Abstract
Background
Loss of olfactory function is well recognised as a symptom of COVID‐19 infection, and the pandemic has resulted in a large number of individuals with abnormalities in their sense of smell. For many, the condition is temporary and resolves within two to four weeks. However, in a significant minority the symptoms persist. At present, it is not known whether early intervention with any form of treatment (such as medication or olfactory training) can promote recovery and prevent persisting olfactory disturbance. This is an update of the 2021 review with four studies added.
Objectives
1) To evaluate the benefits and harms of any intervention versus no treatment for people with acute olfactory dysfunction due to COVID‐19 infection.
2) To keep the evidence up‐to‐date, using a living systematic review approach.
Search methods
The Cochrane ENT Information Specialist searched the Cochrane ENT Register; Central Register of Controlled Trials (CENTRAL); Ovid MEDLINE; Ovid Embase; Web of Science; ClinicalTrials.gov; ICTRP and additional sources for published and unpublished trials. The date of the latest search was 20 October 2021.
Selection criteria
We included randomised controlled trials (RCTs) in people with COVID‐19 related olfactory disturbance, which had been present for less than four weeks. We included any intervention compared to no treatment or placebo.
Data collection and analysis
We used standard Cochrane methods. Our primary outcomes were the presence of normal olfactory function, serious adverse effects and change in sense of smell. Secondary outcomes were the prevalence of parosmia, change in sense of taste, disease‐related quality of life and other adverse effects (including nosebleeds/bloody discharge). We used GRADE to assess the certainty of the evidence for each outcome.
Main results
We included five studies with 691 participants. The studies evaluated the following interventions: intranasal corticosteroid sprays, intranasal corticosteroid drops, intranasal hypertonic saline and zinc sulphate.
Intranasal corticosteroid spray compared to no intervention/placebo
We included three studies with 288 participants who had olfactory dysfunction for less than four weeks following COVID‐19.
Presence of normal olfactory function
The evidence is very uncertain about the effect of intranasal corticosteroid spray on both self‐rated recovery of olfactory function and recovery of olfactory function using psychophysical tests at up to four weeks follow‐up (self‐rated: risk ratio (RR) 1.19, 95% confidence interval (CI) 0.85 to 1.68; 1 study; 100 participants; psychophysical testing: RR 2.3, 95% CI 1.16 to 4.63; 1 study; 77 participants; very low‐certainty evidence).
Change in sense of smell
The evidence is also very uncertain about the effect of intranasal corticosteroid spray on self‐rated change in the sense of smell (at less than 4 weeks: mean difference (MD) 0.5 points lower, 95% CI 1.38 lower to 0.38 higher; 1 study; 77 participants; at > 4 weeks to 3 months: MD 2.4 points higher, 95% CI 1.32 higher to 3.48 higher; 1 study; 100 participants; very low‐certainty evidence, rated on a scale of 1 to 10, higher scores mean better olfactory function). Intranasal corticosteroids may make little or no difference to the change in sense of smell when assessed with psychophysical testing (MD 0.2 points, 95% CI 2.06 points lower to 2.06 points higher; 1 study; 77 participants; low‐certainty evidence, 0‐ to 24‐point scale, higher scores mean better olfactory function).
Serious adverse effects
The authors of one study reported no adverse effects, but their intention to collect these data was not pre‐specified so we are uncertain if these were systematically sought and identified. The remaining two studies did not report on adverse effects.
Intranasal corticosteroid drops compared to no intervention/placebo
We included one study with 248 participants who had olfactory dysfunction for ≤ 15 days following COVID‐19.
Presence of normal olfactory function
Intranasal corticosteroid drops may make little or no difference to self‐rated recovery at > 4 weeks to 3 months (RR 1.00, 95% CI 0.89 to 1.11; 1 study; 248 participants; low‐certainty evidence). No other outcomes were assessed by this study.
Data on the use of hypertonic saline nasal irrigation and the use of zinc sulphate to prevent persistent olfactory dysfunction are included in the full text of the review.
Authors' conclusions
There is very limited evidence available on the efficacy and harms of treatments for preventing persistent olfactory dysfunction following COVID‐19 infection. However, we have identified a number of ongoing trials in this area. As this is a living systematic review we will update the data regularly, as new results become available.
Plain language summary
Interventions for the prevention of persistent smell disorders (olfactory dysfunction) after COVID‐19 infection
Why this is important
COVID‐19 has been found to cause problems with the sense of smell. Sometimes this is a reduction in the ability to smell things, and sometimes it is a complete loss of the sense of smell. For many people this recovers in a short time, but for others it may last for weeks or months. This review considers whether there are treatments that people might take as soon as they have lost their sense of smell (within four weeks of the symptoms starting), to try and stop this becoming a long‐standing problem.
How we identified and assessed the evidence
We searched for all relevant studies in the medical literature to summarise the results. We also looked at how certain the evidence was, considering things like the size of the studies and how they were carried out. Based on this, we classed the evidence as being of very low, low, moderate or high certainty.
What we found
We found five studies that had been completed.
Intranasal corticosteroids compared to no treatment
Three studies looked at this treatment.
Nasal corticosteroid spray might make little or no difference to the sense of smell when measured with specific tests (rather than when asking people about their sense of smell).
The rest of the evidence was of very low certainty, so we do not know whether a nasal corticosteroid spray is better or worse than no treatment at:
‐ helping the sense of smell get back to normal (either people feeling that their sense of smell is back to normal, or having a normal sense of smell according to specific tests);
‐ making people feel that their sense of smell has improved;
‐ causing any unwanted side effects.
Intranasal corticosteroid drops compared to placebo (dummy treatment)
One study looked at this treatment.
Intranasal corticosteroid drops might not make any difference to the number of people who think their sense of smell has recovered at 30 days.
We did find a number of other studies that are being carried out, but no results from these studies were available yet to be included in this review.
What this means
We do not know whether using a nasal corticosteroid spray or nasal drops has any benefit in preventing longer‐term loss of the sense of smell that is related to COVID‐19, or whether they may cause any harm. This review is a 'living systematic review' ‐ meaning that we will keep checking for new studies that might be relevant, and the review will be continually updated when any extra results are available.
How up‐to‐date is this review?
The evidence in this Cochrane Review is current to October 2021.
Summary of findings
Summary of findings 1. Intranasal steroid spray compared to no intervention/placebo for the prevention of persistent post‐COVID‐19 olfactory dysfunction.
| Intranasal steroid spray compared to no intervention/placebo for the prevention of persistent post‐COVID‐19 olfactory dysfunction | ||||||
| Patient or population: people with olfactory dysfunction for less than 4 weeks following COVID‐19 infection Setting: hospitalised or in isolation at home; studies conducted in Egypt, Iran and Turkey Intervention: intranasal steroid spray Comparison: no intervention or placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no intervention/placebo | Risk with intranasal steroid spray | |||||
| Presence of normal olfactory function Assessed by participants as a score of 10 on a VAS (range 0 to 10) ≤ 4 weeks |
Study population | RR 1.19 (0.85 to 1.68) | 100 (1 RCT) | ⊕⊝⊝⊝ very low1,2 | — | |
| 520 per 1000 | 619 per 1000 (442 to 874) | |||||
| Presence of normal olfactory function Assessed with psychophysical testing (Iran‐Smell Identification Test (Iran‐SIT), score ≥ 19/24) ≤ 4 weeks |
Study population | RR 2.31 (1.16 to 4.64) | 77 (1 RCT) | ⊕⊝⊝⊝ very low3,4 | — | |
| 211 per 1000 | 486 per 1000 (244 to 977) | |||||
| Serious adverse events | One study reported that no adverse events were identified during the study | Not estimable | 77 (1 RCT) |
⊕⊝⊝⊝ very low3,5 | — | |
| Change in sense of smell Assessed by participants (VAS, higher score = better, range 0 to 10) ≤ 4 weeks |
The mean change in sense of smell was 5.7 points | MD 0.5 points lower (1.38 lower to 0.38 higher) | — | 77 (1 RCT) | ⊕⊝⊝⊝ very low3,6 | No minimally important difference has been reported. We considered that a difference of 0.5 points was unlikely to be important to participants. |
| Change in sense of smell Assessed by participants (VAS, higher score = better, scale 0 to 10) > 4 weeks to 3 months |
The mean score for sense of smell was 6.1 points at 30 days of follow‐up | MD 2.4 points higher (1.32 higher to 3.48 higher) | — | 100 (1 RCT) | ⊕⊝⊝⊝ very low7,8 | No minimally important difference has been reported. We considered that a difference of 2.4 points may be important to participants. |
| Change in sense of smell Assessed with psychophysical testing (Iran‐SIT, higher = better, scale 0 to 24) ≤ 4 weeks |
The mean change in sense of smell was 7.9 points | MD 0.2 points higher (2.06 lower to 2.46 higher) | — | 77 (1 RCT) | ⊕⊕⊝⊝ low3,8 | No minimally important difference for the Iran‐SIT has been reported. We considered that a difference of 0.2 points was unlikely to be important to participants. |
| Prevalence of parosmia | This was not assessed or reported by any of the included studies. | |||||
| Change in sense of taste | This was not assessed or reported by any of the included studies. | |||||
| Disease‐related quality of life | This was not assessed or reported by any of the included studies. | |||||
| Other adverse effects | One study reported that no adverse events were identified during the study. | Not estimable | 77 (1 RCT) |
⊕⊝⊝⊝ very low3,5 | — | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; RR: risk ratio; VAS: visual analogue scale | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Serious risk of bias due to lack of blinding of participants, personnel or outcome assessors.
2Very serious imprecision as sample size smaller than optimal information size (take as 400 participants, as a rule of thumb) and confidence interval includes both potential harm and considerable benefit.
3Serious risk of bias due to unclear randomisation, blinding of outcome assessors, potential for selective reporting and other biases.
4Very serious imprecision as sample size is smaller than the optimal information size (taken as 400 participants, as a rule of thumb) and the confidence interval for the effect includes the potential for substantial benefit (766 more people per 1000) and a trivial benefit (36 more people per 1000)
5Very serious imprecision as sample size is smaller than the optimal information size (taken as 400 participants, as a rule of thumb) and an effect size cannot be calculated.
6Very serious imprecision as sample size is smaller than the optimal information size (taken as 400 participants, as a rule of thumb) and the confidence interval for the effect includes the potential for considerable harm from the intervention (up to 1.38 points lower) as well as a trivial benefit (up to 0.38 points higher).
Summary of findings 2. Intranasal steroid drops compared to placebo for the prevention of persistent post‐COVID‐19 olfactory dysfunction.
| Intranasal steroid drops compared to placebo for the prevention of persistent post‐COVID‐19 olfactory dysfunction | ||||||
| Patient or population: participants with olfactory dysfunction following COVID‐19 for ≤ 15 days Setting: outpatient departments of 2 hospitals in Iran Intervention: intranasal steroid drops Comparison: placebo (isotonic saline drops) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with intranasal steroid drops | |||||
| Presence of normal olfactory function Assessed by participants > 4 weeks to 3 months |
Study population | RR 1.00 (0.89 to 1.11) | 248 (1 RCT) | ⊕⊕⊝⊝ low1,2 | The authors do not report how participants judged the presence of normal olfactory function. | |
| 840 per 1000 | 840 per 1000 (748 to 932) | |||||
| Serious adverse effects | These were not assessed or reported by any of the included studies. | |||||
| Change in sense of smell | This was not assessed or reported by any of the included studies. | |||||
| Prevalence of parosmia | This was not assessed or reported by any of the included studies. | |||||
| Change in sense of taste | This was not assessed or reported by any of the included studies. | |||||
| Disease‐related quality of life | This was not assessed or reported by any of the included studies. | |||||
| Other adverse effects | These were not assessed or reported by any of the included studies. | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Serious risk of bias due to unclear risk across multiple domains, including randomisation and allocation, selective reporting and other biases (due to lack of detail in reporting of methods).
2Serious imprecision as sample size fails to meet optimal information size (taken as 400 participants, as a rule of thumb).
Background
Description of the condition
Loss of olfactory function (the sense of smell) emerged as a marker of COVID‐19 infection in March 2020 (Hopkins 2020a). Since that time, it has become established that this is a cardinal symptom of COVID‐19 infection (Menni 2020), with a high predictive value (Gerkin 2020). This usually takes the form of complete or partial loss of olfactory function (anosmia and hyposmia respectively) (Lechien 2020).
Olfactory dysfunction, through loss (quantitative changes) or distortion (qualitative changes) of smell, is a debilitating condition with a variety of causes and has a major impact on quality of life (Croy 2014; Erskine 2020; Philpott 2014). It also has safety implications, through the inability to detect odours that may signal danger (such as smoke, gas or spoilt food). Through its intimate relationship with the sense of taste, the disturbance of olfactory function can also hamper the ability to enjoy food.
Post‐infectious olfactory dysfunction (PIOD) is one of the most common causes of olfactory dysfunction, representing up to 20% of all cases in specialist olfactory clinics (Cain 1988; Damm 2004; Seiden 2001). Many viruses have been implicated in PIOD, including the coronavirus family. However, the prominence of SARS‐CoV‐2 (which causes COVID‐19) as a causative agent has been notable, and can perhaps be attributed to the spotlight created by it being the cause of a pandemic.
Accurate estimates of the prevalence of olfactory dysfunction resulting from COVID‐19 are difficult to obtain, and may vary according to the clinical presentation of the disease (which ranges from mild, or relatively asymptomatic, to serious complications requiring intensive care). A recent systematic review identified an overall prevalence of smell loss of 43%, however the authors noted high variation between the estimates from different studies (von Bartheld 2020). Another systematic review showed a prevalence of 62% across the range of studies included (Rocke 2020). A large European cohort, which included hospitalised individuals with mild‐moderate symptoms, as well as individuals who did not require hospital treatment, reported the prevalence of olfactory dysfunction to be 85.6% (Lechien 2020). The majority of individuals included in this study reported anosmia, with a minority reporting hyposmia (20.4%).
The incidence of anosmia or olfactory dysfunction related to COVID‐19 appears to vary across the world, with studies from the USA and Europe typically demonstrating much higher incidence than those from Asia (Meng 2020; von Bartheld 2020). A study from Wuhan, China reported abnormalities of olfactory function in only 5.1% of their cohort (214 patients, with both severe and mild forms of the disease) (Mao 2020). It is not clear why this may be. Gender and age have also been suggested as possible effect modifiers, with some reviews suggesting preponderance in females (Meng 2020), and others suggesting an increased incidence in younger age groups (Fuccillo 2020).
The incidence of olfactory dysfunction may also vary depending on the method used to diagnose it. Studies that used self‐reported symptoms of loss of smell identified a lower prevalence than those that utilised some form of objective assessment (von Bartheld 2020). It is well recognised that, for healthy individuals, self‐rating of the sense of smell may correlate poorly with scores achieved on psychophysical testing (Landis 2003; Lötsch 2019). Correlation is better for those who report olfactory dysfunction (particularly anosmia), but on an individual level there is still considerable variation between the severity of the reported loss, and that identified with psychophysical tests (Welge‐Luessen 2005). With larger numbers reporting COVID‐19 symptoms in general, the data collected by the COVID tracker app is more likely to reflect the prevalence of olfactory dysfunction in the non‐hospitalised population (Menni 2020).
A further complication in obtaining accurate estimates of prevalence is the variety of data sources that are available. Studies conducted in a hospitalised population may present very different estimates to those where data are gathered from internet‐based surveys. This may reflect genuine differences in the presence of olfactory dysfunction in these varied populations, different methods of ascertaining olfactory function, or potentially a different preponderance to report symptoms. Internet‐based surveys may have a greater propensity for responder bias than other cross‐sectional studies ‐ those who have symptoms may be more likely to participate or complete the required data, resulting in inflated estimates of prevalence. However, some prospective series have also identified a high prevalence of olfactory dysfunction (Spinato 2020)
Other symptoms of olfactory dysfunction include phantosmia (qualitative dysfunction in the absence of an odour, or 'olfactory hallucinations') and parosmia (distorted perception of an odour stimulus) (Hummel 2016). A recent survey of individuals with COVID‐19 indicated that these symptoms occurred in fewer than 10% in the short term (Parma 2020). However, longer‐term follow‐up may demonstrate further problems at a later stage (Gerkin 2020), and reports of persisting parosmia as a consequence of COVID‐19 are increasing (Hopkins 2020b; Ohla 2021).
The exact mechanism by which the SARS‐CoV‐2 virus triggers olfactory dysfunction remains unclear (reviewed in Butowt 2020). Many viruses cause conductive olfactory impairment, with inflammation, nasal congestion and rhinorrhoea preventing detection of odours during the acute phase of the infection. These symptoms are not as common in COVID‐19 and, when present, do not correlate well with the degree of olfactory dysfunction (Parma 2020). Symptoms may also be caused by direct damage to, or death of, olfactory neurons or cells within the olfactory bulb. However, olfactory neurons lack ACE2 receptors (which facilitate viral entry to cells) and the rapid recovery for most individuals with COVID‐19 related smell loss makes this less likely. Infection of supporting cells (sustentacular cells) within the olfactory epithelium has been reported (reviewed in Bilinska 2020). These cells play a critical role in supporting the function of olfactory neurons, and their infection may consequently have an adverse effect on olfactory processing.
For many individuals with COVID‐19 related olfactory dysfunction, the condition is temporary and they recover a normal sense of smell relatively quickly (Chary 2020; Klopfenstein 2020). Complete recovery by two weeks was reported for most people (96.7%) in the study by Lechien 2020. A second case series of individuals with mild coronavirus symptoms found that 89% had complete or partial recovery of olfactory function by four weeks from the onset of the disease (Boscolo‐Rizzo 2020). However, for some individuals the problem persists. Some studies report a much higher prevalence of persisting olfactory loss, despite resolution of other COVID‐19 symptoms. Data from the Global Consortium of Chemosensory Research indicates that up to 50.7% of individuals may have persisting olfactory dysfunction at up to 40 days from the onset of COVID‐19 (Gerkin 2020). It remains unclear why some individuals experience longer‐lasting olfactory deficits. This may be due to differing extents of damage (as suggested by Butowt 2020), or different mechanisms for olfactory loss (Hopkins 2020c; Saussez 2020). Differing features of COVID‐19 related smell loss may include a potential impact on true gustatory function, as well as a greater severity of olfactory loss itself (Huart 2020); many larger studies are limited by the reliance on self‐reporting, so this is more difficult to corroborate.
This review is one of a pair that consider the effect of interventions to prevent or treat persisting olfactory dysfunction following COVID‐19. For this review, we considered interventions that may be used in the acute phase (less than four weeks since diagnosis), aiming to prevent individuals from developing persisting olfactory dysfunction. For the companion review ('Interventions for the treatment of persisting olfactory dysfunction following COVID‐19'; O'Byrne 2022), we considered treatment for individuals who already have persisting olfactory dysfunction at four weeks (or longer) following a diagnosis of COVID‐19.
Description of the intervention
As COVID‐19 related persisting olfactory dysfunction is a relatively new condition, there are no established interventions that are known to prevent it. However, a number of interventions have been used for other post‐viral causes of anosmia. It is possible that early intervention for those with short‐lived symptoms could help to prevent the development of persisting, long‐term olfactory dysfunction.
Corticosteroids are commonly prescribed for olfactory dysfunction ‐ these are typically administered locally as a nasal spray, drops or rinse for conductive causes of olfactory loss ‐ where the nasal cavity is blocked, or partially blocked, by inflammation and oedema. Systemic (oral) corticosteroids may also be used, particularly in cases where no conductive cause is identified.
Olfactory training is also frequently suggested for reduced or absent sense of smell ‐ this involves regular exposure to a number of specific odours. It can be performed in a variety of different ways, using household items or essential oils.
A large number of other interventions have been used for PIOD and may therefore be of use for post‐COVID‐19 olfactory dysfunction. A variety of vitamins, minerals and nutritional supplements have been proposed to be of benefit ‐ either taken as an oral supplement, or in some instances used intranasally (such as intranasal vitamin A drops). Glutamate antagonists and xanthine derivatives are used occasionally in the treatment of post‐viral olfactory dysfunction and may therefore be assessed in relation to COVID‐19. Trials of acupuncture have also taken place.
Clinical trials are ongoing to assess a variety of interventions for the treatment of COVID‐19. These include antivirals, such as remdesivir, and monoclonal antibodies. It is possible that these interventions may also benefit individuals with olfactory dysfunction, if these symptoms are assessed.
For many individuals, smell loss is anticipated to improve with time. There is no intervention that could currently be regarded as standard care for individuals with post‐COVID‐19 related anosmia. Interventions are therefore likely to be compared to no treatment, or to placebo (dummy) treatment. However, olfactory training is often suggested as an intervention with few, if any, adverse effects, and may be used alongside other treatments, therefore we anticipate that this may be advised to be undertaken concurrently in some studies.
How the intervention might work
Corticosteroids are frequently prescribed to ensure that any intranasal inflammatory component that is exacerbating the PIOD is adequately treated. Whether they have a persisting effect after discontinuation is unclear. Intranasal corticosteroids are used for a number of other conditions, and serious side effects are rare, but they may cause nasal irritation, nosebleeds or other localised complications. Corticosteroids may also be administered systemically ‐ typically as oral tablets, or sometimes parenterally.
Olfactory training aims to stimulate the olfactory neurons with a variety of odours in order to enhance smell detection. It is unclear whether any changes occur within the olfactory epithelium itself, in the olfactory bulb, or involve reorganisation of neural olfactory pathways. Although olfactory training may not restore olfactory function, it may improve the performance of the olfactory system. Two recent systematic reviews suggest that olfactory training may give some benefit to those with olfactory disorders (Pekala 2016; Sorokowska 2017). However, the majority of included studies were prospective cohorts, with only one RCT included.
A number of vitamins and minerals have been suggested to have a beneficial effect on the olfactory epithelium, including vitamins A, B12 and D, and zinc. It is thought that metabolites of vitamin A may play a role in regeneration of tissue in the olfactory epithelium or olfactory bulb, and this has been used intranasally to treat individuals with post‐viral olfactory loss (Hummel 2017). Vitamin B12 is known to be important in the maintenance of central and peripheral nervous function, and deficiency of vitamin B12 has been associated with olfactory impairment (Derin 2016). Vitamin D deficiency has also been linked to olfactory impairment (Bigman 2020), and there is ongoing interest in the potential use of vitamin D to prevent or treat other symptoms of COVID‐19 infection (Martineau 2020). Zinc deficiency has also been shown to have an association with olfactory dysfunction and zinc was historically used intranasally as a potential treatment for anosmia, although there are concerns over toxicity (Alexander 2006).
Antioxidants, such as alpha lipoic acid and omega 3 fatty acids, have also been suggested as possible interventions to treat anosmia (Hummel 2002). They are thought to have neuroprotective properties that may help restore function within olfactory neurons or the olfactory bulb. Minocycline has also been trialled in post‐viral olfactory loss ‐ due to its neuroprotective properties, rather than its traditional role as an antibiotic (Reden 2011).
It is possible that antiviral agents, some of which have already been shown to impact on the severity of COVID‐19, may also affect the olfactory dysfunction. Reducing viral replication (and consequently lowering the viral load in an individual) may result in reduced severity of olfactory loss, or hasten the recovery. Monoclonal antibodies have also been used to treat COVID‐19, and could also have an impact on the severity and persistence of olfactory impairment.
There have also been small studies to assess the possible benefit of acupuncture in olfactory loss (Dai 2016; Vent 2010).
Glutamate plays an important role in neurotransmission for olfactory neurons and within the olfactory bulb. Glutamate antagonists, such as caroverine, have been proposed to help protect against neurotoxicity, and consequently improve olfactory function (Quint 2002). Finally, xanthine derivatives such as theophylline (sometimes given intranasally) and pentoxifylline have been proposed to stimulate olfactory neuron activity, and may therefore have an effect on olfactory function.
It is possible that individuals with a longer duration of anosmia have a different underlying disease process than those with temporary olfactory dysfunction related to COVID‐19. Consequently the efficacy of different interventions may vary between these groups.
The method of administration for nasal sprays or drops is likely to impact on the efficacy of any treatment. Different techniques of administration may result in the treatment reaching different areas within the nose (Kubba 2000; Raghavan 2000). To treat olfactory dysfunction, interventions are likely intended to reach the olfactory cleft, although this is often not achieved with standard techniques of administration (Scheibe 2008). However, some interventions (such as nasal corticosteroids) may also exert effects on the nasal mucosa. This could impact on nasal airflow and have indirect effects on olfaction. Therefore, the precise location of effect and mechanism of action for these medications may be uncertain.
Why it is important to do this review
The COVID‐19 pandemic has resulted in an enormous number of individuals becoming infected with SARS‐CoV‐2. Fortunately, many individuals recover completely. However, the long‐term consequences of infection are only just becoming apparent. Although the prevalence of persisting olfactory dysfunction may be small, with huge numbers of global infections, the actual number of individuals suffering from post‐COVID‐19 related anosmia is large. We can assume an estimated 60% suffer olfactory dysfunction at the onset of the infection and that at least 10% of these go on to experience PIOD. Of all those infected 5% to 7% have been found to be functionally anosmic 12 months after exposure (Boscolo‐Rizzo 2021b; Vaira 2021b). Given the number of infections (> 295 million infections worldwide, as of December 2021), we estimate that nearly 15 million people may have persistent anosmia, while many others will not have fully recovered. The burden of this disorder is also considerable, with significant effects on quality of life, as well as safety implications (due to the inability to detect harmful or dangerous smells). Therefore, identification of potential treatments that may improve the outcome for sufferers is timely and important.
Many interventions carry a risk of adverse effects. If the beneficial effect of an intervention is small or negligible, then side effects may be such that individuals do not consider it worthwhile. With this review we aimed to comprehensively assess the benefits and harms of interventions to prevent persisting olfactory dysfunction related to COVID‐19, to ensure that patients can make an informed choice regarding the management of their condition.
Given the recent emergence of COVID‐19, there is currently a great deal of uncertainty about how best to manage the olfactory dysfunction that occurs as a result of the virus. The sheer numbers of infected individuals worldwide also means that evidence that supports decision‐making for management of COVID‐19 is a priority for decision‐makers globally. There is also a strong emphasis on COVID‐19 research at present, and we anticipate that there is likely to be new evidence available over the coming months and years. Therefore, this review is a living systematic review, which will be continually updated to incorporate any important new evidence as it becomes available.
Objectives
To assess the effects (benefits and harms) of interventions that have been used, or proposed, to prevent persisting olfactory dysfunction due to COVID‐19 infection.
A secondary objective is to keep the evidence up‐to‐date, using a living systematic review approach.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials and quasi‐randomised trials (where trials were designed as RCTs, but the sequence generation for allocation of treatment used methods such as alternative allocation, birth dates, alphabetical order etc.).
We considered that olfactory dysfunction is unlikely to be stable over long periods of time, and individuals may experience considerable fluctuation of symptoms over a given time period. Therefore, cross‐over trials were unlikely to be identified. If we identified any cross‐over studies, we planned to only include data from the first phase of these studies in the review.
We included studies where the main purpose of the trial was to assess the effect of treatment on olfactory function. Many interventions are used in the treatment of COVID‐19 (such as corticosteroids, antivirals) ‐ these may have beneficial effects on olfactory function, but the primary aim of most trials will be to assess their impact on other features of the disease (such as need for ventilation, mortality etc.). Therefore, we only included studies where olfactory function had been assessed at the trial baseline, and the main aim of the study was to determine the effect of an intervention on olfaction.
We only included studies where patients were followed up for at least one week. The aim of this review was to synthesise evidence for treatments that may have a lasting effect on olfactory function, rather than those that may have a very brief or temporary impact.
We included studies in any language. We planned to include outcome data reported on a trial registry, even if no published results were available. However, we did not identify any studies where this was applicable. If we identified material from a pre‐print server then we planned to note this in the 'What's new' section of the review, pending identification of fully published data. If no published data were identified within four months of the pre‐print article being made available then we planned to incorporate the data in the review. However, we did not identify any pre‐print articles during the searches.
Types of participants
We included studies of adult participants (aged 18 years or older) with a diagnosis of COVID‐19 and olfactory dysfunction that had lasted less than four weeks. We anticipated that some studies would report this as less than four weeks of olfactory dysfunction, rather than less than four weeks since a positive test for COVID‐19 ‐ either of these measures were included in the review.
We included individuals with anosmia (absent sense of smell) or hyposmia (reduced sense of smell). We anticipated that some trials may also include a small number of individuals with symptoms of pure parosmia or phantosmia. We planned to include data from these trials, providing the majority (≥ 80% of participants) report anosmia or hyposmia.
We included studies where olfactory dysfunction was identified with either psychophysical (objective) testing, or through self‐report of symptoms. We planned to investigate whether this had any impact on the effect estimates using subgroup analysis (see Subgroup analysis and investigation of heterogeneity).
We included studies where COVID‐19 has been diagnosed through either objective testing (e.g. viral polymerase chain reaction (PCR) from nasopharyngeal swabs) or through a clinical diagnosis (for example, sudden onset of olfactory dysfunction with other symptoms of COVID‐19, or in the context of contact with an infected individual).
For inclusion in this review, all participants in the trial must have had abnormalities of their sense of smell. We did not include studies where only some participants are eligible (i.e. not all participants had olfactory dysfunction at the start of the trial).
Types of interventions
Interventions
We included any intervention proposed to specifically prevent persisting olfactory dysfunction. We anticipated that this may include the following interventions:
Intranasal corticosteroid drops/rinses
Intranasal corticosteroid sprays
Systemic corticosteroids
Olfactory training
Vitamin A
Zinc
Antioxidants (e.g. omega 3 fatty acids, alpha lipoic acid, minocycline)
Antiviral agents (e.g. remdesivir)
Other vitamins and nutritional supplements (to be analysed according to the type of vitamin/supplement, rather than as a pooled comparison)
Acupuncture
Monoclonal antibodies
Glutamate antagonists (e.g. caroverine)
Xanthine derivatives (e.g. theophylline, pentoxifylline)
Saline irrigation
If we had identified studies of additional interventions then these would also have been included.
All routes of administration, doses and duration of treatment were included.
Olfactory training was considered to be a complex intervention, as the method of delivery varies considerably in different studies. We planned to assess this using subgroup analyses, if we identified any trials of this intervention (see below).
Comparator(s)
The main comparison is:
placebo or no treatment.
Concurrent treatments
We anticipated that some trials may include olfactory training (or other interventions) as concurrent therapy for both arms. We placed no limits on the type of concurrent treatments used. We planned to pool these trials with those where no concurrent treatment was used and use sensitivity analyses to determine whether the effect estimates are changed because of this.
Types of outcome measures
We analysed the following outcomes in the review, but we did not use them as a basis for including or excluding studies. All outcomes were assessed at three possible time points:
≤ 4 weeks;
> 4 weeks to 3 months (this was the main time frame of interest);
> 3 months to 6 months.
These time points relate to the time since treatment was started.
Outcomes at less than four weeks following COVID‐19 were considered too short to comprehensively assess whether individuals have persisting olfactory problems. However, in the absence of other evidence they may provide some indication about the likely efficacy of treatments to prevent later problems.
As most individuals with temporary problems should have complete resolution of their olfactory symptoms by four weeks (Boscolo‐Rizzo 2020), we considered this time frame (> 4 weeks) to be of importance to identify those who truly have persisting problems. However, we recognised that some individuals may experience fluctuations in their symptoms, and develop recurrent olfactory problems at a later stage. We therefore included outcomes that were measured at a later point to identify whether early intervention could help to prevent these problems from developing.
Primary outcomes
-
Presence of normal olfactory function:
as assessed by the participants (e.g. self‐rated complete recovery);
as assessed using psychophysical testing, using Sniffin' Sticks, University of Pennsylvania Smell Identification Test (UPSIT) or another validated test.
Serious adverse effects (as defined by the trialists).
-
Change in sense of smell:
as assessed by the participants (e.g. using a visual analogue score);
as assessed using psychophysical testing, using Sniffin' Sticks, UPSIT or another validated test.
It is well recognised that self‐rated sense of smell correlates poorly with the results of psychophysical testing of olfactory function. Therefore we have included both types of outcome measurements separately for the outcome domains that relate to sense of smell. If data had been obtained for both of these measures we would not have combined them, but would have reported them as two separate analyses. However, at present the only included study includes data using self‐reported olfactory function only.
Secondary outcomes
Prevalence of parosmia, as assessed by the participants.
Change in sense of taste, as assessed by psychophysical gustatory tests, such as the sip and spit method or other validated tests.
Disease‐related quality of life, as assessed by the Olfactory Disorders Questionnaire, or another validated questionnaire (which specifically relates to olfactory dysfunction).
Other adverse effects (including nosebleeds/bloody discharge).
We recognise that parosmia is a challenging symptom to define and assess. If we had identified data for this outcome then we would have included any results reported by the study authors, and described the definitions used in the study. However, this outcome was not assessed by the study included in the review.
Where possible, we planned to compare the threshold for appreciable change in these outcomes to published minimally important differences. These have been reported for psychophysical olfactory testing using Sniffin' Sticks (MID 5.5 points, Gudziol 2006) and the Olfactory Disorders Questionnaire (MID 5.2 points, Mattos 2018). However, we did not identify any data for these outcomes in the review.
Search methods for identification of studies
The Cochrane ENT Information Specialist conducted systematic searches for randomised controlled trials and controlled clinical trials. There were no language or publication status restrictions. Some of the search terms were limited by publication year, due to the novel nature of post‐COVID‐19 olfactory dysfunction. We contacted original authors for clarification and further data if trial reports were unclear and arranged translations of papers where necessary.
Electronic searches
As a living systematic review, the Information Specialist has conducted monthly searches of:
the Cochrane ENT Trials Register (searched via the Cochrane Register of Studies to 20 October 2021);
the Cochrane Central Register of Controlled Trials (CENTRAL) (searched via the Cochrane Register of Studies to 20 October 2021);
Ovid MEDLINE(R) Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) (1946 to 20 October 2021);
Ovid Embase (1974 to 20 October 2021);
Web of Knowledge, Web of Science (1945 to 6 September 2021);
ClinicalTrials.gov, www.clinicaltrials.gov (searched via the Cochrane Register of Studies to 20 October 2021);
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (searched via the Cochrane Register of Studies to 20 October 2021);
Cochrane COVID‐19 Study Register, https://covid-19.cochrane.org/ (searched via the Cochrane Register to 20 October 2021).
The Information Specialist conducts quarterly searches of the following sources, and prior to the publication of any update:
ClinicalTrials.gov (search via www.clinicaltrials.gov to date);
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (search via https://apps.who.int/trialsearch/ to date).
The Information Specialist used appropriate date restrictions and auto‐alerts as available and appropriate for each monthly search. Details available in Appendix 1.
In searches prior to July 2021 we also searched the World Health Organization (WHO) COVID‐19 'Global literature on coronavirus disease', https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov to 16 December 2020.
The Information Specialist modelled subject strategies for databases on the search strategy designed for CENTRAL. The strategies were designed to identify all relevant studies for a pair of reviews (O'Byrne 2022; Webster 2021b). Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials (as described in the Technical Supplement to Chapter 4 of the Cochrane Handbook for Systematic Reviews of Interventions version 6.1) (Lefebvre 2020). In July 2021 the Information Specialist incorporated new Mesh and Emtree terms into the search, and in September 2021 corrected typos in the original search. The current search strategies for major databases are provided in Appendix 2 and the search strategies performed in December 2021 are provided in Appendix 3
Clinical trials are ongoing to assess a variety of interventions for the treatment of COVID‐19. As few studies have currently been published, the search strategy developed is highly sensitive in order to try to capture all interventions as they are introduced. The Information Specialist will review the search methods (the sources and search frequency) and the search terms (index terms and free text terms) on an annual basis. The search strategy may evolve over time, as a greater body of literature is published and a more focused list of interventions are identified.
Searching other resources
We scanned the reference lists of identified publications for additional trials and contacted trial authors where necessary. In addition, the Information Specialist searched Ovid MEDLINE to retrieve existing systematic reviews relevant to this systematic review, so that we could scan their reference lists for additional trials. The Information Specialist also searched of the Web of Knowledge Science Citation Index for articles referencing the published review and its companion (O'Byrne 2022; Webster 2021b) and the primary reference to the included studies of both reviews.
These searches were last conducted on 20 October 2021.
We did not perform a separate search for adverse effects. We considered adverse effects described in included studies only.
We planned to make efforts to identify full‐text papers regardless of language of publication and endeavour to seek help with translation; however, we did not encounter this issue. Any papers that we were unable to source in time for the scheduled living review update, or were unable to get translated, would be listed as awaiting assessment. Fortunately, we were able to identify and locate all papers of relevance for this review, and did not require any translation.
Living systematic review considerations
As a living systematic review, we scanned the reference lists of identified publications for additional trials and contacted trial authors if necessary. In addition, the Information Specialist searched on an annual basis Ovid MEDLINE to retrieve existing systematic reviews relevant to this systematic review, so that we could scan their reference lists for additional trials. The Information Specialist conducted annual searches of the Web of Knowledge Science Citation Index for articles referencing the published review and its included studies and non‐systematic searches of Google Scholar to retrieve grey literature and other sources of potential trials.
For workload and capacity reasons, the monthly searches for this review were temporarily paused following the October 2021 searches and will be restarted later in 2022.
Data collection and analysis
Selection of studies
The Cochrane ENT Information Specialist used the first two components of Cochrane's Screen4Me workflow to help assess the search results. Screen4Me comprises three components:
Known assessments – a service that matches records in the search results to records that have already been screened in Cochrane Crowd and been labelled as 'a RCT' or as 'not a RCT'.
The machine learning classifier (RCT model) (Wallace 2017), available in the Cochrane Register of Studies (CRS‐Web), which assigns a probability of being a true RCT (from 0 to 100) to each citation. For citations that are assigned a probability score below the cut‐point at a recall of 99% we will assume these to be non‐RCTs. For those that score on or above the cut‐point we will either manually dual screen these results or send them to Cochrane Crowd for screening.
Cochrane Crowd is Cochrane's citizen science platform where the Crowd help to identify and describe health evidence. For more information about Screen4Me and the evaluations that have been done, please go to the Screen4Me website on the Cochrane Information Specialist's portal and see Marshall 2018; McDonald 2017; Noel‐Storr 2018 and Thomas 2017.
We did not use the third component because of the relatively small number of results retrieved by the search.
Two review authors (LOB, KW) independently screened the remaining titles and abstracts retrieved by the search to identify potentially relevant studies. The same authors independently evaluated the full text of each potentially relevant study to determine whether it met the inclusion/exclusion criteria for this review. We resolved any differences by discussion and consensus. We planned to involve a third author where necessary, but this was not required.
Living systematic review considerations
We will immediately screen any new citations retrieved by the monthly searches using the approach outlined above.
Data extraction and management
Two review authors (LOB, KW) independently extracted outcome data from each study using a standardised data collection form. Where a study had more than one publication, we retrieved all publications to ensure complete extraction of data (for example, published articles and details from trial registries). Any discrepancies in the data extracted by the two authors were checked against the original reports, and differences were resolved through discussion and consensus. We planned to consult a third author where necessary, but this was not required. If required, we contacted the study authors for clarification.
We collected information on study design and setting, participant characteristics (including disease severity and age), study eligibility criteria, details of the intervention(s) given, the outcomes assessed, the source of study funding and any conflicts of interest stated by the investigators. We also included details of the baseline characteristics of trial participants, with particular regard to prognostic features such as age, gender, severity of infection and duration of time since COVID‐19 infection.
The primary effect of interest for this review was the effect of treatment assignment (which reflects the outcomes of treatment for people who were assigned to the intervention) rather than a per protocol analysis (the outcomes of treatment only for those who completed the full course of treatment as planned). For the outcomes of interest in this review, we extracted the findings from the studies on an available case basis, i.e. all available data from all participants at each time point, based on the treatment to which they were randomised. This was irrespective of compliance, or whether participants had received the intervention as planned.
In addition to extracting prespecified information about study characteristics and aspects of methodology relevant to risk of bias, we extracted the following summary statistics for each trial and outcome:
For continuous data: the mean values, standard deviation and number of patients for each treatment group at the different time points for outcome measurement. Where endpoint data were not available, we extracted the values for change‐from‐baseline data instead. If values for the individual treatment groups were not reported, we planned to extract summary statistics (e.g. mean difference) from the studies.
For binary data: we extracted information on the number of participants experiencing an event, and the number of participants assessed at that time point. If values for the individual treatment groups were not reported, we planned to extract summary statistics (e.g. risk ratio) from the studies.
For ordinal scale data: if we identified data reported on an ordinal scale and if the data appeared to be normally distributed, or if the analysis performed by the investigators indicated that parametric tests were appropriate, then we planned to treat the outcome measure as continuous data. Alternatively, if data were available, we planned to convert these to binary data. However, we were not able to confirm that the ordinal data we obtained (from a visual analogue scale of sense of smell) was normally distributed, therefore this was not possible.
For time‐to‐event data: if we identified data reported as time‐to‐event, we planned to extract data on hazard ratios from individual studies. If these data were not reported then we planned to extract alternative measures of treatment effect, such as the observed and expected number of events in each group, a P value and the number of events in each arm, or data in a Kaplan Meier curve. However, we did not identify any time‐to‐event data.
We prespecified time points of interest for the outcomes in this review. Where studies reported data at multiple time points, we planned to take the longest available follow‐up point within each of the specific time frames. For example, if a study reported an outcome at 6 weeks, 8 weeks and 12 weeks of follow‐up then the 12‐week data would have been included for the time point > 4 weeks to 3 months.
Assessment of risk of bias in included studies
Two authors undertook assessment of the risk of bias of the included trials independently, with the following taken into consideration, as guided by the Cochrane Handbook for Systematic Reviews of Interventions (Handbook 2011):
sequence generation;
allocation concealment;
blinding;
incomplete outcome data;
selective outcome reporting; and
other sources of bias.
We used the Cochrane risk of bias tool in RevMan 5.4 (RevMan 2020), which involves describing each of these domains as reported in the trial and then assigning a judgement about the adequacy of each entry: 'low', 'high' or 'unclear' risk of bias.
Measures of treatment effect
We summarised the effects of dichotomous outcomes (e.g. prevalence of olfactory dysfunction) as risk ratios (RR) with 95% confidence intervals (CIs). For the key outcomes that we presented in the summary of findings tables, we also expressed the results as absolute numbers based on the pooled results and compared to the assumed risk. For future iterations of this living review, we may also calculate the number needed to treat to benefit (NNTB) using the pooled results to aid understanding. The assumed baseline risk is typically either (a) the median of the risks of the control groups in the included studies, this being used to represent a 'medium‐risk population' or, alternatively, (b) the average risk of the control groups in the included studies is used as the 'study population' (Handbook 2020). As a single study was included for each analysis (no meta‐analyses were performed), we used the baseline risk from this study for all calculations. If a large number of studies are available in future, and where appropriate, we may also present additional data based on the assumed baseline risk in (c) a low‐risk population and (d) a high‐risk population.
For continuous outcomes, we planned to express treatment effects as a mean difference (MD) with standard deviation (SD) or as a standardised mean difference (SMD) if different scales have been used to measure the same outcome. We planned to provide a clinical interpretation of the SMD values using either Cohen's d or by conversion to a recognised scale if possible.
For time‐to‐event outcomes we planned to summarise the effects as a hazard ratio (HR) with 95% CI. If necessary, and where possible (if sufficient alternative data were provided), we planned to estimate the HR from individual studies according to the methods outlined in Tierney 2007. However, no time‐to‐event data were identified for the review.
Unit of analysis issues
Cross‐over trials and cluster‐randomised trials were not anticipated for this review topic, and none were identified. Post‐COVID‐19 related anosmia is unlikely to be a stable condition, and interventions may not have a temporary effect. If cross‐over trials were identified then we planned to use only the data from the first phase of the study. If cluster‐randomised trials were identified then we would have ensured that analysis methods were used to account for clustering in the data (Handbook 2020).
Dealing with missing data
We planned to contact study authors via email whenever an outcome of interest was not reported, if the methods of the study suggested that the outcome had been measured. We planned to do the same if not all data required for meta‐analysis had been reported, unless the missing data were standard deviations. If standard deviation data were not available, we would have approximated these using the standard estimation methods from P values, standard errors or 95% CIs if these were reported, as detailed in the Cochrane Handbook for Systematic Reviews of Interventions (Handbook 2020). If it was impossible to estimate these, we would have contacted the study authors.
Apart from imputations for missing standard deviations, we planned to conduct no other imputations. We extracted and analysed all data using the available case analysis method.
Assessment of heterogeneity
We planned to assess clinical heterogeneity (which may be present even in the absence of statistical heterogeneity) by examining the included trials for potential differences between studies in the types of participants recruited, interventions or controls used and the outcomes measured. However, this was not possible due to the inclusion of a single study.
We planned to assess statistical heterogeneity by visually inspecting the forest plots and by considering the Chi² test (with a significance level set at P value < 0.10) and the I² statistic, which calculates the percentage of variability that is due to heterogeneity rather than chance (Handbook 2020). Again, this was not necessary due to the inclusion of a single study.
Assessment of reporting biases
We assessed reporting bias as within‐study outcome reporting bias and between‐study publication bias.
Outcome reporting bias (within‐study reporting bias)
We assessed within‐study reporting bias by comparing the outcomes reported in the published report against the study protocol or trial registry, whenever this could be obtained. If the protocol or trial registry entry was not available, we compared the outcomes reported to those listed in the methods section. If results are mentioned but not reported adequately in a way that allows analysis (e.g. the report only mentions whether the results were statistically significant or not), bias in a meta‐analysis is likely to occur. We planned to seek further information from the study authors. If no further information was found, we noted this as being a 'high' risk of bias when the risk of bias tool is used. If there was insufficient information to judge the risk of bias we noted this as an 'unclear' risk of bias (Handbook 2011).
Publication bias (between‐study reporting bias)
We planned to assess funnel plots if sufficient studies (more than 10) were available for an outcome. If we observed asymmetry of the funnel plot, we planned to conduct more formal investigation using the methods proposed by Egger 1997. We planned to also report on whether there were any studies identified through trial registries and other sources (Searching other resources), with unpublished reports.
Data synthesis
Where possible and appropriate (if participants, interventions, comparisons and outcomes were sufficiently similar in the trials identified), we planned to conduct a quantitative synthesis of results. We planned to conduct all meta‐analyses using a fixed‐effect model in RevMan 5.4. However, at present a single study is included in this review, precluding meta‐analysis.
We planned to include all studies in the meta‐analyses, regardless of their risk of bias. However, we intended to incorporate a summary assessment of risk of bias in the measure of certainty of the evidence for each outcome, using the GRADE system.
For dichotomous data, we analysed treatment differences as a risk ratio (RR) calculated using the fixed‐effect Mantel‐Haenszel methods.
For continuous outcomes, we planned to use the inverse variance, fixed‐effect method of meta‐analysis. If all data were from the same scale, we planned to pool mean follow‐up values with change‐from‐baseline data and report this as a mean difference. If there was a need to report standardised mean differences then we would not pool endpoint and change‐from‐baseline data.
For time‐to‐event data we planned to use a generic inverse variance, fixed‐effect method of meta‐analysis.
Sense of smell may be tested using a variety of methods, which consider different aspects of the sense of smell. These are:
identification ‐ the ability to identify and name a specific odour;
threshold ‐ the concentration of an odour that can be detected;
discrimination ‐ the ability to discriminate between odours.
We included methods that consider any or all of the above aspects of sense of smell. If meta‐analysis is appropriate in future iterations of this review, we will only pool results that look at the same individual aspect (or aspects) of sense of smell.
If meta‐analysis was not possible (for example, due to incompletely reported outcomes/effect estimates or different effect measures that cannot be combined) then we considered presenting alternative synthesis methods. This would have included summarising the effect estimates from individual studies, combining P values or vote counting based on the direction of effect, depending on the data available.
Living systematic review considerations
Whenever new evidence relevant to the review is identified in our monthly searches, we will extract the data, assess risk of bias and incorporate it into the synthesis every four months, as appropriate. Formal sequential meta‐analysis approaches will not be used for updated meta‐analyses.
Subgroup analysis and investigation of heterogeneity
A number of factors are likely to impact on the outcomes included in this review. At present, we have insufficient studies and data to conduct any subgroup analysis. For future versions of this review (if appropriate data are reported), we plan to consider the following subgroups, regardless of whether statistical heterogeneity is identified:
-
Age of participants in the trial (under 60 years versus those aged 60 or over):
age is well recognised to impact on olfactory function, with sense of smell worsening with time. The ability to detect smells may therefore differ considerably between younger and older adults.
-
Gender of participants in the trial (female versus male):
gender has an influence on olfactory function, and may also impact recovery rates.
-
Method used to determine olfactory dysfunction at trial baseline (self‐reported versus psychophysical testing):
rates of olfactory dysfunction vary depending on whether self‐report or psychophysical testing is used to identify olfactory loss. Effect estimates in these two groups may therefore differ.
-
Time elapsed between diagnosis and treatment (< 2 weeks compared to 2 to 4 weeks before commencing treatment):
currently, patients are likely to be required to self‐isolate for two weeks once diagnosed with COVID‐19. Therefore, it would be informative to know whether a delay of two weeks in initiating treatment has an impact on outcomes.
If trials did not report data for particular subgroups of participants, we planned to synthesise data at the level of the individual trial, where appropriate. We would have identified studies as belonging to a particular subgroup if more than 2/3 participants (66%) belong to that category.
If trials had presented data for subgroups of individuals within the trial, we would have used this for subgroup analysis, where applicable, regardless of whether trials had stratified their randomisation according to those subgroups.
We anticipate that the varying methods used for olfactory training may be a source of heterogeneity in effects. If we had identified heterogeneity in the comparison of olfactory training then we would have explored this considering the following factors:
classical versus modified olfactory training (using the same scents throughout, compared to changing the scents);
the duration of the intervention.
Sensitivity analysis
We planned to carry out sensitivity analyses to determine whether the findings are robust to the decisions made in the course of identifying, screening and analysing the trials. We would have conducted sensitivity analysis for the following factors, whenever possible:
impact of model chosen: fixed‐effect versus random‐effects model;
inclusion of studies with concurrent treatments: including and excluding these studies from the pooled estimates of effect for any intervention;
method of COVID‐19 diagnosis: to exclude studies where only a clinical method of COVID‐19 diagnosis was used (rather than laboratory confirmed).
As only five studies were included in the review, and no meta‐analysis was possible, sensitivity analyses were not appropriate at this point.
Summary of findings and assessment of the certainty of the evidence
Two independent authors (LOB/KW) used the GRADE approach to rate the overall certainty of evidence using GRADEpro GDT (https://gradepro.org/). The certainty of evidence reflects the extent to which we are confident that an estimate of effect is correct and we will apply this in the interpretation of results. There are four possible ratings: high, moderate, low and very low. A rating of high certainty of evidence implies that we are confident in our estimate of effect and that further research is very unlikely to change our confidence in the estimate of effect. A rating of very low certainty implies that any estimate of effect obtained is very uncertain.
The GRADE approach rates evidence from RCTs that do not have serious limitations as high certainty. However, several factors can lead to the downgrading of the evidence to moderate, low or very low. The degree of downgrading is determined by the seriousness of these factors:
study limitations (risk of bias);
inconsistency;
indirectness of evidence;
imprecision; and
publication bias.
We planned to include a summary of findings table, constructed according to the recommendations described in Chapter 14 of the Cochrane Handbook for Systematic Reviews of Interventions (Handbook 2020), for the following comparison(s):
intranasal corticosteroid drops/rinses versus no treatment/placebo;
intranasal corticosteroid sprays versus no treatment/placebo;
olfactory training versus no treatment/placebo;
intranasal vitamin A versus no treatment/placebo.
We included the following outcomes in the summary of findings tables:
presence of normal olfactory function (as reported by the participants);
serious adverse effects;
change in sense of smell (as reported by the participants);
prevalence of parosmia;
change in sense of taste;
disease‐related quality of life;
other adverse effects (including nosebleeds/bloody discharge).
Methods for future updates
Living systematic review considerations
We will review the scope and methods of this review approximately yearly (or more frequently if appropriate) in the light of potential changes in the topic area, or the evidence being included in the review (for example, additional comparisons, interventions or outcomes, or new review methods available).
Conditions under which the review will no longer be maintained as a living systematic review
The review will no longer be maintained as a living systematic review once there is high‐certainty evidence obtained for the primary effectiveness outcomes of the review; once new studies are not expected to be conducted regularly for the interventions included in this review; or once the review topic is no longer a priority for health care decision‐making.
Results
Description of studies
Results of the search
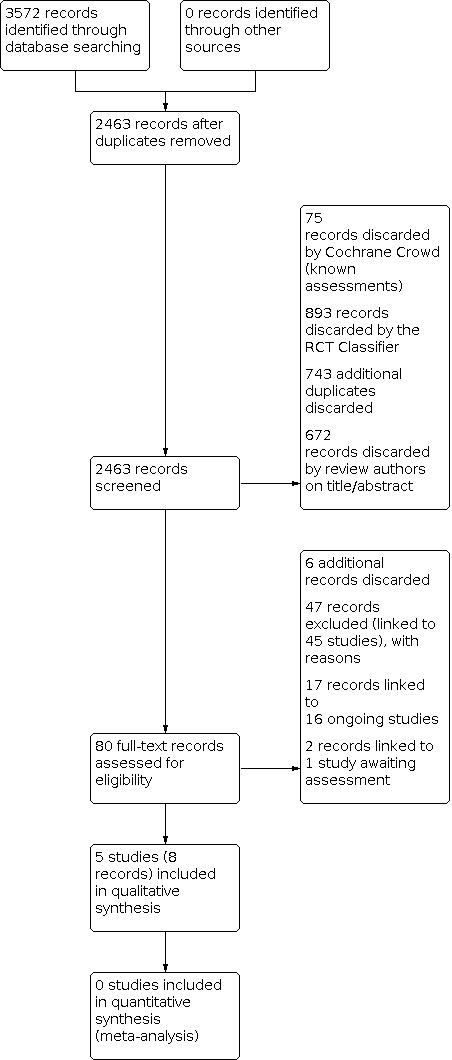
The searches (December 2020, and monthly searches July to October 2021) retrieved a total of 3572 records. This reduced to 2463 after the removal of duplicates. The Cochrane ENT Information Specialist sent all 2463 records to the Screen4Me workflow. The Screen4Me workflow identified 109 records as having previously been assessed: 75 had been rejected as not RCTs and 34 had been assessed as possible RCTs. The RCT classifier rejected an additional 893 records as not RCTs (with 99% sensitivity). We did not send any records to the Cochrane Crowd for assessment. Following this process, the Screen4Me workflow had rejected 968 records and identified 1495 possible RCTs for title and abstract screening.
| Possible RCTs | Rejected | |
| Known assessments | 34 | 75 |
| RCT classifier | 1461 | 893 |
| Total | 1495 | 968 |
We identified 743 additional duplicates. We screened the titles and abstracts of the remaining 752 records. We discarded 672 records and assessed 80 full‐text records. We discarded six additional records at the full‐text screening stage.
We excluded 47 records (linked to 45 studies) with reasons recorded in the review (see Excluded studies).
We included five completed studies (eight records) where results were available (Abdelalim 2021; Abdelmaksoud 2021; Kasiri 2021; Rashid 2021; Yildiz 2021).
One study (two records) is awaiting assessment (Mohamad 2021). It is unclear from this article whether participants had symptoms for less than four weeks at baseline. We have attempted to contact the authors to clarify this, but are awaiting a response.
We identified 16 ongoing studies (17 records). See Characteristics of ongoing studies for further details of all ongoing studies. Some studies will assess more than one intervention. The interventions that will be assessed include:
corticosteroid nasal irrigation or sprays (TCTR20210714006; UMIN000043537);
systemic corticosteroids (NCT04528329; NCT04530409);
"nasal therapy" including corticosteroid spray, nasal irrigation, decongestant and vapour rub (UMIN000045185);
antihistamines (UMIN000043537);
olfactory training (IRCT20210202050231N1; IRCT20210205050247N; NCT04764981; NCT04900415);
vitamin A (IRCT20210205050247N; NCT04900415);
retinoic acid + vitamin D (NCT05002530);
acupuncture (IRCT20210311050671N1; NCT04959747);
omega‐3 (NCT04495816);
ivermectin (NCT04951362);
Imupret, a herbal supplement (NCT04797936);
transauricular vagus nerve stimulation (NCT04638673).
It should be noted that some of the studies assess more than one intervention, and that ‐ for some studies ‐ it is unclear whether participants will have less than four weeks of olfactory loss at baseline. Some of these studies may therefore not be eligible for inclusion in the review once the published data are available.
A flow chart of study retrieval and selection is provided in Figure 1.
1.
Included studies
Five studies were included in the review (Abdelalim 2021; Abdelmaksoud 2021; Kasiri 2021; Rashid 2021; Yildiz 2021).
Study design
All of the included studies were reported to be randomised controlled trials. Two of the included studies were reported to be double‐blinded trials and described the use of placebo (topical saline nasal spray or 0.9% saline drops, respectively) in the comparator group (Kasiri 2021; Rashid 2021). Three studies did not use a placebo, and participants in the control arms received no intervention (Abdelalim 2021; Abdelmaksoud 2021; Yildiz 2021).
The studies varied in size, with the smallest study including 80 participants (Kasiri 2021) and the largest including 276 (Rashid 2021).
Participants
We intended that this review would only include studies where participants had recent onset of symptoms of olfactory dysfunction related to COVID‐19, defined as symptoms lasting for less than one month at entry to the study. However, from the information reported in the individual studies it was difficult to ascertain whether this was the case. Only one study specifically included participants with a duration of anosmia that was ≤ 15 days, and stated that individuals with a longer duration of symptoms were excluded (Rashid 2021).
The other studies did not state a required duration of symptoms in their inclusion/exclusion criteria. However, other information reported in the study or correspondence with the authors indicated that participants were in the early phase of the disease. The authors of Abdelalim 2021 confirmed that symptoms of olfactory disturbance had lasted between 10 and 28 days at baseline for all participants. The study Abdelmaksoud 2021 indicates that participants were hospitalised when they entered the trial, therefore we assume that the majority were within four weeks of diagnosis of COVID‐19. Kasiri 2021 stated that included participants had olfactory disturbance for two weeks, but it was unclear whether this was exactly two weeks, or at least two weeks. However, other details in the study indicated that participants were in the active phase of COVID‐19 at the time of recruitment (a large number of participants had other COVID‐19 symptoms at baseline, such as fever or cough). Therefore we have presumed that the majority of participants were within four weeks of a diagnosis of COVID‐19/the onset of olfactory dysfunction. Similarly, participants in Yildiz 2021 were hospitalised with COVID‐19, and data reported in the article indicate that participants were within four weeks of their diagnosis/onset of symptoms.
All studies were conducted in adults and excluded participants with previous symptoms of olfactory dysfunction, or with underlying medical conditions that may affect olfaction.
Abdelalim 2021, Abdelmaksoud 2021, Rashid 2021 and Yildiz 2021 recruited participants with self‐reported olfactory dysfunction, and did not describe the use of psychophysical testing at baseline to establish the olfactory deficit. Kasiri 2021 included participants with olfactory dysfunction as assessed with the Iranian version of the UPSIT (Iran‐SIT). The authors report that participants with either severe anosmia or microsmia were included ‐ we assume this means a score of < 19 out of 24.
We attempted to contact the authors of all of the studies included in this review, in order to clarify some of the details that were not reported fully in the articles. However, we have, as yet, only had a response from the authors of Abdelalim 2021.
Interventions and comparisons
Comparison 1: intranasal corticosteroid spray compared to placebo/no intervention
Three studies considered this comparison (Abdelalim 2021; Kasiri 2021; Yildiz 2021). Different corticosteroid sprays, doses and frequencies were used by the individual studies. Abdelalim 2021 used 100 μg mometasone furoate, administered once daily for three weeks and compared this to no intervention. Kasiri 2021 used the same spray (100 μg mometasone furoate) but administered it twice daily for four weeks and compared it to the use of topical saline spray. We have assumed this is an isotonic (0.9%) spray, but details are not provided in the report. All participants in this study were also receiving olfactory training. Yildiz 2021 was a three‐armed trial. One intervention group received a nasal corticosteroid spray of triamcinolone acetonide 0.055%, two puffs to each nostril daily, plus hypertonic saline irrigation. One group received hypertonic saline irrigation alone, and one group received no intervention. For this comparison we have compared the group receiving nasal corticosteroid plus hypertonic saline to the study arm that received hypertonic saline irrigation alone, to assess the specific benefit of the corticosteroid spray.
Comparison 2: intranasal corticosteroid drops compared to no intervention
One study considered this comparison (Rashid 2021). The intervention comprised intranasal betamethasone sodium phosphate drops (0.1 mg/mL). Three drops were administered to each nasal cavity, three times daily until recovery, for a maximum of one month. This was compared to placebo, comprising 0.9% saline drops, administered with the same regimen. The authors state that participants were recommended "to apply the nasal drops in Mecca position".
Comparison 3: hypertonic saline irrigation compared to no intervention
One three‐arm study considered this comparison (Yildiz 2021). Hypertonic saline (10 mL; tonicity was not reported) was administered to each nostril, twice daily for one month. This was compared to no intervention.
Comparison 4: zinc compared to no intervention
One study compared 220 mg zinc sulphate (50 mg zinc) twice daily to no intervention (Abdelmaksoud 2021).
Outcomes
Presence of normal olfactory function
Assessed by the participants
All of the included studies reported some data regarding the presence of normal olfactory function at follow‐up. However, the methods used by the individual studies varied. Two studies used a form of visual analogue scale and asked participants to rate their own sense of smell, with scores ranging from 0 (complete olfactory loss) to 10 (completely normal smell sensation) (Abdelalim 2021; Kasiri 2021). One study assessed recovery of sense of smell during telephone follow‐up. No information on how participants were asked to judge their sense of smell was provided (Rashid 2021). Two studies only reported the time to recovery of olfactory function (Abdelmaksoud 2021), or duration of olfactory dysfunction (Yildiz 2021). No dichotomous data were reported on the number of participants who had normal olfaction at follow‐up, and it is not clear how participants reported normal olfaction. Yildiz 2021 describe a range of symptom durations up to and including 30 days (the maximum follow‐up for the study), therefore we assume that they have included all participants in this analysis, and set the duration of olfactory dysfunction to 30 days for those who had not recovered by the end of the study. Abdelmaksoud 2021 describes the median duration of symptoms for each group, and reports the inclusion of all participants in the trial for these data. These data could not be included in any meta‐analysis, but are reported narratively in the text of the review.
Assessed using psychophysical testing
Only one of the included studies used psychophysical testing to assess the presence of normal olfactory function. Kasiri 2021 used the Iran Smell Identification Test, an Iranian version of the UPSIT (Takerkhani 2015). It includes 24 different odours, with results ranging from 0 (inability to identify any odours correctly) to 24 (all odours correctly identified). Anosmia was defined as a score of 0 to 9, severe hyposmia as a score of 10 to 13, mild hyposmia as a score of 14 to 18, and normosmia as a score of 19 to 24. We have been unable to identify a widely used minimally important difference (MID) for the UPSIT. A 10% change (four points on the original, 40‐point scale) has been suggested as a possible MID (Patel 2017). An equivalent change on the Iran‐SIT would therefore equal 2.4 points.
Psychophysical testing was not used by the remaining studies (Abdelalim 2021; Abdelmaksoud 2021; Rashid 2021; Yildiz 2021).
Serious adverse effects
Three of the included studies reported that adverse effects of the intervention were assessed (Kasiri 2021; Rashid 2021; Yildiz 2021). One of these studies included a narrative statement to indicate that no adverse effects occurred (Kasiri 2021). The other studies did not report the presence of adverse effects, therefore it is unclear whether no adverse effects occurred, or whether they are simply not reported. Adverse events were not apparently assessed or reported by Abdelalim 2021 or Abdelmaksoud 2021.
Change in sense of smell
Assessed by the participants
Two studies assessed change in sense of smell over the course of the study using a visual analogue scale, as described above (Abdelalim 2021; Kasiri 2021). Yildiz 2021 used a "Self‐rated Olfactory Score" to assess change in the sense of smell. This score is also reported to use a visual analogue scale (0 = no odour at all, 10 = full odour). The authors report that a variety of odours were presented to participants: "Olfactory functions were evaluated by using drinks with sharp smells (e.g., lemonade, coffee), nutrients (lemon, garlic), spices (mint, black pepper, thyme), and some cleaning agents (soap, bleach, menthol) to evaluate the odor separation of patients. The olfactory function was evaluated with self‐ scoring method. All patients were asked to evaluate olfactory function by giving a score of 1–10 (0 = no odor at all, and 10 = full odor)". It is not clear whether this is a global rating that considers all of the odours presented, or whether there was a method to combine the ratings for different odours. The scores appear to be rated on a scale from 0 to 10. Abdelmaksoud 2021 and Rashid 2021 did not assess subjective change in sense of smell.
Assessed using psychophysical testing
Only one of the included studies used psychophysical testing to assess the change in sense of smell (Kasiri 2021). The method used is described above. Psychophysical testing was not used by the remaining studies (Abdelalim 2021; Abdelmaksoud 2021; Rashid 2021; Yildiz 2021).
Prevalence of parosmia
None of the included studies assessed this outcome.
Change in sense of taste
None of the included studies assessed this outcome.
Disease‐related quality of life
Yildiz 2021 stated that the "Subjective Olfactory Capability’’ (SOC) method was used to evaluate "self‐reported olfactory function and olfaction‐related quality of life". However, no data were reported regarding quality of life, and the description of the SOC method indicates that it considers odour identification only, not quality of life.
Other adverse effects (including nosebleeds/bloody discharge)
Three of the included studies reported that adverse effects of the intervention were assessed (Kasiri 2021; Rashid 2021; Yildiz 2021). However, none of the studies reported on the presence of adverse effects, therefore it is unclear whether no adverse effects occurred, or whether they are simply not reported. Adverse events were not apparently assessed or reported by Abdelalim 2021 or Abdelmaksoud 2021.
Excluded studies
We excluded 45 studies (47 references) from the review. We present the main reasons for the exclusion of the studies below, although some studies had multiple reasons for exclusion:
Twenty‐six studies assessed the wrong population:
11 of these studies included all individuals with a diagnosis of COVID‐19, not just those with olfactory dysfunction (ACTION (NCT04332107); COPPS (NCT04662060); COVIDAtoZ (NCT04342728); CTRI/2020/08/027477; NCT04414124; NCT04458519; NCT04474483; NCT04513184; NCT04622891; NCT04662086; NCT04916639);
a further 13 studies included participants with more than four weeks of olfactory dysfunction prior to enrolment (COVIDORL (NCT04361474)); D'Ascanio 2021; IRCT20200522047542N1; IRCT20210708051817N1; NCT04853836; NCT04952389; NCT04964414; NCT05037110; NL9635; Odorat‐Covid (NCT04598763); SCENT2 (NCT04789499); Vaira 2021a; VOLT (NCT04710394));
two studies included participants with any post‐viral olfactory disturbance, not specifically COVID‐19 (Klug 2021; NCT04406584).
Twelve studies were not randomised controlled trials (Bulbuloglu 2021; IRCT20180205038619N2; IRCT20200629047953N1; Islek 2021; Le Bon 2021; NCT04382547; NCT04427332; NCT04806880; NCT04830943; Saussez 2021; Singh 2021; Varricchio 2021).
Two articles were narrative reviews, without any primary data (Begam 2020; Vroegop 2020).
Three articles were letters to a journal editor, without any primary data (Patel 2021; Pinna 2020; Vaira 2021c).
Finally, two studies would have been relevant for this review, but the studies were withdrawn prior to any participant enrolment (Co‐STAR (NCT04422275); NCT04374474).
Risk of bias in included studies
Many of the included studies lacked detailed description of their methods, resulting in a large number of bias domains being assessed as 'unclear' risk of bias. Where methods were reported fully, we had concerns over performance and detection bias in three studies ‐ due to a lack of blinding of participants and personnel to the allocated intervention. See Figure 2.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Abdelalim 2021 described using random allocation, but did not provide further details of the method used, or details regarding concealment of the allocation sequence. Correspondence with the study authors confirmed that an adequate method was used for randomisation (simple randomisation, using drawing of lots). The remaining four studies did not provide details on their methods for randomisation, or methods used to conceal group allocation.
Blinding
Abdelalim 2021, Abdelmaksoud 2021 and Yildiz 2021 were open‐label studies with no placebo group. All of these studies considered self‐reported olfactory function as an outcome measure, therefore we judged these to be at high risk of performance and detection bias.
Kasiri 2021 used a placebo (topical saline) to blind participants to their group allocation. However, although the authors reported that the study was 'double‐blind' there is no information regarding how outcome assessors were masked to the group allocation. We have therefore judged the risk of detection bias as unclear.
Rashid 2021 included a placebo arm who received isotonic saline drops (as compared to intranasal saline drops). The outcome measures were all reported by the (blinded) participants, therefore we considered this trial to be at low risk of detection bias.
Incomplete outcome data
Most of the studies reported either complete follow‐up of all participants, or few dropouts, with balance in loss to follow‐up between the groups. Therefore we considered the risk of attrition bias to be low. Only one study did not report on the number of participants who were lost to follow‐up (Yildiz 2021), and we therefore judged it to be at unclear risk of attrition bias.
Selective reporting
We were able to identify a registered protocol for Abdelalim 2021, and the outcomes were reported according to the trial registration, therefore we judged this at low risk of reporting bias.
We identified a published protocol for Kasiri 2021 and Rashid 2021. However, these protocols were registered retrospectively, therefore it was not possible to determine whether the reported outcomes aligned with the original analysis plan.
We could not identify a published protocol for the remaining studies, therefore judged them to be at unclear risk of selective reporting bias.
Other potential sources of bias
We did not detect any additional potential sources of bias for Abdelalim 2021. Three studies did not provide sufficient details regarding the methods of the study to adequately assess the risk of other bias (Abdelmaksoud 2021; Kasiri 2021; Rashid 2021).
We considered one study at high risk of bias due to a lack of information on the methods used to assess olfactory function ‐ the primary outcome for the trial (Yildiz 2021). The authors reported the use of a "subjective olfactory capability score" but it is not clear whether the odours used were the same for all participants, or how participants would score their olfactory function. As this outcome was of primary importance to both the study authors, and to this review, we considered this lack of detail to have the potential to create bias in the reported result.
Effects of interventions
Comparison 1: Intranasal corticosteroids compared to no intervention
Three studies compared an intranasal corticosteroid spray to either no intervention or an isotonic saline spray. See Table 1.
Presence of normal olfactory function
As assessed by the participants
At ≤ 4 weeks
One study reported on this outcome (Abdelalim 2021). Recovery of sense of smell was assessed using a visual analogue scale (VAS) of 0 to 10, where 0 represented total loss of smell and 10 represented completely normal smell sensation. At three weeks follow‐up, 31 out of 50 participants in the intranasal corticosteroid group reported completely normal smell sensation, compared to 26 out of 50 in the control group (we assume that this equates to a score of 10 on the VAS). The evidence is very uncertain as to whether intranasal corticosteroids affect the number of people who report completely normal smell sensation at up to four weeks, given the small number of participants included and the wide confidence intervals around the effect (risk ratio (RR) 1.19, 95% confidence interval (CI) 0.85 to 1.68; 1 study; 100 participants; very low‐certainty evidence; Analysis 1.1). All participants in this study also received olfactory training, regardless of their group allocation.
1.1. Analysis.

Comparison 1: Intranasal steroid spray compared to no intervention/placebo, Outcome 1: Presence of normal olfactory function (as assessed by participants)
At > 4 weeks to 3 months
This was not assessed or reported as a dichotomous outcome (i.e. the number of participants who had normal olfactory function at follow‐up). The authors of Yildiz 2021 did report on the median duration of symptoms in each group, which we presume to be the time until self‐reported complete recovery, measured over a period of 30 days. Participants receiving intranasal corticosteroids reported a shorter duration of symptoms by a mean of 6.5 days (95% CI from 7.58 days shorter to 5.42 days shorter; 1 study; 100 participants; very low‐certainty evidence; Analysis 1.2).
1.2. Analysis.

Comparison 1: Intranasal steroid spray compared to no intervention/placebo, Outcome 2: Duration of olfactory dysfunction
No data were reported for later time points of interest in this review.
Presence of normal olfactory function
As assessed by psychophysical testing
At ≤ 4 weeks
One study reported on this outcome (Kasiri 2021). Olfactory function was assessed using the Iranian version of the UPSIT (range 0 to 24), and a score of ≥ 19 was considered to represent normal olfactory function. At four weeks of follow‐up, 19 out of 39 participants in the intervention group had normal olfactory function, compared to 8 out of 38 in the control group, giving a RR of 2.31 (95% CI 1.16 to 4.64; 1 study; 77 participants; very low‐certainty evidence; Analysis 1.3). Intranasal corticosteroids may increase the number of people who have normal olfactory function when assessed using psychophysical tests, but the evidence is very uncertain.
1.3. Analysis.

Comparison 1: Intranasal steroid spray compared to no intervention/placebo, Outcome 3: Presence of normal olfactory function (as assessed with psychophysical testing)
No data were reported for later time points of interest in this review.
Serious adverse effects
Kasiri 2021 stated that "no side effects were reported during the study" but it is unclear whether these were systematically assessed and recorded as part of the study. The remaining studies did not report any information regarding adverse effects.
Change in sense of smell
As assessed by the participants
At ≤ 4 weeks
One study reported the mean change in sense of smell as assessed using a VAS (0 to 10, higher scores mean better olfactory ability) (Kasiri 2021). The mean change in those receiving corticosteroid spray was 0.5 points lower than the change in those receiving isotonic saline spray (95% CI 1.38 points lower to 0.38 points higher; 1 study; 77 participants; very low‐certainty evidence; Analysis 1.4).
1.4. Analysis.

Comparison 1: Intranasal steroid spray compared to no intervention/placebo, Outcome 4: Change in sense of smell (as assessed by participants)
Change in sense of smell was also reported by Abdelalim 2021 according to a VAS of 0 to 10. An estimate of the change in sense of smell was not available ‐ the only data reported were endpoint data, comparing the median sense of smell in the two groups after the treatment period (three weeks). As the data were reported as median values no effect estimate could be calculated. Those receiving corticosteroids had a median sense of smell score of 10 (interquartile range (IQR) 9 to 10) and those not receiving corticosteroids had a median score of 10 (IQR 5 to 10) (P = 0.16; 1 study; 100 participants; very low‐certainty evidence). All participants in this study also received olfactory training, regardless of their group allocation.
As assessed by the participants
At > 4 weeks to 3 months
One study reported the sense of smell at the endpoint of the trial, as assessed using a VAS (Yildiz 2021). At 30 days the VAS score in those receiving corticosteroid spray with saline irrigation was 2.40 points higher than that in those receiving saline irrigation alone (95% CI 1.32 points higher to 3.48 points higher; 1 study; 100 participants; very low‐certainty evidence; Analysis 1.4).
No data were reported for later time points of interest in this review.
Change in sense of smell
As assessed by psychophysical testing
At ≤ 4 weeks
One study reported the mean change in sense of smell as assessed with the Iranian version of the UPSIT (Kasiri 2021). The mean change in the corticosteroid group was 0.2 points higher than those in the control group (95% CI 2.06 points lower to 2.06 points higher; 1 study; 77 participants; low‐certainty evidence; Analysis 1.5). Corticosteroid sprays may result in little or no difference to the change in sense of smell (when measured with psychophysical testing).
1.5. Analysis.

Comparison 1: Intranasal steroid spray compared to no intervention/placebo, Outcome 5: Change in sense of smell (as assessed with psychophysical testing)
Prevalence of parosmia
This was not assessed or reported.
Change in sense of taste
This was not assessed or reported.
Disease‐related quality of life
The authors of Yildiz 2021 state that the "Subjective Olfactory Capability" method was used to evaluate self‐reported olfactory function and olfaction‐related quality of life. However, no data were reported that related to quality of life.
Other adverse effects
These were not assessed or reported.
Comparison 2: Intranasal corticosteroid drops compared to placebo
One study compared intranasal corticosteroid drops to normal saline (placebo) drops (Rashid 2021). See Table 2.
Presence of normal olfactory function
As assessed by the participants
At > 4 weeks to 3 months
Self‐reported recovery of sense of smell was assessed at 30 days of follow‐up. No details were provided regarding how participants were asked about their olfactory function. Out of 123 participants in the intervention group 103 reported normal olfactory function at follow‐up, compared to 105 out of 125 in the placebo group (RR 1.00, 95% CI 0.89 to 1.11; 1 study; 248 participants; low‐certainty evidence; Analysis 2.1). Intranasal corticosteroid drops may make little or no difference to the presence of normal olfactory function at > 4 weeks to 3 months.
2.1. Analysis.

Comparison 2: Intranasal steroid drops compared to placebo, Outcome 1: Presence of normal olfactory function at > 4 weeks to 3 months (as assessed by participants)
No data were reported for other time points of interest in this review.
Presence of normal olfactory function
As assessed by psychophysical testing
This was not assessed or reported.
Serious adverse effects
These were not assessed or reported.
Change in sense of smell
This was not assessed or reported.
Prevalence of parosmia
This was not assessed or reported.
Change in sense of taste
This was not assessed or reported.
Disease‐related quality of life
This was not assessed or reported.
Other adverse effects
These were not assessed or reported.
Comparison 3: Intranasal hypertonic saline irrigation compared to no treatment
One three‐arm study included a comparison of intranasal hypertonic saline irrigation to no treatment (Yildiz 2021). See Table 3.
1. Intranasal hypertonic saline spray compared to no intervention for the prevention of persistent post‐COVID‐19 olfactory dysfunction.
| Intranasal hypertonic saline spray compared to no intervention for the prevention of persistent post‐COVID‐19 olfactory dysfunction | ||||||
| Patient or population: participants with acute olfactory dysfunction related to COVID‐19 Setting: inpatients in a single hospital in Turkey Intervention: intranasal hypertonic saline irrigation Comparison: no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with intranasal saline spray | |||||
| Presence of normal olfactory function | This was not assessed or reported by the study included in the review. | |||||
| Serious adverse effects | These were not assessed or reported by the study included in the review. | |||||
| Change in sense of smell Assessed by participants (VAS, range 0 to 10, higher = better) > 4 weeks to 3 months |
The mean change in sense of smell was 5.2 points | MD 0.9 points higher (0.02 higher to 1.78 higher) | — | 100 (1 RCT) | ⊕⊝⊝⊝ very low1 2 | No minimally important difference has been reported. We considered that a difference of 0.9 points was likely to be of borderline importance to participants, but the evidence is very uncertain. |
| Prevalence of parosmia | This was not assessed or reported by the study included in the review. | |||||
| Change in sense of taste | This was not assessed or reported by the study included in the review. | |||||
| Disease‐related quality of life | This was not assessed or reported by the study included in the review. | |||||
| Other adverse effects | These were not assessed or reported by the study included in the review. | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; VAS: visual analogue scale | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Very serious risk of performance and detection bias, due to lack of blinding. Serious risk of other bias due to lack of clarity on methods of assessing olfactory ability. We judged all other domains at unclear risk of bias due to lack of information.
2Serious imprecision as sample size fails to meet optimal information size (taken to be 400 participants, as a rule of thumb).
3Serious indirectness as the outcome of interest (the number of participants who have normal olfactory function) was not reported.
Presence of normal olfactory function
This was not assessed or reported as a dichotomous outcome (i.e. the number of participants who had normal olfactory function at follow‐up). The authors did report on the median duration of symptoms in each group, which we presume to be the time until self‐reported complete recovery, measured over a period of 30 days. Participants receiving hypertonic saline irrigation reported a shorter duration of symptoms by a mean of 3.1 days when compared to those receiving no treatment (95% CI from 3.98 days shorter to 2.22 days shorter; 1 study; 100 participants; very low‐certainty evidence; Analysis 3.1).
3.1. Analysis.

Comparison 3: Intranasal hypertonic saline spray compared to no intervention, Outcome 1: Duration of olfactory dysfunction
Serious adverse effects
These were not assessed or reported.
Change in sense of smell
As assessed by the participants
At > 4 weeks to 3 months
Self‐reported change in sense of smell was assessed at 30 days of follow‐up. Participants were asked to score their own olfactory function using a VAS of 0 to 10 (0 = no odour at all, 10 = full odour). The mean change in sense of smell was 0.9 points higher in those who had received intranasal saline irrigation, as compared to those who did not receive any treatment (95% CI 0.02 points higher to 1.78 points higher; 1 study; 100 participants; very low‐certainty evidence; Analysis 3.2).
3.2. Analysis.

Comparison 3: Intranasal hypertonic saline spray compared to no intervention, Outcome 2: Change in sense of smell (as assessed by participants)
No data were reported for other time points of interest in this review.
Prevalence of parosmia
This was not assessed or reported.
Change in sense of taste
This was not assessed or reported.
Disease‐related quality of life
The authors state that the "Subjective Olfactory Capability" method was used to evaluate self‐reported olfactory function and olfaction‐related quality of life. However, no data were reported that related to quality of life.
Other adverse effects
These were not assessed or reported.
Comparison 4: Zinc sulphate compared to no treatment
One study assessed this comparison (Abdelmaksoud 2021). We presume that the intervention was administered orally, but this is not explicit from the article. See Table 4.
2. Zinc sulphate compared to no intervention for the prevention of persistent post‐COVID‐19 olfactory dysfunction.
| Zinc sulphate compared to no intervention for the prevention of persistent post‐COVID‐19 olfactory dysfunction | ||||||
| Patient or population: participants with olfactory dysfunction related to COVID‐19 Setting: inpatients in a single centre in Egypt Intervention: zinc sulphate Comparison: no intervention | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no intervention | Risk with zinc | |||||
| Presence of normal olfactory function | This was not assessed or reported by the study included in the review. | |||||
| Serious adverse effects | These were not assessed or reported by the study included in the review. | |||||
| Change in sense of smell | This was not assessed or reported by the study included in the review. | |||||
| Prevalence of parosmia | This was not assessed or reported by the study included in the review. | |||||
| Change in sense of taste | This was not assessed or reported by the study included in the review. | |||||
| Disease‐related quality of life | This was not assessed or reported by the study included in the review. | |||||
| Other adverse effects | These were not assessed or reported by the study included in the review. | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
Presence of normal olfactory function
This was not assessed or reported as a dichotomous outcome (i.e. the number of participants who had normal olfactory function at follow‐up). The authors do report on the median duration of symptoms in each group, which we presume to be the time until self‐reported complete recovery. This was reported as a median of 7 days (interquartile range (IQR) 5 to 9 days) in the intervention group, and a median of 18 days (IQR 14 to 22 days) in the control group, with a P value of < 0.001 (1 study; 105 participants; very low‐certainty evidence).
Serious adverse effects
These were not assessed or reported.
Change in sense of smell
This was not assessed or reported.
Prevalence of parosmia
This was not assessed or reported.
Change in sense of taste
This was not assessed or reported.
Disease‐related quality of life
This was not assessed or reported.
Other adverse effects
These were not assessed or reported.
Discussion
Summary of main results
This review includes five studies that have assessed the use of different interventions in the prevention of persisting olfactory dysfunction related to COVID‐19. Three studies assessed nasal corticosteroid sprays (Abdelalim 2021; Kasiri 2021; Yildiz 2021). Yildiz 2021 also considered hypertonic saline irrigation. One study assessed the use of nasal corticosteroid drops (Rashid 2021) and one study assessed the use of zinc (Abdelmaksoud 2021).
Intranasal corticosteroid spray compared to no intervention/placebo
Three studies considered the use of nasal corticosteroid sprays (Abdelalim 2021; Kasiri 2021; Yildiz 2021). The studies included in these analyses all followed participants for a maximum of 30 days, so we do not have any information on the efficacy or harms of treatment after this time point.
The evidence is very uncertain as to whether intranasal corticosteroid spray changes the number of people who have normal olfactory function at follow‐up, either when self‐assessed or when assessed using psychophysical tests. The evidence is also very uncertain regarding whether people perceive their sense of smell to have changed following treatment, although intranasal corticosteroid spray may have little to no effect on the change in sense of smell as measured with psychophysical testing. The evidence is very uncertain about the occurrence of adverse events with intranasal corticosteroids, as only one study reported this outcome, and simply stated that no adverse events occurred in either group; however, the number of participants is too small for us to assess this accurately.
No data were reported regarding the impact of intranasal corticosteroids on the prevalence of parosmia, the change in sense of taste or on disease‐related quality of life.
Intranasal corticosteroid drops compared to placebo
A single study assessed this comparison (Rashid 2021). This study also followed up participants for one month, so we do not have any evidence at a later time point.
Intranasal corticosteroid drops may make little to no difference to the presence of normal olfactory function at 30 days of follow‐up, as assessed by participants themselves. However, no data were available regarding psychophysical testing for normal olfaction.
There were also no data for any of the other primary or secondary outcomes included in this review (including serious adverse events, change in sense of smell, prevalence of parosmia, change in sense of taste, disease‐related quality of life and other adverse effects).
Intranasal hypertonic saline compared to no intervention
One study assessed this comparison (Yildiz 2021). The evidence is very uncertain as to whether hypertonic saline affects the presence of normal olfactory function or the change in sense of smell at follow‐up, as assessed by the participants themselves. There were no data regarding psychophysical testing for these outcomes.
There were also no data regarding the other outcomes of interest in this review (serious adverse events, prevalence of parosmia, change in sense of taste, disease‐related quality of life and other adverse effects).
Zinc sulphate compared to no intervention
One study assessed this comparison (Abdelmaksoud 2021). The evidence is very uncertain as to whether zinc sulphate affects the presence of normal olfactory function as assessed by the participants themselves. There were no data regarding psychophysical testing for this outcome.
There were also no data regarding the other outcomes of interest in this review (serious adverse events, change in sense of smell, prevalence of parosmia, change in sense of taste, disease‐related quality of life and other adverse effects).
Overall completeness and applicability of evidence
Although the number of studies included in this living systematic review has increased since the first version was published, the amount of evidence for interventions to prevent persisting olfactory dysfunction following COVID‐19 infection is still very limited.
We were unable to identify any evidence for a number of our primary and secondary outcome measures. Importantly, the data for adverse effects were very sparse. A single study provided evidence regarding adverse events, and it was not clear whether these had been systematically assessed and recorded during the study. With any intervention, any expected benefits must be compared to the potential harms, and we would encourage all study authors to assess and report adverse effects systematically to enable informed decisions regarding the use of treatment. However, if the adverse effect profile for intranasal corticosteroids is similar to that seen when they are used for other sinonasal disease, then the adverse events are likely to be modest. They may include epistaxis, gastrointestinal disturbance and headache (Demoly 2008). Systemic effects are thought to be rare (Allen 2000).
The outcome measures used by the individual studies varied, and the primary and secondary outcomes of interest in this review were often not reported. In particular, study authors rarely assessed both self‐reported olfactory function and psychophysical tests of the sense of smell. As it is recognised that there is often a discrepancy between these measures (Welge‐Luessen 2005), we considered that both methods were of importance when assessing the potential benefit of interventions.
Our primary outcome for this review was the presence of normal olfactory function, which we aimed to assess as a dichotomous outcome ‐ to compare the number of people who recovered in each group. However, two studies did not report on the number of individuals who recovered, and instead reported on the time to recovery (Abdelmaksoud 2021; Yildiz 2021). We considered that this was a similar outcome, and gives some useful data regarding the recovery in each group. However, this is based on the assumption that all participants were included in the analysis, and the "time to recovery" for those who did not recover was set to the maximum follow‐up time for the study. We have attempted to contact the authors of both of these studies, but are awaiting a response.
The sense of smell is also important to distinguish flavour ‐ whilst the true tastes of sweet, sour, salty, bitter and umami can be sensed with the tongue, awareness of different flavours requires a functioning olfactory system. Consequently, changes in olfactory function are typically accompanied by altered flavour perception. Assessment of taste using self‐reporting is challenging (due to the need to distinguish between true taste and retronasal olfaction) and there is a lack of widespread use of psychophysical testing methods, which are needed to determine the accurate picture of olfactory and gustatory performance. Therefore, we have focused predominantly on the sense of smell for this review, but we acknowledge that an impaired sense of taste may be a real or perceived issue for many individuals who are recovering from COVID‐19.
Quality of the evidence
We judged the certainty of the evidence to be low or very low for all outcomes assessed. This was predominantly due to the risk of bias in the estimates of effect, and imprecision in the results.
There were a number of concerns regarding the risk of bias across the studies included in the review. Most of the studies were either open‐label, or did not confirm that outcome assessors were masked to group allocation. Where outcome measures can be very subjective (and reported by the participants themselves, such as olfactory function) it is especially important to mask participants and outcome assessors to group allocation, in order to avoid performance or detection bias.
Most of the studies included a relatively small number of participants (from 80 to 150). Furthermore, as few studies assessed the same outcome for the same comparison, we were unable to perform any meta‐analyses in the review. This has led to imprecision in the effect estimates, so the confidence intervals for the effect estimates are wide, leading to uncertainty in the evidence.
Potential biases in the review process
This review is one of a pair that address the prevention and treatment of olfactory dysfunction related to COVID‐19. Therefore, we excluded studies from this review if participants had more than four weeks of olfactory disturbance at baseline ‐ these studies are included in the companion review on treatment of olfactory dysfunction (O'Byrne 2022). We considered that this was an appropriate distinction, due to the high rate of resolution of olfactory dysfunction in the first four weeks after COVID‐19 infection. However, in the course of conducting the review we noted that few studies explicitly stated the duration of symptoms (or time since diagnosis) for participants in the trial. This was stated by only one of the five included studies (Rashid 2021), where all participants had symptoms for ≤ 15 days at the start of the study. Contact with the study authors confirmed that this was also the case for Abdelalim 2021, where all participants had olfactory disturbance for between 10 and 28 days. For the remaining three studies we have inferred that participants were in the early stages of COVID‐19 infection, and were therefore likely to have had olfactory disturbance for fewer than four weeks. This was either because participants were reported to have other symptoms of COVID‐19 (such as fever or cough, suggestive of the acute phase of infection), or because participants were hospitalised with COVID‐19. We acknowledge that this may not be accurate, and that some participants may have had symptoms for a longer period of time, which could bias the results of this review. We have attempted to contact the authors of these studies to clarify the inclusion criteria, but have had no response.
The studies included in this review all followed up participants for a relatively short time, with a maximum follow‐up period of 30 days. Interpretation of this short‐term follow‐up is challenging. People with COVID‐19 may have some conductive olfactory loss in the acute phase of the illness, due to inflammation of the lining of the nose. However, the persistent olfactory disturbance related to COVID‐19 is thought to have a different pathogenic mechanism. Nonetheless, some interventions in this review may have effects on conductive causes, leading to a perceived short‐term improvement in symptoms. This may not necessarily result in improvement in long‐term outcomes.
A limitation of this review is the focus on studies where all participants had olfactory dysfunction at baseline. Whilst these are the population of interest, additional evidence for the prevention of persisting olfactory dysfunction may be available from studies of other interventions for COVID‐19. We are aware that many studies will have enrolled participants with COVID‐19 (regardless of the presence of olfactory dysfunction at baseline) and may have reported on olfactory outcomes. These studies are excluded from this review, as the overall population do not adhere to the inclusion criteria. However, they may provide additional evidence of the benefits and harms of interventions for preventing persisting olfactory dysfunction.
Agreements and disagreements with other studies or reviews
We are not aware of any other systematic reviews that consider the prevention of persisting olfactory dysfunction related to COVID‐19, therefore there are no relevant reviews to compare our findings to.
Authors' conclusions
Implications for practice.
At present there are very few data to assess the effects of interventions on preventing persistent olfactory dysfunction following COVID‐19.
We have a small amount of data regarding the use of nasal steroid sprays. At present, most of this is very low‐certainty evidence, so we cannot be sure whether these treatments return olfactory function to normal, improve people's perception of their sense of smell or cause any harms. We did find some low‐certainty evidence that nasal steroid sprays may have little or no effect on the change in sense of smell when measured with psychophysical tests. Many of our outcomes were not assessed by the studies, so we do not have any information regarding the effect of these treatments on parosmia, sense of taste or quality of life.
We identified one study of intranasal steroid drops. We found that this intervention may not change the number of people who feel that their sense of smell has returned to normal. No other outcomes were reported by this study.
The data regarding zinc sulphate and hypertonic saline were even more sparse. We are uncertain whether hypertonic saline irrigation makes any difference to the number of people who consider their olfactory function to be normal, or leads to an improvement in how people rate their sense of smell. The evidence is also very uncertain regarding whether zinc sulphate affects the number of people who recover their sense of smell. No other outcomes were reported by these studies.
As this is a living systematic review, the data will be updated regularly as new evidence becomes available.
Implications for research.
We are aware of a number of ongoing studies that may be relevant for this review on publication. As a living systematic review, we will update this review as new data become available.
Although olfactory disturbance is a common symptom of COVID‐19, the natural course of the disease does have a relatively high spontaneous resolution rate. Therefore, we believe that it is essential for researchers to clearly define the affected population included in their trial, according to the duration of their symptoms. The risks and benefits of treatment in the early stages of olfactory disturbance may be very different to those for individuals with a longer duration of symptoms. This also has an impact on the number of participants required for a meaningful analysis. If the rate of spontaneous resolution of symptoms is high, then large trials might be required to detect a difference between the groups.
We recognise that there may be poor agreement between self‐rated olfactory function and that assessed using psychophysical testing. A recent study demonstrated that only 18% of patients with COVID‐19 self‐reported ongoing olfactory dysfunction at six months' follow‐up (Boscolo‐Rizzo 2021a). However, 60% of participants were shown to have some olfactory impairment on psychophysical testing. Given this discrepancy, we consider it important to assess recovery of the sense of smell using both patient‐reported and psychophysical testing, to better understand the impact of any interventions.
What's new
| Date | Event | Description |
|---|---|---|
| 4 August 2022 | New citation required but conclusions have not changed | Four additional studies have been incorporated into this review (Abdelmaksoud 2021; Kasiri 2021; Rashid 2021; Yildiz 2021). These provide additional data for the comparison of intranasal corticosteroid sprays with placebo/no treatment. They also provide some data on additional interventions: intranasal corticosteroid drops, hypertonic saline irrigation and zinc sulphate. |
| 28 February 2022 | New search has been performed | This is a living systematic review. Latest searches conducted October 2021. |
History
Protocol first published: Issue 3, 2021 Review first published: Issue 7, 2021
Acknowledgements
This review forms part of NIHR132103 ‐ The prevention and treatment of persisting olfactory dysfunction following COVID‐19 infection; a suite of Cochrane living systematic reviews. This study is one of a number of COVID‐19 studies that have been funded by the National Institute for Health Research (NIHR) as part of its Recovery and Learning call, totalling £5.5m in funding, to help better manage current and future waves of the COVID‐19 pandemic and investigate its long‐term impact on the health and care system beyond the acute phase.
This project was also supported by the National Institute for Health Research, via Cochrane Infrastructure, Cochrane Programme Grant or Cochrane Incentive funding to Cochrane ENT. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Evidence Synthesis Programme, NIHR, NHS or the Department of Health.
Lisa O' Byrne, Evidence Synthesis Ireland Fellow, was part‐supported by the Health Research Board (Ireland) and the HSC Public Health Agency (Grant number CBES‐2018‐001) through Evidence Synthesis Ireland/Cochrane Ireland.
The authors would like to extend their sincere thanks to the board members of AbScent and Fifth Sense for their insights and significant contributions to the development of this protocol. We would also like to thank the many individuals affected by smell loss who took the time to complete our surveys, which were invaluable when prioritising outcomes for this review.
The authors would like to acknowledge Lee Yee Chong for her work on generic methods content, some of which has been adapted for use in this review (with permission).
The authors are grateful to Joanne Abbott, Information Specialist with Cochrane Pain, Palliative and Supportive Care, for providing peer review comments on the draft search methods, and Iris Gordon, Information Specialist with Cochrane Eyes & Vision, for providing peer review comments on the update search methods introduced in July 2021.
Lastly, we would like to thank Professor Peter Tugwell, Senior Editor Cochrane MOSS Network, for acting as sign‐off editor for the initial version of this review and Professor Richard Harvey, Cochrane ENT Editor, for acting as sign‐off editor for the August 2022 update.
Editorial and peer reviewer contributions
Cochrane ENT supported the authors in the development of this review.
The following people conducted the editorial process for this article:
Sign‐off Editor (final editorial decision): Professor Peter Tugwell, Senior Editor Cochrane MOSS Network (initial version) and Professor Richard Harvey, Cochrane ENT Editor (2022 update).
Managing Editor (selected peer reviewers, collated peer reviewer comments, provided editorial guidance to authors, edited the article): Jenny Bellorini, Cochrane ENT
Copy Editor (copy editing and production): Jenny Bellorini, Cochrane ENT
Peer reviewers (provided comments and recommended an editorial decision): Richard Rosenfeld and Richard Harvey, Cochrane ENT Editors (clinical/content review); Emma Jackson, Cochrane Airways (consumer review); Iris Gordon, Information Specialist, Cochrane Eyes & Vision (search review). One additional peer reviewer provided clinical peer review, but chose not to be publicly acknowledged.
Appendices
Appendix 1. Update search ‐ date limits
| CENTRAL | ENT Register | COVID‐19 Register | MEDLINE | Embase | WOS | Trial registries via CRS | ClinicalTrials.gov | ICTRP | |
| July 2021 | 16/11/2020_TO_22/07/2021:CRSINCENTRAL AND CENTRAL:TARGET |
All years | NOT Anosmia_202012_COVID Register FID_109833:FOLDER AND COVID19:INREGISTER | 31 limit 30 to ed=20201116‐20210722 32 limit 30 to dt=20201116‐20210722 33 31 or 32 |
limit 63 to dd=20201116‐20210722 | Monthly alerts: 30/12/2020 28/01/2021 24/02/2021 25/03/2021 21/04/2021 20/05/2021 17/06/2021 15/07/2021 |
16/11/2020_TO_22/07/2021:CRSINCENTRAL AND CENTRAL:TARGET |
n/a | n/a |
| August 2021 | 22/06/2021_TO_17/08/2021:CRSINCENTRAL AND CENTRAL:TARGET | All years | Anosmia_202107_COVID Register FID_133410:FOLDER OR "Anosmia_202012_COVID Register FID_109833":FOLDER | 31 limit 30 to ed=20210622‐20210817 32 limit 30 to dt=20210622‐20210817 33 33 31 or 32 |
limit 63 to dd=20210622‐20210817 | Monthly alert: 11/08/2021 |
22/06/2021_TO_17/08/2021:CRSINCENTRAL AND CENTRAL:TARGET | n/a | n/a |
| September 2021 | All years | All years | All years | All years | All years | All years | All years | n/a | n/a |
Appendix 2. New search strategies ‐ July 2021 onwards
Search strategies were designed to identify all relevant studies for a pair of reviews (O'Byrne 2022; Webster 2021b).
| CENTRAL (CRS) | Cochrane ENT Register (CRS) | COVID‐19 Register (CRS) | MEDLINE (Ovid) |
| 1 MESH DESCRIPTOR COVID‐19 EXPLODE ALL AND CENTRAL:TARGET 2 MESH DESCRIPTOR SARS‐CoV‐2 EXPLODE ALL AND CENTRAL:TARGET 3 (("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2)):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 4 ((Wuhan and (coronavirus or "corona virus"))):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 5 (((coronavirus or "corona virus" or COVID) adj3 "2019")):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 6 ((wuhan adj2 (disease or virus))):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 7 ((coronavirus or "corona virus" or COVID) ):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 8 MESH DESCRIPTOR Coronavirus AND CENTRAL:TARGET 9 #7 or #8 AND CENTRAL:TARGET 10 (2020 or 2021 or 2022):YR AND CENTRAL:TARGET 11 #9 AND #10 AND CENTRAL:TARGET 12 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #11 AND CENTRAL:TARGET 13 MESH DESCRIPTOR Olfaction Disorders EXPLODE ALL AND CENTRAL:TARGET 14 (Olfaction or olfactory or Dysosmia* or Parosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 15 (smell* adj6 (disorder* or loss or distort* or alter* or dysfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*)):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 16 (smell* adj6 (prevent* or rehab* or recover* or therap* or train* or retrain*)):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 17 #13 OR #14 OR #15 OR #16 AND CENTRAL:TARGET 18 #17 AND #12 AND CENTRAL:TARGET |
1 MESH DESCRIPTOR COVID‐19 EXPLODE ALL AND INREGISTER 2 MESH DESCRIPTOR SARS‐CoV‐2 EXPLODE ALL AND INREGISTER 3 (("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2)):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER 4 ((Wuhan and (coronavirus or "corona virus"))):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER 5 (((coronavirus or "corona virus" or COVID) adj3 "2019")):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER 6 ((wuhan adj2 (disease or virus))):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER 7 ((coronavirus or "corona virus" or COVID) ):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER 8 MESH DESCRIPTOR Coronavirus AND INREGISTER 9 #7 or #8 AND INREGISTER 10 (2020 or 2021 or 2022):YR AND INREGISTER 11 #9 AND #10 AND INREGISTER 12 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #11 AND INREGISTER 13 MESH DESCRIPTOR Olfaction Disorders EXPLODE ALL AND INREGISTER 14 (Olfaction or olfactory or Dysosmia* or Parosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER 15 (smell* adj6 (disorder* or loss or distort* or alter* or dysfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*)):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER 16 (smell* adj6 (prevent* or rehab* or recover* or therap* or train* or retrain*)):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER 17 #13 OR #14 OR #15 OR #16 AND INREGISTER 18 #17 AND #12 AND INREGISTER 19 * AND CENTRAL:TARGET 20 #18 NOT #19 |
1 MESH DESCRIPTOR Olfaction Disorders EXPLODE ALL AND COVID19:INREGISTER 2 (Olfaction or olfactory or Dysosmia* or Parosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*) AND COVID19:INREGISTER 3 (smell* adj6 (disorder* or loss or distort* or alter* or dysfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*)) AND COVID19:INREGISTER 4 smell* adj6 (prevent* or rehab* or recover* or therap* or train* or retrain*) AND COVID19:INREGISTER 5 #1 OR #2 OR #3 OR #4 6 (interventional):SY AND COVID19:INREGISTER 7 #5 AND #6 |
1 exp COVID‐19/ 2 exp SARS‐CoV‐2/ 3 ("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2).ab,ti. 4 (Wuhan and (coronavirus or "corona virus")).ab,ti. 5 ((coronavirus or "corona virus" or COVID) adj3 "2019").ab,ti. 6 (wuhan adj2 (disease or virus)).ab,ti. 7 ("LAMP assay" or "COVID‐19" or "COVID‐19 drug treatment" or "COVID‐19 diagnostic testing" or "COVID‐19 serotherapy" or "COVID‐19 vaccine" or "severe acute respiratory syndrome coronavirus 2" or "spike protein, SARS‐CoV‐2").os. 8 (coronavirus or "corona virus" or COVID).ab,ti. 9 Coronavirus/ 10 8 or 9 11 limit 10 to yr="2020 ‐Current" 12 1 or 2 or 3 or 4 or 5 or 6 or 7 or 11 13 exp olfaction disorders/ 14 (Olfaction or olfactory or Dysosmia* or Parosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*).ab,ti. 15 (smell* adj6 (disorder* or loss or distort* or alter* or dysfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*)).ab,ti. 16 (smell* adj6 (prevent* or rehab* or recover* or therap* or train* or retrain*)).ab,ti. 17 13 or 14 or 15 or 16 18 12 and 17 19 randomized controlled trial.pt. 20 controlled clinical trial.pt. 21 randomized.ab. 22 placebo.ab. 23 drug therapy.fs. 24 randomly.ab. 25 trial.ab. 26 groups.ab. 27 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 28 exp animals/ not humans.sh. 29 27 not 28 30 18 and 29 |
| Embase (Ovid) | Web of Science Core Collections (Web of Knowledge) | Trial registries (CRS) | Trial registries |
| 1 exp coronavirus disease 2019/ 2 exp severe acute respiratory syndrome coronavirus 2/ 3 ("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2).ab,ti. 4 (Wuhan and (coronavirus or "corona virus")).ab,ti. 5 ((coronavirus or "corona virus" or COVID) adj3 "2019").ab,ti. 6 (wuhan adj2 (disease or virus)).ab,ti. 7 (coronavir* or "corona virus" or COVID).ab,ti. 8 coronaviridae/ or coronavirinae/ or Coronaviridae infection/ or Coronavirus infection/ or exp sars‐related coronavirus/ 9 7 or 8 10 limit 9 to yr="2020 ‐Current" 11 1 or 2 or 3 or 4 or 5 or 6 or 10 12 exp smelling disorder/ 13 (Olfaction or olfactory or Dysosmia* or Parosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*).ab,ti. 14 (smell* adj6 (disorder* or loss or distort* or alter* or dysfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*)).ab,ti. 15 (smell* adj6 (prevent* or rehab* or recover* or therap* or train* or retrain*)).ab,ti. 16 12 or 13 or 14 or 15 17 11 and 16 18 Randomized controlled trial/ 19 Controlled clinical study/ 20 Random$.ti,ab. 21 randomization/ 22 intermethod comparison/ 23 placebo.ti,ab. 24 (compare or compared or comparison).ti. 25 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 26 (open adj label).ti,ab. 27 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 28 double blind procedure/ 29 parallel group$1.ti,ab. 30 (crossover or cross over).ti,ab. 31 ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 32 (assigned or allocated).ti,ab. 33 (controlled adj7 (study or design or trial)).ti,ab. 34 (volunteer or volunteers).ti,ab. 35 human experiment/ 36 trial.ti. 37 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 38 (random$ adj sampl$ adj7 ("cross section$" or questionnaire$1 or survey$ or database$1)).ti,ab. 39 comparative study/ or controlled study/ 40 randomi?ed controlled.ti,ab. 41 randomly assigned.ti,ab. 42 39 or 40 or 41 43 38 not 42 44 Cross‐sectional study/ 45 randomized controlled trial/ or controlled clinical study/ or controlled study/ 46 (randomi?ed controlled or control group$1).ti,ab. 47 45 or 46 48 44 not 47 49 (((case adj control$) and random$) not randomi?ed controlled).ti,ab. 50 (Systematic review not (trial or study)).ti. 51 (nonrandom$ not random$).ti,ab. 52 Random field$.ti,ab. 53 (random cluster adj3 sampl$).ti,ab. 54 (review.ab. and review.pt.) not trial.ti. 55 we searched.ab. 56 review.ti. or review.pt. 57 55 and 56 58 update review.ab. 59 (databases adj4 searched).ab. 60 (rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys or trout or marmoset$1).ti. and animal experiment/ 61 43 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 57 or 58 or 59 62 37 not 61 63 17 and 62 |
# 13 #12 AND #11 Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 12 TS=((randomised OR randomized OR randomisation OR randomisation OR placebo* OR (random* AND (allocat* OR assign*) ) OR (blind* AND (single OR double OR treble OR triple) ))) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 11 #10 AND #6 Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 10 #9 OR #8 OR #7 Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 9 TS=(smell* NEAR/6 (prevent* or rehab* or recover* or therap* or train* or retrain*) ) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 8 TS=(smell* NEAR/6 (disorder* or loss or distort* or alter* or dysfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*) ) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 7 TS=(Olfaction or olfactory or Dysosmia* or Parosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 6 #5 OR #4 OR #3 OR #2 OR #1 Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 5 TS=(coronavirus or "corona virus" or COVID) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 4 TOPIC: (wuhan NEAR/2 (disease or virus) ) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 3 TS=(((coronavirus or "corona virus" or COVID) NEAR/3 "2019")) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 2 TS=(Wuhan and (coronavirus or "corona virus") ) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years # 1 TS=("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2) Indexes=SCI‐EXPANDED, CPCI‐S Timespan=All years | 1 (("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2)) AND CENTRAL:TARGET 2 ((Wuhan and (coronavirus or "corona virus"))) AND CENTRAL:TARGET 3 (((coronavirus or "corona virus" or COVID) adj3 "2019")) AND CENTRAL:TARGET 4 ((wuhan adj2 (disease or virus))) AND CENTRAL:TARGET 5 (coronavirus or "corona virus" or COVID) AND CENTRAL:TARGET 6 (2020 or 2021 or 2022):YR AND CENTRAL:TARGET 7 #5 AND #6 AND CENTRAL:TARGET 8 #1 OR #2 OR #3 OR #4 OR #7 AND CENTRAL:TARGET 9 (Olfaction or olfactory or Dysosmia* or Parosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia* or smell*) AND CENTRAL:TARGET 10 #8 AND #9 AND CENTRAL:TARGET 11 http*:SO AND CENTRAL:TARGET 12 (NCT0* or ACTRN* or ChiCTR* or DRKS* or EUCTR* or eudract* or IRCT* or ISRCTN* or JapicCTI* or JPRN* or NTR0* or NTR1* or NTR2* or NTR3* or NTR4* or NTR5* or NTR6* or NTR7* or NTR8* or NTR9* or SRCTN* or UMIN0*):AU AND CENTRAL:TARGET 13 #12 OR #11 AND CENTRAL:TARGET 14 #10 AND #13 AND CENTRAL:TARGET |
ClinicalTrials.gov ( COVID‐19 OR 2019‐nCoV OR SARS‐CoV‐2 OR 2019 novel coronavirus OR severe acute respiratory syndrome coronavirus 2 OR Wuhan coronavirus OR coronavirus ) AND ( anosmia OR smell OR Olfaction or olfactory ) | Interventional Studies ICTRP (covid* OR 2019‐nCoV OR SARS‐CoV‐2) AND (anosmia OR smell OR Olfaction OR olfactory OR Dysosmia* OR Paraosmia* OR Anosmia* OR hyposmia* OR phantosmia* OR Cacosmia* OR microsmia*) |
Appendix 3. Search strategies December 2020
CENTRAL (CRS)
1 (("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2)):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 2844
2 ((Wuhan and (coronavirus or "corona virus"))):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 124
3 (((coronavirus or "corona virus" or COVID) adj3 "2019")):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 582
4 ((wuhan adj2 (disease or virus))):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 4
5 ((coronavirus or "corona virus" or COVID) ):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 2919
6 (2020 or 2021):YR AND CENTRAL:TARGET 63399
7 #5 AND #6 AND CENTRAL:TARGET 2801
8 #1 OR #2 OR #3 OR #4 OR #7 AND CENTRAL:TARGET 2877
9 MESH DESCRIPTOR Olfaction Disorders EXPLODE ALL AND CENTRAL:TARGET 118
10 (Olfaction or olfactory or Dysosmia* or Paraosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 1201
11 (smell* adj6 (disorder* or loss or distort* or alter* or dsyfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*)):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 424
12 (smell* adj6 (prevent* or rehab* or recover* or therap* or train* or retrain*)):AB,EH,KW,KY,MC,MH,TI,TO AND CENTRAL:TARGET 151
13 #9 OR #10 OR #11 OR #12 AND CENTRAL:TARGET 1474
14 #13 AND #8 AND CENTRAL:TARGET 34
MEDLINE (Ovid)
1 ("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2).ab,ti. 64357
2 (Wuhan and (coronavirus or "corona virus")).ab,ti. 2686
3 (coronavirus or "corona virus" or COVID) adj3 "2019").ab,ti. 14622
4 (wuhan adj2 (disease or virus)).ab,ti. 69
5 ("LAMP assay" or "COVID‐19" or "COVID‐19 drug treatment" or "COVID‐19 diagnostic testing" or "COVID‐19 serotherapy" or "COVID‐19 vaccine" or "severe acute respiratory syndrome coronavirus 2" or "spike protein, SARS‐CoV‐2").os. 27706
6 (coronavirus or "corona virus" or COVID).ab,ti. 73711
7 limit 6 to yr="2020 ‐Current" 64172
8 1 or 2 or 3 or 4 or 5 or 7 68776
9 exp olfaction disorders/ 4393
10 (Olfaction or olfactory or Dysosmia* or Paraosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*).ab,ti. 49706
11 (smell* adj6 (disorder* or loss or distort* or alter* or dsyfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*)).ab,ti. 2401
12 (smell* adj6 (prevent* or rehab* or recover* or therap* or train* or retrain*)).ab,ti. 180
13 9 or 10 or 11 or 12 51681
14 8 and 13 768
15 randomized controlled trial.pt. 516072
16 controlled clinical trial.pt. 93905
17 randomized.ab. 496684
18 placebo.ab. 212020
19 drug therapy.fs. 2246822
20 randomly.ab. 343595
21 trial.ab. 525027
22 groups.ab. 2108399
23 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 4824610
24 exp animals/ not humans.sh. 4750713
25 23 not 24 4189853
26 14 and 25 72
Cochrane COVID‐19 Study Register (CRS)
1 MESH DESCRIPTOR Olfaction Disorders EXPLODE ALL AND COVID19:INREGISTER 5
2 (Olfaction or olfactory or Dysosmia* or Paraosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*) AND COVID19:INREGISTER 392
3 (smell* adj6 (disorder* or loss or distort* or alter* or dsyfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*)) AND COVID19:INREGISTER 180
4 (smell* adj6 (prevent* or rehab* or recover* or therap* or train* or retrain*)) AND COVID19:INREGISTER 17
5 #1 OR #2 OR #3 OR #4 483
6 (interventional):SY AND COVID19:INREGISTER 3460
7 #6 AND #5 37
Cochrane ENT Register (CRS)
1 (("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2)):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER
2 ((Wuhan and (coronavirus or "corona virus"))):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER
3 (((coronavirus or "corona virus" or COVID) adj3 "2019")):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER
4 ((wuhan adj2 (disease or virus))):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER
5 ((coronavirus or "corona virus" or COVID) ):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER
6 (2020 or 2021):YR AND INREGISTER
7 #5 AND #6 AND INREGISTER
8 #1 OR #2 OR #3 OR #4 OR #7 AND INREGISTER
9 MESH DESCRIPTOR Olfaction Disorders EXPLODE ALL AND INREGISTER
10 (Olfaction or olfactory or Dysosmia* or Paraosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER
11 (smell* adj6 (disorder* or loss or distort* or alter* or dsyfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*)):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER
12 (smell* adj6 (prevent* or rehab* or recover* or therap* or train* or retrain*)):AB,EH,KW,KY,MC,MH,TI,TO AND INREGISTER
13 #9 OR #10 OR #11 OR #12 AND INREGISTER
14 #13 AND #8 AND INREGISTER
Embase (Ovid)
1 ("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2).ab,ti.
2 (Wuhan and (coronavirus or "corona virus")).ab,ti.
3 ((coronavirus or "corona virus" or COVID) adj3 "2019").ab,ti.
4 (wuhan adj2 (disease or virus)).ab,ti.
5 (coronavirus or "corona virus" or COVID).ab,ti.
6 limit 5 to yr="2020 ‐Current"
7 1 or 2 or 3 or 4 or 6
8 exp smelling disorder/
9 (Olfaction or olfactory or Dysosmia* or Paraosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*).ab,ti.
10 (smell* adj6 (disorder* or loss or distort* or alter* or dsyfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*)).ab,ti.
11 (smell* adj6 (prevent* or rehab* or recover* or therap* or train* or retrain*)).ab,ti.
12 8 or 9 or 10 or 11
13 7 and 12
14 Randomized controlled trial/
15 Controlled clinical study/
16 Random$.ti,ab.
17 randomization/
18 intermethod comparison/
19 placebo.ti,ab.
20 (compare or compared or comparison).ti.
21 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab.
22 (open adj label).ti,ab.
23 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab.
24 double blind procedure/
25 parallel group$1.ti,ab.
26 (crossover or cross over).ti,ab.
27 ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab.
28 (assigned or allocated).ti,ab.
29 (controlled adj7 (study or design or trial)).ti,ab.
30 (volunteer or volunteers).ti,ab.
31 human experiment/
32 trial.ti.
33 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32
34 (random$ adj sampl$ adj7 ("cross section$" or questionnaire$1 or survey$ or database$1)).ti,ab.
35 comparative study/ or controlled study/
36 randomi?ed controlled.ti,ab.
37 randomly assigned.ti,ab.
38 35 or 36 or 37
39 34 not 38
40 Cross‐sectional study/
41 randomized controlled trial/ or controlled clinical study/ or controlled study/
42 (randomi?ed controlled or control group$1).ti,ab.
43 41 or 42
44 40 not 43
45 (((case adj control$) and random$) not randomi?ed controlled).ti,ab.
46 (Systematic review not (trial or study)).ti.
47 (nonrandom$ not random$).ti,ab.
48 "Random field$".ti,ab.
49 (random cluster adj3 sampl$).ti,ab.
50 (review.ab. and review.pt.) not trial.ti.
51 "we searched".ab.
52 review.ti. or review.pt.
53 51 and 52
54 "update review".ab.
55 (databases adj4 searched).ab.
56 (rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys or trout or marmoset$1).ti. and animal experiment/
57 39 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 53 or 54 or 55
58 33 not 57
59 13 and 58
Web of Science (Web of Knowledge)
#1 TS=("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2)
#2 TS=(Wuhan and (coronavirus or "corona virus") )
#3 TS=(((coronavirus or "corona virus" or COVID) NEAR/3 "2019"))
#4 TOPIC: (wuhan NEAR/2 (disease or virus) )
#5 TS=(coronavirus or "corona virus" or COVID)
#6 #5 OR #4 OR #3 OR #2 OR #1
#7 TS=(Olfaction or olfactory or Dysosmia* or Paraosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia*)
#8 TS=(smell* NEAR/6 (disorder* or loss or distort* or alter* or dsyfunction or impair* or abscen* or reduce* or different* or sensation* or abnormal* or perception* or change* or expected or decreas* or deficit*) )
#9 TS=(smell* NEAR/6 (prevent* or rehab* or recover* or therap* or train* or retrain*) )
#10 #9 OR #8 OR #7
#11 #10 AND #6
#12 TS=((randomised OR randomized OR randomisation OR randomisation OR placebo* OR (random* AND (allocat* OR assign*) ) OR (blind* AND (single OR double OR treble OR triple) )))
#13 #12 AND #11
World Health Organization (WHO) COVID‐19 'Global literature on coronavirus disease'
(ti:(olfaction OR olfactory OR dysosmia* OR paraosmia* OR anosmia* OR hyposmia* OR phantosmia* OR cacosmia* OR microsmia* OR smell*)) OR (mh:(olfato OR l'olfaction OR cacosmia OR paraosmia OR anosmia))
Trial Registry Records (CENTRAL via CRS)
1 (("2019 nCoV" or 2019nCoV or "COVID 19" or COVID19 or "new coronavirus" or "novel coronavirus" or "novel corona virus" or "SARS CoV‐2" or SARS‐CoV2 or SARSCoV2 or "2019‐novel CoV" or ncov19 or ncov‐19 or nCov 2019 or COVID‐19 or SARSCoV‐2 or SARS‐CoV‐2)) AND CENTRAL:TARGET
2 ((Wuhan and (coronavirus or "corona virus"))) AND CENTRAL:TARGET
3 (((coronavirus or "corona virus" or COVID) adj3 "2019")) AND CENTRAL:TARGET
4 ((wuhan adj2 (disease or virus))) AND CENTRAL:TARGET
5 (coronavirus or "corona virus" or COVID) AND CENTRAL:TARGET
6 (2020 or 2021):YR AND CENTRAL:TARGET
7 #5 AND #6
8 #1 OR #2 OR #3 OR #4 OR #7
9 (Olfaction or olfactory or Dysosmia* or Paraosmia* or Anosmia* or hyposmia* or phantosmia* or Cacosmia* or microsmia* or smell*) AND CENTRAL:TARGET
10 #8 AND #9
11 http*:SO AND CENTRAL:TARGET
12 (NCT0* or ACTRN* or ChiCTR* or DRKS* or EUCTR* or eudract* or IRCT* or ISRCTN* or JapicCTI* or JPRN* or NTR0* or NTR1* or NTR2* or NTR3* or NTR4* or NTR5* or NTR6* or NTR7* or NTR8* or NTR9* or SRCTN* or UMIN0*):AU AND CENTRAL:TARGET
13 #11 OR #12
14 #10 AND #13
ICTRP (WHO Portal)
covid* AND anomsia OR covid* AND smell OR covid* AND olfact* OR coronavirus AND anomsia OR coronavirus AND smell OR coronavirus AND olfact* OR SARS‐CoV* AND anomsia OR SARS‐CoV* AND smell OR SARS‐CoV* AND olfact*
ClinicalTrials.gov
(COVID‐19 OR 2019‐nCoV OR SARS‐CoV‐2 OR 2019 novel coronavirus OR severe acute respiratory syndrome coronavirus 2 OR Wuhan coronavirus OR coronavirus) AND (anosmia OR smell OR Olfaction or olfactory)
AND Interventiona
Data and analyses
Comparison 1. Intranasal steroid spray compared to no intervention/placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Presence of normal olfactory function (as assessed by participants) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1.1 ≤ 4 weeks | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.85, 1.68] |
| 1.2 Duration of olfactory dysfunction | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | ‐6.50 [‐7.58, ‐5.42] |
| 1.3 Presence of normal olfactory function (as assessed with psychophysical testing) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.3.1 ≤ 4 weeks | 1 | 77 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.31 [1.16, 4.64] |
| 1.4 Change in sense of smell (as assessed by participants) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.4.1 At ≤ 4 weeks | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | ‐0.50 [‐1.38, 0.38] |
| 1.4.2 At > 4 weeks to 3 months | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 2.40 [1.32, 3.48] |
| 1.5 Change in sense of smell (as assessed with psychophysical testing) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.5.1 ≤ 4 weeks | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐2.06, 2.46] |
Comparison 2. Intranasal steroid drops compared to placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Presence of normal olfactory function at > 4 weeks to 3 months (as assessed by participants) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.89, 1.11] |
Comparison 3. Intranasal hypertonic saline spray compared to no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Duration of olfactory dysfunction | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | ‐3.10 [‐3.98, ‐2.22] |
| 3.2 Change in sense of smell (as assessed by participants) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abdelalim 2021.
| Study characteristics | ||
| Methods | Two‐arm, non‐blinded, parallel‐group randomised controlled trial with 3 weeks' duration of treatment and follow‐up | |
| Participants |
Location: Egypt, single‐centre study Setting of recruitment and treatment: recruited at Benha University Hospital Sample size: 108
Participants:
Baseline characteristics:
Inclusion criteria for the study:
Exclusion criteria for the study:
|
|
| Interventions |
Intervention group: Topical corticosteroid spray (mometasone furoate nasal spray), 2 puffs (100 µg) once daily in each nostril for 3 weeks Comparator group: No intervention Use of additional interventions in both groups: Olfactory training was recommended to both groups, in the form of sniffing of rose, lemon and clove for 20 seconds each, twice a day |
|
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study: None reported |
|
| Funding sources | No financial support was reported for the study | |
| Declarations of interest | No conflict of interest was declared | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The participants in this study were randomly assigned to two groups (simple 1:1 randomisation)". Comment: correspondence from the author confirmed that adequate methods were used (random selection of groups from an envelope). |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information was provided regarding concealment of allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: open‐label study, with no placebo group. Participants were aware of their allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: open‐label study, with no placebo group. The only outcome assessed was self‐reported by the (unblinded) participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: few dropouts (7.4%) and balanced across the groups. Two participants in each group may have been excluded due to non‐adherence to the trial protocol (intervention group: 1 discontinued treatment, 1 used treatment inconsistently, control group: 2 received other medications). However, the impact of this on the results was not felt to be sufficient to result in high risk of bias. |
| Selective reporting (reporting bias) | Low risk | Comment: trial protocol accessed on clinical trial registry, and no further outcomes were planned. |
| Other bias | Low risk | Comment: no other source of bias detected. |
Abdelmaksoud 2021.
| Study characteristics | ||
| Methods | Two‐arm, non‐blinded, single‐centre, parallel‐group RCT. Duration of treatment is not reported. Duration of follow‐up is only stated as "until complete recovery of COVID‐19". | |
| Participants |
Location: Egypt, single‐centre study Setting of recruitment and treatment: recruited at Qena University Hospital Sample size: 134 participants recruited to study; 105 had olfactory dysfunction and proceeded to randomisation
Participants:
Baseline characteristics:
Inclusion criteria for the study:
Exclusion criteria for the study:
|
|
| Interventions |
Intervention group: Zinc therapy (220 mg zinc sulfate equivocal to 50 mg elemental zinc) twice daily Comparator group: No intervention Use of additional interventions in both groups: Both groups received "the Egyptian protocol of COVID‐19 treatment"; no further details are provided |
|
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
|
| Funding sources | No additional funding was reported | |
| Declarations of interest | The authors declare that they have no conflict of interest | |
| Notes | As all participants were hospitalised in the acute phase of COVID‐19 infection, we have presumed that the presence of olfactory dysfunction was for < 4 weeks at baseline. However, this is not explicit from the paper. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The current prospective clinical trial study included 134 patients with COVID‐19, who were randomly selected from the Quarantine Department of Qena University Hospitals, Faculty of Medicine, South Valley University, Qena, Egypt, during the period from May 2020 to August 2020." "The patients with anosmia and/or hyposmia were divided randomly into two groups". Comment: no further details provided. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The patients with anosmia and/or hyposmia were divided randomly into two groups". Comment: no further details provided. Unable to establish whether allocation concealment was adequate. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: no placebo used, open‐label study. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: no placebo used, open‐label study. Subjective outcome measures. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no dropouts were recorded and data are available from all randomised participants. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol/trial registry entry is available. Insufficient detail in methods to establish whether key outcomes have been omitted. |
| Other bias | Unclear risk | Comment: insufficient detail is provided with regard to the conduct of the study to properly assess any other sources of bias. Very limited information available on the methods used in the study and baseline characteristics of participants. Lack of data on duration of treatment, time frame and methods of follow‐up. |
Kasiri 2021.
| Study characteristics | ||
| Methods | Two‐arm, double‐blind, parallel‐group randomised control trial with 4 weeks' duration of treatment and follow‐up | |
| Participants |
Location: Iran, single‐centre study Setting of recruitment and treatment: recruited from an outpatient clinic in Ibne Sina Hospital Sample size: 80
Participants:
Baseline characteristics:
Inclusion criteria for the study:
Exclusion criteria for the study:
|
|
| Interventions |
Intervention group: Intranasal corticosteroid group: 2 puffs of a 100 μg 0.05% mometasone furoate nasal spray, twice daily in each nostril for 4 weeks Comparator group: 2 puffs of topical saline spray in each nostril twice daily for 4 weeks Use of additional interventions in both groups: Olfactory training was used in both groups, using sniffing of a eucalyptus olfactory pen. No further details on methods of olfactory training or frequency. |
|
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study: None reported |
|
| Funding sources | Research grant funding. This work was supported by a grant from vice chancellery for research affairs of Mazandaran University of Medical Sciences. (Grant number: IRMAZUMS8435). | |
| Declarations of interest | Quote: "The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper". | |
| Notes | No further details in the paper regarding duration of olfactory disturbance, therefore unable to confirm that all participants had symptoms for ≤ 4 weeks. However, authors state that participants had symptoms for 2 weeks, and a large number of participants had symptoms of COVID‐19 at baseline (e.g. fever, sore throat, cough) therefore we have included this study in the prevention review. There is a discrepancy in the reporting of dates for this study. The recruitment dates are given as "between February 20 and Jun 30, 20201". We note that February 2020 was at a very early stage in the pandemic to start trial recruitment, and the trial protocol states "registered while recruiting" on 20 February 2021, with expected recruitment between 18 February 2021 and 18 April 2021. The paper was submitted for publication on 12 May 2021, therefore recruitment had presumably stopped before June 2021. We have attempted to contact the authors to clarify this. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants in this study were randomly assigned to two groups according to permuted block randomization." "A master randomization schedule was prepared by a person not associated with the study who used permuted blocks of random numbers." Comment: no further details provided on methods used to generate the random sequence. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information on concealment of allocation. Unclear if randomisation schedule was securely held. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Comment: the trial is described as "double‐blind" and a placebo was used, although no further details are provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: study states "double‐blind" and placebo used (topical saline) but no further details provided. No information on blinding of outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: few dropouts, balanced across the groups and fully accounted for (n = 1 lost to follow‐up (intervention), n = 1 lost to follow‐up (control), n = 1 discontinued trial (control)) |
| Selective reporting (reporting bias) | Unclear risk | Comment: primary and secondary outcome measures reported according to protocol. However, protocol was registered whilst recruiting, not prior to study commencing. |
| Other bias | Unclear risk | Comment: insufficient detail is provided on the conduct of the study to determine whether there may be additional issues resulting in bias. Discrepancy in study dates reported and article submission. |
Rashid 2021.
| Study characteristics | ||
| Methods | Two‐arm, double‐blind, 2‐centre, parallel‐group RCT with 1 month duration of treatment and follow‐up | |
| Participants |
Location: Iraq, 2‐centre study Setting of recruitment and treatment: recruited from 2 ENT outpatients clinics in Iraq (Al Ramadi Teaching Hospital and Tikrit Hospital) Sample size: 276
Participants:
Baseline characteristics:
Inclusion criteria:
Exclusion criteria:
|
|
| Interventions |
Intervention group: Intranasal betamethasone sodium phosphate drops (0.1 mg/mL); 3 drops to each nasal cavity, 3 times daily until recovery, for a maximum of 1 month Comparator group: Saline placebo 0.9% sodium chloride solution, 3 drops to each nostril 3 times daily until recovery, or for a maximum of 1 month Use of additional interventions in both groups: none reported |
|
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
|
| Funding sources | Quote: "This research did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors." | |
| Declarations of interest | None declared | |
| Notes | Articles states that all participants were analysed, but no information on how this was, given loss to follow‐up (i.e. no description of imputation etc.). Outcome data calculated on the presumption that results are calculated only from those who continued with follow‐up. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly allocated in 1:1 ratio". Comment: no further details provided. |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided. Note equal numbers randomised to each group, but no report of blocked randomisation. This may suggest that alternate allocation was used (in which case, high risk of bias). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Betamethasone drops were prepared by transferring a pharmaceutically available formulation (Ophatamesone® sterile drops for eye, ear, and nose; Dar Al Dawa, Na’ur, Jordan) into a plain container at aseptic conditions. At similar conditions, 0.9% NaCl intravenous solution was used to prepare placebo drops. Drops were prepared by a pharmacist who was not involved in the study. Treatment arms were concealed to patients and investigators." Comment: identical packaging appears to have been used. Preparation of intervention/comparator conducted by a separate individual. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Betamethasone drops were prepared by transferring a pharmaceutically available formulation (Ophatamesone® sterile drops for eye, ear, and nose; Dar Al Dawa, Na’ur, Jordan) into a plain container at aseptic conditions. At similar conditions, 0.9% NaCl intravenous solution was used to prepare placebo drops. Drops were prepared by a pharmacist who was not involved in the study. Treatment arms were concealed to patients and investigators." Comment: subjective outcomes, reported by (blinded) participants. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: loss to follow‐up approximately 10%, and balanced between the groups. |
| Selective reporting (reporting bias) | Unclear risk | Comment: trial registered retrospectively, after patient recruitment was completed (30 September 2020). Primary outcome reported according to registry data. |
| Other bias | Unclear risk | Comment: insufficient detail is provided on the conduct of the study to determine whether there may be additional issues resulting in bias. Authors state that outcomes were analysed on an intention‐to‐treat basis for all randomly assigned participants, but no information provided regarding how missing data were accounted for in analyses. |
Yildiz 2021.
| Study characteristics | ||
| Methods | Three‐arm, (presumed), non‐blinded, parallel‐group RCT with 30 days duration of treatment and follow‐up | |
| Participants |
Location: Turkey, single‐centre study Setting of recruitment and treatment: recruited from hospital inpatients Sample size: 150
Participants:
Baseline characteristics:
Inclusion criteria for the study:
Exclusion criteria for the study:
|
|
| Interventions |
Intervention group A: Saline irrigation: 10 mL of hypertonic saline (tonicity not reported) was administered to each nostril, twice daily for 1 month Intervention group B: Saline irrigation with steroid spray: saline irrigation was administered, as above, together with nasal steroid spray (triamcinolone acetonide 0.055%), 2 puffs to each nostril twice daily Comparator group: No intervention Use of additional interventions in both groups: None reported |
|
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study: None reported |
|
| Funding sources | The authors declared that this study has received no financial support | |
| Declarations of interest | No conflict of interest was declared by the authors | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: described as a single‐centre randomised controlled trial, but methods only state that participants "were divided into 3 equal groups". |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details are provided on allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: one intervention included no treatment, therefore not possible to blind participants to treatment. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: one intervention included no treatment, therefore not possible to blind participants to treatment. Outcomes all reported using subjective reporting measure by the participants themselves. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: no information provided on the number of dropouts. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no trial registration. Limited data in the methods of the trial, therefore unable to assess appropriately. |
| Other bias | High risk | Comment: unclear method for assessing olfactory function. Authors report using a subjective olfactory capability score, but not reported whether all odours were used consistently for all patients, and how patients would judge their olfactory ability across the different odours. Duration of olfactory disturbance is reported, but it is not clear what was used to judge recovery from olfactory disturbance. Unclear how patients recorded the duration of their symptoms when telephone follow‐up was only conducted on day 15 and 30, but duration of symptoms is reported in days. No information on daily diary/questionnaire to monitor symptoms. |
CT: computerised tomography; IQR interquartile range; PCR polymerase chain reaction; RCT: randomised controlled trial; SD: standard deviation; UPSIT: University of Pennsylvania Smell Identification Test; VAS visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTION (NCT04332107) | Wrong population: study does not specifically include participants with olfactory dysfunction |
| Begam 2020 | Narrative review article, no primary data |
| Bulbuloglu 2021 | Wrong study design: not a RCT |
| COPPS (NCT04662060) | Wrong population: study does not specifically include participants with olfactory dysfunction |
| Co‐STAR (NCT04422275) | Although this study fits the inclusion criteria for the review, it was withdrawn prior to any participant enrolment |
| COVIDAtoZ (NCT04342728) | Wrong population: study does not specifically include participants with olfactory dysfunction |
| COVIDORL (NCT04361474) | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This study is relevant for the companion review "Interventions for the treatment of persistent post‐COVID‐19 olfactory dysfunction" (O'Byrne 2022). |
| CTRI/2020/08/027477 | Wrong population: study does not specifically include participants with olfactory dysfunction |
| D'Ascanio 2021 | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This study is relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| IRCT20180205038619N2 | Wrong study design: not a RCT |
| IRCT20200522047542N1 | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This study is relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| IRCT20200629047953N1 | Wrong study design: not a RCT |
| IRCT20210708051817N1 | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This study is an ongoing study relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| Islek 2021 | Wrong study design: not a RCT |
| Klug 2021 | The authors have confirmed that not all participants in this trial had COVID‐19 related olfactory dysfunction |
| Le Bon 2021 | Wrong study design: not a RCT |
| NCT04374474 | Although this study fits the inclusion criteria for the review, it was withdrawn prior to any participant enrolment |
| NCT04382547 | Wrong study design: not a RCT |
| NCT04406584 | Wrong population: includes participants with any post‐viral olfactory disturbance (not specifically COVID‐19) |
| NCT04414124 | Wrong population: study does not specifically include participants with olfactory dysfunction |
| NCT04427332 | Wrong study design: observational study, not a RCT |
| NCT04458519 | Wrong population: study does not specifically include participants with olfactory dysfunction |
| NCT04474483 | Wrong population: study does not specifically include participants with olfactory dysfunction |
| NCT04513184 | Wrong population and wrong comparator: study does not specifically include participants with olfactory dysfunction; intervention is compared to intravenous dexamethasone |
| NCT04622891 | Wrong population: study does not specifically include participants with olfactory dysfunction |
| NCT04662086 | Wrong population: study does not specifically include participants with olfactory dysfunction |
| NCT04806880 | Wrong study design: not a RCT |
| NCT04830943 | Wrong study design: not a RCT |
| NCT04853836 | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This ongoing study is relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| NCT04916639 | Wrong patient population: participants in this trial have nasal obstruction and rhinorrhoea, but not necessarily olfactory disturbance. |
| NCT04952389 | Wrong population: all participants will have olfactory dysfunction for ≥ 4 weeks. This ongoing trial will be suitable for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| NCT04964414 | Wrong population: all participants had olfactory loss for at least 60 days. This ongoing trial may be relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| NCT05037110 | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This ongoing study is relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| NL9635 | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This ongoing study is relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| Odorat‐Covid (NCT04598763) | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This study is relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| Patel 2021 | Letter to the editor: no primary data included |
| Pinna 2020 | Letter to the editor: no primary data included |
| Saussez 2021 | Wrong study design: not a RCT |
| SCENT2 (NCT04789499) | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This study is relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| Singh 2021 | Wrong study design: not a RCT |
| Vaira 2021a | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This study is relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| Vaira 2021c | Wrong study design: this is a letter to the Editor, and does not report any primary data |
| Varricchio 2021 | Wrong study design: not a RCT |
| VOLT (NCT04710394) | Wrong population: all participants in the study have had symptoms of olfactory disturbance for at least 4 weeks. This study is relevant for the companion review that considers the treatment of persisting olfactory dysfunction (O'Byrne 2022). |
| Vroegop 2020 | Narrative review article: no primary data |
RCT: randomised controlled trial
Characteristics of studies awaiting classification [ordered by study ID]
Mohamad 2021.
| Methods | Parallel‐group randomised controlled trial |
| Participants | Adult participants with loss of sense of smell after COVID‐19 infection Inclusion criteria
Exclusion criteria
Planned sample size: estimated enrolment 40 participants |
| Interventions |
Intervention: insulin fast‐dissolving film containing 100 IU of insulin applied intranasally 3 times a week for 4 weeks Comparator: formulated bio‐adhesive fast‐dissolving film containing no drugs applied intranasally 3 times a week for 4 weeks |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Notes | Trial registered in Egypt. It is unclear from the description of this trial whether participants had symptoms of olfactory disturbance for fewer than 4 weeks from the onset of COVID‐19. The duration of anosmia is reported in the publication, with a range of 2 to 10, but it is not clear whether this is days or weeks. We have attempted to contact the authors for clarification, but are awaiting a response. |
Characteristics of ongoing studies [ordered by study ID]
IRCT20210202050231N1.
| Study name | Comparison of the effect of vanilla essential oil with eucalyptus essential oil on the return of olfactory sense in COVID‐19 patients |
| Methods | Parallel‐group, randomised, controlled, double‐blind trial |
| Participants | Individuals with a positive PCR test and olfactory impairment Inclusion criteria:
Exclusion criteria:
Planned sample size: 84 participants |
| Interventions |
Intervention:
Comparator:
|
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal sense of smell
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 30 April 2021 |
| Contact information | Mohamad Ali Yadegary Email: ma.yadegary@gmail.com |
| Notes | Trial registered in Iran Estimated recruitment end date: 21 August 2021 It is unclear if participants will have had symptoms for < 4 weeks at baseline, therefore this study may not be suitable for inclusion in this review. Further details will be obtained when the trial is published. |
IRCT20210205050247N.
| Study name | A comparative study of the effect of olfactory training and vitamin A in the olfactory loss of patients with covid‐19 |
| Methods | Single‐centre, 3‐arm, double‐blind, parallel‐group RCT with 12 weeks duration of treatment and follow‐up |
| Participants | Adults with COVID‐19 and olfactory disturbance for more than 2 weeks Inclusion criteria:
(No details given on COVID‐19 status, but general inclusion criteria indicate that COVID‐19 positive patients will be included) Exclusion criteria:
Estimated sample size: 90 participants |
| Interventions |
Intervention group A:
Olfactory rehabilitation for 12 weeks, using a kit that includes eucalyptus, lemon, rose and dianthus scents. Participants are asked to inhale each scent twice a day for 10 seconds each time. Intervention group B: Olfactory rehabilitation (as above) plus vitamin A tablets (10,000 units per day) for 12 weeks Control group: The third group of patients will not receive any treatment intervention and these patients will be followed up for 12 weeks |
| Outcomes |
Outcomes of interest in the review Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 18 February 2021 |
| Contact information | Abolfazi Taheri Email: abolfzl.taheri@gmail.com |
| Notes | Study registered in Iran. Anticipated study completion date 21 June 2021 It is unclear if participants will have had symptoms for < 4 weeks at baseline, therefore this trial may not be suitable for inclusion in this review. Further details will be obtained when the trial is published. |
IRCT20210311050671N1.
| Study name | Effect of auricular acupuncture with the laser in post‐viral anosmia during the COVID‐19 pandemic |
| Methods | Two‐arm, single‐blind, single‐centre, parallel‐group RCT with 12 weeks duration of treatment and follow‐up |
| Participants | Participants with COVID‐19 and olfactory dysfunction for at least 1 month Inclusion criteria:
Exclusion criteria:
Estimated sample size: 90 participants |
| Interventions |
Intervention group: Acupuncture will be performed in 2 sessions with an interval of 1 week. Each session will last for 20 minutes. Control group: "Laser‐off acupuncture" will be used as a placebo Use of additional interventions in both group; Both groups will received betamethasone drops (no further information is provided) |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal sense of smell
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 4 April 2021 |
| Contact information | Alireza Mohebbi Email: mohebbi.ar@iums.ac.ir |
| Notes | Registered in Iran. Estimated study completion date 6 July 2021. It is unclear if participants will have had symptoms for < 4 weeks at baseline, therefore this study may not be suitable for inclusion in this review. Further details will be obtained when the trial is published. |
NCT04495816.
| Study name | Randomised control trial of omega‐3 fatty acid supplementation for the treatment of COVID‐19 related olfactory dysfunction |
| Methods | Parallel‐group randomised controlled trial |
| Participants | Adults with self‐reported new onset olfactory dysfunction and COVID‐19 infection Inclusion criteria:
Exclusion criteria:
Planned sample size: estimated enrolment 126 participants (from clinical trial register). Additional publication states estimated sample size of 176 (88 per group). |
| Interventions |
Intervention: omega‐3 fatty acid, 1000 mg (administered as 2 soft gels, containing 683 mg eicosapentaenoic acid and 252 mg docosahexaenoic acid) twice daily for 6 weeks Comparator: placebo (administered as 2 placebo soft gels) twice daily for 6 weeks |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 15 July 2020 |
| Contact information | Alfred‐Marc Iloreta Email: alfred-marc.iloreta@mountsinai.org |
| Notes | Estimated study completion date: June 2021 It is unclear from the description of this trial whether participants will have symptoms of olfactory disturbance for fewer than 4 weeks from the onset of COVID‐19. Correspondence with the study team has confirmed that they will recruit a mixed population, comprising individuals with fewer than and longer than 4 weeks of symptoms. |
NCT04528329.
| Study name | Anosmia and/or ageusia and early corticosteroid use |
| Methods | Randomised controlled trial |
| Participants | Adult participants with mild to moderate severity COVID‐19 Inclusion
Exclusion
Planned sample size: 300 participants |
| Interventions |
Intervention: "Early dexamethasone use as early as confirmation of inflammation" Comparator: "Late dexamethasone use as soon as deterioration" |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 30 August 2020 |
| Contact information | Emad R Issak Email: dr.emad.r.h.issak@gmail.com |
| Notes | Estimated study completion date: 15 December 2020 Trial registered in Egypt Uncertainty over future inclusion in the review: It is not clear from the description provided whether participants will all have olfactory dysfunction at baseline and, if so, whether they will have ≤ 4 weeks of olfactory dysfunction. We are awaiting confirmation from the study authors. |
NCT04530409.
| Study name | Timing of corticosteroids in COVID‐19 |
| Methods | Randomised controlled trial |
| Participants | Adult participants with mild or moderate COVID‐19 Included
Excluded
Planned sample size: 450 patients |
| Interventions |
Intervention: "Early dexamethasone use as early as confirmation of inflammation" Comparator: "Late dexamethasone use as soon as deterioration" |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study: Primary:
Secondary:
|
| Starting date | 26 August 2020 |
| Contact information | Emad R Issak Email: dr.emad.r.h.issak@gmail.com |
| Notes | Estimated study completion date: 1 December 2020 Trial registered in Egypt Uncertainty over future inclusion in the review: It is not clear from the description provided whether participants will all have olfactory dysfunction at baseline and, if so, whether they will have ≤ 4 weeks of olfactory dysfunction. |
NCT04638673.
| Study name | NeuroCovid rehab and recovery related to COVID‐19 diagnosis |
| Methods | To evaluate a transcutaneous auricular vagus nerve stimulation (taVNS) in the treatment of the neurological symptoms of COVID‐19 termed NEUROCOVID |
| Participants | Patients with COVID‐19 suffering from the neurological symptoms associated with infection Inclusion criteria:
Exclusion criteria:
Planned sample size: estimated enrolment 30 participants |
| Interventions |
Intervention group: active‐active stimulation group; participants will receive active taVNS stimulation for weeks 1 to 4 of the stimulation portion of this study using Soterix taVNS model 0125‐LTE Comparator group: sham‐active stimulation group; participants will receive sham taVNS stimulation for weeks 1 and 2 and active stimulation for weeks 3 and 4 of the stimulation portion of this study |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 19 November 2020 |
| Contact information | Sarah Huffman
Email: huffmans@musc.edu Morgan Dancy Email: maddoxm@musc.edu |
| Notes | Estimated study completion date: June 2021 Trial registered in USA Uncertainty over future inclusion in the review: It is not clear from the description provided whether participants will all have olfactory dysfunction at baseline and, if so, whether they will have had ≤ 4 weeks of olfactory dysfunction. We are awaiting confirmation from the study authors. |
NCT04764981.
| Study name | Olfactory training for olfactory dysfunction after coronavirus disease ‐ 19 (COVID‐19) |
| Methods | Two‐arm, unblinded, single‐centre, parallel‐group RCT with 3 months duration of treatment and follow‐up NB trial registry states double‐blinded, but no intervention used in comparator group, therefore must be unblinded to participants |
| Participants | Individuals with persistent olfactory dysfunction following COVID‐19; duration of dysfunction unclear Inclusion criteria:
Exclusion criteria:
Estimated sample size: 300 participants (additional 50 healthy controls will be recruited for a separate study arm) |
| Interventions |
Intervention group: Olfactory training: 4 odours (rose, eucalyptus, lemon and cloves), twice daily training for 30 seconds per odour for a total of 3 months Control group: No intervention |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal sense of smell
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | May 2021 |
| Contact information | Alna Carolina Mendes Parahnos, no contact details provided |
| Notes | Registered in Brazil Estimated study completion date 1 May 2024 It is unclear if participants will have had symptoms for < 4 weeks at baseline, therefore this study may not be suitable for inclusion in this review. Further details will be obtained when the trial is published. |
NCT04797936.
| Study name | BNO 1030 extract (Imupret) in the treatment of mild forms of COVID‐19 |
| Methods | Two‐arm, open‐label, parallel‐group RCT with 14 days duration of treatment and follow‐up |
| Participants | Adult participants with mild COVID‐19 and nasal symptoms (either congestion, rhinorrhoea or anosmia/hyposmia) Inclusion criteria:
Exclusion criteria:
Estimated sample size: 133 participants |
| Interventions |
Intervention: Imupret (BNO 1030) 25 drops, given 6 times per day for 14 days. Imupret described elsewhere as a herbal intervention comprising marshmallow root (Radix Althaeae), chamomile flowers (Flores Chamomillae), horsetail herb (Herba Equiseti), walnut leaves (Folia Jungladis), yarrow herb (Herba Millefolii), oak bark (Cortex Quercus), dandelion herb (Herba Taraxaci) Comparator: No intervention. Symptomatic therapy as needed, including anti‐pyretics and saline solutions in the nose 4 times a day for 14 days. We assume that symptomatic therapy will also be provided for the intervention group, but this is not explicit in the protocol. |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 1 May 2020 |
| Contact information | Vasyl Popovych. No contact details provided. |
| Notes | Estimated completion date 8 January 2021 Trial registered in Ukraine We assume that, as symptom scores are assessed during the study, these participants will be in the early stages of COVID‐19 infection and this study will be relevant for this review (< 4 weeks since olfactory dysfunction). However, this is not explicit in the protocol. |
NCT04900415.
| Study name | Olfactory and neurosensory rehabilitation in COVID‐19‐related olfactory dysfunction |
| Methods | 3‐arm, open‐label, parallel‐group RCT with 4 weeks of treatment and follow‐up |
| Participants | Adult participants with persisting olfactory dysfunction following confirmed COVID‐19 Inclusion criteria:
Exclusion criteria:
Estimated sample size: planned enrollment 25 participants |
| Interventions |
Intervention group A
Vitamin A 7500 µg plus smell training 3 times per day for 4 weeks Intervention group B Smell training 3 times per day for 4 weeks Comparator: No intervention |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal sense of smell
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of smell
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 22 July 2020 |
| Contact information | Ivan Fan Ngai Hung Email: ivanhung@hku.hk |
| Notes | Registered in Hong Kong Estimated study completion 30 June 2021 It is unclear if participants will have had symptoms for < 4 weeks at baseline, therefore this study may not be suitable for inclusion in this review. Further details will be obtained when the trial is published. |
NCT04951362.
| Study name | Role of ivermectin nanosuspension as nasal spray in treatment of persistant post covid19 anosmia |
| Methods | Two‐arm, open‐label, parallel‐group RCT with 14 days duration of treatment and follow‐up |
| Participants | Adults with anosmia following COVID‐19 Inclusion criteria:
Exclusion criteria:
Estimated sample size: 117 participants |
| Interventions |
Intervention group: Ivermectin (and corticosteroid?) nanosuspension nasal spray. Unclear whether corticosteroid is co‐administered with the ivermectin spray. Comparator group: Saline nasal spray |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal sense of smell
Serious adverse effects
Change in sense of smell
Secondary outcomes: Change in sense of taste
Prevalence of parosmia
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 20 April 2021 |
| Contact information | Zaky Aref Email: doctor.aref@hotmail.com |
| Notes | Trial registered in Egypt Estimated study completion 12 September 2021 It is unclear if participants will have had symptoms for < 4 weeks at baseline, therefore this study may not be suitable for inclusion in this review. Further details will be obtained when the trial is published. |
NCT04959747.
| Study name | Acupuncture for olfactory dysfunction in infected COVID‐19 patients |
| Methods | Two‐arm, single‐blinded (to the participant), cross‐over RCT with 4 weeks duration of treatment, followed by 2 weeks of follow‐up, then cross‐over to the opposite group |
| Participants | Adult participants, with moderate to severe olfactory dysfunction following COVID‐19 Inclusion criteria:
Exclusion criteria:
Estimated sample size: 20 participants |
| Interventions |
Intervention group:
Body acupuncture will involve 8 acupoints as Yingxiang (LI20), Shangxing (GV23), BiTong, Yintang, Hegu. A disposable acupuncture needle (0.25 mm in diameter and 25 mm to 30mm in length) will be inserted at a depth of 10 mm to 25 mm obliquely into scalp acupuncture points (ShangXing, YinTang) and straight into face/body acupuncture points (Yingxiang, BiTong, Hegu).
Electro‐acupuncture will be applied to the face points at fast and dispersed waves through an electric needle stimulator for 30 minutes. Participants will undergo a total of 8 sessions, 30 minutes per session, delivered twice per week over a 4‐week period. Comparator group: Sham control. Streitberger's non‐invasive acupuncture needles (Gauge 8 x 1.2"/0.30 mm x 30 mm) will be applied to serve as sham control at the same acupuncture points |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 15 July 2020 |
| Contact information | Alfred‐Marc Iloreta Email: alfred‐marc.iloreta@mountsinai.org |
| Notes | Estimated study completion date: June 2021 It is unclear from the description of this trial whether participants will have symptoms of olfactory disturbance for fewer than 4 weeks from the onset of COVID‐19. Correspondence with the study team has confirmed that they will recruit a mixed population, comprising individuals with fewer than and longer than 4 weeks of symptoms. |
NCT05002530.
| Study name | Investigating the potential role of aerosolized retinoic acid, a potent vitamin a metabolite for treating COVID‐19 anosmia and retinoic acid insufficiency. A novel approach for regaining sense of smell |
| Methods | Parallel‐group, multi‐centre, open‐label randomised controlled trial with 3 weeks duration of treatment and follow‐up |
| Participants | Adults with recent onset of olfactory disturbance from COVID‐19, who have recovered from the virus Inclusion criteria:
Exclusion criteria:
Planned sample size: 10,000 participants* *as this sample size is considerably larger than all other studies in this review, and the recruitment period is extremely short (2 months) we have attempted to contact the authors and confirm if this is correct. |
| Interventions |
Intervention: Aerosolised 13 cis retinoic acid or all trans retinoic acid plus vitamin D (2 intervention groups). Retinoic acid therapy will be delivered as an inhalation in 2 divided doses, increasing from 0.2 mg/kg/day to 4 mg/kg/day for 3 weeks. Vitamin D will be administered as an intramuscular injection of 600,000 units for 2 doses given at week 0 and week 4. Comparator: Standard therapy |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | November 2021 |
| Contact information | Mahmoud R Mahmoud Email: mahmoudramadan2051@yahoo.com Tamer Haydara Email: tamerhaydara@yahoo.com |
| Notes | Estimated trial end date December 2021 Registration from Egypt, but multi‐centre trial based in Saudi Arabia, China, USA and Egypt. Note the very large sample size and short duration of the trial (2 months) ‐ we have contacted the trial authors for clarification on this. Also, we note that the outcomes report the use of softgels (some outcomes are described as being "1 week after softgel initiation". This is not described as part of the intervention. It is unclear if participants will have had symptoms for < 4 weeks at baseline, therefore this study may not be suitable for inclusion in this review. Further details will be obtained when the trial is published. |
TCTR20210714006.
| Study name | Corticosteroid nasal irrigation as early treatment of olfactory dysfunction in COVID‐19: a prospective randomized controlled trial |
| Methods | Parallel group, open‐label randomised controlled trial |
| Participants | Patients with new onset of smell dysfunction following a positive COVID‐19 test Inclusion criteria:
Exclusion criteria:
Planned sample size: estimated 200 participants |
| Interventions |
Intervention A:
Intervention B:
Comparator:
|
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | Not reported |
| Contact information | Jidapa Tragoonrungsea Email: janjy.t@gmail.com |
| Notes | Registered in Thailand Estimated completion date 12 January 2022 It is unclear if participants will have had symptoms for < 4 weeks at baseline, therefore this study may not be suitable for inclusion in this review. Further details will be obtained when the trial is published. |
UMIN000043537.
| Study name | Post COVID‐19 anosmia |
| Methods | 4‐arm, double‐blind, parallel‐group RCT. Duration of treatment and follow‐up unclear. |
| Participants | Adults with olfactory dysfunction following COVID‐19 Inclusion criteria:
Exclusion criteria:
Estimated sample size: 200 participants |
| Interventions |
Intervention A Combination of local corticosteroid and antihistamine nasal spray Intervention B Local corticosteroid nasal spray Intervention C Antihistamine nasal spray Comparator: Normal saline nasal spray 0.2% No further details provided on any of the interventions or comparator |
| Outcomes |
Outcomes of interest in the review: Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | 1 January 2021 |
| Contact information | Asmaa Salah Mohamed Email: asmaa.elsadorry@yahoo.com |
| Notes | Registered in Egypt. Trial end date not reported. It is unclear if participants will have had symptoms for < 4 weeks at baseline, therefore this trial may not be suitable for inclusion in this review. Further details will be obtained when the trial is published. |
UMIN000045185.
| Study name | "Additional value" of nasal therapy in standard therapy for COVID‐19 patients with olfactory disorders: a preliminary randomized controlled clinical trial |
| Methods | Parallel‐group randomised controlled trial Study is reported as blinded to participants, but we note that no placebo is used |
| Participants | Confirmed COVID‐19 positive with mild or moderate symptoms Inclusion criteria:
Exclusion criteria:
Estimated sample size: 24 participants |
| Interventions |
Intervention group: Nasal treatment (mometasone nasal spray, normal saline nasal irrigation both nostrils, oxymethazolin 0.5% nasal spray before bedtime, aromatic vapour rub on neck and chest before bedtime) for 2 weeks Comparator: No intervention Additional interventions used in both groups: Standard therapy for COVID‐19 |
| Outcomes |
Outcomes of interest in the review Primary outcomes: Presence of normal olfactory function
Serious adverse effects
Change in sense of smell
Secondary outcomes: Prevalence of parosmia
Change in sense of taste
Disease‐related quality of life
Other adverse effects (including nosebleeds/bloody discharge)
Other outcomes reported by the study:
|
| Starting date | August 2020 |
| Contact information | Indra Pamungkas Email: indraparmaditya@gmail.com |
| Notes | Estimated completion November 2020. Retrospectively registered. Trial registered in Indonesia. |
ALT: alanine aminotransferase; BiPAP bilevel positive airway pressure; BSIT Brief Smell Identification Test; CCCRC: Connecticut Chemosensory Clinical Research Center; CPAP continuous positive airway pressure; CRP: c‐reactive protein; LDH: lactate dehydrogenase; mQOD‐NS Modified Brief Questionnaire of Olfactory Dysfunction; MRI: magnetic resonance imaging; PCR polymerase chain reaction; RCT: randomised controlled trial; SNOT‐22 Sinonasal Outcomes Test; taVNS: transcutaneous auricular vagus nerve stimulation; UPSIT: University of Pennsylvania Smell Identification Test; VAS: visual analogue scale.
Differences between protocol and review
When preparing the protocol for this review we intended to present the following outcomes in the summary of findings tables:
presence of normal olfactory function (as reported by the participants);
serious adverse effects;
change in sense of smell (as identified by psychophysical testing);
prevalence of parosmia;
change in sense of taste;
disease‐related quality of life;
other adverse effects (including nosebleeds/bloody discharge).
As data for many of our outcomes were sparse, we have presented information on olfactory outcomes regardless of whether these were obtained through self‐report or psychophysical testing.
Search methods
The first update search in July 2021 employed a new search strategy, using MeSH and EMTREE terms introduced in January 2021. Details of the searches performed in December 2020 are available in Appendix 3. In December 2020 we also searched the World Health Organization (WHO) COVID‐19 'Global literature on coronavirus disease'.
As part of this living systematic review we planned to run quarterly searches of the following sources. Following assessment of the initial search these sources were dropped because of overlap with others and poor‐quality records.
World Health Organization (WHO) COVID‐19 'Global literature on coronavirus disease' https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov (search to date);
COAP COVID‐19 Living Evidence, Institute of Social and Preventive Medicine (ISPM), University of Bern https://zika.ispm.unibe.ch/assets/data/pub/search_beta/ (search to date).
Contributions of authors
Katie Webster: scoped, designed and drafted the protocol with the help of the other authors. Sifted studies, carried out data extraction, risk of bias assessment, performed analyses and GRADE assessment for included studies, drafted and revised the review.
Lisa O'Byrne: sifted studies, carried out data extraction, risk of bias assessment and GRADE assessment for included studies, drafted and revised the review.
Samuel MacKeith: clinical guidance at all stages of project scoping and protocol development; commented on and edited the draft review, and agreed the final version.
Carl Philpott: clinical guidance at all stages of project scoping and protocol development; commented on and edited the draft review, and agreed the final version.
Claire Hopkins: clinical guidance at all stages of project scoping and protocol development; commented on and edited the draft review, and agreed the final version.
Martin Burton: clinical guidance at all stages of project scoping and protocol development; commented on and edited the draft review, and agreed the final version.
Sources of support
Internal sources
No sources of support provided
External sources
-
National Institute for Health Research, UK
Infrastructure funding for Cochrane ENT
-
NIHR COVID‐19 Recovery and Learning programme, UK
Award NIHR132103
Declarations of interest
Katie Webster: none known.
Lisa O' Byrne: none known.
Samuel MacKeith: Sam MacKeith is Assistant Co‐ordinating Editor of Cochrane ENT, but had no role in the editorial process for this review.
Carl Philpott: Professor Carl Philpott sees and treats patients with COVID‐19 related smell loss. He has written various online publications on the topic and conducted interviews and webinars internationally. He is a Trustee for the charity Fifth Sense. He is the senior author on the Clinical Olfactory Working Group consensus document on the management of post‐infectious olfactory dysfunction and the consensus document on the use of systemic corticosteroids in COVID‐19 related olfactory dysfunction.
Claire Hopkins: Professor Claire Hopkins sees and treats patients with COVID‐19 related smell loss. She has spoken on the association between COVID and smell loss in multiple media outlets. She is senior author of the British Rhinological Society position paper on management of COVID‐19 related smell loss.
Martin Burton: Professor Martin Burton is Co‐ordinating Editor of Cochrane ENT, but had no role in the editorial process for this review.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Abdelalim 2021 {published data only}
- Abdelalim AA, Mohamady AA, Elsayed RA, Elawady MA, Ghallab AF. Corticosteroid nasal spray for recovery of smell sensation in COVID-19 patients: a randomized controlled trial. American Journal of Otolaryngology 2021;42(2):102884. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT04484493. Corticosteroid nasal spray in COVID-19 anosmia [Role of corticosteroid nasal spray in recovery of smell sensation in COVID-19 patients]. https://clinicaltrials.gov/show/NCT04484493 (first received 23 July 2020). [CENTRAL: CN-02145535]
Abdelmaksoud 2021 {published data only}
- Abdelmaksoud AA, Ghweil AA, Hassan MH, Rashad A, Khodeary A, Aref ZF, et al. Olfactory disturbances as presenting manifestation among Egyptian patients with COVID-19: possible role of zinc. Biological Trace Element Research 2021;199(11):4101-8. [CENTRAL: CN-02254314] [EMBASE: 2010124825] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kasiri 2021 {published data only}
- IRCT20190804044429N6. Nasal spray of mometasone 0.05% effects on olfactory improvement in COVID-19 [Efficacy and safety of nasal spray of mometasone 0.05% on olfactory improvement in patients with COVID-19: A randomized, double blind clinical trial]. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20190804044429N6 (first received 2021). [CENTRAL: CN-02240855]
- Kasiri H, Rouhani N, Salehifar E, Ghazaeian M, Fallah S. Mometasone furoate nasal spray in the treatment of patients with COVID-19 olfactory dysfunction: a randomized, double blind clinical trial. International Immunopharmacology 2021;98:107871. [CENTRAL: CN-02283597] [EMBASE: 2013103141] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rashid 2021 {published data only}
- NCT04569825. Effect of nasal steroid in the treatment of anosmia due to COVID-19 disease. https://clinicaltrials.gov/show/NCT04569825 (first received 30 September 2020). [CENTRAL: CN-02181592]
- Rashid RA, Zgair A, Al-Ani RM. Effect of nasal corticosteroid in the treatment of anosmia due to COVID-19: a randomised double-blind placebo-controlled study. American Journal of Otolaryngology 2021;42(5):103033. [CENTRAL: CN-02268100] [EMBASE: 2011632217] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yildiz 2021 {published data only}
- Yildiz E, Koca Yildiz S, Kuzu S, Gunebakan C, Bucak A, Kahveci OK. Comparison of the healing effect of nasal saline irrigation with triamcinolone acetonide versus nasal saline irrigation alone in COVID-19 related olfactory dysfunction: a randomized controlled study. Indian Journal of Otolaryngology and Head and Neck Surgery 2021 Jul 10 [Epub ahead of print]. [PMID: ] [DOI] [PMC free article] [PubMed]
References to studies excluded from this review
ACTION (NCT04332107) {published data only}
- NCT04332107. Azithromycin for COVID-19 treatment in outpatients nationwide [Azithromycin for prevention of disease progression in patients with mild or moderate COVID-19]. https://clinicaltrials.gov/show/NCT04332107 (first received 2 April 2020).
Begam 2020 {published data only}
- Begam N, Bashar MA. Olfactory and taste disorders in patients with SARS-CoV-2 infection. International Archives of Otorhinolaryngology 2020;24(3):e391-2. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bulbuloglu 2021 {published data only}
- Bulbuloglu S, Altun Y. The effect of sniffing Turkish coffee on olfactory disorders in COVID-19 patients: an experimental clinical study. Ideggyogyaszati Szemle 2021;74(3-4):117-23. [PMID: ] [DOI] [PubMed] [Google Scholar]
COPPS (NCT04662060) {published data only}
- NCT04662060. COVID-19 Outpatient Pragmatic Platform Study (COPPS) - Acebilustat Sub-Protocol [COVID-19 Outpatient Pragmatic Platform Study (COPPS): a pragmatic multi-arm, adaptive, phase 2, blinded, randomized placebo-controlled platform trial to assess the efficacy of different investigational therapeutics in reducing time to disease resolution or viral load cessation, as compared to standard supportive care in outpatients with COVID-19]. https://clinicaltrials.gov/show/NCT04662060 (first received 10 December 2020).
Co‐STAR (NCT04422275) {published data only}
- NCT04422275. Coronavirus smell therapy for anosmia recovery. https://clinicaltrials.gov/show/NCT04422275 (first received 9 June 2020). [CENTRAL: CN-02118715]
COVIDAtoZ (NCT04342728) {published data only}
- NCT04342728. Coronavirus 2019 (COVID-19)- using ascorbic acid and zinc supplementation [Coronavirus disease 2019- using ascorbic acid and zinc supplementation (COVIDAtoZ) research study a randomized, open label single center study]. https://clinicaltrials.gov/show/NCT04342728 (first received 13 April 2020).
COVIDORL (NCT04361474) {published data only}
- Daval M, Corre A, Palpacuer C, Housset J, Poillon G, Eliezer M, et al. Efficacy of local budesonide therapy in the management of persistent hyposmia in COVID-19 patients without signs of severity: a structured summary of a study protocol for a randomised controlled trial. Trials 2020;21(1):666. [CENTRAL: CN-02177639] [EMBASE: 632388256] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT04361474. Trial evaluating the efficacy of local budesonide therapy in the management of hyposmia in COVID-19 patients without signs of severity [A randomized controlled trial evaluating the efficacy of local budesonide therapy in the management of hyposmia in COVID-19 patients without signs of severity]. https://clinicaltrials.gov/show/NCT04361474 (first received 24 April 2020). [CENTRAL: CN-02180471]
CTRI/2020/08/027477 {published data only}
- CTRI/2020/08/027477. Evaluation of safety and efficacy of T-AYU-HM premium and onion steam vaporization/nebulization in Covid-19 patients. http://www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2020/08/027477 (first received 2020).
D'Ascanio 2021 {published data only}
- D'Ascanio L, Vitelli F, Cingolani C, Maranzano M, Brenner MJ, Di Stadio A. Randomized clinical trial "olfactory dysfunction after COVID-19: olfactory rehabilitation therapy vs. intervention treatment with Palmitoylethanolamide and Luteolin": preliminary results. European Review for Medical and Pharmacological Sciences 2021 06;25(11):4156-62. [CENTRAL: CN-02288715] [EMBASE: 2013167573] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT04853836. Olfactory disfunction and Co-ultraPEALut [Olfactory disfunction after COVID-19: conventional therapy versus intervention treatment with Co-ultraPEALut]. https://clinicaltrials.gov/show/NCT04853836 (first received 21 April 2021). [CENTRAL: CN-02269702]
IRCT20180205038619N2 {published data only}
- Evaluation of the effectiveness of TDCS (transcranial direct current stimulation) in the treatment of prolonged decreased of sense of smell in patients with Covid-19. http://en.irct.ir/trial/53545 (first received 30 August 2021).
IRCT20200522047542N1 {published data only}
- IRCT20200522047542N1. Effect of Corton on olfactory dysfunction in COVID-19 patients [Effect of inhaled corticosteroids in the treatment of anosmia in patients with COVID-19]. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20200522047542N1 (first received 2020). [CENTRAL: CN-02187839]
IRCT20200629047953N1 {published data only}
- IRCT20200629047953N1. Effect of olfactory training on anosmia of COVID-19 [Assessment of the effect of olfactory training on anosmia following COVID-19 infection]. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20200629047953N1 (first received 2021). [CENTRAL: CN-02282666]
IRCT20210708051817N1 {published data only}
- Whole body cryotherapy (WBC) for treating anosmia / hyposmia. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20210708051817N1.
Islek 2021 {published data only}
- Islek A, Balcı MK. Evaluation of effects of chronic nasal steroid use on rhinological symptoms of COVID-19 with SNOT-22 questionnaire. Pharmacological Reports: PR 2021;73(3):781-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Klug 2021 {published data only}
- Klug T, Rosen D, Chaskes M, Souza GD, Pribitkin E. Treatment of refractory anosmia with topical platelet rich plasma. Otolaryngology - Head and Neck Surgery 2021;165 (Suppl 1):344-5. [Google Scholar]
Le Bon 2021 {published data only}
- Le Bon SD, Konopnicki D, Pisarski N, Prunier L, Lechien JR, Horoi M. Efficacy and safety of oral corticosteroids and olfactory training in the management of COVID-19-related loss of smell. European Archives of Oto-rhino-laryngology 2021;278(8):3113-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT04374474 {published data only}
- NCT04374474. Anosmia rehabilitation in patients post coronavirus disease (COVID 19) [Olfactory retraining therapy and budesonide nasal rinse for anosmia treatment in patients post-COVID 19. A randomized controlled trial]. https://clinicaltrials.gov/show/NCT04374474 (first received 5 May 2020). [CENTRAL: CN-02093904]
NCT04382547 {published data only}
- NCT04382547. Treatment of Covid-19 associated pneumonia with allogenic pooled olfactory mucosa-derived mesenchymal stem cells. https://clinicaltrials.gov/show/NCT04382547 (first received 11 May 2020).
NCT04406584 {published data only}
- NCT04406584. Intranasal injection of PRP versus saline for treatment of olfactory dysfunction [Intranasal injection of platelet-rich plasma versus saline for treatment of olfactory dysfunction]. https://clinicaltrials.gov/show/NCT04406584 (first received 28 May 2020). [CENTRAL: CN-02124993]
NCT04414124 {published data only}
- NCT04414124. A clinical study to assess the natural history of COVID-19 and effects of KB109 and supportive self-care in outpatients with mild-to-moderate COVID-19 [A randomized, open label, prospective, parallel group study to assess the natural history of COVID-19 and effects of KB109 in addition to supportive self care (SSC) compared to SSC alone on measures of health in non-hospitalized patients with mild-moderate COVID-19]. https://clinicaltrials.gov/show/NCT04414124 (first received 4 June 2020).
NCT04427332 {published data only}
- NCT04427332. Smell and taste disorders in COVID-19 patients [Smell and taste disorders in COVID-19 patients: prospective observational study]. https://clinicaltrials.gov/ct2/show/NCT04427332 (first received 11 June 2020).
NCT04458519 {published data only}
- NCT04458519. Efficacy of intranasal probiotic treatment to reduce severity of symptoms in COVID19 infection [Randomised single blinded clinical study of efficacy of intranasal probiotic treatment to reduce severity of symptoms in COVID19 infection]. https://clinicaltrials.gov/show/NCT04458519 (first received 7 July 2020).
NCT04474483 {published data only}
- NCT04474483. Safety and efficacy of melatonin in outpatients infected with COVID-19 [A pilot placebo-controlled randomized double-blind trial of melatonin in outpatients with COVID-19 infection]. https://clinicaltrials.gov/show/NCT04474483 (first received 16 July 2020).
NCT04513184 {published data only}
- NCT04513184. Randomized clinical trial of intranasal dexamethasone as an adjuvant in patients with COVID-19. https://clinicaltrials.gov/show/NCT04513184 (first received 14 August 2020). [CENTRAL: CN-02146132]
NCT04622891 {published data only}
- NCT04622891. Clarithromycin versus azithromycin in treatment of mild COVID-19 infection [Efficacy of clarithromycin in comparison to azithromycin in treatment of mild COVID-19 infection, randomized controlled trial]. https://clinicaltrials.gov/show/NCT04622891 (first received 10 November 2020). [CENTRAL: CN-02184257]
NCT04662086 {published data only}
- NCT04662086. COVID-19 Outpatient Pragmatic Platform Study (COPPS) - master protocol [COVID-19 Outpatient Pragmatic Platform Study (COPPS): a pragmatic multi-arm, adaptive, phase 2, blinded, randomized placebo-controlled platform trial to assess the efficacy of different investigational therapeutics in reducing time to disease resolution or viral load cessation, as compared to standard supportive care in outpatients with COVID-19]. https://clinicaltrials.gov/show/NCT04662086 (first received 10 December 2020).
NCT04806880 {published data only}
- Study evaluating the olfactory recovery of anosmia post COVID-19 by olfactory rehabilitation assisted by web-application. https://clinicaltrials.gov/show/NCT04806880 (first received 19 March 2021).
NCT04830943 {published data only}
- NCT04830943. Cerebrolycin for treatment of Covid-related anosmia and ageusia [The effectiveness of cerebrolycin for treatment of post-covid olfactory and gustatory dysfunctions: a pilot study]. https://clinicaltrials.gov/show/NCT04830943 (first received 5 April 2021).
NCT04853836 {published data only}
- Olfactory disfunction and Co-ultraPEALut. https://clinicaltrials.gov/ct2/show/NCT04853836 (first received 21 April 2021).
NCT04916639 {published data only}
- Seawater nasal wash to relieve COVID-19 nasal symptoms and reduce SARS-CoV-2 viral load. https://clinicaltrials.gov/show/NCT04916639 (first received 7 June 2021).
NCT04952389 {published data only}
- NCT04952389. Acupuncture therapy for COVID-related olfactory loss. https://clinicaltrials.gov/show/NCT04952389 (first received 7 July 2021). [CENTRAL: CN-02290173]
NCT04964414 {published data only}
- NCT04964414. Treatment of pediatric patients that lost sense of smell due to COVID-19 [Prospective randomized study of the treatment of pediatric patients that lost sense of smell due to COVID-19]. https://clinicaltrials.gov/show/NCT04964414 (first received 16 July 2021). [CENTRAL: CN-02283179]
NCT05037110 {published data only}
- Physical activity and smell trainings to help individuals with coronavirus disease (COVID-19) recover from persistent smell and taste impairments - a pilot study. https://clinicaltrials.gov/show/NCT05037110 (first received 8 September 2021).
NL9635 {published data only}
- Corticosteroids for COVID-19 induced loss of smell. https://trialregister.nl/trial/9635 (first received 28 July 2021).
Odorat‐Covid (NCT04598763) {published data only}
- NCT04598763. Evaluation of two methods of olfactory rehabilitation in post-viral loss of smell: classic and intensive. https://clinicaltrials.gov/show/NCT04598763 (first received 22 October 2020).
Patel 2021 {published data only}
- Levy JM. Regarding use of topical steroids in patients with COVID-19-associated olfactory loss - Reply. JAMA Otolaryngology--Head & Neck Surgery 2021;147(1):110-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel ZM. Regarding use of topical steroids in patients with COVID-19-associated olfactory loss. JAMA Otolaryngology - Head and Neck Surgery 2021;147(1):110. [DOI] [PubMed] [Google Scholar]
Pinna 2020 {published data only}
- Pinna FR, Brandao Neto D, Fornazieri MA, Voegels RL. Olfaction and COVID: the little we know and what else we need to know. International Archives of Otorhinolaryngology 2020;24(3):e386-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saussez 2021 {published data only}
- Saussez S, Vaira LA, Chiesa-Estomba CM, Bon SL, Horoi M, Deiana G, et al. Short-term efficacy and safety of oral and nasal corticosteroids in covid-19 patients with olfactory dysfunction: a European multicenter study. Pathogens 2021;10(6):698. [CENTRAL: CN-02284588] [EMBASE: 2007537787] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
SCENT2 (NCT04789499) {published data only}
- NCT04789499. Smell in Covid-19 and efficacy of nasal theophylline. https://clinicaltrials.gov/show/NCT04789499 (first received 9 March 2021). [CENTRAL: CN-02249745]
Singh 2021 {published data only}
- Singh CV, Jain S, Parveen S. The outcome of fluticasone nasal spray on anosmia and triamcinolone oral paste in dysgeusia in COVID-19 patients. American Journal of Otolaryngology 2021;42(3):102892. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vaira 2021a {published data only}
- Vaira LA, Hopkins C, Petrocelli M, Lechien JR, Cutrupi S, Salzano G, et al. Efficacy of corticosteroid therapy in the treatment of long-lasting olfactory disorders in COVID-19 patients. Rhinology 2021;59(1):21-5. [CENTRAL: CN-02210463] [EMBASE: 633663621] [PMID: ] [DOI] [PubMed] [Google Scholar]
Vaira 2021c {published data only}
- Vaira LA, Lechien JR, Dore S, Boccaletti R, Saussez S, De Riu G. Specific therapy of olfactory disorders in COVID-19 patients is essential for the prevention of long-term dysfunction. Indian Journal of Otolaryngology and Head and Neck Surgery 2021;2021:1-2. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Varricchio 2021 {published data only}
- Varricchio A, La Mantia I, Brunese FP, Ciprandi G. Smell recovery in patients with COVID-19: an experience with nebulized nasal treatment. Journal of Biological Regulators and Homeostatic Agents 2021;35(2):683-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
VOLT (NCT04710394) {published data only}
- NCT04710394. Visual- olfactory training in participants with COVID-19 resultant loss of smell [Efficacy of bimodal visual-olfactory training in participants with COVID-19 resultant hyposmia or anosmia using participant-preferred scents]. https://clinicaltrials.gov/show/NCT04710394 (first received 14 January 2021). [CENTRAL: CN-02234021]
Vroegop 2020 {published data only}
- Vroegop AV, Eeckels AS, Van Rompaey V, Vanden Abeele D, Schiappoli M, Alobid I, et al. COVID-19 and olfactory dysfunction - an ENT perspective to the current COVID-19 pandemic. B-ENT 2020;16(1):81-5. [Google Scholar]
References to studies awaiting assessment
Mohamad 2021 {published data only}
- Mohamad SA, Badawi AM, Mansour HF. Insulin fast-dissolving film for intranasal delivery via olfactory region, a promising approach for the treatment of anosmia in COVID-19 patients: design, in-vitro characterization and clinical evaluation. International Journal of Pharmaceutics 2021;601:120600. [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT04657809. Clinical assessment of insulin fast dissolving film in treatment of post infection anosmia [Insulin fast dissolving film for intranasal delivery via olfactory region, a promising approach for the treatment of anosmia in COVID 19 patients: design, in-vitro characterization and clinical evaluation]. https://clinicaltrials.gov/show/NCT04657809 (first received 8 December 2020). [DOI] [PubMed]
References to ongoing studies
IRCT20210202050231N1 {published data only}
- IRCT20210202050231N1. Comparison of the effect of vanilla essential oil with eucalyptus essential oil on the return of olfactory sense in COVID-19 patients. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20210202050231N1.
IRCT20210205050247N {published data only}
- IRCT20210205050247N1. The effect of olfactory training and vitamin A in the olfactory loss of patients with covid-19 [A comparative study of the effect of olfactory training and vitamin A in the olfactory loss of patients with covid-19]. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20210205050247N1 (first received 2021). [CENTRAL: CN-02239119]
IRCT20210311050671N1 {published data only}
- IRCT20210311050671N1. Evaluation of the effect of laser acupuncture on improving the sense of smell in patients with COVID-19 [Effect of auricular acupuncture with the laser in post-viral anosmia during the COVID-19 pandemic]. http://www.who.int/trialsearch/Trial2.aspx?TrialID=IRCT20210311050671N1 (first received 2021). [CENTRAL: CN-02281866]
NCT04495816 {published data only}
- Lerner D, Garvey K, Arrighi-Allisan A, Filimonov A, Filip P, Liu K, et al. Letter to the editor: study summary - randomized control trial of omega-3 fatty acid supplementation for the treatment of COVID-19 related olfactory dysfunction. Trials 2020;21(1):942. [CENTRAL: CN-02200204] [EMBASE: 2007355105] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT04495816. COVID-19 anosmia study. https://clinicaltrials.gov/show/NCT04495816 (first received 3 August 2020). [CENTRAL: CN-02145765]
NCT04528329 {published data only}
- NCT04528329. Anosmia and / or ageusia and early corticosteroid use [Time to recover of anosmia and / or ageusia and early corticosteroid use]. https://clinicaltrials.gov/ct2/show/NCT04528329 (first received 27 August 2020).
NCT04530409 {published data only}
- NCT04530409. Timing of corticosteroids in COVID-19. https://clinicaltrials.gov/show/NCT04530409 (first received 28 August 2020).
NCT04638673 {published data only}
- NCT04638673. NeuroCovid rehab and recovery related to COVID-19 diagnosis [Testing a wearable telemedicine-controllable taVNS device for NeuroCovid recovery and rehab]. https://clinicaltrials.gov/show/NCT04638673 (first received 20 November 2020).
NCT04764981 {published data only}
- NCT04764981. Olfactory training for olfactory dysfunction after coronavirus disease - 19 (COVID-19) [Clinical outcomes of olfactory training for treatment of olfactory dysfunction after COVID-19]. https://clinicaltrials.gov/show/NCT04764981 (first received 21 February 2021). [CENTRAL: CN-02249160]
NCT04797936 {published data only}
- NCT04797936. BNO 1030 extract (Imupret) in the treatment of mild forms of COVID-19 [A randomized, open-label, multicentre, comparative study of therapeutic efficacy, safety, and tolerability of BNO 1030 extract, in the treatment of mild forms of COVID-19]. https://clinicaltrials.gov/show/NCT04797936 (first received 15 March 2021). [CENTRAL: CN-02249917]
NCT04900415 {published data only}
- NCT04900415. Olfactory and neurosensory rehabilitation in COVID-19-related olfactory dysfunction [Olfactory and neurosensory rehabilitation in coronavirus 2019 (COVID-19)-related olfactory dysfunction (OD)]. https://clinicaltrials.gov/show/NCT04900415 (first received 25 May 2021). [CENTRAL: CN-02277857]
NCT04951362 {published data only}
- NCT04951362. Role of ivermectin nanosuspension as nasal spray in treatment of persistant post covid19 anosmia [Studying the expected effect of ivermectin nanosuspension as nasal spray upon post covid19 persistant anosmia]. https://clinicaltrials.gov/show/NCT04951362 (first received 6 July 2021). [CENTRAL: CN-02290152]
NCT04959747 {published data only}
- NCT04959747. Acupuncture for olfactory dysfunction in infected COVID-19 patients [Acupuncture for olfactory dysfunction in infected COVID-19 patients: a randomized, sham-controlled clinical trial]. https://clinicaltrials.gov/show/NCT04959747 (first received 13 July 2021). [CENTRAL: CN-02279670]
NCT05002530 {published data only}
- NCT05002530. Investigating the potential role of aerosolized all-trans retinoic acid for treating COVID-19 anosmia and regaining sense of smell. https://clinicaltrials.gov/show/NCT05002530 (first received 12 August 2021).
TCTR20210714006 {published data only}
- TCTR20210714006. Corticosteroid nasal irrigation as early treatment of olfactory dysfunction in COVID-19: a prospective randomized controlled trial. http://www.who.int/trialsearch/Trial2.aspx?TrialID=TCTR20210714006. [DOI] [PMC free article] [PubMed]
UMIN000043537 {published data only}
- UMIN000043537. Post COVID-19 anosmia [Post COVID-19 anosmia treatments - anosmia treatments]. http://www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-UMIN000043537 (first received 2021). [CENTRAL: CN-02256500]
UMIN000045185 {published data only}
- UMIN000045185. "Additional value" of nasal therapy in standard therapy for COVID-19 patients with olfactory disorders: a Preliminary Randomized Controlled Clinical Trial. https://upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000051620 (first received 18 August 2021).
Additional references
Alexander 2006
- Alexander TH, Davidson TM. Intranasal zinc and anosmia: the zinc-induced anosmia syndrome. Laryngoscope 2006;116(2):217-20. [DOI: 10.1097/01.mlg.0000191549.17796.13] [PMID: ] [DOI] [PubMed] [Google Scholar]
Allen 2000
- Allen DB. Systemic effects of intranasal steroids: an endocrinologist’s perspective . Journal of Allergy and Clinical Immunology 2000;106(4):S179-90. [DOI] [PubMed] [Google Scholar]
Bigman 2020
- Bigman G. Age-related smell and taste impairments and vitamin D associations in the U.S. adults national health and nutrition examination survey. Nutrients 2020;12(4):984. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bilinska 2020
- Bilinska K, Butowt R. Anosmia in COVID-19: a bumpy road to establishing a cellular mechanism. ACS Chemical Neuroscience 2020;11(15):2152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boscolo‐Rizzo 2020
- Boscolo-Rizzo P, Borsetto D, Fabbris C, Spinato G, Frezza D, Menegaldo A, et al. Evolution of altered sense of smell or taste in patients with mildly symptomatic COVID-19. JAMA Otolaryngology - Head & Neck Surgery 2020;146(8):729-32. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Boscolo‐Rizzo 2021a
- Boscolo-Rizzo P, Menegaldo A, Fabbris C, Spinato G, Borsetto D, Vaira LA, et al. Six-month psychophysical evaluation of olfactory dysfunction in patients with COVID-19. Chemical Senses 2021 Feb 12 [Epub ahead of print]. [DOI: 10.1093/chemse/bjab006] [DOI] [PMC free article] [PubMed]
Boscolo‐Rizzo 2021b
- Boscolo-Rizzo P, Hummel T, Hopkins C, Dibattista M, Menini A, Spinato G, et al. High prevalence of long-term olfactory, gustatory, and chemesthesis dysfunction in post-COVID-19 patients: a matched case-control study with one-year follow-up using a comprehensive psychophysical evaluation. Rhinology 2021;59(6):517-27. [DOI: 10.4193/Rhin21.249] [DOI] [PubMed] [Google Scholar]
Butowt 2020
- Butowt R, Bartheld CS. Anosmia in COVID-19: underlying mechanisms and assessment of an olfactory route to brain infection. Neuroscientist 2020 Sep 11 [Epub ahead of print]. [DOI: 10.1177/1073858420956905] [PMID: ] [DOI] [PMC free article] [PubMed]
Cain 1988
- Cain WS, Gent JF, Goodspeed RB, Leonard G. Evaluation of olfactory dysfunction in the Connecticut Chemosensory Clinical Research Center. Laryngoscope 1988;98(1):83-8. [DOI] [PubMed] [Google Scholar]
Chary 2020
- Chary E, Carsuzaa F, Trijolet J-P, Capitaine A-L, Roncato-Saberan M, Fouet K, et al. Prevalence and recovery from olfactory and gustatory dysfunctions in COVID-19 infection: a prospective multicenter study. American Journal of Rhinology & Allergy 2020;34(5):686-93. [DOI: 10.1177/1945892420930954] [DOI] [PMC free article] [PubMed] [Google Scholar]
Croy 2014
- Croy I, Nordin S, Hummel T. Olfactory disorders and quality of life--an updated review. Chemical Senses 2014;39(3):185-94. [DOI: 10.1093/chemse/bjt072] [DOI] [PubMed] [Google Scholar]
Dai 2016
- Dai Q, Pang Z, Yu H. Recovery of olfactory function in postviral olfactory dysfunction patients after acupuncture treatment. Evidence-based Complementary and Alternative Medicine: ECAM 2016;2016:4986034. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Damm 2004
- Damm M, Temmel A, Welge-Lüssen A, Eckel HE, Kreft MP, Klussmann JP, et al. Olfactory dysfunctions. Epidemiology and therapy in Germany, Austria and Switzerland [Riechstörungen. Epidemiologie und Therapie in Deutschland, Osterreich und der Schweiz]. HNO 2004;52(2):112-20. [DOI] [PubMed] [Google Scholar]
Demoly 2008
- Demoly P. Safety of intranasal corticosteroids in acute rhinosinusitis. American Journal of Otolaryngology 2008;29(6):403-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Derin 2016
- Derin S, Koseoglu S, Sahin C, Sahan M. Effect of vitamin B12 deficiency on olfactory function. International Forum of Allergy & Rhinology 2016;6(10):1051-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629. [DOI] [PMC free article] [PubMed] [Google Scholar]
Erskine 2020
- Erskine SE, Philpott CM. An unmet need: patients with smell and taste disorders. Clinical Otolaryngology 2020;45(2):197-203. [DOI] [PubMed] [Google Scholar]
Fuccillo 2020
- Fuccillo E, Saibene AM, Canevini MP, Felisati G. Olfactory disorders in coronavirus disease 2019 patients: a systematic literature review. Journal of Laryngology & Otology 2020 Sep 15 [Epub ahead of print]. [DOI: 10.1017/S0022215120002005] [PMID: ] [DOI] [PMC free article] [PubMed]
Gerkin 2020
- Gerkin RC, Ohla K, Veldhuizen MG, Joseph PV, Kelly CE, Bakke AJ, et al. Recent smell loss is the best predictor of COVID-19 among individuals with recent respiratory symptoms. Chemical Senses 2020 Dec 25 [Epub ahead of print]. [DOI: 10.1093/chemse/bjaa081] [PMID: ] [DOI] [PMC free article] [PubMed]
Gudziol 2006
- Gudziol V, Lötsch J, Hähner A, Zahnert T, Hummel T. Clinical significance of results from olfactory testing. Laryngoscope 2006;116(10):1858-63. [PMID: ] [DOI] [PubMed] [Google Scholar]
Handbook 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Handbook 2020
- Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Hopkins 2020a
- Hopkins C, Kumar N. Loss of sense of smell as a marker of COVID-19 infection. https://www.sforl.org/wp-content/uploads/2020/03/Loss-of-sense-of-smell-as-marker-of-COVID-21-Mar-2020.pdf. [DOI] [PMC free article] [PubMed]
Hopkins 2020b
- Hopkins C, Burges Watson DL, Kelly C, Deary V, Smith BC. Managing long COVID: don't overlook olfactory dysfunction. BMJ 2020;370:m3736. [DOI] [PubMed] [Google Scholar]
Hopkins 2020c
- Hopkins C, Lechien JR, Saussez S. More that ACE2? NRP1 may play a central role in the underlying pathophysiological mechanism of olfactory dysfunction in COVID-19 and its association with enhanced survival. Medical Hypotheses 2021;146:110406. [DOI: 10.1016/j.mehy.2020.110406.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Huart 2020
- Huart C, Philpott C, Konstantinidis I, Altundag A, Whitcroft KL, Trecca EMC, et al. Comparison of COVID-19 and common cold chemosensory dysfunction. Rhinology 2020;58(6):623-5. [DOI: 10.4193/Rhin20.251] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hummel 2002
- Hummel T, Heilmann S, Hüttenbriuk KB. Lipoic acid in the treatment of smell dysfunction following viral infection of the upper respiratory tract. Laryngoscope 2002;112(11):2076-80. [PMID: ] [DOI] [PubMed] [Google Scholar]
Hummel 2016
- Hummel T, Whitcroft KL, Andrews P, Altundag A, Cinghi C, Costanzo RM, et al. Position paper on olfactory dysfunction. Rhinology 2016;56(1):1-30. [DOI] [PubMed] [Google Scholar]
Hummel 2017
- Hummel T, Whitcroft KL, Rueter G, Haehner A. Intranasal vitamin A is beneficial in post-infectious olfactory loss. European Archives of Oto-rhino-laryngology 2017;274(7):2819-25. [PMID: ] [DOI] [PubMed] [Google Scholar]
Klopfenstein 2020
- Klopfenstein T, Kadiane-Oussou NJ, Toko L, Royer PY, Lepiller Q, Gendrin V, et al. Features of anosmia in COVID-19. Medecine et Maladies Infectieuses 2020;50(5):436-9. [DOI: 10.1016/j.medmal.2020.04.006] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kubba 2000
- Kubba H, Spinou E, Robertson A. The effect of head position on distribution of drops within the nose. American Journal of Rhinology 2000;14:83-6. [DOI] [PubMed] [Google Scholar]
Landis 2003
- Landis BN, Hummel T, Hugentobler M, Giger R, Lacroix JS. Ratings of overall olfactory function. Chemical Senses 2003;28(8):691-4. [DOI] [PubMed] [Google Scholar]
Lechien 2020
- Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, Rodriguez A, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. European Archives of Oto-rhino-laryngology 2020;277(8):2251-61. [DOI: 10.1007/s00405-020-05965-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2020
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Technical Supplement to Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.1 (updated September 2020). Cochrane, 2020. Available from training.cochrane.org/handbook.
Lötsch 2019
- Lötsch J, Hummel T. Clinical usefulness of self-rated olfactory performance-a data science-based assessment of 6000 patients. Chemical Senses 2019;44:357-64. [DOI: 10.1093/chemse/bjz029] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mao 2020
- Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurology 2020;77(6):683-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marshall 2018
- Marshall J, Noel-Storr AH, Kuiper J, Thomas J, Wallace BC. Machine learning for identifying randomized controlled trials: an evaluation and practitioner's guide. Research Synthesis Methods 2018;9(4):602-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martineau 2020
- Martineau AR, Forouhi NG. Vitamin D for COVID-19: a case to answer? Lancet. Diabetes & Endocrinology 2020;8(9):735-6. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mattos 2018
- Mattos JL, Schlosser RJ, Mace JC, Smith TL, Soler ZM. Establishing the minimal clinically important difference for the Questionnaire of Olfactory Disorders. International Forum of Allergy & Rhinology 2018;8(9):1041-6. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
McDonald 2017
- McDonald S, Noel-Storr AH, Thomas J. Harnessing the efficiencies of machine learning and Cochrane Crowd to identify randomised trials for individual Cochrane reviews. In: Global Evidence Summit; Sep 13-17, Cape Town, South Africa. 2017.
Meng 2020
- Meng X, Deng Y, Dai Z, Meng Z. COVID-19 and anosmia: a review based on up-to-date knowledge. American Journal of Otolaryngology 2020;41(5):102581. [DOI] [PMC free article] [PubMed] [Google Scholar]
Menni 2020
- Menni C, Valdes AM, Freidin MB, Sudre CH, Nguyen LH, Drew DA, et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nature Medicine 2020;26(7):1037-40. [DOI: 10.1038/s41591-020-0916-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Noel‐Storr 2018
- Noel-Storr AH. The Project Transform Team. Cochrane Crowd: new ways of working together to produce health evidence. In: Evidence Live; 2018 June 18-20; Oxford, UK. 2018.
O'Byrne 2022
- O'Byrne L, Webster KE, MacKeith S, Philpott C, Hopkins C, Burton MJ. Interventions for the treatment of persistent post-COVID-19 olfactory dysfunction. Cochrane Database of Systematic Reviews 2022, Issue 8. Art. No: CD013876. [DOI: 10.1002/14651858.CD013876.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ohla 2021
- Ohla K, Veldhuizen MG, Green T, Hannum ME, Bakke AJ, Moien ST, et al. Increasing incidence of parosmia and phantosmia in patients recovering from COVID-19 smell loss. https://www.medrxiv.org/content/10.1101/2021.08.28.21262763v2 2021. [DOI: ]
Parma 2020
- Parma V, Ohla K, Veldhuizen MG, Niv MY, Kelly CE, Bakke AJ, et al. More than smell - COVID-19 is associated with severe impairment of smell, taste and chemesthesis. Chemical Senses 2020;45(7):609–22. [DOI: 10.1093/chemse/bjaa041] [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2017
- Patel ZM, Wise SK, DelGaudio JM. Randomized controlled trial demonstrating cost‐effective method of olfactory training in clinical practice: essential oils at uncontrolled concentration. Laryngoscope Investigative Otolaryngology 2017;2(2):53-6. [DOI: 10.1002/lio2.62] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pekala 2016
- Pekala K, Chandra RK, Turner JH. Efficacy of olfactory training in patients with olfactory loss: a systematic review and meta-analysis. International Forum of Allergy & Rhinology 2016;6(3):299-307. [DOI] [PMC free article] [PubMed] [Google Scholar]
Philpott 2014
- Philpott CM, Boak D. The impact of olfactory disorders in the United Kingdom. Chemical Senses 2014;39(8):711-8. [DOI: 10.1093/chemse/bju043] [DOI] [PubMed] [Google Scholar]
Quint 2002
- Quint C, Temmel AF, Hummel T, Ehrenberger K. The quinoxaline derivative caroverine in the treatment of sensorineural smell disorders: a proof-of-concept study. Acta Oto-laryngologica 2002;122(8):877-81. [PMID: ] [PubMed] [Google Scholar]
Raghavan 2000
- Raghavan U, Logan BM. New method for the effective instillation of nasal drops. Journal of Laryngology & Otology 2000;114:456-9. [DOI] [PubMed] [Google Scholar]
Reden 2011
- Reden J, Herting B, Lill K, Kern R, Hummel T. Treatment of postinfectious olfactory disorders with minocycline: a double-blind, placebo-controlled study. Laryngoscope 2011;121(3):679-82. [PMID: ] [DOI] [PubMed] [Google Scholar]
RevMan 2020 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: The Cochrane Collaboration, 2020.
Rocke 2020
- Rocke J, Hopkins C, Philpott C, Kumar N. Is loss of sense of smell a diagnostic marker in COVID-19: a systematic review and meta-analysis. Clinical Otolaryngology 2020;45(6):914-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saussez 2020
- Saussez S, Lechien JR, Hopkins C. Anosmia: an evolution of our understanding of its importance in COVID-19 and what questions remain to be answered. European Archives of Oto-rhino-laryngology 2020 Sep 9 [Epub ahead of print]. [DOI: 10.1007/s00405-020-06285-0] [PMID: ] [DOI] [PMC free article] [PubMed]
Scheibe 2008
- Scheibe M, Bethge C, Witt M, Hummel T. Intranasal administration of drugs. Archives of Otolaryngology--Head and Neck Surgery 2008;134(6):643-6. [DOI] [PubMed] [Google Scholar]
Seiden 2001
- Seiden AM, Duncan HJ. The diagnosis of a conductive olfactory loss. Laryngoscope 2001;111(1):9-14. [DOI] [PubMed] [Google Scholar]
Sorokowska 2017
- Sorokowska A, Drechsler E, Karwowski M, Hummel T. Effects of olfactory training: a meta-analysis. Rhinology 2017;55(1):17-26. [DOI] [PubMed] [Google Scholar]
Spinato 2020
- Spinato G, Fabbris C, Polesel J, Cazzador D, Borsetto D, Hopkins C, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA 2020;323(20):2089-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Takerkhani 2015
- Taherkhani S, Moztarzadeh F, Mehdizadeh Seraj J, Hashemi Nazari SS, Taherkhani F, Gharedaghi J, et al. Iran Smell Identification Test (Iran-SIT): a modified cersion of the University of Pennsylvania Smell Identification Test (UPSIT) for Iranian population. Chemosensory Perception 2015;8:183-91. [DOI: ] [Google Scholar]
Thomas 2017
- Thomas J, Noel-Storr AH, Marshall I, Wallace B, McDonald S, Mavergames C, et al, Living Systematic Review Network. Living systematic reviews 2: combining human and machine effort. Journal of Clinical Epidemiology 2017;91:31-7. [DOI] [PubMed] [Google Scholar]
Tierney 2007
- Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007;8:16. [DOI: 10.1186/1745-6215-8-16.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vaira 2021b
- Vaira LA, Salzano G, Le Bon SD, Maglio A, Petrocelli M, Steffens Y, et al. Prevalence of persistent olfactory disorders in patients with COVID-19: a psychophysical case-control study with 1-year follow-up. Otolaryngology - Head and Neck Surgery 2021 Nov 23 [Epub ahead of print]. [DOI: 10.1177/01945998211061511] [DOI] [PubMed]
Vent 2010
- Vent J, Wang DW, Damm M. Effects of traditional Chinese acupuncture in post-viral olfactory dysfunction. Otolaryngology - Head and Neck Surgery 2010;142(4):505-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
von Bartheld 2020
- Bartheld CS, Hagen MM, Butowt R. Prevalence of chemosensory dysfunction in COVID-19 patients: a systematic review and meta-analysis reveals significant ethnic differences. ACS Chemical Neuroscience 2020;11(19):2944-61. [DOI: 10.1021/acschemneuro.0c00460] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wallace 2017
- Wallace BC, Noel-Storr AH, Marshall IJ, Cohen AM, Smalheiser NR, et al. Identifying reports of randomized controlled trials (RCTs) via a hybrid machine learning and crowdsourcing approach. Journal of the American Medical Informatics Association 2017;24(6):1165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Welge‐Luessen 2005
- Welge-Luessen A, Hummel T, Stojan T, Wolfensberger M. What is the correlation between ratings and measures of olfactory function in patients with olfactory loss? American Journal of Rhinology 2005;19(6):567-71. [PubMed] [Google Scholar]
References to other published versions of this review
Webster 2021a
- Webster KE, MacKeith S, Philpott C, Hopkins C, Burton MJ. Interventions for the prevention of persistent post‐COVID‐19 olfactory dysfunction. Cochrane Database of Systematic Reviews 2021, Issue 3. Art. No: CD013877. [DOI: 10.1002/14651858.CD013877] [DOI] [PMC free article] [PubMed] [Google Scholar]
Webster 2021b
- Webster KE, O'Byrne L, MacKeith S, Philpott C, Hopkins C, Burton MJ. Interventions for the prevention of persistent post‐COVID‐19 olfactory dysfunction. Cochrane Database of Systematic Reviews 2021, Issue 7. Art. No: CD013877. [DOI: 10.1002/14651858.CD013877.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


