Abstract
This study examines the relationship among COVID-19-induced social, economic, and educational inequalities on mental health (i.e., anxiety and depression). This study also examines if levels of self-rated health (SRH) moderate the relationship (i.e., COVID-induced inequalities [CII] and mental health), as well as examines the racial/ethnic group differences among 567 young adults in the mid-Atlantic region. Using a moderation model, results indicate that CII were significantly related to depression (b = .221, t(554) = 4.59, p = .000) and anxiety (b = .140, t(555) = 3.23, p = .001). SRH and race/ethnicity also moderated both relationships. At above-average SRH (i.e., moderator), higher CII were also significantly related to lower anxiety (Asian young adults only) and lower depression (Asian and White young adults only). Overall, SRH and race/ethnicity are important factors in the mental health impact of COVID-19 on young adults.
Keywords: COVID-19, Social determinants of health, Anxiety, Depression, Multivariate analysis
The COVID-19 pandemic has disproportionately impacted many lives in the United States (US). Recent reports continue to highlight how COVID-19 has generally exacerbated overall inequalities that already exist [1]. These inequalities also increase the already prevalent rates of mental health challenges among many young adults [2, 3]. However, the impact of distinct COVID-19-induced inequalities and protective factors (i.e., positive self-rated health, SRH) on mental health is understudied. Additionally, reports continue to suggest that not all young adults have been equally impacted by the COVID-19 pandemic, especially when examining those from race/ethnic minoritized communities [2]. This study, therefore, examines the relationship among COVID-induced inequalities (CII), levels of SRH, mental health, and race/ethnicity.
COVID-Induced Inequalities
Social determinants of health suggest that overall health is unevenly distributed throughout the general population, highlighting significant health disparities throughout the US [4]. These overall health disparities are more prominent among individuals of less-advantaged groups that experience a burden of inequalities in the areas of socio-economic factors and overall academic experiences [5, 6]. During the pandemic, social determinants of health have also impacted the disproportionate rates of COVID-19 diagnoses and mortality, as well as increased symptomatology of other comorbid health factors like mental health [2, 7, 8]. These overall inequalities also continue to impact access to social and health services, uncertain finances, household security, and social relationships [9, 10]. More attention, however, is needed on economic and educational inequalities, as well as the social relationships as it continues to relate to the COVID-19 pandemic.
Economic Inequalities
It has been consistently documented that economic inequalities have played a key role in overall health disparities as they contribute to segregation, decreased social mobility, and increased worry around food, as well as decreased access to medical care [3, 11]. Since the COVID-19 pandemic emerged, these economic inequalities became more prevalent due to employment lay-offs and the overall national recession [12–15]. Many of these factors, especially the financial hardships, were positively associated with depression [16]. Additionally, for many young adults who have been impacted by financial inequalities, their type of occupation has also led to further exposure and risks to COVID-19, as they are more likely to be employed as essential workers in high exposure risk settings. This further complicates the inequalities as these individuals may also lack access to healthcare insurance due to their low-income status. Therefore, economic inequalities are a key indicator of the overall COVID-19-induced inequalities with which some US young adults may be confronted with [16]. This is worthy of further investigation as it is related to the mental health of young adults who have experienced these inequalities.
Educational Inequalities
Another key COVID-19-induced inequality that many young adults continue to experience is in the educational domain. During the COVID-19 pandemic, most educational systems transitioned to remote learning [17–19]. Individuals who were not equipped to transition to remote learning may have been at a disadvantage due to their limited resources available to support their educational activities [20]. As a result, many individuals who transitioned to remote learning may not have had the infrastructure for virtual and remote learning [20]. For example, several financial factors (e.g., limited access to the internet, limited technological resources) may have limited young adults to transition to a remote space that nurtures an equitable academic environment during a high-stress global affair [21–23]. Therefore, educational inequalities are a key indicator of the understanding of overall COVID-19-induced inequalities that some young adults may be confronted with. This is worthy of further investigation as the overall consequences could have a lasting impact on young adults who have experienced these inequalities.
Social Relations
COVID-19 has not only augmented the economic and educational inequalities of young adults, but has also affected their social relations. As a result of the prolonged pandemic, emerging studies continue to highlight that social isolation has been on the rise due to social distance policies, and social location closures, and other pandemic-related factors [24, 25]. Son and colleagues note that since the start of the pandemic, 87% (n = 195) of the sampled reported interacting less with others due to social distancing [2]. One-third of the participants also expressed being worried about the lack of in-person interactions in which they were engaging [2]. Similarly, these changes in social relations have invoked concerns around the overall physical and psychological well-being [26]. Most importantly, loneliness has significantly impacted mental health among individuals with pre-existing mental health challenges [26–28]. Overall, the social relations that young adults may experience also serve as support [29]. Without these social relations, these supports may also reduce, making young adults more susceptible to mental health challenges.
COVID-19 Pandemic and Mental Health
The mental health of young adults has shown to be a general area of concern [30, 31]. With COVID-19 adding additional stressors to the everyday lives of young adults, emerging research suggests increased symptomatology around various mental health outcomes [2, 7, 32]. For example, Kecojevic and colleagues, in a study of 162 young adults, found that academic stress during this global pandemic was associated with higher levels of depression, anxiety, somatization, and overall stress [16]. Additionally, among non-US young adults, COVID-19-related financial stress was also negatively associated with depression and anxiety [13]. Additionally, worrying and fearing for their health and the health of their loved ones, difficulty concentrating due to COVID, disrupted sleep, decrease in interactions with others, and a growing concern with their academic performance impacted overall anxiety levels [2]. For example, Son and colleagues, using a sample of 195 young adults in the south, noted that 138 young adults (71%) indicated increased stress and anxiety due to the COVID-19 outbreak [2]. Many factors contributed to increased stress, anxiety, and depressive symptomatology. These factors contributed to additional worry about their health, concentrating difficulties, inability to sleep, and overall academic concerns. Hill and colleagues also noted that substance use increased among young adults as the COVID-19 pandemic progressed [33]. They specifically found that young adults who reported higher levels of substance use were more likely to report higher levels of alcohol consumption. Overall, young adults are experiencing elevated stressors due to the COVID-19 pandemic, which is negatively impacting their mental health.
Positive Self-rated Health: a Potential Moderator
Although these COVID-19-induced inequalities may be highly prevalent across young adults, it is important to also note other factors that may interact with these inequalities and mental health outcomes. SRH, a subjective response to one’s perception of health, has been extensively studied among older and the general adult samples [34–36]. Although subjective in nature, this one item response is reliable and valid, and has significant associations with other comorbid health outcomes [37–39]. However, little is known about SRH among young adults during and after the global pandemic. As noted above, many young adults are confronted with COVID-19-induced inequalities on top of the general stressors associated with academic and daily stressors [22]. Therefore, subjective SRH may further shed light on these associations.
Given that overall positive SRH has been consistently associated with positive health-related outcomes among young adults [40, 41], positive SRH may serve as a protective factor for mental health among young adults. Several psychological theories may explain these self-rated health outcomes. For example, higher self-efficacy and an internal locus of control have been linked with more positive perceptions of self-rated health [40, 42, 43] and adherence to overall health promotion and services [43]. However, studies across the general and older adult populations suggest racial, ethnic, and cultural differences [37, 44, 45]. Studies examining racial differences with SRH are needed to better capture individuals’ lived experiences. Therefore, more attention is needed on race/ethnicity, SRH, and objective mental health outcomes among young adults during and after the global pandemic.
Race/Ethnicity: a Potential Moderator
Literature highlights that racial and ethnic minoritized groups are being affected by COVID-19 at different rates [46–48]. There are many health disparities that may put certain individuals, such as racial minoritized groups, at risk of contracting COVID-19 [49, 50]. For example, discrimination exists in systems that are supposed to improve health and/or well-being of members in society [51–53]. Discrimination can also have a number of negative health outcomes and shape economic and social factors [54, 55] that may increase the likelihood of individuals from racially minoritized backgrounds in getting COVID-19. Additionally, some individuals of some racial/ethnic minoritized backgrounds live in housing conditions that make it challenging to COVID-19 prevention guidelines [56, 57]. Due to the growing unemployment rate caused by COVID-19 [58–60], some individuals may be forced to share housing [56, 57, 61]. Due to COVID-19 disproportionately impacting many young adults, particularly those that identify from an ethnic-racial minoritized group [46–48], it is important to take race/ethnicity into consideration.
Purpose of the Study
The current study aimed to examine the relationship between mental health, CII, SRH, and race. Research questions and hypothesis driven by the gaps in the literature are as follows:
Hypothesis 1: The relationship between CII and depression will be moderated by SRH and race. It is expected that Black, Latine, and Asian Americans who rate their SRH as below average and report more inequalities in economic, education, and social relationships (i.e., CII) will report higher levels of depression.
Hypothesis 2: The relationship between CII and anxiety will be moderated by SRH and race. It is expected that Black, Latine, and Asian Americans who rate their SRH as below average and report more inequalities will report higher levels of anxiety.
Method
The current study used a multiple moderation model to examine the relationship between race, SRH, CII, and mental health. Below is a description of the participants and procedures, the measures, and the data analysis plan.
Participants and Procedure
The participants in this study are from a larger study (n = 897). Participants in the current sample ranged in age from 18 to 21, with 86% of the sample reporting their age as 18. Given the focus of the current study on Asian American, Black, Latine, and Whites, the analytic sample for the current study is 567, which includes participants who identified with one of these four backgrounds. In terms of race, 25.2% (n = 204) identified as Asian, 20.2% (n = 164) as Black, 10.6% (n = 86) as Hispanic, and 44% as White (n = 357). Participants provided their self-reported gender identity, and 79.7% (n = 529) identified as cisgender women, 16.3% (n = 108) as cisgender men, and less than 3% as genderqueer, questioning, transgender male, or did not disclose. Finally, 32% (n = 287) self-reported as a first-generation college student. For the current models, the sample is n = 567.
The larger study is an ongoing, university-wide longitudinal study at an urban, predominantly White public university in the mid-Atlantic region, that focuses on genetic, environmental, and developmental influences on substance use and emotional health outcomes. The larger study was approved by the Institutional Review Board at the university. The supplemental COVID-19 survey was sent to participants in May of 2020 and data were collected for just over 2 months. Participants were informed about the study and provided informed consent. The survey took approximately 15–30 min to complete, and once completed, participants received $10 compensation. The developers utilized REDCap (Research Electronic Data Capture), which is a web-based application designed to assist data capture for research studies, to collect and manage survey data [62].
Measures
COVID-Induced Inequalities
This eight-item dichotomous scale asks participants about inequalities they are facing due to COVID-19 in three distinct domains: (1) Economic questions include the following: (a) has changes related to the coronavirus/COVID-19 crisis created financial problems for you or your family?; (b) to what degree are you concerned about the stability of your living situation?; and (c) do you worry about whether your food will run out because of a lack of money? Descriptive statistics for the economic subscale are as follows: n = 858, min = 0 and max = 3, M = 1.46 (SD = 0.94); (2) Education questions include the following: (a) do you have a lab, art, or other classes that were severely disrupted, i.e., did not transfer well into an online format?; (b) have your professors been easy to communicate with? (reverse coded); and (c) do you have easy access to the internet or a computer (reverse coded)? Descriptive statistics for the education subscale are as follows: n = 875, min = 0 and max = 3, M = 0.81 (SD = 0.69); (3) Social Relationships questions include the following: (a) has the quality of the relationships between you and members of your family changed? and (b) has the quality of relationships with friends changed? Descriptive statistics for the social relationships subscale are as follows: n = 882, min = 0 and max = 2, M = 0.40 (SD = 0.58). A total CII sum variable was created by summing the yes responses for all of the questions. Descriptive statistics for the total scale are as follows: n = 840, min = 0 and max = 7, M = 2.66 (SD = 1.44). A higher score is interpreted as more CII. Also, the CII mean is stratified by race in Table 1.
Table 1.
Correlation coefficients between variables of interest
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Age | - | |||||||
| 2. Race | − .025 | - | ||||||
| 3. Gender | .018 | .067 | - | |||||
| 4. UMI | .025 | .085* | .029 | - | ||||
| 5. SRH | − .043 | − .085* | − .152** | − .141** | - | |||
| 6. CII | − .071* | − .091* | − .035 | .096** | − .201** | - | ||
| 7. Anxiety | .004 | .122** | .182** | .117** | − .210** | .260** | - | |
| 8. Depression | .014 | .130** | .142** | .117** | − .232** | .332** | .715** | - |
*p < .05, **p < .01. UMI, underlying medical conditions; SRH, self-rated health; CII, COVID-induced inequalities
Depression and Anxiety
A subset of anxiety and depression scale items from the Symptoms Checklist-90 (SCL-90) [63] provided information about participant mental health. The SCL-90 is a self-report symptom inventory consisting of 90 items, and has well-established convergent and discriminant validity and reliability [64]. The items assess symptoms within the last 30 days of anxiety (e.g., “spells of terror or panic”) and depression (e.g., “feeling hopelessness about the future”). Responses are indicated on a 5-point scale, from 1 (not at all) to 5 (extremely); previous research has shown sufficient reliability for the anxiety scale (α = 0.85) and the depression scale (α = 0.89) [65]. The range of scores was 0–16 for both the anxiety and depression items. The mean for anxiety symptoms was 3.16 (SD = 4.03) and the mean for depression symptoms was 6.06 (SD = 4.72).
Self-rated Health
Participants provided information on their health through one self-report item, the Behavioral Risk Factor Surveillance System (BRFSS) Section 1 (CDC, 2014). The item read, “How would you describe your overall physical health?” Participants responded on a 5 point Likert scale, with the values as “1- Excellent” (n = 67, 10.6%), “2- Very good” (n = 247, 39.2%), “3- Good” (n = 248, 39.4%), “4- Fair” (n = 62, 9.8%), and “5- Poor” (n = 6, 1%). The mean was 2.51 (SD = 0.85). The item was reverse coded for the current study, so that 1 indicated poor self-rated health and 5 indicated excellent self-rated health. The BRFSS is a highly regarded predictor of global health and has been deemed effective in predicting adverse physical and mental health outcomes [66, 67].
Covariates
Students’ self-reported age in years, gender identity, and underlying medical conditions were included as covariates. To assess underlying medical conditions, the survey asked participants about their chronic health conditions, such as asthma and diabetes. The underlying medical condition variable was created by summing the yes or no responses to medical health conditions that the Centers for Disease Prevention and Control (CDC) determined to place an individual at increased risk for severe illness from COVID-19 [68]. There were a total of 14 dichotomous questions. A dichotomous variable was created, in which no = 0 (n = 653, 72.7%) and is interpreted to mean that a person has no underlying medical condition, and yes = 1 (n = 245, 27.3%) which is interpreted to mean that a person has at least one underlying medical condition.
Analytic Plan
A moderated moderation model was conducted in PROCESS macro for SPSS [69] to examine the moderating effect of race/ethnicity (i.e., Asian, Black, Latine, and White) and SRH on the relationship between COVID-induced social inequalities and mental health (i.e., anxiety and depression). Covariates (i.e., age, gender, underlying medical condition) were chosen based on their potential impact on the predictor and outcome variables. All variables were centered or dummy coded to reduce unnecessary collinearity.
Results
Preliminary Analysis
Preliminary analysis includes descriptive statistics and bivariate correlations. The sample size for each variable means, and standard deviations stratified by racial-ethnic group of participants. Bivariate correlations were used to examine the relationship between the two dependent variables (i.e., anxiety and depression), predictor (CII), moderators (SRH and race/ethnicity), and covariates (age, gender, and UMI; see Tables 2 and 3). The correlational analysis indicated that anxiety and depression were both related to all of the predictors, moderators, and covariates with the exception of age. Lastly, the data were analyzed to ensure regression assumptions of normality, linearity, and homoscedasticity were met [70]; and no major violations were found during the analysis. Missing data was also determined to be minimal (less than 5%).
Table 2.
Moderated moderation analysis assessing depression from variables of interest
| B | SE | t | p | |
|---|---|---|---|---|
| CII | .44 | .07 | 6.42 | .001** |
| SRH | − .17 | .14 | − 1.23 | .22 |
| Asian identity | .06 | .14 | .47 | .64 |
| Black identity | − .42 | .19 | − 2.24 | .03* |
| Latine identity | − .50 | .13 | − 4.03 | .001** |
| White identity | .44 | .12 | 3.54 | .001** |
| CII × SRH | − .17 | .08 | − 2.01 | .04* |
| CII × Asian | .29 | .10 | 2.98 | .003** |
| CII × Black | .35 | .15 | 2.35 | .02* |
| CII × Latine | .13 | .14 | .95 | .35 |
| CII × White | .21 | .08 | 2.53 | .01** |
| SRH × Asian | − .14 | .18 | − .76 | .45 |
| SRH × Black | − .21 | .23 | − .91 | .37 |
| SRH × Latine | − .12 | .16 | − .74 | .46 |
| SRH × White | − .10 | .20 | − .45 | .65 |
| CII × SRH × Asian | .13 | .11 | 1.17 | .24 |
| CII × SRH × Black | .14 | .18 | .74 | .46 |
| CII × SRH × Latine | .10 | .10 | 1.02 | .31 |
| CII × SRH × White | .03 | .17 | .19 | .84 |
| Gender | .18 | .07 | 2.75 | .01** |
| Age | − .08 | .23 | − .36 | .72 |
| UMI | .05 | .11 | .46 | .65 |
R2 = .23, p < .001; *p < .05, **p < .01. UMI, underlying medical conditions; SRH, self-rated health; CII, COVID-induced inequalities
Table 3.
Moderated moderation analysis assessing anxiety from variables of interest
| B | SE | t | p | |
|---|---|---|---|---|
| CII | .35 | .07 | 5.75 | .001** |
| SRH | − .08 | .12 | − .69 | .49 |
| Asian identity | − .32 | .11 | − 2.95 | .003** |
| Black identity | − .28 | .10 | − 2.61 | .01** |
| Latine identity | .28 | .17 | 1.69 | .09 |
| White identity | .28 | .11 | 2.58 | .01** |
| CII × SRH | − .18 | .07 | − 2.46 | .01** |
| CII × Asian | .19 | .08 | 2.56 | .01** |
| CII × Black | .21 | .09 | 2.40 | .02* |
| CII × Latine | .22 | .13 | 1.69 | .09 |
| CII × White | .03 | .13 | .23 | .82 |
| SRH × Asian | − .10 | .16 | − .63 | .53 |
| SRH × Black | − .11 | .20 | − .53 | .60 |
| SRH × Latine | − .11 | .14 | − .79 | .43 |
| SRH × White | − .22 | .18 | − 1.21 | .23 |
| CII × SRH × Asian | .39 | .16 | 2.35 | .02* |
| CII × SRH × Black | .14 | .10 | 1.37 | .17 |
| CII × SRH × Latine | − .31 | .15 | − 1.99 | .04* |
| CII × SRH × White | .07 | .09 | .85 | .39 |
| Gender | .26 | .06 | 4.56 | .001** |
| Age | − .17 | .20 | − .83 | .40 |
| UMI | .14 | .09 | 1.52 | .13 |
R2 = .21, p < .001; *p < .05, **p < .01. UMI, underlying medical conditions; SRH, self-rated health; CII, COVID-induced inequalities
Primary Analyses
For the primary analyses, two moderated moderation analyses were performed, with depression and anxiety as dependent variables in two separate models. The relationship between CII and depression and anxiety symptoms was examined, with race and SRH as moderators, while controlling for age, gender, and underlying medical condition. It was hypothesized that the relationship between CII and mental health would be moderated by SRH and race, such that Black, Latine, and Asian Americans who rate their overall health (i.e., SRH) as below average and report more inequalities in economic, education, and social relationships (i.e., CII) will report higher levels of depression (i.e., hypothesis one) and anxiety (i.e., hypothesis two).
Depression Symptoms: CII Moderated by Race and SRH
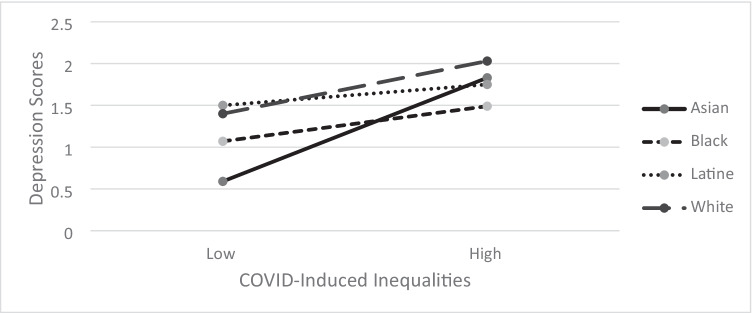
To examine whether race and levels of SRH moderated the relationship between CII and depression symptoms, a moderated moderation analysis was performed using PROCESS. Age, gender, and underlying medical conditions were added as covariates to the model. CII were significantly and positively related to depression (b = 0.44, SE = 0.07, p < 0.001). SRH was not significantly related to depression (b = − 0.17, p = 0.22). Identifying as White was significantly and positively related to depression (b = 0.44, SE = 0.12, p < 0.001). However, identifying as Black or Latine was significantly and negatively related to depression symptoms (b = − 0.42, p = 0.03; b = − 0.50, p < 0.001 respectively). Identifying as Asian was not significantly related to depression (b = 0.06, p = 0.64). There was a significant interaction between CII and SRH (b = − 0.17, SE = 0.08, p = 0.04); when SRH was low, increased CII were related to more depression symptoms. When SRH was high, CII were not associated with depression. There was also a significant interaction between CII and race/ethnicity. The interactions are illustrated in Fig. 1, which shows race/ethnicity moderates the relationship between CII and depression symptoms. For Black, Asian, and Whites, increases in CII were significantly related to depression (b = 0.35, p = 0.02; b = 0.29, p = 0.003; b = 0.21, p = . 01 respectively). For Latines, CII were not significantly related to depression (b = 0.13, p = 0.35). The combined influence of SRH and race on CII and depression scores was not significant (ps > 0.25).
Fig. 1.
The interaction effect of COVID-induced inequalities (CII) and racial-ethnic groups
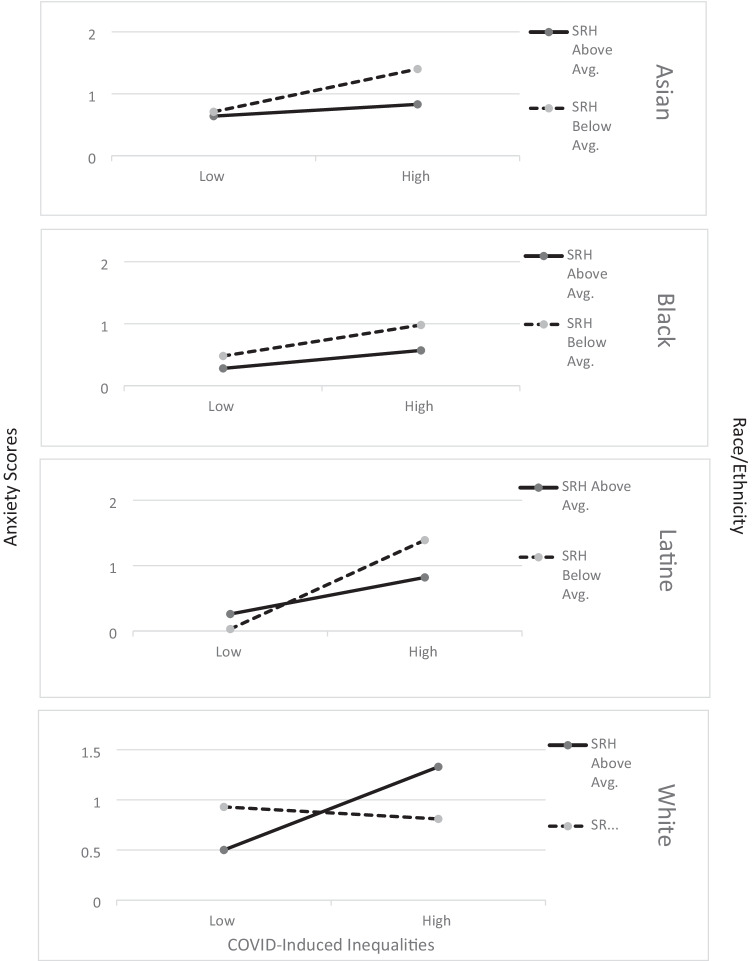
Anxiety Symptoms: CII Moderated by Race/Ethnicity and SRH
To examine whether race/ethnicity and SRH moderated the relationship between CII and anxiety symptoms, a moderated moderation analysis was performed using PROCESS. Age, gender, and underlying medical conditions were added as covariates to the model. CII were significantly and positively related to anxiety (b = 0.35, SE = 0.06, p < 0.001). Identifying as White was significantly and positively related to anxiety (b = 0.28, SE = 0.11, p = 0.01). However, identifying as Black or Asian was significantly and negatively related to anxiety symptoms (b = − 0.32, p = 0.003; b = − 0.28, p = 0.01 respectively). Identifying as Latine was not significantly related to anxiety (b = 0.28, p = 0.09). SRH was also not significantly related to anxiety symptoms (b = − 0.08, p = 0.49). There was a significant interaction between CII and SRH (b = − 0.18, SE = 0.07, p = 0.01); when SRH was low, increased CII experiences were related to more anxiety symptoms. When SRH was high, CII were not associated with anxiety. There were also significant interactions between CII and race/ethnicity. For Black and Asian students, increases in CII were significantly and positively related to anxiety symptoms (b = 0.21, p = 0.02, and b = 0.19, p = 0.01 respectively). For Latine and Whites, CII were not significantly related to anxiety (b = 0.22, p = 0.09; b = 0.03, p = 0.82). As well, the combined influence of SRH and race/ethnicity on the relationship between CII and anxiety symptoms was significant among Asians (b = 0.39, SE = 0.16, p = 0.02) and Latines (b = 0.31, SE = 0.15, p = 0.047). Among Asians who rated their health as below average, increases in CII were positively related to anxiety symptoms. Conversely, among Latines who rated their health as above average, increases in CII were positively related to anxiety symptoms (see Fig. 2).
Fig. 2.
The interaction effect of COVID-induced inequalities (CII), self-rated health (SRH), and racial-ethnic groups
Discussion
Despite widespread consequences of COVID-19 experienced by most, Americans, African Americans, Latine Americans, and Asian Americans in the US have been disproportionately adversely affected, with greater death of loved ones, social isolation, financial uncertainty, job loss, housing instability, and discrimination [71, 72]. Consistent with recent work with adults on COVID-19 inequalities and mental health, findings from the current study indicated that experiencing more COVID-19 inequalities was associated with more anxiety and depression symptoms in young adults as well. Furthermore, SRH exacerbated these experiences for those who reported more CII. Young adults who reported their SRH as lower and experienced more CII also reported more anxiety and depression symptoms. Our findings are consistent with recent work with those experiencing food insecurity during the COVID-19 pandemic [73].
Furthermore, the relationship between COVID-19 inequalities and depression symptoms differed among those of different racial and ethnic groups. When Asian Americans experienced fewer CII, they report fewer depression and anxiety symptoms than those of other racial and ethnic groups. However, when Asian Americans experienced more CII, they reported more depression and anxiety symptoms than other racial and ethnic groups. These results are consistent with other recent studies regarding Asian American individuals’ experiences during the pandemic, many of which have attributed these findings to pandemic-related discrimination [74–76]. Relatedly, when Black Americans experienced fewer CII, there were no differences in their reporting of depression or anxiety symptoms than those of other racial and ethnic groups. However, when Black Americans experienced more CII, they reported more depression and anxiety symptoms than of other racial and ethnic groups. This pattern was also found for White Americans but only for depression symptoms. There were no racial and ethnic group differences found among Latine Americans which is not consistent with previous research. Research focusing solely on young adults of color has found that increases in CII and the visibility of systemic racism during the pandemic have been detrimental to their well-being [77] and that COVID-related stressors are associated with increases in depression and anxiety symptoms [78]. Yet, other researches suggest that White Americans report more psychological symptoms than Black Americans [79]. Given that the majority of recent literature has shown that racial and ethnic young adults bear the burden of CII and discrimination experiences, the mental health burden of COVID-19 should continue to be assessed.
Limitations and Future Research
The current findings provide a more nuanced view of how COVID-19 inequalities influence the mental health of young adults by specifically examining how SRH and race/ethnicity influence this relationship. Although these findings contribute to the current literature on the impacts of COVID-19 on the health and well-being of young adults, they should be taken with a few limitations in mind. First, our sample of young adults resided in the mid-Atlantic region of the US. COVID experiences of our sample may have differed from a sample in other regions of the US. Future research should engage a national sample of young adults from different regions to examine if the relationships between mental health, SRH, CII, and race/ethnicity are sustained. Furthermore, our sample had fewer individuals that identified as Latine. This may have contributed to the lack of findings for this group. The present study should be replicated with a more representative sample of COVID-19 inequalities and pandemic-related experiences. Second, the cross-sectional nature of the study limited our ability to make causal and directional claims. That is, we were not able to draw definitive conclusions on how SRH and race/ethnicity lead to changes in the relationship between CII and mental health among young adults. Future work could investigate these specific patterns overtime, which can assist in the development of age-specific intervention methods. Lastly, the present study provided general insight into young adults’ experiences with COVID inequalities but did not provide contextual information, such as COVID-related discrimination, living situation (e.g., living alone), and loss of loved ones due to COVID. As young adults continue to cope with the daily difficulties of higher education in the time of COVID-19, there is a clear need to adjust existing resources to meet their psychosocial needs.
Conclusion
The unique effects of general life disruption, disruption of education/professional goals, and interpersonal and financial strain coupled with increased isolation and fewer social support resources have left several young adults, and especially those from racial/ethnic minority groups, feeling like mental health services are even further out of reach. As well, racial discrimination due to COVID-19 and systemic racism could have direct negative consequences for Asian American and African Americans’ feelings of safety to utilize mental health services or peer-led support groups. Leveraging telehealth and community organizations to help connect young adults to culturally informed, safe, and supportive environments is essential in promoting positive well-being as the effects of the COVID-19 pandemic continue.
Acknowledgements
The Spit for Science Working Group: Director: Danielle M. Dick. Co-Director: Ananda Amstadter. Registry management: Emily Lilley, Renolda Gelzinis, Anne Morris. Data cleaning and management: Katie Bountress, Amy E. Adkins, Nathaniel Thomas, Zoe Neale, Kimberly Pedersen, Thomas Bannard, Seung B. Cho. Data collection: Amy E. Adkins, Peter Barr, Holly Byers, Erin C. Berenz, Erin Caraway, Seung B. Cho, James S. Clifford, Megan Cooke, Elizabeth Do, Alexis C. Edwards, Neeru Goyal, Laura M. Hack, Lisa J. Halberstadt, Sage Hawn, Sally Kuo, Emily Lasko, Jennifer Lend, Mackenzie Lind, Elizabeth Long, Alexandra Martelli, Jacquelyn L. Meyers, Kerry Mitchell, Ashlee Moore, Arden Moscati, Aashir Nasim, Zoe Neale, Jill Opalesky, Cassie Overstreet, A. Christian Pais, Kimberly Pedersen, Tarah Raldiris, Jessica Salvatore, Jeanne Savage, Rebecca Smith, David Sosnowski, Jinni Su, Nathaniel Thomas, Chloe Walker, Marcie Walsh, Teresa Willoughby, Madison Woodroof, Jia Yan. Genotypic data processing and cleaning: Cuie Sun, Brandon Wormley, Brien Riley, Fazil Aliev, Roseann Peterson, Bradley T. Webb. We would like to thank the Spit for Science participants for making this study a success, as well as the many University faculty, students, and staff who contributed to the design and implementation of the project. We would also like to acknowledge The COVID-19 Black, Indigenous and/or People of Color (BIPOC) Student Experiences Group: Chelsea D. Williams (Chair), Ashlynn Bell, Karen G. Chartier, Eryn N. DeLaney, Lisa Fuentes, Chaz Goodman, Terrell A. Hicks, Kristina B. Hood, Kaprea F. Johnson, and Sydney Judge, Oswaldo Moreno, Roseann E. Peterson, Diamond Reese, Jennifer Rodriguez, and Chloe J. Walker
Author Contribution
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Kaprea Johnson and Kristina Hood. The first draft of the manuscript was written by Kaprea Johnson, Kristina Hood, and Oswaldo Moreno and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
Spit for Science has been supported by Virginia Commonwealth University, P20 AA017828, R37AA011408, K02AA018755, P50 AA022537, and K01AA024152 from the National Institute on Alcohol Abuse and Alcoholism, and UL1RR031990 from the National Center for Research Resources and National Institutes of Health Roadmap for Medical Research. This research was also supported by the National Institute on Drug Abuse (NIDA) of the National Institutes of Health under Award Number U54DA036105 and the Center for Tobacco Products of the US Food and Drug Administration. The content is solely the responsibility of the authors and does not necessarily represent the views of the NIH or the FDA. Data from this study are available to qualified researchers via dbGaP (phs001754.v2.p1). TA Hicks is supported by NIDA F31DA048559. RE Peterson is supported by NIMH K01MH113848 and The Brain & Behavior Research Foundation NARSAD grant 28632 P&S Fund.
Declarations
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board of Virginia Commonwealth University.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
The authors affirm that human research participants provided informed consent for publication of the images in Figs. 1 and 2.
Competing Interests
The authors declare no competing interests.
Footnotes
Ananda B. Amstadter and Danielle M. Dick are responsible for funding and overarching program direction for the Spit for Science COVID-19-related research.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kristina B. Hood, Email: hoodkb@vcu.edu
The Spit for Science Working Group:
Danielle M. Dick, Ananda Amstadter, Emily Lilley, Renolda Gelzinis, Anne Morris, Katie Bountress, Amy E. Adkins, Nathaniel Thomas, Zoe Neale, Kimberly Pedersen, Thomas Bannard, Seung B. Cho, Amy E. Adkins, Peter Barr, Holly Byers, Erin C. Berenz, Erin Caraway, Seung B. Cho, James S. Clifford, Megan Cooke, Elizabeth Do, Alexis C. Edwards, Neeru Goyal, Laura M. Hack, Lisa J. Halberstadt, Sage Hawn, Sally Kuo, Emily Lasko, Jennifer Lend, Mackenzie Lind, Elizabeth Long, Alexandra Martelli, Jacquelyn L. Meyers, Kerry Mitchell, Ashlee Moore, Arden Moscati, Aashir Nasim, Zoe Neale, Jill Opalesky, Cassie Overstreet, A. Christian Pais, Kimberly Pedersen, Tarah Raldiris, Jessica Salvatore, Jeanne Savage, Rebecca Smith, David Sosnowski, Jinni Su, Nathaniel Thomas, Chloe Walker, Marcie Walsh, Teresa Willoughby, Madison Woodroof, Jia Yan, Cuie Sun, Brandon Wormley, Brien Riley, Fazil Aliev, Roseann Peterson, and Bradley T. Webb
References
- 1.van Dorn A, Cooney RE, Sabin ML. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395:1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students’ mental health in the United States: interview survey study. J Med Internet Res. 2020;22:e21279. doi: 10.2196/21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oronce CIA, Scannell CA, Kawachi I, Tsugawa Y. Association between state-level income inequality and COVID-19 cases and mortality in the USA. J Gen Intern Med. 2020;35:2791–2793. doi: 10.1007/s11606-020-05971-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Hedel K, Avendano M, Berkman LF, Bopp M, Deboosere P, Lundberg O, Martikainen P, Menvielle G, van Lenthe FJ, Mackenbach JP. The contribution of national disparities to international differences in mortality between the United States and 7 European countries. Am J Public Health. 2015;105:e112–e119. doi: 10.2105/AJPH.2014.302344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 6.Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, Bergeron A, Cutler D. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315:1750–1766. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhai Y, Du X. Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Res. 2020;288:113003. doi: 10.1016/j.psychres.2020.113003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blundell R, Costa Dias M, Joyce R, Xu X. COVID-19 and inequalities. Fisc Stud. 2020 doi: 10.1111/1475-5890.12232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Witteveen D, Velthorst E. Economic hardship and mental health complaints during COVID-19. Proc Natl Acad Sci U S A. 2020;117:27277–27284. doi: 10.1073/pnas.2009609117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980–2015. Lancet. 2017;389:1475–1490. doi: 10.1016/S0140-6736(17)30571-8. [DOI] [PubMed] [Google Scholar]
- 12.Headey D, Goudet S, Lambrecht I, Maffioli EM, Oo TZ, Russell T. Poverty and food insecurity during COVID-19: phone-survey evidence from rural and urban Myanmar in 2020. Glob Food Sec. 2022;33:100626. doi: 10.1016/j.gfs.2022.100626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lauren BN, Silver ER, Faye AS, et al. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutr. 2021;24(12):3929–3936. doi: 10.1017/S1368980021000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilson JM, Lee J, Fitzgerald HN, Oosterhoff B, Sevi B, Shook NJ. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. J Occup Environ Med. 2020;62:686–691. doi: 10.1097/JOM.0000000000001962. [DOI] [PubMed] [Google Scholar]
- 15.Population Council Institute. Critical needs during COVID-19 lockdown: job, food, cash, medicines—who needs what? 2020. 10.31899/pgy14.1014
- 16.Kecojevic A, Basch CH, Sullivan M, Davi NK. The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study. PLoS ONE. 2020;15:e0239696. doi: 10.1371/journal.pone.0239696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vollbrecht PJ, Porter-Stransky KA, Lackey-Cornelison WL. Lessons learned while creating an effective emergency remote learning environment for students during the COVID-19 pandemic. Adv Physiol Educ. 2020;44:722–725. doi: 10.1152/advan.00140.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ma G. The effectiveness of synchronous online flipped learning in college EFL reading course during the COVID-19 epidemic. Res Square. 2020. 10.21203/rs.3.rs-84578/v1
- 19.Almarzooq ZI, Lopes M, Kochar A. Virtual learning during the COVID-19 pandemic: a disruptive technology in graduate medical education. J Am Coll Cardiol. 2020;75:2635–2638. doi: 10.1016/j.jacc.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Engzell P, Frey A, Verhagen MD. Learning loss due to school closures during the COVID-19 pandemic. SocArXiv. 2020. 10.31235/osf.io/ve4z7. [DOI] [PMC free article] [PubMed]
- 21.Jæger MM, Blaabæk EH. Inequality in learning opportunities during COVID-19: evidence from library takeout. Res Soc Stratif Mobil. 2020;68:100524. doi: 10.1016/j.rssm.2020.100524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martinez S. A political view from social work. In: Lavalette M, Ioakimidis V, Ferguson I, editors. Social work and the COVID-19 pandemic. 1. Bristol: Bristol University Press; 2020. pp. 31–36. [Google Scholar]
- 23.Armitage R, Nellums LB. Considering inequalities in the school closure response to COVID-19. Lancet Glob Health. 2020;8:e644. doi: 10.1016/S2214-109X(20)30116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180:817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 25.Killgore WDS, Cloonan SA, Taylor EC, Dailey NS. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 2020;290:113117. doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saraswathi I, Saikarthik J, Senthil Kumar K, Madhan Srinivasan K, Ardhanaari M, Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. 2020;8:e10164. doi: 10.7717/peerj.10164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. 2020;22:e22817. doi: 10.2196/22817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamza CA, Ewing L, Heath NL, Goldstein AL. When social isolation is nothing new: a longitudinal study on psychological distress during COVID-19 among university students with and without preexisting mental health concerns. Can Psychol. 2021;62:20–30. doi: 10.1037/cap0000255. [DOI] [Google Scholar]
- 29.Johnson KF, Brookover DL, Bradbrook K. Social health needs and promotive health factors scale for college students: scale development and initial validation. J Am Coll Health. 2022;70:74–83. doi: 10.1080/07448481.2020.1725021. [DOI] [PubMed] [Google Scholar]
- 30.Auerbach RP, Mortier P, Bruffaerts R, et al. WHO World Mental Health Surveys International College Student Project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623–638. doi: 10.1037/abn0000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Evans TM, Bira L, Gastelum JB, Weiss LT, Vanderford NL. Evidence for a mental health crisis in graduate education. Nat Biotechnol. 2018;36:282–284. doi: 10.1038/nbt.4089. [DOI] [PubMed] [Google Scholar]
- 32.Williams CD, Hood KB, Moreno O, et al. The impact of COVID-19 disruptions and perceived discrimination on well-being and posttraumatic stress disorder symptoms: testing the moderating role of exercise among African American and Asian American emerging adults. Emerg Adulthood. 2021;9:506–515. doi: 10.1177/21676968211038793. [DOI] [Google Scholar]
- 33.Hicks TA, Chartier KG, Buckley TD, Reese D, Working Group TSFS. Vassileva J, Dick DM, Amstadter AB, Peterson RE, Moreno O. Divergent changes: abstinence and higher-frequency substance use increase among racial/ethnic minority young adults during the COVID-19 global pandemic. Am J Drug Alcohol Abuse. 2022;48:88–99. doi: 10.1080/00952990.2021.1995401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- 35.Altman CE, Van Hook J, Hillemeier M. What does self-rated health mean? Changes and variations in the association of obesity with objective and subjective components of self-rated health. J Health Soc Behav. 2016;57:39–58. doi: 10.1177/0022146515626218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bravo AJ, Villarosa-Hurlocker MC, Pearson MR, Protective Strategies Study Team College student mental health: an evaluation of the DSM-5 self-rated Level 1 cross-cutting symptom measure. Psychol Assess. 2018;30:1382–1389. doi: 10.1037/pas0000628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chandola T, Jenkinson C. Validating self-rated health in different ethnic groups. Ethn Health. 2000;5:151–159. doi: 10.1080/713667451. [DOI] [PubMed] [Google Scholar]
- 38.Assari S. Ethnic groups differ in how poor self-rated mental health reflects psychiatric disorders. J Racial Ethn Health Disparities. 2018;5:728–736. doi: 10.1007/s40615-017-0417-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bailis DS, Segall A, Chipperfield JG. Two views of self-rated general health status. Soc Sci Med. 2003;56:203–217. doi: 10.1016/S0277-9536(02)00020-5. [DOI] [PubMed] [Google Scholar]
- 40.Bunda K, Busseri MA. Lay theories of health, self-rated health, and health behavior intentions. J Health Psychol. 2019;24:979–988. doi: 10.1177/1359105316689143. [DOI] [PubMed] [Google Scholar]
- 41.Molden DC, Dweck CS. Finding “meaning” in psychology: a lay theories approach to self-regulation, social perception, and social development. Am Psychol. 2006;61:192–203. doi: 10.1037/0003-066X.61.3.192. [DOI] [PubMed] [Google Scholar]
- 42.Parkatti T, Deeg DJ, Bosscher RJ, Launer LL. Physical activity and self-rated health among 55- to 89-year-old Dutch people. J Aging Health. 1998;10:311–326. doi: 10.1177/089826439801000303. [DOI] [PubMed] [Google Scholar]
- 43.Luszczynska A, Schwarzer R, Lippke S, Mazurkiewicz M. Self-efficacy as a moderator of the planning-behaviour relationship in interventions designed to promote physical activity. Psychol Health. 2011;26:151–166. doi: 10.1080/08870446.2011.531571. [DOI] [PubMed] [Google Scholar]
- 44.Jylhä M, Guralnik JM, Ferrucci L, Jokela J, Heikkinen E. Is self-rated health comparable across cultures and genders? J Gerontol B Psychol Sci Soc Sci. 1998;53:S144–S152. doi: 10.1093/geronb/53B.3.S144. [DOI] [PubMed] [Google Scholar]
- 45.Assari S. Gender differences in the predictive role of self-rated health on short-term risk of mortality among older adults. SAGE Open Med. 2016;4:2050312116666975. doi: 10.1177/2050312116666975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398–402. doi: 10.1007/s40615-020-00756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gauthier GR, Smith JA, García C, Garcia MA, Thomas PA. Exacerbating inequalities: social networks, racial/ethnic disparities, and the COVID-19 pandemic in the United States. J Gerontol B Psychol Sci Soc Sci. 2021;76:e88–e92. doi: 10.1093/geronb/gbaa117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thakur N, Lovinsky-Desir S, Bime C, Wisnivesky JP, Celedón JC. The structural and social determinants of the racial/ethnic disparities in the U.S. COVID-19 pandemic. What’s our role? Am J Respir Crit Care Med. 2020;202:943–949. doi: 10.1164/rccm.202005-1523PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the US. J Clin Med Res. 2020 doi: 10.3390/jcm9082442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ravi K. Ethnic disparities in COVID-19 mortality: are comorbidities to blame? Lancet. 2020;396:22. doi: 10.1016/S0140-6736(20)31423-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Doubeni CA, Simon M, Krist AH. Addressing systemic racism through clinical preventive service recommendations from the US Preventive Services Task Force. JAMA. 2021;325:627–628. doi: 10.1001/jama.2020.26188. [DOI] [PubMed] [Google Scholar]
- 52.Mensah GA, Glover MJ. Epidemiology of racial and ethnic disparities in health and healthcare. In: Williams RA, editor. Eliminating healthcare disparities in America: beyond the IOM report. Totowa: Humana Press; 2007. pp. 21–40. [Google Scholar]
- 53.Ayanian JZ, Williams RA. Principles for eliminating racial and ethnic disparities in healthcare. In: Williams RA, editor. Eliminating healthcare disparities in America: beyond the IOM report. Totowa: Humana Press; 2007. pp. 377–389. [Google Scholar]
- 54.Fix RL, Risco CM, Fix ST, Bernat EM. How racial identity and worry about discrimination impact coping responses to racial discrimination among Black American community members. J Racial Ethn Health Disparities. 2021 doi: 10.1007/s40615-021-00996-8. [DOI] [PubMed] [Google Scholar]
- 55.Segre LS, Mehner BT, Brock RL. Perceived racial discrimination and depressed mood in perinatal women: an extension of the domain specific stress index. Womens Health Issues. 2021;31:254–262. doi: 10.1016/j.whi.2020.12.008. [DOI] [PubMed] [Google Scholar]
- 56.McKnight-Eily LR, Okoro CA, Strine TW, Verlenden J, Hollis ND, Njai R, Mitchell EW, Board A, Puddy R, Thomas C. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic - United States, April and May 2020. MMWR Morb Mortal Wkly Rep. 2021;70:162–166. doi: 10.15585/mmwr.mm7005a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Snowden LR, Graaf G. COVID-19, social determinants past, present, and future, and African Americans’ health. J Racial Ethn Health Disparities. 2021;8:12–20. doi: 10.1007/s40615-020-00923-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kassa MD, Grace JM. Race against death or starvation? COVID-19 and its impact on African populations. Public Health Rev. 2020;41:30. doi: 10.1186/s40985-020-00139-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Galea S, Abdalla SM. COVID-19 pandemic, unemployment, and civil unrest: underlying deep racial and socioeconomic divides. JAMA. 2020;324:227–228. doi: 10.1001/jama.2020.11132. [DOI] [PubMed] [Google Scholar]
- 60.Moen P, Pedtke JH, Flood S. Disparate disruptions: intersectional COVID-19 employment effects by age, gender, education, and race/ethnicity. Work Aging Retire. 2020;6:207–228. doi: 10.1093/workar/waaa013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.DiMaggio C, Klein M, Berry C, Frangos S. Black/African American communities are at highest risk of COVID-19: spatial modeling of New York city ZIP code-level testing results. Ann Epidemiol. 2020;51:7–13. doi: 10.1016/j.annepidem.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale–preliminary report. Psychopharmacol Bull. 1973;9:13–28. [PubMed] [Google Scholar]
- 64.Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the SCL-90: a study in construct validation. J Clin Psychol. 1977;33:981–989. doi: 10.1002/1097-4679(197710)33:4<981::AID-JCLP2270330412>3.0.CO;2-0. [DOI] [Google Scholar]
- 65.Dick DM, Nasim A, Edwards AC, et al. Spit for Science: launching a longitudinal study of genetic and environmental influences on substance use and emotional health at a large US university. Front Genet. 2014;5:47. doi: 10.3389/fgene.2014.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pierannunzi C, Hu SS, Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med Res Methodol. 2013;13:1–14. doi: 10.1186/1471-2288-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Krause JS, Coker J, Charlifue S, Whiteneck GG. Health behaviors among American Indians with spinal cord injury: comparison with data from the 1996 Behavioral Risk Factor Surveillance System. Arch Phys Med Rehabil. 1999;80:1435–1440. doi: 10.1016/S0003-9993(99)90255-1. [DOI] [PubMed] [Google Scholar]
- 68.Honein MA, Christie A, Rose DA, et al. Summary of guidance for public health strategies to address high levels of community transmission of SARS-CoV-2 and related deaths, December 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1860–1867. doi: 10.15585/mmwr.mm6949e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Press; 2013. [Google Scholar]
- 70.Tabachnick BG, Fidell LS, Ullman JB. Using multivariate statistics. Boston: Pearson; 2007. [Google Scholar]
- 71.Kantamneni N. The impact of the COVID-19 pandemic on marginalized populations in the United States: a research agenda. J Vocat Behav. 2020;119:103439. doi: 10.1016/j.jvb.2020.103439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Poteat T, Millett GA, Nelson LE, Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann Epidemiol. 2020;47:1–3. doi: 10.1016/j.annepidem.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Polsky JY, Gilmour H. Food insecurity and mental health during the COVID-19 pandemic. Health Rep. 2020;31:3–11. doi: 10.25318/82-003-x202001200001-eng. [DOI] [PubMed] [Google Scholar]
- 74.Lee S, Waters SF. Asians and Asian Americans’ experiences of racial discrimination during the COVID-19 pandemic: impacts on health outcomes and the buffering role of social support. Stigma Health. 2021;6:70–78. doi: 10.1037/sah0000275. [DOI] [Google Scholar]
- 75.Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chen JA, Zhang E, Liu CH. Potential impact of COVID-19-related racial discrimination on the health of Asian Americans. Am J Public Health. 2020;110:1624–1627. doi: 10.2105/AJPH.2020.305858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Molock SD, Parchem B. The impact of COVID-19 on college students from communities of color. J Am Coll Health. 2021;1–7. 10.1080/07448481.2020.1865380. [DOI] [PubMed]
- 78.Rudenstine S, McNeal K, Schulder T, et al. Depression and anxiety during the COVID-19 pandemic in an urban, low-income public university sample. J Trauma Stress. 2021;34(1):12–22. doi: 10.1002/jts.22600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Charles NE, Strong SJ, Burns LC, Bullerjahn MR, Serafine KM. Increased mood disorder symptoms, perceived stress, and alcohol use among college students during the COVID-19 pandemic. Psychiatry Res. 2021;296:113706. doi: 10.1016/j.psychres.2021.113706. [DOI] [PMC free article] [PubMed] [Google Scholar]