Abstract
Objectives:
The purpose of this study was to examine associations between psychotherapy session attendance, alcohol treatment outcomes, and Alcoholics Anonymous (AA) attendance.
Method:
Using data from Project MATCH, repeated measures latent class analyses of psychotherapy session attendance were conducted among participants in the outpatient arm who were randomly assigned to complete 12-session cognitive-behavioral therapy (CBT) (n = 301), 12-session twelve-step facilitation (TSF) (n = 335), or 4-session motivational enhancement therapy (MET) (n = 316). Associations between psychotherapy attendance classes, heavy drinking, alcohol-related consequences, psychosocial functioning, and AA attendance were examined at posttreatment (97% retention), one-year posttreatment (92% retention), and three-years posttreatment (85% retention).
Results:
In general, participants who attended all 12 CBT/TSF sessions had significantly fewer heavy drinking days and alcohol-related consequences at all posttreatment time points than participants who attended 0–2 CBT/TSF sessions. Participants who attended all 4 MET sessions generally had significantly fewer heavy drinking days and alcohol-related consequences at posttreatment and one-year posttreatment than participants who attended 0–1 MET sessions. Participants who attended more TSF and MET sessions generally attended more AA meetings, and participants who attended less CBT sessions generally attended fewer AA meetings.
Conclusions:
With some exceptions, attending all sessions in CBT, TSF, and MET was related to the most favorable heavy drinking and alcohol-related consequences outcomes. Alcoholics’ Anonymous and other mutual help groups may be attended differently based on the form and dose of psychotherapy.
Keywords: attendance patterns, dose-response, long-term outcomes, alcohol use disorder, repeated measures latent class analysis
Over three decades of research has investigated the dose-response model in psychotherapy. This model defines dose as a therapy session and response as the therapeutic outcome (Howard et al., 1986). Research suggests a stronger relation between the number of sessions and outcomes during early sessions than during later sessions (Robinson et al., 2020).
Psychotherapy is a common treatment modality for alcohol use disorder (AUD), and research supports a positive relation between session attendance and outcomes in psychotherapy for AUD (Connors et al., 2002; Dearing et al., 2005). Several reviews on AUD treatment show cognitive-behavioral therapy (CBT), motivational enhancement therapy (MET), and twelve-step facilitation (TSF) promote better treatment outcomes than minimally treated comparison conditions (Kelly et al., 2020; Lundahl & Burke, 2009; Magill & Ray, 2009). In these three forms of psychotherapy, there is a positive correlation between the number of sessions attended and the percentage of days abstinent at posttreatment (Connors et al., 2002; Dearing et al., 2005). However, more work is needed to understand the relation between session attendance and longer-term outcomes (i.e., in the years following treatment), because many individuals return to alcohol use during treatment and following psychotherapy termination (Magill & Ray, 2009).
Secondary analyses have examined the correlation between the number of psychotherapy sessions attended and alcohol abstinence outcomes in the landmark clinical trial, Project MATCH (Project MATCH Research Group, 1997). In Project MATCH, participants with AUD were randomized to 12 sessions of CBT, 12 sessions of TSF, or 4 sessions of MET. Cutler and Fishbain (2005) found a positive correlation between the number of sessions attended and the percentage of days abstinent at one-year follow-up in CBT and TSF, but not MET. Similarly, Mattson and colleagues (1998) found a positive correlation between proportion of sessions attended and percentage of days abstinent at one-year follow-up in CBT and TSF, but not MET. Secondary analyses of Project MATCH indicated therapist effects on drinking outcomes, but no therapist effects on the number of sessions attended (Project MATCH Research Group, 1998).
Despite the importance of these prior studies, they have at least three major limitations. First, they did not examine the patterns of session attendance or provide recommendations for how many sessions of psychotherapy are associated with favorable outcomes. Second, they have only modeled abstinence outcomes and neglected other recovery outcomes, including alcohol-related consequences and psychosocial functioning (Witkiewitz et al., 2018). Third, they have not considered how Alcoholics Anonymous (AA) attendance was related to psychotherapy dose, even though attending AA is more common than attending psychotherapy for AUD and AA attendance is common among those in psychotherapy for AUD (Breuninger et al., 2020).
The purpose of this study was to use the Project MATCH data to examine the relation between patterns of psychotherapy session attendance and several AUD outcomes at posttreatment, one-year posttreatment, and three-years posttreatment in CBT, TSF, and MET. Another purpose was to examine the relation between psychotherapy session attendance and the percentage of days attending AA up to three years posttreatment.
Method
Participants and Procedures
The present study was a secondary analysis of data collected in Project MATCH (Project MATCH Research Group, 1997). Participants were those in the outpatient arm (N = 952) who received treatment for DSM-III-R alcohol abuse or dependence (American Psychiatric Association, 1987) from nine sites in the United States. Analyses were conducted separately for 12-session CBT (n = 301), 12-session TSF (n = 335), and 4-session MET (n = 316).
Measures
Psychotherapy Attendance
Binary indicators of psychotherapy session attendance reported in client session report forms were used as indicator variables for the repeated measures latent class analyses.
Baseline Predictors
Baseline predictors of latent class membership included demographic variables, the number of prior alcohol use treatment episodes, social network support for drinking assessed by the Important People and Activities Instrument (Clifford & Longabaugh, 1991), alcohol dependence severity assessed by the Alcohol Dependence Scale (Skinner & Horn, 1984), readiness to change assessed by the University of Rhode Island Change Assessment (DiClemente et al., 2004), Alcoholics Anonymous Involvement (Tonigan et al., 1996), the percentage of days attending AA meetings in the past 90 days, and self-efficacy assessed by the confidence subscale of the Alcohol Abstinence Self-Efficacy Scale (DiClemente et al., 1994).
Posttreatment and Long-Term Recovery Outcomes
Outcomes were heavy drinking, alcohol-related consequences, and psychosocial functioning at posttreatment, one-year posttreatment, and three-years posttreatment. The Form-90 (Miller et al., 1995) measured the percentage of heavy drinking days (PHD; i.e., ≥4/5 drinks in a day for women/men) in the previous 90 days. The Drinker Inventory of Consequences (Miller et al., 1995) measured alcohol-related consequences. The social behavior subscale of the Psychosocial Functioning Inventory (Feragne et al., 1983) measured psychosocial functioning.
Mutual Help Group Attendance
The percentage of days attending AA/12-step groups in the past 90 days was calculated at baseline and all three posttreatment assessments (Miller et al., 1995).
Data Analysis Plan
Mplus version 8.4 was used to estimate latent classes of psychotherapy session attendance and their associations with AUD recovery outcomes via the 3-step Bolck, Croon, and Hagenaars (BCH) approach (Bolck et al., 2004; Nylund et al., 2019). In step 1, separate analyses were conducted to identify latent classes of treatment attendance in CBT, TSF, and MET using weighted maximum likelihood with all available data. Model fit for models with varying numbers of latent classes without covariates were compared using the Lo–Mendell–Rubin likelihood ratio test, the bootstrapped likelihood ratio test, Bayesian information criterion (BIC), and sample size-adjusted BIC to identify the optimal number of classes. In step 2, latent class membership was saved as an observed variable based on posterior probabilities of latent class membership. In step 3, posterior probabilities were used to obtain observed frequencies and means for AUD outcomes and covariate predictors within each latent class. A Wald χ2 statistic was used for omnibus testing of differences between latent classes on distal outcomes at posttreatment, one-year posttreatment, and three-years posttreatment and predictors at baseline, followed by independent samples t-tests for pairwise class comparisons. For all analyses, the multiple research sites were entered as a cluster variable and the standard errors were adjusted for clustering of individuals within sites using a sandwich estimator.
Results
Participants were 72% male, 80% non-Hispanic and White, 35% married, and with mean age of 38.9 years (SD = 10.7). At baseline, participants reported an average of 13.62 drinks per drinking day (SD = 8.76), 65.77% drinking days (SD = 29.83), and 58.33% heavy drinking days (SD = 30.78). Individuals across all three treatment conditions had high follow-up rates at posttreatment (97%), one-year (92%), and three-years posttreatment (85%). Individuals completed, on average, 60.5% (TSF) to 78.0% (MET) of all possible treatment sessions (CBT: M (SD) = 7.99 (3.99); TSF: M (SD) = 7.26 (4.12); MET: M (SD) = 3.12 (1.26)). Prior treatment episodes, baseline AA involvement, alcohol dependence severity, age, and identifying as White were associated with attendance classes.1
Repeated Measures Latent Class Analyses
Repeated measures latent class models were estimated for CBT, TSF, and MET (see Supplemental materials). Nearly identical five-class models were retained as the optimal solutions for CBT and TSF. A three-class model was retained for MET. Collectively, these models characterized individuals who were probabilistically classified based on approximate numbers of sessions attended. In CBT and TSF, individuals with expected classification in class 1 attended approximately 12 sessions (n = 126 in CBT, n = 115 in TSF), class 2 approximately 9–11 sessions (n = 50 in CBT, n = 55 in TSF), class 3 approximately 6–8 sessions (n = 44 in CBT, n = 50 in TSF); class 4 approximately 3–5 sessions (n = 36 in CBT, n = 45 in TSF), and class 5 approximately 0–2 sessions (n = 45 in CBT, n = 70 in TSF). In MET, individuals with expected classification in class 1 attended approximately 4 sessions (n = 233), class 2 approximately 2–3 sessions (n = 43), and class 3 approximately 0–1 sessions (n = 40).
Attendance Patterns and AUD Recovery Outcomes
CBT and TSF participants in class 1, “attending 12 sessions,” generally had significantly lower PHD at posttreatment, one-year posttreatment, and three-years posttreatment than participants in class 5 “attending 0–2 sessions” (Figure 1). One exception was that there was no significant difference in PHD at three-years posttreatment between TSF participants in classes 1 and 5. However, TSF participants in class 2, “attending 9–11 sessions,” had lower PHD at posttreatment, one-year posttreatment, and three-years posttreatment than participants in class 5. TSF participants in class 4, “attending 3–5 sessions,” also had significantly lower PHD at one-year posttreatment and three-years posttreatment than participants in class 5. MET participants in class 1, “attending 4 sessions,” had significantly lower PHD at posttreatment and one-year posttreatment than participants in class 3, “attending 0–1 MET sessions.”
Figure 1.
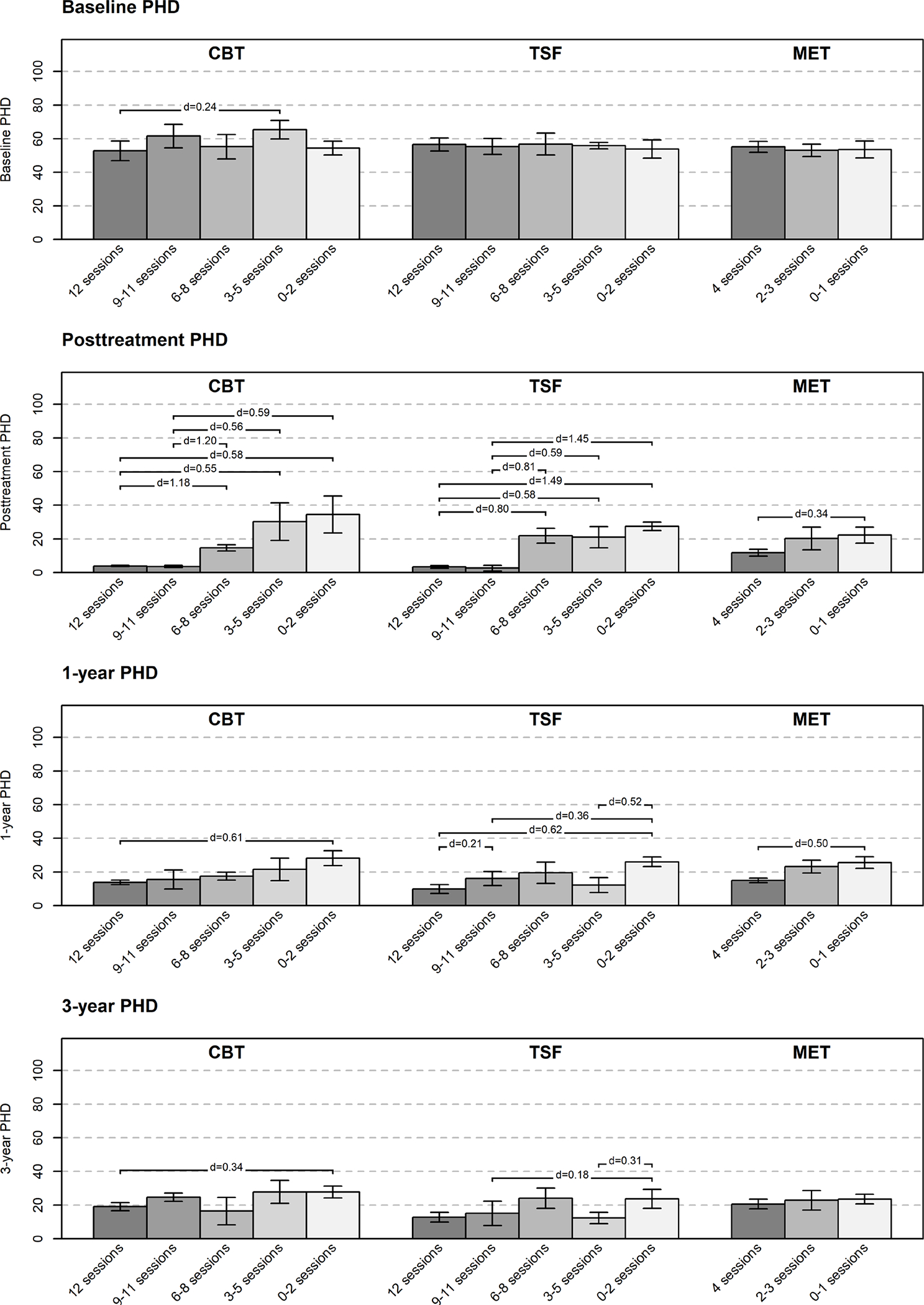
Percentage of Heavy Drinking Days (PHD) Across Attendance Patterns.
Note. Cohen’s d effect sizes are provided when differences between classes are significant (p < .05).
Figure 2 indicates that CBT and TSF participants in class 1, “attending 12 sessions,” generally had significantly fewer alcohol-related consequences at posttreatment, one-year posttreatment, and three-years posttreatment than participants in class 5, “attending 0–2 sessions.” Two exceptions were that there were no significant differences in consequences at posttreatment and one-year posttreatment between TSF participants in classes 1 and 5. However, TSF participants in class 1 had significantly fewer consequences at posttreatment than participants in classes 3, “attending 6–8 sessions,” and 4, “attending 3–5 sessions.” Importantly, CBT and TSF participants in class 5 had more consequences at baseline, but there were also large reductions in consequences across attendance classes from baseline through three-years posttreatment. MET participants in class 1, “attending 4 sessions,” had significantly fewer consequences at posttreatment than participants in class 3, “attending 0–1 sessions.”
Figure 2.
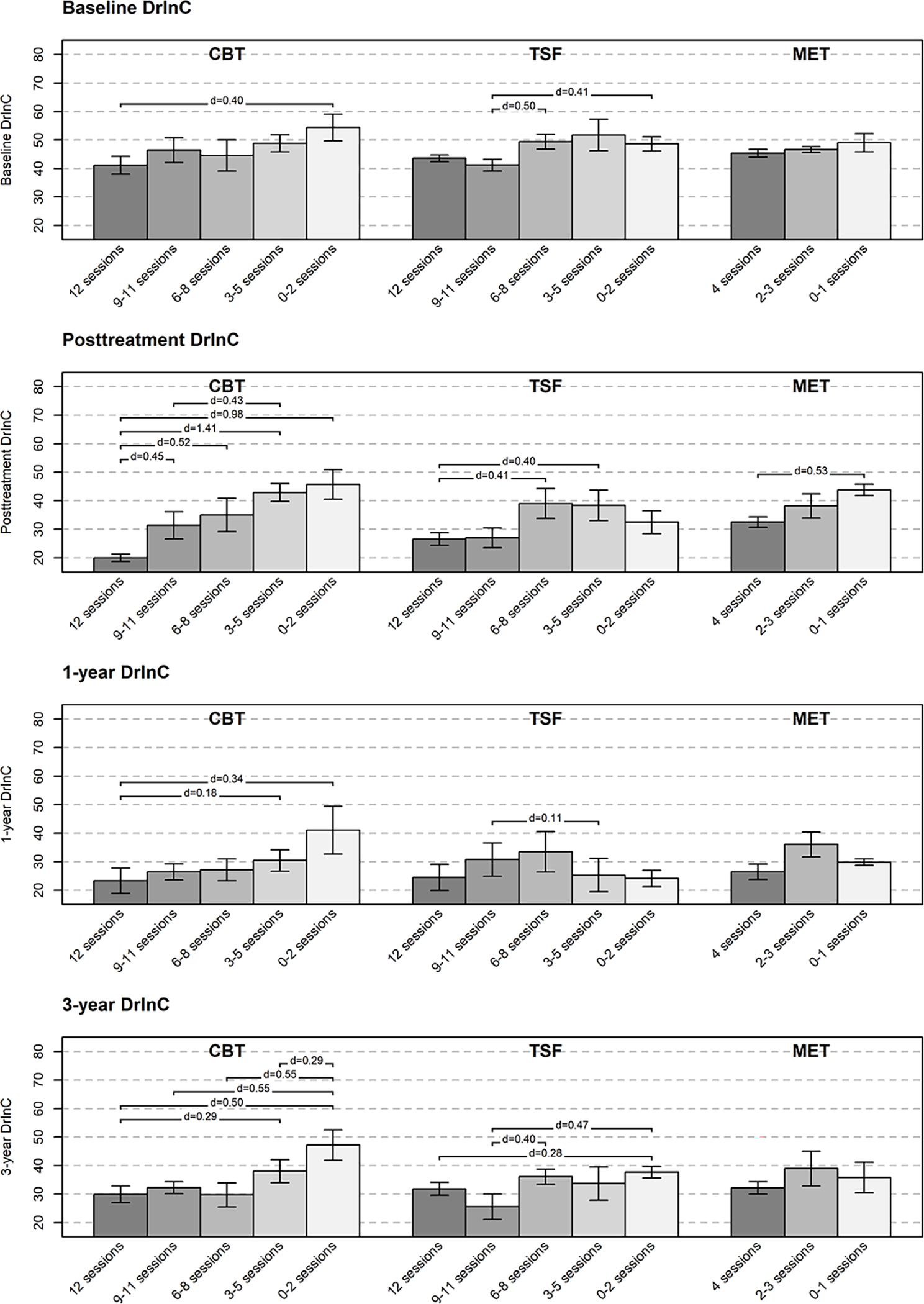
Negative Alcohol-Related Consequences (DrInC Scores) Across Attendance Patterns.
Note. Cohen’s d effect sizes are provided when differences between classes are significant (p < .05).
Figure 3 presents the psychosocial functioning at baseline and all three posttreatment assessments in CBT, TSF, and MET. CBT participants in class 1, “attending 12 sessions,” had significantly better psychosocial functioning at posttreatment, one-year posttreatment, and three-years posttreatment participants in class 5, “attending 0–2 sessions.” However, there were also moderate to large baseline differences in psychosocial functioning across classes, with increases in psychosocial functioning following treatment. No consistent differences in psychosocial functioning were found in TSF and MET.
Figure 3.
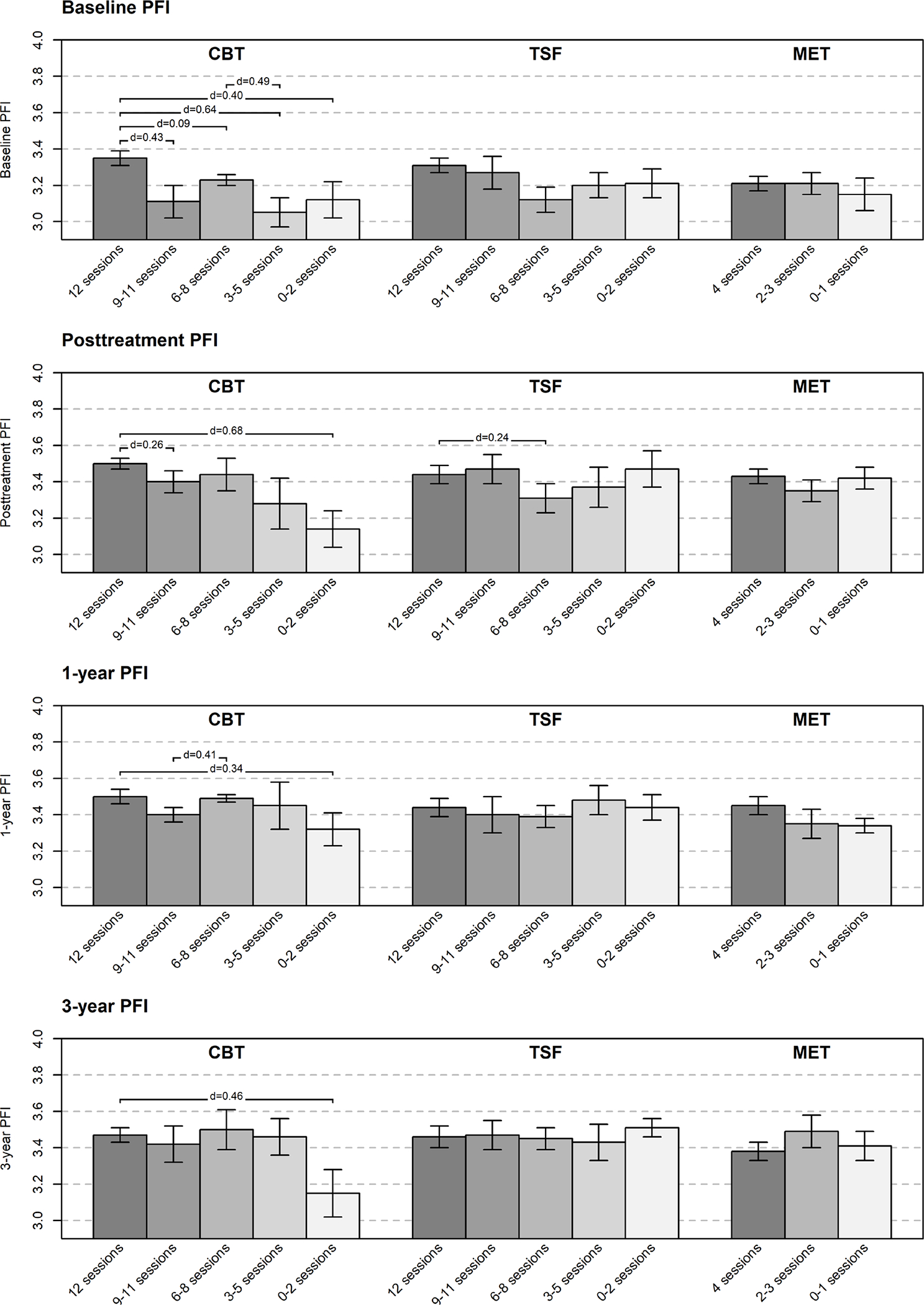
Psychosocial Functioning (PFI Social Behavior Subscale Scores) Across Attendance Patterns
Note. Cohen’s d effect sizes are provided when differences between classes are significant (p < .05).
Attendance Patterns and AA Attendance
Figure 4 presents the percentage of days attending AA meetings in CBT, TSF, and MET. CBT participants in class 5, “attending 0–2 sessions,” generally attended more AA meetings than participants in classes representing higher session attendance. For example, CBT participants in class 5 attended significantly more AA meetings than participants in class 4, “attending 3–5 sessions,” at posttreatment and three-years posttreatment, as well as class 1 “attending 12 sessions,” at one-year posttreatment. TSF participants in class 1, “attending 12 sessions,” generally attended significantly more AA meetings than participants in classes representing lower session attendance. For example, TSF participants in class 1 attended significantly more AA meetings at all three posttreatment assessments than participants in class 2, “attending 9–11 sessions.” MET participants in class 1, “attending 4 sessions,” attended significantly more AA meetings at posttreatment than participants in class 3, “attending 0–1 sessions.”
Figure 4.
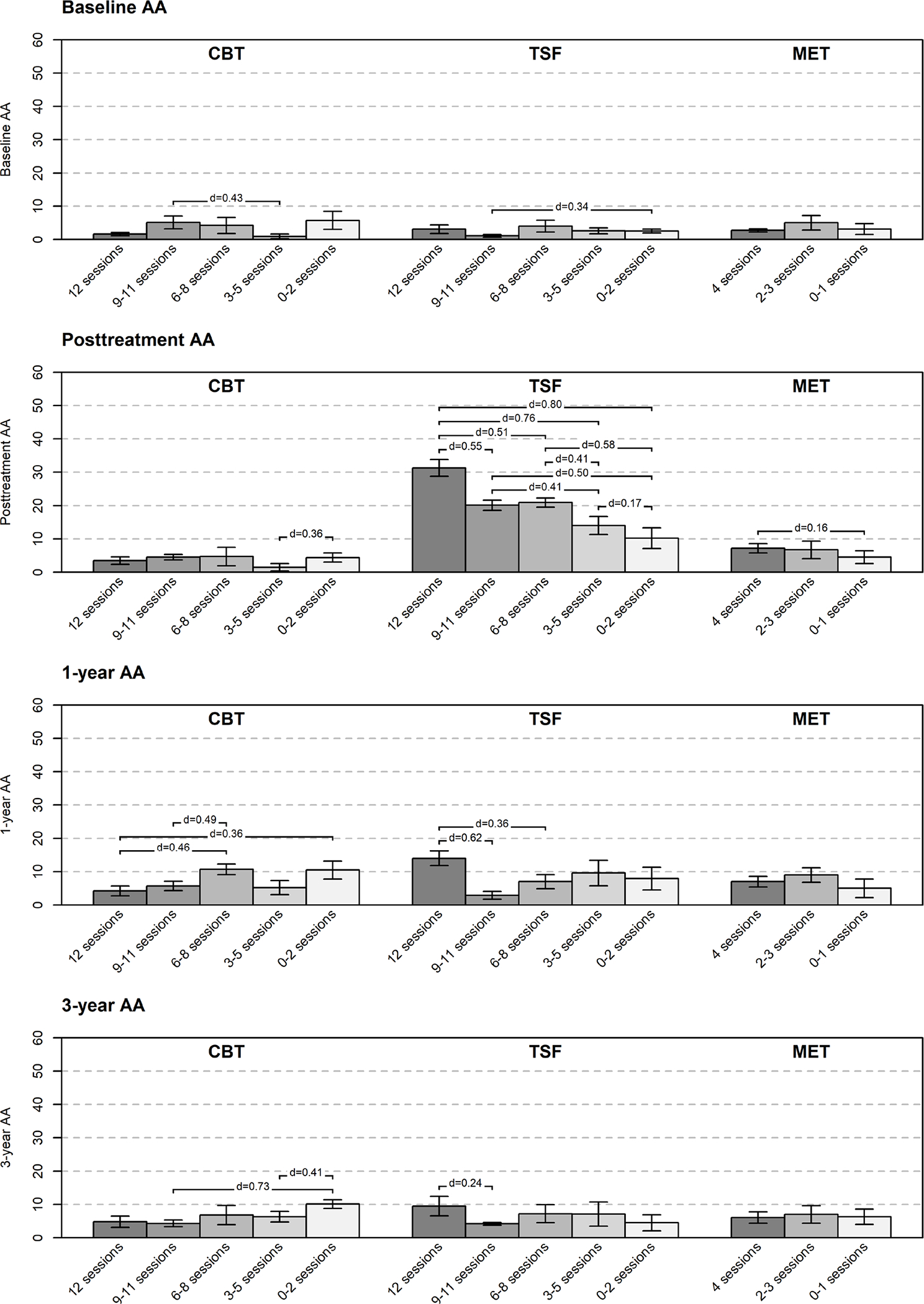
Alcoholics Anonymous (AA) or Other 12-Step Group Attendance Across Attendance Patterns
Note. Cohen’s d effect sizes are provided when differences between classes are significant (p < .05).
Discussion
Consistent with prior research, attending more psychotherapy sessions was related to more favorable outcomes at posttreatment and in the years following treatment (Cutler & Fishbain, 2005; Mattson et al., 1998). The current study improved upon that prior research by indicating the number of sessions that related to favorable outcomes in AUD treatment. In general, attending all 12 CBT sessions and 12 TSF sessions was related to significantly better outcomes than attending 0–2 sessions at all posttreatment assessments. However, there were some exceptions. Effect sizes in the differences in outcomes between attendance classes were moderate-to-large at posttreatment and reduced to small-to-moderate at one- and three-years posttreatment. The lack of significant differences in psychosocial functioning likely reflects the narrow focus on drinking in AUD treatment and the limited attention on enhancing functioning. For MET, attending all 4 sessions was generally related to significantly fewer heavy drinking days and alcohol-related consequences than attending 0–1 sessions. Effect sizes in these outcome differences were small-to-moderate at posttreatment and one-year posttreatment.
The current study also suggested that the function of AA attendance during psychotherapy may depend on the form of psychotherapy and how many sessions are attended. In all treatment approaches, it is important to consider whether AA could serve as a supplement or alternative to psychotherapy. For example, clinicians who offer CBT may encourage clients to participate in AA during early treatment sessions (Breuninger et al., 2020) or as a backup option if clients are unable to continue attending CBT sessions, as greater AA attendance was generally related to classes representing lower CBT attendance. It is possible that mutual help programs may be more accessible and/or more acceptable to some clients, especially those who are unable to attend an adequate “dose” of CBT sessions. By contrast, AA attendance appears to complement TSF and MET session attendance, as greater AA attendance was generally related to classes representing higher TSF attendance and higher MET attendance.
The present study had several limitations. The parent clinical trial was conducted decades ago and involved an outpatient sample that was predominately comprised of middle-aged, White males. Future studies will need to replicate the results in modern and diverse samples. All treatments studied were time-limited, and attendance patterns beyond 12 sessions could not be modeled. The current study could not capture other treatments received after the Project MATCH treatment period, and additional unmeasured treatment attendance may have further impacted the one-year and three-year posttreatment outcomes. Our quantification of “dose” did not account for potential therapeutic benefits associated with completing research assessments that can provide therapeutic benefit (Epstein et al., 2005). Finally, other factors, including physical health, mental health, and psychosocial functioning predict AUD recovery outcomes after treatment termination (Witkiewitz et al., 2019, 2020), and future research could examine how much variance each factor explains in predicting outcomes in the years following treatment.
Despite these limitations, the results of the present study indicated that greater session attendance in outpatient psychotherapy for AUD was related to more favorable outcomes up to three years following treatment. Attending at least 12 weekly CBT and TSF sessions were related to significant and small-to-moderate improvement in heavy drinking and alcohol-related consequences. Attending at least four MET sessions was also related to significant and small improvement in heavy drinking and consequences. Furthermore, AA may serve a complementary form of support for individuals participating in TSF and MET, whereas AA may provide an alternative for individuals participating in CBT. Clinicians should discuss the role of AA with their clients during psychotherapy and after its termination.
Supplementary Material
Public Health Significance Statement.
Attending 12 sessions of cognitive-behavioral therapy, 12 sessions of twelve-step facilitation, and 4-session motivational enhancement therapy is generally related to significant reductions in heavy drinking and alcohol-related consequences at treatment end and up to three years following treatment. Clinicians should talk to clients about the function of AA attendance during CBT, TSF, and MET, as well as after psychotherapy termination.
Acknowledgments
This work was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health, award numbers L30AA029551, T32AA018108, R01AA022328, K05AA016928, K01AA024796, and K01AA023233. The content is the sole responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosures: All authors declare no competing interests.
At baseline, fewer prior treatment episodes, less AA involvement, and lower alcohol dependence severity predicted patterns of greater attendance in CBT (classes 1 and/or 2). There may be multiple explanations why participants attending the most CBT sessions had the fewest prior treatment episodes. For example, there may have been greater need for skills and novelty of learning new CBT skills. Additionally, participants with more prior treatment may have been more prone to attend fewer sessions due to a greater history of treatment dropout. Furthermore, older age and identifying as White predicted the pattern with greatest attendance (class 1). Participants completing the most TSF sessions were more likely to identify as White, which raises debated questions about whether twelve-step treatments equally appeal to non-White individuals (Tonigan et al., 1998). No other baseline variables consistently predicted attendance classes (Supplemental Tables 2–4).
References
- American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders (3rd ed., rev.; DSM-III-R) (3rd ed., r). Author. [Google Scholar]
- Bolck A, Croon M, & Hagenaars J (2004). Estimating latent structure models with categorical variables: One-step versus three-step estimators. Political Analysis, 12, 3–27. [Google Scholar]
- Breuninger MM, Grosso JA, Hunter W, & Dolan SL (2020). Treatment of alcohol use disorder: Integration of Alcoholics Anonymous and cognitive behavioral therapy. Training and Education in Professional Psychology, 14, 19–26. [Google Scholar]
- Clifford PR, & Longabaugh R (1991). Manual for the administration of the Important People and Activities Instrument. Bethesda, MD: NIAAA. [Google Scholar]
- Connors GJ, Walitzer KS, & Dermen KH (2002). Preparing clients for alcoholism treatment: Effects on treatment participation and outcomes. Psychology of Addictive Behaviors, 70, 1161–1169. 10.1037//0022-006X.70.5.1161 [DOI] [PubMed] [Google Scholar]
- Cutler RB, & Fishbain DA (2005). Are alcoholism treatments effective? The Project MATCH data. BMC Public Health, 5, 1–11. 10.1186/1471-2458-5-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dearing RL, Barrick C, Dermen KH, & Walitzer KS (2005). Indicators of client engagement: Influences on alcohol treatment satisfaction and outcomes. Psychology of Addictive Behaviors, 19, 71–78. 10.1037/0893-164X.19.1.71 [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RPG, & Hughes SO (1994). The alcohol abstinence self-efficacy scale. Journal of Studies on Alcohol, 55, 141–148. [DOI] [PubMed] [Google Scholar]
- DiClemente Carlo C, Schlundt D, & Gemmell L (2004). Readiness and stages of change in addiction treatment. American Journal on Addictions, 13, 103–119. [DOI] [PubMed] [Google Scholar]
- Epstein E, Drapkin ML, Yusko DA, Cook SM, McCrady BS, & Jensen NK (2005). Is alcohol assessment therapeutic? Pretreatment change in drinking among alcohol-dependent women. Journal of Studies on Alcohol and Drugs, 66, 369–379. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. (1997). Project MATCH secondary a priori hypotheses. Addiction, 92, 1671–1698. 10.1111/j.1360-0443.1997.tb02889.x [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. (1998). Therapist effects in three treatments for alcohol problems. Psychotherapy Research, 8, 455–474. doi.org/10.1080/10503309812331332527 [Google Scholar]
- Howard KI, Kopta SM, & Orlinsky DE (1986). The dose-effect relationship in psychotherapy. American Psychologist, 41, 159–164. [PubMed] [Google Scholar]
- Kelly JF, Humphreys K, & Ferri M (2020). Alcoholics Anonymous and other 12-step programs for alcohol use disorder. Cochrane Database of Systematic Reviews, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl B, & Burke BL (2009). The effectiveness and applicability of motivational interviewing: A practice-friendly review of four meta-analyses. Journal of Clinical Psychology: In Session, 65, 1232–1245. 10.1002/jclp [DOI] [PubMed] [Google Scholar]
- Magill M, & Ray LA (2009). Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. Journal of Studies on Alcohol and Drugs, 70, 516–527. 10.15288/jsad.2009.70.516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson ME, Del Boca FK, Carroll KM, Cooney NL, DiClemente CC, Donovan D, Kadden RM, McRee B, Rice C, Rycharik RG, & Zweben A (1998). Compliance with treatment and follow-up protocols in Project MATCH: Predictors and relationship to outcome. Alcoholism: Clinical and Experimental Research, 22, 1328–1339. [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, & Longabaugh R (1995). The Drinker Inventory of Consequences (DrInC). Rockville, MD: NIAAA. http://pubs.niaaa.nih.gov/publications/drinc.pdf [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO, Nylund-Gibson K, Grimm RP, & Masyn KE (2019). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14, 535–569. [Google Scholar]
- Robinson L, Delgadillo J, & Kellett S (2020). The dose-response effect in routinely delivered psychological therapies: A systematic review. Psychotherapy Research, 30, 79–96. [DOI] [PubMed] [Google Scholar]
- Skinner HA, & Horn JL (1984). Alcohol Dependence Scale (ADS): User’s guide. Addiction Research Foundation. [Google Scholar]
- Tonigan JS, Connors GJ, & Miller WR (1996). Alcoholics anonymous involvement (AAI) scale: Reliability and norms. Psychology of Addictive Behaviors, 10, 75–80. [Google Scholar]
- Tonigan JS, Connors GJ, & Miller WR (1998). Special populations in Alcoholics Anonymous. Alcohol Research and Health, 22, 281–285. [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Falk DE, Litten RZ, Hasin DS, Kranzler HR, Mann KF, O’Malley SS, & Anton RF (2019). Maintenance of World Health Organization risk drinking level reductions and posttreatment functioning following a large alcohol use disorder clinical trial. Alcoholism: Clinical and Experimental Research, 43, 979–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Heather N, Falk DE, Litten RZ, Hasin DS, Kranzler HR, Mann KF, O’Malley SS, & Anton RF (2020). World Health Organization risk drinking level reductions are associated with improved functioning and are sustained among patients with mild, moderate and severe alcohol dependence in clinical trials in the United States and United Kingdom. Addiction, 115, 1668–1680. 10.1111/add.15011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Kirouac M, Roos CR, Wilson AD, Hallgren KA, Bravo AJ, Montes KS, & Maisto SA (2018). Abstinence and low risk drinking during treatment: Association with psychosocial functioning, alcohol use, and alcohol problems 3 years following treatment. Psychology of Addictive Behaviors, 32, 639–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


