To the Editors,
Myocarditis is one of most critical adverse reactions to messenger RNA (mRNA) COVID-19 vaccination. Globally, the frequency of myocarditis has been shown to be approximately 0.3–5.0 per 100,000 doses of COVID-19 mRNA vaccines [1]. Vaccine-induced myocarditis typically presents within 1 week after vaccination, with chest pain and dyspnea. It occurs predominantly in males between 12 and 29 years old and commonly after the second dose. The symptoms are generally mild, and the cardiac contractility is usually normal despite the presence of electrocardiogram (ECG) abnormalities. Treatment with nonsteroidal anti-inflammatory drugs can resolve symptoms within a few days, but severe vaccine-induced myocarditis has been rarely reported in patients with pre-existing health conditions [2].
Multiple genetic factors have been proposed to underly the development of myocarditis. Rare germline genetic variants of genes encoding inborn errors of immunity and sarcomeric proteins associated with cardiomyopathy as well as specific HLA alleles may predispose some individuals to myocarditis [3]. Since monozygotic twins share the same prenatal and similar postnatal environment and have the same age and gene profile, they may represent a very special resource for investigating the causes of rare complications of disease or adverse effects of drugs.
We herein report 2 cases of COVID19 vaccine-associated myocarditis in 13-year-old monochorionic diamniotic twins, strongly suggesting the presence of underlying genetic factors for predisposition to myocarditis after COVID-19 vaccination.
Patient 1
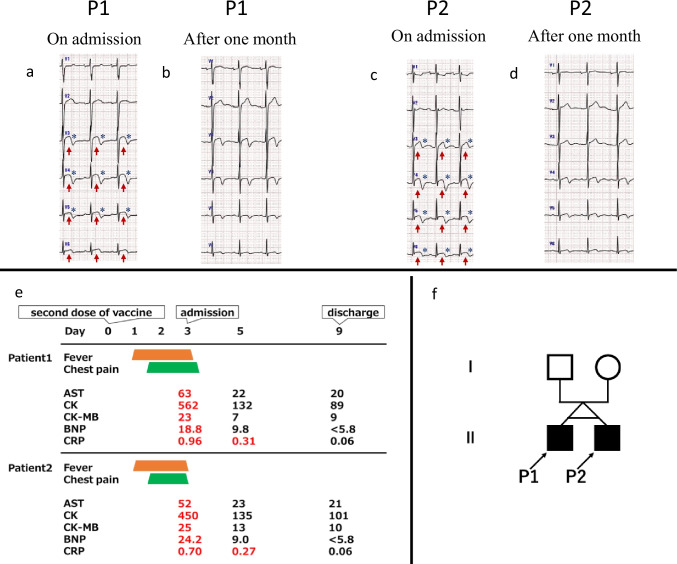
A 13-year-old boy developed a fever and chest pain the day after (about 30 h after) receiving his second dose of the BNT162b2 mRNA (Pfizer-BioNTech) COVID-19 vaccine (day 1). He visited our hospital 3 days after vaccination (day 3). On arrival at our hospital, about 66 h after vaccination, his fever had almost been relieved, and other vital signs were normal. A blood examination revealed mild elevation of C-reactive protein (CRP; 0.96 mg/dL), myocardial deviation enzyme of CK-MB (23 IU/L; normal ≤ 15) and BNP (marker of heart failure; 18.8 pg/mL; normal < 18.4). Electrocardiography (ECG) demonstrated elevations of ST-segment in II, III, aVF, and V3-6 and negative T waves in V3-5 (Fig. 1a). Echocardiography showed a normal cardiac function, with a left ventricular ejection fraction (LVEF) of 63.7% and normal left ventricular wall motion. He was diagnosed with possible myocarditis due to the findings of chest pain, elevated CK-MB, and abnormal ECG findings, based on the Brighton Collaboration diagnostic criteria. We did not perform a cardiac MRI examination due to the technical limitations of our hospital.
Fig. 1.
a–d ECG examination findings. a Patient 1 on admission: ST elevation in V3-6 (red arrows) and negative T waves in V3-5 (blue asterisks). b Patient 1 after one month: ECG changes improved. c Patient 2 on admission: ST elevation at V3-6 (red arrows) and negative T waves at V3-6 (blue asterisks). d Patient 2 after one month: ECG changes improved. e Clinical courses of patients 1 and 2: Both patients developed a fever and chest pain the day after the second vaccination and were hospitalized three days after vaccination. The symptoms resolved quickly. f Family pedigree. The MD twins with myocarditis after COVID-19 vaccine are indicated by black squares and arrows (P1 and P2)
Five days after vaccination, the chest pain spontaneously resolved, and the CK-MB level normalized; he was therefore discharged from the hospital 9 days after vaccination. ECG showed normal examination findings at 1 month after the onset (Fig. 1b).
Patient 2
Patient 2 was the monochorionic diamniotic twin brother of patient 1 and had been healthy from birth. He received the second dose of the Pfizer-BioNTech COVID-19 vaccine on the same day as patient 1. A fever and chest pain developed the day after vaccination (day 1; about 20 h after vaccination). By day 3, about 66 h after vaccination, his fever had already been relieved, but he visited our hospital along with patient 1. At that time, he had no clinical symptoms with stable vital signs.
Blood examinations revealed mild elevations in CRP (0.70 mg/dL), CK-MB (25 IU/L), and BNP (18.8 pg/mL). ECG showed the elevation of ST waves in I, aVL, and V3-6 and negative T waves in V3-6 (Fig. 1c). Echocardiography exhibited a normal LVEF (65.6%) with good left ventricular wall motion. He was diagnosed with myocarditis, similar to his brother. By 5 days after vaccination, the CK-MB level had normalized, and he was ultimately discharged 9 days after vaccination. One month after the onset, his ECG findings were normal (Fig. 1d).
Patients 1 and 2 followed nearly the same clinical course (Fig. 1e). They were healthy by nature and did not play any particular sports, nor were they involved in any club activities before or after vaccination. They had never had SARS-CoV-2 infection. Both had received the first dose of the Pfizer-BioNTech COVID-19 vaccine 21 days before the second dose and had not shown any symptoms after the first dose. Their parents presented with a fever for a few days after the second dose of the Pfizer-BioNTech COVID-19 vaccine without other complications. Neither the patients nor their parents have received boosters. The twins have no other siblings and had no family history of sudden unexpected death or cardiomyopathy (Fig. 1f). Besides the present cases, we experienced only one man in his 20 s who suffered from post-vaccination myocarditis in Nakatsu Municipal Hospital, which is responsible for the medical care of about 240,000 people in the local community, so the incidence of post-vaccination myocarditis in the community is not higher than the estimated incidence.
Discussion
We encountered a pair of adolescent monochorionic diamniotic twin boys who developed mild myocarditis after receiving the second dose of COVID-19 vaccine. As with common COVID-19 mRNA vaccine-related myocarditis (designated here as post-COVID-19 vaccine myocarditis), both cases presented with mild symptoms with spontaneously resolution in 10 days. Considering the rarity of post-COVID-19 vaccine myocarditis, the current monozygotic twin cases strongly suggested the presence of genetic susceptibility to this condition.
The association between severe adverse effects of COVID-19 mRNA vaccination and host genetic factors has been investigated in several studies. For example, in Pfizer-BioNTech (BNT162b2) recipients, HLA-A ∗ 03:01 was associated with chills, a fever, fatigue, and generally feeling unwell after vaccination [4]. Post-COVID-19 vaccine myocarditis may not be exceptional, and the presence of immune and genetic susceptibility to this condition has been assumed [1]. However, no reports have clearly demonstrated an association between specific genetic backgrounds and vaccine-related myocarditis. In general, an analysis of family cases is useful for identifying genetic backgrounds. However, possibly due to its rarity, there has only been one report of a family case of vaccine-related myocarditis so far. The reported cases were siblings (brothers, 14 and 12 years old) who developed chest pain 2 and 3 days after their second COVID-19 vaccination and were diagnosed with mild myocarditis with spontaneous resolution [5].
In this situation where family cases are poorly reported, we presented the first cases of monochorionic diamniotic twins with identical genetic background who developed myocarditis with a similar course after COVID-19 vaccination. These cases’ course strongly suggest the involvement of genetic factors in the development of post-COVID-19 vaccine myocarditis. We further plan to conducted comprehensive genetic analyses of these siblings to identify the genes predisposing patients to post-vaccine myocarditis (whole-exome or genome sequencing). In the future, an international registry of familial cases of post-COVID-19 vaccine myocarditis should be established to aid in more detailed genetic analyses. The identification of genetic factors for myocarditis after vaccination will aid in the pre-assessment of the risk of vaccination and contribute to the safe administration of COVID-19 vaccines.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the patients and their parents for providing their informed consent for the publication of this case. We acknowledge Dr. Sotaro Ito, Department of Pediatrics, Nakatsu Municipal Hospital for treating the patients. We greatly thank Dr. Alexandre Bolze for his critical review of our manuscript, and Dr. Brian Quinn for his support and writing assistance.
Author Contribution
H. N. treated the patients, designed and performed the study, and drafted and revised the manuscript. S. K., K. S., K. I., and S. O. revised and approved the manuscript. All authors approved the final manuscript as submitted.
Funding
This study was supported in part by Grants in Aid for Scientific Research from the Japan Society for the Promotion of Science (Grant Number: 22H03041 to S.O) and was supported in part by the Research Program on Emerging and Re-emerging Infectious Diseases from AMED (Grant Number: JP20fk0108531 to S.O).
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Heymans S, Cooper LT. Myocarditis after COVID-19 mRNA vaccination: clinical observations and potential mechanisms. Nat Rev Cardiol. 2022;19(2):75–77. doi: 10.1038/s41569-021-00662-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oster ME, Shay DK, Su JR, Gee J, Creech CB, Broder KR, et al. Myocarditis cases reported after mRNA-based COVID-19 vaccination in the US from December 2020 to August 2021. JAMA. 2022;327(4):331–340. doi: 10.1001/jama.2021.24110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kontorovich AR, Patel N, Moscati A, Richter F, Peter I, Purevjav E, et al. Myopathic cardiac genotypes increase risk for myocarditis. JACC Basic Transl Sci. 2021;6(7):584–592. doi: 10.1016/j.jacbts.2021.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bolze A, Neveux I, Schiabor Barrett KM, White S, Isaksson M, Dabe S, et al. HLA-A∗03:01 is associated with increased risk of fever, chills, and stronger side effects from Pfizer-BioNTech COVID-19 vaccination. HGG Adv. 2022;3(2):100084. doi: 10.1016/j.xhgg.2021.100084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moosmann J, Gentles T, Occleshaw C, Mitchelson B. COVID vaccine-associated myocarditis in adolescent siblings: does it run in the family? Vaccines (Basel) 2022;10(4):611. doi: 10.3390/vaccines10040611. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.