Background:
The development of automated, smartphone application (app)-assisted home blood pressure monitoring (HBPM) allows for standardized measurement of blood pressure (BP) at home. The aim of this study was to evaluate the (diagnostic) agreement between app-assisted HBPM, automated office BP (OBP), and the reference standard 24-hour ambulatory BP monitoring (ABPM).
Methods:
In this open randomized 5-way cross-over study, patients diagnosed with hypertension were randomized to one of 10 clusters, each containing 5 BP measurement methods (ABPM, HBPM, attended OBP, unattended OBP, and unattended 30-minute BP) in different order.
Results:
In total, 113 patients were included. The average 24-hour ABPM was 126±11/73±8 mm Hg compared with 141±14/82±10 mm Hg with app-assisted HBPM, 134±13/80±9 mm Hg with unattended 30-minute BP, 137±16/81±11 mm Hg with attended OBP, and 135±15/81±10 mm Hg with unattended OBP monitoring. Diagnostic agreement between app-assisted HBPM and 24-hour ABPM for diagnosing sustained (OBP >140/90 mm Hg and ABPM ≥130/80 mm Hg or HBPM ≥135/85 mm Hg), white-coat (OBP ≥140/90 mm Hg and ABPM <130/80 mm Hg or HBPM <135/85 mm Hg), and masked hypertension (OBP <140/90 mm Hg and ABPM ≥130/80 mm Hg or HBPM ≥135/85 mm Hg) was fair-to-moderate (κ statistics ranging from 0.34 to 0.40). App-assisted HBPM had high sensitivities (78%–91%) and negative predictive values (90%–97%) for diagnosing sustained and masked hypertension.
Conclusions:
This study showed a considerable (diagnostic) disagreement between app-assisted HBPM and ABPM. App-assisted HBPM had high sensitivity in the diagnosis of sustained and masked hypertension and may therefore be used as complementary to, but not a replacement of, ABPM.
Keywords: ambulatory blood pressure monitoring, blood pressure, home blood pressure monitoring, hypertension, masked hypertension, white-coat hypertension
Novelty and Relevance.
What Is New?
This is one of the first studies that has directly compared smartphone application (app)-assisted home blood pressure monitoring (HBPM) with office and ambulatory BP monitoring in patients with hypertension.
What Is Relevant?
We demonstrate that app-assisted HBPM substantially overestimates 24-hour ambulatory BP monitoring by 15/8 mm Hg.
Overall, app-assisted HBPM showed fair-to-moderate diagnostic agreement with 24-hour ambulatory BP monitoring for the diagnosis of sustained, white-coat, and masked hypertension.
App-assisted HBPM showed high sensitivities and negative predictive values for diagnosing sustained and masked hypertension.
Clinical/Pathophysiological Implications?
App-assisted HBPM should be considered as complementary rather than competitive to 24-hour ambulatory BP monitoring in the monitoring of patients with hypertension.
Based on its high sensitivity and negative predictive value for diagnosing sustained and masked hypertension, app-assisted HBPM could be used as a screening test for these diagnoses.
Proper diagnosis and monitoring of hypertension relies on accurate measurement of the blood pressure (BP) level.1,2 Traditionally, the diagnosis and monitoring of hypertension is based on conventional office BP (OBP) measurements, either taken by a mercury sphygmomanometer or, nowadays more commonly, an automatic oscillometric device.3 Although OBP readings are obtained conveniently and rapidly, they are easily confounded, leading to incorrect diagnoses of normotension and hypertension called masked hypertension and white-coat hypertension, respectively.4,5 Moreover, several meta-analyses have shown that compared with OBP measurements, out-of-office BP measurements have a stronger association with cardiovascular risk.6,7 Therefore, out-of-office BP monitoring, either performed by home blood pressure monitoring (HBPM) or 24-hour ambulatory blood pressure measurement (ABPM), is recommended for the diagnosis and monitoring of hypertension by several guidelines1,2,8,9 Currently, ABPM is considered the reference standard because of the large evidence base demonstrating its strong association with future cardiovascular events.10
Although ABPM has several unique advantages such as its capability of monitoring BP during sleep and daily activities, it is a burdensome and costly method that is not widely available, especially in primary care settings.11 Home BP monitoring is not only able to capture day-to-day variability and less expensive than ABPM but also allows patients to take a greater role in self-management of hypertension, which may have a beneficial effect on medication adherence and BP control.12 However, the need for manual notation of self-measured BP by the patient, especially in the home setting, is prone to (unintentional) errors, which could compromise the reliability of HBPM.13,14 The introduction of smartphone application (app)-assisted HBPM, in which BP measurements taken with a validated BP device can be automatically transferred to a smartphone app, might improve reliability and widespread use of HBPM in clinical practice.15 How such app-assisted HBPM methods compare to the reference standard ABPM and automated OBP monitoring has not been clarified yet.
Therefore, the objectives of this study were to (1) compare BP measured by automated OBP (attended, unattended, and unattended 30-minute), app-assisted HBPM, and the reference standard ABPM; (2) to evaluate the agreement between app-assisted HBPM, automated OBP (attended, unattended, and unattended 30-minute), and ABPM in diagnosing hypertension; and (3) to evaluate the agreement between app-assisted HBPM and ABPM in diagnosing sustained, white-coat, and masked hypertension, in patients with hypertension.
Methods
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study Design and Participants
The AMUSE-BP study (Ambulant Versus Unattended and Attended Office Versus Self-Home Blood Pressure Measurement) was an open randomized 5-way cross-over study that included patients diagnosed with hypertension in 3 hypertension clinics (University Medical Center Utrecht, Ziekenhuis Gelderse Vallei in Ede, and Rijnstate in Arnhem) in the Netherlands between March 2020 and February 2022. Participants were ≥18 years of age, were stable on antihypertensive medication for at least 2 months, and were familiar with the use of a smartphone or tablet. Participants were ineligible if they had a systolic/diastolic BP (SBP/DBP) ≥180/110 mm Hg or ≤90/60 mm Hg during the screening visit, or suffered from conditions that may result in unstable BP (eg, pregnancy, endocrine disorders, arrhythmias, heart failure ≥ New York Heart Association class II). Supplemental File S1 provides further details on the inclusion and exclusion criteria. The study protocol was approved by the institutional review board, and all participants provided written informed consent. The study is registered at www.trialregister.nl (ID NL8277).
Study Procedures
At screening, BP was measured 3 times simultaneously on the right and left upper arm in an upright position with 1-minute intervals by a trained research nurse using the Microlife WatchBP Office AFIB (Microlife Corp, Widnau, Switzerland) device.16 Screening BP was recorded as the average of these 3 measurements. The arm with the highest average BP value was considered the reference. To collect demographic information a structured questionnaire was administered.
Eligible participants were randomly assigned to one of the 10 randomization arms, each of which prescribed to perform 5 BP measurements methods (attended OBP, unattended OBP, unattended 30-minute OBP, HBPM, and 24-hour ABPM) in different predefined orders over a 3-week period (Figure S1). The randomization arms were generated by the Latin Square method which allows to control for the carry-over effect.17 In addition, we applied a wash-out period of 2 to 4 days between all BP measurement methods, except when an out-of-office BP measurement followed an OBP measurement. If a measurement failed, the measurement was repeated until a valid measurement was obtained. If this was not possible, the measurement was noted as missing data.
OBP Monitoring
Three types of OBP measurements were obtained: an attended OBP, an unattended OBP, and an unattended 30-minute OBP. All OBP measurements were taken by the research nurse who activated the BP monitor.
Attended OBP included triplicate measurements with 1-minute intervals using an automatic oscillometric device (Microlife WatchBP Office AFIB; Microlife Corp, Widnau, Switzerland) device16 that was programmed to measure the BP after the patient had rested for at least 5 minutes in a sitting position. Measurement was performed with an appropriately sized cuff on the reference arm. The research nurse stayed in the office until all measurements were completed. OBP was determined as the mean of all 3 measurements. Unattended OBP was obtained in exactly the same manner as attended OBP but without the research nurse attending the programmed 5-minute resting period and the triplicate BP measurements.
Thirty-minute OBP was obtained from the reference arm, with the Microlife WatchBP Office AFIB 30 minutes (Microlife Corp, Widnau, Switzerland) device.18 This device was programmed to perform 6 consecutive measurements with 5-minute intervals after 5 minutes of seated rest.19 Thirty-minute OBP was performed without the research nurse in the office which also makes it an unattended BP measurement. However, an important difference compared with the unattended OBP described above is that in this measurement, the average value of 6 rather than 3 BP measurements was used for the analysis.
Home BP Monitoring
HBPM was performed with the Microlife A6 BT (Microlife Corp, Widnau, Switzerland)20 combined with the EmmaHBPM app (Medicine Men, Utrecht, the Netherlands)21 with an appropriately sized cuff around the reference arm. The EmmaHBPM app is able to graphically display BP measurements, indicate whether the BP is within the normal range, and thus gives patients more insight into their BP.
Before HBPM, participants were trained on the conditions of HBPM, the use of the device, and use of the EmmaHBPM app. Participants were instructed to measure their BP at home every morning and evening for 7 consecutive days, after 5 minutes of rest in a sitting position. Morning BP had to be measured between 6 am and 9 am, and evening BP had to be measured between 6 pm and 9 pm. BP was measured using the Microlife Average Mode mode, which calculates a weighted average of a minimum of 3 consecutive BP readings with standardized 15-second intervals. In this mode, a specific algorithm takes into account the change in BP between sequential readings to determine the weight for the average of all readings. If the difference in consecutive measurements exceeds 40 mm Hg for SBP and 25 mm Hg for DBP, the highest measurement is rejected and an additional fourth measurement is taken. If the difference is between 18 and 40 mm Hg for SBP and 12 to 25 mm Hg for DBP, the higher measurement contributes only 50% to the average.22 After calculation of the weighted average, the device discards the 3 separate measurements obtained. BP measurements obtained with the Microlife A6 BT device had to be synchronized by the patient via Bluetooth with the EmmaHBPM app installed on the patient’s smartphone or tablet. A valid HBPM was defined as having at least 11 valid Microlife Average Mode readings within a 7-day time period. For calculation of the mean home BP, readings from the first measurement day were discarded, which is in line with the current practice guidelines.11
Ambulatory BP Monitoring
Ambulatory BP was monitored using the Microlife WatchBP O3 BP AFIB device (Microlife Corp, Widnau, Switzerland)23 with an appropriate-sized cuff on the nondominant arm. If the interarm BP difference at screening was ≥20/10 mm Hg, ABPM had to be performed on the arm with the highest BP. BP measurements were taken at 20-minute intervals over a 24-hour period. All individuals were instructed to follow their usual daily activity pattern and to report the performed activities. Reported activities were reviewed and discussed with the patient. If patients performed activities that did not fit into their usual daily pattern, including activities that potentially resulted in extreme BP readings, a repeat ABPM could be considered. Mean awake and asleep BP were calculated using predefined nighttime (10 pm–6 am) and daytime (6 am–10 pm) periods. In line with the European guidelines, a valid ABPM was defined as having ≥20 daytime readings and ≥7 nighttime readings with at least 70% of all attempted BP readings being successful.2 The BP readings during the 24-hour, daytime, and nighttime period were averaged to obtain mean 24-hour, mean daytime, and mean nighttime BP, respectively.
Definition of Hypertension Categories
In line with the current hypertension guidelines,1,2,11 we defined office hypertension as a mean SBP ≥140 mm Hg and mean DBP ≥90 mm Hg when based on the attended/unattended office measurements, and as a mean SBP ≥135 mm Hg and mean DBP ≥85 mm Hg when based on 30-minute BP readings. The corresponding thresholds were 135 mm Hg systolic and 85 mm Hg diastolic for home hypertension, 130 mm Hg systolic and 80 mm Hg diastolic for 24-hour ambulatory hypertension, and 135 mm Hg systolic and 85 mm Hg diastolic for daytime ambulatory hypertension. Sustained hypertension was defined as a consistently elevated office and out-of-office BP (home or 24-hour ambulatory). White-coat hypertension was defined as an elevated office and a normal out-of-office BP and masked hypertension as the reverse (normal office and elevated out-of-office BP).
Data Analysis
To obtain 90% power of detecting a clinical important mean difference in BP of >3 mm Hg between app-assisted HBPM and ABPM assuming a SD of the difference of 8.9 mm Hg,24 a sample of at least 95 participants completing the study was required. Taking into account 25% drop-out, we aimed to include 120 patients.
Patient characteristics were presented as categorical (n [%]), normal distributed continuous (mean±SD) or non-normal distributed continuous (median [interquartile range]). Means and proportions were compared by the Student t test and McNemar test, respectively.
To evaluate the differences between absolute values of the various BP measurement methods, a linear mixed effects model was fitted. Random intercepts for patients accounted for the dependence of repeated measurements and the variability between patients. Models were adjusted for age, sex, body mass index, and smoking. Fundamental assumptions of the linear mixed model (eg, normality of the residuals and homogeneity of variance) were tested to ensure the accuracy of results. The use of a mixed model allowed for appropriate handling of missing data in the outcome variable, assuming that the data were missing at random.25
In addition, Bland-Altman plots were used to provide a visualized assessment of the agreement between the different BP measurement methods. For these plots, the average of measurements evaluated by 2 different methods (eg. HBPM and ABPM) is plotted against their difference for both SBP and DBP. A priori, we defined a difference >3 mm Hg as clinically relevant, based on the previously observed effect on cardiovascular morbidity and mortality associated with this difference.26
The diagnostic agreement between HBPM and ABPM in detecting sustained, white-coat, and masked hypertension was assessed using the kappa (κ) statistic. A κ statistic ≥0.80 was a priori considered to represent good agreement.27 In addition, we computed sensitivity, specificity, positive, and negative predictive values.
For the primary analyses of this study, the average ABPM was based on all BP readings taken during the 24-hour measurement period. However, since office and home BP are only based on BP readings taken during daytime, we also performed a sensitivity analysis in which the average ABPM was based on BP readings taken between 6 am and 10 pm.
All analyses were performed with R statistical software (Version 3.5.1; R foundation for Statistical Computing, Vienna, Austria). All P values were 2-tailed, with statistical significance set at 0.05.
Results
Patient Characteristics
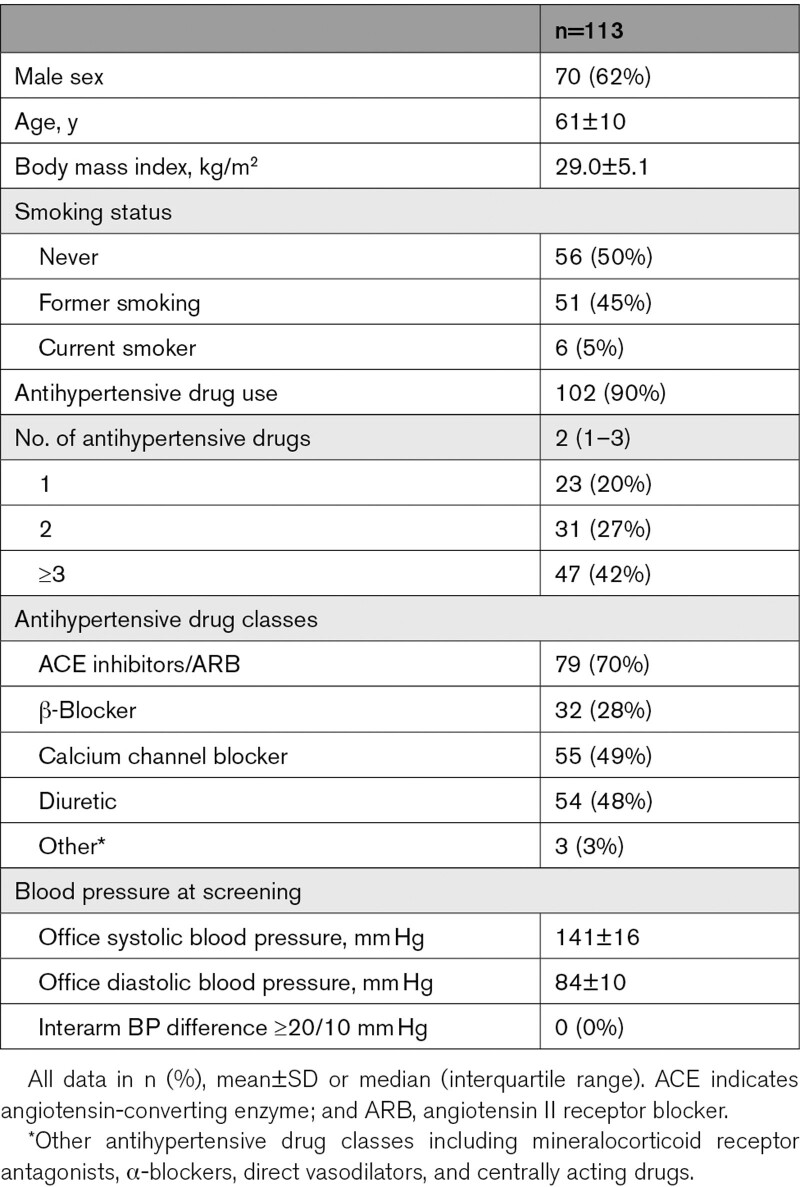
Between February 2020 and March 2022, a total of 120 individuals were screened (Figure S2). Of these, 5 did not meet the eligibility criteria, one due to a recent change in prescribed medication and 4 due to extremely elevated BP (≥180/110 mm Hg). During the study, 2 patients dropped out due to comorbidities unrelated to the study, one of whom was later rescreened. The characteristics of the 113 study participants included in the analyses are shown in Table 1. Mean age of the study population was 61±10 years and 70 (62%) patients were male. Most patients were prescribed antihypertensive drugs (90%) with an average number of 2 antihypertensive drug classes.
Table 1.
Characteristics of the Study Population
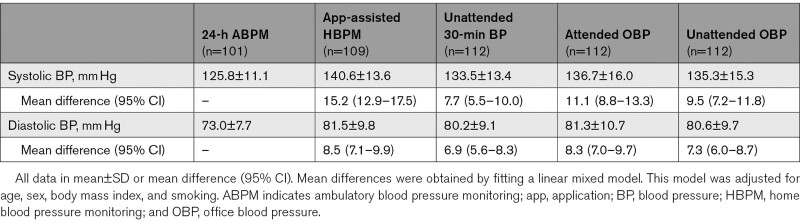
Agreement Between Automated Office, App-Assisted Home, and 24-Hour BP
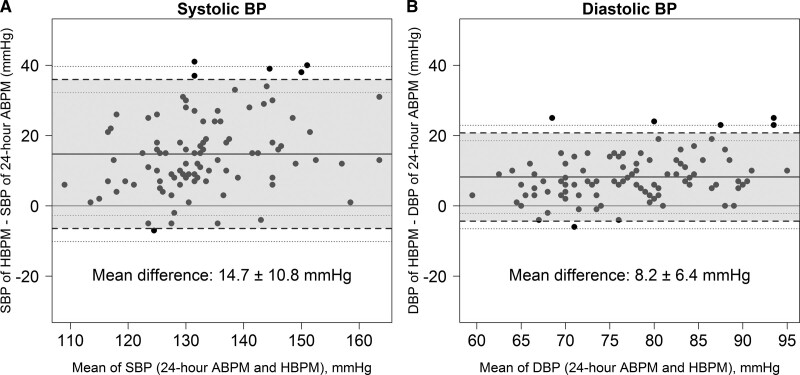
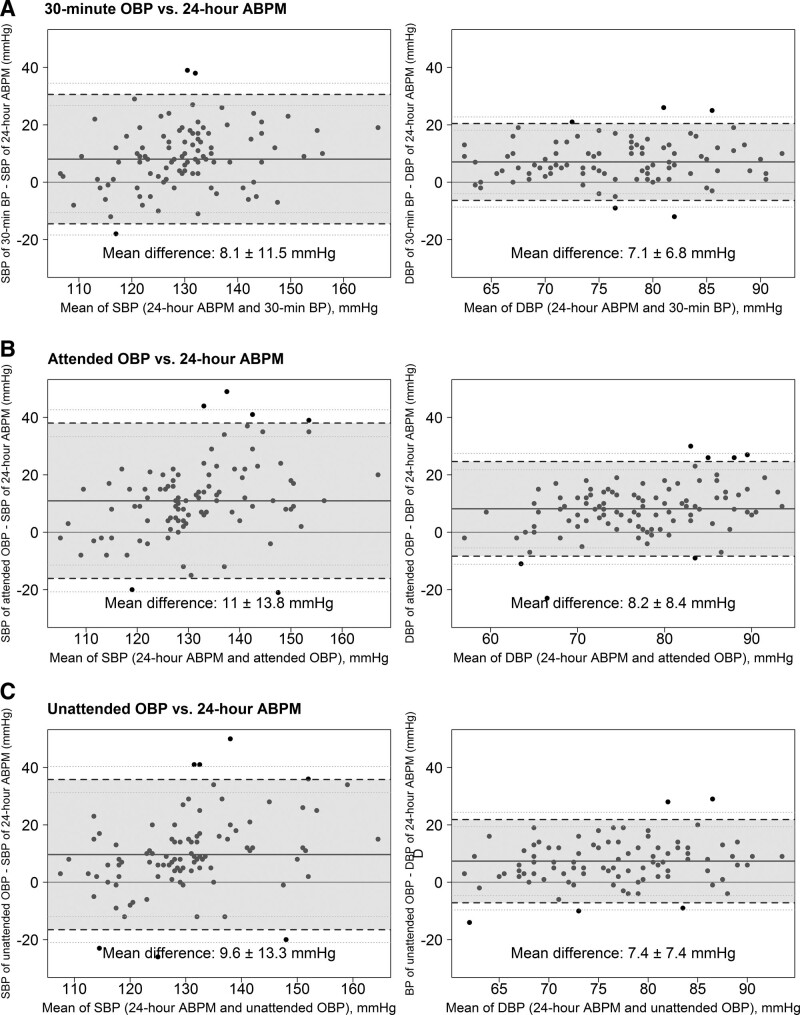
Table 2 reports the mean SBP and DBP for each measurement method and their difference compared with 24-hour ABPM as the reference method. Since not all patients completed all 5 BP measurements, the number of measurements varies per BP measurement method. Of the 113 patients, 101 (89%) had valid ABPM measurements, 109 (96%) had valid HBPM measurements, and 112 (99%) had valid OBP measurements. SBP measured by HBPM and the OBP measurement methods were significantly different from 24-hour ABPM, with the latter being the lowest (Table 2). The mean difference between the HBPM and 24-hour ABPM SBP was 15 mm Hg (95% of the differences were between −6 and 36 mm Hg; 95% limits of agreement; Figure 1), whereas the mean differences between the unattended 30-minute, attended, and unattended OBP and 24-hour ABPM were 8 mm Hg (95% limits of agreement: −14 to 31 mm Hg), 11 mm Hg (95% limits of agreement: −16 to 38 mm Hg), and 10 mm Hg (95% limits of agreement: −16 to 36 mm Hg), respectively (Figure 2). With respect to the DBPs, differences showed a similar pattern (Figure 2). When daytime ABPM was used as the reference, the differences in BP with all BP methods were smaller, but still clinically relevant (>3 mm Hg; Table S1 and Figure S3).
Table 2.
Mean BP Values for Each BP Measurement Method and the Difference Compared With 24-Hour ABPM (Reference)
Figure 1.
Bland-Altman plots of agreement between home and ambulatory systolic (SBP) and diastolic (DBP) blood pressure (BP). Plots comparing the difference between app-assisted home blood pressure monitoring (HBPM) and ambulatory BP monitoring (ABPM) SBP (A) and DBP (B) on the y-axis with the mean of the 2 methods on the x-axis.
Figure 2.
Bland-Altman plots of agreement between automated office and ambulatory systolic (SBP) and diastolic (DBP) blood pressure (BP). Plots comparing the difference between unattended 30-min (A), attended office (B), and unattended office (C) and 24-h ambulatory BP on the y-axis with the mean of the 2 methods on the x-axis. Plots on the left indicate show agreement for systolic BP and plots on the right indicate agreement for diastolic BP. ABPM indicates ambulatory BP monitoring; and OBP, office BP.
Diagnostic Agreement Between Automated Office, App-Assisted HBPM, and 24-Hour ABPM in Diagnosing Hypertension
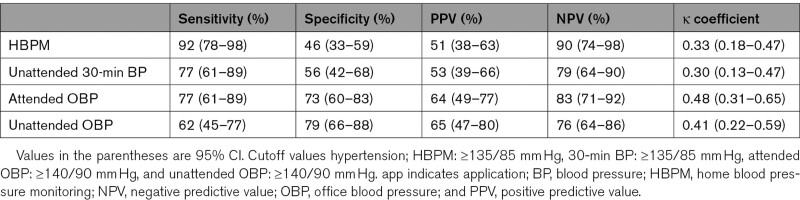
Figure S4 shows the prevalence of hypertension according to each BP measurement method using the method-specific hypertension thresholds. Prevalence of hypertension was 39% for 24-hour ABPM, 69% for app-assisted HBPM, 47% for attended OBP, 38% for unattended OBP, and 56% for unattended 30-minute BP. Compared with the office-based BP measurement methods, app-assisted HBPM showed a higher sensitivity (92% versus 62%–77%) and negative predictive value (90% versus 76%–83%) for the diagnosis of hypertension (Table 3). Sensitivity analyses using daytime ABPM instead of 24-hour ABPM gave similar results with the main analysis (Table S2).
Table 3.
Diagnostic Performance of App-Assisted HBPM and Automated OBP Monitoring in Detecting Hypertension Diagnosed by 24-Hour Ambulatory Blood Pressure Monitoring (Reference)
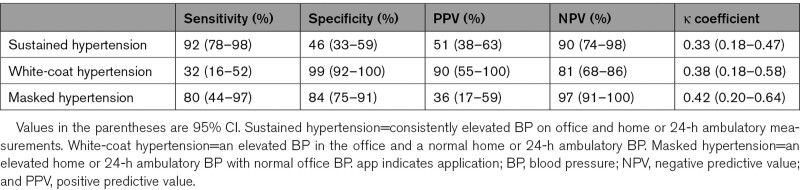
Diagnostic Agreement Between App-Assisted HBPM and 24-Hour ABPM in Diagnosing Sustained, White-Coat, and Masked Hypertension
Compared with 24-hour ABPM, app-assisted HBPM showed a significant higher prevalence of sustained (39% versus 69%; P<0.05) and masked hypertension (10% versus 23%; P<0.05) but showed a significant lower prevalence of white-coat hypertension (23% versus 10%; P<0.05; Figure S5).
If the 24-hour ABPM was considered as the standard for the diagnosis of white-coat, masked, and sustained hypertension, app-assisted HBPM showed fair-to-moderate diagnostic agreement (κ statistics 0.34–0.40; Table 4). Overall, the sensitivity, specificity, positive predictive value, and negative predictive value for each diagnosis indicated moderate diagnostic performance. However, for the diagnosis of sustained and masked hypertension, app-assisted HBPM had relatively high sensitivities (range 80%––90%) and negative predictive values (range 90%–97%; Table 4). Sensitivity analyses using daytime ABPM instead of 24-hour ABPM gave similar results with the main analysis (Table S3 and Figure S6).
Table 4.
Diagnostic Performance of App-Assisted Home Against 24-Hour Ambulatory BP Monitoring (Reference) in Detecting Different Hypertension Phenotypes
Discussion
The present study shows that in patients with hypertension, BP measured by the reference standard 24-hour ABPM was overestimated by 15/8 mm Hg using app-assisted HBPM, 8/7 mm Hg using 30-minute BP, 11/8 mm Hg using attended OBP, and 10/7 mm Hg using unattended OBP. In addition, app-assisted HBPM showed better performance in diagnosing hypertension than automated OBP measurements, using ABPM as the reference. App-assisted HBPM showed fair-to-moderate diagnostic agreement with ABPM for the diagnosis of sustained, white-coat, and masked hypertension.
Although current hypertension guidelines evenly recommend home and ambulatory measurements for the diagnosis and monitoring of BP, the different diagnostic thresholds for hypertension already suggest an essential difference between both methods.1,2 However, the magnitude of the difference between app-assisted home and ambulatory BP found in this study has rarely been described. The HOMERUS (Home Versus Office Measurements, Reduction of Unnecessary Treatment Study), a randomized clinical trial in patients with hypertension that investigated whether one can safely base antihypertensive treatment decisions on HBPM, also described a considerable difference of +12/5 mm Hg between 7-day home and 24-hour ambulatory BP.28 Likewise, a study that evaluated HBPM usefulness in the management of patients with resistant hypertension showed a difference of +11/1 mm Hg between 4-day HBPM and 24-hour ABPM.29
Several explanations for this clinically relevant difference may be considered. Although HBPM and ABPM both measure BP outside the office, the conditions in which BP is measured for both methods greatly differ. HBPM is performed in the morning and evening, whereas ABPM is performed over a period of 24 hours in ambulatory conditions (at home or work, during active and inactive phases, without a period of rest before measurements, and during sleeping hours). Both methods might, therefore, simply reflect different aspects of BP profile and behavior. Also, patients often ensure that they have a quiet schedule on the day of ABPM because of the burdensome aspect (BP recording at 20-minute intervals) of this measurement which might have resulted in a lower BP. In addition, the app-assisted HBPM method as applied in this study was a newly developed method that requires experience using a smartphone and a number of additional actions from the patient. Since this may be more difficult and stressful than standard HBPM methods, it may have led to higher home BP readings. Last, in contrast to many previous studies,24,30,31 home BP values obtained by this study were not self-reported. It has been shown that HBPM readings reported by patients frequently differ from the actually measured values automatically stored in the device memory.13 Therefore, previous studies might suffer from misreporting by the patient which potentially resulted in an underestimated difference between HBPM and ABPM.
While understanding the mechanisms underlying the difference between app-assisted HBPM and 24-hour ABPM is important, the practical question is whether these BP differences actually result in different diagnoses and treatment decisions. The current study showed moderate diagnostic agreement between app-assisted HBPM and ABPM in diagnosing sustained, white-coat, and masked hypertension, which is consistent with findings from previous studies.32,33 Similar to our study, a recent meta-analysis of 4 studies that evaluated the effectiveness of HBPM compared with ABPM for the diagnosis of hypertension found a pooled sensitivity of 0.84 (95% CI, 0.76–0.90) and a pooled specificity of 0.60 (95% CI, 0.48–0.71).34 Due to this limited diagnostic performance, (app-assisted) HBPM should not be relied on for making the final diagnosis of sustained, white-coat, or masked hypertension. However, the high sensitivity and negative predictive value for the diagnosis of sustained hypertension and masked hypertension indicate that app-assisted HBPM seems suitable to be used as a screening method for these diagnoses, which, if positive, requires confirmation with 24-hour ABPM. This is further supported by the fact that in the current study, automated OBP, still the most widely used method for hypertension detection and management today,11 showed worse diagnostic agreement with ABPM for the diagnosis of sustained hypertension than app-assisted HBPM. Since HBPM has also been shown to be a more reliable predictor of cardiovascular outcomes than OBP,35 app-assisted HBPM should, therefore, be the preferred method for screening on sustained hypertension.
Based on the above-mentioned findings, app-assisted HBPM and ABPM appear to have a complementary rather than a competitive role in the evaluation of hypertension and provide similar but also different information about the BP profile and behavior of a patient. This is supported by findings from an outcome study where patients with partial masked hypertension (elevated ambulatory but normal home BP values or the reverse and normal OBP values) were at increased cardiovascular risk compared with patients with sustained normotension (normal BP on OBP, ABPM, and HBPM), but at lower risk compared with patients with sustained hypertension (elevated office and out-of-office BP), implying additive prognostic information provided by each method.36
Although out-of-office BP monitoring by 24-hour ABPM or HBPM is increasingly used and endorsed by the recent hypertension guidelines,1,2,9,11 diagnosis and monitoring of hypertension is still frequently based on OBP measurements, especially in settings with limited financial resources and time. Since conventional auscultatory OBP is known to suffer from observer-related bias and unstandardized measurement conditions,37 validated automated BP devices are increasingly used for this purpose. Such devices can be used with (attended) or without (unattended) the presence of a physician or a nurse. Consistent with results of the SPRINT (Systolic Blood Pressure Intervention Trial)38 and with findings of a previous meta-analysis,37 this study found an unattended-attended automated OBP difference of −1.5/−1.0 mm Hg (Table 2) which is considered a nonclinically relevant difference (<3 mm Hg). These findings suggest that when automated OBP measurements are performed under standardized conditions (resting period, triplicate measurements, no talking), the presence of the observer itself has minimal or no effect on measured OBP. Although unattended automated OBP has the advantage of avoiding several sources of error, it requires additional resources within a routine office visit (office space and time) limiting its app in all health care settings. Therefore, in case out-of-office BP monitoring is not available, attended automated OBP should be considered the most feasible option.
A major strength of this study is the direct comparison of automated office, home, and ambulatory BP levels in a well-defined population within a short time frame. Moreover, BP was assessed with highly standardized BP monitoring protocols consistent with recommendations in the current guidelines. Also, assessment of home BP was based on readings exported by the device memory, thus avoiding potential issues related to inaccurate reporting of readings by patients. Finally, by app of a randomized balanced design and wash-out periods we minimized the risk of order-effect and carry-over bias.
Some limitations also need to be considered. Since the majority of the population was prescribed antihypertensive medication, the findings may not be generalizable to individuals (in primary care) who have not yet been prescribed antihypertensive medications, in whom BP variability is likely to be greater.39 Furthermore, the cross-sectional design of this study did not allow the performance of HBPM to be assessed based on the occurrence of clinical outcomes, which is considered an important aspect in determining the best BP measurement method.
In conclusion, the present study showed that office and app-assisted HBPM substantially overestimate ABPM. Overall, app-assisted HBPM showed fair-to-moderate diagnostic agreement with ABPM for the diagnosis of sustained, white-coat, and masked hypertension. The high sensitivity and negative predictive value for diagnosing sustained and masked hypertension suggest that app-assisted HBPM may be suitable for screening on these hypertension phenotypes.
Perspectives
The emergence of mobile health apps offers an important new strategy to more actively involve patients in their own hypertension management. Smartphone app-assisted HBPM is an important example of such a strategy. Teletransmission of BP readings self-measured by patients at home, especially when combined with education and counseling, appears to be able to improve adherence, the doctor-patient relationship, as well as BP control. However, the present study showed considerable (diagnostic) disagreement between app-assisted HBPM and the reference standard 24-hour ABPM, suggesting that app-assisted HBPM and ABPM have a complementary rather than a competitive role in the evaluation of patients with hypertension. When app-assisted HBPM is considered, the results of this study also suggest that it is important to do so in an objective manner to avoid misreporting by the patient. Whether guiding antihypertensive therapy based on app-assisted HBPM also results in different effects on morbidity and mortality compared with ABPM-guided treatment remains to be studied.
ARTICLE INFORMATION
Acknowledgments
We gratefully acknowledge the contribution of the patients and the study teams from the 3 participating study sites; C.A.M. Joosten, I.P. Klaassen, S. Soldan (University Medical Center Utrecht, Utrecht), A. van de Vendel, J. van den Brink (Ziekenhuis Gelderse Vallei, Ede), M. Krah, and P. Verhoeven (Rijnstate ziekenhuis, Arnhem). We also thank O. van Dijk (Medicine Men BV, Utrecht) for providing the HBPM devices.
Sources of Funding
None.
Disclosures
None.
Supplemental Material
File S1
Table S1–S3
Figures S1–S6
Supplementary Material
Nonstandard Abbreviations and Acronyms
- ABPM
- ambulatory blood pressure measurement
- AMUSE-BP
- Ambulant Versus Unattended and Attended Office Versus Self-Home Blood Pressure Measurement
- App
- application
- BP
- blood pressure
- DBP
- diastolic blood pressure
- HBPM
- home blood pressure monitoring
- OBP
- office blood pressure
- SBP
- systolic blood pressure
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/HYPERTENSIONAHA.122.19685.
For Sources of Funding and Disclosures, see page 2381.
References
- 1.Whelton PK, Carey RM, Aronow WS, Casey DEJ, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical P. J Am Coll Cardiol. 2018;71:e127–e248. doi: 10.1161/HYP.0000000000000066 [DOI] [PubMed] [Google Scholar]
- 2.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, et al. ; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339 [DOI] [PubMed] [Google Scholar]
- 3.Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, Myers MG, Ogedegbe G, Schwartz JE, Townsend RR, et al. Measurement of blood pressure in humans: a scientific statement from the american heart association. Hypertension. 2019;73:e35–e66. doi: 10.1161/HYP.0000000000000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mancia G, Zanchetti A. White-coat hypertension: misnomers, misconceptions and misunderstandings. What should we do next? J Hypertens. 1996;14:1049–1052. doi: 10.1097/00004872-199609000-00001 [DOI] [PubMed] [Google Scholar]
- 5.Bobrie G, Clerson P, Ménard J, Postel-Vinay N, Chatellier G, Plouin PF. Masked hypertension: a systematic review. J Hypertens. 2008;26:1715–1725. doi: 10.1097/HJH.0b013e3282fbcedf [DOI] [PubMed] [Google Scholar]
- 6.Roush GC, Fagard RH, Salles GF, Pierdomenico SD, Reboldi G, Verdecchia P, Eguchi K, Kario K, Hoshide S, Polonia J, et al. Prognostic impact from clinic, daytime, and night-time systolic blood pressure in nine cohorts of 13,844 patients with hypertension. J Hypertens. 2014;32:2332–2340; discussion 2340. doi: 10.1097/HJH.0000000000000355 [DOI] [PubMed] [Google Scholar]
- 7.Bliziotis IA, Destounis A, Stergiou GS. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30:1289–1299. doi: 10.1097/HJH.0b013e3283531eaf [DOI] [PubMed] [Google Scholar]
- 8.Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, Harris KC, Nakhla M, Cloutier L, Gelfer M, et al. ; Hypertension Canada. Hypertension Canada’s 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. 2018;34:506–525. doi: 10.1016/j.cjca.2018.02.022 [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence (NICE). Hypertension in Adults: Diagnosis and Management. 2019. [PubMed] [Google Scholar]
- 10.Krist AH, Davidson KW, Mangione CM, Cabana M, Caughey AB, Davis EM, Donahue KE, Doubeni CA, Kubik M, Li L, et al. Screening for hypertension in adults: US preventive services task force reaffirmation recommendation statement. JAMA. 2021;325:1650–1656. doi: 10.1001/jama.2021.4987 [DOI] [PubMed] [Google Scholar]
- 11.Stergiou GS, Palatini P, Parati G, O’Brien E, Januszewicz A, Lurbe E, Persu A, Mancia G, Kreutz R; European Society of Hypertension Council and the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39:1293–1302. doi: 10.1097/HJH.0000000000002843 [DOI] [PubMed] [Google Scholar]
- 12.McManus RJ, Mant J, Haque MS, Bray EP, Bryan S, Greenfield SM, Jones MI, Jowett S, Little P, Penaloza C, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312:799–808. doi: 10.1001/jama.2014.10057 [DOI] [PubMed] [Google Scholar]
- 13.Nordmann A, Frach B, Walker T, Martina B, Battegay E. Reliability of patients measuring blood pressure at home: prospective observational study. BMJ. 1999;319:1172. doi: 10.1136/bmj.319.7218.1172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nordmann A, Frach B, Walker T, Martina B, Battegay E. Comparison of self-reported home blood pressure measurements with automatically stored values and ambulatory blood pressure. Blood Press. 2000;9:200–205. doi: 10.1080/080370500439083 [DOI] [PubMed] [Google Scholar]
- 15.Santo K, Redfern J. The Potential of mhealth applications in improving resistant hypertension self-assessment, treatment and control. Curr Hypertens Rep. 2019;21:81. doi: 10.1007/s11906-019-0986-z [DOI] [PubMed] [Google Scholar]
- 16.Kollias A, Ntineri A, Kyriakoulis KG, Stambolliu E, Lagou S, Boubouchairopoulou N, Stergiou GS. Validation of the professional device for blood pressure measurement Microlife WatchBP Office in adults and children according to the American National standards institute/association for the advancement of medical instrumentation/international organizat. Blood Press Monit. 2018;23:112–114. doi: 10.1097/MBP.0000000000000307 [DOI] [PubMed] [Google Scholar]
- 17.Cornu C, Kassai B, Fisch R, Chiron C, Alberti C, Guerrini R, Rosati A, Pons G, Tiddens H, Chabaud S, et al. ; CRESim & Epi-CRESim Project Groups. Experimental designs for small randomised clinical trials: an algorithm for choice. Orphanet J Rare Dis. 2013;8:48. doi: 10.1186/1750-1172-8-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng HM, Sung SH, Shih YT, Chuang SY, Yu WC, Chen CH. Measurement accuracy of a stand-alone oscillometric central blood pressure monitor: a validation report for Microlife WatchBP Office Central. Am J Hypertens. 2013;26:42–50. doi: 10.1093/ajh/hps021 [DOI] [PubMed] [Google Scholar]
- 19.Bos MJ, Buis S. Thirty-minute office blood pressure monitoring in primary care. Ann Fam Med. 2017;15:120–123. doi: 10.1370/afm.2041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stergiou GS, Giovas PP, Neofytou MS, Adamopoulos DN. Validation of the Microlife BPA100 Plus device for self-home blood pressure measurement according to the international protocol. Blood Press Monit. 2006;11:157–160. doi: 10.1097/01.mbp.0000209071.84965.bf [DOI] [PubMed] [Google Scholar]
- 21.MedicineMen. EmmaHBPM [Internet]. [cited 2022 Apr 26]. https://medicinemen.eu/consument/producten/emmahbpm/
- 22.Wilton A, De Greef A, Shennan A. Rapid assessment of blood pressure in the obstetric day unit using Microlife MaM technology. Hypertens Pregnancy. 2007;26:31–37. doi: 10.1080/10641950601146558 [DOI] [PubMed] [Google Scholar]
- 23.Ragazzo F, Saladini F, Palatini P. Validation of the Microlife WatchBP O3 device for clinic, home, and ambulatory blood pressure measurement, according to the International Protocol. Blood Press Monit. 2010;15:59–62. doi: 10.1097/MBP.0b013e32833531ca [DOI] [PubMed] [Google Scholar]
- 24.Park JS, Rhee MY, Namgung J, Lee SY, Cho DK, Choi TY, Kim SY, Kim JY, Park SM, Choi JH, et al. Comparison of optimal diagnostic thresholds of hypertension with home blood pressure monitoring and 24-hour ambulatory blood pressure monitoring. Am J Hypertens. 2017;30:1170–1176. doi: 10.1093/ajh/hpx115 [DOI] [PubMed] [Google Scholar]
- 25.Snijders TAB, Bosker RJ. Multilevel analysis: An introduction to basic and advanced multilevel modeling. Sage Publications; 2011. [Google Scholar]
- 26.Blood Pressure Lowering Treatment Trialists’ Collaboration. Age-stratified and blood-pressure-stratified effects of blood-pressure-lowering pharmacotherapy for the prevention of cardiovascular disease and death: an individual participant-level data meta-analysis. Lancet (London, England). 2021;398:1053–1064. doi: 10.1016/S0140-6736(21)01921-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22:276–282. doi: 10.11613/BM.2012.031 [PMC free article] [PubMed] [Google Scholar]
- 28.Verberk WJ, Kroon AA, Lenders JW, Kessels AG, van Montfrans GA, Smit AJ, van der Kuy PH, Nelemans PJ, Rennenberg RJ, Grobbee DE, et al. ; Home Versus Office Measurement, Reduction of Unnecessary Treatment Study Investigators. Self-measurement of blood pressure at home reduces the need for antihypertensive drugs: a randomized, controlled trial. Hypertension. 2007;50:1019–1025. doi: 10.1161/HYPERTENSIONAHA.107.094193 [DOI] [PubMed] [Google Scholar]
- 29.Muxfeldt ES, Barros GS, Viegas BB, Carlos FO, Salles GF. Is home blood pressure monitoring useful in the management of patients with resistant hypertension? Am J Hypertens. 2015;28:190–199. doi: 10.1093/ajh/hpu145 [DOI] [PubMed] [Google Scholar]
- 30.Di Monaco S, Rabbia F, Covella M, Fulcheri C, Berra E, Pappaccogli M, Perlo E, Bertello C, Veglio F. Evaluation of a short home blood pressure measurement in an outpatient population of hypertensives. Clin Exp Hypertens. 2016;38:673–679. doi: 10.1080/10641963.2016.1200600 [DOI] [PubMed] [Google Scholar]
- 31.Almeida AE, Stein R, Gus M, Nascimento JA, Arévalo JR, Fuchs FD, Ribeiro JP. Improved diagnostic accuracy of a 3-day protocol of home blood pressure monitoring for the diagnosis of arterial hypertension. Blood Press Monit. 2013;18:119–126. doi: 10.1097/MBP.0b013e32835ebb18 [DOI] [PubMed] [Google Scholar]
- 32.Viera AJ, Yano Y, Lin FC, Simel DL, Yun J, Dave G, Von Holle A, Viera LA, Shimbo D, Hardy ST, et al. Does this adult patient have hypertension?: The rational clinical examination systematic review. JAMA. 2021;326:339–347. doi: 10.1001/jama.2021.4533 [DOI] [PubMed] [Google Scholar]
- 33.Hodgkinson J, Mant J, Martin U, Guo B, Hobbs FD, Deeks JJ, Heneghan C, Roberts N, McManus RJ. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ. 2011;342:d3621. doi: 10.1136/bmj.d3621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guirguis-Blake JM, Evans CV, Webber EM, Coppola EL, Perdue LA, Weyrich MS. Screening for hypertension in adults: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2021;325:1657–1669. doi: 10.1001/jama.2020.21669 [DOI] [PubMed] [Google Scholar]
- 35.Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens. 2012;30:449–456. doi: 10.1097/HJH.0b013e32834e4aed [DOI] [PubMed] [Google Scholar]
- 36.Satoh M, Asayama K, Kikuya M, Inoue R, Metoki H, Hosaka M, Tsubota-Utsugi M, Obara T, Ishiguro A, Murakami K, et al. Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: the ohasama study. Hypertension. 2016;67:48–55. doi: 10.1161/HYPERTENSIONAHA.115.06461 [DOI] [PubMed] [Google Scholar]
- 37.Kollias A, Stambolliu E, Kyriakoulis KG, Gravvani A, Stergiou GS. Unattended versus attended automated office blood pressure: systematic review and meta-analysis of studies using the same methodology for both methods. J Clin Hypertens (Greenwich). 2019;21:148–155. doi: 10.1111/jch.13462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnson KC, Whelton PK, Cushman WC, Cutler JA, Evans GW, Snyder JK, Ambrosius WT, Beddhu S, Cheung AK, Fine LJ, et al. ; SPRINT Research Group. Blood pressure measurement in SPRINT (Systolic Blood Pressure Intervention Trial). Hypertension. 2018;71:848–857. doi: 10.1161/HYPERTENSIONAHA.117.10479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eguchi K, Imaizumi Y, Kaihara T, Hoshide S, Kario K. Comparison of valsartan and amlodipine on ambulatory blood pressure variability in hypertensive patients. Clin Exp Hypertens. 2016;38:721–724. doi: 10.1080/10641963.2016.1200609 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.