019.10.006. [DOI] [PubMed] [Google Scholar]
- 436.Dong L.F., Neuzil J. Mitochondria in cancer: Why mitochondria are a good target for cancer therapy. Prog. Mol. Biol. Transl. Sci. 2014;127:211–227. doi: 10.1016/B978-0-12-394625-6.00008-8. [DOI] [PubMed] [Google Scholar]
- 437.Zinovkin R.A., Zamyatnin A.A. Mitochondria-Targeted Drugs. Curr. Mol. Pharm. 2019;12:202–214. doi: 10.2174/1874467212666181127151059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Heller A., Brockhoff G., Goepferich A. Targeting drugs to mitochondria. Eur. J. Pharm. Biopharm. 2012;82:1–18. doi: 10.1016/j.ejpb.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 439.Ferrin G., Linares C.I., Muntane J. Mitochondrial drug targets in cell death and cancer. Curr. Pharm. Des. 2011;17:2002–2016. doi: 10.2174/138161211796904803. [DOI] [PubMed] [Google Scholar]
- 440.Huang S., Liu Y., Zhang Y., Zhang R., Zhu C., Fan L., Pei G., Zhang B., Shi Y. Baicalein inhibits SARS-CoV-2/VSV replication with interfering mitochondrial oxidative phosphorylation in a mPTP dependent manner. Signal. Transduct. Target. Ther. 2020;5:266. doi: 10.1038/s41392-020-00353-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441.Martinez-Reyes I., Chandel N.S. Acetyl-CoA-directed gene transcription in cancer cells. Genes Dev. 2018;32:463–465. doi: 10.1101/gad.315168.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 442.Lee J.V., Berry C.T., Kim K., Sen P., Kim T., Carrer A., Trefely S., Zhao S., Fernandez S., Barney L.E., et al. Acetyl-CoA promotes glioblastoma cell adhesion and migration through Ca2+-NFAT signaling. Genes Dev. 2018;32:497–511. doi: 10.1101/gad.311027.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.Lei I., Tian S., Gao W., Liu L., Guo Y., Tang P., Chen E., Wang Z. Acetyl-CoA production by specific metabolites promotes cardiac repair after myocardial infarction via histone acetylation. Elife. 2021;10:e60311. doi: 10.7554/eLife.60311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 444.Carrer A., Trefely S., Zhao S., Campbell S.L., Norgard R.J., Schultz K.C., Sidoli S., Parris J.L.D., Affronti H.C., Sivanand S., et al. Acetyl-CoA Metabolism Supports Multistep Pancreatic Tumorigenesis. Cancer Discov. 2019;9:416–435. doi: 10.1158/2159-8290.CD-18-0567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Wang C., Rajput S., Watabe K., Liao D.F., Cao D. Acetyl-CoA carboxylase-a as a novel target for cancer therapy. Front. Biosci. 2010;2:515–526. doi: 10.2741/s82. [DOI] [PubMed] [Google Scholar]
- 446.Chen L., Liu T., Zhou J., Wang Y., Wang X., Di W., Zhang S. Citrate synthase expression affects tumor phenotype and drug resistance in human ovarian carcinoma. PLoS ONE. 2014;9:e115708. doi: 10.1371/journal.pone.0115708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.Schlichtholz B., Turyn J., Goyke E., Biernacki M., Jaskiewicz K., Sledzinski Z., Swierczynski J. Enhanced citrate synthase activity in human pancreatic cancer. Pancreas. 2005;30:99–104. doi: 10.1097/01.mpa.0000153326.69816.7d. [DOI] [PubMed] [Google Scholar]
- 448.Zaidi N., Swinnen J.V., Smans K. ATP-citrate lyase: A key player in cancer metabolism. Cancer Res. 2012;72:3709–3714. doi: 10.1158/0008-5472.CAN-11-4112. [DOI] [PubMed] [Google Scholar]
- 449.Migita T., Narita T., Nomura K., Miyagi E., Inazuka F., Matsuura M., Ushijima M., Mashima T., Seimiya H., Satoh Y., et al. ATP citrate lyase: Activation and therapeutic implications in non-small cell lung cancer. Cancer Res. 2008;68:8547–8554. doi: 10.1158/0008-5472.CAN-08-1235. [DOI] [PubMed] [Google Scholar]
- 450.Huang L., Wang C.D., Xu H.X., Peng G.Y. Targeting citrate as a novel therapeutic strategy in cancer treatment. BBA-Rev. Cancer. 2020;1873:188332. doi: 10.1016/j.bbcan.2019.188332. [DOI] [PubMed] [Google Scholar]
- 451.Popovici-Muller J., Lemieux R.M., Artin E., Saunders J.O., Salituro F.G., Travins J., Cianchetta G., Cai Z., Zhou D., Cui D., et al. Discovery of AG-120 (Ivosidenib): A First-in-Class Mutant IDH1 Inhibitor for the Treatment of IDH1 Mutant Cancers. ACS Med. Chem. Lett. 2018;9:300–305. doi: 10.1021/acsmedchemlett.7b00421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Han S., Liu Y., Cai S.J., Qian M., Ding J., Larion M., Gilbert M.R., Yang C. IDH mutation in glioma: Molecular mechanisms and potential therapeutic targets. Br. J. Cancer. 2020;122:1580–1589. doi: 10.1038/s41416-020-0814-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453.McMurry H., Fletcher L., Traer E. IDH Inhibitors in AML-Promise and Pitfalls. Curr. Hematol. Malig. Rep. 2021;16:207–217. doi: 10.1007/s11899-021-00619-3. [DOI] [PubMed] [Google Scholar]
- 454.Paschka P., Schlenk R.F., Gaidzik V.I., Habdank M., Kronke J., Bullinger L., Spath D., Kayser S., Zucknick M., Gotze K., et al. IDH1 and IDH2 mutations are frequent genetic alterations in acute myeloid leukemia and confer adverse prognosis in cytogenetically normal acute myeloid leukemia with NPM1 mutation without FLT3 internal tandem duplication. J. Clin. Oncol. 2010;28:3636–3643. doi: 10.1200/JCO.2010.28.3762. [DOI] [PubMed] [Google Scholar]
- 455.Waitkus M.S., Diplas B.H., Yan H. Biological Role and Therapeutic Potential of IDH Mutations in Cancer. Cancer Cell. 2018;34:186–195. doi: 10.1016/j.ccell.2018.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Borger D.R., Tanabe K.K., Fan K.C., Lopez H.U., Fantin V.R., Straley K.S., Schenkein D.P., Hezel A.F., Ancukiewicz M., Liebman H.M., et al. Frequent mutation of isocitrate dehydrogenase (IDH)1 and IDH2 in cholangiocarcinoma identified through broad-based tumor genotyping. Oncologist. 2012;17:72–79. doi: 10.1634/theoncologist.2011-0386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Murphy M.P., O’Neill L.A.J. Krebs Cycle Reimagined: The Emerging Roles of Succinate and Itaconate as Signal Transducers. Cell. 2018;174:780–784. doi: 10.1016/j.cell.2018.07.030. [DOI] [PubMed] [Google Scholar]
- 458.Kula-Alwar D., Prag H.A., Krieg T. Targeting Succinate Metabolism in Ischemia/Reperfusion Injury. Circulation. 2019;140:1968–1970. doi: 10.1161/CIRCULATIONAHA.119.042791. [DOI] [PubMed] [Google Scholar]
- 459.Cui H.T., Chen Y.H., Li K., Zhan R., Zhao M.M., Xu Y.K., Lin Z.Y., Fu Y., He Q.H., Tang P.C., et al. Untargeted metabolomics identifies succinate as a biomarker and therapeutic target in aortic aneurysm and dissection. Eur. Heart J. 2021;42:4373–4385. doi: 10.1093/eurheartj/ehab605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.Kornberg M.D., Bhargava P., Kim P.M., Putluri V., Snowman A.M., Putluri N., Calabresi P.A., Snyder S.H. Dimethyl fumarate targets GAPDH and aerobic glycolysis to modulate immunity. Science. 2018;360:449–453. doi: 10.1126/science.aan4665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461.Angiari S., O’Neill L.A. Dimethyl fumarate: Targeting glycolysis to treat MS. Cell Res. 2018;28:613–615. doi: 10.1038/s41422-018-0045-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 462.Waack I.N., Himmen S., Mueller F., Rohrig R., Roehrborn F., Teloh J.K., de Groot H. L-Malate’s Plasma and Excretion Profile in the Treatment of Moderate and Severe Hemorrhagic Shock in Rats. Biomed Res. Int. 2016;2016:5237148. doi: 10.1155/2016/5237148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463.Pons F., Bellmunt J. Sunitinib malate in the treatment of urothelial cancer. Expert Opin. Investig. Drugs. 2014;23:115–124. doi: 10.1517/13543784.2014.853740. [DOI] [PubMed] [Google Scholar]
- 464.Selinski J., Scheibe R. Malate valves: Old shuttles with new perspectives. Plant Biol. 2019;21((Suppl. S1)):21–30. doi: 10.1111/plb.12869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465.Kayamba F., Faya M., Pooe O.J., Kushwaha B., Kushwaha N.D., Obakachi V.A., Nyamori V.O., Karpoormath R. Lactate dehydrogenase and malate dehydrogenase: Potential antiparasitic targets for drug development studies. Bioorg. Med. Chem. 2021;50:116458. doi: 10.1016/j.bmc.2021.116458. [DOI] [PubMed] [Google Scholar]
- 466.Ma Y.C., Tian P.F., Chen Z.P., Yue D.S., Liu C.C., Li C.G., Chen C., Zhang H., Liu H.L., Zhang Z.F., et al. Urinary malate dehydrogenase 2 is a new biomarker for early detection of non-small-cell lung cancer. Cancer Sci. 2021;112:2349–2360. doi: 10.1111/cas.14845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467.Wiese E.K., Hitosugi S., Loa S.T., Sreedhar A., Andres-Beck L.G., Kurmi K., Pang Y.P., Karnitz L.M., Gonsalves W.I., Hitosugi T. Enzymatic activation of pyruvate kinase increases cytosolic oxaloacetate to inhibit the Warburg effect. Nat. Metab. 2021;3:954–968. doi: 10.1038/s42255-021-00424-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 468.Tungtur S.K., Wilkins H.M., Rogers R.S., Badawi Y., Sage J.M., Agbas A., Jawdat O., Barohn R.J., Swerdlow R.H., Nishimune H. Oxaloacetate treatment preserves motor function in SOD1(G93A) mice and normalizes select neuroinflammation-related parameters in the spinal cord. Sci. Rep. 2021;11:11051. doi: 10.1038/s41598-021-90438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.Gou L., Lee J., Hao H., Park Y.D., Zhan Y., Lu Z.R. The effect of oxaloacetic acid on tyrosinase activity and structure: Integration of inhibition kinetics with docking simulation. Int. J. Biol. Macromol. 2017;101:59–66. doi: 10.1016/j.ijbiomac.2017.03.073. [DOI] [PubMed] [Google Scholar]
- 470.Regenbrecht C.R., Lehrach H., Adjaye J. Stemming cancer: Functional genomics of cancer stem cells in solid tumors. Stem Cell Rev. 2008;4:319–328. doi: 10.1007/s12015-008-9034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471.Ganesh S., Venkatakrishnan K., Tan B. Quantum scale organic semiconductors for SERS detection of DNA methylation and gene expression. Nat. Commun. 2020;11:1135. doi: 10.1038/s41467-020-14774-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472.Morera L., Lubbert M., Jung M. Targeting histone methyltransferases and demethylases in clinical trials for cancer therapy. Clin. Epigenet. 2016;8:57. doi: 10.1186/s13148-016-0223-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 473.Plass C., Pfister S.M., Lindroth A.M., Bogatyrova O., Claus R., Lichter P. Mutations in regulators of the epigenome and their connections to global chromatin patterns in cancer. Nat. Rev. Genet. 2013;14:765–780. doi: 10.1038/nrg3554. [DOI] [PubMed] [Google Scholar]
- 474.Heerboth S., Lapinska K., Snyder N., Leary M., Rollinson S., Sarkar S. Use of epigenetic drugs in disease: An overview. Genet. Epigenet. 2014;6:9–19. doi: 10.4137/GEG.S12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 475.Khan H., Vale C., Bhagat T., Verma A. Role of DNA methylation in the pathogenesis and treatment of myelodysplastic syndromes. Semin. Hematol. 2013;50:16–37. doi: 10.1053/j.seminhematol.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 476.Jabbour E., Issa J.P., Garcia-Manero G., Kantarjian H. Evolution of decitabine development: Accomplishments, ongoing investigations, and future strategies. Cancer. 2008;112:2341–2351. doi: 10.1002/cncr.23463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.Cheng J.C., Matsen C.B., Gonzales F.A., Ye W., Greer S., Marquez V.E., Jones P.A., Selker E.U. Inhibition of DNA methylation and reactivation of silenced genes by zebularine. J. Natl. Cancer Inst. 2003;95:399–409. doi: 10.1093/jnci/95.5.399. [DOI] [PubMed] [Google Scholar]
- 478.Graca I., Sousa E.J., Baptista T., Almeida M., Ramalho-Carvalho J., Palmeira C., Henrique R., Jeronimo C. Anti-tumoral effect of the non-nucleoside DNMT inhibitor RG108 in human prostate cancer cells. Curr. Pharm. Des. 2014;20:1803–1811. doi: 10.2174/13816128113199990516. [DOI] [PubMed] [Google Scholar]
- 479.Borges S., Doppler H.R., Storz P. A combination treatment with DNA methyltransferase inhibitors and suramin decreases invasiveness of breast cancer cells. Breast Cancer Res. Treat. 2014;144:79–91. doi: 10.1007/s10549-014-2857-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 480.Suzuki T., Tanaka R., Hamada S., Nakagawa H., Miyata N. Design, synthesis, inhibitory activity, and binding mode study of novel DNA methyltransferase 1 inhibitors. Bioorg. Med. Chem. Lett. 2010;20:1124–1127. doi: 10.1016/j.bmcl.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 481.Stresemann C., Brueckner B., Musch T., Stopper H., Lyko F. Functional diversity of DNA methyltransferase inhibitors in human cancer cell lines. Cancer Res. 2006;66:2794–2800. doi: 10.1158/0008-5472.CAN-05-2821. [DOI] [PubMed] [Google Scholar]
- 482.Song Y., Zhang C. Hydralazine inhibits human cervical cancer cell growth in vitro in association with APC demethylation and re-expression. Cancer Chemother. Pharm. 2009;63:605–613. doi: 10.1007/s00280-008-0773-z. [DOI] [PubMed] [Google Scholar]
- 483.Singh N., Duenas-Gonzalez A., Lyko F., Medina-Franco J.L. Molecular modeling and molecular dynamics studies of hydralazine with human DNA methyltransferase 1. ChemMedChem. 2009;4:792–799. doi: 10.1002/cmdc.200900017. [DOI] [PubMed] [Google Scholar]
- 484.Datta J., Ghoshal K., Denny W.A., Gamage S.A., Brooke D.G., Phiasivongsa P., Redkar S., Jacob S.T. A new class of quinoline-based DNA hypomethylating agents reactivates tumor suppressor genes by blocking DNA methyltransferase 1 activity and inducing its degradation. Cancer Res. 2009;69:4277–4285. doi: 10.1158/0008-5472.CAN-08-3669. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 485.Garcia-Dominguez P., Dell’aversana C., Alvarez R., Altucci L., de Lera A.R. Synthetic approaches to DNMT inhibitor SGI-1027 and effects on the U937 leukemia cell line. Bioorg. Med. Chem. Lett. 2013;23:1631–1635. doi: 10.1016/j.bmcl.2013.01.085. [DOI] [PubMed] [Google Scholar]
- 486.Manara M.C., Valente S., Cristalli C., Nicoletti G., Landuzzi L., Zwergel C., Mazzone R., Stazi G., Arimondo P.B., Pasello M., et al. A Quinoline-Based DNA Methyltransferase Inhibitor as a Possible Adjuvant in Osteosarcoma Therapy. Mol. Cancer Ther. 2018;17:1881–1892. doi: 10.1158/1535-7163.MCT-17-0818. [DOI] [PubMed] [Google Scholar]
- 487.She S., Zhao Y., Kang B., Chen C., Chen X., Zhang X., Chen W., Dan S., Wang H., Wang Y.J., et al. Combined inhibition of JAK1/2 and DNMT1 by newly identified small-molecule compounds synergistically suppresses the survival and proliferation of cervical cancer cells. Cell Death Dis. 2020;11:724. doi: 10.1038/s41419-020-02934-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 488.Pappalardi M.B., Keenan K., Cockerill M., Kellner W.A., Stowell A., Sherk C., Wong K., Pathuri S., Briand J., Steidel M., et al. Discovery of a first-in-class reversible DNMT1-selective inhibitor with improved tolerability and efficacy in acute myeloid leukemia. Nat. Cancer. 2021;2:1002–1017. doi: 10.1038/s43018-021-00249-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 489.Colyn L., Barcena-Varela M., Alvarez-Sola G., Latasa M.U., Uriarte I., Santamaria E., Herranz J.M., Santos-Laso A., Arechederra M., Ruiz de Gauna M., et al. Dual Targeting of G9a and DNA Methyltransferase-1 for the Treatment of Experimental Cholangiocarcinoma. Hepatology. 2021;73:2380–2396. doi: 10.1002/hep.31642. [DOI] [PubMed] [Google Scholar]
- 490.Du S., Xu G., Zou W., Xiang T., Luo Z. Effect of dihydroartemisinin on UHRF1 gene expression in human prostate cancer PC-3 cells. Anticancer Drugs. 2017;28:384–391. doi: 10.1097/CAD.0000000000000469. [DOI] [PubMed] [Google Scholar]
- 491.Unoki M., Brunet J., Mousli M. Drug discovery targeting epigenetic codes: The great potential of UHRF1, which links DNA methylation and histone modifications, as a drug target in cancers and toxoplasmosis. Biochem. Pharm. 2009;78:1279–1288. doi: 10.1016/j.bcp.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 492.Li X.L., Xu J.H., Nie J.H., Fan S.J. Exogenous expression of UHRF1 promotes proliferation and metastasis of breast cancer cells. Oncol. Rep. 2012;28:375–383. doi: 10.3892/or.2012.1792. [DOI] [PubMed] [Google Scholar]
- 493.Ferry L., Fournier A., Tsusaka T., Adelmant G., Shimazu T., Matano S., Kirsh O., Amouroux R., Dohmae N., Suzuki T., et al. Methylation of DNA Ligase 1 by G9a/GLP Recruits UHRF1 to Replicating DNA and Regulates DNA Methylation. Mol. Cell. 2017;67:550–565.e5. doi: 10.1016/j.molcel.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 494.Jung H.J., Byun H.O., Jee B.A., Min S., Jeoun U.W., Lee Y.K., Seo Y., Woo H.G., Yoon G. The Ubiquitin-like with PHD and Ring Finger Domains 1 (UHRF1)/DNA Methyltransferase 1 (DNMT1) Axis Is a Primary Regulator of Cell Senescence. J. Biol. Chem. 2017;292:3729–3739. doi: 10.1074/jbc.M116.750539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 495.Amato R.J., Stephenson J., Hotte S., Nemunaitis J., Belanger K., Reid G., Martell R.E. MG98, a second-generation DNMT1 inhibitor, in the treatment of advanced renal cell carcinoma. Cancer Investig. 2012;30:415–421. doi: 10.3109/07357907.2012.675381. [DOI] [PubMed] [Google Scholar]
- 496.Nandakumar V., Vaid M., Katiyar S.K. (-)-Epigallocatechin-3-gallate reactivates silenced tumor suppressor genes, Cip1/p21 and p16INK4a, by reducing DNA methylation and increasing histones acetylation in human skin cancer cells. Carcinogenesis. 2011;32:537–544. doi: 10.1093/carcin/bgq285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 497.Li Y.C., Wang Y., Li D.D., Zhang Y., Zhao T.C., Li C.F. Procaine is a specific DNA methylation inhibitor with anti-tumor effect for human gastric cancer. J. Cell. Biochem. 2018;119:2440–2449. doi: 10.1002/jcb.26407. [DOI] [PubMed] [Google Scholar]
- 498.Medina-Franco J.L., Caulfield T. Advances in the computational development of DNA methyltransferase inhibitors. Drug Discov. Today. 2011;16:418–425. doi: 10.1016/j.drudis.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 499.Pereira M.A., Tao L., Liu Y., Li L., Steele V.E., Lubet R.A. Modulation by budesonide of DNA methylation and mRNA expression in mouse lung tumors. Int. J. Cancer. 2007;120:1150–1153. doi: 10.1002/ijc.22468. [DOI] [PubMed] [Google Scholar]
- 500.Alyaqoub F.S., Tao L., Kramer P.M., Steele V.E., Lubet R.A., Gunning W.T., Pereira M.A. Prevention of mouse lung tumors and modulation of DNA methylation by combined treatment with budesonide and R115777 (ZarnestraMT) Carcinogenesis. 2006;27:2442–2447. doi: 10.1093/carcin/bgl088. [DOI] [PubMed] [Google Scholar]
- 501.Neja S.A. Site-Specific DNA Demethylation as a Potential Target for Cancer Epigenetic Therapy. Epigenet. Insights. 2020;13 doi: 10.1177/2516865720964808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 502.Cong B., Zhang Q., Cao X. The function and regulation of TET2 in innate immunity and inflammation. Protein Cell. 2021;12:165–173. doi: 10.1007/s13238-020-00796-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 503.Tang Y., Luo M., Pan K., Ahmad T., Zhou T., Miao Z., Zhou H., Sun H., Xu X., Namaka M., et al. DNA hydroxymethylation changes in response to spinal cord damage in a multiple sclerosis mouse model. Epigenomics. 2019;11:323–335. doi: 10.2217/epi-2018-0162. [DOI] [PubMed] [Google Scholar]
- 504.Nair N., Plant D., Verstappen S.M., Isaacs J.D., Morgan A.W., Hyrich K.L., Barton A., Wilson A.G. MATURA investigators Differential DNA methylation correlates with response to methotrexate in rheumatoid arthritis. Rheumatology. 2020;59:1364–1371. doi: 10.1093/rheumatology/kez411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 505.Rohle D., Popovici-Muller J., Palaskas N., Turcan S., Grommes C., Campos C., Tsoi J., Clark O., Oldrini B., Komisopoulou E., et al. An inhibitor of mutant IDH1 delays growth and promotes differentiation of glioma cells. Science. 2013;340:626–630. doi: 10.1126/science.1236062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 506.Chaturvedi A., Cruz M.M.A., Jyotsana N., Sharma A., Yun H.Y., Gorlich K., Wichmann M., Schwarzer A., Preller M., Thol F., et al. Mutant IDH1 promotes leukemogenesis in vivo and can be specifically targeted in human AML. Blood. 2013;122:2877–2887. doi: 10.1182/blood-2013-03-491571. [DOI] [PubMed] [Google Scholar]
- 507.McCabe M.T., Mohammad H.P., Barbash O., Kruger R.G. Targeting Histone Methylation in Cancer. Cancer J. 2017;23:292–301. doi: 10.1097/PPO.0000000000000283. [DOI] [PubMed] [Google Scholar]
- 508.Min J.R., Feng Q., Li Z.Z., Zhang Y., Xu R.M. Structure of the catalytic domain of human DOT1L, a Non-SET domain nucleosomal histone methyltransferase. Cell. 2003;112:711–723. doi: 10.1016/S0092-8674(03)00114-4. [DOI] [PubMed] [Google Scholar]
- 509.Mao Y., Sun Y., Wu Z., Zheng J., Zhang J., Zeng J., Lee C., Kim J.K. Targeting of histone methyltransferase DOT1L plays a dual role in chemosensitization of retinoblastoma cells and enhances the efficacy of chemotherapy. Cell Death Dis. 2021;12:1141. doi: 10.1038/s41419-021-04431-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 510.Stein E.M., Garcia-Manero G., Rizzieri D.A., Tibes R., Berdeja J.G., Savona M.R., Jongen-Lavrenic M., Altman J.K., Thomson B., Blakemore S.J., et al. The DOT1L inhibitor pinometostat reduces H3K79 methylation and has modest clinical activity in adult acute leukemia. Blood. 2018;131:2661–2669. doi: 10.1182/blood-2017-12-818948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 511.Campbell C.T., Haladyna J.N., Drubin D.A., Thomson T.M., Maria M.J., Yamauchi T., Waters N.J., Olhava E.J., Pollock R.M., Smith J.J., et al. Mechanisms of Pinometostat (EPZ-5676) Treatment-Emergent Resistance in MLL-Rearranged Leukemia. Mol. Cancer Ther. 2017;16:1669–1679. doi: 10.1158/1535-7163.MCT-16-0693. [DOI] [PubMed] [Google Scholar]
- 512.Yi Y., Ge S. Targeting the histone H3 lysine 79 methyltransferase DOT1L in MLL-rearranged leukemias. J. Hematol. Oncol. 2022;15:35. doi: 10.1186/s13045-022-01251-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 513.Kanouni T., Severin C., Cho R.W., Yuen N.Y., Xu J., Shi L., Lai C., Del Rosario J.R., Stansfield R.K., Lawton L.N., et al. Discovery of CC-90011: A Potent and Selective Reversible Inhibitor of Lysine Specific Demethylase 1 (LSD1) J. Med. Chem. 2020;63:14522–14529. doi: 10.1021/acs.jmedchem.0c00978. [DOI] [PubMed] [Google Scholar]
- 514.Minucci S., Pelicci P.G. Histone deacetylase inhibitors and the promise of epigenetic (and more) treatments for cancer. Nat. Rev. Cancer. 2006;6:38–51. doi: 10.1038/nrc1779. [DOI] [PubMed] [Google Scholar]
- 515.Copeland R.A., Solomon M.E., Richon V.M. Protein methyltransferases as a target class for drug discovery. Nat. Rev. Drug Discov. 2009;8:724–732. doi: 10.1038/nrd2974. [DOI] [PubMed] [Google Scholar]
- 516.Janknecht R. The versatile functions of the transcriptional coactivators p300 and CBP and their roles in disease. Histol. Histopathol. 2002;17:657–668. doi: 10.14670/HH-17.657. [DOI] [PubMed] [Google Scholar]
- 517.He Z.X., Wei B.F., Zhang X., Gong Y.P., Ma L.Y., Zhao W. Current development of CBP/p300 inhibitors in the last decade. Eur. J. Med. Chem. 2021;209:112861. doi: 10.1016/j.ejmech.2020.112861. [DOI] [PubMed] [Google Scholar]
- 518.Bedford D.C., Kasper L.H., Fukuyama T., Brindle P.K. Target gene context influences the transcriptional requirement for the KAT3 family of CBP and p300 histone acetyltransferases. Epigenetics. 2010;5:9–15. doi: 10.4161/epi.5.1.10449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 519.Cai L.Y., Chen S.J., Xiao S.H., Sun Q.J., Ding C.H., Zheng B.N., Zhu X.Y., Liu S.Q., Yang F., Yang Y.X., et al. Targeting p300/CBP Attenuates Hepatocellular Carcinoma Progression through Epigenetic Regulation of Metabolism. Cancer Res. 2021;81:860–872. doi: 10.1158/0008-5472.CAN-20-1323. [DOI] [PubMed] [Google Scholar]
- 520.Crabb S., Plummer R., Greystoke A., Carter L., Pacey S., Walter H., Coyle V.M., Knurowski T., Clegg K., Ashby F., et al. A phase I/IIa study to evaluate the safety and efficacy of CCS1477, a first in clinic inhibitor of p300/CBP, as monotherapy in patients with selected molecular alterations. Ann. Oncol. 2021;32:S617. doi: 10.1016/j.annonc.2021.08.1082. [DOI] [Google Scholar]
- 521.Knurowski T., Clegg K., Brooks N., Ashby F., Pegg N.A., West W., Walter H.S., Somervaille T.C.P., Knapper S., Davies A. An Open-Label Phase I/IIa Study to Evaluate the Safety and Efficacy of CCS1477, a First in Clinic Inhibitor of the p300/CPB Bromodomains, As Monotherapy in Patients with Advanced Haematological Malignancies. Blood. 2019;134:1266. doi: 10.1182/blood-2019-124797. [DOI] [Google Scholar]
- 522.Josling G.A., Selvarajah S.A., Petter M., Duffy M.F. The role of bromodomain proteins in regulating gene expression. Genes. 2012;3:320–343. doi: 10.3390/genes3020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 523.Taniguchi Y. The Bromodomain and Extra-Terminal Domain (BET) Family: Functional Anatomy of BET Paralogous Proteins. Int. J. Mol. Sci. 2016;17:1849. doi: 10.3390/ijms17111849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 524.Spriano F., Stathis A., Bertoni F. Targeting BET bromodomain proteins in cancer: The example of lymphomas. Pharm. Ther. 2020;215:107631. doi: 10.1016/j.pharmthera.2020.107631. [DOI] [PubMed] [Google Scholar]
- 525.Filippakopoulos P., Qi J., Picaud S., Shen Y., Smith W.B., Fedorov O., Morse E.M., Keates T., Hickman T.T., Felletar I., et al. Selective inhibition of BET bromodomains. Nature. 2010;468:1067–1073. doi: 10.1038/nature09504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 526.Bose P., Dai Y., Grant S. Histone deacetylase inhibitor (HDACI) mechanisms of action: Emerging insights. Pharm. Ther. 2014;143:323–336. doi: 10.1016/j.pharmthera.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 527.Suraweera A., O’Byrne K.J., Richard D.J. Combination Therapy With Histone Deacetylase Inhibitors (HDACi) for the Treatment of Cancer: Achieving the Full Therapeutic Potential of HDACi. Front. Oncol. 2018;8:92. doi: 10.3389/fonc.2018.00092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 528.Song Y., Wu F., Wu J. Targeting histone methylation for cancer therapy: Enzymes, inhibitors, biological activity and perspectives. J. Hematol. Oncol. 2016;9:49. doi: 10.1186/s13045-016-0279-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 529.Meidhof S., Brabletz S., Lehmann W., Preca B.T., Mock K., Ruh M., Schuler J., Berthold M., Weber A., Burk U., et al. ZEB1-associated drug resistance in cancer cells is reversed by the class I HDAC inhibitor mocetinostat. EMBO Mol. Med. 2015;7:831–847. doi: 10.15252/emmm.201404396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 530.Cai M.H., Xu X.G., Yan S.L., Sun Z., Ying Y., Wang B.K., Tu Y.X. Depletion of HDAC1, 7 and 8 by Histone Deacetylase Inhibition Confers Elimination of Pancreatic Cancer Stem Cells in Combination with Gemcitabine. Sci. Rep. 2018;8:1621. doi: 10.1038/s41598-018-20004-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 531.Rivera-Del Valle N., Gao S., Miller C.P., Fulbright J., Gonzales C., Sirisawad M., Steggerda S., Wheler J., Balasubramanian S., Chandra J. PCI-24781, a Novel Hydroxamic Acid HDAC Inhibitor, Exerts Cytotoxicity and Histone Alterations via Caspase-8 and FADD in Leukemia Cells. Int. J. Cell Biol. 2010;2010:207420. doi: 10.1155/2010/207420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 532.Morschhauser F., Terriou L., Coiffier B., Bachy E., Varga A., Kloos I., Lelievre H., Sarry A.L., Depil S., Ribrag V. Phase 1 study of the oral histone deacetylase inhibitor abexinostat in patients with Hodgkin lymphoma, non-Hodgkin lymphoma, or chronic lymphocytic leukaemia. Investig. New Drugs. 2015;33:423–431. doi: 10.1007/s10637-015-0206-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.