Abstract
Objectives:
Develop and use a casual loop diagram (CLD) of smoking among racial/ethnic minority and lower-income groups to anticipate the intended and unintended effects of tobacco control policies.
Methods:
We developed a CLD to elucidate connections between individual, environmental, and structural causes of racial/ethnic and socioeconomic disparities in smoking. The CLD was informed by a review of conceptual and empirical models of smoking, fundamental cause and social stress theories, and 19 qualitative interviews with tobacco control stakeholders. The CLD was then used to examine the potential impacts of three tobacco control policies.
Results:
The CLD includes 24 constructs encompassing individual (e.g., risk perceptions), environmental (e.g., marketing), and structural (e.g., systemic racism) factors associated with smoking. Evaluations of tobacco control policies using the CLD identified potential unintended consequences that may maintain smoking disparities. For example, the intent of a smoke-free policy for public housing is to reduce smoking among residents. Our CLD suggests that the policy may reduce smoking among residents by reducing smoking among family/friends, which subsequently reduces pro-smoking norms and perceptions of tobacco use as low risk. On the other hand, some residents who smoke may violate the policy. Policy violations may result in financial strain and/or housing instability, which increases stress and reduces feelings of control, thus having the unintended consequence of increasing smoking.
Conclusions:
The CLD may be used to support stakeholder engagement in action planning and to identify non-traditional partners and approaches for tobacco control.
Smoking prevalence has declined significantly in the United States (US), but disparities in smoking remain among demographic groups defined by socioeconomic status and race/ethnicity.[1] In 2018, cigarette smoking was higher among those with an annual household income of less than $35,000 (21.3%) than those with an annual household income of $100,000 or more (7.3%).[1] Cigarette smoking is most prevalent among American Indian/Alaska Native adults (22.6%), followed by Multiracial (19.1%), White (15.0%), and Black (14.6%) adults, and lowest among Hispanic (9.8%) and Asian (7.1%) adults.[1] Furthermore, socioeconomic and racial/ethnic disparities have largely remained unchanged or become worse over time.[2, 3]
Although there are evidence-based strategies for reducing smoking prevalence overall, it is less clear how to reduce racial/ethnic and socioeconomic disparities in smoking.[3, 4] Tobacco control efforts have evolved from high-risk approaches (targeting those identified at most risk) to an emphasis on population-level interventions (changing norms and environments that increase risk exposure).[5] Popular tobacco control strategies like education and awareness campaigns and smoke-free air laws may not impact all populations equally, however, possibly resulting in increased disparities.[6]
Several theories provide insight into why racial/ethnic and socioeconomic disparities in smoking persist. Fundamental cause theory defines root, or “fundamental,” causes of health disparities as factors that emerge or continue to be associated with poor health outcomes, even when proximal risk factors, like prevention and treatment interventions, are developed.[7, 8] Such associations remain over time because fundamental causes limit access to key resources (e.g., money, health services) necessary for maintaining health. Examples of fundamental causes include socioeconomic status,[7] racism,[9] residential segregation,[10] and stigma.[11]
Social stress theory argues that social hierarchies produce higher exposure to stress, including both experiential (e.g., job loss) and structural (e.g., discrimination) stress, among socially disadvantaged groups.[12–14] Both stress sources can negatively impact mental and physical health. Also, coping resources like social connections and personal resources, which can ameliorate the association of stress with health, are theorized to be socially distributed, such that people with lower social status may have less access to coping resources.
Critical race theory (CRT) argues that race is a socially constructed concept used to maintain racial hierarchies that socially, economically, and legally benefit individuals who are White.[15] CRT scholars and practitioners identify and address root causes of structural racism in systems and institutions in an effort to eliminate racism and its influence on health.[15] Researchers have called for the incorporation of CRT into scholarship in areas that are closely tied to tobacco use, such as targeted marketing.[16, 17] Taken together, these theories suggest that underlying contributors to smoking disparities could include factors like financial strain, discrimination, and social capital, which have not traditionally been the focus of tobacco control interventions.
Systems science may elucidate the complex factors that maintain racial/ethnic and socioeconomic disparities in smoking. Systems science is an interdisciplinary field that aims to better understand the nature of an entire system that often cannot be achieved by studying the system’s component parts in isolation.[18] Tobacco control is increasingly recognized as a complex system that includes biological, behavioral, and environmental factors.[5] As such, the National Cancer Institute has called for systems approaches to enhance tobacco control and prevention efforts.[5] Causal loop diagramming is a qualitative systems science method that involves visually depicting how variables within a system influence each other over time.[19] In addition to illuminating key determinants of disparities, causal loop diagrams (CLDs) can be used to explicitly hypothesize both the intended and potential unintended consequences of interventions by examining the multiple pathways of impacts triggered, sometimes reinforcing earlier changes and other times counteracting them.[19]
The purpose of this study is to create a CLD of cigarette smoking among racial/ethnic minority and lower-income adult smokers that encompasses individual, environmental, and root cause or “fundamental” factors. We used the above theories, a review of published theoretical and empirical models of smoking, and qualitative interviews with diverse stakeholders in tobacco control to develop the CLD. We then used the CLD to examine the intended and potential unintended consequences of three tobacco control policies: smoke-free air policies in public housing, menthol cigarette bans, and minimum floor price laws.
Methods
The Causal Loop Diagram
A CLD is a tool used to visualize interconnected variables and feedback mechanisms within a system believed to underlie observed trends.[19] These diagrams consist of the system’s component parts (i.e., variables) and arrows representing relationships between variables such that a change in the first variable triggers a change in the second variable over time, all else equal. In a CLD, a plus or minus sign is attached to each arrow to indicate polarity; a plus sign means the variables in the CLD move in the same direction and a minus sign means the variables in the diagram move in opposite directions.[20] Variables and arrows in a CLD can link together to create feedback loops, which are categorized as either reinforcing or balancing.[19] In a reinforcing loop, change in a given variable (either an increase or decrease) in one direction results in more change in that same direction over time (systematic growth or decline among variables in the loop). In a balancing loop, change in one direction triggers consequences that counteract the initial change.
In this study, CLD development was informed by a literature review and the theoretical frameworks described above. First, three members of our team (M.C.O., P.L., S.D.M.) conducted a rapid review of PubMed to identify studies published since 2000 that used systems science approaches to develop theoretical models of smoking. See Supplementary File 1 for the search strategy. Additionally, one team member (S.D.G) reviewed theoretical frameworks of social determinants of health and social stratification to identify potentially relevant constructs for the CLD. We then developed a CLD of smoking in Vensim software using constructs from established conceptual and empirical models of smoking informed by our rapid review. Based on our theoretical framework review, we added constructs to the CLD that were not traditionally included in conceptual models of smoking, but are critical for explaining racial/ethnic and socioeconomic disparities in smoking.
Iteration of the CLD
After developing a CLD rooted in evidence-based literature and theory, we refined the CLD by soliciting feedback from researchers, practitioners, and advocates with backgrounds in public health, health disparities, and/or tobacco control. First, we conducted a focus group (N = 3) with researchers in tobacco control and cancer-related health disparities to ensure the CLD was comprehensive and understood by experts in the field. The focus group was also used to refine our interview guide.
Next, we solicited feedback on the CLD from a convenience sample of 19 traditional (e.g., tobacco control researcher) and non-traditional (e.g., smoker) stakeholders in tobacco control using a semi-structured interview conducted in-person or virtually. The convenience sample was recruited using snowball sampling, whereby stakeholders interviewed were asked to name others who may be eligible to participate and could offer an informative assessment of the CLD.[21] This method resulted in a diverse sample of stakeholders including members of social service and equity-focused organizations, a mental health professional, and public health researchers from across the US. The interview included questions such as, “Is there anything in the model you would change?” and “Do you think this model would be useful for the field of tobacco control?” Stakeholders provided feedback on the included constructs, relationships between constructs, how best to present the CLD, and how the model could be used to advance tobacco control. Interviews were audio recorded. After the interviews, stakeholders’ feedback was discussed among research team members and recommended changes to the model were incorporated iteratively into the CLD. Interviews were conducted until saturation was reached, defined as no new substantive additions recommended for the CLD. This study was approved by the Institutional Review Board at the University of North Carolina, Chapel Hill.
Tobacco Control Policies
The final version of the CLD was used to explore the intended and possible unintended consequences of three equity-focused tobacco control policies: smoke-free air policies in public housing, menthol cigarette bans, and minimum floor price laws. These policies were selected because they have been hypothesized to reduce racial/ethnic and/or socioeconomic disparities in smoking rates. For each policy, we used the CLD to consider the intended and potential unintended pathways through which the policy affects smoking. Reinforcing and balancing loops were also identified.
Results
Causal Loop Diagram
Table 1 presents the 24 constructs, categorized into individual, environmental, and root cause or “fundamental” factors, in the final version of our CLD of cigarette smoking among racial/ethnic minority and lower-income adults. Figure 1 includes individual and environmental factors associated with smoking based on existing literature; Figure 2 adapts the CLD to account for fundamental factors affecting disparate smoking rates in racial/ethnic minority and lower-income populations identified through both empirical and theoretical literature.
Table 1.
Variables Included in the Casual Loop Diagram
| Construct |
|---|
|
|
| Individual Factors |
| Stress/anxiety |
| Sense of control |
| Menthol preference |
| Cravings/addiction |
| Perceptions of tobacco use as low risk |
| Environmental Factors |
| Normalization of smoking |
| Tobacco use among family/friends |
| Smoke-free homes/workplaces |
| Product and flavor availability |
| Tobacco marketing |
| Access to cessation services |
| Tobacco retailer density/proximity |
| Tobacco prices |
| Tobacco companies’ profit maximization efforts |
| Zoning laws |
| Root Causes or Fundamental Factors |
| Marginalization |
| Discrimination |
| Segregation |
| Social capital |
| Housing instability |
| Structural racism |
| Health care access |
| Low-wage work |
| Financial strain |
| Targeted tobacco marketing* |
| Tobacco retailer density/proximity* |
| Access to culturally relevant cessation services* |
Note. Constructs with an asterisk reflect those that are considered both environmental and fundamental factors.
Figure 1.
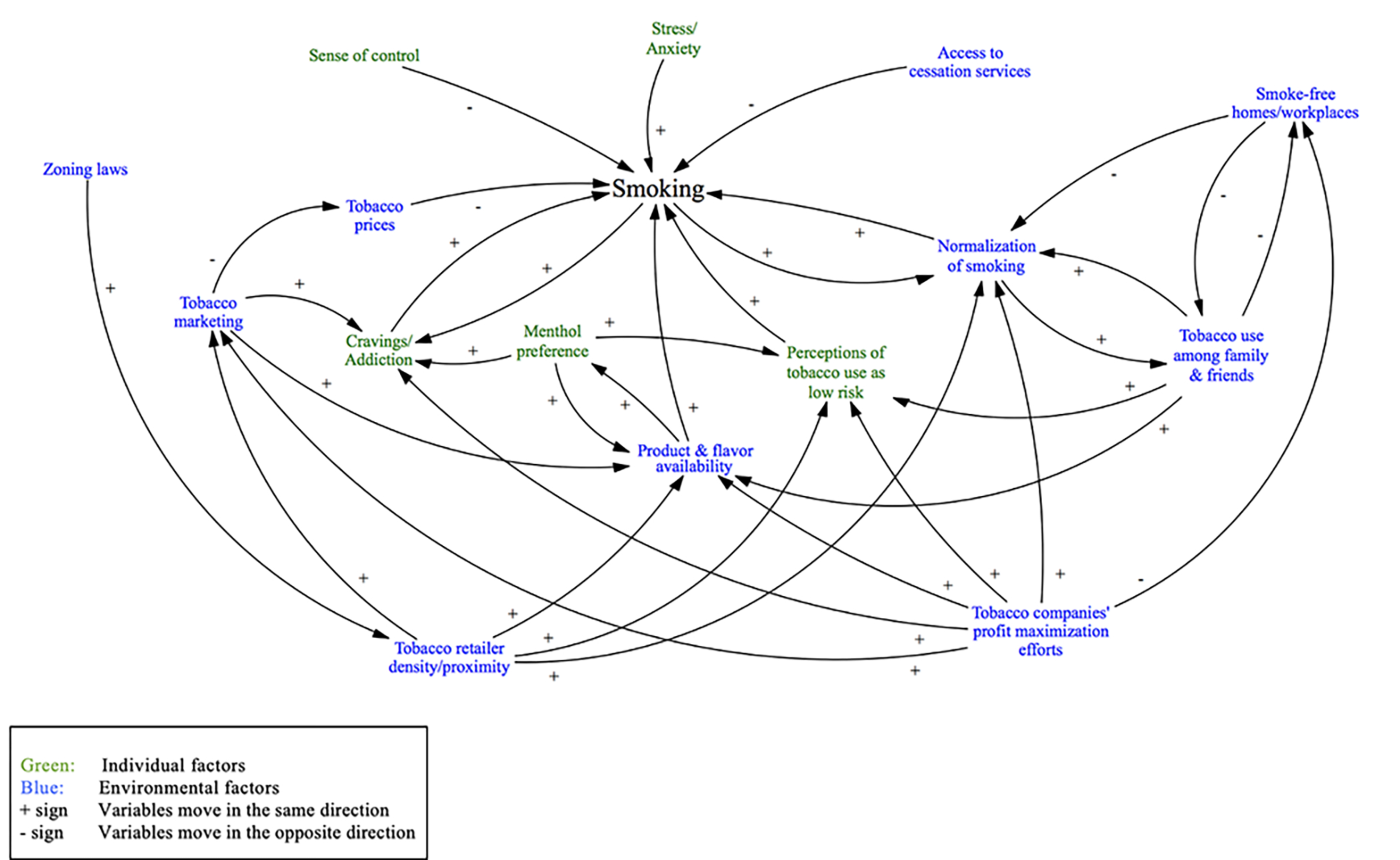
Initial causal loop diagram of smoking with individual and environmental factors
Figure 2.
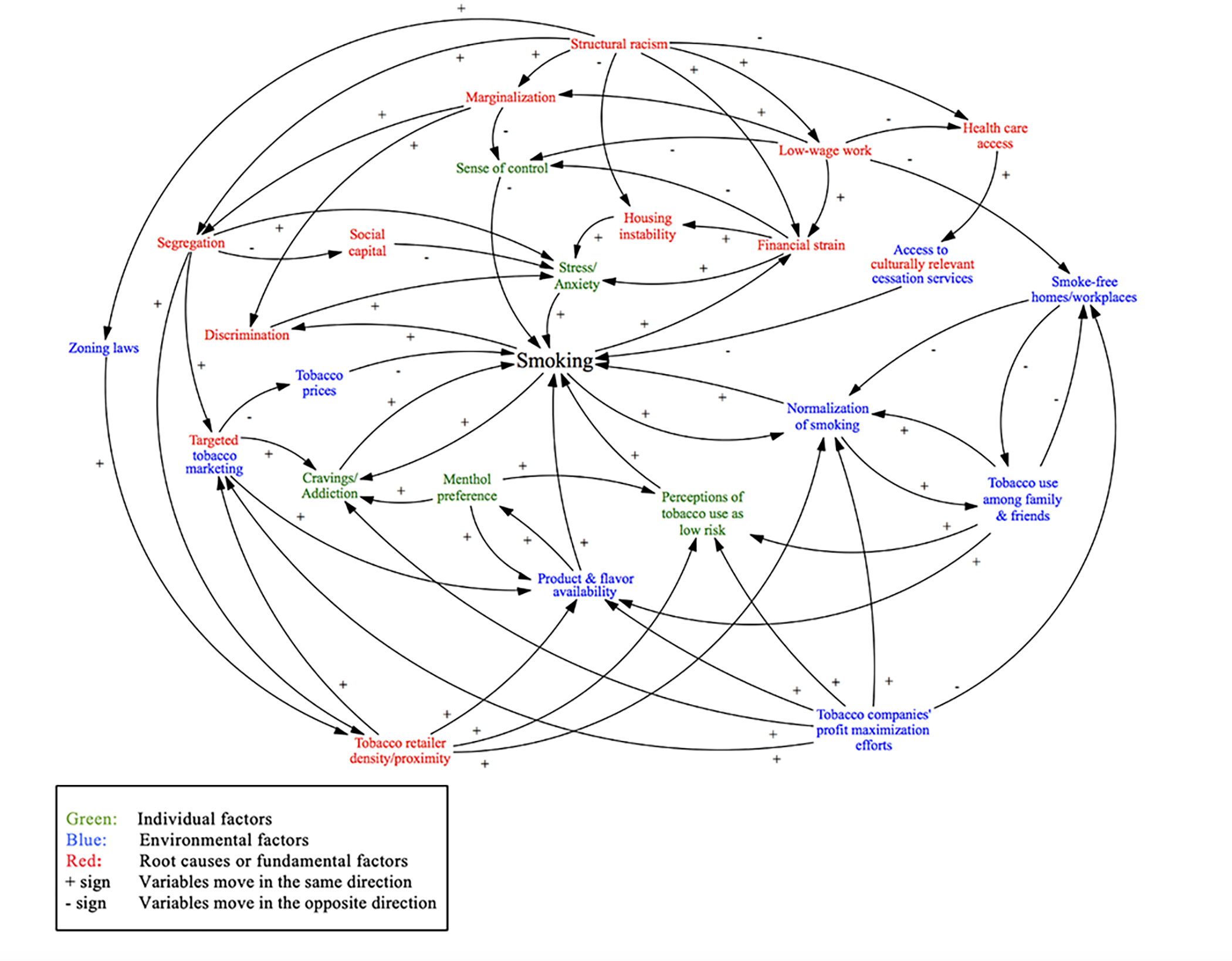
Final causal loop diagram of smoking with individual, environmental, and fundamental factors
Individual Factors.
Individual-level factors in the model include cravings and addiction, perceptions of smoking, preference for menthol cigarettes, stress and anxiety, and sense of control. Robust literature demonstrates that cigarettes are an addictive product and that smoking results in cravings for more cigarettes.[22] In addition, studies show that individuals’ beliefs about the harms of tobacco use are associated with smoking.[23, 24] Lower perceived harm is associated with smoking initiation among non-smokers and continued tobacco use among current smokers. Studies also show that a preference for menthol cigarettes, a type of flavored cigarette commonly used in the focal population, is associated with greater bioavailability of nicotine, greater addiction, and more difficulty quitting.[25, 26] In addition, despite the well-known harm of cigarettes, menthol cigarettes were historically marketed as a healthier option for smokers. Some menthol cigarette smokers perceive lower harms from smoking mentholated cigarettes as compared to non-menthol cigarettes.[25]
The association between stress and smoking is also well-documented.[27] Smoking is a coping behavior for stress and individuals report smoking provides stress relief.[27, 28] The literature also identifies sense of control, which we define as a feeling of control over one’s well-being, as an important factor associated with smoking.[29] Greater feelings of control lower the likelihood of smoking.
Environmental Factors.
Environmental factors in the CLD include the tobacco industry, and more specifically the industry’s profit maximization efforts and tobacco marketing, including control over product and flavor availability and tobacco prices in the retail environment. Exposure to tobacco marketing and lower prices for tobacco products are positively associated with smoking.[30, 31] In addition, a growing literature finds that tobacco retailer density and proximity is associated with greater smoking prevalence.[32, 33] Zoning laws determine, in part, where tobacco retailers can locate in a community. Other important environmental factors include social and environmental norms around smoking, tobacco use among family and friends, and access to cessation services.[34–36] Individuals are more likely to smoke if they perceive that smoking is approved by friends and family members or society broadly. In addition, smokers without access to cessation services are less likely to quit.[36]
Fundamental Factors.
Many models of smoking in the US have been developed using a range of systems science approaches, yet models typically fail to incorporate root cause or “fundamental” factors of smoking disparities. Compartmental simulation models (e.g., SimSmoke), a quantitative systems science approach, have been used to forecast smoking rates and explore the potential impacts of tobacco control polices.[37] These simulation models vary in structure, but the underlying logic models of smoking are typically based on smoking initiation and cessation rates and do not explicitly incorporate other factors associated with smoking.[37] Smoking models in network analysis studies and agent-based models typically go beyond smoking rates to incorporate other individual-level (e.g., peer influence) as well as social and/or environmental (e.g., tobacco retailers) factors.[38] [39] [40] However, existing models are typically developed for the general US population and fail to include “fundamental” causes of smoking disparities. Houle and Siegel, who used causal loop diagramming to examine the impact of workplace policies barring employment to smokers, did include “fundamental” factors such as economic stress, unemployment, and uninsurance.[41] However, no models in our review included factors such as racism and discrimination, despite their important role in smoking behavior.
Grounded in a priority population approach, to effectively reduce disparities in smoking it is critical to consider the root causes of the individual and environmental factors traditionally associated with smoking.[6] Therefore, we include factors that are root causes of smoking among racial/ethnic minorities and lower socioeconomic groups in red in the updated CLD (Figure 2). Low-wage work may represent a root cause of smoking. Smokers may not have access to health care and cessation services if employed in low-wage work that does not provide insurance that covers this service. Low-wage work may also increase financial strain that, in turn, increases stress and lowers feelings of control, which increases the likelihood of smoking. Similarly, housing instability may represent a root cause of smoking because it increases financial strain and stress.[42]
Marginalization may also be an important root cause of smoking among racial/ethnic minority and lower socioeconomic groups. Marginalization in the US has resulted in neighborhood segregation and discrimination, which allows for targeted marketing of tobacco products based on neighborhood demographic characteristics.[43] Connections between marginalization, racism and targeted marketing have been increasingly identified in the marketing literature.[16, 17] Marketing researchers have noted that racism and racist power structures are drivers of targeted marketing of unhealthy products, such as cigarettes, to racial/ethnic minority communities.[16, 44] Segregated communities may also have lower social capital, or the effective functioning of social groups through a sense of shared understanding and trust, and higher levels of stress, which again increases the likelihood of smoking.[45] In addition to being an environmental factor, tobacco retailer density/proximity can also be considered a disparities factor because studies show that tobacco retailer density/proximity is disproportionately high in neighborhoods with a greater percentage of residents who are racial/ethnic minorities and have lower income.[46–50] Finally, the CLD depicts structural racism as a critical component of the model, and is shown as a driver of several disparities constructs. See Table 2 for a description of the reinforcing loops in the CLD. The figure provided in Supplementary File 2 incorporates the reinforcing loops into the CLD.
Table 2.
Feedback Loops Impacting Smoking Among Racial/Ethnic Minority and Lower-Income Adults
| Loop number | Short loop story | Variables in loop |
|---|---|---|
| Reinforcing feedback loops (reinforce earlier changes) | ||
| R1 | Smoking increases stress/anxiety through financial strain | Stress/anxiety –>(+) smoking –>(+) financial strain –>(+) stress/anxiety |
| R2 | R1, with the added impact of housing instability | Stress/anxiety –>(+) smoking –>(+) financial strain –>(+) housing instability –>(+) stress/anxiety |
| R3 | Smoking fuels discrimination, which triggers stress (a trigger for smoking) | Stress/anxiety –>(+) smoking –>(+) discrimination –>(+) stress/anxiety |
| R4 | Smoking lowers sense of control through financial strain | Sense of control –>(−) smoking –>(+) financial strain –>(−) sense of control |
| R5 | Interconnected demand and supply for menthol cigarettes | Menthol preference –>(+) product & flavor availability –>(+) menthol preference |
| R6 | Cycle of smoking and cravings/addiction | Cravings/addiction –>(+) smoking –>(+) cravings/addiction |
| R7 | Social norms are more (less) accepting of smoking when we smoke (abstain) | Normalization of smoking –>(+) smoking –>(+) normalization of smoking |
| R8 | R7, but among our family and friends | Normalization of smoking –>(+) tobacco use among family & friends –>(+) normalization of smoking |
| R9 | R8, with the added impact of smoke-free homes/workplaces on smoking norms | Normalization of smoking –>(+) tobacco use among family & friends –>(−) smoke-free homes/workplaces –>(−) normalization of smoking |
| R10 | Integrating R7 and R8, and adding the impact of health-related perceptions of tobacco use | Perceptions of tobacco use as low risk –>(+) smoking –>(+) normalization of smoking –>(+) tobacco use among family & friends –>(+) perceptions of tobacco use as low risk |
| R11 | Menthol in cigarettes can make smoking feel safer, counteracting the link between perceived risk of smoking and non-smoking | Perceptions of tobacco use as low risk –>(+) smoking –>(+) normalization of smoking –>(+) tobacco use among family & friends –>(+) product & flavor availability –>(+) menthol preference –>(+) perceptions of tobacco use as low risk |
| R12 | Cycle of tobacco use (non-use) among family and friends and smoke-free homes/workplaces | Tobacco use among family & friends –>(−) smoke-free homes/workplaces –>(−) tobacco use among family & friends |
| R13 | Product and flavor availability reinforces family and friends’ smoking and our own smoking | Normalization of smoking –>(+) tobacco use among family & friends –>(+) product & flavor availability –>(+) smoking –>(+) normalization of smoking |
| R14 | Product and flavor availability increases preference for menthol cigarettes, which increases cravings/addiction, smoking, and smoking norms, resulting in increased tobacco use among family and friends and more product and flavor availability to meet demand | Product & flavor availability –>(+) menthol preference –>(+) cravings/addiction –> smoking –>(+) normalization of smoking –>(+) tobacco use among family & friends –>(+) product & flavor availability |
Notes. Where the loops start and stop, as described here, is an arbitrary choice since the ripple effects circle around over time. (+) indicates that variables move in the same direction. (−) indicates that variables move in the opposite direction.
Stakeholder Interviews
Nineteen traditional and non-traditional stakeholders in tobacco control provided feedback on iterations of our CLD through individual interviews. Excerpts from interviews are presented to highlight changes made to our smoking model based on their perspectives and experiences in this field.
Examples of Changes to the CLD
Stakeholders recommended new constructs for the CLD and changes to relationships between constructs. For example, in response to feedback from an advocate in an equity organization, the word ‘targeted’ was added to ‘tobacco marketing.’ The advocate stated: “That should be predatory tobacco marketing rather than just tobacco marketing.” In addition, the ‘tobacco industry’ was added to the CLD after an advocate asked: “Where is the tobacco industry?” The ‘tobacco industry’ was subsequently changed to ‘tobacco companies’ profit maximization efforts’ after a member of an equity organization noted: “tobacco industry…that is too general. What do you mean by tobacco industry?” A public health researcher also stated, “Tobacco industry feels a little vague to me.”
In response to feedback from a public health consultant, ‘culturally relevant’ was added to the term “access to cessation services” when incorporating fundamental factors. The consultant stated, “…you had … cessation, but I was thinking it should say culturally relevant cessation because sometimes you have access… but if they can’t relate to it...”
Tobacco retailer density/proximity is presented as a fundamental factor in the updated CLD in response to a recommendation made by a smoking cessation researcher: “In one case you went from a blue [environmental factor] to a red [root cause]. I wonder if there are other ones that need that…for example, you have … concentration of tobacco retailers...Poor little kids in urban areas go by a whole lot more [tobacco] ads as they walk to school than kids in suburban areas…That partially explains disparities…. It helps [you] understand why smoking is high in certain geographic areas.”
Usefulness of the CLD
Interviews were also used to gather feedback on the model’s perceived utility. An advocate from an equity organization reflected on the model saying: “To me this is a commitment to long-term...” The advocate also discussed the importance of expanding stakeholders to include non-traditional partners:
“… it also helps to identify who partners may be…you’re going to need to work with folks who are working on housing issues, you’re going to need to work with folks who are trying to increase access to healthcare, all these different partners are going to be involved.” A mental health practitioner stated: “me, as a psychologist, focuses on the green [individual-level factors] first. Being able to take a step back and think about all the other factors…it could broaden people’s perspectives in terms of thinking about where we can intervene.”
Overall, interviewees agreed that the root cause/fundamental constructs included in the CLD are important for smoking. They noted the importance of considering root causes of smoking to effectively reduce disparities in priority populations.
Tobacco Control Policies
Using the CLD, the intended and potential unintended effects of three tobacco control policies were explored.
Smoke-free air in public housing.
In July 2018 the Department of Housing and Urban Development required that public housing units implement a smoke-free policy that prohibits the use of all lit tobacco products.[51] The CLD indicates the smoke-free air policy should reduce smoking among public housing residents by reducing tobacco use among family and friends, which subsequently reduces pro-smoking norms and perceptions of tobacco use as low risk. These processes are reinforcing, resulting in further reductions in tobacco use among family and friends and more smoke-free homes (Figure 3a).
Figure 3.
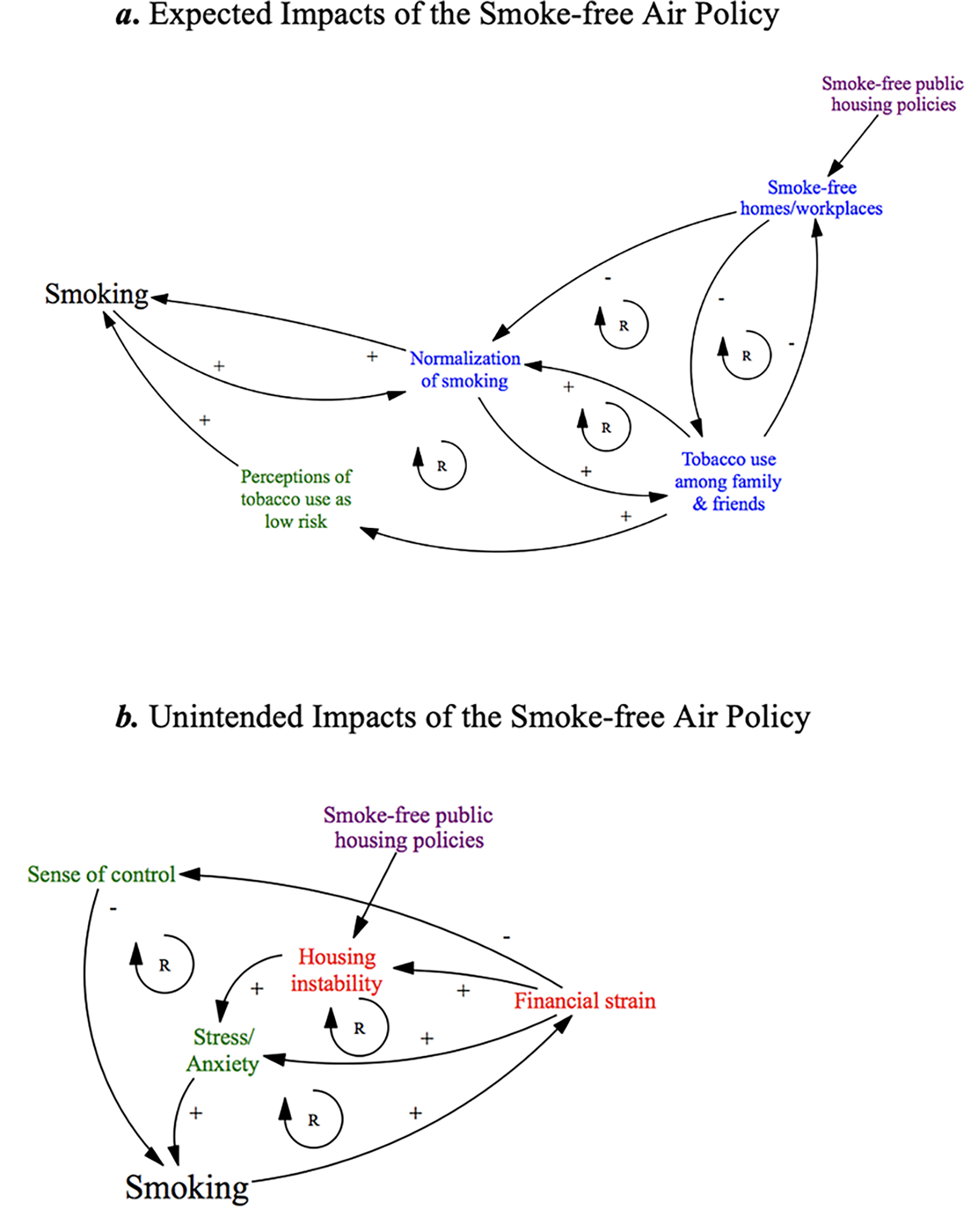
The expected impacts of the smoke-free air policy
On the other hand, it is likely that some public housing residents who smoke may violate the smoke-free air policy, especially considering tobacco’s addictive properties. Violation of the policy may lead to threats of housing instability, which increases financial strain and stress and simultaneously reduces feelings of control, thus having the unintended consequence of increasing smoking, and leaving residents at further risk of housing instability. Relationships among these constructs are reinforcing, as indicated in Figure 3b.
Menthol cigarette ban.
The Food and Drug Administration has regulatory authority over cigarettes and is considering implementing a menthol cigarette ban.[52] Menthol cigarettes are used by more than one-third (39%) of smokers in the US.[53] Due to a history of targeted marketing, menthol cigarettes are disproportionately used among racial/ethnic minority and lower-income smokers.[43] The CLD indicates that a menthol cigarette ban should reduce tobacco use because a portion of menthol cigarette smokers are expected to quit if they no longer have access to their preferred product. On the other hand, the CLD suggests that neighborhood segregation and discrimination allow for the tobacco industry to continue targeted marketing of other tobacco products, likely undermining impacts.
Minimum floor price laws (MFPLs).
MFPLs, which set a floor price below which a tobacco product cannot be sold,[54] have recently been implemented by several cities and counties.[55] Different from other price policies like excise taxes, MFPLs raise prices on the cheapest products the most.[54] If low-income smokers pay less for their cigarettes and tobacco prices are cheaper in predominantly African American or lower-income neighborhoods, as research suggests,[56–58] lower-income and African American populations stand to gain the most health benefits from MFPLs through the price-focused loop. The CLD suggests, however, that higher prices might also trigger the financial strain loop and increase smoking, particularly in the absence of effective cessation supports.
Discussion
This study presents a diagram of smoking that can be used to better understand factors associated with smoking among racial/ethnic minority and lower-income groups. Existing theoretical models of smoking fail to consider root causes (e.g., segregation) of individual (e.g., stress) and environmental (e.g., tobacco marketing) variables that may disproportionately affect smoking for priority populations. This study extends current theoretical models of smoking to also include factors that are root causes of disparities in smoking facing populations at increased risk.
In the CLD, the two constructs that had the most arrows leaving from them were structural racism (n=7) and tobacco companies’ profit maximization efforts (n=6). These two constructs may play critical roles in shaping several factors that directly increase the likelihood of smoking. Stress/anxiety, normalization of smoking, and product and flavor availability were the constructs with the most arrows pointing to them (each with 5 arrows). This suggests that these factors are critical to smoking prevalence and may be particularly difficult to modify. Researchers and public health and medical organizations have called for explicit recognition of the role fundamental factors such as structural racism and discrimination play in health behaviors like smoking.[59–61] Grier et al. noted that discussion of race makes many scholars uneasy and topics like racism go ignored.[17] This CLD calls attention to the pervasiveness of structural racism, low-wage work, and other fundamental factors of smoking disparities.
The CLD can be used to inform the development and evaluation of interventions focused on reducing racial/ethnic and socioeconomic disparities in smoking. Tobacco control interventions are often evaluated in isolation. The CLD may be particularly useful for considering the potential impacts of implementing multiple tobacco control interventions simultaneously or of adapting interventions to increase impact in a given context. The CLD may help elucidate how multi-level (e.g., individual- and root cause-levels) interventions work in potentially cumulative or synergistic ways to product their effects.[62, 63] In addition, many researchers and organizations have called attention to the potential unintended consequences of several tobacco control interventions and have suggested approaches to counter such outcomes.[64–66] For example, readily accessible cessation aids have been recommended for residents of smoke-free public housing.[65] The CLD can be used to systematically examine modifications to existing interventions and to assess whether these changes strengthen desired change and dampen potential undesired consequences.
Although the CLD contains several factors important to smoking, the model should not be considered exhaustive. Instead, the diagram can be a starting point for those interested in using causal loop diagramming to better understand factors associated with smoking in their own community. We designed the CLD to be appropriate for the general US context, but important next steps will include tailoring this model to be appropriate for specific contexts and populations through additional research and community engagement efforts. Through our interviews, we found that diverse stakeholders in this field found the CLD useful in initiating these discussions and considering the intersections between variables affecting smoking.
The CLD also provides insights into the stakeholders needed in tobacco control to effectively reduce demographic disparities in smoking. Traditional stakeholders in tobacco control, like government representatives, academic researchers/practitioners, and tobacco control advocacy groups, may be insufficient to comprehensively address disparities. Other stakeholder perspectives, like housing officials, social service agencies, and mental health practitioners, could help ensure policies reduce demographic disparities in smoking and do not further burden priority populations. Mental health practitioners, for example, can provide support with stress management and inform how and when mental health services may be needed in the context of policy change.
This study has limitations. Use of convenience sampling restricted the group of stakeholders interviewed. Future efforts should include obtaining feedback from more smokers, community members, and cross-sector community-based organizations that work outside of tobacco control. In addition, the CLD was focused on racial/ethnic and socioeconomic disparities in smoking. There may be additional fundamental causes that should be considered when examining factors associated with smoking in other populations with high smoking rates. An assets-based approach may be useful for leveraging strengths of groups with high smoking rates.
This study provides a useful tool that can support continued research and related efforts to reduce smoking prevalence overall and in populations currently shouldering the burden of tobacco use and related disease. By tailoring the CLD developed in this study to specific goals, populations, or contexts, there are opportunities to design, test, and improve tobacco control interventions and policies. For example, interviews, focus groups, and other types of community engagement can be used to obtain feedback from community members and stakeholders about the feasibility, acceptability, and expected impact of tobacco control interventions using the CLD. Further research is needed to test and quantify the relationships hypothesized in our CLD; estimating these associations may provide guidance into where to prioritize limited resources. Finally, our model of smoking can be used to inform quantitative system dynamics models and other systems approaches to tobacco control, providing additional insight into the complex relationships between individual, environmental, and fundamental factors contributing to disparities in smoking.
Supplementary Material
What is already known on this subject?
Although there are evidence-based strategies for reducing overall smoking prevalence rates, it is less clear how to reduce racial/ethnic and socioeconomic disparities in smoking.
What important gaps in knowledge exist on this topic?
Existing theoretical models of smoking fail to consider root causes (e.g., segregation) of individual (e.g., stress) and environmental (e.g., tobacco marketing) variables that may disproportionately affect smoking for priority population groups.
What this study adds.
This study extends current theoretical models of smoking to also include factors that are root causes of disparities in smoking facing racial/ethnic minority and lower-income adults. This study provides a useful tool that can support identification of non-traditional partners and approaches for tobacco control.
Footnotes
Competing Interests
Dr. Sarah Mills, Dr. Shelley Golden, Meghan O’Leary, and Dr. Kristen Hassmiller Lich receive funding from the National Institutes of Health (NIH). Dr. Mills also receives funding from the Food and Drug Administration (FDA) Center for Tobacco Products. Dr. Lich also receives funding from the Centers for Disease Control and Prevention (CDC) and the Health Resources and Services Administration (HRSA). Paige Logan declares no potential conflict of interest. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, CDC, HRSA or the FDA.
References
- [1].Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults - United States, 2018. MMWR Morb Mortal Wkly Rep 2019;68(45):1013–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Mills SD, Golden SD, Queen TL, et al. Are state-level income-based disparities in adult smoking declining? Prev Med 2020;133:106019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Drope J, Liber AC, Cahn Z, et al. Who’s still smoking? Disparities in adult cigarette smoking prevalence in the United States. CA Cancer J Clin 2018;68(2):106–15. [DOI] [PubMed] [Google Scholar]
- [4].King BA, Graffunder C. The Tobacco Control Vaccine: a population-based framework for preventing tobacco-related disease and death. Tob Control 2018;27(2):123–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].National Cancer Institute. Greater than the sum: Systems thinking in tobacco control. Tobacco Control Monograph No. 18. 2007. https://cancercontrol.cancer.gov/brp/tcrb/monographs/monograph-18 (accessed August 4 2021). [Google Scholar]
- [6].Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health 2008;98(2):216–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav 1995:80–94. [PubMed] [Google Scholar]
- [8].Phelan JC, Link BG, Tehranifar P. Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications. Journal of Health and Social Behavior 2010;51(1_suppl):S28–S40. [DOI] [PubMed] [Google Scholar]
- [9].Phelan JC, Link BG. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol 2015;41(1):311–30. [Google Scholar]
- [10].Williams DR, Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Rep 2001;116(5):404–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health 2013;103(5):813–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Aneshensel CS. Social stress: Theory and research. Annu Rev Sociol 1992;18(1):15–38. [Google Scholar]
- [13].Meyer IH, Schwartz S, Frost DM. Social patterning of stress and coping: Does disadvantaged social statuses confer more stress and fewer coping resources? Soc Sci Med 2008;67(3):368–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Dressler WW, Oths KS, Gravlee CC. Race and ethnicity in public health research: models to explain health disparities. Annu Review Anthropol 2005;34(1):231–52. [Google Scholar]
- [15].Ford CL, Airhihenbuwa CO. Critical race theory, race equity, and public health: Toward antiracism praxis. Am J Public Health 2010;100(S1):S30–S35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Poole SM, Grier SA, Thomas KD, et al. Operationalizing critical race theory in the marketplace. J Public Policy Mark 2020;40(2):126–42. [Google Scholar]
- [17].Grier SA, Thomas KD, Johnson GD. Re-imagining the marketplace: Addressing race in academic marketing research. Consump Mark & Cult 2019;22(1):91–100. [Google Scholar]
- [18].Mabry PL, Olster DH, Morgan GD, et al. Interdisciplinarity and systems science to improve population health: A view from the NIH Office of Behavioral and Social Sciences Research. Am J Prev Med 2008;35(2, Supplement):S211–S24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Hassmiller Lich K, Frerichs L, Fishbein D, et al. Translating research into prevention of high-risk behaviors in the presence of complex systems: Definitions and systems frameworks. Transl Behav Med 2016;6(1):17–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Richardson GP. Problems in causal loop diagrams revisited. Sys Dyn Rev 1997;13(3):247–52. [Google Scholar]
- [21].Sadler GR, Lee H, Lim RS, et al. Recruitment of hard-to-reach population subgroups via adaptations of the snowball sampling strategy. Nurs Health Sci 2010;12(3):369–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Benowitz NL. Pharmacology of nicotine: Addiction, smoking-induced disease, and therapeutics. Ann Rev Pharmicol Toxicol 2009;49(1):57–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kaufman AR, Dwyer LA, Land SR, et al. Smoking-related health beliefs and smoking behavior in the National Lung Screening Trial. Addict Behav 2018;84:27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Rutten LJF, Augustson EM, Moser RP, et al. Smoking knowledge and behavior in the United States: Sociodemographic, smoking status, and geographic patterns. Nicotine Tob Res 2008;10(10):1559–70. [DOI] [PubMed] [Google Scholar]
- [25].Gardiner P, Clark PI. Menthol cigarettes: Moving toward a broader definition of harm. Nicotine Tob Res 2010;12(suppl_2):S85–S93. [DOI] [PubMed] [Google Scholar]
- [26].Wickham RJ. The biological impact of menthol on tobacco dependence. Nicotine Tob Res 2020;22(10):1676–84. [DOI] [PubMed] [Google Scholar]
- [27].Heishman SJ. Behavioral and cognitive effects of smoking: Relationship to nicotine addiction. Nicotine Tob Res 1999;1(Suppl_2):S143–S47. [DOI] [PubMed] [Google Scholar]
- [28].Kassel JD, L S, Paronis CA. Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychol Bull 2003;129(2):270–304. [DOI] [PubMed] [Google Scholar]
- [29].Segall ME, Wynd CA. Health conception, health locus of control, and power as predictors of smoking behavior change. Am J Health Promot 1990;4(5):338–44. [DOI] [PubMed] [Google Scholar]
- [30].Robertson L, McGee R, Marsh L, et al. A systematic review on the impact of point-of-sale tobacco promotion on smoking. Nicotine Tob Res 2015;17(1):2–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].National Cancer Institute, World Health Organization. The Economics of Tobacco and Tobacco Control 2017. https://cancercontrol.cancer.gov/brp/tcrb/monographs/monograph-21 (accessed August 4 2021).
- [32].Golden SD, Kuo M, Kong AY, et al. County-level associations between tobacco retailer density and smoking prevalence in the USA, 2012. Prev Med Reports 2020;17:101005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Novak SP, Reardon SF, Raudenbush SW, et al. Retail tobacco outlet density and youth cigarette smoking: A propensity-modeling approach. Am J Public Health 2006;96(4):670–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Karasek D, Ahern J, Galea S. Social norms, collective efficacy, and smoking cessation in urban neighborhoods. Am J Public Health 2011;102(2):343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Cummings KM, Fong GT, Borland R. Environmental influences on tobacco use: Evidence from societal and community influences on tobacco use and dependence. Annu Rev Clin 2009;5(1):433–58. [DOI] [PubMed] [Google Scholar]
- [36].Gollust SE, Schroeder SA, Warner KE. Helping Smokers Quit: Understanding the Barriers to Utilization of Smoking Cessation Services. Milbank Q 2008;86(4):601–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].U.S. Department of Health and Human Services. Appendix 15.1 Tobacco Control Simulation Models. 2014. https://www.hhs.gov/sites/default/files/consequences-smoking-appendix15-1-tobacco-control-simulation-models.pdf (accessed August 4 2021).
- [38].Yang Y A narrative review of the use of agent-based modeling in health behavior and behavior intervention. Transl Behav Med 2019;9(6):1065–75. [DOI] [PubMed] [Google Scholar]
- [39].Schaefer DR, Adams J, Haas SA. Social Networks and Smoking: Exploring the Effects of Peer Influence and Smoker Popularity Through Simulations. Health Educ Behav 2013;40(1_suppl):24S–32S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Hammond RA, Combs TB, Mack-Crane A, et al. Development of a computational modeling laboratory for examining tobacco control policies: Tobacco Town. Health Place 2020;61:102256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Houle B, Siegel M. Smoker-free workplace policies: developing a model of public health consequences of workplace policies barring employment to smokers. Tob Control 2009;18(1):64–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Burgard SA, Seefeldt KS, Zelner S. Housing instability and health: Findings from the Michigan Recession and Recovery Study. Soc Sci Med;75(12):2215–24. [DOI] [PubMed] [Google Scholar]
- [43].Yerger VB, Przewoznik JF, Malone RE. Racialized geography, corporate activity, and health disparities: Tobacco industry targeting of inner cities. J Health Care Poor Underserved 2007;18 (4 Suppl):10–38. [DOI] [PubMed] [Google Scholar]
- [44].Petty RD, Harris A-MG, Broaddus T, et al. Regulating target marketing and other race-based advertising practices. Michigan J Race & L 2003;8(2):335–94. [Google Scholar]
- [45].Ahern J, Galea S, Hubbard A, et al. Neighborhood smoking norms modify the relation between collective efficacy and smoking behavior. Drug Alcohol Depend 2009;100(1):138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Lee JGL, Sun DL, Schleicher NM, et al. Inequalities in tobacco outlet density by race, ethnicity and socioeconomic status, 2012, USA: Results from the ASPiRE Study. J Epid Community Health 2017;71(5):487–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Duncan DT, Kawachi I, Melly SJ, et al. Demographic disparities in the tobacco retail dnvironment in Boston: A citywide spatial analysis. Public Health Rep 2014;129(2):209–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Fakunle D, Morton CM, Peterson NA. The importance of income in the link between tobacco outlet density and demographics at the tract level of analysis in New Jersey. J Ethn Subst 2010;9(4):249–59. [DOI] [PubMed] [Google Scholar]
- [49].Loomis BR, Kim AE, Goetz JL, et al. Density of tobacco retailers and its association with sociodemographic characteristics of communities across New York. Public Health 2013;127(4):333–38. [DOI] [PubMed] [Google Scholar]
- [50].Mayers RS, Wiggins LL, Fulghum FH, et al. Tobacco outlet density and demographics: A geographically weighted regression analysis. Prev Sci 2012;13(5):462–71. [DOI] [PubMed] [Google Scholar]
- [51].US Department of Housing and Urban Development. Implementing HUD’s smoke-free policy in public housing: HUD Guidebook. http://www.nahro.org/sites/default/files/searchable/HUD%20Smoke-Free%20Guidebook.pdf (accessed August 4 2021).
- [52].Villanti AC, Vargyas EJ, Niaura RS, et al. Food and Drug Administration regulation of tobacco: Integrating science, law, policy, and advocacy. Am J Public Health 2011;101(7):1160–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Villanti AC, Mowery PD, Delnevo CD, et al. Changes in the prevalence and correlates of menthol cigarette use in the USA, 2004–2014. Tob Control 2016;25(Suppl 2):ii14–ii20. [DOI] [PubMed] [Google Scholar]
- [54].Golden SD, Smith MH, Feighery EC, et al. Beyond excise taxes: A systematic review of literature on non-tax policy approaches to raising tobacco product prices. Tob Control 2016;25(4):377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Minimum Floor Price Laws. http://changelabsolutions.org/sites/default/files/MFPL_UNC_FactSheet_FINAL_20190130.pdf (accessed August 4 2021).
- [56].Lee JG, Henriksen L, Rose SW, et al. A systematic review of neighborhood disparities in point-of-sale tobacco marketing. Am J Public Health 2015;105(9):e8–e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Mills SD, Henriksen L, Golden SD, et al. Disparities in retail marketing for menthol cigarettes in the United States, 2015. Health Place 2018;53:62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Golden SD, Kong AY, Ribisl KM. Racial and ethnic differences in what smokers report paying for their cigarettes. Nicotine Tob Res 2016;18(7):1649–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Pearson JL, Waa A, Siddiqi K, et al. Naming racism, not race, as a determinant of tobacco-related health disparities. Nicotine Tob Res 2021;23(6):885–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Churchwell K, Elkind MSV, Benjamin RM, et al. Call to action: Structural racism as a fundamental driver of health disparities. Circulation 2020;142:e454–e68. [DOI] [PubMed] [Google Scholar]
- [61].Society of Research on Nicotine and Tobacco. SRNT is Committed to Anti-Racism and Social Justice through Research and Action. https://cdn.ymaws.com/www.srnt.org/resource/resmgr/society_news/srnt_statement_on_antiracis.pdf (accessed August 4 2021)
- [62].Sussman S, Levy D, Lich KH, et al. Comparing effects of tobacco use prevention modalities: need for complex system models. Tob Induc Dis 2013;11(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Weiner BJ, Lewis MA, Clauser SB, et al. In search of synergy: Strategies for combining interventions at multiple levels. JNCI Monographs 2012;2012(44):34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Hirono KT, Smith KE. Australia’s $40 per pack cigarette tax plans: the need to consider equity. Tob Control 2018;27(2):229–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Public Health Law Center. Smoke-free Multi-unit Housing: Equitable Enforcement Strategies. 2020. https://www.publichealthlawcenter.org/resources/smoke-free-multi-unit-housing-equitable-enforcement-strategies-2020 (accessed August 4 2021).
- [66].Greaves L, Johnson J, Bottorff J, et al. What are the effects of tobacco policies on vulnerable populations? A better practices review. Can J Public Health 2006;97(4):310–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


