Abstract
Objective
Prior studies have reported inequitable global access to essential medicines for cardiovascular disease (CVD) prevention, especially statins. Here we examine recent trends and disparities in statin utilisation at the income group, regional and country levels.
Design
Ecological study. Pharmaceutical sales data were used to examine statin utilisation in high-income counties (HICs) and low/middle-income countries (LMICs) from 2015 to 2020. Population estimates were obtained from the Global Burden of Disease. Fixed-effects panel regression analysis was used to examine associations between statin utilisation and country-level factors.
Setting
Global, including 41 HICs and 50 LMICs.
Participants
Population older than 40 years of age.
Primary and secondary outcome measures
Statin utilisation was measured using defined daily doses (DDDs) per 1000 population ≥40 years per day (TPD).
Results
Globally, statin utilisation increased 24.7% from 54.7 DDDs/TPD in 2015 to 68.3 DDDs/TPD in 2020. However, regional and income group disparities persisted during this period. In 2020, statin utilisation was more than six times higher in HICs than LMICs (192.4 vs 28.4 DDDs/TPD, p<0.01). Substantial disparities were also observed between LMICs, ranging from 3.1 DDDs/TPD in West African nations to 225.0 DDDs/TPD in Lebanon in 2020. While statin utilisation increased in most LMICs between 2015 and 2020, several experienced declines in utilisation, most notably Venezuela (−85.1%, from 92.3 to 14.0 DDDs/TPD). In LMICs, every $100 increase in per capita health spending was associated with a 17% increase in statin utilisation, while every 10% increase in out-of-pocket health spending was associated with a 11% decline (both p<0.05).
Conclusions
Despite global increases in statin utilisation, there are substantial regional and country-level disparities between HICs and LMICs. To address global CVD disparities, policymakers should promote increased and equitable access to statins in LMICs.
Keywords: PUBLIC HEALTH, Health policy, Ischaemic heart disease
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Pharmaceutical sales data were used to examine statin utilisation in 41 high-income countries (HICs) and 50 low/middle-income countries (LMICs)—representing approximately 90% of the global population older than 40 years of age.
Comparisons between regions, income groups and countries should be interpreted in the context of the available data and total market coverage of the included countries.
IQVIA does not provide sales data for many low-income countries; therefore, this study may underestimate the magnitude of statin utilisation disparities between HICs and LMICs.
Relationships between changes in statin utilisation and country-level characteristics are not causal.
Introduction
Cardiovascular disease (CVD)—primarily ischaemic heart disease (IHD)—causes approximately one-third of deaths worldwide.1 While age-standardised CVD mortality rates have declined globally, the number of deaths due to CVD has increased from 12.1 million in 1990 to 18.6 million in 2019,1 and substantial regional, income group and country-level disparities exist.2 3 For example, age-standardised CVD mortality rates were lowest in high-income countries (HICs) in Asia-Pacific, Europe and North America, and highest in low/middle-income countries (LMICs) in Eastern Europe, Middle East and North Africa (MENA) and South Asia.4 Moreover, the CVD burden has increased in nearly every LMIC during the past three decades.1 Currently, LMICs account for approximately 80% of global CVD deaths.2
Medicines, alongside lifestyle changes such as diet, exercise and smoking cessation, are a cornerstone of CVD prevention.5 Statins (HMG-CoA reductase inhibitors) are particularly important because they are widely recommended for primary and secondary prevention—that is, among adults with and without known CVD.5–7 Statins have been included in the WHO Model Essential Medicines List (EML)—used to develop national EMLs that guide public procurement—since 2007.8 Despite statins steadily losing patent protections throughout the world since 2006,8 only 60% of LMICs include these medicines in their EMLs as of 2017.9 As medicines included in EMLs have higher availability in the private and public sectors,10 these policies—as well as differences in income, health spending and disease burden—may result in global disparities in statin utilisation.
While utilisation of preventative cardiovascular medicines, including statins, has increased globally in the past decade, large disparities exist.11 12 For example, a study using pharmaceutical sales data from 65 countries found that consumption of cardiovascular medicines was approximately six times higher in HICs than in LMICs in 2018.11 A separate study using sales data from 83 countries found that consumption of lipid-lowering medicines was at least three times higher in HICs than in LMICs in 2018.12 However, these studies do not focus on the population at greatest need, adults older than 40 years,6 7 nor do they evaluate country-level factors associated with statin utilisation. Furthermore, an updated analysis of statin utilisation is imperative considering the ongoing COVID-19 pandemic that has caused severe disruptions to the pharmaceutical supply chain and the provision of healthcare.13–15
This study used global pharmaceutical sales data to estimate statin utilisation per population aged 40 years and older in 91 countries from 2015 to 2020. Disparities across and within regions and income groups were examined over time, including in the 6 months prior to and following the start of the COVID-19 pandemic. To inform global efforts to improve access to essential medicines, we also examined the extent to which country-level factors, such as gross domestic product, health spending and underlying IHD burden, are associated with statin utilisation.
Methods
Design and data sources
We conducted a cross-sectional study examining trends and disparities in statin utilisation in 91 countries using pharmaceutical sales data collected by IQVIA (Multinational Integrated Data Analysis System) from January 2015 to October 2020. These countries represent approximately 90% of the global population older than 40 years of age.16 IQVIA samples pharmaceutical sales from multiple distribution channels (eg, manufacturers, wholesalers and medical facilities) to develop nationally representative estimates of retail and non-retail pharmaceutical sales in each country.17 If necessary, IQVIA projects its samples to represent 100% of the retail and non-retail sales in each country and reports >90% global precision in recent years.17 However, IQVIA does not publicly disclose detailed information on data collection, projection and validation.
Several sources were used to further characterise these countries. Countries were grouped based on their income and geographical regions per the World Bank (2020).18 Population estimates and age-standardised IHD mortality rates (Global Burden of Disease (GBD) 2019 causes of death were mapped to International Classification of Diseases)19 were obtained from the GBD (2015–2019).16 Health expenditures (total, public, out-of-pocket) were also obtained from the World Bank (2015–2018).20 We projected the values of these estimates through 2020 by applying the county-specific growth rates observed from 2015 to 2018 or 2019 (depending on data availability). Finally, whether statins were included in national EMLs was determined, for reference, using the Global Essential Medicines Database (2017).9
Measuring statin utilisation
We extracted country-level dispensing for WHO Anatomical Therapeutic Chemical codes relating to statins (C10AA).21 As IQVIA does not report country-specific data for 6 countries in Central America (Costa Rica, El Salvador, Guatemala, Honduras, Nicaragua and Panama) and 12 countries in West Africa (Benin, Burkina Faso, Cameroon, Chad, Côte d’Ivoire, Democratic Republic of Congo, Gabon, Guinea, Mali, Niger, Senegal and Togo), we examined these countries in aggregate. We examined total market data, or retail and non-retail statin sales, for 52 countries (online supplemental table A). In the 23 countries/groups that lack non-retail sector data, utilisation was estimated by interpolation, using the ratio of statin consumption in the retail and non-retail sectors for other countries in their region for which data were available (85% of all statins were dispensed through the retail sector).
bmjopen-2022-061350supp001.pdf (99.7KB, pdf)
To enable international comparisons over time, we converted statin sales (expressed in milligrams) into defined daily doses (DDDs) using the Anatomical Therapeutic Chemical Classification System developed by the WHO Collaborating Centre for Drug Statistics Methodology.21 To account for differences in population size and age distribution, we report statin utilisation as DDDs per 1000 population ≥40 years per day (TPD) for each country. Global, regional, and income group statin utilisation in DDD/TPD was derived by aggregating statin sale and population estimates.
Statistical analysis
Descriptive statistics were used to examine trends and disparities in statin utilisation from 2015 to 2020. Simple linear regressions were used to determine statistical significance in trends and disparities. Changes in statin utilisation in the pre-COVID-19 (October 2019–March 2020) and post-COVID-19 (April 2020–October 2020) periods were also evaluated.
Fixed-effects panel regression analysis was used to quantify the association between economic and health indicators and the statin utilisation from 2015 to 2020. Annual, country-level statin utilisation estimates were logged in these models to enable interpretation as per cent change associated with each unit of the independent variables examined. The independent variables included time-varying health expenditure per capita, out-of-pocket health expenditure (as a percentage of total expenditure) and age-standardised IHD mortality rate. Errors were clustered by year and country to account for serial correlation.
All p values are two sided. STATA V.17.1 was used for all statistical analyses.
Patient and public involvement
No patients or members of the public were involved in the design of this study.
Results
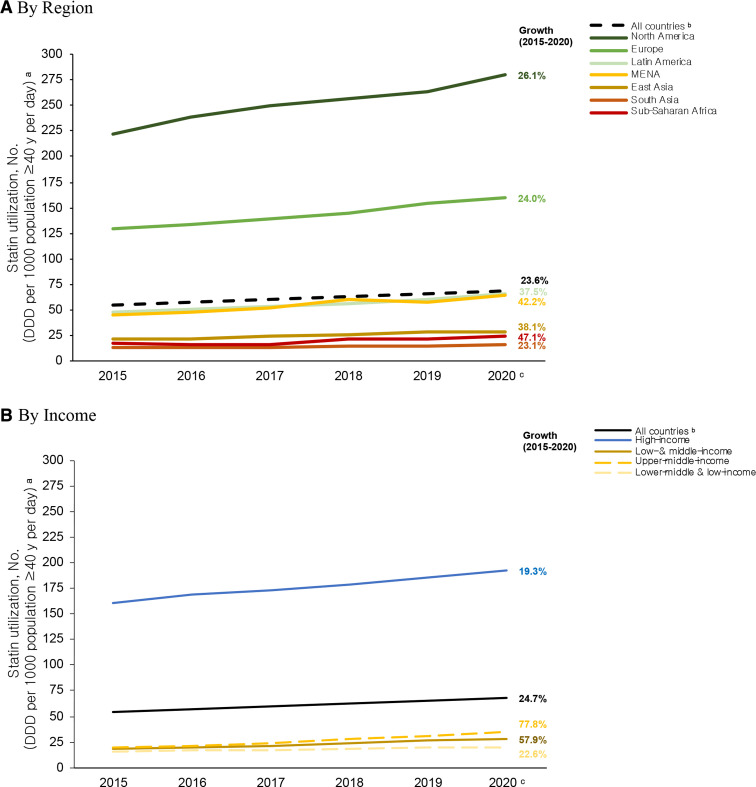
As shown in figure 1, global statin utilisation increased 24.7% from 54.7 DDDs/TPD in 2015 to 68.3 DDDs/TPD (p<0.01). While statin utilisation increased, to varying degrees, in all regions and income groups (all p<0.05), disparities persisted. In 2020, statin utilisation was highest in North America and Europe (279.7 and 159.9 DDDs/TPD, respectively) and substantially lower in Latin America, MENA, East Asia, South Asia and sub-Saharan Africa (66.1, 64.1, 29.3, 16.1 and 24.7 DDD/TPD, respectively). From 2015 to 2020, statin utilisation increased substantially in HICs (19.3% from 161.3 to 192.4 DDDs/TPD) and LMICs (57.9% from 18.0 to 28.4 DDDs/TPD). However, disparities by income group remained throughout this period—by 2020, statin utilisation was seven times greater in HICs than in LMICs.
Figure 1.
Statin utilisation by (A) geographical region and (B) income, 2015–2020. aAll trends in statin utilisation were statistically significant (p<0.05), per simple linear regression. bWe captured statin utilisation for 91 countries. cBased on data from January to September 2020. DDD, defined daily dose; MENA, Middle East and North Africa; No, number.
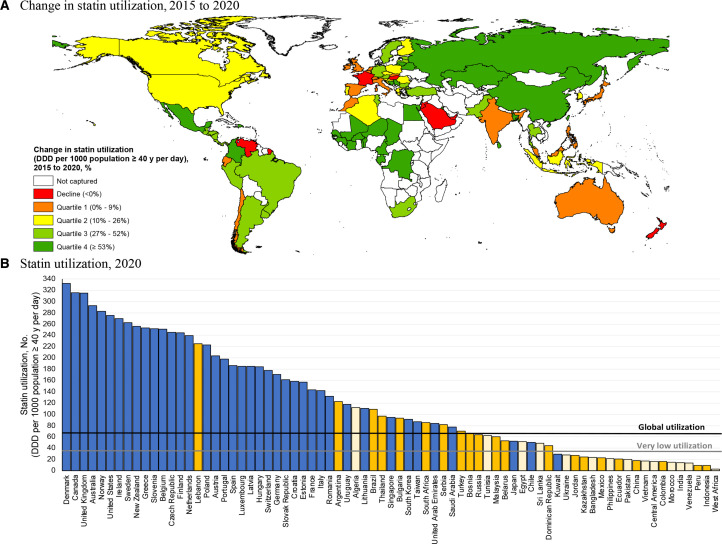
Figure 2 depicts country-specific variation in statin utilisation. From 2015 to 2020, statin utilisation increased or remained stable in most HICs, except Singapore (125.2 to 95.0, –24.1%, p=0.27), the United Arab Emirates (104.4 to 83.9, –19.7%, p=0.02), Luxembourg (216.6 to 185.3, –14.4%, p<0.01) and New Zealand (295.4 to 256.0, –13.4%, p=0.12). HICs located in North America and Europe have substantially higher statin utilisation than comparable countries located in other regions. For example, in 2020, statin utilisation in HICs ranged from over 300 DDDs/TPD in Denmark, Canada, and the UK to less than 50 DDDs/TPD in Japan, Chile, and Kuwait.
Figure 2.
(A and B)Statin utilisation by country, 2015–2020. Data for 2020 are based on statin utilisation from January to September 2020. ‘Very low utilisation’ refers to <0.5 global statin utilisation. DDD, defined daily dose; No, number.
From 2015 to 2020, statin utilisation increased by more than 10% in nearly all LMICs. Exceptions included India (12.9 to 14.1, 9.1%, p=0.02), Malaysia (57.8 to 60.0, 3.9%, p=0.41), Ecuador (20.2 to 20.9, 3.6%, p=0.09) and Jordan (28.6 to 27.1, –5.4%, p=0.20), where utilisation remained relatively stable, and Venezuela, where utilisation sharply declined (92.3 to 13.8, –85.1%, p<0.01). Several LMICs had higher statin utilisation than the global average in 2020, including Lebanon, Algeria, Brazil, Thailand and South Africa (224.9, 111.8, 109.3, 96.8 and 85.4 DDDs/TPD, respectively). Statin utilisation is lower than 34 DDDs/TPD (approximately half the global average) in 35 LMICs, including some of the most populous nations, such as China, India, Indonesia, Pakistan, Bangladesh and Mexico.
Table 1 presents factors associated with changes in statin utilisation. In HICs, only health expenditure per capita was significantly and positively associated with statin utilisation. In LMICs, every $100 increase in health expenditure per capita was associated with a 17% increase in utilisation, while every 10% increase in out-of-pocket health expenditure (as percentage of total health expenditure) was associated with a 11% decline in utilisation (both p<0.05). Greater rates of IHD mortality were also positively associated with more statin utilisation in LMICs.
Table 1.
Factors associated with statin utilisation, 2015–2020
| Exponentiated coefficient (CI)* | ||
| High-income countries | Low/middle-income countries | |
| No† | 40 | 33 |
| Health expenditure per capita ($)‡ | 1.01 (1.01 to 1.02)* | 1.17 (1.12 to 1.22)* |
| OOP health expenditure (%)§ | 0.99 (0.91 to 1.09) | 0.89 (0.82 to 0.96)* |
| IHD mortality rate¶ | 1.00 (0.99 to 1.02) | 1.02 (1.01 to 1.03)* |
*P<0.05.
*Statin utilisation is defined as defined daily doses per 1000 population >40 years per day. Here logged statin utilisation is examined. Data for 2020 are based on statin utilisation from January to September 2020.
†Countries in Central America and West Africa were excluded because IQVIA does not report country-specific information for these regions.
‡Increments of 100.
§Increments of 10.
¶Age-standardised IHD mortality rate, increments of 10.
IHD, ischaemic heart disease; No, number; OOP, out-of-pocket.
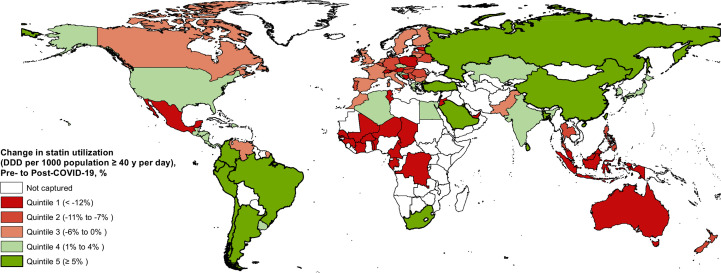
Compared with the pre-COVID-19 period, statin utilisation declined by more than 5.0% in 41 countries, including 19 HICs and 22 LMICs (figure 3). Severe disruptions in statin utilisation—or >10% decline—were found in 13 HICs, including Australia (327.5 to 265.2 DDDs/TPD, −19.0%), the United Arab Emirates (92.7 to 77.8 DDDs/TPD, −16.1%) and Germany (180.6 to 160.6 DDDs/TPD, −11.1%) (online supplemental table B). Some of the most severe disruptions in statin utilisation were observed among LMICs, including in Tunisia (76.5 to 52.7 DDDs/TPD, −31.1%), Vietnam (23.3 to 17.2 DDDs/TPD, −26.3%), Ukraine (32.1 to 26.1 DDDs/TPD, −18.7%) and Mexico (28.4 to 23.8 DDDs/TPD, −16.3%).
Figure 3.
Change in statin utilisation in pre-COVID-19 and post-COVID-19, October 2019–September 2020. Pre-COVID-19 includes the period of October 2019–March 2020 and post-COVID-19 includes the period of April 2020–October 2020. DDD, defined daily dose.
Discussion
Using a global database, representing approximately 90% of the global population older than 40 years of age,16 we found persistent disparities across regions, income groups and countries in statin utilisation, which may contribute to worsening disparities in CVD mortality. While global statin utilisation has increased 25% from 2015 to 2020, statin utilisation remains higher in the ‘global north’ (eg, North America, Europe and Oceania) and in HICs than countries in other regions and LMICs.4 In 2020, statin utilisation was 17 times higher in North America versus South Asia—the region with the highest age-adjusted CVD mortality rate in the world4—and 7 times higher in HICs versus LMICs—that are experiencing a near universal increase in the number of CVD deaths.1
Statin utilisation is also substantially lower in countries with disproportionately high age-standardised CVD mortality rates, namely LMICs in South Asia, MENA and sub-Saharan Africa.4 The WHO Global Non-Communicable Disease (NCD) Action Plan 2013–2020 aimed for a 25% reduction in premature deaths from NCD, especially CVD, from 2010 to 2025 by ensuring that at least half of adults at high CVD risk receive cardiovascular medicines and that 80% of public and private facilities have these essential medicines available on-site.22 Growth in statin utilisation in LMICs was concentrated among those countries with worsening IHD mortality—suggesting reactionary policies for the management of CVD morbidity and mortality versus preventative strategies for the provision of essential medicines. Together, our findings suggest that global efforts to reduce the burden of CVD need to be strengthened—statin utilisation remains inequitable and suboptimal in LMICs, including those with worsening rates of CVD mortality.
Importantly, there is a substantial gap between CVD burden and statin utilisation between HICs and LMICs. For example, statin utilisation is very low (less than half the global average) in 70% of the LMICs examined, yet account for 68% of the global population of middle aged and older adults and 55% CVD deaths worldwide.16 Forty-two per cent of CVD deaths occur in China (25%), India (14%) and Indonesia (4%),16 all of whom have very low statin utilisation and together account for less than 11% of statins dispensed in the world. From 2015 to 2019, the IHD mortality rate has declined or remained stable in most LMICs, with notable exceptions of Bangladesh (5%), Malaysia (5%) and Venezuela (10%) that have experienced substantial increases in recent years.16 These countries, with worsening IHD mortality, have comparatively low statin utilisation given their regional and income group averages. However, Venezuela has also experienced substantial declines in statin utilisation in this period—aggravating the IHD burden experienced by its populace.
Among LMICs, we found that every $100 increase in per capita health spending was associated with a 17% increase in statin utilisation and that every 10% increase in the proportion of out-of-pocket health spending was associated with an 11% decline. These findings suggest that policy efforts to address global disparities in statin utilisation may need to increase health spending while shifting the burden of health spending from individuals to the public sector (either via the direct provision of healthcare and medicines or via insurance schemes). Unfortunately, public investment in health (as measured by government health spending as a percentage of total expenditures) has declined in LMICs during the last two decades.23 Only high-income and upper middle-income countries have seen moderate increases in government health spending,23 countries that consume a disproportionate share of statins. Out-of-pocket spending as a share of total health spending has remained stubbornly high in LMICs (above 40% and twice the percentage in HICs) during this period.23 International aid—a major source of health spending in LMICs—is disproportionately directed to communicable diseases,23 and these policies may aggravate global disparities in the use of essential medicines, including statins, and hinder efforts to reduce CVD mortality. International aid for health, which could alleviate costs of essential medicines for governments and the public, has also stagnated since 2013.23
Economic or political crises, which are often followed by sharp declines in total health spending, may also impact access to essential medicines. The starkest example is Venezuela, where statin utilisation declined 85% between 2015 and 2020. The ongoing sociopolitical crisis began in 2010 and has spiralled into a sustained period of hyperinflation, a 75% decline in health spending, as well as widespread and chronic shortages of essential medicines in the past decade.20 24
Pharmaceutical supply chain disruptions have resulted from a slowdown in the production of medicines that impact domestic and international markets, transportation hurdles and restrictions on movement (internationally and domestically and by providers and patients).25 For example, early in the pandemic, active pharmaceutical ingredient production in China was severely curtailed—leading to shortages and delays in the production of medicines throughout the world, including in the USA, the European Union and India.26
During the first 6 months of COVID-19 pandemic, statin utilisation declined by more than 5% in 41 countries. As a whole, HICs experienced greater declines in statin utilisation during the post-COVID-19 period (−2% vs −4% observed worldwide). Perhaps, because HICs had more severe restrictions on movement to mitigate COVID-19 spread than LMICs early in the pandemic.27 However, the most severe disruptions in individual countries occurred in LMICs, which may be more vulnerable to supply chain disruptions. Several countries in Eastern Europe (eg, Serbia, Bosnia, Belarus and Ukraine), Southeast Asia (eg, Thailand, Malaysia, the Philippines, Vietnam and Indonesia) and MENA (eg, Tunisia and Jordan) saw dramatic declines in statin utilisation, as did West Africa as a region and Mexico. Global COVID-19 disparities, including inequitable access to vaccinations,27 may result in persistent disruptions to statins access in LMICs, as countries prioritise acute health needs. If these trends continue, the COVID-19 pandemic may halt or reverse gains in statin utilisation and worsen regional and country-level CVD disparities between HICs and LMICs.
Limitations
This study had several limitations. First, comparisons between regions, income groups and countries should be interpreted in the context of the available data and total market coverage of the included countries. For example, IQVIA does not provide non-retail sales for 39 of the 91 countries examined. However, 85% of all statins were dispensed through retail pharmacies, and we account for missing non-retail sales through interpolation (using the ratio of statin consumption in the retail and non-retail sectors for other countries in their region for which data were available). Second, IQVIA does not provide sales data for most low-income countries; therefore, this study may underestimate the magnitude of statin utilisation disparities between HICs and LMICs. Finally, relationships between changes in statin utilisation and country-level characteristics are not causal. However, the trends and disparities in statin utilisation described in this study help evaluate the global progress in ensuring equitable access to essential medicines and inform efforts to reduce the global burden of CVD.
Conclusion
Despite a 25% increase in global statin utilisation from 2015 to 2020, there are substantial and persistent regional and country-level disparities between HICs and LMICs. To address worsening CVD disparities, global, regional, and national policymakers should promote increased and equitable access to statins in LMICs.
Supplementary Material
Footnotes
Twitter: @jennyguadamuz, @dimamqato
Contributors: DMQ developed the methodology, wrote the first draft, provided critical revisions to the article resulting in improvemebts in design, analyses and interepretations, and received funding for the study. AS provided administrative support and supplied suggestions for the analyses, data interpretation and article drafting. JSG drafted the article, conducted the data analyses, provided critical revisions to the article resulting in improvements to the design, analyses and interpretations. All authors reviewed, revised and approved the final version of the article. DMQ is the guarantor and accepts full responsibility for the work and/or conduct of the study, had access to the data, and controlled the decision ot publish
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors. The authors would like to thank IQVIA Human Data Science COVID-19 Collaborative for facilitating access to the MIDAS data used in this study.
Disclaimer: Flatiron Health had no role in the design and conduct of the study, analysis or interpretation of the data, and preparation, or final approval of the article before publication.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: JSG currently reports employment with Flatiron Health, which is an independent subsidiary of the Roche Group.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. No data are available. IQVIA data sharing policy does not permit us to share this data.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was considered exempt by the Institutional Review Board at the University of Southern California because this study was not considered human subjects research.
References
- 1.Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol 2020;76:2982–3021. 10.1016/j.jacc.2020.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bowry ADK, Lewey J, Dugani SB, et al. The burden of cardiovascular disease in low- and middle-income countries: epidemiology and management. Can J Cardiol 2015;31:1151–9. 10.1016/j.cjca.2015.06.028 [DOI] [PubMed] [Google Scholar]
- 3.Barquera S, Pedroza-Tobías A, Medina C, et al. Global overview of the epidemiology of atherosclerotic cardiovascular disease. Arch Med Res 2015;46:328–38. 10.1016/j.arcmed.2015.06.006 [DOI] [PubMed] [Google Scholar]
- 4.Roth GA, Johnson C, Abajobir A, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol 2017;70:1–25. 10.1016/j.jacc.2017.04.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . Prevention of cardiovascular disease: guidelines for assessment and management of cardiovascular risk, 2007. Available: https://www.who.int/cardiovascular_diseases/guidelines [Accessed 24 Oct 2021].
- 6.Grundy SM, Stone NJ, Bailey AL. 2018 ACC/AHA/AACVPR/AAPA/ABC/ACPM/ADA/AGS/ APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of cardiology Foundation/American heart association tTask force on clinical practice guidelines. J Am Coll Cardiol 2018. 10.1161/CIR.0000000000000625 [DOI] [Google Scholar]
- 7.Arnett DK, Blumenthal RS, Albert MA. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American heart association task force on clinical practice guidelines. Circulation 20192019;140:e596–646. 10.1161/CIR.0000000000000678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kishore SP, Blank E, Heller DJ, et al. Modernizing the World Health Organization list of essential medicines for preventing and controlling cardiovascular diseases. J Am Coll Cardiol 2018;71:564–74. 10.1016/j.jacc.2017.11.056 [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization . Global essential medicine, 2019. Available: https://global.essentialmeds.org/ [Accessed 25 Jul 2021].
- 10.Bazargani YT, Ewen M, de Boer A, et al. Essential medicines are more available than other medicines around the globe. PLoS One 2014;9:e87576. 10.1371/journal.pone.0087576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yan VKC, Blais JE, Li X, et al. Trends in cardiovascular medicine use in 65 middle- and high-income countries. J Am Coll Cardiol 2021;77:1021–3. 10.1016/j.jacc.2020.12.025 [DOI] [PubMed] [Google Scholar]
- 12.Blais JE, Wei Y, Yap KKW, et al. Trends in lipid-modifying agent use in 83 countries. Atherosclerosis 2021;328:44–51. 10.1016/j.atherosclerosis.2021.05.016 [DOI] [PubMed] [Google Scholar]
- 13.Alexander GC, Qato DM. Ensuring access to medications in the US during the COVID-19 pandemic. JAMA 2020;324:31–2. 10.1001/jama.2020.6016 [DOI] [PubMed] [Google Scholar]
- 14.Lakavage A. Covid-19 has exposed cracks in the global medicines supply chain STAT; 2020. https://www.statnews.com/2020/06/02/covid-19-exposed-cracks-global-medicines-supply-chain/ [Accessed 24 Oct 2021]. [Google Scholar]
- 15.World Health Organization . COVID-19 continues to disrupt essential health services in 90% of countries, 2021. Available: https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries [Accessed 24 Oct 2021].
- 16.Institute for Health Metrics and Evaluation . Global burden of disease study 2019, 2021. Available: http://www.healthdata.org/gbd [Accessed 12 Dec 2021].
- 17.IQVIA . Accuracy and timeliness statistics annual report; 2021. https://www.iqvia.com/library/publications/acts-2020 [Accessed 25 Jul 2021].
- 18.World Bank Data . World bank country and lending groups, 2021. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [Accessed 25 Jul 2021].
- 19.Institute for Health Metrics and Evaluation . Global burden of disease study 2019 (GBD 2019) cause list mapped to ICD codes, 2021. Available: https://ghdx.healthdata.org/record/ihme-data/gbd-2019-cause-icd-code-mappings [Accessed 27 May 2022].
- 20.World Bank . World bank open data, 2021. Available: https://data.worldbank.org/ [Accessed 25 Jul 2021].
- 21.WHO Collaborating Centre for Drug Statistics Methodology . Purpose of the ATC/DDD system. Available: https://www.whocc.no/atc_ddd_methodology/purpose_of_the_atc_ddd_system/ [Accessed 06 Apr 2020].
- 22.World Health Organization (WHO) . Global action plan for the prevention and control of noncommunicable diseases 2013-2020; 2013.
- 23.World Health Organization (WHO) . Global spending on health: Weathering the storm; 2020.
- 24.Raphelson S. Venezuela’s Health Care System Ready To Collapse Amid Economic Crisis NPR; 2018. https://www.npr.org/2018/02/01/582469305/venezuelas-health-care-system-ready-to-collapse-amid-economic-crisis [Accessed 26 Dec 2021]. [Google Scholar]
- 25.McDonell A, Chalkidou K, Yadav P. Understanding the impact of COVID-19 on essential medicine supply chains Center For Global Development; 2020. https://www.cgdev.org/blog/understanding-impact-covid-19-essential-medicine-supply-chains [Accessed 26 Dec 2021]. [Google Scholar]
- 26.Mullin R. COVID-19 is reshaping the pharmaceutical supply chain. 98. Chem Eng News, 2020: 31–5. [Google Scholar]
- 27.Eyawo O, Viens AM, Ugoji UC. Lockdowns and low- and middle-income countries: building a feasible, effective, and ethical COVID-19 response strategy. Global Health 2021;17:1–5. 10.1186/s12992-021-00662-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-061350supp001.pdf (99.7KB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. No data are available. IQVIA data sharing policy does not permit us to share this data.