Background and Objective
Electronic health records (EHRs) have become ubiquitous in medicine and continue to grow in informational content. Little has been documented regarding patient safety from the resultant information overload. The objective of this literature review is to better understand how information overload in EHR affects patient safety.
Methods
A literature search was performed using the Transparent Reporting of Systematic Reviews and Meta-Analyses standards for literature review. PubMed and Web of Science were searched and articles selected that were relevant to EHR information overload based on keywords.
Results
The literature search yielded 28 articles meeting the criteria for the study. Information overload was found to increase physician cognitive load and error rates in clinical simulations. Overabundance of clinically irrelevant information, poor data display, and excessive alerting were consistently identified as issues that may lead to information overload.
Conclusions
Information overload in EHRs may result in higher error rates and negatively impact patient safety. Further studies are necessary to define the role of EHR in adverse patient safety events and to determine methods to mitigate these errors. Changes focused on the usability of EHR should be considered with the end user (physician) in mind. Federal agencies have a role to play in encouraging faster adoption of improved EHR interfaces.
Key Words: EHR safety, electronic health record, information overload, note bloat
Electronic health records (EHRs) continue to increase in usage around the world, in part, because of the improvements in patient safety.1 In the United States, EHR adoption was initially encouraged through financial incentives by congress through the HITECH Act. More recently, the Centers for Medicaid & Medicare Services (CMS) has incentivized EHR adoption by decreasing reimbursement to providers who have not demonstrated themselves as “meaningful users” of EHRs.2 Despite its advantages over paper-based documentation, EHR use has resulted in new physician-related challenges that may increase medical errors.3 In anticipation of potential increased medical errors, the American Medical Informatics Association Board of Directors met in 2012 to create recommendations on enhancing patient safety by improving EHR usability.4 Despite highlighting 14 usability principles to improve EHRs, no further solutions were identified beyond minimizing cognitive load.
A major complaint of physicians is the extraneous patient information in each medical chart.5 Excessive information in a chart, or “note bloat,” may impair comprehension, leading to potential errors.6,7 Studies show that physicians spend nearly twice as much time documenting in EHR than they do interacting with patients.8 This is a source of frustration for physicians, but may also compromise patient safety.9 This is compounded by EHR software that is optimized for billing, not patient care.10 One study looking at adverse patient safety events due to the EHR cited a lack of EHR usability for 28% of these events.11 Overload from EHRs can also negatively affect physician well-being.12
The purpose of this systematic review is to evaluate the effect of EHR information overload on patient safety. Our hypothesis is that information overload in the EHR negatively affects patient safety.
METHODS
A systematic review and qualitative analysis were performed to identify factors related to EHR information overload and patient safety using PubMed and Web of Science. Studies that were published between January 2010 and January 8, 2021, were eligible for inclusion. Eligible articles were reviewed from June 15, 2018, to January 8, 2021, by 2 reviewers. Filters were English only and full-text availability. Articles were screened by first assessing the title and then the abstract for relevance to the topic by keywords. Keywords used included “electronic health record” or “electronic medical record” in conjunction with 1 or more of the following: “information overload,” “cognitive overload,” “note bloat,” “usability,” and “patient safety.” Studies were deemed relevant if they (a) defined the issue of information overload, (b) described how information overload fits into the current model of EHR safety analysis, and/or (c) provided data demonstrating how information overload and poor EHR usability affect physician comprehension of clinical data. References of selected articles were also reviewed as an additional source of literature.
All published study types were included. All data analyses were descriptive. Institutional review board approval was not required for this study.
RESULTS
As of January 8, 2021, a total 7322 records were obtained using PubMed and Web of Science and adding relevant references from the selected articles. Six thousand nine hundred nine titles were discarded because of irrelevant topics or duplication. Of the 413 abstracts reviewed, 339 were discarded because of lack of original research or not being physician focused. This left 51 articles to be assessed for eligibility, of which 29 fulfilled the inclusion criteria (Fig. 1).
FIGURE 1.
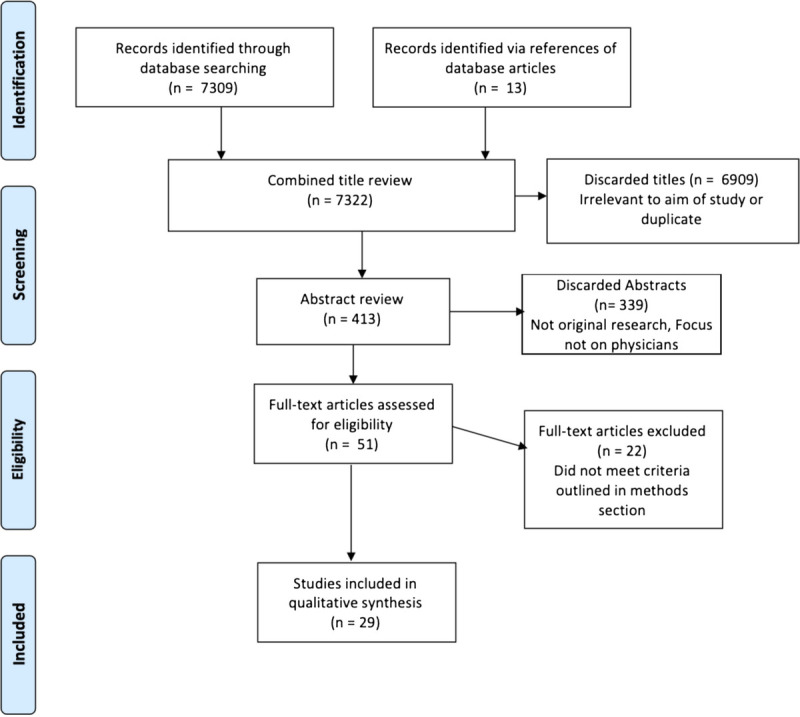
Inclusion flow diagram.
Cognitive Burden of Information Overload
Beasley et al13 define information overload in the context of clinical practice as excessive data, whether that be from the patient’s chart, history, and physical exam, among others, which hinders the provider’s ability to create an appropriate diagnosis and treatment plan. The overload of information stems from copying and pasting into charts, use of templates, excessive alerts, and adding data that are necessary for billing but effectively useless for clinical care.13,14
A study using eye tracker technology determined that vitals and laboratory values in patients’ charts were used the most by physicians, whereas other routine information was unnecessary and impaired usability.15 Another study illustrated that differences in cognitive load can affect error rates when using EHRs via the National Aeronautics and Space Administration task load index. Twenty intensivists reviewed patient data in both a conventional and novel, streamlined EHR only displaying salient information. The median National Aeronautics and Space Administration task load index score for the novel EHR was almost 20 points lower than the conventional EHR. Moreover, the conventional EHR was associated with 4 times as many errors per subject and took approximately twice as long to complete tasks when compared with the novel EHR.16 A similar study determined that a 1-page EHR with a higher density of pertinent information was preferable to one with multiple tabs and improved cognitive workloads.17
Koopman et al10 performed a cognitive task analysis with 16 primary care physicians. Subjects reviewed the assessment and plan first because it provided most of the necessary information in a concise manner. Identified drivers of note overload were as follows: billing, quality improvement measures, avoiding malpractice, compliance, the visit history, and physical exam. Another study found that EHRs were burdensome because they did not align with residents’ workflow, possibly compromising patient safety.18 An earlier study interviewed physicians about their information needs, finding the review of systems “superfluous” and contributing to information overload.9,19
Belden et al20 investigated restructuring the notes in EHR to decrease cognitive overload. The traditional “SOAP” (Subjective, Objective, Assessment, Plan) note was compared with a “APSO” format with an option to hide extraneous information. A simulated case demonstrated that simply changing the format of the note without changing content resulted in better usability, and the physicians endorsed this arrangement as more practical.
The EHR training sessions and the use of templates effectively decrease information overload by helping physicians write more concise notes, ultimately saving 1.3 hours of time.21
A study of physicians reviewing the same information showed a significant increase in reading efficiency with a user composable interface versus a traditional EHR. Seventy-two percent of information was reviewed more than once in conventional EHRs, compared with 17% in the user composable version. The poor usability of conventional EHRs decreases physician comprehension, requiring data to be revisited.22
However, a user composable interface does not guarantee increased efficiency.23 The usability and safety of 2 user composable EHRs were assessed by having 4 groups of 12 to 15 physicians from different institutions (2 groups using Epic, 2 groups using Cerner) complete specific tasks. Performance was assessed by error rates, number of clicks, and completion time. Results showed up to an 8-fold difference in task completion time and clicks between the groups at different sites using the same EHR. Implementation protocols and physician training varied between the 2 sites and were hypothesized to account for the vast difference in proficiency.
Alert fatigue is another source of information overload. In a survey of 2590 primary care physicians, 69.6% reported receiving more information than they could manage. In addition, nearly 30% of participants reported missing test results and delaying patient care as a result.14 Another study demonstrated that a clinician’s likelihood of accepting best practice reminders decreased with increases in volume of reminders, number of repeated reminders, and overall patient complexity.24 A program to decrease alerts of lesser importance in the Department of Veteran’s Affairs was implemented, which reduced daily notifications from 128 to 116 per physician, saving 90 minutes of work per week.25
Murphy et al26 investigated the shortcomings of the EHR inbox by interviewing physicians. Barriers identified included the following: message processing complexity, inbox interface design, cognitive load, team communication, and message content. The authors argue that these barriers decrease efficiency and situational awareness, which in turn undermines patient care (Table 1).
TABLE 1.
Level of Evidence
| Author | Year | Type of Study | Level of Evidence | Summary |
|---|---|---|---|---|
| Pickering et al27 | 2010 | Crossover | III | Simulation cases to test novel EHR in ICU |
| Beasley et al13 | 2011 | Expert opinion | VII | Defining information chaos |
| Ahmed et al16 | 2011 | Randomized crossover study | II | Assessment of physician cognitive load with 2 different EHR interfaces |
| Middleton et al4 | 2013 | Expert opinion | VII | EHR improvement recommendations |
| March et al6 | 2013 | Controlled trial | III | Simulation to assess EHR safety in the ICU setting |
| Singh et al14 | 2013 | Descriptive | VI | Assessment of physician information overload due to excessive alerting |
| Clarke et al19 | 2014 | Descriptive | VI | Physicians identifying important sections of notes |
| Adler-Milstein et al3 | 2015 | Cohort | IV | Hospital performance after EHR adoption |
| Koopman et al10 | 2015 | Descriptive | VI | Assessment of primary care physician interpretation of EHR notes |
| Sinsky et al5 | 2016 | Descriptive | VI | Allocation of physician time in ambulatory practice |
| Sittig et al9 | 2016 | Descriptive | VI | Unintended consequences of EHR |
| Wright et al15 | 2016 | Descriptive | VI | Observation of physician EHR viewing patterns |
| Senathirajah et al22 | 2016 | Mixed methods | V | Comparing user composable EHR versus nonuser composable |
| Zulman et al7 | 2016 | Expert opinion | VII | How EHR takes away from the physician-patient interaction |
| Arndt et al8 | 2017 | Descriptive | VI | Time spent with EHR among primary care physicians |
| Vainiomäki et al12 | 2017 | Descriptive | VI | EHR factors relating to physician well-being |
| Zelmer et al1 | 2017 | Descriptive | VI | International EHR information exchange |
| Belden et al20 | 2017 | Controlled trial | III | Assessing cognitive load based on different note organization |
| Ancker et al24 | 2017 | Retrospective cohort study | IV | Studying the effects of alert fatigue on physicians |
| Howe et al11 | 2018 | Descriptive | VI | Measuring contribution of EHR to patient harm |
| Kahn et al21 | 2018 | Multicenter, nonrandomized prospective trial | III | Assessing improvement in note bloat after intervention |
| Ratwani et al23 | 2018 | Controlled trial | III | Comparing differences in physician EHR competency with differing training levels |
| Khairat et al28 | 2018 | Observational | VI | Survey of physician satisfaction with EHR after performing clinical simulations |
| Shah et al25 | 2019 | Controlled trial | III | Assessing changes in physician workload after reducing unnecessary alerts |
| Murphy et al26 | 2019 | Expert opinion | VII | Interviews to discuss EMR inbox shortfalls |
| Khairat et al29 | 2019 | Cohort | VI | Differences in EHR use between men and women |
| Al Ghalayini et al17 | 2020 | Controlled trial | IV | Assess performance and perception of modified EHR |
| Berg et al18 | 2020 | Descriptive | VI | Residents’ perspectives on EHR use |
| Melnick et al30 | 2020 | Descriptive | VI | Survey to assess usability and EHR perceptions |
| Melnick et al31 | 2020 | Descriptive | VI | Survey to assess EHR usability and physician burnout |
Efficiency of and satisfaction with EHRs have been associated with user characteristics. For example, stage in training (attending versus resident physician) was evaluated by case simulations and a survey assessing perceived workload and EHR satisfaction. Attending physicians had significantly higher levels of frustration with the EHR compared with residents, whereas information overload was more significant in residents.28 Another study investigated how EHR use differs based on gender. Although performance was equal, women were more efficient and reported greater rates of satisfaction when compared with men.29
DISCUSSION
Patient safety is paramount in all aspects of medical care, and any efforts to improve it should be pursued. The EHRs’ effect on patient safety is complex. When implemented properly, it can reduce medication errors and provide a potentially safer alternative to paper-based methods.2,27 However, its use has caused information overload as an unintended consequence.4 Physicians are keenly aware of both its benefits and short comings, and are more likely to have positive perceptions of EHR with improved usability.30
In addition to the growing text within the written notes, information within the EHR has also expanded from radiology results, laboratory results, alerts, demographics, predictive analyses, and more. The massive amount of data required in each patient’s chart has become potentially obstructive to patient care and can hinder the physician-patient interaction. Efficiently extracting clinically relevant information from the EHR can be a difficult task for physicians.15,17,22,23 This increased cognitive load placed on physicians makes them more prone to clinical errors, which puts patient safety at risk.15 A worrisome implication of these results in light of the continuous growth of information is that, without any changes, the rate of medical errors will more than likely continue to worsen over time. Consolidating important information into one area could make a significant impact in combatting this seemingly constant growth of chart data. Consolidation would help ameliorate the ill effects of cognitive overload and improve physicians’ ability to analyze data.15–17
Information overload results in an increase in tedious clerical work, reduction in physician-patient time, and a hampering of physician efficiency.5 To minimize the effects of information overload, various solutions have been proposed. One such solution is a customizable EHR to ensure that important data are easier to find.15,16,22 Studies that tested this type of software showed significant reductions in error rates and improvements in efficiency. Pickering et al27 introduced a novel user interface called AWARE (Ambient Warning and Response Evaluation) for use in the intensive care unit. The program synthesizes all of the data on a patient to a more readable and concise format, thus allowing physicians to make significantly quicker and safer decisions on patient care.
However, customizability does not provide the same benefit for all physicians. For example, a physician’s level of training has implications on how best to customize an EHR. Attendings and residents have significant differences in what they find challenging with the EHR,27,28 and thus, their respective interactions with the EHR must be assessed when customizing the EHR to minimize information overload and improve patient safety. In addition, user composability requires proper training techniques with implementation to maximize its potential.23 In addition, the search feature has been shown to improve efficiency and might be worth emphasizing as a way to decrease cognitive burden.29
Changing the order of the clinical note may also improve usability.20,21 Placing salient information at the beginning of the note may allow physicians to spend less time searching through extraneous information and thus reduce the cognitive burden. However, notes are not only read but also written, and retraining physicians to alter the order of notes may lead to an increased burden in and of itself. Software may potentially be designed to reformat a written SOAP note into presentation as an APSO note, but this has not been developed or studied, to our knowledge. Thus, changing the traditional order of notes may require further research before implementation.
Alert fatigue can further contribute to information overload. Excessive alerting has been shown to alter decision making and cause physicians to deviate from best practice.24 Interventions aimed at reducing unnecessary alerting have been proven to decrease time spent with the EHR.25 Any addition of alerts in EHR’s must be taken with great caution because of the increased risk of information overload, and efforts must constantly be made to minimize their usage.
To mitigate these unintended consequences of EHR use, efforts should be taken to make a more user-friendly design. Other industries have more usable interfaces, and the healthcare field should make a concerted effort to close this gap.31 The authors of this article along with other authors cited in this review want to advocate for a best-practice guideline made up of EHR vendors and stakeholders—importantly including physicians.26 An example of such guidelines is the SAFER Guides. This set of recommended practice guidelines aims to ensure the safety and safe use of EHRs.32 We feel that, even with the suggestion that “the EHR interface is monitored for safe use and user satisfaction is improved over time,” the SAFER guidelines are too general and ultimately fall short of genuinely addressing the challenges secondary to information overload. More must be done.
The Office of National Coordinator for Health Information released a report in February of 2020 discussing many of the points illuminated in this literature review. Despite acknowledging many of the issues facing physicians, the only actionable item of the entire report was revising one element of reimbursement—the Evaluation and Management (E/M) coding compensation by the CMS starting in January 2021.33 Although this is a step in the right direction, significantly more needs to be done. An example of a solution would be a federal commission from the Office of National Coordinator for Health Information comprised of the various stakeholders in the EHR industry—especially currently practicing physicians. This commission should be tasked with working on setting standards for EHR usability, which would be a step in the right direction. In addition, we believe that the federal government, especially the CMS, has a responsibility to ensure that actionable change takes place and goes further than words in a report. Implementation of an outcome-based reimbursement system would be a helpful. The current fee for service system promotes note bloat because reimbursement is often related to how many clinically inconsequential details are included in documentation. Instead, a payment model related to patient outcomes, not superfluous details, could be a solution to the problem of information overload leading to patient safety compromise.
Limitations of this study are inherent because of its review design. These include but are not limited to author bias, current gaps in the literature, and inadvertent omission of pertinent research.
CONCLUSIONS
This review of the literature demonstrates that EHR information overload can negatively impact patient safety. Customizable EHR, shortened clinical notes, reduced alerting, and an emphasis on end-user product usability may be helpful interventions to minimize cognitive load and ultimately improve patient safety. Further research to understand the impact of information overload on patient safety is necessary to more effectively develop improved EHR, with a focus on improving patient safety and reducing the burden on physicians. Finally, federal agencies such as the CMS must do more to promote improved usability by decreasing the amount of superfluous information in the EHR, all to improve patient safety.
Footnotes
There were no sources of support for this project.
The authors disclose no conflict of interest.
Contributor Information
Sohn Nijor, Email: sohnnijor@gmail.com.
Gavin Rallis, Email: tuj36183@temple.edu.
Nimit Lad, Email: nimit.lad@tuhs.temple.edu.
Eric Gokcen, Email: eric.gokcen@tuhs.temple.edu.
REFERENCES
- 1.Zelmer J Ronchi E Hyppönen H, et al. International health IT benchmarking: learning from cross-country comparisons. J Am Med Inform Assoc. 2017;24:371–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United States, Congress, House, Committee on Oversight and Government Reform . The American Recovery and Reinvestment Act of 2009: 111 AD. 111th Congress, 5th Session, Bill Title XIII.
- 3.Adler-Milstein J, Everson J, Lee SD. EHR adoption and hospital performance: time-related effects. Health Serv Res. 2015;50:1751–1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Middleton B Bloomrosen M Dente MA, et al. Enhancing patient safety and quality of care by improving the usability of electronic health record systems: recommendations from AMIA. J Am Med Inform Assoc. 2013;20:e2–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sinsky C Colligan L Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165:753. [DOI] [PubMed] [Google Scholar]
- 6.March CA Steiger D Scholl G, et al. Use of simulation to assess electronic health record safety in the intensive care unit: a pilot study. BMJ Open. 2013;3:e002549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zulman DM, Shah NH, Verghese A. Evolutionary pressures on the electronic health record: caring for complexity. JAMA. 2016;316:923–924. [DOI] [PubMed] [Google Scholar]
- 8.Arndt BG Beasley JW Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15:419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sittig DF Wright A Ash J, et al. New unintended adverse consequences of electronic health records. Yearb Med Inform. 2016;1:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koopman RJ Steege LMB Moore JL, et al. Physician information needs and electronic health records (EHRs): time to reengineer the clinic note. J Am Board Fam Med. 2015;28:316–323. [DOI] [PubMed] [Google Scholar]
- 11.Howe JL Adams KT Hettinger AZ, et al. Electronic health record usability issues and potential contribution to patient harm. JAMA. 2018;319:1276–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vainiomäki S Aalto AM Lääveri T, et al. Better usability and technical stability could lead to better work-related well-being among physicians. Appl Clin Inform. 2017;8:1057–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beasley JW Wetterneck TB Temte J, et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Med. 2011;24:745–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh H Spitzmueller C Petersen NJ, et al. Information overload and missed test results in electronic health record–based settings. JAMA Intern Med. 2013;173:702–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright MC Dunbar S Macpherson BC, et al. Toward designing information display to support critical care. A qualitative contextual evaluation and visioning effort. Appl Clin Inform. 2016;7:912–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmed A Chandra S Herasevich V, et al. The effect of two different electronic health record user interfaces on intensive care provider task load, errors of cognition, and performance. Crit Care Med. 2011;39:1626–1634. [DOI] [PubMed] [Google Scholar]
- 17.Al Ghalayini M, Antoun J, Moacdieh NM. Too much or too little? Investigating the usability of high and low data displays of the same electronic medical record. Health Informatics J. 2020;26:88–103. [DOI] [PubMed] [Google Scholar]
- 18.Berg GM, Shupsky T, Morales K. Resident Indentified violations of usability heuristic principles in local electronic health records. Kans J Med. 2020;13:84–89. [PMC free article] [PubMed] [Google Scholar]
- 19.Clarke MA Steege LM Moore JL, et al. Determining primary care physician information needs to inform ambulatory visit note display. Appl Clin Inform. 2014;5:169–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Belden JL Koopman RJ Patil SJ, et al. Dynamic electronic health record note prototype: seeing more by showing less. J Am Board Fam Med. 2017;30:691–700. [DOI] [PubMed] [Google Scholar]
- 21.Kahn D Stewart E Duncan M, et al. A prescription for note bloat: an effective progress note template. J Hosp Med. 2018;13:378–382. [DOI] [PubMed] [Google Scholar]
- 22.Senathirajah Y, Kaufman D, Bakken S. User-composable electronic health record improves efficiency of clinician data viewing for patient case appraisal: a mixed-methods study. EGEMS (Wash DC). 2016;4:1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ratwani RM Savage E Will A, et al. A usability and safety analysis of electronic health records: a multi-center study. J Am Med Inform Assoc. 2018;25:1197–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ancker JS Edwards A Nosal S, et al. Effects of workload, work complexity, and repeated alerts on alert fatigue in a clinical decision support system. BMC Med Inform Decis Mak. 2017;17:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah T Patel-Teague S Kroupa L, et al. Impact of a national QI programme on reducing electronic health record notifications to clinicians. BMJ Qual Saf. 2019;28:10–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murphy DR Giardina TD Satterly T, et al. An exploration of barriers, facilitators, and suggestions for improving electronic health record inbox-related usability: a qualitative analysis. JAMA Netw Open. 2019;2:e1912638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pickering BW Herasevich V Ahmed A, et al. Novel representation of clinical information in the ICU: developing user interfaces which reduce information overload. Appl Clin Inform. 2010;1:116–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khairat S Burke G Archambault H, et al. Perceived burden of EHRs on physicians at different stages of their career. Appl Clin Inform. 2018;9:336–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khairat S Coleman C Ottmar P, et al. Physicians’ gender and their use of electronic health records: findings from a mixed-methods usability study. J Am Med Inform Assoc. 2019;26:1505–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Melnick ER Sinsky CA Dyrbye LN, et al. Association of perceived electronic health record usability with patient interactions and work-life integration among US physicians. JAMA Netw Open. 2020;3:e207374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Melnick ER Dyrbye LN Sinsky CA, et al. The association between perceived electronic health record usability and professional burnout among US physicians. Mayo Clin Proc. 2020;95:476–487. [DOI] [PubMed] [Google Scholar]
- 32.SAFER Guides. Washington, DC: Office of National Coordinator for Health Information; 2017. [Google Scholar]
- 33.ONC . Strategy on Reducing Regulatory and Administrative Burden Relating to the Use of Health IT and EHRs. 2020. HealthIT.gov Available at: https://www.healthit.gov/sites/default/files/page/2020-02/BurdenReport_0.pdf. Accessed August 21, 2021.


