Abstract
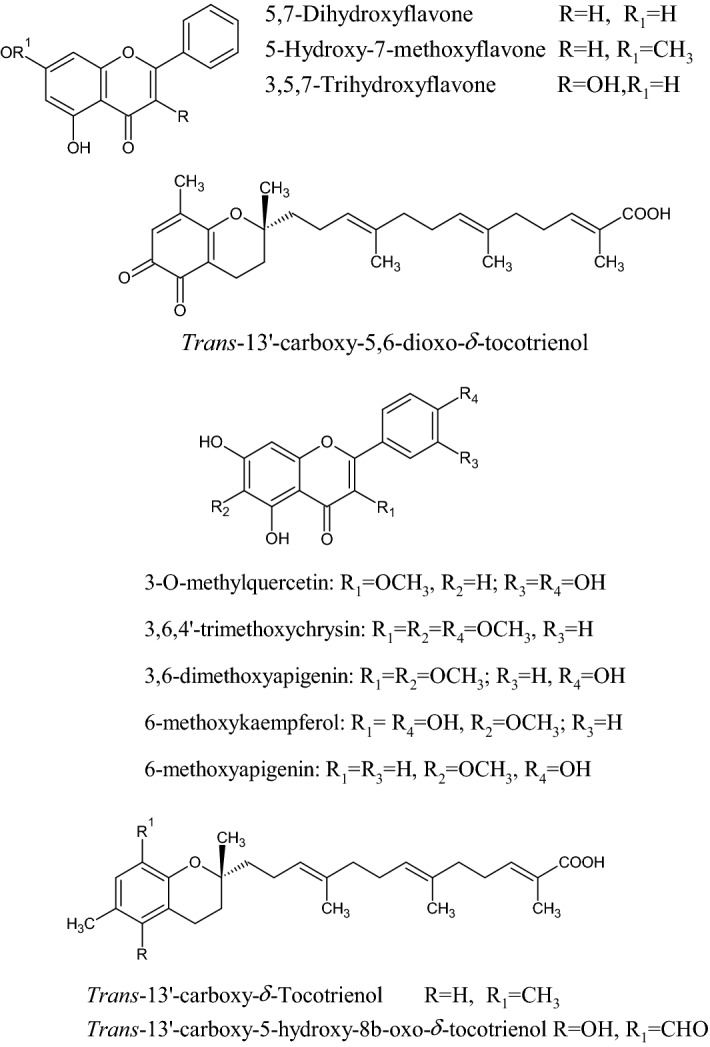
Propolis, a resinous substance produced by honeybees from various plant sources, has been used for thousands of years in traditional medicine for several purposes all over the world. The precise composition of propolis varies according to plant source, seasons harvesting, geography, type of bee flora, climate changes, and honeybee species at the site of collection. This apiary product has broad clinical applications such as antioxidant, anti-inflammatory, antimicrobial, anticancer, analgesic, antidepressant, and anxiolytic as well asimmunomodulatory effects. It is also well known from traditional uses in treating purulent disorders, improving the wound healing, and alleviating many of the related discomforts. Even if its use was already widespread since ancient times, after the First and Second World War, it has grown even more as well as the studies to identify its chemical and pharmacological features, allowing to discriminate the qualities of propolis in terms of the chemical profile and relative biological activity based on the geographic place of origin. Recently, several in vitro and in vivo studies have been carried out and new insights into the pharmaceutical prospects of this bee product in the management of different disorders, have been highlighted. Specifically, the available literature confirms the efficacy of propolis and its bioactive compounds in the reduction of cancer progression, inhibition of bacterial and viral infections as well as mitigation of parasitic-related symptoms, paving the way to the use of propolis as an alternative approach to improve the human health. However, a more conscious use of propolis in terms of standardized extracts as well as new clinical studies are needed to substantiate these health claims.
Keywords: Anticancer, Antioxidant, Anti-inflammatory, Bee glue, Bioactive compounds, Food preservative
Introduction
The name "propolis" derives from two terms of Greek origin, “pro” and “polis”, which literally mean "in favor of the city" [1]. In fact, propolis, which is a sticky, gummy, and balsamic material collected from plants, is used by bees (Apis mellifera L.) to coat the hive and protect it from diseases caused by fungi, yeast, and bacteria as well as from predators [2]. In particular, propolis derives from a resin that is found mainly in the buds and bark of poplars, birches and conifers in general. The foraging bees collect these resins obtaining a mixture of resinous substances, pollen, waxes, and enzymes [3, 4]. Propolis is commonly employed by bees as building material and sealer [5] by maintaining homeostasis, reducing vibrations, keeping airflow, defend the colony against squatters, and prevent putrefaction [6]. It consists of granules of various sizes and shades of color (yellow, red, and dark brown) depending on its botanical source, while its smell is strongly aromatic [7]. Its consistency is hard and crumbly in nature, but as soon as it is handled and slightly heated, it becomes viscous and sticky, melting at temperatures around 70 °C [8].
Propolis has been the topic of several research conducted around the world in recent decades, and its chemical composition and biological properties have been widely explored [9–15]. The most common uses of propolis are as immunostimulant, as an aid to prevent colds thanks to its antibacterial and antiviral action, as a natural remedy in case of skin problems due to its soothing and healing effect, also in the oral cavity to treat small ulcers and canker sores, to relieve redness and itching of the urinary tract and finally to restore the balance of the gastric mucosa [16–18].
Recently, some mechanisms of action have been suggested paving the way to new clinical applications. The aim of this study is to provide a comprehensive review of these recent findings, discussing the current state of propolis research as well as the future prospectives.
History of propolis
In the long and rich history of human beekeeping, apiary products have been widely used due to their recognized beneficial properties. In particular, the traditional use of propolis is known since 300 B.C. The Egyptians worshiped the bee and used propolis in the mummification process [19]. It was also well known to the priests who, at that time, monopolized medicine and chemistry [1]. Bees played an essential role in Greek and Roman religious traditions assuming many symbolic meanings and being featuring in many stories of the Greek and Roman gods. Among them, one tells of Zeus (Jupiter for Romans), who, to escape his father, the god Cronus, was hidden in a secret cave by his mother and fed thanks to the honey of the sacred bees. Probably due to this story, one of Zeus' names was "Melissaios", or "bee-man". According to this legend, it was Zeus himself, who gave the bees their bright gold color and to made them strong enough to withstand the cold and winds.
In traditional Georgian medicine, some ailments were treated using propolis ointments. There was also the custom of putting a propolis cake on the navel of the newborn. During the Anglo-Boer War [2] and World War II, doctors used propolis to heal wounds efficiently. Finally, in the USRR, the orthodox medicine recognized the therapeutic use of propolis (30% alcohol solution) already in 1969 [20]. Propolis was a key component in the Greek fragrance polyanthus, which included propolis, olibanum, styrax, and fragrant plants [21]. It has been extolled by more than 15 Greek and Roman writers (beside honey and wax) such as Aristotele in its “Historia Animalium” and Hippocrates, who is known to have employed propolis to treat wounds and ulcers [21]. Moreover, Dioscorides, in his main book “De materia Medica”, outlined the medicinal applications of propolis, by citing also honey, wax, and different honey wines as medicines [22]. The bee and propolis were likewise highly esteemed by the Romans. Just think of Pliny the Elder, who discussed it, enhancing its multiple therapeutic applications as purifying agent, tumors dispersant, calming agent for tendon pains and for its healing properties [23].
Traditional uses
Propolis has long been used as a bactericidal, antiviral, and antifungal drug in folk medicine to treat inflammations in several body areas worldwide [24]. It was used for skin regeneration, wound healing, and as local anesthetic and, in this sense, it was found in nearly all home first-aid kits [25]. Propolis has also been advised in folk medicine for the treatment of purulent disorders, as it has been shown to improve wound healing and relieve many types of discomfort. Craftsmen utilized propolis also for no-health purposes such as windows sealer, impregnant for valuable timber objects, varnish and repairing instrument [26]. The alternative and complementary medicine used different propolis-based preparations such as sprays, ointments, and powders (mainly consisting of tinctures and ethanolic extracts) for the treatment of colds, flu, bronquial asthma, and other human ailments [27] such as gastric disorders [28]. Moreover, propolis is still used as an active substance in some dietary supplements, cosmetics, and even medicinal sweets. Unlike honey and bee pollen, it has no nutritional value, but exerts a very strong and multidirectional biotic effect [29]. Propolis has recently become popular in food and beverages as a way to boost health and prevent illness [30, 31]. It is still used to treat wounds and burns, as well as sore throats, dental caries, and stomach ulcers [32]. For years, propolis ethanolic extract has been known to have anti-inflammatory properties and used as an immunomodulatory agent [24, 33]. It can be used for various purposes in endodontics and would have a promising role in dentistry [28]. Researchers used nanoparticles to test the usage of propolis for various purposes. The use of nanoparticle-based delivery methods has the potential to make hydrophobic compounds like propolis dispersible in aqueous media, avoiding the problems associated with poor solubility [34].
Chemical composition and physical properties
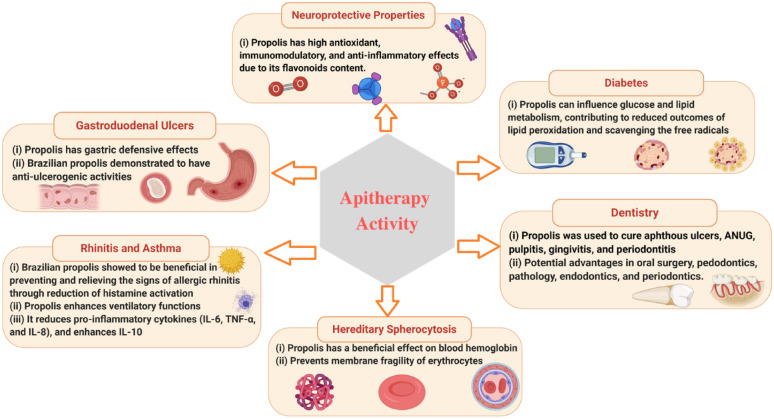
It is well-known that a medicinal plant demonstrates a pharmacological effect thanks to its chemical constituents. Raw propolis contains not only plant resins, but also waxes, essential oil, pollens, and other organic sunstance in different percentage as depicted in Fig. 1. Thanks to this multitude of components, it consists of a rather complex chemical profile as reported in Table 1. Many studies reported that propolis contains, in particular, phenolic acids, flavonoids, ketones, aldehydes, chalcones, dihydrochalcones, terpenoids, amino acids, aliphatic acids, aromatic esters and acids, carbohydrates, vitamins, metals, and also beeswax [35–40].
Fig. 1.
Chemical composition (%) of raw propolis
Table 1.
Chemical composition of raw propolis
| Class | Compounds |
|---|---|
| Alcohols | Benzene methanol, cinnamyl alcohol, glycerol; a-glycerophosphate; hydroquinone; isobutenol, phenethyl alcohol; prenyl alcohol [176, 177, 353] |
| Aldehydes | Benzaldehyde; caproiealdehyde; p-hydroxybenzaldehyde; isovanillin; protocatechuic aldehyde; vanillin [176, 353–356] |
| Aliphatic acids and aliphatic esters | Acetic acid; angelic acid; butyric acid; crotonic acid; fumaric acid; isobutyric acid; methylbutyric acid; isobutyl acetate; isopentyl acetate; isopentenyl acetate [176] |
| Amino acids | Alanine; β-alanine; α-aminobutyric acid; 6-aminobutyric acid; arginine; asparagine; aspartic acid; cystine; cysteine; glutamic acid; glycine; histidine; hydroxyproline; isoleucine; leucine, lysine; methionine; ornithine; phenylalanine; proline; pyroglutamic acid, sarcosine; serine; threonine, tryptophan; tyrosine; valine [49, 50, 176, 357] |
| Aromatic acid | p-Anisic acid; benzoic acid; caffeic acid; cinnamic acid; coumaric (-o,-m,-p) acid; 3,4-dimethoxycinnamic acid; ferulic acid; gallic acid; gentisic acid; hydroxycinnamic acid; p- hydroxybenzoic acid; isoferulic acid; 4-methoxycinnamic acid; protocatechuic acid; salicylic acid; vanillic acid; veratric acid [176, 177, 353–356, 358, 359] |
| Aromatic esters | Benzyl acetate, benzyl benzoate, benzyl caffeate, benzyl coumarate; benzyl-3,4-dimethoxycinnamate; benzyl ferulate; benzyl isoferulate; benzyl salicylate; butenyl caffeate; butyl caffeate; cinnamyl benzoate; cinnamyl caffeate; butyl caffeate; cinnamyl coumarate; cinnamyl isoferulate; ethyl benzoate; ethyl caffeate; methyl benzoate; 2-methyl-2-butenyl caffeate; 3-methyl-2-butenyl caffeate; 3-methyl-3-butenyl caffeate; 3-methyl-3-butenyl coumarate; 3-methyl-2 -butenyl ferulate; 3-methyl -3-butenyl ferulate; 2-methyl-2-butenyl isoferulate, 3-methyl-3-butenyl isoferulate; methyl salicylate; phenyl ethyl caffeate: phenyl ethylcoumarate; phenyl–ethyl isoferulate; pentyl caffeate; pentenyl caffeate, pentenyl ferulate; prenyl caffeate; prenyl coumarate; prenyl ferulate; prenyl isoferulate [176, 177, 353, 358, 359] |
| Chalcones and dihydrochalcones | Alpinetin chalcone; naringenin chalcone; pinobanksin chalcone, pinobanksin-3-acetate chalcone; pinocembrin chalcone; pinostrobin chalcone; sakuranetin chalcone; 2',4’,6' -trihydroxy-4'-methoxychalcone; 2',6'-dihydroxy-4'-methildihydrochalcone; 2’,4',6’- trihydroxydihydrochalcone [176, 177, 353, 359]; 3,4,2',3'-tetrahydroxychalcone [360], isoliquiritigenin, 4,4'-dihydroxy-2'-methoxychalcone; 4,2',4',alpha-tetrahydroxydihydrochalcone, 2',4'-dihydroxychalcone [361] |
| Flavanones | Naringenin; pinobanksin; pinobanksin-3-acetate; pinobanksin-3-butyrate; pinobanksin-3-hexanoate, pinobanksin-3-methyl ether; pinobanksin-3-pentanoate; pinobanksin-3-pentenoate; pinobanksin-3-propanoate; pinocembrin; pinostrobin; sakuranetin; 3,7-dihydroxy-5-methoxytlavanone; 2,5-dihydroxy-7-methoxyflavanone [49, 176, 177, 355, 359, 362–364]; 5,7-dihydroxy-6-methoxy-2,3-dihydroflavonol-3-acetate [365], 5-methoxy-3-hidroxyflavanone [366], (2R, 3R)-3,6,7-trihydroxyflavanone [367], alnustinol, (2R,3R)-3,7-dihydroxy-6-methoxyflavanone, garbanzol, (2R,3R)-3,7-dihydroxyflavanone, (2S)-dihydrooroxylin A, (2S)-dihydrobaicalein, (2S)-nNaringenin, (2S)-7-hydroxy-6-methoxyflavanone, (2S)-liquiritigenin, (2S)-7-hydroxyflavanone [361], sophoraflavanone A, solophenol A, bonannione A [368], sigmoidin B, propolin E, propolin B, propolin A [369], 5,7,3',4'-tetrahydroxy-2'-C-geranyl-6-prenlyflavanone, 5,7,3',4'-tetrahydroxy-2'-C-geranylflavanone, 5,7,3',4'-tetrahydroxy-6-C-geranylflavanone, 5,7,3',4'-tetrahydroxy-5'-C-geranylflavanone [48]; 3',4',6-trihydroxy-7-methoxy flavanone [367], (2R,3R)-6[1-(4'-hydroxy-3'-methoxyphenyl) prop-2en-1-yl]-pinobanksin-3-acetate, (2R,3R)-6[1-(4'-hydroxy-3'-methoxyphenyl) prop-2en-1-yl] pinobanksin [370], (2R,3R)-3,5-dihydroxy-7-methoxyflavanone 3-(2-methyl)-butyrate [97]; 7-O-prenylpinocembrin, 7-O-prenylstrobopinin [371]; pinobanksin-5-methyl-ether-3-O-pentanoate, hesperitin-5,7-dimethyl ether [366], (2S)-5,7-dihydroxy-4'-methoxy-8-prenylflavanone [368], 3-O-[(S)-2-methylbutyroyl] pinobanksin [372] |
| Flavones and flavonols | Acacetin; apigenin; apigenin-7-methyl ether; chrysin, fisetin; galangin; galangin-3-methyl ether; izalpinin; isorhamnetin; kaempferide; kaempferol; kaempterol-3-methyl ether; kaempferol-7-methyl ether; kaempferol-7,4’-dimethyl ether; pectolinarigenin; quercetin; quercetin-3,7-dimethyl ether; ramnetin; ramnocitrin, tectocrisin [49, 176, 177, 353–356, 364]; luteolin [373]; 6-cinnamylchrysin [372]; 3',5-dihydroxy-4',7-dimenthoxy flavones [374]; hexamethoxy flavones [375]; (7''R)-8-[1-(4'-hydroxy-3'-methoxyphenyl) prop-2-en-1-yl] chrysin [97]; (7"R)-8-[1-(4'-hydroxy-3'-methoxyphenyl)prop-2-en-1-yl]-galangin [97]; macarangin [376]; 2'-geranylquercetin, 8-(8"-hydroxy-3",8"-dimethyl-oct-2"-enyl)-quercetin, 2'-(8"-hydroxy-3",8"-dimethyl-oct-2"-enyl)-quercetin [368] |
| Isoflavones | 4',7-dimethoxy-2'-isoflavonol, medicarpin, homopterocarpin, 7,4'-dihydroxyisoflavone [377], calycosin [361], 5,7-dihydroxy-4'-methoxyisoflavonoid, 7-hydroxy-4'-methoxyisoflavonoid [378], 7,3'-dihydroxy-6,5'-methoxyisoflavonoid, 6,7,3'-trihydroxy-4'-methoxyisoflavonoid, 7,3',4'-trihydroxy-5'-methoxyisoflavonoid, odoratin [367]; biochanin [379], (3R)-4'-Methoxy-2',3,7-trihydroxyisoflavanone, (3S)-ferreirin, (3S)-violanone, (3S)-vestitone, 2'-hydroxybiochanin A, pratensein, biochanin A, xenognosin B, formononetin, daidzein [361] |
| Flavans and Isoflavans | 8-[(E)-4-phenylprop-2-en-1-one]-(2R,3S)-2-(3,5-dihydroxyphenyl)-3,4-dihydro-2H-2-be-nzopyran-5-methoxyl-3,7-diol, 8-[(E)-4-phenylprop-2-en-1-one]-(2S,3R)-2-(3,5-dihydroxyphenyl)-3,4-dihydro-2H-2-benzopyran-5-methoxyl-3,7-diol, 8-[(E)-4-phenylprop-2-en-1-one]-(2R,3S)-2-(3-methoxyl-4-hydroxyphenyl)-3,4-dihydro-2H-2-benzopyran-5-methoxyl-3,7-diol [380]; 3-hydroxy-5,6-dimethoxyflavan [381]; (3S)-vestitol, (3S)-isovestitol, (3S)-7-O-methylvestitol, (3S)-mucronulatol [361]; 7,4'-dihydroxy-2'-methoxyisoflavone [378]; neovestitol [379] |
| Open-chain neoflavonoids and other flavonoids | (S)-4-methoxydalbergione, (S)-3',4'-dihydroxy-4-methoxydalbergione, (S)-3'-hydroxy-4-methoxydalbergione [367], neoflavonoid 1–10 [382], (Z)-1-(2'-methoxy-4',5'dihydroxyphenyl)-2-(3-phenyl)propene, 1-(3',4'-dihydroxy-2'-methoxyphenyl)-3-(phenyl)propane [381], 2-(2',4'-dihydroxyphenyl)-3-methyl-6-methoxybenzofuran, 2,6-dihydroxy-2-[(4-hydroxyphenyl)methyl]-3-benzofuranone [361] |
| Hydrocarbon esters ethers, hydroxyl and keto waxes | Heneicosane; hentriacontane; heptacosane; hexacosane; nonacosane; pentacosane; tricosane; tripentacontane; tritriacontane; dotriacontyl hexadecanoate; dotriacontyl-[(Z)-octadec-9-enoate]; hexacosyl hexadecanoate; hexacosyl-[(Z)-octadec-9-enoate]; octacosylhexa decanoate; octacosyl-[(Z)-octadec-9-enoate] tetracosyl-hexadecanoate; tetracosyl-[(Z)-octadec-9-enoate]; tetratriacontyl-hexadecanoate tetratriacontyl-[(Z)-octadec-9-enoate]; triacontyl-hexadecanoate; triacontyl–[(Z)-octadec-9-enoate] [177, 353, 383, 384] |
| Pterocarpins (a type of neoflavonoid) | (6aR,11aR)-4-methoxymedicarpin, 6a-ethoxymedicarpin, 3,10-dihydroxy-9-methoxypterocarpan [361], 3,4-dihydroxy-9-methoxypterocarpan, 3-hydroxy-8,9-dimethoxypterocarpan, 3,8-dihydroxy-9-methoxypterocarpan, 4'-methoxy-5'hydroxyvesticarpan, homopterocarpin, 4-hydroxymedicarpin, medicarpin [378] |
| Fatty acids | Arachid acid; behenic acid; cerotic acid; lauric acid; linoleic acid; lignoceric acid; montanic acid; myristic acid; oleic acid; palmitic acids; stearic acid [177, 353, 359, 383] |
| Ketones | Acetophenone; p-acetophenolacetophenone; dihydroxy-acetophenone; methylacetophenone; hept-5-en-2-one; 6-methylketone [177, 353, 359] |
| Terpenoids and other compounds | α-Acetoxibetulenol; β-bisabolol; 1,8-cineole; α-copaene; cymene; limonene; pterostilbene; styrene; xanthorreol; xylitol; naphthalene; 4-hexanoIactone; sesquiterpene alcohol; sesquiterpene diol [49, 177, 353, 354, 363]; linalool [385], trans-β-terpineol [386], camphor [387]; junipene [386], γ-elemene, α-ylangene, valencene [385], 8-βH-cedran-8-ol, 4-βH,5α-eremophil-1(10)-ene, α-bisabolol, α-eudesmol, α-cadinol [388], patchoulene, manoyl oxide, ferruginol, ferruginolone, 2-hydroxyferruginol, 6/7-hydroxyferruginol, sempervirol, abietic acid, 18-succinyloxyabietadiene, 18-succinyloxyhydroxyabietatriene, 18-hydroxyabieta-8,11,13-triene, imbricataloic acid, diterpenic acid, neoabietic acid, labda-8(17),12,13-triene, hydroxydehydroabietic acid, dihydroxyabieta-8,11,13-triene, 13(14)-dehydrojunicedric acid, dehydroabietic acid, 18-hydroxyabieta-8,11,13-triene [389], junicedric acid, 14,15-dinor-13-oxo-8(17)-labden-19-oic acid, tran-communal, palmitoyl isocupressic acid, oleoyl isocupressic acid, 13-hydroxy-8(17),14-labdadien-19-oic acid, 15-oxolabda-8(17),13(E)-dien-19-oic acid, pimaric acid, totarolone [390]; lupeol alkanoates, lupeol, 24-methylene-9,19-ciclolanostan-3β-ol [391], lupeol acetate, lanosterol, germanicol acetate, germanicol, β-amyrin acetate, β-amyrone, α-amyrin acetate, α-amyrone [392], lanosterol acetate [375], (22Z,24E)-3-Oxocycloart-22,24-dien-26-oic acid, (24E)-3-oxo-27,28-dihydroxycycloart-24-en-26-oic acid [393], 3,4-seco-cycloart-12-hydroxy-4(28),24-dien-3-oicacid, cycloart-3,7-dihydroxy-24-en-28-oic acid [390], 3-oxo-triterpenic acid methyl ester [394]; 2H-cyclopentacyclooctene,4,5,6,7,8,9-hexahydro-1,2,2; 3-tetramethyl; germanicol; dimethyl-1,3,5,6-tetramethyl-[1,3-(13C2)] bicycle; dodeca-1,3,5,6,8,10-hexaene-9,10-dicarboxylate; spiro[benzo[α]cyclopenta [3, 4]cyclobuta[1,2-c]cycloheptene-8(5H),2'-[1,3]dioxane]; 6,7,7β,10α-tetrahydro-1; 14-methyl-cholest-7-en-3-ol-15-one; (3α,4α)- 4-methyl-stigmast-22-en-3-ol [28] |
| Lignans | Tetrahydrojusticidin B, 6-methoxydiphyllin, phyllamricin C [376] |
| Phenylpropanoids | cis-3-Methoxy-4-hydroxycinnamic acid, trans-3-methoxy-4-hydroxycinnamic acid [395]; 3-prenyl cinnamic acid allyl ester, p-methoxycinnamic acid, dihydrocinnamic acid, 3-methyl-2-butenyl isoferulate, 3-methyl-3-butenyl caffeate, hexadecyl caffeate [396]; 3-prenyl-4-hydroxycinnamic acid, 3,5-diprenyl-4-hydroxycinnamic acid [397]; methyl(E)-4-(4'-hydroxy-3'-methylbut-(E)-2'-enyloxy) cinnamate [398]; tetradecenyl caffeate (isomer), tetradecenyl caffeate [375]; 2-methyl-2-butenyl ferulate [48] |
| Chlorogenic acids | 4-Feruoyl quinic acid [399]; 5-ferruoyl quinic acid [373]; 3,4,5-tri-O-caffeoylquinic acid [400] |
| Stilbenes | 5'-Farnesyl-3'-hydroxyresveratrol [368]; schweinfurthin A, B [376]; 5,4'-dihydroxy-3'-methoxy-3-prenyloxy-E-stilbene, 3,5,3',4'-tetrahydroxy-2-prenyl-E-stilbene, 3,5,4'-trihydroxy-3'-methoxy-2-prenyl-E-stilbene, 5,3',4'-trihydroxy-3-methoxy-2-prenyl-E-stilbene, 5,4'-dihydroxy-3,3'-dimethoxy-2-prenyl-E-stilbene, 5,4'-dihydroxy-3-prenyloxy-E-stilbene, 3',4'-dihydroxy-E-stilbene, 3',4'-dihydroxy-3,5-dimethoxy-E-stilbene, diprenylated dihydrostilbene, 3,5-dihydroxy-2-prenyl-E-stilbene, 4-prenyldihydroresveratrol, 3-prenylresveratrol [398]; ( +)-pinoresinol dimethyl ether, ( +)-pinoresinol, ( +)-syringaresinol [361] |
| Other phenolics | 8-(Methyl-butanechromane)-6-propenoic acid, 3-hydroxy-2,2-dimethyl-8-prenylchromane-6-propenoic acid, 2,2-dimethyl-8-prenylchromene-6-propenoic acid, 2,2-dimethylchromene-6-propenoic acid, 2,2-dimethyl-6-carboxyethnyl-2H-1-benzopyran, 2,2-dimethyl-6-carboxyethenyl-8-prenyl-2H-1-benzopyran [401]; nemorosone, 7-epi-clusianone, xanthochymol, gambogenone, hyperibone A [402]; 5-pentadecylresorcinol, 5-(8'Z,11'Z-heptadecadienyl)-resorcinol, 5-(11'Z-heptadecenyl)-resorcinol, 5-heptadecylresorcinol [95]; 1,3-bis(trimethylsilylloxy)-5,5-proylbenzene, 3,4-dimethylthioquinoline, 4-oxo-2-thioxo-3-thiazolidinepropionic acid, D-glucofuranuronic acid, dofuranuronic acid, 3-quinolinecarboxamine [403], baccharin [20], suberosin, tschimgin, tschimganin, bornyl p-hydroxybenzoate, bornyl vanillate, ferutinin, tefernin, ferutinol p-hydroxybenzoate, ferutinol vanillate [387]; 2-acetoxy-6-p-methoxybenzoyl jaeschkeanadiol, 2-acetoxy-6-p-hydroxybenzoyl jaeschkeanadiol [404] |
| Steroids | Calinasterol acetate; β-dihydrofucosterol acetate; ucosterol acetate; stigmasterol acetate [178] |
| Sugars | Fructofuranose-1; fructofuranose-2; α-D-glucopyranose; β-D-glucopyranose [177, 353, 358]; galactitol, gluconic acid, galacturonic acid and 2-O-glycerylgalactose [394] |
The color and melting point of propolis varies according to area and the plant source [4]. Propolis melts on 60 °C to 70 °C while some of its kinds melt on 100 °C [4, 26]. Ethanol is the best suitable solvent to obtain commercially extracts of propolis but is also used methanol, chloroform, ether and acetone [4, 26, 41].
Compounds isolated from propolis
According to literature up to now about 300 different chemicals components have been determined in propolis of different sources [4, 9, 42–44]. Moreover, the major chemical constituents are varied in amount and type and depend on the extraction process associated with the extraction solvents. Recently, Bankova et al. [45] reviewed classical and modern methods of extraction of propolis such as maceration, Soxhlet, ultrasound-assisted and microwave-assisted extraction, supercritical CO2 extraction, high-pressure methods, and the application of different solvents. The authors concluded that ultrasound-assisted extraction is the best optimal method, considering into account extraction time and extraction yield, and concerning the solvents, mixtures of water and ethanol are most effective.
Propolis has a very rich and complex chemical composition, which varies according to several parameters such as plant source, seasons harvesting, geography, type of bee flora, climate changes, and honey bee species at the collection site [15, 44, 46, 47]. Indeed, more than 300 different compounds have been isolated and identified from this natural product. Many studies conducted on various propolis samples have shown that the main secondary metabolites are phenolic substances, especially flavonoids, belonging to different sub-classes such as flavanones, flavones, flavonols and dihydroflavonols, which constitute more than 50% of the propolis weight [4, 9, 42–44]. These compounds, generally present in the plant kingdom as glycosides, are mostly present in propolis as aglycones, probably due to the action of bees’enzymes (glucosidase) during harvesting and transport. Other phenolic compounds found abundantly in propolis are hydroquinones, caffeic acids and related esters and phenolic aldehydes [48]. Propolis has also proved to be a rich source of essential elements such as magnesium, nickel, calcium, iron, zinc, cesium, manganese, silver, copper, aluminum, vanadium, vitamins B, C and E [49], as well as amino acids [50]. In addition, in propolis, some non-phenolic substances belonging to different classes such as aliphatic acids, coumarins, aliphatic and aromatic hydrocarbons, terpenoids, steroids and isoprenylated benzophenones, have also been found. The chemical composition of propolis is closely related to the place of origin, the time of harvest and the plant source from which it derives, and it is for this reason it is difficult to achieve a univocal classification of the chemical substances and therapeutic properties of this natural product. Moreover, these remarkable qualitative-quantitative phytochemical differences related to its geographical distribution that diversify and characterize propolis, make it unique both from chemical and biological point of view. For example, Tunisian propolis is distinguished by the presence of characteristic methoxyylated flavonoids, such as quercetin 3,7,3 ‘-trimethyl ether and myricetin 3,7,4',5' tetramethylether from Cistus spp., Cistaceae, leaf exudates [51], while a study carried out on New Zealand propolis has shown that hydroflavonoids such as pinocembrin and pinobanksin and make up about 70% of the total flavonoids from Populus nigra L., Salicaceae, bud exudates [52].
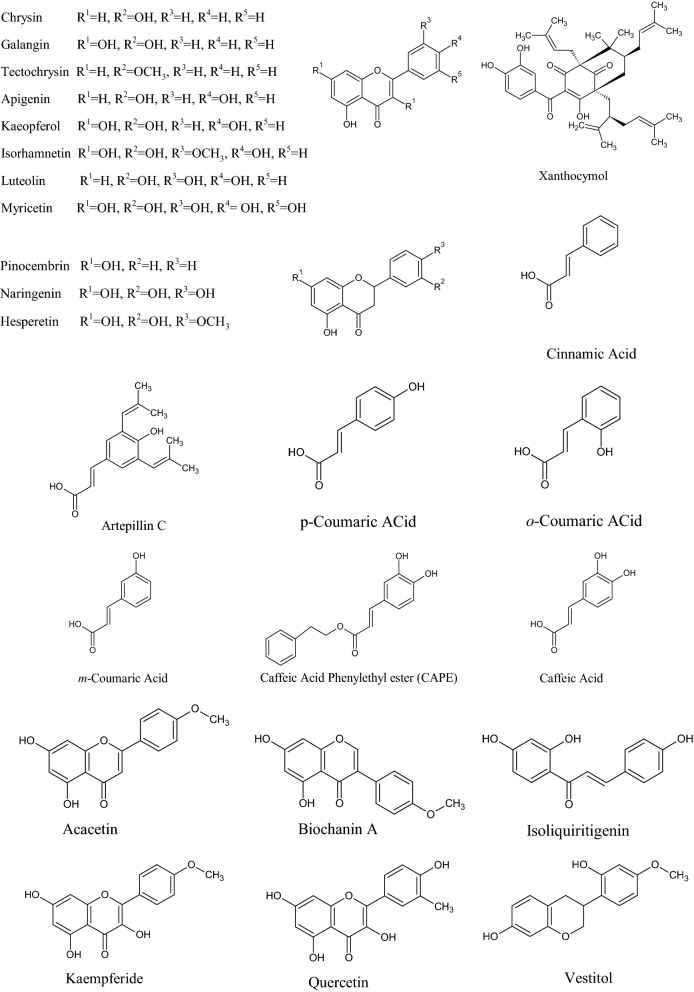
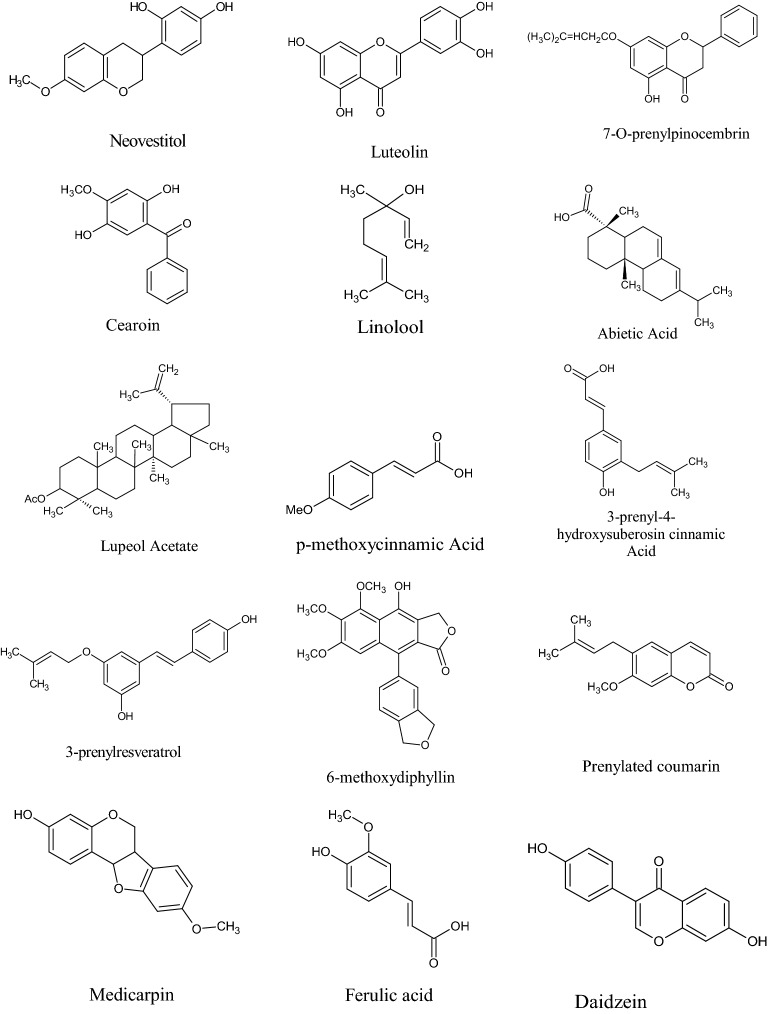
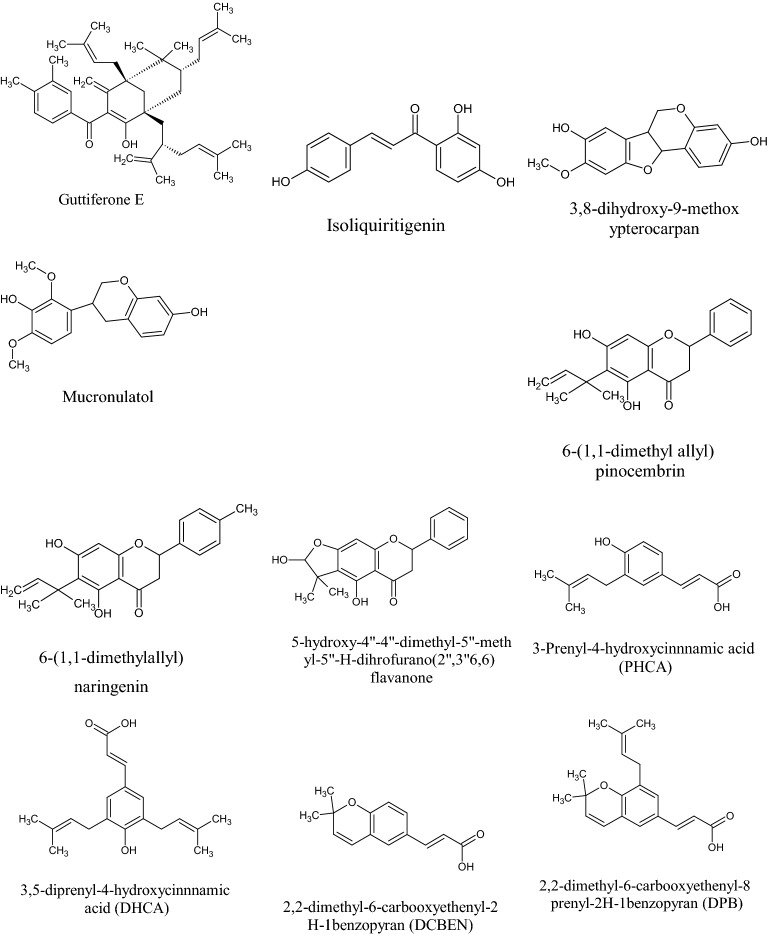
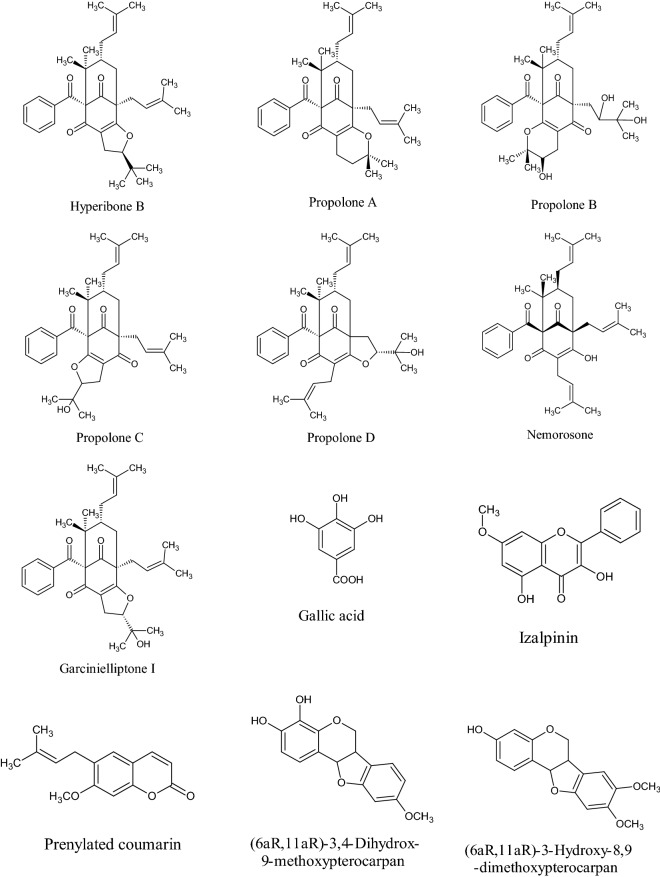
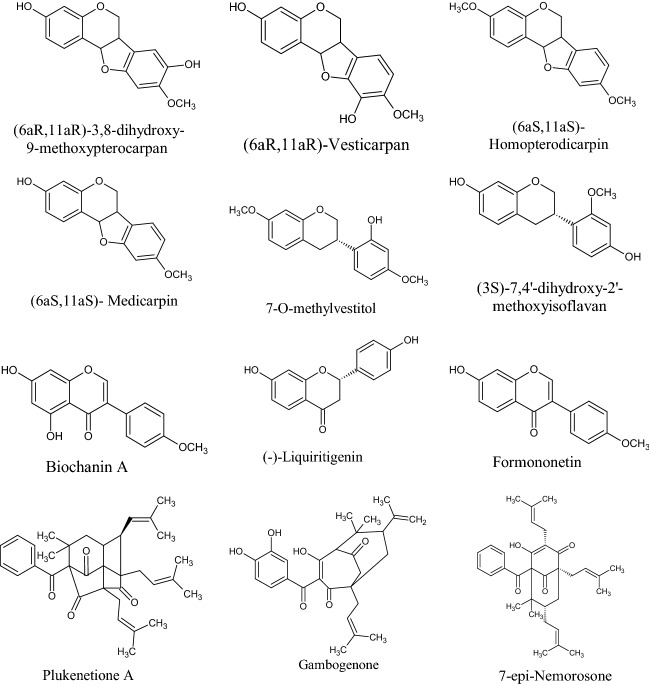
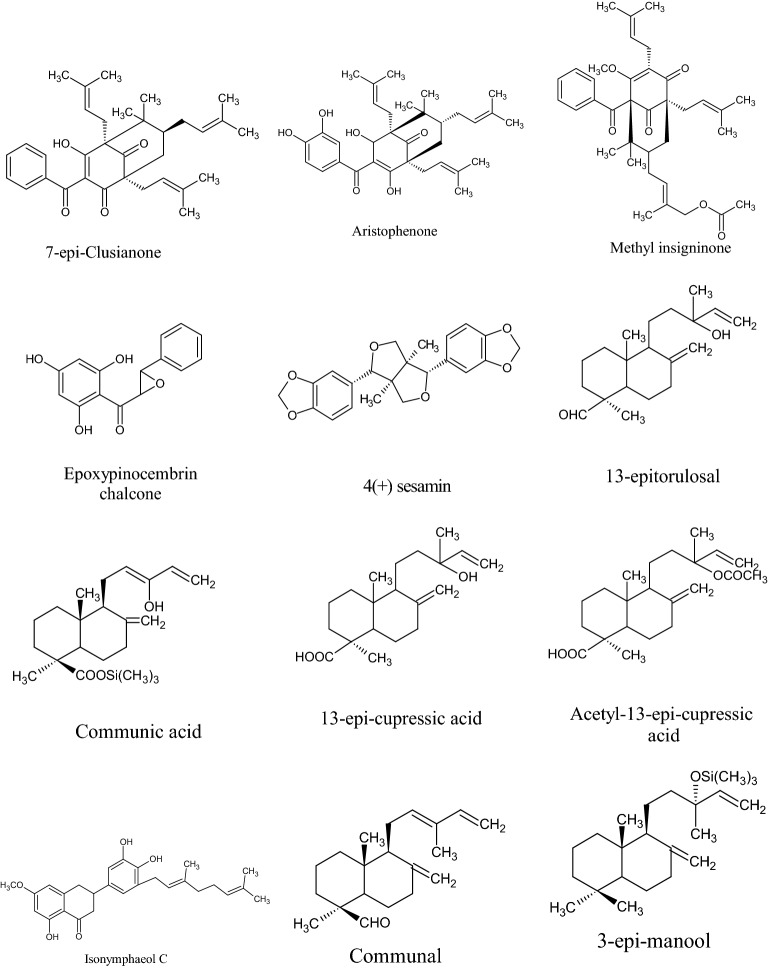
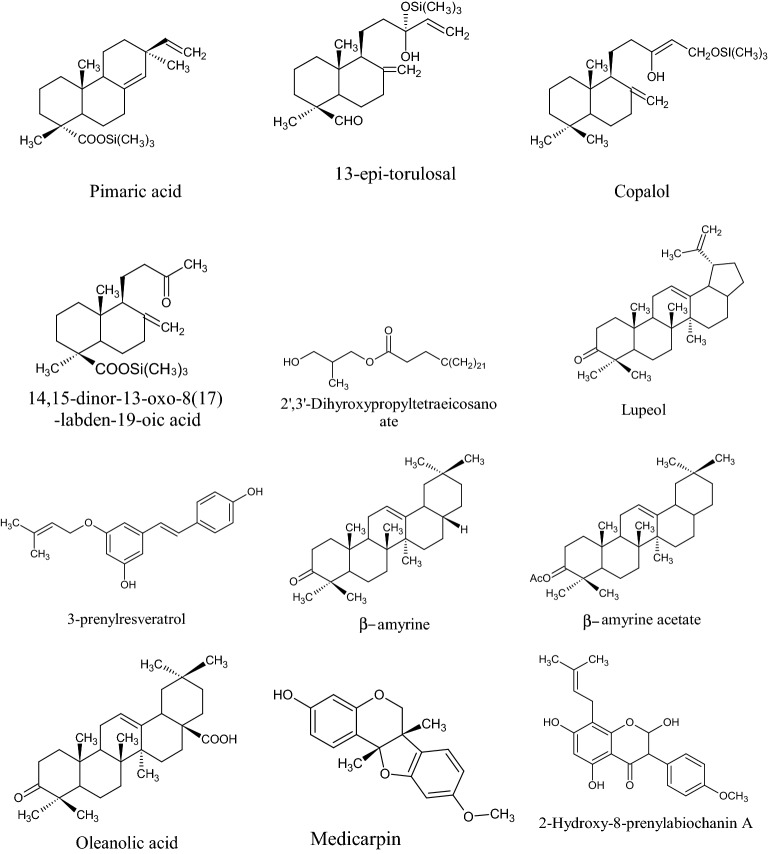
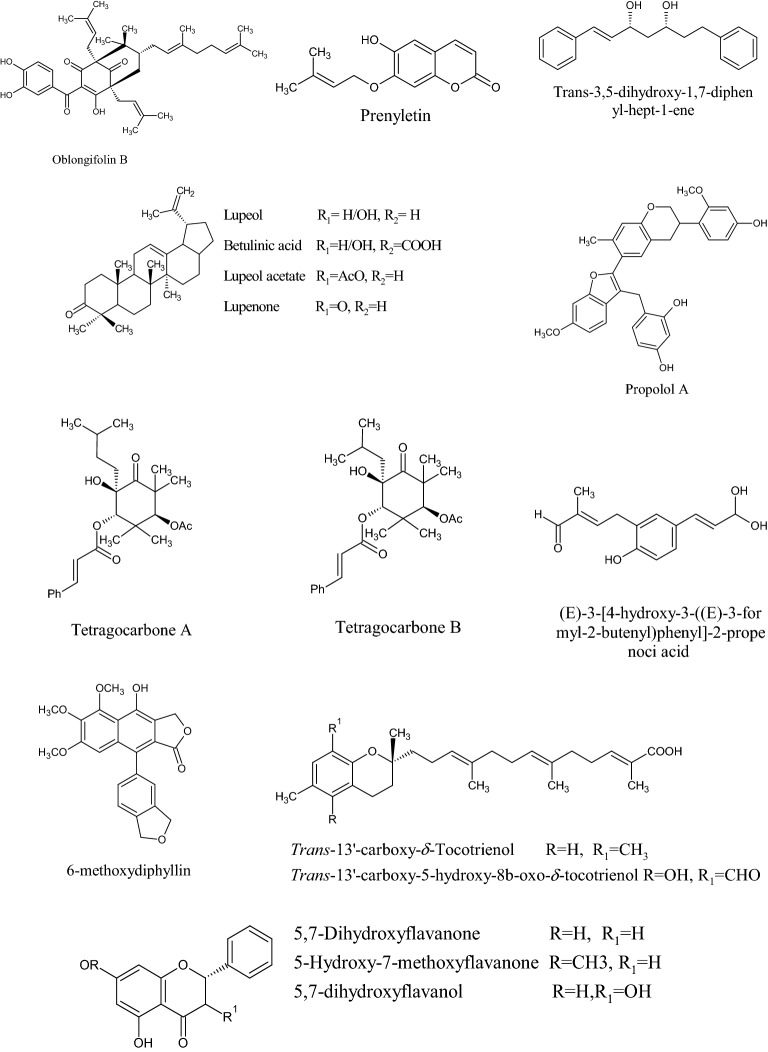
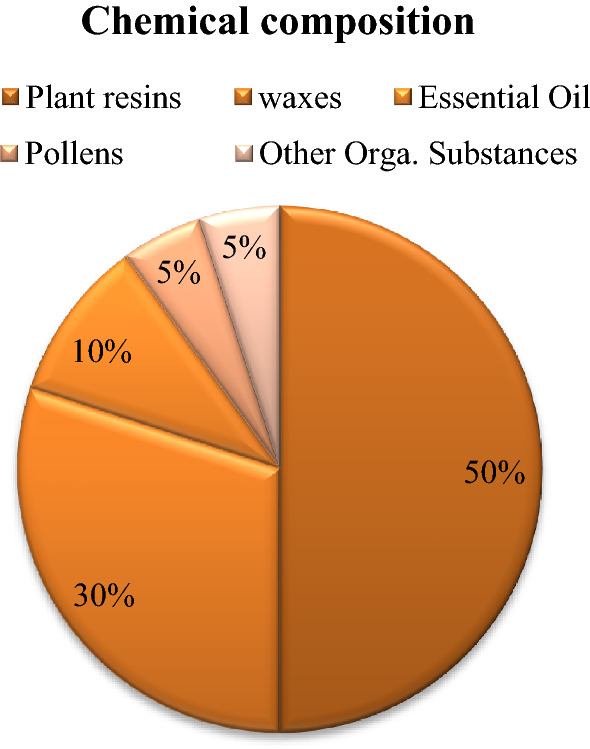
In the Uruguayan and the Chinese [53], however, these hydroflavonoids are present in less than 10%; while in Brazil they make up as much as 50% [49, 54, 55]. In the Chinese and Uruguayan varieties, the predominant flavonoids are substantially flavones and flavonols [53]. Extensive comparisons have been made on the chemical composition between propolis samples from Europe, South America and Asia [49], and from this point of view, it was possible to establish that European and Chinese propolis mainly abound in various species of flavonoids, phenolic acids and relative esters, while the predominant compounds of Brazilian propolis are terpenoids and prenylated derivatives of p-coumaric acid [49, 54, 55], such as artepillin C of Brazilian green propolis from the plant Baccharis dracunculifolia DC, Asteraceae, in southeastern and western-central Brazil [56, 57]. Therefore, there is a considerable difference between propolis originating in tropical areas (South America) with respect to those of temperate areas (Europe). Indeed, the first one is caractherized by substances with a hydroxycinnamic acid nucleus (C6–C3 backbone), whereas in the second one the flavonoid (C6-C3–C6 backbone) composition predominates [49]. In Fig. 2, the 2D structures of the main isolated compounds from propolis were depicted, whereas the main compounds isolated from African, American, Australian and Asian propolis were reported in Tables 2, 3, 4, 5, and 6.
Fig. 2.
Isolated compounds from propolis
Table 2.
Compounds isolated from African propolis
| Country | Compound | Class | References |
|---|---|---|---|
| Cameroon | Lupenone, α-amyrin, β-amyrin, methyl-3β,27-dihydroxycycloart-24-en-26-oate, oleanolic acid, β-amyrin acetate, lupeol, betulinic acid, lupeol acetate, ψ-taraxasterol-acetate, taraxasterol acetate, lanosterol, 3α-hydroxy-olean-12-en-30-ol, α-amyrone, β-acetoxy-amyrin, bacchara12,21dien3β-ol, betulinaldehyde and erythrodiol | Terpenoid | [405, 406] |
| 3-Undecylphenol, 3-tetradecylphenol, 3-pentadecylphenol, 3-hexadecylphenol, 3-heptadecylphenol, 3-nonadecylphenol, 3-((100 z)-pentadecenyl)-phenol, 3-((120 z)-pentadecenyl)-phenol, 3-((80 z)-heptadecenyl)-phenol, 3-((120 z)-heptadecenyl)-phenol, 3-((140 z)-heptadecenyl)-phenol, 3-((130 z)-nonadecenyl)-phenol, 3-((140 z)-nonadecenyl)-phenol, 5-pentadecylresorcinol, 5-hexadecylresorcinol, 5-heptadecylresorcinol, 5-((100 z)-pentadecenyl)-resorcinol, 5-((80 z)-heptadecenyl)-resorcinol, 5-((110 z)-heptadecenyl)-resorcinol, 5-((120 z)-heptadecenyl)-resorcinol, 5-((140 z)-hheptadecenyl)-resorcinol, 5-((140 z)-nonadecenyl)-resorcinol | Phenolic lipids | [407] | |
| Cameroon | α-Terpineol and 1,8-terpineol | Monoterpene alcohols | [406] |
| Ethyl palmitate | Fatty acid ester | ||
| Lonchocarpol a, 6,8-diprenyl-aromadendrin and lespedezaflavanone C | Diprenyl-flavonoids | ||
| Congo | Lupenone, β-amyrin and lupeol | Triterpenes | |
| lonchocarpol A and 6,8-diprenyl-eriodictyol | Diprenyl-flavonoids | ||
| Cameroon | 10-O-Eicosanylglycerol, deperoxidized derivative of plukenetione C | Miscellanous | [405, 408] |
| Egyptian |
2,3-dihydroxy-4-methyl-octanoic acid hexacosanoic acid; 3,4- dimethoxy-cinnamic acid; 3-methyl-3-butenyl-trans-caffeate ester, tectochrysin 5-hydroxy-7-methoxy isoflavone |
[409] | |
| Egyptian | Isonymphaeol C | Prenylated flavonoid | [409] |
| Libya/Nigeria/cameroon | Cycloartanol, mangiferolic acid, mangiferonic acid, ambolic acid, 27-hydroxymangiferonic acid | Cycloartane triterpene | [405] |
| Nigeria | Ambonic acid | [410] | |
| Libya | 13-Epitorulosol, acetylisocupressic acid, agathadiol, isocupressic acid, isoagatholal | Diterpene | [411] |
| Cameroon | 2-Hydroxy-8-prenylbiochanin A | Flavonoid | |
| Libya | Taxifolin-3-acetyl-4′methyl ether | ||
| Nigeria | 3,8-Dihydroxy-9-methoxy-pterocarpan, astrapterocarpan, vesticarpan, vestitol, broussonin B, calycosin, liquiritigenin, pinocembrin, isosativan, 2′-hydroxy-7,4′-dimethoxyisoflavan, medicarpin | Flavonoid | [411] |
| Algeria | Pectolinarigenin; 6,7-dihydroxy-7,4′-dimethoxyflavone (ladanein), acacetin, quercetin, 3-O-methyl-quercetin, kaempferol, chrysin, tectochrysin, galangin, myricetin-3,7,40,50-tetramethyl ether, apigenin, pectolinarigenin, pilosin, ladanein, pinocembrin, pinobanksin, pinobanksin-3-acetate, pinobanksin-3-(E)-caffeate, pinostrobin, genistein, | Flavonoid | [412, 413] |
| (E)-resveratrol, tyrosol | Miscellanous | [413] | |
| pimaric acid, totarol, 18-hydroxy-cis-clerodan-3-en-15-oic acid, cistadiol, isoagathotal, imbricatoloic acid, cupressic acid, isocupressic acid, torulosol, agathadiol, torulosal | Terpenoids | [412, 413] | |
| caffeic acid, prenyl caffeate, methyl caffeate, isopentyl caffeate, 2-methyl-2-butenyl (E)-caffeate, 3-methyl-3-butenyl-(E)-caffeate, phenethyl-(E)-caffeate (CAPE), p-coumaric acid, p-coumaric acid methyl ester, cinnamic acid (isoferulic acid, caftaric acid, caftaric acid methyl ester, ( +)-chicoric acid, ( +)-chicoric acid methyl ester, | Phenylpropanoids | [412–414] | |
| Egypt | Isoferulic acid | Phenylpropanoids | [415] |
| Chrysin, tectochrysin, galangin, pinocembrin, pinostrobin, quercetin-3,7-di-o-methyl ether, 3-methoxy-5,7,40 –trihydroxyflavone, 3,30 -dimethoxy-5,7,40 –trihydroxyflavone, izalpinin, isonymphaeol C, isonymphaeol B, isonymphaeol D, nymphaeol B, | Flavonoids | [409, 415] | |
| 3β-Cycloartenol, 3β-cycloartenol-26-oic acid, 3α-cycloartenol-26-oic acid, β-amyrin acetate, | Terpenoids | [416] | |
| Nigeria | Macarangin, 8-prenylnaringenin, pinocembrin, nymphaeol b, liquiritigenin, calycosin, (3S)-vestitol | Flavonoids | [417] |
| Ambonic acid, mangiferonic acid, α-amyrin | Terpenoids | [405, 410] | |
| Medicarpin, riverinol, gerontoxanthone h, 6-deoxy-γ-mangostin, 1,7-dihydroxy-3-o-(3-methylbut-2-enyl)-8-(3-methylbut-2-enyl) xanthone | Miscellanous | [410] | |
| 8-prenylnaringenin, 6-prenylnaringenin, propolin d, macarangin | Prenylated flavonoid | [405, 410] | |
| Gerontoxanthone H, 6-deoxy-γ-mangostin; 1,7-dihydro-3-o-(3-methylbut-2-enyl)-8(3-methylbut-2-enyl) xanthone | Xanthone | ||
| Libya | 13-Epitorulosal, acetyl-13-epi-cupressic acid, 13-epi-cupressic acid | Diterpenes | [418] |
| Sesamin | Lignin | ||
| Taxifolin-3-acetyl-4′-methyl ether | Flavanonol | ||
| 13-Epitorulosolol | Diterpene | ||
| Demethylpiperitol, 5′-methoxypiperitol | Lignan | ||
| Cycloartanol, mangiferolic acid, mangiferonic acid, ambolic acid, 27-hydroxymangiferonic acid | Cycloartane triterpene | ||
| Cardol | Resorcinol | ||
| Agathadiol, isocupressic acid, isoagatholal, acetylisocupressic acid | Diterpene | ||
| bilobol | |||
| Libya | Demethylpiperitol, 5′-methoxypiperitol | Lignan | [411] |
| Nigeria | Riverinol | Benzofuran | |
| Cameroon | Triacontyl ρ-coumarate | Coumarin | |
| Arachic/arachidic acid ethyl ester (PEN4) | Alkylphenol | ||
| Libya/Cameroon | Cardol | Alkylresorcinol | |
| Cameroon | 1′-O-Eicosanyl glycerol | Acylglycerol | [405] |
| Nigeria | Oleic acid; propyl stearate | Fatty acid and ester | [410] |
| Cameroon | Hexatriacontanoic acid, 2′,3′-dihydroxypropyltetraeicosanoate | Fatty acid | [411] |
| Zambian and Tanzanian | 6(1,1, dimethyl allyl) pinocembrin; 6(1,1, dimethyl allyl) naringenin; 5-hydroxy-4″,4″-dimethyl-5″-methyl-5″-H-dihydrofuranol [2″,3″,6,7] flavanone | Flavanone | [419] |
| Mediterranean | Copalol; 3-epi-manool; communal; 14,15-dinor-13-oxo-8(17)-labden-19-oic acid; pimaric acid; 13-epi-torulosal; communic acid; | Diterpene | [389] |
| Cameroon | 2-Hydroxy-8-prenylabiochanin A, 2’,3’-dihydroxypropyltetraeicosanoate, β-amyrine, oleanolic acid, β-amyrine acetate, lupeol, betulinic acid, lupeol acetate, lupenone | Isoflavonol | [219] |
| Kenya | Tetrahydrojusticidin B, phyllamyricin C, and 6-methoxydiphyllin | Arylnaphtalene lignan | [376] |
| Kenya | Macarangin, schweinfurthin A and B | Geranylated flavonol (geranylstilbenes) | [376] |
| Kenya | Phyllamyricin C, tetrahydrojusticidin B, 6-methoxydiphyllin | Micellanous | [376] |
| Cameroon | (E)-5-(2-(8-hydroxy-2-methyl-2-(4-methylpent-3-en-1-yl)-2H-chromen-6-yl) vinyl)-2-(3-methylbut-2-en-1-yl) benzene-1,3-diol; 5-((E)-3,5-dihydroxystyryl)-3- ((E)-3,7-dimethylocta-2,6-dien-1-yl) benzene-1,2-diol; | Prenylated stilbenes | [408] |
Table 3.
Compounds isolated from American propolis
| Country | Compound | Class | References |
|---|---|---|---|
| Brazil | β-Amyrin, glutinol | Triterpenoid | [420] |
| Bolivia | Cycloart-24-en-3β-ol, cycloart-24-en-3β,26-diol, | ||
| 24(E)-Cycloart-24-en-26-ol-3-one, cycloart-24-en-3-one, lupeol, cycloartenone | Cycloartane triterpene | [421] | |
| Brazil | Liquiritigenin, isoliquiritigenin, formononetin, vestitol, neovestitol, medicarpin, 7-O-neovestitol, 3-O-methylquercetin, 3,6,4′-trimethoxychrysin, 3,6-dimethoxyapigenin, 6-methoxykaempferol, 6-methoxyapigenin, 5,7-dihydroxy-2-(3,4-dihydroxy)-4 h-chromen-4-one, dihydrokaempferide | Flavonoid | [103, 422, 423] |
|
3-O-Methylquercetin, 3,6,4'-trimethoxychrysin, 3,6-dimethoxyapigenin 6-methoxyapigenin, 6-methoxykaempferol |
Flavones | [103] | |
| 3-Prenyl-4-hydroxycinnamic acid, 3,5-diprenyl-4-hydroxycinnamic acid, 2,2-dimethyl-6-carbooxyethyl-2-H-1-benzopyran, 2,2-dimethyl-6-carbooxyethyl-2–8-prenyl-2H-1-benzopyran | Polyphenol | [397] | |
| nemorosone, gambogenone, 7-epi-Nemorosone, 7-epi-clusianone, methylinsigninone, aristophenone, hyperibone B | Polyisoprenylated benzophenones | [95, 424] | |
| [425] | |||
| Propolonones A, propolonones B, propolonones C, propolol A | Flavonoid derived dimer | [102] | |
| (E)-3-[4-Hydroxy-3-((E)-3-formyl-2-butenyl)phenyl]-2- propenoic acid, 3,4-dihydroxy-5-prenyl-(E)-cinnamic acid, capillartemisin A, 2,2-dimethylchromene-6-(E)-propenoic acid | Cinnamic acid derivative | [423] | |
| Chile | 5,7-Dihydroxyflavanone, 5-hydroxy-7-methoxyflavanone, 5,7-dihydroxyflavanol, 5,7-dihydroxyflavone, 5,hydroxy-7-methxyflavone, 3,5,7-trihydroxyflavone | Flavonoid | [426] |
| Colombian | Trans-13’-carboxy-5-hydroxy-8b-oxo-δ-tocotrienol, trans-13’-carboxy-5,6-dioxo-δ-tocotrienol, trans-13’-carboxy-δ-tocotrienol | d-Tocotrienol | [427] |
| Central Chilean Matorral | Prenyletin, trans-3,5-dihydroxy-1,7-diphenyl-hept-1-ene, acacetin, izalpinin, kaempferide | Phenolic | [428] |
| Cuba/ Brazil | Propolone A, propolone B, propolone C, propolone D | Polyisoprenylated Benzophenones/ Flavonoid | [102, 424, 429] |
| Cuba |
Gallic acid, isoliquiritigenin, liquiritigenin, formononetin, biochanin A, (3S)-7,4’-dihydroxy-2’-methoxyisoflavan, 7-O-methylvestitol, (6aS,11aS)-medicarpin,(6aS,11aS)-homopterodicarpin, (6aR,11aR)-vesticarpin,(6aR,11aR)-3,8-dihydroxy-9-methoxypterocarpan, (6aR,11aR)-3-hydroxy-8,9 dimethoxypterocarpan, (6aR,11aR)-3,4-dihydroxy-9-methoxypterocarpan |
Isoflavonoids | [378] |
| Plukenetione A | Polyprenylated acylphloroglucinol | [430] | |
| Mexican |
Pinocenbrin, pinobanksin chrysin, galangin-5-methylether, isorhamnetin, pinobanksin-5-methylether, alpinetin, alpinone, pinostrobin, kaempferide |
Flavonoid | [431] |
| Ecuador | Naringenin, Sakuranetin, Eupatolitin, Rhamnazin | [432] | |
| Chile | Pinocembrin, chrysin | [433] | |
| Bolivia | Kaempferol 3-methyl ether, kaempferol 7-O-methyl ether | [421] | |
| Brazil | 2-Phenoxychromone | Benzopyran derivative | [434] |
| Bolivia | Cinnamic acid | Phenyl propanoid | [421] |
| 3-Prenyl-p-coumaric acid (drupanin) | Coumarin | ||
| Benzyl benzoate | Benzyl ester | ||
| Brazil | Guttiferone E, oblongifolin B | Polyprenylated benzophenone | [434] |
| 2-Phenoxychromone | Flavones | [103] | |
| Chile | (E)-3-Hydroxy-1,7-diphenylhept-1-ene-5-acetate, (E)-5-hydroxy-1,7-diphenylhept-1-ene-3-acetate | Diarylheptanoid | [435] |
Table 4.
Compounds isolated from Australian propolis
| Country | Compound | Class | References |
|---|---|---|---|
| Pitcairn Island | 3-oxo-cycloart-24e-en-21,26-diol-21,26-diacetate, 3-oxo-cycloart-24e-en-21,26-diol, 3-oxo-cycloart-24e-en-21,26-diol-21-acetate, 3-oxo-cycloart-24e-en-21,26-diol-26-acetate, 3-oxo-cycloart-24-en-26-al | Triterpenoid | [436, 437] |
| Australia |
7,8,18-Trihydroxyserrulat-14-ene, 5,18-epoxyserrulat-14-en-7,8-dione, (18RS)-5,18-epoxyserrulat-14-en-8,18-diol |
Diterpene | [12] |
| Pitcairn Island | Abietinal | Diterpene | [436, 437] |
| Fiji Island | Glyasperin | Flavonoid | [438] |
| Kangaroo Island |
(E)-4-(3-Methyl-2-buten-1-yl)-3,4′,5-trihydroxy-3′-methoxystilbene, (E)-2-(3-methyl-2-buten-1-yl)-3,4′,5-trihydroxystilbene (2-prenylresveratrol), (E)-2,4-bis(3-methyl-2-buten-1-yl)-3,3′,4′,5-tetrahydroxystilbene (E)-2-(3-methyl-2-buten-1-yl)-3-(3-methyl-2-butenyloxy)-3′,4′,5-trihydroxystilbene, (E)-2,6-bis(3-methyl-2-buten-1-yl)-3,3′,5,5′-tetrahydroxystilbene (E)-2,6-bis-(3-methyl-2-buten-1-yl)-3,4′,5-trihydroxy-3′-methoxystilbene |
Stilbene | [398, 439, 440] |
| Fiji Islands | Solomonin B, solomonin C | Stilbene | [438] |
| Glyasperin A, kumatakenin, macarangin, mangiferolic acid | Flavonid |
Table 5.
Compound isolated from Asian propolis
| Country | Compounds | Class | Refs. |
|---|---|---|---|
| Indonesia/Vietnam | Mangiferolic acid, cycloartenol, mangferonic acid, ambonic acid, ambolic acid | Cycloartane triterpenoid | [238, 441] |
| Cardol | Alkyresorcinol | [138] | |
| Vietnam |
23-Hydroxyisomangiferolic acid B, 23-hydroxyisomangiferolic acid A, 27-acetoxymangoferolic acid, (5R,8 S,9 S,10 R,13 R,14 S,17 R,20 R)-27-methoxycarbonyloxymangiferonic acid, 27-acetoxymangoferonic acid, lanosterol, cycloartenone, mangiferonic acid, 23-hydroxymangiferonic acid, 27-hydroxymangiferonic acid, (23E)-27-nor-3β-hydroxycycloart-23-en-25-one, (24E)-3βhydroxycycloart-24-en-26-al, 27-hydroxyisomangiferolic acid |
Cycloartane triterpenoid | [442] |
| Thailand/Vietnam | 3-O-Acetyl ursolic acid, ocotillone I, ocotillone II, ursolic aldehyde, oleanolic aldehyde, dipterocarpol, cabralealactone, isocabralealactone | Triterpenoid | [441, 443] |
| Thailand | Methylpinoresinol | Lignan | [443] |
| Malaysia | 20-Hydroxy-24-dammaren-3-one, β-panasinsene | Sesquiterpene | |
| Thailand/Vietnam | α-Mangostin, γ-mangostin, cochinchinone t, β-mangostin, gartanin, 8-deoxygartanin, 9-hydroxycalabaxanthone, mangostanol, mangostanin, garcinone B | Prenylated xanthone | [441, 443] |
| Vietnam | Hydroxyhopanone | Micellanuous | [441] |
| (13E,17E)-polypoda-7,13,17,21-tetraen-3β-ol | |||
| Lisofurvin, | Dihydrochromene | [441] | |
| Dihydrobrasixanthone B, cochichinone A, cochichinone I, cochichinone J, cratoxylumxanthone B, α-mangostanin, pruniflorone S, 2-hydroxyl-6-(14'Z -nonadecenyl) benzoic acid | Xanthone | ||
| Alkenylphenol | [444] |
Table 6.
In vitro antimicrobial effects of some propolis extracts, doses, and studied microorganisms
| Country/Region | Solvent | Dose/Concentration | Microorganism | Effect | References |
|---|---|---|---|---|---|
| Tunisia | Ethanol | 10 μl | Aspergillus flavus, Aspergillus niger, Streptococcus mutans, Penicillium nordicum, Penicillium expansium, Penicillium commune, Lactobacillus plantarum, Escherichia coli | Growth inhibition | [83] |
| Chile | Ethanol | MIC, 256 to 1024 μg/ml | Helicobacter pylori ATCC 43,504, Helicobacter pylori 84C | Growth inhibition | [37] |
| Brazil | Ethanol | MIC 7.44 to 29.76 mg/ml | Streptococcus mutans ATCC 25,175, Streptococcus sanguinis ATCC 10,566, Streptococcus salivarius ATCC 7073, Lactobacillus casei ATCC 393 | Growth inhibition | [93] |
| - | - | 200 μl | Streptococcus mutans ATCC 25,175, Streptococcus sanguinis ATCC 10,566, Candida albicans ATCC 1023 | Growth inhibition | [92] |
| Mexico | Ethanol | MIC 1.62 to 2.50 μg/ml | Candida albicans ATCC 10,231 | Growth inhibition | [46] |
| Turkey | Ethanol–water (8:2) | 0.25, 0.50, 1 mg/well | Streptococcus sanguinis, Streptococcus pyogenes, Streptococcus mutans, Candida albicans | Growth inhibition | [47] |
| Algeria | Ethanol–water | 500 μg/ml | Shewanellaputrefaciens, Photobacterium damselae, Vibrio harveyi | Growth inhibition | [87] |
| India | Chloroform, ethanol, acetone | 5,10,15 mg/ml |
Pseudomonas flurorescens, Pseudomonas citrea, Pseudomonas aeruginosa, Staphylococcus aureus, Escherichia coli, Vibrio cholera, Vibrio parahaemlyticus, Vibrio harveyi, Vibrio fischeri, Bacilliussubstillus |
Growth inhibition | [76] |
| Brazil | Ethanol–Water | 1. 64 to ≥ 1024 μg/ml | Pseudomonas aeruginosa, Staphylococcus aureus, Escherichia coli | Growth inhibition | [445] |
| Russia | Ethanol | 2 μg/ml | Staphylococcus aureus, Escherichia coli | Anti-biofilm | [35] |
| Romania | Ethanol | 10 mg/ml | Paenibacillus larvae | Growth inhibition | [88] |
| Argentina | Ethanol | MIC, 4.7 to 152 g GAE/ml | Erwinia carotovorasppcarotovora CECT 225, Pseudomonas syringaepvar tomato CECT 126, Pseudomonas corrugata CECT 124, Xanthomonas campestris pvarvesicatoria CECT 792 | Growth inhibition | [86] |
| Korea | Ethanol | 0.036 to 2.3 mg/ml | Bacillius cereus, Listeria monocytogenes, Staphylococcus aureus, Pseudomonas fluorescence | Growth inhibition | [84] |
| Brazil | Ethanol | 0.69 to 42.8 mg/ml | Staphylococcus aureus, Staphylococcus intermedius, Malassezia pachydermatis | Growth inhibition | [251] |
| Turkey | Ethanol | MIC, 4 to 512 mg/ml | Peptostreptococcusanaerobius, Peptostreptococcus micros, Lactobacillus acidophilus, Actinomyces naeslundii, Prevotellaoralis, Prevotellamelaninogenica, Porphyromonasgingivalis, Fusobacterium nucleatum, Veillonellaparvula | Growth inhibition | [38] |
| Brazil | Ethanol | 0.4 to 0.5 mg | Staphylococcus aureus 209, Escherichia coli, Candida albicans 562 | Growth inhibition | [446] |
Propolis from Egypt reported to possess constituent of P. nigra and esters of caffeic acid and long-chain fatty alcohols including tetradecanol, hexadecanol and dodecanol [9]. Cuban propolis is mainly from Clusia rosea Jacq. and contains polyisoprenylated benzophenone which is distinct from both European and Brazilian propolis [2, 9]. Birch propolis from Russia contained flavonols and flavones from Betula pendula Roth. Anjum et al. [4].
Analytical techniques
Each propolis type is characterized by the specific proportion of the dominant plant material. Various chromatographic techniques were used for evaluation of the botanical origin of propolis samples such as high performance thin-layer chromatography [58], high-performance liquid chromatography (HPLC) [59–61], gas chromatography-mass spectrometry (GC–MS) [62], capillary electrophoresis [63], microscopic techniques [64]. Furthermore, structure elucidation techniques such as direct analysis in real time (DART) mass spectrometry [52], nuclear magnetic resonance (NMR) [65], and infrared spectroscopy (IR) [66] have been applied to screen compositional differences between propolis samples supplied from various origins.
Using high-performance thin-layer chromatographic (HPTLC) fingerprinting analyses to explore the chemical composition of propolis, studies have confirmed the existence of two different subtypes of European propolis, as orange and blue types (O-type and B-type), originating from P. nigra and Populus tremulas L., respectively. Green type (G-type) propolis is distinguished by its mixture of light orange, dark green, and blue bands. O-type propolis is characterized by quercetin, while B-type corresponds mostly to galangin, caffeic acid, feruloyl, and p-coumaroyl derivatives. G-type corresponds to apigenin or naringenin. For instances, HPTLC profiles of plant resins as potential botanical sources of propolis, were compared with profiles of Turkish propolis extracts [58]. Based on phenolics fingerprint, O-type of Turkish propolis showed similarity with P. nigra buds, while B-type has similar HPTLC pattern with P. tremula bud.
Recently, a reversed-phase HPLC-ESI-TOF–MS analysis of an ethyl acetate extract of propolis prepared from Apis mellifera beehives using liquid–liquid extraction was described. Two flavonoids, galangin and apigenin, were identified as the major constituents present in this bee glue, which were responsabible for the inhibitory activity in head and neck squamous cell carcinoma on the key enzymes matrix metalloprotease (MMP)-2 and MMP-9 that destroyed the basement membrane and degrade the extracellular matrix, leading to tumor invasion Niyomtham et al. [59].
Pharmacological activities
Antioxidant activity
The screening of the biological activity of bee products has attracted considerable attention due to their health benefits. Bee products including propolis, are considered to be a potential source of naturally occurring antioxidant and antimicrobials [67–72].
Several antioxidant tests such as 2,2-diphenyl-1-picrylhydrazyl (DPPH), trolox equivalent antioxidant capacity (TEAC), ferric reducing antioxidant power (FRAP), iron-chelating activity (ferrozine assay), cupric ions reducing antioxidant power (CUPRAC), hydroxyl radical scavenging ability, lipid peroxidation inhibition, N,N-dimethyl-p-phenylenediamine (DMPD), O2 scavenging ability, H2O2 scavenging ability, β-carotene bleaching, superoxide anion radical scavenging ability have been used to evaluate the in vitro antioxidant activity of propolis [43, 67, 73]. These tests have different mechanisms, reaction environments, principles, charged radicals, and use difference reference compounds. Therefore, the antioxidant ability of natural compounds is generally evaluated with at least two or more antioxidant methods. Besides this, the phenolic content and composition of natural products is determined and correlated with the antioxidant capability in order to validate the obtained results [42, 74].
The extraction method greatly influences the type and quantity of bioactive compounds, because their solubility also depends on the solvent type and polarity [75, 76]. The antioxidant efficacy of propolis extracts (ethanol and water) as well as that of its fractions has been already reported in several studies [7, 43, 67, 77]. Ahn et al. [67] evaluated the antioxidant activity of ethanol extracts of propolis from various Chinese areas using the DPPH, TEAC and β-carotene bleaching assays. Chinese propolis extracts showed strong antioxidant activity with a positive correlation with the high total phenols content, such as flavonoids and phenolic acid esters, identified by HPLC coupled with a photodiode array (PDA) and mass spectrometry (MS) detection [60]. There are many other reports concerning the antioxidant potential of ethanol extract of propolis [44, 78, 79]. In addition, there are also some reports about the antioxidant capacity of water extracts of propolis [7]. The antioxidant activity of a water extract of propolis from Brazil was evaluated using the superoxide scavenging ability assay, the DPPH assay, and the hydroxyl radical scavenging abilit assay. The extract showed the best free-radical scavenging ability against superoxide anion radical and hydroxyl radical at 50 and 100 µg/ml, respectively. Similarly, in the study of Gülçin et al. [43], who investigated the in vitro antioxidant activity of a water extract of propolis from Erzurum province of Turkey by using FRAP, CUPRAC, iron-chelating activity, H2O2 and O2 sscavenging ability as well as DPPH and TEAC assays, the water extract showed an interesting antioxidant profile. The aqueous extract was analyzed by HPLC and LC–MS/MS reporting a large number of antioxidative compounds such as caffeic acid, ferulic acid, syringic acid, ellagic acid, quercetin, α-tocopherol, pyrogallol, p-hydroxy benzoic acid, vanillin, p-coumaric acid, gallic acid, and ascorbic acid [43]. In the study conducted by Aldemir et al. [80], the effect of different solvents (ethanol, water and polyethylene glycol) on the antioxidant activity of propolis was determined using TEAC and FRAP methods. However, they did not find any statistically significant differences in the antioxidant activity between the different propolis extracts. In another study, propolis extracts from different regions of Korea were evaluated and compared to extracts obtained from Brazilian propolis [79]. Korea propolis extracts, which contained the highest total phenols and flavonoids content, showed the highest antioxidant activity in the linoleic peroxidation and DPPH assays. Flavonoids present in propolis play a crucial role in photoaging and psoriasis [81].
Hochheim et al. [77] examined the antioxidant activity of methanol, water, 70% ethanol, dichloromethane, ethyl acetate and butanol extract fractions in native Brazilian bee Melipona quadrifasciata propolis. The authors found that the aqueous extract showed the best antioxidant potential, followed by methanol extract. Moreover, the methanol extract showed the highest radical scavenging capacity in the DPPH assay with an IC50 value of 151.37 ± 7.9 μg/ml followed by ethyl acetate (IC50 = 311.47 ± 8.2 μg/ml), dichloromethane (IC50 = 489.8 ± 0.0 μg/ml), and butanol (IC50 = 588.8 ± 0.0 μg/ml) fractions. In addition, crude extracts and fractions showed different activity in the lipid peroxidation assay. Ethyl acetate fraction [64.93 ± 0.6 mg gallic acid equivalent (GAE)/g], showed the highest total phenols content followed by methanol extract (57.53 ± 0.2 mg GAE/g), aqueous extract (11.96 ± 1.5 mg GAE/g), dichloromethane fraction (8.10 ± 0.3 mg GAE/g), hydroalcoholic extract (4.87 ± 0.2 mg GAE/g), and was not observed in butanol fraction. On the contrary, the highest content of flavonoids was detected in the methanol extract [8.48 ± 0.3 mg quercetin equivalents (QUE)/g], followed by ethyl acetate fraction (4.23 ± 0.5 mg QUE/g), hydroalcoholic extract (3.99 ± 0.4 mg QUE/g), aqueous extract (3.67 ± 0.3 mg QUE/g), dichloromethane fraction (2.20 ± 0.3 mg QUE/g), and butanol fraction (0.78 ± 0.2 mg QUE/g).
In another study, twelve propolis samples from Greece, Greek island, and east Cyprus were analyzed for their antioxidant activity, as well as chemical composition [42]. The propolis ethanol extracts possessed potent DPPH scavenging activities from 0.33 to 1.11 mmol trolox equivalents (TE)/g extract and reducing power ability from 2.14 to 3.35 mmol ascorbic acid equivalent (AAE)/g. The antioxidant activity of propolis samples correlated with total phenol content as well as with the amount of the main identified compounds such as phenolic acids and their esters, anthraquinones, flavonoids and terpenes. Kumazawa et al. [74] performed an extensive study investigating the antioxidant potential of propolis collected from Argentina, Australia, Brazil, Bulgaria, Chile, China, Hungary, New Zealand, South Africa, Thailand, Ukraine, Uruguay, United States and Uzbekistan by using β-carotene bleaching and DPPH assays. HPLC–PDA and LC–MS analysis were also used to identify the major constituents of their ethanol extracts. All the propolis extracts exhibited significant free-radical scavenging activity against DPPH radical and inhibitory effects on β-carotene-bleaching, mainly attributable to the phenolic acids and flavonoids content. Regarding this, Lee et al. [68] isolated ten phenylpropanoic acid esters from ethanol extracts of Korean propolis. The antioxidant potential of these compounds, specifically caffeic acid phenethyl ester, caffeic acid benzyl ester, caffeic acid ethyl ester, ferulic acid benzyl ester, ferulic acid 3′,3′-dimethylallyl ester, 3,4-dimethoxycaffeic acid cinnamyl ester, coumaric acid cinnamyl ester, coumaric acid benzyl ester, cinnamic acid phenethyl ester, and cinnamic acid cinnamyl ester, were investigated by DPPH and ABTS assays. Among the tested compounds, caffeic acid phenethyl ester (CAPE), caffeic acid benzyl ester, and caffeic acid ethyl ester exhibited significant activity, ferulic acid benzyl ester, ferulic acid 3′,3′-dimethylallyl ester had moderate activity, and the other compounds did not show any activity. Russo et al. [71] reported that the antoxidant activity of the propolis extract is mainly ascribable to CAPE and galangin. In particular, the results showed that propolis extract (with and without CAPE), galangin and CAPE exhibited a dose-dependent antioxidant activity. Moreover, CAPE possessed a higher antioxidant activity with respect to galangin. On the contrary, regarding Portugal propolis, the collected in Bornes region showed the higest antioxidant capacity with the following IC50 values than the propolis from Fundão region [82]. The values varied between IC50 = 6.22 μg/ml (Bornes) and IC50 = 52.00 μg/ml (Fundão) in DPPH assay, and IC50 = 9.00 μg/ml (Bornes) and IC50 = 55.00 μg/ml (Fundão) in CUPRAC assay. Moreover, the results obtained showed a positive correlation with the phenolic content of propolis extracts.
Ozdal et al. [36] determined the antioxidant activity of propolis collected in 11 different geographical areas of Turkey by using DPPH and CUPRAC methods. Moreover, the bioaccessibility of propolis samples in terms of total antioxidant capacity of propolis extracts after in vitro simulated gastrointestinal digestion was evaluated. The antioxidant capacity of samples recorded by DPPH method ranging from 1370.6 ± 198 mg trolox equivalents (TE)/100 g and 6332.9 ± 114 mg TE/100 g, whereas in CUPRAC assay the antioxidant capacity ranging from 2461.6 ± 278 mg TE/100 g and 8580.3 ± 234 mg TE/100 g. Moreover, for most samples, the antioxidant capacity of propolis recorded by both methods increased after in vitro gastrointestinal digestion from oral to intestinal phase.
Despite the litle information available in literature, the content of bioactive compounds in propolis may be different in relation to the seasonal collection. The antioxidant ability of propolis collected in three different regions of Algarve in winter and spring (Serra do Algarve, Transição and Barrocal) as well as in South Portugal (Bornes and Fundão regions) were evaluated by using DPPH, TEAC, superoxide anion radical and metal-chelating activity assays [73]. Samples collected in winter showed the highest free-radical scavenging activity in DPPH assay (IC50 = 0.027–0.031 mg/ml) whereas samples collected in spring showed the highest metal-chelating activity. Moreover, propolis samples collected in Barrocal region possessed the higher radical scavenging capacity with respect to Serra do Algarve and Transição regions, without any correlation between seasonal variation and antioxidant assays.
Considering all these results, it is possible to affirm that the antioxidant activity of propolis is certainly correlated with its phytochemical profile, which can vary not only according to the pedoclimatic characteristics of the territory but also according to the harvest season. In any case, certainly, propolis has shown a strong antioxidant activity which supports its use as a replacement for many synthetic antioxidant agents such as butylatedhydroxyanisole, butylatedhydroxytoluene, and tertiary butyl hydroquinone.
Antimicrobial activity
Propolis is also increasingly recognized for its antimicrobial (antibacterial/antifungal) properties. The antimicrobial efficiency of propolis mainly depends on its broad chemical diversity, extraction methods, applied concentration, collected season, region, and bee species. However, despite this variability, propolis maintained its functional properties [46, 75, 76, 83]. Because it contains many bioactive compounds, propolis possesses antibacterial and antifungal activity on a board range of microorganisms. Propolis extract was effective specifically on various foodborne pathogens [84], agricultural bacterial pathogens [85], phytopathogenic bacteria [86], marine opportunistic pathogenic bacteria [87] other than honeybee pathogens [88]. The antibacterial effects of propolis samples collected in different countries/regions around the word have been investigated by several studies grouped in Table 1. The antibacterial properties, either bactericidal or bacteriostatic, highlighted by in vitro studies, depends on concentration, treatment time, and bacterial mode of action [84], although the mechanism is often unknown. Propolis acts either by directly interacting with the microbial cells or by stimulating the immune system of the host cells [89]. The hypothesized mechanisms include the inhibition of bacterial adherence and division, decrease of bacterial mobility, disturbance of membrane potential, and increase in cell membrane permeability [47, 90]. These biological activities are strictly related to the presence of phenolic acids, flavonoids, terpene esters, chalcones, dihydrochalcones, terpenoids, aliphatic acids and esters, aromatic compounds, and metals [35]. As mentioned before, several factors play a key role on the propolis activity, being one of this the extraction method. For example, Gargouri et al. [83] demonstrated that ultrasonic extraction method increased notably the biological activity of the propolis extract with respect to the conventional liquid–liquid extraction method. Concerning the effect of the extraction method used, a study was conducted to evaluate different extraction solvents [75]. In particular, the antimicrobial efficacy of polyethylene glycol (PEG) 400, water, olive oil and the combination of them was investigated against Staphylococcus aureus ATCC 25,923, Escherichia coli 25,922, Pseudomonas aeruginosa ATCC 27,853, Klebsiella pneumoniae ATCC 33,499, Bacillus cereus ATCC 8035, Candida albicans ATCC 60,193. Among them, PEG/olive oil/water, PEG/water, showed similar or a higher significant inhibition in comparison with the hydroalcholic extract. From phytochemical point of view, caffeic acid, trans-p-cumaric acid, and galangin were determined in all extracts under investigations, whereas naringenin, kaempferol, and galangin were determined in PEG/olive oil/water and hydroalcholic extracts. Selvaraj et al. [76] demonstrated the effect of different solvents (ethanol, chloroform, and acetone) on the propolis antibacterial activity. The ethanol extract, in particular, was found to be the most effective against microbial growth.
Moreover, the propolis composition varies also between bee species, which can modify its antimicrobial capacity. Ramón-Sierra et al. [46] reported the antifungal activity of ethanol extracts of propolis obtained from two different bee species (Apis mellifera and Melipona beecheii) against C. albicans ATCC 10,231. According to their findings, M. beecheii propolis extract showed a lower MIC with respect to the A. mellifera propolis extract. Furthermore, Campos et al. [91] reported that propolis ethanol extract of Melipona orbignyi (Hymenoptera, Apidae), very rich in aromatic acids, phenolic compounds, alcohols, terpenes, and sugars, is effective against Staphylococcus aureus and C. albicans.
The antibacterial activity of the various propolis samples also varied according to the collection region. Ristivojević et al. [47] compared the antimicrobial activity of forty-eight propolis ethanol extract from various Turkey regions against Streptococcus sanguinis, Streptococcus pyogenes, Streptococcus mutans, C. albicans as well as examined the phytochemical composition and antioxidant activity. They concluded that the samples with strongest antimicrobial activity contain the highest total phenols, total flavonoid as well as cinnamic, ferulic, caffeic, chlorogenic, and p-coumaric acid content. Similarly, the antimicrobial activity of propolis extracts from different regions of Korea was evaluated and compared to Brazil propolis [79]. Korea and Brazil propolis extracts showed high antimicrobial activity against S. aureus, Bacillus subtilis, Salmonella Typhimurium and C. Albicans, whereas they did not show any activity against P. aeruginosa. The Yeosu and Cheorwon extracts showed higher antibacterial activity with respect to Yangpyeong, mainly related to their higher total phenols and flavonoid contents. Ambi et al. [35] hypothesized that metals may be involved in the antimicrobial properties of Russian propolis, by testing a crude ethanol extract and a metal-free ethanol extract against S. aureus and E. coli biofilm formation. The crude ethanol extract was more active than the metal-free ethanol extract on biofilm formation. However, at the same concentration, increasing the time exposure to 40 h, both extracts completely inhibit the S. aureus and E. coli biofilms. Several studies have been carried out also about the antimicrobial properties of propolis gainst oral cavities infections. Its efficacy was tested against several oral microorganisms such as S. mutans ATCC 25,175, S. sanguinis ATCC 10,566, C. albicans ATCC 1023 and Lactobacillus casei ATCC 393 [92, 93]. Propolis showed a good inhibitory activity on all oral pathogens, paving the way to an alternative application of this natura product to mouthwashes and toothpastes. From these studies, it can be highlighted that propolis antimicrobial potential varied according to its chemical composition. However, among extraction methods, solvent type and bee species, it may be concluded that floral diversity is the most responsible for the bioactivity of propolis.
Anticancer activity
In vitro studies
Cytotoxic, antioxidant and apoptotic effects
Cytotoxic and apoptotic effects have been described for propolis and correlacted with its capacity to improve the antioxidant capacity in various disease states [94]. Castro et al. [95] isolated prenylated benzophenone and isoprenylated benzophenone from Brazilian propolis in order to evaluate their cytotoxic effects. They carried out an in vitro study using HeLa cervical cancer cells and they found that the both compounds exhibited good cytotoxic effects at 0.18 µM concentration [95]. A study by Vukovic et al. [96] reported antioxidant, cytotoxic and pro-apoptotic activities of flavonoids derived from propolis in colon (HCT-116) and breast (MDA-MB-231) cancer cell lines at 115.68 μM, 114.75 μM, 66.86 μM, and 50 μM concentrations [96]. Flavones from Mexican propolis at 4.6 μM concentration significantly triggered apoptosis-like morphological changes/cytotoxic effects in PANC-1 human pancreatic cell line [97]. Additionally, in a recent study, Rivero-Cruz et al. [98] revealed the cytotoxic activity of an ethanol extract of propolis (92.2 µg/ml) in glioblastoma cells cancer line. Another study by Alday et al. [99] evaluated the antiproliferative activity by using the flavoinds and derived esters isolated from propolis at various concentrations (49.1 µM; 52.1 µM; 67.0 µM; 49.9 µM; 51.3 µM; 76.6 µM) in B-cell lymphoma cell line. All the isolated compounds exhibited the antiproliferative activity through apoptotic induction [99]. The ethanolic extract of Turkish propolis at 76.9 ± 2.9 µg/ml concentration showed cytotoxic activity in human normal foreskin fibroblast cells at 31.7 ± 0.26 µg/ml concentration arresting the cell cycle in G1 phase, inducing endoplasmic reticulum stress, caspase activity, and apoptosis and reducing mitochondrial membrane potential in Human adenocarcinomic alveolar basal epithelial (A549) cancer cell line [100]. In another study, the ethanol extract of polish propolis displayed anti-proliferative and pro-apoptotic effect at 100 µM concentration on HCT 116 colon cancer and Me45 malignant melanoma cells [101].
In a recent study, Banzato et al. [102] isolated rare flavanoid dimers, propolones A−D, with a 3-{3-[(2- phenylbenzofuran-3-yl)methyl]phenyl}chromane skeleton, and propolonones A−C, with a 3-[3-(3-benzylbenzofuran-2-yl)phenyl]-chromane skeleton, as constituents of Brazilian red propolis by cytotoxicity-guided assays. Results of the chiral-phase HPLC analysis of these propolis dimers confirmed that they represented scalemic mixtures in which the (+)-enantiomers predominate. The bees that produce this type of red propolis feed on Dalbergia ecastophyllum (L.) Taub. Propolone B and propolonone A display significant cytotoxic activities against an ovarian cancer cell line expressing a multiple drug resistance phenotype when compared with doxorubicin. They reported that the isolated compounds at 19.1 ± 2.4 µM and 29.9 ± 3.4 µM concentration exhibited suitable anti-proliferative activity in ovarian cancer cell line [102].
Mitsui et al. [103] also isolated flavones from Brazilian propolis and performed an in vitro study to evaluate the activity of these isolated compounds. They reported that 3-methoxy-flavones, such as 3-O-methylquercetin (MCF-7: IC50 16.2 μM), 3,6-dimethoxyapigenin (MCF-7: IC50 31.0 μM), and 3,6,4’-trimethoxychrysin (MCF-7: IC50 17.1 μM), exhibited anti-proliferative effect and inhibited cell growth in DLD-1 (human colorectal adenocarcinoma), MCF-7 (human breast cancer), and A549 (human lung cancer) cancer cell lines. Interestengly, the novel 5,7-dihydroxy-2-[3,4-dihydroxyphenoxy-4H-chromen-4-one] also displayed an anti-proliferative effect on cancer cells (MCF-7: IC50 65.8 μM).
The extract of Sonoran Desert propolis at 22.4 ± 1.3 μM concentration displayed suitable antiproliferative activity against cancerous cell line M12.C3.F6 (murine B cell lymphoma). The antiproliferative activity through apoptosis induction was exhibited by pinobanksin and its ester derivatives, pinobanksin-3-O-propanoate, pinobanksin-3-O-butyrate, and pinobanksin-3-O-pentanoate [104]. Moreover, Catchpole et al. [105] evaluated the antiproliferative activity of a commercial New Zealand propolis tincture (Bio30™) reporting that the extract at 200 μg/ml concentration exerted suitable antiproliferative activity in DLD-1 cells and anti-inflammatory potential (TNF-α, COX-1, COX-2). Phenolic compounds were responsible for these activities. New Zealand wax-free Bio30™ propolis tincture solids had very high levels of the dihydroflavonoids pinocembrin and pinobanksin-3-O-acetate, and high levels of the dimethylallyl, benzyl and 3-methyl-3-butenyl caffeates relative to CAPE (caffeic acid phenethyl ester). Another study by Asgharpour et al. [106], described the capability of Iranian propolis to inhibit the proliferation of cancer cells. They isolated flavonoids and then, performed the in vitro test using various concentrations. The isolated compounds inhibited cancer cell proliferation at 40 ± 8.9 μM and 195 ± 14.9 μM concentrations, respectively in mouth epidermoid carcinoma (KB) cell line and, at 98 μM, and 195 μM concentrations, in skin squamous cell carcinoma (A431) cell line [106]. The ethanol extract of propolis from stingless bees Tetragonisca fiebrigi induced cell death by necrosis at 250 and 500 μg/mL concentrations against K562 erythroleukemia cells [107]. Santos et al. [108] reported that the extract of Brazilian red propolis exerted antitumor activity at 75.15 ± 3.35, and 70.81 ± 4.18 concentrations, respectively in diverse colon cancer cell lines.
In another study, Assumpcao et al. [109] described that the p-coumaric acid derived from propolis displayed cytotoxic activity at 17.02, 13.94, 22.85, and 23.55 µM concentrations, respectively against triple-negative breast cancer cell lines. Besides, the ethanol extract of propolis inhibited the growth and proliferation of AGS human gastric cancer cells in a concentration range from 15 to 60 µg/ml [110]. In addition, the ethanol extract of propolis displayed significant cytotoxic activity and induced apoptosis at 50 and 100 μg/ml concentrations in human breast cancer and colon adenocarcinoma cell lines [111]. Khacha-ananda et al. [112] reported that the ethanol extract of propolis exerted cytotoxic and antiproliferative activity at a concentration of 80.96 μg/ml in HeLa cells. A study by Ishihara et al. [113] demonstrated the effects of the ethanol extract of Chinese and Brazilian propolis using different concentrations in vitro. They found that the extract at concentration > 50 μg/ml, 38 μg/ml, and 20 μg/ml induced apoptosis via growth inhibitory activity in human colon carcinoma cell lines [113]. Turan et al. [114] utilized the ethanol extract of Turkish propolis to examine the cytotoxic activity. They reported that the propolis extract at 20.7 ± 3.4 μg/ml concentration showed the highest cytotoxic activity against PC-3 cell line preventing the proliferation of cancer cells [114]. It has been reported that propolis displayed suitable cytotoxic activity at 25 and 50 μg/ml concentrations in human tongue squamous cell carcinoma cell line [115]. Besides, Lee et al. [116] described that propolis inhibited the proliferation of cells at 10 μg/ml in human rectal and colon cancer cell. Another study by Markiewicz-Żukowska et al. [117] reported that propolis reduced the growth of U87MG glioblastoma cell via nuclear factor kappa B (NF-κB) pathway at concentration ranging from 10 to100 μg/ml.
Bhargava et al. [118] stated that the isolated artepillin C from Brazilian green propolis abrogated mortalin-p53 complex, causing the activation of p53 and the growth arrest of cancer cells at 275 µM concentration in HT1080 (fibrosarcoma), A549 (lung carcinoma) and U2OS (osteosarcoma) human cell lines. In another study, Ishida et al. [119] examined the effects of isolated caffeic acid phenethyl ester from propolis on human cancer cells, SKOV3 (ovarian carcinoma), HT1080 (fibrosarcoma), A549 (lung carcinoma), HeLa (cervical carcinoma), U2OS (osteosarcoma), MCF7 and MDA-MB-231 (breast adenocarcinoma), reporting that this compound displayed suitable anticancer activity at 50 µM. A recent study by Mohamed et al. [120] reported that the ethanol extract of propolis significantly inhibited the proliferation of MCF7 cells cells at 62.24 μg/ml. Utispan et al. [121] reported that the propolis extract exerted cytotoxic activity and inhibited the proliferation of metastatic cells at 76.33 ± 1.24 µg/ml concentration in head and neck squamous cell carcinoma (HNSCC) cell lines. In a study, propolis at a concentration of 0.38 mg/mL reduced the viability of K562 erythroleukemia tumour cell line [122]. Sun et al. [123] stated that the chyrsin from propolis suppressed MDA-MB-231 breast cancer cell growth at 40 μM and 60 μM concentrations. In another study, Mutallip et al. [124] isolated pinobanksin-3-acetate from propolis, which inhibited the human colon cancer cell proliferation and induced apoptosis through up-regulation and down-regulation of multiple genes at 163.61 μg/ml concentration. Motomura et al. [125] stated that the methanol extract of propolis induced the cell cycle arrest and apoptosis in HML cells U937 at 300–500 μg/ml. It has been reported that the Brazilian red propolis produced apoptosis-like cell death and alleviated migration potential in carcinoma BCL-5637 cell line at 25, 50 and 100 μg/ml [126]. High-resolution direct-infusion mass spectrometry (HR-DIMS) was used for chemical characterization of the red propolis extract. The main components were dereplicated as follows: m/z 257.0764 (liquiritigenin); 269.0769 (formononetin); 271.0921 (medicarpin); 285.0718 (biochanin A); 523.1641 (retusapurpurin B). Exact mass, fragmentation pathway, and isotopic ratio were used for confirmation. Salim et al. [127] demonstrated that the ethanol extract of Egyptian propolis revealed antioxidant and antitumoral activities at 38.48 μg/ml in prostate cancer cell lines [127]. In addition, the ethanol extract of Brazilian green propolis induced apoptosis in human lung carcinoma cell line at 17.29 μg/ml [128]. Sulaiman et al. [129] experimented the effects of Iraq propolis demonstrating that its extract exhibited suitable anti-tumor activity against HL-60 and HCT-116 cell lines at 25 μg/ml.
Kamiya et al. [130] evaluated the effects of ethanol propolis extract. They observed that the extract at 10 and 20 μg/ml induced apoptosis in MCF-7 cells [130]. Frión-Herrera et al. [131] demonstrated the cytotoxic effect of ethanol propolis extract on HEp-2 human laryngeal carcinoma cell. They reported that propolis extract at 14 and 16 μg/ml displayed cytotoxic effect and induced apoptosis [131]. Motomura et al. [125] reported that the methanol propolis extract at 100, 300 and 500 μg/ml arrested the cell cycle and induced apoptosis in human leukemic U937 cells. Xuan et al. [132] stated that the ethanol extract of Chinese propolis displayed antitumoral activity against breast cancer lines MCF-7 and MDAMB-231 at 50, 100 and 200 μg/ml. Besides, the ethanol extract of Thai propolis averted the proliferation of cancer cell via apoptosis in HeLa cell line at 125 μg/mL and 250 μg/ml [133]. Czyżewska et al. [115] described that the ethanol propolis extract exerted pro-apoptotic activity against human tongue carcinoma cell line (CAL-27) at a dose of 200 μg/ml. Moreover, Vatansever et al. [134], in another study, stated that the ethanol extract of Turkish propolis induced apoptosis in MCF-7 cells at 63, 125 and 250 μg/ml via activating caspases. The ethanol extract of Brazilian propolis generated apoptosis in MCF-7 cells at 20 μg/ml [130]. It has been reported that the Brazilian propolis produced apoptosis through ROS generation in HEp-2 human laryngeal carcinoma cell at a dose of 80 μg/ml [135]. Demir et al. [100] used the ethanol extract of Turkish propolis to examine the antiproliferative and pro-apoptotic activity. They found that the propolis extract was able to alleviate mitochondrial membrane potential and enhance caspase activity in A549 cells at a concentration of 35 μg/ml [100]. Szliszka et al. [136, 137] reported that the ethanolic extract of Brazilian and Polish propolis induced apoptosis via upregulation of tumor necrosis factor-related apoptosis-inducing ligand receptor 2 (TRAIL-R2) in LNCaP prostate cancer cells at 25–50 μg/ml [136, 137]. Cardol or 5-pentadecyl resorcinol, a compound isolated from Trigona incisa stingless bee propolis, displayed significant antiproliferative effect, alleviated mitochondrial membrane potential, and induced apoptosis at 4.51 ± 0.76 μM concentration in SW620 human colorectal cancer cell line. Members of the Anarcadiaceae plant family are the source for this compound [138].
Anti-angiogeninic properties
Kunimasa et al. [139] demonstrated that the Brazilian propolis reduced angiogenesis by inducing apoptosis in human umbilical vein endothelial cells (HUVECs) at 6.25–25 μg/ml concentration. Another study by Park et al. [140] stated that the Brazilian propolis inhibited angiogenesis by preventing phosphatidylcholine-hydrolysing phospholipase C (PC-PLC) activity, p53 and ROS levels in HUVECs at 6.25–25 μg/ml concentration. The Korean propolis at 3.13–25 μg/ml concentrations suppressed angiogenesis through the inhibition of tube formation and proliferation, decreasing the number of newly formed vessels in HUVECs [141]. Moreover, Meneghelli et al. [142] reported that the ethanol propolis extract at 100–200 μg/ml concentration averted the tube-like structure formation (tubulogenesis) in HUVECs.
Cell migration
Red propolis induced an apoptosis-like cell death and attenuated cell migration in carcinoma BCL-5637 cell line at 25 and 50 μg/ml [126]. Xuan et al. [132], in in vitro studies, found that the green extract of propolis significantly alleviated the cells migration in breast cancer line MDA-MB-231 at 100 and 200 μg/ml. In another experimentation, Borawska et al. [143] revealed that the green propolis inhibited cells migration in glioblastoma multiforme cell line U87MG at 30 μg/ml. Finally, Taira et al. [144] evaluated the effects of ethanol propolis extract supplied by the Okinawa Yoho Bee-farm (Okinawa, Japan). They found that the propolis extract blocked the serine/threonine p21-activating kinase 1 (PAK1) and the melanogenesis by downregulating intracellular tyrosinase at 1, 6, 12 and 30 μg/ml. The main constituents were identified as prenylflavonoids by LC–MS and corresponded to nymphaeols A-C, isonymphaeol-B, and 3′- geranyl-naringenin.
In vivo studies
Chemopreventive effects
Doi et al. [145] revealed that ethanol propolis extract alleviated colon tumorigenesis in male F344 rats. According to Alizadeh et al. [146], Iranian propolis remarkably prevented the immunohistochemistry positive for β-catenin positive tumors in female Wistar rats. In a female Wistar rat model, propolis extract exhibited chemo preventive activity against rat bladder carcinogenesis [147, 148]. In a report, Salehi et al. [149] examined the Iranian propolis chemo-preventive effects. They found that the propolis extract at 100–400 mg/kg dose alleviated tongue dysplasia in male Wistar rats [149]. In another report, Xie et al. [150] stated that the ethanol propolis extract increased the N-butyl-N-(4-hydroxybutyl)-nitrosamine (BBN)-induced carcinogenesis of urinary bladder through non-mutagenicity activity in male F344 rats.
Immunomodulatory effects
Orsolić, Basić [151] reported that the ethanol propolis extract not only averted the tumor growth and proliferation but also enhanced the activity of tumoricidal macrophages. In another study, the ethanol propolis extract significantly suppressed the tumor growth and metastasis. In this study, the anti-metastatic activity was mediated by the immunomodulatory effects of propolis [152, 153]. Sulaiman et al. [129] reported that ethanol propolis extract at 500 or 1000 mg/kg increased the endoreduplication and p53 expression, with a reduction of mitotic cells and the Ki-67 expression in female N1-nu/nu mice. According to Missima et al. [154, 155], the ethanol propolis extract stimulated cytokine production and thereby, displayed stress in C57BL/6 male mice at 200 mg/kg. An investigation by Doi et al. [145] reported the the activation of NK cell cytotoxicity after the treatment with 500 mg/kg/day ethanol propolis extract in wild-type and RAG 2-deficient C57BL/6 mice.
Anti-angiogenic effects
Ahn et al. [156] reported that the Brazilian propolis at 2.5 and 5% exerted suppressive effects against tumor-induced angiogenesis in female ICR mice. Moreover, an experiment carried out by Chikaraishi et al. [157] used green propolis extract to determine the angiogenic effects. In this study, they found that propolis at 300 mg/kg/day significantly alleviated the retinal neovascularization in C57BL/6 mice [157]. In another study, de Moura et al. [158] showed the anti-angiogenic effects of 500 mg/kg/day water propolis extract in female Swiss mice by morphometric analysis and evaluating the hemoglobin content. They reported that the number of blood vessels decreased gradually in the treated group in comparison to the control group [158]. Dornelas et al. [159] found that the microvascular density in bladder carcinomas was lower when applying propolis extract at the concentration of 150 mg/Kg/day in female Wistar rats. Anticancer properties of propolis ethanol, water, methanol and hydroalcholic extracts and their isolated compounds are shown in Table 7.
Table 7.
Anticancer properties of propolis ethanol, water, methanol and hydroalcholic extracts (EE, WE, ME and HAE, respectively) and their isolated compounds
| Compound/extract | Model | Concentration/dose | Study type | Mechanism | Origin | References |
|---|---|---|---|---|---|---|
| Hyperibone A | HeLa tumor cells | IC50 = 0.18 µM | In vitro | Cytotoxic | Brazil | [95] |
| Nemorosone | HeLa tumor cells | IC50 = 3.3 µM | In vitro | Cuba | [95] | |
| Luteolin | Human colon cancer (HCT-116) | IC50 = 115.68 μM | In vitro | Cytotoxic/apoptosis | Serbia | [96] |
| Luteolin | Human triple negative breast cancer (MDA-MB-231) cell lines | IC50 = 66.86 μM | In vitro | |||
| Myricetin | Human triple negative breast cancer (MDA-MB-231) cell lines | IC50 = 114.75 μM | In vitro | Inhibition of cell growth and apoptosis | ||
| Galangin | Human colon cancer and human triple negative breast cancer cell lines | IC50 = 50 μM | In vitro | Apoptosis | ||
| EE | glioblastoma cells cancer line | IC50 = 92.2 µg/mL | In vitro | Cytotoxic | Mexico | [98] |
| (7′′R)-8-[1-(4′-Hydroxy-3′-methoxyphenyl) prop-2-en-1-yl] galangin | PANC-1 humanpancreatic cell line | IC50 = 4.6 μM | In vitro | Apoptosis-like morphological changes/Cytotoxic | [97] | |
| Chrysin, pinobanksin, pinobanksin-3-O-propanoate, pinobanksin-3-O-butyrate, pinobanksin-3-O-pentanoate, pinobanksin-3-O-hexanoate | B-cell lymphoma cell line | IC50 = 49.1 µM; 52.1 µM; 67.0 µM; 49.9 µM; 51.3 µM; 76.6 µM | In vitro | Antiproliferative activity through apoptotic induction | Sonaran | [99] |
| Turkish propolis EE | Human adenocarcinomic alveolar basal epithelial (A549) cancer | IC50 = 31.7 µg/mL | In vitro | Cell cycle arrest (G1 phase), induction of endoplasmic reticulum stress, caspase activity, and apoptosis; decrease ofmitochondrial membrane potential | Turky | [100] |
| Turkish EE | human normal foreskin fibroblast cells | IC50 = 76.9 µg/mL | In vitro | Cytotoxic activity | ||
| Turkish EE | Human adenocarcinomic alveolar basal epithelial (A549) cancer | 31.7 and 57.1 µg/mL | In vitro |
Increase of caspase activity; decrease of mitochondrial membrane potential; up-regulation CHOP mRNA expression; cell cycle arrest (G1phase)—apoptosis |
Turky | [100] |
| EE | HCT 116 Colon Cancer and Me45 Malignant Melanoma Cells | IC50 = 100 µM | In vitro | Anti-proliferative and pro-apoptotic Effect | Poland | |
| Propolone A-B | Ovarian cancer cell line | LC50 = 19.1 µM and 29.9 µM | In vitro | Anti-proliferative | Brazil | [102] |
| Novel 2-phenoxychromone; 3-O-methylquercetin; 3,6,4′-trimethoxychrysin; 3,6-dimethoxyapigenin | DLD-1 (human colon cancer), | IC50 = 65.8; 16.2; 17.1; 31.0 μM | In vitro | Anti-proliferative effect; cell growth inhibition | Brazil | [103] |
| MCF-7 (human breast cancer) and | IC50 = 174.4; 16.7; 50.5; 41.9 μM | |||||
| A549 (human lung cancer) cancer cell lines | IC50 = 81.9; 34.2; 19.9; 47.0 μM | |||||
| Sonoran Desert EE | Cancerous cell line M12.C3.F6 (murine B cell lymphoma) | IC50 = 22.4 μM | In vitro | Antiproliferative | Sonoran Desert | [104] |
| Caffeic acid and pinocembrin | Human colorectal adenocarcinoma DLD-1 cells | IC50 = 200 μM | In vitro | Antiproliferative | New Zealand | [105] |
| Ardabil EE and quercetin | Mouth epidermoid carcinoma (KB) cell line | IC50 = 40 mM and 195 μM | In vitro | Cell proliferation inhibition | Iran | [106] |
| Ardabil EE and quercetin | Skin squamous cellcarcinoma (A431) cell line | IC50 = 98 μM, and 195 μM | In vitro | Cell proliferation inhibition | Iran | [106] |
| EE from stingless bees Tetragoniscafiebrigi | K562 erythroleukemia cells | IC50 = 250 and 500 μg/mL | In vitro | Necrosis | Brazil | [107] |
| Brazilian red EE | Colon cancer cell lines (human colorectal adenocarcinoma and human colorectal carcinoma) | IC50 = 75.15 and 70.81 μg/mL | In vitro | Antitumor activity | Brazil | [108] |
| p-Coumaric acid | Four triple-negative breast cancer cell lines (BT-20, BT-549, MDA-MB-231, and MDA-MB-436 cells) | IC50 = 17.02, 13.94, 22.85, and 23.55 µM | In vitro | Cytotoxic; decrease of cell viability | Brazil | [109] |
| ( −)-Epigallocatechin-3-gallate | BT-20, BT-549, MDA-MB-231, and MDA-MB-436 cells, | IC50 = 20.10, 19.16, 24.97 and 18.16 µM | In vitro | Cytotoxic; decrease of cell viability | Brazil | [109] |
| EE | AGS human gastric cancer cell | 60, 30, and 15 µg/mL | In vitro | Cell growth and proliferation inhibition | Iran | [110] |
| Human breast cancer, colon adenocarcinoma, epithelial colorectal adenocarcinoma, murine melanoma | 50 and 100 μg/mL | In vitro | Cytotoxic/apoptosis | India | [111] | |
| HeLa cervical cancer cells | IC50 = 80.96 μg/mL | In vitro | Cytotoxic/anti-proliferative effect | Thailand | [112] | |
| EE | Human colon carcinoma cell lines CaCo2 | IC50 = 50 μg/ml | In vitro | Growth inhibitory activity by apoptosis | China | [113] |
| Human colon carcinoma cell lines CaCo2 | 20 μg/ml | In vitro | Decrease of cells in G1, S and G2-M phases, modulation of p53 protein | China | [113] | |
| HCT116 | 38.9 μg/ml | In vitro | Growth inhibitory activity by apoptosis | Brazil | [113] | |
| EE | Human colon carcinoma cell lines CaCo2 | > 50 | In vitro | Growth inhibitory activity by apoptosis | Brazil | [113] |
| Turkish EE | PC-3 cell line | IC50 = 20.7 μg/mL | In vitro | Cytotoxic activity | [114] | |
| Flavonoids and phenolic acid | Human tongue squamous cell carcinoma cell line | 25 and 50 μg/mL | In vitro | Activation of caspases-3, -8 and -9 | [115] | |
| Human rectal and colon cancer cell | 10 μg/mL | In vitro | Proliferation inhibition | [116] | ||
| Human U87MG glioblastoma cell | TMZ (10–100 μM), EE (10-100 μg/mL) | In vitro | Glioblastoma cell growth inhibition NF-κB activity down-regulation | [117] | ||
| Artepillin C | HT1080 (fibrosarcoma), A549 (lung carcinoma) and U2OS (osteosarcoma) human cell lines | IC50 = 275 µM | In vitro | Abrogation of mortalin-p53 complexes causing the activation of p53 | Brazil | [118] |
| Caffeic acid phenethyl ester | Human cancer cells, SKOV3 (ovarian carcinoma), HT1080 (fibrosarcoma), A549 (lung carcinoma), HeLa (cervical carcinoma), U2OS (osteosarcoma), MCF7 and MDA-MB-231 (breast adenocarcinoma | 50 µM | In vitro | Down-regulation of mortalin and up-regulation of GADD45α and p53 tumor suppressor proteins | New Zealand | [119] |
| EE | MCF7 cells | IC50 = 62.24 μg/mL | In vitro | Proliferation inhibition | [120] | |
| DMEP-A-C | head and neck squamous cell carcinoma (HNSCC) cell lines | IC50 = 76.33 µg/mL | In vitro | Cytotoxic activity; metastatic proliferation inhibition | [121] | |
| P. droryana propolis | the K562 erythroleukemia tumour line | IC50 = 0.38 mg/mL | In vitro | Cell viability decrease | [122] | |
| Chyrsin | MDA-MB-231breast cancer cell | 40 μM and 60 μM | In vitro | Up-regulation of p21(waf1/cip1) gene expression and inhibition of histone deacetylase 8 | China | [123] |
| xenograft animalmodel |
90 mg/Kg/day per os |
Cell growth suppression | ||||
| Pinobanksin-3-acetate | human colon cancer | IC50 = 163.61 μg/mL | In vitro | proliferation inhibition and apoptosis induction through up-regulation and down-regulation of multiple genes involved in cell apoptosis, cytokinetics, colorectal carcinogenesis, Wnt, and calcium signaling | [124] | |
| ME | HML cells U937 | 300–500 μg/mL | In vitro |
Dose-dependent decrease of Bcl-2 expression, no changes in Bax expression, apoptosis |
[125] | |
|
Liquiritigenin, formononetin, medicarpin, biochanin A, retusapurpurin |
Carcinoma BCL- 5637 |
25, 50 and 100 μg/mL |
In vitro | Increase of Bax/Bcl-2 ratio levels | Brazil | [126] |
| EE |
Prostate Cancer cell lines PC-3 |
IC50 = 38.48 μg/mL |
In vitro | Slight increase on Bax mRNA | Egypt | [127] |
| EE |
Human lung carcinoma cell line |
1/4 IC50= 17.29 μg/mL |
In vitro |
Decrease of mitochondrial membrane potential by overexpression of pro-apoptotic genes (Bax and Noxa) and decrease of the Anti-apoptotic gene Bcl-XL |
Brazil | [128] |
| WE° |
HL-60 and HCT-116 cell lines |
25 μg/mL | In vitro | Increase of Bax | Iraq | [129] |
| EE |
Breast Cancer lines MCF-7 |
10 and 20 μg/mL |
In vitro | Increase of Bax mRNA and decrease ofBcl-2 mRNA | Brazil | [130] |
| EE |
HEp-2 human laryngeal carcinoma cell |
1/4 IC50 = 14 and 16 μg/mL |
In vitro |
Down-regulation of Bcl-2 and Bcl-XL mRNA; Up-reguation of Bax; apoptosis |
Brazil | [131] |
| ME | HML cells U937 |
100, 300 and 500 μg/mL |
In vitro | Caspase-3 activation | Japan | [125] |
| EE |
Breast Cancer lines MCF-7 and MDAMB- 231 |
50, 100 and 200 μg/mL | In vitro | Caspase-3 activation | Chinese | [132] |
| EE | HeLa |
Nan: 125 μg/mL Chiang Mai: 250 μg/mL |
In vitro | Caspase-3 activation | Thailand | [133] |
| EE | Human tongue carcinoma cell line (CAL-27) | 200 μg/mL | In vitro | Caspase − 3,-8 and -9 activation | Poland | [115] |
| EE |
Breast Cancer lines MCF-7 |
63, 125 and 250 μg/mL | In vitro | Activation of caspase-6 than caspases-8 and 9 | Turkey | [134] |
| EE |
Breast Cancer lines MCF-7 |
20 μg/mL | In vitro | Caspase-3 activation | China and Brazil | [130] |
|
HEp-2 human laryngeal carcinoma cell |
IC50 = 80 μg/mL | In vitro | Apoptosis due to ROS generation and caspase-3 activation | Brazil | [135] | |
| EE |
Human lung carcinoma cell line A549 |
35 μg/mL | In vitro | Mitochondrial membrane potential decrease and caspase activity increase | Turkey | [100] |
| EE | LNCaP prostate cancer cells | 25–50 μg/mL | In vitro | Up-regulation of TRAIL-R2 | [136, 137] | |
| Cardol | SW620 human colorectal cancer cell line | IC50 = 4.51 ± 0.76 μM | In vitro | Increase of caspase-3 and -9 activityand PARP; apoptosis; mitochondrial membrane potential decrease; antiproliferative effect; G0/G1 cell cycle arrest | Indonesian propolis | [138] |
| EE | HUVECs | 6.25–25 μg/mL | In vitro |
Apoptosis in tube-forming endothelial cells through inactivation of survival signal ERK1/2 |
Chinase | [139] |
| EE | HUVECs | 6.25–25 μg/mL | In vitro |
Decrease of PC-PLC activity, p53 and ROS levels |
Brazil | [140] |
| EE | HUVECs | 3.13–25 μg/mL | In vitro | Angiogenesis suppression through inhibition of tube formation and proliferation; decrease of the number of newly formed vessels | Korean | [141] |
| HAE | HUVECs |
100–200 μg/mL; 50–450 mg/Kg |
In vitro |
Inhibition of the tube-like structure formation (tubulogenesis) |
[142] | |
| EE | Carcinoma BCL-5637 | 25 and 50 μg/mL | In vitro | Cell migrationinhibition | Brazil | [126] |
| EE |
Breast Cancer line MDA-MB -231 |
25, 50, 100 and 200 μg/mL | In vitro | Cells migration inhibition | China | [132] |
| EE | Glioblastoma multiforme cell line U87MG | 30 μg/mL | In vitro | Cell migration inhibition | Poland | [143] |
| EE |
Human lung cancer A549 cell, melanoma cell line B16F10 |
1, 6, 12 and 30 μg/mL | Block of PAK1 and melanogenesis by down-regulation of intracellular tyrosinase activity | Japan | [144] | |
| EE |
Colon Tumorigenesis in male F344 rats |
1% EE or WE, basal diet, 25 weeks | In vivo | Tumorigenesis decrease | Brazil | [145] |
| EE |
Gastric cancer in Male Wistar rats |
Enriched feed, 36 weeks | In vivo | Significantly decrease of IHC β-catenin positive tumors | Iran | [146] |
| EE |
Bladder cancer in female Wistar rats |
150 mg/Kg/day, intragastric, 40 weeks | In vivo | Chemo-preventive effects | Brazil | [147, 148] |
| EE |
Dysplasia of tongue in male Wistar rats |
100–400 mg/Kg, intraperitoneall, 20 weeks | In vivo | Tumor decrese | Iran | [149] |
| EE |
Bladder Carcinogenesis in male F344 rats |
0.125 to 1%, dietary administration, 32 weeks | In vivo | Enhances of BBN-initiated urinary bladder carcinogenesis via non-mutagenic mechanisms | Brazil | [150] |
| EE |
Male Swiss albino mice |
50 mg/Kg, gastric incubation, 7 days | In vivo |
Tumor growth and proliferation inhibition; Increase of macrophages tumoricidal activity |
Brazil; Zagreb, Croatia | [151] |
| EE | Male and female CBA inbred mice | 50 or 150 mg/Kg, gauge administration, 3 days | In vivo |
Suppression of tumor growth and metastases; Antimetastatic activity mediated by immunomodulatory effects |
Brazil, Zagreb, Croatia | [152, 153] |
| EE |
Female athymic Fox N1-nu/nu mice |
500 or 1000 mg/Kg/day, p.o., 3 weeks | In vivo |
Mitotic cell and Ki-67 expression decrease and increase in endoreduplications and p53 expression |
Mosul, Iraq | [129] |
| EE |
C57BL/6 male mice |
200 mg/Kg, 14 days | In vivo |
Transcription of stress stimulated Th1 cytokine (IL-2 and IFN-γ) and Th2 cytokine IL-10 |
Brazil | [154, 155] |
| EE |
Female ICR mice |
2.5 and 5%, oral administration, 6 days | In vivo |
Suppressive effects on tumor-induced angiogenesis |
Brazil | [156] |
| EE | OIRM in C57BL/6 mice | 300 mg/Kg/day, subcutaneous administration, 5 days | In vivo | Suppression of retinal neovascularization | Brazil | [157] |
| EE | Female Swiss mice | 500 mg/Kg/day, orally, 14 days | In vivo | Progressively increase of blood vessel number | Brazil | [158] |
| EE |
Bladder cancer in female Wistar rats |
150 mg/Kg/day, 40 weeks | In vivo | Decrease of microvascular density | Brazil | [159] |
Analgesic effects
One of the most prevalent complaints seen in medical practice is pain [160]. Following tissue damage and/or injury, nociceptors (specialist peripheral sensory neurons) are triggered by noxious stimuli (chemical, mechanical, and thermal stimuli). Muscle, cutaneous tissues, connective tissues, arteries, viscera, and bone are all places where nociceptors may be found [161]. The release of inflammatory mediators, which can lower the threshold of nociception, and direct activation of nociceptive afferent fibers owing to pH lowering may both be involved in the acetic acid-induced nociceptive response [162]. Propolis red extract showed analgesic effect on mice model [163] via suppression of NF-kB [164]. Bulgarian propolis was reported to inhibit the contraction of trachea smooth muscle induced by histamine, capsaicin, and carbachol in vitro displaying analgesic effect [165]. Furthermore, Brazilian propolis exhibited anti-nociceptic effect and reduced paw oedema via activating the opioid receptors in rats [166]. Arachidonic acid ethyl ester, a bioactive substance isolated from Cameroonian propolis, reduced acute central pain sensation [167].
Propolis and its chemical constituents presented antinociceptive action on inflammatory and neurogenic pain without motor side effects [168]. Also, one the main chemical analogues of propolis, formononetin, showed antinociceptic effect [168]. Chinese propolis also showed central and peripheral antinociceptive properties due to the presence of flavonoids [169]. In the writhing model, propolis reduced the number of writhes, leading to antinociceptive effect [170].
Propolis demonstrated antinociceptic properties via two possible ways against acetic acid writhing model, i. by local peritoneal receptors; ii. by inhibition of prostaglandin synthesis or action [171, 172]. Furthremore, propolis was used to treat a wide variety of gynecologic, dental, and dermatological issues, where pain is a most frequent issue [173]. The release or production of mediators (e.g., serotonin, kinins, prostaglandin and aminoacids) from neurons or injured tissues is involved in the inflammatory process and in pain processing responses [174, 175].
A number of phytochemical constituents were identified in differents propolis samples such as chalcones and dihydrochalcones [176, 177], flavanones, flavones and flavonols, hydrocarbons esters ethers, terpenoids, lignans, steroids [49, 178]. Brazilian red and, green propolis, Chinese propolis, Bulgarian propolis, Iranian propolis and Cameroonian propolis have the ability to reduce pain sensation in mice/rat models [165, 167, 169, 170]. Brazilian propolis suppressed acetic acid-induced pain and increased the pain threshold reducing the nociceptive response [160]. As a result, the high flavonoids content in green Brazilian propolis could explain these anti-inflammatory properties [179]. Propolis extract promotes the down-regulation of pro-inflammatory cytokines (e.g., interleukin (IL)-1, TNF-α, and IL-6), inhibits the purine nucleoside phosphorylase, and increase the anti-inflammatory IL-10 according to previous results [180, 181]. Several investigations have tried to understand the processes behind the analgesic action of propolis [182]. Previous studies have established that propolis contains several polyphenols, terpenoids and lignans such as artepillin C, neovestitol, vestitol [165], pinocembrin, chrysin, galangin, kaempferol, quercetin, isoliquiritigenin, acetyl-1-coumaroyl-3-cinnamoylglycerol, (+)-2-acetyl-1-feruloyl-3-cinnamoylglycerol, ( −)-2-acetyl-1-feruloyl-3-cinnamoylglycerol, 2-acetyl-1,3-dicinnamoylglycerol and ( −)-2-acetyl-1-(E)-feruloyl-3-(3″,16″)-dihydroxy-palmitoylglycerol, 3,3-dimethylallyl caffeate, caffeic acid phenethyl ester, which showed anti-inflammatory properties in different experimental systems [183–186]. It has been reported that flavonoids suppressed the release of arachidonic acid and interact with GABA-ergic, serotonin and L-arginine–nitric oxide (NO) system [187].
Anti-inflammatory activity
The anti-inflammatoy activities of propolis are shown in Table 8. Propolis has great impact on inflammation [188], because it up-regulates or down regulates several inflammatory mediators [189]. A number of compounds were isolated from propolis, which have anti-inflammatory effects [190]. Artepillin C showed anti-inflammatory potential in adipocytes via down-regulation of adiponectin mediated by TNF-α and c-Jun N-terminal kinase (JNK) pathways [189], and decreasing inflammatory cells through modulation of matrix remodeling [190]. Furthermore, in an in vivo experimental model, artepillin C, reduced oedema by decreasing neutrophils, NO and prostaglandin E2 (PGE2) release [191] and by down-regulation of the NF-κB pathway, which help to attenuate the release of pro-inflammatory cytokines such as TNF-α [191]. These data were confirmed by Szliszka et al. [179], who demonstrated that artepillin C have the ability to in vitro down-regulate the inflammatory chemokines IL-1β, IL-3, IL-4, IL-5, IL-9, IL-12 p40, IL-13, IL-17, TNF-α, G-CSF, GMCSF, MCP-1, MIP-1α, MIP-1β, RANTES by modulating the NF-κB pathway [179]. Other studies reported that propolis extract and artepillin C decreased cysteinyl leukotrienes and histamine in peripheral leukocytes [192, 193]. Moreover, propolis extract inhibited granuloma and exudate formation [194]. Ethanol propolis extract with CAPE exerted anti-inflammatory effects in wistar rat model through inhibition of carrageenin oedema, pleurisy, and adjuvant arthritis [195]. Further studies showed that propolis extract accelerated the down-regulation process of pro-inflammatory cytokines release (e.g., IL-1β, TNF-α and IL-6), inhibited purine nucleoside phosphorylase and increased the anti-inflammatory IL-10 in macrophage cell line [180, 181]. Several inflammatory illnesses have been linked to excessive production of these mediators [196].
Table 8.
Anti-inflammatory properties of propolis ethanol and water extract (EE and WE, respectively) and their isolated bioactive compounds
| Compound/extract | Origin | Concentration /Dose | Study type | Test system | Mechanism | References |
|---|---|---|---|---|---|---|
| Artepillin C | Brazil | 25 μM | In vitro | 3 T3-L1 adipocytes |
Inhibition of TNF-α Down regulation of adiponectin, increase of PPAR-γ activity; inhibition of TNF-α-induced JNK signaling |
[189] |
| Brazil | 500 mg/Kg, orally, 14 days | In vivo | Female Swiss mice |
Decrease of inflammatory Cells, modulation of matrix remodeling |
[190] | |
| Brazil | 10 mg/Kg, single oral dose | In vivo | Male Swiss mice |
Decrease of oedema, reduction of neutrophils number, decrease of prostaglandin E2 level |
[191] | |
| Brazil |
10 μM 100 μM |
In vitro | RAW 264.7 cells |
Reduction in NO synthesis |
[191] | |
| HEK 293 cells | Decrease of the NF-κB levels | |||||
|
50 μM 100 μM |
In vitro | RAW 264.7 cells |
Inhibition of IL-1β, IL-3, IL-4, IL-5, IL-9, IL-12 p40, IL-13, IL-17, TNF-α, G-CSF, GMCSF, MCP-1, MIP-1α, MIP-1β, RANTES, KC and NF-κB pathway |
[179] | ||
| Brazil |
30 μg/mL 100 μg/mL |
In vitro |
Peripheral leukocytes of human blood |
Decrease cysteinyl leukotrienes and histamine | [192] | |
| Propolis extract | - | 10 mg/kg | In vivo | Carrageenan rat paw oedema rat model | Reduce prostaglandins, leukotrienes and histamine | [193] |
| 50 and 100 mg/Kg, orally, 7 days | In vivo | Carrageenin paw edema rat model | Inhibitory effect on granuloma and exudate formation | [194] | ||
| EPE with CAPE | 100–600 mg/Kg, 35 days | In vivo | Male Wistar rat model | Inhibit carrageenin oedema, carrageenin pleurisy and adjuvant arthritis | [195] | |
| Propolis extracts | Cameroon | 30 μg/mL | In vitro | THP-1-derived macrophage cells | Inhibits pro-inflammatory IL-1β, TNF-α and IL-6, increase IL-10 and inhibition of purine nucleoside phosphorylase | [181] |
| Neovestitol and vestitol | Brazil | 10 mg/Kg | In vivo | Male Balb/c mice | Neutrophil migration | [197] |
| Bulgarian Propolis | Bulgary | ID50 = 2.5 0.4 mgkg-1 | Swiss male mice | [165] | ||
| Apigenin | 50 mg/Kg, intraperitoneally, 30 days | In vivo | LPS- induced Male mice | Inhibit inflammatory cytokines, ERK1/2, NF-kB activation, and neutrophill migration | [204, 205] | |
| Galangin | 50 μM | In vitro | RAW 264.7 murine macrophages | Inhibit inflammatory cytokines IL-1β and IL-6, and proinflammatory genes, such as iNOS, ERK1/2, NFkB p65 activation, and neutrophill migration | [203, 206] | |
| pinocembrin | 20 or 50 mg/Kg ip | In vitro | RAW macrophage cells | Modulate the production of TNF-α, IL-1β, IL-6 and IL-10 via inhibiting the phosphorylation of IκBα, ERK1/2, JNK and p38MAPK | [212] | |
| Formononetin | 10 mg/Kg, orally | In vivo | Carrageenan-induced hindpaw oedema rat model | Inhibition of leukocyte migration and activation of NF-κB | [168] | |
| HERP | 10 and 30 mg/Kg, orally | |||||
| Formononetin | 10 mg/Kg | In vitro | INS-1 rat insulinoma cell line | Prevent IL-1β and cytokine-induced apoptotic signaling, reducethe Bax/Bcl-2 ratio and caspase-3 activity; activateNF-κB, decease NO release | [210] | |
| Neovestitol and vestitol | 10 mg/Kg | In vivo | LPS mice model | Inhibition of neutrophil migration, rolling and adhesion; inhibition of CXCL1/KC and CXCL2/MIP2 levels and neutrophil chemotaxis via blocking calcium influx | [198, 199] | |
| Isoliquiritigenin | 10 mg/mL | In vitro | Human primary endothelial cells | Inhibit adhesion of neutrophil, ICAM-1, VCAM1,E-selectin and TNF-α expression, translocation of the p65 subunit of NF-κB by blocking the phosphorylation and subsequent degradation of IκBα | [213] | |
| Daidzein | 2, 4, 8 mg/Kg, i.p | In vivo | Adult male Sprague–Dawley rats model | Inhibited macrophages and neutrophils infiltration, attenuated MPO activity, inhibited TLR4,MyD88 protein and NF-κB activation | [214] | |
| Chinese propolis extract | China | 15 μg/mL | In vitro | RAW 264.7 cells | Inhibit the production of NO, IL-1β, and IL-6; suppress the phosphorylation of IκBα and AP-1; block the activation of NF-κB in TNF-α-stimulated HEK | [8] |
| Senegalese propolis | Senegal | 30 μg/mL | In vitro | J774.1 cells | Inhibited iNOS | [216] |
| EE | China | 25 and 100 mg/Kg, orally, 3 days | In vivo | RAW 264.7 cells/endotoxemic mice | Suppress the secretion of LPS-stimulated inflammatory cytokines, such as IL-6, IL-10, MCP-1, TNF-α and IL-12p70 production | [447] |
| Propolis, coumaric and cinnamic acids | 50 and 100 mg/well | In vivo/ vitro | Male BALB/c mice/ Peritoneal macrophages | Inhibited IL-10 and IL-6 | [180] | |
| Propolis extract | 10 μg/mL | In vitro | RAW 264.7 mouse macrophage cells | Inhibition of IL-1β, IL-6 and COX-2 mRNA expression | [211] | |
| 2-Acetyl-1-coumaroyl-3-cinnamoylglycerol, ( +)-2-acetyl-1-feruloyl-3-cinnamoylglycerol, ( −)-2-acetyl-1-feruloyl-3-cinnamoylglycerol, 2-acetyl-1,3-dicinnamoylglycerol and ( −)-2-acetyl-1-(E)-feruloyl-3-(3″(ζ),16″)-dihydroxy-palmitoylglycerol | 10 and 100 μM | In vitro | Lipopolysaccharide (LPS)-stimulated RAW 264.7 mouse macrophage cells | Inhibitory effects on interleukin IL-1β, IL-6, and COX-2 | [215] | |
| 3,3-Dimethylallyl caffeate in mixture with isopent-3-enyl caffeate | IC50 = 0.49 μM | In vivo | Ear edema test in mice | Anti-inflammatory activity | [218] | |
| Arachic acid ethyl ester | 50.0 mg/Kg | In vivo | Carrageenan-induced paw edema, xylene-induced ear edema mice | Anti-inflammatory effect | [167] | |
| Polyphenol-rich propolis extracts | 100 mg of CPPE/Kg | In vitro | Lipopolysaccharide (LPS)-challenged mice/HEK 293 T cells | Suppressed NF-κB activation via inhibiting the ubiquitination of TRAF6; inhibitory effects on IκBα phosphorylation and p65 nuclear translocation; lowered serum IL-6, MCP-1, IFN-γ, TNF-α and IL-12p70 | [208] | |
| 2-Hydroxy-8-prenylbiochanin A | IC50 = 23.3 µg/mL | In vitro | Lipopolysaccharide (LPS) stimulated J774.2 mouse macrophages | NO inhibition | [219] | |
| β-Amyrine acetate | IC50 = 4.3 µg/mL | ROS inhibition | ||||
| Lupeol acetate | IC50 = 1.1 µg/mL | |||||
| South Brazilian organic propolis | Brazil | 0.1, 1, and 10 μg/mL | In vitro | RAW 264.7 macrophages | Decreased NF-kB activation and TNF-α release | [207] |
| 3′,4′-Dihydroxy-4-methoxydalbergione, 4-methoxydalbergion, cearoin, and chrysin | Nepal | 30 μg/mL | In vitro | Bone marrow-derived mast cells (BMMC) and cell cultures | Inhibited IL-33-induced mRNA expression of inflammatory genes including IL-6, TNFα and IL-13 and activation of NF-κB | [182] |
| WE | 50 mg/kg, i.p | In vivo | Male Wistar albino rats | Reduced ciliary body NF-κB/p65 immunoreactivity and AH levels of HIF-1α and TNF-α | [201] | |
| EE | 50 μL | In vitro | Hyaluronidase assay | Inhibited the hyaluronidase enzyme | [107] | |
| Brazilian organic propolis | Brazil | 10 μg/mL | In vivo | C57BL/J6 SPF male mice | Reduced NF-κB activation, TNF-α release, and neutrophil migration | [448] |
| EE | 1 mg/Kg | In vivo | Carrageenan-induced paw oedema in rats model | Decreased PGE2 and NO levels, inhibited the IL-6 increase | [217] | |
| Daidzein, formononetin Aand biochanin A | 4.68 μg/mL, 31.81 μg/mL, 9.58 μg/mL | In vivo | Adult male Wistar rats | Anti-inflammatory | [209] | |
| Luteolin, galangin, quercetin | 0.5 mg | In vivo | Croton oil-induced oedema in rats | Inhibited IL-1β and TNF-α | [202] | |
| Lebanese propolis EE | Lebanon | 30 μg/mL | In vitro | LPS-activated RAW monocytes | Inhibited COX-2 and iNOS protein expression, as well as PGE2 and NO release | [222] |
| Malaysian propolis | Malaysia | 300 mg/kg b.w | In vivo | Male Sprague Dawley rats | Reduced malondialdehyde, NFkB (p65), TNF-α, IL-1β | [221] |
| CAPE | 30 mg/kg | In vivo | High-fat diet-induced obesity in mice | Reduced the induction of the inflammatory pathway, c-jun-N-terminal kinase, NF-κB, COX-2 expression | [186] | |
| 100 and 200 mM | In vitro | Human middle ear epithelial cells | Inhibited upregulation of TNF-α and COX-2 | [185] | ||
| 2.8 × 10–4–2.8 µgmL– | In vitro | Murine monocyte/macrophage J774 cell line | Inhibited COX-1 and COX-2 | [184] | ||
| 30 mg/kg | In vivo | Gy gamma whole-body irradiation of rats | Decreased IL‐6R, IL‐6, IL‐8, enhanced IL10, suppressed cytokine signaling-3, | [223] | ||
| Caffeic acid | 10 μg/mL | In vitro | Raw 264.7 macrophages | Inhibited NO production, p38 MAPK, JNK1/2 and NF-κB | [224] | |
| EEP, chrysin, galangin, kaempferol quercetin | 30 μg/mL | In vitro | J774A.1 macrophages | Suppressed both IL-1β mRNA (P < 0.02) and iNOS mRNA (P < 0.001) expression, decreased the IL-1β mRNA level and IL-1β protein concentration | [183] | |
| Neovestitol | 0.22 µM | In vitro | RAW264.7 murine macrophages | Inhibited NO production and reduced GM-CSF, IFN-γ, IL-1β, IL-4, TNF-α and IL-6 levels, increased IL-10 production, down-regulated genes related to nitric oxide production, NF-κB, IL-1β, and TNF-α signaling pathways | [200] | |
| Okinawa propolis | Japan | 200 μM | In vitro | RAW 264.7 cells | Reduced iNOS, COX-2, and PGE2 | [220] |
Vestitol, neovestitol, and Bulgerian propolis extract suppressed the neutrophil migration [165, 197]. Besides, in a lipopolysaccharide (LPS)-induced inflammatory mouse model, vestitol and neovestitol blocked neutrophil migration, rolling, and adhesion, as well as inhibiting the levels of the chemokines CXCL1/KC and CXCL2/MIP2 and neutrophil chemotaxis by preventing calcium influx [198, 199]. Neovestitol inhibited NO production and reduced GM-CSF, IFN-γ, IL-1β, IL-4, TNF-α and IL-6 levels, increased IL-10 production and down-regulated genes related to NO production, NF-κB, IL-1β, and TNF-α signaling pathways [200].
Brazil propolis extract inhibited inducible nitric oxide synthase (iNOS) gene expression [164], TNF-α release, and neutrophil migration via reducing NF-κB activation [201]. Apigenin, luteolin, quercetin and galangin, active constituents isolated from propolis, down-regulated inflammatory cytokines such as IL-1β and IL-6, TNF-α and inflammatory genes, such as iNOS, extracellular signal-regulated kinase 1/2 (ERK1/2) and NF-kB and inhibited neutrophill migration [202–206]. Formononetin also suppressed the activation of NF-kB pathway via ubiquitination of TRAF6 [168, 207, 208] and arrest IL-1β, cytokine-induced apoptotic signaling by blocking Bax/Bcl-2 ratio, caspase-3 activity and NO release, exerting anti-inflammatory effect [209, 210]. Furthermore, both IL-1 and iNOS mRNA expression were decreased by chrysin, galangin, kaempferol, and quercetin in macrophages [183].
Pinocembrin inhibited the phosphorylation of IkBα, ERK1/2, JNK, and p38/MAPK pathways, which controlled the production of inflammatory cytokines (TNF-α, IL-1, IL-6, and IL-10) [180, 211, 212]. Isoliquiritigenin inhibited neutrophil adhesion, adhesion molecule 1 (ICAM-1), vascular cell adhesion molecule 1 (VCAM-1) and E-selectin expression and translocation of the p65 subunit of NF-κB by blocking the phosphorylation and subsequent degradation of IκBα in human primary endothelial cells [213]. Daidzein also blocked the activation of NF-κB, inhibiting macrophages and neutrophils infiltration in the inflammatory response. Furthermore, it attenuated myeloperoxidase (MPO) activity and MyD88 protein [209, 214].
Propolis extract from China also exerted anti-inflammatory properties via attenuating the production of NO, IL-1β, and IL-6 mediated by the phosphorylation of IκBα, AP-1 and NF-κB pathways [8, 215]. Senegalese propolis blocked the inflammatory gene iNOS [216]. Propolis extract and the isolated bioactives 2-acetyl-1-coumaroyl-3-cinnamoylglycerol, ( +)-2-acetyl-1-feruloyl-3-cinnamoylglycerol, ( −)-2-acetyl-1-feruloyl-3-cinnamoylglycerol, 2-acetyl-1,3-dicinnamoylglycerol and ( −)-2-acetyl-1-(E)-feruloyl-3-(3″,16″)-dihydroxy-palmitoylglycerol down-regulated the IL-1β, IL-6, cyclooxygenase (COX)-2 mRNA expression in mouse macrophage cells [211, 215]. Propolis aqueous extract decreased ciliary body NF-kB/p65 immunoreactivity as well as hypoxia inducible factor (HIF-1) and TNF-α levels in the aqueous humor [201]. Ethanol extract of propolis attenuated hyaluronidase enzyme [107]. Hu et al. [217] demonstrated that ethanol extract of propolis decreased PGE2 and NO levels and inhibited IL-6 release in carrageenan-induced paw oedema in a rat model. Furthermore, a mixture of three bioactive compound isolated from Mexican propolis (3,3-dimethylallyl caffeate, isopent-3-enyl caffeate and arachic acid ethyl ester) reduced inflammation in ear and paw edema [167, 218]. Moreover, 2-hydroxy-8-prenylbiochanin A, β-amyrine acetate and lupeol acetate increased the NO inhibition in macrophages [219]. In bone marrow-derived mast cells (BMMC), 3′,4′-dihydroxy-4-methoxydalbergione, 4-methoxydalbergion, cearoin, and chrysin isolated from Nepalese propolis, reduced the IL-33-induced activation of NF-kB [182]. Ethanol extract of Lebanese and Malaysian propolis induced anti-inflammatory reaction through blocking TNF-α, IL-1β, COX-2 PGE2, NO release and iNOS protein expression, as well as malondialdehyde (MDA) and NF-kB (p65) expression [220–222]. Furthermore, CAPE suppressed the activation of NF-kB p65, decreasing the inflammatory pathway. In addition, it reduced the expression of JNK, COX-1 and COX-2, and TNF-α in obese mice [184–186] and the release of IL‐6 and IL-8, enhanced the anti-inflammatory cytokines IL-10 and suppressed the cytokine signaling-3 pathway [223]. Caffeic acid prevented macrophages from producing NO, via activating p38 MAPK, JNK1/2, and NF-kB [224].
Antidiabetic effects
Diabetes is a prevalent chronic metabolic health condition [225]. α-Amylase and α-glucosidase are enzymes necessary for the uptake of glucose from starch or maltose. α-glucosidase is essential for disaccharides hydrolisis and, suppressing this enzyme, it is possible to attenuate the blood glucose absoption [226]. Many drugs, that inhibit α-glucosidase have been shown to reduce post-prandial hyperglycemic peaks, making them effective in the treatment of type 2 diabetes. However, a variety of side effects such as stomach pains or diarrhea may make it difficult for patients to stick to their treatment regimen [226]. As a result, natural compounds that inhibit α-glucosidase might be promising therapeutic candidates for the treatment of diabetic mellitus. In this sense, propolis showed hypoglycemic effect by blocking α-glucosidase (IC50 3.77 µM) [220, 227]. Many compounds isolated from propolis such as astrapterocarpan, medicarpin and 8-prenylnaringenin exert antidiabetic effect via suppressing α-amylase and α-glucosidase enzymes in in vivo assays [228]. Furthermore, propolis extract reduceed blood glucose levels in a dose-dependent manner [229–237]. The inhibitory impact of numerous triterpenes isolated from propolis such as cycloartenol, ambonic acid, mangiferonic acid and ambolic acid on α-glucosidase was investigated by Pujirahayu et al. [238]. Mangiferonic acid showed the highest inhibitory impact on α-glucosidase with an IC50 of 3.46 µM [238]. Moreover, propolis and bee pollen extracts ameliorated the insulin resistance [233] as well as the α-glucosidase and α-amylase [239] activity, helping to reduce blood glucose.
The insulin receptor, acting like a tyrosine kinase receptor, shows a wide range of function in human body. Insulin receptor signal pathway helps to regulate glucose transporter in membranes of several cells including hepatocytes, adipocytes, and skeletal muscle cells for energy metabolism [240]. Insulin resistance can be caused by disruptions in various signaling pathways. Modulating insulin receptor signaling at various points along the intracellular route can improve insulin responsiveness in a variety of tissues and, reduce insulin resistance [240]. Several studies demonstrated that natural compounds may modulate the insulin receptor signal with promising results. Liu et al. [241] revealed that propolis with its main compounds galangin and pinocembrin can modulate insulin receptor signaling through regulating Akt/mammalian target of rapamycin (mTOR) signaling pathway [241]. Furthermore, these two phytochemicals attenuated insulin resistance via increasing the insulin sensitivity, Akt, and glycan synthse kinase-3 (GSK3) β and decreasing insulin receptor substrate 1 (IRS-1) phosphorylation. Propolis inhibited the expression of glucose 6-phosphatase (G6Pase) by inhibiting the autophosphorylation of of GSK3α and β, which are involved in the activation of GSK3 [242]. In diabetes, IRS-1 phosphorylation has been established to be related to insulin signal transduction, hence galangin, and pinocembrin reinstate the sensitivity of insulin receptors and diminish insulin resistance [241]. Another study reported that CAPE increased the IRS-1. On the contrary, p-JNK, p-NF-B p65, and nuclear translocation of p-NF-B p6 were suppressed [243]. Tectochrysin (5-hydroxy-7-methoxyflavone) is a bioactive substance from propolis, which exerted hypoglycemic effect by blocking the α-glucosidase enzyme [244]. Besides, propolis with chitosan polyacrylic (CS-PAA) nanoparticles diminished blood glucose levels [245]. Finally, propolis reduced body cholesterol and triglycerides levels and increased peroxisome proliferator activated receptor alpha (PPAR-α) protein expression in the liver [246]. In mice, an ethanol extract of propolis showed anti-hyperlipidemic and antioxidant activity and exhibited protective action on the cardiovascular system and hepatorenal functions [247]. Anvarifard et al. [248] recently reviewed the cellular mechanisms of Propolis on preserving renal functions. Antidiabetic effects of propolis extracts and their isolated bioactive compounds are shown in Table 9.
Table 9.
Antidiabetic effects of propolis extracts (PE) and their isolated bioactive compounds
| Extract/Compound | Concentration | Study level | M/A | References |
|---|---|---|---|---|
| PE | IC50 3.77 µM | In vitro | α-Glucosidase inhibition | [220] |
| Chihuahua propolis | 300 mg/kg/day, orally, 15 days | In vivo | Suppress Blood glucose levels | [234] |
| Astrapterocarpan, medicarpin, 8-prenylnaringenin | 8.0, 5.0 and 4.0 mg/g | In vivo | α-Amylase and α-glucosidase inhibition | [228] |
| Propolis and bee pollen extracts | 100–200 mg/Kg b.w., orally, 16 weeks | In vivo | Reduction of blood glucoseand insulin resistance | [233] |
| PE | 300 mg/Kg b.w., orally, 4 weeks | In vivo | Reduction of fasting blood glucose | [232] |
| PE | 50–100 mg/Kg b.w., orally, 15 days | In vivo | Reduction of blood glucose | [231] |
| PE | 300 mg/Kg b.w., orally, 15 days | In vivo | Reduction of blood glucose | [234] |
| PE | IC50 70.79 µg/mL | In vitro | α-Glucosidase inhibition | [227] |
| PE | IC50 0.09 mg/mL | In vitro | α-Amylase and α-glucosidase inhibition | [239] |
| PE | 200–300 mg/Kg b.w./day, orally, 28 days | In vivo | Reduction of blood glucose, conservation of normal pancreatic cell architecture | [235] |
| PE | 100 mg/Kg b.w., oral intubation, twice daily, 8 weeks | In vivo | Reduction of fasting blood glucose, reduction of glycated hemoglobin; restoration of hepatorenal functions | [236] |
| PE | 200 mg/Kg b.w., orally, 5 weeks | In vivo | Reduction of serum glucose, reduction of oxidative stress parameters | [237] |
| PE | 100–300 mg/Kg b.w., orally, 8 weeks | In vivo | Reduction of plasma level of insulin and HOMA-R index of insulin resistance | [229] |
| PE | 1 mL/100 g, intragastrically, twice daily, 8 weeks | In vivo | Reduction of blood glucose, reduction of fructosamine, malonaldehyde and nitric oxide | [230] |
| PE | IC50 4.7 mg/mL | In vitro | Maltase and α -amylase inhibition | [400] |
| PE | 1–2% w/w | In vivo | Reduction of cholesterol, triacylgycerol and ALT | [449] |
| PE | 70 µL of 85% PE/animal, 60 days | In vivo | Increase of plasmatic HDL, prevention of LVH and arterial atherogenesis | [450] |
| PE | 160 mg/Kg b.w., 14 weeks | In vivo | Reduction of total cholesterol and triglycerides, without any effect on HDL, decrease of atherosclerotic lesion development in aortic root | [451] |
| PE | 250 mg/Kg b.w./day, orally, 4 weeks | In vivo | Normalisation of lipid profile/down-regulation of VCAM, FGF, VEGF and MMP-9 gene expression | [247] |
| PE | 75 mg/Kg b.w., orally | In vivo | Reduction of total cholesterol, LDL and triglycerides | [266] |
| PE | 0.05–0.5% w/w, orally, 8 weeks | Reduction of cholesterol and triglycerides/increase of PPARα protein level in the liver | [246] | |
| CAPE | 60 ng/mL | In vitro and in vivo | Increase of p-Akt and p-insulin receptor substrate (IRS)-1, inhibition of p-JNK, p-NF-κB p65, and nuclear translocation of p-NF-κB p6 | [243] |
| PE conjugated with chitosan polyacrylic (CS-PAA) nanoparticles | In vivo | Suppress blood glucose levels | [245] | |
| PE | 300, 600 mg/Kg b.w., orally, 4 weeks | In vivo | Reduce glucagon, FBG level, and improve insulin and islet of Langerhans regeneration | [452] |
| Tectochrysin | 60 μl/mL | In vitro | α-Glucosidase inhibition | [244] |
| PE | 200, 600 mg/Kg b.w./day, orally, 6 weeks | In vivo | Decrease of glucose level | [453] |
| PE | 100 g/Kg b.w., oral intubation, twice daily, 8 weeks | In vivo | Decrease of glucose level | [236] |
| PE | 240 μM | In vitro | Decrease the of G6Pase expression by inhibiting the autophosphorylation of GSK3α and β, which are involved in the activation of GSK3 | [242] |
Wound healing activity
Wound healing is a complex, multi-step process that can be hampered by a variety of internal and environmental causes [249]. Skin is one of the most prominent part of human body and acts as first line defence system. It can be pertubated by several factors including inflammation and bacterial infections and, these events often require long therapy to achieve a perfect healing [250]. According to recent findings, propolis aids wound healing in a time-dependent manner. The immunomodulatory [10], antimicrobial [251], antioxidant [252], analgesic, and anti-inflammatory [253] properties of propolis might account for accelerating the wound healing [254]. Vascular endothelial growth factor (VEGF), is a growth factor related to endothelial cell growth and migratory activation. VEGF promotes the growth of fibroblasts [255, 256], which play a pivotal role in the wound healing process [257]. Collagen deposition is an integral part of the healing process. It has been proved that propolis contributes also to increase the cell influx and collagen deposition [258].
Propolis has been shown in recent research to have a significant wound healing impact by up regulating the healing process at the tissue level. The preventive impact of propolis is mainly attributed to aminoacids, flavonoids, phenolic acids, terpenes, and vitamins [259]. Propolis extract displayed protective activity by regulating antioxidant-related genes including heme oxygenase 1 (HO-1), GCLM, GCLC in wounded tissue [260]. Propolis bioflavonoids improved immunity and induced the production of interferon by white blood cells or lymphocytes. In a rat experiment model, propolis also activated the thymus, the immune system's master gland, and healed wounds. Furthermore, it has a greater wound healing activity than silver sulfadiazine when used as a skin cream [261].
Mast cells, characterized by inflammatory, proliferative, and remodeling phases, play important roles in wound healing. Mast cell enhance skin wound healing throughout the release of vasochemical madiators such as histamine, proteases, TNF-α and arachidonic acid metabolites [262], and promote the anticoagulant activity. Furthermore, mast cell attach leukocyte to the injured areas, and with macrophages, contribute to phagocytosis and debridement [262]. Mast cells also help to enhances angiogenesis, fibroplasia and re-epithelialization [263]. Propolis used topically reduce the number of mast cells, favouring wound healing [264]. Isolated bioactive constituents from propolis, like CAPE and other active compounds reduced the levels of mast cell and improved surgecial wound during acute inflammation phase [263]. Furthermore, CAPE attenuated histamine release and inflammatory cytokines in wounded tissue [265, 266]. Propolis and its components, such as chysin and kaempferol, have anti-inflammatory properties [267]. Chrysin have the ability to inhibits inflammatory cytokines gene expression such TNF-α, IL-1, IL-4, and IL-6 in mast cells through NF-kB and caspase-1 related mechanistic pathways [267, 268]. Moreover, kaempferol can also inhibit degranulation and cytokine production by the activated mast cells [267] and improved wound healing capacity of propolis in experimental wound healing model.
Because oxidative stress occurs after wound, the antioxidant activities of propolis could favour tissue repair [269, 270]. Some studies reported that release of pro-oxidant mediators, such as reactive oxygen and nitrogen species, is linked to severe burns [270, 271]. Free radicals in burns disrupt the functionality of cellular membranes and intracellular oganelles, and numerous inflammatory signaling processes, reducing the wound healing activity [271]. Hence, antioxidant compounds represent promising therapeutic agents for attenuating burn related injuries [270]. In several studies, it has been demonstrated that propolis exert antioxidant qualities, making it a viable alternative for regulating burn wound healing [71, 74, 272, 273]. Okinczyc et al. [273] reported that propolis from Eurasian areas have potentiall antioxidant activity. Propolis exert antioxidant activity in burn wound healing process due to its flavonoid and phenols content [274]. Mohammadzadeh et al. [274] stated that there is a strong relationship between the chemical composition of propolis and its antioxidant activity. The flavonoids (including flavones, flavonols, flavanones and dihydroflavonols) and other phenolics (mainly cinnamic acids and their esters) are able to scavenge free radicals [247, 275]. Polyphenolic compounds of propolis displayed a protecting role by reducing the proteins break down, and maintaining the integrity of cellular membrane decreasing peroxidation and hemolysis [272]. CAPE with some other polyphenols can upregulate the expression of aminopeptidase (AMP) gene, which helps re-epithelialize skin cell in chronic wound [276, 277] and reduce lipid peroxidation reducing the DNA and protein breakage [71]. In addition, propolis extract rich in galangin, has the ability to inhibit superoxide anion production and suppress oxidative stress in wound injuries [71].
In association with nanoparticles (polymeric nanofibrous wound dressing of polyvinyl alcohol (PVA), propolis, showed significant potential tissue regeneration [278]. Furthermore, biogenic silver nanoparticles (Bio AgNP) with propolis showed antibacterial activity against Gram– and Gram + bacteria stimulating fibroblast cell proliferation and heal wound in surgical sutures [279]. In a study, propolis extract incorporated in a biocompatible polyurethane-hyaluronic acid (PU-HA) nanofiber in wound dressing, displayed a potent activity favouring the fibroblast cells adhesion, deposition of collagen fibers and cell proliferation in wounded areas [280, 281]. A propolis mixture of two different geographical location evidenced better potential effect than individually on wound healing through re-epithelization process in rat chronic wound by bacterial inhibition [282]. It has been demonstrated that topical application of propolis paste (30%) showed a beneficial effect on cutaneous wound healing in dog experimental model [283]. Furthermore, propolis has dermal construction effect evidencing significant reduction in the wound surface area [30].
CAPE, a component of propolis, has immunosuppressive properties in T-cells, which play a significant role in the development of inflammatory disorders. CAPE also reduced both the expression of IL-2 gene and the production of IL-2 in activated T-cells [283]. Propolis also includes antiviral compounds such as 3-methyl-but-2-enyl caffeate, isopentyl ferulate, and moronic acid [5]. Additionally, together with ascorbic acid, propolis promoted wound healing in diabetic patients through dermal regeneration in a rat model [284].
Re-epithelialization is a critical phase in wound healing involving keratinocyte migration and proliferation [285]. Propolis along with its chemical constituents increases aquaporin-3 (AQP3) gene expression [254]. AQP3-facilitated water transport plays a pivotal role in cell migration and hyperproliferation and accelerates the healing of cutaneous wounds stimulating epidermal keratinocytes [254]. Therefore, in conclusion propolis from different countries heal wounds by regulating a plenty of signalling pathways including mast cell regulating via and AQP-3, VEGF, NF-kB and caspase-1 pathways.
Antiviral activity
The world has witnessed the outbreak of several detrimental viral epidemics and/or pandemics since the creation of human civilization that have established a remarkable spotlight in the sectors of public health, education, and economy. The substantive example is the ongoing Covid-19 pandemic that nobly alters human lifestyle and creates a frenzied challenge for researchers to deliver safe, tolerable, and effective treatment strategies, including natural product therapy [286], experimental drug candidates [287], and vaccines [287]. Various researchers in most of the countries are continuously trying to overcome this hectic challenge by computational technologies to determine predictable therapeutic responses at fast along with cost and time saving matters [288–290]. Regarding all kinds of viral issues, the alternative and complementary ethnomedical practices (i.e., plants, natural products, and natural compounds) in various holistic approaches led to the greatest concern in the direction of the therapeutic development throughout the world [286]. At the same time, to establish an appropriate therapeutic candidate, some non-clinical and pre-clinical studies before the clinical studies must be established and find out the satisfactory results that can lead to the clinical trial [291]. Based on these perspectives, some researchers began to investigate the antiviral properties of propolis and several isolated compounds.
Various propolis extracts (e.g., aqueous, ethanolic, and hydroalcholic) at controllable laboratory condition have been found to exeret substantial antiviral activity against several types of viruses such as Herpes simplex virus type 1 and 2 (HSV-1 and HSV-2), Canine distemper virus, Human rhinovirus type 2, 3 and 4 (HRV-2, HRV-3 and HRV-4), Influenza virus type A and B, Parainfluenza virus, Human immunodeficiency virus (HIV), and Adenovirus [292, 293].Research findings demonstrated that aqueous and ethanol propolis extracts exhibited a strong antiviral activity against HSV-1 [294] and HSV-2 [295] on RC-37 cells by affecting viral plaque formation and viral infection cycle. On the other hand, 0.5% aqueous extract of propolis showed potent antiviral activity against HSV-1 infected rats and rabbits thorough prevention of virus absorption into the host and inhibition of an internal step(s) during the viral replication cycle [296]. In addition, ethanol Mexican propolis extract exerted antiviral activity against Canine distemper virus through the inhibition of the relative expression of the virus nucleoprotein gene [297]. It has been cited that a 5% alcoholic solution of propolis strongly prevented influenza viral proliferation in experimental influenza virus-infected mice [298]. Furthermore, the Brazilian propolis ethanolic extract adequately blocked the entry of viruses (HRV-2, HRV-3, and HRV-4) into the experimental HeLa cells protecting them from the virus destruction and reducing virus replication [299].
Some flavones and flavonols (especially galangin, kaempferol, and quercetin) extracted from propolis have been cited to exert antiviral activity against HSV-1 in variable doses [300]. Another investigation by Amoros et al. [301] reported that 3-methyl-but-2-enyl caffeate showed anti-HSV-1 activity through preventing the viral DNA synthesis. Finally, recent studies, showed that both propolis and its constituents had potential efficacy against SARS-CoV-2 by modulating multiple pathogenic pathways [302–311]. Molecular docking studies have demonstrated high binding affinities of propolis compounds to several SARS-CoV-2 proteins, including 3C-like protease, papain-like protease, RNA-dependent RNA polymerase, the receptor-binding domain of the spike protein and helicase. Moreover, these studies showed a high affinity against the viral target angiotensin-converting enzyme 2 (ACE2). Among these compounds, the most promising one was the retusapurpurin A, which showed the best affinity for the most viral targets mentioned above inhibiting the viral entry by forming hydrogen bonds with aminoacid residues within viral and human target proteins [312]. Table 10 shown the antiviral activity of propolis water, ethanol and hydroalcholic extracts and isolated compounds.
Table 10.
Antiviral activity of propolis water, ethanol and hydroalcholic extracts (WE, EE and HAE, respectively) and isolated compounds
| Extract/Compound | Concentration /Dose | Test system | Results/Mechanisms | References |
|---|---|---|---|---|
| WE and EE | 0–120 pfu (%) | HSV-1 on RC-37 cells | Affects viral infection cycle | [294] |
| WE and EE | 0.00005–0.005 pfu (%) | HSV-2 on cells RC-37 | Inhibition of HSV-2 plaque formation (IC50 0.0005% and 0.0004%, respectively) | [295] |
| 0.5% WE | _ | Rat and rabbit infected with HSV-1 | 50% inhibition of HSV infection | [296] |
| Mexican EE | 250 µg/mL | Canine distemper virus | Inhibition of the virus nucleoprotein gene expression | [297] |
| 5% HAE | _ | Influenza virus in mice | Prevents influenza viral proliferation | [298] |
| Brazilian EE | 50–100 µg/mL | HRV-2, HRV-3, and HRV-4 in HeLa cells | Block virus entrance into the cells, avoiding virus destruction and replication | [299] |
| Galangin, kaempferol, quercetin | 0.05–1.0 µM | HSV-1 | Reduce the viral titer by 2log10 | [300] |
| 3-methyl-but-2- enyl caffeate | 6.25, 12.5, 25 and 50 µg/mL | HSV-1 | Reduce the viral titer by 3log10 and viral DNA synthesis by 32-fold | [301] |
| CAPE | 5 µM | HTLV-1 | Inhibits NF-kB activation during in vitro infection | [454] |
| Green propolis EE | 5 mg | Suid herpesvirus type 1 (SuHV-1) | Increases humoral and cellular response in mice immunized with SuHV-1 | [455] |
| Quercetin |
5–25 µM 50 µM 1–50 µM |
Rhinovirus (RV) Hepatitis C virus (HCV) Hepatitis B virus (HBV) |
Inhibits rhinovirus replication in vitro and in vivo; Prevents up-regulation of diacylglycerol acyltransferase (DGAT) required for HCV replication in vitro; Decreases heat shock proteins and HBV transcription levels in vitro |
[456] [457] [458] |
| Caffeic acid |
IC50 = 3.9 µM—100 mg/kg b.w. per os; 4 mM IC50 = 7.2 and 8.5 µM on NA1 and NA2, respectively |
HBV Influenza A virus (IAV) IAV |
Inhibits HBV-DNA replication in vitro and in vivo; Inhibits replication IAV in vitro; Inhibits IAV activity through neuraminidases (NA) in vitro |
[277] [459] [460] |
| Rutin | Binding energy -8.97 kcal/mol (in silico) | SARS-CoV-2 | Inhibitory potential on ACE2 | [302] |
| Anatolia propolis EE, hesperetin (HE), pinocembrin (PI), CAPE | IC50 = 0.57–1.14 µL, 16.88 mM, 29.53 mM, 79.09 mM; Binding energy to spike S1 protein: -7.28, -7.54, 7.17 respectively for HE, PI and CAPE | SARS-CoV-2 |
Binds spike S1 protein and ACE-2 receptor as both in vitro and in silico studies |
[303] |
| Optimized liposomal formula of propolis, rutin and CAPE |
IC50 = 1.18 mM, ICM score: -92.8 and -67.8 agaist 3CL protease; ICM score: -94.3 and -77.8 agaist S1 spike protein |
SARS-CoV-2 | Bind COVID-3CL protease and S1 spike protein; inhibit the viral replication | [304] |
| Glyasperin A and broussoflavonol F | Binding affinity -7.8 kcal/mol | SARS-CoV-2 | Bind SARS-CoV-2 main protease | [305] |
| Withaferin-A, Withanone and CAPE | Binding affinity: -5.6, -4.3 and -6.20 kcal/mol, respectively | SARS-CoV-2 |
Bind transmembrane protease serine 2 (TMPRSS2) in molecular docking studies |
[306] |
| Withanone and CAPE | Binding affinity: -4.42 and -4.79 kcal/mol, respectively | SARS-CoV-2 | Bind SARS-CoV-2 protease Mpro | [307] |
|
3'-Methoxydaidzin (MD), neoblavaisoflavone, methylophiopogonone A and genistin |
Binding affinity: -7.7 for MD and -7.6 kcal/mol for other compounds against Mpro; -8.1, -8.2, -8.3, and -8.3 kcal/mol, respectively against spike protein S2 | SARS-CoV-2 | Bind main protease (Mpro) and spike protein subunit 2 (S2) | [308] |
| Glyasperin A, broussoflavonol F, sulabiroins A, (2S)-5,7-dihydroxy-4'-methoxy-8-prenylflavanone and isorhamnetin | Docking score of -10.8, -9.9, -9.5, -9.3 and -9.2 kcal/mol respectively | SARS-CoV-2 | ACE-2 inhibitors | [309] |
| 2,2-Dimethyl-8-prenylchromene, Artepillin C, 3-Prenyl cinnamic acid allyl ester, Isocupressic acid, 13C-symphyoreticulic acid, ellagic acid, syringic acid, caffeic acid phenethyl ester, p-coumaric acid, hesperetin, naringenin, kaempferol, quercetin, chrysin | Binding scores: -5.6—-7.8 kcal/mol against Mpro; -5.3—-6.4 kcal/mol against RdRp | SARS-CoV-2 |
Main protease (Mpro) and RNA-dependent RNA polymerase (RdRp) enzymes |
[310] |
Antidepressant and anxiolytic-like effects
Diverse estudies have been reported the effects of propolis in the central nervious system (CNS) as a neuroprotector and in amelioraitng alterations in behavior. Propolis extract (10–50 mg/kg) improved the locomotor activity and exert anxiolytic-and antidepressant effects in vivo like diazepam, as observed by in vivo open field (OF), elevated plus-maze (EPM) and forced swimming tests, respectively [313]. Moreover, propolis extract decreased the NO release in response to swim stress induced in experimental model [313]. Theses pharmacological effects are mainly attributed to its polyphenolic constituents such as flavonoids, phenolic acids and terpenes [314–316]. In the OF test, Lee et al. [317] revealed that propolis extract had an antidepressant-like effect without affecting locomotor function or spontaneous movement in a dose-dependent manner. Furthermore, they hypothesized that the antidepressant effect may be mediated by an elevation in hippocampal glucocorticoid receptor (GR) activity, which modulates the hypothalamic–pituitary–adrenal (HPA) axis by attenuating corticosterone response and, reducing c-fos neurons in brain tissue and lipid peroxidation in CNS. Moreover, CAPE, an active biocomponent of propolis, down-regulated c-fos levels in neurons, which relate with antidepressant-like effect [318]. Additionally, CAPE knocked down the expression of p38/MAPK signaling pathway, improving GR function and exerting antidepressant effect [69]. Chrysin, another active chemical constituents of propolis, exerted an antidepressant activity in vivo by elevating the brain-derived neurotropic factor (BDNF) and nerve growth factor (NGF), Na+, K+-ATPase, non-protein thiol (NPSH), corticosterone level [319] and down-regulated ROS levels [320]. Moreover, chrysin, as already demonstrated for the CAPE, exhibited antidepressant modulation via regulating the HPA axis [319]. Finally, chrysin contributed to reduce the stress by decreasing the release of several pro-inflammatory cytokines such as TNF-α, IL-1β and IL-6 [319].
A recent study had revealed that propolis extract drastically reduce cortisol (CORT), adrenocorticotropic hormone (ACTH) and MDA and elevate superoxide dismutase (SOD) levels in a stressed mice model. Therefore, this study clearly demonstrated that propolis extract exerted anti-anxiety properties through the inhibition of the hyperfunction of the HPA axis and stimulation of antioxidation processes in nervous system [321]. In the OP test, however, anxiolytic-like agents led to an increase in central locomotion [322], and a diminution in grooming [323]. Propolis, on the contrary, increased locomotion in OF test [317, 321], thus the anxiolytic effect of propolis remains a bit controversial and further studies are needed to corroborate this hypotesis.
Apitherapy
Apitherapy is a set of treatments aimed at recovering well-being, both in the human and veterinary fields, with products collected, processed, and secreted by bees including honey, propolis, pollen, bee venom, and royal jelly. Bee products are conventional drugs in several countries. The apitherapy has its origin in the pharmacy of Antique Egypt about 6000 years ago. Also, the ancient Greeks and Romans have used the ingredients of bees for various types of remedies [324, 325] (Fig. 3).
Fig. 3.
Apitherapy: therapeutic effects of propolis
Propolis possess several helath properties including antiallergic, antimicrobial, antioxidant, cardioprotective effects, anti-cancer, anti-inflammatory, antiulcer, antitumor, hepatoprotective, neuroprotective and antidiabetic effects. The efficacy of neuroprotective flavonoids primarily depends on their high antioxidant, immunomodulatory and anti-inflammatory functions [217, 326–330]. In addition, an in vitro study showed that green propolis enhanced the differentiation, mitigation, and proliferation of stromal cells in bone marrow [331]. The therapeutic properties of the bioactive substances in propolis have been investigated in recent drug screening studies [290, 332, 333]. In dentistry, propolis was used to cure aphthous ulcers, acute necrotizing ulcerative gingivitis, pulpitis, gingivitis, and periodontitis. Because of its medicinal and biological effects, propolis investigation has been expanded. Present dental propolis study includes a wide variety of areas and emphasizes the anti-inflammatory as well as antimicrobial activities of this bee product, notably in oral surgery, pedodontics, pathology, endodontics, and periodontics [334].
Diabetes is a metabolic condition defined by hyperglycemia as well as glycosuria attributed to complete or relative insulin insufficiency. Oxidative stress has been involved in the improvement of diabetic nephropathy. Most investigators showed the streptozotocin (STZ) exposure as a diabetes-inducing factor. One study revealed that propolis extract induced pancreatic β-cells survival against STZ toxicity in rats [335]. Also, researchers found that the administration of water or ethanolic extract of propolis for seven weeks to STZ-induced diabetic rats influenced glucose and lipid metabolism, contributing to reduced outcomes of lipid peroxidation and scavenging the free radicals in diabetic rats [230]. However, it has been documented that the treatment with propolis for 8 weeks to 15% fructose-exposed rats, led to a decrease in body weight as well as insulin concentration without influencing blood glucose concentration [229].
Gastroduodenal ulcers may arise from the unbalance between inflammatory and protective processes in the stomach, such as alteration of the mucosal barrier, acid–pepsin secretion, cellular regeneration, mucus secretion, and epidermal growth factors [336]. It has been reported that propolis has gastric protective effects in mice at several doses (e.g., 50, 250, or 500 mg/kg) [337]. Also, the Brazilian propolis (50 mg/kg or 250 mg/kg) showed anti-ulcerogenic activities in different models [338]. Moreover, the authors investigated the impact of the essential oil derived from the most significant botanical source (Baccharisdracun culifolia) of the Brazilian green propolis on gastric ulcers, showing that it may be a successful therapeutic agent for the development of novel phytotherapeutic approach to treat gastric ulcers [339]. Recently, Boeing et al. [340] observed that the hydroalcoholic extract of red propolis from Northeastern Brazil displays gastroprotective property against ethanol/HCl-induced damage in mice.
Rhinitis is a form of sinusitis characterized by nasal congestion, purulence and sneezing due to bacterial or viral infections. It is a world health issue that affects people's work, education, sleep, and social lives [341, 342]. Brazilian propolis showed to be beneficial in preventing and relieving the signs of allergic rhinitis through the reduction of histamine release. The study showed that a single administration of 1 g/kg propolis was ineffective in preventing antigen-induced nasal rubbing and sneezing, but substantial improvement was described after continuous administration for 2 weeks at this dose [341]. Another respiratory tract disease to consider is asthma as an inflammatory disease of the airways related to overexposure to allergens characterized by congestion, inflammation, as well as repetitive movements and remodeling [343]. Khayyal et al. [344] observed that the daily administration of an aqueous sample of propolis (13%) to patients with mild to severe asthma for two months led to a decrease in night-time attacks and enhanced ventilatory functions. These improvements seemed to be related to a decrease in the release of pro-inflammatory cytokines (IL-6, TNF-α, and IL-8) and an increase of the anti-inflammatory cytokine IL-10, [344].
Hereditary spherocytosis (HS) is an aberrant disease of red blood cells (RBCs). The disease is triggered by a mutation in the genes responsible for the production and maintenance of hemoglobin. Ordinary red blood cells are biconcave disks, and those with HS have a spherical shape (spherocytosis) [345–347]. A recent study evaluated the influence of the propolis extracts on the ability of the red blood cell membrane to retain ions. It has been observed that propolis had a beneficial effect on blood hemoglobin. This result has been attributed to the high content of phenolics in the propolis. The findings of the in vitro evaluation suggested that the membrane fragility improves in a patient's RBCs, and tat the protective advantage of propolis was attributable to its antioxidant properties [348].
Propolis as food preservative
The utilization of propolis in the human diet should be increased to take advantatge of the benefits of its biological actions on human health. It also meets consumer demand for natural antioxidants and antimicrobials rather than synthetic food additives. Therefore, adding propolis to food products as a natural food additive and increasing food quality has become a trending topic [332]. Many of the compounds found in propolis have been utilized as functional food additives and are considered to be safe for human health [13, 30]. However, although propolis is generally considered safe, some people may experience side effects such as dermatitis [11].
Propolis is commonly used in food formulations such as oils, dairy, meat, seafood, fruits, and juice to extend the shelflife, to reduce lipid oxidation, and to provide health advantages to consumers [349]. Vargas-Sánchez et al. [350] observed that propolis extracts can be applied to increase lipid oxidation stability and to prevent microbial growth on beef patties during cold storage. Cottica et al. [351] reported that adding propolis aqueous extract to dairy beverages resulted in increased antioxidant capacity and lower aldehyde generation during storage with exposure to light. Considering that the use of propolis to coat quail eggs protected egg quality metrics, its use may help delay the loss of quality during storage [352].
Conclusions and future directions
Propolis is a unique natural remedy, used since ancient times in traditional medicine, whose pharmacological properties are in constantly updated. The present study summarized the known chemical pofile of propolis until to date collecting data from multiple databases and shelding light also to the phytochemcal differences due to the origin and grow pedo-climatic conditions. Summarizing, about 500 chemical compounds have been described till date, mainly belonging to the flavonoids, terpenoids and phenolic acids classes. However, other secondary metabolites like alkaloids and iridoids were overlooked but have not been yet isolated. Available scientific literature confirms the efficacy of propolis and its bioactive components against bacterial and viral infections and cancer. However, the big problem about the study of therapeutic applications of propolis is its varied composition that depends on the flora of the area, the time of collection, weather conditions, environmental pollution, inclusion of polluting waxes, among others. This makes it difficult to define propolis for medicinal use since its composition varies greatly. Added to the above is the use of different extraction methodologies and solvents used in the different preclinical studies. To solve these problems in the future, standardization should be worked on by establishing exact chemical tests in order to control quality. Currently there is a problem of quality control in propolis products on the market. Apart from its innumerable health uses, some of which have been described recently, such as the possibility of using propolis extracts and its bioactive compounds against SARS-COV-2 infection, propolis can also be used for food preservation. However, further studies are needed to substantiate these claims, in particular, clinical studies with standardized extracts, in order to guarantee the reproducibility of the health properties observed and to translate on humans what observed in the numerous in vitro and animal studies.
Acknowledgements
Miquel Martorell wants to thank ANID CENTROS BASALES ACE210012.
Author contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas. That is, revising or critically reviewing the article; giving final approval of the version to be published; agreeing on the journal to which the article has been submitted; and, confirming to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Funding
No funding received.
Availability of data and materials
Yes.
Declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
No competing interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rajib Hossain, Email: rajibhossainrh021@gmail.com.
Cristina Quispe, Email: elquispe@unap.cl.
Rasel Ahmed Khan, Email: raselahmed358@gmail.com.
Abu Saim Mohammad Saikat, Email: asmsaikat.bmb@gmail.com.
Pranta Ray, Email: raypranta96@gmail.com.
Damira Ongalbek, Email: dami_6@mail.ru.
Balakyz Yeskaliyeva, Email: balakyz@mail.ru.
Divya Jain, Email: divyajain31011996@gmail.com.
Antonella Smeriglio, Email: antonella.smeriglio@unime.it.
Domenico Trombetta, Email: domenico.trombetta@unime.it.
Roghayeh Kiani, Email: t.kiani2020@yahoo.com.
Farzad Kobarfard, Email: farzadkf@yahoo.com.
Naheed Mojgani, Email: seveneart@yahoo.com.
Parvaneh Saffarian, Email: dnmoj@yahoo.com.
Seyed Abdulmajid Ayatollahi, Email: majid_ayatollahi@yahoo.com.
Chandan Sarkar, Email: csarkar1053@gmail.com.
Mohammad Torequl Islam, Email: dmt.islam@bsmrstu.edu.bd.
Dılhun Keriman, Email: dkucar@bingol.edu.tr.
Arserim Uçar, Email: kerimanarserim@gmail.com.
Miquel Martorell, Email: mmartorell@udec.cl.
Antoni Sureda, Email: antoni.sureda@uib.es.
Monica Butnariu, Email: monicabutnariu@yahoo.com.
Javad Sharifi-Rad, Email: javad.sharifirad@gmail.com.
William C. Cho, Email: chocs@ha.org.hk
References
- 1.Makashvili Z. Remarkable hive product: Propolis. Scientific data and suggestions concerning its composition, properties and possible use in therapeutics. In: From the history of Propolis. APIMONDIA standing commission on Bee keeping technology and equipment, Bucharest. 1978.
- 2.Bankova V. Recent trends and important developments in propolis research. Evid Based Complement Alternat Med. 2005;2(1):29–32. doi: 10.1093/ecam/neh059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sforcin JM. Biological properties and therapeutic applications of propolis. Phytother Res. 2016;30(6):894–905. doi: 10.1002/ptr.5605. [DOI] [PubMed] [Google Scholar]
- 4.Anjum SI, Ullah A, Khan KA, Attaullah M, Khan H, Ali H, Bashir MA, Tahir M, Ansari MJ, Ghramh HA, Adgaba N, Dash CK. Composition and functional properties of propolis (bee glue): a review. Saudi J Biol Sci. 2019;26(7):1695–1703. doi: 10.1016/j.sjbs.2018.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khalil ML. Biological activity of bee propolis in health and disease. Asian Pac J Cancer Prev. 2006;7(1):22–31. [PubMed] [Google Scholar]
- 6.Simone-Finstrom M, Spivak M. Propolis and bee health: the natural history and significance of resin use by honey bees. Apidologie. 2010;41(3):295–311. doi: 10.1051/apido/2010016. [DOI] [Google Scholar]
- 7.Nagai T, Inoue R, Inoue H, Suzuki N. Preparation and antioxidant properties of water extract of propolis. Food Chem. 2003;80(1):29–33. doi: 10.1016/S0308-8146(02)00231-5. [DOI] [Google Scholar]
- 8.Wang K, Ping S, Huang S, Hu L, Xuan H, Zhang C, Hu F. Molecular mechanisms underlying the in vitro anti-inflammatory effects of a flavonoid-rich ethanol extract from chinese propolis (poplar type) Evid Based Complement Alternat Med. 2013;2013:127672. doi: 10.1155/2013/127672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bankova VS, de Castro SL, Marcucci MC. Propolis: recent advances in chemistry and plant origin. Apidologie. 2000;31(1):3–15. doi: 10.1051/apido:2000102. [DOI] [Google Scholar]
- 10.Sforcin JM. Propolis and the immune system: a review. J Ethnopharmacol. 2007;113(1):1–14. doi: 10.1016/j.jep.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 11.de Groot AC. Propolis: a review of properties, applications, chemical composition, contact allergy, and other adverse effects. Dermatitis. 2013;24(6):263–282. doi: 10.1097/der.0000000000000011. [DOI] [PubMed] [Google Scholar]
- 12.Huang S, Zhang CP, Wang K, Li GQ, Hu FL. Recent advances in the chemical composition of propolis. Molecules. 2014;19(12):19610–19632. doi: 10.3390/molecules191219610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silva-Carvalho R, Baltazar F, Almeida-Aguiar C. Propolis: a complex natural product with a plethora of biological activities that can be explored for drug development. Evid Based Complement Alternat Med. 2015;2015:206439. doi: 10.1155/2015/206439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sforcin JM, Bankova V. Propolis: is there a potential for the development of new drugs? J Ethnopharmacol. 2011;133(2):253–260. doi: 10.1016/j.jep.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 15.Stojanović S, Najman SJ, Bogdanova-Popov B, Najman SS. Propolis: chemical composition, biological and pharmacological activity – a review. Acta Medica Medianae. 2020;59(2):108–113. doi: 10.5633/amm.2020.0215. [DOI] [Google Scholar]
- 16.McLoone P, Tabys D, Fyfe L. Honey combination therapies for skin and wound infections: a systematic review of the literature. Clin Cosmet Investig Dermatol. 2020;13:875–888. doi: 10.2147/ccid.S282143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zulhendri F, Chandrasekaran K, Kowacz M, Ravalia M, Kripal K, Fearnley J, Perera CO. 2021. Antiviral, antibacterial, antifungal, and antiparasitic properties of propolis: a review. Foods. [DOI] [PMC free article] [PubMed]
- 18.Li Z, Li J, Wang G, Tao Y, Chang X, Xia H, Gui S. Reviewing propolis with multi-components in the treatment of oral diseases through multi-pathways and multi-targets. Mini Rev Med Chem. 2021;21(12):1406–1420. doi: 10.2174/1389557521666210126141314. [DOI] [PubMed] [Google Scholar]
- 19.Wali AF, Mushtaq A, Rehman MU, Akbar S, Masoodi MH. In vitro antioxidant and antimicrobial activities of propolis from Kashmir Himalaya region. Free Radicals Antioxidants. 2016;6:51–57. doi: 10.5530/fra.2016.1.6. [DOI] [Google Scholar]
- 20.Hegazi AG, Abd El Hady FK, Abd Allah FA. Chemical composition and antimicrobial activity of European propolis. Z Naturforsch C J Biosci. 2000;55(1–2):70–75. doi: 10.1515/znc-2000-1-214. [DOI] [PubMed] [Google Scholar]
- 21.Cardinault N, Cayeux MO, Percie du Sert P. Propolis: origin, composition and properties. Phytotherapie (Paris) 2012;10(5):298–304. doi: 10.1007/s10298-012-0733-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ransome H. The Sacred Bee in Ancient Times and Folklore. London, UK. 1937.
- 23.Bostock J, Riley HT. Pliny the Elder: The natural history. 1855.
- 24.Wagh VD. Propolis: a wonder bees product and its pharmacological potentials. Adv Pharmacol Sci. 2013;2013:308249–308249. doi: 10.1155/2013/308249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stawiarz E, Dyduch J. The use of honey bee products of plant origin in apitherapy. Episteme. 2014;25:111–127. [Google Scholar]
- 26.Martinotti S, Ranzato E. Propolis: a new frontier for wound healing? Burns Trauma. 2015;3:9. doi: 10.1186/s41038-015-0010-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matuszewska E, Klupczynska A, Maciołek K, Kokot ZJ, Matysiak J. Multielemental analysis of bee pollen, propolis, and royal jelly collected in West-Central Poland. Molecules. 2021;26(9):2415. doi: 10.3390/molecules26092415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahangari Z, Naseri M, Vatandoost F. Propolis: chemical composition and its applications in endodontics. Iran Endod J. 2018;13(3):285–292. doi: 10.22037/iej.v13i3.20994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pasupuleti VR, Sammugam L, Ramesh N, Gan SH. Honey, propolis, and royal jelly: a comprehensive review of their biological actions and health benefits. Oxid Med Cell Longev. 2017;2017:1259510–1259510. doi: 10.1155/2017/1259510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burdock GA. Review of the biological properties and toxicity of bee propolis (propolis) Food Chem Toxicol. 1998;36(4):347–363. doi: 10.1016/s0278-6915(97)00145-2. [DOI] [PubMed] [Google Scholar]
- 31.Ackermann T. Fast chromatographic study of propolis crude. Food Chem. 1991;42:135–138. doi: 10.1016/0308-8146(91)90028-M. [DOI] [Google Scholar]
- 32.Krol W, Scheller S, Czuba Z, Matsuno T, Zydowicz G, Shani J, Mos M. Inhibition of neutrophils' chemiluminescence by ethanol extract of propolis (EEP) and its phenolic components. J Ethnopharmacol. 1996;55(1):19–25. doi: 10.1016/s0378-8741(96)01466-3. [DOI] [PubMed] [Google Scholar]
- 33.Song YS, Park EH, Hur GM, Ryu YS, Kim YM, Jin C. Ethanol extract of propolis inhibits nitric oxide synthase gene expression and enzyme activity. J Ethnopharmacol. 2002;80(2–3):155–161. doi: 10.1016/s0378-8741(02)00023-5. [DOI] [PubMed] [Google Scholar]
- 34.Afrasiabi S, Pourhajibagher M, Chiniforush N, Bahador A. Propolis nanoparticle enhances the potency of antimicrobial photodynamic therapy against Streptococcus mutans in a synergistic manner. Sci Rep. 2020;10(1):15560–15560. doi: 10.1038/s41598-020-72119-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ambi A, Bryan J, Borbon K, Centeno D, Liu T, Chen TP, Cattabiani T, Traba C. Are Russian propolis ethanol extracts the future for the prevention of medical and biomedical implant contaminations? Phytomedicine. 2017;30:50–58. doi: 10.1016/j.phymed.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 36.Ozdal T, Ceylan FD, Eroglu N, Kaplan M, Olgun EO, Capanoglu E. Investigation of antioxidant capacity, bioaccessibility and LC-MS/MS phenolic profile of Turkish propolis. Food Res Int. 2019;122:528–536. doi: 10.1016/j.foodres.2019.05.028. [DOI] [PubMed] [Google Scholar]
- 37.Romero M, Freire J, Pastene E, García A, Aranda M, González C. Propolis polyphenolic compounds affect the viability and structure of Helicobacter pylori in vitro. Rev Bras. 2019;29(3):325–332. doi: 10.1016/j.bjp.2019.03.002. [DOI] [Google Scholar]
- 38.Koru O, Toksoy F, Acikel CH, Tunca YM, Baysallar M, Uskudar Guclu A, Akca E, Ozkok Tuylu A, Sorkun K, Tanyuksel M, Salih B. In vitro antimicrobial activity of propolis samples from different geographical origins against certain oral pathogens. Anaerobe. 2007;13(3–4):140–145. doi: 10.1016/j.anaerobe.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 39.Teixeira EW, Message D, Negri G, Salatino A, Stringheta PC. Seasonal variation, chemical composition and antioxidant activity of Brazilian propolis samples. Evid Based Complement Alternat Med. 2010;7(3):307–315. doi: 10.1093/ecam/nem177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tzankova V, Aluani D, Yordanov Y, Kondeva-Burdina M, Petrov P, Bankova V, Simeonova R, Vitcheva V, Odjakov F, Apostolov A, Tzankov B, Yoncheva K. Micellar propolis nanoformulation of high antioxidant and hepatoprotective activity. Rev Bras. 2019;29(3):364–372. doi: 10.1016/j.bjp.2018.12.006. [DOI] [Google Scholar]
- 41.Trusheva B, Popova M, Bankova V, Simova S, Marcucci MC, Miorin PL, da Rocha PF, Tsvetkova I. Bioactive constituents of brazilian red propolis. Evid Based Complement Alternat Med. 2006;3(2):249–254. doi: 10.1093/ecam/nel006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kalogeropoulos N, Konteles SJ, Troullidou E, Mourtzinos I, Karathanos VT. Chemical composition, antioxidant activity and antimicrobial properties of propolis extracts from Greece and Cyprus. Food Chem. 2009;116(2):452–461. doi: 10.1016/j.foodchem.2009.02.060. [DOI] [Google Scholar]
- 43.Gülçin I, Bursal E, Sehitoğlu MH, Bilsel M, Gören AC. Polyphenol contents and antioxidant activity of lyophilized aqueous extract of propolis from Erzurum. Turkey Food Chem Toxicol. 2010;48(8–9):2227–2238. doi: 10.1016/j.fct.2010.05.053. [DOI] [PubMed] [Google Scholar]
- 44.Woźniak M, Mrówczyńska L, Waśkiewicz A, Rogoziński T, Ratajczak I. The role of seasonality on the chemical composition, antioxidant activity and cytotoxicity of Polish propolis in human erythrocytes. Rev Bras. 2019;29(3):301–308. doi: 10.1016/j.bjp.2019.02.002. [DOI] [Google Scholar]
- 45.Bankova V, Trusheva B, Popova M. Propolis extraction methods: a review. J Apic Res. 2021;60(5):734–743. doi: 10.1080/00218839.2021.1901426. [DOI] [Google Scholar]
- 46.Ramón-Sierra J, Peraza-López E, Rodríguez-Borges R, Yam-Puc A, Madera-Santana T, Ortiz-Vázquez E. Partial characterization of ethanolic extract of Melipona beecheii propolis and in vitro evaluation of its antifungal activity. Rev Bras. 2019;29(3):319–324. doi: 10.1016/j.bjp.2019.04.002. [DOI] [Google Scholar]
- 47.Ristivojević P, Dimkić I, Guzelmeric E, Trifković J, Knežević M, Berić T, Yesilada E, Milojković-Opsenica D, Stanković S. Profiling of Turkish propolis subtypes: Comparative evaluation of their phytochemical compositions, antioxidant and antimicrobial activities. LWT. 2018;95:367–379. doi: 10.1016/j.lwt.2018.04.063. [DOI] [Google Scholar]
- 48.Kumazawa S, Goto H, Hamasaka T, Fukumoto S, Fujimoto T, Nakayama T. A new prenylated flavonoid from propolis collected in Okinawa. Japan Biosci Biotechnol Biochem. 2004;68(1):260–262. doi: 10.1271/bbb.68.260. [DOI] [PubMed] [Google Scholar]
- 49.Marcucci MC. Propolis: chemical composition, biological properties and therapeutic activity. Apidologie. 1995;26(2):83–99. doi: 10.1051/apido:19950202. [DOI] [Google Scholar]
- 50.Gabrys J, Konecki J, Krol W, Scheller S, Shani J. Free amino acids in bee hive product (propolis) as identified and quantified by gas-liquid chromatography. Pharmacol Res Commun. 1986;18(6):513–518. doi: 10.1016/0031-6989(86)90146-3. [DOI] [PubMed] [Google Scholar]
- 51.Martos I, Cossentini M, Ferreres F, Tomás-Barberán FA. Flavonoid Composition of Tunisian Honeys and Propolis. J Agric Food Chem. 1997;45(8):2824–2829. doi: 10.1021/jf9609284. [DOI] [Google Scholar]
- 52.Ristivojević P, Trifković J, Andrić F, Milojković-Opsenica D. Poplar-type Propolis: Chemical Composition. Botanical Origin and Biological Activity: Natural Product Commun; 2015. [PubMed] [Google Scholar]
- 53.Markham KR, Mitchell KA, Wilkins AL, Daldy JA, Lu Y. HPLC and GC-MS identification of the major organic constituents in New Zeland propolis. Phytochemistry. 1996;42(1):205–211. doi: 10.1016/0031-9422(96)83286-9. [DOI] [Google Scholar]
- 54.Bankova V, Dyulgerov A, Popov S, Marekov N. A GC/MS Study of the Propolis Phenolic Constituents. Zeitschrift für Naturforschung C. 1987;42(1–2):147–151. doi: 10.1515/znc-1987-1-224. [DOI] [Google Scholar]
- 55.Arruda C, Ribeiro VP, Mejía JAA, Almeida MO, Goulart MO, Candido ACBB, dos Santos RA, Magalhães LG, Martins CHG, Bastos JK. Green propolis: cytotoxic and leishmanicidal activities of artepillin c, p-coumaric acid, and their degradation products. Rev Bras. 2020;30(2):169–176. doi: 10.1007/s43450-020-00043-3. [DOI] [Google Scholar]
- 56.Beserra FP, Gushiken LFS, Hussni MF, Ribeiro VP, Bonamin F, Jackson CJ, Pellizzon CH, Bastos JK. Artepillin C as an outstanding phenolic compound of Brazilian green propolis for disease treatment: A review on pharmacological aspects. Phytother Res. 2020 doi: 10.1002/ptr.6875. [DOI] [PubMed] [Google Scholar]
- 57.Shahinozzaman M, Basak B, Emran R, Rozario P, Obanda DN. Artepillin C: A comprehensive review of its chemistry, bioavailability, and pharmacological properties. Fitoterapia. 2020;147:104775. doi: 10.1016/j.fitote.2020.104775. [DOI] [PubMed] [Google Scholar]
- 58.Guzelmeric E, Ristivojević P, Trifković J, Dastan T, Yilmaz O, Cengiz O, Yesilada E. Authentication of Turkish propolis through HPTLC fingerprints combined with multivariate analysis and palynological data and their comparative antioxidant activity. LWT. 2018;87:23–32. doi: 10.1016/j.lwt.2017.08.060. [DOI] [Google Scholar]
- 59.Niyomtham N, Koontongkaew S, Yingyongnarongkul BE, Utispan K. Apis mellifera propolis enhances apoptosis and invasion inhibition in head and neck cancer cells. PeerJ. 2021;9:e12139. doi: 10.7717/peerj.12139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vieira de Morais D, Rosalen PL, Ikegaki M, de Souza Silva AP, Massarioli AP, de Alencar SM. Active Antioxidant Phenolics from Brazilian Red Propolis: An Optimization Study for Their Recovery and Identification by LC-ESI-QTOF-MS/MS. Antioxidants (Basel) 2021 doi: 10.3390/antiox10020297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bozkuş TN, Değer O, Yaşar A. Chemical characterization of water and ethanolic extracts of Turkish propolis by HPLC-DAD and GC-MS. J Liq Chromatogr Relat Technol. 2021;44(1–2):77–86. doi: 10.1080/10826076.2021.1883648. [DOI] [Google Scholar]
- 62.Park YK, Alencar SM, Aguiar CL. Botanical origin and chemical composition of Brazilian propolis. J Agric Food Chem. 2002;50(9):2502–2506. doi: 10.1021/jf011432b. [DOI] [PubMed] [Google Scholar]
- 63.Silva BB, Rosalen PL, Cury JA, Ikegaki M, Souza VC, Esteves A, Alencar SM. Chemical composition and botanical origin of red propolis, a new type of brazilian propolis. Evid-Based Complement Altern Med. 2008;5(3):313–316. doi: 10.1093/ecam/nem059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Salasa A, Mercadoc MI, Zampini IC, Ponessa GI, Isla MI. Determination of botanical origin of propolis from monte region of argentina by histological and chemical methods. Nat Prod Commun. 2016;11(5):627–630. [PubMed] [Google Scholar]
- 65.Jiang X, Tian J, Zheng Y, Zhang Y, Wu Y, Zhang C, Zheng H, Hu F. A new propolis type from changbai mountains in north-east china: chemical composition. Bot Origin Biol Act Mol. 2019;24(7):1369. doi: 10.3390/molecules24071369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yang J, Chen LZ, Xue XF, Wu LM, Li Y, Zhao J, Wu ZB, Zhang YN. A feasibility study on the discrimination of the propolis varieties based on near infrared spectroscopy. Guang Pu Xue Yu Guang Pu Fen Xi. 2016;36(6):1717–1720. [PubMed] [Google Scholar]
- 67.Ahn M-R, Kumazawa S, Hamasaka T, Bang K-S, Nakayama T. Antioxidant activity and constituents of propolis collected in various areas of Korea. J Agric Food Chem. 2004;52(24):7286–7292. doi: 10.1021/jf048726s. [DOI] [PubMed] [Google Scholar]
- 68.Lee IK, Han MS, Kim DW, Yun BS. Phenylpropanoid acid esters from Korean propolis and their antioxidant activities. Bioorg Med Chem Lett. 2014;24(15):3503–3505. doi: 10.1016/j.bmcl.2014.05.065. [DOI] [PubMed] [Google Scholar]
- 69.Lee MS, Kim YH, Lee BR, Kwon SH, Moon WJ, Hong KS, Song YS, Morita K, Hahm DH, Shim I, Her S. Novel antidepressant-like activity of caffeic Acid phenethyl ester is mediated by enhanced glucocorticoid receptor function in the hippocampus. Evid Based Complement Alternat Med. 2014;2014:646039. doi: 10.1155/2014/646039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mak K-K, Tan J, Marappan P, Balijepalli MK, Choudhury H, Ramamurthy S, Pichika MR. Galangin s potential as a functional food ingredient. J Funct Foods. 2018;23:78. [Google Scholar]
- 71.Russo A, Longo R, Vanella A. Antioxidant activity of propolis: role of caffeic acid phenethyl ester and galangin. Fitoterapia. 2002;73(Suppl 1):S21–29. doi: 10.1016/s0367-326x(02)00187-9. [DOI] [PubMed] [Google Scholar]
- 72.Martinello M, Mutinelli F. Antioxidant Activity in Bee Products: A Review. Antioxidants (Basel) 2021 doi: 10.3390/antiox10010071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Miguel MG, Nunes S, Dandlen SA, Cavaco AM, Antunes MD. Phenols and antioxidant activity of hydro-alcoholic extracts of propolis from Algarve. South Portugal Food Chem Toxicol. 2010;48(12):3418–3423. doi: 10.1016/j.fct.2010.09.014. [DOI] [PubMed] [Google Scholar]
- 74.Kumazawa S, Hamasaka T, Nakayama T. Antioxidant activity of propolis of various geographic origins. Food Chem. 2004;84(3):329–339. doi: 10.1016/S0308-8146(03)00216-4. [DOI] [Google Scholar]
- 75.Kubiliene L, Laugaliene V, Pavilonis A, Maruska A, Majiene D, Barcauskaite K, Kubilius R, Kasparaviciene G, Savickas A. Alternative preparation of propolis extracts: comparison of their composition and biological activities. BMC Complement Altern Med. 2015;15(1):156. doi: 10.1186/s12906-015-0677-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Selvaraj R, Priyadarshini F, Jayaprakash P, Selvaraj R, Kanakarajan S, Kamalanathan A. Phytochemical profiling and antibacterial activity of propolis. Int J Scı Res. 2018;7:6. [Google Scholar]
- 77.Hochheim S, Guedes A, Faccin-Galhardi L, Rechenchoski DZ, Nozawa C, Linhares RE, Filho HHdS, Rau M, Siebert DA, Micke G, Cordova CMMd. Determination of phenolic profile by HPLC–ESI-MS/MS, antioxidant activity, in vitro cytotoxicity and anti-herpetic activity of propolis from the Brazilian native bee Melipona quadrifasciata. Rev Bras. 2019;29(3):339–350. doi: 10.1016/j.bjp.2018.12.010. [DOI] [Google Scholar]
- 78.Calegari MA, Ayres BB, dos Santos Tonial LM, de Alencar SM, Oldoni TLC. Fourier transform near infrared spectroscopy as a tool for predicting antioxidant activity of propolis. J King Saud Univ Sci. 2020;32(1):784–790. doi: 10.1016/j.jksus.2019.02.006. [DOI] [Google Scholar]
- 79.Choi YM, Noh DO, Cho SY, Suh HJ, Kim KM, Kim JM. Antioxidant and antimicrobial activities of propolis from several regions of Korea. LWT Food Sci Technol. 2006;39(7):756–761. doi: 10.1016/j.lwt.2005.05.015. [DOI] [Google Scholar]
- 80.Aldemir O, Yildirim HK, Sözmen EY. Antioxidant and anti-inflammatory effects of biotechnologically transformed propolis. J Food Proces Preserv. 2018 doi: 10.1111/jfpp.13642. [DOI] [Google Scholar]
- 81.Rivera-Yañez CR, Ruiz-Hurtado PA, Mendoza-Ramos MI, Reyes-Reali J, García-Romo GS, Pozo-Molina G, Reséndiz-Albor AA, Nieto-Yañez O, Méndez-Cruz AR, Méndez-Catalá CF, Rivera-Yañez N. Flavonoids Present in Propolis in the Battle against Photoaging and Psoriasis. Antioxidants (Basel) 2021 doi: 10.3390/antiox10122014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Moreira L, Dias LG, Pereira JA, Estevinho L. Antioxidant properties, total phenols and pollen analysis of propolis samples from Portugal. Food Chem Toxicol. 2008;46(11):3482–3485. doi: 10.1016/j.fct.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 83.Gargouri W, Osés SM, Fernández-Muiño MA, Sancho MT, Kechaou N. Evaluation of bioactive compounds and biological activities of Tunisian propolis. LWT. 2019;111:328–336. doi: 10.1016/j.lwt.2019.05.044. [DOI] [Google Scholar]
- 84.Kim Y-H, Chung H-J. The effects of Korean propolis against foodborne pathogens and transmission electron microscopic examination. New Biotechnol. 2011;28(6):713–718. doi: 10.1016/j.nbt.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 85.Basim E, Basim H, Özcan M. Antibacterial activities of Turkish pollen and propolis extracts against plant bacterial pathogens. J Food Eng. 2006;77(4):992–996. doi: 10.1016/j.jfoodeng.2005.08.027. [DOI] [Google Scholar]
- 86.Ordóñez RM, Zampini IC, Moreno MIN, Isla MI. Potential application of Northern Argentine propolis to control some phytopathogenic bacteria. Microbiol Res. 2011;166(7):578–584. doi: 10.1016/j.micres.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 87.Soltani EK, Cerezuela R, Charef N, Mezaache-Aichour S, Esteban MA, Zerroug MM. Algerian propolis extracts: Chemical composition, bactericidal activity and in vitro effects on gilthead seabream innate immune responses. Fish Shellfish Immunol. 2017;62:57–67. doi: 10.1016/j.fsi.2017.01.009. [DOI] [PubMed] [Google Scholar]
- 88.Mihai CM, Mărghitaş LA, Dezmirean DS, Chirilă F, Moritz RF, Schlüns H. Interactions among flavonoids of propolis affect antibacterial activity against the honeybee pathogen Paenibacillus larvae. J Invertebr Pathol. 2012;110(1):68–72. doi: 10.1016/j.jip.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 89.Bouchelaghem S. Propolis characterization and antimicrobial activities against Staphylococcus aureus and Candida albicans: A review. Saudi Journal of Biological Sciences. 2022;29(4):1936–1946. doi: 10.1016/j.sjbs.2021.11.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Przybyłek I, Karpiński TM. Antibacterial properties of propolis. Molecules (Basel, Switzerland) 2019;24(11):2047. doi: 10.3390/molecules24112047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Campos JF, dos Santos UP, Macorini LF, de Melo AM, Balestieri JB, Paredes-Gamero EJ, Cardoso CA, de Picoli SK, dos Santos EL. Antimicrobial, antioxidant and cytotoxic activities of propolis from Melipona orbignyi (Hymenoptera, Apidae) Food Chem Toxicol. 2014;65:374–380. doi: 10.1016/j.fct.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 92.Djais AA, Putri N, Jemmy PAR, Darwita RR, Bachtiar BM. Effect of Propolis on Streptococcus mutans Biofilm Formation. Pesquisa Brasileira em Odontopediatria e Clínica Integrada. 2019;19(1):1–9. doi: 10.4034/pboci.2019.191.138. [DOI] [Google Scholar]
- 93.Martins ML, Monteiro ASN, Guimarães JEC, Guimarães M, da Silva RF, Cabral LM, Farah A, dePaula J, Romanos MTV, Maia LC, Cavalcanti YW, Fonseca-Gonçalves A. Cytotoxic and antibacterial effect of a red propolis mouthwash, with or without fluoride, on the growth of a cariogenic biofilm. Arch Oral Biol. 2019;107:104512. doi: 10.1016/j.archoralbio.2019.104512. [DOI] [PubMed] [Google Scholar]
- 94.Coskun ZM, Ersoz M, Gecili M, Ozden A, Acar A. Cytotoxic and apoptotic effects of ethanolic propolis extract on C6 glioma cells. Environ Toxicol. 2020;35(7):768–773. doi: 10.1002/tox.22911. [DOI] [PubMed] [Google Scholar]
- 95.Castro ML, Nascimento AMd, Ikegaki M, Costa-Neto CM, Alencar SM, Rosalen PL. Identification of a bioactive compound isolated from Brazilian propolis type 6. Bioorg Med Chem. 2009;17(14):5332–5335. doi: 10.1016/j.bmc.2009.04.066. [DOI] [PubMed] [Google Scholar]
- 96.Vukovic NL, Obradovic AD, Vukic MD, Jovanovic D, Djurdjevic PM. Cytotoxic, proapoptotic and antioxidative potential of flavonoids isolated from propolis against colon (HCT-116) and breast (MDA-MB-231) cancer cell lines. Food Res Int. 2018;106:71–80. doi: 10.1016/j.foodres.2017.12.056. [DOI] [PubMed] [Google Scholar]
- 97.Li F, Awale S, Tezuka Y, Esumi H, Kadota S. Study on the constituents of Mexican propolis and their cytotoxic activity against PANC-1 human pancreatic cancer cells. J Nat Prod. 2010;73(4):623–627. doi: 10.1021/np900772m. [DOI] [PubMed] [Google Scholar]
- 98.Rivero-Cruz JF, Granados-Pineda J, Pedraza-Chaverri J, Perez-Rojas JM, Kumar-Passari A, Diaz-Ruiz G, Rivero-Cruz BE. Phytochemical constituents, antioxidant, cytotoxic, and antimicrobial activities of the ethanolic extract of mexican brown propolis. Antioxidants (Basel) 2020 doi: 10.3390/antiox9010070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Alday E, Valencia D, Carreño AL, Picerno P, Piccinelli AL, Rastrelli L, Robles-Zepeda R, Hernandez J, Velazquez C. Apoptotic induction by pinobanksin and some of its ester derivatives from Sonoran propolis in a B-cell lymphoma cell line. Chem Biol Interact. 2015;242:35–44. doi: 10.1016/j.cbi.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 100.Demir S, Aliyazicioglu Y, Turan I, Misir S, Mentese A, Yaman SO, Akbulut K, Kilinc K, Deger O. Antiproliferative and proapoptotic activity of Turkish propolis on human lung cancer cell line. Nutr Cancer. 2016;68(1):165–172. doi: 10.1080/01635581.2016.1115096. [DOI] [PubMed] [Google Scholar]
- 101.Kubina R, Kabała-Dzik A, Dziedzic A, Bielec B, Wojtyczka RD, Bułdak RJ, Wyszyńska M, Stawiarska-Pięta B, Szaflarska-Stojko E. The ethanol extract of polish propolis exhibits anti-proliferative and/or pro-apoptotic effect on HCT 116 colon cancer and me45 malignant melanoma cells in vitro conditions. Adv Clin Exp Med. 2015;24(2):203–212. doi: 10.17219/acem/31792. [DOI] [PubMed] [Google Scholar]
- 102.Banzato TP, Gubiani JR, Bernardi DI, Nogueira CR, Monteiro AF, Juliano FF, de Alencar SM, Pilli RA, Lima CAd, Longato GB, Ferreira AG, Foglio MA, Carvalho JEd, Vendramini-Costa DB, Berlinck RGS. Antiproliferative Flavanoid Dimers Isolated from Brazilian Red Propolis. J Nat Prod. 2020;83(6):1784–1793. doi: 10.1021/acs.jnatprod.9b01136. [DOI] [PubMed] [Google Scholar]
- 103.Mitsui T, Hotta S, Tazawa S, Arai Y, Kato K, Ichihara K. Chemical constituents of Brazilian Propolis from the state of Bahia and their growth inhibitory activities against cancer cells. Biosci Biotechnol Biochem. 2018;82(3):417–421. doi: 10.1080/09168451.2018.1427550. [DOI] [PubMed] [Google Scholar]
- 104.Alday E, Valencia D, Garibay-Escobar A, Domínguez-Esquivel Z, Piccinelli AL, Rastrelli L, Monribot-Villanueva J, Guerrero-Analco JA, Robles-Zepeda RE, Hernandez J, Velazquez C. Plant origin authentication of Sonoran Desert propolis: an antiproliferative propolis from a semi-arid region. Naturwissenschaften. 2019;106(5–6):25. doi: 10.1007/s00114-019-1620-2. [DOI] [PubMed] [Google Scholar]
- 105.Catchpole O, Mitchell K, Bloor S, Davis P, Suddes A. Antiproliferative activity of New Zealand propolis and phenolic compounds vs human colorectal adenocarcinoma cells. Fitoterapia. 2015;106:167–174. doi: 10.1016/j.fitote.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 106.Asgharpour F, Moghadamnia AA, Zabihi E, Kazemi S, Ebrahimzadeh Namvar A, Gholinia H, Motallebnejad M, Nouri HR. Iranian propolis efficiently inhibits growth of oral streptococci and cancer cell lines. BMC Complement Altern Med. 2019;19(1):266–266. doi: 10.1186/s12906-019-2677-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Campos JF, Santos UPd, Rocha PdSd, Damião MJ, Balestieri JBP, Cardoso CAL, Paredes-Gamero EJ, Estevinho LM, de Picoli SK, Santos ELd. Antimicrobial, antioxidant, anti-inflammatory, and cytotoxic activities of propolis from the stingless Bee Tetragonisca fiebrigi (Jataí) Evid-Based Complement Altern Med. 2015;2015:296186. doi: 10.1155/2015/296186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Santos DAd, Munari FM, Frozza COdS, Moura S, Barcellos T, Henriques JAP, Roesch-Ely M. Brazilian red propolis extracts: study of chemical composition by ESI-MS/MS (ESI+) and cytotoxic profiles against colon cancer cell lines. Biotechnol Res Innov. 2019;3(1):120–130. doi: 10.1016/j.biori.2019.02.001. [DOI] [Google Scholar]
- 109.Assumpcao JHM, Takeda AAS, Sforcin JM, Rainho CA. Effects of propolis and phenolic acids on triple-negative breast cancer cell lines: potential involvement of epigenetic mechanisms. Molecules. 2020 doi: 10.3390/molecules25061289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Amini-Sarteshnizi N, Mobini-Dehkordi M, Khosravi-Farsani S, Teimori H. Anticancer activity of ethanolic extract of propolis on AGS cell line. J Herbmed Pharmacol. 2015;4(1):29–34. [Google Scholar]
- 111.Choudhari MK, Haghniaz R, Rajwade JM, Paknikar KM. Anticancer Activity of Indian Stingless Bee Propolis: An In Vitro Study. Evid-Based Complement Alternat Med. 2013;2013:928280. doi: 10.1155/2013/928280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Khacha-ananda S, Tragoolpua K, Chantawannakul P, Tragoolpua Y. Antioxidant and anti-cancer cell proliferation activity of propolis extracts from two extraction methods. Asian Pac J Cancer Prev. 2013;14(11):6991–6995. doi: 10.7314/apjcp.2013.14.11.6991. [DOI] [PubMed] [Google Scholar]
- 113.Ishihara M, Naoi K, Hashita M, Itoh Y, Suzui M. Growth inhibitory activity of ethanol extracts of Chinese and Brazilian propolis in four human colon carcinoma cell lines. Oncol Rep. 2009;22(2):349–354. [PubMed] [Google Scholar]
- 114.Turan I, Demir S, Misir S, Kilinc K, Mentese A, Aliyazicioglu Y, Deger O. Cytotoxic effect of turkish propolis on liver, colon, breast, cervix and prostate cancer cell lines. Trop J Pharma Res. 2015 doi: 10.4314/tjpr.v14i5.5. [DOI] [Google Scholar]
- 115.Czyżewska U, Siemionow K, Zaręba I, Miltyk W. Proapoptotic activity of propolis and their components on human tongue squamous cell carcinoma cell line (CAL-27) PLoS ONE. 2016;11(6):e0157091–e0157091. doi: 10.1371/journal.pone.0157091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lee SH, Kim DC, Lee JY, Moonjae C, Hwang WI. A study on the anticancer activity of propolis. Prev Nutr Food Sci. 2000;5(1):54–57. [Google Scholar]
- 117.Markiewicz-Żukowska R, Borawska MH, Fiedorowicz A, Naliwajko SK, Sawicka D, Car H. Propolis changes the anticancer activity of temozolomide in U87MG human glioblastoma cell line. BMC Complement Altern Med. 2013;13:50. doi: 10.1186/1472-6882-13-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bhargava P, Grover A, Nigam N, Kaul A, Dopi M, Ishida Y, Kakuta H, Kaul SC, Terao K, Wadhwa R. Anticancer activity of the supercritical extract of Brazilian green propolis and its active component, artepillin C: Bioinformatics and experimental analyses of its mechanisms of action. Int J Oncol. 2018;52(3):925–932. doi: 10.3892/ijo.2018.4249. [DOI] [PubMed] [Google Scholar]
- 119.Ishida Y, Gao R, Shah N, Bhargava P, Furune T, Kaul SC, Terao K, Wadhwa R. Anticancer activity in honeybee propolis: functional insights to the role of caffeic acid phenethyl ester and its complex with γ-Cyclodextrin. Integr Cancer Ther. 2018;17(3):867–873. doi: 10.1177/1534735417753545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Mohamed WAS, Ismail NZ, Omar EA, Abdul Samad N, Adam SK, Mohamad S. GC-MS evaluation, antioxidant content, and cytotoxic activity of propolis extract from peninsular malaysian stingless bees, tetrigona apicalis. Evid Based Complement Alternat Med. 2020;2020:8895262. doi: 10.1155/2020/8895262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Utispan K, Chitkul B, Koontongkaew S. Cytotoxic activity of propolis extracts from the stingless bee trigona sirindhornae against primary and metastatic head and neck cancer cell lines. Asian Pac J Cancer Prev. 2017;18(4):1051–1055. doi: 10.22034/apjcp.2017.18.4.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bonamigo T, Campos JF, Oliveira AS, Torquato HFV, Balestieri JBP, Cardoso CAL, Paredes-Gamero EJ, de Picoli SK, Dos Santos EL. Antioxidant and cytotoxic activity of propolis of Plebeia droryana and Apis mellifera (Hymenoptera, Apidae) from the Brazilian Cerrado biome. PLoS ONE. 2017;12(9):e0183983. doi: 10.1371/journal.pone.0183983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sun LP, Chen AL, Hung HC, Chien YH, Huang JS, Huang CY, Chen YW, Chen CN. Chrysin: a histone deacetylase 8 inhibitor with anticancer activity and a suitable candidate for the standardization of Chinese propolis. J Agric Food Chem. 2012;60(47):11748–11758. doi: 10.1021/jf303261r. [DOI] [PubMed] [Google Scholar]
- 124.Mutallip A, Abulizi A, Abiban A, Sheng L, Buweihailiqiemu A, Amina M, Takigchi Y, Yamaguchi T, Yimit R. Anticancer activity of propolis flavonoid pinobanksin-3-acetate against human colon cancer in vitro. Int J Biosci. 2015;7(2):4555. [Google Scholar]
- 125.Motomura M, Kwon KM, Suh SJ, Lee YC, Kim YK, Lee IS, Kim MS, Kwon DY, Suzuki I, Kim CH. Propolis induces cell cycle arrest and apoptosis in human leukemic U937 cells through Bcl-2/Bax regulation. Environ Toxicol Pharmacol. 2008;26(1):61–67. doi: 10.1016/j.etap.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 126.Begnini KR, Moura de Leon PM, Thurow H, Schultze E, Campos VF, Martins Rodrigues F, Borsuk S, Dellagostin OA, Savegnago L, Roesch-Ely M, Moura S, Padilha FF, Collares T, Pêgas Henriques JA, Seixas FK. Brazilian red propolis induces apoptosis-like cell death and decreases migration potential in bladder cancer cells. Evid Based Complement Alternat Med. 2014;2014:639856. doi: 10.1155/2014/639856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Salim EI, Abd El-Magid AD, Farara KM, Maria DS. Antitumoral and antioxidant potential of egyptian propolis against the PC3 Prostate Cancer Cell Line. Asian Pac J Cancer Prev. 2015;16(17):7641–7651. doi: 10.7314/apjcp.2015.16.17.7641. [DOI] [PubMed] [Google Scholar]
- 128.Frión-Herrera Y, Díaz-García A, Ruiz-Fuentes J, Rodríguez-Sánchez H, Sforcin JM. Brazilian green propolis induced apoptosis in human lung cancer A549 cells through mitochondrial-mediated pathway. J Pharm Pharmacol. 2015;67(10):1448–1456. doi: 10.1111/jphp.12449. [DOI] [PubMed] [Google Scholar]
- 129.Sulaiman GM, Ad'hiah AH, Al-Sammarrae KW, Bagnati R, Frapolli R, Bello E, Uboldi S, Romano M, Panini N, Scanziani E, Pezzolato M, Erba E, D'Incalci M. Assessing the anti-tumour properties of Iraqi propolis in vitro and in vivo. Food Chem Toxicol. 2012;50(5):1632–1641. doi: 10.1016/j.fct.2012.01.022. [DOI] [PubMed] [Google Scholar]
- 130.Kamiya T, Nishihara H, Hara H, Adachi T. Ethanol extract of Brazilian red propolis induces apoptosis in human breast cancer MCF-7 cells through endoplasmic reticulum stress. J Agric Food Chem. 2012;60(44):11065–11070. doi: 10.1021/jf303004n. [DOI] [PubMed] [Google Scholar]
- 131.Frión-Herrera Y, Díaz-García A, Ruiz-Fuentes J, Rodríguez-Sánchez H, Maurício Sforcin J. Mechanisms underlying the cytotoxic effect of propolis on human laryngeal epidermoid carcinoma cells. Nat Prod Res. 2018;32(17):2085–2091. doi: 10.1080/14786419.2017.1363749. [DOI] [PubMed] [Google Scholar]
- 132.Xuan H, Li Z, Yan H, Sang Q, Wang K, He Q, Wang Y, Hu F. Antitumor Activity of Chinese Propolis in Human Breast Cancer MCF-7 and MDA-MB-231 Cells. Evid Based Complement Alternat Med. 2014;2014:280120. doi: 10.1155/2014/280120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Khacha-Ananda S, Tragoolpua K, Chantawannakul P, Tragoolpua Y. Propolis extracts from the northern region of Thailand suppress cancer cell growth through induction of apoptosis pathways. Invest New Drugs. 2016;34(6):707–722. doi: 10.1007/s10637-016-0392-1. [DOI] [PubMed] [Google Scholar]
- 134.Vatansever HS, Sorkun K, Ismet Deliloğlu Gurhan S, Ozdal-Kurt F, Turkoz E, Gencay O, Salih B. Propolis from Turkey induces apoptosis through activating caspases in human breast carcinoma cell lines. Acta Histochem. 2010;112(6):546–556. doi: 10.1016/j.acthis.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 135.da Silva LM, Frión-Herrera Y, Bartolomeu AR, Gorgulho CM, Sforcin JM. Mechanisms involved in the cytotoxic action of Brazilian propolis and caffeic acid against HEp-2 cells and modulation of P-glycoprotein activity. J Pharm Pharmacol. 2017;69(11):1625–1633. doi: 10.1111/jphp.12789. [DOI] [PubMed] [Google Scholar]
- 136.Szliszka E, Sokół-Łętowska A, Kucharska AZ, Jaworska D, Czuba ZP, Król W. Ethanolic Extract of Polish Propolis: Chemical Composition and TRAIL-R2 death receptor targeting apoptotic activity against prostate cancer cells. Evid Based Complement Alternat Med. 2013;2013:757628. doi: 10.1155/2013/757628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Szliszka E, Zydowicz G, Janoszka B, Dobosz C, Kowalczyk-Ziomek G, Krol W. Ethanolic extract of Brazilian green propolis sensitizes prostate cancer cells to TRAIL-induced apoptosis. Int J Oncol. 2011;38(4):941–953. doi: 10.3892/ijo.2011.930. [DOI] [PubMed] [Google Scholar]
- 138.Kustiawan PM, Lirdprapamongkol K, Palaga T, Puthong S, Phuwapraisirisan P, Svasti J, Chanchao C. Molecular mechanism of cardol, isolated from Trigona incisa stingless bee propolis, induced apoptosis in the SW620 human colorectal cancer cell line. BMC Pharmacol Toxicol. 2017;18(1):32–32. doi: 10.1186/s40360-017-0139-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Kunimasa K, Ahn MR, Kobayashi T, Eguchi R, Kumazawa S, Fujimori Y, Nakano T, Nakayama T, Kaji K, Ohta T. Brazilian propolis suppresses angiogenesis by inducing apoptosis in tube-forming endothelial cells through inactivation of survival signal ERK1/2. Evid Based Complement Alternat Med. 2011;2011:870753. doi: 10.1093/ecam/nep024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Park SI, Ohta T, Kumazawa S, Jun M, Ahn MR. Korean propolis suppresses angiogenesis through inhibition of tube formation and endothelial cell proliferation. Nat Prod Commun. 2014;9(4):555–560. [PubMed] [Google Scholar]
- 141.Xuan H, Zhu R, Li Y, Hu F. Inhibitory effect of chinese propolis on phosphatidylcholine-specific phospholipase C activity in vascular endothelial cells. Evid Based Complement Alternat Med. 2011;2011:985278. doi: 10.1155/2011/985278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Meneghelli C, Joaquim LS, Félix GL, Somensi A, Tomazzoli M, da Silva DA, Berti FV, Veleirinho MB, Recouvreux Dde O, de Mattos Zeri AC, Dias PF, Maraschin M. Southern Brazilian autumnal propolis shows anti-angiogenic activity: an in vitro and in vivo study. Microvasc Res. 2013;88:1–11. doi: 10.1016/j.mvr.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 143.Borawska MH, Naliwajko SK, Moskwa J, Markiewicz-Żukowska R, Puścion-Jakubik A, Soroczyńska J. Anti-proliferative and anti-migration effects of Polish propolis combined with Hypericum perforatum L on glioblastoma multiforme cell line U87MG. BMC Complement Altern Med. 2016;16:367. doi: 10.1186/s12906-016-1351-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Taira N, Nguyen BC, Be Tu PT, Tawata S. Effect of Okinawa Propolis on PAK1 Activity, Caenorhabditis elegans Longevity, Melanogenesis, and Growth of Cancer Cells. J Agric Food Chem. 2016;64(27):5484–5489. doi: 10.1021/acs.jafc.6b01785. [DOI] [PubMed] [Google Scholar]
- 145.Doi K, Fujioka M, Sokuza Y, Ohnishi M, Gi M, Takeshita M, Kumada K, Kakehashi A, Wanibuchi H. Chemopreventive action by ethanol-extracted brazilian green propolis on post-initiation phase of inflammation-associated rat colon tumorigenesis. In Vivo. 2017;31(2):187–197. doi: 10.21873/invivo.11044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Alizadeh AM, Afrouzan H, Dinparast-Djadid N, Sawaya AC, Azizian S, Hemmati HR, Mohagheghi MA, Erfani S. Chemoprotection of MNNG-initiated gastric cancer in rats using Iranian propolis. Arch Iran Med. 2015;18(1):18–23. [PubMed] [Google Scholar]
- 147.Dornelas CA, Cavalcanti BC, Magalhães HI, Jamacaru FV, Furtado FN, Juanes Cde C, Melo Nde O, Moraes MO. Potential chemoprotective effects of green propolis, L-lysine and celecoxib on bone marrow cells and peripheral blood lymphocytes of Wistar rats subjected to bladder chemical carcinogenesis. Acta Cir Bras. 2014;29(7):423–428. doi: 10.1590/s0102-86502014000700003. [DOI] [PubMed] [Google Scholar]
- 148.Dornelas CA, Fechine-Jamacaru FV, Albuquerque IL, Magalhães HI, Souza AJ, Alves LA, Almeida PR, Lemos TL, Castro JD, Moraes ME, Moraes MO. Chemoprevention with green propolis green propolis extracted in L-lysine versus carcinogenesis promotion with L-lysine in N-Butyl-N-[4-hydroxybutyl] nitrosamine (BBN) induced rat bladder cancer. Acta Cir Bras. 2012;27(2):185–192. doi: 10.1590/s0102-86502012000200015. [DOI] [PubMed] [Google Scholar]
- 149.Salehi M, Motallebnejad M, Moghadamnia AA, Seyemajidi M, Khanghah SN, Ebrahimpour A, Molania T. An intervention airing the effect of iranian propolis on epithelial dysplasia of the tongue: a preliminary study. J Clin Diagn Res. 2017;11(7):67–70. doi: 10.7860/jcdr/2017/24887.10249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Xie XL, Gi M, Fujioka M, Doi K, Yamano S, Tachibana H, Fang H, Kakehashi A, Wanibuchi H. Ethanol-extracted propolis enhances BBN-initiated urinary bladder carcinogenesis via non-mutagenic mechanisms in rats. Food Chem Toxicol. 2015;83:193–200. doi: 10.1016/j.fct.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 151.Orsolić N, Basić I. Water-soluble derivative of propolis and its polyphenolic compounds enhance tumoricidal activity of macrophages. J Ethnopharmacol. 2005;102(1):37–45. doi: 10.1016/j.jep.2005.05.036. [DOI] [PubMed] [Google Scholar]
- 152.Orsolić N, Knezević AH, Sver L, Terzić S, Basić I. Immunomodulatory and antimetastatic action of propolis and related polyphenolic compounds. J Ethnopharmacol. 2004;94(2–3):307–315. doi: 10.1016/j.jep.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 153.Orsolić N, Sver L, Terzić S, Tadić Z, Basić I. Inhibitory effect of water-soluble derivative of propolis and its polyphenolic compounds on tumor growth and metastasizing ability: a possible mode of antitumor action. Nutr Cancer. 2003;47(2):156–163. doi: 10.1207/s15327914nc4702_8. [DOI] [PubMed] [Google Scholar]
- 154.Missima F, Pagliarone AC, Orsatti C, Sforcin J. The effect of propolis on pro-inflammatory cytokines produced by melanoma-bearing mice submitted to chronic stress. J ApiProd ApiMed Sci. 2009;1:11–15. doi: 10.3896/IBRA.4.01.1.05. [DOI] [Google Scholar]
- 155.Missima F, Pagliarone AC, Orsatti CL, Araújo JP, Jr, Sforcin JM. The Effect of propolis on Th1/Th2 cytokine expression and production by melanoma-bearing mice submitted to stress. Phytother Res. 2010;24(10):1501–1507. doi: 10.1002/ptr.3142. [DOI] [PubMed] [Google Scholar]
- 156.Ahn M-R, Kunimasa K, Ohta T, Kumazawa S, Kamihira M, Kaji K, Uto Y, Hori H, Nagasawa H, Nakayama T. Suppression of tumor-induced angiogenesis by Brazilian propolis: major component artepillin C inhibits in vitro tube formation and endothelial cell proliferation. Cancer Lett. 2007;252(2):235–243. doi: 10.1016/j.canlet.2006.12.039. [DOI] [PubMed] [Google Scholar]
- 157.Chikaraishi Y, Izuta H, Shimazawa M, Mishima S, Hara H. Angiostatic effects of Brazilian green propolis and its chemical constituents. Mol Nutr Food Res. 2010;54(4):566–575. doi: 10.1002/mnfr.200900115. [DOI] [PubMed] [Google Scholar]
- 158.de Moura SA, Ferreira MA, Andrade SP, Reis ML, Noviello Mde L, Cara DC. Brazilian green propolis inhibits inflammatory angiogenesis in a murine sponge model. Evid Based Complement Alternat Med. 2011;2011:182703. doi: 10.1093/ecam/nep197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Dornelas CA, Fechine-Jamacaru FV, Albuquerque IL, Magalhães HI, Dias TA, Faria MH, Alves MK, Rabenhorst SH, de Almeida PR, Lemos TL, Castro JD, Moraes ME, Moraes MO. Angiogenesis inhibition by green propolis and the angiogenic effect of L-lysine on bladder cancer in rats. Acta Cir Bras. 2012;27(8):529–536. doi: 10.1590/s0102-86502012000800003. [DOI] [PubMed] [Google Scholar]
- 160.Al-Hariri MT, Abualait TS. Effects of green brazilian propolis alcohol extract on nociceptive pain models in rats. Plants. 2020;9(9):1102. doi: 10.3390/plants9091102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Zakaria ZA, Abdul Rahim MH, Mohd Sani MH, Omar MH, Ching SM, Abdul Kadir A, Ahmed QU. Antinociceptive activity of petroleum ether fraction obtained from methanolic extract of Clinacanthus nutans leaves involves the activation of opioid receptors and NO-mediated/cGMP-independent pathway. BMC Complement Altern Med. 2019;19(1):79. doi: 10.1186/s12906-019-2486-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ribeiro RA, Vale ML, Thomazzi SM, Paschoalato AB, Poole S, Ferreira SH, Cunha FQ. Involvement of resident macrophages and mast cells in the writhing nociceptive response induced by zymosan and acetic acid in mice. Eur J Pharmacol. 2000;387(1):111–118. doi: 10.1016/s0014-2999(99)00790-6. [DOI] [PubMed] [Google Scholar]
- 163.Ledón N, Casacó A, González R, Merino N, González A, Tolón Z. Antipsoriatic, anti-inflammatory, and analgesic effects of an extract of red propolis. Zhongguo Yao Li Xue Bao. 1997;18(3):274–276. [PubMed] [Google Scholar]
- 164.Paulino N, Teixeira C, Martins R, Scremin A, Dirsch VM, Vollmar AM, Abreu SR, de Castro SL, Marcucci MC. Evaluation of the analgesic and anti-inflammatory effects of a Brazilian green propolis. Planta Med. 2006;72(10):899–906. doi: 10.1055/s-2006-947185. [DOI] [PubMed] [Google Scholar]
- 165.Paulino N, Dantas AP, Bankova V, Longhi DT, Scremin A, de Castro SL, Calixto JB. Bulgarian propolis induces analgesic and anti-inflammatory effects in mice and inhibits in vitro contraction of airway smooth muscle. J Pharmacol Sci. 2003;93(3):307–313. doi: 10.1254/jphs.93.307. [DOI] [PubMed] [Google Scholar]
- 166.Junior OD, Andreucci VC, da Silva Cunha IB, Araujo CEP, de Oliveira F, Marcucci MC. Investigation of the anti-inflammatory and analgesic activities of a sample of Brazilian propolis. Acta Farm Bonaerense. 2004;23(3):285–291. [Google Scholar]
- 167.Sokeng SD, Talla E, Sakava P, Fokam Tagne MA, Henoumont C, Sophie L, Mbafor JT, Tchuenguem Fohouo F-N. Anti-inflammatory and analgesic effect of arachic acid ethyl ester isolated from propolis. Biomed Res Int. 2020;2020:8797284. doi: 10.1155/2020/8797284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Lima Cavendish R, de Souza SJ, Belo Neto R, Oliveira Paixão A, Valéria Oliveira J, Divino de Araujo E, Berretta ESAA, Maria Thomazzi S, Cordeiro Cardoso J, Zanardo Gomes M. Antinociceptive and anti-inflammatory effects of Brazilian red propolis extract and formononetin in rodents. J Ethnopharmacol. 2015;173:127–133. doi: 10.1016/j.jep.2015.07.022. [DOI] [PubMed] [Google Scholar]
- 169.Sun L, Liao L, Wang B. Potential antinociceptive effects of Chinese propolis and identification on its active compounds. J Immunol Res. 2018;2018:5429543. doi: 10.1155/2018/5429543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Parandin R, Daroogari S. Anti-inflammatory and antinociceptive activities of the ethanolic extract of propolis in male mice and rats. Zahedan J Res Med Sci. 2019 doi: 10.5812/zjrms.84150. [DOI] [Google Scholar]
- 171.Atta AH, Alkofahi A. Anti-nociceptive and anti-inflammatory effects of some Jordanian medicinal plant extracts. J Ethnopharmacol. 1998;60(2):117–124. doi: 10.1016/s0378-8741(97)00137-2. [DOI] [PubMed] [Google Scholar]
- 172.Adzu B, Amos S, Wambebe C, Gamaniel K. Antinociceptive activity of Zizyphus spina-christi root bark extract. Fitoterapia. 2001;72(4):344–350. doi: 10.1016/s0367-326x(00)00289-6. [DOI] [PubMed] [Google Scholar]
- 173.Castro SL. Propolis: biological and pharmacological activities. therapeutic uses of this bee-product. Annu Rev Biomed Sci. 2001;3:49–83. doi: 10.5016/1806-8774.2001v3p49. [DOI] [Google Scholar]
- 174.Corrêa CR, Calixto JB. Evidence for participation of B1 and B2 kinin receptors in formalin-induced nociceptive response in the mouse. Br J Pharmacol. 1993;110(1):193–198. doi: 10.1111/j.1476-5381.1993.tb13791.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Malmberg AB, Yaksh TL. Cyclooxygenase inhibition and the spinal release of prostaglandin E2 and amino acids evoked by paw formalin injection: a microdialysis study in unanesthetized rats. J Neurosci. 1995;15(4):2768–2776. doi: 10.1523/jneurosci.15-04-02768.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Greenaway W, Scaysbrook T, Whatley FR. The composition and plant origins of propolis: a report of work at Oxford. Bee World. 1990;71(3):107–118. doi: 10.1080/0005772X.1990.11099047. [DOI] [Google Scholar]
- 177.García-Viguera C, Greenaway WT, Whatley FR. Composition of propolis from two different Spanish Regions. Zeitschrift für Naturforschung C. 1992;47:634–637. doi: 10.1515/znc-1992-7-824. [DOI] [Google Scholar]
- 178.Maciejewicz W, Daniewski M, Mielniczuk Z, Suprynowicz Z. Gas chromatography-mass spectrometry investigation of propolis-analysis of beta-steroids. Acta Pol Pharm. 1982;39(4):277–279. [Google Scholar]
- 179.Szliszka E, Mertas A, Czuba ZP, Król W. Inhibition of Inflammatory Response by Artepillin C in Activated RAW264.7 macrophages. Evid Based Complement Alternat Med. 2013;2013:735176. doi: 10.1155/2013/735176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Bachiega TF, Orsatti CL, Pagliarone AC, Sforcin JM. The effects of propolis and its isolated compounds on cytokine production by murine macrophages. Phytother Res. 2012;26(9):1308–1313. doi: 10.1002/ptr.3731. [DOI] [PubMed] [Google Scholar]
- 181.Alqarni AM, Niwasabutra K, Sahlan M, Fearnley H, Fearnley J, Ferro VA, Watson DG. Propolis Exerts an Anti-Inflammatory Effect on PMA-Differentiated THP-1 Cells via Inhibition of Purine Nucleoside Phosphorylase. Metabolites. 2019 doi: 10.3390/metabo9040075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Funakoshi-Tago M, Okamoto K, Izumi R, Tago K, Yanagisawa K, Narukawa Y, Kiuchi F, Kasahara T, Tamura H. Anti-inflammatory activity of flavonoids in Nepalese propolis is attributed to inhibition of the IL-33 signaling pathway. Int Immunopharmacol. 2015;25(1):189–198. doi: 10.1016/j.intimp.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 183.Blonska M, Bronikowska J, Pietsz G, Czuba ZP, Scheller S, Krol W. Effects of ethanol extract of propolis (EEP) and its flavones on inducible gene expression in J774A1 macrophages. J Ethnopharmacol. 2004;91(1):25–30. doi: 10.1016/j.jep.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 184.Rossi A, Ligresti A, Longo R, Russo A, Borrelli F, Sautebin L. The inhibitory effect of propolis and caffeic acid phenethyl ester on cyclooxygenase activity in J774 macrophages. Phytomedicine. 2002;9(6):530–535. doi: 10.1078/09447110260573164. [DOI] [PubMed] [Google Scholar]
- 185.Song JJ, Lim HW, Kim K, Kim KM, Cho S, Chae SW. Effect of caffeic acid phenethyl ester (CAPE) on H2O2 induced oxidative and inflammatory responses in human middle ear epithelial cells. Int J Pediatr Otorhinolaryngol. 2012;76(5):675–679. doi: 10.1016/j.ijporl.2012.01.041. [DOI] [PubMed] [Google Scholar]
- 186.Bezerra RM, Veiga LF, Caetano AC, Rosalen PL, Amaral ME, Palanch AC, de Alencar SM. Caffeic acid phenethyl ester reduces the activation of the nuclear factor κB pathway by high-fat diet-induced obesity in mice. Metabolism. 2012;61(11):1606–1614. doi: 10.1016/j.metabol.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 187.Azevedo MI, Pereira AF, Nogueira RB, Rolim FE, Brito GA, Wong DV, Lima-Júnior RC, de Albuquerque RR, Vale ML. The antioxidant effects of the flavonoids rutin and quercetin inhibit oxaliplatin-induced chronic painful peripheral neuropathy. Mol Pain. 2013;9:53. doi: 10.1186/1744-8069-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Silva JC, Rodrigues S, Feás X, Estevinho LM. Antimicrobial activity, phenolic profile and role in the inflammation of propolis. Food Chem Toxicol. 2012;50(5):1790–1795. doi: 10.1016/j.fct.2012.02.097. [DOI] [PubMed] [Google Scholar]
- 189.Ikeda R, Yanagisawa M, Takahashi N, Kawada T, Kumazawa S, Yamaotsu N, Nakagome I, Hirono S. Tsuda T (2011) Brazilian propolis-derived components inhibit TNF-α-mediated downregulation of adiponectin expression via different mechanisms in 3T3-L1 adipocytes. Biochim Biophys Acta. 1810;7:695–703. doi: 10.1016/j.bbagen.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 190.de Moura SA, Negri G, Salatino A, Lima LD, Dourado LP, Mendes JB, Andrade SP, Ferreira MA, Cara DC. Aqueous extract of brazilian green propolis: primary components, evaluation of inflammation and wound healing by using subcutaneous implanted sponges. Evid Based Complement Alternat Med. 2011;2011:748283. doi: 10.1093/ecam/nep112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Paulino N, Abreu SR, Uto Y, Koyama D, Nagasawa H, Hori H, Dirsch VM, Vollmar AM, Scremin A, Bretz WA. Anti-inflammatory effects of a bioavailable compound, Artepillin C. Brazilian propolis Eur J Pharmacol. 2008;587(1–3):296–301. doi: 10.1016/j.ejphar.2008.02.067. [DOI] [PubMed] [Google Scholar]
- 192.Tani H, Hasumi K, Tatefuji T, Hashimoto K, Koshino H, Takahashi S. Inhibitory activity of Brazilian green propolis components and their derivatives on the release of cys-leukotrienes. Bioorg Med Chem. 2010;18(1):151–157. doi: 10.1016/j.bmc.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 193.Khayyal MT, el-Ghazaly MA, el-Khatib AS, Mechanisms involved in the antiinflammatory effect of propolis extract. Drugs Exp Clin Res. 1993;19(5):197–203. [PubMed] [Google Scholar]
- 194.Park E-H, Kim S-H, Park S-S. Anti-inflammatory activity of propolis. Arch Pharmacal Res. 1996;19(5):337–341. doi: 10.1007/BF02976375. [DOI] [Google Scholar]
- 195.Borrelli F, Maffia P, Pinto L, Ianaro A, Russo A, Capasso F, Ialenti A. Phytochemical compounds involved in the anti-inflammatory effect of propolis extract. Fitoterapia. 2002;73(Suppl 1):S53–63. doi: 10.1016/s0367-326x(02)00191-0. [DOI] [PubMed] [Google Scholar]
- 196.Lin WW, Karin M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J Clin Invest. 2007;117(5):1175–1183. doi: 10.1172/jci31537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Bueno-Silva B, Alencar SM, Koo H, Ikegaki M, Silva GV, Napimoga MH, Rosalen PL. Anti-inflammatory and antimicrobial evaluation of neovestitol and vestitol isolated from Brazilian red propolis. J Agric Food Chem. 2013;61(19):4546–4550. doi: 10.1021/jf305468f. [DOI] [PubMed] [Google Scholar]
- 198.Franchin M, Cólon DF, Castanheira FV, da Cunha MG, Bueno-Silva B, Alencar SM, Cunha TM, Rosalen PL. Vestitol isolated from brazilian red propolis inhibits neutrophils migration in the inflammatory process: elucidation of the mechanism of action. J Nat Prod. 2016;79(4):954–960. doi: 10.1021/acs.jnatprod.5b00938. [DOI] [PubMed] [Google Scholar]
- 199.Franchin M, Colón DF, da Cunha MG, Castanheira FV, Saraiva AL, Bueno-Silva B, Alencar SM, Cunha TM, Rosalen PL. Neovestitol, an isoflavonoid isolated from Brazilian red propolis, reduces acute and chronic inflammation: involvement of nitric oxide and IL-6. Sci Rep. 2016;6:36401. doi: 10.1038/srep36401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Bueno-Silva B, Rosalen PL, Alencar SM, Mayer MPA. Anti-inflammatory mechanisms of neovestitol from Brazilian red propolis in LPS-activated macrophages. J Funct Foods. 2017;36:440–447. doi: 10.1016/j.jff.2017.07.029. [DOI] [Google Scholar]
- 201.Ertürküner SP, Yaprak Saraç E, Göçmez SS, Ekmekçi H, Öztürk ZB, Seçkin İ, Sever Ö, Keskinbora K. Anti-inflammatory and ultrastructural effects of Turkish propolis in a rat model of endotoxin-induced uveitis. Folia Histochem Cytobiol. 2016;54(1):49–57. doi: 10.5603/FHC.a2016.0004. [DOI] [PubMed] [Google Scholar]
- 202.Du Toit K, Buthelezi S, Bodenstein J. Anti-inflammatory and antibacterial profiles of selected compounds found in South African propolis. S Afr J Sci. 2009;105:470–472. [Google Scholar]
- 203.Jung YC, Kim ME, Yoon JH, Park PR, Youn HY, Lee HW, Lee JS. Anti-inflammatory effects of galangin on lipopolysaccharide-activated macrophages via ERK and NF-κB pathway regulation. Immunopharmacol Immunotoxicol. 2014;36(6):426–432. doi: 10.3109/08923973.2014.968257. [DOI] [PubMed] [Google Scholar]
- 204.Cardenas H, Arango D, Nicholas C, Duarte S, Nuovo GJ, He W, Voss OH, Gonzalez-Mejia ME, Guttridge DC, Grotewold E, Doseff AI. Dietary apigenin exerts immune-regulatory activity in vivo by reducing NF-κB activity, halting leukocyte infiltration and restoring normal metabolic function. Int J Mol Sci. 2016;17(3):323. doi: 10.3390/ijms17030323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Zhang X, Wang G, Gurley EC, Zhou H. Flavonoid apigenin inhibits lipopolysaccharide-induced inflammatory response through multiple mechanisms in macrophages. PLoS ONE. 2014;9(9):e107072. doi: 10.1371/journal.pone.0107072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Santos EO, Kabeya LM, Figueiredo-Rinhel AS, Marchi LF, Andrade MF, Piatesi F, Paoliello-Paschoalato AB, Azzolini AE, Lucisano-Valim YM. Flavonols modulate the effector functions of healthy individuals' immune complex-stimulated neutrophils: a therapeutic perspective for rheumatoid arthritis. Int Immunopharmacol. 2014;21(1):102–111. doi: 10.1016/j.intimp.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 207.Tiveron AP, Rosalen PL, Franchin M, Lacerda RC, Bueno-Silva B, Benso B, Denny C, Ikegaki M, Alencar SM. Chemical characterization and antioxidant, antimicrobial, and anti-inflammatory activities of south brazilian organic propolis. PLoS ONE. 2016;11(11):e0165588. doi: 10.1371/journal.pone.0165588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Wang K, Hu L, Jin X-L, Ma Q-X, Marcucci MC, Netto AAL, Sawaya ACHF, Huang S, Ren W-K, Conlon MA, Topping DL, Hu F-L. Polyphenol-rich propolis extracts from China and Brazil exert anti-inflammatory effects by modulating ubiquitination of TRAF6 during the activation of NF-κB. J Funct Foods. 2015;19:464–478. doi: 10.1016/j.jff.2015.09.009. [DOI] [Google Scholar]
- 209.Batista CM, Alves AVF, Queiroz LA, Lima BS, Filho RNP, Araújo AAS, de Albuquerque Júnior RLC, Cardoso JC. The photoprotective and anti-inflammatory activity of red propolis extract in rats. J Photochem Photobiol B. 2018;180:198–207. doi: 10.1016/j.jphotobiol.2018.01.028. [DOI] [PubMed] [Google Scholar]
- 210.Wang Y, Zhu Y, Gao L, Yin H, Xie Z, Wang D, Zhu Z, Han X. Formononetin attenuates IL-1β-induced apoptosis and NF-κB activation in INS-1 cells. Molecules. 2012;17(9):10052–10064. doi: 10.3390/molecules170910052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Shi H, Yang H, Zhang X, Yu LL. Identification and quantification of phytochemical composition and anti-inflammatory and radical scavenging properties of methanolic extracts of Chinese propolis. J Agric Food Chem. 2012;60(50):12403–12410. doi: 10.1021/jf3042775. [DOI] [PubMed] [Google Scholar]
- 212.Soromou LW, Chu X, Jiang L, Wei M, Huo M, Chen N, Guan S, Yang X, Chen C, Feng H, Deng X. In vitro and in vivo protection provided by pinocembrin against lipopolysaccharide-induced inflammatory responses. Int Immunopharmacol. 2012;14(1):66–74. doi: 10.1016/j.intimp.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 213.Kumar S, Sharma A, Madan B, Singhal V, Ghosh B. Isoliquiritigenin inhibits IkappaB kinase activity and ROS generation to block TNF-alpha induced expression of cell adhesion molecules on human endothelial cells. Biochem Pharmacol. 2007;73(10):1602–1612. doi: 10.1016/j.bcp.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 214.Feng G, Sun B, Li TZ. Daidzein attenuates lipopolysaccharide-induced acute lung injury via toll-like receptor 4/NF-kappaB pathway. Int Immunopharmacol. 2015;26(2):392–400. doi: 10.1016/j.intimp.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 215.Shi H, Yang H, Zhang X, Sheng Y, Huang H, Yu L. Isolation and characterization of five glycerol esters from Wuhan propolis and their potential anti-inflammatory properties. J Agric Food Chem. 2012;60(40):10041–10047. doi: 10.1021/jf302601m. [DOI] [PubMed] [Google Scholar]
- 216.Inui S, Hosoya T, Yoshizumi K, Sato H, Kumazawa S. Phytochemical and anti-inflammatory properties of Senegalese propolis and isolated compounds. Fitoterapia. 2021;151:104861. doi: 10.1016/j.fitote.2021.104861. [DOI] [PubMed] [Google Scholar]
- 217.Hu F, Hepburn HR, Li Y, Chen M, Radloff SE, Daya S. Effects of ethanol and water extracts of propolis (bee glue) on acute inflammatory animal models. J Ethnopharmacol. 2005;100(3):276–283. doi: 10.1016/j.jep.2005.02.044. [DOI] [PubMed] [Google Scholar]
- 218.Guzman-Gutierrez SL, Nieto-Camacho A, Castillo-Arellano JI, Huerta-Salazar E, Hernandez-Pasteur G, Silva-Miranda M, Arguello-Najera O, Sepulveda-Robles O, Espitia CI, Reyes-Chilpa R. Mexican propolis: a source of antioxidants and anti-inflammatory compounds, and isolation of a novel chalcone and epsilon-caprolactone derivative. Molecules. 2018 doi: 10.3390/molecules23020334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Tamfu AN, Sawalda M, Fotsing MT, Kouipou RMT, Talla E, Chi GF, Epanda JJE, Mbafor JT, Baig TA, Jabeen A, Shaheen F. A new isoflavonol and other constituents from Cameroonian propolis and evaluation of their anti-inflammatory, antifungal and antioxidant potential. Saudi J Biol Sci. 2020;27(6):1659–1666. doi: 10.1016/j.sjbs.2019.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Shahinozzaman M, Taira N, Ishii T, Halim MA, Hossain MA, Tawata S. Anti-inflammatory, anti-diabetic, and anti-alzheimer's effects of prenylated flavonoids from Okinawa Propolis: an investigation by experimental and computational studies. Molecules. 2018 doi: 10.3390/molecules23102479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Nna VU, Abu Bakar AB, Md Lazin M, Mohamed M. Antioxidant, anti-inflammatory and synergistic anti-hyperglycemic effects of Malaysian propolis and metformin in streptozotocin-induced diabetic rats. Food Chem Toxicol. 2018;120:305–320. doi: 10.1016/j.fct.2018.07.028. [DOI] [PubMed] [Google Scholar]
- 222.Zeitoun R, Najjar F, Wehbi B, Khalil A, Fayyad-Kazan M, Dagher-Hamalian C, Faour WH, El-Makhour Y. Chemical composition, antioxidant and anti-inflammatory activity evaluation of the lebanese propolis extract. Curr Pharm Biotechnol. 2019;20(1):84–96. doi: 10.2174/1389201020666190206201241. [DOI] [PubMed] [Google Scholar]
- 223.Linard C, Marquette C, Mathieu J, Pennequin A, Clarençon D, Mathé D. Acute induction of inflammatory cytokine expression after gamma-irradiation in the rat: effect of an NF-kappaB inhibitor. Int J Radiat Oncol Biol Phys. 2004;58(2):427–434. doi: 10.1016/j.ijrobp.2003.09.039. [DOI] [PubMed] [Google Scholar]
- 224.Búfalo MC, Ferreira I, Costa G, Francisco V, Liberal J, Cruz MT, Lopes MC, Batista MT, Sforcin JM. Propolis and its constituent caffeic acid suppress LPS-stimulated pro-inflammatory response by blocking NF-κB and MAPK activation in macrophages. J Ethnopharmacol. 2013;149(1):84–92. doi: 10.1016/j.jep.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 225.Chinthammit C, Axon DR, Mollon L, Taylor AM, Pickering M, Black H, Warholak T, Campbell PJ. Evaluating the relationship between quality measure adherence definitions and economic outcomes in commercial health plans: a retrospective diabetes cohort study. J Manag Care Spec Pharm. 2021;27(1):64–72. doi: 10.18553/jmcp.2021.27.1.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Chiba S. Molecular mechanism in alpha-glucosidase and glucoamylase. Biosci Biotechnol Biochem. 1997;61(8):1233–1239. doi: 10.1271/bbb.61.1233. [DOI] [PubMed] [Google Scholar]
- 227.Vongsak B, Kongkiatpaiboon S, Jaisamut S, Machana S, Pattarapanich C. In vitro alpha glucosidase inhibition and free-radical scavenging activity of propolis from Thai stingless bees in mangosteen orchard. Rev Bras. 2015;25(5):445–450. doi: 10.1016/j.bjp.2015.07.004. [DOI] [Google Scholar]
- 228.Alaribe CS, Esposito T, Sansone F, Sunday A, Pagano I, Piccinelli AL, Celano R, Cuesta Rubio O, Coker HA, Nabavi SM, Rastrelli L, Picerno P. Nigerian propolis: chemical composition, antioxidant activity and α-amylase and α-glucosidase inhibition. Nat Prod Res. 2021;35(18):3095–3099. doi: 10.1080/14786419.2019.1682576. [DOI] [PubMed] [Google Scholar]
- 229.Zamami Y, Takatori S, Koyama T, Goda M, Iwatani Y, Doi S, Kawasaki H. Effect of propolis on insulin resistance in fructose-drinking rats. Yakugaku Zasshi. 2007;127(12):2065–2073. doi: 10.1248/yakushi.127.2065. [DOI] [PubMed] [Google Scholar]
- 230.Fuliang HU, Hepburn HR, Xuan H, Chen M, Daya S, Radloff SE. Effects of propolis on blood glucose, blood lipid and free radicals in rats with diabetes mellitus. Pharmacol Res. 2005;51(2):147–152. doi: 10.1016/j.phrs.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 231.El Menyiy N, Al-Wali N, El Ghouizi A, El-Guendouz S, Salom K, Lyoussi B. Potential therapeutic effect of Moroccan propolis in hyperglycemia, dyslipidemia, and hepatorenal dysfunction in diabetic rats. Iran J Basic Med Sci. 2019;22(11):1331–1339. doi: 10.22038/ijbms.2019.33549.8004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Nna VU, Abu Bakar AB, Ahmad A, Eleazu CO, Mohamed M. Oxidative Stress, NF-kappaB-Mediated Inflammation and Apoptosis in the Testes of Streptozotocin-Induced Diabetic Rats: Combined Protective Effects of Malaysian Propolis and Metformin. Antioxidants (Basel) 2019 doi: 10.3390/antiox8100465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Laaroussi H, Bakour M, Ousaaid D, Aboulghazi A, Ferreira-Santos P, Genisheva Z, Teixeira JA, Lyoussi B. Effect of antioxidant-rich propolis and bee pollen extracts against D-glucose induced type 2 diabetes in rats. Food Res Int. 2020;138(Pt B):109802. doi: 10.1016/j.foodres.2020.109802. [DOI] [PubMed] [Google Scholar]
- 234.Rivera-Yañez N, Rodriguez-Canales M, Nieto-Yañez O, Jimenez-Estrada M, Ibarra-Barajas M, Canales-Martinez MM, Rodriguez-Monroy MA. Hypoglycaemic and antioxidant effects of propolis of chihuahua in a model of experimental diabetes. Evid Based Complement Alternat Med. 2018;2018:4360356. doi: 10.1155/2018/4360356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Babatunde IR, Abdulbasit A, Oladayo MI, Olasile OI, Olamide FR, Gbolahan BW. Hepatoprotective and pancreatoprotective properties of the ethanolic extract of nigerian propolis. J Intercult Ethnopharmacol. 2015;4(2):102–108. doi: 10.5455/jice.20150202023615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Zhu W, Chen M, Shou Q, Li Y, Hu F. Biological activities of chinese propolis and Brazilian propolis on streptozotocin-induced type 1 diabetes mellitus in rats. Evid Based Complement Alternat Med. 2011;2011:468529. doi: 10.1093/ecam/neq025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.el El-Sayed SM, Abo-Salem OM, Aly HA, Mansour AM. Potential antidiabetic and hypolipidemic effects of propolis extract in streptozotocin-induced diabetic rats. Pak J Pharm Sci. 2009;22(2):168–174. [PubMed] [Google Scholar]
- 238.Pujirahayu N, Bhattacharjya DK, Suzuki T, Katayama T. alpha-glucosidase inhibitory activity of cycloartane-type triterpenes isolated from indonesian stingless bee propolis and their structure-activity relationship. Pharmaceuticals (Basel) 2019 doi: 10.3390/ph12030102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Popova M, Lyoussi B, Aazza S, Antunes D, Bankova V, Miguel G. Antioxidant and α-Glucosidase Inhibitory Properties and Chemical Profiles of Moroccan Propolis. Nat Prod Commun. 2015;10(11):1961–1964. [PubMed] [Google Scholar]
- 240.Boucher J, Kleinridders A, Kahn CR. Insulin receptor signaling in normal and insulin-resistant states. Cold Spring Harb Perspect Biol. 2014 doi: 10.1101/cshperspect.a009191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Liu Y, Liang X, Zhang G, Kong L, Peng W, Zhang H. Galangin and Pinocembrin from Propolis Ameliorate Insulin Resistance in HepG2 Cells via Regulating Akt/mTOR Signaling. Evid Based Complement Alternat Med. 2018;2018:7971842. doi: 10.1155/2018/7971842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Kang LJ, Lee HB, Bae HJ, Lee SG. Antidiabetic effect of propolis: reduction of expression of glucose-6-phosphatase through inhibition of Y279 and Y216 autophosphorylation of GSK-3α/β in HepG2 cells. Phytother Res. 2010;24(10):1554–1561. doi: 10.1002/ptr.3147. [DOI] [PubMed] [Google Scholar]
- 243.Nie J, Chang Y, Li Y, Zhou Y, Qin J, Sun Z, Li H. Caffeic Acid Phenethyl Ester (Propolis Extract) Ameliorates Insulin Resistance by Inhibiting JNK and NF-κB Inflammatory Pathways in Diabetic Mice and HepG2 Cell Models. J Agric Food Chem. 2017;65(41):9041–9053. doi: 10.1021/acs.jafc.7b02880. [DOI] [PubMed] [Google Scholar]
- 244.Salah NM, Souleman AMA, Shaker KH, Hawary SSE, El-hady FKA. Acetylcholinesterase, Alpha-Glucosidase and Tyrosinase Inhibitors from Egyptian Propolis. Int J Pharmacogn Phytochem Res. 2017;9:528–536. [Google Scholar]
- 245.Hegazy SS, Helmy H, Salama MS, Lotfy NM, Mahmoud DM. The Anti-Diabetic Effect of Nano-Encapsulated Propolis from Apis mellifera on Type 2 Diabetes. Current Appl Sci Technol. 2021;6:88–103. [Google Scholar]
- 246.Ichi I, Hori H, Takashima Y, Adachi N, Kataoka R, Okihara K, Hashimoto K, Kojo S. The beneficial effect of propolis on fat accumulation and lipid metabolism in rats fed a high-fat diet. J Food Sci. 2009;74(5):H127–131. doi: 10.1111/j.1750-3841.2009.01147.x. [DOI] [PubMed] [Google Scholar]
- 247.Daleprane JB, Freitas Vda S, Pacheco A, Rudnicki M, Faine LA, Dörr FA, Ikegaki M, Salazar LA, Ong TP, Abdalla DS. Anti-atherogenic and anti-angiogenic activities of polyphenols from propolis. J Nutr Biochem. 2012;23(6):557–566. doi: 10.1016/j.jnutbio.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 248.Anvarifard P, Anbari M, Ostadrahimi A, Ardalan M, Ghoreishi Z. A comprehensive insight into the molecular and cellular mechanisms of the effects of Propolis on preserving renal function: a systematic review. Nutr Metab (Lond) 2022;19(1):6. doi: 10.1186/s12986-021-00639-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Rojczyk E, Klama-Baryła A, Łabuś W, Wilemska-Kucharzewska K, Kucharzewski M. Historical and modern research on propolis and its application in wound healing and other fields of medicine and contributions by Polish studies. J Ethnopharmacol. 2020;262:113159. doi: 10.1016/j.jep.2020.113159. [DOI] [PubMed] [Google Scholar]
- 250.Medellín-Luna MF, Castañeda-Delgado JE, Martínez-Balderas VY, Cervantes-Villagrana AR. Medicinal plant extracts and their use as wound closure inducing agents. J Med Food. 2019;22(5):435–443. doi: 10.1089/jmf.2018.0145. [DOI] [PubMed] [Google Scholar]
- 251.Cardoso RL, Maboni F, Machado G, Alves SH, de Vargas AC. Antimicrobial activity of propolis extract against Staphylococcus coagulase positive and Malassezia pachydermatis of canine otitis. Vet Microbiol. 2010;142(3–4):432–434. doi: 10.1016/j.vetmic.2009.09.070. [DOI] [PubMed] [Google Scholar]
- 252.Ramadan A, Soliman G, Mahmoud SS, Nofal SM, Abdel-Rahman RF. Evaluation of the safety and antioxidant activities of Crocus sativus and Propolis ethanolic extracts. J Saudi Chem Soc. 2012;16(1):13–21. doi: 10.1016/j.jscs.2010.10.012. [DOI] [Google Scholar]
- 253.Ramos IFdAS, Biz MT, Paulino N, Scremin A, Della Bona Á, Barletta FB, de Figueiredo JAP. Histopathological analysis of corticosteroid-antibiotic preparation and propolis paste formulation as intracanal medication after pulpectomy: an in vivo study. J Appl Oral Sci. 2012;20:50–56. doi: 10.1590/S1678-77572012000100010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Martinotti S, Pellavio G, Laforenza U, Ranzato E. Propolis Induces AQP3 expression: a possible way of action in wound healing. Molecules. 2019 doi: 10.3390/molecules24081544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Li Z, Van Bergen T, Van de Veire S, Van de Vel I, Moreau H, Dewerchin M, Maudgal PC, Zeyen T, Spileers W, Moons L, Stalmans I. Inhibition of vascular endothelial growth factor reduces scar formation after glaucoma filtration surgery. Invest Ophthalmol Vis Sci. 2009;50(11):5217–5225. doi: 10.1167/iovs.08-2662. [DOI] [PubMed] [Google Scholar]
- 256.Westergren-Thorsson G, Bagher M, Andersson-Sjöland A, Thiman L, Löfdahl CG, Hallgren O, Bjermer L, Larsson-Callerfelt AK. VEGF synthesis is induced by prostacyclin and TGF-β in distal lung fibroblasts from COPD patients and control subjects: Implications for pulmonary vascular remodelling. Respirology. 2018;23(1):68–75. doi: 10.1111/resp.13142. [DOI] [PubMed] [Google Scholar]
- 257.Jacob A, Parolia A, Pau A, Davamani Amalraj F. The effects of Malaysian propolis and Brazilian red propolis on connective tissue fibroblasts in the wound healing process. BMC Complement Altern Med. 2015;15:294. doi: 10.1186/s12906-015-0814-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Kyriakides TR, Zhu YH, Yang Z, Huynh G, Bornstein P. Altered extracellular matrix remodeling and angiogenesis in sponge granulomas of thrombospondin 2-null mice. Am J Pathol. 2001;159(4):1255–1262. doi: 10.1016/s0002-9440(10)62512-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Iyyam Pillai S, Palsamy P, Subramanian S, Kandaswamy M. Wound healing properties of Indian propolis studied on excision wound-induced rats. Pharm Biol. 2010;48(11):1198–1206. doi: 10.3109/13880200903578754. [DOI] [PubMed] [Google Scholar]
- 260.Cao XP, Chen YF, Zhang JL, You MM, Wang K, Hu FL. Mechanisms underlying the wound healing potential of propolis based on its in vitro antioxidant activity. Phytomedicine. 2017;34:76–84. doi: 10.1016/j.phymed.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 261.Khorasgani A. A comparison of healing effects of propolis and silver sulfadiazine on full thickness skin wounds in rats. Pak Vet J. 2010;30(2):72–74. [Google Scholar]
- 262.Noli C, Miolo A. The mast cell in wound healing. Vet Dermatol. 2001;12(6):303–313. doi: 10.1046/j.0959-4493.2001.00272.x. [DOI] [PubMed] [Google Scholar]
- 263.Weller K, Foitzik K, Paus R, Syska W, Maurer M. Mast cells are required for normal healing of skin wounds in mice. Faseb j. 2006;20(13):2366–2368. doi: 10.1096/fj.06-5837fje. [DOI] [PubMed] [Google Scholar]
- 264.Barroso PR, Lopes-Rocha R, Pereira EM, Marinho SA, de Miranda JL, Lima NL, Verli FD. Effect of propolis on mast cells in wound healing. Inflammopharmacology. 2012;20(5):289–294. doi: 10.1007/s10787-011-0105-5. [DOI] [PubMed] [Google Scholar]
- 265.Cho MS, Park WS, Jung WK, Qian ZJ, Lee DS, Choi JS, Lee DY, Park SG, Seo SK, Kim HJ, Won JY, Yu BC, Choi IW. Caffeic acid phenethyl ester promotes anti-inflammatory effects by inhibiting MAPK and NF-κB signaling in activated HMC-1 human mast cells. Pharm Biol. 2014;52(7):926–932. doi: 10.3109/13880209.2013.865243. [DOI] [PubMed] [Google Scholar]
- 266.Nader MA. Caffeic acid phenethyl ester attenuates IgE-induced immediate allergic reaction. Inflammopharmacology. 2013;21(2):169–176. doi: 10.1007/s10787-012-0138-4. [DOI] [PubMed] [Google Scholar]
- 267.Nakamura R, Nakamura R, Watanabe K, Oka K, Ohta S, Mishima S, Teshima R. Effects of propolis from different areas on mast cell degranulation and identification of the effective components in propolis. Int Immunopharmacol. 2010;10(9):1107–1112. doi: 10.1016/j.intimp.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 268.Bae Y, Lee S, Kim SH. Chrysin suppresses mast cell-mediated allergic inflammation: involvement of calcium, caspase-1 and nuclear factor-κB. Toxicol Appl Pharmacol. 2011;254(1):56–64. doi: 10.1016/j.taap.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 269.Daleprane JB, Abdalla DS. Emerging roles of propolis: antioxidant, cardioprotective, and antiangiogenic actions. Evid Based Complement Alternat Med. 2013;2013:175135. doi: 10.1155/2013/175135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Parihar A, Parihar MS, Milner S, Bhat S. Oxidative stress and anti-oxidative mobilization in burn injury. Burns. 2008;34(1):6–17. doi: 10.1016/j.burns.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 271.Olczyk P, Ramos P, Komosinska-Vassev K, Stojko J, Pilawa B. Positive effect of propolis on free radicals in burn wounds. Evid Based Complement Alternat Med. 2013;2013:356737. doi: 10.1155/2013/356737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Valente MJ, Baltazar AF, Henrique R, Estevinho L, Carvalho M. Biological activities of Portuguese propolis: protection against free radical-induced erythrocyte damage and inhibition of human renal cancer cell growth in vitro. Food Chem Toxicol. 2011;49(1):86–92. doi: 10.1016/j.fct.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 273.Okinczyc P, Widelski J, Szperlik J, Zuk M, Mroczek T, Skalicka-Wozniak K, Sakipova Z, Widelska G, Kus PM. Impact of plant origin on Eurasian propolis on phenolic profile and classical antioxidant activity. Biomolecules. 2021 doi: 10.3390/biom11010068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Mohammadzadeh S, Sharriatpanahi M, Hamedi M, Amanzadeh Y, Sadat Ebrahimi SE, Ostad SN. Antioxidant power of Iranian propolis extract. Food Chem. 2007;103(3):729–733. doi: 10.1016/j.foodchem.2006.09.014. [DOI] [Google Scholar]
- 275.Najafi MF, Vahedy F, Seyyedin M, Jomehzadeh HR, Bozary K. Effect of the water extracts of propolis on stimulation and inhibition of different cells. Cytotechnology. 2007;54(1):49–56. doi: 10.1007/s10616-007-9067-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Niyonsaba F, Ushio H, Nakano N, Ng W, Sayama K, Hashimoto K, Nagaoka I, Okumura K, Ogawa H. Antimicrobial peptides human beta-defensins stimulate epidermal keratinocyte migration, proliferation and production of proinflammatory cytokines and chemokines. J Invest Dermatol. 2007;127(3):594–604. doi: 10.1038/sj.jid.5700599. [DOI] [PubMed] [Google Scholar]
- 277.Wang T, Chen L, Wu W, Long Y, Wang R. Potential cytoprotection: antioxidant defence by caffeic acid phenethyl ester against free radical-induced damage of lipids, DNA, and proteins. Can J Physiol Pharmacol. 2008;86(5):279–287. doi: 10.1139/y08-029. [DOI] [PubMed] [Google Scholar]
- 278.Alberti TB, Coelho DS, de Prá M, Maraschin M, Veleirinho B. Electrospun PVA nanoscaffolds associated with propolis nanoparticles with wound healing activity. J Mater Sci. 2020;55(23):9712–9727. doi: 10.1007/s10853-020-04502-z. [DOI] [Google Scholar]
- 279.Baygar T. Characterization of silk sutures coated with propolis and biogenic silver nanoparticles (AgNPs); an eco-friendly solution with wound healing potential against surgical site infections (SSIs) Turk J Med Sci. 2020;50(1):258–266. doi: 10.3906/sag-1906-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Eskandarinia A, Kefayat A, Gharakhloo M, Agheb M, Khodabakhshi D, Khorshidi M, Sheikhmoradi V, Rafienia M, Salehi H. A propolis enriched polyurethane-hyaluronic acid nanofibrous wound dressing with remarkable antibacterial and wound healing activities. Int J Biol Macromol. 2020;149:467–476. doi: 10.1016/j.ijbiomac.2020.01.255. [DOI] [PubMed] [Google Scholar]
- 281.Afonso AM, Gonçalves J, Luís Â, Gallardo E, Duarte AP. Evaluation of the In Vitro Wound-Healing Activity and Phytochemical Characterization of Propolis and Honey. Appl Sci 2020;10 (5):1845
- 282.Al-Waili N. Mixing two different propolis samples potentiates their antimicrobial activity and wound healing property: a novel approach in wound healing and infection. Vet World. 2018;11(8):1188–1195. doi: 10.14202/vetworld.2018.1188-1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Abu-Seida AM. Effect of propolis on experimental cutaneous wound healing in dogs. Vet Med Int. 2015;2015:672643. doi: 10.1155/2015/672643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Voss GT, Gularte MS, Vogt AG, Giongo JL, Vaucher RA, Echenique JVZ, Soares MP, Luchese C, Wilhelm EA, Fajardo AR. Polysaccharide-based film loaded with vitamin C and propolis: A promising device to accelerate diabetic wound healing. Int J Pharm. 2018;552(1–2):340–351. doi: 10.1016/j.ijpharm.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 285.Hara-Chikuma M, Verkman AS. Aquaporin-3 facilitates epidermal cell migration and proliferation during wound healing. J Mol Med (Berl) 2008;86(2):221–231. doi: 10.1007/s00109-007-0272-4. [DOI] [PubMed] [Google Scholar]
- 286.Islam MT, Sarkar C, El-Kersh DM, Jamaddar S, Uddin SJ, Shilpi JA, Mubarak MS. Natural products and their derivatives against coronavirus: A review of the non-clinical and pre-clinical data. Phytother Res. 2020;34(10):2471–2492. doi: 10.1002/ptr.6700. [DOI] [PubMed] [Google Scholar]
- 287.Sarkar C, Mondal M, Torequl Islam M, Martorell M, Docea AO, Maroyi A, Sharifi-Rad J, Calina D. Potential Therapeutic Options for COVID-19: current status, challenges, and future perspectives. Front Pharmacol. 2020;11:572870. doi: 10.3389/fphar.2020.572870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Sarkar C, Jamaddar S, Mondal M, Khalipha ABR, Islam MT, Mubarak MS. Natural Products as Anti-COVID-19 Agents: An In Silico Study. Coronaviruses. 2021 doi: 10.2174/2666796701999201116124851. [DOI] [Google Scholar]
- 289.Mondal M, Sarkar C, Jamaddar S, Khalipha ABR, Islam MT, Mahafzah A, Mubarak MS. Evaluation of the binding affinity of anti-viral drugs against main protease of SARS-CoV-2 through a Molecular Docking Study. Infect Disord Drug Targets. 2020 doi: 10.2174/1871526520666201207124408. [DOI] [PubMed] [Google Scholar]
- 290.Lavinas FC, Macedo EHBC, Sá GBL, Amaral ACF, Silva JRA, Azevedo MMB, Vieira BA, Domingos TFS, Vermelho AB, Carneiro CS, Rodrigues IA. Brazilian stingless bee propolis and geopropolis: promising sources of biologically active compounds. Rev Bras. 2019;29(3):389–399. doi: 10.1016/j.bjp.2018.11.007. [DOI] [Google Scholar]
- 291.Sarkar C, Jamaddar S, Mollick B, Akter M, Ahmed T, Mahir M, Mondal M, Islam M. Importance and the unique aspects of modalities for conducting non-clinical and pre-clinical studies of compartmental and non- compartmental analysis. Pharmacologyonline. 2019;3:1–15. [Google Scholar]
- 292.Bachevski D, Damevska K, Simeonovski V, Dimova M. Back to the basics: Propolis and COVID-19. Dermatol Ther. 2020;33(4):e13780–e13780. doi: 10.1111/dth.13780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Magnavacca A, Sangiovanni E, Racagni G, Dell'Agli M. The antiviral and immunomodulatory activities of propolis: An update and future perspectives for respiratory diseases. Med Res Rev. 2022;42(2):897–945. doi: 10.1002/med.21866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Schnitzler P, Neuner A, Nolkemper S, Zundel C, Nowack H, Sensch KH, Reichling J. Antiviral activity and mode of action of propolis extracts and selected compounds. Phytother Res. 2010;24(Suppl 1):S20–28. doi: 10.1002/ptr.2868. [DOI] [PubMed] [Google Scholar]
- 295.Nolkemper S, Reichling J, Sensch KH, Schnitzler P. Mechanism of herpes simplex virus type 2 suppression by propolis extracts. Phytomedicine. 2010;17(2):132–138. doi: 10.1016/j.phymed.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 296.Huleihel M, Isanu V. Anti-herpes simplex virus effect of an aqueous extract of propolis. Isr Med Assoc J. 2002;4(11 Suppl):923–927. [PubMed] [Google Scholar]
- 297.González-Búrquez MJ, González-Díaz FR, García-Tovar CG, Carrillo-Miranda L, Soto-Zárate CI, Canales-Martínez MM, Penieres-Carrillo JG, Crúz-Sánchez TA, Fonseca-Coronado S. Comparison between in vitro antiviral effect of mexican propolis and three commercial flavonoids against canine distemper virus. Evid Based Complement Alternat Med. 2018;2018:7092416. doi: 10.1155/2018/7092416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Shevchenko LF, Chasovodtseva OA, Peschanskii AN. Inhibiting activity of propolis on the influenza virus. Chem Abstr. 1972;82:11. [Google Scholar]
- 299.Kwon MJ, Shin HM, Perumalsamy H, Wang X, Ahn Y-J. Antiviral effects and possible mechanisms of action of constituents from Brazilian propolis and related compounds. J Apic Res. 2020;59(4):413–425. doi: 10.1080/00218839.2019.1695715. [DOI] [Google Scholar]
- 300.Amoros M, Simões CM, Girre L, Sauvager F, Cormier M. Synergistic effect of flavones and flavonols against herpes simplex virus type 1 in cell culture. Comparison with the antiviral activity of propolis. J Nat Prod. 1992;55(12):1732–1740. doi: 10.1021/np50090a003. [DOI] [PubMed] [Google Scholar]
- 301.Amoros M, Lurton E, Boustie J, Girre L, Sauvager F, Cormier M. Comparison of the anti-herpes simplex virus activities of propolis and 3-methyl-but-2-enyl caffeate. J Nat Prod. 1994;57(5):644–647. doi: 10.1021/np50107a013. [DOI] [PubMed] [Google Scholar]
- 302.Guler HI, Tatar G, Yildiz O, Belduz AO, Kolayli S. Investigation of potential inhibitor properties of ethanolic propolis extracts against ACE-II receptors for COVID-19 treatment by molecular docking study. Arch Microbiol. 2021;203(6):3557–3564. doi: 10.1007/s00203-021-02351-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Guler HI, Sal FA, Can Z, Kara Y, Yildiz O, Belduz AO, Çanakci S, Kolayli S. Targeting CoV-2 Spike RBD and ACE-2 Interaction with Flavonoids of Anatolian Propolis by in silico and in vitro Studies in terms of possible COVID-19 therapeutics. Turk J Biol. 2021;45:530–548. doi: 10.3906/biy-2104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Refaat H, Mady FM, Sarhan HA, Rateb HS, Alaaeldin E. Optimization and evaluation of propolis liposomes as a promising therapeutic approach for COVID-19. Int J Pharm. 2021;592:120028. doi: 10.1016/j.ijpharm.2020.120028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Sahlan M, Irdiani R, Flamandita D, Aditama R, Alfarraj S, Ansari MJ, Khayrani AC, Pratami DK, Lischer K. Molecular interaction analysis of Sulawesi propolis compounds with SARS-CoV-2 main protease as preliminary study for COVID-19 drug discovery. J King Saud Univ Sci. 2021;33(1):101234. doi: 10.1016/j.jksus.2020.101234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Kumar V, Dhanjal JK, Bhargava P, Kaul A, Wang J, Zhang H, Kaul SC, Wadhwa R, Sundar D. Withanone and Withaferin-A are predicted to interact with transmembrane protease serine 2 (TMPRSS2) and block entry of SARS-CoV-2 into cells. J Biomol Struct Dyn. 2020 doi: 10.1080/07391102.2020.1775704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Kumar V, Dhanjal JK, Kaul SC, Wadhwa R, Sundar D. Withanone and caffeic acid phenethyl ester are predicted to interact with main protease (M(pro)) of SARS-CoV-2 and inhibit its activity. J Biomol Struct Dyn. 2021;39(11):3842–3854. doi: 10.1080/07391102.2020.1772108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Harisna AH, Nurdiansyah R, Syaifie PH, Nugroho DW, Saputro KE, Firdayani PCD, Rochman NT, Maulana NN, Noviyanto A, Mardliyati E. In silico investigation of potential inhibitors to main protease and spike protein of SARS-CoV-2 in propolis. Biochem Biophys Rep. 2021;26:100969. doi: 10.1016/j.bbrep.2021.100969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Khayrani AC, Irdiani R, Aditama R, Pratami DK, Lischer K, Ansari MJ, Chinnathambi A, Alharbi SA, Almoallim HS, Sahlan M. Evaluating the potency of Sulawesi propolis compounds as ACE-2 inhibitors through molecular docking for COVID-19 drug discovery preliminary study. J King Saud Univ Sci. 2021;33(2):101297. doi: 10.1016/j.jksus.2020.101297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Shaldam MA, Yahya G, Mohamed NH, Abdel-Daim MM, Al Naggar Y. In silico screening of potent bioactive compounds from honeybee products against COVID-19 target enzymes. Environ Sci Pollut Res Int. 2021;28(30):40507–40514. doi: 10.1007/s11356-021-14195-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Berretta AA, Silveira MAD, Cóndor Capcha JM, De Jong D. Propolis and its potential against SARS-CoV-2 infection mechanisms and COVID-19 disease: Running title: Propolis against SARS-CoV-2 infection and COVID-19. Biomed Pharmacother. 2020;131:110622. doi: 10.1016/j.biopha.2020.110622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Yosri N, Abd El-Wahed AA, Ghonaim R, Khattab OM, Sabry A, Ibrahim MAA, Moustafa MF, Guo Z, Zou X, Algethami AFM, Masry SHD, AlAjmi MF, Afifi HS, Khalifa SAM, El-Seedi HR. Anti-viral and immunomodulatory properties of propolis: chemical diversity, pharmacological properties, preclinical and clinical applications, and in silico potential against SARS-CoV-2. Foods. 2021;10(8):1776. doi: 10.3390/foods10081776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Reis JS, Oliveira GB, Monteiro MC, Machado CS, Torres YR, Prediger RD, Maia CS. Antidepressant- and anxiolytic-like activities of an oil extract of propolis in rats. Phytomedicine. 2014;21(11):1466–1472. doi: 10.1016/j.phymed.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 314.Lu Y, Wu C, Yuan Z. Determination of hesperetin, cinnamic acid and nicotinic acid in propolis with micellar electrokinetic capillary chromatography. Fitoterapia. 2004;75(3–4):267–276. doi: 10.1016/j.fitote.2003.12.026. [DOI] [PubMed] [Google Scholar]
- 315.Silva MdSSd, Citó AMdGL, Chaves MH, Lopes JAD. Triterpenóides tipo cicloartano de própolis de Teresina - PI. Quim Nova. 2005;28(5):801–804. doi: 10.1590/s0100-40422005000500013. [DOI] [Google Scholar]
- 316.Albuquerque IL, Alves LA, Lemos TLG, Monte FJQ, Braz-Filho R. Ácido canárico (3,4-seco derivado do lupano) em própolis do Ceará. Quim Nova. 2007 doi: 10.1590/s0100-40422007000400013. [DOI] [Google Scholar]
- 317.Lee MS, Kim YH, Park WS, Ahn WG, Park OK, Kwon SH, Morita K, Shim I, Her S. Novel antidepressant-like activity of propolis extract mediated by enhanced glucocorticoid receptor function in the hippocampus. Evid Based Complement Alternat Med. 2013;2013:217853. doi: 10.1155/2013/217853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Ha J, Choi HS, Lee Y, Lee ZH, Kim HH. Caffeic acid phenethyl ester inhibits osteoclastogenesis by suppressing NF kappaB and downregulating NFATc1 and c-Fos. Int Immunopharmacol. 2009;9(6):774–780. doi: 10.1016/j.intimp.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 319.Filho CB, Jesse CR, Donato F, Del Fabbro L, de Gomes MG, Goes ATR, Souza LC, Giacomeli R, Antunes M, Luchese C, Roman SS, Boeira SP. Neurochemical factors associated with the antidepressant-like effect of flavonoid chrysin in chronically stressed mice. Eur J Pharmacol. 2016;791:284–296. doi: 10.1016/j.ejphar.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 320.Filho CB, Jesse CR, Donato F, Giacomeli R, Del Fabbro L, da Silva AM, de Gomes MG, Goes AT, Boeira SP, Prigol M, Souza LC. Chronic unpredictable mild stress decreases BDNF and NGF levels and Na(+), K(+)-ATPase activity in the hippocampus and prefrontal cortex of mice: antidepressant effect of chrysin. Neuroscience. 2015;289:367–380. doi: 10.1016/j.neuroscience.2014.12.048. [DOI] [PubMed] [Google Scholar]
- 321.Li YJ, Xuan HZ, Shou QY, Zhan ZG, Lu X, Hu FL. Therapeutic effects of propolis essential oil on anxiety of restraint-stressed mice. Hum Exp Toxicol. 2012;31(2):157–165. doi: 10.1177/0960327111412805. [DOI] [PubMed] [Google Scholar]
- 322.Prut L, Belzung C. The open field as a paradigm to measure the effects of drugs on anxiety-like behaviors: a review. Eur J Pharmacol. 2003;463(1–3):3–33. doi: 10.1016/s0014-2999(03)01272-x. [DOI] [PubMed] [Google Scholar]
- 323.Moody TW, Merali Z, Crawley JN. The effects of anxiolytics and other agents on rat grooming behavior. Ann N Y Acad Sci. 1988;525:281–290. doi: 10.1111/j.1749-6632.1988.tb38613.x. [DOI] [PubMed] [Google Scholar]
- 324.Hellner M, Winter D, von Georgi R, Münstedt K. Apitherapy: usage and experience in german beekeepers. Evid Based Complement Alternat Med. 2008;5(4):475–479. doi: 10.1093/ecam/nem052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Zhu F, Wongsiri S. A Brief Introduction to Apitherapy Health Care. J Thai Tradit Altern Med. 2018;3:303–312. [Google Scholar]
- 326.Popova M, Dimitrova R, Al-Lawati HT, Tsvetkova I, Najdenski H, Bankova V. Omani propolis: chemical profiling, antibacterial activity and new propolis plant sources. Chem Cent J. 2013;7(1):158–158. doi: 10.1186/1752-153X-7-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Díaz-Carballo D, Ueberla K, Kleff V, Ergun S, Malak S, Freistuehler M, Somogyi S, Kücherer C, Bardenheuer W, Strumberg D. Antiretroviral activity of two polyisoprenylated acylphloroglucinols, 7-epi-nemorosone and plukenetione A, isolated from Caribbean propolis. Int J Clin Pharmacol Ther. 2010;48(10):670–677. doi: 10.5414/cpp48670. [DOI] [PubMed] [Google Scholar]
- 328.Farooqui T, Farooqui A. Molecular mechanism underlying the therapeutic activities of propolis: a critical review. Curr Nutr Food Sci. 2010;6(3):186–199. doi: 10.2174/157340110792389136. [DOI] [Google Scholar]
- 329.Farooqui T, Farooqui AA. Beneficial effects of propolis on human health and neurological diseases. Front Biosci (Elite Ed) 2012;4:779–793. doi: 10.2741/418. [DOI] [PubMed] [Google Scholar]
- 330.Kurek-Górecka A, Rzepecka-Stojko A, Górecki M, Stojko J, Sosada M, Swierczek-Zieba G. Structure and antioxidant activity of polyphenols derived from propolis. Molecules. 2013;19(1):78–101. doi: 10.3390/molecules19010078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Elkhenany H, El-Badri N, Dhar M. Green propolis extract promotes in vitro proliferation, differentiation, and migration of bone marrow stromal cells. Biomed Pharmacother. 2019;115:108861. doi: 10.1016/j.biopha.2019.108861. [DOI] [PubMed] [Google Scholar]
- 332.Pobiega K, Kraśniewska K, Gniewosz M. Application of propolis in antimicrobial and antioxidative protection of food quality – A review. Trends Food Sci Technol. 2019;83:53–62. doi: 10.1016/j.tifs.2018.11.007. [DOI] [Google Scholar]
- 333.Ueda T, Inden M, Shirai K, Sekine SI, Masaki Y, Kurita H, Ichihara K, Inuzuka T, Hozumi I. The effects of Brazilian green propolis that contains flavonols against mutant copper-zinc superoxide dismutase-mediated toxicity. Sci Rep. 2017;7(1):2882. doi: 10.1038/s41598-017-03115-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Silva FB, Almeida JM, Sousa SM. Natural medicaments in endodontics – a comparative study of the anti-inflammatory action. Braz Oral Res. 2004;18(2):174–179. doi: 10.1590/s1806-83242004000200015. [DOI] [PubMed] [Google Scholar]
- 335.Matsushige K, Basnet P, Hase K, Kadota S, Tanaka K, Namba T. Propolis protects pancreatic β-cells against the toxicity of streptozotocin (STZ) Phytomedicine. 1996;3(2):203–209. doi: 10.1016/s0944-7113(96)80037-7. [DOI] [PubMed] [Google Scholar]
- 336.Lima ZP, Severi JA, Pellizzon CH, Brito AR, Solis PN, Cáceres A, Girón LM, Vilegas W, Hiruma-Lima CA. Can the aqueous decoction of mango flowers be used as an antiulcer agent? J Ethnopharmacol. 2006;106(1):29–37. doi: 10.1016/j.jep.2005.11.032. [DOI] [PubMed] [Google Scholar]
- 337.de Barros MP, Sousa JP, Bastos JK, de Andrade SF. Effect of Brazilian green propolis on experimental gastric ulcers in rats. J Ethnopharmacol. 2007;110(3):567–571. doi: 10.1016/j.jep.2006.10.022. [DOI] [PubMed] [Google Scholar]
- 338.Barros MP, Lemos M, Maistro EL, Leite MF, Sousa JP, Bastos JK, Andrade SF. Evaluation of antiulcer activity of the main phenolic acids found in Brazilian Green Propolis. J Ethnopharmacol. 2008;120(3):372–377. doi: 10.1016/j.jep.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 339.Jang MH, Piao XL, Kim JM, Kwon SW, Park JH. Inhibition of cholinesterase and amyloid-beta aggregation by resveratrol oligomers from Vitis amurensis. Phytother Res. 2008;22(4):544–549. doi: 10.1002/ptr.2406. [DOI] [PubMed] [Google Scholar]
- 340.Boeing T, Mejía JAA, Ccana-Ccapatinta GV, Mariott M, Vilhena M, de Andrade Fonseca Da Silva RdC, de Souza P, Mariano LNB, Oliveira GR, da Rocha IM, da Costa GA, de Andrade SF, da Silva LM, Bastos JK, The gastroprotective effect of red propolis extract from Northeastern Brazil and the role of its isolated compounds. J Ethnopharmacol. 2021;267:113623. doi: 10.1016/j.jep.2020.113623. [DOI] [PubMed] [Google Scholar]
- 341.Shinmei Y, Yano H, Kagawa Y, Izawa K, Akagi M, Inoue T, Kamei C. Effect of Brazilian propolis on sneezing and nasal rubbing in experimental allergic rhinitis of mice. Immunopharmacol Immunotoxicol. 2009;31(4):688–693. doi: 10.3109/08923970903078443. [DOI] [PubMed] [Google Scholar]
- 342.Hellgren J, Cervin A, Nordling S, Bergman A, Cardell LO. Allergic rhinitis and the common cold–high cost to society. Allergy. 2010;65(6):776–783. doi: 10.1111/j.1398-9995.2009.02269.x. [DOI] [PubMed] [Google Scholar]
- 343.Sy LB, Wu YL, Chiang BL, Wang YH, Wu WM. Propolis extracts exhibit an immunoregulatory activity in an OVA-sensitized airway inflammatory animal model. Int Immunopharmacol. 2006;6(7):1053–1060. doi: 10.1016/j.intimp.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 344.Khayyal MT, el-Ghazaly MA, el-Khatib AS, Hatem AM, de Vries PJ, el-Shafei S, Khattab MM, A clinical pharmacological study of the potential beneficial effects of a propolis food product as an adjuvant in asthmatic patients. Fundam Clin Pharmacol. 2003;17(1):93–102. doi: 10.1046/j.1472-8206.2003.00117.x. [DOI] [PubMed] [Google Scholar]
- 345.Perrotta S, Gallagher PG, Mohandas N. Hereditary spherocytosis. Lancet. 2008;372(9647):1411–1426. doi: 10.1016/s0140-6736(08)61588-3. [DOI] [PubMed] [Google Scholar]
- 346.Satchwell TJ, Shoemark DK, Sessions RB, Toye AM. Protein 42: a complex linker. Blood Cells Mol Dis. 2009;42(3):201–210. doi: 10.1016/j.bcmd.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 347.Trompeter S, King M-J. Hereditary spherocytosis. Paediatr Child Health. 2019;29(8):359–364. doi: 10.1016/j.paed.2019.05.006. [DOI] [Google Scholar]
- 348.Moreira LL, Dias T, Dias LG, Rogão M, Da Silva JP, Estevinho LM. Propolis influence on erythrocyte membrane disorder (hereditary spherocytosis): a first approach. Food Chem Toxicol. 2011;49(2):520–526. doi: 10.1016/j.fct.2010.11.042. [DOI] [PubMed] [Google Scholar]
- 349.Spinelli S, Conte A, Lecce L, Incoronato AL, Del Nobile MA. Microencapsulated propolis to enhance the antioxidant properties of fresh fish burgers. J Food Process Eng. 2015;38(6):527–535. doi: 10.1111/jfpe.12183. [DOI] [Google Scholar]
- 350.Vargas-Sánchez RD, Torrescano-Urrutia GR, Acedo-Félix E, Carvajal-Millán E, González-Córdova AF, Vallejo-Galland B, Torres-Llanez MJ, Sánchez-Escalante A. Antioxidant and antimicrobial activity of commercial propolis extract in beef patties. J Food Sci. 2014;79(8):C1499–C1504. doi: 10.1111/1750-3841.12533. [DOI] [PubMed] [Google Scholar]
- 351.Cottica SM, Sabik H, Bélanger D, Giroux HJ, Visentainer JV, Britten M. Use of propolis extracts as antioxidant in dairy beverages enriched with conjugated linoleic acid. Eur Food Res Technol. 2015;241(4):543–551. doi: 10.1007/s00217-015-2483-1. [DOI] [Google Scholar]
- 352.Akpinar GC, Canogullari S, Baylan M, Alasahan S, Aygun A. The use of propolis extract for the storage of quail eggs. J Appl Poultry Res. 2015;24(4):427–435. doi: 10.3382/japr/pfv043. [DOI] [Google Scholar]
- 353.Greenaway W, Scaysbrook T, Whatley FR. The analysis of bud exudate of Populus x euramericana, and of propolis, by gas chromatography–mass spectrometry. Proc R Soc Lond B. 1987;232(1268):249–272. doi: 10.1098/rspb.1987.0073. [DOI] [Google Scholar]
- 354.Vanhaelen M, Van Haelen Fastre R. Propolis. II: Identification par chromatographies haute-performance (liquide gaz-liquide et sur couches minces) des constituants. Bioautographie des chromatogrammes des composes antibacteriens. Belgique apicole; 1979. [PubMed]
- 355.Vanhaelen M, Van Haelen Fastre R. Propolis. I: Origine, Micrographie, Composition Chimique Et Activite Therapeutique. Belgique apicole; 1979. [PubMed]
- 356.Vanhaelen M, Vanhaelen-Fastré R. High-performance liquid, gas-liquid and thin-layer chromatography of naturally occurring flavonoids, phenolic and related compounds. J Chromatogr A. 1980;187:225–260. doi: 10.1016/S0021-9673(00)87897-8. [DOI] [Google Scholar]
- 357.Moreira TF. Composição química da própolis: vitaminas e aminoácidos. Rev Bras. 1986;1(1):12–19. doi: 10.1590/s0102-695x1986000100003. [DOI] [Google Scholar]
- 358.García-Viguera C, Ferreres F, Tomás-Barberán FA. Study of Canadian Propolis by GC-MS and HPLC. Zeitschrift für Naturforschung C. 1993;48(9–10):731–735. doi: 10.1515/znc-1993-9-1009. [DOI] [Google Scholar]
- 359.Bankova V, Dyulgerov A, Popov S, Evstatieva L, Kuleva L, Pureb O, Zamjansan Z. Propolis produced in Bulgaria and Mongolia: phenolic compounds and plant origin. Apidologie. 1992;23(1):79–85. doi: 10.1051/apido:19920109. [DOI] [Google Scholar]
- 360.Righi AA, Alves TR, Negri G, Marques LM, Breyer H, Salatino A. Brazilian red propolis: unreported substances, antioxidant and antimicrobial activities. J Sci Food Agric. 2011;91(13):2363–2370. doi: 10.1002/jsfa.4468. [DOI] [PubMed] [Google Scholar]
- 361.Li F, Awale S, Tezuka Y, Kadota S. Cytotoxic constituents from Brazilian red propolis and their structure-activity relationship. Bioorg Med Chem. 2008;16(10):5434–5440. doi: 10.1016/j.bmc.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 362.Villanueva VR, Barbier M, Gonnet M, Lavie P. The flavonoids of propolis Isolation of a new bacteriostatic substance: pinocembrin (dihydroxy-5, 7 flavanone)] Ann Inst Pasteur (Paris). 1970;118(1):84–87. [PubMed] [Google Scholar]
- 363.Ghisalberti EL, Jefferies PR, Lanteri R, Matisons J. Constituents of propolis. Experientia. 1978;34(2):157–158. doi: 10.1007/bf01944648. [DOI] [Google Scholar]
- 364.Bankova VS, Popov SS, Marekov NL. A Study on Flavonoids of Propolis. J Nat Prod. 1983;46(4):471–474. doi: 10.1021/np50028a007. [DOI] [Google Scholar]
- 365.Tran VH, Duke RK, Abu-Mellal A, Duke CC. Propolis with high flavonoid content collected by honey bees from Acacia paradoxa. Phytochemistry. 2012;81:126–132. doi: 10.1016/j.phytochem.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 366.Falcão SI, Vilas-Boas M, Estevinho LM, Barros C, Domingues MR, Cardoso SM. Phenolic characterization of Northeast Portuguese propolis: usual and unusual compounds. Anal Bioanal Chem. 2010;396(2):887–897. doi: 10.1007/s00216-009-3232-8. [DOI] [PubMed] [Google Scholar]
- 367.Shrestha SP, Narukawa Y, Takeda T. Chemical constituents of Nepalese propolis: isolation of new dalbergiones and related compounds. J Nat Med. 2007;61(1):73–76. doi: 10.1007/s11418-006-0024-8. [DOI] [Google Scholar]
- 368.Inui S, Shimamura Y, Masuda S, Shirafuji K, Moli RT, Kumazawa S. A new prenylflavonoid isolated from propolis collected in the Solomon Islands. Biosci Biotechnol Biochem. 2012;76(5):1038–1040. doi: 10.1271/bbb.120021. [DOI] [PubMed] [Google Scholar]
- 369.Chen CN, Wu CL, Shy HS, Lin JK. Cytotoxic prenylflavanones from Taiwanese propolis. J Nat Prod. 2003;66(4):503–506. doi: 10.1021/np0203180. [DOI] [PubMed] [Google Scholar]
- 370.Li F, He YM, Awale S, Kadota S, Tezuka Y. Two new cytotoxic phenylallylflavanones from Mexican propolis. Chem Pharm Bull (Tokyo) 2011;59(9):1194–1196. doi: 10.1248/cpb.59.1194. [DOI] [PubMed] [Google Scholar]
- 371.Melliou E, Chinou I. Chemical analysis and antimicrobial activity of Greek propolis. Planta Med. 2004;70(6):515–519. doi: 10.1055/s-2004-827150. [DOI] [PubMed] [Google Scholar]
- 372.Usia T, Banskota AH, Tezuka Y, Midorikawa K, Matsushige K, Kadota S. Constituents of Chinese propolis and their antiproliferative activities. J Nat Prod. 2002;65(5):673–676. doi: 10.1021/np010486c. [DOI] [PubMed] [Google Scholar]
- 373.Cao YH, Wang Y, Yuan Q. Analysis of flavonoids and phenolic acid in propolis by capillary electrophoresis. Chromatographia. 2004;59:135–140. doi: 10.1365/s10337-003-0138-z. [DOI] [Google Scholar]
- 374.Maciejewicz W. Isolation of flavonoid aglycones from propolis by a column chromatography method and their identification by Gc-Ms and Tlc Methods. J Liq Chromatogr Relat Technol. 2006;24(8):1171–1179. doi: 10.1081/jlc-100103439. [DOI] [Google Scholar]
- 375.Hegazi AG, Hady FK. Egyptian propolis: 3 Antioxidant, antimicrobial activities and chemical composition of propolis from reclaimed lands. Z Naturforsch C J Biosci. 2002;57(3–4):395–402. doi: 10.1515/znc-2002-3-432. [DOI] [PubMed] [Google Scholar]
- 376.Petrova A, Popova M, Kuzmanova C, Tsvetkova I, Naydenski H, Muli E, Bankova V. New biologically active compounds from Kenyan propolis. Fitoterapia. 2010;81(6):509–514. doi: 10.1016/j.fitote.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 377.Alencar SM, Oldoni TL, Castro ML, Cabral IS, Costa-Neto CM, Cury JA, Rosalen PL, Ikegaki M. Chemical composition and biological activity of a new type of Brazilian propolis: red propolis. J Ethnopharmacol. 2007;113(2):278–283. doi: 10.1016/j.jep.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 378.Piccinelli AL, Campo Fernandez M, Cuesta-Rubio O, Márquez Hernández I, De Simone F, Rastrelli L. Isoflavonoids isolated from Cuban propolis. J Agric Food Chem. 2005;53(23):9010–9016. doi: 10.1021/jf0518756. [DOI] [PubMed] [Google Scholar]
- 379.Campo Fernández M, Cuesta-Rubio O, Rosado Perez A, De Oca M, Porto R, Márquez Hernández I, Piccinelli AL, Rastrelli L. GC-MS determination of isoflavonoids in seven red Cuban propolis samples. J Agric Food Chem. 2008;56(21):9927–9932. doi: 10.1021/jf801870f. [DOI] [PubMed] [Google Scholar]
- 380.Sha N, Guan SH, Lu ZQ, Chen GT, Huang HL, Xie FB, Yue QX, Liu X, Guo DA. Cytotoxic constituents of chinese propolis. J Nat Prod. 2009;72(4):799–801. doi: 10.1021/np900118z. [DOI] [PubMed] [Google Scholar]
- 381.Lotti C, Campo Fernandez M, Piccinelli AL, Cuesta-Rubio O, Márquez Hernández I, Rastrelli L. Chemical constituents of red Mexican propolis. J Agric Food Chem. 2010;58(4):2209–2213. doi: 10.1021/jf100070w. [DOI] [PubMed] [Google Scholar]
- 382.Awale S, Shrestha SP, Tezuka Y, Ueda JY, Matsushige K, Kadota S. Neoflavonoids and related constituents from Nepalese propolis and their nitric oxide production inhibitory activity. J Nat Prod. 2005;68(6):858–864. doi: 10.1021/np050009k. [DOI] [PubMed] [Google Scholar]
- 383.Seifert M. Haslinger E (1991) Über die Inhaltsstoffe der Propolis. II Liebigs Annalen der Chemie. 1991;2:93–97. doi: 10.1002/jlac.199119910118. [DOI] [Google Scholar]
- 384.Seifert M. Haslinger E (1989) Über die Inhaltsstoffe der Propolis. I Liebigs Annalen der Chemie. 1989;11:1123–1126. doi: 10.1002/jlac.198919890279. [DOI] [Google Scholar]
- 385.Oliveira AP, França HS, Kuster RM, Teixeira LA, Rocha LM. Chemical composition and antibacterial activity of Brazilian propolis essential oil. J Venomous Animals Toxins Trop Dis. 2010;16(1):121–130. doi: 10.1590/s1678-91992010005000007. [DOI] [Google Scholar]
- 386.Melliou E, Stratis E, Chinou I. Volatile constituents of propolis from various regions of Greece – Antimicrobial activity. Food Chem. 2007;103(2):375–380. doi: 10.1016/j.foodchem.2006.07.033. [DOI] [Google Scholar]
- 387.Trusheva B, Todorov I, Ninova M, Najdenski H, Daneshmand A, Bankova V. Antibacterial mono- and sesquiterpene esters of benzoic acids from Iranian propolis. Chem Cent J. 2010;4:8. doi: 10.1186/1752-153x-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Silici S, Kutluca S. Chemical composition and antibacterial activity of propolis collected by three different races of honeybees in the same region. J Ethnopharmacol. 2005;99(1):69–73. doi: 10.1016/j.jep.2005.01.046. [DOI] [PubMed] [Google Scholar]
- 389.Popova MP, Graikou K, Chinou I, Bankova VS. GC-MS profiling of diterpene compounds in Mediterranean propolis from Greece. J Agric Food Chem. 2010;58(5):3167–3176. doi: 10.1021/jf903841k. [DOI] [PubMed] [Google Scholar]
- 390.Popova MP, Chinou IB, Marekov IN, Bankova VS. Terpenes with antimicrobial activity from Cretan propolis. Phytochemistry. 2009;70(10):1262–1271. doi: 10.1016/j.phytochem.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 391.Pereira AS, Nascimento EA, de Aquino NF. Lupeol alkanoates in Brazilian propolis. Z Naturforsch C J Biosci. 2002;57(7–8):721–726. doi: 10.1515/znc-2002-7-829. [DOI] [PubMed] [Google Scholar]
- 392.Márquez Hernández I, Cuesta-Rubio O, Campo Fernández M, Rosado Pérez A, de Oca M, Porto R, Piccinelli AL, Rastrelli L. Studies on the constituents of yellow Cuban propolis: GC-MS determination of triterpenoids and flavonoids. J Agric Food Chem. 2010;58(8):4725–4730. doi: 10.1021/jf904527n. [DOI] [PubMed] [Google Scholar]
- 393.Li F, Awale S, Zhang H, Tezuka Y, Esumi H, Kadota S. Chemical constituents of propolis from Myanmar and their preferential cytotoxicity against a human pancreatic cancer cell line. J Nat Prod. 2009;72(7):1283–1287. doi: 10.1021/np9002433. [DOI] [PubMed] [Google Scholar]
- 394.El-Hady FKA, Hegazi AG. Egyptian propolis: 2. Chemical composition, antiviral and antimicrobial activities of East Nile Delta propolis. Z Naturforsch C J Biosci. 2002;57(3–4):386–394. doi: 10.1515/znc-2002-3-431. [DOI] [PubMed] [Google Scholar]
- 395.Teixeira EW, Negri G, Meira RM, Message D, Salatino A. Plant Origin of Green Propolis: Bee Behavior, Plant Anatomy and Chemistry. Evid Based Complement Alternat Med. 2005;2(1):85–92. doi: 10.1093/ecam/neh055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Salatino A, Teixeira EW, Negri G, Message D. Origin and Chemical Variation of Brazilian Propolis. Evid Based Complement Alternat Med. 2005;2(1):33–38. doi: 10.1093/ecam/neh060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Marcucci MC, Ferreres F, García-Viguera C, Bankova VS, De Castro SL, Dantas AP, Valente PH, Paulino N. Phenolic compounds from Brazilian propolis with pharmacological activities. J Ethnopharmacol. 2001;74(2):105–112. doi: 10.1016/s0378-8741(00)00326-3. [DOI] [PubMed] [Google Scholar]
- 398.Abu-Mellal A, Koolaji N, Duke RK, Tran VH, Duke CC. Prenylated cinnamate and stilbenes from Kangaroo Island propolis and their antioxidant activity. Phytochemistry. 2012;77:251–259. doi: 10.1016/j.phytochem.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 399.dos Santos PA, de Miranda Pereira AF, Trugo LC, de Aquino Neto FR. Distribution of quinic acid derivatives and other phenolic compounds in Brazilian propolis. Z Naturforsch C J Biosci. 2003;58(7–8):590–593. doi: 10.1515/znc-2003-7-824. [DOI] [PubMed] [Google Scholar]
- 400.Matsui T, Ebuchi S, Fujise T, Abesundara KJ, Dopi S, Yamada H, Matsumoto K. Strong antihyperglycemic effects of water-soluble fraction of Brazilian propolis and its bioactive constituent, 3,4,5-tri-O-caffeoylquinic acid. Biol Pharm Bull. 2004;27(11):1797–1803. doi: 10.1248/bpb.27.1797. [DOI] [PubMed] [Google Scholar]
- 401.Marcucci MC, Ferreres F, Custódio AR, Ferreira MM, Bankova VS, García-Viguera C, Bretz WA. Evaluation of phenolic compounds in Brazilian propolis from different geographic regions. Z Naturforsch C J Biosci. 2000;55(1–2):76–81. doi: 10.1515/znc-2000-1-215. [DOI] [PubMed] [Google Scholar]
- 402.Trusheva B, Popova M, Koendhori EB, Tsvetkova I, Naydenski C, Bankova V. Indonesian propolis: chemical composition, biological activity and botanical origin. Nat Prod Res. 2011;25(6):606–613. doi: 10.1080/14786419.2010.488235. [DOI] [PubMed] [Google Scholar]
- 403.Syamsudin WS, Simanjunta P, Heffen WL. Chemical Composition of Propolis from Different Regions in Java and their Cytotoxic Activity. Am J Biochem Biotechnol. 2009;5(4):180–183. doi: 10.3844/ajbbsp.2009.180.183. [DOI] [Google Scholar]
- 404.Popova M, Trusheva B, Antonova D, Cutajar S, Mifsud D, Farrugia C, Tsvetkova I, Najdenski H, Bankova V. The specific chemical profile of Mediterranean propolis from Malta. Food Chem. 2011;126(3):1431–1435. doi: 10.1016/j.foodchem.2010.11.130. [DOI] [Google Scholar]
- 405.Talla E, Tamfu AN, Gade IS, Yanda L, Mbafor JT, Laurent S, Elst LV, Popova M, Bankova V. New mono-ether of glycerol and triterpenes with DPPH radical scavenging activity from Cameroonian propolis. Nat Prod Res. 2017;31(12):1379–1389. doi: 10.1080/14786419.2016.1253077. [DOI] [PubMed] [Google Scholar]
- 406.Papachroni D, Graikou K, Kosalec I, Damianakos H, Ingram V, Chinou I. Phytochemical analysis and biological evaluation of selected African propolis samples from Cameroon and Congo. Nat Prod Commun. 2015;10(1):67–70. [PubMed] [Google Scholar]
- 407.Kardar MN, Zhang T, Coxon GD, Watson DG, Fearnley J, Seidel V. Characterisation of triterpenes and new phenolic lipids in Cameroonian propolis. Phytochemistry. 2014;106:156–163. doi: 10.1016/j.phytochem.2014.07.016. [DOI] [PubMed] [Google Scholar]
- 408.Almutairi S, Eapen B, Chundi SM, Akhalil A, Siheri W, Clements C, Fearnley J, Watson DG, Edrada-Ebel R. New anti-trypanosomal active prenylated compounds from African propolis. Phytochem Lett. 2014;10:35–39. doi: 10.1016/j.phytol.2014.07.002. [DOI] [Google Scholar]
- 409.El-Bassuony A, AbouZid S. A new prenylated flavanoid with antibacterial activity from propolis collected in Egypt. Nat Prod Commun. 2010;5(1):43–45. [PubMed] [Google Scholar]
- 410.Omar R, Igoli JO, Zhang T, Gray AI, Ebiloma GU, Clements CJ, Fearnley J, Edrada Ebel R, Paget T, de Koning HP, Watson DG. The chemical characterization of nigerian propolis samples and their activity against Trypanosoma brucei. Sci Rep. 2017;7(1):923. doi: 10.1038/s41598-017-01038-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411.Blicharska N, Seidel V. Chemical diversity and biological activity of african propolis. Prog Chem Org Nat Prod. 2019;109:415–450. doi: 10.1007/978-3-030-12858-6_3. [DOI] [PubMed] [Google Scholar]
- 412.Piccinelli AL, Mencherini T, Celano R, Mouhoubi Z, Tamendjari A, Aquino RP, Rastrelli L. Chemical composition and antioxidant activity of Algerian propolis. J Agric Food Chem. 2013;61(21):5080–5088. doi: 10.1021/jf400779w. [DOI] [PubMed] [Google Scholar]
- 413.Boufadi YM, Soubhye J, Riazi A, Rousseau A, Vanhaeverbeek M, Nève J, Boudjeltia KZ, Van Antwerpen P. Characterization and antioxidant properties of six Algerian propolis extracts: ethyl acetate extracts inhibit myeloperoxidase activity. Int J Mol Sci. 2014;15(2):2327–2345. doi: 10.3390/ijms15022327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Segueni N, Magid AA, Decarme M, Rhouati S, Lahouel M, Antonicelli F, Lavaud C, Hornebeck W. Inhibition of stromelysin-1 by caffeic acid derivatives from a propolis sample from Algeria. Planta Med. 2011;77(10):999–1004. doi: 10.1055/s-0030-1270713. [DOI] [PubMed] [Google Scholar]
- 415.Ibrahim R, Wanas A, El-Din AA, Radwan M, Elsohly M, Metwally A. Isolation of eleven phenolic compounds from Propolis (Bee Glue) collected in Alexandria. Egypt. 2014 doi: 10.1055/s-0034-1382569. [DOI] [Google Scholar]
- 416.El Hady FA, Shaker KH, Imhoff JF, Zinecker H, Salah NM, Ibrahim AM. Bioactive Metabolites from Propolis Inhibit Superoxide Anion Radical, Acetylcholinesterase and Phosphodiesterase (PDE4) Int J Pharm Sci Rev Res. 2013;21:338–344. [Google Scholar]
- 417.Omar RM, Igoli J, Gray AI, Ebiloma GU, Clements C, Fearnley J, Ebel RA, Zhang T, De Koning HP, Watson DG. Chemical characterisation of Nigerian red propolis and its biological activity against Trypanosoma Brucei. Phytochem Anal. 2016;27(2):107–115. doi: 10.1002/pca.2605. [DOI] [PubMed] [Google Scholar]
- 418.Siheri W, Igoli JO, Gray AI, Nasciemento TG, Zhang T, Fearnley J, Clements CJ, Carter KC, Carruthers J, Edrada-Ebel R, Watson DG. The isolation of antiprotozoal compounds from Libyan propolis. Phytother Res. 2014;28(12):1756–1760. doi: 10.1002/ptr.5194. [DOI] [PubMed] [Google Scholar]
- 419.Siheri W, Ebiloma GU, Igoli JO, Gray AI, Biddau M, Akrachalanont P, Alenezi S, Alwashih MA, Edrada-Ebel R, Muller S, Lawrence CE, Fearnley J, Watson DG, De Koning HP. Isolation of a novel flavanonol and an alkylresorcinol with highly potent anti-trypanosomal activity from libyan propolis. Molecules (Basel, Switzerland) 2019;24(6):1041. doi: 10.3390/molecules24061041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Ito J, Chang FR, Wang HK, Park YK, Ikegaki M, Kilgore N, Lee KH. Anti-AIDS agents. 48.(1) Anti-HIV activity of moronic acid derivatives and the new melliferone-related triterpenoid isolated from Brazilian propolis. J Nat Prod. 2001;64(10):1278–1281. doi: 10.1021/np010211x. [DOI] [PubMed] [Google Scholar]
- 421.Nina N, Quispe C, Jiménez-Aspee F, Theoduloz C, Giménez A, Schmeda-Hirschmann G. Chemical profiling and antioxidant activity of Bolivian propolis. J Sci Food Agric. 2016;96(6):2142–2153. doi: 10.1002/jsfa.7330. [DOI] [PubMed] [Google Scholar]
- 422.Boeing T, Mejía JAA, Ccana-Ccapatinta GV, Mariott M, Vilhena M, de Andrade Fonseca Da Silva RC, de Souza P, Mariano LNB, Oliveira GR, da Rocha IM, da Costa GA, de Andrade SF, da Silva LM, Bastos JK, The gastroprotective effect of red propolis extract from Northeastern Brazil and the role of its isolated compounds. J Ethnopharmacol. 2021;267:113623. doi: 10.1016/j.jep.2020.113623. [DOI] [PubMed] [Google Scholar]
- 423.Tani H, Hikami S, Takahashi S, Kimura Y, Matsuura N, Nakamura T, Yamaga M, Koshino H. Isolation, identification, and synthesis of a new prenylated cinnamic acid derivative from brazilian green propolis and simultaneous quantification of bioactive components by LC-MS/MS. J Agric Food Chem. 2019;67(44):12303–12312. doi: 10.1021/acs.jafc.9b04835. [DOI] [PubMed] [Google Scholar]
- 424.Hernández IM, Fernandez MC, Cuesta-Rubio O, Piccinelli AL, Rastrelli L. Polyprenylated benzophenone derivatives from Cuban propolis. J Nat Prod. 2005;68(6):931–934. doi: 10.1021/np0495884. [DOI] [PubMed] [Google Scholar]
- 425.de Castro Ishida VF, Negri G, Salatino A, Bandeira MFCL. A new type of Brazilian propolis: Prenylated benzophenones in propolis from Amazon and effects against cariogenic bacteria. Food Chem. 2011;125(3):966–972. doi: 10.1016/j.foodchem.2010.09.089. [DOI] [Google Scholar]
- 426.Astudillo L, Avila F, Morrison R, Gutierrez M, Bastida J, Codina C, Schmeda-Hirschmann G. Biologically active compounds from chilean propolis. Boletín Sociedad Chilena Química. 2000;45:577–581. doi: 10.4067/S0366-16442000000400008. [DOI] [Google Scholar]
- 427.Popova MP, Trusheva BS, Nedialkov PT, Tsvetkova I, Pardo-Mora DP, Najdenski H, Torres-García OA, Sforcin JM, Bankova VS. New Δ-tocotrienol derivatives from Colombian propolis. Nat Prod Res. 2020;34(19):2779–2786. doi: 10.1080/14786419.2019.1590710. [DOI] [PubMed] [Google Scholar]
- 428.Muñoz O, Peña R, Ureta E, Montenegro G, Caldwell C, Timmermann B. Phenolic compounds of propolis from Central Chilean Matorral. Zeitschrift für Naturforschung C J Biosci. 2001;56:273–277. doi: 10.1515/znc-2001-3-417. [DOI] [PubMed] [Google Scholar]
- 429.Cuesta-Rubio O, Frontana-Uribe BA, Ramírez-Apan T, Cárdenas J. Polyisoprenylated benzophenones in cuban propolis; biological activity of nemorosone. Z Naturforsch C J Biosci. 2002;57(3–4):372–378. doi: 10.1515/znc-2002-3-429. [DOI] [PubMed] [Google Scholar]
- 430.Díaz-Carballo D, Malak S, Bardenheuer W, Freistuehler M, Peter Reusch H. The contribution of plukenetione A to the anti-tumoral activity of Cuban propolis. Bioorg Med Chem. 2008;16(22):9635–9643. doi: 10.1016/j.bmc.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 431.Granados-Pineda J, Uribe-Uribe N, Garcia-Lopez P, Ramos-Godinez MDP, Rivero-Cruz JF, Perez-Rojas JM. Effect of Pinocembrin Isolated from Mexican Brown Propolis on Diabetic Nephropathy. Molecules. 2018 doi: 10.3390/molecules23040852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Cuesta-Rubio O, Campo Fernández M, Márquez Hernández I, Jaramillo CGJ, González VH, De Oca M, Porto R, Marrero Delange D, Monzote Fidalgo L, Piccinelli AL, Campone L, Rastrelli L. Chemical profile and anti-leishmanial activity of three Ecuadorian propolis samples from Quito, Guayaquil and Cotacachi regions. Fitoterapia. 2017;120:177–183. doi: 10.1016/j.fitote.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 433.Valcic S, Montenegro G, Timmermann BN. Lignans from Chilean propolis. J Nat Prod. 1998;61(6):771–775. doi: 10.1021/np980017j. [DOI] [PubMed] [Google Scholar]
- 434.Aga H, Shibuya T, Sugimoto T, Kurimoto M, Nakajima S. Isolation and Identification of Antimicrobial Compounds in Brazilian Propolis. Biosci Biotechnol Biochem. 1994;58(5):945–946. doi: 10.1271/bbb.58.945. [DOI] [Google Scholar]
- 435.Nina N, Quispe C, Jiménez-Aspee F, Theoduloz C, Feresín GE, Lima B, Leiva E, Schmeda-Hirschmann G. Antibacterial activity, antioxidant effect and chemical composition of propolis from the Región del Maule. Central Chile Molecules. 2015;20(10):18144–18167. doi: 10.3390/molecules201018144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436.Trusheva B, Georgieva K, Popova M, Uzunova V, Stoyanova T, Valcheva V, Tzoneva R, Bankova V. New Insights into Tropical Propolis: Propolis from Pitcairn Island. J Apitherapy Nat. 2018;1(3):30. doi: 10.1016/j.fitote.2018.05.024. [DOI] [PubMed] [Google Scholar]
- 437.Georgieva K, Trusheva B, Uzunova V, Stoyanova T, Valcheva V, Popova M, Tzoneva R, Bankova V. New cycloartane triterpenes from bioactive extract of propolis from Pitcairn Island. Fitoterapia. 2018;128:233–241. doi: 10.1016/j.fitote.2018.05.024. [DOI] [PubMed] [Google Scholar]
- 438.Trusheva B, Stancheva K, Gajbhiye N, Dimitrova R, Popova M, Saraf R, Bankova V. Two New Prenylated Stilbenes with an Irregular Sesquiterpenyl Side Chain from Propolis from Fiji Islands. Records Nat Products. 2016;10:465–471. [Google Scholar]
- 439.Duke CC, Tran VH, Duke RK, Abu-Mellal A, Plunkett GT, King DI, Hamid K, Wilson KL, Barrett RL, Bruhl JJ. A sedge plant as the source of Kangaroo Island propolis rich in prenylated p-coumarate ester and stilbenes. Phytochemistry. 2017;134:87–97. doi: 10.1016/j.phytochem.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 440.King DI, Hamid K, Tran VH, Duke RK, Duke CC. Kangaroo Island propolis types originating from two Lepidosperma species and Dodonaea humilis. Phytochemistry. 2021;188:112800. doi: 10.1016/j.phytochem.2021.112800. [DOI] [PubMed] [Google Scholar]
- 441.Thanh LN, Thoa HT, Oanh VTK, Phuong DTL, Van HT, Chı NQ, Gıap TH, Oanh NTT, Hang NTM, Hung NV, Mınh CV, Bankova V. Isolated xanthones from lisotrigona furva propolis in Vietnam. J Apither Nat. 2018;1(3):74–74. [Google Scholar]
- 442.Nguyen HX, Nguyen MTT, Nguyen NT, Awale S. Chemical Constituents of Propolis from Vietnamese Trigona minor and their antiausterity activity against the PANC-1 Human Pancreatic Cancer Cell Line. J Nat Prod. 2017;80(8):2345–2352. doi: 10.1021/acs.jnatprod.7b00375. [DOI] [PubMed] [Google Scholar]
- 443.Sanpa S, Popova M, Bankova V, Tunkasiri T, Eitssayeam S, Chantawannakul P. Antibacterial Compounds from Propolis of Tetragonula laeviceps and Tetrigona melanoleuca (Hymenoptera: Apidae) from Thailand. PLoS ONE. 2015;10(5):e0126886. doi: 10.1371/journal.pone.0126886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 444.Nguyen HX, Van Do TN, Nguyen MTT, Dang PH, Tho LH, Awale S, Nguyen NT. A New Alkenylphenol from the Propolis of Stingless Bee Trigona minor. Natural Product Commun. 2018;13(1):19345. doi: 10.1177/1934578X1801300121. [DOI] [Google Scholar]
- 445.Regueira MSN, Tintino SR, da Silva ARP, Costa MDS, Boligon AA, Matias EFF, de Queiroz BV, Menezes IRA, Melo Coutinho HD. Seasonal variation of Brazilian red propolis: antibacterial activity, synergistic effect and phytochemical screening. Food Chem Toxicol. 2017;107(Pt B):572–580. doi: 10.1016/j.fct.2017.03.052. [DOI] [PubMed] [Google Scholar]
- 446.Velikova M, Bankova V, Sorkun K, Houcine S, Tsvetkova I, Kujumgiev A. Propolis from the Mediterranean region: chemical composition and antimicrobial activity. Z Naturforsch C J Biosci. 2000;55(9–10):790–793. doi: 10.1515/znc-2000-9-1019. [DOI] [PubMed] [Google Scholar]
- 447.Wang K, Zhang J, Ping S, Ma Q, Chen X, Xuan H, Shi J, Zhang C, Hu F. Anti-inflammatory effects of ethanol extracts of Chinese propolis and buds from poplar (Populus×canadensis) J Ethnopharmacol. 2014;155(1):300–311. doi: 10.1016/j.jep.2014.05.037. [DOI] [PubMed] [Google Scholar]
- 448.Nani BD, Sardi JCO, Lazarini JG, Silva DR, Massariolli AP, Cunha TM, de Alencar SM, Franchin M, Rosalen PL. Anti-inflammatory and anti-Candida Effects of Brazilian Organic Propolis, a Promising Source of Bioactive Molecules and Functional Food. J Agric Food Chem. 2020;68(10):2861–2871. doi: 10.1021/acs.jafc.8b07304. [DOI] [PubMed] [Google Scholar]
- 449.Albokhadaim I. Influence of dietary supplementation of propolis on hematology, biochemistry and lipid profile of rats fed high cholesterol diet. J Advan Veter Anim Res. 2015;2(1):1. doi: 10.5455/javar.2015.b49. [DOI] [Google Scholar]
- 450.Silva DB, Miranda AP, Silva DB, D'Angelo LR, Rosa BB, Soares EA, Ramalho JG, Boriollo MF, Garcia JA. Propolis and swimming in the prevention of atherogenesis and left ventricular hypertrophy in hypercholesterolemic mice. Braz J Biol. 2015;75(2):414–422. doi: 10.1590/1519-6984.15313. [DOI] [PubMed] [Google Scholar]
- 451.Fang Y, Sang H, Yuan N, Sun H, Yao S, Wang J, Qin S. Ethanolic extract of propolis inhibits atherosclerosis in ApoE-knockout mice. Lipids Health Dis. 2013;12:123. doi: 10.1186/1476-511x-12-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452.Usman UZ, Abu Bakar A, Zin A, Mohamed M. LC-MS analysis and effects of Malaysian propolis on insulin, glucagon, pancreas and oxidative stress status in streptozotocin-induced diabetic rats. J Med Biomed Res. 2017;16:15–27. [Google Scholar]
- 453.Ugbaja RN, Fatokun TP, Akinloye DI, James AS, Onabanjo OO, Akinloye OA. Propolis ethanol extract abrogates hyperglycemia, lipotoxicity, and lowered hepatic poly (ADP-ribose) polymerase protein level in male albino rats. J Diabetes Metab Disord. 2021;20(1):683–696. doi: 10.1007/s40200-021-00800-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454.Shvarzbeyn J, Huleihel M. Effect of propolis and caffeic acid phenethyl ester (CAPE) on NFκB activation by HTLV-1 Tax. Antiviral Res. 2011;90(3):108–115. doi: 10.1016/j.antiviral.2011.03.177. [DOI] [PubMed] [Google Scholar]
- 455.Fischer G, Conceição FR, Leite FP, Dummer LA, Vargas GD, Hübner Sde O, Dellagostin OA, Paulino N, Paulino AS, Vidor T. Immunomodulation produced by a green propolis extract on humoral and cellular responses of mice immunized with SuHV-1. Vaccine. 2007;25(7):1250–1256. doi: 10.1016/j.vaccine.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 456.Ganesan S, Faris AN, Comstock AT, Wang Q, Nanua S, Hershenson MB, Sajjan US. Quercetin inhibits rhinovirus replication in vitro and in vivo. Antiviral Res. 2012;94(3):258–271. doi: 10.1016/j.antiviral.2012.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Rojas Á, Del Campo JA, Clement S, Lemasson M, García-Valdecasas M, Gil-Gómez A, Ranchal I, Bartosch B, Bautista JD, Rosenberg AR, Negro F, Romero-Gómez M. Effect of Quercetin on Hepatitis C Virus Life cycle: from viral to host targets. Sci Rep. 2016;6:31777. doi: 10.1038/srep31777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Cheng Z, Sun G, Guo W, Huang Y, Sun W, Zhao F, Hu K. Inhibition of hepatitis B virus replication by quercetin in human hepatoma cell lines. Virol Sin. 2015;30(4):261–268. doi: 10.1007/s12250-015-3584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Utsunomiya H, Ichinose M, Ikeda K, Uozaki M, Morishita J, Kuwahara T, Koyama AH, Yamasaki H. Inhibition by caffeic acid of the influenza A virus multiplication in vitro. Int J Mol Med. 2014;34(4):1020–1024. doi: 10.3892/ijmm.2014.1859. [DOI] [PubMed] [Google Scholar]
- 460.Xie Y, Huang B, Yu K, Shi F, Liu T, Xu W. Caffeic acid derivatives: a new type of influenza neuraminidase inhibitors. Bioorg Med Chem Lett. 2013;23(12):3556–3560. doi: 10.1016/j.bmcl.2013.04.033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Zulhendri F, Chandrasekaran K, Kowacz M, Ravalia M, Kripal K, Fearnley J, Perera CO. 2021. Antiviral, antibacterial, antifungal, and antiparasitic properties of propolis: a review. Foods. [DOI] [PMC free article] [PubMed]
Data Availability Statement
Yes.