Abstract
Recent years have shown that the diagnosis and monitoring of biomarkers involved in inflammatory-associated medical conditions such as cancer, neurological disorders, viral infections, or daily physical activities offer real benefits in increasing the quality of medical care and patient life quality. In this context, the use of integrated and portable platforms as point-of-care testing devices for biomedical analysis to enable early disease diagnosis and monitoring, which can be successfully used even at the patient’s bed, is an emergency nowadays. The development of low-cost, miniaturized, and portable, user-friendly devices that provide an answer in a timely manner, such as electrochemical sensors, is relevant for the elaboration of point-of-care testing devices. This review focuses on the recent progress in bioanalysis of both specific biomarkers and inflammatory-associated biomarkers present in several diseases like neoplasia, severe neurological disorders, viral infections, and usual physical activity and provides an overview of the state of the art over the most recent electrochemical (bio)sensors for the detection of inflammation-related biomarkers. Future perspectives of point-of-care testing to improve healthcare management are also discussed.
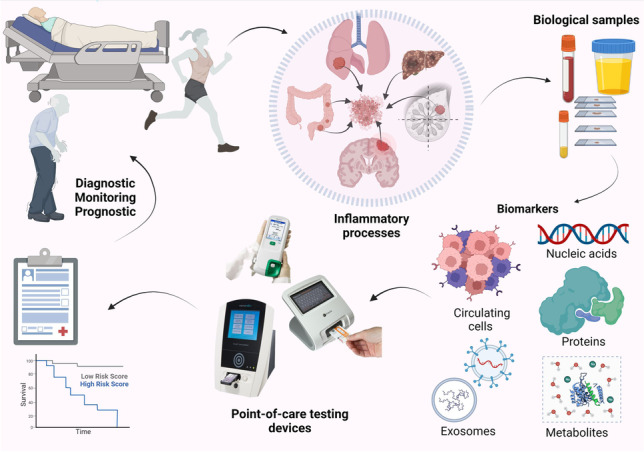
Graphical abstract
Keywords: Point-of-care testing, Biomarkers, Inflammation, Electroanalytical methods, Wearable sensors
Introduction
Inflammation is a defense process of the body triggered by tissue damage. The etiology of inflammation is diverse and can be represented by physical factors (trauma, extreme temperatures), chemical factors (endogenous or exogenous acids and bases), or infectious factors (bacteria, viruses, fungi, parasites). The inflammatory process can be acute, accompanied by heat, redness, swelling, pain, and loss of function, or chronic when the processes of fibrosis and repair also occur.
In acute inflammation, the following molecules and systems are involved:
Vasoactive amines: histamine, serotonin, involved in vasodilation and increase vascular permeability;
Kinine: bradykinin, involved in vascular changes, and pain;
Complement system: involved in immune defense and inflammation;
Coagulation: fibrinolysis system: fibrin network blocks foreign particles;
Mediators formed in the arachidonic acid cascades: prostaglandins, prostacyclins, leukotrienes, and thromboxane, involved in pain, fever or inflammation, and vascular processes;
PAF-platelet activation factor: involved in activation of thrombocytes and platelet aggregation;
Reactive oxygen species: superoxide anion, H2O2, hydroxyl radical, singlet oxygen;
Reactive nitrogen species: nitric oxide;
Cytokines: interleukins: IL-1, IL-6, IL-8; tumor necrosis factors: TNF-α, TNF-β; interferons: IFN-α, β, γ; colony-stimulating factors G, M, GM: involved in pain and vascular and chemotactic processes [1, 2].
In the case of chronic inflammation, the aforementioned signs are not present, but the final consequences can be fibrosis, tissue destruction, and eventually necrosis. The cells and molecules involved in chronic inflammation are monocytes, macrophages, lymphocytes, and cytokines. Cytokines are protein molecules that intervene in intercellular signaling and participate in cell growth and differentiation, apoptosis, and appearance and maintenance of inflammation, respectively in angiogenesis. Regarding inflammation, IL-6 and TNF-alpha are the most well-known cytokines with a pro-inflammatory role. IL-6 supports inflammation through the secretion of cytokines and monocytes as well as through the activation of signaling pathways involved in tissue destruction. TNF-alpha supports and promotes inflammation by stimulating the secretion of some proteins and immune cells and by stimulating coagulation (which can lead to occlusion or disseminated intravascular coagulation in case of severe inflammation) [3]. Because prolonged inflammatory processes have serious consequences on the patient’s health and can lead to the appearance or aggravation of other pathologies, its early diagnosis is of interest. All these molecules can be used as fluid biomarkers for the effective diagnosis of inflammation [1, 2].
A biomarker is a molecule (i.e., a protein) or a biological process (alterations of nucleic acids) that can be identified and quantified to help diagnose and monitor a physiological/pathological process. Depending on their clinical role, biomarkers can be classified into diagnostic, monitoring, response, predictive, risk, and safety biomarkers [4]. Biomarkers are true indicators of pharmacological reactions to a therapeutic strategy, thus being important to find effective strategies for early-stage diagnosis and for monitoring the treatment of different medical conditions [5]. Also, some diseases, such as cancer or neurodegenerative diseases, severely affect the general condition of the patient and are potentially fatal; thus, it is important to administer a specific treatment as early as possible [6].
Several medical conditions are accompanied by a chronic inflammatory process that can trigger the activation of other processes such as tissue destruction or degeneration, and the release of metabolites with local or systemic toxicity, respectively. Besides the specific markers of inflammation, the products determined by inflammatory processes can also be considered biomarkers. This is mainly due to the fact that inflammatory biomarkers do not provide information on the location of the inflammation or the affected organ, respectively, of the actual diagnosis. Thus, it is necessary to correlate the markers of inflammation with those characteristic of that condition [7].
According to the International Standard ISO22870, Point-of-care testing (POCT): Requirements for quality and competence, a POCT is a test “performed near or at the site of a patient with the result leading to a possible change in the care of the patient” [8]. A POCT can be performed in different locations such as at home, pharmacies, ambulances, nursing homes, physician’s offices, remote medical centers, hospitals, sports clinics, or workplaces. POC are analytical devices such as test kits or glucometers that are provided for in situ testing of the patient/user rather than sample collection and analysis in a traditional environment such as a clinical laboratory.
Biosensors are analytical devices composed of a transducer, bioreceptor, and digital output detector that can convert a biological or biochemical event into a measurable signal via the transducer. Depending on the type of the detection method, the signal is generated directly at the transducer surface (impedance or surface plasmon resonance) or indirectly by means of signaling molecules, such as fluorophores, enzymes, and electrochemically active molecules [9]. Based on the signal from the biorecognition reaction that undergoes transduction, the electrochemical biosensor market is segmented into potentiometric, impedimetric, conductometric, voltammetric, and others [10].
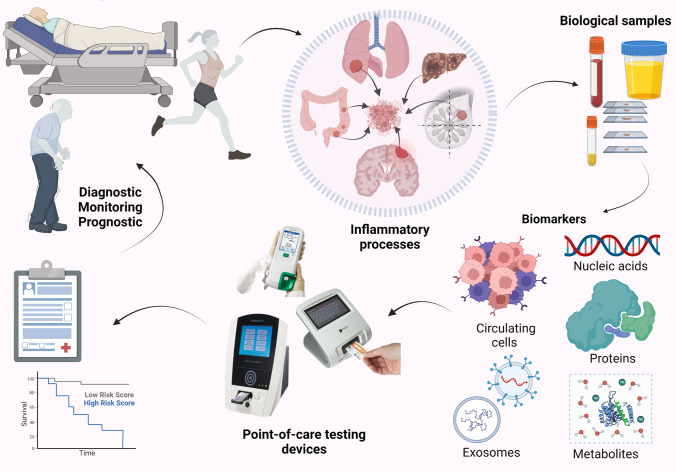
In this review, inflammation markers involved in diseases characterized by inflammatory processes such as cancer, neurological and neurodegenerative diseases, and SARS-CoV-2 infection (COVID-19) are presented. Moreover, examples of markers associated with inflammation produced by sports activities are also discussed. An overview of the electrochemical detection methods for these types of biomarkers and the ones suitable for POCT was discussed in the following sections. Figure 1 outlines the main directions approached in this review, highlighting the specific characteristics of POCT.
Fig. 1.
General illustration of the use of POCT devices for diagnosis, monitoring, or prognosis purposes in inflammatory-related diseases for improved healthcare management (original figure created with Biorender.com)
Point-of-care electrochemical testing
The development of new methods for POCT using streamlined and ideally reagent-free assays is a timely, critical, but challenging issue. Although reference methods achieve clinically relevant results in terms of accuracy, sensitivity, and selectivity, they oftentimes are lengthy, expensive, and require laboratory settings [11].
Recently, electrochemical methods have received increased attention due to advantages such as fast response, low use of reagents, and high selectivity and sensitivity, making them suitable for custom-made sensors [12]. A fast search on the ScienceDirect platform by using “point-of-care detection” as a keyword has generated 365,181 results, including articles, reviews, and book chapters. By adding “electrochemical” as a supplementary keyword, 21,464 results were generated, which is roughly 6%, highlighting the increased interest in this topic.
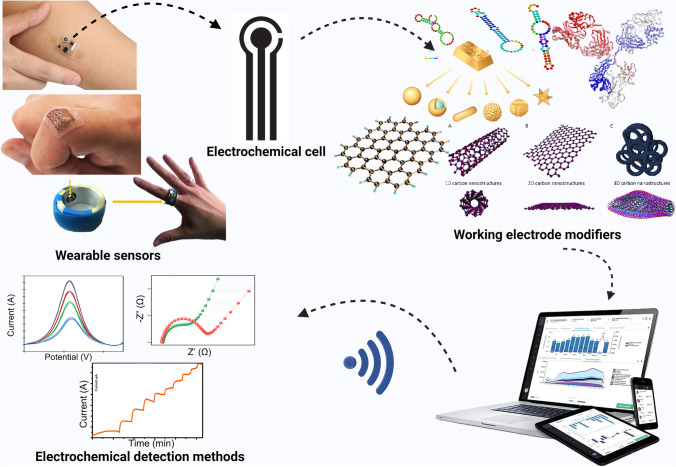
Several features of electrochemical (bio)sensors must be considered for efficient POCT device development (Fig. 2): new electrochemical substrates and simple detection methods, nanomaterials for increased sensitivity and reduced biofouling of targets, bioreceptors for increased specificity and multiplexed analyses, easy powering and low-cost electrochemical analyzers, digital outputs, and the combination with other technologies [13–16].
Fig. 2.
Schematic representation of POCT electrochemical devices (original figure created with Biorender.com)
Two different approaches in the field of POCT emerge from the literature with the involvement of electrochemical biosensors: the miniaturization of components, to ensure portability, and the integration of bioelements to ensure selectivity for the target. In addition, it is very important that the system be tested in clinical-related settings. There are regulations imposed by the World Health Organization (WHO) in this regard, according to which the systems can be classified as POCT only if they meet all the conditions included in the ASSURED guidelines: “Affordable,” “Sensitive,” “Specific,” “User-friendly,” “Robust and rapid,” “Equipment-free,” “Deliverable” to all people needing the test, including low-resource communities [17].
Some of the molecules determined by using POCT devices are represented by functional nucleic acids (DNA, RNA, aptamers), proteins (cytokines, enzymes, and antibodies), hormones, toxins, infectious particles (viruses and bacteria), and cells. The main purpose of the elaboration of biosensors is to specifically detect these molecules at their very low levels found in complex biological matrices. An important category of POCT devices applied in the biomedical field is based on antibodies and aptamers as modifiers for highly selective transducers [18, 19]. The analytical performances of these devices can be increased by using the new findings and developments in nanomaterials, in chemical and biological domains. Furthermore, the outstanding progress accomplished in miniaturization, electronics, artificial intelligence (AI), and the Internet of Things (IoT) allowed the development of wearable and portable (bio)sensors suitable for POCT device fabrication [11, 17].
Biomarkers involved in inflammatory diseases
Cancer biomarkers
Medical aspects related to cancer biomarkers
Cancer biomarkers can be classified into two major categories: molecular and processes (apoptosis, angiogenesis, and proliferation) biomarkers. The molecular biomarkers comprise nucleic acids (include modification of the entire genome and of genes primary sequence, such as rearrangements, amplifications, deletions, fragmentation of DNA/RNA), proteins (Bence-Jones proteins, carcinoembryonic antigen (CEA), cancer antigen-125 (CA-125), prostate-specific antigen (PSA), ApoA1, human epididymal secretory protein 4 (HER4), β-2 microglobulin, programmed death ligand1 (PD-L1), hypoxia-inducible factor1alpha (HIF-1α), tumor-associated and specific antigens), metabolites (fumarate, succinate, D-2-hydroxyglutarate (D-2HG); H2O2), exosomes (glypican-1 (GPC1), CD9, CD81, GTPases, miRNA), and circulating tumor cells (CTCs)[14, 20–26].
Cancer biomarkers are secreted into tissues and biological fluids, allowing early detection by minimally invasive and non-invasive methods [27, 28]. Here, we can include all analytical devices and methods that can be applied for the detection and/or monitoring of biomarkers from biological samples that can be collected in a minimally invasive manner (saliva, perspiration, tears), such as portable and wearable electrochemical detection devices. Any biomarkers in the category of inflammatory factors such as tumor necrosis factor (TNF-α), interferon-gamma (IFN-γ), and interleukin-6 (IL-6) can be also considered biomarkers for cancer. Numerous studies in the literature are based on the detection of these compounds, for which an attempt is made to find a correlation between their levels in different biological fluids and the stage of the disease [16].
POCT electrochemical sensors
Due to the advantages of portable and wearable devices in biomedical applications, there is an increase in the number of studies focused on electrochemical platforms developed for the analysis of cancer biomarkers [14, 21, 29]. Electrochemical portable devices for monitoring key biomarkers are the potential next frontier of wearable technologies for POCT diagnosis, including cancer. Furthermore, the extraordinary development in the field of microfluidics allows the detection of traces of biomarkers in small volumes of biological samples because it involves a pre-concentration step before detection [15, 30]. Numerous approaches have been published regarding the detection of a large number of biomarkers expressed in cancers using miniaturized devices or sensors suitable for miniaturization [15, 31, 32]. The aspect related to miniaturization is decisive when the development of POCT or point-of-use (POU) devices for decentralized detection, in the field, at the patient’s bedside is aimed. Thus, easy to manufacture, and low-cost detection of cancer biomarkers is crucial for fighting early-stage disease and increasing the patient’s chances of healing and survival. Some examples of such detection devices and their analytical parameters are presented in Table 1, the analytical methods being further discussed pointing out the most important components (nanomaterials and bioelements) and if real samples were analyzed.
Table 1.
Examples of electrochemical sensors and biosensors applied for the detection of cancer biomarkers
| Analyte | Platform | Bioelement or biomimetic element | Detection method | LOD | Linear range | Interferences | Sample type | Ref |
|---|---|---|---|---|---|---|---|---|
| CA 15–3 | AuSPE | Antibody | SWV | 0.95 U/mL | 1.0–1000 U/mL | CA 125 and CA 19–9 | Artificial serum | [33] |
| SPCE/GO/2D-MoSe2/P3ABA/AuNPs | Antibody | DPV | 0.07 ng/mL, 0.05 ng/mL | 0.07–60 ng/mL, 10–0.05 ng/mL | AFP, IgG, GM2, Gluc, AA, UA, BSA | Human serum | [34] | |
| CoS2-GR-AuNPs/GSPE | Antibody | DPV | 0.03 U/mL | 0.1–150 U/mL | CEA, BSA, TNF-α | Human serum | [35] | |
| Ag/TiO2/rGO/GCE | Antibody | CA | 0.07 U/mL | 0.1–300 U/mL | CA 27–29, PSA, CA 19–9, tyrosine, lysine, glycine, cysteine, K+, Na+, Ca2+, Mg2+, Zn2+, Fe3+ | Human serum | [36] | |
| GSPE | MIP | DPV | 1.5 U/mL | 5–50 U/mL | Her-2-ECD, CC | Human serum | [37] | |
| GSPE | MIP | DPV | 0.10 U/mL | 0.10–100 U/mL | - | Human serum | [38] | |
| HER-2 | Fe3O4@ TMU-21-MWCNT/GCE | Antibody | CA | 0.0003 ng/mL | 0.001–100 ng/mL | IgG, CEA, Muc1, HBS, HAS | Human serum | [39] |
| LSG/AuNS | MIP | SWV | 0.43 ng/mL | 1–200 ng/mL | cTn-I, (cTn-T, cTn-C, Gluc, DA, myoglobin, Chol | Human serum | [40] | |
| LSG.AuNS | Aptamer | SWV | 0.008 ng/mL | 0.1–200 ng/mL | Gluc, cTn-I, DA, Chol, | Human serum | [41] | |
| Au–Si-MNA | Antibody | DPV | 4.8 ng/mL | 10–250 ng/mL | Gluc, glycine, insulin, T4 bacteriophage, | Artificial interstitial fluid | [26] | |
| SPCE | Antibody | SWV | 0.28 ng/mL | 1–100 ng/mL | Gluc, AA, BSA | Human serum | [42] | |
| P53 antigen | BNC-SPE | Antibody | EIS | 0.16 U/mL | 0.01–1000 U/mL | CA-199, fetal bovine serum, Gluc | MCF57 cell lysates | [31] |
| SP-17 | APTMS/ITO | Antibody | DPV | 0.07 ng/mL | 0.1–5 ng/mL | Gluc, urea, ascorbic acid, oxalic acid, uric acid, IL-8, TNF-α, | Human serum | [43] |
| IL-8 | MWCNT-COOH/GE | Antibody | EIS | 0.0001 ng/mL | 0.001–1 ng/mL | IL-1, IL-6 | Artificial plasma | [44] |
| CEA | CC-Pt/Ru | MIP | CP |
3.52 ng/mL 4.41 ng/mL |
30–30,000 ng/mL | CA 15–3, Gluc, urea | - | [45] |
| HER-2-ECD | SPCE/CdSe@ZnS QDs | Antibody | DPASV | 2.1 ng/mL | 10–150 ng/mL | CA 15–3, cystatin C | Human serum | [46] |
| CA 27–29 | AuNPs/MoS2/rGO/GCE | Antibody | CA | 0.08 U/mL | 0.1–100 U/mL | CA 19–9, Ca 15–3, PSA | Human serum | [47] |
| PSA | MOF-235/MB | Antibody | DPV | 0.003 ng/mL | 0.01–1.2 ng/mL | AFP, CA-125, BSA | Human serum | [48] |
| AuNPs-ATPGO/GCE d-Ti3C2TX MXene@AuNPs | Antibody | DPV | 0.000003 ng/mL | 0.00001–0.001 ng/mL | CEA, IgG, HBS, BSA | - | [49] | |
| AuNPs/CHI/SPE | Antibody | SWV | 0.001 ng/mL | 1–18 ng/mL | AA, Gluc, glycin, BSA, tryptophan, | Human serum, plasma, urine | [50] | |
| Au@Th/GO PtCu@rGO/g-C3N4 | Antibody | CA | 0.0000166 ng/mL | 0.00005–40 ng/mL | CEA, IgG, HBS, Gluc, BSA | Human serum | [51] | |
| Au@PDA@BCN/GCE Pep/MB/AuPt@MnO2@COF | Antibody | DPV | 0.0000167 ng/mL | 0.00005–10 ng/ml | AA, BSA, lysine, ovalbumin, Gluc, lysozyme, sucrose, lipase | Artificial serum | [52] | |
| Ivory sheet or photographic paper/citrate AgNPs-GQDs nano-ink/CysA-Au NPs | Antibody | DPV | 0.07 ng/mL, 0.05 ng/mL | 0.07–60 ng/mL, 10–0.05 ng/mL | CA 15–3, CEA, CA-125, BSA | Human plasma | [53] | |
| GIDE | Aptamer | EIS | 0.51 ng/mL | 0.5–5000 ng/mL | HAS, hK2 | Human serum | [54] | |
| AuNPs/MoS2-Gas/GCE | Antibody | DPV | 0.000003 ng/mL | 0.00001–50 ng/mL | Gluc, AA, AFP, BSA | Human serum | [55] | |
| AuPtAgANCs/GCE | Antibody | DPV | 0.017 ng/mL | 0.05–50 ng/mL | BSA, AA, CEA, CA-199 | Human serum | [56] | |
| H2O2 | Nano-Au/CNTs/PDMS | - |
CV CA |
0.27 ng/mL | 0.675–871 ng/mL | DA, Gluc, AA, UA | HeLa and HUVEC cells | [57] |
| NiCo2S4@CoS2 NAs@CC | - | CA | 0.067 ng/mL | 0.43–71 ng/mL | AA, UA, DA, FA Gluc, nitrite, NO | Raw 264.7 cells | [58] | |
| CC/Co@C-CNTs | - | CA | 9.1 ng/mL | 13.5–243,000 ng/mL | NaCl, Gluc, DA, AA UA, E2, EE, E3, AMX, LVX | MDA-MB-231 cells and HeLa cells | [59] | |
| AuPd-ANPs/GQDs/CF | - | CA | 16.9 ng/mL | 33.8–622,350 ng/mL | Gluc, UA, AA, Cys, CA, Hcys, NAC, GSH, DTE, DHLA | MCF-7, MDA-MB-231 cells | [60] | |
| CF@NCNTAs–AuNPs | - | CA | 1.69 ng/mL | 3.4–145,125 ng/mL | Gluc, AA, UA, DA | MCF-7 and MBA-MD-231 | [61] | |
| TNF-α | ITO/PMMA-CD | Antibody | DPV | 0.00005 ng/mL | 0.00005–0.16 ng/mL | Gluc, KCl, IL-8, MUC-16, CYFRA-21, NaCl | Human serum | [62] |
| MoS2 nf/ITO | Antibody | EIS | 0.0002 ng/mL | 0.001–0.2 ng/mL | Gluc, NACl, Cyfra 21–1, MUC-16, IL-8 | Human serum | [63] | |
| IFN-γ | IFN-γ-3wj/GE | Aptamer | SWV | 0.00067 ng/mL | 0.001–0.01 ng/mL | Myoglobin, HB, BSA, IFN-γ, CRP, TNF-α | Human serum | [64] |
| Ag/ZnO | Antibody | EIS | 0.001 ng/mL | 0.001–0.512 ng/mL | IL-6, IL-8, IL-10, IP-10 | Human sweat | [65] | |
| IL-6 | GCE/pABA/pATP/AuNps/Apt-IL-6/MCH | Aptamer | EIS | 0.0016 ng/mL | 0.005–0.1 ng/mL |
CEA, MUC1, MUC4, MUC16 |
Human serum | [66] |
| ITO/PPyr-NHS | Antibody | EIS | 0.00001 ng/mL | 0.00003–0.0225 ng/mL | IL 1α, TNF α, p53 | Human serum | [67] | |
| AuNPs/PPyNPs/SPCE | Aptamer | EIS | 0.00033 ng/mL | 0.001–15,000 ng/mL | BSA, CEA, MUC1, MUC4, MUC16 | Human serum | [68] |
CA 15–3 cancer antigen 15–3, AuSPE gold screen–printed electrode, SWV square wave voltammetry, LSG laser-scribed graphene, AuNS gold nanostructured, MIP molecular imprinted polymer, HER-2 human epidermal growth factor receptor 2, cTn-I cardiac troponin-I, cTn-T cardiac troponin-T, cTn-C cardiac troponin-C, Gluc glucose, DA dopamine, Chol cholesterol, Apt aptamer, Au–Si-MNA high-density gold-coated silicon microneedle arrays, DPV differential pulse voltammetry, BNC bacterial nanocellulose, CA-199 cancer antigen 199, SPE screen-printed electrodes, WVFY tryptophan–valine–phenylalanine–tyrosine, SP17 sperm protein 17, ITO indium tin oxide, APTMS alkoxysilane substituted polymer, MUC1 mucin 1, IgG immunoglobulin G, BSA bovine serum albumin, MWCNT-COOH multi-walled carbon nanotubes, GE gold electrodes, IL interleukin, CEA carcinoembryonic antigen, Her-2-ECD extracellular domain of the human epidermal growth factor receptor 2, DPASV differential pulse anodic stripping voltammetry, QD quantum dots, SPCE screen-printed carbon electrode, GO graphene oxide, AuNPs gold nanoparticles, P3ABA/2D-MoSe2/GO poly(3-aminobenzylamine)/two-dimensional (2D) molybdenum selenide/graphene oxide, PSA prostate-specific antigen, UA uric acid, AA ascorbic acid, AFP alpha-fetoprotein, GM2 ganglioside GM2 activator protein, citrate AgNPs citrate-capped silver nanoparticles, GQDs graphene quantum dots, Cys-AuNPs cysteamine with gold nanoparticles, GIDE gold interdigitated electrode, HSA human serum albumin, hK2 human glandular kallikrein 2, HE4 human epididymis protein 4, MBs magnetic beads, SPCE Au NCs/MWCNT-NH2 gold nanocage coupled with an amidated multi-walled carbon nanotube, lncRNAs long non-coding RNAs, HOTAIR, H19, miRNA129 oligonucleotide sequences, AuNPs/MoS2-Gas Au nanoparticles/MoS2-graphene aerogels nanocomposite, GCE glassy carbon electrode, AuPtAg ANCs AuPtAg-alloyed nanocrystals, CoS2-GR cobalt sulfide/graphene nanocomposite, GSPE graphite screen–printed electrodes, Au/MoS2/rGO gold nanoparticles/molybdenum disulfide/reduced graphene oxide nanocomposite, Ca chronoamperometry, CC cystatin C, TB toluidine blue, miRNA-155, miRNA-141, let-7a oligonucleotides, PEI-Ag NPs polyethyleneimine-silver nanoparticles, HAS human serum albumin, HBS hepatitis B surface antigen, Fe3O4@TMU-21 magnetic framework, PbS QDs lead sulfide quantum dots, MOFs metal organic frame, MB methylene blue, ATP p-aminothiophenol, d-Ti3C2TX MXene@AuNPs delaminated MXene-gold nanoparticles, CHI chitosan, Au@Th/GO Au loaded on thionine-functionalized graphene oxide, PtCu@rGO/g-C3N4 PtCu bimetallic hybrid loaded on 2D/2D reduced graphene oxide/graphitic carbon nitride, Au@PDA@BCN polydopamine-coated boron-doped carbon nitride, AuNPs-MG gold nanoparticles–magnetic graphene composite, CC/Co@C-CNTs Co-embedded N-doped carbon nanostructures, GQDs graphene quantum dots, AuPd-ANPs AuPd alloy nanoparticles, CF carbon nanofiber, NCNTAs nitrogen-doped carbon nanotube arrays, PMMA-CD polymethyl methacrylate carbon dots, PPy polypyrrole, p-ABA p-aminobenzoic, pATP p-aminothiophenol, PPyr-NHS polypyrrole N-hydroxy succinimide
The use of nanomaterials and composite materials for the functionalization of electrodes before the immobilization of biocomponents for the elaboration of electrochemical biosensors proved to be beneficial, especially in increasing the sensitivity for the detection of targets [35, 36, 43, 44, 46]. An example of such a material which is intensively used in the electrochemical analysis of biological compounds, including cancer biomarkers, is graphene. Graphene improves the analytical performance of platforms due to its excellent electrical and thermal conductivity, mechanical strength, large surface area, and the possibility of being further functionalized with various compounds or nanostructures [13, 40, 69]. The development of portable (bio)sensors based on nanomaterials and composite materials is also related with the discovery of versatile materials, which in addition to special conductive properties, must be suitable for functionalization and structural handling. The methods by which graphene-based materials are transferred to the electrode are in continuous development, allowing to obtain high-purity, stable, and uniform films via chemical vapor deposition (CVD) technique [70] or laser-associated technique [41, 71]. The functionalization of graphene with CoS2 and gold nanoparticles (AuNPs) was exploited for the modification of the surface of carbon-based SPEs, which allowed the detection and quantification of CA15-3 protein with good analytical performance, due to the excellent electrocatalytic activity of the nanocomposite and increased amount of CA 15–3-specific antibodies immobilized at the electrode [35]. Another graphene-based immunosensor for the CA15-3 detection in serum employed the use of ternary Ag, TiO2, and reduced graphene oxide (rGO) to undergo signal amplification for the amperometric detection of H2O2 promoted upon the antibody-antigen immunoreaction [36]. Good analytical parameters were obtained for the detection of PSA using an ultra-sensitive electrochemical immunosensor based on AuNPs, p-aminothiophenol, and GO nanocomposite, and a self-assembled delaminated MXene-AuNP nanocomposite. By combining these nanomaterials, an increase in the amount of PSA antibodies captured at the electrode was obtained [49]. After the functionalization of the transducer with gold structure loaded on thionine functionalized GO layer, the immobilization of a high amount of antibodies and the acceleration of the electron transfer rate were both facilitated. This composite was further functionalized with PtCu bimetallic hybrid and loaded on 2D/2D rGO/graphitic carbon nitride, resulting in a complex material with excellent electrocatalytic properties, amplified detection signal, and biocompatibility [51]. Citrate-capped AgNP-modified graphene QDs were synthesized, embedded in nano-ink, and applied as a starting platform for the development of an ultrasensitive sandwich-type portable device for the detection of PSA in raw plasma. Signal amplification was obtained using cysteamine functionalized with AuNPs [53]. An aerogel porous network nanocomposite was synthesized based on graphene functionalized with AuNPs and MoS2 for the immobilization of a high amount of anti-PSA antibodies and the development of a label-free electrochemical immunosensor with good perspective for early diagnosis [55]. A highly sensitive porous and highly biocompatible microgel nanocomposite based on AuNPs, polyacrylic acid, and N-isopropylacrylamide was used and allowed the covalent immobilization of the amino-modified oligonucleotide capture probe complementary to the target. An optimized DPV procedure was applied to monitor the hybridization of miRNA-21 with the capture probe in serum [72].
The category of carbon-based nanomaterial with special properties and which meets the necessary criteria in the development of electrochemical (bio)sensors also includes carbon nanotubes (CNTs). This material is suitable for functionalization with other materials, chemicals, or biocomponents, presenting many applications in the biomedical field. For example, the electrocatalytic activity of the magnetic framework Fe3O4@TMU-21 multi-walled carbon nanotubes (MWCNT) was exploited for the construction of an electrochemical immunosensor for HER2 as a tumor biomarker in clinical monitoring. The immobilization of TMU-21 units at the surface of the Fe3O4-NPs was facilitated by methacrylic acid. The final composite material provided electrocatalytic activity toward the reduction of H2O2 used for the indirect detection of the target in human serum [39]. Hence, using Au nanocage coupled with an amidated MWCNT-functionalized SPEs enabled the efficient detection of lncRNAs in clinical settings [73].
In addition to carbon-based materials, nanoparticles or nanostructures of noble metals are involved in the development of electrochemical biosensors. In the case of noble metal nanostructures, AuNPs and silver nanoparticles (AgNPs) represent the most common forms applied in this field [50, 74]. In this case, the utility is related both to the improvement of the electrochemically active surface and implicitly of the sensitivity, and in facilitating the immobilization by strong and stable bonds of the structures with thiol group, especially in aptasensor development [50].
The use of antibody-type biological components in the fabrication of electrochemical immunosensors represented the starting point for the development of this field ensuring promising perspectives for the biomedical domain. The presence of antibodies in the structure of electrochemical biosensors allowed the extraordinary improvement of the analytical performances in terms of selectivity for the target, this being mainly due to the specific antigen–antibody interaction [22, 33, 35, 39, 46, 62].
The most common strategy for immobilizing antibodies on the electrode surface is by amide, covalent bonding. For this purpose, carboxyl groups must be generated at the electrode to bind to amino groups in the antibody [62, 63]. Thus, an innovative portable immunosensor based on a gold chip-type transducer functionalized with a self-assembled monolayer of mercaptosuccinic acid was designed for the detection of the CA 15–3. The covalent immobilization of the CA 15–3–specific antibodies via EDC/NHS chemistry with the carboxyl groups provided by the polymer ensured the selectivity of the immunosensor for the target protein in serum [33]. In another study, antibody immobilization is performed by interaction with the functions present on the composite film based on core/shell CdSe@ZnSQD, which also acts as an electroactive label, for the detection of HER2 in spiked serum [46]. A nano-biosensor for TNF-α was fabricated starting from a nanoflower-like structure of MoS2 and applied for the evaluation of this biomarker in cancer patients’ serum. The optimized biosensor showed excellent analytical performance, and good perspectives for application in decentralized analysis, being validated on cancer patient serum and by the standard ELISA method[63].
Indirect amperometric detection via the reduction of H2O2 in the presence of horseradish peroxidase (HRP) used as a label for the secondary antibody is the most common strategy for the detection of sandwich-type electrochemical immunosensors [50, 75]. Conventional electrochemical immunosensors based on electroactive materials often suffer from leakage and signal instability. To overcome this issue, label-free detection was applied and, in this case, nanomaterials and redox samples play an important role in amplifying the signal [47, 56, 63, 76]. Thus, an electrochemical immunosensor based on a fluffy metal porous material, MOF-235, and methylene blue (MB) as an effective signal amplification strategy was designed and applied for the sensitive detection of PSA [48]. A lead sulfide QDs-conjugated secondary HER2 antibody was used as a label. The indirect detection was obtained based on the SWV signal of the Pb2+ ions after their dissolution in HCl, enabling the detection of HER2 in serum with good recovery and selectivity [42].
Another fairly common strategy in recent decades for the design of electrochemical sensors is the use of biomimetic components, of which aptamers, microRNAs (miRNAs), and molecularly imprinted polymers (MIPs) have proven very useful, especially in terms of lower cost and better stability compared to antibodies, without negatively influencing the selectivity for the targets [23, 41, 54, 66, 67, 77]. For example, a MIP-based electrochemical sensor was elaborated for CA 15–3 on AuSPEs. The imprinting process consisted of the preconcentration of the target protein on the electrode followed by the electropolymerization of the 2-aminophenol monomer. The extraction of protein after this step allowed to obtain of the MIP-type sensor, which was then tested by voltammetry in the presence of a redox probe [37]. When poly(toluidine blue)-imprinted film was produced for the same biomarker, a signal decrease of the redox probe in DPV was observed with increased protein concentration [38]. The in situ electropolymerization was exploited for the generation of a MIP network consisting of poly(3,4-ethylenedioxythiophene) (PEDOT) and polypyrrole (PPy) at the surface of a carbon fabric anode containing Pt/Ru nanoparticles. This MIP-based sensor was designed as a simple, inexpensive, and effective tool for the detection of CEA in serum, being promising for further development of POCT [45]. The combination of nanomaterials with MIP films was also applied and has led to an improvement in parameters such as sensitivity, simplicity, porosity, and flexibility. Exploiting these advantages, a MIP sensor was developed using electrodes functionalized with graphene, nanostructured gold, and MIPs obtained after the electro-polymerization. All these components embedded together in the film deposited on the surface of the transducer allowed the selective and high-sensitivity detection of HER2in spiked undiluted serum [40].
Aptamers represent another category of biomimetic elements, different from MIPs, that are short, single-stranded DNAs or RNAs. Aptamers are versatile and bind targets with high selectivity and specificity since recognition and binding involve three-dimensional, shape-dependent, and hydrophobic interactions, base-stacking, and intercalation [78]. The targets can range from small molecules, peptides, and carbohydrates to proteins or live cells, and bend into a variety of shapes due to their tendency to form helices and single-stranded loops. Being synthetic compounds, with superior stability and versatility to bioelements such as antibodies, aptamers have found numerous applications in the field of electrochemical aptasensors [65, 79]. Thus, an aptamer with a high affinity for HER2 was immobilized onto the nanostructured electrode surface based on graphene and gold to enable the detection of HER2 in undiluted serum using an integrated handheld electrochemical system operated by a custom mobile application [41]. Polymer films (other than MIPs) deposited or generated on the electrode can also play an important role in the immobilization of the aptamer. Thus, p-aminobenzoic acid [66], PPy [67], or a conjugated poly(pyrrole N-hydroxy succinimide) (PPyr-NHS) polymer [68] are only some examples that have found their utility in the biomedical field and were applied in the development of electrochemical aptasensors for IL-6 cytokine.
Detection of a single biomarker is usually not sufficient for accurate diagnosis. Thus, the selection of a panel of biomarkers that express themselves in the same condition would be extremely beneficial for the biomedical field. Such approaches have also been attempted with respect to the simultaneous detection of tumor biomarkers with portable POCT devices. For example, a dual-mode electrochemical biosensor was developed for the simultaneous detection of two breast cancer biomarkers: CA15-3 and miRNA-21. The sensor composes of an SPE dual electrode array functionalized with a poly(3-aminobenzylamine)/two-dimensional/molybdenum selenide/GO nanocomposite. The two working electrodes were functionalized individually with 2,3-diaminophenazine-AuNPs and toluidine blue (TB)–AuNPs. The redox probe-AuNPs were employed as signaling molecules and supports for immobilization of anti-CA15-3 antibodies and capture DNA-21 probes, also providing good selectivity, and sensitivity for the dual target detection, and great potential to be further developed for the simultaneous detection of other miRNAs and proteins for POCT diagnostic applications[34].
Some recent examples of electrochemical (bio)sensors for the detection of cancer biomarkers are presented comparatively in Table 1.
Neurological-associated biomarkers
Medical aspects related to neurological-associated biomarkers
Neural inflammation is a defense mechanism of the organism which can represent a major symptom in many neurological disorders. Although acute inflammation of the neural tissue may be beneficial, it can cause harm if the inflammatory reaction is prolonged or exacerbated. In some cases, tissue destruction can occur which can lead to irreversible degradation of the nervous tissue with the appearance of various forms of clinically manifest dysfunctions (i.e., epilepsy, Alzheimer’s disease, Parkinson’s disease, systemic lupus erythematosus, etc.) [1, 80–83].
Among the biomarkers most frequently associated with neurological disorders are amyloid beta peptide (associated with Alzheimer’s disease), the tau protein, and alpha-synuclein (secreted in Parkinson's disease). Even if these biomarkers are specific to certain neurological diseases, they can also be considered biomarkers associated with inflammatory processes because they determine the occurrence of oxidative stress and other inflammatory mechanisms (as seen in Table 2) [84]. Biomarkers can be used for the rapid and effective diagnosis of neurological inflammatory processes. As in the case of neoplastic diseases, biomarkers specific for inflammation and non-specific biomarkers which accompany inflammation and concomitant processes (indirect determination) can be used [85, 86]. A new category of biomarkers that have been recently introduced for diagnosis and monitoring of inflammatory neurological disorders is represented by neurofilaments, the building blocks of proteins, and the basic structure of axons. The concentration of these proteins has been found to increase both in cerebrospinal fluid (CSF) and blood during neurological disorders and has been intensively studied. Neurofilaments can be used as biomarkers in neurological diseases such as stroke, traumatic brain injury, Parkinson’s disease, multiple sclerosis, encephalitis, epilepsy, and peripheral neuropathies [87, 88].
Table 2.
Examples of biomarkers involved in neurological disorders. Adapted after [84]
| Biomarker | Physiological implications | Pathological effect | Disorder |
|---|---|---|---|
| Amyloid beta | Lipid homeostasis, memory formation, regulation of synaptic activity, neural viability | Oxidative stress, synaptic dysfunction, inflammation, apoptosis, neurite damage | Alzheimer’s disease |
| Tau protein | Promotes microtubules polymerization, stability, and flexibility | Neuronal damage, pro-apoptotic | Alzheimer’s disease, Parkinson’s disease |
| Alpha-synuclein | Intervenes in the release of neurotransmitters, modulates DNA repair processes | Synaptic and mitochondrial dysfunctions, oxidative stress, dysregulation of calcium signaling, microtubule impairment | Parkinson’s disease |
| Chromogranin A | Vasoconstriction, regulation of glucose metabolism and storage, modulator of the neuroendocrine system | Oxidative stress, inflammation, neuronal damage | Amyotrophic lateral sclerosis |
| Micro-RNAs | Nervous system development and function | Microglial activation, increase of proinflammatory cytokine release, and neuron loss | Autist spectrum disorders |
The existence of validated markers for each action, but especially of fast, accessible methods of determination and allowing a decentralized use, at the patient’s bed would be very beneficial for an early diagnosis of the disease. To date, numerous biomarkers have been reported correlated with neurological conditions. The most important of these are centralized in Table 2, where the physiological implications, the pathological effect, and the type of disorder in which is expressed are also presented.
POCT electrochemical sensors
Given that neurological diseases are often accompanied by inflammatory processes whose consequences can be irreversible, early diagnosis of these diseases is of particular importance. There are many studies in this regard and the most recent will be discussed in this section of the review.
Based on the study of literature found on this topic, it is observed that the inclusion of nanocomposite materials has a crucial role in improving analytical parameters so the obtained sensors allow the detection of low concentrations of biomarkers when tested in complex matrix, as they are expressed in the neurological diseases for which rapid diagnosis is desired. The main advantage gained by the presence of nanomaterials in the sensor includes the existence of a greater number of active sites and functions available for immobilizing a larger number of bioelements and through stable interactions. This increases the sensitivity and stability of the (bio)sensors developed, catalyzes electrochemical reactions applied for the detection, enhances the electron transfer at the electrode, and assures the immobilization of different types of labels, which can highly improve the performance of the device [13, 89]. Thus, either graphene combined with metal nanoparticles [89], polymers combined with metallic foams [90] or particles [91], or composites based on noble metal particles or alloys [92], or with MOFs [93], were deposited on the electrode for increased sensitivity.
A small, portable magneto-immunosensor was developed for the amperometric detection of IL-6 by using a micro-fabricated electrode functionalized with rGO/AuNP nanocomposite to increase active surface useful for the immobilization of the antibody, fast charge transfer, and signal amplification [30]. Streptavidin-inorganic hybrid nanoflowers decorated with graphene were synthesized and used as substrates to modify GCEs and specifically bind a diblock dual-aptamer allosteric hairpin, functionalized with AuNPs and a streptavidin-labeled aptamer for the detection of IFN-γ [94].
The use of highly porous graphitic carbon deposited on polyimide tapes has proven useful in the development of a high-performance biosensor for IL-6 [95]. A poly(curcumin-Ni foam)-based sensor was fabricated and successfully applied for the quantification of amyloid β oligomer (AβO), a circulating biomarker applied for early diagnosis of Alzheimer’s disease [90]. For the same biomarker, another detection strategy was proposed using superhydrophobic carbon fiber paper and AuPt-NPs to immobilize the aptamer strands specific for AβO and indirectly minimize the nonspecific adsorption effect due to its hydrophobic character [92]. After the functionalization of GCEs with cerium oxide nanofiber electrospun, embedded in a Nafion layer, the composite film generated at the electrode proved to be permeable in a selective way for the TNF-α biomarker, with fast electron transfer and excellent analytical performance in serum [96].
Improving the analytical performance by using nanomaterials is not always adequate in the case of electrochemical sensors taking into account the principle on which their detection is based [97]. Thus, in complex matrices such as real samples used to detect biomarkers involved in neurological disorders, the redox properties of the compounds simultaneously present in the sample can lead to mutual interference. To prevent this issue, the additional functionalization of nanostructured surfaces with bioelements and biomimetic elements is frequently applied strategies [75, 98–100]. An electrochemical immunosensor based on carbon SPEs functionalized with nanomaterials was designed for the accurate determination of unfolded p53 in plasma from patients diagnosed with mild cognitive impairment and Alzheimer’s disease. The optimized detection method was validated by comparison with an ELISA assay, and the cheap, simple, and prone to miniaturization detection device has proved promising for POC applications [101]. The presence of carboxyl groups provided by the 4-carboxymethylaniline substrates allowed the immobilization of the anti-TNF-α antibodies by an amide bond. A secondary antibody labeled with HRP was used for the detection, in which tetramethylbenzidine was also involved as a substrate for the electrochemical reaction. The optimized biosensor has been shown to be highly selective for the target when tested in the presence of other analytes secreted in the acute stage of inflammation such as IL-10 and cortisol [75]. The generation of amino groups on the transducer can also be used for the immobilization of antibodies, since the latter have complementary carboxyl groups to achieve amide bonding [9]. A polystyrene-polyamidoamine dendritic polymer nanofiber–based platform was designed and provided a high density of amino groups useful for the covalent immobilization of a large number of capture antibodies with high selectivity for TNF-α in the presence of IL-10 and good perspective for clinical diagnosis [102].
Another strategy applied for the immobilization of biocomponents on the surface of the transducer is the esterification reaction in which the epoxy groups are involved. For example, the ultrasensitive detection of IL-6 has been achieved using a platform based on ITO substrate modified with acetylene black and epoxy-substituted-poly(pyrrole) composite with good biocompatibility and conductivity. The high abundance of epoxy groups was useful for the esterification reaction applied for the reproducible and stable immobilization of the antibodies to promote the determination of IL-6 in samples from patients with neurological disorders [103].
The use of aptamers as a biomimetic element for the selective detection of biomarkers involved in neuro-zone diseases has also been reported. Thus, a large number of AβO-specific aptamers were immobilized on a composite layer based on CNF and AuPt alloy that allowed the elaboration of a high-performance electrochemical aptasensor for AβO [92]. The suitability of aptamers for functionalization allows the addition on their chain of some compounds or composites with a role in detection. For example, an innovative aptasensor was developed for IFN-γ based on target-induced DNA strand and signal amplification with MB as a redox probe. It was observed a linear relationship between the signal of MB and IFN-γ content that could be successfully exploited for detection [91]. An aptamer-tethered gold nanoflower was synthesized on the electrode, having a role in immobilizing both target capture and aptamer-tagged AuNPs/Cu-MOF conjugates. The use of MOFs as signal probes determined the amplification of the detected signal and the increase of the sensitivity for AβO electrochemical detection with a real perspective for the early diagnosis of Alzheimer’s disease [93]. The use of impedance as a detection method is another useful strategy that has found applications in the field of aptasensors. A simple platform based on GO and AuNPs, embedded in a hydrogel layer, was used for the elaboration of an impedimetric label-free and selective detection of AβO in CSF or plasma [89]. A label-free electrochemical aptasensor for TNF-α was fabricated based on a multifunctional DNA 4-way junction. The main advantage of this system was that it does not require additional labeling and signal amplification processes [99]. An aptasensor for TNF-α was presented based on SPEs modified with gold hexacyanoferrate, AuNPs, and thiolated aptamers specific for the target cytokine. The high sensitivity and wide detection range of this method allowed TNF-α to be detected in serum even at very low concentrations as found in biological fluids [104]. By combining an aptamer with silver nanoclusters and AuNPs immobilized on the amine-terminated electrode surface, a sensitive and specific aptasensor for the detection of IFN-γ secreted by human cells was developed [105].
The use of platforms based on biomimetic elements, such as MIPs, has also been shown to be suitable for the detection of IL-6, as a biomarker for Alzheimer’s disease, and the development of POCT devices [100, 106]. The MIP film was obtained by the co-electropolymerization of pyrrole and carboxylated pyrrole in the presence of IL-6 protein, and SPCEs. This MIP-based sensor showed a detection limit at a level below pg/mL for IL-6 in spiked serum, good sensitivity, reproducibility, accuracy, and fast response being promising for the development of early diagnostics POCT for neurological diseases [100].
Some relevant and recent examples of electrochemical (bio)sensors for the detection of biomarkers involved in neurological disorders are presented in Table 3.
Table 3.
Examples of electrochemical sensors and biosensors applied for the detection of neurological biomarkers
| Analyte | Platform | Bioelement or biomimetic element | Detection method | LOD | Linear range | Interferences | Sample type | Ref |
|---|---|---|---|---|---|---|---|---|
| P53 protein | AuNPs/SPCE | Antibody | LSV | 0.05 nM | 2–50 nM | - | Human plasma | [101] |
| AβO | Poly(Ni-curcumin) | - | EIS | 0.001 nM | 0.001–5 nM | - | Artificial CSF | [90] |
| CFP/AuPt | Aptamer | DPV | 0.00016 ng/mL | 0.0005–10 ng/mL | HSA, NFL, tau441, Aβ42 monomer, Aβ40 monomer | Human serum | [92] | |
| AuNFs/GCE AuNPs/Cu-MOFs | Aptamer | DPV | 0.45 nM | 1–2000 nM | Aβ1–42 monomers, Aβ1–40 monomers, Aβ1–42 oligomers, Aβ1–40 oligomers, Aβ1–42 fibrils, and Aβ1–40 fibrils | Artificial CSF | [93] | |
| GO/AuNP hydrogel | PrPC | EIS | 0.0001 nM | 0.0001–10 nM | BSA, Gluc, NaCl | Artificial CSF, plasma | [89] | |
| Tau-381 | /GE | Aptamer and antibody | DPV | 0.00042 nM | 0.0005–0.1 nM | AA, tau-441, Gluc, L-cys | Human serum | [98] |
| PARK7/DJ-1 | Pt/bio-PET | Antibody | EIS | 7.5 ng/mL | 40–150 ng/mL | - | Artificial urine artificial serum | [107] |
| TNF-α | GE/CMA | Antibody | CA | 0.001 ng/mL | 0.001–0.03 ng/mL | IL-10, cortisol | Human saliva | [75] |
| CeNF/GCE/Nafion/MPA | Antibody | EIS | 0.000011 ng/mL | 0.000001–10,000 ng/mL | HSA, FIB, TNT, FIP, sTREM-1 | Human plasma | [96] | |
| GE/TNF-MF/DNA-4WJ | Aptamer | CV | 0.000073 ng/mL | 0.00015–0.15 ng/mL | CRP, IFN, HB | Human serum | [99] | |
| PS/PAMAM/NFs | Antibody | EIS | 0.000669 ng/mL | 0.01–0.2 ng/mL | IL-10 | PBS | [102] | |
| SPGE/AuHCF/AuNPs | Aptamer | DPV | 0.0055 ng/mL | 0.01–400,000 ng/mL | HSA, IgG | Human serum | [104] | |
| IFN-γ | SPCE | Antibody | CA | 0.0016 ng/mL | 0.0025–2 ng/mL | AA, BSA, Gluc, HB, IgG, Il-1β, IL-6, IL-8, RANKL, UA, TGF-β1, TNF-α | Saliva | [86] |
| GCE/AgNCs | Aptamer | CV | 0.0017 ng/mL | 0.0005–1 ng/mL | BSA, IFN-α, IFN-β, IgG, IL-6, TNF-α | Cells, human serum | [105] | |
| DDAHSH&AuN/SFG/GCE | Aptamer | DPSV | 0.000019 ng/mL | 0.0001–0.5 ng/mL | HB, L-cys, BSA, CEA, Gluc | Human serum | [94] | |
| AuNPs-PAMAM/MoS2/MB/GCE | Aptamer | SWV | 0.000002 ng/mL | 0.00001–1 ng/mL | AA, L-cys, UA, Gluc, myoglobin, BSA, Ig G, IL-22 | Human serum, urine | [91] | |
| IL-6 | EC-MIS-GE/rGO/AuNPs | Antibody | CA | 0.00042 ng/mL | 0.00097–0.25 ng/mL | CCL-2, IL-1, TNF-α, CRP | Human serum | [30] |
| ITO/AB/EpxS-PPyr | Antibody |
EIS CV |
0.000003 ng/mL | 0.00001–0.05 ng/mL | TNF α, p53, IL-1β, IL 1α, IL-8 | Human serum | [103] | |
| GC | Antibody | DPV | 0.0051 ng/mL | 0.01–0.5 ng/mL | IL-4 | Serum | [95] | |
| SPCE/PPy | MIP | EIS | 0.00002 ng/mL | 0.00002–2000 ng/mL | - | Spiked human serum | [100] | |
|
IL-6 TNF-α |
SAV-pHRP | Antibodies | CA |
0.04 ng/mL 0.02 ng/mL |
- | - | 3D muscle skeletal tissue | [106] |
LSV linear sweep voltammetry, AβO amyloid β oligomer, CFP/AuPt superhydrophobic carbon fiber paper with AuPt alloy nanoparticles, Aβ40, Aβ42 amyloid beta oligonucleotides, tau441 protein, NFL neurofilament protein, AuNFs Au nanoflowers, L-cys L-cysteine, PARK7/DJ-1 protein deglycase DJ-1, bio-PET bio-based poly(ethylene terephthalate), HUVEC human umbilical vein endothelial cells, CNTs carbon nanotubes, PDMS polydimethylsiloxane, NiCo2S4@CoS2 NAs@CC nickel cobalt sulfide/cobalt sulfide nanostructured arrays on carbon cloth, Raw 264.7 mammalian cells, CC/Co@C-CNTs Co nanoparticles embedded both in carbon sheets and in the tips of CNTs, CSF cerebrospinal fluid; MDA-MB-231 cells human breast cancer cell lines, E2 estradiol, EE ethynylestradiol, E3 estriol, AMX amoxicillin, LVX levofloxacin, AuPd-ANPs/GQDs/CF AuPd alloy nanoparticle–decorated graphene quantum dots on carbon fiber, Cys cysteine, CA cysteamine, Hcys homocysteine, NAC-N acetylcysteine, GSH glutathione, DTE 1,4-dithioerythritol, DHLA dihydrolipoic acid, NCNTAs nitrogen-doped carbon nanotube arrays (NCNTAs), FIB fibronectin, TNT troponin-t, FIP fipronil, sTREM-1 soluble triggering receptor expressed on myeloid cells-1, CYFRA-21 cytokeratin 19 fragment, HB hemoglobin, TGF-β1 transforming growth factor β1, RANKL receptor activator of nuclear factor kappa-Β ligand, CRP C-recative protein, CCL-2 chemokine ligand 2, CeNF cerium oxide nanofiber, MF-4WJ multifunctional DNA 4-way junction, PS polystyrene, PAMAM-NFs polyamidoamine dendritic polymer nanofibers, GSPPE graphene screen–printed paper electrode, DDAH diblock dual-aptamer allosteric hairpin, SFG graphene composite, AuHCF gold hexacyanoferrate, AB acetylene black, EpxS-Ppyr epoxy-substituted-poly(pyrrole) polymer, GC glassy carbon, SAV-pHRP streptavidin-poly horseradish peroxidase, CMA 4-carboxymethylaniline, EC-MIS electrochemical magnetoimmunosensor
COVID-19-associated biomarkers
Viral infection outbreaks are a great menace to groups of individuals due to their fast and easy spread but also for the incubation period which varies depending both on the viral pathogen and the infected person. The contemporary COVID-19 outbreak became in such a short time a matter of great concern for the global population. As of half of June 2022, according to WHO, there were reported almost 532 million confirmed cases and 6 million deaths, respectively [108].
SARS-CoV-2 disease stands for “severe acute respiratory syndrome coronavirus 2.” This virus makes patients experience in the first instance flu-like symptoms with possible outcomes such as acute respiratory distress syndrome (ARDS) and multiple organ failure (MOF) [109, 110], and the severity of the disease is topped up by an important pathophysiological aspect—the aggressive inflammatory response, which causes serious damage to the airways [109, 111, 112].
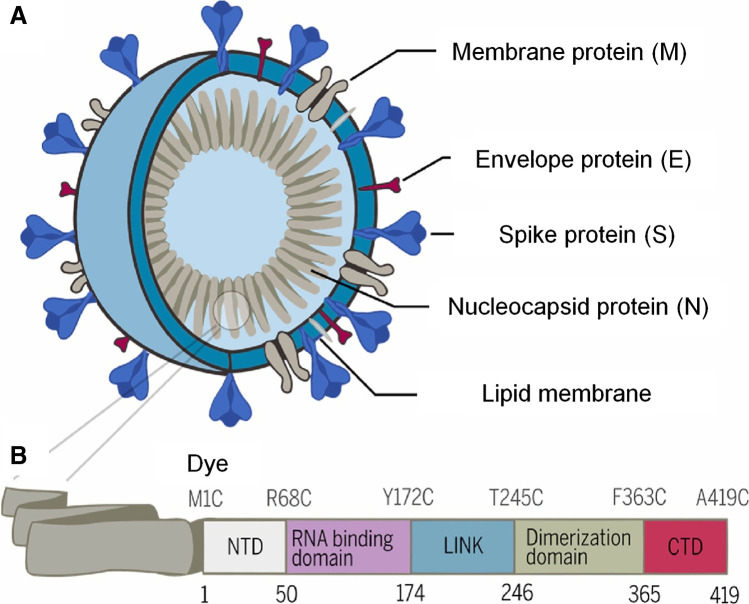
The SARS-CoV-2 virus has four main structural proteins (Fig. 3A): membrane protein (M), an envelope protein (E), spike protein (S), and one multifunctional structural nucleocapsid protein (ncovNP). The N protein is the main component of the ncovNP and is responsible for packaging and protecting coronavirus the genomic RNA, being divided into five distinct regions (Fig. 3B) [12]. The S protein is cleaved into two separate polypeptides S1 and S2 within the host by a furin-like protease [113]. Due to its affinity toward the human angiotensin-converting enzyme 2 (hACE2), it easily penetrates and infects human cells [114, 115].
Fig. 3.
Schematic representation of A SARS-CoV-2 virus; B domain architecture of SARS-CoV-2 N protein. Reprinted with permission by Elsevier from [12]
Upon the infection with the SARS-CoV-2 virus, the B cells of the host immune system respond and produce antibodies against the N-protein. Antibodies for S-protein are formed only after 4–8 days since the first symptoms appear. However, the Ig antibodies against SARS-CoV, such as IgA, IgM, and IgG, can be detected at different moments after the illness onset: IgA and IgM by the third week and IgG by the sixth week, respectively. Nevertheless, the accuracy of the detection reduces to 84% and 53% for IgG and IgA and IgM, respectively, after the seventh week since the patient got infected [116–118].
The reference detection method for SARS-CoV-2 infection uses real-time reverse transcriptase polymerase chain reaction (RT-qPCR) for the amplification of specific viral sequences from the virus genome such as E, RdRP, N, and S genes. Besides the requirements for skilled and trained personnel as well as bio-safety level-3 (BSL-3) laboratories, possible mutations of the SARS-CoV-2 virus can reduce the accuracy of the gold detection method. Given these inconveniences, the identification of prognostic biomarkers that can forecast the clinical course of a patient and the development of fast and accurate POC assays that provide (i) information on diagnosis, (ii) correlation with the immune response, and (iii) evaluation of the severity of the disease remain important objectives for the scientific community.
Therefore, this section evaluates possible prognostic markers involved in the immune-pathogenesis of SARS-CoV-2 infection and provides an overview of the POC electrochemical assays developed to confirm the infection with the SARS-CoV-2 virus.
Possible prognostic markers of the immune response
Several biomolecules involved in hyper-immune responsiveness, bradykinin and cytokine storms, and vascular leakage are assumed to be potential prognostic biomarkers for the COVID-19 disease [109, 119, 120]. A list of potential biomarkers to predict the outcome of the COVID19 disease was realized by Mariappan et al. [119] (Table 4). The level of some cytokines, including the previously mentioned ones, undergoes a characteristic change in the so-called cytokine storm. It has also been observed that in post-COVID, their level remains elevated [119]. This may be caused by the appearance of some inflammatory impairments located in some organs or tissues. The importance of cytokines in the detection of the COVID infection and the post-COVID status consists both in the rapid identification of the infection and in the determination of the general status of the patient and the evaluation of the prognosis. This can be particularly relevant in clinical practice, especially in the case of patients with severe damage and associated comorbidities. However, these need to be first validated by clinical studies and prove their efficacy in predicting the degree of the disease’s severity and long-term effects.
Table 4.
List of potential biomarkers to predict the COVID disease short- and long-term outcomes (reprinted with permission by Elsevier from [119])
| Type of biomarkers | Representatives |
|---|---|
| Cytokine storm biomarkers | IL-1, IL-2, IL-6, IL-7, IL-12, IL-17, IL-18, TNF-α, M-CSF, G-CSF, CXCL-10/IP-10, CCL-3, CCL-5, IFN-γ, MCP-1 |
| Macrophage biomarker | CD14, CD163, TLR2, TLR4, CD86, CD80, CD68, SOCS3, CD200R, CD206, ferritin |
| Endothelial biomarkers | Endoglin, syndecan-1, endothelin-1, cluadin-5, angiopoietin-1 (Ang-1), Ang-2, PECAM, S1P, VCAM, vWF, Tie2 |
| Bradykinin storm biomarkers | Bradykinin (BK), des-Arg9-bradykinin (DAKB), bradykinin-1 receptor (B1R), B2R, neprilysin (NEP), kallikrein, kininogen (LW & HW) |
| Clinical biochemical biomarker | D-mer, C-reactive protein (CRP), ferritin |
IL-1 interleukin-1, IL-2 interleukin-2, IL-6 interleukin-6, IL-12 interleukin-12, IL-17 interleukin-17, IL-18 interleukin-18, TNF-α tumor necrosis factor alpha, M-CSF macrophage colony-stimulating factor, G-CSF granulocyte colony-stimulating factor, CXCL-10 C-X-C motif chemokine ligand 10, CCL-3 chemokine (C–C motif) ligand 3, CCL-5 chemokine (C–C motif) ligand 5, IFN- γ interferon gamma, MCP-1 monocyte chemoattractant protein-1, CD14 cluster of differentiation 14, CD163 cluster of differentiation 163, TLR2 Toll-like receptor 2, TLR4 Toll-like receptor 4, CD86 cluster of differentiation 86, CD80 cluster of differentiation 80, CD68 cluster of differentiation 68, SOCS3 suppressor of cytokine signaling 3, CD200R receptor for membrane glycoprotein OX-2, CD206 cluster of differentiation 206 also known as the mannose receptor C type 1 (MRC1), PECAM platelet endothelial cell adhesion molecule-1, S1P sphingosine-1-phosphate, VCAM vascular cell adhesion molecule, vWF von Willebrand factor, Tie2 receptor of angiopoietin
POCT electrochemical assays for SARS-CoV-2 virus detection
Besides the challenges of analysis methods encountered when subjected to miniaturization, to enable the production of POCT tools, the quantification of SARS-CoV-2 must be realized at low levels and fast pace. Otherwise, false-negative results could increase the spread rate of the disease through incorrectly tested individuals. Compact and cost-effective devices for fast and accurate detection of the virus are the need of the hour. Recently published POCT electrochemical devices for the detection of COVID19-related diagnostic markers were analyzed and the most important characteristic and figures of merit are summarized in Table 5. For more exhaustive research on COVID19-associated diagnosis tools reporting other detection mechanisms, besides the electrochemical ones, several recent reviews are recommended[121–126].
Table 5.
Examples of electrochemical sensors and biosensors applied for the detection of COVID-19 diagnostic biomarkers
| Analyte | Platform | Bioelement and biomimetic element | Detection method | LOD | Linear range | Interferences | Sample type | Ref |
|---|---|---|---|---|---|---|---|---|
| SARS-CoV-2 antigen nucleoprotein (ncovNP) | GCE/4-ABA/Ab/BSA, BDDE/4-ABA/Ab/BSA, Au-E/4-ATP/Ab/BSA | Antibody | EIS |
0.227 ng/mL (GCE) 0.334 ng/mL (BDDE) 0.362 ng/mL (Au-E) |
0.0044–4.4 ng/mL | IVA, IVB, RSV, EBV, NoV | Saliva swab | [12] |
| Au-TFE/4-ATP/DTSSP/ncovNP-PmPD | MIP | DPV | 0.000027 nM | 0.00000022–0.000333 nM | S1, E2 HCV, BSA, CD48 | Nasopharyngeal swab | [127] | |
| ncovNP, S1-IgG, S1-IgM and CRP | Graphene electrodes/Ab/BSA/HRP-goat anti-rabbit IgG | Antibody | CA | - | 0–5 ng/mL ncovNP, 0–500 ng/mL S1-IgG, 0–500 ng/mL S1-IgM, 0–50 ng/mL CRP | SARS-CoV, MERS-CoV | Saliva and blood | [128] |
| N-gene of SARS-CoV-2 | AuNPs/graphene nanoplatelets | ssDNA | CP | 6.9 copies/µL | 585.4–5.854 × 107 copies/µL | MERS-CoV and SARS-CoV viral RNA genes | Nasopharyngeal and nasal swab, saliva | [129] |
| SARS-CoV-2 spike protein | AuSPE/MB/anti-spike Ab/spike/ACE-2/anti-ACE-2 Ab-biotin/streptavidin-HRP | Antibody | CA | 22.55 ng/mL | 1–106 copies/mL | RBD, β-1,4-GALT-5, MERS, SARS-CoV-1, SARS-CoV-2, VSV pseudovirion | Cell cultures, nasopharyngeal swab | [130] |
| DNA linker (Fc) and antibody/anti-spike S1 protein Ab | DNA and antibody | CA | 0.001 ng/mL | 0.001–0.1 ng/mL | RuV, EBOV, HCoV-229E, HCoV-NL63, MERS-CoV, BcoV | Saliva | [131] | |
| Graphene sheets/anti-spike Ab | Antibody | FET | 0.0001 ng/mL | - | - | Nasopharyngeal swab | [132] | |
| SPCE/AuNPs/MAA/EDC-NHS | Antibody | EIS | 0.0837 pg/mL | - | BSA | Saliva | [133] | |
| SARS-CoV-2 spike protein and cTnI | AuNPs spike protein Ab and cTnI Ab (Si-MOSFET) | Antibody | FET |
0.0001 ng/mL spike protein 0.1 ng/mL cTnI |
- | - | Saliva | [134] |
| SARS-CoV-2 spike S1 protein | FTO/AuNPs/anti-spike S1 protein Ab | Antibody | DPV | 0.00001 nM | 0.000001–1000 nM | HIV, JEV, IAV | Saliva | [135] |
| SPCE/anti-SARS-CoV-2 S1 monoclonal antibody/secondary antibody and HRP-IgG/TMB | Antibody | CA | 0.19 ng/mL | 0.5–10 ng/mL | IAV | Artificial saliva | [136] | |
| Au-TFME/4-ATP/DTSSP/PAPBA | MIP | SWV | 0.000015 nM (0.00112 ng/mL) | - | - | Nasopharyngeal samples | [137] | |
| SARS-CoV-2 spike protein RBD | Co-TNTs | - | CA | 0.7 nM | 14–1400 nM | - | - | [138] |
| SARS-CoV-2 spike protein and N protein | SPCEs/CB/MBs/Abs complex | Antibody | DPV |
19 ng/mL (for S protein) 8 ng/mL (for N protein) |
50–10,000 ng/mL (for S protein) 10–1000 ng/mL (for N protein) |
H1N1 influenza pandemic and seasonal viruses | Saliva and nasopharyngeal swabs | [139] |
| S- and N-genes of SARS-CoV-2 | SiNPs@Mb and AO/RCA | - | DPV | 1.0 copy/µL for both genes | 1–109 copies/µL | IAV, IVB, DNA mismatches | Nasopharyngeal, throat swab | [140] |
| SARS-CoV-2 antibody for spike protein | GCE/Au/CysOH/BSA | S-gene | SWV | 0.00000003 ng/mL | 0.0000001–0.01 ng/mL |
M-S-gene InfA-S-gene Pneu |
Saliva oropharyngeal swab samples |
[141] |
| SARS-CoV-2 antibody for spike protein RBD | 16-well plate integrated with electrodes | RBD antigen | EIS | - | 100,000–10,000,000 ng/mL | - | Serum | [142] |
| SARS-CoV-2 antibodies for spike S1 protein and RBD | 3D Au/rGO/PDMS microfluidic channel | S1 and RBD antigens | EIS |
0.0000028 nMS1 Ab 0.0000169 RBD Ab |
S1 Ab 0.00000001–30 nM RBD Ab 0.00000001–20 nM |
RBD Ab, N Ab, IL-6, S1 Ab | - | [143] |
| SARS-CoV-2 IgG and IgM for S protein | ePAD printed GO electrode/spike protein RBD | Proteins | SWV |
0.96 ng/mL IgG 0.14 ng/mL IgM |
1–1000 ng/mL | Anti-HBsAg, anti-HCV, anti-EBV, anti-Rubella, and anti-CMV | Serum | [144] |
| SARS-CoV-2 IgG antibody for N protein |
SPCE@capillary-flow device NCM/N-proteins/HRP-labeled antibodies |
N-protein antigen | CA | 5 ng/mL | 10–1000 ng/mL | - | Spiked whole human blood | [145] |
| SPCE/CNF@diazonium chemistry/N-protein | N-protein antigen | SWV | 0.0008 ng/mL | 0.001 ng/mL–1000 ng/mL | IVA, HCoV antigens | Spiked nasal swabs | [146] | |
| ORF1ab RNA | SPCE/Au@Fe3O4/CP/HT/Au@SCX8-TB-RGO sandwich assay | RNA | DPV | 0.000000003 nM | 0.00000001–0.001 nM | Mismatches RNAs | Sputum, throat swabs, urine, plasma samples, whole blood, saliva | [147] |
2-ME 2-mercaptoethanol, DTSSP 3,3′-dithiobis [sulfosuccinimidyl propionate], 4-ATP 4-aminothiophenol, 4-ABA 4-aminobenzoic acid, AO acridine orange, Au-E gold-based electrodes, Au-TFE gold-based thin-film electrodes, AuNPs gold nanoparticles, BCoV bovine coronavirus, BDDE boron-doped diamond electrode, BSA bovine serum albumin, CA chronoamperometry, CB carbon black, CD48 cluster of differentiation 48 protein, CMV cytomegalovirus, CNF carbon nanofibers, Co-TNTs cobalt-functionalized TiO2 nanotubes, CP chronopotentiometry, CRP C-reactive protein, CV cyclic voltammetry, cTnI cardiac troponin I, CP capture probe, CysOH mercaptoethanol, DPV differential pulse voltammetry, E2 surface viral antigen, EBV Epstein-Barr virus, EBoV Ebola virus, EIS electrochemical impedance spectroscopy, Fc ferrocene, FET field-effect transistor, FTO fluorine-doped tin oxide electrode, GCE glassy carbon electrode, GO graphene oxide, β-1,4-GALT-5 β-1,4-galactosyltransferase 5, HBsAg hepatitis B surface antigen, HCV hepatitis C virus, HCoV human coronavirus, HCoV-229E human coronavirus strain 229E, HCoV-NL63 human coronavirus strain NL63, HIV human immunodeficiency virus, HRP horseradish peroxidase, IL-6 interleukin-6, IVA influenza A virus, IVB influenza B virus, InfA-S-gene influenza A spike protein, JEV Japanese encephalitis virus, MB magnetic beads, Mb methylene blue, MAA mercaptoacetic acid, M-S-gene MERS-CoV spike protein, NCM nitrocellulose membrane, ncovNP SARS-CoV-2 nucleoprotein, NoV norovirus, PmPD poly-m-phenylenediamine, Pneu Streptococcus pneumoniae antigen, RBD receptor-binding domain, RCA rolling circle amplification, rGO reduced graphene oxide, RuV recombinant Rubella virus, RSV respiratory syncytial virus, S1 subunit of SARS-CoV-2 spike protein, Si-MOSFET metal-oxide semiconductor field-effect transistor, SiNPs silica nanoparticles SCX8 p-sulfocalix[8]arene, SPCE screen-printed carbon electrode, SWV square wave voltammetry, S-gene SARS-CoV-2 spike antigen protein, TMB 3,3′,5,5′-tetramethylbenzidine, Au-TFME thin-film gold electrode, PAPBA poly(3-aminophenylboronic acid), TB toluidine blue, VSV vesicular stomatitis virus
Electrochemical immunosensors for the N-protein of SARS-CoV-2 based on lab-produced and purified anti-SARS-CoV-2 ncovNP antibodies were evaluated in clinical samples. For example, Białobrzeska et al. [12] reported an immunosensor for the RNA binding domain of ncovNP of SARS-CoV-2 at different electrodes (diamond/gold/GCE). The highest non-adsorption effect was seen at the BDDE-modified biosensor, regardless of the low capacity and background currents extending sensory efficiency [12]. Different strategies to replace biological receptors were investigated in the last decades. Besides aptamers as biomimetic elements, MIPs electrochemically generated have been extensively exploited for the sensitive and selective detection of COVID19-related biomarkers based on the antibody-like affinity that allows discrimination among similar molecules [148]. A more sensitive electrochemical approach for the detection of SARS-CoV-2 ncovNP was developed by Raziq et al. [127] based on a MIP disposable sensor chip at thin-film electrodes (TFE). The sensor showed an LOD about twice higher in the nasopharynx swabs of patients (27 fM) [127], but still about 3 orders of magnitude lower than the immunosensors developed by Białobrzeska et al. [12].
A multiplexed, portable, wireless electrochemical platform was developed for the analysis of ncovNP, IgM and IgG antibodies, and the inflammatory biomarker C-reactive protein in saliva and blood at an electrochemical device of four working electrodes of laser-engraved graphene (LEG). The graphene surface was modified by drop-casting the SARS-CoV-2-associated antigen, N-protein, and S1 with the help of a cross-linker reagent to bind with selective immunoglobulin isotypes against both antigens in the same electrode [128]. Another graphene-based electrochemical approach was realized for the detection of the N-gene of SARS-CoV-2 in nasopharyngeal and nasal swab and saliva within 5 min. However, the affinity was realized by means of the hybridization reaction with an antisense ssDNA strand that was immobilized at a graphene-modified paper surface, leading to increased sensitivity [129].
The nucleocapsid and spike proteins of SARS-CoV-2 are the most promising biomarkers for antigen-based rapid diagnostics tests. A sandwich immunosensor enabled the detection of the S-protein with a good sensitivity and a LOD in the ng/mL range, using the streptavidin (poly) HRP-80 enzymatic complex as an amplification system [130]. Another approach that implemented the chronoamperometry for the fast detection (5 min) of S-protein was based on the combination of antibodies against the specific antigen for increased selectivity and DNA linkers tethered with a redox probe (ferrocene) for signal achievement [131]. By contrast, an impedimetric immunoassay enabled the more sensitive detection of S-protein by using AuNPs as electrode modifiers [133]. Seo et al. [132] reported a graphene-based field-effect transistor (FET) biosensor to detect S-protein in the fg/mL range in nasopharyngeal swab samples collected from 19 patients. Another FET electrochemical immunosensor allowed the dual detection of S-protein and cardiac troponin I (cTnI) at a gold-modified glass slide [134], but the LOD was 100 times higher than DNA-sensor proposed by Seo et al. [132]. By contrast, Vadlamani et al. [138] propose the detection of the S-protein within 30 s using a cobalt-functionalized TiO2 nanotube–based sensor. However, both prototypes still need to be validated at different levels of S-protein in clinical samples and in the presence of cross-interferents.
Several assays for the detection of the S1 polypeptide of the S-protein were developed based on antibody-target affinity reaction [135, 136] or biomimetic induced affinity reaction (MIP) [137]. Although the sensing principles were different in terms of the electrode support, detection method, or signal amplification, all approaches enabled the detection of the S1 subunit in the fM to pM range.
The simultaneous quantification of S- and N-proteins was performed by a sandwich immunoassay that used an enzyme (alkaline phosphatase) for both signal generation and amplification. The sensor configuration enabled the detection of S- and N-proteins in untreated saliva as low as ng/mL, within 30 min [139]. One of the recent strategies for DNA amplification is represented by the isothermal technique named rolling circle amplification (RCA) [149]. A voltammetric biosensor that used the RCA amplification for the simultaneous detection of S- and N-genes of SARS-CoV-2 in nasopharyngeal and throat swab was developed by Chaibun et al. [140]. Silicon nanoparticles were functionalized with acridine orange and MB to target the S- and N-genes, respectively. Sandwich hybridization of redox-active labels with RCA amplicons was realized. The efficiency of the method was proven by the very low LOD of 1.0 copy/mL in clinical samples. Hence, the applicability of the sensor was evaluated in 106 clinical samples, the results being fully in accordance standard RT-PCR method [140].
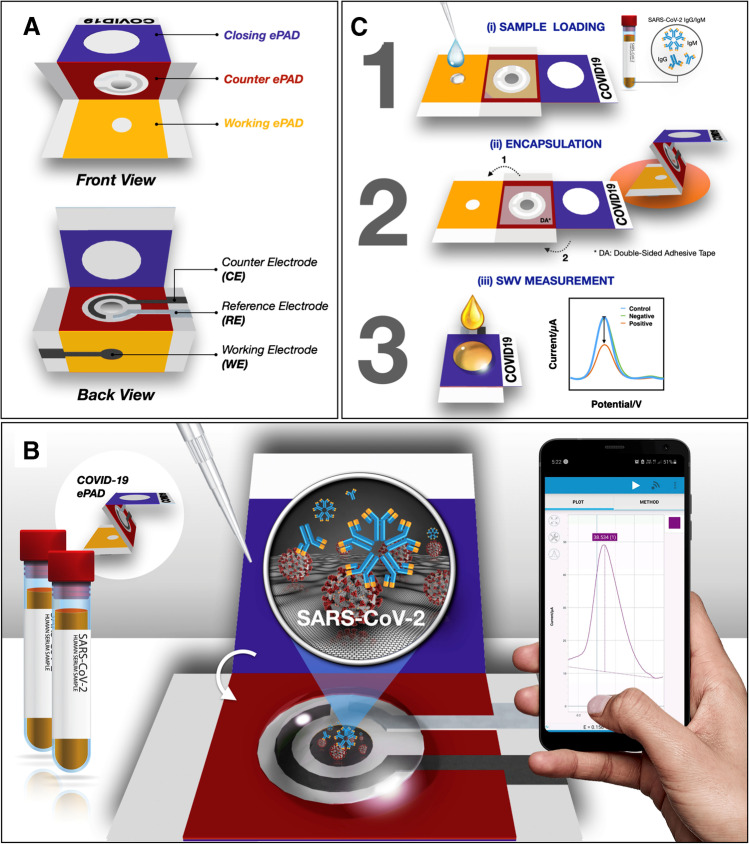
Antibody detection from clinical samples has been proven to be a great alternative to the reference RT-PCR method, particularly after the second week of infection. For example, one voltametric [141] and two impedimetric biosensors were developed for the single detection of SARS-CoV-2 antibodies for the S-protein [142] and simultaneously with the antibodies for the S1 subunit [143]. Besides the multiplexed ability of the approach proposed by Ali et al. [143], the microfluidic channel employed in this sensing strategy enabled the ultrafast (11.5 s) and sensitive (2.8 fM for S1 Ab and 16.9 fM for RBD Ab) detection of the targets. Another advantage of this approach was the regeneration property that was tested in an acidic medium and was performed at least 9 times without any significant change in their performance [143]. A very cheap alternative could be represented by electrochemical paper-based devices (ePADs). An ePAD as a screening tool to detect SARS-CoV-2 immunoglobulins (IgG and IgM) was developed by Yakoh et al. [144]. The sensing scheme relies on the disruption of the redox conversion of [Fe(CN)6]3−/4− which was triggered by the formation of IgG–S-protein immunocomplex (Fig. 4). The fast (30 min) and sensitive detection of SARS-CoV-2 antibodies was recorded with a LOD of 1 ng/mL that enabled the application of the sensor only in serum samples as for human nasopharyngeal swabs the values of IgG and IgM go down to pg/mL [144]. Unlike lateral flow immunoassay (LFA) platforms where multiple antibodies are exploited in charge of the reporter, no antibodies are required if label-free electrochemical systems are applied [150]. Although sensitive and cost-effective, ePADs fail to accurately and uniformly control the flow rate that dramatically influences the performance of the sensor. To this, capillary-driven microfluidic systems were developed to overcome these limitations [151]. SARS-CoV-2 IgG antibodies for N-protein were detected by a low-cost electrochemical capillary-flow device by chronoamperometry. The antibodies were captured on the nitrocellulose membrane and further electrochemically detected at modified SPCEs, with a LOD of 5 ng/mL [145].
Fig. 4.
Schematic representation of the detection procedure of the COVID-19 ePAD for IgG and IgM antibodies. Illustration of the A device components, B detection principle, and C detection procedure of the COVID-19 ePAD. Reprinted with permission by Elsevier [144]
A more sensitive electrochemical biosensor for IgG antibodies for N-protein was developed based on the synergistic effect between electrode modification with CNF and diazonium chemistry for antigen grafting. Unlike other approaches, the sample collection and detection tools are integrated into the same device by coating the SPCEs with absorbing cotton padding [146]. A sandwich assay electrochemical biosensor for the diagnosis of ORF1ab RNA of SARS-CoV-2 was developed based on a nanocomposite of Au@Fe3O4, GO, p-sulfocalix[8]arene (SCX8), AuNPs, and a fluorescent material, like TB, to obtain Au@SCX8-RGO-TB. The LODs of this assay in synthetic solutions and clinical samples were 3 aM and 200 copies/mL, respectively, being the lowest LOD among the published RNA-based sensors [147].
As the antibody response is produced only after 4–6 days since the onset of the infection, one must consider the prevalence of false-negative results and the spread of the disease without suitable diagnostic tools at the proper timing.
Sports biomarkers
Self-monitoring in sports activities has attracted significant attention since there are several markers mirroring the physiological and metabolic changes in the human body. Thus, athletes can monitor their health, performance, and recovery via on-site analysis provided by POC devices. Additionally, dopants can be easily identified/monitored in performance athletes. Unlike pathological biomarkers, physiological biomarkers tend to vary their levels depending on diet, circadian rhythm, training, and rest cycles. The physiological range of most markers also depends on factors such as age, ethnicity, and gender. For regular monitoring, one must correlate all these variables to fully understand the output data; otherwise, wrong conclusions are drawn. Hence, multiplexed analysis of several biomarkers is of interest for better oversight of the overall performance and health status. Moreover, due to high-tech advancements and continuous improvement of smartphone apps, users and trainers have the possibility to optimize regime training, track their nutrition, and online measure their performances. Wearable sensors are even more popular among athletes, due to attributes such as affordability and ergonomics provided by advances in miniaturized electronics, enabling them to monitor physiological parameters without any expert guidance and during physical activities [152]. For example, Table 6 presents a list of wearable electrochemical biosensors for glucose monitoring that can be applied for sport-related activities, but also by patients suffering from diabetes.
Table 6.
Wearable electrochemical biosensors for glucose released on the market. Adapted from [153]
| Wearable platform | Sample | Product/company | Current stage | Website |
|---|---|---|---|---|
| Contact lens | Tears | Smart contact lens, Google, and Novartis | First published in 2014, last update in 2020; the project is on hold | - |
| Smartwatch | Interstitial fluid | GlucoWatch, Cygnus Inc | FDA-approved, but retracted | - |
| Wrist strap | Blood | BioMKR, Prediktor Medical | Under clinical testing for approval and market launch in Europe | https://www.prediktor.com/ |
| Patch | Interstitial fluid | Freestyle Libre, Abbott | FDA-approved in the USA in July 2018 | https://www.freestyle.abbott/us-en/home.html |
| Patch | Interstitial fluid | Dexcom G6 CGM, Dexcom | FDA-approved | https://www.dexcom.com/global |
| Patch | Sweat | MAX3013, Maxim Integrated | Active in production | https://www.maximintegrated.com |
| Extra-small stick to be placed under the lower eyelid | Tears | NovioSense tear glucose sensor, NovioSense | Phase 2 Clinical Trial | http://noviosense.com/ |
More insights about sports biomarker classification and their detection by laboratory and POCT can be found in some recent reviews [154, 155]. A list of sports biomarkers was reported and classified into: (i) performance markers (i.e., testosterone, cortisol, growth hormone, insulin-like growth factor-1, erythropoietin, soluble transferrin receptor, hepcidin, lactate, taurine, glutamine, branched chained amino acids, estrogen, progesterone); (ii) injury, inflammation, and recovery markers (i.e., S-100B, neurofilament light, Tau protein, C-reactive protein, interleukin-6, creatine kinase); and (iii) nutrition markers (i.e., glucose, albumin, blood urea nitrogen, vitamin D).
Injuries among athletes are very common and the determination of the state of the injury is important in the recovery and healing process because it could aid practitioners in implementing the best therapy. Although mainly secreted in high levels into the CSF, the markers are also expressed at lower levels in the bloodstream [156]. To be noted that not many biomarkers reveal the exact state of injuries, the majority of them being non-specific. Besides injury, inflammation is also implicated in the physio-pathological sports-correlated processes. Biomarkers for muscle damage and inflammation often go hand-in-hand leveling up to even 100 times after intensive exercise, being an effect of the body’s immune response [154]. Therefore, sensitive POC devices for the detection of injury, inflammation, and recovery biomarkers could help athletes to schedule their training sessions depending on their health status.
There are several potential POC devices reporting the analysis of inflammation biomarkers, such as cortisol [157–159], C-reactive protein [160–162], Tau protein [163–166], or S-100B [167]. For example, cortisol was analyzed using an impedimetric SPCE-modified electrochemical cell [157] and a voltammetric Au-interdigitated modified microelectrode [158] from saliva and plasma, respectively. By contrast, the detection of cortisol as low as 100 pM in saliva regardless of the presence of interferences such as β-estradiol, testosterone, progesterone, or corticosterone was realized using a voltammetric immunosensor [159]. Liu et al. [167] developed a disposable microchip immunosensor for S-100B based on a PMMA channel functionalized with S-100B-specific monoclonal antibodies. Upon the affinity reaction, polyclonal anti-S100 were sequentially coupled by antigen–antibody specific interaction, followed by the conjugation with alkaline phosphatase (ALP). The strategy enabled the sensitive detection of S-100B as low as 0.1 pg/mL [167].
However, these biomarkers are commonly expressed after a traumatic event or in neurodegenerative disorders and a few reported papers in the literature make a connection with the levels over a sports activity. Currently, performance and nutrition markers are more subjected to the development of wearable devices for online monitoring [155].
One challenge is associated with the expression site of inflammation markers. Despite performance and nutrition markers, injury and inflammation biomarkers are usually measured in serum or plasma. However, inflammation may occur locally, in abscesses [168]. Nevertheless, some latest studies show that there are injury and inflammation biomarkers expressed in saliva or perspiration [157, 169]; therefore, novel approaches for POC development for applications in sports science could be explored.
Conclusions, future perspectives, and challenges
The improvement of health care services is primarily based on the improvement of the management in the health system, which, in turn, is directly correlated with a quick decision regarding diagnosis and treatment based on a functional diagnostics system, which also benefits from a consistent and well-documented smart therapeutics system. Nowadays, the concept of smart therapeutics must first of all consider the patient’s profile and thus every decision in terms of progression and monitoring evaluation must be personalized with his particularities and needs. The need of the hour is detecting relevant markers at the clinical point-of-care/use by a cheap, user-friendly, sensitive, and reliable detection platform that may facilitate rapid treatment and disease prevention. Especially, medical and sports fields could tremendously benefit from POC-based technologies with superior specificity and sensitivity. Hence, fast and reliable analyses may shorten the output of a disease or offer critical information over a patient’s health status. However, key points and challenges for POCT accreditation that must be addressed are (i) method performance and validation, (ii) internal and external quality assurance, (iii) staff/user training and competency, and (iv) continuous improvement [8].
Electrochemical (bio)sensors have attracted attention for the development of smart diagnosis tools with great potential for POCT applications needed for personalized health care, especially due to their advantages, which are related to the suitability for portability and miniaturization, large-scale and low-cost production, high sensitivity wide detection range, and low detection limits, as well as easy integration on other systems. The recent developments in the field of nanoscience and nanotechnology, the discovery of smart electroactive functionalized nanostructures allowing for signal amplification, emerging micro-electronics such as miniaturized analyzer, and innovative fabrication technologies such as interdigitated electrodes have also been useful to design and develop miniaturized, automated, and precise sensing systems suitable for clinical applications.
The WHO regulation regarding POCT devices is clear, and according to it, only devices that fully meet the following criteria: “Affordable,” “Sensitive,” “Specific,” “User-friendly,” “Robust and rapid,” “Equipment-free,” and “Deliverable” to all people needing, which are included under the generic name ASSURED, can be included in this category. After a careful analysis of the recent literature data on the subject of this study, there are many studies that meet most of the criteria mentioned in the WHO regulations, these being centralized in Table 7. Taking into account that none of the presented devices are commercially available and are not in clinical trials, we included in the “Fully” category all the devices that meet the ASSURED criteria except for the last one, namely to be “Deliverable to all people need.” Also, it can be observed that most of the detection devices presented do not meet the “Equipment-free” criterion, and this shortcoming is due to the operation mode of the electrochemical sensors and biosensors, which require the presence of a potentiostat and implicitly an energy source. In several studies from the examples presented, it was possible to solve this shortcoming by developing miniaturized, portable, and ultraportable potentiostats, accessible in terms of price and which allow the operation of the elaborated sensors in a decentralized manner [36, 42, 71, 98, 104, 128–130, 136, 137, 139, 141, 144, 146, 147, 149, 152, 158, 159]. In addition, taking into account the special progress in the field of electronics in recent years, we are confident that this shortcoming will be overcome very soon, especially if the advantages that accompany electrochemical detection systems are considered. Among these, we mention the high sensitivity ensured by the easy functionalization with nanomaterials, the high selectivity when using biological or biomimetic elements, the fast response, but especially their suitability for miniaturization and automation, basic properties in the field of POCT sensing devices. It can be observed that only one example of detection devices does not meet the criteria “Specific” [36], respectively, “Sensitive” [150], which can be a justification for the large number of recent studies that include electrochemical sensors and biosensors aimed at the development of POCT devices for biomedical and clinical practice, where real, biological samples are very complex in composition and usually contain very low concentrations of analytes.
Table 7.
Comparative presentation of the degree of fulfillment of the ASSURED criteria for the examples of electrochemical sensors and biosensors included in the current study
| Electrochemical sensor configuration/biomarker | Meeting the ASSURED criteria | Unfulfilled criteria | Tested in clinical-related settings | Commercial availability | Ref |
|---|---|---|---|---|---|
| Fully automated lab-on-a-chip-based biosensor device prototype (MiSens)/PSA | Partially | Equipment-free; deliverable | Yes | No | [15] |
| Electrochemical MIP–based detection device/IL-6 | Partially | Equipment-free; deliverable | No | No | [32] |
| Self-assembled peptide–modified flexible field effect transistor/tyrosinase | Partially | Specific; deliverable | No | No | [36] |
| Laser-scribed graphene MIP–based electrochemical sensor/Her-2 | Fully | Deliverable | No | No | [71] |
| Laser-scribed graphene electrochemical aptasensor/Her-2 | Partially | Specific; deliverable | No | No | [51] |
| Sandwich-type electrochemical immunosensor/PSA | Partially | Equipment-free; deliverable | No | No | [72] |
| Sandwich-type portable biosensor device/PSA | Partially | Equipment-free; deliverable | Yes | No | [39] |
| Amperometric immunosensor/CA 15–3 | Partially | Equipment-free; deliverable | No | No | [75] |
| Electrochemical immunosensor/TNF-α | Partially | Equipment-free; deliverable | Yes | No | [56] |
| Self-calibrating IoT portable electrochemical immunosensor/HE4 | Fully | Deliverable | Yes | No | [42] |
| MIP-based electrochemical sensor/CA15-3 | Partially | Equipment-free; deliverable | No | No | [78] |
| MIP-based electrochemical sensor/CA15-3 | Partially | Equipment-free; deliverable | No | No | [79] |
| Electrochemical MIP-based sensor/CEA | Partially | Equipment-free; deliverable | No | No | [65] |
| 3D-printed electrochemical aptasensor/MUC 1 | Partially | Equipment-free; deliverable | Yes | No | [34] |
| Electrochemical immunosensor/CA15-3 and microRNA-21 | Partially | Equipment-free; deliverable | No | No | [58] |
| Stretchable and transparent electrochemical cell–sensing platform/H2O2 | Partially | Equipment-free; deliverable | No | No | [60] |
| Amperometric sensor/endogenous H2O2 | Partially | Equipment-free; deliverable | Yes | No | [61] |
| Flexible nanohybrid microelectrode amperometric sensor/Endogenous H2O2 | Partially | Equipment-free; deliverable | Yes | No | [81] |
| Electrochemical label-free immunosensor/IL-6 | Fully | Deliverable | No | No | [98] |
| MIP-based electrochemical sensor/IL-6 | Partially | Equipment-free; deliverable | No | No | [103] |
| Electrochemical immunosensor/P53 protein | Fully | Deliverable | Yes | No | [104] |
| 5 Amperometric immunosensor/IL-6;TNF-α | Partially | Equipment-free; deliverable | No | No | [109] |
| Flexible electrochemical immunosensor/PARK7/DJ-1 | Partially | Equipment-free; deliverable | Yes | No | [110] |
| MIP-based electrochemical sensor/ncovNP | Fully | Deliverable | Yes | No | [128] |
| Electrochemical immunosensor/ncovNP, S1-IgG, S1-IgM, and CRP | Fully | Deliverable | Yes | No | [129] |
| Paper-based electrochemical sensor chip/N-gene of SARS-CoV-2 | Partially | Equipment-free; deliverable | Yes | No | [130] |
| Electrochemical immunosensor/SARS-CoV-2 spike protein | Fully | Deliverable | Yes | No | [131] |
| Electrochemical immunosensor with DNA linker/SARS-CoV-2 Spike protein | Partially | Equipment-free; deliverable | Yes | No | [133] |
| Amperometric immunosensor/SARS-CoV-2 spike protein RBD | Partially | Equipment-free; deliverable | No | No | [135] |
| Amperometric immunosensor/SARS-CoV-2 spike S1 protein | Fully | Deliverable | No | No | [136] |
| Amperometric immunosensor/SARS-CoV-2 spike S1 protein | Fully | Deliverable | No | No | [137] |
| MIP-based electrochemical sensor/SARS-CoV-2 spike S1 protein | Fully | Deliverable | Yes | No | [139] |
| Amperometric immunosensor/SARS-CoV-2 spike protein and N protein | Fully | Deliverable | Yes | No | [149] |
| Electrochemical sensor/S- and N-genes of SARS-CoV-2 | Fully | Deliverable | Yes | No | [141] |
| Electrochemical sensor/SARS-CoV-2 antibodies for spike S1 protein and RBD | Fully | Deliverable | No | No | [144] |
| Paper-based electrochemical sensor/SARS-CoV-2 IgG and IgM for S protein | Partially | Sensitive; deliverable | Yes | No | [150] |
| Electrochemical capillary-flow device/SARS-CoV-2 IgG antibody for N protein | Fully | Deliverable | Yes | No | [146] |
| Cotton-tipped electrochemical immunosensor/SARS-CoV-2 IgG antibody for N protein | Fully | Deliverable | Yes | No | [147] |
| Ultrasensitive sandwich-type electrochemical sensor/ORF1ab RNA | Fully | Deliverable | Yes | No | [152] |
| Portable and microfluidic electrochemical device/cortisol | Fully | Deliverable | Yes | No | [158] |
| Portable and microfluidic electrochemical device/cortisol | Fully | Deliverable | Yes | No | [159] |
| Disposable electrochemical biosensor/creatine kinase | Partially | Equipment-free; deliverable | Yes | No | [161] |
The development of electrochemical (bio)sensors usually involves a laborious protocol with functionalization steps with nanomaterials and biocomponents, which can represent a drawback. However, the development of the electrochemical sensors is performed before use depending on their stability. Thus, at the moment of the analysis, they can be directly used, obtaining the results easier and faster than in the case of the standard methods applied in clinical analysis. For example, the RT-PCR results may take 1–2 days to report and are expensive, and require laboratory equipment and highly qualified personnel, rapid POCT diagnostic tests provide the possibility of early detection of infectious COVID-19 cases, and many have been developed since the onset of the disease [170]. Another disadvantage encountered in some of the examples of POCT discussed previously is the lack of comparison with the standard methods used for the analysis of those biomarkers in clinical practice. However, it has been observed recently that more importance has been given to the validation of new methods and devices in relation to standard methods.
Concerning the samples for POC analysis, saliva is considered one of the most compliant biological fluids due to the minimally invasive prelevation methods and ease of manipulation and storage. Being rich in compounds that can be used as markers, saliva is an important tool to assure an easy and simple diagnosis of several diseases [119, 171]. However, further clinical trials are needed to establish the role of each salivary molecule as a marker for health status or disease monitoring as little is known about the correlation between the level of biomarkers in the blood or the fluid where it is secreted and its level in saliva.
Another advantage of using electrochemical sensors is that both potentiostats and electrochemical cells could be integrated into a whole disposable system that would eliminate the need for any dedicated instrumentation as the tests could be run from a smartphone only, making it useable at the point-of-need/use. Portable nano-devices incorporating a cocktail of tests would be ideal for large screening of the population, especially during disease outbreaks, but also for telemedicine diagnosis and monitoring, and sports science. The need for widespread analysis and control over the spread of different pathogens has previously faced challenges either due to lack of instrumentation or reduced accuracy of the tests. The use of POCT-based detection devices is more and more often associated with the so-called mobile health (mHealth) equipment. Many wearable sensors (wrist bands, chest straps, and skin mountings) incorporate the integrated sensing transducer, circuitry, biomolecules, and power sources for continuous monitoring of relevant markers. However, the flexibility of materials and users’ comfort could suffer some improvements to make wearable sensors more user-friendly and cost-effective [172, 173].
Driven by a highly competitive market, innovative technologies, AI, and IoT have become the pile point of companies. Smartphones are beyond being a luxury, but an integral part of human lifestyle, keeping all of us connected to worldwide data. Sports sciences have benefited the most from the smartphone technology, where sports activities and health apps are popular among athletes and smartphone users [174]. Recent advancements in POCT domain enabled the integration of an analytical platform with smartphones to allow increased mobility, accuracy, and user-friendliness. Although sometimes futuristic, modern technologies have as ultimate goal the development of fast diagnostic and monitoring tools to reduce hospital stays and overall costs and improve life expectancy and style.
Without the aim to cover all POCT electrochemical sensing approaches for the determination of inflammation-related biomarkers, this review treats in a critical manner the importance of this emerging scientific topic. Nowadays, it is expected that the monitoring of biomarkers involved in inflammatory processes occurring in several pathological conditions will gain more interest in healthcare management.
Monitoring inflammation biomarkers may aid physicians in their practice. In this regard, the use of various electrochemical approaches toward multiplexed detection of inflammatory biomarkers, in particular, can be of much help. Since POCT devices are characterized by small dimensions, low cost, and high sensitivity and it allows the real-time determination of biomarkers through online-assisted equipment, they offer an excellent perspective for easily obtaining an accurate diagnosis. We can assume that all the efforts and research in this field will overcome the present obstacles and barriers, and the integration of innovative nanomaterials, nanocomposites, microfluidic systems, wireless transmission of the data, and mobile-based biosensing assays will contribute to enhanced overall analytical performance of the developed POCT.
Author contribution
All authors contributed to the study conception and design. Material preparation and data collection were performed by Diana-Gabriela Macovei and Maria-Bianca Irimes. Data collection and analysis and the first draft of the manuscript were performed and written by Diana-Gabriela Macovei, Maria-Bianca Irimes, Oana Hosu, and Mihaela Tertis. Cecilia Cristea critically revised the manuscript and supervised the work. All authors reviewed and approved the final manuscript.
Funding
This work was supported by the Romanian Ministry of Education and Research, CNCS-UEFISCDI, project number PN–III–P1-1.1-TE-2021–1543, and the “Iuliu Hatieganu” University of Medicine and Pharmacy Cluj-Napoca, Romania for the internal grant number 35184/17.12.2021.
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Published in the topical collection Electrochemical Biosensors – Driving Personalized Medicine with guest editors Susana Campuzano Ruiz and Maria Jesus Lobo-Castañón.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Diana-Gabriela Macovei and Maria-Bianca Irimes contributed equally to this work.
References
- 1.The Editors of Encyclopaedia Britannica. Inflammation | Definition, Symptoms, Treatment, & Facts | Britannica. Encycopaedia Br. Inc.; 2019.
- 2.Chakraborty C, Sharma AR, Sharma G, Lee SS. The interplay among miRNAs, major cytokines, and cancer-related inflammation. Mol Ther - Nucleic Acids. 2020;20:606–620. doi: 10.1016/J.OMTN.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kany S, Vollrath JT, Relja B. Cytokines in inflammatory disease. Int J Mol Sci. 2019;20.10.3390/IJMS20236008. [DOI] [PMC free article] [PubMed]
- 4.Rosival L. Biomarkers. Lek Obz. 2022;49:693–724. doi: 10.1016/B978-0-12-820472-6.00060-8. [DOI] [Google Scholar]
- 5.Califf RM. Biomarker definitions and their applications. Exp Biol Med. 2018;243:213–221. doi: 10.1177/1535370217750088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.biomarker | biology | Britannica. https://www.britannica.com/science/biomarker. Accessed 4 Jul 2022
- 7.Khusnurrokhman G, Wati FF. Tumor-promoting inflammation in lung cancer: a literature review. Ann Med Surg. 2022;79:104022. doi: 10.1016/J.AMSU.2022.104022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oliver P, Fernandez-Calle P, Buno A. POCT accreditation ISO 15189 and ISO 22870: making the point. Electron J Int Fed Clin Chem Lab Med. 2021;32:131–139. [PMC free article] [PubMed] [Google Scholar]
- 9.Hosu O, Florea A, Cristea C, Sandulescu R. Advanced biosensors for health care applications. Amsterdam, The Netherlands: Elsevier; 2019. Functionalized advanced hybrid materials for biosensing applications; pp. 171–207. [Google Scholar]
- 10.Global Electrochemical Sensors Market - 2022–2029, DataM Intelligence 4Market Research LLP. 2022. https://www.marketresearch.com/DataM-Intelligence-4Market-Research-LLP-v4207/Global-Electrochemical-Sensors-31490006/.
- 11.Campuzano S, Pedrero M, Yáñez-Sedeño P, Pingarrón JM. New challenges in point of care electrochemical detection of clinical biomarkers. Sensors Actuators B Chem. 2021;345:130349. doi: 10.1016/J.SNB.2021.130349. [DOI] [Google Scholar]
- 12.Białobrzeska W, Ficek M, Dec B, Osella S, Trzaskowski B, Jaramillo-Botero A, Pierpaoli M, Rycewicz M, Dashkevich Y, Łęga T, Malinowska N, Cebula Z, Bigus D, Firganek D, Bięga E, Dziąbowska K, Brodowski M, Kowalski M, Panasiuk M, Gromadzka B, Żołędowska S, Nidzworski D, Pyrć K, Goddard WA, Bogdanowicz R. Performance of electrochemical immunoassays for clinical diagnostics of SARS-CoV-2 based on selective nucleocapsid N protein detection: boron-doped diamond, gold and glassy carbon evaluation. Biosens Bioelectron. 2022;209:114222. doi: 10.1016/j.bios.2022.114222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mathew M, Radhakrishnan S, Vaidyanathan A, Chakraborty B, Rout CS. Flexible and wearable electrochemical biosensors based on two-dimensional materials: recent developments. Anal Bioanal Chem. 2020;4133(413):727–762. doi: 10.1007/S00216-020-03002-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oktaviyanti IK, Ali DS, Awadh SA, Opulencia MJC, Yusupov S, Dias R, Alsaikhan F, Mohammed MM, Sharma H, Mustafa YF, Saleh MM. Recent advances on applications of immunosensing systems based on nanomaterials for CA15-3 breast cancer biomarker detection. Anal Bioanal Chem. 2022;2022:1–12. doi: 10.1007/S00216-022-04150-Z. [DOI] [PubMed] [Google Scholar]
- 15.Uludag Y, Narter F, Sağlam E, Köktürk G, Gök MY, Akgün M, Barut S, Budak S. An integrated lab-on-a-chip-based electrochemical biosensor for rapid and sensitive detection of cancer biomarkers. Anal Bioanal Chem. 2016;40827(408):7775–7783. doi: 10.1007/S00216-016-9879-Z. [DOI] [PubMed] [Google Scholar]
- 16.Xu J, Yu X, Xie L, Shao M. Facile incorporation of DNA-templated quantum dots for sensitive electrochemical detection of the oral cancer biomarker interleukin-8. Anal Bioanal Chem. 2020;41211(412):2599–2606. doi: 10.1007/S00216-020-02487-X. [DOI] [PubMed] [Google Scholar]
- 17.Yáñez-Sedeño P, Campuzano S, Pingarrón JM. Screen-printed electrodes: promising paper and wearable transducers for (bio)sensing. Biosensors. 2020;10:76. doi: 10.3390/BIOS10070076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kokkinos C, Economou A, Prodromidis MI. Electrochemical immunosensors: critical survey of different architectures and transduction strategies. TrAC Trends Anal Chem. 2016;79:88–105. doi: 10.1016/j.trac.2015.11.020. [DOI] [Google Scholar]
- 19.Dhiman A, Kalra P, Bansal V, Bruno JG, Sharma TK. Aptamer-based point-of-care diagnostic platforms. Sensors Actuators B Chem. 2017;246:535–553. doi: 10.1016/j.snb.2017.02.060. [DOI] [Google Scholar]
- 20.Chang JYH, Ladame S. Diagnostic, prognostic, and predictive biomarkers for cancer.Bioeng Innov Solut Cancer. 2020;3–21.10.1016/B978-0-12-813886-1.00001-2.
- 21.Hassanpour S, Hasanzadeh M. Label-free electrochemical-immunoassay of cancer biomarkers: recent progress and challenges in the efficient diagnosis of cancer employing electroanalysis and based on point of care (POC) Microchem J. 2021;168:106424. doi: 10.1016/J.MICROC.2021.106424. [DOI] [Google Scholar]
- 22.Muñoz-San Martín C, Gamella M, Pedrero M, Montero-Calle A, Pérez-Ginés V, Camps J, Arenas M, Barderas R, Pingarrón JM, Campuzano S. Anticipating metastasis through electrochemical immunosensing of tumor hypoxia biomarkers. Anal Bioanal Chem. 2021;4141(414):399–412. doi: 10.1007/S00216-021-03240-8. [DOI] [PubMed] [Google Scholar]
- 23.Crulhas BP, Karpik AE, Delella FK, Castro GR, Pedrosa VA. Electrochemical aptamer-based biosensor developed to monitor PSA and VEGF released by prostate cancer cells. Anal Bioanal Chem. 2017;40929(409):6771–6780. doi: 10.1007/S00216-017-0630-1. [DOI] [PubMed] [Google Scholar]
- 24.Cancer. https://www.who.int/news-room/fact-sheets/detail/cancer. Accessed 28 Apr 2022
- 25.Introduction - Accelerating the Development of Biomarkers for Drug Safety - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK32710/#ch1.r1. Accessed 28 Apr 2022
- 26.Dervisevic M, Alba M, Adams TE, Prieto-Simon B, Voelcker NH. Electrochemical immunosensor for breast cancer biomarker detection using high-density silicon microneedle array. Biosens Bioelectron. 2021;192:113496. doi: 10.1016/J.BIOS.2021.113496. [DOI] [PubMed] [Google Scholar]
- 27.Normanno N, Apostolides K, de Lorenzo F, Beer PA, Henderson R, Sullivan R, Biankin AV, Horgan D, Lawler M. Cancer biomarkers in the era of precision oncology: addressing the needs of patients and health systems. Semin Cancer Biol. 2021 doi: 10.1016/J.SEMCANCER.2021.08.002. [DOI] [PubMed] [Google Scholar]
- 28.Zhang W, Xiao G, Chen J, Wang L, Hu Q, Wu J, Zhang W, Song M, Qiao J, Xu C. Electrochemical biosensors for measurement of colorectal cancer biomarkers. Anal Bioanal Chem. 2021;4139(413):2407–2428. doi: 10.1007/S00216-021-03197-8. [DOI] [PubMed] [Google Scholar]
- 29.Gonçalves M de L, Truta LAN, Sales MGF, Moreira FTC. Electrochemical point-of care (PoC) determination of interleukin-6 (IL-6) using a pyrrole (Py) molecularly imprinted polymer (MIP) on a carbon-screen printed electrode (C-SPE). 2021;54:2611–2623. 10.1080/00032719.2021.1879108.
- 30.Zhang C, Shi D, Li X, Yuan J. Microfluidic electrochemical magnetoimmunosensor for ultrasensitive detection of interleukin-6 based on hybrid of AuNPs and graphene. Talanta. 2022;240:123173. doi: 10.1016/J.TALANTA.2021.123173. [DOI] [PubMed] [Google Scholar]
- 31.Bondancia TJ, Soares AC, Popolin-Neto M, Gomes NO, Raymundo-Pereira PA, Barud HS, et al. Oliveira ON. Low-cost bacterial nanocellulose-based interdigitated biosensor to detect the p53 cancer biomarker. Mater Sci Eng C. 2022;112676.10.1016/J.MSEC.2022.112676. [DOI] [PubMed]
- 32.Ren H, Xu T, Liang K, Li J, Fang Y, Li F, Chen Y, Zhang H, Li D, Tang Y, Wang Y, Song C, Wang H, Zhu B. Self-assembled peptides-modified flexible field-effect transistors for tyrosinase detection. iScience. 2022;25:103673. doi: 10.1016/J.ISCI.2021.103673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rebelo TSCR, Ribeiro JA, Sales MGF, Pereira CM. Electrochemical immunosensor for detection of CA 15–3 biomarker in point-of-care. Sens Bio-Sensing Res. 2021;33:100445. doi: 10.1016/J.SBSR.2021.100445. [DOI] [Google Scholar]
- 34.Pothipor C, Bamrungsap S, Jakmunee J, Ounnunkad K. A gold nanoparticle-dye/poly(3-aminobenzylamine)/two dimensional MoSe2/graphene oxide electrode towards label-free electrochemical biosensor for simultaneous dual-mode detection of cancer antigen 15–3 and microRNA-21. Colloids Surfaces B Biointerfaces. 2022;210:112260. doi: 10.1016/J.COLSURFB.2021.112260. [DOI] [PubMed] [Google Scholar]
- 35.Khoshroo A, Mazloum-Ardakani M, Forat-Yazdi M. Enhanced performance of label-free electrochemical immunosensor for carbohydrate antigen 15–3 based on catalytic activity of cobalt sulfide/graphene nanocomposite. Sensors Actuators B Chem. 2018;255:580–587. doi: 10.1016/J.SNB.2017.08.114. [DOI] [Google Scholar]
- 36.Shawky AM, El-Tohamy M. Signal amplification strategy of label-free ultrasenstive electrochemical immunosensor based ternary Ag/TiO2/rGO nanocomposites for detecting breast cancer biomarker CA 15–3. Mater Chem Phys. 2021;272:124983. doi: 10.1016/J.MATCHEMPHYS.2021.124983. [DOI] [Google Scholar]
- 37.Pacheco JG, Silva MSV, Freitas M, Nouws HPA, Delerue-Matos C. Molecularly imprinted electrochemical sensor for the point-of-care detection of a breast cancer biomarker (CA 15–3) Sensors Actuators B Chem. 2018;256:905–912. doi: 10.1016/J.SNB.2017.10.027. [DOI] [Google Scholar]
- 38.Ribeiro JA, Pereira CM, Silva AF, Sales MGF. Disposable electrochemical detection of breast cancer tumour marker CA 15–3 using poly(toluidine blue) as imprinted polymer receptor. Biosens Bioelectron. 2018;109:246–254. doi: 10.1016/J.BIOS.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 39.Ehzari H, Samimi M, Safari M, Gholivand MB. Label-free electrochemical immunosensor for sensitive HER2 biomarker detection using the core-shell magnetic metal-organic frameworks. J Electroanal Chem. 2020;877:114722. doi: 10.1016/J.JELECHEM.2020.114722. [DOI] [Google Scholar]
- 40.Lahcen AA, Rauf S, Aljedaibi A, de Oliveira Filho JI, Beduk T, Mani V, Alshareef HN, Salama KN. Laser-scribed graphene sensor based on gold nanostructures and molecularly imprinted polymers: application for Her-2 cancer biomarker detection. Sensors Actuators B Chem. 2021;347:130556. doi: 10.1016/J.SNB.2021.130556. [DOI] [Google Scholar]
- 41.Rauf S, Lahcen AA, Aljedaibi A, Beduk T, de Oliveira I, Filho J, Salama KN. Gold nanostructured laser-scribed graphene: a new electrochemical biosensing platform for potential point-of-care testing of disease biomarkers. Biosens Bioelectron. 2021;180:113116. doi: 10.1016/J.BIOS.2021.113116. [DOI] [PubMed] [Google Scholar]
- 42.Lah ZMANH, Ahmad SAA, Zaini MS, Kamarudin MA. An electrochemical sandwich immunosensor for the detection of HER2 using antibody-conjugated PbS quantum dot as a label. J Pharm Biomed Anal. 2019;174:608–617. doi: 10.1016/J.JPBA.2019.06.024. [DOI] [PubMed] [Google Scholar]
- 43.Yadav AK, Gulati P, Sharma R, Thakkar A, Solanki PR. Fabrication of alkoxysilane substituted polymer-modified disposable biosensing platform: towards sperm protein 17 sensing as a new cancer biomarker. Talanta. 2022;243:123376. doi: 10.1016/J.TALANTA.2022.123376. [DOI] [PubMed] [Google Scholar]
- 44.Azzouzi S, Ben Ali M, Bellagambi F, Elaissari A, Jaffrezic-Renault N, Errachid A, Zine N. Spatially hierarchical nano-architecture for real time detection of Interleukin-8 cancer biomarker. Talanta. 2022;246:123436. doi: 10.1016/J.TALANTA.2022.123436. [DOI] [PubMed] [Google Scholar]
- 45.Carneiro LPT, Pinto AMFR, Mendes A, Goreti M. An all-in-one approach for self-powered sensing: a methanol fuel cell modified with a molecularly imprinted polymer for cancer biomarker detection. J Electroanal Chem. 2022;906:116009. doi: 10.1016/J.JELECHEM.2022.116009. [DOI] [Google Scholar]
- 46.Freitas M, Neves MMPS, Nouws HPA, Delerue-Matos C. Quantum dots as nanolabels for breast cancer biomarker HER2-ECD analysis in human serum. Talanta. 2020;208:120430. doi: 10.1016/J.TALANTA.2019.120430. [DOI] [PubMed] [Google Scholar]
- 47.Alarfaj NA, El-Tohamy MF, Oraby H. New label-free ultrasensitive electrochemical immunosensor-based Au/MoS2/rGO nanocomposites for CA 27–29 breast cancer antigen detection. New J Chem. 2018;42:11046–11053. doi: 10.1039/C8NJ01388H. [DOI] [Google Scholar]
- 48.Zhang M, Hu X, Mei L, Zhang L, Wang X, Liao X, Qiao X, Hong C. PSA detection electrochemical immunosensor based on MOF-235 nanomaterial adsorption aggregation signal amplification strategy. Microchem J. 2021;171:106870. doi: 10.1016/J.MICROC.2021.106870. [DOI] [Google Scholar]
- 49.Medetalibeyoglu H, Kotan G, Atar N, Yola ML. A novel and ultrasensitive sandwich-type electrochemical immunosensor based on delaminated MXene@AuNPs as signal amplification for prostate specific antigen (PSA) detection and immunosensor validation. Talanta. 2020;220:121403. doi: 10.1016/J.TALANTA.2020.121403. [DOI] [PubMed] [Google Scholar]
- 50.Suresh L, Brahman PK, Reddy KR, Bondili JS. Development of an electrochemical immunosensor based on gold nanoparticles incorporated chitosan biopolymer nanocomposite film for the detection of prostate cancer using PSA as biomarker. Enzyme Microb Technol. 2018;112:43–51. doi: 10.1016/J.ENZMICTEC.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 51.Feng J, Li Y, Li M, Li F, Han J, Dong Y, Chen Z, Wang P, Liu H, Wei Q. A novel sandwich-type electrochemical immunosensor for PSA detection based on PtCu bimetallic hybrid (2D/2D) rGO/g-C3N4. Biosens Bioelectron. 2017;91:441–448. doi: 10.1016/J.BIOS.2016.12.070. [DOI] [PubMed] [Google Scholar]
- 52.Zheng J, Zhao H, Ning G, Sun W, Wang L, Liang H, Xu H, He C, Li CP. A novel affinity peptide–antibody sandwich electrochemical biosensor for PSA based on the signal amplification of MnO2-functionalized covalent organic framework. Talanta. 2021;233:122520. doi: 10.1016/J.TALANTA.2021.122520. [DOI] [PubMed] [Google Scholar]
- 53.Farschi F, Saadati A, Hasanzadeh M. A novel immunosensor for the monitoring of PSA using binding of biotinylated antibody to the prostate specific antigen based on nano-ink modified flexible paper substrate: efficient method for diagnosis of cancer using biosensing technology. Heliyon. 2020;6:e04327. doi: 10.1016/J.HELIYON.2020.E04327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ibau C, Md Arshad MK, Subash CBG, Nuzaihan M, Fathil MFM, Estrela P. Gold interdigitated triple-microelectrodes for label-free prognosticative aptasensing of prostate cancer biomarker in serum. Biosens Bioelectron. 2019;136:118–127. doi: 10.1016/J.BIOS.2019.04.048. [DOI] [PubMed] [Google Scholar]
- 55.Xu Q, Jia H, Duan X, Lu L, Tian Q, Chen S, Xu J, Jiang F. Label-free electrochemical immunosensor for the detection of prostate specific antigen based three-dimensional Au nanoparticles/MoS2-graphene aerogels composite. Inorg Chem Commun. 2020;119:108122. doi: 10.1016/J.INOCHE.2020.108122. [DOI] [Google Scholar]
- 56.Shi YC, Wang AJ, Yuan PX, Zhang L, Luo X, Feng JJ. Highly sensitive label-free amperometric immunoassay of prostate specific antigen using hollow dendritic AuPtAg alloyed nanocrystals. Biosens Bioelectron. 2018;111:47–51. doi: 10.1016/J.BIOS.2018.03.052. [DOI] [PubMed] [Google Scholar]
- 57.Li J, Jiang M, Su M, Tian L, Shi W, Yu C. Stretchable and transparent electrochemical sensor based on nanostructured Au on carbon nanotube networks for real-time analysis of H2O2 release from cells. Anal Chem. 2021;93:6723–6730. doi: 10.1021/ACS.ANALCHEM.1C00336/SUPPL_FILE/AC1C00336_SI_001.PDF. [DOI] [PubMed] [Google Scholar]
- 58.Mani V, Shanthi S, Peng TK, Lin HY, Ikeda H, Hayakawa Y, Ponnusamy S, Muthamizhchelvan C, Huang ST. Real-time quantification of hydrogen peroxide production in living cells using NiCo2S4@CoS2 heterostructure. Sensors Actuators B Chem. 2019;287:124–130. doi: 10.1016/J.SNB.2019.02.015. [DOI] [Google Scholar]
- 59.Long L, Liu H, Liu X, Chen L, Wang S, Liu C, Dong S, Jia J. Co-embedded N-doped hierarchical carbon arrays with boosting electrocatalytic activity for in situ electrochemical detection of H2O2. Sensors Actuators B Chem. 2020;318:128242. doi: 10.1016/J.SNB.2020.128242. [DOI] [Google Scholar]
- 60.Xu Q, Yuan H, Dong X, Zhang Y, Asif M, Dong Z, He W, Ren J, Sun Y, Xiao F. Dual nanoenzyme modified microelectrode based on carbon fiber coated with AuPd alloy nanoparticles decorated graphene quantum dots assembly for electrochemical detection in clinic cancer samples. Biosens Bioelectron. 2018;107:153–162. doi: 10.1016/J.BIOS.2018.02.026. [DOI] [PubMed] [Google Scholar]
- 61.Zhang Y, Xiao J, Sun Y, Wang L, Dong X, Ren J, He W, Xiao F. Flexible nanohybrid microelectrode based on carbon fiber wrapped by gold nanoparticles decorated nitrogen doped carbon nanotube arrays: in situ electrochemical detection in live cancer cells. Biosens Bioelectron. 2018;100:453–461. doi: 10.1016/J.BIOS.2017.09.038. [DOI] [PubMed] [Google Scholar]
- 62.Sri S, Lakshmi GBVS, Gulati P, Chauhan D, Thakkar A, Solanki PR. Simple and facile carbon dots based electrochemical biosensor for TNF-α targeting in cancer patient’s sample. Anal Chim Acta. 2021;1182:338909. doi: 10.1016/J.ACA.2021.338909. [DOI] [PubMed] [Google Scholar]
- 63.Sri S, Chauhan D, Lakshmi GBVS, Thakar A, Solanki PR. MoS2 nanoflower based electrochemical biosensor for TNF alpha detection in cancer patients. Electrochim Acta. 2022;405:139736. doi: 10.1016/J.ELECTACTA.2021.139736. [DOI] [Google Scholar]
- 64.Noh S, Kim J, Park C, Min J, Lee T. Fabrication of an electrochemical aptasensor composed of multifunctional DNA three-way junction on Au microgap electrode for interferon gamma detection in human serum. Biomed. 2021;9:692. doi: 10.3390/BIOMEDICINES9060692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kothari A, Jagannath B, Muthukumar S, Prasad S. An observational study for detection and quantification of interferon- γ in sweat toward inflammation monitoring. Biosens Bioelectron X. 2022;10:100122. doi: 10.1016/J.BIOSX.2022.100122. [DOI] [Google Scholar]
- 66.Tertis M, Leva PI, Bogdan D, Suciu M, Graur F, Cristea C. Impedimetric aptasensor for the label-free and selective detection of Interleukin-6 for colorectal cancer screening. Biosens Bioelectron. 2019;137:123–132. doi: 10.1016/J.BIOS.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 67.Aydin EB, Aydin M, Sezgintürk MK. The development of an ultra-sensitive electrochemical immunosensor using a PPyr-NHS functionalized disposable ITO sheet for the detection of interleukin 6 in real human serums. New J Chem. 2020;44:14228–14238. doi: 10.1039/D0NJ03183F. [DOI] [Google Scholar]
- 68.Tertiş M, Ciui B, Suciu M, Săndulescu R, Cristea C. Label-free electrochemical aptasensor based on gold and polypyrrole nanoparticles for interleukin 6 detection. Electrochim Acta. 2017;258:1208–1218. doi: 10.1016/J.ELECTACTA.2017.11.176. [DOI] [Google Scholar]
- 69.Abdelhalim AOE, Semenov KN, Nerukh DA, Murin IV, Maistrenko DN, Molchanov OE, Sharoyko VV. Functionalisation of graphene as a tool for developing nanomaterials with predefined properties. J Mol Liq. 2022;348:118368. doi: 10.1016/J.MOLLIQ.2021.118368. [DOI] [Google Scholar]
- 70.Ghaemi F, Ali M, Yunus R, Othman RN. Synthesis of carbon nanomaterials using catalytic chemical vapor deposition technique. Elsevier Inc.; 2019. [Google Scholar]
- 71.Ye R, James DK, Tour JM. Laser-induced graphene. Acc Chem Res. 2018;51:1609–1620. doi: 10.1021/acs.accounts.8b00084. [DOI] [PubMed] [Google Scholar]
- 72.Hou Z, Zheng J, Zhang C, Li T, Chen D, Hu L, Hu J, Xiong B, Ye H, Jaffrezic-Renault N, Guo Z. Direct ultrasensitive electrochemical detection of breast cancer biomarker-miRNA-21 employing an aptasensor based on a microgel nanoparticle composite. Sensors Actuators B Chem. 2022;367:132067. doi: 10.1016/J.SNB.2022.132067. [DOI] [Google Scholar]
- 73.Chen M, Wu D, Tu S, Yang C, Chen DJ, Xu Y. A novel biosensor for the ultrasensitive detection of the lncRNA biomarker MALAT1 in non-small cell lung cancer. Sci Rep. 2021;111(11):1–11. doi: 10.1038/s41598-021-83244-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hakimian F, Ghourchian H. Ultrasensitive electrochemical biosensor for detection of microRNA-155 as a breast cancer risk factor. Anal Chim Acta. 2020;1136:1–8. doi: 10.1016/J.ACA.2020.08.039. [DOI] [PubMed] [Google Scholar]
- 75.Barhoumi L, Baraket A, Bellagambi FG, Karanasiou GS, Ben AM, Fotiadis DI, Bausells J, Zine N, Sigaud M, Errachid A. A novel chronoamperometric immunosensor for rapid detection of TNF-α in human saliva. Sensors Actuators B Chem. 2018;266:477–484. doi: 10.1016/J.SNB.2018.03.135. [DOI] [Google Scholar]
- 76.Bianchi V, Mattarozzi M, Giannetto M, Boni A, De Munari I, Careri M. A self-calibrating IoT portable electrochemical immunosensor for serum human epididymis protein 4 as a tumor biomarker for ovarian cancer. Sensors. 2020;20:2016. doi: 10.3390/S20072016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kivrak E, Ince-Yardimci A, Ilhan R, Kirmizibayrak PB, Yilmaz S, Kara P. Aptamer-based electrochemical biosensing strategy toward human non-small cell lung cancer using polyacrylonitrile/polypyrrole nanofibers. Anal Bioanal Chem. 2020;41228(412):7851–7860. doi: 10.1007/S00216-020-02916-X. [DOI] [PubMed] [Google Scholar]
- 78.Ștefan G, Hosu O, De Wael K, Lobo-Castañón MJ, Cristea C. Aptamers in biomedicine: selection strategies and recent advances. Electrochim Acta. 2021;376:137994. doi: 10.1016/J.ELECTACTA.2021.137994. [DOI] [Google Scholar]
- 79.Crevillen AG, Mayorga-Martinez CC, Zelenka J, Rimpelová S, Ruml T, Pumera M. 3D-printed transmembrane glycoprotein cancer biomarker aptasensor. Appl Mater Today. 2021;24:101153. doi: 10.1016/J.APMT.2021.101153. [DOI] [Google Scholar]
- 80.Granata T, Fusco L, Matricardi S, Tozzo A, Janigro D, Nabbout R. Inflammation in pediatric epilepsies: update on clinical features and treatment options. Epilepsy Behav. 2022;131:107959. doi: 10.1016/J.YEBEH.2021.107959. [DOI] [PubMed] [Google Scholar]
- 81.Forloni G, La Vitola P, Cerovic M, Balducci C. Inflammation and Parkinson’s disease pathogenesis: mechanisms and therapeutic insight. Prog Mol Biol Transl Sci. 2021;177:175–202. doi: 10.1016/BS.PMBTS.2020.11.001. [DOI] [PubMed] [Google Scholar]
- 82.Frangou E, Vassilopoulos D, Boletis J, Boumpas DT. An emerging role of neutrophils and NETosis in chronic inflammation and fibrosis in systemic lupus erythematosus (SLE) and ANCA-associated vasculitides (AAV): implications for the pathogenesis and treatment. Autoimmun Rev. 2019;18:751–760. doi: 10.1016/J.AUTREV.2019.06.011. [DOI] [PubMed] [Google Scholar]
- 83.Visser K, Koggel M, Blaauw J, van der Horn HJ, Jacobs B, van der Naalt J. Blood-based biomarkers of inflammation in mild traumatic brain injury: a systematic review. Neurosci Biobehav Rev. 2022;132:154–168. doi: 10.1016/J.NEUBIOREV.2021.11.036. [DOI] [PubMed] [Google Scholar]
- 84.Farah R, Haraty H, Salame Z, Fares Y, Ojcius DM, Said Sadier N. Salivary biomarkers for the diagnosis and monitoring of neurological diseases. Biomed J. 2018;41:63–87. doi: 10.1016/J.BJ.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Goldoni R, Dolci C, Boccalari E, Inchingolo F, Paghi A, Strambini L, Galimberti D, Tartaglia GM. Salivary biomarkers of neurodegenerative and demyelinating diseases and biosensors for their detection. Ageing Res Rev. 2022;76:101587. doi: 10.1016/J.ARR.2022.101587. [DOI] [PubMed] [Google Scholar]
- 86.Sánchez-Tirado E, González-Cortés A, Yáñez-Sedeño P, Pingarrón JM. Electrochemical immunosensor for the determination of the cytokine interferon gamma (IFN-γ) in saliva. Talanta. 2020;211:120761. doi: 10.1016/J.TALANTA.2020.120761. [DOI] [PubMed] [Google Scholar]
- 87.Khalil M, Teunissen CE, Otto M, Piehl F, Sormani MP, Gattringer T, Barro C, Kappos L, Comabella M, Fazekas F, Petzold A, Blennow K, Zetterberg H, Kuhle J. Neurofilaments as biomarkers in neurological disorders. Nat Rev Neurol. 2018;1410(14):577–589. doi: 10.1038/s41582-018-0058-z. [DOI] [PubMed] [Google Scholar]
- 88.Tavakolian-Ardakani, Hosu, Cristea, Mazloum-Ardakani, Marrazza. Latest trends in electrochemical sensors for neurotransmitters: a review. Sensors. 2019;19:2037. 10.3390/s19092037. [DOI] [PMC free article] [PubMed]
- 89.Sun LP, Zhong Y, Gui J, Wang XW, Zhuang XR, Weng J. A hydrogel biosensor for high selective and sensitive detection of amyloid-beta oligomers. Int J Nanomedicine. 2018;13:843. doi: 10.2147/IJN.S152163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Qin J, Park JS, Jo DG, Cho M, Lee Y. Curcumin-based electrochemical sensor of amyloid-β oligomer for the early detection of Alzheimer’s disease. Sensors Actuators B Chem. 2018;273:1593–1599. doi: 10.1016/J.SNB.2018.07.078. [DOI] [Google Scholar]
- 91.Jin H, Gui R, Gao X, Sun Y. An amplified label-free electrochemical aptasensor of γ-interferon based on target-induced DNA strand transform of hairpin-to-linear conformation enabling simultaneous capture of redox probe and target. Biosens Bioelectron. 2019;145:111732. doi: 10.1016/J.BIOS.2019.111732. [DOI] [PubMed] [Google Scholar]
- 92.Liu Y, Xu Q, Zhang Y, Ren B, Huang L, Cai H, Xu T, Liu Q, Zhang X. An electrochemical aptasensor based on AuPt alloy nanoparticles for ultrasensitive detection of amyloid-β oligomers. Talanta. 2021;231:122360. doi: 10.1016/J.TALANTA.2021.122360. [DOI] [PubMed] [Google Scholar]
- 93.Zhou Y, Li C, Li X, Zhu X, Ye B, Xu M. A sensitive aptasensor for the detection of β-amyloid oligomers based on metal–organic frameworks as electrochemical signal probes. Anal Methods. 2018;10:4430–4437. doi: 10.1039/C8AY00736E. [DOI] [Google Scholar]
- 94.Xu L, Lei S, Liu Z, Ouyang G, Zou L, Ye B. A label-free IFN-γ aptasensor based on target-triggered allosteric switching of aptamer beacon and streptavidin-inorganic hybrid composites. Anal Chim Acta. 2019;1087:29–35. doi: 10.1016/J.ACA.2019.08.034. [DOI] [PubMed] [Google Scholar]
- 95.Tan PS, Vaughan E, Islam J, Burke N, Iacopino D, Tierney JB. Laser scribing fabrication of graphitic carbon biosensors for label-free detection of interleukin-6. Nanomater. 2021;11:2110. doi: 10.3390/NANO11082110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kumar S, Tripathy S, Singh OK, Singh SG. Cerium oxide nanofiber based electroanalytical sensor for TNF-α detection: improved interfacial stability with Nafion. Bioelectrochemistry. 2021;138:107725. doi: 10.1016/J.BIOELECHEM.2020.107725. [DOI] [PubMed] [Google Scholar]
- 97.Islam MN, Channon RB. Electrochemical sensors. Bioeng Innov Solut Cancer. 2020;47–71.10.1016/B978-0-12-813886-1.00004-8.
- 98.Shui B, Tao D, Cheng J, Mei Y, Jaffrezic-Renault N, Guo Z. A novel electrochemical aptamer–antibody sandwich assay for the detection of tau-381 in human serum. Analyst. 2018;143:3549–3554. doi: 10.1039/C8AN00527C. [DOI] [PubMed] [Google Scholar]
- 99.Kim J, Noh SW, Park C, Lee JH, Cho HY, Min J, Lee T. Fabrication of electrochemical biosensor composed of multi-functional DNA 4 way junction for TNF-α detection in human serum. Bioelectrochemistry. 2021;142:107939. doi: 10.1016/J.BIOELECHEM.2021.107939. [DOI] [PubMed] [Google Scholar]
- 100.Gonçalves M de L, Truta LAN, Sales MGF, Moreira FTC. Electrochemical point-of care (PoC) determination of interleukin-6 (IL-6) using a pyrrole (Py) molecularly imprinted polymer (MIP) on a carbon-screen printed electrode (C-SPE) Anal Lett. 2021;54:2611–2623. doi: 10.1080/00032719.2021.1879108. [DOI] [Google Scholar]
- 101.Amor-Gutiérrez O, Costa-Rama E, Arce-Varas N, Martínez-Rodríguez C, Novelli A, Fernández-Sánchez MT, Costa-García A. Competitive electrochemical immunosensor for the detection of unfolded p53 protein in blood as biomarker for Alzheimer’s disease. Anal Chim Acta. 2020;1093:28–34. doi: 10.1016/J.ACA.2019.09.042. [DOI] [PubMed] [Google Scholar]
- 102.Razmshoar P, Bahrami SH, Rabiee M, Hangouet M, Martin M, Errachid A, Jaffrezic-Renault N. A novel electrochemical immunosensor for ultrasensitive detection of tumor necrosis factor α based on polystyrene - PAMAM dendritic polymer blend nanofibers. Microchem J. 2022;175:107206. doi: 10.1016/J.MICROC.2022.107206. [DOI] [Google Scholar]
- 103.Aydın EB, Aydın M, Sezgintürk MK. A novel electrochemical immunosensor based on acetylene black/epoxy-substituted-polypyrrole polymer composite for the highly sensitive and selective detection of interleukin 6. Talanta. 2021;222:121596. doi: 10.1016/J.TALANTA.2020.121596. [DOI] [PubMed] [Google Scholar]
- 104.Ghalehno MH, Mirzaei M, Torkzadeh-Mahani M. Aptamer-based determination of tumor necrosis factor α using a screen-printed graphite electrode modified with gold hexacyanoferrate. Microchim Acta. 2018;185:1–8. doi: 10.1007/s00604-018-2704-y. [DOI] [PubMed] [Google Scholar]
- 105.Zhou Y, Liu J, Dong H, Liu Z, Wang L, Li Q, Ren J, Zhang Y, Xu M. Target-induced silver nanocluster generation for highly sensitive electrochemical aptasensor towards cell-secreted interferon-γ. Biosens Bioelectron. 2022;203:114042. doi: 10.1016/J.BIOS.2022.114042. [DOI] [PubMed] [Google Scholar]
- 106.Hernández-Albors A, Castaño AG, Fernández-Garibay X, Ortega MA, Balaguer J, Ramón-Azcón J. Microphysiological sensing platform for an in-situ detection of tissue-secreted cytokines. Biosens Bioelectron X. 2019;2:100025. doi: 10.1016/J.BIOSX.2019.100025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Oliveira GCM de, Carvalho JH de S, Brazaca LC, Vieira NCS, Janegitz BC.Flexible platinum electrodes as electrochemical sensor and immunosensor for Parkinson’s disease biomarkers. Biosens Bioelectron. 2020;152:112016. 10.1016/J.BIOS.2020.112016. [DOI] [PubMed]
- 108.WHO Coronavirus (COVID-19) Dashboard | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data.
- 109.Hu B, Huang S, Yin L. The cytokine storm and COVID-19. J Med Virol. 2021;93:250–256. doi: 10.1002/jmv.26232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Batah SS, Fabro AT. Pulmonary pathology of ARDS in COVID-19: a pathological review for clinicians. Respir Med. 2021;176:106239. doi: 10.1016/j.rmed.2020.106239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shanmugam C, Mohammed AR, Ravuri S, Luthra V, Rajagopal N, Karre S. COVID-2019 – a comprehensive pathology insight. Pathol - Res Pract. 2020;216:153222. doi: 10.1016/j.prp.2020.153222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kang S, Yang M, Hong Z, Zhang L, Huang Z, Chen X, He S, Zhou Z, Zhou Z, Chen Q, Yan Y, Zhang C, Shan H, Chen S. Crystal structure of SARS-CoV-2 nucleocapsid protein RNA binding domain reveals potential unique drug targeting sites. Acta Pharm Sin B. 2020;10:1228–1238. doi: 10.1016/j.apsb.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Xia S, Liu M, Wang C, Xu W, Lan Q, Feng S, Qi F, Bao L, Du L, Liu S, Qin C, Sun F, Shi Z, Zhu Y, Jiang S, Lu L. Inhibition of SARS-CoV-2 (previously 2019-nCoV) infection by a highly potent pan-coronavirus fusion inhibitor targeting its spike protein that harbors a high capacity to mediate membrane fusion. Cell Res. 2020;30:343–355. doi: 10.1038/s41422-020-0305-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Verdecchia P, Cavallini C, Spanevello A, Angeli F. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur J Intern Med. 2020;76:14–20. doi: 10.1016/j.ejim.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tan YJ, Goh PY, Fielding BC, Shen S, Chou CF, Fu JL, Leong HN, Leo YS, Ooi EE, Ling AE, Lim SG, Hong W. Profiles of antibody responses against severe acute respiratory syndrome coronavirus recombinant proteins and their potential use as diagnostic markers. Clin Diagn Lab Immunol. 2004;11:362–371. doi: 10.1128/CDLI.11.2.362-371.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Li G, Chen X, Xu A. Profile of specific antibodies to the SARS-associated coronavirus. N Engl J Med. 2003;349:508–509. doi: 10.1056/NEJM200307313490520. [DOI] [PubMed] [Google Scholar]
- 118.Hueston L, Kok J, Guibone A, McDonald D, Hone G, Goodwin J, et al. The antibody response to SARS-CoV-2 infection. Open Forum Infect Dis. 2020;7.10.1093/ofid/ofaa387. [DOI] [PMC free article] [PubMed]
- 119.Mariappan V, Manoharan PS, Pajanivel R, Shanmugam L, Rao SR, Pillai AB. Potential biomarkers for the early prediction of SARS-COV-2 disease outcome. Microb Pathog. 2021;158:105057. doi: 10.1016/j.micpath.2021.105057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ragab D, Salah Eldin H, Taeimah M, Khattab R, Salem R. The COVID-19 cytokine storm; what we know so far. Front Immunol. 2020;11:1446. doi: 10.3389/fimmu.2020.01446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sloan-Dennison S, O’Connor E, Dear JW, Graham D, Faulds K. Towards quantitative point of care detection using SERS lateral flow immunoassays. Anal Bioanal Chem. 2022;414:4541–4549. doi: 10.1007/S00216-022-03933-8/FIGURES/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Szunerits S, Pagneux Q, Swaidan A, Mishyn V, Roussel A, Cambillau C, Devos D, Engelmann I, Alidjinou EK, Happy H, Boukherroub R. The role of the surface ligand on the performance of electrochemical SARS-CoV-2 antigen biosensors. Anal Bioanal Chem. 2022;414:103–113. doi: 10.1007/S00216-020-03137-Y/FIGURES/5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Garg M, Sharma AL, Singh S. Advancement in biosensors for inflammatory biomarkers of SARS-CoV-2 during 2019–2020. Biosens Bioelectron. 2021;171:112703. doi: 10.1016/j.bios.2020.112703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Farzin MA, Abdoos H, Saber R. AuNP-based biosensors for the diagnosis of pathogenic human coronaviruses: COVID-19 pandemic developments. Anal Bioanal Chem. 2022;2022:1–16. doi: 10.1007/S00216-022-04193-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Dhar BC. Diagnostic assay and technology advancement for detecting SARS-CoV-2 infections causing the COVID-19 pandemic. Anal Bioanal Chem. 2022;414:2903–2934. doi: 10.1007/s00216-022-03918-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Rasmi Y, Li X, Khan J, Ozer T, Choi JR. Emerging point-of-care biosensors for rapid diagnosis of COVID-19: current progress, challenges, and future prospects. Anal Bioanal Chem. 2021;413:4137–4159. doi: 10.1007/S00216-021-03377-6/TABLES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Raziq A, Kidakova A, Boroznjak R, Reut J, Öpik A, Syritski V. Development of a portable MIP-based electrochemical sensor for detection of SARS-CoV-2 antigen. Biosens Bioelectron. 2021;178:113029. doi: 10.1016/j.bios.2021.113029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Torrente-Rodríguez RM, Lukas H, Tu J, Min J, Yang Y, Xu C, Rossiter HB, Gao W. SARS-CoV-2 RapidPlex: a graphene-based multiplexed telemedicine platform for rapid and low-cost COVID-19 diagnosis and monitoring. Matter. 2020;3:1981–1998. doi: 10.1016/j.matt.2020.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Alafeef M, Dighe K, Moitra P, Pan D. Rapid, ultrasensitive, and quantitative detection of SARS-CoV-2 using antisense oligonucleotides directed electrochemical biosensor chip. ACS Nano. 2020;14:17028–17045. doi: 10.1021/acsnano.0c06392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Vásquez V, Navas M-C, Jaimes JA, Orozco J. SARS-CoV-2 electrochemical immunosensor based on the spike-ACE2 complex. Anal Chim Acta. 2022;1205:339718. doi: 10.1016/j.aca.2022.339718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yousefi H, Mahmud A, Chang D, Das J, Gomis S, Chen JB, Wang H, Been T, Yip L, Coomes E, Li Z, Mubareka S, Mcgeer A, Christie N, Gray-Owen S, Cochrane A, Rini JM, Sargent EH, Kelley SO. Detection of SARS-CoV-2 viral particles using direct, reagent-free electrochemical sensing. J Am Chem Soc. 2021;143:1722–1727. doi: 10.1021/jacs.0c10810. [DOI] [PubMed] [Google Scholar]
- 132.Seo G, Lee G, Kim MJ, Baek SH, Choi M, Ku KB, Lee CS, Jun S, Park D, Kim HG, Kim SJ, Lee JO, Kim BT, Park EC, Il KS. Rapid detection of COVID-19 causative virus (SARS-CoV-2) in human nasopharyngeal swab specimens using field-effect transistor-based biosensor. ACS Nano. 2020;14:5135–5142. doi: 10.1021/acsnano.0c02823. [DOI] [PubMed] [Google Scholar]
- 133.Brazaca LC, Imamura AH, Gomes NO, Almeida MB, Scheidt DT, Raymundo-Pereira PA, Oliveira ON, Janegitz BC, Machado SAS, Carrilho E. Electrochemical immunosensors using electrodeposited gold nanostructures for detecting the S proteins from SARS-CoV and SARS-CoV-2. Anal Bioanal Chem. 2022;414:5507–5517. doi: 10.1007/S00216-022-03956-1/FIGURES/5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Xian M, Carey PH, Fares C, Ren F, Shan SS, Liao Y Te, Esquivel-Upshaw JF, Pearton SJ. Rapid electrochemical detection for SARS-CoV-2 and cardiac troponin I using low-cost, disposable and modular biosensor system. 2020 IEEE Res Appl Photonics Def Conf RAPID 2020 - Proc. 2020. 10.1109/RAPID49481.2020.9195689.
- 135.Subhasis Mahari, Akanksha Roberts, Deepshikha Shahdeo, Sonu Gandhi. eCovSens-ultrasensitive novel in-house built printed circuit board based electrochemical device for rapid detection of nCovid-19 antigen, a spike protein domain 1 of SARS-CoV-2. Biorxiv 2020.04.24.059204. 2020. 10.1101/2020.04.24.059204.
- 136.Erdem A, Senturk H, Yildiz E, Maral M. Amperometric immunosensor developed for sensitive detection of SARS-CoV-2 spike S1 protein in combined with portable device. Talanta. 2022;244:123422. doi: 10.1016/j.talanta.2022.123422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ayankojo AG, Boroznjak R, Reut J, Öpik A, Syritski V. Molecularly imprinted polymer based electrochemical sensor for quantitative detection of SARS-CoV-2 spike protein. Sensors Actuators B Chem. 2022;353:131160. doi: 10.1016/j.snb.2021.131160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Vadlamani BS, Uppal T, Verma SC, Misra M. Functionalized TiO2 nanotube-based electrochemical biosensor for rapid detection of SARS-CoV-2. Sensors. 2020;20:5871. doi: 10.3390/S20205871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Fabiani L, Saroglia M, Galatà G, De Santis R, Fillo S, Luca V, Faggioni G, D’Amore N, Regalbuto E, Salvatori P, Terova G, Moscone D, Lista F, Arduini F. Magnetic beads combined with carbon black-based screen-printed electrodes for COVID-19: a reliable and miniaturized electrochemical immunosensor for SARS-CoV-2 detection in saliva. Biosens Bioelectron. 2021;171:112686. doi: 10.1016/J.BIOS.2020.112686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Chaibun T, Puenpa J, Ngamdee T, Boonapatcharoen N, Athamanolap P, O’Mullane AP, Vongpunsawad S, Poovorawan Y, Lee SY, Lertanantawong B. Rapid electrochemical detection of coronavirus SARS-CoV-2. Nat Commun. 2021;12:802. doi: 10.1038/s41467-021-21121-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Liv L, Yener M, Çoban G, Can ŞA. Electrochemical biosensing platform based on hydrogen bonding for detection of the SARS-CoV-2 spike antibody. Anal Bioanal Chem. 2022;414:1313–1322. doi: 10.1007/S00216-021-03752-3/TABLES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Rashed MZ, Kopechek JA, Priddy MC, Hamorsky KT, Palmer KE, Mittal N, Valdez J, Flynn J, Williams SJ. Rapid detection of SARS-CoV-2 antibodies using electrochemical impedance-based detector. Biosens Bioelectron. 2021;171:112709. doi: 10.1016/j.bios.2020.112709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Ali MA, Hu C, Jahan S, Yuan B, Saleh MS, Ju E, Gao SJ, Panat R. Sensing of COVID-19 antibodies in seconds via aerosol jet nanoprinted reduced-graphene-oxide-coated 3D electrodes. Adv Mater. 2021;33:2006647. doi: 10.1002/adma.202006647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Yakoh A, Pimpitak U, Rengpipat S, Hirankarn N, Chailapakul O, Chaiyo S. Paper-based electrochemical biosensor for diagnosing COVID-19: detection of SARS-CoV-2 antibodies and antigen. Biosens Bioelectron. 2021;176:112912. doi: 10.1016/j.bios.2020.112912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Samper IC, Sánchez-Cano A, Khamcharoen W, Jang I, Siangproh W, Baldrich E, Geiss BJ, Dandy DS, Henry CS. Electrochemical capillary-flow immunoassay for detecting anti-SARS-CoV-2 nucleocapsid protein antibodies at the point of care. ACS Sensors. 2021;6:4067–4075. doi: 10.1021/ACSSENSORS.1C01527/ASSET/IMAGES/LARGE/SE1C01527_0007.JPEG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Eissa S, Zourob M. Development of a low-cost cotton-tipped electrochemical immunosensor for the detection of SARS-CoV-2. Anal Chem. 2021;93:1826–1833. doi: 10.1021/acs.analchem.0c04719. [DOI] [PubMed] [Google Scholar]
- 147.Zhao H, Liu F, Xie W, Zhou T-C, OuYang J, Jin L, Li H, Zhao C-Y, Zhang L, Wei J, Zhang Y-P, Li C-P. Ultrasensitive supersandwich-type electrochemical sensor for SARS-CoV-2 from the infected COVID-19 patients using a smartphone. Sensors Actuators B Chem. 2021;327:128899. doi: 10.1016/j.snb.2020.128899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Herrera-Chacón A, Cetó X, del Valle M. Molecularly imprinted polymers - towards electrochemical sensors and electronic tongues. Anal Bioanal Chem. 2021;413:6117–6140. doi: 10.1007/s00216-021-03313-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Melinte G, Hosu O, Cristea C, Marrazza G. DNA sensing technology a useful food scanning tool. TrAC Trends Anal Chem. 2022;154:116679. doi: 10.1016/j.trac.2022.116679. [DOI] [Google Scholar]
- 150.Cavalera S, Di Nardo F, Chiarello M, Serra T, Colitti B, Guiotto C, Fagioli F, Cagnazzo C, Denina M, Palazzo A, Artusio F, Pisano R, Rosati S, Baggiani C, Anfossi L. Bacterial ligands as flexible and sensitive detectors in rapid tests for antibodies to SARS-CoV-2. Anal Bioanal Chem. 2022;414:5473–5482. doi: 10.1007/S00216-022-03939-2/TABLES/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Jang I, Kang H, Song S, Dandy DS, Geiss BJ, Henry CS. Flow control in a laminate capillary-driven microfluidic device. Analyst. 2021;146:1932–1939. doi: 10.1039/d0an02279a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Heikenfeld J, Jajack A, Rogers J, Gutruf P, Tian L, Pan T, Li R, Khine M, Kim J, Wang J, Kim J. Wearable sensors: modalities, challenges, and prospects. Lab Chip. 2018;18:217–248. doi: 10.1039/C7LC00914C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Kim J, Campbell AS, de Ávila BE-F, Wang J. Wearable biosensors for healthcare monitoring. Nat Biotechnol. 2019;37:389–406. doi: 10.1038/s41587-019-0045-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Sharma A, Tok AIY, Alagappan P, Liedberg B. Point of care testing of sports biomarkers: potential applications, recent advances and future outlook. TrAC Trends Anal Chem. 2021;142:116327. doi: 10.1016/j.trac.2021.116327. [DOI] [Google Scholar]
- 155.Ray T, Choi J, Reeder J, Lee SP, Aranyosi AJ, Ghaffari R, Rogers JA. Soft, skin-interfaced wearable systems for sports science and analytics. Curr Opin Biomed Eng. 2019;9:47–56. doi: 10.1016/J.COBME.2019.01.003. [DOI] [Google Scholar]
- 156.Shahim P, Politis A, van der Merwe A, Moore B, Chou YY, Pham DL, Butman JA, Diaz-Arrastia R, Gill JM, Brody DL, Zetterberg H, Blennow K, Chan L. Neurofilament light as a biomarker in traumatic brain injury. Neurology. 2020;95:e610–e622. doi: 10.1212/WNL.0000000000009983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Gevaerd A, Watanabe EY, Belli C, Marcolino-Junior LH, Bergamini MF. A complete lab-made point of care device for non-immunological electrochemical determination of cortisol levels in salivary samples. Sensors Actuators B Chem. 2021;332:129532. doi: 10.1016/j.snb.2021.129532. [DOI] [Google Scholar]
- 158.Kaushik A, Yndart A, Jayant RD, Sagar V, Atluri V, Bhansali S, Nair M. Electrochemical sensing method for point-of-care cortisol detection in human immunodeficiency virus-infected patients. Int J Nanomedicine. 2015;10:677–685. doi: 10.2147/IJN.S75514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Liu X, Hsu SPC, Liu W-C, Wang Y-M, Liu X, Lo C-S, Lin Y-C, Nabilla SC, Li Z, Hong Y, Lin C, Li Y, Zhao G, Chung R-J. Salivary electrochemical cortisol biosensor based on tin disulfide nanoflakes. Nanoscale Res Lett. 2019;14:189. doi: 10.1186/s11671-019-3012-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Moreira FTC, Dutra RAF, Noronha JP, Sales MGF. Novel sensory surface for creatine kinase electrochemical detection. Biosens Bioelectron. 2014;56:217–222. doi: 10.1016/j.bios.2013.12.052. [DOI] [PubMed] [Google Scholar]
- 161.Wang XY, Chen Y, Mei LP, Wang AJ, Yuan PX, Feng JJ. Confining signal probe in porous PdPtCoNi@Pt-skin nanopolyhedra to construct a sandwich-type electrochemical immmunosensor for ultrasensitive detection of creatine kinase-MB. Sensors Actuators, B Chem. 2020;315.10.1016/j.snb.2020.128088.
- 162.Cen SY, Feng YG, Zhu JH, Wang XY, Wang AJ, Luo X, Feng JJ. Eco-friendly one-pot aqueous synthesis of ultra-thin AuPdCu alloyed nanowire-like networks for highly sensitive immunoassay of creatine kinase-MB. Sensors Actuators, B Chem. 2021;333:129573. doi: 10.1016/j.snb.2021.129573. [DOI] [Google Scholar]
- 163.Wang SX, Acha D, Shah AJ, Hills F, Roitt I, Demosthenous A, Bayford RH. Detection of the tau protein in human serum by a sensitive four-electrode electrochemical biosensor. Biosens Bioelectron. 2017;92:482–488. doi: 10.1016/j.bios.2016.10.077. [DOI] [PubMed] [Google Scholar]
- 164.Razzino CA, Serafín V, Gamella M, Pedrero M, Montero-Calle A, Barderas R, Calero M, Lobo AO, Yáñez-Sedeño P, Campuzano S, Pingarrón JM. An electrochemical immunosensor using gold nanoparticles-PAMAM-nanostructured screen-printed carbon electrodes for tau protein determination in plasma and brain tissues from Alzheimer patients. Biosens Bioelectron. 2020;163:112238. doi: 10.1016/j.bios.2020.112238. [DOI] [PubMed] [Google Scholar]
- 165.Sonuç Karaboga MN, Sezgintürk MK. Analysis of Tau-441 protein in clinical samples using rGO/AuNP nanocomposite-supported disposable impedimetric neuro-biosensing platform: towards Alzheimer’s disease detection. Talanta. 2020;219:121257. doi: 10.1016/j.talanta.2020.121257. [DOI] [PubMed] [Google Scholar]
- 166.Eduarda Schneider M, Guillade L, Correa-Duarte MA, Moreira FTC. Development of a biosensor for phosphorylated Tau 181 protein detection in early-stage Alzheimer’s disease. Bioelectrochemistry. 2022;145:108057. doi: 10.1016/j.bioelechem.2022.108057. [DOI] [PubMed] [Google Scholar]
- 167.Liu Y, Wang H, Chen J, Liu C, Li W, Kong J, Yang P, Liu B. A sensitive microchip-based immunosensor for electrochemical detection of low-level biomarker s100b. Electroanalysis. 2013;25:1050–1055. doi: 10.1002/elan.201200525. [DOI] [Google Scholar]
- 168.Pfäfflin A, Schleicher E. Inflammation markers in point-of-care testing (POCT) Anal Bioanal Chem. 2009;393:1473–1480. doi: 10.1007/S00216-008-2561-3/TABLES/2. [DOI] [PubMed] [Google Scholar]
- 169.Knight EL, Jiang Y, Rodriguez-Stanley J, Almeida DM, Engeland CG, Zilioli S. Perceived stress is linked to heightened biomarkers of inflammation via diurnal cortisol in a national sample of adults. Brain Behav Immun. 2021;93:206–213. doi: 10.1016/j.bbi.2021.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.FIND. Test directory - FIND. In: Found. Innov. New Diagnostics. 2020. https://www.finddx.org/covid-19/.
- 171.Gug IT, Tertis M, Hosu O, Cristea C. Salivary biomarkers detection: analytical and immunological methods overview. TrAC Trends Anal Chem. 2019;113:301–316. doi: 10.1016/J.TRAC.2019.02.020. [DOI] [Google Scholar]
- 172.Sempionatto JR, Montiel VRV, Vargas E, Teymourian H, Wang J. Wearable and mobile sensors for personalized nutrition. ACS Sensors. 2021;6:1745–1760. doi: 10.1021/ACSSENSORS.1C00553/ASSET/IMAGES/MEDIUM/SE1C00553_0005.GIF. [DOI] [PubMed] [Google Scholar]
- 173.Teymourian H, Tehrani F, Mahato K, Wang J. Lab under the skin: microneedle based wearable devices. Adv Healthc Mater. 2021;10:2002255. doi: 10.1002/ADHM.202002255. [DOI] [PubMed] [Google Scholar]
- 174.Hosu O, Mirel S, Săndulescu R, Cristea C. Minireview: smart tattoo, microneedle, point-of-care, and phone-based biosensors for medical screening, diagnosis, and monitoring. Anal Lett. 2019;52:78–92. doi: 10.1080/00032719.2017.1391826. [DOI] [Google Scholar]