Abstract
Prevalence of food allergy has been increasing over the last decades. It may appear as an immediate or a delayed reaction. The disease has a major impact on the quality of life of patients and their families, and it is associated to elevated costs. Primary care physicians are the first healthcare providers who assist children with food allergy, especially in mild to moderate forms. Through the present review, we examine the steps that should be followed in primary care to manage food allergy, and to promptly prescribe an elimination diet and an emergency kit in case of accidental exposure to the allergen. We also focus on the special management of IgE and non-IgE mediated cow’s milk allergy, and on management and prevention of egg and peanuts allergy. (www.actabiomedica.it)
Keywords: food allergy, primary care, milk allergy, egg allergy, peanut allergy
Introduction
Food allergy (FA) is a disease resulting from an immunological reaction towards food allergens, mainly protidic ones. It may appear as a type I IgE mediated immediate allergic reaction, following Gell and Coombs classification, or as a type IV delayed reaction (1). Primary care physicians are those who deal the most with patients suffering from possible allergic symptoms due to food allergy. It is therefore important to assure an appropriate evaluation even in this setting, to promptly start an elimination diet, and to target those patients who need a specialized consultation. In addition, food allergy is considered as a financial burden with a substantial impact on the quality of life of both patients and their family (2).
Over the last few years, the overall prevalence of food allergies has increased globally, and especially in westernized countries and in children (3). Indeed, according to the Canadian Pediatric Society, in 2020, food allergy affects an estimated 2% to 10% of the pediatric general population, with evidence of increasing prevalence over time; for such reason, the issue of preventing food allergies has become an important public health goal (4). Even though any food might possibly elicit an allergic reaction, the most common allergens in children are cow’s milk, hen’s egg, peanuts, tree nuts, fish, shellfish, wheat, and soy (5).
Through the present review, we aimed at clarifying in a simple way the best management of food allergy in primary care settings, with a special focus on the three most common allergens in pediatrics, which are cow’s milk, eggs, and peanuts.
General management of food allergy
The most recent evidence about preventing food allergy show a need to reduce social healthcare costs and improve the quality of life of allergic children and their families. To do so, primary care physicians play an essential role: an early diagnosis or prevention may indeed change the patient’s history and the social impact of the disease on healthcare costs. In 2014, the EAACI guidelines on food allergy prevention, concluded that introducing well-cooked egg into infant’s diet between 4 and 6 months probably reduces the risk of hen’s egg allergy, but also that further studies are needed to propose a firm conclusion on this topic (6).In 2016, a meta-analysis showed a statistically significant role of early introduction of eggs and peanuts, under a strict medical control, between 4-6 months of age, in preventing food allergy, in high risks infants (7,8). However, there is no agreement on the precise definition of “high risks infants”, even though published studies mainly focus on those with a personal history of atopy (especially eczema), or with an atopic first-degree relative (e.g. eczema, food allergy, allergic rhinitis, or asthma) (4).
In primary care, physicians may be able to assess if a child presented a reaction evocative of food challenge, and even perform some diagnostic tests, and then prescribe an elimination diet and an emergency kit, to provide the initial treatment before a specialized consultation.
Clinical History
The first step to diagnose food allergy in a child is to collect a detailed clinical history. This step is crucial since it allows to distinguish between IgE mediated and non-IgE mediated mechanisms (9). Whenever a patient suffers from food allergy, symptoms appear after each consumption. If a child reports the appearance of symptoms not systematically after exposure to a certain food, the diagnosis of IgE mediated food allergy may be ruled out, unless the reaction is elicited only in the presence of enhancing cofactors (10). Indeed, some cofactor may induce the appearance of allergic symptoms: these mainly include fever, menses, physical activity up to 4-6 hours after allergen exposure, therapy with non-steroidal anti-inflammatory drugs or with proton pump inhibitors. If this is the case, physicians should continue investigating the patient for a possible food allergy.
As a second step, whenever there is a clinical orientation for a possible food allergy, the next question that should arise is the delay between food consumption and symptoms appearance (figure 1). In case of IgE mediated allergy, symptoms appear usually within 15-20 minutes (but even up to 1 hour) after consumption. Main symptoms may affect (11):
the skin and the mucosa (mostly urticaria, oedema, pruritus, conjunctivitis, and rhinitis);
the gastrointestinal tract (mostly vomiting, abdominal pain, and diarrhea);
the respiratory tract (mainly laryngeal oedema, cough, wheezing, sneezing, and dyspnea);
the cardiovascular system (hypotension, tachycardia, and up to cardiac arrest).
Figure 1. Basic questions to rule out or suspect food allergy in primary care practice.
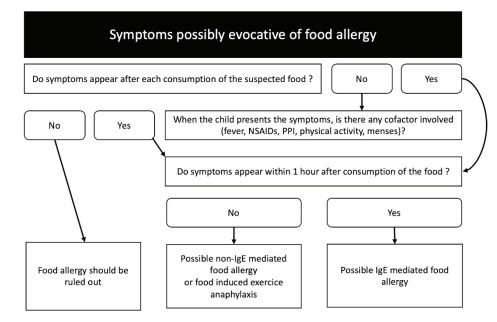
On the other hand, non-IgE mediated reactions appear usually more than 1 hour after the contact with the food allergen, therefore it may sometimes be challenging to highlight the association between food exposure and symptoms appearance. Non-IgE mediated mainly include food protein induced entero-colitis/proctocolitis syndrome, protein enteropathy, contact dermatitis, dermatitis herpetiformis, Heiner’s syndrome (11). These delayed forms of food allergy tend to self-resolution as the child grows. Two delayed forms of food allergy are nonetheless IgE mediated: these include exercise food-induced anaphylaxis and alpha-gal allergy. Nevertheless, these two conditions should be assessed in specialized settings. Mixed forms of food allergy mainly include atopic eczema/dermatitis, and eosinophilic disorders of the gastro-intestinaltract (11).
Diagnosis
The gold standard for IgE mediated food allergy is the oral food challenge. Prior to such test, physicians should perform skin prick tests and dose specific IgE levels. In trained physicians, these last two tests may be performed in clinical practice, even in primary care settings, while food challenges should only be performed in specialized centers.
Skin prick tests are usually performed on the patient’s forearm. Negative (saline 0.9%) and positive (histamine 10 mg/ml) controls are required, and the maximum wheal diameter is reported with an arbitrary positive cut-off diameter >3 mm recorded 15 minutes after the test is performed (10). When commercial extracts are not available, physicians may use the real food, which is currently the preferred method, with the prick-by-prick technique. Specific serum IgE directed towards an allergen might be considered as well if primary care physicians have the possibility to perform such test. On the other hand, performing component-resolved diagnosis (therefore dosing IgE directed against molecular allergenic proteins) should be limited to specialized doctors.
Skin prick tests and specific IgE show a reasonable sensitivity (70-100%), but a moderate specificity (4070%): for such reason, the oral food challenge remains today the gold standard for the ultimate diagnosis. Nevertheless, it should be pointed out that the best sensitivity and specificity are observed for allergens such as peanut, egg, milk, hazelnut, fish, and shrimp. Physicians should remember, when discussing the results of the tests with patients that the size of the prick wheal and the level of specific IgE don’t correlate with the possible severity of the reaction, in case of accidental exposure (12).
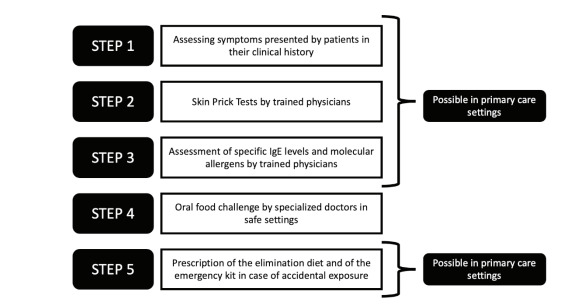
These tests should be performed if the symptoms presented by the patient seems to be associated with an IgE mediated reaction. In the absence of a previous reaction, a positive test simply correlates with a sen-sitization (presence of IgE), but not necessarily with a clinical allergy. Therefore, in these cases, a useless elimination diet may be prescribed, which is something that should be avoided. For such reason, these tests should always be performed after the first step, the assessment of the clinical history and of the possible link between allergen exposure and allergic symptoms appearance (figure 2).
Figure 2. Steps to be followed to diagnose and manage a food allergy, in primary care setting.
In case of non-IgE mediated, there are no clinical nor biological test allowing to diagnose a delayed food allergy. In these patients, an elimination diet should correlate with symptoms improvement. Atopy patch tests are not an appropriate test to diagnose these forms of food allergy (13), following current guidelines from the European Academy of Allergy and Clinical Immunology (10). The diagnosis is reached when symptoms reappear, by reintroducing the culprit food in the child’s diet after at least 4 weeks of elimination.
Treatment
Management of food allergy is mainly based on an elimination diet and on patients’ and caregivers’ education on avoiding food containing the allergen and treating an allergic reaction in case of accidental exposure (14). Patients and their families should carefully read product labels, on which main allergens are indicated. In addition, school staff should be advised about the child’s allergy and be able to treat a possible reaction occurring during school hours. Educational programs should be implemented, even in primary care, to verify that both patients and the families are capable of promptly recognizing possible symptoms of an allergic reaction and of adequately administering the rescue drugs contained in the emergency kit (mainly antihis-tamines and, in needed, epinephrine) that should be prescribed in each food allergic patient.
In specialized settings, and mainly in pediatric patients aged at least 5 years, oral immunotherapy is a therapeutical option for milk, egg, and peanut allergy, following the European guidelines (15).
Most common food allergens in children
Cow’s milk
Cow’s milk allergy (CMA) may be considered as the most common expression of food allergy in children, and especially in infants, affecting 2% of this age group (16). Nevertheless, it is also one of the most complex allergies to diagnose and treat because it may often present as non-IgE mediated. In most cases, the natural history of CMA is toward a natural acquisition of the immunological tolerance before school age (17). Primary care physicians play an essential role in the diagnosis and management of CMA. In fact, in 2010, a study conducted in the UK showed that 86% of children suffering from CMA were first diagnosed in primary care settings (18). The management of CMA is the same as the one of other food allergies, that has been discussed above. What is peculiar in CMA is the higher prevalence of non-IgE mediated forms, if compared with other food allergies in pediatrics. Also, it is usually the first food allergy appearing in a patient’s life, and management is different if children are breastfed or if they are nourished with formula.
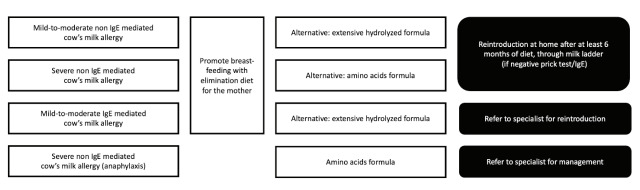
The 2019 international Milk Allergy in Primary (i-MAP) Care guideline well address this topic and the best current management in clinical practice (19). Except for patients presenting with Food Protein-Induced Enterocolitis Syndrome (FPIES), non-IgE mediated CMA rarely occurs in exclusively breast-fed infants. In patients fed with formula or with mixed breast milk and formula, symptoms mostly occur within 2 to 72 hours after exposure to the allergen. Main symptoms are gastro-intestinal (persisting irritability, discomfort, gastro-esophageal reflux, blood and/or mucus in stool, and vomiting and/or diarrhea of different degrees of severity) (19). It is debated whether isolated failure to growth might also be a potential sign of non-IgE mediated CMA and should be carefully investigated (19,20). Skin symptoms usually include non-specific rashes and atopic dermatitis at different severity degrees. Since no test is available to assess this form of food allergy, an elimination diet should correlate with symptoms improvement after no more than 3 to 7 days, and allow a diagnosis, when symptoms reappear when the infant is re-exposed to milk, after at least 4 weeks of diet. Breast-feeding mother should follow the elimination diet as well. In mild to moderate forms an extensively hydrolyzed formula should be prescribed, while in severe ones an amino acids formula would be advisable, whenever breast-feeding is not possible (19). The diet should be followed at least until the age of 9-12 months and for at least 6 months. If no sign of immediate IgE mediated allergy is present (negative prick tests and specific IgE), the reintroduction may be performed at home, using a milk ladder (19).
In case of delayed symptoms evocative for cow’s milk proteins induced enterocolitis syndrome, the mother should avoid milk proteins from her diet or, if breastfeeding is impossible, the patient should be put on amino acids formula. In any case, with these symptoms, the patient should be referred to a specialized center.
In case of IgE mediated CMA, presenting with the previously described typical signs and symptoms, exclusion of cow’s milk proteins from maternal diet is advised for breast-fed infants, while an extensively hydrolyzed formula should be prescribed in the presence of mild to moderate symptoms (19). In case of anaphylaxis, an amino acids formula is needed, and a specialized consultation required. In these cases, the reintroduction of milk will be carried out in specialized settings. Figure 3 summarizes what’s stated in this paragraph, for a more practical approach. Regarding prevention, exposure to cow’s milk formula in the first days of life potentially may potentially increase the risk for CM sensitization in infants with allergic family history (21).
Figure 3. Overall management in primary care, for children presenting with cow’s milk allergy.
Hen’s egg
Hen’s egg allergy is caused by an allergic reaction to egg proteins and, like CMA, is one of the most common food allergies during childhood. Culprit proteins are mainly those in the egg white, but patients may also be allergic to yolk (22). Such allergy is common in children younger than 5 years and usually first noticed in infancy when egg is introduced into the diet for the first time. In most cases, as for CMA, the natural history of egg allergy is toward a spontaneous im-munological tolerance before school age (17).
Most reactions to egg are mild and IgE mediated. The more the egg is cooked or processed the less likely it is to cause a reaction. Moreover, using the egg as an ingredient for wheat containing baked food, in patients who don’t present symptoms with cooked egg, may help acquire an immunological tolerance towards raw egg as well (23). This same aspect has also been highlighted for baked food containing milk. Being egg allergy mainly IgE mediated, in case of a history in favor of such diagnosis, primary care physicians may start an elimination diet before addressing the child to a specialist to evaluate the possibility of performing a challenge in a supervised setting. Non-IgE mediated reactions to egg are mostly related to gastro-intestinal symptoms, and the most common non immediate disease due to egg allergy seems to be esophageal esophagitis (24). The elimination diet, in these cases, might correlate with symptoms relief.
An increasing interest, in recent years, has been put towards the possibility of preventing the appearance of egg allergy in infants at risk. The Starting Time of Egg Protein (STEP) randomized trial, run on a group of 820 infants, showed no evidence that regular egg intake from 4-6 months of age substantially alters the risk of developing egg allergy in infants who are at hereditary risk of allergic disease, but without signs of eczema (25). The Prevention of Egg Allergy with Tiny amount InTake (PETIT) study, on the other hand, showed that children suffering from eczema and consuming heated egg powder from the age of 6 months presented a statistically significant lower incidence of egg allergy at the age of 1 year, if compared with those (presenting with eczema as well) avoiding egg until 12 months of age (26). A meta-analysis, based on 4 studies, showed that the risk of egg sensitization is lower in infants with early egg introduction, even though the random-effects model was not statistically significant (risk ratio 0.77; 95% CI, 0.53-1.11) (24). On the other hand, the risk of egg allergy, based on 5 studies, is significantly reduced in infants with early egg introduction (risk ratio 0.56; 95% CI, 0.36-0.87) (7). Currently, it should be considered that oral tolerance induction, with 2 grams of well-cooked egg per week, from the beginning of weaning, at 4 months of age, is safe for nutrition, growth and general child health and is more effective in preventing egg allergy than later introduction (8).
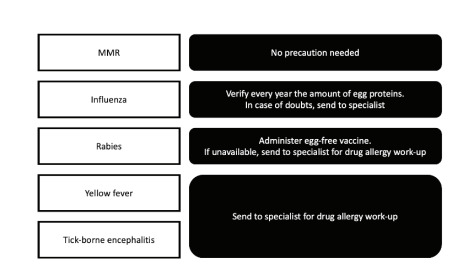
One last important issue concerning egg allergy is the risk of reaction due to vaccines administration. Egg allergic patients should undergo a drug allergy work-up with the vaccines, before being injected with those for yellow fever, and tick-borne encephalitis; for rabies, it is currently available a vaccine not containing egg proteins; for the flu vaccine, the amount of egg proteins should be verified each year, being variable depending on the production of the vaccinal strain (27). No restriction is advisable for egg allergic patients for the MMR vaccine (figure 4). The nasal influenza vaccine (Fluenz®) is safe for egg allergic children as well.
Figure 4. Primary care management of different vaccines in egg allergic patients.
Peanuts
In addition to CMA and egg’s allergies, peanut allergy may also be considered as a common cause food allergy in children. Unlike what has been observed for egg and milk, patients suffering from peanut allergy tend to present a persistent allergy through their life (17). Most reactions are IgE mediated and immediate. Peanut allergy is often severe and associated with a high risk of anaphylaxis. Direct or indirect contact with peanuts may elicit clinical symptoms in severely allergic patients (28).
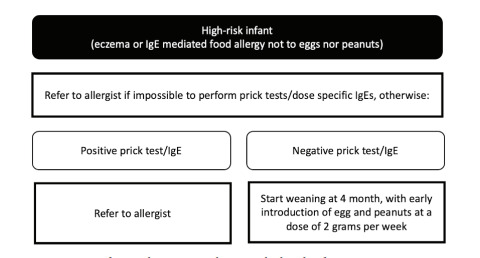
Today, several studies focus on the possibility of treating peanut allergy through oral immunotherapy, to provide patients a lowered risk of accident in case of accidental exposure and to improve the quality of life of both children and caregivers (14). The other strategy to avoid the spreading of this potentially severe allergy is to seek for primary prevention. The Learning Early About Peanut (LEAP) and the Enquiring About Tolerance (EAT) trials showed a risk reduction of peanut allergy in eczematous at-risk children consuming peanuts from the age of 4 month, in an appropriate form, compared with control groups (29,30). A previously mentioned meta-analysis, based on 1 study only, showed that the risk of peanut sensitization is lower (even though not statistically significant) in infants with early peanut introduction (risk ratio 0.68; 95% CI, 0.40-1.15) (7). On the other hand, the risk of peanut allergy, based on 2 studies, is reduced in infants with early peanut introduction, with a statistically significant random-effects model (risk ratio 0.29; 95% CI, 0.11-0.74) (17). Today, it should be considered that a dosing regimen of 2 grams per week of peanuts in early infancy is more effective in inducing oral tolerance than a later introduction (8) (figure 5).
Figure 5. Primary care management of egg and peanut introduction in high-risk infants.
Conclusion
In children, food allergy, and especially IgE mediated forms, are associated to the risk of severe allergic reactions, including anaphylaxis, and have a strong impact on the quality of life of patients and families. Primary care physicians are the first healthcare providers to which families refer in case of the appearance of mild-to moderate symptoms. It is therefore important for doctors to know the first steps to diagnose food allergies and to start an adequate treatment, including an elimination diet and the emergency kit prescription. In case of milk allergy, a proper management, especially of non-IgE mediated reactions, is essential to provide the best advises to the parents of the allergic child. Also, primary care providers should be aware of the new preventive strategies, focused mainly on egg and peanuts allergy, that should be provided in children at risk of developing food allergies. The role of primary care is essential not only for improving life’s quality of children and their families, but also for reducing health care costs.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
References
- Longo G, Berti I, Burks AW, Krauss B, Barbi E. IgE-mediated food allergy in children. Lancet. 2013;382:1656–64. doi: 10.1016/S0140-6736(13)60309-8. [DOI] [PubMed] [Google Scholar]
- De Silva D, Halken S, Singh C, et al. Preventing immediate- onset food allergy in infants, children and adults: Systematic review protocol. Pediatr Allergy Immunol. 2020;31:243–9. doi: 10.1111/pai.13177. [DOI] [PubMed] [Google Scholar]
- Branum AM, Lukacs SL. Food allergy among children in the United States. Pediatrics. 2009;124:1549–55. doi: 10.1542/peds.2009-1210. [DOI] [PubMed] [Google Scholar]
- Abrams EM, Hildebrand K, Blair B, Chan ES. Timing of introduction of allergenic solids for infants at high risk. Health. 2019;24:56–7. doi: 10.1093/pch/pxy195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce JA, Assa’ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126(6 Suppl):S1–58. doi: 10.1016/j.jaci.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muraro A, Halken S, Arshad SH, et al. EAACI food allergy and anaphylaxis guidelines. Primary prevention of food allergy. Allergy. 2014;69:590–601. doi: 10.1111/all.12398. [DOI] [PubMed] [Google Scholar]
- Ierodiakonou D, Garcia-Larsen V, Logan A, et al. Timing of allergenic food introduction to the infant diet and risk of allergic or autoimmune disease: a systematic review and meta-analysis. JAMA. 2016;316:1181–92. doi: 10.1001/jama.2016.12623. [DOI] [PubMed] [Google Scholar]
- Fisher HR, Lack G, Roberts G, Bahnson HT, Du Toit G. Medical algorithm: early introduction of food allergens in high-risk populations. Allergy. 2021;76:1592–4. doi: 10.1111/all.14717. [DOI] [PubMed] [Google Scholar]
- Dowling PJ. Food allergy: practical considerations for primary care. Mo Med. 2011;108:344–9. [PMC free article] [PubMed] [Google Scholar]
- Muraro A, Werfel T, Hoffmann-Sommergruber K, et al. EAACI food allergy and anaphylaxis guidelines: diagnosis and management of food allergy. Allergy. 2014;69:1008–25. doi: 10.1111/all.12429. [DOI] [PubMed] [Google Scholar]
- Sampson HA. Update on food allergy. J Allergy Clin Immunol. 2004;113:805–19. doi: 10.1016/j.jaci.2004.03.014. [DOI] [PubMed] [Google Scholar]
- Bindslev-Jensen C, Ballmer-Weber BK, Bengtsson U, et al. Standardization of food challenges in patients with immediate reactions to foods-position paper from the European Academy of Allergology and Clinical. Immunology. Allergy. 2004;59:690–7. doi: 10.1111/j.1398-9995.2004.00466.x. [DOI] [PubMed] [Google Scholar]
- Sozmen Caglayan, Povesi Dascola C, Gioia E, et al. Diagnostic accuracy of patch test in children with food allergy. Pediatr Allergy Immunol. 2015;26:416–22. doi: 10.1111/pai.12377. [DOI] [PubMed] [Google Scholar]
- Mori F, Giovannini M, Barni S, et al. Oral immunotherapy for food-allergic children a procon debate. Preprints. 2021 doi: 10.3389/fimmu.2021.636612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pajno GB, Fernandez-Rivas M, Arasi S, et al. EAACI Guidelines on allergen immunotherapy: IgE-mediated food allergy. Allergy. 2018;73:799–815. doi: 10.1111/all.13319. [DOI] [PubMed] [Google Scholar]
- Venter C, Brown T, Meyer R, et al. Better recognition, diagnosis and management of non-IgE-mediated cow’s milk allergy in infancy: iMAP-an international interpretation of the MAP (Milk Allergy in Primary Care) guideline. Clin Transl Allergy. 2017;7:26. doi: 10.1186/s13601-017-0162-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juchet A, Chabbert-Broue A. Multiple food allergies in children. Rev Fr Allergol [Google Scholar]
- Sladkevicius E, Nagy E, Lack G, Guest JF. Resource implications and budget impact of managing cow milk allergy in the UK. J Med Econ. 2010;13:119–28. doi: 10.3111/13696990903543242. [DOI] [PubMed] [Google Scholar]
- Fox A, Brown T, Walsh J, et al. An update to the milk allergy in primary care guideline. Clin Transl Allergy. 2019;9:40. doi: 10.1186/s13601-019-0281-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaferio L, Caimmi D, Verga MC, et al. May failure to thrive in infants be a clinical marker for the early diagnosis of cow’s milk allergy? Nutrients. 2020;12:466. doi: 10.3390/nu12020466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastrorilli C, Santoro A, Caffarelli C. Primary prevention of allergic diseases: The role of early exposure to cow’s milk formula. Front Pediatr. 2020;8:420. doi: 10.3389/fped.2020.00420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anagnostou A. Optimizing patient care in egg allergy diagnosis and treatment. J Asthma Allergy. 2021;14:621–8. doi: 10.2147/JAA.S283307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rare Fiocchi A., Nowak-Wegrzyn A. medium, or well done? The effect of heating and food matrix on food protein allergenicity. Curr Opin Allergy Clin Immunol. 2009;9:234–7. doi: 10.1097/ACI.0b013e32832b88e7. [DOI] [PubMed] [Google Scholar]
- Benhamou AH, Caubet JC, Eigenmann PA, et al. State of the art and new horizons in the diagnosis and management of egg allergy. Allergy. 2010;65:283–9. doi: 10.1111/j.1398-9995.2009.02251.x. [DOI] [PubMed] [Google Scholar]
- Palmer DJ, Sullivan TR, Gold MS, Prescott SL, Makrides M. Randomized controlled trial of early regular egg intake to prevent egg allergy. J Allergy Clin Immunol. 2017;139:1600–7. doi: 10.1016/j.jaci.2016.06.052. [DOI] [PubMed] [Google Scholar]
- Natsume O, Kabashima S, Nakazato J, et al. Two-step egg introduction for prevention of egg allergy in high-risk infants with eczema (PETIT): a randomised, double-blind, placebo-controlled trial. Lancet. 2017;389:276–86. doi: 10.1016/S0140-6736(16)31418-0. [DOI] [PubMed] [Google Scholar]
- Egg allergy. Available online at: http://e-allergie.fr . Accessed on June 18th 2021.
- Lieberman JA, Gupta RS, Knibb RC, et al. The global burden of illness of peanut allergy: A comprehensive literature review. Allergy. 2021;76:1367–84. doi: 10.1111/all.14666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Toit G, Roberts G, Sayre PH, et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015;372:803–13. doi: 10.1056/NEJMoa1414850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkin MR, Logan K, Tseng A, et al. Randomized trial of introduction of allergenic foods in breast-fed infants. J Med. 2016;374:1733–43. doi: 10.1056/NEJMoa1514210. [DOI] [PubMed] [Google Scholar]


