Abstract
The number of mental health problems in children and adolescents has been increasing. One of the causes of mental health problems is trauma in the family, such as childhood adversities. The aim of this study was to review the relationship between childhood adversities and mental health problems. The method in this study was a systematic review using three databases: CINAHL, PubMed, and SCOPUS. The results of the review were reported according to the PRISMA guidelines. The keywords used in this study were mental health or mental illness or mental disorder or psychiatric illness AND adolescents or teenagers or teenagers or youth AND parental divorce or parental separation OR parental death or parental loss or parentally bereaved. The inclusion criteria for the articles were English language and published from 2017 to 2021. This study recorded 477 articles, screened according to the topic, and then the final articles were 35. The results of the systematic review showed evidence that childhood adversities were related to mental health problems according to the ICD-10 diagnosis, ADHD and personality disorders, depression, post-traumatic, smoking behavior, and alcohol abuse, and distress. Interventions for children with childhood adversities were needed to prevent mental health disorders.
Keywords: Adolescents, child, mental health
Introduction
The number of mental health problems has been increasing, especially among children and adolescents.1–3 Stressors of life, as well as trauma, can cause mental health problems. 4 The first onset of mental health problems usually happens before the age of 18 years 5 and the most common mental health problems are depression and anxiety. This mental health problem also can trigger suicidal attempts. 4
More than 30,000 children were adopted by individuals who are not their family members. Furthermore, several surveys indicated that they did not live with their families or parents.6–8 These conditions are life-threatening for children as well as parents. 9 Children feel loss of support, loss of affection, decrease in cognitive stimulation, also social interaction is disrupted. 10 Parents with these conditions also tend to be frustrated and uncontrolled, so the role of parents cannot be maximized. 11 Further, it also leads to childhood adversities (CA).
Data from WHO stated that more than 38% of adults in 21 countries have experienced CA. 12 The definition of CA is still being debated, but several studies define it as abuse and neglect that occurs during childhood and adolescence. 12 CA also can be defined as parental divorce, parental death, parental substance abuse, parental hospitalization, parental criminality, residential instability, household living on public assistance, or parental migration. 13
Several studies regarding the relationship between childhood adversities and mental health have been published and well-documented.10,14–16 There was one study related to the meta-analysis about the effect of parental divorce on mental health among children. 17 So, the aim of this study was to conduct a systematic review of the relationship between childhood adversities and mental health problems.
Research methods
This procedure of systematic review was registered in PROSPERO number CRD42021277448 to avoid duplicates and bias.
Literature search strategy
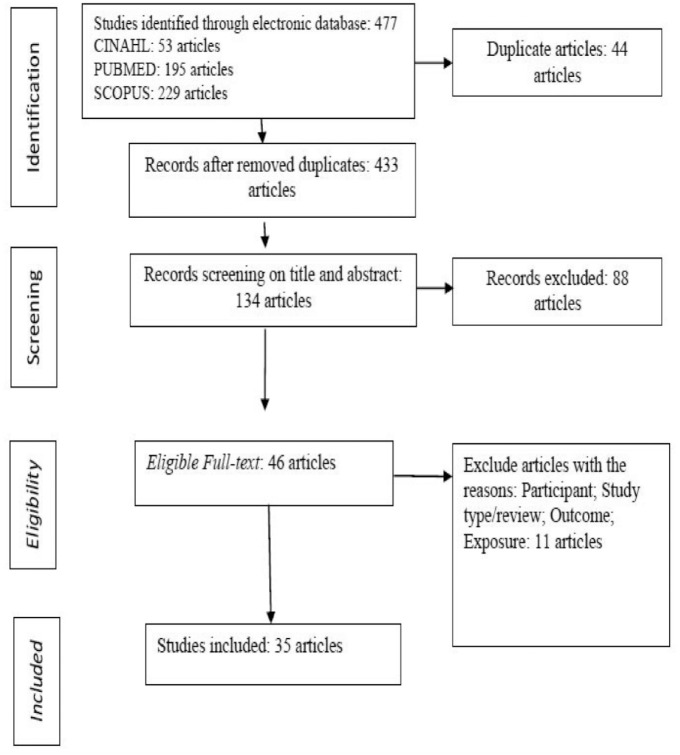
We performed a systematic review to search original studies from three databases, CINAHL, PubMed, and SCOPUS. This study followed the previous study for guiding the systematic review.17,18 We reported the systematic reviews according to the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) guideline. 19 The keywords were used in this study were mental health or mental illness or mental disorder or psychiatric illness) AND (adolescents or teenagers or teen or youth) AND (parental divorce or parental separation) OR (parental death or parental loss or parentally bereaved) for CINAHL. We used the combination TITLE-ABS-KEY (mental AND health) OR TITLE-ABS-KEY (mental AND illness) OR TITLE-ABS-KEY (mental AND disorder) OR TITLE-ABS-KEY (psychiatric AND illness) AND TITLE- ABS-KEY (adolescents) OR TITLE-ABS-KEY (teenagers) AND TITLE-ABS-KEY (parental AND divorce) OR TITLE-ABS-KEY (parental AND separation) OR TITLE-ABS-KEY (parental AND death) OR TITLE -ABS-KEY (parental AND loss)) for SCOPUS. Furthermore, we used the combination (((((((((mental health[MeSH Terms]))) OR (mental illness[MeSH Terms]))) OR (mental disorder[MeSH Terms])) OR (psychiatric illness[MeSH Terms] )) AND (adolescents[MeSH Terms])) OR (teenagers[MeSH Terms])) AND (Parental divorce[MeSH Terms])) OR (Parental separation[MeSH Terms]))) OR (Parental: Abstract, Full text, English, Adolescent: 13–18 years, from 2017 to 2021) for PubMed. The articles were restricted from 2017 to 2021 and only English language. We recorded 477 articles (Figure 1).
Figure 1.
Flowchart of study selection.
Inclusion criteria
We performed a systematic review that focused on the relationship between childhood adversities, such as parental divorce, parental death, parental substance abuse, parental hospitalization, parental criminality, residential instability, household living on public assistance, and parental migration (left behind children). 10 The outcome was mental health based on the WHO ICD 10 classification of Mental and Behavioral Disorders, depression, anxiety disorder, stress, suicide, and behavioral disorder due to alcohol, drugs, and smoking. However, it does not limit it to other mental health disorders. 17
Results
Figure 1 describes the article selection procedure. In this study, we recorded 477 articles. Then we removed duplicate articles. Two independent authors screened on titles and abstracts, and 46 eligible articles were obtained. Also, we excluded articles that did not correspond to our interests. So, in total, we had 35 articles in this study.
This review showed that 35 articles focused on mental health problems based on the WHO ICD 10 classification of Mental and Behavioral Disorders: mental health disorders (9 articles), ADHD and personality disorders (2 articles), depression (7 articles), post-traumatic (1 article), substance abuse (4 articles), and stress (1 article), and most of the articles were predominantly concerned with suicide (11 articles). In terms of exposure, all of the articles focused on childhood adversities; one or more types of childhood adversities (30 articles), household dysfunction (1 article), parent hospitalized (1 article), adoptive parents (1 article), and left behind children (LBC) (1 article) (Table 1).
Table 1.
Characteristic of samples included in the systematic review.
| Variable | Category | Number of samples |
|---|---|---|
| Location | Europe | |
| Denmark | 4 | |
| Finland | 1 | |
| Sweden | 6 | |
| Norway | 2 | |
| England | 2 | |
| Bosnia | 2 | |
| Australia | 2 | |
| Asia | ||
| Turkey | 1 | |
| Taiwan | 2 | |
| India | 1 | |
| Korea | 2 | |
| China | 4 | |
| Japan | 1 | |
| Lebanon | 1 | |
| Saudi Arabia | 1 | |
| USA | 3 | |
| Total | 35 | |
| Study design | Prospective | 21 |
| Cross-Sectional and case control study | 12 | |
| Qualitative | 2 | |
| Total | 35 | |
| Gender | Male | 0 |
| Female | 1 | |
| Both male and female | 34 | |
| Total | 35 | |
| Type of mental health problems | Mental health problems and mental health disorders | 9 |
| Suicide | 11 | |
| ADHD and personality disorder | 2 | |
| Depression | 7 | |
| Post traumatic | 1 | |
| Substances abuse | 4 | |
| Stress | 1 | |
| Total | 35 | |
| Type of childhood adversities | Household dysfunction | 1 |
| Parent hospitalized | 1 | |
| Stepfamily | 1 | |
| Childhood adversities (one or more childhood adversities) | 30 | |
| Left behind children (LBC) | 2 | |
| Total | 35 | |
| Age | Childhood (0–10 years) | 1 |
| Adolescence (11–19 years) | 9 | |
| Childhood, adolescence, and young adult | 20 | |
| Not known | 5 | |
| Total | 35 |
The articles were predominantly from the European continent, Denmark, Finland, Norway, England, and Bosnia (17 articles). Studies from Asia (Turkey, Taiwan, India, Korea, China, Saudi Arabia, Japan, and Lebanon) were 13 articles, from the USA three articles and Australia two articles (Table 1).
In terms of study design, most of the articles were predominantly prospective studies (21 articles). The age of the respondents varied from children to adults; however, the studies were limited by the time of childhood adversities as children or adolescents (Table 1).
Mental health problems, post-traumatic growth (PTG), and stress
Table 2 shows that mental health problems were the outcome of exposures such as household dysfunction, parental divorce, parent jobless for more than 9 months, parents who were in prison, parents who were hospitalized at the psychiatric hospitals, children who live in orphanages, parent died, parents who were undergoing treatment, adoptive parents, and parental abuse. Mental health problems were determined using a self-report questionnaire or mental health based on the WHO ICD 10 classification (ICD-10 code: F00-F99). In addition, the review showed that PTG was the outcome of children who lost their parents due to cancer. PTG was measured using a self-report questionnaire (Japanese version of PTGI). Distress is also the outcome of parental divorce among children.
Table 2.
Study characteristics of mental health problems.
| Author | Year | Study design | Country | Total sample | Age | Outcome | Childhood adversities | Focus of study | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Andersen 20 | 2020 | Cohort study | Denmark | 605,344 | From birth to 17 years old |
Mental health problems
Diagnosed with a mental disorder (ICD-10 code: F00- F99) at a mental health facility at age 18 or 19. |
Household dysfunction 1. Parental divorce 2. Prolonged unemployment 3. Incarceration of father 4. Inpatient treatment of parent for mental illness 5. Foster care placement of the child 6. Parental death |
Household dysfunctions were associated with an increased risk of adverse outcome |
| 2 | Marcussen et al. 21 | January 2017–June 2018 | Qualitative study | Denmark | 27 | Participants were children and young adults from divorced families or double bereavement at the age between 7 and 15 years old | Mental health problem: stress overload and decreased wellbeing | Parental divorce and parental cancer | Children and young adults’ double bereavement related to stress overload and mental health problems |
| 3 | Merikukka et al. 22 | Data from Finnish Birth Cohort | Cohort | Finland | 59,476 | 9–24 years old | Mental disorder | Parental psychiatric illness | Parental psychiatric illness is a risk for mental health children |
| 4 | Perales et al. 23 | May 2013–April 2014 | Cohort | Australia | 6310 | 4–11 years old 12–17 years old |
Mental disorder
1. Anxiety 2. Major depressive disorder 3. ADHD 4. Conduct disorder 5. Any disorder |
1. Original family 2. Stepfamily 3. Blended family 4. Other families |
Children who live with one parent, are blended, and step experience mental disorders compared to children who live in their original family. |
| 5 | Turner et al. 24 | - | Cross-sectional | Australia | 1825 | 18–34 35–65 years |
The Diagnostic Interview for Psychosis (DIP) Depressive symptoms, mania, self-reproach, delusion, hallucination, and subjective thought disorder |
Adverse event: sexual abuse, physical abuse, emotional abuse and, neglect. Interpersonal loss (loss of a parent, sibling, divorce) | All adverse event types were associated with anxiety, depression, and a definite psychosocial stressor |
| 6 | Hadžikapetanović et al. 25 | Mai–June 2011 | Case-control study | Bosnia | 168 | High School Students and University students | Beck Depression Inventory -II | Divorced parents | Adolescents from divorced families had a significantly higher levels of depression |
| 7 | Houtepen et al. 26 | Data from the Avon Longitudinal Study of parents and children | Cohort study | UK | 4917 | Children born in 1991–1992 | Depression, regular smoking, harmful drinking, illicitly use of drugs |
Adverse childhood experiences (ACE) (sexual, physical, or emotional abuse; emotional neglect; parental substance abuse; parental mental illness or suicide attempt; violence between parents; parental separation; bullying; and parental criminal conviction, with data collected on multiple occasions between birth and age 16) |
Adverse childhood experiences were associated with depression, drug use, and smoking |
| 8 | Lee et al. 10 | 2003–2007 | Cohort | Taiwan | 10,416 | 15–19 age years old | Depressive symptoms, suicidal ideation, and substance abuse | Childhood adversities: Physical abuse, parental problematic drinking, parental divorce, parental death, parental catastrophic health problems, family economic hardship | Physical abuse among children, family economic hardship had affected on depressive and suicidal ideation. Chronic parental problematic drinking had the highest levels of substance abuse |
| 9 | Shaikh et al. 27 | November 2017–December 2017 | Cross-sectional | Saudi Arabia | 296 female | 12–16 age years old | Depression, anxiety, and stress | Marital discord | Marital discord related to poor psychosocial health in the child |
| 10 | Hirooka et al. 28 | January 2014 | Cross-sectional | Japan | 57 adolescents | 15–23 age years old | Post traumatic growth | Parental bereavement (parental death) | Parental bereavement was associated with PTG |
| 11 | Johnsen et al. 29 | January–February 2017 | Qualitative | Norwegian | 12 children | 10–13 years old And living in two homes due to parental divorce |
Distress | Parental divorce | Parents separation and living in two homes can be stressful for children |
Suicide and self-harm
Table 3 shows that suicide, including suicidal ideations and suicidal attempts, were outcomes of childhood adversities (parental divorce, parental abuse, childhood experience of parental death (CEPD), and parental suicide). Suicide was diagnosed according to ICD 10 as well as a self-report questionnaire to report suicidal ideation such as the KOWEPS questionnaire.
Table 3.
Study characteristics of suicide and self-harm.
| Author | Year | Study design | Country | Total sample | Age | Outcome | Childhood adversities | Focus of study | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Björkenstam et al. 30 | December 2011–June 2012 | Cohort study | Sweden | 548,721 | Individual born between 1987 and 1991 and childhood adversities before 15 age years old | Suicide | Childhood adversities before 15 age years old Parental death 1. Parental substance abuse 2. Parental crime 3. Parental psychiatric disorder 4. Parental separation 5. Receipt Public assistance 6. Residential instability |
Childhood adversities are a risk factor for suicide |
| 2 | Carr et al. 31 | Danish Data Protection Agency | Cohort study | Denmark | 1,698,821 | Adolescents with parental death before 15 age years old | Self-harm | Parental death during childhood | Self-harm was increased following parental death during childhood |
| 3 | Guvendeger Doksat et al. 32 | January 2011–December 2013 | Longitudinal | Turkey | 2518 | Children and adolescents | History of suicide attempts (HAS) | Parental separation/divorce, parental mental disorder, alcohol, and drug use, and crime | Parental separation/divorce, parental mental disorder, alcohol, and drug use, and crime were the risk of HSA |
| 4 | Lee et al. 33 | - | Retrospective Cohort Design | Taiwan | 40,249 Comparison (N = 398,081) |
Individual born 1978–1997 0–31 age years old |
Suicide | Parental suicide | Individuals with parental suicide more likely to die by suicide |
| 5 | Mathew et al. 34 | 2014 | Qualitative | India | 22 | Adolescents: 7 Young adult: 15 |
Suicide attempts | Parental conflicts and separation, conflict with a sibling, and marital disharmony | Hostile family environment contributed to suicidal behavior among adolescents and young adult |
| 6 | Park and Park 35 | 2017–2018 | Longitudinal study | Korea | 118,715 | Middle and high school students | Suicidal behavior | Remarriage and loss of parents | Suicidal behavior was related to the remarriage and loss of parents among adolescents |
| 7 | Spremo 36 | 2020 | Cross-sectional | Bosnia | 590 | 14–18 age years old | Suicidal ideas | Incomplete families (divorce) | Children with incomplete families were thinking about suicidal |
| 8 | Stansfeld et al. 37 | 2008 | Cohort Study | UK | 9377 female | 7, 11, and 16 | Suicidal attempts | Childhood adversity | Childhood adversity was a predictor of suicidal attempts among adolescents |
| 9 | Thompson et al. 38 | 2001–2002 | Cohort study | USA | 1073 | More than 18 years old | Suicidal attempts | Parental divorce and maternal paternal alcohol problems | The individual who experience a parental divorce as children or adolescents and who have parental alcohol abuse are more likely for suicidal attempts |
| 10 | Wang et al. 39 | 2016 | Cross-sectional | China | 6284 | 15–25 | Suicidal ideation in the past 12 months | Parental separation | Family factors had the most influence on suicidal ideation |
| 11 | Yoon et al. 40 | - | Longitudinal | Korea | 8609 | >19 years old | Suicidal ideation | Childhood experience of parental death (CEPD) | CEPD was related to suicidal ideation |
ADHD and personality disorders
Table 4 showed that childhood adversities were strongly related to ADHD and personality disorders.
Table 4.
Study characteristics for ADHD and personality disorder.
| Author | Year | Study design | Country | Total sample | Age | Outcome | Childhood adversities | Focus of study | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Björkenstam et al. 41 | Medical birth register | Cohort | Sweden | 543,650 | Individuals born 1987–1991 | ADHD | CA: 1. Family death 2. Substantial parental substance abuse 3. Substantial parental psychiatric disorder 4. Substantial parental criminality 5. Parental separation 6. Household living on public assistance 7. Residential instability |
CA was a risk factor for ADHD |
| 2 | Björkenstam et al. 42 | - | Cohort study | Sweden | 116,087 | CA was measured between birth and age 14 | Personality disorder | Childhood adversities (CA) | Childhood adversities (CA) were strongly associated with PD (personality disorder) |
Depression
Table 5 showed that depression was an outcome of exposure to childhood adversities, parental divorce, parents who were hospitalized, parents who were in prison, parental death, parental disabilities, and mental disorders, broken families, leaving orphanages, and childhood abuse. Also, children with LBC (left behind children), because their parents have to go to work for more than 6 months. Depression was determined using self-report questionnaires such as the Beck Depression Inventory 2, Childhood Depression Inventory as well as medical diagnoses (DSM IV, ICD 10).
Table 5.
Study characteristics for depression.
| Author | Year | Study design | Country | Total sample | Age | Outcome | Childhood adversities | Focus of study | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Björkenstam et al. 43 | - | Cohort study | Sweden | 478,141 | Individuals born in 1984–1988 Before 23 years old |
Depression | Childhood adversities (CA) | CA predicted depression |
| 2 | Bohman et al. 18 | - | Case-control study | Sweden | 382 | Adolescent | Major depression disorder (MDD) in adulthood | Separated parents | Parental separation was associated with an increase in depression |
| 3 | Dahl et al. 44 | - | Prospective, cohort study | Denmark | 978,647 | All individuals born between 1980 and 1988, before 18 years old | Depression | Exposure Adversity included parental illness, incarceration, death, disability, and psychiatric diagnosis, family disruption, out of home, and childhood abuse | All adversities were significantly associated with increased risk for moderate to severe depression |
| 4 | Guang et al. 45 | December 2012–June 2013 | Cross-sectional design | China | 6227 | 7–17 years old | Depression | Left behind children: parents migrating to work in cities | LBC is more stressed and depressed compared to NLBC |
| 5 | Kravdal and Grundy 46 | 2004 | Case-control | Norway | 1,125,257 | 20–44 age years old | Depression | Experiencing Parental divorce aged 0–20 age years old | Children who were aged 15–19 when their parents divorced were less likely to purchase antidepressants |
| 6 | Pham et al. 47 | - | Case-control study | USA | 216 youths who lost a parent 172 youths non-parental death |
7–18 age years old | Depression, post-traumatic stress disorder (PTSD) and functional impairment | Parental death | Youth with parental death showed higher depression |
| 7 | Sun et al. 48 | - | Longitudinal study | China | 1620 students of elementary school | 8–15 | Depression | LBC more than 6 months | LBC was a predictor of depression |
Substance abuse
Substance abuse in this review was alcohol abuse, smoking and drugs abuse (table 6). Children with a history of parental divorce, parental divorce plus alcoholics, and children with parental divorce living with adoptive parents were predictors of substance abuse.
Table 6.
Study characteristics for tobacco smoking and alcohol abuse.
| Author | Year | Study design | Country | Total sample | Age | Outcome | Childhood adversities | Focus of study | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Lindström and Rosvall 49 | 2012 | Cross-sectional | Sweden | 28,029 | 18–80 | Tobacco smoking | Parental divorce | Parental divorce was related to tobacco smoking among children |
| 2 | Jabbour et al. 50 | January and May 2019 | Cross-sectional | Lebanon | 1810 | Mean Age: 15.42 years old | Alcohol abuse, higher cigarette, higher water pipe | Parental divorce | Parental divorce is correlated to higher alcohol and smoking |
| 3 | Waldron et al. 51 | - | Longitudinal Study | USA | 3539 | African America Twin: 17.22 European American Twins: 3539 |
Problem drinking | Parental separation, mothers who have a history of problem drinking | Parental divorce as moderator risk to children of mothers with a history of problem drinking |
| 4 | Watkins and Ohannessian 52 | 2016 | Longitudinal study | USA | 863 | 11–15 age years old | VAPE | Parental marital status (parental divorce) | Adolescents with parental divorce more likely to use VAPE |
Discussion
This systematic review study provided evidence of the relationship between childhood adversities and mental health problems. The results showed that childhood adversities were significantly related to mental health problems. The original studies in this systematic review were published from 2017 to 2021.
There are several pathways that explain the relationship between childhood adversities and mental health problems. Childhood adversities such as family dysfunction usually occur in families with low socioeconomic status, and have effects on the psychological development of children. 20 This situation also leads to stress among children 21 as well as depression.25,43,44,46,47 In addition, parental conflict or parental divorce causes children to lose love and caring. Several studies also indicated that childhood adversities were associated with changes in the brain, specifically decreased hippocampal volume and impaired HPA axis. 53
Childhood adversities that contributed to mental health problems in this study were: family dysfunction (household dysfunction, parental divorce, jobless parents for more than 9 months, parental criminality, parental hospitalization at psychiatric hospital, children living in orphanages, parent died, parents who were undergoing treatment, adoptive parents, and parental abuse. These childhood adversities had a strong relationship with mental health problems such as stress overload and decreased wellbeing, mental disorders such as anxiety, major depressive disorder, ADHD, personality disorders, mania, delusions, and hallucinations.20–24 Based on these results, programs and interventions for children and adolescents, are needed especially to develop resilience and coping to deal with trauma in the family.
Another type of mental health problem related to childhood adversities was suicidal ideation and suicidal attempt.30–40 Children with a parental history of suicide had more risk of suicide as well; this idea was caused by disruption of self-regulation. In addition, they were more likely to be depressed and tended to conduct self-injury. 30 Meanwhile, children with parental died and parental divorce also felt loneliness and sadness. These feelings also can lead to suicidal ideation. 36
Childhood adversities were also associated with mental health problems: personality disorder 42 and ADHD. 41 Personality disorder was caused by the disruption of educational performance. The process of children’s education was disrupted due to problematic families, 20 while ADHD was caused by parents with alcohol abuse. Pregnant women who are alcoholics can affect the fetus. 41 Childhood adversities were also associated with children’s smoking behavior and alcohol abuse. This situation was caused by a lack of parental control over children’s behavior, especially children who lived with only one parent due to divorce or living with adoptive parents.
Limitation of the study
Some limitations in this study need to be considered and used as suggestions for further research. This study conducted a systematic review and has not yet measured the quantitative effect of the impact of family dysfunction, including childhood adversities on mental health. So a meta-analysis study is needed for further research.
Conclusion
Childhood adversities such as household dysfunction, parental hospitalization, adoptive parents, and left behind children (LBC) were closely related to mental health problems according to the ICD-10 mental health disorders, ADHD and personality disorders, depression, post traumatic and stress, substance abuse, and suicide. Interventions for children with childhood adversities are needed to prevent mental health disorders among them.
Acknowledgments
We would like to thank LPDP for their support of this study.
Footnotes
Author contributions: The authors contributed equally.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: the work was supported by LPDP Indonesia.
Ethics approval: We did not apply ethics because we conducted a systematic review. However, the protocol of this study was registered at Prospero number CRD42021277448.
Significance for public health: A childhood adversity (CA) is a public health issue with broad implications for mental health. Data from WHO stated that more than 38% of adults in 21 countries have experienced CA. These conditions are life-threatening. So, therefore, the aim of this study was to conduct a systematic review of the relationship between childhood adversities and mental health problems. Childhood adversities such as household dysfunction, parental hospitalization, adoptive parents, and left-behind children (LBC) were closely related to mental health problems according to the ICD-10 mental health disorders, ADHD and personality disorders, depression, post traumatic ad stress, substance abuse, and suicide. Interventions for children with childhood adversities are needed to prevent mental health disorders among them.
References
- 1. Olfson M, Blanco C, Wang S, et al. National trends in the mental health care of children, adolescents, and adults by office-based physicians. JAMA Psychiatry 2014; 71(1): 81–90. [DOI] [PubMed] [Google Scholar]
- 2. Kessler RC, Amminger GP, Aguilar-Gaxiola S, et al. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 2007; 20(4): 359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Olfson M, Druss BG, Marcus SC. Trends in mental health care among children and adolescents. N Engl J Med 2015; 372(21): 2029–2038. [DOI] [PubMed] [Google Scholar]
- 4. Michaud P-A, Fombonne E. Common mental health problems. BMJ 2005; 330(7495): 835–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Andrews G, Hall W, Teesson M, et al. The mental health of Australians: national survey of mental health and wellbeing. Canberra: Mental Health Branch, Commonwealth Department of Health and Aged Care, 1999. Vol. 2, pp.29–30. [Google Scholar]
- 6. Bjarnason T, Bendtsen P, Arnarsson AM, et al. Life satisfaction among children in different family structures: A comparative study of 36 western societies. Child Soc 2012; 26(1): 51–62. [Google Scholar]
- 7. Låftman SB, Bergström M, Modin B, et al. Joint physical custody, turning to parents for emotional support, and subjective health: a study of adolescents in Stockholm, Sweden. Scand J Public Health 2014; 42(5): 456–462. [DOI] [PubMed] [Google Scholar]
- 8. Bergström M, Fransson E, Modin B, et al. Fifty moves a year: is there an association between joint physical custody and psychosomatic problems in children? J Epidemiol Community Health 2015; 69(8): 769–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McLaughlin KA, DeCross SN, Jovanovic T, et al. Mechanisms linking childhood adversity with psychopathology: learning as an intervention target. Behav Res Ther 2019; 118: 101–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lee M-C, Huang N, Chen C-Y. Effects of childhood adversity trajectories on mental health outcomes in late adolescence: the buffering role of parenting practices in Taiwan. Child Abuse Negl 2020; 109: 104705. [DOI] [PubMed] [Google Scholar]
- 11. Eisman AB, Stoddard SA, Heinze J, et al. Depressive symptoms, social support, and violence exposure among urban youth: A longitudinal study of resilience. Dev Psychol 2015; 51(9): 1307–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kessler RC, McLaughlin KA, Green JG, et al. Childhood adversities and adult psychopathology in the WHO world mental health surveys. Br J Psychiatry 2010; 197(5): 378–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am J Prev Med 1998; 14(4): 245–258. [DOI] [PubMed] [Google Scholar]
- 14. Scott KM, Von Korff M, Angermeyer MC, et al. Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Arch Gen Psychiatry 2011; 68(8): 838–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pirkola S, Isometsä E, Aro H, et al. Childhood adversities as risk factors for adult mental disorders: results from the Health 2000 study. Soc Psychiatry Psychiatr Epidemiol 2005; 40(10): 769–777. [DOI] [PubMed] [Google Scholar]
- 16. Pietrek C, Elbert T, Weierstall R, et al. Childhood adversities in relation to psychiatric disorders. Psychiatry Res 2013; 206(1): 103–110. [DOI] [PubMed] [Google Scholar]
- 17. Auersperg F, Vlasak T, Ponocny I, et al. Long-term effects of parental divorce on mental health - a meta-analysis. J Psychiatr Res 2019; 119: 107–115. [DOI] [PubMed] [Google Scholar]
- 18. Bohman H, Låftman SB, Päären A, et al. Parental separation in childhood as a risk factor for depression in adulthood: a community-based study of adolescents screened for depression and followed up after 15 years. BMC Psychiatry 2017; 17(1): 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. PRISMA. Welcome to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) website! http://www.prisma-statement.org/ (2021, accessed 26 July 2021).
- 20. Andersen SH. Association of youth age at exposure to household dysfunction with outcomes in early adulthood. JAMA Netw Open 2021; 4(1): e2032769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Marcussen J, Thuen F, O’Connor M, et al. Double bereavement, mental health consequences and support needs of children and young adults—when a divorced parent dies. J Clin Nurs 2020; 29(7–8): 1238–1253. [DOI] [PubMed] [Google Scholar]
- 22. Merikukka M, Räsänen S, Hakko H, et al. Association between parental hospital-treated somatic illnesses in childhood and later mental disorders among offspring up to early adulthood: an explorative study in the 1987 Finnish birth cohort. Scand J Public Health 2020; 48(2): 214–223. [DOI] [PubMed] [Google Scholar]
- 23. Perales F, Johnson SE, Baxter J, et al. Family structure and childhood mental disorders: new findings from Australia. Soc Psychiatry Psychiatr Epidemiol 2017; 52(4): 423–433. [DOI] [PubMed] [Google Scholar]
- 24. Turner S, Harvey C, Hayes L, et al. Childhood adversity and clinical and psychosocial outcomes in psychosis. Epidemiol Psychiatr Sci 2019; 29: e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hadžikapetanović H, Babić T, Bjelošević E. Depression and intimate relationships of adolescents from divorced families. Medicinski glasnik : official publication of the Medical Association of Zenica-Doboj Canton. Bosnia Herzegovina 2017; 14(1): 132–138. [DOI] [PubMed] [Google Scholar]
- 26. Houtepen LC, Heron J, Suderman MJ, et al. Associations of adverse childhood experiences with educational attainment and adolescent health and the role of family and socioeconomic factors: a prospective cohort study in the UK. PLoS Med 2020; 17(3): e1003031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shaikh Q, Aljasser DS, Albalawi AM. Parenting behaviors, marital discord and the mental health of young females: a cross-sectional study from Saudi Arabia. Ann Saudi Med 2020; 40(1): 49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hirooka K, Fukahori H, Akita Y, et al. Posttraumatic growth among Japanese parentally bereaved adolescents: a web-based survey. Am J Hosp Palliat Med 2017; 34(5): 442–448. [DOI] [PubMed] [Google Scholar]
- 29. Johnsen IO, Litland AS, Hallström IK. Living in two worlds - children’s experiences after their parents’ divorce - a qualitative study. J Pediatr Nurs 2018; 43: e44–e51. [DOI] [PubMed] [Google Scholar]
- 30. Björkenstam C, Kosidou K, Björkenstam E. Childhood adversity and risk of suicide: cohort study of 548 721 adolescents and young adults in Sweden. BMJ 2017; 357: j1334. [DOI] [PubMed] [Google Scholar]
- 31. Carr MJ, Mok PLH, Antonsen S, et al. Self-harm and violent criminality linked with parental death during childhood. Psychol Med 2020; 50(7): 1224–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Guvendeger Doksat N, Zahmacioglu O, Ciftci Demirci A, et al. Association of Suicide attempts and Non-Suicidal self-injury behaviors with substance use and family characteristics among children and adolescents seeking treatment for substance use disorder. Subst Use Misuse 2017; 52(5): 604–613. [DOI] [PubMed] [Google Scholar]
- 33. Lee KY, Li CY, Chang KC, et al. Age at exposure to parental suicide and the subsequent risk of suicide in young people. Crisis 2018; 39(1): 27–36. [DOI] [PubMed] [Google Scholar]
- 34. Mathew A, Saradamma R, Krishnapillai V, et al. Exploring the family factors associated with suicide attempts among adolescents and young adults: a qualitative study. Indian J Psychol Med 2021; 43(2): 113–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Park YS, Park EC. Association between parental marital status and types of suicidal behavior among Korean adolescents: a cross-sectional study. J Prev Med Public Health 2020; 53(6): 419–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Spremo M. Children and divorce. Psychiatr Danub 2020; 32(Suppl 3): 353–359. [PubMed] [Google Scholar]
- 37. Stansfeld SA, Clark C, Smuk M, et al. Childhood adversity and midlife suicidal ideation. Psychol Med 2017; 47(2): 327–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Thompson RG Jr, Alonzo D, Hu MC, et al. The influences of parental divorce and maternal-versus-paternal alcohol abuse on offspring lifetime suicide attempt. Drug Alcohol Rev 2017; 36(3): 408–414. [DOI] [PubMed] [Google Scholar]
- 39. Wang M, Kou C, Bai W, et al. Prevalence and correlates of suicidal ideation among college students: a mental health survey in Jilin Province, China. J Affect Disord 2019; 246: 166–173. [DOI] [PubMed] [Google Scholar]
- 40. Yoon J, Kim JY, Kim JH, et al. Role of SES on the association between childhood parental death and adulthood suicidal ideation: a mediation analysis using longitudinal dataset in South Korea. BMC Psychiatry 2021; 21(1): 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Björkenstam E, Björkenstam C, Jablonska B, et al. Cumulative exposure to childhood adversity, and treated attention deficit/hyperactivity disorder: a cohort study of 543 650 adolescents and young adults in Sweden. Psychol Med 2018; 48(3): 498–507. [DOI] [PubMed] [Google Scholar]
- 42. Björkenstam E, Ekselius L, Burström B, et al. Association between childhood adversity and a diagnosis of personality disorder in young adulthood: a cohort study of 107,287 individuals in Stockholm County. Eur J Epidemiol 2017; 32(8): 721–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Björkenstam E, Vinnerljung B, Hjern A. Impact of childhood adversities on depression in early adulthood: a longitudinal cohort study of 478,141 individuals in Sweden. J Affect Disord 2017; 223: 95–100. [DOI] [PubMed] [Google Scholar]
- 44. Dahl SK, Larsen JT, Petersen L, et al. Early adversity and risk for moderate to severe unipolar depressive disorder in adolescence and adulthood: a register-based study of 978,647 individuals. J Affect Disord 2017; 214: 122–129. [DOI] [PubMed] [Google Scholar]
- 45. Guang Y, Feng Z, Yang G, et al. Depressive symptoms and negative life events: what psycho-social factors protect or harm left-behind children in China? BMC Psychiatry 2017; 17(1):402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kravdal Ø, Grundy E. Children’s age at parental divorce and depression in early and mid-adulthood. Popul Stud 2019; 73(1): 37–56. [DOI] [PubMed] [Google Scholar]
- 47. Pham S, Porta G, Biernesser C, et al. The burden of bereavement: early-onset depression and impairment in youth bereaved by parental sudden death in a 7-year prospective study. Am J Psychiatr 2018; 175(9): 887–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sun X, Qin X, Zhang M, et al. Prediction of parental alienation on depression in left-behind children: a 12-month follow-up investigation. Epidemiol Psychiatr Sci 2021; 30: e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lindström M, Rosvall M. Parental separation/divorce in childhood and tobacco smoking in adulthood: a population-based study. Scand J Public Health 2020; 48(6): 657–666. [DOI] [PubMed] [Google Scholar]
- 50. Jabbour N, Abi Rached V, Haddad C, et al. Association between parental separation and addictions in adolescents: results of a National Lebanese study. BMC Public Health 2020; 20(1): 965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Waldron M, Watkins NK, Bucholz KK, et al. Interactive effects of maternal alcohol problems and parental separation on timing of daughter’s first drink. Alcohol Clin Exp Res 2018; 42(1): 120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Watkins NK, Ohannessian CM. Timing of vape use among adolescents: differences by family structure. Drug Alcohol Depend 2020; 209: 107953. [DOI] [PubMed] [Google Scholar]
- 53. Teicher MH, Tomoda A, Andersen SL. Neurobiological consequences of early stress and childhood maltreatment: are results from human and animal studies comparable? Ann N Y Acad Sci 2006; 1071(1): 313–323. [DOI] [PubMed] [Google Scholar]