Abstract
Background:
Trajectories of affect vary across development, with normative increases in positive affect (PA) occurring during childhood and declines in positive affect appearing across adolescence. Little is known, however, about predictors of the trajectories of affect across adolescence. The present study examined associations between changes in adolescent affect across adolescence and maternal history of depression and child sex.
Methods:
Participants were 240 adolescents and their mothers; 185 mothers had a history of depression (i.e., high risk) and 55 mothers did not (i.e., low risk). Youth were assessed annually from 6th grade (meanage = 11.86 years, SD = 0.57, 54.2% female, 82% White) through 12th grade. Latent growth models tested the relation of maternal depression history and adolescent sex with trajectories of adolescent affect.
Results:
High-risk adolescents exhibited lower levels of positive affect as compared to low-risk youth (coefficient = −2.74, p = .012, 95% CI [−4.88, −0.59]. Girls experienced earlier increases in negative affect (NA) as compared to boys, with more positive linear (coefficient = 2.071, p = .002, 95% CI [0.774, 3.368]) and quadratic (coefficient = −0.292, p = .025, 95% CI [−0.548, −0.036]) slopes.
Limitations:
Use of self-report measures and limited generalizability.
Conclusion:
Maternal depression significantly predicted decreases in offspring positive affect and distinct trajectories of negative affect in girls and boys. Interventions aimed at reducing risk in adolescent offspring of depressed parents may benefit from targeting positive affect and supporting girls in early adolescence.
Keywords: Adolescent depression, maternal depression, positive affect, negative affect, sex
Introduction
Substantial research has identified positive (PA) and negative (NA) affect as central correlates and predictors of depression. Diminished PA specifically characterizes depression and elevated NA is associated with both depression and anxiety (Clark & Watson, 1991; Joiner & Lonigan, 2000). Longitudinal studies have shown that such atypical affect in childhood predicts increased risk for depression in adolescence and adulthood (Caspi et al.,1996; van Os et al.,1997). In adolescence, during which rates of depression increase and sex differences in depression prevalence emerge (e.g., Dalsgaard et al., 2020; Hankin et al., 1998; Kessler et al., 2001; Thapar et al., 2012), lower PA and elevated NA are associated with greater risk for subsequent depression (Lindahl et al., 2013). Given the importance of PA and NA in relation to depression, the purpose of the present study was to examine how these constructs change across development and whether certain risk factors are associated with such change.
Affect Trajectories
Over the course of childhood, PA increases and NA declines (Olino et al., 2011), whereas in adolescence, these trends are largely reversed (Griffith et al., 2021; Larson et al., 2002; Moneta et al., 2001; Weinstein et al., 2007), such that PA declines and NA increases. A longitudinal study of working- and middle-class European American children in 5th through 8th grade at baseline (10 to 14 years old) found that scores on measures of daily emotional states, using a bipolar index (e.g., unhappy to happy) became less positive and more negative until 10th grade (Larson et al., 2002). Such scales are difficult to interpret, however, as they treat NA and PA as opposite ends of the same affective continuum rather than as orthogonal constructs. Another longitudinal study followed students in Grades 6, 8, 10, and 12 (ages 12 to 18) for 4 years, and found that PA declined quadratically across adolescence, such that participant reports of “feeling good” declined across adolescence with steeper decreases in early adolescence (Moneta et al., 2001). Similarly, a one-year study of 8th and 10th graders using Ecological Momentary Assessment (EMA) found that PA declined, and NA remained relatively stable from grades 8 through 11 (Weinstein et al., 2007). Finally, another one-year longitudinal study reported mean-level declines in PA but periodic increases and decreases in NA for youth aged 9 to 17 (Griffith et al., 2021).
These results provide consistent evidence of declining trajectories for PA but differing trajectories of NA across adolescence. PA tends to decline across adolescence and shows steeper decreases in early relative to late adolescence. Conversely, NA does not show a consistent pattern of change in adolescence, perhaps indicating greater individual variability in levels of NA throughout this developmental period.
Some of the variability in trajectories of NA may be attributable to characteristics of self-report measures. Twenge and Nolen-Hoeksema (2002) found that self-report measures of depressive symptoms often show declines after the first wave in longitudinal studies, but such declines may not reflect changes in the construct itself. Such artifacts might bias estimates of longitudinal trajectories of depression-related variables (see also Ge et al., 2001; Shrout et al., 2018; Long et al., 2020). Therefore, in the current study, we controlled for this initial decline.
Predictors of Affect
Several variables are broadly associated with affect contemporaneously and prospectively.
Among Swedish adolescents, PA was associated with life satisfaction (r = .43, p < .001), psychological well-being (r = .4, p < .001), environmental mastery (r = .48, p < .001), self-acceptance (r = .4, p < .001), personal growth (r = .32, p < .001), and purpose in life (r = .21, p < .01), whereas NA exhibited similar inverse associations with many of these constructs (Garcia et al., 2013). Sleep-deprived adolescents and adults exhibited diminished PA for 9 of 12 PA items compared to rested individuals, but not elevated NA (Talbot et al., 2010). Importantly, affect is also closely related to environmental experiences. For instance, Fox et al., 2010 noted that among adolescent females, negative life events were positively associated with NA (r = .47, p < .001) and not significantly related to PA. Additionally, researchers found that PA was associated with family expressiveness of positive emotions (.49, p < .01), maternal warmth (.47, p < .01), and negatively associated with family expressiveness of negative emotions (−.2, p < .05) and maternal psychological control (−.3, p < .01) (Luebbe et al., 2014). In contrast, NA was negatively associated with maternal warmth (−.49, p < .01) and positively associated with family expressiveness of negative emotions (.56, p < .01) and maternal psychological control (.41, p < .01).
Sex & Gender.
Two factors related to trajectories of PA and NA across adolescence are adolescent sex and gender. Understanding the independent roles of sex assigned at birth and gender is vitally important to depression research, yet few studies clearly differentiate these constructs (including our own). Consequently, we sought to describe findings from studies based on current understandings of sex and gender. Gender differences in rates of depression and reports of depressive symptoms emerge in early adolescence and persist across adolescence (Salk et al., 2017) such that girls exhibit more instances of depression than boys. These differences in depression may result from several factors, including sex differences in hormonal and physiological changes associated with puberty, or from cognitive vulnerabilities and familial and social relationships (Hyde et al., 2008; Rapee et al., 2019).
Sex differences in PA and NA also are apparent in adolescence, although findings vary across studies. Moneta et al. (2001) found that girls reported lower levels of “feeling good” relative to boys during adolescence. Conversely, Larson et al. (2002) reported that girls showed higher average affect than boys across adolescence, although both girls and boys reported decreases in positive emotional states over time.
Griffith et al. (2021) also identified distinct trajectories of change in PA and NA for girls versus boys. Whereas girls showed consistent declines in PA across adolescence, boys exhibited an initial increase followed by a decline in PA. Additionally, girls showed a curvilinear change in NA across adolescence (decreases, then increases, followed by decreases), whereas boys exhibited quadratic change (initial declines followed by increases) in NA (Griffin et al. (2021). Weinstein et al. (2007) also reported sex differences in trajectories, such that boys showed a greater decline in PA during adolescence than girls. Weinstein and colleagues also found decreases in NA over time for girls, but stable NA scores for boys. Thus, sex differences in the trajectories of PA and NA have been observed, although the results have not been consistent across studies. Variability in the measures of affect used and sample characteristics likely contribute to this heterogeneity.
Offspring of depressed parents.
Another important factor that may be related to trajectories of affect is maternal depression. Exposure to maternal depression in infancy and childhood is not only a known risk factor for depression in adolescence (e.g., Côté et al., 2018; Spence et al., 2002) but it also is associated with blunted PA and elevated NA in at-risk offspring (Davis et al., 2020; Goodman et al., 2011; Olino et al., 2011). A meta-analysis of maternal depression and outcomes in children (mean age = 7.13, SD = 5.08) revealed small but significant associations between maternal depression and lower PA and higher NA in their offspring (Goodman et al., 2011). Davis et al. (2020) showed that 12-month-old children who had been exposed to maternal depression exhibited higher NA at 26 months. Similarly, children exposed to maternal depression in infancy exhibited lower PA from infancy through age 9 (Olino et al., 2011). Importantly, maternal depression may be associated with child affective health both prospectively and concurrently. For instance, a 13-year longitudinal study found that maternal postnatal depression was only associated with depressive symptoms in adolescent offspring when mothers experienced later bouts of depression (Halligan et al., 2007). Thus, maternal history of depression may represent a risk factor for adolescent affective health because it also predicts future depression in mothers.
Researchers have posited that diminished positive emotionality is a source of vulnerability for depression (Durbin et al., 2005; Meehl, 1975; Olino et al., 2011). Deficits in PA in infancy and childhood may indicate vulnerability that persists into adolescence. Thus far, however, only cross-sectional studies have examined relations between maternal history of depression and affect in their adolescent offspring. In a sample of 8- to 17-year old’s, Dietz et al. (2008) found that children whose first- and second-degree relatives had a history of depression exhibited lower PA in interactions with their mothers than did children with no family history of depression.
Characterizing trajectories of affect and their predictors may guide early interventions for depression in several ways. First, knowledge about such trajectories could inform the timing of preventive interventions by identifying developmental periods in which youth are particularly at risk. For example, an inflection point for PA, in which trajectories shift from increasing to decreasing, may indicate a particularly salient time for intervention. Additionally, understanding predictors of these trajectories may improve identification of high-risk populations who could benefit most from timely intervention. Girls and boys may experience a shift in PA from increasing to decreasing at about the same time, but girls may experience a steeper decline as compared to boys. Finally, distinct trajectories as a function of different predictors may indicate which specific interventions are warranted. For instance, greater increases in NA across adolescence among offspring of mothers with a depression history but no differences in trajectories of PA may suggest that this population would benefit more from interventions that target negative emotionality. Characterizing these features of affect trajectories may enhance large-scale interventions for teens, but for individual clinicians and patients, tailoring treatment to the patient’s own affective experiences will remain an important component of treatment.
In the present study, we examined the longitudinal trajectories of PA and NA in youth from grade 6 to grade 12. First, we hypothesized that PA would decrease across adolescence (see Larson et al., 2002; Moneta et al., 2010; Weinstein et al., 2007). Second, we expected that youth with a maternal history of depression (high-risk) would show lower average PA and higher average NA than offspring of mothers with no depression history (low-risk) (Goodman et al., 2011; Dietz et al., 2008; Olino et al., 2011). We also examined potential differences in the shape and magnitude of growth of PA and NA across adolescence as a function of adolescent risk and gender. Last, we conducted two post-hoc, exploratory analyses; first, to examine whether prediction by adolescent risk was mediated by current maternal depressive symptoms, and second, to determine whether the number of depressive episodes mothers’ experienced predicted adolescent PA or NA.
Methods
Participants
Participants included 240 adolescents (mean age = 11.86 years, SD = 0.57) and their mothers who were evaluated annually beginning in the sixth grade. The adolescent sample was 82% White, 14.7% African American, and 3.3% Hispanic, Asian, or Native American. Participants were asked which sex they identified as and were given the option of boy or girl. 54.2% of participants identified as a girl. Mean socioeconomic status in the sample (Hollingshead, 1975) was 41.84 (SD = 13.25), which represents lower middle (e.g., retail sales, childcare workers) to middle class (e.g., teachers, nurses).
Procedure
Parents of children in grade 5 from public schools in the greater metropolitan area of a medium size city in the midsouth region of the United States were invited to participate in a study about parents and children. We sent parents a letter describing the study, along with a brief health history questionnaire inquiring about 24 medical conditions (e.g., diabetes, heart disease, depression) and 34 medications (e.g., Prozac, Elavil, Valium). Of the 1,495 mothers who indicated an interest in participating, 587 endorsed either a history of depressive symptoms, use of antidepressants, or no history of psychopathology. We conducted phone interviews with these mothers. Of the 587 families screened, we excluded 238 because they did not report having had sufficient symptoms to meet criteria for a depressive disorder (38%), they had other psychiatric disorders that did not also include a depressive disorder (19%), either the mother or the target child had a serious medical condition (14%), the family was no longer Interested (21%), the target child was not in 5th grade (6%), or the family had moved out of the area (2%). Using the Structured Clinical Interview for DSM diagnoses (SCID; Spitzer, Williams, Gibbon, & First, 1990), we conducted in-person interviews with the remaining 349 mothers. Based on the SCID, 149 families then were excluded because (a) the mother reported a history of either a psychiatric diagnosis that did not also include a mood disorder or had a serious and disabling medical condition (e.g., cancer, multiple sclerosis), or (b) the child had a serious or chronic medical illness or a pervasive developmental disorder. The final sample of 240 families consisted of 185 mothers who had experienced a depressive disorder during the child’s life (high risk) and 55 mothers who were life-time free of psychopathology (low risk).
Measures
Positive and Negative Affect.
Adolescents completed the child version of the Positive and Negative Affect Schedule (PANAS-C; Laurent et al. 1999; Watson, Clark, & Tellegen, 1988). The PANAS-C is a 27-item measure comprised of adjectives describing different moods. Adolescents rated how much they had experienced each affect over the past week. Each item was rated on a 5-point Likert scale from 1 (not at all) to 5 (very much) and previously displayed good internal consistency (αPA = .89, αNA = .92; Laurent et al., 1999). In the study sample, alphas ranged from .83 to .92 for PA and from .84 to .91 for NA across time points. Participants completed the PANAS-C in grades 6, 7, 8, 9, 11, and 12 (data collection was reduced in the 10th grade year due to a gap in funding).
Risk.
We assessed mothers’ history of depression using the Structured Clinical Interview for DSM diagnoses (Spitzer, Williams, Gibbon, & First, 1990). We used risk as a dichotomous (high vs. low-risk), time-invariant predictor in each growth curve model. Children of mothers with a history of depression comprised the high-risk group, and children of mothers with no history of depression were in the low-risk group.
Current Maternal Depression.
We assessed mothers’ current depression using the Beck Depression Inventory (CITATION). DESCRIPTION
Data Analytic Plan
We conducted analyses using the lavaan package in R for Structural Equation Modeling (Rosseel, 2012; R Core Team, 2021). We assessed missing data using Little’s MCAR test. We used full information maximum likelihood (FIML) estimation, a method that allows utilization of partial data under the assumption that missingness is random. We first fit unconditional growth curve models, then identified the best fitting unconditional model using multiple fit indices, and finally incorporated predictors of latent factors.
Affect Growth Models.
Following procedures outlined by Cole et al. (in press) to examine trajectories of growth in continuous variables, we conducted a series of latent growth curve analyses, testing the latent intercept, linear trend, and quadratic trend of PA and NA (taken separately). This analytic approach allowed us to isolate features of affect trajectories and evaluate how they related to other variables. To account for previous reports of an initial decline in self-reported scores as outlined by Twenge & Nolen-Hoeksema (2002), Shrout et al., (2018), and Long et al., (2020), we used two different strategies to account for this decline. One involved an orthogonal latent change score approach; the other involved dropping the initial wave of data. We centered all latent variables at Time 1. We defined good fit as root mean square error of approximation (RMSEA) <.06, comparative fit index (CFI) >.95, and standardized root mean square residual (SRMR) <.08, whereas we defined “acceptable fit” as RMSEA <.08 and CFI >.90 (Hu & Bentler, 1999).
Predicting Affect Growth.
After identifying growth models with adequate fit for both positive and negative affect, we introduced risk and gender as time-invariant predictors of the latent growth factors. This approach allowed us to assess associations of risk and gender with affect trajectories concurrently. For risk, children of mothers with a history of depression comprised the high-risk group, and children of mothers with no history of depression were in the low-risk group. We allowed risk and gender to covary.
Post Hoc Analyses.
After obtaining results for these models, we added maternal BDI scores at Time 1 as a predictor of the latent intercept of adolescent PA and NA and retained adolescent sex and risk as a predictor of the latent intercept and used adolescent risk to predict current maternal BDI scores. We also conducted analyses replacing the dichotomous maternal HOD with mothers’ depressive episodes during their lifetime or their child’s lifetime and predicted adolescent PA and NA trajectories as in earlier conditional models.
Results
Descriptive Statistics
Descriptive statistics are presented in the supplementary materials. High-risk adolescents exhibited significantly lower PA in grades 6 (40.49 vs. 43.26, p = .019) and 7 (33.60 vs. 36.81, p = .03), and elevated NA in grade 6 (21.77 vs. 19.58, p = .018). Girls reported similar PA as boys across timepoints but exhibited significantly higher NA in grades 9 (18.26 vs. 16.71, p = .005) and 11 (20.41 vs. 16.61, p < .001). Data were missing at each time point from 14% to 24%. Patterns of missing data suggested that data were missing completely at random through examining Little’s MCAR test (X2237 = 260.27, p = 0.14).
Unconditional Univariate Growth Models for PA and NA
We tested five models for both PA and NA. The first three were conventional growth models: (1) intercept only, (2) intercept and linear trend, and (3) intercept, linear, and quadratic trend. Only the quadratic model for NA provided a moderately good fit across indices (see Table 1), whereas the quadratic model for PA did not achieve good fit across indices. Next, using the quadratic model for NA and PA, we tested two other models, designed not only to test intercept, linear, and quadratic trends but also to control for the wave 1 to wave 2 drop described by Twenge and Nolen-Hoeksema (2002). Model 4 accounted for this effect by incorporating a fourth latent variable representing the change from wave 1 to wave 2. In contrast, model 5 dropped wave 1 from the analysis. Both models fit well for PA and NA; however, Model 4 generated several out-of-range parameter estimates. Consequently, we focused on Model 5 for both PA and NA.
Table 1 -.
Correlations among sex, risk, NA, and PA in grades 6, 7, 8, 9, 11, and 12
| Negative Affect | Positive Affect | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||
| Variable | Mean (S.D.) | Sex | Risk | Grade 6 | Grade 7 | Grade 8 | Grade 9 | Grade 11 | Grade 12 | Grade 6 | Grade 7 | Grade 8 | Grade 9 | Grade 11 | Grade 12 |
|
| |||||||||||||||
| Sex | 0.54 (0.50) | 1 | |||||||||||||
| Risk | 0.77 (0.42) | 0.06 | 1 | ||||||||||||
| NA – Grade 6 | 21.27 (6.5) | 0.01 | 0.14* | 1 | |||||||||||
| NA – Grade 7 | 18.24 (5.85) | −0.04 | 0.05 | 0.39** | 1 | ||||||||||
| NA – Grade 8 | 17.70 (5.45) | 0.02 | 0.02 | 0.31** | 0.54** | 1 | |||||||||
| NA – Grade 9 | 18.26 (6.02) | 0.23** | 0.14 | 0.25** | 0.4** | 0.41** | 1 | ||||||||
| NA – Grade 11 | 18.75 (6.93) | 0.27** | 0.16* | 0.13 | 0.35** | 0.38** | 0.56** | 1 | |||||||
| NA – Grade 12 | 21.16 (8.13) | 0.12 | 0.18* | 0.15* | 0.37** | 0.43** | 0.43** | 0.5** | 1 | ||||||
| PA – Grade 6 | 41.12 (7.19) | −0.04 | 0.16* | −0.33** | −0.08 | −0.04 | −0.19* | −0.02 | −0.04 | 1 | |||||
| PA – Grade 7 | 34.35 (8.57) | 0.12 | 0.16* | −0.03 | 0.09 | 0.02 | 0.06 | 0 | −0.03 | 0.42** | 1 | ||||
| PA – Grade 8 | 34.46 (9.54) | 0.13 | −0.07 | −0.04 | 0.02 | −0.04 | −0.03 | −0.04 | 0.02 | 0.44** | 0.55** | 1 | |||
| PA – Grade 9 | 32.26 (8.98) | 0.06 | −0.07 | −0.08 | −0.08 | −0.06 | −0.02 | 0.03 | −0.09 | 0.37** | 0.47** | 0.59** | 1 | ||
| PA – Grade 11 | 32.62 (9.35) | −0.03 | −0.05 | −0.02 | −0.01 | −0.08 | −0.01 | −0.16* | −0.03 | 0.21** | 0.4** | 0.43** | 0.47** | 1 | |
| PA – Grade 12 | 33.62 (8.93) | −0.07 | −0.06 | −0.01 | −0.17* | −0.18* | −0.21** | −0.08 | −0.19** | 0.24** | 0.24** | 0.33** | 0.43** | 0.5** | 1 |
p < .05.
p<.01.
The model for PA exhibited a significant latent intercept (intercept = 34.62, p < .001, 95% CI [33.484, 35.749]), latent slope (slope = −1.404, p = .002, 95% CI [−2.301, −.0507]), and latent quadratic trend (latent quadratic = 0.242, p = .006, 95% CI [0.070, 0.414]).
The NA model exhibited a significant latent intercept (intercept = 18.27, p < .001, 95% CI [17.497, 19.043]) and quadratic trend (quadratic = .224, p = .001, 95% CI [0.096, 0.352]); the linear trend was not significant (intercept = −.645, p = .055, 95% CI [−1.302, 0.013]).
Conditional Models
Next, using the unconditional models for PA and NA that omitted wave 1, we tested conditional models that concurrently included adolescent risk and gender as time-invariant predictors of the latent intercept, slope, and quadratic trends. Both models fit the data well (see Table 2).
Table 2 -.
Positive Affect
| Sex | Risk | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Timepoint | Overall1 | Boys1 | Girls1 | p-value2 | Low1 | High1 | p-value2 |
|
| |||||||
| Negative Affect | |||||||
|
| |||||||
| Grade 6 | 21.27 (6.5) | 21.19 (6.2) | 21.34 (6.76) | 0.98 | 19.58 (5.59) | 21.77 (6.68) | 0.018 |
| Grade 7 | 18.24 (5.85) | 18.53 (6.08) | 18.01 (5.67) | 0.63 | 17.73 (5.57) | 18.40 (5.94) | 0.57 |
| Grade 8 | 17.70 (5.45) | 17.6 (5.82) | 17.79 (5.15) | 0.54 | 17.5 (5.39) | 17.77 (5.48) | 0.75 |
| Grade 9 | 18.26 (6.02) | 16.71 (4.95) | 19.45 (6.51) | 0.005 | 16.82 (5.00) | 18.72 (6.26) | 0.091 |
| Grade 11 | 18.75 (6.93) | 16.61 (5.89) | 20.41 (7.24) | <0.001 | 16.85 (4.03) | 19.42 (7.60) | 0.18 |
| Grade 12 | 21.16 (8.13) | 19.96 (7.00) | 21.97 (8.75) | 0.18 | 18.82 (5.55) | 22.04 (8.76) | 0.051 |
|
| |||||||
| Positive Affect | |||||||
|
| |||||||
| Grade 6 | 41.12 (7.19) | 41.46 (7.39) | 40.84 (7.02) | 0.61 | 43.26 (6.04) | 40.49 (7.39) | 0.019 |
| Grade 7 | 34.35 (8.57) | 33.21 (8.64) | 35.27 (8.43 | 0.081 | 36.81 (6.48) | 33.60 (8.99) | 0.03 |
| Grade 8 | 34.46 (9.54) | 33.13 (9.88) | 35.58 (9.14) | 0.1 | 35.65 (7.81) | 34.06 (10.04) | 0.37 |
| Grade 9 | 32.26 (8.98) | 31.67 (8.65) | 32.71 (9.23) | 0.54 | 33.34 (7.39) | 31.91 (9.42) | 0.28 |
| Grade 11 | 32.62 (9.35) | 32.94 (8.85) | 32.37 (9.76) | 0.65 | 33.33 (8.61) | 32.36 (9.62) | 0.45 |
| Grade 12 | 33.62 (8.93) | 34.35 (8.81) | 33.14 (9.02) | 0.3 | 34.54 (9.31) | 33.28 (8.79) | 0.34 |
Mean (SD)
Wilcoxon Rank Sum Test
Figure 1 shows trajectories of PA for adolescents at low and high risk for depression. The intercept of PA scores for the high-risk group was significantly lower compared to the low-risk group (coefficient = −2.739, p = .012). In both groups, PA initially declined and then increased. Figure 2 shows trajectories of PA for girls and boys. Both girls and boys experienced declines in PA in early adolescence with increases beginning in 11th grade for girls and in 9th grade for boys. No significant differences in either the intercept or slope emerged between girls and boys for PA.
Fig. 1.
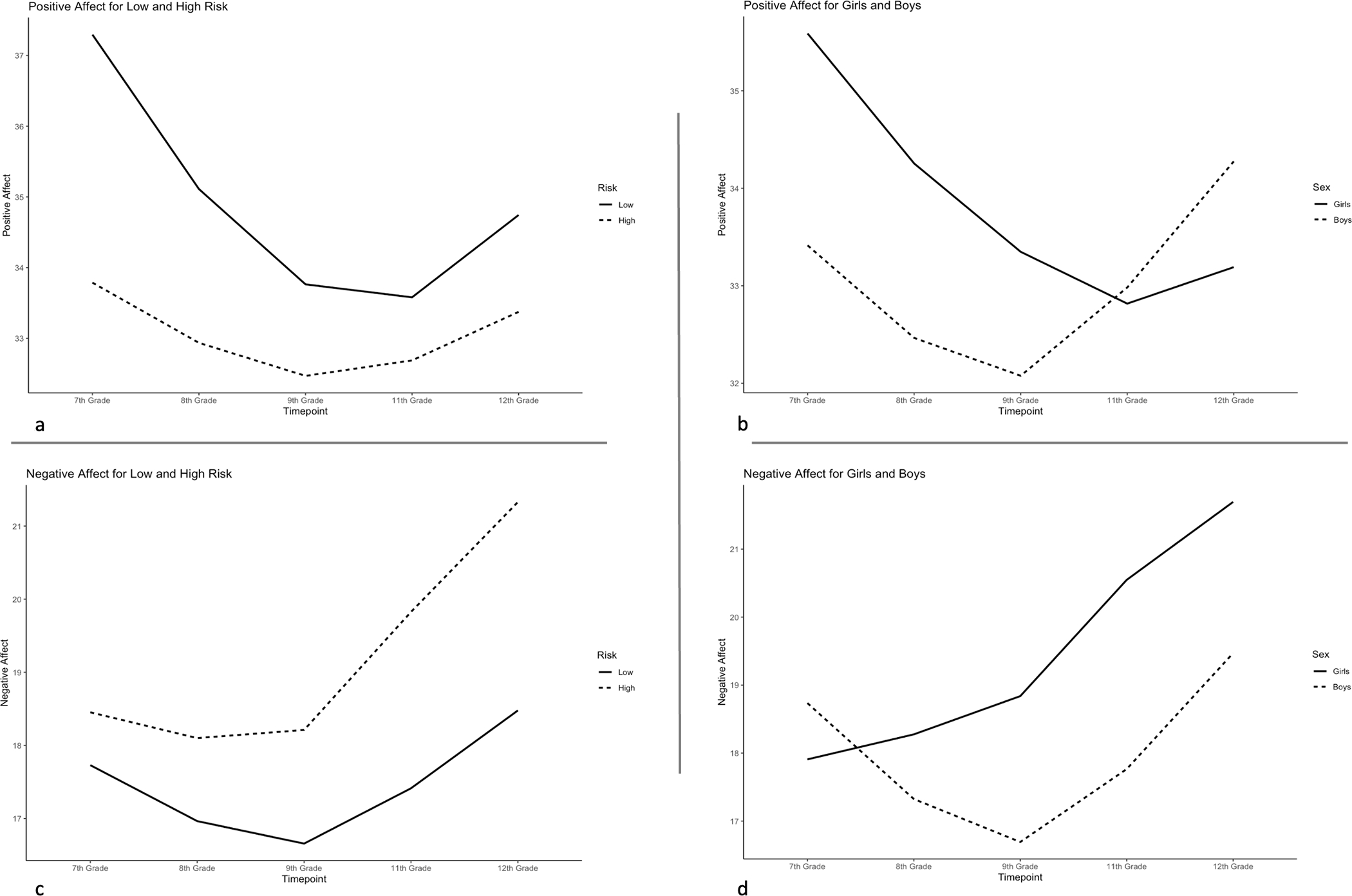
Conditional model trajectories.
Figure 3 shows the NA trajectories by risk group. Adolescents experienced slight declines in NA from grade 7 through grades 8 and 9 for high-risk and low-risk youth, respectively, followed by increases in NA through 12th grade. Figure 4 depicts the NA trajectories for girls and boy. Girls reported increases in NA from 7th through 12th grade, with significant differences in both linear (coefficient = 2.071, p = .002, 95% CI [0.774, 3.368]) and quadratic (coefficient = −0.292, p = .025, 95% CI [−0.548, −0.036]) slopes compared to boys. Boys showed declines in NA from 7th through 9th grade followed by increases through 12th grade.
When we included maternal BDI scores at Time 1 as a predictor of PA, we found that the direct effect of adolescent risk on the intercept of adolescent PA became non-significant (estimate = −2.43, p = .091), and the association between current maternal depression and the intercept of adolescent PA was not significant (estimate = −.145, p = .06). The association between maternal history of depression and current maternal depression was significant, however, such that mothers with a history of depression showed BDI scores on average 7 points higher than mothers with no history of depression (estimate = 7.11, p < .001). When we replaced dichotomous maternal HOD with mothers’ depressive episodes, we found the number of depressive episodes over the mother’s lifetime was associated with elevated NA (estimate = .481, p = .041). In other words, for every additional depressive episode mothers ever experienced, their offspring showed an increase of .481 in their average NA score.
Discussion
Three main findings emerged from the current study. First, we characterized trajectories of change for PA and NA across adolescence. Second, maternal history of depression explained variability in the intercept but not longitudinal trends of PA, and post hoc analyses found that number of lifetime maternal depressive episodes was associated with NA. Third, we found differences in linear and quadratic trends of NA but not PA as a function of adolescent sex.
First, we observed slight declines in PA from 7th to 9th grade, followed by minimal increases in PA through 12th grade. Similarly, NA exhibited small decreases from 7th to 9th grade and larger increases through 12th grade. Our omission of PA and NA data from grade 6 also allowed us to avoid modeling the artifactual initial decline in self-report measures identified by Twenge and Nolen-Hoeksema, 2002. These findings align with other studies that reported declines in PA in early adolescence (Griffith et al., 2021; Larson et al., 2002; Moneta et al., 2001; Weinstein et al., 2007). There still was considerable heterogeneity in the overall trajectories of PA across adolescence, however. The trajectory of PA found here aligns with findings reported in earlier studies (e.g., Larson et al., 2002; Moneta et al., 2001) that used composite measures of PA and NA on a single bipolar scale, whereas we evaluated these constructs as orthogonal dimensions. Although the trajectories looked similar, comparisons of these findings should be made with caution because of our differing conceptualizations of affect.
Weinstein and colleagues identified modest declines in PA from 8th to 11th grade and relative stability in NA. Their use of ecological momentary assessments over a week likely captured different aspects of affective change compared to the measure used here; thus, some of the variability may be attributable to the differences in assessment methodology. Differences across studies may also reflect variability in the construct assessed. Our study included intervals of one year between assessments and 2-week retrospective questions about affect, and consequently may capture more stable, trait-like affect constructs than studies with shorter inter-assessment intervals and momentary assessment of affect. Studies using methods like ecological momentary assessment to evaluate affect multiple times daily over a week, for instance, likely tap into state affect. Future research employing state-trait models may best clarify which construct is assessed and better understand how these distinct affect constructs relate to adolescent depression. Our method was most like that of Griffith and colleagues (2021), who showed linear decreases in PA across adolescence. Differences between our PA trajectories and those reported by Griffith et al. may be due, in part, to differences in the timing and number of assessments, and in part from variability in the measurement of affect across study samples. Our account of NA differs from that reported by Weinstein and colleagues (2007), who found relative stability in NA, and by Griffith et al. (2021), who demonstrated curvilinear change in NA.
Second, the current study expanded upon previous research by assessing the trajectories of PA and NA as a function of risk (i.e., maternal history of depression). High-risk adolescents showed diminished PA across adolescence, which aligns with longitudinal studies of younger children (Olino et al., 2011) and cross-sectional studies of adolescent offspring of mothers with a history of depression (Dietz et al., 2008). We demonstrated persistent deficits in PA across adolescence for offspring of mothers with a history of depression. Future studies should explore the trajectories of affect in conjunction with biological and environmental factors related to maternal depression to identify additional factors that account for individual differences in these trajectories. Maternal depression is associated with blunted responses to happy faces among emotionally healthy children (Morgan et al., 2019), reduced reward-related ventral striatum activation in depressed and never-depressed daughters (Sharp et al., 2014), attenuated response to social reward (Olino et al., 2015), and reduced putamen volume in children with and without depression (Pagliaccio et al., 2020). Understanding specific factors related to deficits in PA may provide insight into etiological mechanisms and viable treatment targets.
Post-hoc analyses also examined potential mediation of these effects by current maternal depression, and whether the number of depressive episodes experienced relate to child affect. Although we did not identity a significant mediation of the relation between maternal HOD and child average PA, investigating maternal HOD and current depression in larger samples may be warranted. The post-hoc analysis examining number of maternal depressive episodes found that the number of depressive episodes experienced during the mother’s lifetime, not the child’s, predicted higher NA, but not diminished PA. These results may reflect the contribution of genetics in the intergenerational transmission of depression or may occur because mothers whose depression began earlier in life experienced the most episodes, perhaps indicating greater severity than for mothers whose episodes primarily occurred during their child’s lifetime.
Third, we identified differences in trajectories of NA as a function of adolescent sex. Compared to boys, girls experienced earlier increases in NA, such that NA increased for girls beginning in 7th grade, whereas for boys it declined from 7th through 9th grade before increasing. These results partially mirror those of Griffith and colleagues (2021) who found that girls exhibited increases in NA around age 12, although we did not observe a decline in NA among girls after age 15. Additionally, these results suggest a quadratic trajectory of NA in boys across adolescence, with decreases in early adolescence followed by increases starting in 9th grade. There are several reasons the earlier increase in NA may occur. Girls typically begin puberty two years earlier than boys, and with earlier physical changes to their bodies, girl may experience earlier self-surveillance and body shame than boys do (Hyde & Mezulis, 2020). Additionally, peer sexual harassment is more frequent for girls than boys and may emerge earlier in adolescence due to the earlier start of puberty. Indeed, negative life events in adolescence may affect girls more strongly than boys, as such events account for greater variance in depressive symptoms for girls than boys (Spence et al., 2002). Although multiple studies have identified gender and sex as predictors of adolescent affect, future research should examine control variables and potential moderators to further account for the variability of observed results.
Strengths, Limitations, and Future Directions
Strengths of the current study include its multi-year, longitudinal design, and its focus on affect in low- and high-risk adolescents. Nevertheless, limitations in the current study suggest avenues for future research. First, our sample was 82% White, which limits the generalizability of our findings to more diverse racial and ethnic groups. Experiences of discrimination are common in the U.S.; a recent study by English et al. (2020) using ecological momentary assessment found that African American adolescents experienced an average of 5.21 instances of racial discrimination each day. Perceived racial or ethnic discrimination among adolescents is associated with increased depressive symptoms (r = .26), diminished positive well-being (r = −.14) and lower self-esteem (r = −.17) according to a recent meta-analytic review (Benner et al., 2018). Adolescent offspring of mothers with a history of depression who experience discrimination regularly may be particularly vulnerable to depression and may benefit from early intervention.
Second, missing data ranged from 14% to 24% across timepoints. This level of missingness can be adequately addressed when data are missing at random, which appeared to be the case in the current study. Although missingness was moderate, our data analytic approach reduced the risk of bias despite this limitation.
Third, we examined a relatively limited set of factors that may predict trajectories of adolescent affect. As noted by Kujawa and colleagues (2020), many RDoC-related factors likely interact to influence the developmental trajectory of affect. Greater granularity in the assessment of risk is important. For offspring of mothers with histories of depression specifically, comorbid psychopathology, timing of first onset of depression, and frequency of recurrence of depressive episodes also may be related to differences in trajectories over time. Using integrated data from multiple samples may address such questions from a dimensional perspective and improve the consistency of findings regarding predictors of the trajectories of adolescent affect.
Fourth, although our results largely align with prior studies that used observational measures of adolescent affect, our exclusive use of self-report measures is a limitation. If adolescent self-reported affect is an indicator of vulnerability to depression, then understanding how self-reported affect relates to affect observed during tasks and interactions with parents/ caregivers may be valuable. For instance, Olino and colleagues (2011) examined child affective displays in response to developmentally appropriate tasks intended to elicit affect. Dietz and colleagues (2008) examined affect using observed affect during mother-child problem-solving interaction tasks in which they discussed two issues that caused conflict in their relationship. These measures revealed specific situations in which offspring of mothers with a history of depression exhibited lower levels of PA. Use of similar behavioral measures in addition to self-reported affect may help identify intervention targets to ameliorate lower levels of PA in at-risk youth.
Clinical Implications
This study contributes to the literature showing a relation between maternal depression and alterations in positive valence systems in offspring. Importantly, not all high-risk children develop depression; maternal depression may predict greater risk of adolescent depression in offspring only with other vulnerabilities such as blunted or average reward responses (Kujawa et al., 2019). Effective coping may be protective, as at-risk offspring with better coping show higher positive mood and lower depressive symptoms (Jaser et al., 2011), and adaptive responses to peer stress in offspring of depressed mothers are related to reduced risk of depression (Monti et al., 2017).
Several promising interventions target positive valence systems. Behavioral activation (BA) therapy aims to increase engagement in reward activities (Curry & Meyer, 2016). Recent meta-analyses have reported positive findings for BA but also highlight study heterogeneity and recommend conducting additional large-sample trials to evaluate the generalizability of the findings (Martin & Oliver, 2019; Tindall et al., 2017). Positive Affect Treatment (PAT) is a neuroscience-based intervention that targets PA in adult populations (Craske et al., 2019). Positive affect treatment produced greater improvements in PA and reductions in NA compared to negative affect treatment at post-test and at a 6-month follow-up in adults. Adapting PAT for adolescents would provide another potentially valuable intervention in addition to BA, both of which should be studied in at-risk youth.
Implementing interventions that target family interactions also may be important considering our findings that current maternal depression mediates the association between maternal history of depression and diminished adolescent PA. Mothers’ aggressive responses to adolescents’ PA correlate with a larger volume of orbitofrontal cortex, dorsal anterior cingulate cortex, and in boys, larger amygdala volume (Whittle et al., 2009). Additionally, maternal dampening of adolescents’ positive affective behaviors correlates with greater depressive symptoms and emotion dysregulation (Yap et al., 2008). Brooding and dampening also mediate the relation between anxious attachment and increases in depressive symptoms among adolescents (Verhees et al., 2021). These studies highlight the potential utility of family-based interventions, which have been found to prevent elevations in adolescents’ depressive symptoms for up to 2-years (Compas et al., 2015).
In summary, the current study provided further evidence of lower levels of PA in adolescent offspring of mothers with a history of depression. Additionally, we found earlier increases in NA among girls as compared to boys. Understanding trajectories of affect across adolescence may inform the timing of interventions targeting positive and negative valence systems. Additionally, identifying consistent predictors of affect in future prospective studies that measure multiple contextual factors may improve the efficacy and specificity of interventions. Therapies that target adolescents’ reward systems and interpersonal relationships (e.g., between mothers and offspring) may enhance treatment outcomes for this population.
Table 3 -.
Unconditional Model Fit
| Fit Indices | Intercept | Linear | Quadratic | Twenge | Quadratic without Time 1 |
|---|---|---|---|---|---|
|
| |||||
| Positive Affect | |||||
| comparative fit index (CFI) | 0.18 | 0.45 | 0.91 | 0.98 | 0.98 |
| standardized root mean square residual (SRMR) | 0.33 | 0.18 | 0.07 | 0.04 | 0.04 |
| root mean square error of approximation (RMSEA) | 0.23 | 0.21 | 0.1 | 0.04 | 0.06 |
| Akaike’s information criterion (AIC) | 8448.18 | 8367.2 | 8233.29 | 8212.22 | 6636.51 |
| Bayesian information criterion (BIC) | 8476.03 | 8405.49 | 8285.5 | 8271.39 | 6684.71 |
| Chi-square | 268.8 | 181.82 | 39.9 | 14.84 | 11.08 |
| degrees of freedom (df) | 19 | 16 | 12 | 10 | 6 |
| p-value | 0 | 0 | 0 | 0.14 | 0.09 |
|
| |||||
| Negative Affect | |||||
| comparative fit index (CFI) | 0.61 | 0.69 | 0.96 | 0.99 | 0.99 |
| standardized root mean square residual (SRMR) | 0.15 | 0.12 | 0.05 | 0.04 | 0.04 |
| root mean square error of approximation (RMSEA) | 0.15 | 0.15 | 0.06 | 0.03 | 0.04 |
| Akaike’s information criterion (AIC) | 7622.84 | 7603.8 | 7536.6 | 7528.02 | 5980.58 |
| Bayesian information criterion (BIC) | 7650.69 | 7642.09 | 7588.81 | 7587.19 | 6028.77 |
| Chi-square | 124.35 | 99.31 | 24.11 | 11.53 | 7.8 |
| degrees of freedom (df) | 19 | 16 | 12 | 10 | 6 |
| p-value | 0 | 0 | 0.02 | 0.32 | 0.25 |
Table 4 -.
Conditional Model Fit
| Fit Indices | Positive Affect | Negative Affect |
|---|---|---|
|
| ||
| comparative fit index (CFI) | 0.99 | 1 |
| standardized root mean square residual (SRMR) | 0.03 | 0.04 |
| root mean square error of approximation (RMSEA) | 0.03 | 0.01 |
| Akaike’s information criterion (AIC) | 7256.8 | 6587.76 |
| Bayesian information criterion (BIC) | 7343.82 | 6674.77 |
| Chi-square | 12.36 | 10.39 |
| degrees of freedom (df) | 10 | 10 |
| p-value | 0.26 | 0.41 |
Table 5 -.
Conditional Model Results
| Positive Affect (PA) |
||||||||||
| Estimate | Intercept Standard Error | P-value | Estimate | Linear Slope Standard Error | P-value | Estimate | Quadratic Slope Standard Error | P-value | ||
| Predictor | Risk | −3.507 | 1.325 | 0.008 | 1.559 | 1.047 | 0.136 | −0.226 | 0.2 | 0.258 |
| Sex | 2.173 | 1.126 | 0.054 | −0.317 | 0.909 | 0.727 | −0.067 | 0.175 | 0.703 | |
|
| ||||||||||
|
Negative Affect (NA)
|
||||||||||
| Estimate | Intercept Standard Error | P-value | Estimate | Linear Slope Standard | P-value | Estimate | Quadratic Slope Standard Error | P-value | ||
| Predictor | Risk | 0.723 | 0.935 | 0.439 | 0.409 | 0.766 | 0.593 | 0.003 | 0.15 | 0.982 |
| Sex | −0.828 | 0.794 | 0.297 | 2.071 | 0.661 | 0.002 | −0.292 | 0.13 | 0.025 | |
Acknowledgements
This research was supported in part from the National Institute of Mental Health grants (R61MH119270; R33 MH115125) and training grant (T32 MH018921).
Footnotes
Conflict of interest
All authors declared no competing interests.
Ethics statement
This study was approved by the Vanderbilt University Institutional Review Board #5212
References
- Benner AD, Wang Y, Shen Y, Boyle AE, Polk R, & Cheng YP (2018). Racial/ethnic discrimination and well-being during adolescence: A meta-analytic review. American Psychologist, 73(7), 855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A (1996). Behavioral observations at age 3 years predict adult psychiatric disorders: Longitudinal evidence from a birth cohort. Archives of General Psychiatry, 53(11), 1033. 10.1001/archpsyc.1996.01830110071009 [DOI] [PubMed] [Google Scholar]
- Clark LA, & Watson D (1991). Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100(3), 316. [DOI] [PubMed] [Google Scholar]
- Cole DA, Ciesla JA, & Liu Q (In press). Latent variable modeling of continuous growth, Chapter IX. In Harris Cooper (Editor), Handbook of Research Methods in Psychology, 2nd Edition, American Psychological Association. [Google Scholar]
- Compas BE, Forehand R, Thigpen J, Hardcastle E, Garai E, McKee L, Keller G, Dunbar JP, Watson KH, Rakow A, Bettis AH, Reising M, Cole DA, & Sterba S (2015). Efficacy and moderators of a family cognitive behavioral preventive intervention for children of depressed parents. Journal of Consulting and Clinical Psychology, 83, 541–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Côté SM, Ahun MN, Herba CM, Brendgen M, Geoffroy M-C, Orri M, Liu X, Vitaro F, Melchior M, Boivin M, & Tremblay RE (2018). Why Is Maternal Depression Related to Adolescent Internalizing Problems? A 15-Year Population-Based Study. Journal of the American Academy of Child & Adolescent Psychiatry, 57(12), 916–924. 10.1016/j.jaac.2018.04.024 [DOI] [PubMed] [Google Scholar]
- Craske MG, Meuret AE, Ritz T, Treanor M, Dour H, & Rosenfield D (2019). Positive affect treatment for depression and anxiety: A randomized clinical trial for a core feature of anhedonia. Journal of Consulting and Clinical Psychology, 87(5), 457–471. 10.1037/ccp0000396 [DOI] [PubMed] [Google Scholar]
- Curry JF, & Meyer AE (2016). Can less yield more? Behavioral activation for adolescent depression. Clinical Psychology: Science and Practice, 23(1), 62–65. 10.1111/cpsp.12141 [DOI] [Google Scholar]
- Dalsgaard S, Thorsteinsson E, Trabjerg BB, Schullehner J, Plana-Ripoll O, Brikell I, Wimberley T, Thygesen M, Madsen KB, Timmerman A, Schendel D, McGrath JJ, Mortensen PB, & Pedersen CB (2020). Incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders in childhood and adolescence. JAMA Psychiatry, 77(2), 155. 10.1001/jamapsychiatry.2019.3523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JAG, Alto ME, Oshri A, Rogosch F, Cicchetti D, & Toth SL (2020). The effect of maternal depression on mental representations and child negative affect. Journal of Affective Disorders, 261, 9–20. 10.1016/j.jad.2019.09.073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz LJ, Birmaher B, Williamson DE, Silk JS, Dahl RE, Axelson DA, Ehmann M, & Ryan ND (2008). Mother-Child Interactions in Depressed Children and Children at High Risk and Low Risk for Future Depression. Journal of the American Academy of Child & Adolescent Psychiatry, 47(5), 574–582. 10.1097/CHI.0b013e3181676595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durbin CE, Klein DN, Hayden EP, Buckley ME, & Moerk KC (2005). Temperamental Emotionality in Preschoolers and Parental Mood Disorders. Journal of Abnormal Psychology, 114(1), 28–37. 10.1037/0021-843X.114.1.28 [DOI] [PubMed] [Google Scholar]
- English D, Lambert SF, Tynes BM, Bowleg L, Zea MC, & Howard LC (2020). Daily multidimensional racial discrimination among Black US American adolescents. Journal of Applied Developmental Psychology, 66, 101068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge X, Conger RD, & Elder GH (2001). Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Developmental Psychology, 37(3), 404–417. 10.1037/0012-1649.37.3.404 [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, & Heyward D (2011). Maternal Depression and Child Psychopathology: A Meta-Analytic Review. Clinical Child and Family Psychology Review, 14(1), 1–27. 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- Griffith JM, Clark HM, Haraden DA, Young JF, & Hankin BL (2021). Affective development from middle childhood to late adolescence: Trajectories of mean-level change in negative and positive affect. Journal of Youth and Adolescence. 10.1007/s10964-021-01425-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, & Angell KE (1998). Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology, 107(1), 128. [DOI] [PubMed] [Google Scholar]
- Hollingshead A Four Factor Index of Social Status. New Haven, CT: Yale University Department of Psychology; 1975. [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hyde JS, Mezulis AH, & Abramson LY (2008). The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychological Review, 115(2), 291–313. 10.1037/0033-295X.115.2.291 [DOI] [PubMed] [Google Scholar]
- Jaser SS, Champion JE, Dharamsi KR, Riesing MM, & Compas BE (2011). Coping and positive affect in adolescents of mothers with and without a history of depression. Journal of Child and Family Studies, 20(3), 353–360. 10.1007/s10826-010-9399-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE, & Lonigan CJ (2000). Tripartite model of depression and anxiety in youth psychiatric inpatients: Relations with diagnostic status and future symptoms. Journal of Clinical Child Psychology, 29(3), 372–382. 10.1207/S15374424JCCP2903_8 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch JR, Laska EM, Leaf PJ, … & Wang PS. (2001). The prevalence and correlates of untreated serious mental illness. Health Services Research, 36(6 Pt 1), 987. [PMC free article] [PubMed] [Google Scholar]
- Kujawa A, Hajcak G, & Klein DN (2019). Reduced reward responsiveness moderates the effect of maternal depression on depressive symptoms in offspring: Evidence across levels of analysis. Journal of Child Psychology and Psychiatry, 60(1), 82–90. 10.1111/jcpp.12944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kujawa A, Klein DN, Pegg S, & Weinberg A (2020). Developmental trajectories to reduced activation of positive valence systems: A review of biological and environmental contributions. Developmental Cognitive Neuroscience, 43, 100791. 10.1016/j.dcn.2020.100791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson RW, Moneta G, Richards MH, & Wilson S (2002). Continuity, stability, and change in daily emotional experience across adolescence. Child Development, 73(4), 1151–1165. 10.1111/1467-8624.00464 [DOI] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, Joiner TE Jr, Rudolph KD, Potter KI, Lambert S, … & Gathright T. (1999). A measure of positive and negative affect for children: Scale development and preliminary validation. Psychological Assessment, 11(3), 326. [Google Scholar]
- Lindahl M, & Archer T (2013). Depressive expression and anti-depressive protection in adolescence: Stress, positive affect, motivation, and self-efficacy. Psychology, 04(06), 495–505. 10.4236/psych.2013.46070 [DOI] [Google Scholar]
- Long EE, Haraden DA, Young JF, & Hankin BL (2020). Longitudinal patterning of depression repeatedly assessed across time among youth: Different trajectories in self-report questionnaires and diagnostic interviews. Psychological Assessment, 32(9), 872–882. 10.1037/pas0000915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin F, & Oliver T (2019). Behavioral activation for children and adolescents: A systematic review of progress and promise. European Child & Adolescent Psychiatry, 28(4), 427–441. 10.1007/s00787-018-1126-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meehl PE (1975). Hedonic capacity: Some conjectures. Bulletin of the Menninger Clinic, 39(4), 295–307. [PubMed] [Google Scholar]
- Moneta GB, Schneider B, & Csikszentmihalyi M (2001). A longitudinal study of the self-concept and experiential components of self-worth and affect across adolescence. Applied Developmental Science, 5(3), 125–142. 10.1207/S1532480XADS0503_2 [DOI] [Google Scholar]
- Monti JD, & Rudolph KD (2017). Maternal depression and trajectories of adolescent depression: The role of stress responses in youth risk and resilience. Development and Psychopathology, 29(4), 1413–1429. 10.1017/S0954579417000359 [DOI] [PubMed] [Google Scholar]
- Morgan JK, Silk JS, Woods BK, & Forbes EE (2019). Differential neural responding to affective stimuli in 6- to 8-year-old children at high familial risk for depression: Associations with behavioral reward seeking. Journal of Affective Disorders, 257, 445–453. 10.1016/j.jad.2019.06.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Lopez-Duran NL, Kovacs M, George CJ, Gentzler AL, & Shaw DS (2011). Developmental trajectories of positive and negative affect in children at high and low familial risk for depressive disorder: Familial depression risk and children’s affect development. Journal of Child Psychology and Psychiatry, 52(7), 792–799. 10.1111/j.1469-7610.2010.02331.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Silk JS, Osterritter C, & Forbes EE (2015). Social reward in youth at risk for depression: A preliminary investigation of subjective and neural differences. Journal of Child and Adolescent Psychopharmacology, 25(9), 711–721. 10.1089/cap.2014.0165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagliaccio D, Alqueza KL, Marsh R, & Auerbach RP (2020). Brain volume abnormalities in youth at high risk for depression: Adolescent Brain and Cognitive Development Study. Journal of the American Academy of Child & Adolescent Psychiatry, 59(10), 1178–1188. 10.1016/j.jaac.2019.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM, Oar EL, Johnco CJ, Forbes MK, Fardouly J, Magson NR, & Richardson CE (2019). Adolescent development and risk for the onset of social-emotional disorders: A review and conceptual model. Behaviour Research and Therapy, 123, 103501. 10.1016/j.brat.2019.103501 [DOI] [PubMed] [Google Scholar]
- R Core Team (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/ [Google Scholar]
- Rosseel Y (2012). lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software, 48(2). 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- Salk RH, Hyde JS, & Abramson LY (2017). Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychological Bulletin, 143(8), 783–822. 10.1037/bul0000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp C, Kim S, Herman L, Pane H, Reuter T, & Strathearn L (2014). Major depression in mothers predicts reduced ventral striatum activation in adolescent female offspring with and without depression. Journal of Abnormal Psychology, 123(2), 298–309. 10.1037/a0036191 [DOI] [PubMed] [Google Scholar]
- Shrout PE, Stadler G, Lane SP, McClure MJ, Jackson GL, Clavél FD, … & Bolger N. (2018). Initial elevation bias in subjective reports. Proceedings of the National Academy of Sciences, 115(1), E15–E23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence SH, Najman JM, Bor W, O’Callaghan MJ, & Williams GM (2002). Maternal anxiety and depression, poverty and marital relationship factors during early childhood as predictors of anxiety and depressive symptoms in adolescence. Journal of Child Psychology and Psychiatry, 43(4), 457–469. 10.1111/1469-7610.00037 [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, & First MB (1990). User’s guide for the structured clinical interview for DSM-III-R: SCID. American Psychiatric Association. [Google Scholar]
- Thapar A, Collishaw S, Pine DS, & Thapar AK (2012). Depression in adolescence. The Lancet, 379(9820), 1056–1067. 10.1016/S0140-6736(11)60871-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tindall L, Mikocka-Walus A, McMillan D, Wright B, Hewitt C, & Gascoyne S (2017). Is behavioural activation effective in the treatment of depression in young people? A systematic review and meta-analysis. Psychology and Psychotherapy: Theory, Research and Practice, 90(4), 770–796. 10.1111/papt.12121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tram JM, & Cole DA (2006). A multimethod examination of the stability of depressive symptoms in childhood and adolescence. Journal of Abnormal Psychology, 115(4), 674–686. 10.1037/0021-843X.115.4.674 [DOI] [PubMed] [Google Scholar]
- Twenge JM, & Nolen-Hoeksema S (2002). Age, gender, race, socioeconomic status, and birth cohort difference on the children’s depression inventory: A meta-analysis. Journal of Abnormal Psychology, 111(4), 578–588. 10.1037/0021-843X.111.4.578 [DOI] [PubMed] [Google Scholar]
- van Os J (1997). Developmental Precursors of Affective Illness in a General Population Birth Cohort. Archives of General Psychiatry, 54(7), 625. 10.1001/archpsyc.1997.01830190049005 [DOI] [PubMed] [Google Scholar]
- Verhees MWFT, Finet C, Vandesande S, Bastin M, Bijttebier P, Bodner N, Van Aswegen T, Van de Walle M, & Bosmans G (2021). Attachment and the development of depressive symptoms in adolescence: The role of regulating positive and negative affect. Journal of Youth and Adolescence, 50(8), 1649–1662. 10.1007/s10964-021-01426-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Weinstein SM, Mermelstein RJ, Hankin BL, Hedeker D, & Flay BR (2007). Longitudinal patterns of daily affect and global mood during adolescence. Journal of Research on Adolescence, 17(3), 587–600. 10.1111/j.1532-7795.2007.00536.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittle S, Yap MBH, Yücel M, Sheeber L, Simmons JG, Pantelis C, & Allen NB (2009). Maternal responses to adolescent positive affect are associated with adolescents’ reward neuroanatomy. Social Cognitive and Affective Neuroscience, 4(3), 247–256. 10.1093/scan/nsp012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yap MBH, Allen NB, & Ladouceur CD (2008). Maternal Socialization of Positive Affect: The Impact of Invalidation on Adolescent Emotion Regulation and Depressive Symptomatology. Child Development, 79(5), 1415–1431. 10.1111/j.1467-8624.2008.01196.x [DOI] [PubMed] [Google Scholar]


