Abstract
Objective Lumbar spinal stenosis (LSS) patients suffer from significant pain and disability. To assess long-term safety and efficacy of laminectomy in LSS patients, a systematic review and meta-analysis study was conducted.
Methods Literature review in MEDLINE, Embase, Scopus, Web of Science, and Cochrane Library databases was performed using a predefined search strategy. Articles were included if they met the following characteristics: human studies, LSS, and at least 5 years of follow-up. Outcome measures included patient satisfaction, pain, disability, claudication, reoperation rates, and complications.
Results Twelve articles met the eligibility criteria for our study. Overall, there was low-quality evidence that patients undergoing laminectomy, with at least 5 years of follow-up, have significantly more satisfaction, and less pain and disability, compared with the preoperative baseline. Assessment of neurogenic intermittent claudication showed significant improvement in walking abilities. We also reviewed the postoperative complication and adverse events in the included studies. After meta-analysis was performed, the reoperation rate was found to be 14% (95% confidence interval: 13–16%).
Conclusion Our study provides low-quality evidence suggesting that patients undergoing laminectomy for LSS have less disability and pain and can be more physically active postoperatively.
Keywords: laminectomy, spinal stenosis, lumbar spinal stenosis, intermittent claudication
Introduction
Patients suffering from lumbar spinal stenosis (LSS) can have difficulty walking especially more than 500 m, 1 imposing significant restrictions on their daily living 2 and further financial burden on the health care system. 3 There are various surgical methods used to relieve pressure on the spinal cord and nerve roots in the lumbar segment, most notably laminectomy, laminotomy, laminoplasty, and use of interspinous spacer implantation. 4 5 More recently, minimally invasive trends such as microendoscopic approaches can also be considered for the treatment of LSS. 6 Currently, laminectomy is the preferred method for the majority of cases and is indicated in LSS without concurrent lumbar instability. 5 7
Additionally, there are several complications for the aforementioned procedures and can be divided into three stages depending on the time of occurrence: acute (up to 3 days after surgery), subacute (3 days to 2 weeks after surgery), and chronic (greater than 2 weeks following surgery). 4 5 The prevalence of these complications varies between 0.5 and 2.3%. Risk factors for more severe complications include depression, comorbidities restricting walking ability, scoliosis, cardiovascular diseases, and smoking. 8
Previously, few studies have evaluated long-term outcomes after laminectomy in patients with LSS. 7 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 There is limited evidence regarding long-term outcomes after laminectomy. Considering the potential complications of laminectomy and limited evidence with long-term follow-up, further investigation is needed to assess clinical outcomes after laminectomy to assist with surgical decision-making regarding the choice of surgical or conservative treatment. Therefore, the goal of this study was to conduct a systematic review and meta-analysis to assess patient satisfaction, pain, disability, claudication, complications, and adverse event in patients with LSS undergoing either single or multilevel laminectomy procedures.
Material and Methods
Search Strategy
A comprehensive electronic search of MEDLINE, Embase, Scopus, Web of Science, and the Cochrane Library was conducted and updated until August 2020 using Medical Subject Headings terms and related keywords ( Appendix Table A1 ). Additionally, the list of references of relevant articles was manually reviewed to discover potential further related articles. Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for systematic review were followed as shown in Fig. 1 . No language limits were imposed for this literature search.
Appendix Table A1.
| PubMed | ("Lumbar Vertebrae"[Mesh] OR "Lumbar Stenosis, Familial" [Supplementary Concept] OR "Spinal Stenosis"[Mesh] OR (Lumbar[TIAB] AND (Vertebrae[TIAB] OR Vertebra[TIAB] OR vertebralis[TIAB] ) ) OR ( (spine [TIAB] OR spinal[TIAB] OR spinalis[TIAB] OR lumb* [TIAB] ) AND (stenosis[TIAB] OR Stenoses[TIAB] OR stenotic[TIAB])) OR "Cauda Equina"[Mesh] OR ((equaine[TIAB] OR Equina[TIAB] ) AND Cauda[TIAB] ) OR (Filum[TIAB] AND Terminale[TIAB]) ) AND ( "Decompression, Surgical"[Mesh] OR ((Decompression*[TIAB] OR decompressive[TIAB] ) AND (surger*[TIAB] OR operation[TIAB] )) OR "Laminectomy"[Mesh] OR hemilaminectomy[TIAB] OR Laminectom* [TIAB] OR Laminotom*[TIAB] OR "Minimally Invasive Surgical Procedures"[Mesh] OR ( (minimally[TIAB] OR Mini[TIAB] ) AND ( Invasive[TIAB] OR Procedur*[TIAB] )) OR endoscop*[TIAB] OR (PEDICLE[TIAB] AND SCREW[TIAB] ) OR ((Nerve[TIAB] AND Root[TIAB]) AND Compression*[TIAB] ) OR "Arthrodesis"[Mesh] OR Arthrodes*[TIAB] OR arthrodesia[TIAB] OR (articular[TIAB] AND process[TIAB] AND fusion[TIAB] ) OR ( joint [TIAB] AND fusion[TIAB] )) AND (Year [tiab] OR Years[tiab] OR TERM [tiab] OR TERMS[tiab] OR CHRONIC [tiab] OR CHRONICS[tiab]) AND ("Clinical Trials as Topic"[Mesh] OR "Clinical Trial" [Publication Type] OR RCT[TIAB] OR RANDOMIZED[TIAB] OR RANDOM*[TIAB] OR TRIAL*[TIAB] OR "Follow-Up Studies"[Mesh] OR “Follow Up” [TIAB] OR Followup [TIAB] OR "Cohort Studies"[Mesh] OR Cohort [TIAB] OR Concurrent [TIAB] OR (Incidence[TIAB] AND (Study[TIAB] OR studies[tiab]))) NOT (("Animals"[Mesh] OR animal*[TIAB] OR rat [TIAB] OR rats[TIAB] OR mice[TIAB] OR mouse[TIAB]) NOT (("Humans"[Mesh] OR human*[TIAB] ) AND ("Animals"[Mesh] OR animal*[TIAB] OR rat [TIAB] OR rats[TIAB] OR mice[TIAB] OR mouse[TIAB]))) |
Fig. 1.
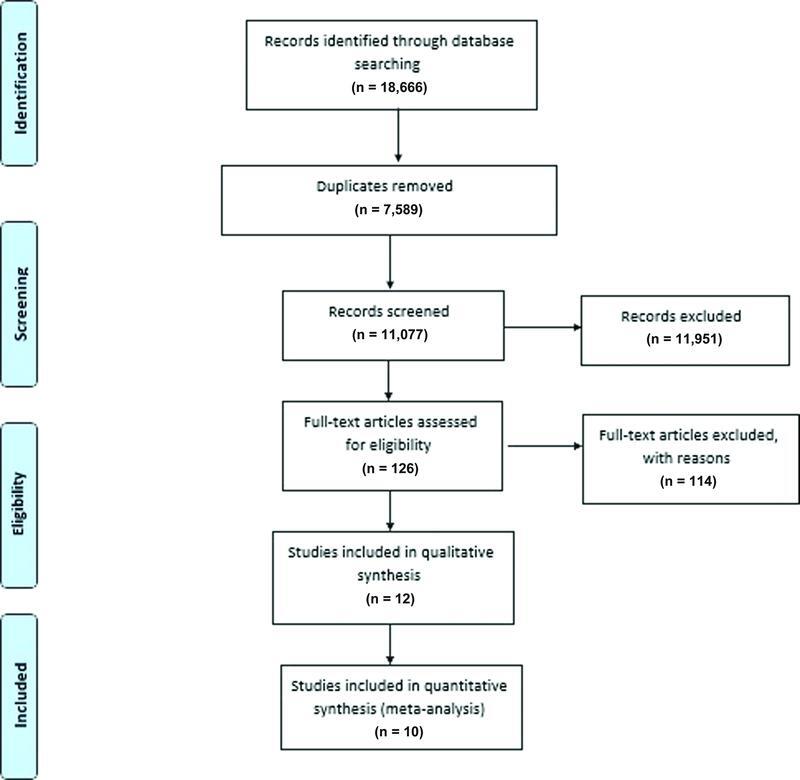
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart.
Selection Method
After the removal of duplicates, four reviewers were divided into two groups, independently reviewing titles and abstracts of the studies. After collecting the full text of eligible papers, four reviewers in two groups (M.H.R., S.R., K.S., and A.A.H.) independently reviewed each article for inclusion and exclusion criteria. The third reviewer (M.G.H.) resolved any discrepancy regarding the eligibility of studies.
Inclusion and Exclusion Criteria
All cohort studies and randomized controlled trials reporting conventional laminectomy due to LSS and related outcomes with at least a 5-year follow-up were included in this study. In articles that described the outcomes of various types of surgical procedures, only the data of patients with conventional laminectomy were obtained for the analysis. For studies using the same data set, only the one with a higher number of cases and data that are more complete was included. Exclusion criteria included patients suffering from concomitant spondylolisthesis, patients undergoing fusion surgery, and congenital stenosis.
Data Extraction
Clinical and functional outcome measures that were evaluated included patient satisfaction, pain, disability, neurogenic intermittent claudication, reoperation rate, complications, and adverse events. Any association between single or multilevel laminectomy and patient outcomes was also assessed.
From each study, we collected general information (first author, year of study, country, journal), methods (study design, sample size), participants (age, gender, preoperative neurological score), outcomes of surgery, and follow-up time. Two independent reviewers reviewed each study (K.S. and A.A.H.). If any discordance were present, they were settled through focused discussion and reference to the original article.
Assessment of Methodological Quality
The risk of bias of the included studies was evaluated using the Newcastle-Ottawa checklist for cohort studies ( Table 1 ). We considered studies with at least seven stars to be at low risk of bias, leading to eight studies being determined to have a low risk of bias 9 10 11 12 13 14 15 20 and the remaining four as high risk. 16 17 18 19
Table 1. Quality assessment according to Newcastle-Ottawa quality assessment for cohort studies.
| Study/Quality assessment questions | Foulongne et al, 2013 | Shabat et al, 2011 | Malter et al, 1998 | Iguchi et al, 2000 | Kim et al, 2013 | Kao et al, 2018 | Lehto and Honkanen, 1995 | Chang et al, 2005 | Mannion et al, 2010 | Lurie et al, 2015 | Lee et al, 2014 | Atlas and Delitto, 2006 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Representativeness of the exposed cohort | * | * | * | * | * | * | * | * | * | * | * | |
| 2. Selection of the non-exposed cohort | * | * | * | * | * | * | * | * | * | * | * | * |
| 3. Ascertainment of exposure | * | * | * | * | * | * | * | * | * | * | ||
| 4. Demonstration that outcome of interest was not present at start of study | ||||||||||||
| 5. Comparability of cohorts on the basis of the design or analysis controlled for confounders | ** | ** | ** | ** | ** | ** | ** | ** | ** | * | ** | |
| 6. Assessment of outcome | * | * | * | * | * | * | * | * | * | * | * | |
| 7. Was follow-up long enough for outcomes to occur | * | * | * | * | * | * | * | * | * | * | * | * |
| 8. Adequacy of follow-up of cohorts | * | * | * | * | ||||||||
| Low | Low | Low | Low | Low | Low | Low | High | High | High | High | Low |
Note: This scale evaluates each study based on eight items, categorized into three groups: selection, comparability, and outcome. Each item numbered in the Selection and Outcome categories was given a maximum of one star and a maximum of two stars within the comparability category.
Statistical Analysis
Meta-analysis was only performed for reoperation rate. Heterogeneity among the results of studies was quantified using I 2 statistics. The results were reported using a random-effects model with 95% confidence interval (CI). Subgroup analysis was performed based on the quality of the included studies. A meta-analytic approach was not feasible for other outcome measures due to heterogeneous methods of reporting among the studies. Statistical analysis was performed using Stata V.14.
Results
Included Studies
Initially, 18,666 records were retrieved from the databases and after removing the duplicate documents and screening the titles and abstracts, 126 articles were selected for full-text screening. Finally, 12 records met all eligibility criteria, all of which were included for qualitative analysis, and 10 articles were included for meta-analysis 9 10 11 12 13 14 15 16 17 18 19 20 ( Fig. 1 ). Our search results did not yield any published randomized clinical trials, therefore, all included studies were cohort studies with at least 5 years of follow-up. A total number of 83,492 LSS patients were included in these articles ( Table 2 ). All patients had undergone standard decompression laminectomy with a follow-up period between 5 and 10 years. Outcomes assessed included patient satisfaction, leg and lumbar pain intensity, disability, neurogenic intermittent claudication, reoperation rate, complications, and adverse events which are summarized in Table 3 . The effect of multilevel compared with single-level laminectomy on patient outcomes was also assessed in a few studies.
Table 2. Baseline characteristic of the 12 included studies.
| Code | Title | First author | Study design | Study population | Age (mean ± SD) | Surgery method | Follow-up (y) | Outcomes |
|---|---|---|---|---|---|---|---|---|
| 1 | Lumbar spinal stenosis: Which predictive factors of favorable functional results after decompressive laminectomy | E. Foulongne | Prospective cohort | 98 (94 M, 4 F) | 67.3 ± 8.8 | Decompressive laminectomy in lumbar stenosis | 5 | Walking distance, reoperation rate, complication |
| 2 | Long-term follow-up of revision decompressive lumbar spinal surgery in elderly patients | Shay Shabat | Retrospective cohort | 31 | > 65 | Lumbar decompressive spinal surgery | 10 | Pain, reoperation rate, patient's satisfaction |
| 3 | 5-year reoperation rates after different types of lumbar spine surgery | Alex D. Malter | Population-based cohort study | 6,376 (3,764 M, 2,612 F) | 48 | Lumbar surgery | 5 | Reoperation rate, complication |
| 4 | Minimum 10-year outcome of decompressive laminectomy for degenerative lumbar spinal stenosis | Tetsuhiro Iguchi | Retrospective cohort | 151 | 60 | Decompressive laminectomy | 10 | Back pain, leg pain, neurogenic claudication, patient's satisfaction, multilevel laminectomy |
| 5 | Reoperation rate after surgery for lumbar spinal stenosis without spondylolisthesis: a nationwide cohort study | Chi Heon Kim | Retrospective cohort | 8,795 (55.6 F, 44.4 M) | 56.7 ± 12.1 | Decompression without fusion (laminectomy and/or discectomy) | 6 | Reoperation rate, complication |
| 6 | Short-term and long-term revision rates after lumbar spine discectomy versus laminectomy: a population-based cohort study | Feng-Chen Kao | Retrospective cohort | 66,754 (47.88 F, 52.11 M) | 59.91 ± 14.02 | Laminectomy | 5 | Reoperation rate |
| 7 | Factors influencing the outcome of operative treatment for lumbar spinal stenosis | M.U. Lehto | Retrospective cohort | 96 (50 M, 46 F) | 59 | Laminectomy | 5.5 | Satisfaction, multilevel laminectomy, complication |
| 8 | The effect of surgical and nonsurgical treatment on longitudinal outcomes of lumbar spinal stenosis over 10 years | Yuchiao Chang | Prospective observational cohort | 144 (54 M, 90 F) | 65 | LSS | 10 | Pain, disability, reoperation rate, patient's satisfaction |
| 9 | Five-year outcome of surgical decompression of the lumbar spine without fusion | Anne F. Mannion | Prospective cohort | 143 (92 M, 51 F) | 64 | Lumbar decompression surgery without fusion | 5 | Leg pain and back pain intensity, self-rated disability, reoperation rates |
| 10 | Long-term outcomes of lumbar spinal stenosis: 8-year results of the spine patient outcomes research trial (sport) | Jon D. Lurie | Randomized trial with a concurrent observational cohort study | 654 (385 M, 249 F) | 64 | Decompressive laminectomy | 8 | Patient's satisfaction, reoperation rate, complication |
| 11 | Clinical and radiological outcomes following microscopic decompression utilizing tubular retractor or conventional microscopic decompression in lumbar spinal stenosis with a minimum of 10-year follow-up | Gun Woo Lee | Retrospective cohort | 102 | 56 | Lumbar spinal stenosis | 10 | Pain, disability, walking distance, reoperation rate |
| 12 | Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis | Steven J. Atlas | Prospective observational cohort | 148 | 65 | LSS | 10 | Patient-reported symptoms of leg and back pain, disability, reoperation rate, patient's satisfaction |
Abbreviations: F, female; LLS, lumbar spinal stenosis; M, male; SD, standard deviation.
Table 3. Main findings of included 12 articles.
| Article | Satisfaction | Pain | Disability | Neurogenic intermittent claudication | Reoperation rate | Complication and adverse events |
|---|---|---|---|---|---|---|
| Foulongne et al (2013) | Walking distance increased from 795.61 ± 1,303.58 preoperatively to 2,083.3 ± 2,131.6 at 5 years | Reoperation rate was 10.2% | Four patients needed early surgery due to postoperative complications and 10 patients needed reoperation due to adjacent level stenosis or destabilization | |||
| Shabat et al (2011) | Quote: 72% of patients very or somewhat satisfied with overall results of the operation | Using VAS score there was 4.3 points change in score before and after surgery | Quote: The overall rate of revision was 8.7% at a mean follow-up of 70 months (10% in females and 7% in males, p > 0.05) | |||
| Malter et al (1998) | The 5-year reoperation rate was ∼12% | 7% of patients had postoperative complications In-hospital mortality was 0.3% |
||||
| Iguchi et al (2000) | 75% of patients were satisfied with the result of surgery at 7- to 10-year follow-up; however, 33% of them had severe back pain, and 53% were unable to walk for two blocks | JOA score of low back pain improved slightly from 1.4 ± 0.7 to 1.9 ± 0.7 points. The score of leg pain, however, changed from 0.7 ± 0.6 to 2.1 ± 0.7 points. Postoperatively, 32.4% and 21 0.6% of patients had persistent back and leg pain, respectively | Preoperatively, 62.2% patients unable to walk for 100 m that decreased to 8.1% patients, postoperatively | |||
| Kim et al (2013) | Reoperation rate was 14.8% at 6 years | During the first 90 days 33 patients died | ||||
| Kao et al (2018) | The revision spinal surgery rates was 13.44% | |||||
| Lehto and Honkanen (1995) | Of all the operated patients 9 (14%) considered the outcome of operation as excellent, 28 (43%) as good, 14 (21.5%) as satisfactory, and 14 (21.5%) as poor | Seven patients died during the follow-up period due to illness not related to the spinal stenosis or its operative treatment | ||||
| Chang et al (2005) | 7 grade scoring for satisfaction (terrible = 0 to delighted = 6), it was 4 after surgery and reduced to 3.6 at 10-year follow up | Using leg symptom frequency index (0–24), changes in leg symptom frequency index was 11.1 after surgery. This difference was 8.8 at 5 years and 9.4 at 10 years. Back pain frequency change for back pain was 2.5 after surgery and was 1.9 at 10-year follow-up. After 5 years, change in leg symptoms and functional status continued to favor surgical treatment, but change in frequency of low back pain and satisfaction with the current state were no longer statistically significant |
Modified Roland scale change was 8.6 (baseline = 16 ± 4.2) immediate postoperatively. This change was 6.8 at a 10-year follow-up | Fifteen of 77 patients initially treated surgically underwent a second operation during follow-up | ||
| Mannion et al (2010) | In graphic rating scale from preoperative to 2 months postoperative, there was a significant reduction in mean leg pain of 3.6 ± 2.5 points and 2.2 ± 2.5 points for back pain. While there was no significant further change from 2 months up to 5 years' follow-up in leg pain, there was significant but clinically irrelevant increase of 0.5 ± 2.1 points in back pain | There was a significant decrease of 2.7 ± 5.2 points in the mean Roland-Morris (RM) score from before surgery to 2 months postoperatively ( p < 0.0001) and a further decrease of 2.5 ± 3.6 points up to 5 months postoperatively ( p 0.0001) ( fig. 1C ). After this, no further changes were seen up to 5 years postoperatively | By the time of the 5-year follow-up, 34/143 patients (24%) had undergone reoperation, at an average of 29.1 ± 20.9 months | |||
| Lurie et al (2015) | 67% of patients were satisfied after surgery at 8 years | 18% of patients had reoperation rate at 8 years | Most common intraoperative complication: dural tear (9%), most common postoperative: wound infection 7% |
|||
| Lee et al (2014) | Using VAS score, pain (leg and back pain was not differentiated) improved from mean score 8.4 preoperatively to 3.8 one-month and 2.8 one-year postoperatively. It was increased to 4.8 at six- and ten-year follow-up | ODI 41.2 ± 6.3 preoperative decreased gradually to 24.7 ± 5.6 at 1 year postop and increased to 32.1 ± 3.2 at 10 years postoperatively | Walking distance without pain was 20.1 ± 5.7 preoperatively and increased to 38.1 ± 5.2 postoperatively. It decreased to 25.9 ± 2.7 at 10-year follow-up. | Revision rate was 6.12% | ||
| Atlas et al (2005) | 59.5% were satisfied 8- to 10-year after surgery | Bothersome score and frequency score changed from 4.5 at baseline to 2.5 for LBP at 8 to 10 years' follow-up. This change was from 4.8 to 1.6 for leg pain. 52.8% and 66.7% of patients reported improvement at 8 to 10 years after surgery for LBP and leg pain, respectively | Modified Roland scale changed from 15.9 at baseline to 8.7 at 8- to 10-year follow-up | The 10-year reoperation rate was 23% |
Abbreviations: JOA, Japanese Orthopedic Association; LBP, low back pain; ODI, Oswestry Disability Index; VAS, Visual Analog Scale.
Satisfaction
Six of the 12 included studies assessed satisfaction among LSS patients; four had a low risk of bias, 10 12 15 20 whereas two had a high risk of bias. 16 18 Since the method of measuring satisfaction varied in each study, a meta-analysis was not performed. One study measured satisfaction by asking patients whether they were satisfied with the results of laminectomy 5 years after surgery and revealed that 72% were satisfied. 10 In another study, 14% of patients considered the outcome of surgery as excellent, 43% as good, 21.5% as satisfactory, and 21.5% as poor. 15 In another study, 75% of patients were satisfied with the result of surgery at 7- to 10-year follow-up. 12 When comparing surgical and nonsurgical treatments one study measured satisfaction with the following question: “If you were to spend the rest of your life with your back symptoms just the way they are now, how would you feel about that?” 16 and another study asked patients whether they would choose their initial treatment again. 20 Both of these studies showed no significant difference between the surgical and nonsurgical groups 5 to 10 years after the treatment. In contrast, another study reported that the percentage of surgical patients with severe dissatisfaction was significantly higher than that of the nonsurgical patients (77% vs. 52%, p < 0.001). 18
Pain
Six of the 12 studies reported pain as an outcome measure; three of which had a high risk of bias 16 17 19 and the other three were low risk. 10 12 20 All studies showed a significant reduction in pain following surgery. 10 12 16 17 19 20 Two studies did not differentiate leg and back pain; one showed a reduction of 4.53 points in Visual Analog Scale scores after 64 months ( p < 0.001), 10 while another study showed a change from 8.4 points preoperatively to 4.8 points at 6 and 10 years postoperatively 19
Four studies assessed low back pain and leg pain separately. 12 16 17 20 Two of these four studies compared surgical with nonsurgical treatments and after adjusting for baseline patient characteristics, the data suggested that surgery was more effective than nonsurgical treatment in reducing leg and back pain frequency at 5 years of follow-up. 16 Although from 5 to 10 years there was no significant difference in low back pain between groups, leg pain recovered significantly more after surgical intervention in this time period. 16 In another study with 8 to 10 years of follow-up, the frequency and inconvenience of low back pain were not significantly different between the surgical and nonsurgical groups; however, these scores significantly improved for leg pain in patients treated with surgical management. 20 In another study using a graphic rating scale, the mean (±standard deviation) reduction in leg and back pain intensity was 3.6 ± 2.5 points ( p < 0.0001) and 2.2 ± 2.5 points ( p < 0.001), respectively, 2 months following laminectomy 1 ; however, there were no significant changes from the 2-month to the 5-year follow-up. 17 In another study using the Japanese Orthopedic Association score, patients showed a significant improvement in pain from baseline (5.4 ± 2.0 points) to follow-up (10.7 ± 3.2 points). There was minimal change in back pain (1.4 ± 0.7 to 1.9 ± 0.7 points), compared with the greater improvement in leg pain (0.7 ± 0.6 to 2.1 ± 0.7 points). 12
Disability
The modified Roland scale 17 20 and the Oswestry Disability Index (ODI) 19 were used for measurement of disability. Four of the 12 studies assessed disability, three of which had a high risk of bias 16 17 19 and one showed a low risk of bias. 20
In one study, the modified Roland scale change at the 10-year follow-up was 6.8 from a preoperative baseline of 16 ± 4.2. This change was 8.6 immediate postoperatively. 16 In another study with 8 to 10 years of follow-up, patients treated surgically had a significantly greater improvement in the modified Roland disability scale compared with nonsurgically treated patients (improvement in surgical patients: 7.3 ± 6.5, nonsurgical patients: 1.2 ± 7.8, p = 0.02). 20 In another study, by 2 months after the procedure, the decrease in Roland-Morris Scale was 2.7 ± 5.2 points ( p < 0.0001), and by 5 months, there was 2.5 ± 3.6 points further decrease, but the index remained relatively the same up to the 5-year follow-up. 17 Using the ODI scale, up to 6 years of follow-up showed a decrease in scores from 41.2 ± 6.3 preoperatively to 29.3 ± 4.8 postoperatively, which is suggestive of improvement in patients undergoing standard laminectomy. 19 In a study comparing disability among patients undergoing first-time surgery and patients requiring reoperation, by the 5-year follow-up, the improvement in the modified Roland disability scale was significantly less in patients with revision surgery (improvement of 1.8 ± 4.8 points vs. 5.6 ± 6.2 points in those without revision surgery; p = 0.0012). 17
Neurogenic Intermittent Claudication
Three studies assessed neurogenic claudication. These studies were observational, two with a low risk of bias 9 12 and the other with a high risk of bias. 19 All studies showed a significant improvement in patients' walking ability. The maximum walking distance in one study improved from 705.61 ± 1,303.58 m preoperatively to 2,083.3 ± 2,131.6 m at 5 years. 9 In another study, 62.2% of patients were not able to walk more than 100 m without pain, which decreased to 8.1% of patients postoperatively. 12 Another study showed an improvement in pain-free walking distance from 20.1 ± 5.7 m preoperatively to 37.2 ± 3.6 at 6 years and 25.9 ± 2.7 at 10 years; however, the significance of the progress was not reported. 19
Reoperation Rate
The reoperation rate was reported in 10 of the 12 studies, six had a low risk of bias, 9 10 11 13 14 20 and four had a high risk of bias. 16 17 18 19 Meta-analysis revealed a 14% (95% CI: 13–16%, I 2 = 84.20%) reoperation rate among the studies ( Fig. 2 ). The reoperation rate in the subgroup meta-analysis was 16% (95% CI: 8–25%) in studies with a high risk of bias and 14% (95% CI: 12–15%) in studies with a low risk of bias ( Fig. 3 ). When assessing risk factors that may influence the reoperation rate, no correlation was found with sex, obesity, and body mass index. 10 This study also showed that laminectomy with concurrent discectomy had a higher chance of further surgical requirements compared with laminectomy alone. 10
Fig. 2.

Forest plot of reoperation rate after laminectomy. CI, confidence interval.
Fig. 3.
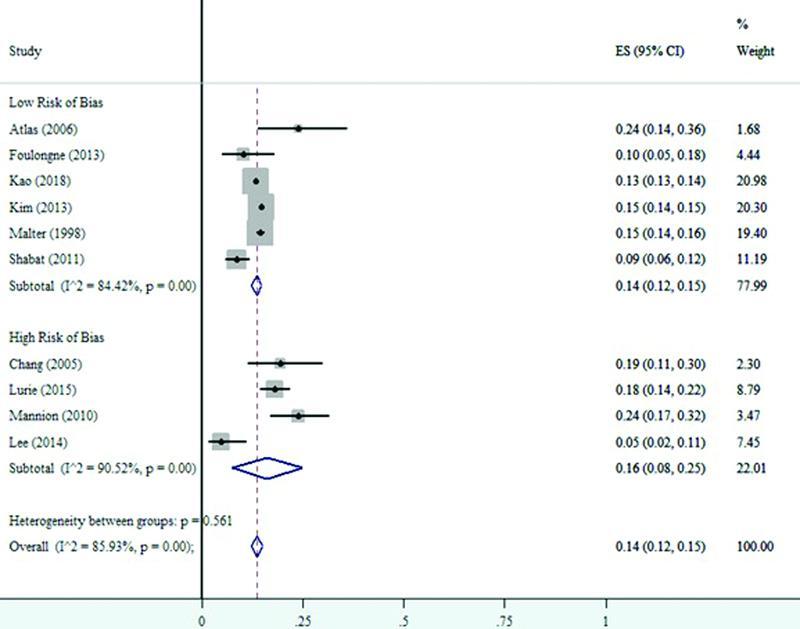
Forest plot of reoperation rate according to quality of studies
Multilevel Laminectomy and Patient Outcomes
The effect of multilevel surgery was explored in two studies, which showed a low risk of bias. 12 15 The improvement of walking distance was found in 33% of patients who underwent three-level surgery, 47% with two-level, and 79% with single-level laminectomy ( p = 0.015). 15 The second study also suggested improved outcomes after single-level laminectomy. 12
Complications and Adverse Events
Complications and adverse events were reported in five studies. 9 11 13 15 18 The most common complications were dural tear (9%) and wound infection (6%) in one study. 15 In another study, four patients needed early revision surgery due to postoperative complications. 9 Malter et al 11 reported the incidence of postoperative complications as 7%. Kim et al reported 33 deaths in the first 90 days after surgery. 13 In another study, four patients (4.1%) had an early complication requiring further surgery (three local infections) 18 ( Table 3 ).
Discussion
Surgery for degenerative lumbar diseases is the most common operation within the spine. Laminectomy and decompression have been commonly utilized for several decades but still, there is a paucity of evidence for the long-term efficacy of laminectomy for LSS. The present study investigates the long-term efficacy and safety of surgery for this condition.
Our review consisted of 83,492 patients with LSS undergoing decompression laminectomy. The results of this study demonstrate that after at least 5 years of follow-up, compared with preoperative baseline patients were more satisfied, 10 12 15 16 18 20 had less pain, both in the leg and low back pain, 10 12 16 17 19 20 were less disabled, 16 17 19 20 could walk further without claudication, 9 12 19 and had a 14% probability of reoperation. 9 10 11 13 14 16 17 18 19 20 Moreover, very low-quality evidence demonstrated that LSS surgery had better outcomes in single-level laminectomy compared with multilevel surgical decompressive laminectomy. 12 15 The overall quality of evidence was low, considering the nonrandomized design of the studies, low patient numbers, and lack of precise results reflected by the wide 95% CIs presented.
Several studies have explored short-term outcomes of laminectomy in LSS. Fritsch et al conducted a systematic review in 2017 to assess pain and disability after laminectomy surgery and demonstrated that patients with spinal stenosis experience substantial reductions in pain and disability in the first 3 months after the surgery but little further improvement is observed afterwards. 21 In 2016, Lurie and Tomkins-Lane suggested that patients who underwent laminectomy reported increased improvement in leg pain compared with the nonsurgical group, which is consistent with the results from this study. 22 In another systematic review from 2016 performed by Zaina et al comparing surgically and nonsurgically treated patients, the authors reported no significant differences at 6-month and 1-year follow-up but there was a significant difference favoring decompression after 24 months. 23 In a study conducted in 2013 by Macedo et al comparing surgery and conservative treatment, the authors reported that surgery was more effective in improving pain and disability; however, changes in claudication were not found to be significantly different between the two groups. 24 In contrast, Mo et al in a study from 2018 comparing the effectiveness of surgery and exercise therapy reported relatively equivocal result in mitigating pain and improving physical activity. 25 The results of this study showed that patients could walk farther after laminectomy, which can be interpreted as an improvement in neurogenic intermittent claudication. Similarly, in a study from 2012, Ammendolia et al compared surgery with conservative treatment and reported improvement of LSS in the surgery group. 26 After meta-analysis, our results demonstrated that with a low level of evidence there is a 14% (95% CI: 13–16%) probability that patients will require reoperation at least 5 years after surgery. In 2018, Goel and Modi reported that comorbid diseases, smoking, and method of surgery might influence the reoperation rate. 27
Patients with a single-level disease are much simpler to treat and have less comorbidity, which might explain why the outcomes appeared to be better in single-level laminectomy in the reviewed studies. In general, standard laminectomy seems to be effective for relieving the symptoms of patients with LSS, but considering that LSS is a progressive degenerative disease and the surgery does not prevent disease progression, the results of surgery are less prominent during the long-term follow-up.
Conclusion
Our review of the available evidence suggests that LSS patients undergoing standard laminectomy may self-report less pain and disability and walk further without claudication on long-term follow-up. Despite the high prevalence of the condition, there is a lack of high-quality evidence for long-term outcomes of surgery. High-quality randomized studies with long-term follow-ups are warranted to ascertain the benefits of laminectomy.
Acknowledgment
None.
Funding Statement
Funding This work was funded by Sina Trauma and Surgery Research Center, Tehran University of Medical Sciences [grant number is 94-03-38-30374]. This systematic review is the thesis of the first author for certification of general practice in medicine under supervision of the corresponding author.
Conflict of Interest The authors declare no conflict of interest except Alexander R. Vaccaro that presented in ( Appendix Table A2 ).
Ethical Approval
The Ethics Committee of Sina Trauma and Surgery Research Center, Tehran University of Medical Sciences, approved the study, and the reference number is IR.TUMS.MEDICINE.REC.1397.875.
Appendix Table A2. Health care entity relationships and investments of Dr Alexander R. Vaccaro.
| Entity | Relationship |
| Replication Medica | d |
| Medtronics | c |
| Stryker Spine | c, |
| Globus | c,d |
| Paradigm Spine | d |
| Stout Medical | d |
| Progressive Spinal Technologies | d |
| Advanced Spinal Intellectual Properties | d |
| Aesculap | c |
| Spine Medica | d |
| Computational Biodynamics | d |
| Spinology | d |
| Flagship Surgical | d |
| Cytonics | d |
| Bonovo Orthopaedics | d |
| Electrocore | d |
| Insight Therapeutics | d |
| FlowPharma | d |
| Rothman Institute and Related Properties | d |
| AO Spine | g |
| Innovative Surgical Design | d |
| Orthobullets | d |
| Thieme | c |
| Jaypee | c |
| Elseviere | c |
| Taylor Francis/Hodder and Stoughton | c |
| Expert testimony | g |
| Vertiflex | d |
| Avaz Surgical | d |
| Dimension Orthotics, LLC | d |
| SpineWave | c |
| Atlas Spine | c |
| Nuvasive | d |
| Parvizi Surgical Innovation | d |
| Franklin Bioscience | d |
| Deep Health | d |
Legend
Consulting/independent contractor
Service on scientific advisory board/board of directors/service on committees
Receipt of royalty payments
Stock/stock option ownership interests
Institutional/educational grant
Deputy editor/editor/editorial board
Member in good standing/independent contractor
References
- 1.Kobayashi S. Pathophysiology, diagnosis and treatment of intermittent claudication in patients with lumbar canal stenosis. World J Orthop. 2014;5(02):134–145. doi: 10.5312/wjo.v5.i2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hobart J, Gilkes C, Adams W, Germon T. Interspinous spacers for lumbar foraminal stenosis: formal trials are justified. Eur Spine J. 2013;22 01:S47–S53. doi: 10.1007/s00586-012-2650-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harrop J S, Hilibrand A, Mihalovich K E, Dettori J R, Chapman J.Cost-effectiveness of surgical treatment for degenerative spondylolisthesis and spinal stenosis Spine 201439(22, Suppl 01)S75–S85. [DOI] [PubMed] [Google Scholar]
- 4.Porter R W, Ward D. Cauda equina dysfunction. The significance of two-level pathology. Spine. 1992;17(01):9–15. [PubMed] [Google Scholar]
- 5.Suri P, Rainville J, Kalichman L, Katz J N. Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis? JAMA. 2010;304(23):2628–2636. doi: 10.1001/jama.2010.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pao J L, Chen W C, Chen P Q. Clinical outcomes of microendoscopic decompressive laminotomy for degenerative lumbar spinal stenosis. Eur Spine J. 2009;18(05):672–678. doi: 10.1007/s00586-009-0903-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atlas S J, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443(443):198–207. doi: 10.1097/01.blo.0000198722.70138.96. [DOI] [PubMed] [Google Scholar]
- 8.Amirdelfan K, McRoberts P, Deer T R. The differential diagnosis of low back pain: a primer on the evolving paradigm. Neuromodulation. 2014;17 02:11–17. doi: 10.1111/ner.12173. [DOI] [PubMed] [Google Scholar]
- 9.Foulongne E, Derrey S, Ould Slimane M. Lumbar spinal stenosis: which predictive factors of favorable functional results after decompressive laminectomy? Neurochirurgie. 2013;59(01):23–29. doi: 10.1016/j.neuchi.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Shabat S, Arinzon Z, Gepstein R, Folman Y. Long-term follow-up of revision decompressive lumbar spinal surgery in elderly patients. J Spinal Disord Tech. 2011;24(03):142–145. doi: 10.1097/BSD.0b013e3181de4b61. [DOI] [PubMed] [Google Scholar]
- 11.Malter A D, McNeney B, Loeser J D, Deyo R A. 5-year reoperation rates after different types of lumbar spine surgery. Spine. 1998;23(07):814–820. doi: 10.1097/00007632-199804010-00015. [DOI] [PubMed] [Google Scholar]
- 12.Iguchi T, Kurihara A, Nakayama J, Sato K, Kurosaka M, Yamasaki K. Minimum 10-year outcome of decompressive laminectomy for degenerative lumbar spinal stenosis. Spine. 2000;25(14):1754–1759. doi: 10.1097/00007632-200007150-00003. [DOI] [PubMed] [Google Scholar]
- 13.Kim C H, Chung C K, Park C S. Reoperation rate after surgery for lumbar spinal stenosis without spondylolisthesis: a nationwide cohort study. Spine J. 2013;13(10):1230–1237. doi: 10.1016/j.spinee.2013.06.069. [DOI] [PubMed] [Google Scholar]
- 14.Kao F C, Hsu Y C, Wang C B, Tu Y K, Liu P H. Short-term and long-term revision rates after lumbar spine discectomy versus laminectomy: a population-based cohort study. BMJ Open. 2018;8(07):e021028. doi: 10.1136/bmjopen-2017-021028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lehto M U, Honkanen P.Factors influencing the outcome of operative treatment for lumbar spinal stenosis Acta Neurochir (Wien) 1995137(1-2):25–28. [DOI] [PubMed] [Google Scholar]
- 16.Chang Y, Singer D E, Wu Y A, Keller R B, Atlas S J. The effect of surgical and nonsurgical treatment on longitudinal outcomes of lumbar spinal stenosis over 10 years. J Am Geriatr Soc. 2005;53(05):785–792. doi: 10.1111/j.1532-5415.2005.53254.x. [DOI] [PubMed] [Google Scholar]
- 17.Mannion A F, Denzler R, Dvorak J, Grob D. Five-year outcome of surgical decompression of the lumbar spine without fusion. Eur Spine J. 2010;19(11):1883–1891. doi: 10.1007/s00586-010-1535-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lurie J D, Tosteson T D, Tosteson A. Long-term outcomes of lumbar spinal stenosis: eight-year results of the Spine Patient Outcomes Research Trial (SPORT) Spine. 2015;40(02):63–76. doi: 10.1097/BRS.0000000000000731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee G W, Jang S J, Shin S M, Jang J H, Kim J D. Clinical and radiological outcomes following microscopic decompression utilizing tubular retractor or conventional microscopic decompression in lumbar spinal stenosis with a minimum of 10-year follow-up. Eur J Orthop Surg Traumatol. 2014;24 01:S145–S151. doi: 10.1007/s00590-013-1287-x. [DOI] [PubMed] [Google Scholar]
- 20.Atlas S J, Keller R B, Wu Y A, Deyo R A, Singer D E. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the Maine Lumbar Spine Study. Spine. 2005;30(08):936–943. doi: 10.1097/01.brs.0000158953.57966.c0. [DOI] [PubMed] [Google Scholar]
- 21.Fritsch C G, Ferreira M L, Maher C G. The clinical course of pain and disability following surgery for spinal stenosis: a systematic review and meta-analysis of cohort studies. Eur Spine J. 2017;26(02):324–335. doi: 10.1007/s00586-016-4668-0. [DOI] [PubMed] [Google Scholar]
- 22.Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016;352:h6234. doi: 10.1136/bmj.h6234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus nonsurgical treatment for lumbar spinal stenosis. Spine. 2016;41(14):E857–E868. doi: 10.1097/BRS.0000000000001635. [DOI] [PubMed] [Google Scholar]
- 24.Macedo L G, Hum A, Kuleba L. Physical therapy interventions for degenerative lumbar spinal stenosis: a systematic review. Phys Ther. 2013;93(12):1646–1660. doi: 10.2522/ptj.20120379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mo Z, Zhang R, Chang M, Tang S. Exercise therapy versus surgery for lumbar spinal stenosis: a systematic review and meta-analysis. Pak J Med Sci. 2018;34(04):879–885. doi: 10.12669/pjms.344.14349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ammendolia C, Stuber K J, Rok E. Nonoperative treatment for lumbar spinal stenosis with neurogenic claudication. Cochrane Database Syst Rev. 2013;(08):CD010712. doi: 10.1002/14651858.CD010712. [DOI] [PubMed] [Google Scholar]
- 27.Goel S A, Modi H N. Reoperations following lumbar spinal canal stenosis. Indian J Orthop. 2018;52(06):578–583. doi: 10.4103/ortho.IJOrtho_380_17. [DOI] [PMC free article] [PubMed] [Google Scholar]


