Abstract
Objectives
To investigate the perceived barriers and enablers experienced by physiotherapists whilst delivering community and outpatient services during the COVID-19 pandemic.
Methods
Qualitative study undertaken at a University-affiliated hospital in Melbourne, Australia. Physiotherapists working in the outpatient setting participated in a semi-structured interview. Interviews were analysed using Framework Analysis, with themes mapped to the Theoretical Domains Framework (TDF).
Results
From 19 interviews, we identified major themes and mapped these to the TDF domains: 1. The pandemic rapidly closed the knowledge-practice gap; 2. Adaptation of existing skills and integration of new skills were required; 3. Supportive senior leadership helped the transition; 4. Capabilities and confidence improved with time; 5. Environmental factors were crucial to success or failure of telehealth; 6. Access to and delivery of care improved for some; 7. Identification of appropriate patients and future hybrid models of care; 8. Changes in work practices, role certainty and identity; 9. Development of educational resources consolidated knowledge; 10. Socialisation of telehealth and optimism for the future. Within each domain, key barriers and enablers were also identified.
Conclusions
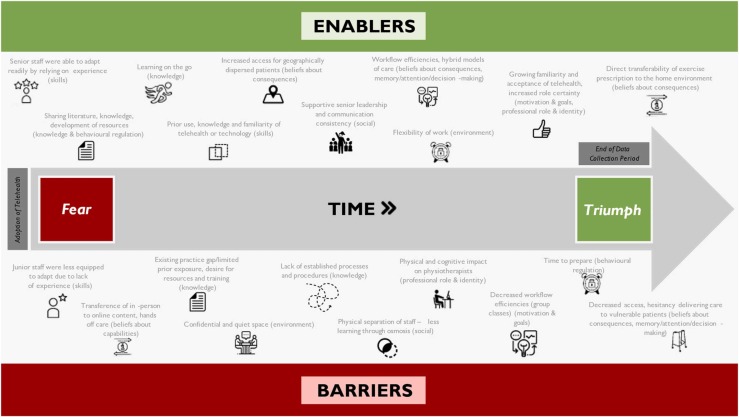
The findings of this study suggest that the delivery of community and outpatient physiotherapy via telehealth during the COVID-19 pandemic was an initial challenge. Growing knowledge, confidence and ability to problem solve barriers enabled physiotherapists to move along the continuum of ‘fear’ to ‘triumph’ as the pandemic progressed. These results can be used by clinicians, managers, and academics to guide future workforce planning, hospital environmental design, and service delivery.
Clinical message
-
•
Physiotherapists described telehealth as a challenge. Growing experience, confidence and problem-solving ability allowed therapists to provide effective and efficient care to patients over time.
-
•
The results can be used by clinicians, managers, and academics to guide resource development, optimise clinical efficiencies and reduce inequities for vulnerable patients in future.
Keywords: Covid-19, Telehealth, Physiotherapy, Barriers, Enablers, Theoretical Domains Framework
Introduction
The emergence of the coronavirus (COVID-19) pandemic necessitated rapid change in community and outpatient services delivery to maintain infection control and social distancing requirements. Pre-existing digital health technology, including telehealth, became the prominent mode of physiotherapy outpatient service delivery, to reduce or replace in-person contact [1].
Telehealth, which in this service incorporated clinical consultation via video or phone, has provided an alternative mode of delivering care for many years, yet prior to the pandemic, uptake into clinical practice has anecdotally been variable. Telehealth involves using telecommunication technologies to connect up points of care, and facilitate the sharing of health information [2]. The efficacy of telehealth has previously been established in musculoskeletal [3], [4], [5], [6], [7], and cardiorespiratory [8], [9] physiotherapy care. Until the COVID-19 pandemic, there had been minimal research into the logistics, safety, and security of telehealth practices [11], [12]. Additionally, health system barriers such as reimbursement and resistance to change [10] have been reported to limit the widespread uptake of telehealth [13].
The rapid implementation of telehealth within physiotherapy services at the start of the COVID-19 pandemic posed significant challenges for clinicians [11] due to limited prior clinical experience or training [14]. This disruption has provided a unique opportunity to use an implementation science approach to understand the telehealth research-practice gap. While some studies exist investigating perceptions of clinicians and patients regarding their telehealth experience during the pandemic [11], [13], [14], few studies have used an in-depth qualitative approach to investigate the perceptions in a diverse cohort of physiotherapists regarding the rapid adoption of telehealth for musculoskeletal and cardiorespiratory conditions. Therefore, the aim of this phenomenological study was to investigate the barriers and enablers to using telehealth by physiotherapists for outpatient service delivery during the COVID-19 pandemic.
Methods
The Consolidated Reporting of Qualitative Research checklist [15] was used to report this study. This was a single-site study undertaken within a Physiotherapy Department at a major academic hospital in Melbourne, Australia between November 2020 and May 2021. The hospital provides specialist inpatient, outpatient and community physiotherapy services for both adults and children. Pre-pandemic, physiotherapy services were predominantly delivered individually via in-person appointments, and also via group classes (e.g., post joint replacement surgery, pulmonary rehabilitation and hydrotherapy). During the start of the pandemic, these services transitioned to telehealth, using a state-based platform (Health Direct), a predominantly video-based platform. Patients received their care via telehealth (including video-platform or via telephone) and/or in-person, depending on the clinical decision making of physiotherapists, and local COVID-19 restrictions. Telephone may have been used if participants were unable to undertake video-based consultations due to equipment or technology literacy liitations. Ethical approval was obtained prior to commencing data collection (HREC/64629/Austin-2020).
Study design
A qualitative study design underpinned by the Framework Analysis method was used to explore the perceived barriers and enablers to using telehealth. An interview guide was developed, which was informed by the Theoretical Domains Framework (TDF), a review of the prior literature and discussion amongst the research team to structure a range of interview questions and prompts. The questions were piloted in a small group of clinicians [16]. The TDF is a rigorous implementation science framework, within which the researchers were particularly interested in the barriers and enablers to delivering care via telehealth. This framework was chosen as provides a comprehensive approach to qualitative data analysis to ensure that key domains are not missed.
Participants
Physiotherapists were purposively sampled from a total of 165 clinicians (85 were employed full time), ranging from grade 1–4 (least to most experience). Eligible physiotherapists were those who had worked in the community and outpatient setting in the musculoskeletal and cardiorespiratory fields throughout the COVID-19 period. Prior to this qualitative study being undertaken, a separate survey-based study was undertaken with clinicians within the Department. When clinicians consented to taking part in the survey, they were also given the option to consent to be contacted by a researcher about taking part in in an interview. If they provided consent to be contacted, a researcher made contact by email or phone to clarify their interest in taking part, undertake informed consent, and arrange a time for an interview. The researcher sent an electronic PICF directly to the participant.
Data collection
Data were collected by one researcher (KH) using a semi-structured interview guide (Supplement-1). Preliminary interview questions were piloted and then altered in response to feedback. Following feedback, two of the domains were merged with other domains based on the pilot feedback (i.e. emotion with memory attention and decision processes; optimism with motivation and goals). Interviews were completed by an experienced qualitative researcher who was unknown to most clinicians and held minimal bias due to working in a different hospital and field of physiotherapy (intensive care). Similarly, the researcher who conducted the analysis (AS) had knowledge of the health department and health landscape, but did not work in the same department of clinicians sampled. Interviews lasted 30–50 min, were conducted via Zoom©, audio-recorded, and professionally transcribed verbatim. Clinicians (participants) were given the option to undertake transcript checking, though no changes were requested.
Data analysis
A framework analysis approach using a combination of deductive and inductive processes were used to analyse interview data. Two independent, experienced qualitative researchers (KH/AS) undertook thorough review of each transcript, followed by coding of the transcript data into an Excel spreadsheet. Deductive processes were then used to map to the TDF framework, while then describing inductive themes within the TDF framework [17]. The researchers compared data between musculoskeletal and cardiorespiratory physiotherapists (Supplemental Table 1). After preliminary coding was conducted on a third of the transcripts in Excel, the researchers met to group the data and to elicit the major themes that subsequent data were mapped against until data saturation was reached. Fortnightly crosschecking of analyses was undertaken for rigor. Themes were then formally defined together by both researchers.
Results
Clinicians were predominantly female (89%), worked in the musculoskeletal setting (50%), and had a median (range) of 8 (1−29) years of clinical experience ( Table 1).
Table 1.
Characteristics of Clinicians.
| Gender (% female) | 89 |
| Years of Physiotherapy Experience (median [range]) | 8 [1–29] |
| Current Area of Work n (%) | |
| Musculoskeletal/Orthopaedic | 12 (50) |
| Sports and Exercise | 2 (8) |
| Neurology | 1 (4) |
| Cardiorespiratory | 8 (34) |
| Cancer, Palliative Care and Lymphoedema | 1 (4) |
| Postgraduate Qualifications n (%) | 7 (39) |
| Specific Prior Telehealth Training n (%) | 2 (11) |
| Motivational Interviewing Training n (%) | 10 (56) |
From 19 interviews, 10 major themes were mapped to the TDF domains, with barriers and enablers were identified. We observed the emergence of an overarching conceptual theme across all domains -over time clinicians moved from feelings of fear and hesitation, to triumph and acceptability with increased telehealth familiarity ( Fig. 1).
Fig. 1.
Barriers and Enablers to Telehealth Summary.
TDF domain: knowledge – the pandemic rapidly closed the knowledge-practice gap to adopt telehealth
Many clinicians described telehealth as an existing practice gap. They expressed a vague understanding of telehealth prior to the pandemic, but that it was not widely used, and many had limited prior exposure: “Even before the pandemic, telehealth to me was something talked about, but it wasn’t really something that was in place as such” (Participant [P] 01; Musculoskeletal [M]). Barriers to acquiring knowledge rapidly during the pandemic related to a lack of established processes and procedures to support knowledge translation: “There was just no time to set it up properly.the first month was pretty rocky.” (P14; Cardiorespiratory [C]) Another described: “We were very gung-ho very early on… we haven’t got policies in place.” (P06;M). Clinicians described a range of enablers that helped develop knowledge: using literature to support practice, sharing knowledge with peers, development of learning resources, and building confidence by teaching students. However, the key enabler clinicians consistently described was learning through doing: “We were figuring it out as we went” (P02;M) and “It was all just trial by fire”(P08;C).
Cardiorespiratory clinicians described enhanced prior knowledge of telehealth via research participation that was a key enabler: “We knew what we wanted to do; it was just working out the logistics”(P11;C). However, the knowledge-translation gap was also highlighted: “From the cardiac rehab perspective.there’s really strong evidence for the use of telehealth as an alternate model of care to provide access…but a lot of us haven't actually made the switch to that”(P18;C).
TDF domain: skills - adaptation of existing skills and integration of new skills were required to use telehealth
Clinicians described adapting their assessment, treatment, and communication to use telehealth: “It’s essentially a new skillset that you’ve got to integrate into your normal practice” (P10; M). For musculoskeletal clinicians, the removal of hands-on assessment was an initial barrier (irrespective of clinical experience): “Clinically I had to adjust heaps, because all of a sudden you can’t do strength tests the way you normally strength test” (P04;M).
Prior experience with telehealth was a key enabler for skill development. Cardiorespiratory clinicians (of increasing seniority) with previous telehealth experience were able to adapt more readily: “I think I did have the necessary skills to do telehealth, especially with the cardiac rehab programmes…you do a lot of health coaching one-on-one anyway.So, essentially, all you’re doing is changing it to remote education” (P06;C). Time and repeated practice were key enablers to integrate new skills for all clinicians. They described the evolution of their skill acquisition over time: “At the start, I was relying heavily on educating the patient and trying to help them, whereas I think towards the end we started looking at other ways we could bring in other mediums to help their care such as exercise programs and using online applications to facilitate a better outcome” (P02;M). Another key enabler was pre-existing familiarity with technology and digital skills: “It probably helps that I’m quite tech savvy…it wasn’t hard in terms of the technical aspect of adopting it” (P01;M).
TDF domain: social influences – supportive senior leadership helped the transition to telehealth
There were no barriers regarding social influences reported by clinicians. Instead, clinicians described supportive senior leadership as a key enabler in developing their knowledge, skills, and practice in telehealth: “They (leaders) were very supportive…they explored all the options on telehealth and sent around a YouTube video they made that showed us all the features…we also did a lot of co-treatments with junior staff” (P13;M). Clinicians spoke about consistency in communication from leaders: “From quite high up, the message was always quite consistent…” (P05; M) and how the optimism and positivity from leaders helped them transition to telehealth and provided reassurance: “They were really optimistic about how this could be really helpful…that was helpful in an unsettling time” (P07; M).
TDF domain: beliefs about capabilities – capabilities and confidence in telehealth improved with increased experience and exposure
Initially, the removal of usual clinical cues was viewed as a barrier that impacted clinicians’ capability to undertake therapy via telehealth: “Delivering therapy over telehealth is a lot more challenging than face-to-face, because you’ve removed so many cues” (P06;C). While some clinicians felt that the removal of hands-on care was a particular barrier to effective care, others adapted and felt this was less of an issue when placing a greater emphasis on exercise prescription: “Limitations certainly were that we couldn’t do any hands-on things.But it was okay in the outpatient setting because we tend to focus on exercise anyway” (P03;C). Numerous clinicians, regardless of specialty area, described barriers to effective care when having to rely on telephone consults only, if video consulting was not possible.
A key enabler was increased familiarity with technology and understanding how to adapt therapy to deliver effective and efficient care: “I think my sessions earlier on were of lower quality and lower efficacy than my sessions later” (P10; M). Comparatively, cardiorespiratory clinicians familiar with telehealth had already made this conceptual transition to tailor therapeutic interventions: “All you’re trying to achieve is behaviour change.you worry about the intensity being perfect to achieve physiological change and you worry about the assessment being perfect, but at the end of the day, you actually want them to come out of that program and adopt long-term lifestyle changes” (P11;C).
Another key enabler that increased confidence was the ability to deliver care to the patients in their home environment. This led to greater specificity and transferability of exercise prescription: “…You can actually do functional things that really mattered to the patient…it’s easier for them to remember, because they were doing the exercise in the environment that they would continue to do the home exercise in” (P03;C).
TDF domain: environmental context – environmental factors were crucial to success or failure of telehealth
The impact of the environmental set-up was discussed extensively by clinicians. The most common barriers related to clinicians accessing a quiet, private space: “It almost felt like being a call centre” (P05; M), and patients: “Patients would often be in their family home with people walking in and out”(P02; M); access to suitable equipment: “Initially we didn’t have really the right set up for it, in regards to headphones or split screens” (P18;C); and a stable internet connection for clinicians and patients: “Internet connection.you’d be dropping out of patient calls…that’s a major limitation”(P15;C). For some clinicians, working from home was also a barrier dependent upon their home environment: “I had two kids at home because we lost childcare. My partner was trying to do their job, and I’m on my video calls.it was a bit chaotic to be honest..” (P07;M). However, for the majority, working from home was an important enabler that created an environment conducive to successful delivery of telehealth, and was an important strategy to increase space at the hospital: “It helped that all of our staff did some work from home, so that we could then free up some space here” (P09;M). Clinician problem-solving and adaptation was a key enabler to overcome some of the environmental limitations such as equipment: “I just would usually bring my laptop to work and find any quiet space” (P01;M); and finding necessary solutions to maintain privacy: “There were no privacy issues.you’d do things like slide the chest of drawers in front of the door so they (children) are not going to walk in. You just adapt” (P07;M).
TDF domain: beliefs about consequences – telehealth improved the access to and delivery of care (for some)
Clinicians described tension delivering physiotherapy via telehealth to patients with challenging clinical, cultural and environmental presentations, for example, those with complex complaints, elderly, non-English speaking background (NESB) patients (even with professional interpreter use), and those with lower health literacy. Clinicians tended to identify these cohorts as the patients they would elect to treat in person: “. In terms of choosing to have them come in person…might be someone with a non-English speaking background.highly anxious or extreme pain or you just felt like I needed to see them in person from a safety point of view” (P03; C).
Conversely, a key enabler was that telehealth overcame issues related to in-person attendance at the health service. For example, geographical distance was no longer a barrier to deliver and receive care, with reduced travel and parking costs: “You can reach patients who perhaps could be isolated otherwise or have other socioeconomic barriers to receiving care by travelling” (P02;M). Other enablers included greater ease of skills transfer for the patient doing therapy in their home, a positive impact on workflow and increased efficiency of care delivery as the physiotherapist could multitask across electronic systems.
TDF domain: memory, attention and decision-making processes – identification of appropriate patients and adopting future hybrid models of care
Clinicians described decision-making challenges related to the identification of appropriate patients to receive care via telehealth. This was often based upon complexity of the presentation, subsequent care needs, and associated risk: “There’s definitely a proportion of patients that just you can’t effectively manage on telehealth. They’re probably the more complex patients” (P01; M). Whereas there was increased clinician confidence in decision-making related to those with less complexity: “I think for some of those straightforward patients we can really effectively manage them on telehealth” (P04;M). Clinicians also described the cognitive impacts of undertaking telehealth: “You get Zoom fatigue after a while…” (P04;M).
Clinicians highlighted hybrid (combination of in-person and telehealth) models of care as a key enabler to ongoing successful use of telehealth post-pandemic: “I really appreciate the limitations in telehealth now.sometimes it’s just they might need one session in clinic and then we can transition back to managing them on telehealth” (P03;C). Some cardiorespiratory clinicians reflected on their readiness to adopt new models of care: “I think for our service we’ve probably been advantaged by being involved in research. By being heavily involved in research specifically looking at alternative models of care we’ve always had that ‘let’s try something new’.” (P15;C).
TDF domain: professional role and identity – telehealth necessitated changes to work practices, yet provided role certainty and identity at a difficult time
Clinicians described changes to their workflow during the conversion to telehealth, which impacted their professional role and identity. Many clinicians described usually being active in their daily roles with varied work tasks. However, telehealth use had physical “Sitting all day at a computer is quite different. I’m used to getting up, walking, using my hands, using my body, so I definitely noticed ergonomic strains on my body” (P03;C). Clinicians also described feeling less job satisfaction in caring for patients solely via telehealth and missed the opportunities to build in-person rapport with patients: “It’s less fulfilling. As a therapist, if I was to purely be on my screen all day, I probably did feel a sense of less fulfilment in the role…There’s something in that therapeutic exchange that you can’t substitute with a screen” (P07;M).
In contrast, telehealth provided an essential element of role certainty, professional identity and hope, at a professionally and personally tumultuous time: “There was a lot of uncertainty in that early phase.over time it became clear that we could manage patients on telehealth and there was still a need. Then I think our jobs, our plan for how our jobs were going to look like was a bit more secure” (P01;M).
TDF domain: behavioural regulation – development of educational resources consolidated knowledge and supported continual improvement in telehealth skills
The speed of telehealth adoption and lack of preparation time was a key barrier, impacting behavioural regulation: “Time was a factor. No-one really saw this coming, so I think time was definitely a factor and we didn’t have time perhaps to prepare” (P02;M). Enablers that helped clinicians increase their confidence in use of telehealth was the development of resources throughout the initial waves of the pandemic. However, clinicians also expressed a desire for more training and resources to support decision making and to improve the quality of care delivered via telehealth: “I think if there’s a learning package, that would be really good troubleshooting if things go wrong with telehealth how to effectively do motivational interviewing” (P12;M).
TDF domain: motivation and goals – socialisation of telehealth and optimism for the future
Despite initial challenges, telehealth became increasingly acceptable to clinicians and reportedly patients over time: “If they continue to allow telehealth to be funded, I think as a community and consumer point of view, it’ll start to slowly ingrain into the culture and the norm” (P10;M). Clinicians highlighted the benefits to patients: “I think it will be really good to integrate with access to the service and reducing the burden of wait time and people having to actually to pay for parking and come to the hospital particularly for just getting results” (P16;C). Clinicians had a strong sense of optimism for the future of telehealth, as a well-accepted modality for care delivery: “I hope it’s here to stay. I think there’s a real place for it” (P17;M).
Discussion
In this qualitative study of community and outpatient physiotherapists, confidence in telehealth use grew over time, leading to a shift in perception from initial feelings of fear and hesitation, to triumph and acceptability. Ten major themes were mapped to the TDF. The TDF is a well-established rigorous framework that comprehensively considers all domains of implantation science. The TDF was used as the foundation for assisting to explain the data. This framework was particularly useful in ensuring that the researchers captured all possible facets of telehealth use, and made some challenges more visible, for example, the challenges around equipment and environment to support the use of telehealth that may have otherwise been missed or under appreciated.
Our comprehensive findings report similar barriers and enablers to the largest mixed methods study of physiotherapists and patients in Australia during 2020 [14]. The most novel aspects of our findings relate to future workforce planning, hospital environmental design, and service delivery considerations for vulnerable and traditionally disadvantaged cohorts. Future workforce planning should consider that telehealth is currently embedded into clinical practice and, consistent with other research, is considered to be feasible and acceptable by physiotherapists [13]. Data from the interviews supported the notion that senior clinicians felt that they were able to adapt readily during telehealth implementation as they drew upon their years of experience and prior knowledge. In contrast, data from the interviews supported the notion that junior clinicians typically felt unprepared to undertake assessment and deliver care via telehealth, particularly new graduates. Clinically, refinement of educational resources and enhancement of supervisory structures would support ongoing telehealth use. Further, education may be needed to realise the full potential of telehealth as a health behavioural modification tool, where the role of clinician evolves to support patient self-management, and to address common attitudes and beliefs that telehealth removes hands-on care and therefore limits the scope and applicability [18]. Consistent with previous research, the acceptability of telehealth improved over the course of the pandemic and clinicians described positive experiences [14].
Health services must consider telehealth use in future environmental design and to support sustained telehealth use over time. Environmental constraints related to securing a quiet, private and confidential space, accessing equipment such as computers, and stable internet connection, were found to be crucial to the success or failure telehealth care delivery [14]. While individual therapists problem-solved these issues, the health system needs to consider these issues in, for example, the build of new hospitals and environments [19].
Telehealth provided the potential for increased access to physiotherapy services for vulnerable and traditionally disadvantaged patients. However, the benefits of this were paradoxical when clinicians triaged patients who faced pre-existing challenges accessing care. In comparison with other recent research [13], [20], the application of telehealth could potentially reinforce access issues for vulnerable patients. For example, patients from NESB and older patients were commonly described as patients who would benefit from in person care due to limited internet access and/or uncertainty about comprehension of information provided virtually. Issues of health inequity have been highlighted by others regarding telehealth use during the pandemic [21], and may further reinforce lack of access. While younger, English speaking patients could more easily access hospital-based care via telehealth, NESB and older patients may not have these same options to access care so easily. Our data found evidence of patients having to ‘fit the system’ rather than the system adjusting to suit individual needs.
The strengths of this study include the diverse sample of physiotherapists caring for patients with musculoskeletal and cardiorespiratory conditions. The sample size is modest, however, we were able to reach data saturation and our cohort is broadly representative of a typical major metropolitan hospital physiotherapy department. Finally, interviewing consumers was outside of the scope of this work.
Our findings also have implications for future research, particularly how to approach research translation in a high-pressure clinical environment. The situation created by the COVID-19 pandemic created disruption that facilitated the rapid translation of research into practice, and our findings systematically describe the impacts of this on clinicians. Key lessons that are transferrable to other areas of research translation relate to the barriers to mitigate (e.g. ensuring adequate educational resources are developed early to support knowledge acquisition, provision of necessary equipment and addressing environmental issues early), and the enablers to leverage (e.g. ensuring supportive senior leadership, and utilising the problem-solving capacity of clinicians).
Conclusion
The delivery of physiotherapy via telehealth during the COVID-19 pandemic was an initial challenge. Growing knowledge, confidence and ability to problem solve barriers enabled physiotherapists to move from ‘fear’ to ‘triumph’ as the pandemic progressed. These results can be used by clinicians, managers, and academics to guide resource and professional development, optimise clinical efficiencies and reduce inequities for vulnerable patients in the future.
Acknowledgements
The authors would like to acknowledge the physiotherapist from Austin Health in Melbourne, Australia who gave up their time to participate in the semi-structured interviews.
Conflicts of Interest and Source of Funding
No specific funding was received to undertake this study. The authors have no conflicts of interest to declare.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.physio.2022.09.003.
Appendix A. Supplementary material
Supplementary material
.
References
- 1.Webster P. Virtual health care in the era of COVID-19. Lancet. 2020;395(10231):1180–1181. doi: 10.1016/S0140-6736(20)30818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Australian Digital Healthcare Agency: National Digital Healthcare Strategy. Available at: 〈https://conversation.digitalhealth.gov.au/sites/default/files/adha-strategy-doc-2ndaug_0_1.pdf〉. Accessed Apr 30, 2020.
- 3.Cottrell M.A., Hill A.J., O'Leary S.P., Raymer M.E., et al. Service provider perceptions of telerehabilitation as an additional service delivery option within an Australian neurosurgical and orthopaedic physiotherapy screening clinic: a qualitative study. Musculoskelet Sci Pract. 2017;32:7–16. doi: 10.1016/j.msksp.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Cottrell M.A., Russell T.G. Telehealth for musculoskeletal physiotherapy. Musculoskelet Sci Pract. 2020;48 doi: 10.1016/j.msksp.2020.102193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dario A.B., Moreti Cabral A., Almeida L., Ferreira M.L., et al. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J. 2017;17(9):1342–1351. doi: 10.1016/j.spinee.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Grona S.L., Bath B., Busch A., Rotter T., et al. Use of videoconferencing for physical therapy in people with musculoskeletal conditions: a systematic review. J Telemed Telecare. 2018;24(5):341–355. doi: 10.1177/1357633X17700781. [DOI] [PubMed] [Google Scholar]
- 7.Shukla H., Nair S.R., Thakker D. Role of telerehabilitation in patients following total knee arthroplasty: evidence from a systematic literature review and meta-analysis. J Telemed Telecare. 2017;23(2):339–346. doi: 10.1177/1357633X16628996. [DOI] [PubMed] [Google Scholar]
- 8.Chan C., Yamabayashi C., Syed N., Kirkham A., et al. Exercise telemonitoring and telerehabilitation compared with traditional cardiac and pulmonary rehabilitation: a systematic review and meta-analysis. Physiother Can. 2016;68(3):242–251. doi: 10.3138/ptc.2015-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rawstorn J.C., Gant N., Direito A., Beckmann C., et al. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016;102(15):1183–1192. doi: 10.1136/heartjnl-2015-308966. [DOI] [PubMed] [Google Scholar]
- 10.Lawford B.J., Delany C., Bennell K.L., Hinman R.S. "I was really sceptical.But it worked really well": a qualitative study of patient perceptions of telephone-delivered exercise therapy by physiotherapists for people with knee osteoarthritis. Osteoarthr Cartil. 2018;26(6):741–750. doi: 10.1016/j.joca.2018.02.909. [DOI] [PubMed] [Google Scholar]
- 11.Gilbert A.W., Booth G., Betts T., Goldberg A. A mixed-methods survey to explore issues with virtual consultations for musculoskeletal care during the COVID-19 pandemic. BMC Musculoskelet Disord. 2021;22(1) doi: 10.1186/s12891-021-04113-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilbert A.W., Davies L., Doyle J., Patel S., et al. Leadership reflections a year on from the rapid roll-out of virtual clinics due to COVID-19: A commentary. BMJ Lead. 2021 [Google Scholar]
- 13.Miller M.J., Pak S.S., Keller D.R., Barnes D.E. Evaluation of pragmatic telehealth physical therapy implementation during the COVID-19 pandemic. Phys Ther. 2021;101(1) doi: 10.1093/ptj/pzaa193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bennell K.L., Lawford B.J., Metcalf B., Mackenzie D., et al. Physiotherapists and patients report positive experiences overall with telehealth during the COVID-19 pandemic: a mixed-methods study. J Physiother. 2021;67(3):201–209. doi: 10.1016/j.jphys.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care: J Int Soc Qual Health Care / ISQua. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 16.Atkins L., Francis J., Islam R., O'Connor D., et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1) doi: 10.1186/s13012-017-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gale N.K., Heath G., Cameron E., Rashid S., et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13 doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malliaras P., Merolli M., Williams C.M., Caneiro J.P., et al. ‘It's not hands-on therapy, so it's very limited’: telehealth use and views among allied health clinicians during the coronavirus pandemic. Musculoskelet Sci Pract. 2021;52 doi: 10.1016/j.msksp.2021.102340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duane J.N., Blanch-Hartigan D., Sanders J.J., Caponigro E., et al. Environmental considerations for effective telehealth encounters: a narrative review and implications for best practice. Telemed J E Health. 2021:1–8. doi: 10.1089/tmj.2021.0074. [DOI] [PubMed] [Google Scholar]
- 20.James S., Ashley C., Williams A., Desborough J., et al. Experiences of Australian primary healthcare nurses in using telehealth during COVID-19: a qualitative study. BMJ Open. 2021;11(8) doi: 10.1136/bmjopen-2021-049095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chunara R., Zhao Y., Chen J., Lawrence K., et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J Am Med Inform Assoc. 2021;28(1):33–41. doi: 10.1093/jamia/ocaa217. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material