Abstract
Forcibly displaced persons, such as refugees, are at an increased risk of physical and mental health conditions and so would benefit from novel healthcare technologies, research on which can be conducted under an ethical framework.
According to the United Nations Refugee Agency, persecution, conflict, violence, and human rights violations have resulted in the forced displacement of more than 82 million persons worldwide in 2020—a record-breaking figure. The migration journey exposes displaced populations to multiple traumas, such as gender-based violence, detention, poor sanitation, infectious diseases, and family separation.1,2 After reaching their destination, many forcibly displaced individuals experience loss of social status and discrimination and face barriers to healthcare, employment, education, and housing.3 Owing to the compounding effects of traumas experienced before, during, and after migration, forcibly displaced populations are at risk of suffering from chronic psychophysical conditions.4
The use of novel technologies in this population, in addition to routine clinical care, provides an opportunity to reduce health disparities for forcibly displaced individuals. New technologies in healthcare are rapidly expanding, from three-dimensional bioprinting of tissues and organs to on-site portable sequencing to detect disease. Two novel technologies that are especially relevant to displaced persons, which have revolutionized healthcare for the general population in high-income countries, are: omics and digital healthcare technology. Each of these can benefit forcibly displaced populations if applied appropriately and responsibly.
Omics and digital technology
Advances in omics technology (e.g., genomics, epigenomics, transcriptomics, proteomics, metabolomics, and microbiomics) improve knowledge of disease progression on a molecular level and have contributed to the development of targeted therapeutics and preventative measures. Cancer therapeutics include microbiome profiling and manipulation through designer probiotics, diet, and lifestyle changes to improve the efficacy of cancer immunotherapy.5 The gut microbiome influences autoimmune disorders, mental health, inflammatory bowel disease, diabetes, obesity, and hypertension. Omics-based health analyses have become mainstream in some parts of the world, with the emergence of direct-to-consumer testing kits, such as 23andMe, EpigenCare, and Thryve. These products inform users about their risk for diseases and food intolerances, provide an analysis of the composition of their gut microbiome, and offer recommendations for lifestyle changes to attain desired health outcomes.
Digital technology is ubiquitous in clinical settings. Telehealth, via web or smartphone apps, is used for a variety of purposes, including obtaining informed consent for research, streamlining the management of patient care, and tracking medical conditions remotely using synchronized sensors.6 In addition, advanced computational techniques such as artificial intelligence are being used to improve the accuracy and predictive potential of complex multi-level data including electronic medical records, environmental exposures, and clinical and biological profiles. These techniques enable accurate diagnoses, the prediction of predispositions to illnesses, and the design of highly effective drugs in short timeframes.7
Tailored healthcare plans
Forcibly displaced persons suffer from multiple barriers to healthcare in their host country and experience unique stressors that are associated with poor health outcomes.4 While these individuals may benefit from healthcare technologies, such as omics tools and digital tools, such healthcare advances are not readily accessible to this population.
Improving the participation of forcibly displaced persons in omics and digital healthcare research has significant potential to improve the identification of people at higher risk for developing mental health, communicable, and non-communicable disease in a high-throughput manner. These technologies can also promote cost-effective preventative measures, and improve the accuracy of digital phenotypes and omics biomarkers of disease. Collectively, this approach can guide the curation of evidence-based, tailor-made healthcare plans for displaced persons (Figure 1).
Figure 1. Research priorities for novel technologies with forcibly displaced populations.
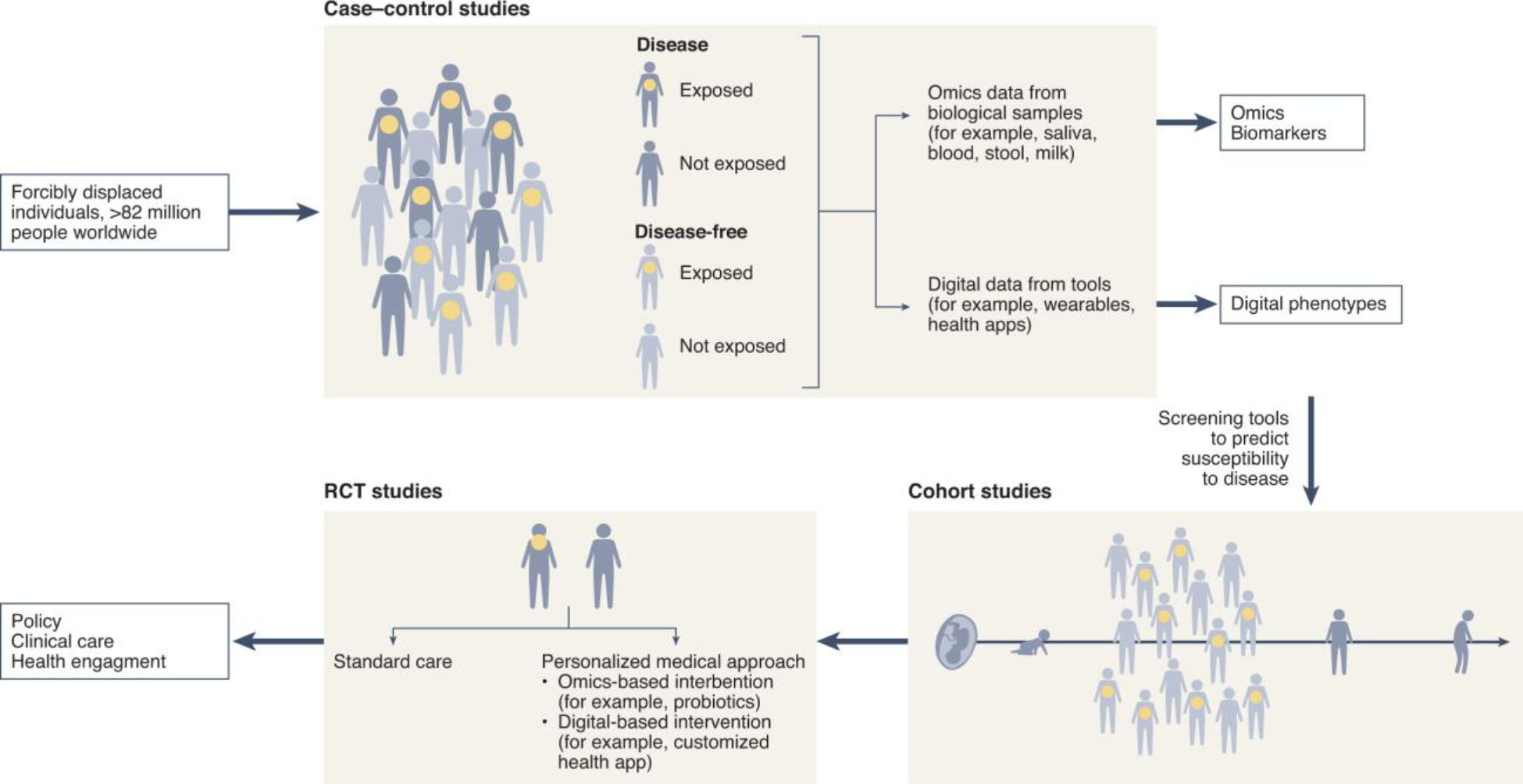
Forcibly displaced populations can greatly benefit from case-control studies with omics and digital tools to identify potential omics biomarkers and digital phenotypes associated with disease. Omics biomarkers and digital phenotypes can then be employed in cohort studies to evaluate their validity as screening tools for diseases among these populations. Randomized control trials (RCTs) can evaluate the effectiveness of omics or digital-based interventions in preventing or managing diseases that are prevalent in these communities.
Integrating environmental risk factors, such as stress associated with family separation or immigration detention, with other omics profiling can provide an improved understanding of the relationship between environment and physiology.8 Longitudinal cohort studies with omics profiling coupled with a detailed survey of the exposome (i.e., the timing, duration, and intensity of adverse lifetime exposures) enable the identification of temporal molecular changes that precede the emergence of disease. This methodology has previously been utilized successfully. For example, researchers employed prospective methylation9 and metabolite10 biomarker analysis and correctly predicted all individuals from the general population who developed cerebro-cardiovascular disease (CCVD). Similar methods could be utilized for the screening of displaced populations, who have limited access to specialists and primary care services. Such high throughput screening methods are necessary to guide precise, preventative medicine on both an individual and population level (Figure 1).
In forcibly displaced populations, digital health technology can reduce communication and transportation barriers, provide critical, otherwise inaccessible, information about routine screening and available healthcare resources,11 and facilitate the surveillance of exposures.8 Such populations suffer from higher risks for pregnancy complications, mental illness, and cardiovascular disease. Digital tools have been shown to improve health outcomes for the general population.12–14 Those tools should be tailored for displaced populations and evaluated through observational and randomized study designs. Identifying specific resettlement risk factors that are associated with suboptimal omics and digital profiles can suggest disease predisposition and guide clinical care. For example, customized probiotics could be prescribed for individuals with microbial dysbiosis that predisposes them to diabetes. A digital approach could also improve adherence by guiding people on how to take the supplement under remote observation.
Data from these studies can also influence policy. Epigenetic profiling could show predisposition to cardiovascular disease in individuals experiencing forced family separation. This information would suggest that immigration policies may result in a permanent, and potentially transgenerational, impact on the health of such immigrants.
Logistical and ethical challenges
At the time of writing, only 112 out of 383110 registered clinical studies included forcibly displaced populations; only 1 of 4012 asthma and 34 of 7754 depression studies included this population. None of the 948 epigenetic studies or the 2464 microbiome studies, and only 2 of the 8275 digital clinical trials included forcibly displaced populations. This is not surprising given the underrepresentation of displaced populations in health-related investigations due to research challenges, combined with limitations in the design of research in general.
Novel technology research with forcibly displaced persons is associated with logistical and ethical challenges and is also influenced by the socio-political environment. As with any research in this population, access is challenging, particularly in refugee camps. Additionally, the majority of forcibly displaced persons (>80%) reside in low- and middle-income countries and consequently have limited access to novel technologies.
Digital healthcare is also lagging in low- and middle-income countries due to structural barriers including the lack of 5th Generation (5G) telecommunication networks, minimal infrastructure for the Internet of Things (loT), and the absence of basic services such as constant supply of electrical power. Many displaced persons have not permanently resettled and are at the mercy of immigration policies in their temporary countries of residence. As a result, some individuals might be hesitant or unwilling to participate in novel technology research due to privacy concerns related to their legal status. Moreover, the socio-political environment can influence priority research areas. Less than 10% of funding spent on research focuses on diseases that afflict 90% of the world’s population.15 Medical conditions like tuberculosis, malaria, diarrhea, and pneumonia, which account for more than 20% of the world’s health problems and are more common in underserved communities, received less than 1% of the world’s total healthcare research funding.16 Similar is the inequity in distribution of effective and life-saving SARS-CoV-2 vaccines to low-income countries and vulnerable groups.17
Public health technology research is rarely configured to serve forcibly displaced populations, as has been made apparent by the COVID-19 pandemic. Research projects attempting to collect data on the spread of the virus remotely have disproportionately excluded individuals who live in overcrowded spaces that lack privacy, who experience mobility restrictions or lack internet access, and are unfamiliar with using, or lack autonomy over, digital tools.18 Moreover, omics and digital technology research with forcibly displaced populations has not been made scalable or sustainable. Omics-based approaches have been used to track antibiotic resistance and outbreaks of infectious disease and to identify determinants of metabolic disease and mental health in vulnerable groups (Table 1). However, this work is not reproduced in multiple settings and is not incorporated in a unified portal, such as the Migration Data Portal (https://www.migrationdataportal.org/), which allows meta-analyses or integrated analyses with exposomics data to be conducted. Similarly, while some digital tools have been designed to manage diseases, track vaccination, train healthcare providers in trauma-informed care, mitigate communication barriers, improve antenatal care, and treat mental health disorders (Table 1), the majority of these tools have not been evaluated or maintained, are focused on specific medical conditions, and are not integrated into a comprehensive and accessible healthcare system.19
Table 1.
Existing omics and digital tools studies with forcibly displaced populations.
| Existing studies | Purpose | Population | Country | Reference |
|---|---|---|---|---|
| Omics | Microbiome-based analysis to evaluate the prevalence of antibiotic resistance. | Refugees from Syria, Iraq and Afghanistan | Germany | PMID: 29458422 |
| Whole-genome sequencing approach to track the transmission of Mycobacterium tuberculosis. | Refugees from several African countries | Netherlands & Denmark | PMID: 29167288 | |
| Cohort study to evaluate the associations between microbial compositions in the nasopharynx and infants’ health in the first two years of life. | Myanmar, predominantly of Karenic ethnicity | Maela refugee camp on the Thailand-Myanmar border | PMID: 28968382 | |
| Cross-sectional and cohort studies to evaluate the effect of migration on the microbiome and its association with body mass index (BMI). The microbiome was stratified by BMI in refugees and immigrants in countries of origin versus after migrating to the USA. | Hmong and Karenic immigrants and refugees | USA | PMID: 30388453 | |
| Evaluation of mental health and epigenome-wide DNA methylation in response to pre/post-natal exposure to violence. | Included Middle Eastern refugees | Germany | PMID: 31040859 | |
| Longitudinal cohort study to evaluate the effect of migration and resettlement stressors on mental health, genetic and DNA methylation in children and their parents. | Syrian and Iraqi refugees | USA | PMID: 33791438 | |
| Digital | Diabetes prevention intervention through portable computer technology integrating diabetes risk screening with behavior change. | Arab refugees | Jordan | PMID: 26835181 |
| Randomized control trial (RCT) study to evaluate the improvement of daily adherence to tuberculosis medication through an edible ingestion sensor (IS)) | Refugees from different ethnic backgrounds | USA | PMID: 31584944 | |
| Tailoring a free, bilingual, digital application designed to empower individuals to manage their vaccination records. | Predominantly Arab refugees | Canada | PMID: 29482427 | |
| RCT study to evaluate the effectiveness of a multicomponent health information technology mental health screening intervention to aid primary health care providers in diagnosing and treating mental illness among refugees. | Health care providers for Cambodian refugees | USA | PMID: 31095060 | |
| RCT study to evaluate the effectiveness of a modular, interactive self-help app, which will be grounded on cognitive-behavioral models for the treatment of posttraumatic stress. | Syrian refugees | Germany | PMID: 31039786 | |
| Single arm feasibility trial to evaluate the effectiveness of a smartphone health app based on culturally adapted methods from cognitive behavioral therapy in the reduction of substance use among youth. | Refugees | Germany | PMID: 33869122 | |
| A non-randomized controlled trial to evaluate the effectiveness of a digital communication assistance tool in collecting medical history and health outcomes. | Refugees and health care providers | Germany | PMID: 32093286, PMID: 30728030 | |
| A feasibility study to evaluate mobile Health (mHealth) in perinatal health (smartphone app to collect medical information and provide education on pregnancy and birth, diagnostic platform to send test results and enable remote supervision). | Refugees | Italy | PMID: 29143900 | |
| A feasibility pilot study to evaluate mHealth in perinatal health (smartphone app to receive healthcare appointment reminders, access health-related communication, store medical records, contact emergency services, and navigate the healthcare system). | Syrian refugees | Turkey | PMID: 33117656 | |
| A pilot study to evaluate the use of a smartphone-assisted ecological momentary assessment (EMA) to assess daily mood, sleep patterns, and mental health. | Refugee children and adolescents | Germany | PMID: 33524043 |
BMI, body mass index; EMA, ecological momentary assessment; IS, ingestion sensor; mHealth, mobile health; PMID, PubMed ID; RCT, randomized control trial.
Strides are being made in the safe and ethical use of novel technologies research in other vulnerable populations such as children, pregnant women, and people with HIV. However, forcibly displaced populations continue to be excluded from this promising research. Rather than excluding this group entirely, strategies learned from prior efforts with other vulnerable communities should be harnessed and utilized. Fear of harm should not be a barrier to progress.
Minimizing risk
Care must be taken when including forcibly displaced populations in research involving novel technologies. The World Medical Association’s Declaration of Helsinki notes that “medical research with a vulnerable group is only justified if the research is responsive to the health needs or priorities of this group…[and] this group should stand to benefit from the knowledge, practices, or interventions that result from the research.” As described above, novel technology research is indeed justified in displaced persons, and they deserve access to the benefits of this cutting-edge and individualized technology.
The World Medical Association also notes that “some research populations are particularly vulnerable and need special protection. These include those who cannot give or refuse consent for themselves and those who may be vulnerable to coercion or undue influence.” In the context of novel technologies, this issue is perhaps compounded by the difficulty of communicating complex results and interpreting complicated statistical risks for potential future diseases to patients. Health privacy challenges associated with digital technology are inherent to all patients; however, breaches in the privacy of this digital information have disproportionate impact for individuals involved in immigration or resettlement applications. Digital data are immortal and such information is valuable and at risk of being bought and sold commercially. These data may also be identifiable and difficult to keep anonymous. Medical research involving extremely vulnerable populations must clearly communicate such risks thoroughly and clearly to participants while striving to ensure that the likelihood of such negative outcomes is minimized.
Community-based participatory research
One approach to improve the accessibility of clinical research on novel technologies is through community-based health care models such as The European Union’s Mig-HealthCare. Involving representatives from forcibly displaced populations in the research design will improve recruitment, retention, adherence, and success of the intended research by reducing communication and cultural barriers.20 This approach can promote the participation of these populations in national and state longitudinal cohort survey studies (e.g., the National Health and Nutrition Examination Survey and the NYC Social Determinants of Health survey).
Such tools should also collect information regarding immigration status rather than a generic data point of ‘foreign born’. This will enable the evaluation of social determinants of health that are specific to this population. Another approach is to highlight the healthcare contributions of forcibly displaced physicians and researchers to promote public engagement with advocacy groups.21 Table 2 summarizes the challenges and risks, as well as potential solutions to including forcibly displaced persons in novel technology research.
Table 2.
Challenges, risks and suggested solutions for the inclusion of forcibly displaced populations in novel technology research.
| Challenges | Solutions |
| Research funding is not equitable between vulnerable and non-vulnerable populations and does not prioritize forcibly displaced persons. | There should be an increased focus on providing funding to research inclusive of vulnerable populations, including forcibly displaced persons. |
| Forcibly displaced populations may be hesitant to join research efforts for a multitude of reasons. | Community-based participatory research approaches should be implemented in study design stages when possible. Forcibly displaced populations should be involved in the research planning process so that concerns can be adequately addressed early.22 |
| Researchers may intentionally avoid forcibly displaced populations due to perceived difficulties in attaining research approval with these populations. | Efforts should be made to incentivize research projects with forcibly displaced populations and streamline Institutional Review Board (IRB) approval processes with these groups. IRBs should include reviewers with experience in vulnerable populations research. |
| Technical research challenges include finding appropriate control populations, accounting for potentially low retention and adherence rates, the possibility of re-traumatization in participants, and navigating selection bias due to convenient sampling strategies. | Non-forcibly displaced immigrants from similar ethnic backgrounds have been used as controls, though there are limitations to this approach. Nested case-control study designs can also be used for association analyses. Community-based approaches that improve the patients’ engagement in research will likely improve retention and adherence rates to the study procedure. Such approaches can be supplemented with innovative communication strategies, such as animation and the use of simple analogies to explain the study goals and procedure. Trauma-informed training for researchers can mitigate re-traumatization. Adopting homogenous convenience sampling strategies (i.e., to one or more sociodemographic factor(s)) can improve generalizability and accuracy of the findings.23 |
| Risks | Solutions |
| Forcibly displaced populations may have difficulty comprehending the informed consent process. | IRBs should seek counsel from experts in conducting research with forcibly displaced or at-risk populations. Advisory boards from forcibly displaced populations should be established to guide the development of informed consent forms, the study risks and potential benefits, and the interpretation of findings.24 Language-concordant research nurses or research assistants should be trained in integrating social and clinical data with omics and digital health data. In turn, they will help in developing and implementing clear communication modalities about the research tools and findings for this population.25 |
| Ethical standards are needed to ensure that research involving forcibly displaced persons is efficacious and practical. | Standardized protocols should be developed for novel technology research, such as omics and digital tools, with forcibly displaced persons. This includes ensuring the voluntary nature of participating in such research and its dissociation from receiving any benefits that they may be otherwise eligible for as well as maximizing non-coercive benefits, by providing opportunities for participants to learn about health or settlement issues during participation in the project. |
| Efforts to maintain the autonomy, safety, and confidentiality of extremely vulnerable populations are imperative. | The well-being and rights of forcibly displaced persons that participate in research must be protected. Sensitive data should be protected, and comprehensive security measures should be implemented. Researchers should seek Certificates of Confidentiality and receive extensive training in handling identifiable information for extremely vulnerable populations including forcibly displaced populations. |
IRB, institutional review board.
Acknowledgements
Research was supported by the National Institute Of Neurological Disorders and Stroke of the National Institutes of Health (NIH) under award number K23NS116114. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflicts of interest statement
The authors declare no conflicts of interest.
References
- 1.Lunde I & Ortmann J Lancet 336, 289–291 (1990). [DOI] [PubMed] [Google Scholar]
- 2.Patel N et al. Cochrane Database Syst. Rev 11, CD009317 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO. Health of Refugees and Migrants: Regional Situation Analysis, Practices, Experiences, Lessons Learned and Ways Forward (2018).
- 4.Yun K et al. J. Immigr. Minor. Health 14, 933–940 (2012). [DOI] [PubMed] [Google Scholar]
- 5.Gopalakrishnan V et al. Cancer Cell 33, 570–580 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang CJ et al. Pediatr. Clin. North Am.67, 603–611 (2020). [DOI] [PubMed] [Google Scholar]
- 7.Yu KH et al. Nat. Biomed. Eng 2, 719–731 (2018). [DOI] [PubMed] [Google Scholar]
- 8.Jiang C et al. Cell 175, 277–291 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang CS & Kao CY J. Biomed. Sci 26, 59 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeong A et al. Environ. Int 119, 334–345 (2018). [DOI] [PubMed] [Google Scholar]
- 11.Talhouk R et al. J. Med. Internet. Res 22, e14283 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frey DP et al. Anesth Analg.128, e93–e96 (2019). [DOI] [PubMed] [Google Scholar]
- 13.Kim JY et al. J. Med. Internet Res 18, e116 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marvel FA et al. Circ. Cardiovasc. Qual. Outcomes 14, e007741 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yegros-Yegros A et al. Health Res. Policy Sys 18, 47 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Global Forum for Health Research (WHO, 2000). [Google Scholar]
- 17.Binagwaho A et al. Lancet Glob. Health 9, e1169–e1171 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh NS et al. Lancet 397, 560–562 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arsenijevic J et al. J. Med. Internet Res 22, e11613 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Riza E et al. Healthcare 8, 115 (2020). [Google Scholar]
- 21.Adida C, Lo A, Prather L, & Williamson SJ Exp. Polit. Sci 10.1017/XPS.2021.11 (2021). [DOI]
- 22.Culhane-Pera KA et al. J. Commun. Genet 8, 117–125 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jager J et al. Monogr. Soc. Res. Child Dev 82, 13–30 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Culhane-Pera K et al. J. Commun. Genet 8, 117–125 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Taylor JY & de Mendoza VB J. Nurs. Scholar 10.1111/jnu.12358 (2017). [DOI] [Google Scholar]


