Abstract
Internalized weight stigma (IWS) is independently associated with less intuitive eating (i.e., eating based on endogenous hunger/satiety cues) and higher Body Mass Index (BMI), and intuitive eating training is commonly conceptualized as protective against the effects of IWS on poor behavioral health. The 3-way relationship between IWS, intuitive eating, and BMI has yet to be examined, and it is unclear whether the link between IWS and BMI is buffered by high intuitive eating. This secondary preliminary analysis examined baseline data of stressed adults with poor diet (N=75, 70% female, 64.1% White, 42.7% with overweight/obesity) in a parent clinical trial that tested the effects of yoga on diet and stress. Validated self-report surveys of IWS and intuitive eating were analyzed with objectively-assessed BMI. Moderated regression analyses using the SPSS PROCESS macro tested whether intuitive eating moderated the IWS-BMI link. The analysis revealed IWS was positively associated with BMI except among people with high intuitive eating. Results extend observational findings linking intuitive eating to lower BMI, and offer preliminary support for the hypothesis that this link may hold even among those with greater IWS. It’s possible that individuals with lower BMI and greater IWS may gravitate more towards intuitive eating than those with greater BMI, and/or intuitive eating may be an important target for ameliorating the adverse association of IWS with behavioral and physical health indicators linked to BMI. Continued work is warranted in larger, more generalizable samples using causal and prospective designs.
Keywords: Intuitive eating, internalized weight stigma, internalized weight bias, body mass index, stress
Weight-based discrimation is endemic in the United States of America (USA) and is increasingly observed internationally as well (Puhl & Heuer, 2009; Rubino et al., 2020). Internalization of harmful weight-related stereotypes (internalized weight stigma; IWS, also frequently termed internalized weight bias) is similarly prevalent across weight categories in the USA (Puhl et al., 2018) and is associated with stress and poor dietary/eating behaviors that can foster increased risk of chronic diseases and/or unhealthy weight gain (Pearl & Puhl, 2018). Research indicates that IWS affects eating behaviors and exercise through maladaptive coping in response to increased negative affect (Pearl & Puhl, 2018; Webb & Hardin, 2015). One study also suggests IWS may disrupt responsiveness to endogenous hunger and satiety cues (i.e., intuitive eating; eating in response to internal, vs. external cues) (Mensinger et al., 2016).
Intuitive eating interventions that restore awareness of internal hunger and satiety mechanisms while de-emphasizing dieting or weight loss are often taught to improve behavioral health (e.g., binge eating) in eating pathology treatment and non-dieting programs, such as Health At Every Size (HAES®) (Bacon, 2010; Mathieu, 2009; Richards et al., 2017; Tribole & Resch, 1995), trademarked by the Association for Size Diversity and Health (ASDAH) and used with permission. Intuitive eating training problematizes the excessive sociocultural emphasis on body weight, weight loss, and dieting in the USA and seeks to combat weight related myths and misperceptions (e.g., thin-ideal internalization) related to “diet culture,” including self-blame (Tribole & Resch, 2012). Diet culture is conceptualized by intuitive eating and HAES to foster distress and poor behavioral and physical health, including chronic dieting that can lead to binge eating and weight gain. This view aligns with compelling evidence that the adverse effects of weight stigma on health may objectively exceed those of body mass index (BMI) alone through pathways implicating IWS, distress, unhealthy weight control behaviors, poor biomarker profiles, and weight instability, including gain (Pearl & Puhl, 2018; Pearl & Puhl, 2016; Schvey & Roberto, 2013; Tomiyama et al., 2018; Wellman et al., 2018). Indeed, the three factors that comprise the intuitive eating construct – eating primarily for physical rather than emotional reasons, unconditional permission to eat, and reliance on internal hunger and satiety cues – are designed to break the habit of dieting (Tylka, 2006). Developers have emphatically noted that intuitive eating is not to be used as a weight loss strategy (Tribole & Resch, 2012).
Intuitive eating training (and HAES) does not specifically address “internalized weight stigma” (Mensinger et al., 2016), despite an analogous emphasis on combating external and internal sociocultural appearance norms. Indeed, a recent meta-analytic review (89% cross-sectional) found intuitive eating consistently associated with fewer body image disturbances (a construct that shares close conceptual and empirical associations with IWS) as well as less eating pathology and lower BMI (Linardon et al., 2021), consistent with prior reviews (Bruce & Ricciardelli, 2016; Warren et al., 2017). More recent prospective analyses of Project EAT (Eating and Activity Over Time, a population-based cohort study of young adults) have observed intuitive eating predictive of lower body dissatisfaction as well as less dieting, unhealthy weight control behaviors, and binge eating at 5-year follow-up (Cristoph et al., 2021; Hazzard et al 2021). Intuitive eating has also been prospectively associated with lower eating disorder symptom onset (Linardon, 2021) and lower subsequent BMI, post-partum weight retention, fasting glucose, and HbA1c among women with gestational diabetes mellitus (Quansah et al 2019). This preliminary evidence suggests that intuitive eating could potentially protect against IWS-related sequelae and thereby prevent poor health behaviors, biomarker profiles, and/or weight gain that may increase cardiometabolic disease risk over time; yet more research is needed. Further, intuitive eating has rarely been examined in relation to IWS, despite a promising theoretical and empirical rationale for its potential as an intervention target to disrupt the adverse effects of IWS on behavioral and physical health.
To date, we are aware of two studies that have examined the association between IWS and intuitive eating. The first, a cross-sectional analysis, found higher IWS to be associated with lower intuitive eating through lower body image flexibility and self-compassion (Webb & Hardin, 2015). The second study found that greater baseline IWS predicted lower gains in intuitive eating during a healthy lifestyle intervention (Mensinger et al., 2016), suggesting IWS could deplete or lower dispositional intuitive eating over time. Yet evidence showing that intuitive eating is inversely associated with binge eating and BMI and prospectively predicts fewer factors linked to IWS (e.g., body dissatisfaction) clearly implicates the factor as protective against IWS-related sequelae (Cristoph et al., 2021; Hazzard et al., 2020; Linardon et al., 2021). Indeed, intuitive eating also positively connects with factors implicated as protective against IWS and eating pathology, including self-compassion and positive body image (Braun et al., 2020; Bruce & Ricciardelli, 2016).
Despite these data and the frequent utilization of intuitive eating training to disrupt the effects of poor body image in non-dieting programs, to our knowledge no research has yet examined whether intuitive eating buffers the association of the IWS construct with BMI. Delivery of intuitive eating training in a weight-neutral context is critical to retain fidelity to its unique weight-inclusive approach. Yet, better understanding the links between IWS, intuitive eating, and BMI may lead to novel insights that could inform further research examining whether intuitive eating training might serve a preventive strategy to promote behavioral health and weight maintenance/stability, and prevent adverse indices of cardiometabolic health linked to increased BMI in various populations. Indeed, Lindardon and Tylka (2021) note that following their meta-analytic finding linking intuitive eating to lower BMI, we cannot rule out the possibility that intuitive eating may also (or instead) support or be relevant to weight management. Further, better understanding the connections between IWS, intuitive eating, and BMI will assist our comprehension of whether intuitive eating training might serve as a treatment target for improvement of IWS-related behavioral health concerns in those at heightened susceptibility for chronic diseases.
In this cross-sectional preliminary study, we explored (a) the proportion of variance in BMI accounted for by IWS and intuitive eating, (b) whether intuitive eating buffers against (i.e., moderates) the positive link between IWS and BMI.
Materials and Method
Participants and Procedure
The current cross-sectional study is based on an analysis of pre-treatment data from a parent clinical trial examining the effects of a yoga intervention on dietary behavior, conducted from 2015 to 20161. Described in greater detail elsewhere (Greenberg et al., 2018; Braun et al., 2021), the parent study enrolled 84 healthy adults ages 23–67 years of age who reported feeling stressed, consumed fewer than 5 servings of fruits/vegetables per day, were free of conditions or practices known to impact appetite (e.g., psychiatric disorders, certain medications, engagement in weight loss or lifestyle change programs) or those that would limit the ability to do exercise, and had no history of eating pathology or significant yoga experience. Those who completed baseline assessments for all study variables (N=75) were retained for complete case analysis. All participants were screened for eligibility and those eligible were enrolled at one of the two study sites (University of Connecticut, a rural public university, and Massachusetts General Hospital, an urban academic medical center) after completing written informed consent administered by study research personnel. The study protocol was approved by the Massachusetts General Hospital and University of Connecticut’s Institutional Review Boards.
Measures
Body Mass Index (BMI)
BMI (weight in kg/height in m2; Thompson, Pescatello, & Gordon, 2009) was calculated from height and weight using a professional scale with a stadiometer (e.g., Health o meter® 597KL, Pelstar, Bridgeville, IL) by a trained research assistant.
Internalized weight stigma (IWS)
The 11-item item Weight Bias Internalization Scale-Modified (WBIS-M; Pearl & Puhl 2014) assessed IWS. Consistent with prior work indicating improved reliability, the first item was eliminated (Hilbert et al., 2014). Items are ranked on a 7-point Likert scale ranging from 1 (Strongly Disagree) to 7 (Strongly Agree). The WBIS-M generates a global score of internalized weight stigma (e.g., “Because of my weight, I don’t feel like my true self”; “I wish I could drastically change my weight”). Higher WBIS-M scores indicate greater internalized weight stigma. The WBIS-M has demonstrated adequate internal consistency and predictive validity. In the present study, alpha was 0.92.
Intuitive eating
The 23-item Intuitive Eating Scale-2 (IES-2; Tylka & Kroon Van Diest, 2013) assessed intuitive eating. Items are ranked on a 5-point Likert scale ranging from 1 (Strongly Disagree) to 5 (Strongly Agree). The IES-2 comprises four subscales – Unconditional Permission to Eat (e.g., “I get mad at myself for eating something unhealthy”), Eating for Physical Rather than Emotional Reasons (e.g., “I find other ways to cope with stress and anxiety than by eating”), Reliance on Hunger and Satiety Cues (e.g., “I rely on my hunger signals to tell me when to eat”), and Body-Food Choice Congruence (e.g., “Most of the time, I desire to eat nutritious foods”) – as well as a global score, used here. Higher scores are indicative of a greater degree of intuitive eating. Prior research has indicated the IES-2 has strong internal consistency reliability and validity (Tylka & Kroon Van Dienst, 2015). In the present study, alpha was 0.90.
Statistical Analysis
Following review of construct distributions and computation of scale reliabilities, BMI was log-transformed to approximate normality for analysis (Sedgwick, 2012) given consistent positive skew in the general population (Flegal & Troiano, 2000; Johnson et al., 2015). Preliminary analyses were then conducted to examine differences in IWS, inituitive eating, or BMI by categorical demographic variables using independent samples t-tests (study site, gender, ethnicity) and ANOVA (race). To facilitate meaningful comparisons by ethnicity given non-reporting by three participants, this variable was recorded as (1) Hispanic/Latino/a/x, (2) Non-Hispanic/Latino/x, excluding the non-reporters from analysis. For race given low frequency of some identities, this variable was recoded as Asian (1), Multiracial (2), White (3), and Other or Not Reported (4). Pearson’s correlations were used to assess associations between age and study constructs, and between IWS, intuitive eating, and BMI.
Age and gender were used as covariates in all subsequent regression analyses, given findings in preliminary analyses and known and/or implicated connections of these and related factors with IWS, intuitive eating, and BMI (Hales et al., 2018; Marvin-Dowle et al., 2018; Pearl & Puhl, 2018). Hierarchical regression analysis next probed the unique variance in BMI accounted for by IWS and intuitive eating after covarying for gender and age. Covariates were entered in step one, IWS in step two, and intuitive eating in step three.
Last, we tested whether intuitive eating moderated the association between IWS and BMI (i.e., IWS X intuitive eating -> BMI), using Hayes’ (2013) PROCESS macro, model 1. Per Hayes’ recommendation, this macro generates unstandardized estimates (beta; B). Thus, all reported statistics (SE, t, F, p-values, 95% confidence intervals) refer to the model computed with unstandardized (B) estimates. However, to facilitate reader interpretation, standardized betas (β) are also reported. IWS and intuitive eating were mean-centered prior to analysis to reduce multicollinearity per the recommendation of Aiken and West (1991). In the event of a significant interaction, a simple slopes analysis was conducted in PROCESS for M + − 1 SD of intuitive eating to determine the conditional effects of IWS on BMI.
Results
Participant characteristics
Sample characteristics can be viewed in Table 1. Participants were predominantly female (69%), non-Hispanic/Latino/a/x (87%), 4-year college educated (85%), and White (65%); all BMI categories were represented (19.03 – 39.39 kg/m2), with 43% with overweight or obesity. Mean levels of IWS in the current sample (2.66±1.33) are lower than those reported in a national online sample (3.36±1.51; Puhl et al 2018), and mean intuitive eating (3.37±0.63) was similar to an undergraduate sample (3.32±0.89; Linardon & Mitchell, 2017) and slightly lower than in a sample of women yoga practitioners (3.5±0.53; Dittmann & Freedman, 2009).
Table 1.
Sociodemographic sample characteristics
| Characteristics | Valid n | M (SD) or percentage |
|---|---|---|
| Age | 75 | 39.44 (14.04) |
| Body Mass Index (BMI; kg/m2) | 75 | 25.54 (4.57) |
| With overweight (BMI≥25, <30) | 20 | 26.7 |
| With obesity (BMI≥30) | 12 | 16.0 |
| Education | ||
| Some high school or college | 6 | 8.0 |
| 2-year college | 5 | 6.7 |
| 4-year college | 27 | 36.0 |
| Graduate school | 37 | 49.3 |
| Female | 52 | 69.3 |
| Non-Hispanic/Latino/a | 65 | 86.7 |
| Race | ||
| Asian | 10 | 13.3 |
| American Indian or Alaskan | ||
| Native | 1 | 1.3 |
| Multiracial | 9 | 12.0 |
| Other/undisclosed | 6 | 8.0 |
| White | 49 | 65.3 |
| Study Site | ||
| Rural public university | 31 | 41.3 |
| Urban medical school | 44 | 58.7 |
Note. Age and BMI are mean (standard deviation). All other data are n (%).
Tests examining demographic variation by study constructs are shown in Table 2. There were no differences among urban academic medical center research participants when compared to rural public university participants on IWS (p=.230), intuitive eating (p=.418), or BMI (p=.999). While men and women did not differ on IWS (p=.637) or intuitive eating scores (p=.862), findings revealed that men had a greater BMI than women (p=.014). There were no differences in by race or ethnicity in IWS (p=.371 and p=.505), intuitive eating (p=.140 and p=.850), or BMI (p=.449 and p=.317). Age was unrelated to IWS (r=−0.05, p=.501) or intuitive eating (r=.068, p=.562) yet was positively correlated with BMI (r=0.26, p=.027). Body mass index was positively associated with IWS (r=0.31, p=.008) and negatively associated with intuitive eating (r=−0.39, p=.001). IWS and intuitive eating were negatively associated with one another (r=−0.43, p<.001).
Table 2.
Baseline demographic comparisons for study constructs.
| Baseline Factors | t or F-test (df) | ||
|---|---|---|---|
|
| |||
| IWS | Intuitive Eating | BMI | |
| Site | t(73)=−1.21 | t(73)=0.82 | t(73)=0.002 |
| Gender | t(73)=−0.47 | t(73)=0.18 | t(73)=2.52* |
| Ethnicity | t(70)=0.67 | t(70)=0.19 | t(70)=−1.01 |
| Race | F(3,71)=1.06 | F(3,71)=1.88 | F(3,71)=0.89 |
p < .05. Internalized Weight Stigma (IWS), Body Mass Index (BMI).
IWS, intuitive eating, and BMI: Multivariate and Moderated Regression Analyses
Next, we tested the proportion of variance in BMI accounted for by IWS and intuitive eating after controlling for age and gender, using multiple regression analysis. Significant covariates are reported for step one only; detailed results can be viewed in Table 3. In step one, gender predicted BMI (p=.031). As anticipated, in steps two and three, respectively, IWS (ΔR2=0.10, p=.003) and intuitive eating (ΔR2=0.09, p=.004) each accounted for significant unique variance in BMI, total model F(4,70)=7.82, p<.001.
Table 3.
Regression models predicting Body Mass Index (BMI) from Internalized Weight Stigma (IWS) and Intuitive Eating, reporting unstandardized and standardized beta’s (β) and standard errors (SE)
| Predictor | Model 1 | Model 2 | Model 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| B | SE | β | t | B | SE | β | t | B | SE | β | t | |
| Age | 0.002 | 0.001 | 0.20 | 1.78† | 0.003 | 0.001 | 0.22 | 2.10* | 0.003 | 0.001 | 0.24 | 2.33* |
| Gender | −0.09 | 0.04 | −0.25 | −2.20* | −0.10 | 0.04 | −0.26 | −2.46* | −0.09 | 0.04 | −0.26 | −2.56* |
| IWS | 0.04 | 0.01 | 0.32 | 3.04** | 0.02 | 0.01 | 0.18 | 1.60 | ||||
| Intuitive Eating | −0.09 | 0.03 | −0.33 | −3.01** | ||||||||
| R squared | 0.117 | 0.219 | 0.309 | |||||||||
p<.05
p<.01
p<=.001
p<.10
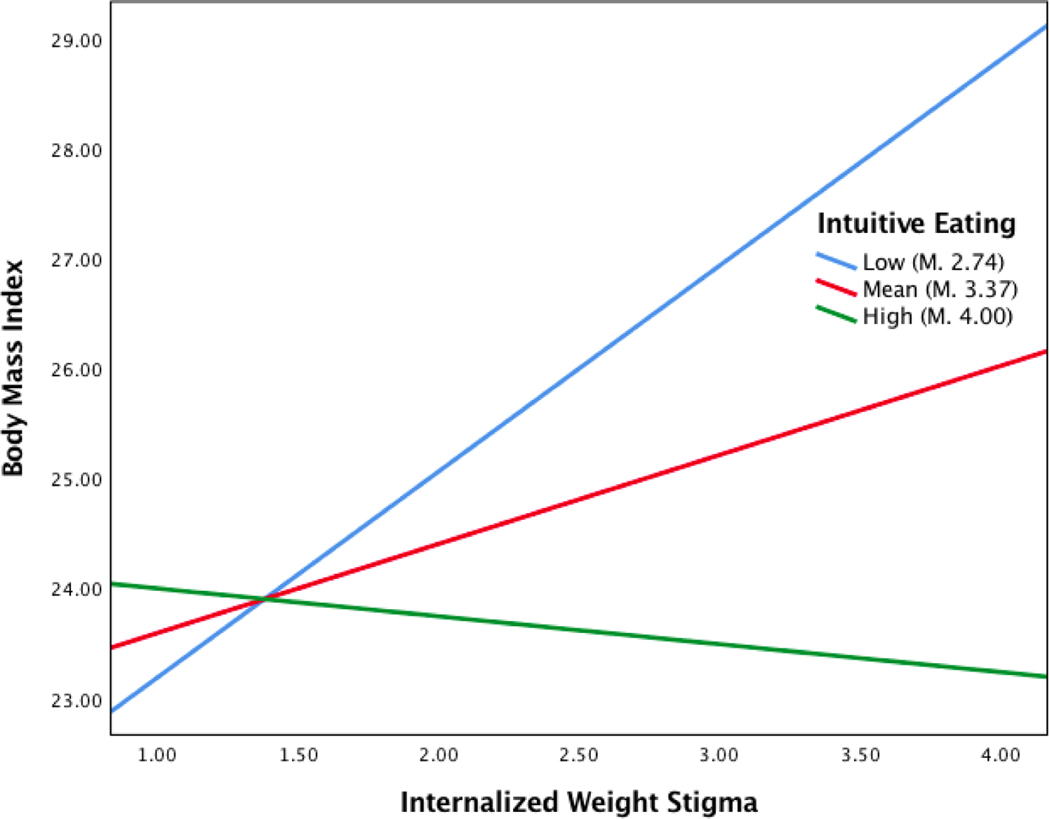
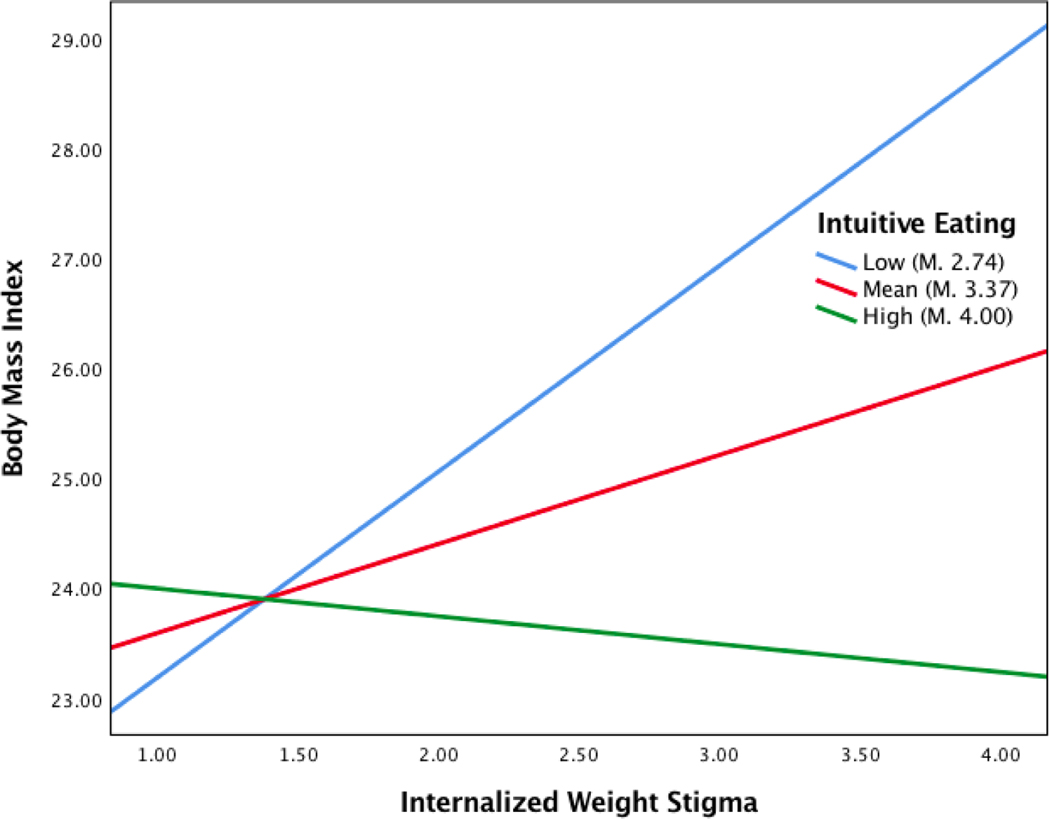
Last, PROCESS was used to test whether intuitive eating moderated the association between IWS and BMI (i.e., IWS X intuitive eating -> BMI). As shown in Table 4, controlling for covariates, intuitive eating (p=.004) moderated the relationship between IWS (p=.044) and BMI (overall model R2=.404, F(5,69)=9.37, p<.001). The interaction effect accounted for an added 9.5% of variance in BMI, F(1,69)=11.06, p=.001. The interaction was probed by testing the conditional effects of IWS at three levels of intuitive eating, one standard deviation below the mean, at the mean, and one standard deviation above the mean (see Figure 1). As demonstrated in Table 5, IWS was associated with BMI when intuitive eating was one standard deviation below the mean (p<.001) or at the mean (p=.044), but not when intuitive eating was one standard deviation above the mean (p=.506). Overall, the slope of the positive relationship between IWS and BMI decreased in magnitude with increasing intuitive eating, as shown by the differences by slope and significance of regression lines.
Table 4.
Moderated regression PROCESS model predicting Body Mass Index (BMI) from Internalized Weight Stigma (IWS) and Intuitive Eating, reporting unstandardized (B) and standardized beta’s (β), standard errors (SE), and 95% Confidence Intervals (CI).
| Predictor | B | SE | β | t | 95% CI | |
|---|---|---|---|---|---|---|
| Age | 0.003 | 0.001 | 0.27 | 2.87** | 0.001 | 0.01 |
| Gender | −0.09 | 0.03 | −0.26 | −2.73** | −0.16 | −0.03 |
| IWS | 0.03 | 0.01 | 0.21 | 2.05* | 0.001 | 0.05 |
| Intuitive Eating | −0.08 | 0.03 | −0.31 | −2.97** | −0.14 | −0.03 |
| IWS x Intuitive Eating | −0.06 | 0.02 | −0.30 | 3.33*** | −0.10 | −0.02 |
| R squared | 0.404 | |||||
p<.05
p<.01
p<=.001
Figure 1.
Simple slopes equations of the relationship between internalized weight stigma (IWS) and body mass index (BMI) when intuitive eating is low (one SD below the mean), mean, or high (one SD above the mean), demonstrating a buffering effect of intuitive eating on the association between IWS and BMI. Note: IWS and intuitive eating were mean centered for analysis, however to facilitate Figure interpretation, mean scores are represented. Similarly, although log-transformed BMI scores were used in analysis, raw BMI data are reported here.
Table 5.
Conditional effects of Internalized Weight Stigma (IWS) on Body Mass Index (BMI), reporting unstandardized (B) and standardized beta’s (β), standard errors (SE), and 95% Confidence Intervals (CI).
| Intuitive Eating | B | SE | β | t | 95%CI | |
|---|---|---|---|---|---|---|
| One SD below mean | 0.07 | 0.02 | 0.51 | 3.55** | 0.03 | 0.10 |
| At the mean | 0.03 | 0.01 | 0.21 | 2.05* | 0.001 | 0.05 |
| One SD above mean | −0.01 | 0.02 | −0.09 | −0.67 | −0.04 | 0.02 |
p<.05
p<.01
Discussion
This cross-sectional preliminary study is the first to examine an important factor – intuitive eating – that may weaken the association between internalized weight stigma (IWS) and body mass index (BMI). Our finding that high intuitive eating associated with lower BMI even among those reporting higher levels of IWS contributes to and unites the proliferating weight stigma and intuitive eating literatures, suggesting that the inverse link between intuitive eating and BMI may extend to those who experience higher IWS. The present study also replicates the extant literature on weight stigma and health, which observes strong and consistent linkages between IWS and greater BMI (Pearl & Puhl, 2018). Ours marks the first indication of these associations among stressed adults reporting low fruit and vegetable intake, a population at high risk of poor eating behaviors and chronic diseases and in critical need of intervention.
Participants in our study who reported greater intuitive eating evidenced no significant association between IWS and BMI, with nearly one-third of the variance in BMI accounted for by IWS, intuitive eating, and their interaction. Concerns have been expressed that intuitive eating may lead to weight gain given the lack of caloric restriction (Anglin, 2012; Fulvio, 2018). Such concerns run counter to the first principle of intuitive eating, Reject the Diet Mentality (including food restriction for the purpose of weight loss), which states that a focus on weight loss fundamentally impedes the process of learning intuitive eating (Tribole & Resch, 1995). Nonetheless, consistent with extant literature, participants in our study who reported greater intuitive eating were not more likely have a greater BMI, including those who reported the highest levels of IWS. Although our correlational findings in no way suggest that intuitive eating training may promote lower BMI, they do nevertheless provide some support for the idea that intuitive eating may not increase BMI. Additionally, recent cross-sectional evidence links intuitive eating to greater weight stability (linked to improved health outcomes when compared to weight instability or fluctuation; Bangalore et al., 2017; Montani et al., 2015) in comparison to associations of flexible and rigid dietary control with weight instability (Tylka et al., 2020). A fruitful area of continued investigation is better understanding the temporality and causality of intuitive eating in relation to IWS, weight stability, and indices of cardiometabolic health using prospective population-based cohort studies and intervention research with randomized and controlled designs.
Due to the cross-sectional design, our results can alternately be interpreted as supporting the equally plausible hypothesis that IWS may moderate the association between intuitive eating and BMI (i.e., Intuitive eating X IWS -> BMI), with the association between greater BMI and lower intuitive eating disappearing at low levels of IWS, and strongest at high levels of IWS. Thus, people reporting greater IWS may be least likely to intuitively eat when they have a high BMI, presenting a potential risk factor for poor eating behaviors and cardiometabolic health. This conceptualization is consistent with prior work in this area (Mensinger et al., 2016; Webb et al. 2015), as well as Linardon et al.’s (2021) alternate explanation for the meta-analytic link between intuitive eating and lower BMI. People with a lower BMI experience less weight stigma (Spahlholz et al., 2016) and may therefore be less likely to internalize weight stigma and to experience a desire to control their weight and shape. Because IWS, similar to disturbances in body image (Fairburn et al., 2003), is an established predictor of external food rules and dietary restraint (Pearl & Puhl, 2018), the potentially lower IWS among individuals with lower BMI could contribute to an increased likelihood of honoring endogenous hunger and satiety cues.
Importantly, while evidence suggests those with higher weight experience greater IWS, individuals across body weights can internalize weight stigma, and corresponding deficits in intuitive eating could prove a key risk pathway for the development of maladaptive eating behaviors and poor health sequelae (Pearl & Puhl, 2018). This interpretation is particularly resonant with a weight-inclusive approach to health (Tylka et al., 2014), as it offers a putative explanation for how IWS may indirectly and adversely influence biomarkers and cardiometabolic disease risk (i.e., through less intuitive, and hence healthy, eating) among people across weight categories. Given these alternate conceptualizations and implications for behavioral health and weight maintenance in stressed adults, the temporality, mechanisms, and causal associations between IWS, BMI, and intuitive eating over time warrant continued investigation in prospective and controlled intervention studies. Approaches such as Ecological Momentary Assessment (EMA) would be particularly well suited to reveal the momentary mechanisms between these factors.
Additionally related to the cross-sectional design, it is also possible that intuitive eating buffers the reverse link between BMI and greater IWS (BMI X intuitive eating -> IWS), such that people with higher BMIs who experience greater intuitive eating are less likely to develop or experience internalized weight stigma. Research suggests the IWS-BMI link may be cyclical (Pearl & Puhl, 2018; Spahlholz et al., 2016; Tomiyama, 2014). IWS is connected to poor health behaviors such as chronic dieting that may foster greater BMI over time, and higher BMI is associated in turn with greater likelihood of experiencing weight stigma. Individuals who experience weight stigma are at increased vulnerability for internalizing its effects (i.e., IWS) – in turn, potentially further increasing the risk of weight gain through poor health behaviors in a cyclical fashion. As such, it is possible that among people with higher BMI, intuitive eating could buffer against the effects of experienced weight stigma and IWS on poor eating behaviors, thereby protecting against increases in IWS-related weight gain and/or enhancing weight stability/maintenance (Van Dyke & Drinkwater, 2013). However, when we tested this alternate conceptualization in our sample – i.e., intuitive eating as a moderator of the link between BMI and greater IWS – there was only marginal evidence for its support (R-square increase due to interaction 0.033, F(1,69)=3.10, p=.083, model R2=0.257). Given implications for prevention and intervention development, future research would benefit from examining the cyclicity and temporality of interactions between these variables prospectively, using controlled designs that afford causal inference.
Relatedly, our pilot findings may plausibly be interpreted as preliminary support of the hypothesis that intuitive eating training could be a promising strategy to help individuals to lose weight or maintain weight loss in the context of existing or novel weight loss programs. As noted, present evidence does not rule out the possibility that intuitive eating may also (or instead) support or be relevant to weight management (Linardon et al., 2021). However, to retain fidelity with the intuitive eating approach, such an intepretation is discouraged. Intuitive eating training is “weight-inclusive,” and emphasizes the adoption of adaptive health behaviors and overall self-care without a focus on weight loss or diet, irrespective of one’s weight status (Tylka et al., 2014). Through improvements in behavioral health, it is also possible that intuitive eating training could implicitly prevent weight gain, foster adaptive weight loss, and ultimately promote weight stability, improving health (Tylka et al., 2020). However, any weight-related outcome would not be explicitly emphasized in the context of the intuitive eating intervention, which seeks to retrain participants often accustomed to a lifetime of dieting to embracing a new relationship with food and their bodies that is not contingent on the numbers on the weight loss scale (Tribole & Resch, 2012).
Weight-inclusive approaches to health are based on emerging evidence that health behaviors may play a stronger role in population health than body weight or BMI (Stefan et al., 2018) – as well as some evidence that “weight normative” medical discourses (i.e., viewing body weight as a determinant of health) and interventions (e.g., dieting) may increase weight discrimination, IWS, chronic dieting, and weight instability, and ultimately cause more harm than benefit (Tomiyama et al., 2018; Tylka et al., 2014). Evidence also shows that long-term weight loss outcomes among individuals in weight-normative programs, such as standard behavioral weight loss (SBWL), are less than optimal (Anderson et al., 2001; Brownell, 2010). No more than 20% of participants, for example, have been estimated to maintain weight loss one year following SWBL (Wing & Phelan, 2005). These poor rates of success, coupled with heightened rates of obesity and a culture that normalizes dieting in the USA, underscore the limitations of weight-normative approaches to health (Gagliardi, 2018; Hales et al., 2017). Thus, despite our assessment of BMI as an outcome, we have interpreted our findings in alignment with an intuitive eating and weight-inclusive approach to health.
Additionally, it is important to note that different approaches will likely be needed for different individuals. Within the context of HAES and intuitive eating interventions some individuals are less responsive (e.g., Cloutier-bergeron et al., 2019). Recent EMA findings also suggest that dietary restriction may be most challenging for those who experience heightened stress or emotional eating (Reichenberger et al., 2019). While stressed, our sample had relatively lower BMIs and no current psychiatric conditions, history of eating pathology, or other conditions known to impact appetite. Patient-centered care is needed to determine the most beneficial approach for each patient, as well as continued research to inform the evidence base and guide such care. Research examining moderators of the associations between intuitive eating, IWS, and health is needed using rigorous longitudinal and causal designs to identify whether and for whom intuitive eating may counter the effects of IWS on related distress and poor psychological, behavioral, and physical health.
Last, while the present study found preliminary evidence that the association between greater IWS and BMI is weakened among those with high intuitive eating (i.e., statistical moderation), one prospective study suggests IWS may be a vulnerability factor for decreased gains in intuitive eating during a lifestyle intervention (Mensinger, Calogero, & Tylka, 2016), implicating lower intuitive eating as a potential risk mechanism through which IWS may exert adverse effects on behavioral health. Thus, research would benefit from continued elucidation using prospective and controlled intervention designs as to whether intuitive eating acts as a mediator or a moderator, or both under different conditions, of the associations between IWS, health behaviors, and indicators of health.
Limitations
Several limitations warrant noting. First, the cross-sectional design was a helpful first step for demonstrating associations between IWS, BMI, and intuitive eating, but it was unable to prove the causality, directionality, or temporality of these relationships. Indeed, findings in no way suggest that intuitive eating causes low BMI, as it is equally possible that people with lower BMI and greater IWS are more likely to practice intuitive eating or to seek training in this approach than people with higher BMI, who may be more likely to actively attempt dieting or weight loss. Future research is required using prospective designs and randomized controlled interventions to rectify these limitations. Second, the sample size was very small to test statistical moderation. While our finding may thus be indicative of a large effect size, it is also quite possible that it is attributable to a Type I error. Future research is needed to test this finding in larger and more generalizable samples with designs that provide improved causal inference.
Third, the BMIs of those in our study ranged from normal to obesity, with 27% of participants with overweight and 16% with obesity. BMI positively skewed with a non-normal distribution. While similar to the distribution of BMI in the general population, this skew coupled with our small sample size increases the likelihood that our results are biased, making it difficult to draw conclusions about the meaning of our results given the relatively smaller number of participants with higher BMI. To help address this limitation, we log-transformed BMI prior to analysis, although results must still be viewed as highly preliminary and interpreted with significant caution. Future research is necessary that uses larger and clinical samples to attempt replication of our findings and improve inference and generalizability. Indeed, associations between intuitive eating and body image may differ by BMI category (Keirns & Hawkins, 2019), underscoring the importance of sampling a broader range of BMIs to examine these effects both within and across body weight statuses.
Fourth, the sample selected for the parent study was intentionally screened to report high stress and low fruit/vegetable intake and to be free of conditions known to impact diet, including no engagement in dietary or weight loss programs, no history of eating pathology, and no current psychiatric conditions or medical conditions that may alter the ability to exercise. These criteria clearly limit the generalizability of our results to individuals who may be at greatest risk of developing IWS-related adverse sequelae. Indeed, those in our sample reported lower levels of IWS than have been reported in other samples. Still, our sample was selected due to its high probable risk of developing chronic diseases and extends the literature on intuitive eating with college student samples, strengths that partially counteract these limitations. Future research is clearly needed with population, clinical, and community-based samples to assess replicability and improve generalizability.
Fifth, the sample primarily comprised White, non-Hispanic/Latino/a/x, and 4-year college-educated women, limiting generalizability of results to Black, Indigenous, and People of Color, those of Hispanic/Latino/a/x descent, those with diverse educational experiences, and men. Sixth, sexual orientation and gender identity were not assessed, limiting our ability to characterize the sample on these important dimensions. Future research should incorporate and rigorously apply plans for inclusion of diverse samples into the earliest stages of the research design process. Such work would benefit from considering the intersectionality of weight stigma and internalization with other forms of multilevel social identity stigma and minority stress (e.g., related to race, sexual orientation, or gender) as well as other health-related stigmas (e.g., cancer, HIV/AIDS, psychiatric conditions) in relation to intuitive eating and psychological, behavioral, and metabolic health.
Concluding remarks
Our findings with stressed adults reporting low fruit and vegetable intake suggest that greater intuitive eating may be associated with lower BMI even among individuals who experience greater IWS. This preliminary finding contributes to the burgeoning literatures on weight stigma and intuitive eating and, pending further research, implicates intuitive eating as a potential intervention target to prevent or combat the adverse effects of IWS on poor behavioral health. While our pilot findings are at best hypothesis-generating given the cross-sectional design and noted limitations, they support the need for continued and more rigorous research to attempt replication and better understand the observed associations between IWB, intuitive eating, and BMI in relation to health. Such research would benefit from considering these linkages in the context of structural, interpersonal, and biopsychosocial health determinants and indicators that may modify the observed associations over time (e.g., built environment, access to resources, varied forms of stigma, trauma, psychiatric disorders, loss of control eating, weight instability, diverse weight statuses).
Additional research is particularly needed among people who report heightened levels of IWS and other people and groups at heightened risk of chronic diseases including those who experience health disparities. Future research would also benefit from examining the temporality and causality of these associations in experimental and longitudinal population cohort studies as well as controlled interventions to elucidate whether intuitive eating mediates and/or moderates the IWS-BMI link, associations with indices of metabolic health more informative of health status than BMI, and the conditions under which, and for whom, these associations may differ.
Figure 2.
Simple slopes equations of the relationship between internalized weight stigma (IWS) and body mass index (BMI) when intuitive eating is low (one SD below the mean), mean, or high (one SD above the mean), demonstrating a buffering effect of intuitive eating on the association between IWS and BMI. Note: IWS and intuitive eating were mean centered for analysis, however to facilitate Figure interpretation, mean scores are represented. Similarly, although log-transformed BMI scores were used in analysis, raw BMI data are reported here.
Acknowledgments
Funding: This work was supported by the National Institutes of Health, National Institute of Complementary and Integrative Health (R34-AT007197) and National Heart, Lung, and Blood Institute (T32 HL076134).
Ethics approval:
The study was approved by the Institutional Review Boards of the Massachusetts General Hospital (#2013P001153) and the University of Connecticut (#H14–215).
Footnotes
Declaration of Interest: None
Disclosures: This study obtained ethics approval from the IRBs of Massachusetts General Hospital and the University of Connecticut (see ethical statement). All participants completed written informed consent prior to participating in the study.
Declaration of Interest Statement: None
Published works and works under review from this project have examined different research questions in the context of the longitudinal parent trial. This include three published papers that report on the effects of random assignment to varied duration of home yoga practice on stress levels (Greenberg et al., 2018), psychosocial mechanisms of reductions in stress (Park et al., 2020), and changes in dietary patterns and BMI (Braun et al., 2021). A final manuscript from the project (Braun et al., in press) reports on prospective changes in IWS and intuitive eating across the four study timepoints and associations with mindfulness and self-compassion, and does not examine statistical moderation.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions. Sage Publications. [Google Scholar]
- Anderson JW, Konz EC, Frederich RC, & Wood CL (2001). Long-term weight-loss maintenance: a meta-analysis of US studies. The American Journal of Clinical Nutrition, 74(5), 579–584. http://ajcn.nutrition.org/content/74/5/579.full [DOI] [PubMed] [Google Scholar]
- Anglin JC (2012). Assessing the effectiveness of intuitive eating for weight loss - Pilot study. Nutrition and Health, 21(2), 107–115. 10.1177/0260106012459994 [DOI] [PubMed] [Google Scholar]
- Bacon L. (2010). Health at every size: The surprising truth about your weight. BenBella Books, Inc. [Google Scholar]
- Bangalore S, Fayyad R, Laskey R, DeMicco DA, Messerli FH, & Waters DD (2017). Body-Weight Fluctuations and Outcomes in Coronary Disease. New England Journal of Medicine, 376(14), 1332–1340. 10.1056/nejmoa1606148 [DOI] [PubMed] [Google Scholar]
- Braun TD, Quinn DM, Stone A, Gorin AA, Ferrand J, Puhl RM, Sierra J, Tishler D, & Papasavas P. (2020). Weight bias, shame, and self-compassion: Risk/protective mechanisms of depression and anxiety in prebariatric surgery patients. Obesity, 28(10), 1974–1983. 10.1002/oby.2292. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Braun TD, Schifano ED, Finkelstein-Fox L, Park CL, Conboy LA, Deshpande R, Riley KE, Lazar SW (2021). Yoga participation associated with changes in dietary patterns and stress: A pilot study in stressed adults with poor diet. Complementary Therapies in Clinical Practice, 45, 101472. 10.1016/j.ctcp.2021.101472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun TD, Riley K, Kunicki J, Finkelstein-Fox L, Conboy LA, Park CL, Schifano ED, Abrantes AM, Lazar SW (in press). Internalized weight stigma and intuitive eating among stressed adults during a mindful yoga intervention: Associations with changes in mindfulness and self-compassion. Health Psychology and Behavioral Medicine. 10.1080/21642850.2021.1992282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownell KD (2010). The humbling experience of treating obesity: Should we persist or desist? Behaviour Research and Therapy, 48(8), 717–719. 10.1016/j.brat.2010.05.018 [DOI] [PubMed] [Google Scholar]
- Bruce LJ, & Ricciardelli LA (2016). A systematic review of the psychosocial correlates of intuitive eating among adult women. Appetite, 96, 454–472. 10.1016/j.appet.2015.10.012 [DOI] [PubMed] [Google Scholar]
- Cloutier-bergeron A, Provencher V, Mongeau L, & Paquette M. (2019). Does Health At Every Size ® fit all ? A group-based trajectory modeling of a non-diet intervention. Appetite, 143(August), 104403. 10.1016/j.appet.2019.104403 [DOI] [PubMed] [Google Scholar]
- Christoph M, Järvelä-Reijonen E, Hooper L, Larson N, Mason SM, & Neumark-Sztainer D. (2021). Longitudinal associations between intuitive eating and weight-related behaviors in a population-based sample of young adults. Appetite, 160, 105093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dittmann KA, & Freedman MR (2009). Body awareness, eating attitudes, and spiritual beliefs of women practicing yoga. Eating Disorders, 17(4), 273–292. 10.1080/10640260902991111 [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, & Shafran R. (2003). Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41(5), 509–528. http://www.sciencedirect.com/science/article/pii/S0005796702000888 [DOI] [PubMed] [Google Scholar]
- Flegal KM, & Troiano RP (2000). Changes in the distribution of body mass index of adults and children in the US population. International Journal of Obesity, 24(7), 807–818. 10.1038/sj.ijo.0801232 [DOI] [PubMed] [Google Scholar]
- Fulvio L. (2018). Q & A Friday – Intuitive Eating is Making Me Fat. Binge Eating Therapy. [Google Scholar]
- Gagliardi N. (2018). Dieting in the Long Sixties: Constructing the Identity of the Modern American Dieter. Gastronomica, 18(3), 66–81. 10.1525/gfc.2018.18.3.66 [DOI] [Google Scholar]
- Greenberg J, Braun TD, Schneider ML, Finkelstein-Fox L, Conboy LA, Schifano ED, Park C, & Lazar SW (2018). Is less more? A randomized comparison of home practice time in a mind-body program. Behaviour Research and Therapy, 111, 52–56. 10.1016/j.brat.2018.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert A, Baldofski S, Zenger M, Löwe B, Kersting A, & Braehler E. (2014). Weight bias internalization scale: psychometric properties and population norms. PloS one, 9(1), e86303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales CM, Carroll MD, Fryar CD, & Ogden CL (2017). Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. NCHS data brief, no 288. Hyattsville, MD: National Center for Health Statistics. NCHS Data Brief, 288, 1–8. https://pubmed.ncbi.nlm.nih.gov/26633046/ diakses 21 November 2020 [Google Scholar]
- Hales CM, Fryar CD, Carroll MD, Freedman DS, Aoki Y, & Ogden CL (2018). Differences in obesity prevalence by demographic characteristics and urbanization level among adults in the United States, 2013–2016. JAMA - Journal of the American Medical Association, 319(23), 2419–2429. 10.1001/jama.2018.7270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis. Guilford Press. [Google Scholar]
- Hazzard VM, Telke SE, Simone M, Anderson LM, Larson NI, & Neumark-Sztainer D. (2021). Intuitive eating longitudinally predicts better psychological health and lower use of disordered eating behaviors: findings from EAT 2010–2018. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 26(1), 287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert A, Baldofski S, Zenger M, Löwe B, Kersting A, & Braehler E. (2014). Weight bias internalization scale: psychometric properties and population norms. PloS one, 9(1), e86303. 10.1371/journal.pone.0086303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson W, Li L, Kuh D, & Hardy R. (2015). How has the age-related process of overweight or obesity development changed over time? Co-ordinated analyses of individual participant data from five United Kingdom birth cohorts. PLoS Medicine, 12(5), 1–20. 10.1371/journal.pmed.1001828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keirns NG, & Hawkins MAW (2019). The relationship between intuitive eating and body image is moderated by measured body mass index. Eating Behaviors, 33, 91–96. 10.1016/j.eatbeh.2019.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linardon J, & Mitchell S. (2017). Rigid dietary control, flexible dietary control, and intuitive eating: Evidence for their differential relationship to disordered eating and body image concerns. Eating Behaviors, 26, 16–22. 10.1016/j.eatbeh.2017.01.008 [DOI] [PubMed] [Google Scholar]
- Linardon J, Tylka TL, & Fuller-Tyszkiewicz M. (2021). Intuitive eating and its psychological correlates: A meta-analysis. International Journal of Eating Disorders, February, 1–26. 10.1002/eat.23509 [DOI] [PubMed] [Google Scholar]
- Linardon J. (2021). Positive body image, intuitive eating, and self‐ compassion protect against the onset of the core symptoms of eating disorders: A prospective study. International Journal of Eating Disorders. [DOI] [PubMed] [Google Scholar]
- Marvin-Dowle K, Kilner K, Burley V, & Soltani H. (2018). Differences in dietary pattern by maternal age in the born in bradford cohort: A comparative analysis. PLoS ONE, 13(12), 1–14. 10.1371/journal.pone.0208879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathieu J. (2009). What should you know about mindful and intuitive eating? Journal of the American Dietetic Association, 109(12), 1982–1987. 10.1016/j.jada.2009.10.023 [DOI] [PubMed] [Google Scholar]
- Mensinger JL, Calogero RM, & Tylka TL (2016). Internalized weight stigma moderates eating behavior outcomes in women with high BMI participating in a healthy living program. Appetite, 102, 32–43. 10.1016/j.appet.2016.01.033 [DOI] [PubMed] [Google Scholar]
- Montani JP, Schutz Y, & Dulloo AG (2015). Dieting and weight cycling as risk factors for cardiometabolic diseases: Who is really at risk? Obesity Reviews, 16(S1), 7–18. 10.1111/obr.12251 [DOI] [PubMed] [Google Scholar]
- Park CL, Finkelstein-Fox L, Sacco SJ, Braun TD, & Lazar S. (2020). How does yoga reduce stress? A clinical trial testing psychological mechanisms. Stress and Health, March. 10.1002/smi.2977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl RL, & Puhl RM (2018). Weight bias internalization and health: A systematic review. Obesity Reviews, 19(8), 1141–1163. 10.1111/obr.12701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl Rebecca L, & Puhl RM (2016). The distinct effects of internalizing weight bias: An experimental study. Body Image, 17, 38–42. 10.1016/j.bodyim.2016.02.002 [DOI] [PubMed] [Google Scholar]
- Pearl RL & Puhl RM (2014). Measuring internalized weight attitudes across body weight categories: Validation of the Modified Weight Bias Internalization Scale Body Image, 11, 89–92, 10.1016/j.bodyim.2013.09.005 [DOI] [PubMed] [Google Scholar]
- Puhl RM, & Heuer C. a. (2009). The stigma of obesity: a review and update. Obesity (Silver Spring, Md.), 17(5), 941–964. 10.1038/oby.2008.636 [DOI] [PubMed] [Google Scholar]
- Puhl RM, Himmelstein MS, & Quinn DM (2018). Internalizing weight stigma: Prevalence and sociodemographic considerations in US adults. Obesity, 26(1), 167–175. 10.1002/oby.22029 [DOI] [PubMed] [Google Scholar]
- Quansah DY, Gilbert L, Gross J, Horsch A, & Puder JJ (2021). Intuitive eating is associated with improved health indicators at 1-year postpartum in women with gestational diabetes mellitus. Journal of health psychology, 26(8), 1168–1184. [DOI] [PubMed] [Google Scholar]
- Reichenberger J, Smyth JM, Kuppens P, & Blechert J. (2019). “I will fast … tomorrow”: Intentions to restrict eating and actual restriction in daily life and their person-level predictors. Appetite, 140(April), 10–18. 10.1016/j.appet.2019.04.019 [DOI] [PubMed] [Google Scholar]
- Richards PS, Crowton S, Berrett ME, Smith MH, & Passmore K. (2017). Can patients with eating disorders learn to eat intuitively? A 2-year pilot study. Eating Disorders, 25(2), 99–113. 10.1080/10640266.2017.1279907 [DOI] [PubMed] [Google Scholar]
- Rubino F, Puhl RM, Cummings DE, Eckel RH, Ryan DH, Mechanick JI, Nadglowski J, Ramos Salas X, Schauer PR, Twenefour D, Apovian CM, Aronne LJ, Batterham RL, Bertoud H-R, Boza C, Busetto L, Dicker D, De Grooth M, Eisenberg D, … Dixon JB (2020). Joint international consensus statement for ending stigma of obesity. Nature Medicine. 10.1038/s41591-020-0803-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schvey NA, & Roberto CA (2013). Clinical correlates of the Weight Bias Internalization Scale in overweight adults with binge and purge behaviours. Advances in Eating Disorders, 1(3), 213–223. 10.1080/21662630.2013.794523 [DOI] [Google Scholar]
- Sedgwick P. (2012). Log transformation of data. BMJ, 345, 1–2. 10.1136/bmj.e6727 [DOI] [Google Scholar]
- Spahlholz J, Baer N, König HH, Riedel-Heller SG, & Luck-Sikorski C. (2016). Obesity and discrimination - a systematic review and meta-analysis of observational studies. Obesity Reviews, 17(1), 43–55. 10.1111/obr.12343 [DOI] [PubMed] [Google Scholar]
- Stefan N, Häring HU, & Schulze MB (2018). Metabolically healthy obesity: the low-hanging fruit in obesity treatment? The Lancet Diabetes and Endocrinology, 6(3), 249–258. 10.1016/S2213-8587(17)30292-9 [DOI] [PubMed] [Google Scholar]
- Thompson WR, Pescatello LS, & Gordon NF (Eds.). (2009). ACSM’s Guidelines for Exercise Testing and Prescription (8th ed.). Lippincott Williams & Wilkins. [Google Scholar]
- Tomiyama AJ, Carr D, Granberg EM, Major B, Robinson E, Sutin AR, & Brewis A. (2018). How and why weight stigma drives the obesity “epidemic” and harms health. BMC Medicine, 16(1), 1–6. 10.1186/s12916-018-1116-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tribole E, & Resch E. (1995). Intuitive eating: a recovery book for the chronic dieter: rediscover the pleasures of eating and rebuild your body image. St. Martin’s Griffin. [Google Scholar]
- Tribole E, & Resch E. (2012). Intuitive Eating (3rd ed.). St. Martin’s Press. [Google Scholar]
- Tylka TL (2006). Development and psychometric evaluation of a measure of intuitive eating. Journal of Counseling Psychology, 53(2), 226–240. 10.1037/0022-0167.53.2.226 [DOI] [Google Scholar]
- Tylka TL, Annunziato RA, Burgard D, Danielsdottir S, Shuman E, Davis C, & Calogero RM (2014). The weight inclusive versus the weight normative approach to health: Evaluating the evidence for prioritising wellbeing over weight loss. Journal of Obesity, 18. 10.1155/2014/983495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tylka TL, Calogero RM, & Daníelsdóttir S. (2020). Intuitive eating is connected to self-reported weight stability in community women and men. Eating Disorders, 28(3), 256–264. 10.1080/10640266.2019.1580126 [DOI] [PubMed] [Google Scholar]
- Tylka TL, & Kroon Van Dienst AM (2015). Protective Factors. In Smolak L. & Levine MP (Eds.), The Wiley Handbook of Eating Disorders (First, pp. 430–444). John Wiley & Sons, Ltd. [Google Scholar]
- Tylka TL, & Kroon Van Diest AM (2013). The Intuitive Eating Scale-2: item refinement and psychometric evaluation with college women and men. Journal of Counseling Psychology, 60(1), 137–153. 10.1037/a0030893 [DOI] [PubMed] [Google Scholar]
- Van Dyke N, & Drinkwater EJ (2013). Review Article Relationships between intuitive eating and health indicators: literature review. Public Health Nutrition, 13, 1–10. 10.1017/S1368980013002139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren JM, Smith N, & Ashwell M. (2017). A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: Effectiveness and associated potential mechanisms. Nutrition Research Reviews, 30(2), 272–283. 10.1017/S0954422417000154 [DOI] [PubMed] [Google Scholar]
- Webb JB, & Hardin AS (2015). An integrative affect regulation process model of internalized weight bias and intuitive eating in college women. Appetite, 102, 60–69. 10.1016/j.appet.2016.02.024 [DOI] [PubMed] [Google Scholar]
- Wellman JD, Araiza AM, Newell EE, & McCoy SK (2018). Weight stigma facilitates unhealthy eating and weight gain via fear of fat. Stigma and Health, 3(3), 186–194. 10.1037/sah0000088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, & Phelan S. (2005). Long-term weight loss maintenance. The American Journal of Clinical Nutrition, 82(1 Suppl), 222–225. 10.1093/ajcn/82.1.222s [DOI] [PubMed] [Google Scholar]