Abstract
Objective
To examine the association of physician burnout with the career engagement and the quality of patient care globally.
Design
Systematic review and meta-analysis.
Data sources
Medline, PsycINFO, Embase, and CINAHL were searched from database inception until May 2021.
Eligibility criteria for selecting studies
Observational studies assessing the association of physician burnout (including a feeling of overwhelming emotional exhaustion, feelings of cynicism and detachment from job defined as depersonalisation, and a sense of ineffectiveness and little personal accomplishment) with career engagement (job satisfaction, career choice regret, turnover intention, career development, and productivity loss) and the quality of patient care (patient safety incidents, low professionalism, and patient satisfaction). Data were double extracted by independent reviewers and checked through contacting all authors, 84 (49%) of 170 of whom confirmed their data. Random-effect models were used to calculate the pooled odds ratio, prediction intervals expressed the amount of heterogeneity, and meta-regressions assessed for potential moderators with significance set using a conservative level of P<0.10.
Results
4732 articles were identified, of which 170 observational studies of 239 246 physicians were included in the meta-analysis. Overall burnout in physicians was associated with an almost four times decrease in job satisfaction compared with increased job satisfaction (odds ratio 3.79, 95% confidence interval 3.24 to 4.43, I2=97%, k=73 studies, n=146 980 physicians). Career choice regret increased by more than threefold compared with being satisfied with their career choice (3.49, 2.43 to 5.00, I2=97%, k=16, n=33 871). Turnover intention also increased by more than threefold compared with retention (3.10, 2.30 to 4.17, I2=97%, k=25, n=32 271). Productivity had a small but significant effect (1.82, 1.08 to 3.07, I2=83%, k=7, n=9581) and burnout also affected career development from a pooled association of two studies (3.77, 2.77 to 5.14, I2=0%, n=3411). Overall physician burnout doubled patient safety incidents compared with no patient safety incidents (2.04, 1.69 to 2.45, I2=87%, k=35, n=41 059). Low professionalism was twice as likely compared with maintained professionalism (2.33, 1.96 to 2.70, I2=96%, k=40, n=32 321), as was patient dissatisfaction compared with patient satisfaction (2.22, 1.38 to 3.57, I2=75%, k=8, n=1002). Burnout and poorer job satisfaction was greatest in hospital settings (1.88, 0.91 to 3.86, P=0.09), physicians aged 31-50 years (2.41, 1.02 to 5.64, P=0.04), and working in emergency medicine and intensive care (2.16, 0.98 to 4.76, P=0.06); burnout was lowest in general practitioners (0.16, 0.03 to 0.88, P=0.04). However, these associations did not remain significant in the multivariable regressions. Burnout and patient safety incidents were greatest in physicians aged 20-30 years (1.88, 1.07 to 3.29, P=0.03), and people working in emergency medicine (2.10, 1.09 to 3.56, P=0.02). The association of burnout with low professionalism was smallest in physicians older than 50 years (0.36, 0.19 to 0.69, P=0.003) and greatest in physicians still in training or residency (2.27, 1.45 to 3.60, P=0.001), in those who worked in a hospital (2.16, 1.46 to 3.19, P<0.001), specifically in emergency medicine specialty (1.48, 1.01 to 2.34, P=0.042), or situated in a low to middle income country (1.68, 0.94 to 2.97, P=0.08).
Conclusions
This meta-analysis provides compelling evidence that physician burnout is associated with poor function and sustainability of healthcare organisations primarily by contributing to the career disengagement and turnover of physicians and secondarily by reducing the quality of patient care. Healthcare organisations should invest more time and effort in implementing evidence-based strategies to mitigate physician burnout across specialties, and particularly in emergency medicine and for physicians in training or residency.
Systematic review registration
PROSPERO number CRD42021249492.
Introduction
Burnout is defined as a syndrome related to work that involves three key dimensions. Firstly, emotional exhaustion, which represents the basic individual stress dimension of burnout and refers to feelings of being overextended and depleted of emotional and physical resources. Secondly, depersonalisation, which is the cynicism component and represents a motivational, interpersonal distancing dimension of burnout and refers to a negative, callous, or excessively detached response to various aspects of the job. Finally, a sense of reduced personal accomplishment, which represents the self-evaluation dimension of burnout and refers to feelings of incompetence and inadequate achievement and productivity at work.1 Burnout is rampant and reaching global levels among physicians.2 In the US, four in 10 physicians report at least one symptom of burnout,3 and in the UK, a third of trainee doctors report that they experience burnout to a high or very high degree.4 In a recent review of low and middle income countries the overall single-point prevalence of burnout ranged from 2.5% to 87.9% among 43 studies.5 Moreover, the covid-19 pandemic has created new causes for stress with unsafe working conditions and higher workloads, which have further exacerbated burnout in physicians.6 7
Physicians with burnout often report poor work-life balance and career dissatisfaction.8 9 However, previous systematic reviews that focused on the potential effects of physician burnout on healthcare efficiency have overlooked the association of burnout with career engagement of physicians. Healthcare provider burnout was associated with lower quality patient care in a recent systematic review.10 However, no pooled estimates of these associations were provided due to high heterogeneity, which was partly caused by analysing mixed samples of healthcare providers and studies with little to no flexibility of the quality metrics used for patient outcome subgroups.
A joint synthesis of the links of physician burnout with the career engagement of physicians and the quality of care provided to patients is important because these aspects are complementary of the overall efficiency of healthcare organisations according to existing theoretical frameworks and research evidence.11 12 13 These reciprocal relations should be made available to governments and policy organisations to encourage financial investments and policies to mitigate physician burnout internationally. No previous systematic reviews has taken this approach.14 15 16 For instance, a meta-analysis published in 2022 that assessed the association of burnout with only self-reported medical errors among physicians found an increased risk of self-reported errors.16 Two further systematic reviews,14 15 which assessed the association between physician or healthcare professionals’ wellbeing and burnout with patient safety, did so through a narrative review approach due to large heterogeneity.
Therefore, we aimed to add value through a larger and more robust meta-analysis that controlled for heterogeneity and other possible biases in career engagement (which is currently unknown at the systematic review level) and quality-of-care outcomes. In this systematic review and meta-analysis, we examined the association of physician burnout with the career engagement of physicians focusing on job satisfaction, career choice regret, career development, productivity loss and turnover intention; and the quality of patient care focusing on patient safety incidents, low professionalism, and patient satisfaction. Based on existing frameworks that have studied the relation between occupational distress and impairment related to sleep deprivation in physicians and unsolicited patient complains,13 a flow diagram of the anticipated associations is presented in figure 1. We also conducted meta-regressions to uncover important moderators of these associations.
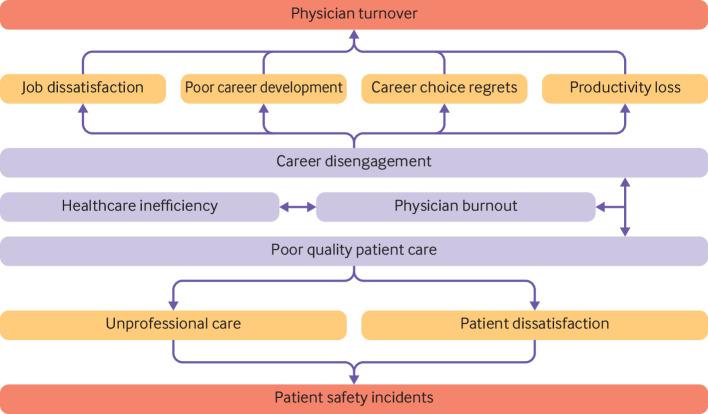
Fig 1.
Flow diagram of examined associations of physician burnout with career engagement and quality of patient care. Outcomes assessed in the analysis are in yellow or red. Outcomes in red emphasise the potential heightened risk of the outcome compared with the outcomes in yellow (which could be less serious to the physician and healthcare system
Methods
This systematic review followed a registered (PROSPERO CRD42021249492) protocol17 and is reported in accordance with the Reporting Checklist for Meta-analyses of Observational Studies (MOOSE)18 and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance.19 A protocol amendment was made in November 2021 to exclude grey literature from this review. The completed checklists are available in appendix 1.
Search strategy and study eligibility
We included quantitative observational studies involving physicians working in any healthcare setting. We reported comparative data on the association between burnout and career engagement of physicians (ie, job satisfaction, career choice regret, turnover intention, reduced productivity indicated by presenteeism or absenteeism, and career development) and quality of patient care outcomes (ie, patient safety incidents including medication errors, suboptimal patient care due to low professionalism based on an established definition,20 and patient satisfaction). Definitions for each of the outcomes are provided in appendix 2. Studies that did not report their sample had this missing information confirmed by contacting authors. Randomised controlled trials were excluded because our study focus is on associations and not interventions, qualitative studies and quantitative studies involving fewer than 70% of responses from physicians were also excluded. This 70% threshold is an arbitrary criterion that we have used in previous reviews in this area.21 The reason we adopted this criterion is because we did not want to exclude relevant studies that included only a small number of other health professionals in addition to physicians.
We searched Medline, PsycINFO, Embase, and CINAHL from database inception to May 2021 for citations in English. The searches included combinations of key blocks of terms involving Medical Subject Headings terms and text words. The full search strategies are detailed in the appendix 3. The reference lists of relevant systematic reviews and eligible studies were manually searched to identify additional literature.
Two independent reviewers (AH and AZ or MP and AZ) rated the eligibility of each of the abstracts and full texts in Covidence.22 Disagreements were resolved by consensus, and we measured inter-rater agreement with the κ statistic.
Data extraction and quality assessment
Using a standardised form that was pilot tested, we extracted data for study characteristics (country, recruitment, healthcare setting, and design), physician characteristics (sample size, mean age, sex (percentage of men), specialty, and work experience), burnout (measure characteristics) and the outcome measures including the method of reporting. The outcomes of interest were each assessed against overall burnout and any of the three subscales of burnout including emotional exhaustion, depersonalisation, and personal accomplishment. Where all three subscales were reported and the overall burnout score was not, we calculated burnout by pooling across the three subscale scores. We transformed extracted quantitative data to the uniform log scale and standardised mean difference using the statistical software Comprehensive Meta-Analysis.23 The formulae for these transformations are provided in appendix 4. One of six reviewers (AH, MP, JJ, KG, RR, and AZ) completed data extractions and double checked with any disagreements being resolved by consensus.
We emailed all the study authors to confirm the accuracy and validity of their data and to obtain any missing data. 84 (49%) of 170 of the study authors confirmed their data and our extractions were found to be accurate in 96% of these studies (appendix 5).
The Newcastle Ottawa critical appraisal tool was used to assess the quality of the studies.24 Pairs of reviewers in three groups (AH and AZ, MP and KG, or JJ and RR) appraised the fundamental criteria: (1) representativeness of the sample, (2) sample size, (3) non-respondents, (4) ascertainment of the exposure, (5) controlled for confounding factors, (6) assessment of outcome, and (7) adequate statistical tests. Explanations of how each variable was coded is detailed in the appendix. The total maximum score was 7, and we classified overall scores of 0-2 as high risk, 3-5 as medium risk, and 6-7 as low risk.
Data synthesis
We used DerSimonian-Laird random effects while pooling the log odds,25 then exponentiated these results to odds ratio and presented the data in forest plots. A fixed effect method of pooling was considered in meta-analysis with fewer than five studies and varied sample and effect sizes. Heterogeneity in the meta-analysis was quantified using the I2 statistic with its 95% confidence intervals.26 Because of the high level of heterogeneity, Hartung-Knapp method of pooling and estimating 95% confidence intervals were used to account for uncertainty in the variance estimate.27 Overall burnout and its three subscales (emotional exhaustion, depersonalisation, and personal accomplishment) were synthesised individually and presented as so within the forest plots. In total, 32 possible meta-analysis comparisons were found. A subgroup meta-analysis was performed to assess for differences between the four burnout measures (full 22-item Maslach Burnout Inventory, abbreviated (shortened) version of the Maslach Burnout Inventory, Copenhagen burnout inventory, and use of another inventory). Differences between these groups were assessed using the statistic ratio of odds ratio.28 In a meta-analysis involving 10 or more studies, funnel plots and Egger’s test were used to assess for publication bias,29 and prediction intervals were calculated to express the amount of heterogeneity.30
We used univariable and multivariable meta-regressions using the following variables: region (US, UK/European Union, Commonwealth, South East Asia/other); setting (primary care, hospital, mixed); design (cross sectional, prospective cohort or longitudinal); age (≤30, 31-50, and ≥51 years); sex (female, male, mixed); specialty or position of profession ((1) physician or internal medicine, (2) general practitioners (GPs), (3) surgery including neurosurgery, (4) emergency medicine and intensive care, (5) cancer or oncology, (6) intern or resident, (7) paediatrics, (8) psychiatry, (9) mixed, (10) neurology, and (11) other); work experience (experienced with over 6 years, less experienced intern/resident ≤6 years, mixture of experience), and burnout measure (Maslach Burnout Inventory, any iteration,31 or other classified burnout inventory v mixed and other32). Variables from the univariable regressions with a more conservative level of significance of P<0.10 rather than p<0.05 were used in the multivariable model.33 The variables were added by using forward selection process.34 Sensitivity analyses for risk of bias was done based on the three categories for the total score of the Newcastle Ottawa assessment (low, medium, and high). All meta-analyses were conducted in R version 4.0.5 (R Foundation for Statistical Computing)35 using the meta36 and metafor37 packages.
Patient and public involvement
We consulted five GPs in the Greater Manchester region who were members of an established patient and public involvement group about the appropriateness of our research questions and classification of outcomes and appropriateness of wellbeing measures used. These GPs also advised on the interpretation of our findings and will help with the dissemination strategy.
Results
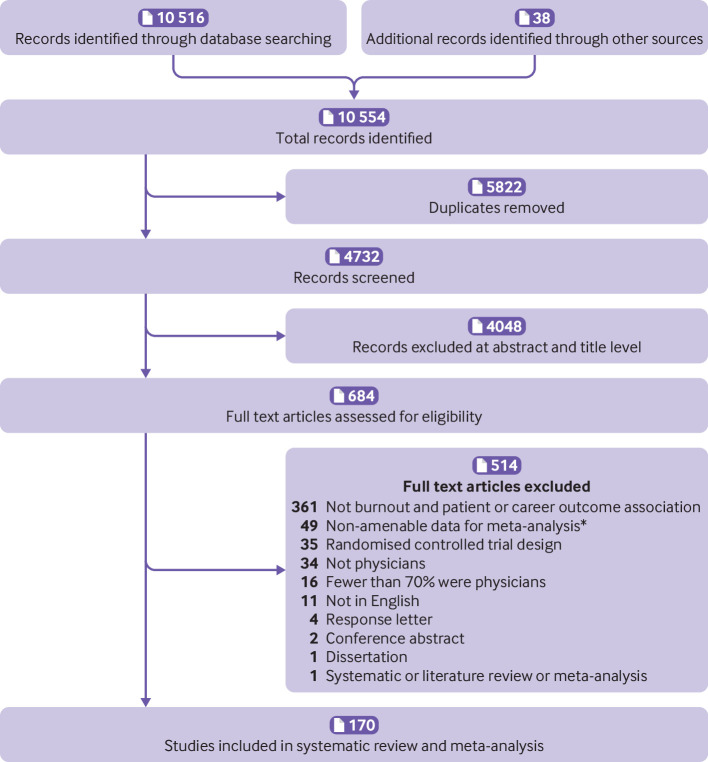
Our search strategy identified 4732 articles, of which 684 met the criteria for full text review (fig 2). A total of 170 studies involving 239 246 physicians (150 cross sectional studies including 231 964 physicians and 20 prospective or longitudinal studies including 7282 physicians) met the eligibility criteria. The characteristics of the included studies are summarised in appendix 6, and citations are provided in appendix 7. Agreement between reviewers for study inclusion was high (κ 0.89, 95% confidence interval 0.81 to 0.96).
Fig 2.
Study selection. *See references in appendix 6
Study characteristics
77 (45%) of the 170 studies were conducted in the US, 48 (28%) in European countries, four (2%) of which were in the UK two (1%) in the African Region, eight (5%) in the Region of the Americas, two (1%) in the South-East Asian Region, three (2%) in the Eastern Mediterranean Region, 29 (17%) in the Western Pacific Region, and one (1%) multinational study.38 39 40 41 42 43 44 107 (63%) of the studies were based in a hospital setting, 33 (19%) involved mixed settings, 29 (17%) were based in primary care setting, and one study45 was unclear but involved medically qualified academics. We aimed to exclude studies with fewer than 70% of responses from physicians, however, in reality, only three (2%) of 170 studies with a mixed sample of physicians (70% and over) and other health professionals were included in our analyses.
The median number of physicians across studies was 312 (interquartile range 162-1015 ) with a median age of 42 years (32-48) and where data for sex were reported, 112 (66%) studies involved mostly male physicians. The physician specialty varied across studies: 42 (25%) mixed specialties, 32 (19%) internal medicine, 21 (12%) surgery (ie, trauma, plastic, and neurosurgical), 19 (11%) emergency medicine and intensive care, 11 (6%) general practitioners, eight (5%) interns or residents, eight (5%) paediatrics, seven (4%) oncology (ie, gynaecologist, radiation, or palliative care), six (4%) neurology, three (2%) psychiatry, and 13 (8%) involving other specialties. Physicians had more than seven years of experience in 52 (31%) studies, a mixture of experience was reported in 47 (28%) studies, and 38 (22%) studies involved residents, junior doctors, or interns with fewer than seven years of experience.
The most common measure of burnout was the full 22-item Maslach Burnout Inventory (81 (48%) of 170 studies). An abbreviated version of the Maslach Burnout Inventory was used in 50 (29%) studies, other types were used in 34 (20%) studies and only five (3%) studies used the Copenhagen burnout inventory (see appendix 8 in supplement for breakdown of the measures used). Thirty one (18%) studies reported secondary measures of depression and 24 (14%) studies reported emotional distress, which were analysed separately. In terms of career engagement for physicians, 81 (48%) studies reported on decreased job satisfaction compared with increased job satisfaction, 19 (11%) on career choice regret compared with being satisfied with career choice, three (2%)42 46 47 48 poor career development compared with good career development, nine (5%)47 49 50 51 52 53 54 55 56 57 58 59 on reduced productivity compared with sustained productivity, and 36 (21%) on turnover intention compared with retention. Concerning quality of patient care outcomes, 39 (23%) studies reported patient safety incidents compared with no patient safety incidents, 43 (25%) reported indicators of low professionalism compared with maintained professionalism, and eight (5%) studies reported measures of patient dissatisfaction compared with satisfied patients. Nineteen (11%) studies reported more than one of these outcomes.
Of the 119 (70%) studies reporting career engagement, all were self-reported by the physician. Physicians self-reported across most of the studies for patient safety incidents (31 (79%) of 39) and professionalism (37 (80%) of 46 studies), whereas the remaining studies used patient record reviews and surveillance systems. Patient satisfaction was based on self-reports by patients.
Quality assessment
One hundred and 30 studies provided a representative sample of the target population (76% met criterion 1); 103 studies provided an ample sample size of physicians (61% met criterion 2); 58 studies reported a response rate of 60% or greater (34% met criterion 3); 25 studies satisfied low risk of bias for the ascertainment of exposure mostly due to many of the surveys being self-reported (15% met criterion 4); 100 of the studies adequately adjusted for confounding factors (59% met criterion 5); 165 reported a low risk of bias due to assessment of outcome (97% met criterion 6); and 118 studies had used adequate statistical tests and measures to report their findings (69% met criterion 7). Overall, 32 (19%) of the studies reported low risk of bias (total score 6-7), 23 (14%) reported high risk of bias (total score: 0-2), and 115 (67%) studies reported medium risk of bias (total score 3-5). The full results of the Newcastle Ottawa critical appraisals are presented in appendix 9.
Meta-analysis of association of burnout with career engagement and quality of patient care
The results of all the meta-analyses are provided in table 1. All forest plots for each outcome are available in appendix 10. Only significant results are reported here.
Table 1.
Meta-analysis of the association of burnout with outcomes based on the career engagement of physicians and quality of patient care
| Burnout and submeasure | No of studies (No of physicians) | Direction of association | Odds ratio (95% CI); (95% PI) | I2 (95% CI) | Publication bias† |
|---|---|---|---|---|---|
| Career engagement of physicians | |||||
| Career choice regret: | |||||
| Burnout | 16 (33 871) | Favours career choice regret compared with being satisfied with their career choice | 3.49 (2.43 to 5.00); (0.90 to 13.49) | 97 (96 to 98) | P=0.004 |
| Emotional exhaustion* | 4 (2014) | 4.16 (3.34 to 5.19) | 90 (77 to 95) | NA | |
| Depersonalisation* | 2 (274) | 1.54 (0.97 to 2.45) | 65 (0 to 92) | NA | |
| Personal accomplishment* | 1 (147) | 1.12 (0.36 to 3.48) | NA | NA | |
| Career development: | |||||
| Burnout* | 2 (3411) | Favours negative career development compared with positive career development | 3.77 (2.77 to 5.14) | 0 | NA |
| Emotional exhaustion* | 1 (593) | 1.08 (0.80 to 1.44) | NA | NA | |
| Depersonalisation* | 1 (593) | 1.12 (0.83 to 1.49) | NA | NA | |
| Personal accomplishment | No data | No data | No data | NA | |
| Job satisfaction: | |||||
| Burnout | 73 (146 980) | Favours decreased job satisfaction compared with increased job satisfaction | 3.79 (3.24 to 4.43); (1.13 to 12.77) | 97 (96.6 to 98) | P=0.002 |
| Emotional exhaustion | 33 (22 699) | 4.81 (3.67 to 6.30); (1.11 to 20.93) | 98 (97 to 98.3) | P=0.04 | |
| Depersonalisation | 30 (22 002) | 2.89 (2.37 to 3.53); (1.07 to 7.82) | 92 (90 to 94) | P=0.98 | |
| Personal accomplishment | 32 (27 374) | 2.88 (2.28 to 3.63); (0.86 to 9.66) | 93 (91 to 95) | P=0.83 | |
| Productivity loss: | |||||
| Burnout | 7 (9581) | Favours increase in productivity loss compared with sustained productivity | 1.82 (1.08 to 3.07) | 83 (66 to 91) | NA |
| Emotional exhaustion* | 4 (3421) | 1.06 (1.00 to 1.12) | 90 (77 to 96) | NA | |
| Depersonalisation* | 3 (2969) | 1.23 (1.18 to 1.28) | 96 (92 to 98) | NA | |
| Personal accomplishment* | 3 (2969) | 1.53 (1.43 to 1.63) | 97 (94 to 99) | NA | |
| Turnover intention: | |||||
| Burnout | 25 (32 271) | Favours turnover intention compared with retention | 3.10 (2.30 to 4.17); (0.71 to 13.56) | 97 (96 to 97.3) | P<0.001 |
| Emotional exhaustion | 16 (23 625) | 2.81 (1.80 to 4.40); (0.46 to 17.11) | 99 (98.8 to 99.2) | P=0.001 | |
| Depersonalisation | 11 (23 257) | 1.82 (1.26 to 2.62); (0.53, 6.26) | 99 (98.7 to 99.2) | P=0.03 | |
| Personal accomplishment | 5 (11 028) | 1.28 (0.98 to 1.68) | 86 (70 to 94) | NA | |
| Quality of patient care | |||||
| Professionalism: | |||||
| Burnout | 40 (32 321) | Favours low professionalism compared with maintained professionalism | 2.33 (1.96 to 2.70); (0.88 to 6.16) | 96 (95.5 to 97.4) | P<0.001 |
| Emotional exhaustion | 16 (11 861) | 2.45 (1.71 to 3.53); (0.63 to 9.62) | 94 (91.8 to 95.6) | P<0.001 | |
| Depersonalisation | 12 (10 488) | 2.93 (1.93 to 4.46); (0.72 to 11.94) | 93 (89.9 to 95.1) | P=0.03 | |
| Personal accomplishment | 9 (2992) | 2.17 (1.36 to 3.46) | 92 (87 to 95) | NA | |
| Patient safety incidents: | |||||
| Burnout | 35 (41 059) | Favours patient safety incidents compared with no patient safety incidents | 2.04 (1.69 to 2.45); (0.71 to 5.81) | 87 (84 to 90) | P=0.04 |
| Emotional exhaustion | 17 (20 213) | 2.15 (1.82 to 2.53); (1.19 to 3.86) | 73 (56 to 83) | P<0.001 | |
| Depersonalisation | 14 (19 616) | 2.44 (1.84 to 3.23); (0.92 to 6.44) | 90 (85 to 94) | P<0.001 | |
| Personal accomplishment | 14 (19 616) | 1.47 (1.20 to 1.80); (0.78 to 2.76) | 87 (79 to 91) | P<0.001 | |
| Patient satisfaction: | |||||
| Burnout | 8 (1,002) | Favours lower patient satisfaction compared with them being satisfied | 2.22 (1.38 to 3.57) | 75 (53.4 to 86.6) | NA |
| Emotional exhaustion | 5 (527) | 2.79 (0.75 to 10.42) | 77 (44.2 to 90.5) | NA | |
| Depersonalisation | 6 (571) | 3.82 (1.57 to 9.29) | 81 (60 to 91) | NA | |
| Personal accomplishment | 5 (527) | 1.79 (1.14 to 2.81) | 5 (0 to 80) | NA | |
Results pooled using the standardised mean difference are provided in appendix 11. No changes in significance were found when pooling using standardised mean difference. CI=confidence interval; PI=prediction intervals were calculated only for meta-analysis involving 10 or more studies as advised in Cochrane handbook; NA=Estimate not applicable.
Fixed effect results were reported when fewer than five studies were reported and the meta-analysis involved varied sample and effect sizes.
Assessment of publication bias was done using Eggers’s test in all meta-analysis of 10 or more studies as advised in Cochrane handbook, and also checked using trim-and-fill method (see appendix 13 for full results). Forest plots for each analysis are provided in appendix 10, where the log odds ratio estimates are also available within the plots.
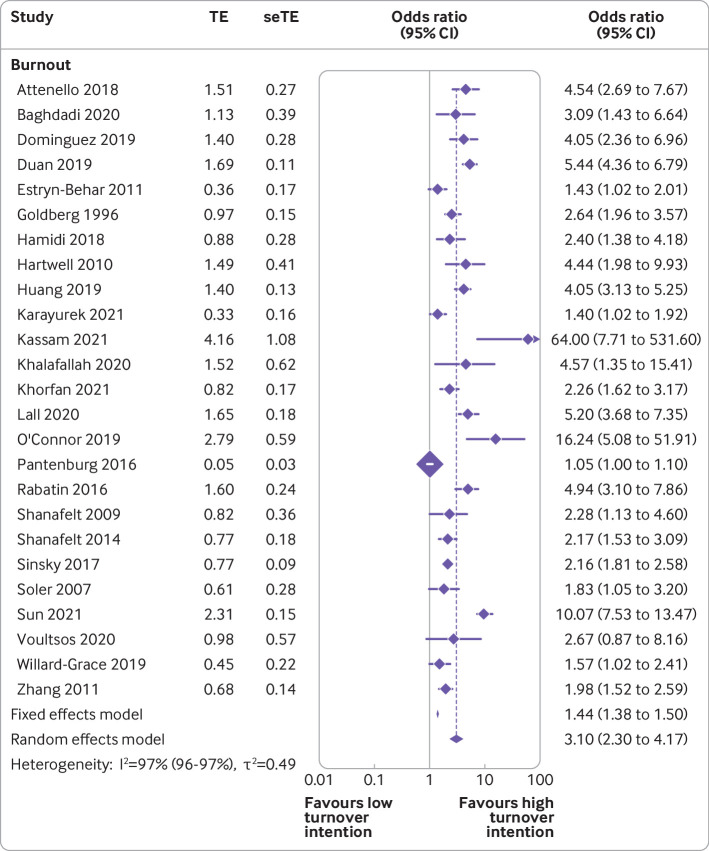
Physician burnout was associated with almost fourfold decreases in job satisfaction compared with increased job satisfaction based on measures of overall burnout (3.79, 95% confidence interval 3.24 to 4.43, I2=97%, k=73 studies, n=146 980 physicians), emotional exhaustion (4.81, 3.67 to 6.30, I2=98%, k=33, n=22 699), depersonalisation (2.89, 2.37 to 3.53, I2=92%, k=30, n=22 002) and personal accomplishment (2.88, 2.28 to 3.63, I2=93%, k=32, n=27 374). Burnout was associated with threefold increases in career choice regrets compared with being satisfied with their career choice based on measures of overall burnout (3.49, 2.43 to 5.00, I2=97%, k=16, n=33 871) and emotional exhaustion (4.16, 3.34 to 5.19, I2=90%, k=4, n=2014). Burnout was associated with up to threefold increases in turnover intention compared with retention based on measures of overall burnout (3.10, 2.30 to 4.17, I2=97%, k=25, n=32 271; fig 3), emotional exhaustion (2.81, 1.80 to 4.40, I2=99%, k=16, n=23 625), and depersonalisation (1.82, 1.26 to 2.62, I2=99%, k=11, n=23 257; fig 4) but no effect was seen for personal accomplishment. Burnout was associated with small but significant decreases in productivity compared with sustained productivity based on measures of overall burnout (1.82, 1.08 to 3.07, I2=83%, k=7, n=9581), depersonalisation (1.23, 1.18 to 1.28, I2=96%, k=3, n=2969) and personal accomplishment (1.53, 1.43 to 1.63, I2=97%, k=3, n=2969). Finally, only two studies46 47 48 reported a significant pooled association between overall burnout and career development concerns compared with good career development (3.77, 2.77 to 5.14, I2=0%, k=2, n=3411).
Fig 3.
Association of physician burnout with turnover intention. TE=log odds ratio; seTE=standard error of log odds ratio; OR=odds ratio; CI=confidence interval
Fig 4.
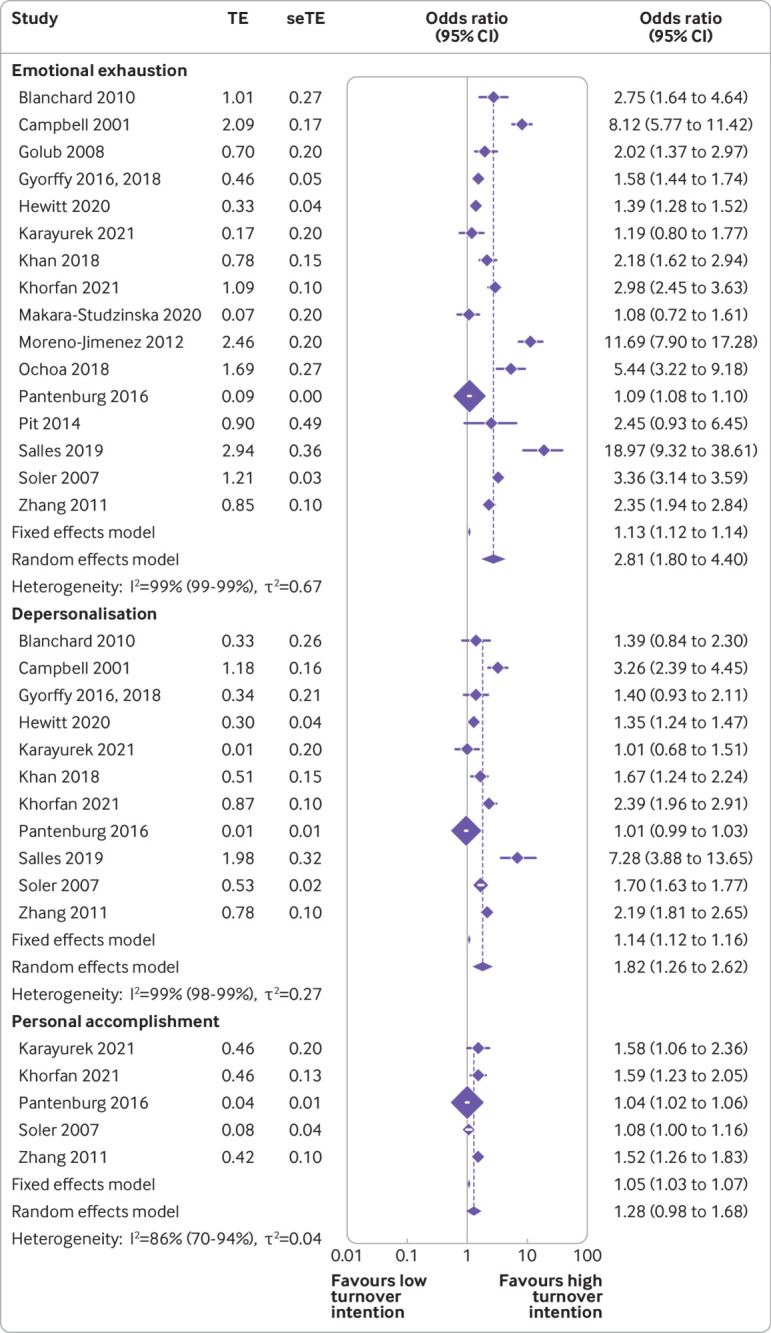
Association of emotional exhaustion, depersonalisation, and personal accomplishment of physicians with turnover intention. TE=log odds ratio; seTE=standard error of log odds ratio; OR=odds ratio; CI=confidence interval
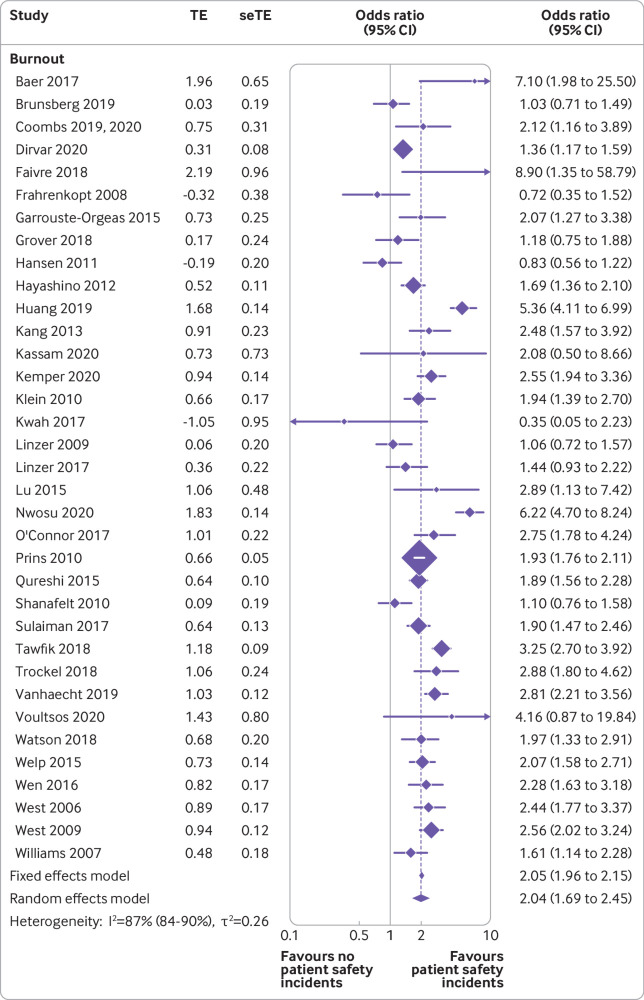
Physician burnout was associated with double the risk of patient safety incidents compared with no patient safety incidents based on measures of overall burnout (odds ratio 2.04, 95% confidence interval 1.69 to 2.45, I2=87%, k=35, n=41 059; fig 5), emotional exhaustion (2.15, 1.82 to 2.53, I2=73%, k=17, n=20 213), depersonalisation (2.44, 1.84 to 3.23, I2=90%, k=14, n=19 616), and personal accomplishment (1.47, 1.20 to 1.80, I2=87%, k=14, n=19 616; fig 6). Burnout was associated with more than twofold decreases in professionalism compared with maintained professionalism based on measures of overall burnout (2.33, 1.96 to 2.70, I2=96%, k=40, n=32 321), emotional exhaustion (2.45, 1.71 to 3.53, I2=94%, k=16, n=11 861), depersonalisation (2.93, 1.93 to 4.46, I2=93%, k=12, n=10 488), and personal accomplishment (2.17, 1.36 to 3.46, I2=92%, k=9, n=2992). Burnout was also associated with up to threefold decreases in patient satisfaction compared with patients being satisfied based on measures of overall burnout (2.22, 1.38 to 3.57, I2=75%, k=8, n=1002), depersonalisation (3.82, 1.57 to 9.29, I2=81%, k=6, n=571), and personal accomplishment (1.79, 1.44 to 2.81, I2=5%, k=5, n=527). Publication bias was found after visual inspection of funnel plots and the test statistics for most comparisons were significant (appendix 13).
Fig 5.
Association of burnout with patient safety incidents. TE=Log odds ratio; seTE=standard error of log odds ratio; OR=odds ratio; CI=confidence interval
Fig 6.
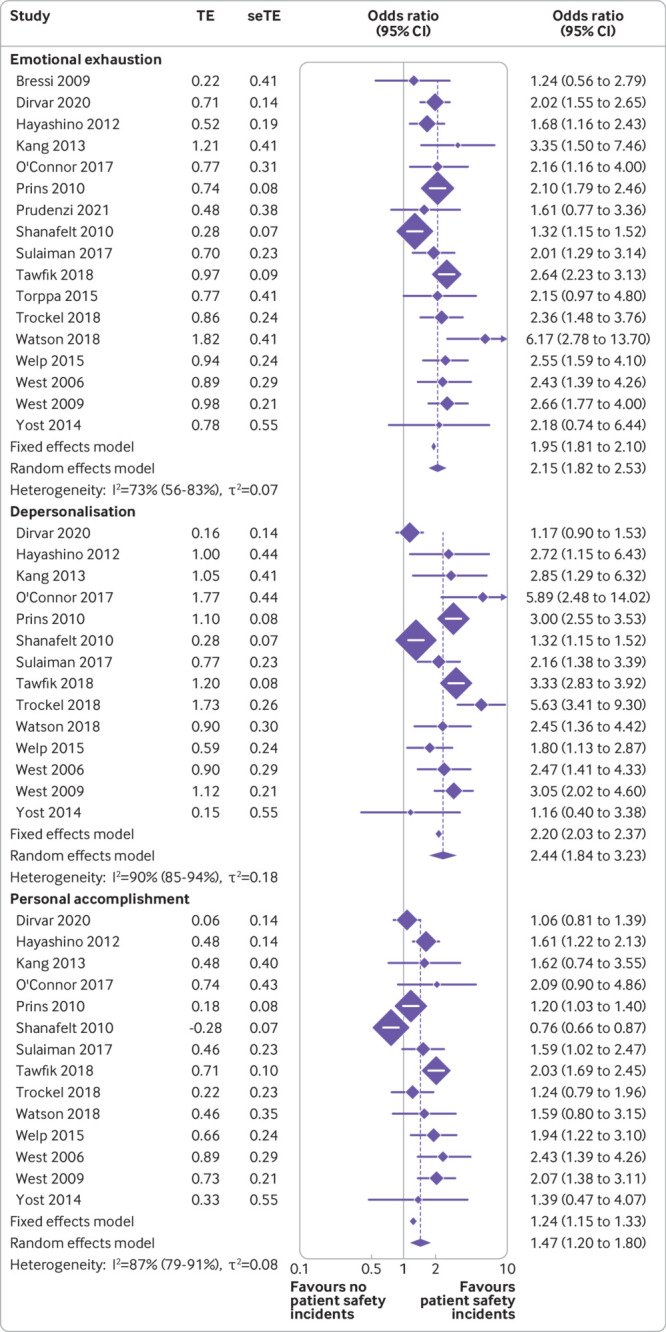
Association of emotional exhaustion, depersonalisation, and personal accomplishment with patient safety incidents. TE=Log odds ratio; seTE=standard error of log odds ratio; OR=odds ratio; CI=confidence interval
Some studies had used different scales to measure burnout, therefore, we also did analyses using standardised mean difference to account for measures of different length (see forest plots in appendix 11). However, we found no significant differences in this analysis and the results were consistent with those reported when analysed with the odds ratio.
The subgroup meta-analyses for the different measures of burnout used for the outcomes job satisfaction, patient safety incident, professionalism, and turnover intention is provided in appendix 8 in supplement.
For job satisfaction, the abbreviated version of Maslach Burnout Inventory provided the largest association with burnout (odds ratio 4.62, 95% confidence interval 3.21 to 6.65, I2=99%) and smallest with the Copenhagen burnout inventory (2.59, 2.22 to 3.01, I2=95%). The Copenhagen inventory had the highest association of burnout with patient safety incidents (3.59, 2.92 to 4.42, I2=95%) and the abbreviated versions of the Maslach Burnout Inventory had the lowest association (1.68, 1.16 to 2.43, I2=79%). The association between burnout and low professionalism was greatest when using an abbreviated version of the Maslach Burnout Inventory (2.91, 1.65 to 5.13, I2=87%) and lowest when using the Copenhagen inventory (1.89, 1.69 to 2.12, I2=43%). The association between burnout and turnover intention was greatest when other non-specific measures of burnout were used (7.23, 5.93 to 3.18, I2=77%) and lowest when an abbreviated version of Maslach Burnout Inventory was used (2.53, 1.39 to 4.59, I2=98%). No significant differences were noted between the different burnout measures when tested using the ratio of odds ratios (appendix 8).
Meta regressions
The results of the univariable and multivariable meta-regression analyses are provided in appendix 12. In the univariable regression results, a stronger association of overall burnout with low job satisfaction was found in physicians working in hospitals compared with primary care settings (1.88, 0.91 to 3.86, P=0.09), and more specifically in emergency medicine and intensive care (2.16, 0.98 to 4.76, P=0.06) compared with a general internal medicine specialty, and in physicians older than the age of 50 years compared with individuals aged 31-50 years (2.41, 1.02 to 5.64, P=0.04). The association was weakest in GPs (0.16, 0.03 to 0.88, P=0.04). However, these associations did not remain significant in the multivariable regressions. The association between burnout and patient safety incidents in the univariable regression results was found to be larger in younger physicians (20-30 years; 1.88, 1.07 to 3.29, P=0.03), working in emergency medicine and intensive care settings (2.10, 1.09 to 3.56, P=0.02), or in training based in the Commonwealth region (3.03, 0.83 to 11.25, P=0.09). The only association to remain significant in the multivariable regression results was that found in younger physicians (1.55, 0.94 to 2.56, P=0.08). The univariable regression results of the association of burnout with low professionalism was found to be smaller in physicians aged older than 50 years (0.36, 0.19 to 0.69, P=0.003) and larger in physicians still in training or residency (2.27, 1.45 to 3.60, P=0.001), who worked in a hospital (2.16, 1.46 to 3.19, P<0.001), specifically in the emergency medicine specialty and intensive care (1.48, 1.01 to 2.34, P=0.04), or when situated in a low to middle income country (1.68, 0.94 to 2.97, P=0.08). Multivariable regression results show that the association remained significant in middle aged physicians aged 31-50 years (0.45, 0.26 to 0.76, P=0.003), working in a hospital (3.82, 1.84 to 8.00, P<0.001), or specialising in cancer (0.25, 0.09 to 0.74, P=0.01) or neurology (0.22, 0.07 to 0.73, P=0.01). The univariable regression results of the association of burnout with career choice regret was found to be largest in physicians with a specialisation in emergency medicine and intensive care (2.89, 0.97 to 14.89, P=0.10) and neurology (2.52, 0.82 to 7.80, P=0.10). The association between burnout and turnover intentions did not vary according to any other factors included in the univariable regression analyses (appendix 12). No significant associations were found between burnout and job satisfaction.
Discussion
Principal findings
This systematic review and meta-analysis provides compelling evidence that physician burnout is strongly associated with the career disengagement of physicians and suboptimal patient care. However, even after confirming the consistency of the data in up 84 (49%) of 170 study authors, the results should be considered in tandem with the large amount of heterogeneity presented in all comparisons.
We found that physicians with burnout were up to four times more likely to be dissatisfied with their job compared with being satisfied with their job, three times as likely to have thoughts or intentions to quit their job (turnover) compared with job retention, and three times as likely to regret their career choice compared with being satisfied with their career choice. Emotional exhaustion contributed most to increases in the turnover intention of physicians compared with retention. The association of physician burnout with lower job satisfaction compared with increased job satisfaction was more prevalent in older physicians working in emergency medicine and intensive care.
Physicians with burnout are twice as likely to be involved in patient safety incidents compared with no patient safety incidents and show low professionalism compared with maintained professionalism, and over two times more likely to receive low satisfaction ratings from patients compared with satisfied patient ratings. The depersonalisation subscale of burnout appeared to have the most adverse association with the quality of care and patient dissatisfaction. Patient safety incidents compared with no patient safety incidents were more likely to occur in younger physicians working in emergency medicine and intensive care.
Comparisons with similar research
No previous meta-analysis has examined the association of burnout with the career engagement of physicians. Only one review,60 predominately based on studies of nurses, has linked inter-professional work with employee outcomes. A number of systematic reviews have assessed the association of burnout with the quality of patient care, however, these studies mostly included mixed samples of healthcare professionals and rarely used meta-analysis due to heterogeneous samples and outcomes.14 15 We chose to focus on physicians because they are twice as likely to experience burnout than any other worker, including other healthcare professionals8 12 and this choice has improved our confidence in using a meta-analysis. Moreover, both career engagement of physicians and quality of patient care were chosen because these dimensions of health service quality are complimentary and some of our outcomes including low professionalism, low job satisfaction, and reduced patient satisfaction, are precursors of safety risks with potential to lead to active patient safety incidents and have serious career implication on the physician.61 This balanced approach (to be comprehensive in terms of outcomes but specific on physicians) was agreed by our core research team involving physicians and patients.
Policy implications
Many countries including the US and the UK have described levels of physician burnout as the highest in the history of health and care systems.2 62 63 Our findings affirm that physician burnout can be a catalyst for the career disengagement of physicians and burnout is associated with unsafe patient care,64 65 which costs billions to healthcare systems annually.66 67 68 Physician burnout deepens the workforce crisis and undermines a fundamental societal need to be in receipt of safe care. In line with our results, a survey from the US concluded that physicians at the front line of care access are at greatest risk of burnout, work longer hours, and have greater struggles with work-life balance and job satisfaction than other healthcare workers.69 These factors often unite as a result of burnout, and can lead to higher physician turnover rates,70 which in itself has substantial costs in terms of both the interruption in continuity of care relationships and high expense associated with recruiting new clinicians and staff.71
Effective interventions that can curtail physician burnout are needed now more than ever as health and care systems across the globe are encountering a workforce crisis.72 A range of effective interventions for reducing burnout in physicians are available, including interventions focusing on improving the culture on healthcare organisations, interventions supporting individual physicians through organisational funded initiatives, and multicomponent interventions.21 73 We found that physicians with high scores of depersonalisation are especially likely to be involved in lower quality of patient care whereas physicians with high scores of emotional exhaustion are especially likely to express intentions to leave their job. Thus, interventions targeting specific dimensions of burnout could be offered to subgroups of physicians with career concerns or adverse patient care experiences taking also into consideration their reciprocal relationships between burnout, career engagement, and quality of patient care. For example, physicians experiencing burnout might have less time or commitment to optimise the care of their patients, can take more unnecessary risks, or might lack accountability.74 Conversely, exposure to adverse patient events or recognition of poor quality of care can result in burnout, which in turn could force physicians to quit. This process can often be referred to as secondary trauma, particularly in relation to sentinel events or important safety incidents.75
Our results highlight subgroups of physicians with burnout who could be at particularly high risk for career disengagement and provision of unsafe patient care. These physicians are mainly frontline physicians in emergency medicine and intensive care. Unsurprisingly, reports from frontline physicians advocate that the field of medicine is almost reaching crisis point with an increasing number of physicians working part time, resigning from their job, or retiring early in response to excessive workload and symptoms of burnout.6 76
Limitations
The large heterogeneity for some of the outcomes such as, patient safety, professionalism, and job satisfaction, might have been due to variations of outcome definition. Despite this variation, we selected these definitions based on theories and consultations with stakeholders. For example, the outcome job dissatisfaction includes many different aspects such as poor work engagement, dissatisfaction with workload, and poor relationships with patients. This diversity in the outcome definition might lead to overestimating the association with physician burnout, as the prediction intervals (which conveniently express heterogeneity) suggest. Therefore, the results should be interpreted with this potential overestimation in mind. Similarly, patient safety incidents often originate from complex and interchangeable factors including the different nature and types (preventable or not), severity, dispensing stage, and systems used.77 Meaning that the observed meta-analytical association with physician burnout might be more attributable to general factors of the whole organisation or work setting in healthcare.78 Additionally, our definition for the patient safety incidents was broad and captured any of the following incidents; potentially avoidable readmission, prescribing errors, monitoring errors, and potentially avoidable adverse events. Thus, owing to the large variation in the possible cause of a safety incident, we urge some caution when interpreting the pooled effect sizes for patient safety incidents.
The tools or questionnaires used to assess these above outcomes varied considerably and this variation did not allow us to make any meaningful subgroup or sensitivity analyses. Reaching consensus about a gold standard set of tools to assess at least some of these outcomes would be an important step for improving the precision of the effect sizes in future meta-analyses. Moreover, career engagement outcomes have conceptual similarities with the personal accomplishment subscale of burnout but exclusive focus on only the other two subscales of burnout (emotional exhaustion and depersonalisation) could introduce more bias than omitting personal accomplishment would avoid. Our findings call for future studies to examine the causal and temporal relations (eg, structural equation modelling) between the different career engagement outcomes and the three subscales of burnout.
We extracted and analysed the rawest available data in each study where possible, standardised these data using odds ratios (and standardised mean differences), and then performed several meta-regressions and sensitivity analyses to validate the findings. Despite these precautions, some degree of imprecision is still possible in the pooled effect sizes driven by variations in the aggregate data that we used. Accessing individual participant data could considerably improve the precision of the effect sizes, which we strongly recommend in future research.
Although the focus of this investigation was on physicians, this population should still be considered as working in various settings and specialties. We performed meta-regressions, which did explain some of the heterogeneity due to specialty area, but because of the low numbers of participants in some groups, these meta-regressions had to be combined into hierarchical categories of healthcare settings or specialties, which could conflate some findings. Furthermore, because fewer patient safety incidents were found in studies with response rates above 70%, this might have attributed to possible bias in studies with lower response rates.79
Our protocol amendment resulted in excluding grey literature from this review. Although the exclusion of this type of literature could actually lead to an increase in publication bias80; the sheer high volume of additional grey literature (eg, mostly engagement surveys by medical associations or colleges and universities) were of poor quality and provided limited, if any, association data that could be used in a meta-analysis. Thus, we have captured the highest quality of evidence providing meta-analytical pertinent data. However, peer reviewed literature is likely to be subject to some exaggeration of the association of burnout when assessed against similar patient care outcomes.10 Also, only English language publications were included so other studies could have been missed.
Sensitivity analysis of the reporting method (ie, by physician or patient surveillance system) was not possible because more than 79% of the reports were self-reports by physicians for both patient safety incidents and low professionalism. The design of the original studies (mostly cross-sectional) inevitably imposes limits on our ability to establish causal links between physician burnout and patient care or career engagement, and the mechanisms that underpin these links.81 However, with only 20 prospective cohort or longitudinal studies, assessment of direct causality would not have been feasible in this study. Finally, method bias is a common problem in cross-sectional studies, when measuring one or more constructs with the same method it can have significant effects on the relationship between them.82 Method bias can influence inventory validation and reliabilities as well as the covariation between latent constructs, such as measures of physician wellness. Thus, researchers need to be knowledgeable about ways to control for method biases thorough the use of more suited statistical remedies, such as structural equational models, which provide an explicit assessment of measurement error and estimation of latent constructs.83
Conclusions
Burnout is a strong predictor for career disengagement in physicians as well as for patient care. Moving forward, investment strategies to monitor and improve physician burnout are needed as a means of retaining the healthcare workforce and improving the quality of patient care. Scalable implementation of effective interventions for physician burnout, such as those improving the culture of healthcare organisations, and multicomponent interventions are strongly supported by our findings.21 73
What is already known on this topic
Burnout is reaching global epidemic levels among physicians and many physicians advocate that the capacity in the field of medicine is almost reaching crisis point
A better understanding of the association of burnout with the career engagement of physicians is urgently needed now more than ever as health and care systems across the globe are facing a critical workforce crisis
No meta-analysis to date has examined the association of burnout with the career engagement of physicians, nor have they presented this relationship in parallel with the potential impacts on the quality of patient care
What this study adds
The largest and most comprehensive systematic review and meta-analysis assessing the association of burnout with the career engagement of physicians and the quality of patient care, summarising results from 170 observational studies with 239 246 physicians
Physicians with burnout are up to four times more likely to be dissatisfied with their job and more than three times as likely to have thoughts or intentions to leave their job (turnover) or to regret their career choice
Physicians with burnout are twice as likely to be involved in patient safety incidents and show low professionalism, and over twice as likely to receive low satisfaction ratings from patients
Acknowledgments
We thank the following for confirming their study data: Colin West, Mark Linzer, Daniel S Tawfik, Sami Abdo Radman Al-Dubai, Hamzeh Mohammad Alrawashdeh, Ala’a B Al-Tammemi, Tamara Elizabeth Baer, Suphi Bahadirli, Pierre Blanchard, Tom Bourne, Katherine A Brunsberg, Neil A Busis, Demetrius M Coombs, Risal Djohan, Mao Ding, Oksana Babenko, Sergio Dominguez-Lara, Ingrid Gilles, Justin S Golub, Michael M Johns III, Zsuzsa Győrffy, Rikke P Hansen, D Brock Hewitt, Karl Y Bilimoria, Matthew R Janko, Matthew R Smeds, Hakan Demirci, Julie Welch, Kathi J Kemper, Debraj Mukherjee, Atir Khan, Jens Klein, Michael Kriss, Henry M Kuerer, Shailesh Kumar, Jason Kwah, Michelle D Lall, John Leung, Kerry H Levin, Dave W Lu, Laxmi S Mehta, Leonardo Potenza, Maha Sulaiman Younis, Bernardo Moreno-Jiménez, Paul O’Connor, Alec O’Connor, Geon Ho Bahn, Sabrina Pit, Jelle T Prins, Vinay Rawlani, Ashim Roy, Arghavan Salles, Wilmar B Schaufeli, Christine A Sinsky, James A Sliwa, Leyla Ozturk Sonmez, Colm M P O’Tuathaigh, Lois J Surgenor, Hyo Jung Tak, Okan Taycan, Yasuharu Tokuda, Wakako Umene-Nakano, Deborah Seys, David Ring, Krzysztof A Tomaszewski, Lars Peterson, Alexander G Watson, Matthias Weigl, Hui-Ching Weng, Robin R Whitebird, Rachel Willard-Grace, James Gardner Wright, Xiaowei Zhang, Morgan G Yost, Sandeep Grover, and Peng Xie.
Web extra.
Extra material supplied by authors
Web appendix 1: Supplementary tables and text
Contributors: MP, AH, and AE had the initial research idea and obtained funding for this study. AH, MP, AE formulated the research questions and designed the study. AH searched for published work, selected articles, extracted and analysed data, and drafted the protocol and manuscript. MP, AZ, JJ, RR, AZ, and KG helped in the searching of articles and data selection and extraction. Data extraction was confirmed by 49% of the authors. MP substantially contributed to designing the searches and the statistical analysis plan, writing of the manuscript, and interpreting the findings. AE, CAC-G, JJ, DP, and RR substantially contributed to the manuscript by providing review comments and edits. AH is the guarantor. All authors have read and approved the final manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This study is funded by the UK National Institute for Health Research (NIHR) School for Primary Care Research (project 411). AH is also funded by the University of Manchester through his Presidential Fellowship. The NIHR Greater Manchester Patient Safety Translational Research Centre funded MP’s time contributed to this project. CCG would also like to acknowledge the NIHR Applied Research Collaboration West Midlands who is responsible for partly funding her research. The study funder had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. The views expressed are those of the author(s) and not necessarily those of the UK National Institute for Health Research or the Department of Health and Social Care.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: support from the UK National Institute for Health and Care Research School for Primary Care Research for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
The lead author AH (the manuscript’s guarantor) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: The results will be presented at this year’s Annual Society of Academic Primary Care (SAPC) Annual Scientific Meeting 2022 (https://sapc.ac.uk/conference/2022) and at the WELL-Med’s 4th International Meeting on Well Being and Performance in Clinical Practice (https://www.well-med.gr). The results will also be shared through press releases through the affiliated universities of the author’s involved, social medial including twitter and with funders including the NIHR SPCR.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Ethical approval
Not required in this study.
Data availability statement
Because this meta-analysis was based on data extracted from previously published research, most of the data and study materials are available in the public domain. However, the raw data extractions, transformed data sheets and author emails confirming the data will be made available and will be published on Mendeley.
References
- 1. Maslach C. Burnout, Psychology of. In: Wright JD, ed. International Encyclopedia of the Social & Behavioral Sciences. 2nd ed. Elsevier, 2015: 929-32 10.1016/B978-0-08-097086-8.26009-1. [DOI] [Google Scholar]
- 2. The Lancet . Physician burnout: a global crisis. Lancet 2019;394:93. 10.1016/S0140-6736(19)31573-9. [DOI] [PubMed] [Google Scholar]
- 3. Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2020. Mayo Clin Proc 2022;97:491-506. 10.1016/j.mayocp.2021.11.021. [DOI] [PubMed] [Google Scholar]
- 4. General Medical Council . National Training Survey 2021 results. 2021. https://www.gmc-uk.org/-/media/documents/national-training-survey-results-2021-summary-report_pdf-87050829.pdf.
- 5. Wright T, Mughal F, Babatunde OO, Dikomitis L, Mallen CD, Helliwell T. Burnout among primary health-care professionals in low- and middle-income countries: systematic review and meta-analysis. Bull World Health Organ 2022;100:385-401A. 10.2471/BLT.22.288300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gergen K. The self as social construction. Psychol Stud (Mysore) 2011;56:108 10.1007/s12646-011-0066-1. [DOI] [Google Scholar]
- 7.American Medical Association (AMA). Coping with covid-19 for caregivers survey. National comparison report prepared May 2021. https://www.ama-assn.org/system/files/coping-with-covid-19-caregivers-survey-national-comparison-report.pdf.
- 8. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015;90:1600-13. 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 9. Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg 2009;250:463-71. 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 10. Tawfik DS, Scheid A, Profit J, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med 2019;171:555-67. 10.7326/M19-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Olson KD. Physician burnout-a leading indicator of health system performance? Mayo Clin Proc 2017;92:1608-11. 10.1016/j.mayocp.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 12. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet 2009;374:1714-21. 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 13. Welle D, Trockel MT, Hamidi MS, et al. Association of occupational distress and sleep-related impairment in physicians with unsolicited patient complaints. Mayo Clin Proc 2020;95:719-26. 10.1016/j.mayocp.2019.09.025. [DOI] [PubMed] [Google Scholar]
- 14. Hall LH, Johnson J, Watt I, Tsipa A, O’Connor DB. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS One 2016;11:e0159015. 10.1371/journal.pone.0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dewa CS, Loong D, Bonato S, Trojanowski L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ Open 2017;7:e015141. 10.1136/bmjopen-2016-015141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Owoc J, Mańczak M, Jabłońska M, Tombarkiewicz M, Olszewski R. Association between physician burnout and self-reported errors: meta-analysis. J Patient Saf 2022;18:e180-8. 10.1097/PTS.0000000000000724. [DOI] [PubMed] [Google Scholar]
- 17.Hodkinson A, Johnson J, Geraght K, et al. Associations of physician burnout with patient care and career outcomes: a systematic review and meta-analysis. PROSPERO 2021 CRD42021249492. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021249492.
- 18. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-12. 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 19. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kanter MH, Nguyen M, Klau MH, Spiegel NH, Ambrosini VL. What does professionalism mean to the physician?. Perm J 2013;17:87-90. 10.7812/TPP/12-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med 2017;177:195-205. 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
- 22. Conner KR, Beautrais AL, Brent DA, Conwell Y, Phillips MR, Schneider B. The next generation of psychological autopsy studies. Part I. Interview content. Suicide Life Threat Behav 2011;41:594-613. 10.1111/j.1943-278X.2011.00057.x [DOI] [PubMed] [Google Scholar]
- 23. Holm AL, Severinsson E. Struggling to recover by changing suicidal behaviour: narratives from women with borderline personality disorder. Int J Ment Health Nurs 2011;20:165-73. 10.1111/j.1447-0349.2010.00713.x [DOI] [PubMed] [Google Scholar]
- 24. Wells G, Shea B, O'Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analysis. 2000; https://www.researchgate.net/publication/261773681_The_Newcastle-Ottawa_Scale_NOS_for_Assessing_the_Quality_of_Non-Randomized_Studies_in_Meta-Analysis
- 25. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 26. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-58. 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 27. IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol 2014;14:25. 10.1186/1471-2288-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ 2003;326:219. 10.1136/bmj.326.7382.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sterne JA, Egger M, Smith GD. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 2001;323:101-5. 10.1136/bmj.323.7304.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Riley RD, Higgins JPT, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011;342:d549. 10.1136/bmj.d549. [DOI] [PubMed] [Google Scholar]
- 31. Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav 1981;2:99-113. 10.1002/job.4030020205. [DOI] [Google Scholar]
- 32. Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA 2018;320:1131-50. 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Thiese MS, Ronna B, Ott U. P value interpretations and considerations. J Thorac Dis 2016;8:E928-31. 10.21037/jtd.2016.08.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Harrell FE, Jr. Regression modeling strategies. Springer International Publishing, 2016. [Google Scholar]
- 35.Lather P. Getting lost: feminist practices toward a double(d). State University of New York Press. 2007. [Google Scholar]
- 36. Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 2019;22:153-60. 10.1136/ebmental-2019-300117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Marsh I. Suicide: Foucault, history and truth. Cambridge University Press. 2010. [Google Scholar]
- 38. Bourne T, Wynants L, Peters M, et al. The impact of complaints procedures on the welfare, health and clinical practise of 7926 doctors in the UK: a cross-sectional survey. BMJ Open 2015;5:e006687. 10.1136/bmjopen-2014-006687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bourne T, De Cock B, Wynants L, et al. Doctors’ perception of support and the processes involved in complaints investigations and how these relate to welfare and defensive practice: a cross-sectional survey of the UK physicians. BMJ Open 2017;7:e017856. 10.1136/bmjopen-2017-017856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bourne T, Shah H, Falconieri N, et al. Burnout, well-being and defensive medical practice among obstetricians and gynaecologists in the UK: cross-sectional survey study. BMJ Open 2019;9:e030968. 10.1136/bmjopen-2019-030968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hall LH, Johnson J, Watt I, O’Connor DB. Association of GP wellbeing and burnout with patient safety in UK primary care: a cross-sectional survey. Br J Gen Pract 2019;69:e507-14. 10.3399/bjgp19X702713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Khan A, Teoh KR, Islam S, Hassard J. Psychosocial work characteristics, burnout, psychological morbidity symptoms and early retirement intentions: a cross-sectional study of NHS consultants in the UK. BMJ Open 2018;8:e018720. 10.1136/bmjopen-2017-018720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sharma A, Sharp DM, Walker LG, Monson JR. Stress and burnout in colorectal and vascular surgical consultants working in the UK National Health Service. Psychooncology 2008;17:570-6. 10.1002/pon.1269. [DOI] [PubMed] [Google Scholar]
- 44. Prudenzi AD, Graham C, Flaxman PE, et al. Wellbeing, burnout, and safe practice among healthcare professionals: predictive influences of mindfulness, values, and self-compassion. Psychol Health Med 2022;27:1130-43. 10.1080/13548506.2021.1898651. [DOI] [PubMed] [Google Scholar]
- 45. van Wulfften Palthe OD, Neuhaus V, Janssen SJ, Guitton TG, Ring D, Science of Variation Group . Among musculoskeletal surgeons, job dissatisfaction is associated with burnout. Clin Orthop Relat Res 2016;474:1857-63. 10.1007/s11999-016-4848-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Estryn-Behar M, Doppia MA, Guetarni K, et al. Emergency physicians accumulate more stress factors than other physicians-results from the French SESMAT study. Emerg Med J 2011;28:397-410. 10.1136/emj.2009.082594. [DOI] [PubMed] [Google Scholar]
- 47. Kassam AF, Cortez AR, Winer LK, et al. Extinguishing burnout: National analysis of predictors and effects of burnout in abdominal transplant surgery fellows. Am J Transplant 2021;21:307-13. 10.1111/ajt.16075. [DOI] [PubMed] [Google Scholar]
- 48. McAbee JH, Ragel BT, McCartney S, et al. Factors associated with career satisfaction and burnout among US neurosurgeons: results of a nationwide survey. J Neurosurg 2015;123:161-73. 10.3171/2014.12.JNS141348. [DOI] [PubMed] [Google Scholar]
- 49. Block L, Wu AW, Feldman L, Yeh HC, Desai SV. Residency schedule, burnout and patient care among first-year residents. Postgrad Med J 2013;89:495-500. 10.1136/postgradmedj-2012-131743. [DOI] [PubMed] [Google Scholar]
- 50. Ochoa P. Impact of Burnout on Organizational Outcomes, the Influence of Legal Demands: The Case of Ecuadorian Physicians. Front Psychol 2018;9:662-62. 10.3389/fpsyg.2018.00662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pei P, Lin G, Li G, Zhu Y, Xi X. The association between doctors’ presenteeism and job burnout: a cross-sectional survey study in China. BMC Health Serv Res 2020;20:715. 10.1186/s12913-020-05593-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and career satisfaction among US oncologists. J Clin Oncol 2014;32:678-86. 10.1200/JCO.2013.51.8480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016;165:753-60. 10.7326/M16-0961. [DOI] [PubMed] [Google Scholar]
- 54. Yuguero O, Marsal JR, Buti M, Esquerda M, Soler-González J. Descriptive study of association between quality of care and empathy and burnout in primary care. BMC Med Ethics 2017;18:54. 10.1186/s12910-017-0214-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Pit SW, Hansen V. Factors influencing early retirement intentions in Australian rural general practitioners. Occup Med (Lond) 2014;64:297-304. 10.1093/occmed/kqu028. [DOI] [PubMed] [Google Scholar]
- 56. Coleman DM, Money SR, Meltzer AJ, et al. SVS Wellness Task Force . Vascular surgeon wellness and burnout: a report from the Society for Vascular Surgery Wellness Task Force. J Vasc Surg 2021;73:1841-1850.e3. 10.1016/j.jvs.2020.10.065. [DOI] [PubMed] [Google Scholar]
- 57. Dinibutun SR. Factors associated with burnout among physicians: an evaluation during a period of COVID-19 pandemic. J Healthc Leadersh 2020;12:85-94. 10.2147/JHL.S270440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kelker H, Yoder K, Musey P, Jr, et al. Prospective study of emergency medicine provider wellness across ten academic and community hospitals during the initial surge of the COVID-19 pandemic. BMC Emerg Med 2021;21:36. 10.1186/s12873-021-00425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Makara-Studzińska M, Wontorczyk A, Izydorczyk B. Stress and occupational burnout in a population of Polish doctors - Organizational-professional and non-professional-social predictors. Ann Agric Environ Med 2020;27:456-68. 10.26444/aaem/110846. [DOI] [PubMed] [Google Scholar]
- 60. Kaiser S, Patras J, Martinussen M. Linking interprofessional work to outcomes for employees: a meta-analysis. Res Nurs Health 2018;41:265-80. 10.1002/nur.21858. [DOI] [PubMed] [Google Scholar]
- 61. Panagioti M, Stokes J, Esmail A, et al. Multimorbidity and patient safety incidents in primary care: a systematic review and meta-analysis. PLoS One 2015;10:e0135947. 10.1371/journal.pone.0135947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Parliament UK. House of Commons Health and Social Care Committee. Workforce burnout and resilience in the NHS and social care. Second Report of Session 2021-22, HC 22: Published on 8 June 2021. https://committees.parliament.uk/publications/6158/documents/68766/default/
- 63. Yates SW. Physician stress and burnout. Am J Med 2020;133:160-4. 10.1016/j.amjmed.2019.08.034. [DOI] [PubMed] [Google Scholar]
- 64. Hodkinson A, Tyler N, Ashcroft DM, et al. Preventable medication harm across health care settings: a systematic review and meta-analysis. BMC Med 2020;18:313. 10.1186/s12916-020-01774-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Panagioti M, Khan K, Keers RN, et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. BMJ 2019;366:l4185. 10.1136/bmj.l4185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Bates DW, Spell N, Cullen DJ, et al. Adverse Drug Events Prevention Study Group . The costs of adverse drug events in hospitalized patients. JAMA 1997;277:307-11. 10.1001/jama.1997.03540280045032 [DOI] [PubMed] [Google Scholar]
- 67. Estimating the attributable cost of physician burnout in the United States . Ann Int Med 2019;170:784- 90. 10.7326/m18-1422%m31132791. [DOI] [PubMed] [Google Scholar]
- 68. Kaushik D. COVID-19 and health care workers burnout: a call for global action. EClinicalMedicine 2021;35:100808. 10.1016/j.eclinm.2021.100808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med 2012;172:1377-85. 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 70. Scanlan JN, Still M. Relationships between burnout, turnover intention, job satisfaction, job demands and job resources for mental health personnel in an Australian mental health service. BMC Health Serv Res 2019;19:62. 10.1186/s12913-018-3841-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. JAMA 2017;317:901-2. 10.1001/jama.2017.0076. [DOI] [PubMed] [Google Scholar]
- 72. Kirch DG, Petelle K. Addressing the physician shortage: the peril of ignoring demography. JAMA 2017;317:1947-8. 10.1001/jama.2017.2714. [DOI] [PubMed] [Google Scholar]
- 73. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016;388:2272-81. 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 74. Halbesleben JR, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev 2008;33:29-39. 10.1097/01.HMR.0000304493.87898.72. [DOI] [PubMed] [Google Scholar]
- 75. Van Gerven E, Vander Elst T, Vandenbroeck S, et al. Increased risk of burnout for physicians and nurses involved in a patient safety incident. Med Care 2016;54:937-43. 10.1097/MLR.0000000000000582. [DOI] [PubMed] [Google Scholar]
- 76. Hartzband P, Groopman J. Physician burnout, interrupted. N Engl J Med 2020;382:2485-7. 10.1056/NEJMp2003149. [DOI] [PubMed] [Google Scholar]
- 77. Smaggus A. Safety-I, Safety-II and burnout: how complexity science can help clinician wellness. BMJ Qual Saf 2019;28:667-71. 10.1136/bmjqs-2018-009147. [DOI] [PubMed] [Google Scholar]
- 78. National Academy of Medicine (NAM) Annual Reports . 2019. https://nam.edu/wp-content/uploads/2020/06/NAM-Annual-Report-2019.pdf
- 79. Coggon D, Rose GA, Barker DJP. Epidemiology for the uninitiated. BMJ Books, 2003. [Google Scholar]
- 80. McAuley L, Pham B, Tugwell P, Moher D. Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses? Lancet 2000;356:1228-31. 10.1016/S0140-6736(00)02786-0. [DOI] [PubMed] [Google Scholar]
- 81. Sedgwick P. Bias in observational study designs: cross sectional studies. BMJ 2015;350:h1286. 10.1136/bmj.h1286. [DOI] [PubMed] [Google Scholar]
- 82. Podsakoff PM, MacKenzie SB, Podsakoff NP. Sources of method bias in social science research and recommendations on how to control it. Annu Rev Psychol 2012;63:539-69. 10.1146/annurev-psych-120710-100452. [DOI] [PubMed] [Google Scholar]
- 83. Gunzler DD, Perzynski AT, Carle AC. Structural Equation Modeling for Health and Medicine. 1st ed. Chapman and Hall/CRC, 2021, 10.1201/9780203701133. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix 1: Supplementary tables and text
Data Availability Statement
Because this meta-analysis was based on data extracted from previously published research, most of the data and study materials are available in the public domain. However, the raw data extractions, transformed data sheets and author emails confirming the data will be made available and will be published on Mendeley.