Abstract
Research is emerging on the use of Photobiomodulation therapy (PBMT) and its potential for augmenting human performance, however, relatively little research exists utilizing full-body administration methods. As such, further research supporting the efficacy of whole-body applications of PBMT for behavioral and physiological modifications in applicable, real-world settings are warranted. The purpose of this analysis was to observe cardiorespiratory and sleep patterns surrounding the use of full-body PBMT in an elite cohort of female soccer players. Members of a women’s soccer team in a “Power 5 conference” of the National Collegiate Athletic Association (NCAA) were observed across one competitive season while wearing an OURA Ring nightly and a global positioning system (GPS) sensor during training. Within-subject comparisons of cardiorespiratory physiology, sleep duration, and sleep composition were evaluated the night before and after PBMT sessions completed as a standard of care for team recovery. Compared to pre-intervention, mean heart rate (HR) was significantly lower the night after a PBMT session (p = 0.0055). Sleep durations were also reduced following PBMT, with total sleep time (TST) averaging 40 min less the night after a session (p = 0.0006), as well as significant reductions in light sleep (p = 0.0307) and rapid eye movement (REM) sleep durations (p = 0.0019). Sleep durations were still lower following PBMT, even when controlling for daily and accumulated training loads. Enhanced cardiorespiratory indicators of recovery following PBMT, despite significant reductions in sleep duration, suggest that it may be an effective modality for maintaining adequate recovery from the high stress loads experienced by elite athletes.
Keywords: athlete monitoring, exercise training, red light therapy, soccer, wearable device
1. Introduction
Sports at the collegiate, semi-professional, and professional levels each amount to multi-billion-dollar industries in the United States [1]. At elite levels of play, extensive focus is garnered towards athlete recovery to maximize performance and minimize the risk of injury. Undoubtedly, a substantial degree of physiological and mental stress is exerted on the body during highly competitive and physical sports, such as soccer. Recent considerations have also shed light on the additional cognitive and emotional loads that sports can exert on an athlete and how this may interplay with physical demands to ultimately affect performance [2]. The common understanding that sport performance is multi-dimensional should emphasize the concept that recovery should also be multi-dimensional.
A developing modality for augmented recovery and performance enhancement is Photobiomodulation Therapy (PBMT). This therapy, often termed red light therapy, utilizes specific wavelengths between 620–1100 nm, or combinations thereof, ranging from visible red light up to infrared light on the spectrum [3]. Many theories have been proposed as to the potential cellular mechanisms of PBMT; however, nearly all suggest a strong relationship with enhanced adenosine triphosphate (ATP) production from the mitochondria and cell proliferation [4,5,6,7,8,9,10]. These theories are supportive of recovery at the cellular level, which may translate to tissue or systematic-wide relief from oxidative stress [7,11].
Previous research is suggestive of performance enhancements in athletes following PBMT [12,13,14,15,16], as is recovery from high-intensity exercise, which has most commonly been quantified via blood biomarkers [17]. Despite some auspicious results, other studies refute these claims, with evidence that suggests little to no impact on recovery [18,19]. Until the recent development of full-body beds, PBMT has primarily been administered through localized laser treatments to a target-specific tissue or bodily region. Newer technologies utilizing light emitting diodes (LEDs) have aided in providing treatment to larger anatomical areas. PBMT applications utilizing LEDs and lasers differ in that LEDs have a wider bandwidth and emits light in an incoherent fashion [20]. Presently, much of the existing research regarding PBMT has utilized lasers, though numerous clinical studies have reported a comparable [21,22] or greater effects from LED applications [23,24,25]. Variation among delivery methods and anatomical location, in combination with a wide range of applied wavelengths and dosages, contribute to substantial variation in methodology and findings among extant literature [15,26,27,28].
Much of the existing research assessing PBMT on human subjects has been conducted through strict laboratory controlled clinical trials, often obtaining relatively low sample sizes [12,13,18,26,29,30,31,32]. While many of these studies carefully controlled for administration of treatment conditions and the quantification of effects, few studies have assessed free-living use of PBMT while accounting for the inter-individual loads that are accumulated outside of the controlled laboratory setting. As such, strong evidence attesting to the efficacy of implementing PBMT for enhancement of athlete performance and recovery is still warranted.
Autonomic status and balance have been identified as valuable indicators of fatigue and recovery [33,34,35,36,37]. With external influences minimized during sleep, nocturnal monitoring of heart rate (HR) and heart rate variability (HRV) during rest are said to exhibit the strongest degree of reliability for quantifying recovery [37,38], specifically in athletes [39,40,41]. Nocturnal trends in HR and HRV can be influenced by a multitude of factors impacting recovery status, including physical training and sleep quality [41,42,43,44,45]. Despite this, few studies have evaluated sleep or nocturnal physiology in response to PBMT; though, limited research has suggested improvements in subjective sleep quality and serum melatonin [30] despite no effect on next morning HRV [32].
The present analysis was conducted to observe natural, free-living trends in sleep and recovery surrounding the use of PBMT in a team of Division I NCAA women’s soccer athletes. Given the intense physical workloads demanded of athletes at this level, in combination with the mental and emotional stress of intra- and inter-team competition, full day-to-day recovery is of the utmost importance for this population to prevent injury or overreaching [46,47]. It was hypothesized that PBMT would be associated with improved physiological indicators of recovery.
2. Materials and Methods
2.1. Study Procedures
Data were analyzed from a NCAA Division I collegiate women’s soccer team following one competitive season. Only data collected from active, non-injured athletes during in-season training were included. All participants provided their written informed consent to retrospectively share personal data collected by the team. Study procedures were approved by the West Virginia University Institutional Review Board, and all study procedures are in accordance with the Declaration of Helsinki guidelines.
As a standard practice for team recovery, athletes were provided the opportunity to complete 20-min PBMT sessions using a NovoTHOR full-body light bed (THOR Photomedicine Ltd., Chesham, United Kingdom) emitting visible red (660 nm) and near infra-red (NIR, 850 nm) light. Dose and beam parameters for each session completed with the NovoTHOR bed are provided in Table 1 [48]. Whole-body doses were applied to exposed skin without the hinderance of clothing. As per the team standards, athletes were allowed to complete up to two sessions per week and were not permitted to complete sessions on subsequent days.
Table 1.
Dose and Beam Parameters.
| Parameter | Visible Red | NIR |
|---|---|---|
| Wavelength | 660 ± 25 nm | 850 ± 30 nm |
| LED Quantity | 1200 | 1200 |
| Power per LED | 0.267 W | 0.267 W |
| Irradiance (at patient skin) | 0.012 W/cm2 | 0.012 W/cm2 |
| Total Emitted Power | 321 W | 321 W |
| Treatment Time | 1200 s | 1200 s |
| Energy Emitted | 385,056 J | 385,056 J |
| Fluence | 14.4 J/cm2 | 14.4 J/cm2 |
Dosage and beam parameters for each completed session were provided by the device manufacturer, NovoTHOR. (cm, centimeters; FWHM, full width half-maximum; J, joules; NIR, near infra-red; nm, nanometers; s, seconds; W, watts).
Each athlete wore a properly sized second-generation OURA ring (OURA Health, Oulu, Finland) each night on a consistent finger (2nd, 3rd, or 4th digit) of the dominant hand, which captured sleep and physiological parameters. Athletes were also monitored during all training periods with a Catapult Vector S7 (Catapult Sports, Melbourne, Australia) GPS tracker to capture daily training and competitive physical loads.
2.2. Obtained Samples
Twelve athletes, all of which were field players, completed at least one PBMT session throughout the season, totaling 106 sessions. Fourteen sessions were excluded from analysis due to failure to wear the OURA ring either the night immediately before or after the PBMT session. Of the 93 sessions included (average 8.5 ± 7.5 sessions/player), 37 sessions were completed on rest days, in which no physical training took place, and 56 were completed on training days. None of the participating individuals had a diagnosed sleep disorder.
2.3. Measures
2.3.1. Cardiorespiratory Physiology
Summary physiological variables, which are representative of the full night and collected via the OURA ring, were obtained for analysis including average HR, average HRV (RMSSD), and average respiration rate (RR). Additionally, five-minute epochs of average HR and HRV were further analyzed throughout each half of the night for intra-night trends. Given that the first and second halves of the sleep phase traditionally differ in NREM and REM propensity, cardiac parameters were evaluated for each half independently, in addition to full night averages. Maximum, average, and average rate of change/hour for HR and HRV, as well as minimum HR, were calculated individually for the first and second half of each sleep period.
2.3.2. Sleep
Summary sleep variables, which are representative of the full night, were collected via the OURA ring and included total sleep time (TST), sleep efficiency (SE), awake duration, light sleep duration, deep sleep duration, and REM sleep duration. Proportions of each sleep stage were further calculated and are included as % Light, % Deep, and % REM.
2.3.3. External Training Load
Training load data collected during training and competitive sessions via Catapult sensors were quantified using player load, which is the tri-axial sum of acceleration during a session. Player loads were compiled as the total player load recorded each day, as well as a cumulative four-day total that included summated values from the day of record and three days prior.
2.4. Statistical Analyses
All statistical analyses were conducted in JMP Pro 14 (SAS Institute, Cary, NC, USA). Full night pre-intervention and post-intervention physiological and sleep variables were checked for unequal variance using Bartlett’s test and were determined to have equal variance. Two-tailed paired t-tests were used to identify within-individual differences in pre-intervention (night before a session) and post-intervention (night after a session) measures (variable indicated as night). Cohen’s d was utilized to calculate the standardized differences between the paired comparisons.
2.4.1. Intra-Night Relationships
To identify the relationship that sleep duration may have with physiological indicators of recovery, linear mixed models were run on pre-intervention and post-intervention data using a residual structure; three fixed effects were explored for their impact on each of the cardiorespiratory variables including a main effect (ME) of night, ME of TST, and the interaction between night*TST.
Evaluation of HR and HRV variables by half of the night were checked using Bartlett’s test and were determined to have unequal variance; thus, two-way repeated measure Analysis of Variance (ANOVA) assessing within participant fixed effects of night and half of night on HR and HRV were run using a mixed model with an unequal variance structure. All two-way ANOVAs were modeled with three fixed effects (two ME and an interaction of the two). Tukey’s HSD was used to correct for multiple comparisons and identify any resultant pairwise differences.
2.4.2. External Training Load
Linear mixed effects were modeled based upon single-day (designated as 1D player loads) and cumulative four-day player loads (designated as 4D player loads) to identify effects of varying training loads on physiological and sleep parameters.
3. Results
Nocturnal physiology and sleep parameters comparing pre-intervention measures to post-intervention measures are listed in Table 2. Of the nocturnal cardiorespiratory measures assessed, only average HR was found to be significantly lower after PBMT as compared to pre-intervention. With regard to sleep, TST, light sleep duration, REM duration, and REM proportion were significantly lower the night after a PBMT session as compared to pre-intervention.
Table 2.
Pre-intervention vs. Post-intervention Nocturnal Parameters.
| Variable | Pre | Post | Mean Difference | p-Value | d | |
|---|---|---|---|---|---|---|
| Physiology | Average HR (bpm) | 54.31 | 53.31 | 0.996 (0.300, 1.691) | 0.0055 * | 0.175 |
| Average HRV (ms) | 100.46 | 103.73 | −3.269 (−6.899, 0.362) | 0.0770 | 0.251 | |
| Average RR (rpm) | 16.85 | 16.80 | 0.058 (−0.094, 0.210) | 0.4504 | 0.022 | |
| Sleep | Total Sleep Time (h) | 7.93 | 7.29 | 0.635 (0.282, 0.989) | 0.0006 * | 0.156 |
| Awake Time (h) | 1.35 | 1.28 | 0.070 (−0.061, 0.200) | 0.2935 | 0.028 | |
| Sleep Efficiency (%) | 85.65 | 85.13 | 0.516 (−0.602, 1.634) | 0.3616 | 0.071 | |
| Light Duration (h) | 4.62 | 4.30 | 0.322 (0.031, 0.613) | 0.0307 * | 0.087 | |
| Deep Duration (h) | 2.24 | 2.12 | 0.114 (−0.030, 0.258) | 0.1188 | 0.044 | |
| REM Duration (h) | 1.07 | 0.87 | 0.200 (0.075, 0.324) | 0.0019 * | 0.083 | |
| % Light | 57.84 | 58.70 | −0.862 (−3.178, 1.453) | 0.4614 | 0.083 | |
| % Deep | 28.97 | 29.90 | −0.933 (−3.109, 1.243) | 0.3966 | 0.092 | |
| % REM | 13.21 | 11.41 | 1.798 (0.41, 3.185) | 0.0117 * | 0.223 |
Mean difference expressed as Mean (lower 95% CI, upper 95% CI). Variables determined to be significantly different (α < 0.05) between pre-intervention and post-intervention by a paired t-test are in bold and denoted by an asterisk (*). (bpm, beats per minute; HR, heart rate; h, hours; HRV, heart rate variability; ms, milliseconds; pre, preintervention; post, postintervention; rpm, respirations per minute; REM, rapid eye movement; RR, respiration rate).
3.1. Intra-Night Relationships
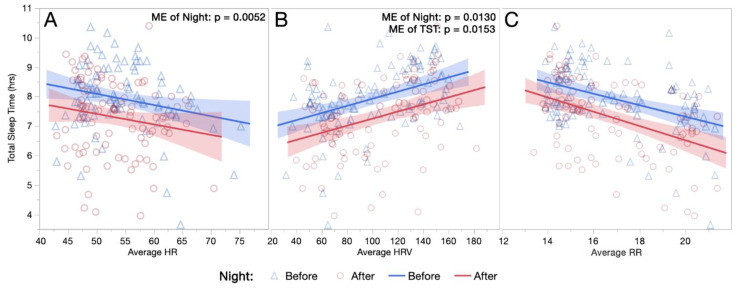
Figure 1A–C demonstrates the relationship between average physiological parameters and TST by night. All fixed effects from the linear mixed model analyses demonstrating the relationships between these variables are listed in Table 3; despite a significant reduction of almost 40 min in post-intervention TST, significant ME of night existed on average HR and average HRV.
Figure 1.
(A–C) Relationships between Total Sleep Durations and Nocturnal Physiology. The relationship between total sleep duration and nocturnal physiological parameters are demonstrated for both the night before and the night after a PBMT session, including (A) average HR, (B) average HRV, and (C) average RR. (HR, heart rate; hrs, hours; HRV, heart rate variability; ME, main effect; RR, respiration rate).
Table 3.
Fixed Effects of Sleep on Cardiorespiratory Physiology.
| Outcome Measure | Fixed Effect | F | df | p-Value |
|---|---|---|---|---|
| Average HR | Night | 8.18 | 1, 90.7 | 0.0052 * |
| TST | 0.41 | 1, 102.4 | 0.5254 | |
| Night*TST | 0.59 | 1, 102.7 | 0.4451 | |
| Average HRV | Night | 6.43 | 1, 89.0 | 0.0130 * |
| TST | 6.09 | 1, 98.5 | 0.0153 * | |
| Night*TST | 3.05 | 1, 98.8 | 0.0839 | |
| Average RR | Night | 1.05 | 1, 88.9 | 0.3090 |
| TST | 0.86 | 1, 93.0 | 0.3552 | |
| Night*TST | 0.01 | 1, 93.1 | 0.9051 |
Linear mixed model fixed effect statistics demonstrating the relationship between sleep duration (TST) and night (pre-intervention vs. post-intervention) on cardiorespiratory parameters. Fixed effects determined to have a significant effect on the specified cardiorespiratory variable (α < 0.05) are in bold and denoted with an asterisk (*). (HR, heart rate; HRV, heart rate variability; night*TST, interaction between night and total sleep time; RR, respiration rate; TST, total sleep time).
Evaluation of HR trends by half via two-way ANOVA determined significant ME of half on minimum HR (F(1,267.3) = 29.15, p < 0.0001), maximal HR (F(1,275.6) = 61.74, p < 0.0001), average HR (F(1,263.2) = 127.11, p < 0.0001), and rate of HR reduction per hour (F(1,269.8) = 249.44, p < 0.0001). Significant ME of night existed for minimum HR (F(1,267.3) = 9.15, p = 0.0027) and average HR (F(1,263.2) = 13.57, p = 0.0003). A significant interaction between half*night existed only for maximal HR (F(1,275.6) = 5.55, p = 0.0192). These patterns in HR by half of night are exhibited in Figure 2A–D.
Figure 2.
(A–D) Heart Rate Trends by Half of Night. Least squares means interaction plots demonstrating the effects of night half (first and second halves of each sleep period) and night (before or after PBMT intervention) on (A) Minimum HR (bpm). (B) Maximum HR (bpm). (C) Average HR (bpm). (D) Average rate of change in HR per hour (bpm/hour). (*) denotes significant pairwise differences between the first and second halves of the night before PBMT intervention, (§) denotes significant pairwise differences between first and second halves of the night after PBMT intervention, (‡) denotes significant pairwise differences between the night before and night after PBMT intervention during the first half of the night only, and (¥) denotes significant pairwise differences between the night before and night after PBMT during the second half of the night only. (bpm, beats per minute; half*night, interaction between half of night and night; HR, heart rate; ME, main effect).
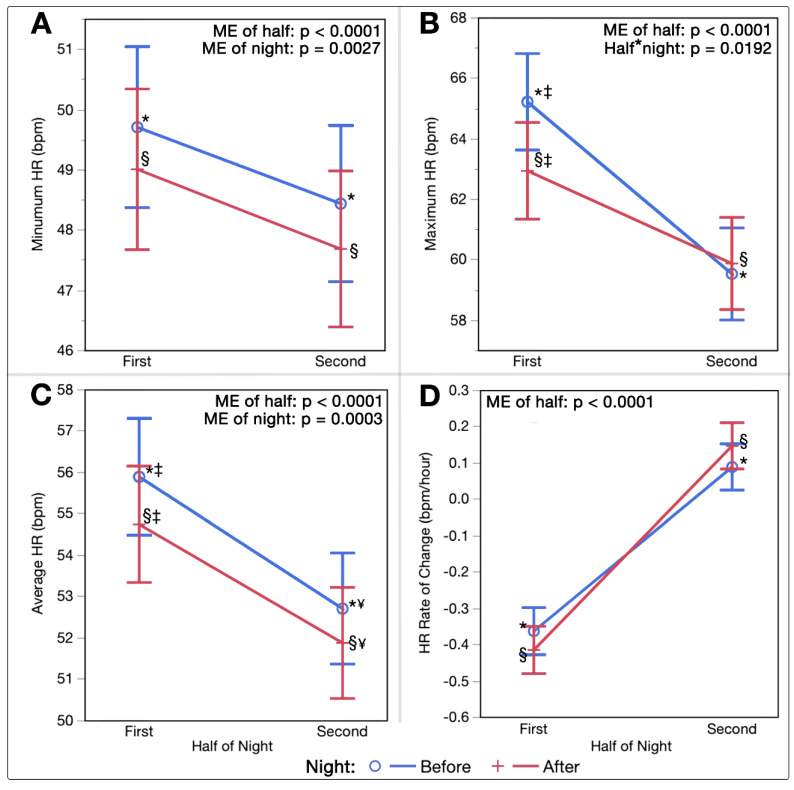
Two-way ANOVAs assessing nightly HRV trends by half also resulted in significant ME of half on maximal HRV (F(1,268.6) = 30.89, p < 0.0001), average HRV (F(1,265.1) = 48.23, p < 0.0001), and rate of HRV increase per hour (F(1,273.6) = 68.51, p < 0.0001). Significant ME of night existed on maximal HRV (F(1,268.6) = 9.19, p = 0.0027) and average HRV (F(1,265.1) = 5.33, p = 0.0217). No significant interactions between half*night existed for HRV parameters. Figure 3A–C displays these patterns in HRV by half.
Figure 3.
(A–C) Heart Rate Variability Trends by Half of Night. Least squares means interaction plots demonstrating the effects of night half (first and second halves of each sleep period) and night (before or after PBMT intervention) on (A) Maximum HRV (ms). (B) Average HRV (ms). (C) Average rate of change in HRV per hour (ms/hour). (*) denotes significant pairwise differences between the first and second halves of the night before the PBMT intervention, (§) denotes significant pairwise differences between first and second halves of the night after the PBMT intervention, and (‡) denotes significant pairwise differences between the night before and night after PBMT intervention during the first half of the night only. (HRV, heart rate variability; ME, main effect; ms, milliseconds).
3.2. Training Load
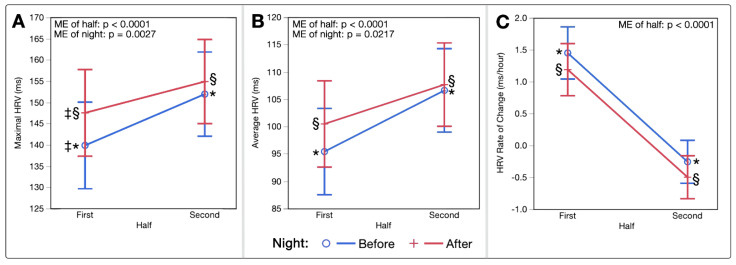
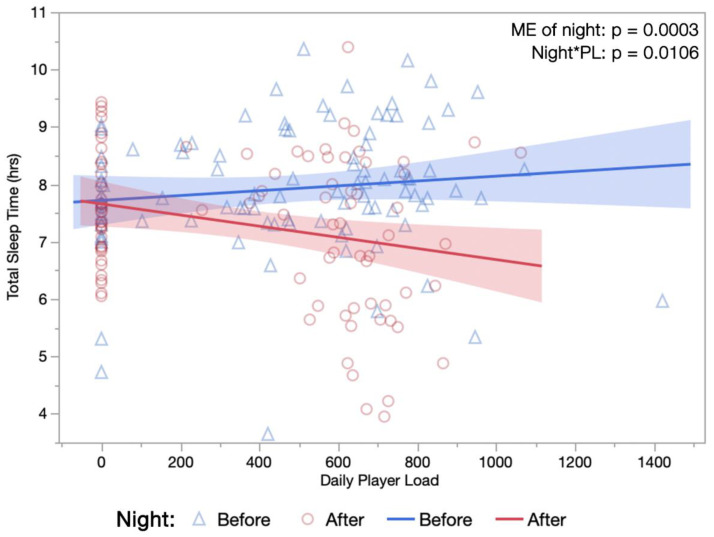
Table 4 lists fixed effect p-values from linear effect models evaluating single-day and cumulative, four-day player loads. Daily and cumulative player loads were found to have notable impacts on multiple physiological and sleep parameters, including TST; the significant ME of night (F(1,93.2) = 14.42, p = 0.0003) and interaction occurring between night*one-day player load (F(1,178.1) = 6.67, p = 0.0106) can be seen in Figure 4.
Table 4.
Effect of Daily and Cumulative Training Loads on Sleep and Nocturnal Physiology.
| Single-Day PL | 4D Cumulative PL | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Night | PL | Night*PL | Night | PL | Night*PL | |
| Physiology | Average HR (bpm) | 0.0643 | <0.0001 * | 0.0761 | 0.0089 * | 0.0132 * | 0.6472 |
| Average HRV (ms) | 0.1598 | 0.1793 | 0.1916 | 0.0912 | 0.5113 | 0.6187 | |
| Average RR (rpm) | 0.8956 | 0.0004 * | 0.0549 | 0.6076 | 0.0140 * | 0.6390 | |
| Sleep | Total Sleep Time (h) | 0.0003 * | 0.3309 | 0.0106 * | 0.0005 * | 0.1993 | 0.8867 |
| Awake Time (h) | 0.2438 | 0.4530 | 0.9029 | 0.2798 | 0.4659 | 0.9330 | |
| Sleep Efficiency (%) | 0.4060 | 0.7732 | 0.2514 | 0.3742 | 0.8003 | 0.8906 | |
| Light Duration (h) | 0.0299 * | 0.8949 | 0.0401 * | 0.0301 * | 0.7022 | 0.7982 | |
| Deep Duration (h) | 0.0881 | 0.3869 | 0.1862 | 0.1087 | 0.3192 | 0.5547 | |
| REM Duration (h) | 0.0016 * | 0.6175 | 0.2155 | 0.0018 * | 0.3259 | 0.7460 | |
| % Light | 0.4304 | 0.7136 | 0.9402 | 0.4461 | 0.5736 | 0.4394 | |
| % Deep | 0.4016 | 0.9552 | 0.4968 | 0.3929 | 0.8361 | 0.7182 | |
| % REM | 0.0098 * | 0.6314 | 0.2001 | 0.010 5 * | 0.3244 | 0.4464 | |
Fixed effect p-values for linear mixed effect models evaluating the relationship that night and physical training loads have with physiological and sleep parameters. Each variable was evaluated for main effect of player load (PL, separately for single-day and cumulative four-day load), main effect of night (pre-intervention vs. post-intervention), and interactions between player load and night. Fixed effects determined to have a significant effect on the specified physiological variable (α < 0.05) are in bold and denoted with an asterisk (*). (bpm, beats per minute; HR, heart rate; h, hours; HRV, heart rate variability; ms, milliseconds; night*PL, interaction between night and player load; PL, player load; REM, rapid eye movement; rpm, respirations per minute; RR, respiration rate; 4D, four day).
Figure 4.
Relationship between Total Sleep Time and Daily Training Load. Single-day player loads (au) measured via GPS during training sessions are plotted against subsequent night sleep durations, occurring both the night before and night after a PBMT session. (hrs, hours; ME, main effect; night*PL, interaction between night and player load).
4. Discussion
The present analysis is the first to observe free-living trends in sleep and cardiorespiratory physiology surrounding the use of full-body Photobiomodulation therapy (PBMT) in a cohort of female athletes within a NCAA “Power 5” conference. Athletes averaged 40 min less sleep the night after a PBMT session, while also demonstrating reductions in HR and trending increases in HRV, as compared to the night before the session. Collectively, higher physical training loads recorded during training had a tendency to increase HR and RR, independent of PBMT; however, changes in sleep quantity and composition demonstrated stronger associations with timing of the intervention, independent of daily or cumulative training loads.
Previous research has shown HR to decrease throughout the night, most substantially during the high proportions of deep sleep in the first half, with a plateau sometimes reached prior to waking [49,50]. Opposing patterns are often seen in HRV, with values and their variability becoming greater with longer periods of REM sleep [37,38,50]. In the present analysis, longer sleep durations were associated with lower HR, higher HRV, and lower RR (Figure 1A–C); this is consistent independent of whether the sleep occurred before or after a PBMT session. Following PBMT, this relationship shifted to shorter sleep durations associated with a given HR, HRV, and RR. Interestingly, values across the first and second half of the night for HR and HRV followed the same relative patterns, although slight improvements existed in both halves post-intervention (Figure 2A–D and Figure 3A–C), keeping in mind that each half was on average 20 min shorter in duration post-intervention.
With consideration to external training load, single-day and cumulative player loads corresponded positively with higher HR and RR, both before and after PBMT. Conversely, findings demonstrated that the PBMT intervention had a substantial influence on sleep, with decreases in TST, light duration, REM duration, and REM proportion following treatment, often unaffected by training loads. As demonstrated previously, one would expect higher training loads to be associated with longer sleep durations [51,52] and higher nocturnal HRs [44,53] as the body responds to greater physical stress; however, findings herein opposed these expected outcomes, with greater reductions in duration of total sleep and light sleep occurring after PBMT sessions when completed on days with higher single-day loads (Figure 4 and Table 4). These findings again demonstrate the same cardiorespiratory responses following exercise of varying intensity, through reductions in the amount of corresponding sleep obtained.
Potential mechanisms justifying the relationship between sleep and PBMT have not yet been suggested in the literature. Given that most sleep research has only demonstrated the consequences of failing to obtain sufficient sleep, as well as what may inhibit it, there is a scarce understanding of what may cause a reduction in required sleep. Augmented waste clearance from PBMT, which has been demonstrated previously [54,55], could enhance physiological efficiency and may justify the changes observed in sleep architecture. Both PBMT and sleep have been suggested to have implications in similar damage-repairing mechanisms; thus, it is possible that participation in full-body PBMT reduces the degree of restoration required during a subsequent sleep period, though this has not been evaluated. The present analysis did not consider post-PBMT physical or cognitive performance, nor immune function, albeit extensive prior research suggests PBMT results in enhancements across each domain [16,56,57,58]. While it cannot be ascertained that sleep herein was not inhibited, augmentations in HR and HRV patterns do not suggest a consequence on autonomic profile.
Sleep was monitored herein using the OURA Ring; the finger-worn ring estimates sleep related parameters via motion collected by 3D accelerometers and cardiorespiratory variables captured via photoplethysmography (PPG) [59]. In prior assessments, the OURA ring was found to quantify cardiac physiology and sleep durations with high degrees of accuracy [60,61,62,63,64]. It should be noted, however, that higher error rates have been found for the validation of sleep stage classification [60,63]. It should also be noted that sleep stages are estimated via relative changes in movement and cardiorespiratory parameters (HR, HRV and RR). The literature does not support whether PBMT could alter normal second-by-second relationships for these variables, which would ultimately impact algorithmic stage classification during sleep. Thus, further evaluation of sleep stages and cortical activity via EEG should be a focus of future research.
Findings presented herein are novel to existing literature in that data was obtained in a free-living manner, rather than within laboratory conditions; this emphasizes the real-world translation of findings, but also presents with limitations. Sleep is a vulnerable behavior that is susceptible to changes by influence of exercise, nutrition, stress, and psychology, just to name a few [46]. While it is of high value to understand the relationships that each of these factors can hold with PBMT, it is also vital that evaluations are made under conditions that allow for high variability within each confound, similar to that of a real-world setting. As such, the possibility of a placebo effect cannot be ruled out from this observational analysis, as with any clinical intervention. Though, it should be noted that subjects were unaware of the hypothesis discussed herein at the time of collection, as data was not collected specifically for research purposes.
Extensive future research should be focused towards replicating these observations in the laboratory, as well as assessing performance longitudinally to ensure that these findings do not exist in combination with corresponding factors (e.g., reductions in psychomotor vigilance). Further, additional EEG-based assessments are needed for affirmation of these findings along with associated biological variables that may occur in combination, such as levels of metabolic waste, proinflammatory markers, and blood perfusion, to name a few.
In summary, casual integration of full-body PBMT by elite athletes was associated with observed single-night reductions in sleep duration concurrent with augmentations in autonomic profile (HR & HRV). Sleep is an active process involving most of the body’s systems that contributes to recovery through the maintenance of homeostasis [37,38]. A similar integrated perspective should be considered when using full-body PBMT to promote recovery. The involvement of numerous bodily systems in the recovery process suggests added utility for full-body PBMT as compared to the localized administration methods utilized throughout much of the literature, which tends to focus only on the obvious source of damage (i.e., key muscle groups). The findings presented herein provide a novel approach to determining the efficacy of PBMT that warrant continued research.
Author Contributions
Conceptualization, L.E.R.; formal analysis, J.R. and L.E.R.; investigation, L.E.R.; resources, A.R. and S.M.G.; data curation, L.E.R. and J.R.; writing—original draft preparation, L.E.R. and R.W.B.; writing—review and editing, L.E.R., R.W.B., J.R., A.R. and S.M.G.; visualization, L.E.R.; supervision, A.R. and S.M.G.; project administration, L.E.R. and S.M.G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of West Virginia University (protocol #2009105273, approved September 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data underlying this article cannot be shared publicly due to certain elements of the data being owned by a third party and are considered confidential. The data will be shared on reasonable request to the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Humphreys B., Ruseski J. The Size and Scope of the Sports Industry in the United States; Proceedings of the 10th Annual International Association of Sports Economists Conference; Gijón, Spain. 29–31 August 2008. [Google Scholar]
- 2.Dos Santos M.L., Uftring M., Stahl C.A., Lockie R.G., Alvar B., Mann J.B., Dawes J.J. Stress in Academic and Athletic Performance in Collegiate Athletes: A Narrative Review of Sources and Monitoring Strategies. Front. Sports Act. Living. 2020;2:42. doi: 10.3389/fspor.2020.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramezani F., Neshasteh-Riz A., Ghadaksaz A., Fazeli S.M., Janzadeh A., Hamblin M.R. Mechanistic Aspects of Photobiomodulation Therapy in the Nervous System. Lasers Med. Sci. 2021;37:11–18. doi: 10.1007/s10103-021-03277-2. [DOI] [PubMed] [Google Scholar]
- 4.de Freitas L.F., Hamblin M.R. Proposed Mechanisms of Photobiomodulation or Low-Level Light Therapy. IEEE J. Sel. Top. Quantum Electron. 2016;22:348–364. doi: 10.1109/JSTQE.2016.2561201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dompe C., Moncrieff L., Matys J., Grzech-Leśniak K., Kocherova I., Bryja A., Bruska M., Dominiak M., Mozdziak P., Skiba T.H.I., et al. Photobiomodulation—Underlying Mechanism and Clinical Applications. J. Clin. Med. 2020;9:1724. doi: 10.3390/jcm9061724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sommer A.P. Mitochondrial Cytochrome C Oxidase is Not the Primary Acceptor for Near Infrared Light—It is Mitochondrial Bound Water: The Principles of Low-Level Light Therapy. Ann. Transl. Med. 2019;7:S13. doi: 10.21037/atm.2019.01.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hamblin M.R. Mechanisms and Applications of the Anti-Inflammatory Effects of Photobiomodulation. AIMS Biophys. 2017;4:337–361. doi: 10.3934/biophy.2017.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glass G.E. Photobiomodulation: A Review of the Molecular Evidence for Low Level Light Therapy. J. Plast. Reconstr. Aesthet Surg. 2021;74:1050–1060. doi: 10.1016/j.bjps.2020.12.059. [DOI] [PubMed] [Google Scholar]
- 9.Hamblin M.R. Photobiomodulation for Alzheimer’s Disease: Has the Light Dawned? Photonics. 2019;6:77. doi: 10.3390/photonics6030077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ravera S., Colombo E., Pasquale C., Benedicenti S., Solimei L., Signore A., Amaroli A. Mitochondrial Bioenergetic, Photobiomodulation and Trigeminal Branches Nerve Damage, What’s the Connection? A Review. Int. J. Mol. Sci. 2021;22:4347. doi: 10.3390/ijms22094347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dos Santos S.A., Serra A.J., Stancker T.G., Simões M.C.B., Vieira M.A.D.S., Leal-Junior E.C., Prokic M., Vasconsuelo A., Santos S.S., Carvalho P.D.T.C.D. Effects of Photobiomodulation Therapy on Oxidative Stress in Muscle Injury Animal Models: A Systematic Review. Oxidative Med. Cell. Longev. 2017;2017:5273403. doi: 10.1155/2017/5273403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Toma R.L., Oliveira M.X., Renno A.C.M., Laakso E.-L. Photobiomodulation (PBM) Therapy at 904 nm Mitigates Effects of Exercise-Induced Skeletal Muscle Fatigue in Young Women. Lasers Med. Sci. 2018;33:1197–1205. doi: 10.1007/s10103-018-2454-4. [DOI] [PubMed] [Google Scholar]
- 13.Pinto H.D., Vanin A.A., Miranda E., Tomazoni S.S., Johnson D.S., Albuquerque-Pontes G.M., Aleixo I.D.O., Grandinetti V.D.S., Casalechi H.L., Carvalho P.D.T.D., et al. Photobiomodulation Therapy Improves Performance and Accelerates Recovery of High-Level Rugby Players in Field Test: A Randomized, Crossover, Double-Blind, Placebo-Controlled Clinical Study. J. Strength Cond. Res. 2016;30:3329–3338. doi: 10.1519/JSC.0000000000001439. [DOI] [PubMed] [Google Scholar]
- 14.Miranda E.F., Vanin A.A., Tomazoni S.S., Grandinetti V.d.S., de Paiva P.R.V., Machado C.d.S.M., Monteiro K.K.D.S., Casalechi H.L., de Carvalho P.d.T.C., Leal-Junior E.C.P. Using Pre-Exercise Photobiomodulation Therapy Combining Super-Pulsed Lasers and Light-Emitting Diodes to Improve Performance in Progressive Cardiopulmonary Exercise Tests. J. Athl. Train. 2016;51:129–135. doi: 10.4085/1062-6050-51.3.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dellagrana R.A., Rossato M., Sakugawa R.L., Lazzari C.D., Baroni B.M., Diefenthaeler F. Dose-Response Effect of Photobiomodulation Therapy on Neuromuscular Economy during Submaximal Running. Lasers Med. Sci. 2018;33:329–336. doi: 10.1007/s10103-017-2378-4. [DOI] [PubMed] [Google Scholar]
- 16.Ferraresi C., Huang Y.-Y., Hamblin M.R. Photobiomodulation in Human Muscle Tissue: An Advantage in Sports Performance? J. Biophotonics. 2016;9:1273–1299. doi: 10.1002/jbio.201600176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Marchi T., Leal-Junior E.C.P., Lando K.C., Cimadon F., Vanin A.A., Pase da Rosa D., Salvador M. Photobiomodulation Therapy Before Futsal Matches Improves the Staying Time of Athletes in the Court and Accelerates Post-Exercise Recovery. Lasers Med. Sci. 2019;34:139–148. doi: 10.1007/s10103-018-2643-1. [DOI] [PubMed] [Google Scholar]
- 18.Malta E.d.S., de Lira F.S., Machado F.A., Zago A.S., Amaral S.L.d., Zagatto A.M. Photobiomodulation by LED Does Not Alter Muscle Recovery Indicators and Presents Similar Outcomes to Cold-Water Immersion and Active Recovery. Front. Physiol. 2019;9:1948. doi: 10.3389/fphys.2018.01948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zagatto A.M., Dutra Y.M., Santos Lira F., Antunes B.M., Faustini J.B., Malta E.d.S., Lopes V.H.F., de Poli R.A.B., Brisola G.M.P., dos Santos G.V., et al. Full Body Photobiomodulation Therapy to Induce Faster Muscle Recovery in Water Polo Athletes: Preliminary Results. Photobiomodul. Photomed. Laser Surg. 2020;38:766–772. doi: 10.1089/photob.2020.4803. [DOI] [PubMed] [Google Scholar]
- 20.Heiskanen V., Hamblin M.R. Photobiomodulation: Lasers vs. light emitting diodes? Photochem. Photobiol. Sci. 2018;17:1003–1017. doi: 10.1039/C8PP00176F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lima A.C., Fernandes G.A., Gonzaga I.C., de Barros Araujo R., de Oliveira R.A., Nicolau R.A. Low-Level Laser and Light-Emitting Diode Therapy for Pain Control in Hyperglycemic and Normoglycemic Patients Who Underwent Coronary Bypass Surgery with Internal Mammary Artery Grafts: A Randomized, Double-Blind Study with Follow-Up. Photomed. Laser Surg. 2016;34:244–251. doi: 10.1089/pho.2015.4049. [DOI] [PubMed] [Google Scholar]
- 22.Ammar T.A. Monochromatic Infrared Photo Energy versus Low Level Laser Therapy in Patients with Knee Osteoarthritis. J. Lasers Med. Sci. 2014;5:176–182. [PMC free article] [PubMed] [Google Scholar]
- 23.Leal E.C.P., Lopes-Martins R.A.B., Baroni B.M., De Marchi T., Rossi R.P., Grosselli D., Generosi R.A., de Godoi V., Basso M., Mancalossi J.L., et al. Comparison Between Single-Diode Low-Level Laser Therapy (LLLT) and LED Multi-Diode (Cluster) Therapy (LEDT) Applications Before High-Intensity Exercise. Photomed. Laser Surg. 2009;27:617–623. doi: 10.1089/pho.2008.2350. [DOI] [PubMed] [Google Scholar]
- 24.Esper M.A.L.R., Nicolau R.A., Arisawa E.A.L. The effect of two phototherapy protocols on pain control in orthodontic procedure-a preliminary clinical study. Lasers Med. Sci. 2011;26:657–663. doi: 10.1007/s10103-011-0938-6. [DOI] [PubMed] [Google Scholar]
- 25.Freitas A.C.C., Campos L., Brandao T.B., Cristofaro M., Eduardo F.D., Luiz A.C., Marques M.M., Eduardo C.D., Simoes A. Chemotherapy-Induced Oral Mucositis: Effect of LED and Laser Phototherapy Treatment Protocols. Photomed. Laser Surg. 2014;32:81–87. doi: 10.1089/pho.2013.3576. [DOI] [PubMed] [Google Scholar]
- 26.Dellagrana R.A., Rossato M., Sakugawa R.L., Baroni B.M., Diefenthaeler F. Photobiomodulation Therapy on Physiological and Performance Parameters During Running Tests: Dose–Response Effects. J. Strength Cond. Res. 2018;32:2807–2815. doi: 10.1519/JSC.0000000000002488. [DOI] [PubMed] [Google Scholar]
- 27.Rossato M., Dellagrana R.A., Sakugawa R.L., Baroni B.M., Diefenthaeler F. Dose–Response Effect of Photobiomodulation Therapy on Muscle Performance and Fatigue During a Multiple-Set Knee Extension Exercise: A Randomized, Crossover, Double-Blind Placebo Controlled Trial. Photobiomodul. Photomed. Laser Surg. 2020;38:758–765. doi: 10.1089/photob.2020.4820. [DOI] [PubMed] [Google Scholar]
- 28.Tuner J. Photobiomodulation: How Many Sessions and How Often? Photomed. Laser Surg. 2018;36:59–60. doi: 10.1089/pho.2017.4387. [DOI] [PubMed] [Google Scholar]
- 29.Dutra Y.M., Claus G.M., Malta E.d.S., Brisola G.M.P., Esco M.R., Ferraresi C., Zagatto A.M. Acute Photobiomodulation by LED Does Not Alter Muscle Fatigue and Cycling Performance. Med. Sci. Sports Exerc. 2020;52:2448–2458. doi: 10.1249/MSS.0000000000002394. [DOI] [PubMed] [Google Scholar]
- 30.Zhao J., Tian Y., Nie J., Xu J., Liu D. Red Light and the Sleep Quality and Endurance Performance of Chinese Female Basketball Players. J. Athl. Train. 2012;47:673–678. doi: 10.4085/1062-6050-47.6.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rossato M., Dellagrana R.A., Sakugawa R.L., Lazzari C.D., Baroni B.M., Diefenthaeler F. Time Response of Photobiomodulation Therapy on Muscular Fatigue in Humans. J. Strength Cond. Res. 2018;32:3285–3293. doi: 10.1519/JSC.0000000000002339. [DOI] [PubMed] [Google Scholar]
- 32.Ghigiarelli J.J., Fulop A.M., Burke A.A., Ferrara A.J., Sell K.M., Gonzalez A.M., Pelton L.M., Zimmerman J.A., Coke S.G., Marshall D.G. The Effects of Whole-Body Photobiomodulation Light-Bed Therapy on Creatine Kinase and Salivary Interleukin-6 in a Sample of Trained Males: A Randomized, Crossover Study. Front. Sports Act. Living. 2020;2:48. doi: 10.3389/fspor.2020.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kiviniemi A.M., Hautala A.J., Kinnunen H., Tulppo M.P. Endurance Training Guided Individually by Daily Heart Rate Variability Measurements. Eur. J. Appl. Physiol. 2007;101:743–751. doi: 10.1007/s00421-007-0552-2. [DOI] [PubMed] [Google Scholar]
- 34.Buchheit M. Monitoring Training Status with HR Measures: Do All Roads Lead to Rome? Front. Physiol. 2014;5:73. doi: 10.3389/fphys.2014.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al Haddad H., Laursen P.B., Chollet D., Ahmaidi S., Buchheit M. Reliability of Resting and Postexercise Heart Rate Measures. Int. J. Sports Med. 2011;32:598–605. doi: 10.1055/s-0031-1275356. [DOI] [PubMed] [Google Scholar]
- 36.Eyal S., Altman Y., Baharav A. 1010 Sleep Related Recovery in Athletes: The Role of Heart Rate Variability Parameters. Sleep. 2019;42:A406–A407. doi: 10.1093/sleep/zsz067.1007. [DOI] [Google Scholar]
- 37.Chokroverty S., Cortelli P., editors. Autonomic Nervous System and Sleep: Order and Disorder. Springer Nature; New York, NY, USA: 2021. [Google Scholar]
- 38.de Zambotti M., Trinder J., Silvani A., Colrain I.M., Baker F.C. Dynamic Coupling Between the Central and Autonomic Nervous Systems During Sleep: A Review. Neurosci. Biobehav. Rev. 2018;90:84–103. doi: 10.1016/j.neubiorev.2018.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roche F., Gaspoz J.-M., Court-Fortune I., Minini P., Pichot V., Duverney D., Costes F., Lacour J.-R., Barthélémy J.-C. Screening of Obstructive Sleep Apnea Syndrome by Heart Rate Variability Analysis. Circulation. 1999;100:1411–1415. doi: 10.1161/01.CIR.100.13.1411. [DOI] [PubMed] [Google Scholar]
- 40.Otzenberger H., Gronfier C., Simon C., Charloux A., Ehrhart J., Piquard F., Brandenberger G. Dynamic Heart Rate Variability: A Tool for Exploring Sympathovagal Balance Continuously During Sleep in Men. Am. J. Physiol. Heart Circ. Physiol. 1998;275:H946–H950. doi: 10.1152/ajpheart.1998.275.3.H946. [DOI] [PubMed] [Google Scholar]
- 41.Waldeck M.R., Lambert M.I. Heart Rate During Sleep: Implications for Monitoring Training Status. J. Sports Sci. Med. 2003;2:133–138. [PMC free article] [PubMed] [Google Scholar]
- 42.Burton A.R., Rahman K., Kadota Y., Lloyd A., Vollmer-Conna U. Reduced Heart Rate Variability Predicts Poor Sleep Quality in a Case–Control Study of Chronic Fatigue Syndrome. Exp. Brain Res. 2010;204:71–78. doi: 10.1007/s00221-010-2296-1. [DOI] [PubMed] [Google Scholar]
- 43.Pichot V., Roche F., Gaspoz J.-M., Enjolras F., Antoniadis A., Minini P., Costes F., Busso T., Lacour J.-R., Barthelemy J.C. Relation Between Heart Rate Variability and Training Load in Middle-Distance Runners. Med. Sci. Sports Exerc. 2000;32:1729–1736. doi: 10.1097/00005768-200010000-00011. [DOI] [PubMed] [Google Scholar]
- 44.Myllymaki T., Rusko H., Syvaoja H., Juuti T., Kinnunen M.-L. Effects of Exercise Intensity and Duration on Nocturnal Heart Rate Variability and Sleep Quality. Eur. J. Appl. Physiol. 2012;112:801–809. doi: 10.1007/s00421-011-2034-9. [DOI] [PubMed] [Google Scholar]
- 45.Costa J., Figueiredo P., Nakamura F., Rago V., Rebelo A., Brito J. Intra-Individual Variability of Sleep and Nocturnal Cardiac Autonomic Activity in Elite Female Soccer Players During an International Tournament. PLoS ONE. 2019;14:e0218635. doi: 10.1371/journal.pone.0218635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Watson A.M. Sleep and Athletic Performance. Curr. Sports Med. Rep. 2017;16:413–418. doi: 10.1249/JSR.0000000000000418. [DOI] [PubMed] [Google Scholar]
- 47.Hainline B., Derman W., Vernec A., Budgett R., Deie M., Dvorak J., Harle C., Herring S.A., McNamee M., Meeuwisse W., et al. International Olympic Committee Consensus Statement on Pain Management in Elite Athletes. Br. J. Sports Med. 2017;51:1245–1258. doi: 10.1136/bjsports-2017-097884. [DOI] [PubMed] [Google Scholar]
- 48.Jenkins P.A., Carroll J.D. How to report low-level laser therapy (LLLT)/photomedicine dose and beam parameters in clinical and laboratory studies. Photomed. Laser Surg. 2011;29:785–787. doi: 10.1089/pho.2011.9895. [DOI] [PubMed] [Google Scholar]
- 49.Burgess H.J., Holmes A.L., Dawson D. The Relationship Between Slow-wave Activity, Body Temperature, and Cardiac Activity During Nighttime Sleep. Sleep. 2001;24:343–349. doi: 10.1093/sleep/24.3.343. [DOI] [PubMed] [Google Scholar]
- 50.Brandenberger G., Buchheit M., Ehrhart J., Simon C., Piquard F. Is Slow Wave Sleep an Appropriate Recording Condition for Heart Rate Variability Analysis? Auton. Neurosci. 2005;121:81–86. doi: 10.1016/j.autneu.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 51.Costa J.A., Figueiredo P., Nakamura F.Y., Rebelo A., Brito J. Monitoring Individual Sleep and Nocturnal Heart Rate Variability Indices: The Impact of Training and Match Schedule and Load in High-Level Female Soccer Players. Front. Physiol. 2021;12:678462. doi: 10.3389/fphys.2021.678462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thornton H., Delaney J.A., Duthie G.M., Dascombe B.J. Effects of Preseason Training on the Sleep Characteristics of Professional Rugby League Players. Int. J. Sports Physiol. Perform. 2018;13:176–182. doi: 10.1123/ijspp.2017-0119. [DOI] [PubMed] [Google Scholar]
- 53.Aloulou A., Duforez F., Bieuzen F., Nedelec M. The Effect of Night-Time Exercise on Sleep Architecture Among Well-Trained Male Endurance Runners. J. Sleep Res. 2020;29:e12964. doi: 10.1111/jsr.12964. [DOI] [PubMed] [Google Scholar]
- 54.Taboada L.D., Yu J., El-Amouri S., Gattoni-Celli S., Richieri S., McCarthy T., Streeter J., Kindy M.S. Transcranial Laser Therapy Attenuates Amyloid-β Peptide Neuropathology in Amyloid-β Protein Precursor Transgenic Mice. J. Alzheimers Dis. 2011;23:521–535. doi: 10.3233/JAD-2010-100894. [DOI] [PubMed] [Google Scholar]
- 55.Grillo S.L., Duggett N.A., Ennaceur A., Chazot P.L. Non-invasive Infra-red Therapy (1072 nm) Reduces b-Amyloid Protein Levels in the Brain of an Alzheimer’s Disease Mouse Model, TASTPM. J. Photochem. Photobiol. 2013;123:13–22. doi: 10.1016/j.jphotobiol.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 56.Salehpour F., Majdi A., Pazhuhi M., Ghasemi F., Khademi M., Pashazadeh F., Hamblin M.R., Cassano P. Transcranial Photobiomodulation Improves Cognitive Performance in Young Healthy Adults: A Systematic Review and Meta-Analysis. Photobiomodul. Photomed. Laser Surg. 2019;37:635–643. doi: 10.1089/photob.2019.4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vanin A.A., Verhagen E., Barboza S.D., Pena Costa L.O., Leal-Junior E.C.P. Photobiomodulation Therapy for the Improvement of Muscular Performance and Reduction of Muscular Fatigue Associated with Exercise in Healthy People: A Systematic Review and Meta-analysis. Lasers Med. Sci. 2018;33:181–214. doi: 10.1007/s10103-017-2368-6. [DOI] [PubMed] [Google Scholar]
- 58.Soheilifar S., Fathi H., Naghdi N. Photobiomodulation Therapy as a High Potential Treatment Modality for COVID-19. Lasers Med. Sci. 2021;36:935–938. doi: 10.1007/s10103-020-03206-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rentz L.E., Ulman H.K., Galster S.M. Deconstructing Commercial Wearable Technology: Contributions toward Accurate and Free-Living Monitoring of Sleep. Sensors. 2021;21:5071. doi: 10.3390/s21155071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stone J.D., Rentz L.E., Forsey J., Ramadan J., Markwald R.R., Finomore V.S., Galster S.M., Rezai A., Hagen J.A. Evaluations of Commercial Sleep Technologies for Objective Monitoring During Routine Sleeping Conditions. Nat. Sci. Sleep. 2020;12:821–842. doi: 10.2147/NSS.S270705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kinnunen H., Rantanen A., Kentta T., Koskimaki H. Feasible Assessment of Recovery and Cardiovascular Health: Accuracy of Nocturnal HR and HRV Assessed via Ring PPG in Comparison to Medical Grade ECG. Physiol. Meas. 2020;41:04NT01. doi: 10.1088/1361-6579/ab840a. [DOI] [PubMed] [Google Scholar]
- 62.Stone J.D., Ulman H.K., Tran K., Thompson A.G., Halter M.D., Ramadan J.H., Stephenson M., Finomore V.S., Galster S.M., Rezai A.R., et al. Assessing the Accuracy of Popular Commercial Technologies That Measure Resting Heart Rate and Heart Rate Variability. Front. Sports Act. Living. 2021;3:37. doi: 10.3389/fspor.2021.585870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.de Zambotti M., Rosas L., Colrain I.M., Baker F.C. The Sleep of the Ring: Comparison of the OURA sleep tracker against polysomnography. Behav. Sleep Med. 2019;17:124–136. doi: 10.1080/15402002.2017.1300587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cao R., Azimi I., Sarhaddi F., Niela-Vilen H., Axelin A., Liljeberg P., Rahmani A.M. Accuracy Assessment of Oura Ring Nocturnal Heart Rate and Heart Rate Variability in Comparison With Electrocardiography in Time and Frequency Domains: Comprehensive Analysis. J. Med. Internet. Res. 2022;24:e27487. doi: 10.2196/27487. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article cannot be shared publicly due to certain elements of the data being owned by a third party and are considered confidential. The data will be shared on reasonable request to the corresponding author.