Abstract
Context:
Anterior cruciate ligament (ACL) reconstruction (ACLR) and postoperative rehabilitation continues to be a multidisciplinary focus in both research and clinical environments. Recent research on ACLR warrants a reexamination of clinicians’ current rehabilitation practices to optimize the strikingly variable clinical outcomes after ACLR and return to sport. The purpose of the article and updated guidelines is to use contemporary evidence to systematically revisit our practice guidelines and validate our clinical milestones with data from our university-based practice.
Evidence Acquisition:
Using the PubMed search engine, articles that reported on ACLR rehabilitation and protocols, guidelines, graft type, healing and strain, return to sport, psychological considerations, and secondary injury prevention published from 1979 to 2020 were identified using the search terms ACLR protocols, guidelines, ACLR rehabilitation, ACL graft, ACL open kinetic chain (OKC) exercise and closed kinetic chain (CKC) exercise, ACLR return to sport, ACLR psychological factors, and ACL injury prevention.
Study Design:
Clinical review.
Level of Evidence:
Level 5.
Results:
Clinical milestones after ACLR were validated using clinical data collected from 2013 to 2017 at a university-based practice. Variables including knee joint range of motion, effusion, Knee Outcome Survey–Activities of Daily Living Scale, and quadriceps strength index were tracked throughout rehabilitation and analyzed to help inform an updated ACLR rehabilitation guideline.
Conclusion:
Incorporating the latest research, combined with direct clinical data, provides a current, realistic, and clinically benchmarked strategy for ACLR rehabilitation. Commonly held clinical beliefs regarding rehabilitation after ACL injury must be challenged by the latest research to improve patient outcomes and decrease the risk of reinjury. Key updates to the practice guidelines include the use of frequent and accurate quadriceps strength testing, delayed return-to-sport timeline, immediate use of open kinetic chain exercise, criterion-based progressions for running, sprinting, plyometrics, agility, cutting/pivoting, return to competition, and the inclusion of a secondary prevention program after return to sport.
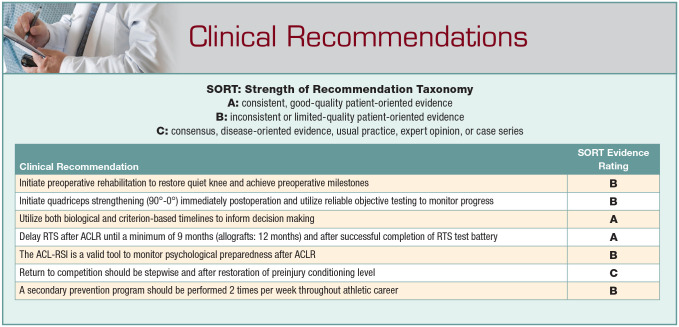
Strength of Recommendation Taxonomy (SORT):
B.
Keywords: ACL reconstruction, ACLR rehabilitation, return to sport, open kinetic chain versus closed kinetic chain exercise, quadriceps strength
Anterior cruciate ligament (ACL) injury is the most common athletic knee injury, and rehabilitation is the key to successful outcome after ACL reconstruction (ACLR), the usual treatment for athletes with ACL rupture. Research on ACL injury and reconstruction has increased exponentially since 2012 and has changed practice patterns. The advent of international and US ACL registries provided data that belied the rosy outcomes portrayed in the literature.7,8 Significant reinjury is common after ACLR; graft rupture and contralateral ACL rupture approaches 30% in athletes who return to level I activity.3,50 The striking likelihood of reinjury after ACL rupture requires rehabilitation specialists to reexamine their approaches and align them with the best available evidence.
ACL graft healing after surgery, among many proposed factors in reinjury, is an essential consideration as it pertains to rehabilitation progression and return to sport (RTS). Graft healing time frames were not the driving consideration in the RTS decision. Criterion-based guidelines allowed external measures of recovery to push the limits of the surgery. 1 Over the years, patients returned to sport sooner and sooner after ACLR. In light of recent studies, it appears delaying RTS to align with graft integration and maturation decreases reinjury risk. 26 Therefore, RTS is not recommended until 9 to 12 months after surgery, 23 once all physical impairments and performance deficits have been normalized. In addition, recent work has continued to challenge the notion that open kinetic chain exercise is harmful to the ACL graft.18,53,61
Our understanding of the ACL injury sequela continues to improve, and rehabilitation guidelines must adjust to mitigate negative impact where possible. The purpose of the article and updated guideline (see Appendix, available in the online version of this article) is to use contemporary evidence to systematically revisit our practice guidelines and validate our clinical milestones with data from our university-based practice.
Validating Clinical Milestones
Deidentified data collected at the University of Delaware Physical Therapy Clinic between 2013 and 2017 were used in the validation of our clinical milestones (research classified as exempt by the University of Delaware Institutional Review Board). Our sample included 75 young, active patients separated into 2 groups, primary ACLR with or without meniscectomy (ACLR) and primary ACLR with meniscal repair (ACLR + R). The variables of effusion, range of motion (ROM), Knee Outcome Survey–Activities of Daily Living Scale (KOS-ADLS), and quadriceps strength index (QI) were analyzed to determine the mean and median time points that milestones were achieved (Table 1). For analysis of quadriceps strength, each group was further subdivided by ACL graft selection, bone–patellar tendon–bone grafts (BPTB; n = 24) and hamstring (HS) and allografts (n = 51). On average, both groups achieved trace to zero effusion by week 13. The ACLR + R versus ACLR groups achieved full active extension by week 1 and 2, respectively. The ACLR + R versus ACLR groups achieved KOS-ADLS scores >80% by week 11 and 13, respectively. The ACLR + R BPTB group achieved QI >80% and >90% at weeks 16 to 20 and weeks 26 to 35, respectively, while the ACLR + R HS and allograft group, achieved QI >80% and >90% at week 12 and 13, respectively. The ACLR BPTB group, achieved QI >80% and >90% at weeks 12 to 14 and week 30, respectively. The ACLR + HS and allograft group, achieved QI >80% and >90% at week 9 and 15, respectively.
Table 1.
Validation of clinical milestones
| ACLR (n = 57) | ACLR + R (n = 18) | |||
|---|---|---|---|---|
| Effusion (trace) | Week 13 | Week 13 | ||
| Active knee extension | Week 2 | Week 1 | ||
| Passive knee extension | Week 1 | Week 2 | ||
| KOS-ADLS >80% | Week 13 | Week 11 | ||
| BPTB (n = 19) | Hamstring/Allograft (n = 38) | BPTB (n = 5) | Hamstring/Allograft (n = 13) | |
| QI >80% | Week 12-14 | Week 9 | Week 16-20 | Week 12 |
| QI >90% | Week 30 | Week 15 | Week 26-35 | Week 13 |
ACLR, anterior cruciate ligament reconstruction with or without meniscectomy; ACLR + R, anterior cruciate ligament reconstruction with meniscal repair; BPTB, bone–patellar tendon–bone graft; KOS-ADLS, Knee Outcome Survey–Activities of Daily Living Scale; QI, quadriceps strength index; Week = mean timeline of achieved milestone.
Despite the potential for variable weightbearing precautions for those with meniscal repairs, our data suggest that trace to zero effusion is achieved in those with meniscal repair by 13 weeks. Our previous guidelines allowed for the initiation of level ground running as early as week 8; however, given our recent data suggesting effusion commonly persists beyond 12 weeks, level ground running begins between 12 and 16 weeks in our current guideline. Our clinical data support the timeline of 4 weeks to achieve full active knee extension, irrespective of concomitant meniscal procedures. This is in agreement with the data of Noll et al 47 in which knee extension ROM at 4 weeks was predictive of knee extension loss at 12 weeks. Not surprisingly, quadriceps strength deficits persisted longer for those with graft types directly affecting the extensor mechanism; however, similar strength deficits were observed in both the ACLR and the ACLR + R groups. The HS and allograft group achieved QI >80% and >90% significantly faster than those in the BPTB group. This is consistent with the data of Smith et al 60 in which those with BPTB grafts required 4 months longer to achieve RTS criteria versus allografts and HS grafts. Therefore, the initiation of running, agilities, plyometrics, and sport-specific activities may be further delayed for those with BPTB and quad tendon grafts.
Presurgical Preparation
The immediate and long-term benefits of presurgical rehabilitation has been repeatedly described in the ACL literature.4,21,25,55,66 The restoration of a “quiet” knee after an acute ACL injury includes return of full active and passive knee extension, knee flexion ROM, trace to zero effusion, no quadriceps lag with straight leg raise, and quadriceps strength index ≥80%. Meeting all presurgical milestones has been associated with improved long-term outcomes after ACL reconstruction. Preoperative quadriceps strength is a significant predictor of postoperative knee function, further highlighting the importance of quad strengthening prior to reconstructive surgery. 35 Clinical milestones have largely remained unchanged over the years and despite more patients referred for presurgical rehabilitation, emerging evidence suggests patient expectations, outcomes, and RTS timelines lack harmony. Feucht et al 22 reported that 100% of patients expected normal or near normal knee function after ACLR surgery, 91% expected to RTS at the same level and 98% expected no or only a slightly increased risk of developing posttraumatic knee osteoarthritis (OA). Unfortunately, these drastically differ from data that suggest, irrespective of position played, 63% of National Football League athletes return to play 56 and only 42% of nonprofessional athletes return to competitive sports after ACLR. 3 In addition to RTS difficulty, patients with history of ACL rupture show posttraumatic knee OA rates of around 50% at 10- to 20-year follow-up.30,36,37 Furthermore, 21% to 48% with concomitant meniscal resections develop knee OA within 10 years. 48 Given the connections between quadriceps weakness and knee OA development, 49 rehabilitation professionals should focus on quadriceps strength to decrease modifiable factors of OA development in the years after initial ACL injury. While many factors contribute to this discrepancy, the stark contrast between patient expectations and outcomes is alarming. Therefore, rehabilitation specialists should be cautious when making prognostic claims that are counter to the abundance of literature. Instead, rehabilitation specialists should use the best available evidence to educate patients on a minimum of 9- to 12-month RTS timeline (pending successful completion of RTS test battery), the importance of immediate postoperative rehabilitation focused on progressive impairment resolution, risk of reinjury, and the long-term knee health risks associated with ACL injuries and reconstruction.
Open Kinetic Chain Exercise
While clinicians understand that the quadriceps and lower extremity muscles must be loaded after ACLR, strengthening exercise selection varies. Specifically, the persistent resistance to include lower extremity open kinetic chain (OKC) exercises is perplexing given the evidence of relatively low strain on the ACL during OKC knee extension and the poor quadriceps strength outcomes after ACL. 29 The primary concern for those leery of OKC knee strengthening is loosening of the healing ACL graft via excess strain at the tibiofemoral joint. Such concerns were first raised almost 4 decades ago in studies examining strain and anterior tibial displacement during OKC knee extension in populations with partial ACL tears and those who were ACL deficient.27,69 Both groups concluded OKC knee extension exercises loading the quadriceps should be avoided if intending to minimize ACL strain, noting strain peaked in positions of increasing knee extension. Such beliefs are still quite prevalent among clinicians and can be seen in rehabilitation guidelines despite studies reporting peak ACL strain of similar values between OKC knee extension and squatting (4%-5%).11,12,19,24 Most recently, Belloir et al 10 examined the influence of OKC isokinetic dynamometer exercises introduced at 3 months after ACL reconstruction on HS autograft distension. Again, there was no difference in graft laxity at 6 months when compared with the control group who did not perform isokinetic exercises. When discussing peak ACL strain it is important to compare the strain during resistive exercise to the strain imparted during common activities of daily living. Multiple studies have now shown gait, particularly at midstance and late swing phases of the involved limb, imparts ACL straining forces up to 13% with each step.18,61 Beynnon et al 12 demonstrated peak ACL strain of 4.4% during OKC knee isometric at 15° against 30 N·m extension torque, whereas dynamic OKC 90° to 0° with 45 N (roughly 10 lbs) resulted in peak ACL strain of 3.8%. Furthermore, peak ACL strain of 3.7% was reported during a Lachman test (150 N of anterior shear load at 30°) commonly performed intraoperatively immediately after graft fixation. OKC exercise results in approximately one-third of the strain observed during walking. 12 Therefore, OKC knee extension exercise should be considered safe if patients are immediately walking after ACLR or performing closed kinetic chain (CKC) exercise. 57 On further examination, Roldan et al 53 found walking to result in higher ACL strain (0.132 ± 0.00248 newton/body weight [N/BW] compared with running (0.097 ± 0.00249 N/BW), maximal effort single-leg horizontal jumping (0.047 ± 0.01616 N/BW), and sidestep cutting (0.107 ± 0.04027 N/BW). Maximal effort vertical jumping with 2 legs resulted in the greatest peak ACL strain during the flight phase of the jump (0.175 ± 0.01284 N/BW). Therefore, it appears greater concern should be placed on the restoration of quadriceps strength and a normalized gait pattern versus concerns regarding ACL strain between OKC versus CKC exercises.
In light of low-strain measures observed during isolated quadriceps strengthening exercise, the University of Delaware ACLR rehabilitation guidelines have been adapted to include OKC knee extension exercise through full ROM immediately after surgery (see Appendix file “Immediate Post-Operative Phase,” available online). Exercises such as long arc quads are begun 90° to 0° with light ankle cuff weight resistance in the immediate postoperative phase, with progression to a resisted knee extension machine using knee soreness and effusion as a guide for exercise progression. Modification to prescribed ROM is warranted based on graft-site pain and patellofemoral stress considerations, but should not be made based on perceived strain on the ACL graft. Knee effusion and pain should be routinely monitored to assess the joint response to all selected exercises (Tables 2 and 3).
Table 2.
Measuring effusion: sweep test a
| Instructions: | 1. Milk out swelling distal to proximal several times along the
medial aspect of the knee 2. Sweep proximal to distal on the lateral aspect of knee 3. View the medial sulcus for return of swelling |
| Grade zero: | None |
| Grade trace: | Small amount returns |
| Grade 1+: | Can milk out the swelling and it does not return on its own but returns with lateral sweep |
| Grade 2+: | Can milk out the swelling and it returns immediately to fill the pouch |
| Grade 3+: | Cannot milk out swelling |
| Rules: 1. Patients should not progress in their exercise program when the effusion is >1+ 2. When patients are holding anything above a 2+ for prolonged periods, contact MD 3. Any drastic changes of 2 grades or appearance of effusion when it was absent, decrease activity and gradually reintroduce activity when possible | |
Modified with permission from Journal of Orthopaedic & Sports Physical Therapy (Adams et al 1 ).
Table 3.
Soreness rules a
| Criterion | Action |
|---|---|
| Soreness during warm-up that continues | 2 days off, drop down 1 level |
| Soreness during warm-up that goes away | Stay at same level that led to soreness |
| Soreness during warm-up that goes away but redevelops during session | 2 days off, drop down 1 level |
| Soreness the day after lifting (not muscular soreness) | 1 day off, do not advance program to next level |
| No soreness | Advance 1 level per week or as instructed by health care professional |
Modified with permission from Journal of Orthopaedic & Sports Physical Therapy (Adams et al 1 ).
Delayed Return to Sport and Sport-related Activities
Criterion-based ACL guidelines were introduced in the late 1990s and have been a mainstay for managing athletes after ACLR since. 39 Initially proposed as a means to safeguard clinicians from progressing athletes until objective milestones had been achieved, recent trends are pointing toward using both objective milestones and time from surgery (as a surrogate for graft healing) to inform rehabilitation and RTS. The evidence remains conclusive that returning to cutting and pivoting sports is the single greatest risk factor for experiencing a subsequent ACL injury within 2 years after ACLR.26,66 Timing of when an athlete returns to level I sports also has a significant influence. Filbay and Grindem 23 advocate 3 main factors in determining RTS: biologic healing, physical readiness, and psychological readiness. With regard to biologic healing, studies assessing the neoligamentization process have demonstrated that ACL maturation continues upward of 2 years beyond initial fixation.51,63,70 These studies highlight considerations for biologic healing that are often disregarded with exclusively criterion-based guidelines. With the greatest risk of retear occurring within the first 2 years, some have proposed delaying RTS for 2 years. 45 However, the prospect of missing 2 full years of athletics has been heavily contested by clinicians and athletes. The Delaware-Oslo ACL cohort study revealed a 51% reduction in reinjury rate for each month RTS was delayed up to 9 months. 26 Furthermore, Beischer et al 9 reported a 7 times increased risk of new ACL injury for athletes returning to sport prior to 9 months. Additionally, a battery of RTS tests should be performed prior to returning to sport. A minimum test battery of hop testing and quadriceps isokinetic strength testing should be performed. 14
Paterno et al 50 reported that of the patients in their cohort who sustained a second ACL tear, 52% occurred within the first 72 athletic exposures and 30% within the first 20 athletic exposures. It is important to note that no data regarding RTS testing and time to clearance were reported. This highlights the importance of sport-specific physical preparedness when transitioning from rehabilitation to sports performance. Currently no data specific to athletes after ACLR exists, however advancements in wearable technology to monitor athlete workload has become more useful in understanding the relationship between external workload and risk of injury. A recent systematic review by Maupin et al 40 revealed that acute to chronic workload ratios (ACWR) >2.0 increased the risk of injury, whereas ACWR of 0.8 to 1.30 revealed the lowest risk of injury. Given the significant reduction in total workload after ACL injury, it appears plausible that sudden increases in workload after clearance to RTS may place athletes at an increased risk of reinjury. Therefore, a stepwise progression after RTS clearance and return to competition should be prescribed based on each athlete’s individual sport (see Appendix file “Return to Sport Phase V,” available online). Such progression may begin with a resumption of noncontact practice, followed by small-sided contact practices (1 vs 1, 2 vs 2, 3 vs 3 drills, etc), full unrestricted practice, return to competition at restricted workload, and last, return to competition unrestricted (Table 4). While the transition between each phase may be specific to each athlete, attention should be placed on the athlete’s movement quality and confidence. Apprehension, pain, and/or effusion may be signs of exceeding the athlete’s current capacity, warranting a modification to his or her current workload.
Table 4.
Return-to-competition progression (months 9-12, allograft 12+)
| Return-to-competition progression: • Noncontact practice • Small-sided contact practices (1 vs 1, 2 vs 2, 3 vs 3) • Full practice • Return to competition with restricted workload • Return to competition unrestricted *All without apprehension, pain, instability, effusion, or compensations |
| Anterior cruciate ligament (ACL) secondary prevention
program: • 2× per week moving forward • Maintain quadriceps strength and periodically assess with 1 repetition maximum (RM knee) extension strength test (pre-/postseason) • See knee injury prevention clinical practice guidelines for guidelines and video examples • Consider long-term implementation of Copenhagen planks and Nordic hamstring curls for lower extremity injury risk reduction strategies If functional ACL brace is used: may discontinue use after 1 year |
| Additional considerations: • No effusion, pain, or apprehension with sport-specific training and practice progressions • Return to preinjury conditioning level • Minimal to no dynamic knee valgus with jumping and landing • Hamstring/quadriceps ratio • Vertical hop symmetry assessment |
Psychological Considerations
Over the past decade, increased attention has been placed on psychological readiness in RTS decision making for patients after ACLR. Everhart et al 20 reviewed 3 basic psychological theories in context of ACL injuries: fear-avoidance model of pain, the theory of self-efficacy and stress, and health and the buffering hypothesis of social support theory. Their study concluded that psychological traits such as self-confidence, optimism, and motivation are likely contributors to an athlete’s psychological readiness and may be predictive of future self-reported outcomes such as pain, function, and RTS. The scope of practice for rehabilitation specialists restricts diagnosing psychological disorders and various interventions; however, recognition of when an athlete may be limited by a psychological factor may help assist in early detection and referral to additional medical personnel. Various screening tools have been developed to assist in early recognition, such as the Anterior Cruciate Ligament Return to Sport After Injury (ACL-RSI) questionnaire, which has acceptable reliability, validity, and test-retest reliability. 65 Recently, Webster and Feller 64 validated the ACL-RSI short version, and their study suggests that athletes scoring greater than 60% at 6 months after surgery were highly likely to RTS by 12 months. Conversely, those scoring less than 39 points were not likely to RTS by 12 months. 64 Currently, the ability to interpret scores between 39 and 60 at the 6-month timeline and minimum cutoff scores prior to RTS are unknown. The ACL-RSI short version may be best used to assist in early detection of athletes struggling with psychosocial issues, with equivalent psychometric properties and predictive validity to the original form (KE Webster, PhD Webster, personal communication, August 19, 2020). Meierbachtol et al 41 conducted a 5-week study using advanced-level, group plyometric training during the late stages of rehabilitation (mean, 8.1 months postoperative) prior to RTS that revealed appreciable improvements (effect size, 1.04; Cohen d) in psychological readiness on the ACL-RSI after primary ACLR. Only 53.4% of participants, however, were categorized as both psychologically and functionally (via hop testing) ready to RTS at the time of training completion, which further highlights the importance of using a comprehensive test battery for RTS clearance. Certainly, the assessment of these constructs via patient-reported outcome measures with good measurement properties (eg, ACL-RSI Short Form) should be a component of late rehabilitation (4-6 months), when impairments are resolved.
In summary, emerging evidence necessitates the need to update existing primary ACLR guidelines to account for biologic healing, psychological readiness, and physical preparedness prior to RTS and, additionally, to address inadequate rehabilitation and premature RTS decisions by providing realistic clinical milestones and systematic exercise progressions. RTS decision should be made using a minimum criteria of 9 months after surgery, isokinetic/isometric quadriceps strength symmetry ≥90%, hop testing (single, triple, crossover, and 6-m timed) of ≥90%, KOS-ADLS ≥90%, and trace to zero effusion (see Appendix file “Return to Sport Phase V,” available online). Additional considerations should include assessing psychological readiness (ACL-RSI, ≥80%) and ensuring sport-specific physical preparedness has resumed to near preinjury level and is without apprehension, pain, or effusion. Late stages of rehabilitation may be safely and cost-effectively completed in group-based settings for those making expected progress; however, those who struggled to meet prior phase milestones may require a more individualized approach.
Secondary Prevention Programs
Young athletes who return to pivoting and cutting sports after primary ACLR are roughly 4 times more likely to sustain a second ipsilateral ACL rupture and 5 times more likely to sustain a contralateral rupture. 66 Such elevated risks of reinjury challenge conventional management of ACL injuries and necessitate inquiry into novel strategies to help reduce this risk. Much of the current literature focuses on primary prevention for knee injuries. The Exercise-Based Knee and Anterior Cruciate Ligament Injury Prevention: Clinical Practice Guidelines (2017) provides strong evidence supporting the efficacy, cost-effectiveness, and feasibility of primary injury prevention programs. 5 However, less is known of the potential benefits of secondary prevention programs after a primary ACL reconstruction. The ACL–Specialized Post-Operative Return to Sports (ACL-SPORTS) trial was developed as a sport-specific secondary prevention program utilizing primary prevention program principles and evidence-based postoperative rehabilitation considerations. 67 Contrary to other published data indicating a second ACL injury range of 23% to 36% in young athletes,50,66,68 the male arm of the ACL-SPORTS trial cohort had a 1-year incidence rate of 2.5%. 6 However, the female cohort of the ACL-SPORTS trial had a 2-year incident rate of 22.8%, further highlighting the higher prevalence of reinjury among young female athletes. 31 All athletes were enrolled when they had achieved quadriceps strength >80%, minimal effusion, no pain, and full ROM and had successfully completed a running progression. Full details on the training session methods can be found in the ACL-SPORTS trial protocol article. 5 All participants were required to satisfy all components of the RTS criteria, including ≥90% quad strength symmetry, ≥90% on all hop testing (single, triple, crossover, and 6-m timed hop), ≥90% on the KOS-ADLS, and ≥90% Global Rating Scale. At 1-year follow-up, 95% of the male cohort had returned to some level of sport and 78% at their preinjury level. At 2-year follow-up, 100% of the male athletes had returned to some level of sport and 95% at their preinjury level with only 1 sustaining a retear. For the female cohort, 100% returned to some level of sport at 2 years and 87% at their preinjury level. 13 Despite a slightly lower overall incident rate of reinjury, Johnson et al 31 agree that secondary prevention strategies are a step in the right direction to reducing reinjury risk, but are still insufficient for young female athletes. Those in the ACL-SPORTS trial significantly outperformed those from the Multicenter Orthopaedic Outcomes Network and Delaware-Oslo cohorts for all outcome measures at 2 years. The results of these studies highlight the potential for secondary prevention programs to reduce the risk of second ACL injuries. The results of the ACL-SPORTS trial strengthen the RTS criteria included in this revised guideline. Therefore, it is advised that athletes continue a secondary injury prevention program at least 2 times per week as a maintenance program throughout their athletic career (see Appendix file “Return to Sport Phase V,” available online). Such programs may include the 11+ or similar programs in addition to progressive lower extremity strength training. 5
Rehabilitation Implications Based on Graft Type
Rehabilitation for patients after ACLR should consider the specific graft type. Common ACL graft sources include autografts—BPTB, quadriceps tendon (QT), and medial HS tendons—as well as allografts. Our sample of 75 patients consisted of BPTB n = 24 or 32%, QT n = 0 or 0%, and HS + allograft n = 51 or 68%. Consistent with our absence of patients with QT grafts during 2013-2017, this graft source appears to be a minority when studied in 2010 with van Eck et al 62 reporting QT grafts at just 2.5% of all autograft sources. In 2015, an international group of 35 surgeons specializing in ACLR reported that 11% of their combined ACLR cases used QT autografts. 42 Despite low QT graft selection usage in the past decade, it is expected to become more popular. 38 Therefore, rehabilitation specialists must be prepared to treat such patients as distinct. As is consistent with our ACLR rehabilitation guidelines regardless of graft type, Hunnicutt et al 28 encourage early (<6 weeks) isolated quadriceps OKC exercise through a full ROM to promote strength and activation in patients with QT autografts. A surgically induced tendinopathy is anticipated as a result of harvesting the QT, specifically the rectus femoris tendon. Generally, tendinopathy cases are treated with tendon loading exercise programs and pain management strategies such as noxious electrical stimulation. 58 So, it is logical to follow a similar thought process for loading of the quadriceps tendon to regain necessary tendon properties and manage symptoms locally. To properly isolate the rectus femoris tendon during quadriceps strengthening and tendon loading exercises, the hip must be extended. 16 For example, during the long arc quad exercise the patient will be positioned supine with thigh supported and shank hanging from the table. Similar positions should be used by reclining the trunk during quadriceps exercise on an electromechanical dynamometer or other similar instrumented training options. Of note, QT loading and quadriceps muscle strengthening exercises will overlap and should follow accepted strength-training parameters and tendon pain monitoring strategies. 58
The specific rehabilitation implications related to use of an allograft during ACLR are centered around graft healing time frames, and avoidance of graft failure. It is widely understood that graft healing is delayed after ACLR with allograft versus autograft sources (see Appendix, available online). Basic science studies such as Scheffler et al 54 show delayed allograft healing versus autografts in sheep that underwent ACLR, with delayed recellularization and revascularization at weeks 6 and 12, in addition to reduced mechanical properties at 52 weeks. Such studies were supported by an observed slower onset and rate of revascularization on serial contrast-enhanced magnetic resonance imagings of BPTB allografts versus autografts in humans monitored for 2 years after ACLR. 44 In line with delayed healing, allograft failure appears higher than in patients receiving autografts. Such increased failure rates may be highlighted in patients younger than 25 years. 15 Given that the majority of patients undergoing ACLR are young and active, it is crucial that rehabilitation specialists follow a delayed rehabilitation and RTS timeline, as has been reflected in the updated ACL guidelines. Patients with ACLR with allograft delay return to running and other higher level activities by at least 1 month after reaching milestones for the activity and delay RTS until at least 1 year postoperation.
BPTB autograft selection for ACLR has its own individual rehabilitation implications. Similar to the QT autograft, a surgically induced tendinopathy at the graft harvest site should be considered as part of a patient’s rehabilitation. Graft-site pain should be managed with pain modalities such as noxious electrical stimulation, and the remaining patellar tendon should be loaded to facilitate optimal tendon properties. The recent work of Smith et al 60 in conjunction with the data analyzed from our patient pool suggest patients who receive ACLR with BPTB regain quadriceps strength and meet RTS testing criteria at a slower rate than patients with allograft and HS grafts. These findings emphasize the importance of accurate, periodic quadriceps strength testing throughout a course of ACLR rehabilitation to identify such strength deficits and modify rehabilitation progressions accordingly.
Load Monitoring and Strength Testing
The importance of quadriceps strengthening after the ACLR is irrefutable; yet, unfortunately, periodic and accurate means to objectively assess quadriceps strength appear scarce in most rehabilitation settings. The failure to objectively measure quadriceps strengthening may be among the most troubling trends within the rehabilitation field. 46 Work by Ebert et al 17 suggests that nearly 50% of physical therapists do not assess quadriceps strength at all and as little as 38.5% are utilizing some form of instrumented strength testing. Isokinetic dynamometers have been the gold standard for quantifying muscular strength; however, they are expensive and less readily available outside of research facilities. Sinacore et al 59 investigated the accuracy of various alternatives to isokinetic quadriceps strength testing and revealed findings that challenge the criteria used in many guidelines. Often touted as a “functional” assessment of lower extremity strength, the 1 repetition maximum (1-RM) strength testing on a leg press machine was the most likely to overestimate quadriceps strength because of the ability to compensate with other lower extremity muscles, leading to premature clearance for running (23.6%) and sport (27.3%). 59 Knee extension machine 1-RM testing from 90° to 45° and handheld dynamometry with fixation via gait belt at 85° to 90° revealed the greatest accuracy for quadriceps strength estimation when compared with isokinetic dynamometers, closely followed by 1-RM knee extensions from 90° to 0° (see Appendix file “Intermediate Post-Operative Phase,” available online). One additional benefit of utilizing 1-RM strength testing on the knee extension machine is the ability to appropriately dose strengthening exercises in accordance with the American College of Sports Medicine strength and hypertrophy guidelines (65%-85% of 1-RM). However, effusion, pain, and fear may limit patients from tolerated 1-RM strength testing altogether and from exercises at a desired percentage of 1-RM, suggesting the need for alternative methods. Alternative strategies utilizing external load constraints include percentage of 5-RM, variable rates of loading/tempo, and manipulation of work/rest ratios (see Appendix file “Late Post-Operative Phase,” available online). For patients with donor-site pain, slower rates of loading/tempo may be tolerated better while allowing a greater time under tension to adequately stimulate tendon remodeling and muscular strengthening. Conversely, when 1-RM or 5-RM strength testing cannot be tolerated because of pain, effusion, or fear, internal load constraints such as rate of perceived exertion and repetitions in reserve may be used to estimate loads for strengthening. The “daily adjustable progressive resistive exercises” and “repetition in reserve” methods are examples of training strategies that allow clinicians and athletes to use actual repetitions completed and theoretical repetitions able to be completed beyond the number prescribed to determine whether a load modification is necessary. Additionally, self-reported rates of perceived exertion during exercises between 6 to 8 of 10 have been successfully used when dosing strengthening exercises.2,32-34,43,52,71
The impacts of underloading the quadriceps after ACL reconstruction can be detrimental for achieving recovery milestones and knee function. However, the current lack of accurate and quantifiable quadriceps strength assessments being completed in clinical practices leaves many clinicians blind and ill-equipped to modify their intervention strategies to address the individualized needs of their athletes. There are many normalization methods for quadriceps strength (eg, limb symmetry index, peak torque/body weight), none without its limitations. We advocate for a measure of the uninvolved knee as close to injury as possible for quadriceps strength. Our strongest recommendation is to, in fact, measure, which is often not performed or performed using manual muscle testing. Therefore, we advocate for frequent assessments of quadriceps strength utilizing isokinetic dynamometers or handheld dynamometry with fixation if able, or via 1-RM knee extension strength testing in ranges of 90° to 45° or 90° to 0°.
Conclusion
The success of an ACLR is predicated on pre- and postoperative rehabilitation. Evidence-informed rehabilitation guidelines are essential to optimize outcomes and address the high incidence of retear rates among athletes after ACLR. The following recommendations are made to optimize postoperative outcomes: initiate preoperative rehabilitation immediately to reestablish a so-called quiet knee while utilizing preoperative milestones as guidelines. Inform patients of the postoperative rehabilitation process and timelines to establish realistic goals and expectations. A combination of both biologic healing timelines and successful completion of criterion-based milestones are critical to inform RTS decision making and to reduce the incidence of retear. Isolated quadriceps strengthening, including OKC methods, is safe to initiate immediately postoperation and is a key predictor of successful postoperative outcomes. Quantification of quadriceps strength should be periodically assessed using reliable methods such as with isokinetic dynamometer, handheld dynamometer with fixation, or 1-RM quadriceps strength testing on a knee extension machine in the range of 90° to 45° or 90° to 0°. Extrapolating strength testing via hop testing and manual muscle testing or leg press strength testing is discouraged because of the potential to overestimate quadriceps strength. Increased awareness should be placed on monitoring the psychological impact of recovery after ACLR. Utilizing a reliable self-reported outcome measure such as the ACL-RSI may help identify athletes struggling with psychological variables, allowing for early detection and appropriate referral. Addressing postoperative impairments immediately, providing appropriate patient education, and utilizing objective milestones to guide rehabilitation may help indirectly reduce risk of psychological variables. Sufficient physical preparedness, a gradual reintegration into sport participation, and the continuation of a secondary prevention program can help reduce risk of retear after ACLR. However, young women are at a heightened risk of reinjury and further research is required to address this disparity. Determining appropriate phase progressions should be based on objective criteria (strength, swelling, and soreness), and specific modifications are warranted based on graft type and concomitant procedures. The minimum RTS criteria include at least 9 months postoperation, ≥90% quad strength symmetry, ≥90% on all hop testing, ≥90% on the KOS-ADLS, and ≥80% on ACL-RSI. Return to competition should be stepwise, ensuring the athlete has achieved preinjury conditioning levels and performs a maintenance secondary prevention program at least 2 times per week during one’s athletic career.
Supplemental Material
Supplemental material, sj-pdf-1-sph-10.1177_19417381211056873 for ACL Reconstruction Rehabilitation: Clinical Data, Biologic Healing, and Criterion-Based Milestones to Inform a Return-to-Sport Guideline by Alexander W. Brinlee, Scott B. Dickenson, Airelle Hunter-Giordano and Lynn Snyder-Mackler in Sports Health: A Multidisciplinary Approach
Acknowledgments
The authors to recognize and acknowledge the clinical staff at the University of Delaware Physical Therapy Clinic for their outstanding patient care and contributions to this manuscript; and Dan Chapman, DPT, OCS, for spearheading the collection of the validation data.
Footnotes
The following author declared potential conflicts of interest: L.S.-M. reports grants from the National Institutes of Health.
References
- 1. Adams D, Logerstedt D, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42:601-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American College of Sports Medicine. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41(3):687-708. [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543-1552. [DOI] [PubMed] [Google Scholar]
- 4. Arnold T, Shelbourne KD. A perioperative rehabilitation program for anterior cruciate ligament surgery. Phys Sportsmed. 2000;28:31-44. [DOI] [PubMed] [Google Scholar]
- 5. Arundale AJH, Bizzini M, Giordano A, et al. Exercise-based knee and anterior cruciate ligament injury prevention. J Orthop Sports Phys Ther. 2018;48(9):A1-A25. [DOI] [PubMed] [Google Scholar]
- 6. Arundale AJH, Capin JJ, Zarzycki R, Smith AH, Snyder-Mackler L. Two year ACL reinjury rate of 2.5%: outcomes report of the men in a secondary ACL injury prevention program (ACL-Sports). Int J Sports Phys Ther. 2018;13:422-431. [PMC free article] [PubMed] [Google Scholar]
- 7. Bach BR, Levy ME, Bojchuk J, Tradonsky S, Bush-Joseph CA, Khan NH. Single-incision endoscopic anterior cruciate ligament reconstruction using patellar tendon autograft. Am J Sports Med. 1998;26:30-40. [DOI] [PubMed] [Google Scholar]
- 8. Bach BR, Tradonsky S, Bojchuk J, Levy ME, Bush-Joseph CA, Khan NH. Arthroscopically assisted anterior cruciate ligament reconstruction using patellar tendon autograft. Five- to nine-year follow-up evaluation. Am J Sports Med. 2000;26:20-29. [DOI] [PubMed] [Google Scholar]
- 9. Beischer S, Gustavsson L, Senorski EH, et al. Young athletes who return to sport before 9 months after anterior cruciate ligament reconstruction have a rate of new injury 7 times that of those who delay return. J Orthop Sports Phys Ther. 2020;50:83-90. [DOI] [PubMed] [Google Scholar]
- 10. Belloir M, Mazeas J, Traullé M, et al. Influence of the open kinetic chain on the distension of the transplant after anterior cruciate ligament surgery with hamstring graft: search for risk factors. Int J Physiother. 2020;7:256-263. [Google Scholar]
- 11. Beynnon B, Howe JG, Pope MH, Johnson RJ, Fleming BC. The measurement of anterior cruciate ligament strain in vivo. Int Orthop. 1992;16:1-12. [DOI] [PubMed] [Google Scholar]
- 12. Beynnon BD, Fleming BC, Johnson RJ, Nichols CE, Renström PA, Pope MH. Anterior cruciate ligament strain behavior during rehabilitation exercises in vivo. Am J Sports Med. 1995;23:24-34. [DOI] [PubMed] [Google Scholar]
- 13. Capin JJ, Failla M, Zarzycki R, et al. Superior 2-year functional outcomes among young female athletes after ACL reconstruction in 10 return-to-sport training sessions: comparison of ACL-SPORTS randomized controlled trial with Delaware-Oslo and MOON cohorts. Orthop J Sports Med. 2019;7:2325967119861311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Capin JJ, Snyder-Mackler L, Risberg MA, Grindem H. Keep calm and carry on testing: a substantive reanalysis and critique of “What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis.” Br J Sports Med. 2019;53:1444-1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Claes S, Verdonk P, Forsyth R, Bellemans J. The “ligamentization” process in anterior cruciate ligament reconstruction: what happens to the human graft? A systematic review of the literature. Am J Sports Med. 2011;39:2476-2483. [DOI] [PubMed] [Google Scholar]
- 16. Diermeier T, Tisherman R, Hughes J, et al. Quadriceps tendon anterior cruciate ligament reconstruction. Knee Surgery Sports Traumatol Arthrosc. 2020;28:2644-2656. [DOI] [PubMed] [Google Scholar]
- 17. Ebert JR, Webster KE, Edwards PK, et al. Current perspectives of Australian therapists on rehabilitation and return to sport after anterior cruciate ligament reconstruction: a survey. Phys Ther Sport. 2019;35:139-145. [DOI] [PubMed] [Google Scholar]
- 18. Englander ZA, Garrett WE, Spritzer CE, DeFrate LE. In vivo attachment site to attachment site length and strain of the ACL and its bundles during the full gait cycle measured by MRI and high-speed biplanar radiography. J Biomech. 2020;98:109443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Escamilla RF, Macleod TD, Wilk KE, Paulos L, Andrews JR. ACL strain and tensile forces for weight bearing and non-weight-bearing exercises after ACL reconstruction: a guide to exercise selection. J Orthop Sport Phys Ther. 2012;42:208-220. [DOI] [PubMed] [Google Scholar]
- 20. Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23:752-762. [DOI] [PubMed] [Google Scholar]
- 21. Failla MJ, Arundale AJH, Logerstedt DS, Snyder-Mackler L. Controversies in knee rehabilitation: anterior cruciate ligament injury. Clin Sports Med. 2015;34:301-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Feucht MJ, Cotic M, Saier T, et al. Patient expectations of primary and revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:201-207. [DOI] [PubMed] [Google Scholar]
- 23. Filbay SR, Grindem H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract Res Clin Rheumatol. 2019;33:33-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Fleming BC, Oksendahl H, Beynnon BD. Open- or closed-kinetic chain exercises after anterior cruciate ligament reconstruction? Exerc Sport Sci Rev. 2005;33:134-140. [DOI] [PubMed] [Google Scholar]
- 25. Grindem H, Granan LP, Risberg MA, Engebretsen L, Snyder-Mackler L, Eitzen I. How does a combined preoperative and postoperative rehabilitation programme influence the outcome of ACL reconstruction 2 years after surgery? A comparison between patients in the Delaware-Oslo ACL cohort and the Norwegian National Knee Ligament Registry. Br J Sports Med. 2015;49:385-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50:804-808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Henning CE, Lynch MA, Glick KR. An in vivo strain gage study of elongation of the anterior cruciate ligament. Am J Sports Med. 1985;13:22-26. [DOI] [PubMed] [Google Scholar]
- 28. Hunnicutt JL, Slone HS, Xerogeanes JW. Implications for early postoperative care after quadriceps tendon autograft for anterior cruciate ligament reconstruction: a technical note. J Athl Train. 2020;55:623-627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ithurburn MP, Altenburger AR, Thomas S, Hewett TE, Paterno MV, Schmitt LC. Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Knee Surg Sports Traumatol Arthrosc. 2018;26:426-433. [DOI] [PubMed] [Google Scholar]
- 30. Janssen RPA, du Mée AWF, van Valkenburg J, Sala HAGM, Tseng CM. Anterior cruciate ligament reconstruction with 4-strand hamstring autograft and accelerated rehabilitation: a 10-year prospective study on clinical results, knee osteoarthritis and its predictors. Knee Surg Sports Traumatol Arthrosc. 2013;21:1977-1988. [DOI] [PubMed] [Google Scholar]
- 31. Johnson JL, Capin JJ, Arundale AJH, Zarzycki R, Smith AH, Snyder-Mackler L. A secondary injury prevention program may decrease contralateral anterior cruciate ligament injuries in female athletes: 2-year injury rates in the ACL-SPORTS randomized controlled trial. J Orthop Sports Phys Ther. 2020;50:523-530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Knight KL. Knee rehabilitation by the daily adjustable progressive resistive exercise technique. Am J Sports Med. 1979;7:336-337. [DOI] [PubMed] [Google Scholar]
- 33. Krzysztofik M, Wilk M, Wojdała G, Gołaś A. Maximizing muscle hypertrophy: a systematic review of advanced resistance training techniques and methods. Int J Environ Res Public Health. 2019;16:4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lesinski M, Prieske O, Granacher U. Effects and dose-response relationships of resistance training on physical performance in youth athletes: a systematic review and meta-analysis. Br J Sports Med. 2016;50:781-795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Logerstedt D, Lynch A, Axe MJ, Snyder-Mackler L. Pre-operative quadriceps strength predicts IKDC 2000 scores 6 months after anterior cruciate ligament reconstruction. Knee. 2013;20:208-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries. Am J Sports Med. 2007;35:1756-1769. [DOI] [PubMed] [Google Scholar]
- 37. Lohmander LS, Östenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145-3152. [DOI] [PubMed] [Google Scholar]
- 38. Lubowitz JH. Editorial commentary. Quadriceps tendon autograft use for anterior cruciate ligament reconstruction predicted to increase. Arthroscopy. 2016;32:76-77. [DOI] [PubMed] [Google Scholar]
- 39. Manal TJ, Snyder-Mackler L. Practice guidelines for anterior cruciate ligament rehabilitation: a criterion-based rehabilitation progression. Oper Tech Orthop. 1996;6:190-196. [Google Scholar]
- 40. Maupin D, Schram B, Canetti E, Orr R. The relationship between acute:chronic workload ratios and injury risk in sports: a systematic review. Open Access J Sports Med. 2020;11:51-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Meierbachtol A, Yungtum W, Paur E, Bottoms J, Chmielewski TL. Psychological and functional readiness for sport following advanced group training in patients with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2018;48:864-872. [DOI] [PubMed] [Google Scholar]
- 42. Middleton KK, Hamilton T, Irrgang JJ, Karlsson J, Harner CD, Fu FH. Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc. 2014;22:1467-1482. [DOI] [PubMed] [Google Scholar]
- 43. Morishita S, Tsubaki A, Takabayashi T, Fu JB. Relationship between the rating of perceived exertion scale and the load intensity of resistance training. Strength Cond J. 2018;40:94-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Muramatsu K, Hachiya Y, Izawa H. Serial evaluation of human anterior cruciate ligament grafts by contrast-enhanced magnetic resonance imaging: comparison of allografts and autografts. Arthroscopy. 2008;24:1038-1044. [DOI] [PubMed] [Google Scholar]
- 45. Nagelli CV, Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med. 2017;47:221-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Noehren B, Snyder-Mackler L. Who’s afraid of the big bad wolf? Open-chain exercises after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2020;50:473-475. [DOI] [PubMed] [Google Scholar]
- 47. Noll S, Craig Garrison J, Bothwell J, Conway JE. Knee extension range of motion at 4 weeks is related to knee extension loss at 12 weeks after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2015;3:2325967115583632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434-1443. [DOI] [PubMed] [Google Scholar]
- 49. Øiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23:171-177. [DOI] [PubMed] [Google Scholar]
- 50. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL. Am J Sports Med. 2015;42:1567-1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Rabuck SJ, Baraga MG, Fu FH. Anterior cruciate ligament healing and advances in imaging. Clin Sports Med. 2013;32:13-20. [DOI] [PubMed] [Google Scholar]
- 52. Reiman MP, Lorenz DS. Integration of strength and conditioning principles into a rehabilitation program. Int J Sports Phys Ther. 2011;6:241-253. [PMC free article] [PubMed] [Google Scholar]
- 53. Roldán E, Reeves ND, Cooper G, Andrews K. In vivo mechanical behaviour of the anterior cruciate ligament: a study of six daily and high impact activities. Gait Posture. 2017;58:201-207. [DOI] [PubMed] [Google Scholar]
- 54. Scheffler SU, Schmidt T, Gangéy I, Dustmann M, Unterhauser F, Weiler A. Fresh-frozen free-tendon allografts versus autografts in anterior cruciate ligament reconstruction: delayed remodeling and inferior mechanical function during long-term healing in sheep. Arthroscopy. 2008;24:448-458. [DOI] [PubMed] [Google Scholar]
- 55. Shaarani SR, O’Hare C, Quinn A, Moyna N, Moran R, O’Byrne JM. Effect of prehabilitation on the outcome of anterior cruciate ligament reconstruction.Am J Sports Med. 2013;41:2117-2127. [DOI] [PubMed] [Google Scholar]
- 56. Shah VM, Andrews JR, Fleisig GS, McMichael CS, Lemak LJ. Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med. 2010;38:2233-2239. [DOI] [PubMed] [Google Scholar]
- 57. Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1992;15:256-264. [DOI] [PubMed] [Google Scholar]
- 58. Silbernagel KG, Thomeé R, Eriksson BI, Karlsson J. Continued sports activity, using a pain-monitoring model, during rehabilitation in patients with Achilles tendinopathy: a randomized controlled study. Am J Sports Med. 2007;35:897-906. [DOI] [PubMed] [Google Scholar]
- 59. Sinacore JA, Evans AM, Lynch BN, Joreitz RE, Irrgang JJ, Lynch AD. Diagnostic accuracy of handheld dynamometry and 1-repetition maximum tests for identifying meaningful quadriceps strength asymmetries. J Orthop Sports Phys Ther. 2017;47:97-107. [DOI] [PubMed] [Google Scholar]
- 60. Smith AH, Capin JJ, Zarzycki R, Snyder-Mackler L. Athletes with bone–patellar tendon–bone autograft for anterior cruciate ligament reconstruction were slower to meet rehabilitation milestones and return-to-sport criteria than athletes with hamstring tendon autograft or soft tissue allograft: secondary analysis from the ACL-SPORTS trial. J Orthop Sports Phys Ther. 2020;50:259-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Taylor KA, Cutcliffe HC, Queen RM, et al. In vivo measurement of ACL length and relative strain during walking. J Biomech. 2013;46:478-483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. van Eck CF, Schreiber VM, Mejia HA, et al. “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy. 2010;26(9)(suppl):S2-S12. [DOI] [PubMed] [Google Scholar]
- 63. Vogl TJ, Schmitt J, Lubrich J, et al. Reconstructed anterior cruciate ligaments using patellar tendon ligament grafts: diagnostic value of contrast-enhanced MRI in a 2-year follow-up regimen. Eur Radiol. 2001;11:1450-1456. [DOI] [PubMed] [Google Scholar]
- 64. Webster KE, Feller JA. Development and validation of a short version of the Anterior Cruciate Ligament Return to Sport After Injury (ACL-RSI) Scale. Orthop J Sports Med. 2018;6:2325967118763763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9:9-15. [DOI] [PubMed] [Google Scholar]
- 66. Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641-647. [DOI] [PubMed] [Google Scholar]
- 67. White K, Di Stasi SL, Smith AH, Snyder-Mackler L. Anterior cruciate ligament–specialized postoperative return-to-sports (ACL-SPORTS) training: a randomized control trial. BMC Musculoskelet Disord. 2013;14:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1861-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Yack HJ, Collins CE, Whieldon TJ. Comparison of closed and open kinetic chain exercise in the anterior cruciate ligament-deficient knee. Am J Sports Med. 1993;21:49-54. [DOI] [PubMed] [Google Scholar]
- 70. Zaffagnini S, De Pasquale V, Marchesini Reggiani L, et al. Neoligamentization process of BTPB used for ACL graft: histological evaluation from 6 months to 10 years. Knee. 2007;14:87-93. [DOI] [PubMed] [Google Scholar]
- 71. Zourdos MC, Klemp A, Dolan C, et al. Novel resistance training–specific rating of perceived exertion scale measuring repetitions in reserve. J Strength Cond Res. 2016;30:267-275. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-sph-10.1177_19417381211056873 for ACL Reconstruction Rehabilitation: Clinical Data, Biologic Healing, and Criterion-Based Milestones to Inform a Return-to-Sport Guideline by Alexander W. Brinlee, Scott B. Dickenson, Airelle Hunter-Giordano and Lynn Snyder-Mackler in Sports Health: A Multidisciplinary Approach